Abstract
Introduction:
African Americans, especially those in the South, suffer a disproportionate burden of obesity and are at high risk for perceived discrimination (PD). This study investigates the association between PD and weight status among African Americans and clarifies the role of perceived stress and health behaviors in this relationship.
Methods:
Data came from the Jackson Heart Study, Examination 1 (2000–2004; analyses conducted in 2016 using Stata, version 14). African Americans from Jackson, Mississippi, aged 21–95 years were recruited (N=5,301). Weight status was measured using anthropometric data with BMI; waist circumference (in centimeters); and obesity class (I, II, III). Survey instruments were used to measure PD, perceived global stress, and health behaviors. Multivariate regression was used to model weight status outcomes as a function of PD, perceived stress, and health behaviors.
Results:
After controlling for sociodemographic factors and health status, perceived everyday discrimination was associated with higher BMI (b=0.33, p<0.01); higher waist circumference (b=0.70, p<0.01); and higher relative risk of Class III obesity versus non-obesity (relative risk ratio, 1.18; p<0.001). Global perceived stress was linked to higher BMI (b=0.42, p<0.05) and higher waist circumference (b=1.18; p<0.01) and partially mediated the relationships between PD and these weight status outcomes. Health behaviors led to suppression rather than mediation between PD and weight status and between stress and weight status.
Conclusions:
PD and perceived stress are potential risk factors for higher weight status. They should be considered as a part of a comprehensive approach to reduce obesity among African Americans.
INTRODUCTION
African Americans suffer a disproportionately high prevalence of obesity and are more likely to suffer from obesity comorbidities.1 Although the causes of this disparity are not entirely understood, higher rates of perceived discrimination (PD) among African Americans compared with any other racial/ethnic group2,3 have been suggested as a potential factor.4 Yet, there are inconsistent findings concerning the role of PD in obesity and other aspects of weight status, including BMI; waist circumference (WC) and hip circumference; and body composition measures (e.g., fat content and types of adipose tissue accumulation). The interpretation of these findings is complicated by differences in samples and recruitment, as well as by differences in the measurement of weight status and PD, either everyday PD (e.g., how often people treat you with less respect) or lifetime PD (e.g., unfair treatment on the job and in other life areas). In addition, PD instruments vary in how they treat the attributed reason for discrimination. In most studies, respondents first report perceived discrimination due to any reason and later are asked to select the main reason for discrimination (e.g., race, gender, age). Some studies, however, use instruments specifically designed to measure racial discrimination. In this paper, the term “PD” is used to refer to discrimination due to any reason and “perceived racism” for racial discrimination.
The evidence concerning the relationship between PD and weight status falls into three groups. The first group suggests a positive relation between PD and weight status. Hunte,5 for instance, finds that everyday PD relates to over-time increases in WC in the general population of midlife Americans. Cozier and colleagues6 report that among women participating in Black Women’s Health Study, over-time weight gain increases as perceived lifetime and everyday racism increase.
The second group of studies suggests a lack of a positive relationship between PD and weight status. Shelton et al.7 observe no relationship between perceived lifetime racism and BMI in a sample of lower-income African American and Hispanic Bostonians. Vines and colleagues8 find that after controlling for daily stress, perceived racism is linked to lower, not higher, waist-to-hip ratio among African American women whereas daily stress is linked to higher waist-to-hip ratio.
Finally, the third group of studies focuses specifically on adiposity and suggests that the role of PD varies by sex and the manner by which adiposity and PD are measured. Everyday discrimination is positively associated with visceral fat, but not subcutaneous fat among middle-aged African American and Caucasian women residing in Chicago.9 By contrast, among female African Americans residing in Mississippi, subcutaneous and visceral fat volume is positively related to non-racial (height/weight, age, gender, or other) lifetime discrimination, but not everyday non-racial discrimination.10 Among male African Americans in this sample, everyday discrimination is linked to higher subcutaneous fat but not to visceral fat.
Although methodologic differences likely contribute to empirical inconsistencies, a more serious limitation is the lack of a theoretically grounded framework in most studies. To overcome this limitation, this study used the stress process theory11 to develop a conceptual model of the role of PD in weight status. This theory argues that the placement of an individual in a social hierarchy explains exposure to stressors and their patterning. Low-social status individuals, including racial/ethnic minorities, tend to experience more stressful events and more chronic stress. In addition, stress often proliferates in the lives of low–social status individuals, with stressors in one life area begetting stressors in other areas.12,13 This is substantiated by research arguing that along with direct effects and health behaviors, discrimination affects health comprehensively by increasing overall levels of stress.4 Overall, low–social status individuals experience higher levels of stress, which in turn can lead to an array of adverse health consequences.
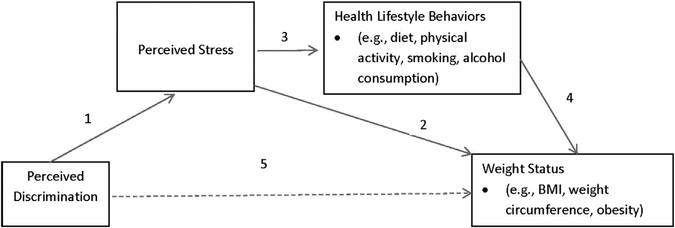
Using this theoretic framework, a conceptual model that clarifies the relationship between PD and weight status is proposed. PD is conceptualized as a stressor (Figure 1, Arrow 1) causing physiologic and behavioral changes that make one more susceptible to gaining weight4 (Figure 1, Arrows 2–4). Physiologically, stress activates the hypothalamic–pituitary–adrenal axis, which governs the metabolic process.14 Additionally, stress-induced changes in lifestyle behaviors, including eating, physical activity, alcohol consumption, and sleep quality, can all lead to weight gain.15–20 Exposure to stress, for instance, is linked to overeating, selecting foods high in sugar and fat, and “comfort eating,”21 and physical activity, a well-established tool in weight management, tends to be low in highly stressed adults.15,16,22 Thus, the positive relationship between PD and weight status is mediated by stress and lifestyle behaviors (Figure 1, Arrow 5).
Figure 1.
Conceptual model of the relationships among perceived discrimination, perceived stress, health lifestyle behaviors, and weight status.
Note: The dashed line indicates a mediated relationship.
Based on this conceptual model, the following hypotheses are derived that consider whether the relationship between PD and weight status operates through measures such as global stress and negative health behaviors:
Higher levels of perceived everyday discrimination are related to higher weight status measured by BMI; obesity class (I, II, and III); and WC.
Global perceived stress mediates the relationship between PD and weight status.
Lifestyle measures (physical activity, diet, alcohol consumption, smoking) further mediate the relationship between global perceived stress and weight status.
METHODS
Study Sample
Data were drawn from Examination 1 (2000–2004) of the Jackson Heart Study (JHS), a community-based cohort study of non-institutionalized African Americans aged 21–95 years residing in three counties of Mississippi.23,24 Participants were enrolled from four sources: random (17%); volunteer (22%); the Atherosclerosis Risk in Communities Study (30%); and family members (31%). The final sample (N=5,301) is geographically representative of the study population.23 Details of the study design are published elsewhere.24,25 The study was approved by the IRBs of University of Mississippi Medical Center, Jackson State University, and Tougaloo College. All participants provided informed consent.
Roughly 5% of the survey respondents lacked complete information on the study variables. Data were examined to determine whether they were missing at random by creating a dichotomous variable representing missingness on any of the study variables and was used to predict weight status in the full model. This indicator was not significant, indicating data were missing at random and multiple imputations were appropriate.26 Five multiply-imputed data sets were created and analyzed, and results for non-imputed data were similar. All analyses were performed in 2016 using Stata, version 14.
Measures
Weight status was measured using anthropometric data collected by trained staff. It was assessed using three measures:
a continuous measure of BMI defined as weight (kg)/height (m)2;
a continuous measure of WC in centimeters; and
a categorical measure of obesity defined as non-obese (BMI<30, ref); obese I (BMI 30–34.9); obese II (BMI 35–39.9); and obese III (BMI ≥40).
Everyday PD was assessed using a nine-item instrument adapted from Williams27 and validated in the JHS by Sims et al.28 with good internal reliability (α=0.88). Participants were asked, How often on a day-to-day basis do you have the following experiences? Options included you are treated with less courtesy, you are treated with less respect, people act as if you are dishonest, poor service at restaurants, people think you aren’t smart, people are afraid of you, people think you’re not as good as they are, called names/insulted, and threatened/harassed. Responses were recorded on a Likert-type scale ranging from 1 (never) to 7 (several times a day). All but 2% of respondents had complete information for all nine items. The mean of the nine responses was used to indicate the overall everyday discrimination score and was calculated for all respondents who answered at least one item. Following the discrimination questions, participants were asked which of the following they believed was the reason for discrimination (age, gender, race, height/weight, or some another reason). Dummy variables were constructed for each reason, with no discrimination as the ref.
Perceived global chronic stress (henceforth “perceived stress”) was measured by an instrument created specifically for the JHS25 and based on three existing measures.29–31 Respondents rated the severity of stress, 1=not stressful to 4=very stressful, that they have experienced over the past 12 months in the following eight domains: employment, relationships, the neighborhood, caring for others, legal problems, medical problems, experiences of racism and discrimination, and meeting basic needs. The mean of the responses across the eight domains was used to indicate perceived stress, with only 2% of respondents not answering all eight items. Cronbach’s alpha was 0.72.
Health behaviors included currently using tobacco (yes=1, no=0) and having drank alcohol during the past 12 months (yes=1, no=0). Physical activity and nutritional status were assessed using Life’s Simple Seven metrics developed by American Heart Association.32 A dichotomous indicator of ideal physical activity indicated whether or not the respondent achieves the recommended level of physical activity based on active living score, sports index score, home/life score, and work score.33 A dichotomous indicator for ideal nutrition indicated whether or not the respondent meets the recommended criteria concerning consumption of fruit and vegetables, fish, fiber-rich foods, sugar-sweetened beverages, and sodium.34 All health behaviors were based on self-report.
Covariates included health status, measured using self-rated health (5-point scale ranging from 1=“poor” to 5=“excellent”) and sociodemographic background including age in years (centered); the quadratic of age; gender (male versus female); education (less than high school, high school or General Educational Development test, some college or vocational school, college/associate degree or more); and whether the respondent has health insurance (yes=1, no=0).
Statistical Analysis
Descriptive statistics for the whole sample and by obesity status were calculated. To assess relationships between main predictors and obesity prior to adjustment, bivariate tests were used. Next, nested multivariate regression models predicting weight status outcomes were estimated. Linear regression was used for the continuous dependent variables, BMI and WC, and multinomial logistic regression for the obesity categories. To address Hypothesis 1, which argues that PD is positively associated with weight status, Model 1 included daily PD, reasons for discrimination, and the control variables. Model 2 addressed Hypothesis 2, which argues that perceived stress mediates the association between PD and weight status, by adding perceived stress to Model 1. Mediation was tested by examining whether the indirect effect of PD on weight status through stress was significant. Hypothesis 3 argues that health behaviors mediate the relationship between stress and weight status. It was examined in Model 3 by adding the health behaviors (smoking, alcohol use, physical activity, and nutrition) and examining indirect effects. As the final step, sensitivity analyses were conducted to examine whether the role of PD varied by gender or age.
RESULTS
Table 1 presents descriptive statistics by obesity grades and for the total sample. The overall prevalence of obesity in the sample was 53.3% (obese I, 26.6%; obese II, 14.9%; obese III, 11.9%), which was high but similar to the prevalence found in the National Health and Nutrition Examination Survey for African American adults.35 Obese individuals had higher mean scores on the everyday discrimination scale (obese I, 2.08; obese II, 2.07; obese III, 2.26) compared with the non-obese (2.04). The obese also had higher mean perceived stress scores (non-obese, 1.60; obese I, 1.63; obese II, 1.69; obese III, 1.77) and were less likely to achieve the recommended level of physical activity (non-obese, 21.7%; obese I, 19.2%; obese II, 14.5%; obese III, 14.5%). By contrast, obese participants showed better health behaviors for smoking (non-obese, 16.1%; obese I, 11.1%; obese II, 10.0%; obese III, 10.5%) and alcohol consumption (non-obese, 49.5%; obese I, 45.2%; obese II, 39.7%; obese III, 40.9%). Compared with their non-obese counterparts, obese respondents tended to be younger, be more commonly women, have poorer self-rated health, have lower levels of education, and less commonly have health insurance. Table 2 presents the multivariate regression models predicting weight status outcomes. Hypothesis 1 was supported in Model 1, which included everyday PD, perceived reason for the discrimination, and sociodemographic controls. Higher scores on the PD scale were associated with higher BMI (b=0.33, p<0.01); higher WC (b=0.70, p<0.01); and higher risk of being class III obese compared with non-obese (relative risk ratio, 1.18; p<0.001). Hypothesis 2 was supported for BMI and WC (Model 2). Perceived stress was significantly associated with BMI (b=0.42, p<0.05) and WC (b=1.18, p<0.01) and partially mediated the coefficients between PD and BMI (b=0.26, p<0.05) and PD and WC (b=0.52, p<0.05). The indirect effect of PD on BMI through stress was significant (b=0.06, p<0.05) and explained 19.2% of the total effect of PD on BMI. Examining the model for WC, the indirect effect was significant (b=0.18, p<0.01) and explained 26.2% of the total effect. Lastly, Model 3 (full model) addressed Hypothesis 3 by including the health behaviors. Rather than finding mediation between perceived stress and the weight status outcomes, there was a suppression effect, as the magnitude of PD coefficients in Model 3 slightly increased compared with that in Model 2. This was likely due to the fact that tobacco use and alcohol use were associated with lower (not higher) weight status (Tables 3 and 4). At the same time, these two behaviors increased among individuals with higher levels of perceived stress (mean stress for tobacco users compared with non-users, 1.77 vs 1.62, p<0.001; mean stress for alcohol users compared with non-users, 1.71 vs 1.58, p<0.001).
Table 1.
Characteristics of Study Participants by Obesity Status and for the Total Sample
| Characteristics | Non-obese (n=2,472; 46.7%) | Obese I (n=1,407; 26.6%) | Obese II (n=789; 14.9%) | Obese III (n=628; 11.9%) | Total (N=5,301) |
|---|---|---|---|---|---|
| Weight status | |||||
| BMI (range: 14.6–91.8) | 26.1 (0.06) | 32.3 (0.04) | 37.1 (0.05) | 46.0 (0.25) | 31.7 (0.10) |
| Waist circumference (cm; range: 32–244) | 89.6 (0.19) | 102.9 (0.24) | 112.0 (0.38) | 125.3 (0.64) | 100.7 (0.22) |
| Perceived discrimination | |||||
| Everyday discrimination (range: 1–7) | 2.04 (0.02) | 2.08 (0.03) | 2.07 (0.04) | 2.26 (0.04) | 2.08 (0.01) |
| Reason for discrimination (%) | |||||
| Weight/height | 1.6 | 1.5 | 3.1 | 12.6 | 3.0 |
| Gender | 5.7 | 6.4 | 5.5 | 6.2 | 6.0 |
| Age | 12.0 | 12.4 | 11.0 | 9.1 | 11.6 |
| Race | 40.0 | 38.9 | 37.9 | 35.7 | 38.9 |
| Other | 22.4 | 23.6 | 25.0 | 23.3 | 23.2 |
| No discriminationa | 18.3 | 17.2 | 17.5 | 13.1 | 17.3 |
| Socio-demographic background | |||||
| Male (%) | 45.9 | 34.8 | 25.0 | 17.6 | 36.5 |
| Age (years; range: 20.5–95.5) | 56.2 (0.27) | 55.7 (0.32) | 55.0 (0.45) | 52.0 (0.49) | 55.4 (0.18) |
| Highest education (%) | |||||
| Less than high school | 20.5 | 20.9 | 20.7 | 18.4 | 20.4 |
| High school diploma | 17.8 | 18.8 | 19.0 | 19.6 | 18.5 |
| Some college | 20.0 | 23.2 | 23.0 | 24.6 | 21.9 |
| College degreea | 41.7 | 37.1 | 37.3 | 37.4 | 39.2 |
| Has health insurance (%) | 88.5 | 86.2 | 84.1 | 83.2 | 86.6 |
| Self-rated health (range: 1–5) | 2.59 (0.02) | 2.56 (0.02) | 2.50 (0.03) | 2.46 (0.03) | 2.55 (0.01) |
| Health behaviors | |||||
| Current tobacco user (%) | 16.1 | 11.1 | 10.0 | 10.5 | 13.2 |
| Alcohol use past 12 months (%) | 49.5 | 45.2 | 39.7 | 40.9 | 45.9 |
| Ideal physical activity (%) | 21.7 | 19.2 | 14.5 | 14.5 | 19.1 |
| Ideal nutrition (%) | 1 | 1.3 | 0.5 | 0.6 | 0.9 |
| Global perceived chronic stress (range: 1–4) | 1.60 (0.01) | 1.63 (0.01) | 1.69 (0.02) | 1.77 (0.02) | 1.64 (0.01) |
Source: Jackson Heart Study, Examination 1 (2000–2004).
Note: Boldface indicates statistical significance between non-obese (BMI <30) (p<0.05). SEs are in parentheses. BMI defined as weight (kg)/height (m)2.
Reference category.
Table 2.
Nested Multivariate Linear and Multinomial Logistic Regression Estimates Predicting Weight Status (n=5,301)
| Covariates | Model 1,a RRR/b (95% CI) | Model 2,b RRR/b (95% CI) | Model 3,c RRR/b (95% CI) |
|---|---|---|---|
| Linear regression | |||
| BMI | |||
| Perceived everyday discrimination | 0.33** (0.11, 0.54) | 0.26* (0.04, 0.49) | 0.29** (0.07, 0.52) |
| Global perceived chronic stress | - | 0.42* (0.04, 0.80) | 0.52** (0.14, 0.90) |
| Waist circumference (cm)5 | |||
| Perceived everyday discrimination | 0.70** (0.21, 1.19) | 0.52* (0.01, 1.03) | 0.57* (0.06, 1.07) |
| Global perceived chronic stress | - | 1.18** (0.30, 2.05) | 1.37** (0.50, 2.24) |
| Multinomial logistic regression (ref=non-obese, BMI <30) | |||
| Obese I (BMI 30–34.9) | |||
| Perceived everyday discrimination | 1.05 (0.97, 1.13) | 1.05 (0.97, 1.14) | 1.06 (0.98, 1.15) |
| Global perceived chronic stress | - | 0.97 (0.84, 1.11) | 0.99 (0.86, 1.14) |
| Obese II (BMI 35–39.9) | |||
| Perceived everyday discrimination | 1.05 (0.95, 1.15) | 1.03 (0.93, 1.13) | 1.03 (0.94, 1.14) |
| Global perceived chronic stress | - | 1.14 (0.97, 1.34) | 1.17 (0.99, 1.22) |
| Obese III (BMI ≥40) | |||
| Perceived everyday discrimination | 1.18*** (1.07, 1.30) | 1.15** (1.04, 1.28) | 1.16** (1.05, 1.30) |
| Global perceived chronic stress | - | 1.15 (0.96, 1.37) | 1.20 (1.00, 1.43) |
Source: Jackson Heart Study, Examination 1 (2000–2004).
Note: Boldface indicates statistical significance (*p<0.05; **p<0.01; ***p<0.001). BMI defined as weight (kg)/height (m)2.
Model 1 controls for gender, age, age squared, education, insurance status, self-rated health, and reason for discrimination.
Model 2 adds global perceived chronic stress to Model 1.
Model 3 adds health behaviors, alcohol consumption, smoking, diet, and physical activity, to Model 2. RRR, relative risk ratio; b, unstandardized coefficient.
Table 3.
Multivariate Linear Regression Models Predicting Weight Status (n=5,301)
| Covariates | BMI, b (95% CI) | Waist circumference (cm), b (95% CI) |
|---|---|---|
| Perceived discrimination | ||
| Everyday discrimination | 0.29** (0.07, 0.52) | 0.57* (0.06, 1.07) |
| Reason for discriminationa | ||
| Weight/height | 6.52*** (5.31, 7.74) | 13.50*** (10.72, 16.27) |
| Gender | −1.08* (−2.05, −0.12) | −2.83* (−4.98, −0.68) |
| Age | −0.54 (−1.31, 0.24) | −0.39 (−2.18, 1.41) |
| Race | −0.22 (−0.86, 0.42) | −0.55 (−2.00, 0.91) |
| Other | −0.16 (−0.83, 0.51) | −0.36 (−1.90, 1.18) |
| Perceived global chronic stress | 0.52** (0.14, 0.90) | 1.37** (0.50, 2.24) |
| Socio-demographic background | ||
| Male | −2.70** (−3.11, −2.30) | 1.75*** (0.82, 2.67) |
| Age (centered) | −0.05*** (−0.07, −0.04) | 0.07** (0.03, 0.11) |
| Age squared | 0.00*** (0.00, 0.00) | 0.00*** (−0.01, 0.00) |
| Highest educationb | ||
| Less than high school | 0.83** (0.25, 1.40) | 2.65*** (1.33, 3.97) |
| High school | 0.44 (−0.10, 0.98) | 1.34* (0.10, 2.58) |
| Some college | 0.89** (0.38, 1.39) | 2.48*** (1.33, 3.64) |
| Has health insurance | −0.59* (−1.15, −0.02) | −1.10 (−2.40, 0.20) |
| Self-rated health | −0.27* (−0.50, −0.04) | −0.85** (−1.38, −0.32) |
| Health behaviors | ||
| Current tobacco user | −2.19*** (−2.77, −1.61) | −4.08*** (−5.40, −2.75) |
| Alcohol use in past 12 months | −0.62** (−1.03, −0.22) | −1.46** (−2.38, −0.53) |
| Ideal physical activity | −0.87*** (−1.36, −0.39) | −2.71*** (−3.82, −1.60) |
| Ideal nutrition | −0.30 (−2.23, 1.63) | −1.14 (−5.55, 3.26) |
Source: Jackson Heart Study, Examination 1 (2000–2004).
Note: Boldface indicates statistical significance (*p<0.05; **p<0.01; ***p<0.001). BMI is defined as weight (kg)/height (m)2.
Ref= no discrimination.
Ref= college degree.
, unstandardized coefficient.
Table 4.
Multinomial Logistic Regression Models Predicting Obese I, II, or III Compared to Non-obese (n=5,301)
| Covariates | Obese I (BMI 30–34.9), RRR (95% CI) | Obese II (BMI 35–39.9), RRR (95% CI) | Obese III (BMI <40), RRR (95% CI) |
|---|---|---|---|
| Perceived discrimination | |||
| Everyday discrimination | 1.06 (0.98, 1.15) | 1.03 (0.94, 1.14) | 1.16** (1.05, 1.29) |
| Reason for discriminationa | |||
| Weight/height | 0.93 (0.51, 1.68) | 1.90* (1.05, 3.46) | 7.87*** (4.72, 13.12) |
| Gender | 0.95 (0.68, 1.33) | 0.74 (0.48, 1.13) | 0.79 (0.49, 1.28) |
| Age | 1.02 (0.77, 1.34) | 0.87 (0.62, 1.23) | 0.82 (0.54, 1.24) |
| Race | 0.96 (0.76, 1.21) | 0.96 (0.73, 1.27) | 0.95 (0.68, 1.32) |
| Other | 1.02 (0.80, 1.29) | 1.04 (0.78, 1.38) | 0.99 (0.70, 1.39) |
| Perceived global chronic stress | 0.99 (0.86, 1.14) | 1.17 (0.99, 1.39) | 1.19 (1.00, 1.43) |
| Socio-demographic background | |||
| Male | 0.64*** (0.56, 0.74) | 0.42*** (0.35, 0.51) | 0.25*** (0.20, 0.32) |
| Age (centered) | 0.99* (0.99, 1.00) | 0.99** (0.98, 1.00) | 0.97*** (0.96, 0.98) |
| Age squared | 1.00*** (1.00, 1.00) | 1.00** (1.00, 1.00) | 1.00*** (1.00, 1.00) |
| Highest educationb | |||
| Less than high school | 1.38** (1.12, 1.69) | 1.30* (1.01, 1.68) | 1.54** (1.15, 2.08) |
| High school diploma | 1.22* (1.00, 1.48) | 1.17 (0.92, 1.48) | 1.35* (1.03, 1.76) |
| Some college | 1.37** (1.14, 1.64) | 1.28* (1.02, 1.60) | 1.35* (1.05, 1.73) |
| Has health insurance | 0.86 (0.70, 1.06) | 0.76* (0.60, 0.97) | 0.84 (0.65, 1.10) |
| Self-rated health | 0.97 (0.89, 1.06) | 0.90* (0.81, 1.00) | 0.87* (0.77, 0.98) |
| Health behaviors | |||
| Current tobacco user | 0.61*** (0.49, 0.75) | 0.56*** (0.43, 0.75) | 0.54*** (0.40, 0.74) |
| Alcohol use in past 12 months | 0.95 (0.82, 1.09) | 0.77** (0.65, 0.93) | 0.74** (0.61, 0.91) |
| Ideal physical activity | 0.90 (0.76, 1.07) | 0.66*** (0.53, 0.83) | 0.64** (0.50, 0.84) |
| Ideal nutrition | 1.32 (0.70, 2.47) | 0.54 (0.19, 1.59) | 0.87 (0.29, 2.58) |
Source: Jackson Heart Study, Examination 1 (2000–2004).
Note: Boldface indicates statistical significance (*p<0.05; **p<0.01; ***p<0.001). BMI defined as weight (kg)/height (m)2.
Ref= no discrimination.
Ref= college degree.
RRR, relative risk ratio.
Sensitivity analyses indicated that the interaction effects between PD and gender and between PD and age were not significant. These results suggest that the effects of PD on weight status do not differ for men and women and for different age groups.
DISCUSSION
This study reveals that in a large community-based sample of African Americans residing in the South, PD is linked to higher BMI, higher WC, and higher risk of class III obesity. The relationships of PD to BMI and to WC are partially mediated by perceived stress, suggesting that stress may constitute one pathway through which PD contributes to higher weight status.
Interestingly, health behaviors did not attenuate the association between perceived stress and weight status. Perhaps the explanation may lie in the weight-lowering effects of smoking and drinking, well-known stress-related behaviors. Prior investigations revealed that people with higher levels of PD are indeed more likely to use tobacco.36–38 These findings highlight the multifaceted ways through which discrimination may lead to poorer overall health. PD harms different facets of health as different types of coping behaviors are employed in response to PD. Unhealthy diet and lack of physical activity, for instance, contribute to higher weight, thus increasing cardiovascular disease risk. Smoking and drinking further increase this risk,39 even as they may lead to lower weight status.40,41
Although these analyses were able to explain some of the effect of PD on weight status through stress, PD remained a significant predictor, suggesting that other mechanisms not considered here contribute to higher body weight among individuals exposed to discrimination. Individuals who report discrimination have poorer healthcare access,42,43 potentially including limited counseling on weight control, diet, and physical activity.44,45 An alternative explanation lies in individuals experiencing discrimination not having the energy or resources for making healthy choices or participating in behaviors that promote good health.4 Additionally, self-report measures of diet are prone to error and may be why these analyses fail to find mediation between perceived stress and weight status.46 Finally, PD may represent a unique stressor that operates differently from the aspects of stress captured by the measures used in these analyses.
Limitations
This study is not without its limitations. First, it uses cross-sectional data, which do not allow one to assess trends over time or make causal conclusions. The theoretic framework suggests that PD contributes to obesity, but obesity may also contribute to increased PD. These analyses attempted to lessen this possibility by controlling for attributed reasons for PD, particularly weight/height. Lastly, the data set used in this study is a non-random sample from a single site in a southern state that has a large African American population as well as some of the highest rates of obesity in the nation. Results from this study should be replicated using data from other sources.
There are also strengths of this study. JHS is the largest study of cardiovascular disease among African Americans, containing anthropometric (as opposed to self-reported) measures of weight status and complex assessment of discrimination including attributed reason. Few studies have examined the extent to which attribution of discrimination is linked to weight status among African American individuals. As one may expect, African Americans with higher weight status in this study were more likely to attribute discrimination to their weight/height. At the same time, however, weight/height was among the least common reasons, even across obesity grades. Results for other reasons were less expected. Respondents who attributed discrimination to gender had lower BMI and WC compared with those who reported no discrimination (after controlling for sex and other covariates). Interestingly, race as a reason did not relate to weight status, suggesting that perceiving everyday discrimination in general (but not specifically attributing it to race) plays a role in weight status among African Americans. This conclusion is consistent with research suggesting that discrimination of any type is stressful and therefore potentially harmful to health.47–49
CONCLUSIONS
Interventions aiming to reduce health disparities associated with obesity should consider addressing PD as a potential mechanism for the high levels of obesity in African American communities. As high rates of PD among African Americans fundamentally stem from social inequalities on the structural level, structural intervention to address health inequalities must be developed and implemented. In addition, individual-level interventions such as counseling and education focusing on stress management and behavior modification may be useful in stemming the adverse effects of persisting systemic inequalities on minority health. Health professional–community partnerships may work against factors contributing to obesity through planning, implementing, and evaluating community-based health promotion programs.
Past research has consistently demonstrated that African American individuals, particularly those in the South, are at greater risk for obesity compared with other populations.35,50,51 Efforts to reduce obesity prevalence among African Americans must incorporate a complex set of factors, often related to their marginalized status, that contribute to obesity. Perceived discrimination and stress are among potential risk factors and thus should be considered as a part of a comprehensive approach to obesity prevention among African Americans.
ACKNOWLEDGMENTS
The authors thank the Jackson Heart Study team (University of Mississippi Medical Center, Jackson State University, and Tougaloo College) and participants for their long-term commitment that continues to improve the understanding of the epidemiology of cardiovascular and other chronic diseases.
The study was supported in part by a grant from the National Institute of Minority Health and Health Disparities (U54MD008176). The Jackson Heart Study is supported by contracts HHSN 268201300046C, HHSN268201300047C, HHSN2682013000 48C, HHSN268201300049C, and HHSN268201300050C from the National Heart, Lung, and Blood Institute and the National Institute on Minority Health and Health Disparities. Dr. Sims is supported by the grants P60MD002249 and U54MD008176 from the National Institute on Minority Health and Health Disparities.
The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; NIH; or U.S. DHHS.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat 10. 2012;252:1–207. [PubMed] [Google Scholar]
- 2.Purnell JQ, Peppone LJ, Alcaraz K, et al. Perceived discrimination, psychological distress, and current smoking status: results from the Behavioral Risk Factor Surveillance System reactions to race module, 2004–2008. Am J Public Health. 2012;102(5):844–851. 10.2105/AJPH.2012.300694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corral I, Landrine H. Racial discrimination and health-promoting vs damaging behaviors among African-American adults. J Health Psychol. 2012:1176–1184. 10.1177/1359105311435429. [DOI] [PubMed] [Google Scholar]
- 4.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hunte HER. Association between perceived interpersonal everyday discrimination and waist circumference over a 9-year period in the midlife development in the United States Cohort Study. Am J Epidemiol. 2011;173(11):1232–1239. 10.1093/aje/kwq463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cozier YC, Wise LA, Palmer JR, Rosenberg L. Perceived racism in relation to weight change in the Black Women’s Health Study. Ann Epidemiol. 2009;19(6):379–387. 10.1016/j.annepidem.2009.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shelton RC, Puleo E, Bennett GG, McNeill LH, Sorensen G, Emmons KM. The association between racial and gender discrimination and body mass index among residents living in lower-income housing. Ethn Dis. 2009;19(3):251–264. [PMC free article] [PubMed] [Google Scholar]
- 8.Vines AI, Baird DD, Stevens J, Hertz-Picciotto I, Light KC, McNeilly M. Associations of abdominal fat with perceived racism and passive emotional responses to racism in African American women. Am J Public Health. 2007;97(3):526–530. 10.2105/AJPH.2005.080663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis TT, Kravitz HM, Janssen I, Powell LH. Self-reported experiences of discrimination and visceral fat in middle-aged African-American and Caucasian women. Am J Epidemiol. 2011;173(11):1223–1231. 10.1093/aje/kwq466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hickson DA, Lewis TT, Liu J, et al. The associations of multiple dimensions of discrimination and abdominal fat in African American adults: the Jackson Heart Study. Ann Behav Med. 2012;43(1):4–14. 10.1007/s12160-011-9334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. 1981;22(4):337–356. 10.2307/2136676. [DOI] [PubMed] [Google Scholar]
- 12.Pearlin LI, Aneshensel CS, LeBlanc AJ. The forms and mechanisms of stress proliferation: the case of AIDS caregivers. J Health Soc Behav. 1997;38(3):223–236. 10.2307/2955368. [DOI] [PubMed] [Google Scholar]
- 13.Pearlin LI. The stress process revisited: reflections on concepts and their interrelationships In: Aneshensel CS, Phelan JC, eds. Handbook of the Sociology of Mental Health. New York: Plenum; 2000:395–415. [Google Scholar]
- 14.Youn J-Y, Siu KL, Lob HE, Itani H, Harrison DG, Cai H. Role of vascular oxidative stress in obesity and metabolic syndrome. Diabetes. 2014;63(7):2344–2355. 10.2337/db13-0719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychol. 2003;22(6):638 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- 16.Kashani M, Eliasson A, Vernalis M. Perceived stress correlates with disturbed sleep: a link connecting stress and cardiovascular disease. Stress. 2012;15(1):45–51. 10.3109/10253890.2011.578266. [DOI] [PubMed] [Google Scholar]
- 17.Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011;14(4):402 10.1097/MCO.0b013e3283479109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jääskeläinen A, Nevanperä N, Remes J, Rahkonen F, Järvelin M-R, Laitinen J. Stress-related eating, obesity and associated behavioural traits in adolescents: a prospective population-based cohort study. BMC Public Health. 2014;14(1):321–334. 10.1186/1471-2458-14-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsenkova V, Boylan JM, Ryff C. Stress eating and health. Findings from MIDUS, a national study of US adults. Appetite. 2013;69:151–155. 10.1016/j.appet.2013.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Groesz LM, McCoy S, Carl J, et al. What is eating you? Stress and the drive to eat. Appetite. 2012;58(2):717–721. 10.1016/j.appet.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449–458. 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 22.Schnohr P, Kristensen T, Prescott E, Scharling H. Stress and life dissatisfaction are inversely associated with jogging and other types of physical activity in leisure time—the Copenhagen City Heart Study. Scand J Med Sci Sports. 2005;15(2):107–112. 10.1111/j.1600-0838.2004.00394.x. [DOI] [PubMed] [Google Scholar]
- 23.Fuqua SR, Wyatt SB, Andrew ME, et al. Recruiting African-American research participation in the Jackson Heart Study: methods, response rates, and sample description. Ethn Dis. 2005;15(4)(suppl 6):S6–S18. [PubMed] [Google Scholar]
- 24.Taylor HA Jr, Wilson JG, Jones DW, et al. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study . Ethn Dis. 2005;15(4)(suppl 6): S6–S4. [PubMed] [Google Scholar]
- 25.Payne TJ, Wyatt SB, Mosley TH, et al. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis. 2005;15(suppl 6):S6–S38. [PubMed] [Google Scholar]
- 26.Acock AC. Working with missing values. J Marriage Fam. 2005;67(4):1012–1028. 10.1111/j.1741-3737.2005.00191.x. [DOI] [Google Scholar]
- 27.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351. 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 28.Sims M, Diez-Roux AV, Dudley A, et al. Perceived discrimination and hypertension among African Americans in the Jackson Heart Study. Am J Public Health. 2012;102(suppl 2):S258–S265. 10.2105/AJPH.2011.300523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kohn PM, Macdonald JE. The survey of recent life experiences: a decontaminated hassles scale for adults. J Behav Med. 1992;15(2):221–236. 10.1007/BF00848327. [DOI] [PubMed] [Google Scholar]
- 30.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983:385–396. 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 31.Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the Life Experiences Survey. J Consult Clin Psychol. 1978;46(5):932 10.1037/0022-006X.46.5.932. [DOI] [PubMed] [Google Scholar]
- 32.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 33.Smitherman TA, Dubbert PM, Grothe KB, et al. Validation of the Jackson Heart Study physical activity survey in African Americans. J Phys Act Health. 2009;6(1):S124. [DOI] [PubMed] [Google Scholar]
- 34.Djoussé L, Petrone AB, Blackshear C, et al. Prevalence and changes over time of ideal cardiovascular health metrics among African-Americans: the Jackson Heart Study. Prev Med. 2015;74:111–116. 10.1016/j.ypmed.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 36.Sims M, Diez-Roux AV, Gebreab SY, et al. Perceived discrimination is associated with health behaviours among African-Americans in the Jackson Heart Study. J Epidemiol Community Health. 2016;70(2):187–194. 10.1136/jech-2015-206390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Borrell LN, Roux AVD, Jacobs DR, et al. Perceived racial/ethnic discrimination, smoking and alcohol consumption in the Multi-Ethnic Study of Atherosclerosis (MESA). Prev Med. 2010;51(3):307–312. 10.1016/j.ypmed.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chae DH, Takeuchi DT, Barbeau EM, Bennett GG, Lindsey J, Krieger N. Unfair treatment, racial/ethnic discrimination, ethnic identification, and smoking among Asian Americans in the National Latino and Asian American Study. Am J Public Health. 2008;98(3):485–492. 10.2105/AJPH.2006.102012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Albert MA, Williams DR. Invited commentary: discrimination—an emerging target for reducing risk of cardiovascular disease? Am J Epidemiol. 2011;173(11):1240–1243. 10.1093/aje/kwq514. [DOI] [PubMed] [Google Scholar]
- 40.Albanes D, Jones DY, Micozzi MS, Mattson ME. Associations between smoking and body weight in the U.S. population: analysis of NHANES II. Am J Public Health. 1987;77(4):439–444. 10.2105/AJPH.77.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shimokata H, Muller DC, Andres R. Studies in the distribution of body fat: III. Effects of cigarette smoking. JAMA. 1989;261(8): 1169–1173. 10.1001/jama.1989.03420080089037. [DOI] [PubMed] [Google Scholar]
- 42.Paradies Y A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35(4):888–901. 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- 43.Gee GC, Ro A, Shariff-Marco S, Chae D. Racial discrimination and health among asian americans: evidence, assessment, and directions for future research. Epidemiol Rev. 2009;31(1):130–151. 10.1093/epirev/mxp009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gonzales KL, Harding AK, Lambert WE, Fu R, Henderson WG. Perceived experiences of discrimination in health care: a barrier for cancer screening among American Indian women with type 2 diabetes. Womens Health Issues. 2013;23(1):e61–e67. 10.1016/j.whi.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Trivedi AN, Ayanian JZ. Perceived discrimination and use of preventive health services. J Gen Intern Med. 2006;21(6):553–558. 10.1111/j.1525-1497.2006.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vitolins MZ, Rand CS, Rapp SR, Ribisl PM, Sevick MA. Measuring adherence to behavioral and medical interventions. Control Clin Trials. 2000;21(5):S188–S194. 10.1016/S0197-2456(00)00077-5. [DOI] [PubMed] [Google Scholar]
- 47.Chae DH, Krieger N, Bennett GG, Lindsey JC, Stoddard AM, Barbeau EM. Implications of discrimination based on sexuality, gender, and race/ethnicity for psychological distress among working-class sexual minorities: the United for Health Study, 2003–2004. Int J Health Serv. 2010;40(4):589–608. 10.2190/HS.40.4.b. [DOI] [PubMed] [Google Scholar]
- 48.Krieger N Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30(12):1273–1281. 10.1016/0277-9536(90)90307-E. [DOI] [PubMed] [Google Scholar]
- 49.Krieger N Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv. 1999;29(2):295–352. 10.2190/M11WVWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- 50.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29(1):6–28. 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 51.Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity among adults in the United States—no statistically significant chance since 2003–2004. NCHS Data Brief. 2007;1:1–8. [PubMed] [Google Scholar]