Abstract
Despite concerns about recent trends in the health and functioning of older Americans, little is known about dynamics of depression among recent cohorts of U.S. older adults and how these dynamics differ across sociodemographic groups. This study examined sociodemographic differences in mid- and late-life depressive symptoms over age, as well as changes over time. Using nationally representative data from the Health and Retirement Study (1994–2014), we estimated mixed effects models to generate depressive symptoms over age by gender, race/ethnicity, education, and birth cohort in 33,280 adults ages 51–90 years. Depressive symptoms were measured using the 8-item Center for Epidemiological Studies Depression scale. Women compared to men, low compared to high education groups, and racial/ethnic minorities compared to whites exhibited higher depressive symptoms. The largest disparity resulted from education, with those without high school degrees exhibiting over two more predicted depressive symptoms in midlife compared to those with college degrees. Importantly, war babies and baby boomers (born 1942–1959) exhibited slightly higher depressive symptoms with more decreasing symptoms over age than their predecessors (born 1931–1941) at ages 51–65. We additionally observed an age-as-leveler pattern by gender, whereby females compared to males had higher depressive symptomology from ages 51–85, but not at ages 86–90. Our findings have implication for gauging the aging population's overall well-being, for public health policies aimed at reducing health disparities, and for anticipating demand on an array of health and social services.
Highlights
-
•
Depressive symptoms in mid- and late-life are higher among socially disadvantaged groups.
-
•
Education levels generated the largest sociodemographic disparity, especially in mid-life.
-
•
Recent birth cohorts had higher symptoms with more declining curves than predecessors ages 51-65.
-
•
Trajectories of depressive symptoms in sociodemographic subgroups converged at higher ages.
-
•
Depressed mood and somatic complaints both rose in late life but men reported lower depressed mood.
1. Introduction
In addition to changes in physical health, aging brings about profound changes in affective functioning (Alexopoulos, 2005). While often preventable and treatable, depression is one of the most common causes of emotional suffering and poor quality of life in the aging population (Sivertsen, Bjørkløf, Engedal, Selbæk, & Helvik, 2015; Volkert, Schulz, Härter, Wlodarczyk, & Andreas, 2013). Depression and depressive symptoms in late life have important implications for the progression of chronic diseases (Chiang et al., 2015; de Groot, Anderson, Freedland, Clouse, & Lustman, 2001; Penninx, 2017), informal care giving needs (Langa, Valenstein, Fendrick, Kabeto, & Vijan, 2004), and healthcare utilization and costs (Luppa, Sikorski, Motzek, et al., 2012). The rate at which depressive symptoms changes during the aging process is an informative indicator of well-being, with increasing symptoms over age predictive of cognitive decline (Mirza et al., 2016) and mortality (Chui, Gerstorf, Hoppmann, & Luszcz, 2015).
Depressive symptoms have long been understood to follow a U-shaped curve over age with a sharp increase beginning around age 65 (Mirowsky & Ross, 1992; Sutin et al., 2013; Tampubolon & Maharani, 2017). Age-related factors like disability, comorbidity, and changes in social support account for the positive association between age and depression in late life (Yang, 2007). Recently, aging researchers have given much attention to alarming trends in physical functioning and mortality among middle- and older-aged American cohorts (Bezruchka, 2012; Martin, Freedman, Schoeni, & Andreski, 2010; Seeman, Merkin, Crimmins, & Karlamangla, 2010). Especially concerning are the widening of disparities in life expectancy and disability-free life years by race and socioeconomic status (Chetty et al., 2016; Freedman & Spillman, 2016; Olshansky et al., 2012). Little is known, however, about the dynamics of depression among recent cohorts of U.S. older adults and particularly differences by gender, race/ethnicity, and educational attainment.
The objective of this analysis was to investigate differences in levels and age-related changes in depressive symptoms by gender, race/ethnicity, education level, and birth cohort among American adults ages 51–90 using recent nationally representative panel data. We sought to describe and visualize subpopulation differences in how depressive symptoms change in mid and late life given the importance of depressive symptom count, even without diagnosis, as an indicator of poor well-being and risk factor for other poor health outcomes.
1.1. Differences by gender
The higher prevalence of depressive symptoms among women compared to men at various stages of the life-course has been well documented in the United States (Alexopoulos, 2005; Kessler et al., 2010; Luppa, Sikorski, Luck, et al., 2012; Mirowsky, 1996). Based on cross-sectional data from the 1980s and 1990s, Mirowsky conducted a component curve analysis to determine differences in men's and women's depressive symptom curves starting at age 18 (Mirowsky, 1996). He found a U-shaped curve with men and women both starting at about 1.4 depressive symptoms at age 18; men's depressive symptoms dropped faster and longer than did women's in ages 20–49, creating a large gender gap in ages 50–69. The gap's growth slowed in older ages, but the disparity remained. Mirowsky conducted mediation tests revealing that gender differences were partially explained by marital status, employment, and other measures of social and economic status that differ by gender at specific ages (Mirowsky, 1996). A more recent evaluation of depression prevalence over the life-course confirmed than women's higher odds of major depressive episodes was especially large at ages sixty-five and older (Kessler et al., 2010), potentially resulting from a cumulative effect of differences in social status throughout the life course compounded by inequities specific to old age, such as women's higher morbidity burden (Cairney & Krause, 2005; Luppa, Sikorski, Luck, et al., 2012; Musliner, Munk-Olsen, Eaton, & Zandi, 2016). A meta-analysis using 24 studies on samples ages 75 and older found the depression prevalence ratio of men to women was 1:1.4–2.2 (Luppa, Sikorski, Luck, et al., 2012).
1.2. Differences by education and race/ethnicity
For decades, there has been evidence that formal educational attainment is inversely related to depressive symptoms in late life (Mirowsky & Ross, 1992). A recent systematic literature review found that low educational attainment was associated with higher depressive symptom burden in all seven of the studies that tested the association in older adults (Musliner et al., 2016). In late life, the relationship between educational attainment and psychological distress has been found to be mediated almost entirely by stress exposure (chronic stress, recent life events, and childhood adversities) and psychosocial resources (mastery and self-esteem) (Cairney & Krause, 2005). Other factors that could link education to late-life depression include cognitive ability, economic resources, social status, social networks, and health behaviors (J. Lee, 2011).
Similarly, social status and psychological stressors are unequally distributed across racial/ethnic groups in the United States (Thoits, 2010; Turner & Avison, 2003). While there is evidence that Black older adults have higher depressive symptoms and psychological distress than whites (Assari, Moazen-Zadeh, Lankarani, & Micol-Foster, 2016; Barnes & Bates, 2017), some studies find that Blacks have lower lifetime prevalence of major depressive episodes (Barnes & Bates, 2017; Mezuk et al., 2013). Showing a similar paradox, Hispanics exhibit a pattern of high depressive symptoms despite low rates of major depression (Breslau et al., 2006; Liang, Xu, Quiñones, Bennett, & Ye, 2011). When considering racial/ethnic differences in how depressive symptoms change with age, Liang et al. (2011) found that, compared to non-Hispanic white Americans, Black and Hispanic Americans were more likely to be in latent trajectories with elevated symptoms and less likely to be in stable (unchanging) trajectories (Liang et al., 2011). Little is known about the age patterns of depression in older adults of numerically small minority populations.
1.3. Current study
This study makes several contributions to our understanding of late-life depressive symptoms across sociodemographic groups. First, we examined recent cohorts of Americans, updating prior analyses. Yang (2007), which used data from 1986 to 1996, found evidence of an age-by-cohort interaction and called for future work with more waves of data, a broader age range, more birth cohorts, and larger datasets to examine non-linear age patterns in different groups (Yang, 2007). Cohorts born after 1940 have worse disability compared to their predecessors (Martin et al., 2010; Seeman et al., 2010), potentially due in part to depression and other emotional problems (Martin, 2014). Examining the dynamics of depressive symptoms in these recent cohorts compared to earlier cohorts provides insight into how affective functioning is changing over time at certain ages.
A second contribution of this paper is special attention to the measurement of depressive symptoms in old age. Some evidence demonstrates that adults ages 65 and older are less likely than young adults to endorse feelings of dysphoria – unease or generalized dissatisfaction (Gallo, Anthony, & Muthen, 1994, pp. P251–P264). There is also concern that gauging somatic depressive symptoms (e.g. changes in appetite or sleep) in older adults might capture physical aspects of aging or disease, rather than specifically measuring affective functioning (Mirowsky, 1996). As sensitivity analyses, we separately examined two aspects of depressive symptoms based on a factor analysis of the CESD-8 – depressed mood and somatic complaints (Wallace et al., 2000). In addition, we compared results of symptom count to those of a high-symptom threshold. These measurement assessments improve the robustness and utility of our findings.
Finally, prior analyses have often relied on latent class models (Diegelmann, Schilling, & Wahl, 2016; Kaup et al., 2016; Liang et al., 2011; Mirza et al., 2016; Musliner et al., 2016). A review of these analyses concluded that female gender, minority race, and low socioeconomic status predict depression trajectories with high and increasing symptoms over the lifecourse (Musliner et al., 2016). However, studies that identify latent trajectories and then associate factors with membership into a trajectory group do not identify the shape of depressive symptom curves over age specifically within men versus women, different racial/ethnic groups, and different educational attainment levels. Our study visualizes changes in average depressive symptoms within these key sociodemographic groups, which can inform policy by highlighting the dynamics of mental health needs in the growingly diverse elderly population.
2. Methods
2.1. Sample
Our data came from the Health and Retirement Study (HRS), an on-going nationally representative longitudinal survey of U.S. men and women aged 51 and older who were not institutionalized at baseline (Sonnega et al., 2014). HRS data collection began in 1992 with individuals born between 1931 and 1941 and their spouses. Several other cohorts have since been added to the sample, and participants are interviewed every two years, even if they enter institutional settings. The study is conducted and distributed by the Institute for Social Research at the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740) (Sonnega et al., 2014). We used the RAND dataset (Version P), which has been cleaned and compiled by Rand Corporation (RAND Center for the Study of Aging, 2016).
Our observation window spanned from Wave 2 (1994)—the first wave with consistent depressive symptom questions—through Wave 12 (2014). We included 199,106 observations from 35,618 individuals who completed interviews between the ages of 51–90 at any time during the 1994–2014 period. After excluding 6,654 observations with zero weights and 14,449 observations with missing data on depressive symptoms or sociodemographic variables, the analytic sample consisted of 178,003 observations from 33,280 individuals. Depressive symptoms were only asked of respondents, and therefore responses given by a proxy were excluded (Wallace et al., 2000).
The six HRS birth cohorts in our study were the Asset and Health Dynamics Among the Oldest Old (AHEAD) born 1890–1923, the Children of the Depression (CODA) born 1924–1930, the original HRS cohort born 1931–1941, the War Babies born 1942–1947, the Early Baby Boomers born 1948–1953, and the Mid Baby Boomers born 1954–1959.
2.2. Measures
Depressive symptoms were measured using the 8-item Center for Epidemiologic Studies Depression scale (CESD-8). Respondents were asked about whether they felt each of the following eight symptoms “much of the week”: felt depressed, everything was an effort, sleep was restless, was happy (reverse coded), felt lonely, felt sad, could not get going, and enjoyed life (reverse coded). The final depressive symptoms score was the number of symptoms that respondents reported feeling much of the week, ranging from zero to eight symptoms. Respondents who did not answer three or more of the eight CESD items were considered missing on the total depressive symptoms score.
The CESD-8 is a commonly-used depressive symptom measure in older adults (Karim, Weisz, Bibi, & ur Rehman, 2015; Lewinsohn, Seeley, Roberts, & Allen, 1997; Turvey, Wallace, & Herzog, 1999). A longer form of the CESD has been validated against diagnostic interviews in adults ages 50 and older and showed internal consistency and test-retest reliability that were acceptable and consistent across gender and age groups (Lewinsohn et al., 1997). In 2015, the 8-item CESD was tested for psychometric properties in a large sample of older adults in Europe, and higher CESD-8 scores were significantly and inversely associated with life satisfaction, happiness, social trust, self-esteem, optimism, subjective health, autonomy, and social relationships (Karim et al., 2015). A psychometric evaluation of the CESD-8 in waves 2 and 3 of HRS identified two factors – depressed mood and somatic complains (Wallace et al., 2000).
To explore whether physical changes with age explain the rise in depressive symptoms after around age 65, we grouped items into two subcategories based on prior psychometric work—“somatic complaints” (everything was an effort, sleep was restless, and could not get going) and “depressed mood” (the remaining five feelings) (Mirowsky, 1996; Wallace et al., 2000). Another measurement concern arises from the fact that the CESD was designed to gauge symptomology, rather than diagnose major depression (Karim et al., 2015). While some have dichotomized this measure at four symptoms to classify high depressive symptoms (Han, 2002; Stevens, Lang, Guralnik, & Melzer, 2008), we examined mean symptom count using the full variation in symptoms to more fully characterize changes in psychological well-being in late life. As a sensitivity analysis, we analyzed the probability of having four to eight symptoms compared to zero to three symptoms.
Our main independent variable was age, which was defined in years and ranged from 51 to 90. We created five-year age intervals—51-55, 56–60, 61–65, 66–70, 71–75, 76–80, 81–85, and 86–90. Using five-year groups allowed age to have a potentially non-linear relationship with depressive symptoms but did not force any certain shape onto the data or give differential influence to higher age values, as would occur with quadratic specifications. Another advantage of this strategy was that when examining potential differential effects of age by cohort, the age effect in each cohort was estimated using only those ages in which each cohort was observed. Mid Baby Boomers, for example, were only observed in their fifties.
Race and ethnicity were self-reported by respondents at baseline and grouped into four categories— non-Hispanic white (henceforth, white), non-Hispanic Black (henceforth, Black), Hispanic, and non-Hispanic other. Education was operationalized as categories based on highest education level attained—less than high school degree, high school degree or General Education Development (GED, certificate equivalent to a high school diploma), some college, and college or more. If a respondent has a high school degree or a GED and another degree less than a bachelor's degree, such as an Associate's Degree, they were considered “some college”. The final sociodemographic variable of interest in this analysis was birth cohort, with six groups defined as noted above.
2.3. Statistical analysis
We used mixed-effects negative binomial models to predict depressive symptoms based on age and sociodemographic covariates. This modeling strategy properly fit the count nature of depressive symptoms, which exhibited over-dispersion in variation, while using a log link to adjust for the skewed distribution of depressive symptoms. Random intercepts accounted for the clustering of observations within respondents (Rabe-Hesketh, Skrondal, & Skrondal, 2008). To adjust for sampling, models were weighted at the observation and respondent level, sampling stratum were included in all models, and standard errors were clustered by unique sampling error computing unit (Heeringa, West, & Berglund, 2017). We exponentiated coefficients into incident rate ratios.
Model 1 predicted depressive symptoms by age groups. In Model 2, we added all sociodemographic variables—gender, race/ethnicity, education, and birth cohort. We then implemented a series of models with age groups, all sociodemographic variables, and an interaction between age groups and one sociodemographic variable, leading to four interaction models (Models 3–6). Postestimation Wald tests evaluated the overall significance of interactions between age groups and sociodemographic variables. We plotted predicted depressive symptoms over age within each sociodemographic subgroup (i.e., men and women), holding other covariates at their mean.
For sensitivity analyses, we ran Model 2 separately predicting depressed mood and somatic complaints. We also ran the gender interaction model with these two outcomes to test whether observed gender differences in depressive symptoms were due to ability or willingness to report certain types of symptoms. Models predicting somatic complaints did not converge and so this sensitivity analysis used unweighted generalized estimating equations with negative binomial families, log links, and exchangeable correlation structures. Finally, we ran all six models using mixed effect logistic regression predicting the binary outcome of four or more symptoms, then generating predicted probabilities of having high depressive symptoms. Analyses were conducted in Stata 15 (StataCorp, 2017) with significance levels set at alpha = 0.05.
3. Results
Table 1 shows the unweighted distribution of sociodemographic characteristics and depressive symptoms at each respondent's first wave of observation. The mean age was 63 years (SD = 9.90) and 56% of the sample was female. Sixty-nine percent of the sample was white, 17% was Black, 11% was Hispanic, and 3% was non-Hispanic other races/ethnicities. The majority of the sample (60%) had a high school degree or less education.
Table 1.
Unweighted characteristics of sample at respondents' entry, Health and Retirement Study 1994–2014, N = 33,280.
| Variable | Ns or means | Percentages or SDs |
|---|---|---|
| Age Groups | ||
| 51-55 | 12,545 | 37.70 |
| 56-60 | 6,648 | 19.98 |
| 61-65 | 2,940 | 8.83 |
| 66-70 | 2,555 | 7.68 |
| 71-75 | 4,650 | 13.97 |
| 76-80 | 2,044 | 6.14 |
| 81-85 | 1,346 | 4.04 |
| 86-90 | 552 | 1.66 |
| Mean Age | 63.07 | 9.90 |
| Gender | ||
| Male | 14,544 | 43.70 |
| Female | 18,736 | 56.30 |
| Race/ethnicity | ||
| NH white | 22,987 | 69.07 |
| NH Black | 5,839 | 17.55 |
| NH other | 871 | 2.62 |
| Hispanic | 2,583 | 10.77 |
| Education | ||
| Less than HS degree | 8,645 | 25.98 |
| HS Grad/GED | 11,167 | 33.55 |
| Some college | 7,253 | 21.79 |
| College + | 6,215 | 18.67 |
| Birth Cohort | ||
| AHEAD (1890–1923) | 6,872 | 20.65 |
| CODA (1924–1930) | 3,764 | 11.31 |
| HRS (1931–1941) | 9,689 | 29.11 |
| War Babies (1942–1947) | 3,467 | 10.42 |
| Early baby boomers (1948–1953) | 4,616 | 13.87 |
| Mid baby boomers (1954–1959) | 4,872 | 14.64 |
| Depressive Symptoms | ||
| 0 | 14,214 | 42.71 |
| 1 | 7,503 | 22.55 |
| 2 | 3,813 | 11.46 |
| 3 | 2,304 | 6.92 |
| 4 | 1,652 | 4.96 |
| 5 | 1,192 | 3.58 |
| 6 | 1,126 | 3.38 |
| 7 | 937 | 2.82 |
| 8 | 539 | 1.62 |
| Dep. Symptoms 4+ | 5,446 | 16.36 |
| Mean Dep. Symptoms | 1.57 | 2.04 |
Note. NH = Non-Hispanic; HS = High School; GED = General Education Development; AHEAD = Asset and Health Dynamics Among the Oldest Old; CODA= Children of the Depression; HRS = original Health and Retirement Study.
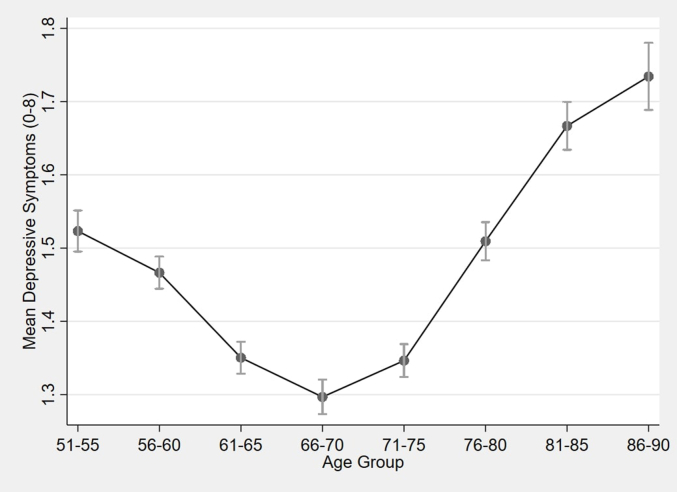
The unweighted baseline distribution of depressive symptoms was right skewed, with 43% of the sample reporting no symptoms and 16% reporting four or more symptoms (high depressive symptoms) (Table 1). The mean depressive symptom count was 1.57 (SD = 2.04) and the median was 1.00 symptom. Supplemental Fig. 1 (Appendix) shows the U-shaped curve of weighted mean depressive symptoms over age. Weighted mean symptoms decreased from 1.52 for those ages 51–55 to the low point of 1.29 at ages 66–70, and then increased through age 90 to a high point of 1.73 symptoms.
The incident rate ratios from the unadjusted and adjusted models can be found in Table 2, with interaction results shown in Supplemental Table 1. In Model 1, the rate of depressive symptoms was statistically significantly different in every age group compared to the reference group 51–55, with the exception of ages 71–75. There were decreasing depressive symptoms in ages 56–70 and increasing symptoms in ages 76–90. When adding the sociodemographic variables in Model 2, there was the same age pattern for rates of changing depressive symptoms, this time with significant decreases in ages 71-75. Women had higher rates of depressive symptoms compared to men, as did minority race/ethnicities compared to non-Hispanic whites, and low levels of education compared to those with at least college degrees. Compared to the AHEAD birth cohort, the HRS cohort had lower rates of depressive symptoms.
Table 2.
Incident Rate Ratios for Increasing Depressive Symptoms, Health and Retirement Study 1994–2014, N = 178,003 depressive symptom observations.
| Dep. Symptoms | Model 1 | Model 2 |
|---|---|---|
| Age Group | ||
| 51-55 | 1.00 | 1.00 |
| 56-60 | 0.971* | 0.968* |
| 61-65 | 0.911*** | 0.905*** |
| 66-70 | 0.904*** | 0.893*** |
| 71-75 | 0.964 | 0.934*** |
| 76-80 | 1.114*** | 1.066** |
| 81-85 | 1.292*** | 1.220*** |
| 86-90 | 1.495*** | 1.396*** |
| Gender | ||
| Male | 1.00 | |
| Female | 1.272*** | |
| Race/Ethnicity | ||
| NH White | 1.00 | |
| NH Black | 1.349*** | |
| NH Other | 1.432*** | |
| Hispanic | 1.267*** | |
| Education | ||
| <HS | 2.546*** | |
| GED/HS Grad | 1.762*** | |
| Some College | 1.428*** | |
| College+ | 1.00 | |
| Birth Cohort | ||
| AHEAD (1890–1923) | 1.00 | |
| CODA (1924–1930) | 1.037 | |
| HRS (1931–1941) | 0.929** | |
| War Babies (1942–1947) | 1.010 | |
| Early baby boomers (1948–1953) | 1.068 | |
| Mid baby boomers (1954–1959) | 1.077 | |
| var(cons[ID]) | 3.459*** | 2.984*** |
Note. NH = Non-Hispanic; HS = High School; GED = General Education Development; AHEAD = Asset and Health Dynamics Among the Oldest Old; CODA= Children of the Depression; HRS = original Health and Retirement Study; var(cons[ID]) = Variance component corresponding to the random intercept; Interaction Models 3–6 in Supplemental Table 1; * = p < 0.05, ** = p < 0.01, *** = p < 0.001.
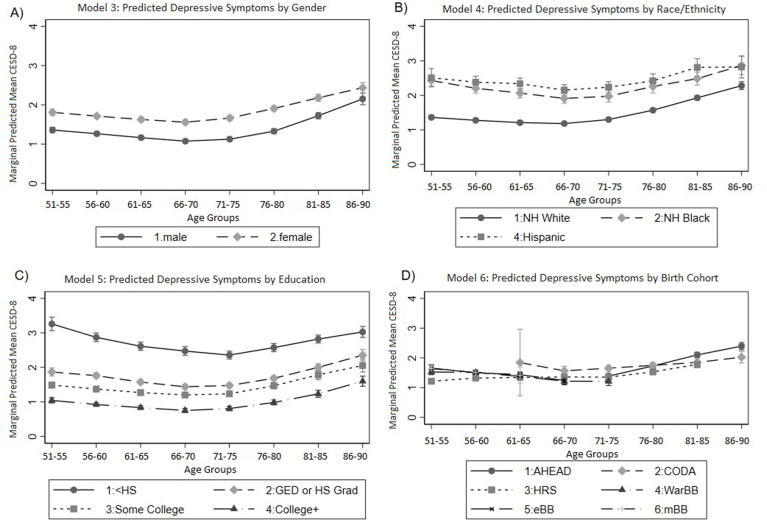
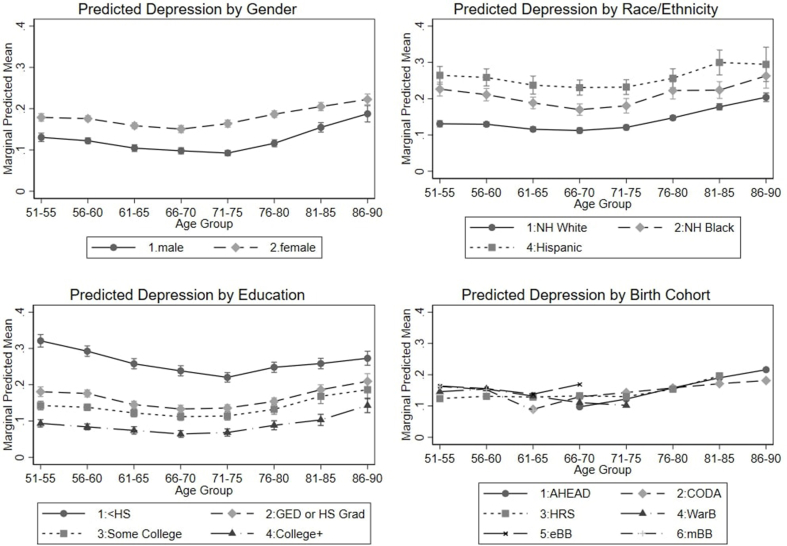
The differences in age group effects by sociodemographic variables (Models 3–6) are depicted in Fig. 1 as predicted depressive symptoms with all other covariates held at mean. Postestimation Wald tests revealed that interactions of age groups with each sociodemographic characteristic were statistically significant at the p < 0.0001 level (Supplemental Table 1). While many interactions between specific age groups and specific sociodemographic sub-groups were not significant, those that reached statistical significance were generally at the oldest ages, resulting in converging group differences at the oldest ages. For example, women had consistently higher depressive symptoms through age 85, but men's symptoms increased faster over ages 81–90, leading to no significant gender difference at ages 86–90 (Fig. 1a).
Fig. 1.
Adjusted Predicted Depressive Symptoms from Interactions between Age Group and Gender, Race/Ethnicity, Education, and Birth Cohort, Health and Retirement Study 1994–2014, N = 178,003 depressive symptom observations. Note. NH = Non-Hispanic; HS = High School; GED = General Education Development; AHEAD = Asset and Health Dynamics Among the Oldest Old; CODA= Children of the Depression; HRS = original Health and Retirement Study; WarB = War Babies; eBB = Early Baby Boomers; mBB = Mid Baby Boomers.
As seen in Fig. 1b, predicted symptoms by race/ethnicity show that Hispanic older adults had the highest depressive symptoms, followed by Blacks, with whites having the lowest symptoms. Mean depressive symptoms for non-Hispanics of other races/ethnicities fell between Blacks and whites, but with wide confidence intervals that made the shape of the curve uninterpretable. At ages 56–60, there were no significant interactions between age and race/ethnicity. At ages 61–75, non-Hispanic Black respondents had decreasing slopes relative to whites, while Hispanics showed no significant interactions. At ages 76–90, depressive symptoms in whites rose faster than in Blacks and Hispanics, resulting in the narrowing of Black-white and Hispanic-white disparities.
Education differences in depressive symptoms followed a clear inverse pattern, with the lowest education group showing the highest depressive symptoms throughout the age range and the highest education group showing the lowest symptoms throughout (Fig. 1c). Older adults with less than high school degree had substantially higher depressive symptoms than those with a high school degree or GED, whose levels were more closely aligned with the two higher education levels. In ages 51–55, the lowest education group had a mean predicted depressive score over two symptoms higher than the highest education group. While these lines were mostly parallel, the gap was reduced by about one-third in ages 86–90.
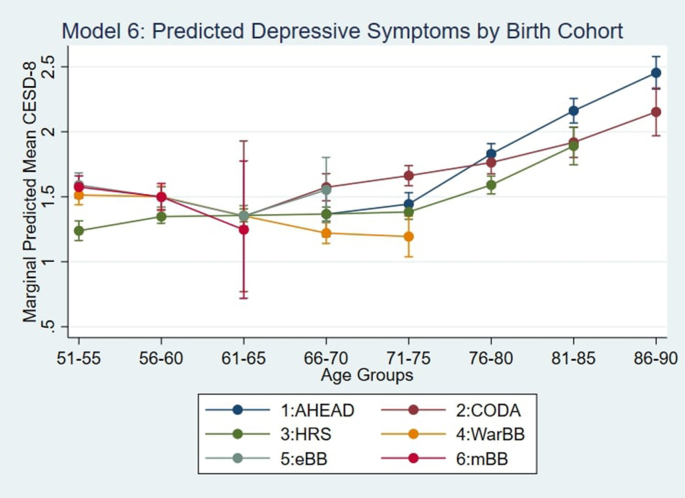
Fig. 1d shows age-related changes in the number of depressive symptoms by birth cohort. We predicted the number of symptoms only at the ages at which each cohort was observed in the data. The original HRS cohort (born 1931–1941) was observed over the widest age range (51–55 to 81–85). For this cohort, the predicted number of depressive symptoms increased throughout the age range. However, there was a faster growth in the number of symptoms at ages 71–85 than at ages 51–70. AHEAD, the earliest cohort (born 1890–1923 and observed from ages 66–70 to 86–90), showed a monotonic increase in the number of depressive symptoms over the observed ages. CODA (born 1924–1930 and observed from ages 61–65 to 68–90) also showed a monotonically increasing pattern over age. The three most recent birth cohorts— War Babies (born 1942–1947), Early Baby Boomers (born 1948–1953), and Mid Baby Boomers (born 1954–1959) displayed mostly decreasing depressive symptoms over age, with the exception of Early Baby Boomers at ages 66-70.
A test of the age group by cohort interactions in midlife (ages 51–65) showed significant differences in the age pattern of depressive symptoms by cohort (chi-squared (7) = 43.87, p < 0.001). More recent cohorts displayed decreasing symptoms over ages 51-65, while the original HRS cohort exhibited increasing symptoms. In addition, at ages 51–55, the original HRS cohort had significantly lower predicted depressive symptoms (1.24, 95% CI = 1.16, 1.31) compared to more recent cohorts of War Babies (1.51, 95% CI = 1.44, 1.59), Early Baby Boomers (1.59, 95% CI = 1.50, 1.68) and Mid Baby Boomers (1.58, 95% CI = 1.48, 1.66). Though substantively small, this difference remained significant through ages 55–59. The age-cohort interaction (Fig. 1D) is shown in more detail in Supplemental Fig. 2.
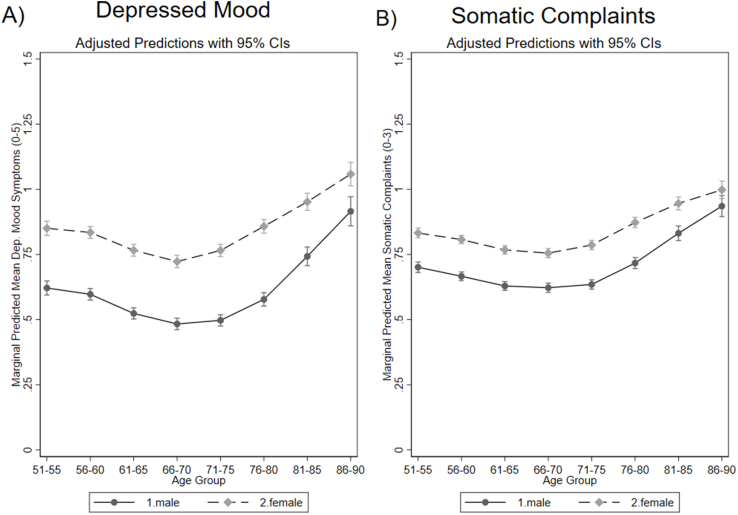
Results from the sensitivity analyses are shown in Fig. 2 and Supplemental Fig. 3 (Appendix). The separate outcomes of depressed mood and somatic complaints showed similar U-shaped patterns, both rising at older ages to reach a mean around 1 by ages 86–90. Depressed mood fell a bit lower than somatic complaints at the minimum at ages 66–70. Interactions with gender showed that the gender gap was wider in symptoms of depressed mood compared to somatic complaints. Women's scores did not differ between the two outcomes, but men reported fewer symptoms of depressed mood than somatic complaints, especially in their sixties and seventies.
Fig. 2.
Adjusted Predicted Symptoms of Depressed Mood and Somatic Complaints from Generalized Estimating Equations over Age Groups by Gender, Health and Retirement Study 1994–2014. Note. While the sadness models has all 178,003 observations, the malaise model has 177,444 observations due to item level missingness (295 missing on “could not get going”, 187 missing on “everything was an effort”, and 100 missing on “sleep was restless”, with 23 missing on more than one of these items).
Looking at the probability of having 4–8 symptoms (Supplemental Fig. 3), all four interactions looked similar to the analysis of continuous symptom count. For example, those with less than high school educations had a 0.3 probability of high symptoms compared to 0.1 for those with college educations, rather than 3 and 1 predicted symptoms respectively. When looking at probability of high depressive symptoms, women's curves hit a low point at ages 66–70 and then started increasing, whereas men's lowest probability of high depressive symptoms was at ages 71–75. In addition, these models reveal statistically significant differences between Hispanics and Blacks at ages 56–75.
4. Discussion
Overall, our analysis revealed that gender, race/ethnicity, education, and birth cohort were associated with different levels of depressive symptoms in mid and late life and different rates of age-related changes. One key finding is that among the sociodemographic characteristics evaluated, differences in educational attainment produced the largest disparities in depressive symptomology. In addition, our results reveal that recent birth cohorts are experiencing slightly higher levels of depressive symptoms in midlife compared to earlier cohorts. Differences in depressive symptoms shrank in the oldest ages, especially by gender. This pattern supports the “age as leveler” hypothesis that posits that group differences converge in old age because universal health declines from aging overwhelm the disadvantage of low social status (Angel, Mudrazija, & Benson, 2016).
Women had higher depressive symptoms, but men's symptoms rose faster in the oldest ages, shrinking the gender gap. Sensitivity analyses showed that the gender gap is larger when looking only at feelings of depressed mood rather than somatic complaints, suggesting that gender differences may be partially due to men's ability or willingness to report feelings of depressed mood relative to somatic complaints. In both cases, the gender gap is smallest in the oldest age group. This result contrasts Mirowsky's finding that the gender gap increased with age (Mirowsky, 1996). While Mirowsky relied on cross-sectional data, this longitudinal analysis modeled gender differences in age-based changes in depressive symptoms in actual birth cohorts as they age. In addition, our analysis included more recent data.
Differences in depressive symptoms by race/ethnicity and by education level were also smallest in ages 86–90. Finding higher depressive symptoms in Black older adults than whites is consistent with prior work (Assari et al., 2016), but contrasts findings that whites have higher rates of diagnosable major depression disorder (Breslau et al., 2006; Mezuk et al., 2013). This discrepancy could be due to racial/ethnic differences in resilience (Keyes, 2009), problems with measuring depressive symptoms (Perreira & Harris, 2005), or systematic bias in the diagnostic algorithm (Barnes & Bates, 2017). Hispanics also exhibit a pattern of high depressive symptoms, as seen in our results and some prior work (Liang et al., 2011), despite lower rates depression disorder (Breslau et al., 2006). High depressive symptoms in Hispanics supports the idea that lower mortality in this population is not necessarily accompanied by lower levels of disability (Melvin, Hummer, Elo, & Mehta, 2014). Given that Hispanic older adults are a rapidly growing population, it is important to understand patterns and causes of late-life depression in this group. Future work should collect data that enables testing differences by nativity and country of origin.
Of all sociodemographic comparisons, the most disadvantaged group in this study was those with less than a high school education, who averaged two depressive symptoms higher at ages 51–55 than those with a college degree or more. In addition, educational differences remained into ages 86–90. Using the U.S. National Health Interview Survey, Case and Deaton (2017) reported an increase in mental distress in midlife between birth cohorts born from 1940 to 1988, specifically for non-Hispanic whites without a bachelor's degree (Case & Deaton, 2017). Our findings echo concerns about the health, and especially mental well-being, of the low educated adult population in the U.S. (Case & Deaton, 2017; Goldman, Glei, & Weinstein, 2018). As educational attainment has increased over time, those without a high school degree have experienced deteriorating health relative to other groups (Olshansky et al., 2012). While the lowest education group is becoming a more select population (Dowd & Hamoudi, 2014), compositional changes appear to only account for part of the growing mortality disadvantage among those without high school degrees compared to others (Hendi, 2015).
Looking to cohorts, our results indicate that recent birth cohorts had slightly higher depressive symptoms in their fifties than did their predecessors, but with more decreasing rather than increasing slopes. This finding suggests a small increase in depressive symptomology over time in midlife, with a shift in the low-point of the depressive symptom curve occurring at higher ages. Our findings suggest previously reported trends in increasing mid-life despair may hold in the overall population, not just for whites of low education. Future work can employ a life-course perspective to test explanations of cohort differences in mid- and late-life depression, such as differential education quality in childhood, increased educational attainment over time, access to antidepressants, and experiences retiring in strong and weak economies.
Our findings of little-to-no cohort difference in symptom increases at older ages contrast those reported by Tampubolon and Maharani (2017), who used HRS to find that post-war birth cohorts (born in 1946 or later) experienced inversed u-shaped curves over age (Tampubolon & Maharani, 2017). As suggested by Blazer (2017), the trajectory reported by Tampubolon and Maharani may be an artifact of using a quadratic specification for age when cohorts have different observed age ranges (Blazer, 2017). Our results, in contrast, were based on discrete age-categories that did not force any parametric shape on the age curves. In addition, while the Tampubolon and Maharani study was restricted to white respondents, our analysis included all race/ethnic groups.
These results should be considered in light of the study's limitations. Our data cannot distinguish between the force of age leveling out sociodemographic differences versus the effects of selective mortality. Higher mortality at younger ages in disadvantaged groups may result in converging population trajectories because respondents with high symptoms in these groups are not observed in older ages (Dupre, 2007). Another limitation is that the CESD does not measure diagnoses, and thus our results do not translate to depression prevalence. In addition, HRS data did not allow for comparisons of birth cohorts across the full age range, as the entry age differed between cohorts and some have not yet reached the highest ages of interest. The AHEAD cohort was recruited at age 70, and so HRS criteria of being non-institutionalized at baseline likely resulted in a more selective AHEAD sample than other cohorts that fulfilled this criterion at age 50 or 60. Further, our statistical approach modeled average depressive symptoms within subgroups and did not examine within-group heterogeneity. However, characterizing age-related changes in depressive symptoms in sociodemographic subgroups is important to understanding population dynamics in mental health, with implications for caregiving needs, healthcare utilization, disability, and disease outcomes.
A strength of this study was the sensitivity analyses, which considered the effect of how depressive symptoms are measured and operationalized. The first analysis demonstrated that increases in depressive symptoms at older ages is not primarily driven by somatic complaints. In addition, dropping individual CESD-8 items due to concern that they misrepresent depression in old age will affect the size of the gender gap in depressive symptoms. While depressive symptomology is useful for characterizing the mental well-being of populations, diagnosis is important to accessing mental health services. Our second sensitivity using a dichotomized variable for high depressive showed overall similar U-shaped patterns over age. However, important changes over age likely occur within the categories of low and high depressive symptoms, making symptom count a more informative outcome. It would be useful for future work to directly compare depressive symptomology and major depressive diagnosis over age in sociodemographic subgroups of older adults.
Besides providing insights into recent patterns of population health, our findings have important policy implications. Population trends in depressive symptoms can help predict demand for mental health services, which is especially important given shortages in geriatricians and geriatric psychiatrists ( Lee & Sumaya, 2013). Elevated depressive symptoms are associated with incident and exacerbated disability (Bruce, 2001) and falls (Hoffman, Hays, Wallace, Shapiro, & Ettner, 2017), so depressive symptoms may drive social security disability applications (Bilder & Mechanic, 2003), demands on caregivers (Langa et al., 2004), and healthcare utilization and cost (Luppa, Sikorski, Luck, et al., 2012). In addition, depressive symptoms relate to health outcomes and service utilization via poor disease management, such as lower adherence to medication (Hennein et al., 2018), dietary, and exercise regimens (Ciechanowski, Katon, Russo, & Hirsch, 2003; Gonzalez et al., 2008). Differences in depressive symptoms between subpopulations indicate that these consequences are disproportionately faced by those with low education and by racial/ethnic minorities—priority populations for designing and targeting prevention and treatment programs. In addition, the observed impact of educational attainment points to the importance of interventions earlier in life. Further research in this area can improve current understanding of the mechanisms that link low social status with late-life depression.
4.1. Conclusions
This study depicted changes in depressive symptoms in mid and late life by major sociodemographic groups in the United States. Education level was the largest disparity and more recent birth cohorts exhibited higher depressive symptoms in midlife. As the population ages and the older population becomes increasingly diverse, understanding trends and disparities in depression is essential to ensuring the well-being of older adults.
Conflicts of interest
None.
Funding
This work was supported by a T32 Training Grant from the National Institute on Aging at the National Institutes of Health (Grant Number: 2T32AG027708-06A1).
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100399.
Contributor Information
Leah R. Abrams, Email: Lrabrams@umich.edu.
Neil K. Mehta, Email: Nkmehta@umich.edu.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
figs1.
figs2.
figs3.
References
- Alexopoulos G.S. Depression in the elderly. The Lancet. 2005;365(9475):1961–1970. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- Angel J., Mudrazija S., Benson R. Chapter 6 - racial and ethnic inequalities in health. In: Ferraro K., George L., editors. Handbook of aging and the social sciences. 8th ed. 2016. p. 531. [Google Scholar]
- Assari S., Moazen-Zadeh E., Lankarani M.M., Micol-Foster V. Race, depressive symptoms, and all-cause mortality in the United States. Frontiers in Public Health. 2016;4:40. doi: 10.3389/fpubh.2016.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes D.M., Bates L.M. Do racial patterns in psychological distress shed light on the black–white depression paradox? A systematic review. Social Psychiatry and Psychiatric Epidemiology. 2017;52(8):913–928. doi: 10.1007/s00127-017-1394-9. [DOI] [PubMed] [Google Scholar]
- Bezruchka S. The hurrider I go the behinder I get: The deteriorating international ranking of U.S. Health status. Annual Review of Public Health. 2012;33(1):157–173. doi: 10.1146/annurev-publhealth-031811-124649. [DOI] [PubMed] [Google Scholar]
- Bilder S., Mechanic D. Navigating the disability process: Persons with mental disorders applying for and receiving disability benefits. The Milbank Quarterly. 2003;81(1):75–106. doi: 10.1111/1468-0009.00039. table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer D. Do we ever outlive depression? American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry. 2017;25(11):1196–1197. doi: 10.1016/j.jagp.2017.07.011. [DOI] [PubMed] [Google Scholar]
- Breslau J., Aguilar-Gaxiola S., Kendler K.S., Su M., Williams D., Kessler R.C. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2006;36(1):57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce M.L. Depression and disability in late life: Directions for future research. American Journal of Geriatric Psychiatry. 2001;9(2):102–112. doi: 10.1097/00019442-200105000-00003. [DOI] [PubMed] [Google Scholar]
- Cairney J., Krause N. The social distribution of psychological distress and depression in older adults. Journal of Aging and Health. 2005;17(6):807–835. doi: 10.1177/0898264305280985. [DOI] [PubMed] [Google Scholar]
- Case A., Deaton A. Mortality and morbidity in the 21st century. Brookings Papers on Economic Activity. 2017:397–476. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty R., Stepner M., Abraham S., Lin S., Scuderi B., Turner N. The association between income and life expectancy in the United States, 2001-2014. Journal of the American Medical Association. 2016;315(16):1750. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang H.-H., Guo H.-R., Livneh H., Lu M.-C., Yen M.-L., Tsai T.-Y. Increased risk of progression to dialysis or death in CKD patients with depressive symptoms: A prospective 3-year follow-up cohort study. Journal of Psychosomatic Research. 2015;79(3):228–232. doi: 10.1016/J.JPSYCHORES.2015.01.009. [DOI] [PubMed] [Google Scholar]
- Chui H., Gerstorf D., Hoppmann C.A., Luszcz M.A. Trajectories of depressive symptoms in old age: Integrating age-, pathology-, and mortality-related changes. Psychology and Aging. 2015;30(4):940–951. doi: 10.1037/pag0000054. [DOI] [PubMed] [Google Scholar]
- Ciechanowski P.S., Katon W.J., Russo J.E., Hirsch I.B. The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. General Hospital Psychiatry. 2003;25(4):246–252. doi: 10.1016/s0163-8343(03)00055-0. [DOI] [PubMed] [Google Scholar]
- Diegelmann M., Schilling O.K., Wahl H.-W. Feeling blue at the end of life: Trajectories of depressive symptoms from a distance-to-death perspective. Psychology and Aging. 2016;31(7):672–686. doi: 10.1037/pag0000114. [DOI] [PubMed] [Google Scholar]
- Dowd J.B., Hamoudi A. Is life expectancy really falling for groups of low socio-economic status? Lagged selection bias and artefactual trends in mortality. International Journal of Epidemiology. 2014;43(4):983–988. doi: 10.1093/ije/dyu120. [DOI] [PubMed] [Google Scholar]
- Dupre M.E. Educational differences in age-related patterns of disease an empirical test of cumulative disadvantage theory. Journal of Health and Social Behavior. 2007;48(March):1–15. doi: 10.1177/002214650704800101. https://search-proquest-com.ezp-prod1.hul.harvard.edu/pqdtglobal/docview/304994864/fulltextPDF/A58CE5D01CC44135PQ/15?accountid=11311 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Freedman V.A., Spillman B.C. Active life expectancy in the older US population, 1982-2011: Differences between blacks and whites persisted. Health Affairs (Project Hope) 2016;35(8):1351–1358. doi: 10.1377/hlthaff.2015.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo J.J., Anthony J.C., Muthen B.O. Age differences in the symptoms of depression: A latent trait analysis. Journal of Gerontology. 1994;49(6):P251–P264. doi: 10.1093/geronj/49.6.p251. http://www.ncbi.nlm.nih.gov/pubmed/7963280 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Goldman N., Glei D.A., Weinstein M. Declining mental health among disadvantaged Americans. Proceedings of the National Academy of Sciences of the United States of America. 2018;115(28):7290–7295. doi: 10.1073/pnas.1722023115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez J.S., Safren S.A., Delahanty L.M., Cagliero E., Wexler D.J., Meigs J.B. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabetic Medicine: A Journal of the British Diabetic Association. 2008;25(9):1102–1107. doi: 10.1111/j.1464-5491.2008.02535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Groot M., Anderson R., Freedland K.E., Clouse R.E., Lustman P.J. Association of depression and diabetes complications: A meta-analysis. Psychosomatic Medicine. 2001;63(4):619–630. doi: 10.1097/00006842-200107000-00015. http://www.ncbi.nlm.nih.gov/pubmed/11485116 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Han B. Depressive symptoms and self-rated health in community-dwelling older adults: A longitudinal study. Journal of the American Geriatrics Society. 2002;50(9):1549–1556. doi: 10.1046/j.1532-5415.2002.50411.x. [DOI] [PubMed] [Google Scholar]
- Heeringa S.G., West B.T., Berglund P.A. Applied survey data analysis. CRC Press; Boca Raton, FL: 2017. Analysis of longitudinal complex sample survey data; pp. 371–426. [Google Scholar]
- Hendi A.S. Trends in U.S. Life expectancy gradients: The role of changing educational composition. International Journal of Epidemiology. 2015;44(3):946–955. doi: 10.1093/ije/dyv062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennein R., Hwang S.-J., Au R., Levy D., Muntner P., Fox C.S. Barriers to medication adherence and links to cardiovascular disease risk factor control: The framingham heart study. Internal Medicine Journal. 2018;48(4):414–421. doi: 10.1111/imj.13687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman G.J., Hays R.D., Wallace S.P., Shapiro M.F., Ettner S.L. Depressive symptomatology and fall risk among community-dwelling older adults. Social Science & Medicine. 2017;178:206–213. doi: 10.1016/J.SOCSCIMED.2017.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim J., Weisz R., Bibi Z., ur Rehman S. Validation of the eight-item center for epidemiologic studies depression scale (CES-D) among older adults. Current Psychology. 2015;34(4):681–692. doi: 10.1007/s12144-014-9281-y. [DOI] [Google Scholar]
- Kaup A.R., Byers A.L., Falvey C., Simonsick E.M., Satterfield S., Ayonayon H.N. Trajectories of depressive symptoms in older adults and risk of dementia. JAMA Psychiatry. 2016;73(5):525. doi: 10.1001/jamapsychiatry.2016.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Birnbaum H., Bromet E., Hwang I., Sampson N., Shahly V. Age differences in major depression: Results from the national comorbidity survey replication (NCS-r) Psychological Medicine. 2010;40(02):225. doi: 10.1017/S0033291709990213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes C.L.M. The black-white paradox in health: Flourishing in the face of social inequality and discrimination. Journal of Personality. 2009;77(6):1677–1706. doi: 10.1111/j.1467-6494.2009.00597.x. [DOI] [PubMed] [Google Scholar]
- Langa K.M., Valenstein M.A., Fendrick A.M., Kabeto M.U., Vijan S. Extent and cost of informal caregiving for older Americans with symptoms of depression. American Journal of Psychiatry. 2004;161(5):857–863. doi: 10.1176/appi.ajp.161.5.857. [DOI] [PubMed] [Google Scholar]
- Lee J. Pathways from education to depression. Journal of Cross-Cultural Gerontology. 2011;26(2):121–135. doi: 10.1007/s10823-011-9142-1. [DOI] [PubMed] [Google Scholar]
- Lee W.-C., Sumaya C.V. Geriatric workforce capacity: A pending crisis for nursing home residents. Frontiers in Public Health. 2013;1:24. doi: 10.3389/fpubh.2013.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn P.M., Seeley J.R., Roberts R.E., Allen N.B. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging. 1997;12(2):277–287. doi: 10.1037/0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- Liang J., Xu X., Quiñones A.R., Bennett J.M., Ye W. Multiple trajectories of depressive symptoms in middle and late life: Racial/ethnic variations. Psychology and Aging. 2011;26(4):761–777. doi: 10.1037/a0023945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luppa M., Sikorski C., Luck T., Ehreke L., Konnopka A., Wiese B. Age- and gender-specific prevalence of depression in latest-life - systematic review and meta-analysis. Journal of Affective Disorders. 2012;136(3):212–221. doi: 10.1016/j.jad.2010.11.033. [DOI] [PubMed] [Google Scholar]
- Luppa M., Sikorski C., Motzek T., Konnopka A., König H.-H., Riedel-Heller S.G. Health service utilization and costs of depressive symptoms in late life - a systematic review. Current Pharmaceutical Design. 2012;18(36):5936–5957. doi: 10.2174/138161212803523572. http://www.ncbi.nlm.nih.gov/pubmed/22681171 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Martin L.G. Trends in disability and related chronic conditions among the forty-and-over population: 1997–2010. Disability and Health Journal. 2014;7(1):S4–S14. doi: 10.1016/J.DHJO.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin L.G., Freedman V.A., Schoeni R.F., Andreski P.M. Trends in disability and related chronic conditions among people ages fifty to sixty-four. Health Affairs. 2010;29(4) doi: 10.1377/hlthaff.2008.0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melvin J., Hummer R., Elo I., Mehta N. Age patterns of racial/ethnic/nativity differences in disability and physical functioning in the United States. Demographic Research. 2014;31:497–510. doi: 10.4054/DemRes.2014.31.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B., Abdou C.M., Hudson D., Kershaw K.N., Jane A., Lee H. “White box” epidemiology and the social neuroscience of health behaviors: The environmental affordances model. Society and Mental Health. 2013;3(2):1–22. doi: 10.1177/2156869313480892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirowsky J. Age and the gender gap in depression. Journal of Health and Social Behavior. 1996;37(4):362. doi: 10.2307/2137263. [DOI] [PubMed] [Google Scholar]
- Mirowsky J., Ross C.E. Age and depression. Source Journal of Health and Social Behavior. 1992;33(3):187–205. http://www.jstor.org/stable/2137349 Retrieved from. [PubMed] [Google Scholar]
- Mirza S.S., Wolters F.J., Swanson S.A., Koudstaal P.J., Hofman A., Tiemeier H. 10-year trajectories of depressive symptoms and risk of dementia: A population-based study. The Lancet Psychiatry. 2016;3(7):628–635. doi: 10.1016/S2215-0366(16)00097-3. [DOI] [PubMed] [Google Scholar]
- Musliner K.L., Munk-Olsen T., Eaton W.W., Zandi P.P. Heterogeneity in long-term trajectories of depressive symptoms: Patterns, predictors and outcomes. Journal of Affective Disorders. 2016;192:199–211. doi: 10.1016/j.jad.2015.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olshansky J., Antonucci T., Berkman L., Binstock R., Boersch-Supan A., Cacioppo J. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Affairs. 2012;31(8) doi: 10.1377/hlthaff.2011.0746. [DOI] [PubMed] [Google Scholar]
- Penninx B.W.J.H. Depression and cardiovascular disease: Epidemiological evidence on their linking mechanisms. Neuroscience & Biobehavioral Reviews. 2017;74:277–286. doi: 10.1016/J.NEUBIOREV.2016.07.003. [DOI] [PubMed] [Google Scholar]
- Perreira K.M., Harris K.M. 2005. What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation.https://academic.oup.com/sf/article-abstract/83/4/1567/2234830 Retrieved from. [Google Scholar]
- Rabe-Hesketh S., Skrondal A., Skrondal A. Stata Press Publication; 2008. Multilevel and longitudinal modeling using stata. [Google Scholar]
- RAND Center for the Study of Aging, with funding from the N. I. on A. and the S. S. A. 2016. RAND HRS data, Version P, Santa Monica, CA. [Google Scholar]
- Seeman T.E., Merkin S.S., Crimmins E.M., Karlamangla A.S. Disability trends among older Americans: National health and nutrition examination surveys, 1988-1994 and 1999-2004. American Journal of Public Health. 2010;100(1):100–107. doi: 10.2105/AJPH.2008.157388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivertsen H., Bjørkløf G.H., Engedal K., Selbæk G., Helvik A.-S. Depression and quality of life in older persons: A review. Dementia and Geriatric Cognitive Disorders. 2015;40(5–6):311–339. doi: 10.1159/000437299. [DOI] [PubMed] [Google Scholar]
- Sonnega A., Faul J.D., Ofstedal M.B., Langa K.M., Phillips J.W., Weir D.R. Cohort profile: The health and retirement study (HRS) International Journal of Epidemiology. 2014;43(2):576–585. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . StataCorp LLC; College Station, TX: 2017. Stata statistical software: Release 15. [Google Scholar]
- Stevens K.N., Lang I.A., Guralnik J.M., Melzer D. Epidemiology of balance and dizziness in a national population: Findings from the English longitudinal study of ageing. Age and Ageing. 2008;37(3):300–305. doi: 10.1093/ageing/afn019. [DOI] [PubMed] [Google Scholar]
- Sutin A.R., Terracciano A., Milaneschi Y., An Y., Ferrucci L., Zonderman A.B. The trajectory of depressive symptoms across the adult life span. JAMA Psychiatry. 2013;70(8):803–811. doi: 10.1001/jamapsychiatry.2013.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tampubolon G., Maharani A. When did old age stop being depressing? Depression trajectories of older Americans and britons 2002–2012. American Journal of Geriatric Psychiatry. 2017;25(11):1187–1195. doi: 10.1016/j.jagp.2017.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits P.A. Stress and health: Major findings and policy implications. Journal of Health and Social Behavior. 2010;51(1_suppl):S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Turner R.J., Avison W.R. Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior. 2003;44(4):488–505. [PubMed] [Google Scholar]
- Turvey C.L., Wallace R.B., Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics. 1999;11(2):139–148. doi: 10.1017/s1041610299005694. http://www.ncbi.nlm.nih.gov/pubmed/11475428 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Volkert J., Schulz H., Härter M., Wlodarczyk O., Andreas S. The prevalence of mental disorders in older people in Western countries – a meta-analysis. Ageing Research Reviews. 2013;12(1):339–353. doi: 10.1016/J.ARR.2012.09.004. [DOI] [PubMed] [Google Scholar]
- Wallace R.B., Regula A., Mary H., Ofstedal B., Steffick D., Fonda S. 2000. HRS/AHEAD documentation report documentation of affective functioning measures in the health and retirement study.http://hrsonline.isr.umich.edu/sitedocs/userg/dr-005.pdf Retrieved from. [Google Scholar]
- Yang Y. Is old age depressing? Growth trajectories and cohort variations in late-life depression. Journal of Health and Social Behavior. 2007 doi: 10.2307/27638688. American Sociological Association. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.