Abstract
Childhood adversity is a potent risk factor for mental health conditions via disruptions to stress response systems. Dysregulations in oxidative stress systems have been associated with both childhood adversity and several psychological disorders (e.g., major depressive disorder) in adult populations. However, few studies have examined associations between childhood adversity, oxidative stress, and mental health in pediatric populations. Childhood adversity (Adverse Childhood Events [ACE]), oxidative stress [F2t-isoprostanes (IsoPs)], and mental health pathology were assessed in 50 adolescent females recruited primarily through the Department of Youth Services. Standard ordinary least squares regression models were run co-varying for age, race/ethnicity, adolescent nicotine use, study condition, and parent history of ACEs. Adolescents who reported experiencing four or more ACEs had significantly elevated IsoP levels. Further, internalizing symptom scores across diagnoses were significantly associated with elevated IsoPs, whereas no externalizing symptoms scores, except Attention Deficit Hyperactivity Disorder, were related to altered oxidative stress. Results indicate that IsoPs may be a global marker of childhood adversity and mental health symptomatology, particularly within internalizing symptom domains. A limitation is that body mass index was not collected for this sample. Future studies are needed to replicate and extend these findings in larger, more diverse samples.
Introduction
Childhood adversity encompasses a range of exposures across infancy through adolescence, such as parental separation or divorce, abuse and neglect, parental substance use problems, family psychiatric illnesses, parental incarceration, and witnessing intimate partner violence. Notably, childhood adversity has been linked to a range of maladaptive outcomes spanning across physical and mental health domains [1] and is a strong predictor of all classes of psychological disorders [2], even after accounting for poor health behaviors [3]. Further, high levels of early life stress and childhood adversity also place individuals at elevated risk of developing physical ailments, such as cardiovascular diseases, obesity, and diabetes mellitus [1, 4, 5]. Mounting evidence suggests that early adversity contributes to maladaptive stress response systems, which in turn, underlie the development of deleterious mental and physical health trajectories throughout the lifespan [1, 6, 7].
Childhood adversity and mental health
Both retrospective and prospective studies have examined whether childhood adversity is a risk factor for adult-onset psychopathology [8]. Depending upon the specific outcome evaluated, the findings generally indicate that childhood adversity is linked to the development of psychopathology across the lifespan [9], including adolescent-onset [9–12]. A large epidemiological study estimated that childhood adversity is associated with approximately 45% of all childhood-onset disorders and with up to 32% of all later-onset disorders [13]. During adolescence, there is a precipitous rise in several psychiatric illnesses [14], including depression, certain anxiety disorders (e.g., social anxiety disorder, panic disorders), and substance abuse disorder [15]. A review of epidemiological research found that nearly all mental health disorders start by adolescence [16].
Adolescence is an important period of developmental plasticity and sensitivity when brain development is highly dynamic [17]. Significant pubertal, hormonal, neuroendocrine, and metabolic changes occur during adolescence that may interact with early risk factors (e.g., adversity) and contribute to the onset and progression of mental health pathology. Delineating the mechanisms through which childhood adversity confers risk for emerging mental health problems prior to adulthood is imperative to understanding the etiology and progression of psychiatric illness.
Oxidative stress
Childhood adversity is associated with both physical and mental health outcomes, with limited understanding of the specific mediators of these associations [18]. Metabolic and immune systems have been implicated as potential putative mechanistic pathways underpinning the childhood adversity-health relationship [6, 19, 20]. McEwen and colleagues hypothesized that childhood adversity disrupts development by altering homeostasis through a process termed ‘allostatic load’, which can have targeted effects on mitochondrial function and the production of reactive oxygen species (ROS), as well as systemic effects on brain, immune and metabolic systems [21–23]. Reactive oxygen species refers to a range of molecules and free radicals that derive from molecular oxygen [24]. The majority of ROS are byproducts of cellular metabolism of oxygen that are internally produced by mitochondria, peroxisomes, and cytosolic enzyme systems; however, stress can also externally increase the production of ROS [25]. The dramatic increase in ROS following periods of prolonged stress can be detrimental [26], contributing to redox imbalance which occurs as antioxidant systems are unable to neutralize the effects of the ROS. Altogether, the imbalance between the ROS and antioxidant defenses results in oxidative stress. Oxidative stress has emerged as a candidate homeostatic disruption, with the brain particularly susceptible due to high oxygen consumption [27]. Common measures of oxidative stress include ROS, hydrogen peroxide, sphingolipid and glutathione metabolites, and eicosanoids, such as the family of isoprostanes and catalase activity [28]. Elevated isoprostanes, in particular, have been identified as a gold standard measure of oxidative stress, with the advantage revealing acute elevation in response to pathophysiological states, demonstrated maintenance of elevation over time, and normalized when pathophysiology is resolved [29, 30]. While initially applied in studies of pathogenesis in adults [31–33], more recent studies have demonstrated the capacity to measure elevated isoprostanes in early infancy and throughout childhood related to prematurity, diet and diagnosed disorders [34–38]. Thus, measures of elevated oxidative stress are reflected by isoprostane increases across the lifespan, indicating that the field will benefit from greater inclusion of the isoprostane measure in different contexts.
Childhood adversity and oxidative stress
Few studies have explicitly examined potential relations between childhood adversity and oxidative stress, particularly in pediatric populations. However, preliminary research from both animal and human models suggests that childhood adversity may contribute to oxidative stress. Animal studies have demonstrated that stressful stimuli lead to an increase of oxidative stress in the brain (as reviewed in, [39]). Overall, maternal deprivation paradigms in rodent models have shown an increase in brain lipid peroxidation and other markers of oxidative stress [40].
The literature on oxidative stress and childhood adversity in humans is limited. To date, the majority of these studies have been conducted in adult survivors of early trauma and most studies rely on indirect biomarkers of oxidative stress, such as telomere shortening, which can be induced and accelerated by ROS, and oxidative stress broadly [41, 42]. In general, adults with a history of childhood maltreatment and trauma have shorter telomeres [43–45], with a small-medium effect size [46].
To our knowledge, few studies have explicitly examined oxidative stress and childhood adversity. Epel and colleagues found that adult women with higher perceived life stress had both shorter telomeres and higher oxidative stress compared to the low-stress group, though these findings were not specific to stress during childhood [47]. In a study of children aged 6–14, perinatal complications were associated with elevations in a marker of lipid peroxidation compared to an unexposed group. Further, lipid peroxidation partially mediated the association between perinatal complications and child externalizing problems [48]. Overall, findings support that childhood adversity and oxidative stress are related, but with limited studies and evidence in pediatric populations.
Mental health and oxidative stress
A rich body of literature has already established key links between oxidative stress and physical health conditions that are often comorbid with mental health illnesses in adolescent populations, including diabetes mellitus [49] and obesity [50]. Several studies have provided evidence of elevated oxidative stress in depressed adults [51]. A meta-analysis of 18 studies found that oxidative stress is increased in adults with depression, although larger-scale studies are needed [52]. There also is evidence for elevated oxidative stress in adults with anxiety symptomatology [53], Attention Deficit Hyperactivity Disorder (ADHD) [54], and schizophrenia [55].
While the majority of such studies have been conducted with adults, one study did find preliminary evidence of high serum uric acid in adolescents with depression compared to a control group, which may indicate redox disruption [56]. A separate study documented a positive relationship between increased oxidative stress and elevated externalizing problem behaviors in a large community sample of 6–13 year old children [57]. A positive association between oxidative stress and mental health problems also was observed in a study of 495 children aged 6–12. Notably, this relationship was moderated by socioeconomic disadvantage, such that the association was only significant in children with more severe socioeconomic disadvantage [58]. Overall, these studies provide evidence to support the hypothesis that oxidative stress is linked to emerging mental health pathology in child and adolescent populations, and that childhood adversities, such as socioeconomic disadvantage, may play a key role in this association.
Oxidative stress as a pathway linking childhood adversity and mental health
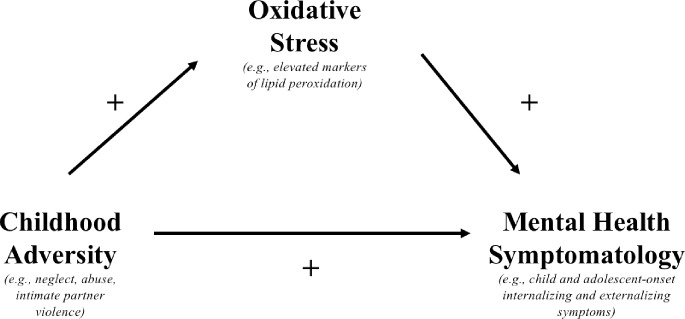
Oxidative stress may be a significant contributor to mental health disorders and brain alterations following early life stress, such as child abuse [47]. In adolescence, along with the increase in prevalence of many forms of psychopathology, gender disparities also emerge (as reviewed in, [14]). Most specifically, internalizing disorders are higher in females compared to males [59]. Further, recent evidence has suggested that elevations in oxidative stress for mood disorders, such as depression, are more robust in individuals with early traumatic experiences, particularly childhood sexual abuse [51]. Due to the emerging evidence linking oxidative stress to internalizing psychopathology, and the increase in internalizing pathology in female adolescents, female teenagers represent an important group to investigate for putative relations between childhood adversity, oxidative stress, and mental health. Altogether, while there are a limited number of studies, compelling results suggest that oxidative stress may serve as a mechanistic pathway linking childhood adversity and mental health symptom development. An important future direction will be to examine if oxidative stress mediates the association between childhood adversity and mental health (see Fig 1). A mediation model would indicate that oxidative stress accounts for the association between childhood adversity and mental health problems.
Fig 1. Proposed Mechanistic model of early life adversity, oxidative stress, and mental health symptoms.
Current study
In the current study, we aimed to explore the individual associations between childhood adversity, oxidative stress, and mental health in an adolescent sample of girls who were involved in the juvenile-justice system or receiving support services through schools or community agencies. We present results from a supplemental pilot study added to an ongoing intervention trial with 50 adolescent females with a range of early adversity exposure. We first hypothesized that the current study would replicate the common finding that childhood adversity, as indexed by adverse childhood experiences (ACEs) exposure, would be associated with elevated mental health pathology. Next, we sought to characterize a potential association between ACEs and oxidative stress. We hypothesized that ACEs and oxidative stress would be positively associated, such that adolescents with elevated exposure to ACEs would have comparatively higher levels of IsoPs. Next, we examined relative association between IsoPs and a range of mental health symptoms. Given the support for links between oxidative stress and several psychiatric illnesses, we did not have a specific hypothesis regarding differential associations between oxidative stress and certain disorders. Oxidative stress has been linked to a wide range of mental health disorders, including both internalizing disorders (e.g., depression; [51]) and externalizing disorders (e.g., ADHD; [54]). We first examined associations between IsoPs and externalizing and internalizing mental health composite scores. We then tested associations between individual clinical disorders (e.g., depression, ADHD) and IsoPs to explore any possible differential relationships in order to inform future theory development. Optimally, a next step would be to examine a mediation model to examine if and how much IsoPs account for the association between ACEs and mental health. However, due to the pilot and cross-sectional nature of this study, and limited sample size, it was beyond the scope of current study. A power analysis was conducted to confirm the required sample size given an α = .05, 95% power, and a medium effect size, with three predictors. The power analysis determined a minimum sample size of N = 63 and confirmed that the current study’s sample size was too small with predicted effects to examine mediation. Thus, this is instead explored as an important future direction with larger sample sizes [60, 61].
Methods
Participants
The sample comprised a subgroup of participants from an ongoing randomized control study of an intervention, Safe, Healthy, Adolescent Relationships and Peers (SHARP). SHARP aims to prevent drug use and risk behaviors in adolescent girls. Data in the current study were drawn only from the post-intervention assessment, and therefore detailed information on the intervention can be found elsewhere (Clinicaltrials.gov NCT02420548). The original study included 123 adolescent females aged 13–17 who were assessed both pre and post-intervention after recruitment primarily from the Department of Youth Services (DYS) and through schools and community organizations. For this study, a subsample of 50 adolescents were recruited at the post-intervention assessment. The pilot study was designed during the ongoing study and relevant measures were added following the initial Institutional Review Board (IRB) approval. This project was approved by the University of Oregon Research Compliance Services IRB (IRB Protocol Number: 10312013.040). Written consent for study participation was obtained from parents or legal guardians. Adolescents also provided written assent for participation. The consent procedure was approved by the IRB. Following study initiation, recruitment of the sample was continuous. The subsample did not differ from the larger sample of any key variables of interest (i.e., predictors/outcomes and covariates, p>.05).
The self-reported racial and ethnic breakdown of the sample was: 60% non-Hispanic White, 14% multiracial, 8% Black American, and 6% Native American. Further, 20% of individuals identified as Hispanic or Latinx. At the time of assessment, adolescents were between ages 14–19 with a mean age of 16.3 (SD = 1.4). The majority of the sample was recruited through DYS (64%) with the remaining participants recruited through community agencies that provide social services for adolescent girls at-risk for behavioral or emotional difficulties.
Measures
Childhood adversity
At the original study’s baseline assessment, childhood adversity was defined by and indexed through the Adverse Childhood Experiences-Screening Tool (ACE-ST) Scale, a shortened version of the original ACEs measure that assesses 10 possible adverse events occurring prior to the age 18 [1]. These events include: emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect, witnessing intimate partner violence, household substance abuse, parental separation or divorce, criminal household member, and mental illness in household. The ACE-ST has been found to demonstrate adequate internal consistency and good construct validity [62]. To preserve confidentiality, participants were instructed to indicate only the total number of ACEs they had experienced. The total number of ACEs experienced by respondents was their calculated ACE score. ACEs were examined as both a continuous variable and a categorical variable (dichotomized as Low to Moderate ACE group (0–3 ACEs) and High ACE group (4+ ACEs).
Mental health
Children’s mental health symptoms were assessed with the Youth’s Inventory (YI)-4 [63]. The YI-4 is a symptom inventory that contains the behavioral symptoms of 17 emotional and behavioral disorders from the Diagnostic Statistical Manual (DSM-IV). T-scores were calculated for the following disorders: ADHD (Inattention (α = .91), Hyperimpulsive (α = .87), and Combined Type (α = .93), Conduct Disorder (α = .92), Oppositional Defiant Disorder (α = .85), Generalized Anxiety Disorder (GAD) (α = .87), Schizophrenia (α = .74), Depressive Disorder (α = .87), Dysthymic Disorder (α = .85), Bipolar Disorder (α = .69), Anorexia Nervosa (α = .79), Bulimia Nervosa (α = .82), and Substance Use Disorder (α = .86). T-scores were all analyzed as continuous variables.
Control variables
The following variables were collected as potential confounders: child age, child race/ethnicity (categorical variable), household income (categorical variable), parent history of ACES (continuous variable), intervention vs control (study condition), and adolescent’s nicotine use (current yes/no).
Urine collection and biomarkers assessment
A urine sample was obtained from participants at the post-intervention interview. The sample was aliquoted and stored at a -80°C freezer without preservative. For assessment of oxidative stress, urine was analyzed for levels of F2-IsoPs, a stable marker of lipid peroxidation, following previously published protocols [29, 30, 36, 64]. Briefly, 1 ng of [2H4]-8-isoPGF2α an internal standard, was added to 1ml of thawed urine, followed by F2-IsoP extraction using C18 and Sep-pak cartridges. Pentaflurobenzyl esters were generated, purified, converted to trimethylsilyl ether derivatives and then subjected to analysis by tandem gas chromatography/negative ion chemical ionization-mass spectrometry. Urine creatinine was measured to adjust for variation of urine concentration between samples, with measures expressed as ng F2-isoprostanes/mg creatinine (ng/mg Cr).
Statistical analysis
Descriptive statistics are presented as means and standard deviations. Statistical analyses were performed with SPSS, v. 22 [65].
We first ran zero-order bivariate correlations to examine the following potential confounders: age, household income, parent history of ACES. We ran a one-way ANOVA to examine if there were significant differences in predictors and outcomes for the following categorical variables: nicotine use (Y/N), race and ethnicity, and intervention versus control. All covariates significantly associated with either adolescent ACEs, F2-isoprostanes, or adolescent mental health were included in subsequent analyses.
Three standard ordinary least squares (OLS) regression models were run (Model 1: If ACES predict mental health symptoms, Model 2: If ACEs predict F2-IsoPs, Model 3: If F2-IsoPs predict mental health symptoms). For the first two models, we first defined a Low to Moderate ACE Group as fewer than four ACE exposures and a High ACE Group as four or more ACE exposures [1]. We also ran the models with the continuous ACE score as a predictor to capture the full range of ACE exposure on mental health symptoms and F2-IsoP levels.
For Model 1, a one-way ANOVA was run to test mean difference of mental health T-scores between Low to Moderate and High ACE group. Pearson’s correlations were calculated to assess if the degree to which continuous ACEs were associated with children’s mental health symptoms. If the T-score for a mental health disorder had a non-normal distribution, a Spearman’s rank-order correlation was calculated. In Model 2, we calculated a one-way ANOVA to test if mean F2-IsoP levels differed between the Low to Moderate ACE and High ACE Group. A Pearson’s correlation was calculated to test the strength of correlation between continuous ACEs and F2-IsoP levels. In Model 3, we assessed the association between F2-IsoP concentration and mental health symptoms. We tested correlations between F2-IsoP concentration and the T-score of each mental health disorder. We also analyzed whether F2-IsoPs were related to composite mental health scores for internalizing disorders (i.e., Anorexia Nervosa, Bulimia Nervosa, Depressive Disorders, Dysthymic Disorder, and GAD) and externalizing disorders (i.e., Conduct Disorder, Oppositional Defiant Disorder, ADHD, Schizophrenia, Substance Use Disorder, and Bipolar Disorder).
Level of significance for all analysis was p < .05. However, we also present results with a Bonferroni corrected alpha level of < .004 to adjust for multiple comparisons for a more conservative approach.
Results
Clinical and demographic characteristics of the sample
Urine samples were successfully obtained from 50 adolescent females. Clinical and demographic characteristics of the sample are described in Table 1. Slightly less than half of the sample (n = 24, 48%) were assigned to the control condition, while the remaining 52% (n = 26) of the sample were in the active intervention condition. The number of ACEs endorsed ranged from 0–8, with an average ACE score of 2.69 (SD = 2.26). Thirty percent (n = 15) of the sample was in the High Ace Group (4+ ACE Exposures).
Table 1. Clinical and demographic characteristics of the sample.
| Variable | |
|---|---|
| Age in years; mean (SD) | 16.33(1.40) |
| Race (N, %) | |
| Caucasian | 30(60) |
| Black American | 4(8) |
| Native American | 3(6) |
| Multiracial | 7(14) |
| Other | 6(12) |
| Ethnicity (N, %) | |
| Non-Hispanic White | 33(66) |
| Hispanic | 10(20) |
| Other | 7(14) |
| Income (N, %)+ | |
| Less than $20,000 | 13(26) |
| $20,000-$39,999 | 14(28) |
| $40,000-$59,999 | 7(14) |
| $60,000-$79,999 | 9(18) |
| $80,000-$99,999 | 2(4) |
| $100,000 or more | 3(6) |
| Child ACE History (N, %) | |
| Low to Moderate (0–3 Exposures) | 35(70) |
| High (4–8 Exposures) | 15(30) |
| F2-Isoprostane Concentration (ng/mg Cr (M, SD) | 1.27(.44) |
| Mental Health T-Scores (M, SD) | |
| Internalizing Disorders | |
| Anorexia Nervosa | 50.10(10.02) |
| Bulimia Nervosa | 47.06(11.19) |
| Depressive Disorder | 50.81(10.33) |
| Dysthymic Disorder | 50.85(11.51) |
| Generalized Anxiety Disorder | 53.31(11.79) |
| Externalizing Disorders | |
| ADHD-Combined Type | 50.49(12.07) |
| Bipolar Disorder | 48.42(9.30) |
| Conduct Disorder | 47.37(7.10) |
| Oppositional Defiant Disorder | 47.04(11.09) |
| Schizophrenia | 49.13(8.75) |
| Substance Use Disorder | 49.76(8.82) |
+ two participants did not report their income.
Preliminary covariate analyses
Zero-order correlations between all variables of interest and potential confounders, including age, household income (continuous), parent history of ACE (continuous) were conducted (Table 2). One-way ANOVAs were conducted between all variables of interest and the following potential categorical confounders: race and ethnicity, intervention vs control (study condition), and adolescent nicotine use (current yes/no).
Table 2. Zero-Order bivariate correlations.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Child Age | - | 0.08 | -0.06 | 0.14 | 0.12 | -0.13 | 0.13 |
| 2. Household Income | - | - | -0.05 | -0.08 | -0.2 | -0.22 | 0.15 |
| 3. Parent ACEs | - | - | - | -0.24 | -0.14 | 0.11 | -0.16 |
| 4. Child ACEs | - | - | - | - | .40** | .44** | .34* |
| 5. Child Internalizing | - | - | - | - | - | .45** | .52*** |
| 6. Child Externalizing | - | - | - | - | - | - | 0.33 |
| 7. Child F2-Isoprostanes | - | - | - | - | - | - | - |
* p < .05
** p < .005
*** p < .001
For race, there was no significant association with child ACES (F = 1.18, p = .34), the internalizing composite score (F = .99, p = .46), the externalizing composite score (F = 1.13, p = .37), or F2-IsoPs (F = .76, p = .63). For ethnicity, there was no significant association with child ACES (F = .61, p = .62), the internalizing composite score (F = 1.08, p = .37), the externalizing composite score (F = .44, p = .73) or F2-IsoPs (F = .19, p = .91). There were no significant associations between race or ethnicity and any mental health disorder T-score (p>.10).
There were not significant associations between study condition with child ACES (F = 1.02, p = .32), the internalizing composite score (F = .38, p = .54), the externalizing composite score (F = .28, p = .60), or F2-IsoPs (F = 1.02, p = .32. There were no significant associations between study condition and any mental health disorder T-score (p >.10).
A marginally significant association was observed between nicotine use and child ACEs (F = 3.39, p = .05), There was no significant association observed between nicotine use and or F2-IsoPs (F = 2.21, p = .14). Significant associations were observed between adolescent nicotine use and internalizing composite score (F = 5.54, p = .02) and externalizing composite score (F = 24.42, p < .001). For internalizing disorders, adolescent nicotine use was significantly correlated with: GAD (F = 5.39, p = .03), depressive disorder (F = 5.64, p = .022), and dysthymic disorder (F = 4.82, p = .03). For externalizing disorders, adolescent nicotine use was significantly correlated with: ADHD-Inattentive Type (F = 6.69, p = .01), ADHD-Hyperimpulsive Type (F = 7.41, p = .01), ADHD-Combined Type (F = 10.40, p = .003), Conduct Disorder (F = 31.64, p < .001), Oppositional Defiant Disorder (F = 5.13, p = .03), Schizophrenia (F = 6.73, p = .01), and Substance Use Disorder (F = 36.10, p < .001). Therefore, for models examining the correlation between F2-IsoPs and the disorders listed above, adolescent nicotine use was entered as a covariate.
Additionally, a T-score of 70 or higher on the YI-4 indicates a higher degree of clinical severity. For each individual disorder, the proportion of adolescents who endorsed a T-score of 70 or higher can be found in S1 File. It should be noted that the YI-4 is not a diagnostic tool.
Missing data
There was no missing data for the ACEs or F2-isoprostanes. There was a modest amount of missing data for each of the mental health disorders and thus sample sizes dropped due to listwise deletion procedures for relevant analyses. The data were assumed to be missing completely at random. We tested if missingness was related to any of the relevant variables. Missingness was not related to any of the key variables or covariates (p>.1). Lastly, all analyses with predictors and outcomes were re-run with mean imputation and results remained consistent.
The sample size for these analyses is as follows: Internalizing Disorders: Composite Score (n = 42), GAD (n = 49), depressive disorder (n = 43), Dysthymic disorder (n = 46), Anorexia Nervosa (n = 49), and Bulimia Nervosa (n = 49). For externalizing Disorders: Composite Score (n = 36), ADHD-Inattentive Type (n = 44), ADHD-Hyperimpulsive Type (n = 45), ADHD-Combined Type (n = 43), Conduct Disorder (n = 46), Oppositional Defiant Disorder (n = 48), Schizophrenia (n = 48), Bipolar Disorder (n = 49), and Substance Use Disorder (n = 46).
Conduct Disorder, Oppositional Defiant Disorder, and Bulimia Nervosa had skewed distributions (kurtosis > 2). Results for analyses including these T-scores are non-parametric Spearman’s rank-order correlations.
ACEs and mental health
There was a significant difference observed between “Low to Moderate” versus “High “ACE group for mental health symptoms, such that adolescents in the High ACE group were more likely to endorse elevated symptoms from the following disorders: ADHD-Inattentive Type (F = 10.25, p = .003), ADHD-Hyperimpulsive Type (F = 4.39, p = .042), ADHD-Combined Type (F = 4.57, p = .038), GAD (F = 6.11, p = .017), Depressive Disorder (F = 8.59, p = .01), and Dysthymic Disorder (F = 6.44, p = .015). There were no significant correlations observed between ACE group membership and Conduct Disorder, Oppositional Defiant Disorder, Bipolar Disorder, Schizophrenia, Anorexia Nervosa, or Bulimia Nervosa. Further, continuous number of ACEs was significantly correlated with all the disorders listed except GAD (p>.05). Continuous number of ACEs was also associated with Substance Use Disorder (p < .05). Only ADHD-Inattentive Type was significantly correlated with the High ACE group with the more conservative Bonferroni correction of significance at α < .004.
An internalizing composite score was created for all internalizing disorders (α = .89) and externalizing disorders (α = .74). High ACE group membership was significantly and positively associated with the composite internalizing score (F = 7.59, p = .009) and marginally associated with the composite externalizing score (F = 3.91, p = .06).
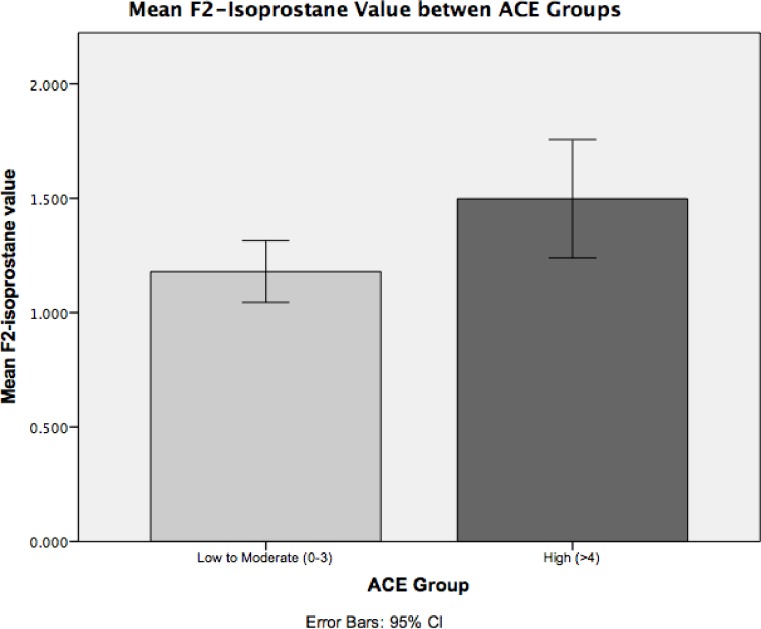
ACEs and F2-Isoprostanes
F2-IsoP levels were significantly elevated in the High ACE group compared to the Low to Moderate ACE group (F = 6.13, p = .017). F2-IsoP levels were .318 ng/mg higher in the High ACE group (n = 15) compared to the Low to Moderate ACE group (n = 35) (t = 2.48, p = .017) (see Fig 2). Continuous number of ACE exposures was not significantly related to F2-IsoP levels (r = .20, p = .16).
Fig 2. Mean F2-Isoprostane Value in Low to Moderate v High ACE Groups.
F2-Isoprostanes and mental health
Results between F2-IsoP levels and mental health symptoms are detailed in Table 3. At α < .05, F2-IsoP levels were significantly and positively correlated with all internalizing disorders and the internalizing disorder composite score (r = .52, p < .001). The correlations between F2-IsoP and the following disorders remained significant after statistical adjustment for adolescent nicotine use: GAD (r = .37, p = .01), Depressive Disorder (r = .46, p = .003), and Dysthymic Disorder (r = .37, p = .03). Significant and positive correlations persisted with the conservative Bonferroni correction, and statistical adjustment for nicotine use, between F2-IsoP levels and the internalizing composite score (r = .50, p = .001) and Depressive Disorder (r = .46, p = .003). The correlation between F2-IsoP and GAD remained marginally significant for GAD under the Bonferroni correction of p = .004 (r = .39, p = .005), even when adjusting for nicotine use (p = .005).
Table 3. Associations between mental health symptom T-scores and F2-isoprostane values.
| Disorder | B | SE | β | t | p |
|---|---|---|---|---|---|
| Internalizing Disorders | |||||
| Composite Scorea | 51.81 | 13.37 | 0.52 | 3.88 | <0.001+ |
| Anorexia Nervosa | 7.26 | 3.14 | 0.32 | 2.31 | 0.025 |
| Bulimia Nervosa | 8.96 | 3.47 | 0.35 | 2.59 | 0.013 |
| Depressive Disorderb | 11.08 | 3.11 | 0.49 | 3.56 | .001+ |
| Dysthymic Disorderb | 9.49 | 3.56 | 0.37 | 2.66 | 0.011 |
| Generalized Anxiety Disorderb | 10.55 | 3.59 | 0.39 | 2.94 | 0.005 |
| Externalizing Disorders | |||||
| Composite Scorea | 37.11 | 18.53 | 0.33 | 2 | 0.053 |
| ADHD-Cb | 12.03 | 3.65 | 0.46 | 3.3 | .002+ |
| ADHD-Ib | 10.11 | 4.23 | 0.35 | 2.39 | 0.022 |
| ADHD-Hb | 10.48 | 3.41 | 0.42 | 3.07 | .004+ |
| Bipolar Disorder | 1.41 | 3.07 | 0.07 | 0.46 | 0.648 |
| Conduct Disorder | 1.33 | 2.35 | 0.09 | 0.57 | 0.574 |
| Oppositional Defiant Disorder | -0.053 | 3.69 | 0 | -0.02 | 0.998 |
| Schizophrenia | 2 | 2.89 | 0.1 | 0.69 | 0.494 |
| Substance Use Disorder | 5.14 | 2.88 | 0.26 | 1.79 | 0.081 |
a Composite scaled score of all internalizing disorders (α = .89) and externalizing disorders (α = .74)
b Nicotine use was significantly associated with these disorders, and analyses were repeated with nicotine use as a covariate: GAD (r = .37, p = .01), Depressive Disorder (r = .46, p = .003), Dysthymic Disorder (r = .37, p = .03), ADHD-Combined Type; r = .41, p = .007, ADHD-Inattentive Type (r = .31, p = .045), ADHD-Hyperimpulsive Type, r = .38, p = .01).
+ indicates significant at Bonferroni corrected α = .004
There was a marginally significant correlation observed between F2-IsoP levels and the composite externalizing score (r = .33, p = .053), although this effect was not seen once we statistically adjusted the model for nicotine use (r = .30, p = .08). In the unadjusted models, F2-IsoP levels and ADHD-Combined Type (r = .46, p = .002) and ADHD-Hyperimpulsive Type (r = .42, p = .004) were significantly correlated, even following Bonferroni correction. However, when adjusting for nicotine use, the significance diminished, and the correlations were only significant at α < .05 (ADHD-Combined Type; r = .41, p = .007 and ADHD-Hyperimpulsive Type, r = .38, p = .01). At α < .05, F2-IsoP levels were also significantly correlated with ADHD-Inattentive Type (r = .35, p = .022), although this also attenuated after adjustment for nicotine use (r = .31, p = .045).
Discussion
This study provides preliminary evidence for significant associations between childhood adversity, mental health pathology, and an elevated biomarker measure, F2-IsoPs, that may indicate oxidative stress in a female adolescent sample. Thus, the results are the first to demonstrate that exposure to four or more ACEs is linked to potential dysregulation of systemic homeostasis. Further, elevated F2-IsoPs were also associated with emerging mental health symptomatology, highlighting that oxidative stress may occur even in subclinical presentations and adolescent expression of psychiatric illness. While it was not a primary aim of this study, we also confirmed that ACE exposure is associated with adolescent internalizing and externalizing problems, a result observed in several prior studies [66–68].
Childhood adversity and oxidative stress
Results from this pilot study extend the existing literature that childhood adversity is associated with dysregulation of several stress response systems, including metabolic pathways [19]. We demonstrate an explicit link between childhood ACES and oxidative stress in a pediatric population. The initial ACE study found a strong graded relationship between ACE exposure and physical and mental health risk factors and disorders. Specifically, it was noted that persons with four or more categories of childhood exposure exhibited a 4–12 fold increase in risk for smoking, alcoholism, depression, and suicide attempts [1]. Here, we established a similar graded relationship, but between adversity exposure and an elevated biomarker of oxidative stress. Specifically, these results indicated that increased risk (i.e., elevated F2-IsoP levels) was observed in individuals who had been exposed to four or more ACEs. Given these findings, further studies are warranted to examine if children exposed to a high degree of childhood adversity are more likely to exhibit oxidative stress across the lifespan.
To date, the majority of this research has been conducted in adult populations with retrospective reports of childhood adversity. However, evidence derived from animal and clinical studies have illustrated that extreme early adversity can “get under the skin” throughout the developmental lifespan [7]. Early adverse experiences contribute to vulnerable phenotypes to psychopathology in childhood via the persistent activation and sensitization of stress-response systems [69]. Dysregulation of metabolic systems during early ages can have persisting, and potentially deleterious, impact on brain structure-function development [7, 70, 71]. The significant elevation of lipid peroxidation in the group exposed to higher childhood adversity events is comparable to findings from animal studies, which have found that early stress exposure (e.g., maternal deprivation) is linked to lipid peroxidation [39, 40, 72]. Prior studies have demonstrated associations between certain forms of early adversity, such as socioeconomic disadvantage [58] and perinatal complications [48], with oxidative stress in human pediatric samples. Increased oxidative stress also has been observed in adult populations with a history of childhood maltreatment [73].
However, we also note that the relationship between continuous ACEs and F2-IsoP was non-significant. The significant association between the High ACE group and IsoP was only significant at α = .05, but not following Bonferroni correction. Therefore, results must be interpreted with caution. Additionally, the majority of the sample was exposed to relatively lower levels of childhood adversity (i.e., three or fewer ACEs). Thus, results indicate that in pediatric populations, we may not be able to detect metabolic impacts of lower exposure to childhood adversity. Nonetheless, these findings present preliminary evidence that there may be an important association between childhood adversity and F2-IsoPs. Future studies with larger sample sizes, and greater distribution of childhood adversity exposure, will help to establish if this finding is replicable.
Oxidative stress and mental health symptoms
There is an increasing understanding of the complex relations between brain and peripheral immune and metabolic systems. The challenge remains in elucidating the etiology in mediating the progression of mental health disorders [20]. In adults, there is ample evidence that oxidative stress is observed in individuals with a range of psychiatric illnesses, particularly major depressive disorder [74]. Given the high degree overlap in symptoms and underlying genetic associations between psychiatric illnesses [75], with a renewed emphasis on transdiagnostic associations, it is not surprising that oxidative stress has been reported in other mental health disorders and symptoms [53–55]. Here, we found that higher F2-IsoPs was associated with elevated symptoms of all internalizing disorders as well as ADHD. In particular, associations between F2-IsoPs and Depressive Disorder were the strongest, remaining significant after a stringent Bonferroni correction and adjustment for nicotine use. We also found a significant association with GAD (p = .005), which remained significant at α < .05, and marginally significant with a more conservative Bonferonni correction of α < .004. Recently, in adults, both GAD and depression have been associated with increased lipid peroxidation [76]. Our results indicate that the relationship between oxidative stress with anxiety and depression may also be observed in adolescence and prior to the full onset of the disorder. Lastly, we found a significant correlation between F2-IsoPs and ADHD, although this was attenuated following adjustment for nicotine use. Nonetheless, these findings build upon a meta-analysis of six studies reporting that oxidative stress markers were associated with ADHD. Notably, in five of those six studies, the mean age of the population was 9–10 [54].
It should be noted that the mean T-score for all disorders ranged between 48–51. For the YI-4, while it is not a diagnostic tool, a score above 70 indicates a higher degree of clinical severity. It should also be noted that depressive disorder and ADHD (all types) had the highest proportion of adolescent females with a score of 70 or greater (see Supplementary Material). Therefore, it is possible that the strongest associations were observed with these disorders as there were more participants endorsing a greater number of symptoms and severity. Importantly, our results also indicate that F2-IsoP concentration is associated with subclinical and emerging levels of internalizing and ADHD psychopathology. An implication of this finding is that F2-IsoPs may be a biomarker for the earlier onset of internalizing and ADHD symptoms, which could be useful in detecting children at higher risk for developing the clinically diagnosed disorder. Future prospective longitudinal research is needed to determine whether elevated F2-IsoPs predict mental health disorder diagnosis.
The present data do not support an association between oxidative stress and externalizing disorders other than ADHD. Other pediatric studies have found evidence for an association between externalizing symptoms and oxidative stress [57], but no support for this relationship was obtained from the current cohort. It is important to note that the sample in the current study was female, and internalizing symptoms were generally endorsed at higher rates than those in externalizing categories, with the exception of eating disorders. Further, during adolescence, rates of internalizing disorders are greater in females than males [59]. It is possible that in a larger and gender-diverse sample, it would be possible to detect associations between oxidative stress and externalizing symptomatology.
Additional research across development is necessary to characterize the associations between oxidative stress and specific clinical symptoms. For example, an important future direction will be to examine links between transdiagnostic clusters (e.g., sleep disruptions, anhedonia) and oxidative stress. Such research would contribute to a more precise understanding of any differential metabolic functioning between phenotypes. Overall, this would enhance the predictive power of biomarkers, such as F2-isoprostanes, in more effective identification of high-risk children, but also to increase the likelihood of predicting the most likely emergence of specific mental health symptoms.
Limitations
There are several limitations to the present study. First, there is a limited sample size for this pilot study that was added to an on-going clinical trial. The sample was also non-diverse in terms of gender and relatively less diverse regarding race and ethnicity. Second, there was missing data for the analyses of mental health disorders. Third, this was a moderate risk sample (i.e., 70% of the sample experienced three or fewer ACE exposures) and the majority of the sample reported relatively low levels of mental health pathology (i.e., less than a quarter of the sample endorsed clinically elevated symptom levels, see Supplemental material). However, we did observe robust associations (r>.4), particularly between F2-IsoPs and Depressive Disorders, ADHD-Hyperimpulsive Type, and GAD. Given the restricted range of T-scores, it is possible that lower correlations were observed than if there were a greater distribution of scores. While F2-IsoP concentration was associated with all internalizing disorder symptoms and ADHD, there are weaknesses due to multiple comparisons and elevated risk for Type I error. To mitigate this, Bonferroni correction was applied, and demonstrated a strong association between F2-IsoPs and Depressive Disorders, while other relationships were significant at α< .05 (e.g., eating disorders and oxidative stress), suggesting that conclusions should be drawn more carefully.
The study also was unable to collect data on significant confounders that are important in oxidative stress-related research [77]. Of highest concern is the lack of data for body mass index (BMI) or waist circumference. Increased oxidative stress has been associated with obesity in adults, and adiposity can be causally related to the production of ROS [78, 79]. Therefore, we cannot be certain that our findings would not have been modified by adiposity. It should be noted that compared to adults, obesity in childhood may be less chronic and therefore potentially less of a strong confounder with metabolic disruption [80] and psychopathology [81]. Other important confounders include parental mental health and medication use by study subjects. A future direction will be to replicate these findings in a larger study designed specifically to examine these variables.
Additionally, we did not have item-level data on ACE exposures. Therefore, we can only characterize that high ACE exposure broadly was associated with elevated F2-IsoPs and mental health. It is possible that certain types of ACE exposure are more heavily associated with disruptions to metabolic functioning. Further, while we did not find evidence of a relationship between continuous number of ACEs with oxidative stress, we note that the High ACE group only contained an n = 15, with the majority of the sample having fewer than 4 ACE exposures. A larger sample likely will provide a wider range of adversity exposure to explore more fully the associations between childhood adversity and oxidative stress.
Conclusions and future directions
Our results, obtained in a pilot study, provide initial support that there are potentially important relations between childhood adversity, oxidative stress, and mental health symptom development. These relationships have been explored more fully in adult samples; the present study provides emerging support that associations can be detected in adolescence. Future research will benefit from extending these results in adolescence and exploring these relations at earlier stages of development (e.g., infancy, middle childhood) using a longitudinal framework.
The study was too small to examine a full mediation model. However, our results provide a foundation for examining whether oxidative stress may mediate the association between childhood adversity and mental health symptomatology. It is also possible that F2-IsoPs also moderates this association. Future well-powered studies with longitudinal designs will be able to fully explore whether F2-IsoPs mediate or moderate the association between childhood adversity and mental health pathology. It is possible that childhood adversity may only predict mental health symptomatology, or would be a stronger predictor, in individuals with dysregulation of metabolic pathways, such as oxidative stress. If there is a moderation or mediation effect this would support the hypothesis that F2-IsoPs, an index of lipid peroxidation and oxidative stress, is a reliable biomarker of toxic stress to help identify children at highest risk. This will have strong implications for prevention and intervention work.
The potential outcomes of childhood adversity are severe. We urgently need innovative strategies to delineate how and why adversity impacts health so broadly, to understand developmental trajectories, and to recognize the children in most need of support. Taken together, this knowledge can be leveraged to alleviate the consequences of childhood adversity and toxic stress.
Supporting information
(XLSX)
(DOCX)
Acknowledgments
Analysis of eicosanoids (include specific compounds such as isoprostanes, prostaglandins, or leukotrienes) were performed in the Vanderbilt University Eicosanoid Core Laboratory. We acknowledge Rachel Kovensky for recruitment, Alex Wagnon for research coordination, and Sally Guyer for data processing.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The research was supported in part by the Simms/Mann Chair in Developmental Neurogenetics and Research Fund (PL), The WM Keck Chair in Neurogenetics (PL). Research was also supported by P50 DA035763, NIDA, U.S. PHS, Research Component 2. Leslie Leve was supported by P50 DA035763, NIDA, U.S. PHS. Sarah R. Horn received support from National Science Foundation Graduate Research Fellowship Program, Fellow ID: 2017244647.
References
- 1.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–58. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. The British Journal of Psychiatry. 2010;197(5):378–85. 10.1192/bjp.bp.110.080499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137(6):959–97. 10.1037/a0024768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Rand AM, Hamil-Luker J. Processes of cumulative adversity: Childhood disadvantage and increased risk of heart attack across the life course. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60:S117–S24. [DOI] [PubMed] [Google Scholar]
- 5.Thomas C, Hyppönen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics. 2008;121(5):e1240–e9. 10.1542/peds.2007-2403 [DOI] [PubMed] [Google Scholar]
- 6.Fagundes CP, Glaser R, Kiecolt-Glaser JK. Stressful early life experiences and immune dysregulation across the lifespan. Brain, Behavior, and Immunity. 2013;27:8–12. 10.1016/j.bbi.2012.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e46. 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- 8.Oh DL, Jerman P, Marques SS, Koita K, Boparai SKP, Harris NB, et al. Systematic review of pediatric health outcomes associated with childhood adversity. BMC pediatrics. 2018;18(1):83 10.1186/s12887-018-1037-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clark C, Caldwell T, Power C, Stansfeld SA. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Annals of epidemiology. 2010;20(5):385–94. 10.1016/j.annepidem.2010.02.008 [DOI] [PubMed] [Google Scholar]
- 10.Benjet C, Borges G, Medina-Mora ME. Chronic childhood adversity and onset of psychopathology during three life stages: childhood, adolescence and adulthood. Journal of psychiatric research. 2010;44(11):732–40. 10.1016/j.jpsychires.2010.01.004 [DOI] [PubMed] [Google Scholar]
- 11.Lumley MN, Harkness KL. Specificity in the relations among childhood adversity, early maladaptive schemas, and symptom profiles in adolescent depression. Cognitive Therapy and Research. 2007;31(5):639–57. [Google Scholar]
- 12.Johnson JG, Cohen P, Gould MS, Kasen S, Brown J, Brook JS. Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Archives of general psychiatry. 2002;59(8):741–9. [DOI] [PubMed] [Google Scholar]
- 13.Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Archives of general psychiatry. 2010;67(2):113–23. 10.1001/archgenpsychiatry.2009.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rutter M. Psychopathological development across adolescence. Journal of youth and adolescence. 2007;36(1):101–10. [Google Scholar]
- 15.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of general psychiatry. 2003;60(8):837–44. 10.1001/archpsyc.60.8.837 [DOI] [PubMed] [Google Scholar]
- 16.Kessler RC, Amminger GP, Aguilar‐Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: a review of recent literature. Current opinion in psychiatry. 2007;20(4):359–64. 10.1097/YCO.0b013e32816ebc8c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gee DG, Casey B. The impact of developmental timing for stress and recovery. Neurobiology of stress. 2015;1:184–94. 10.1016/j.ynstr.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McLaughlin KA. Future directions in childhood adversity and youth psychopathology. Journal of Clinical Child & Adolescent Psychology. 2016;45(3):361–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Danese A, Lewis SJ. Psychoneuroimmunology of early-life stress: the hidden wounds of childhood trauma? Neuropsychopharmacology. 2017;42(1):99–114. 10.1038/npp.2016.198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dantzer R, O'Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nature Reviews Neuroscience. 2008;9(1):46–56. 10.1038/nrn2297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Picard M, McEwen BS. Psychological stress and mitochondria: a systematic review. Psychosomatic medicine. 2018;80(2):141–53. 10.1097/PSY.0000000000000545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Picard M, McEwen BS. Psychological stress and mitochondria: a conceptual framework. Psychosomatic medicine. 2018;80(2):126–40. 10.1097/PSY.0000000000000544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peters A, McEwen BS, Friston K. Uncertainty and stress: Why it causes diseases and how it is mastered by the brain. Progress in neurobiology. 2017;156:164–88. 10.1016/j.pneurobio.2017.05.004 [DOI] [PubMed] [Google Scholar]
- 24.Turrens JF. Mitochondrial formation of reactive oxygen species. The Journal of physiology. 2003;552(2):335–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Finkel T, Holbrook NJ. Oxidants, oxidative stress and the biology of ageing. Nature. 2000;408(6809):239–47. 10.1038/35041687 [DOI] [PubMed] [Google Scholar]
- 26.Halliwell B, Cross CE. Oxygen-derived species: their relation to human disease and environmental stress. Environmental health perspectives. 1994;102(suppl 10):5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Floyd RA, Carney JM. Free radical damage to protein and DNA: mechanisms involved and relevant observations on brain undergoing oxidative stress. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 1992;32(S1):S22–S7. [DOI] [PubMed] [Google Scholar]
- 28.Naviaux RK. Metabolic features of the cell danger response. Mitochondrion. 2014;16:7–17. 10.1016/j.mito.2013.08.006 [DOI] [PubMed] [Google Scholar]
- 29.Milne GL, Sanchez SC, Musiek ES, Morrow JD. Quantification of F 2-isoprostanes as a biomarker of oxidative stress. Nature protocols. 2007;2(1):221–26. 10.1038/nprot.2006.375 [DOI] [PubMed] [Google Scholar]
- 30.Milne GL, Yin H, Hardy KD, Davies SS, Roberts LJ. Isoprostane generation and function. Chemical reviews. 2011;111(10):5973–96. 10.1021/cr200160h [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Czerska M, Zielinski M, Gromadzinska J. Isoprostanes-A novel major group of oxidative stress markers. International journal of occupational medicine and environmental health. 2015. [DOI] [PubMed] [Google Scholar]
- 32.Milne GL, Dai Q, Roberts LJ II. The isoprostanes—25 years later. Biochimica et Biophysica Acta (BBA)-Molecular and Cell Biology of Lipids. 2015;1851(4):433–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sottero B, Rossin D, Poli G, Biasi F. Lipid oxidation products in the pathogenesis of inflammation-related gut diseases. Current medicinal chemistry. 2018;25(11):1311–26. 10.2174/0929867324666170619104105 [DOI] [PubMed] [Google Scholar]
- 34.Matthews M, Aschner JL, Stark A, Moore P, Slaughter J, Steele S, et al. Increasing F2-isoprostanes in the first month after birth predicts poor respiratory and neurodevelopmental outcomes in very preterm infants. Journal of Perinatology. 2016;36(9):779 10.1038/jp.2016.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.See V, Mas E, Prescott S, Beilin L, Burrows S, Barden A, et al. Effects of postnatal omega-3 fatty acid supplementation on offspring pro-resolving mediators of inflammation at 6 months and 5 years of age: A double blind, randomized controlled clinical trial. Prostaglandins, Leukotrienes and Essential Fatty Acids (PLEFA). 2017;126:126–32. [DOI] [PubMed] [Google Scholar]
- 36.Frederiksen BN, Seifert J, Kroehl M, Lamb MM, Milne GL, Rewers M, et al. Timing of solid food introduction is associated with urinary F 2-isoprostane concentrations in childhood. Pediatric research. 2015;78(4):451 10.1038/pr.2015.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rendo-Urteaga T, Puchau B, Chueca M, Oyarzabal M, Azcona-Sanjulián MC, Martinez JA, et al. Total antioxidant capacity and oxidative stress after a 10-week dietary intervention program in obese children. European journal of pediatrics. 2014;173(5):609–16. 10.1007/s00431-013-2229-7 [DOI] [PubMed] [Google Scholar]
- 38.Gorrindo P, Lane CJ, Lee EB, McLaughlin B, Levitt P. Enrichment of elevated plasma F2t-isoprostane levels in individuals with autism who are stratified by presence of gastrointestinal dysfunction. PloS one. 2013;8(7):e68444 10.1371/journal.pone.0068444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schiavone S, Jaquet V, Trabace L, Krause K-H. Severe life stress and oxidative stress in the brain: from animal models to human pathology. Antioxidants & redox signaling. 2013;18(12):1475–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Uysal N, Gonenc S, Acikgoz O, Pekçetin Ç, Kayatekin BM, Sonmez A, et al. Age-dependent effects of maternal deprivation on oxidative stress in infant rat brain. Neuroscience letters. 2005;384(1–2):98–101. 10.1016/j.neulet.2005.04.052 [DOI] [PubMed] [Google Scholar]
- 41.Kawanishi S, Oikawa S. Mechanism of telomere shortening by oxidative stress. Annals of the New York Academy of Sciences. 2004;1019(1):278–84. [DOI] [PubMed] [Google Scholar]
- 42.Correia-Melo C, Hewitt G, Passos JF. Telomeres, oxidative stress and inflammatory factors: partners in cellular senescence? Longevity & healthspan. 2014;3(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tyrka AR, Price LH, Kao H-T, Porton B, Marsella SA, Carpenter LL. Childhood maltreatment and telomere shortening: preliminary support for an effect of early stress on cellular aging. Biological psychiatry. 2010;67(6):531–4. 10.1016/j.biopsych.2009.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O'Donovan A, Epel E, Lin J, Wolkowitz O, Cohen B, Maguen S, et al. Childhood trauma associated with short leukocyte telomere length in posttraumatic stress disorder. Biological psychiatry. 2011;70(5):465–71. 10.1016/j.biopsych.2011.01.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kiecolt-Glaser JK, Gouin J-P, Weng N-p, Malarkey WB, Beversdorf DQ, Glaser R. Childhood adversity heightens the impact of later-life caregiving stress on telomere length and inflammation. Psychosomatic medicine. 2011;73(1):16–22. 10.1097/PSY.0b013e31820573b6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ridout K, Levandowski M, Ridout S, Gantz L, Goonan K, Palermo D, et al. Early life adversity and telomere length: a meta-analysis. Molecular psychiatry. 2018;23(4):858 10.1038/mp.2017.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Epel ES, Blackburn EH, Lin J, Dhabhar FS, Adler NE, Morrow JD, et al. Accelerated telomere shortening in response to life stress. Proceedings of the National Academy of Sciences. 2004;101(49):17312–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mansur RB, Cunha GR, Asevedo E, Zugman A, Rios AC, Salum GA, et al. Perinatal complications, lipid peroxidation, and mental health problems in a large community pediatric sample. European child & adolescent psychiatry. 2017;26(5):521–9. [DOI] [PubMed] [Google Scholar]
- 49.Martín-Gallán P, Carrascosa A, Gussinyé M, Domínguez C. Biomarkers of diabetes-associated oxidative stress and antioxidant status in young diabetic patients with or without subclinical complications. Free Radical Biology and Medicine. 2003;34(12):1563–74. [DOI] [PubMed] [Google Scholar]
- 50.Karamouzis I, Pervanidou P, Berardelli R, Iliadis S, Papassotiriou I, Karamouzis M, et al. Enhanced oxidative stress and platelet activation combined with reduced antioxidant capacity in obese prepubertal and adolescent girls with full or partial metabolic syndrome. Hormone and metabolic research. 2011;43(09):607–13. [DOI] [PubMed] [Google Scholar]
- 51.Anderson G, Maes M. The Biological Underpinnings of Mood Disorders Interact With Early Trauma, Sexual Abuse and Neuroticism: Implications for Psychiatric Classification and Treatment Inflammation and Immunity in Depression: Elsevier; 2018. p. 549–67. [Google Scholar]
- 52.Black CN, Bot M, Scheffer PG, Cuijpers P, Penninx BW. Is depression associated with increased oxidative stress? A systematic review and meta-analysis. Psychoneuroendocrinology. 2015;51:164–75. 10.1016/j.psyneuen.2014.09.025 [DOI] [PubMed] [Google Scholar]
- 53.Steenkamp LR, Hough CM, Reus VI, Jain FA, Epel ES, James SJ, et al. Severity of anxiety–but not depression–is associated with oxidative stress in Major Depressive Disorder. Journal of affective disorders. 2017;219:193–200. 10.1016/j.jad.2017.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Joseph N, Zhang-James Y, Perl A, Faraone SV. Oxidative stress and ADHD: a meta-analysis. Journal of attention disorders. 2015;19(11):915–24. 10.1177/1087054713510354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Flatow J, Buckley P, Miller BJ. Meta-analysis of oxidative stress in schizophrenia. Biological psychiatry. 2013;74(6):400–9. 10.1016/j.biopsych.2013.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tao R, Li H. High serum uric acid level in adolescent depressive patients. Journal of affective disorders. 2015;174:464–6. 10.1016/j.jad.2014.12.031 [DOI] [PubMed] [Google Scholar]
- 57.Cunha GR, Asevedo E, Mansur RB, Zugman A, Pan PM, Gadelha A, et al. Inflammation, neurotrophism and oxidative stress and childhood psychopathology in a large community sample. Acta Psychiatrica Scandinavica. 2016;133(2):122–32. 10.1111/acps.12453 [DOI] [PubMed] [Google Scholar]
- 58.Mansur RB, Cunha GR, Asevedo E, Zugman A, Zeni-Graiff M, Rios AC, et al. Socioeconomic disadvantage moderates the association between peripheral biomarkers and childhood psychopathology. PloS one. 2016;11(8):e0160455 10.1371/journal.pone.0160455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Angold A, Rutter M. Effects of age and pubertal status on depression in a large clinical sample. Development and psychopathology. 1992;4(1):5–28. [Google Scholar]
- 60.Cohen J, Cohen P, West SG, Aiken LS. Applied multiple correlation/regression analysis for the behavioral sciences. UK: Taylor & Francis; 2003. [Google Scholar]
- 61.Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychological science. 2007;18(3):233–9. 10.1111/j.1467-9280.2007.01882.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Meinck F, Steinert JI, Sethi D, Gilbert R, Bellis MA, Mikton C, Alink L, Baban A. Measuring and monitoring national prevalence of child maltreatment: a practical handbook. [Google Scholar]
- 63.Gadow KD, Sprafkin J, Carlson GA, Schneider J, Nolan EE, Mattison RE, et al. A DSM-IV–referenced, adolescent self-report rating scale. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(6):671–9. [DOI] [PubMed] [Google Scholar]
- 64.Milne GL, Gao B, Terry ES, Zackert WE, Sanchez SC. Measurement of F2-isoprostanes and isofurans using gas chromatography–mass spectrometry. Free Radical Biology and Medicine. 2013;59:36–44. 10.1016/j.freeradbiomed.2012.09.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. [Google Scholar]
- 66.Herringa RJ, Birn RM, Ruttle PL, Burghy CA, Stodola DE, Davidson RJ, et al. Childhood maltreatment is associated with altered fear circuitry and increased internalizing symptoms by late adolescence. Proceedings of the National Academy of Sciences. 2013;110(47):19119–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schroeder A, Slopen N, Mittal M. Accumulation, timing, and duration of early childhood adversity and behavior problems at age 9. Journal of Clinical Child & Adolescent Psychology. 2018:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Grasso DJ, Dierkhising CB, Branson CE, Ford JD, Lee R. Developmental patterns of adverse childhood experiences and current symptoms and impairment in youth referred for trauma-specific services. Journal of abnormal child psychology. 2016;44(5):871–86. 10.1007/s10802-015-0086-8 [DOI] [PubMed] [Google Scholar]
- 69.Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biological psychiatry. 2001;49(12):1023–39. [DOI] [PubMed] [Google Scholar]
- 70.Shonkoff JP, Levitt P. Neuroscience and the future of early childhood policy: Moving from why to what and how. Neuron. 2010;67(5):689–91. 10.1016/j.neuron.2010.08.032 [DOI] [PubMed] [Google Scholar]
- 71.Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, et al. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Archives of pediatrics & adolescent medicine. 2009;163(12):1135–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Réus GZ, Fernandes GC, de Moura AB, Silva RH, Darabas AC, de Souza TG, et al. Early life experience contributes to the developmental programming of depressive-like behaviour, neuroinflammation and oxidative stress. Journal of psychiatric research. 2017;95:196–207. 10.1016/j.jpsychires.2017.08.020 [DOI] [PubMed] [Google Scholar]
- 73.Boeck C, Koenig AM, Schury K, Geiger ML, Karabatsiakis A, Wilker S, et al. Inflammation in adult women with a history of child maltreatment: the involvement of mitochondrial alterations and oxidative stress. Mitochondrion. 2016;30:197–207. 10.1016/j.mito.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 74.Maes M, Galecki P, Chang YS, Berk M. A review on the oxidative and nitrosative stress (O&NS) pathways in major depression and their possible contribution to the (neuro) degenerative processes in that illness. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2011;35(3):676–92. 10.1016/j.pnpbp.2010.05.004 [DOI] [PubMed] [Google Scholar]
- 75.Plummer JT, Gordon AJ, Levitt P. the Genetic intersection of Neurodevelopmental Disorders and shared Medical comorbidities–relations that translate from Bench to Bedside. Frontiers in psychiatry. 2016;7:142 10.3389/fpsyt.2016.00142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Maes M, Bonifacio KL, Morelli NR, Vargas HO, Moreira EG, Stoyanov DS, et al. Generalized Anxiety Disorder (GAD) and Comorbid Major Depression with GAD Are Characterized by Enhanced Nitro-oxidative Stress, Increased Lipid Peroxidation, and Lowered Lipid-Associated Antioxidant Defenses. Neurotoxicity research. 2018:1–22. [DOI] [PubMed] [Google Scholar]
- 77.Horn SR, Long MM, Nelson BW, Allen NB, Fisher PA, Byrne ML. Replication and reproducibility issues in the relationship between C-reactive protein and depression: A systematic review and focused meta-analysis. Brain, behavior, and immunity. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. The Journal of clinical investigation. 2017;114(12):1752–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fernández-Sánchez A, Madrigal-Santillán E, Bautista M, Esquivel-Soto J, Morales-González Á, Esquivel-Chirino C, et al. Inflammation, oxidative stress, and obesity. International journal of molecular sciences. 2011;12(5):3117–32. 10.3390/ijms12053117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Reid BM, Harbin MM, Arend JL, Kelly AS, Dengel DR, Gunnar MR. Early Life Adversity with Height Stunting Is Associated with Cardiometabolic Risk in Adolescents Independent of Body Mass Index. The Journal of pediatrics. 2018;202:143–9. 10.1016/j.jpeds.2018.06.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003;111(4):851–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.