Abstract
Background
This review is an update of the original Cochrane review published in July 2012. Missed appointments are a major cause of inefficiency in healthcare delivery with substantial monetary costs for the health system, leading to delays in diagnosis and appropriate treatment. Patients' forgetfulness is one of the main reasons for missed appointments. Patient reminders may help reduce missed appointments. Modes of communicating reminders for appointments to patients include face‐to‐face communication, postal messages, calls to landlines or mobile phones, and mobile phone messaging. Mobile phone messaging applications, such as Short Message Service (SMS) and Multimedia Message Service (MMS), could provide an important, inexpensive delivery medium for reminders for healthcare appointments.
Objectives
To update our review assessing the effects of mobile phone messaging reminders for attendance at healthcare appointments. Secondary objectives include assessment of costs; health outcomes; patients' and healthcare providers' evaluation of the intervention and perceptions of safety; and possible harms and adverse effects associated with the intervention.
Search methods
Original searches were run in June 2009. For this update, we searched the Cochrane Central Register of Controlled Trials (CENTRAL,The Cochrane Library 2012, Issue 8), MEDLINE (OvidSP) (January 1993 to August 2012), EMBASE (OvidSP) (January 1993 to August 2012), PsycINFO (OvidSP) (January 1993 to August 2012) and CINAHL (EbscoHOST) (January 1993 to August 2012). We also reviewed grey literature (including trial registers) and reference lists of articles.
Selection criteria
Randomised controlled trials (RCTs) assessing mobile phone messaging as reminders for healthcare appointments. We only included studies in which it was possible to assess effects of mobile phone messaging independent of other technologies or interventions.
Data collection and analysis
Two review authors independently assessed all studies against the inclusion criteria, with any disagreements resolved by a third review author. Study design features, characteristics of target populations, interventions and controls, and results data were extracted by two review authors and confirmed by a third author. Two authors assessed the risk of bias of the included studies. As the intervention characteristics and outcome measures were similar across included studies, we conducted a meta‐analysis to estimate an overall effect size.
Main results
We included eight randomised controlled trials involving 6615 participants. Four of these studies were newly identified during this update.
We found moderate quality evidence from seven studies (5841 participants) that mobile text message reminders improved the rate of attendance at healthcare appointments compared to no reminders (risk ratio (RR) 1.14 (95% confidence interval (CI) 1.03 to 1.26)). There was also moderate quality evidence from three studies (2509 participants) that mobile text message reminders had a similar impact to phone call reminders (RR 0.99 (95% CI 0.95 to 1.02). Low quality evidence from one study (291 participants) suggests that mobile text message reminders combined with postal reminders improved the rate of attendance at healthcare appointments compared to postal reminders alone (RR 1.10 (95% CI 1.02 to 1.19)). Overall, the attendance to appointment rates were 67.8% for the no reminders group, 78.6% for the mobile phone messaging reminders group and 80.3% for the phone call reminders group. One study reported generally that there were no adverse effects during the study period; none of the studies reported in detail on specific adverse events such as loss of privacy, data misinterpretation, or message delivery failure. Two studies reported that the costs per text message per attendance were respectively 55% and 65% lower than costs per phone call reminder. The studies included in the review did not report on health outcomes or people's perceptions of safety related to receiving reminders by text message.
Authors' conclusions
Low to moderate quality evidence included in this review shows that mobile phone text messaging reminders increase attendance at healthcare appointments compared to no reminders, or postal reminders.
Text messaging reminders were similar to telephone reminders in terms of their effect on attendance rates, and cost less than telephone reminders. However, the included studies were heterogeneous and the quality of the evidence therein is low to moderate. Further, there is a lack of information about health effects, adverse effects and harms, user evaluation of the intervention and user perceptions of its safety. The current evidence therefore still remains insufficient to conclusively inform policy decisions.
There is a need for more high‐quality randomised trials of mobile phone messaging reminders, that measure not only patients’ attendance rates, but also focus on the cost‐effectiveness of these interventions. Health outcomes, patients’ and healthcare providers’ evaluation and perceptions of the safety of the interventions, potential harms, and adverse effects of mobile phone messaging reminders should be assessed. Studies should report message content and timing in relation to the appointment.
Keywords: Humans, Appointments and Schedules, Cell Phone, Randomized Controlled Trials as Topic, Reminder Systems, Reminder Systems/economics, Text Messaging, Text Messaging/economics
Mobile phone messaging reminders for attendance at healthcare appointments
Failure to attend healthcare appointments impacts not only the health of the patients but also health system efficiency. In this review, an update of the original review published in July 2012, we assessed whether sending patients appointment reminders using mobile phone text messaging (Short Message Service (SMS) and Multimedia Message Service (MMS)) could improve attendance.
The review included eight randomised controlled trials published up to August 2012, involving 6615 participants. Four of these trials were newly included in this update. Low to moderate quality evidence included in this review shows that mobile phone text messaging reminders increase attendance at healthcare appointments compared to no reminders and postal reminders, and have the same impact on attendance as phone call reminders. Two studies reported that the costs per attendance of mobile phone text message reminders are less than phone call reminders.
One study reported generally that there were no adverse effects during the study period; none of the studies reported in detail on specific adverse events such as loss of privacy, data misinterpretation, or message delivery failure. The studies included in the review did not report on health outcomes or people's perceptions of safety related to receiving reminders by text message. Further randomised trials are needed to assess the effects of mobile phone messaging reminders for attendance at healthcare appointments.
Summary of findings
Summary of findings for the main comparison.
Mobile phone text message reminders compared to no reminders for patients with scheduled healthcare appointments
| Patient or population: Patients with healthcare appointments Settings: All settings (primary, hospital, community, outpatient) Intervention: Mobile phone text message reminders Comparison: No reminders | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| No reminders | Mobile phone text message reminders | ||||
| Attendance rate at healthcare appointments | 678 per 1000 | 773 per 1000 (698 to 854) |
RR 1.14 (1.03 to 1.26) |
5841 (7 studies) | ⊕⊕⊕⊝ moderatea,b |
| Other outcomes | None of the included studies reported on health outcomes, costs, user evaluation of the intervention, user perception of safety, potential harms or adverse effects of the intervention. | ||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
a Unclear risk of bias for several categories in the included studies. b In one study the unit of analysis was appointment rather than the individual participant which may have resulted in clustering of data.
Summary of findings 2.
Mobile phone message text reminders plus postal reminders compared to postal reminders alone for patients with scheduled healthcare appointments
| Patient or population: Patients with healthcare appointments Settings: All settings (primary, hospital, community, outpatient) Intervention: Mobile phone message text plus postal reminders Comparison: Postal reminders | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Postal reminders | Mobile phone message text plus postal reminders | ||||
| Attendance rate at healthcare appointments | 858 per 1000 | 944 per 1000 (875 to 1000) | RR 1.10 (1.02 to 1.19) | 291 (1 study) | ⊕⊕⊝⊝ lowa |
| Other outcomes | The included study did not report on health outcomes, costs, user evaluation of the intervention, user perception of safety, potential harms or adverse effects of the intervention. | ||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
aOnly one study included, with small number or participants. No information provided about the method of randomisation, allocation concealment, blinding and selective outcome reporting (unclear risk of bias). Low risk only for attrition bias.
Summary of findings 3.
Mobile phone message reminders compared to phone call reminders for patients with scheduled healthcare appointments
| Mobile phone message reminders compared to phone call reminders for patients with healthcare appointments | |||||
| Patient or population: patients with healthcare appointments Settings: all settings (primary, hospital, community, outpatient) Intervention: Mobile phone message reminders Comparison: phone call reminders | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Phone call reminders | Mobile phone message reminders | ||||
| Attendance rate at healthcare appointments | 803 per 1000 | 795 per 1000 (763 to 819) | RR 0.99 (0.95 to 1.02) | 2509 (3 studies) | ⊕⊕⊕⊝ moderatea,b |
| Costs | While the attendance rates after text messages versus phone reminders were similar, the costs per text message per attendance were 55% and 65% lower than costs per phone call reminder in two included studies. | ||||
| Adverse outcomes | One study reported that there were no adverse events during the study period. Two studies did not report on adverse events. | ||||
| Other outcomes | None of the included studies reported on health outcomes, user evaluation of the intervention or user perception of safety. | ||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
a Unclear risk of bias for several categories in the included studies. b In one study the unit of analysis was appointment rather than the individual participant which may have resulted in clustering of data.
Background
Most mobile phones provide Short Message Service (SMS), whereby up to 160 characters of text are sent from a mobile phone (or the Internet) to one or more mobile phones, and Multimedia Message Service (MMS) for similarly transmitting graphics, video or sound. In the two decades since the first basic text message was sent, these services, collectively known as mobile phone messaging (MPM), have become increasingly popular (Guardian 2012). Whilst initially mainly used by young adults, MPM has since developed into an important means of communication across all population groups, as the global mobile phone penetration rate has risen to 87%, with nearly 6 billion subscriptions by the end of 2011 (ITU 2012a). Globally, an estimated 8.6 trillion text messages are sent each year (Kelly 2012). A recent study by Ofcom found that in the United Kingdom (UK) text messaging has even overtaken speaking on a mobile phone and face‐to‐face contact as the most‐used method of daily communication between friends and family (Ofcom 2012). Although mobile phone coverage in lower‐income and middle‐income countries lags behind that of high‐income countries, by 2011 there were 78 mobile phone subscriptions per 100 inhabitants in developing countries (ITU 2012b).
Compared to other modes of communication, text messages have the advantage of instant transmission and low cost. There is also a smaller chance of messages being misplaced compared to print materials, and text messages are generally perceived as being less invasive to daily lives than phone calls (Kaplan 2006). Features such as ubiquity, mobility, direct and instantaneous access and direct communication offer the possibility of using mobile phones for health information transfer (Atun 2006). Several reviews of the literature on the use of mobile phones in health care have illustrated the wide application and potential of mobile phones to increase access to health care; enhance efficiency of service delivery; improve diagnosis, treatment and rehabilitation; and support public health programmes (Atun 2006; Car 2012; Free 2013a; Free 2013b). Mobile phone messaging has, for example, been used to provide appointment reminders (Bos 2005), to improve patient compliance with medications (Fairley 2003; Marquez Contreras 2004; Vilella 2004), to monitor chronic conditions (Ferrer‐Roca 2004; Kwon 2004; Ostojic 2005) and to provide psychological support (Bauer 2003; Franklin 2003). Mobile phones have also been used in managing communicable diseases and in health promotion programmes (e.g. in smoking cessation (Obermayer 2004; Rodgers 2005)). Furthermore, the use of mobile phones has been shown to improve service utilisation among population groups such as teenagers and young adult males who do not typically use health services, by providing the opportunity to remotely access care providers for advice (Atun 2006b). However, for older adults, some of whom are less able or willing to use mobile phones, the effect on service utilisation could be more limited (Atun 2006b). Other challenges in using mobile phone applications in health care include incomplete coverage of mobile networks, lack of standards, and possible information overload (Adler 2007).
Note that, whilst the terms text message, text, or txt are more commonly used in North America, the UK, Spain and the Philippines, in many other countries the term SMS is preferred. In this review we will use the term ‘text messaging’ when referring to the use of SMS only, distinguishing it from the term ‘mobile phone messaging’, which encompasses both SMS and MMS. Increasingly, the latter term also refers to mobile email and ‘instant messaging’ delivered to the mobile phone using mobile internet, but these types of communication are not considered in this review.
This review is an update of a review first published in 2012 (Car 2012) and complements a second updated review by the same authors that aims to assess the effectiveness of mobile phone messaging in supporting delivery of health care services (de Jongh in preparation).
Description of the condition
Missed appointments are a major cause of inefficiency in healthcare delivery, with substantial monetary costs to health systems; and delays in diagnosis and appropriate treatment for the non‐attending patient. In England's National Health System (NHS), over a one‐year period the direct costs alone were 185 million UK pounds for GP appointments, 34 million UK pounds for practice nurse appointments and estimated to be around 575 million UK pounds for hospital appointments (DoH 2004; DPP 2003). Economic incentives, such as imposing a fine on non‐attendees, could reduce non‐attendance rates, and this strategy has been suggested in Denmark and the UK (Bech 2005).
A number of reviews have assessed the factors leading to missed appointments (Deyo 1980; George 2003; Sharp 2001), in a range of country settings, including Canada, Denmark, Finland, Hong Kong, New Zealand, Norway, Saudi Arabia, Scotland, Singapore, Spain, UK, and the United States of America (USA). Studies have found differences in the appointment keeping behaviour of patients by demographic factors, such as age and gender (Hon 2002; Mantyjarvi 1994; Moore 2001; Simmons 1997; Skaret 1998; Waller 2000), race and ethnicity (Clarke 1998; Gatrad 1997; Gatrad 2000); and socio‐economic status, such as unemployment, perceived social support (Brown 1999; Catz 1999; Ramm 2001; Reekie 1998), lower levels of community functioning (Coodin 2004) and living in a deprived area (Neal 2001).
Detailed surveys among non‐attendees and their healthcare providers identify the main patient‐related factors for missing scheduled appointments as: health beliefs (Al Faris 2002; Mirotznik 1998); lack and difficulty of transportation (Campbell 2000; Collins 2003; Mohamed 2002; Paul 1997; Pesata 1999); scheduling problems (Campbell 2000; King 1995; Ross 1995); health status (Cashman 2004; Kane 1991; Killaspy 2000; Richardson 1998; van Baar 2006); resistance to consultation (Grunebaum 1996; Wogelius 2005); insurance status (Canizares 2002; Iben 2000; Majeroni 1996; Weingarten 1997; Yoon 2005); and frustration with outpatient clinic organisation resulting in long waiting times and discontinuity of care (van Baar 2006). Health system‐related factors include: inadequate communication between healthcare providers and patients (Bottomley 1994; Lloyd 1993; Martin 2005), which are worsened by patients missing appointments (Husain‐Gambles 2004); waiting times (Pesata 1999); quality of consultation; facilities in the waiting area (Chung 2004); time interval between scheduling/referrals and appointments (Grunebaum 1996; Hamilton 2002; Livianos‐Aldana 1999); administrative and/or clerical problems (Hull 2002; Potamitis 1994); and site of care (Lasser 2005; Specht 2004).
However, one of the most frequently cited reasons for missing an appointment is simply that patients forget that they had an appointment (Hong Kong (Hon 2005); Scotland (Herrick 1994; Hull 2002); Saudi Arabia (Mohamed 2002); UK (Murdock 2002; Neal 2005; Pal 1998; Potamitis 1994); Northern Ireland (Richardson 1998); Norway (Skaret 2000); Malaysia (Zailinawati 2006); USA (Carrion 1993)). Any form of reminders may thus decrease the rate of missed appointments, reducing the inefficiencies and costs generated by non‐attendance. Importantly, reminders give patients an opportunity to cancel an appointment either by a return mobile phone message or a phone call.
Description of the intervention
We identified seven possible modes of communicating reminders for healthcare appointments to patients: face‐to‐face, postal message, call to landline, call to mobile, via web‐based electronic health records, email and SMS/MMS. In Table 7 we outline basic characteristics and a comparison of these modes of communication. Existing literature on appointment reminders focuses on postal messages, phone calls, emails and text reminders.
Table 1.
Characteristics of communication modes
| Face‐to‐face | Postal Letter | Call to Landline | Call to Mobile | Web Based (Electronic Health Record) | SMS / MMS | ||
| Immediacy | Slow: Requires a visit to the provider | Slow: around 2 days | Immediate, if person is at home. Return call may be necessary. | Immediate, if person answers (more likely than landline). Return call may be necessary. | Immediate | Immediate or stored | Immediate or stored |
| Privacy and Confidentiality | High: Personal communication | High: Personally addressed | Low: Confidentiality prevents message being left as others may answer or retrieve it. | High: Personal device enables possibility of message being left. | Moderate: dependent on whether device is personal or public. | Moderate: dependent on whether device is personal or public. | High, if personal device. |
| Likelihood of misinterpretation | Low | Moderate | Low, as patient can request immediate clarification | Low, as patient can request immediate clarification | Moderate | Moderate | Moderate |
| Delivery confirmation possible | Not applicable | Yes, but only at significant expense | Unnecessary if call is answered. No, if message was left. | Unnecessary if call is answered. No, if message was left. | Not applicable | Yes | Yes |
| Cost | High | Moderate | Low | Moderate | Low | Low | Low |
How the intervention might work
Various communication channels such as phone calls, letters and text messages have been used for reminders that aim to reduce missed appointments. A study conducted in a Dutch orthodontic clinic did not find evidence that reminders reduced failed attendance rates. When given the choice, patients in this study preferred mail reminders to telephone and text message reminders. Some patients were also negative about the usefulness of reminders (Bos 2005). A systematic review on prompts to encourage attendance for people with serious mental illness concluded that prompts close to the time of appointment may increase attendance and that a simple orientation letter would be more effective than a telephone prompt (Reda 2010). A study which compared postal, manual telephone and automated telephone reminders (or all three combined) in a general dental practice in the UK found that all reminder methods resulted in net cost savings, and that both postal and manual telephone techniques were effective in improving attendance rates (Reekie 1998).
Benefits of using phone call reminders have also been reported in RCTs in adolescent and public health clinic settings in Australia and USA (Dini 1995; Hashim 2001; Sawyer 2002). Benefits of using postal reminders have been reported in RCTs in orthodontic clinic settings in the UK (Can 2003; Thomas 2004).
There are studies of the impact of text message reminders on missed appointments in the NHS (Milne 2006), in Australia (Downer 2005; Downer 2006) and in Malaysia (Leong 2006). A review of the use of text messaging in health care reported applications in imaging diagnostics, dermatology and sexual health clinics in the UK; outpatient clinics in the USA and Norway; and private dental and chiropractic clinics in Sweden (Atun 2006).
Acceptability and risks of the intervention
In some UK pilot programmes, confidentiality issues surrounding text‐messaging reminders have been addressed by an 'opt‐out' scheme, or information leaflets have acted as consent forms (Atun 2006). Another concern regarding text‐messaging reminders is their possible impact on health inequalities, as people in higher socio‐economic groups, who are more likely to own a mobile phone, will be less likely to miss appointments (Fahey 2003). However, this concern may not be realised, given mobile phone ownership statistics and other unpublished studies regarding mobile phone use and socio‐economic status (Ellenbogen 2003; Vernon 2003). Patients who receive text reminders may be more inclined to ignore other paper‐based communication, which may also include key information (Vodafone 2004).
Possible disadvantages of using mobile phone messaging include the risk of inaccurate data input (Norwell 2003), lack of understanding or misinterpretation of the information, and difficulties in reading for those with poor vision or problems with literacy.
Having correct patient contact information and securely stored health records are essential to adhere to privacy, confidentiality and data protection requirements. Failures or delays in message delivery are rare, but possible. However, harm is unlikely as senders are usually notified instantly in cases where there was a transmission problem. There may be additional monetary and time costs, as backup systems may be needed. Lastly, risks associated with mobile phone messaging in general may apply, for instance increased risk of car accidents as a result of messaging whilst driving (Owens 2011).
Why it is important to do this review
Although there is some evidence on the use and effectiveness of mobile phones in healthcare delivery, answers to questions regarding the implementation of mobile phone messaging technologies in routine care, such as their impact on patient‐related outcomes or on the processes of healthcare delivery, are unclear. Given the topical nature of mobile phone messaging we updated this review to identify answers to these questions and propose directions for future research. This review complements several parallel Cochrane reviews on mobile phone messaging for a range of other healthcare purposes (de Jongh 2012; Gurol‐Urganci 2012; Vodopivec‐Jamsek 2012), which are currently being updated (de Jongh in preparation).
Objectives
To assess the effects of mobile phone messaging reminders for attendance at healthcare appointments. Secondary objectives include assessment of costs; patients' and healthcare providers' evaluation of the intervention; and possible risks and harms associated with the intervention.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomised controlled trials (RCTs) in this review. (In the original version of this review (Car 2012) we had planned to also include quasi‐RCTs, controlled before and after studies, and interrupted time series, but none were identified; see Differences between protocol and review).
Types of participants
We included all study participants regardless of age, gender and ethnicity, as well as all types and stages of diseases. We included studies in all settings, i.e. primary care settings (services of primary health care), outpatient settings (outpatient clinics), community settings (public health services) and hospital settings. We did not exclude studies according to the type of healthcare provider (e.g. nurse, doctor, allied staff).
Types of interventions
We included interventions using SMS or MMS as reminders for healthcare appointments. The messaging needed to be between a healthcare provider (either in person or automated) and a patient. The review did not include reminders to people other than those who had an appointment.
We excluded studies in which SMS/MMS was part of a multifaceted intervention, as it would not be possible to separate the effects of messaging alone. SMS messages sent as reminders for routine drug collection for managing long‐term conditions were excluded from this review, but discussed in de Jongh 2012.
We aimed to make comparisons between mobile phone messaging and no intervention, as well as other modes of communication such as face‐to‐face, postal letters, calls to landline or mobile telephones, email or via electronic health records; and if applicable, automated versus personal text messaging.
Types of outcome measures
A number of processes and outcomes may be affected by mobile phone messaging interventions that aim to facilitate the communication between patients and healthcare providers.
Primary outcomes
Rate of attendance at healthcare appointments
Secondary outcomes
Health outcomes as a result of the intervention, including physiological measures, e.g. blood pressure; clinical assessments; biomarker values; self reporting of symptom resolution or quality of life;
Costs (direct and indirect) of the intervention;
User (patient, carer or healthcare provider) evaluation of the intervention, including satisfaction, readiness to use, timeliness, availability and/or convenience;
User (patient, carer or healthcare provider) perceptions of safety;
Potential harms or adverse effects of the intervention, such as misreading or misinterpretation of data, transmission of inaccurate data, loss of verbal and non‐verbal communication cues, issues of privacy and disclosure, or failure or delay in the message delivery.
Search methods for identification of studies
We used a common search strategy for this review and a parallel review (de Jongh in preparation) and allocated relevant studies to their respective reviews before assessing their risk of bias and extracting data. The studies reported in this review focused exclusively on the usefulness of mobile phone messaging as appointment reminders. The search strategies for each of the databases are given in Appendix 1 to Appendix 6.
Electronic searches
We restricted the searches to studies published since 1993 as the first commercial SMS message was sent in December 1992 (Wikipedia 2007). There were no language restrictions.
One review author (IGU) searched the following electronic databases on August 23, 2012:
The Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, issue 8 2012)
MEDLINE (OvidSP) (1993 to August 23, 2012)
EMBASE (OvidSP) (1993 to August 23, 2012)
PsycINFO (OvidSP) (1993 to August 23, 2012)
CINAHL (EbscoHOST) (1993 to August 23, 2012)
Searching other resources
We searched the following trials registers:
WHO Clinical Trial Search Portal (www.who.int/trialsearch);
Current Controlled Trials (www.controlled‐trials.com)
We searched the reference lists of included studies to identify additional studies. We contacted study authors for further information on their studies and to enquire whether they were aware of any other published or ongoing studies that would meet our inclusion criteria.
Data collection and analysis
Revised methods for the 2012‐13 update of this review (see Differences between protocol and review) were approved by the Cochrane Consumers and Communication Group before we commenced the new searches.
Selection of studies
The selection of studies was done by IGU, TdJ and VVJ. IGU and TdJ independently assessed the relevance of all titles and abstracts identified from the electronic searches. We retrieved full text copies of all articles judged to be potentially relevant from the titles and abstracts. TdJ and IGU independently assessed these articles for inclusion. TdJ checked the final list of included and excluded studies, and any disagreements were resolved by discussion with VVJ and JC. We also reviewed the reference lists of key publications. Where the description of the intervention was not sufficiently detailed to allow the review authors to judge whether it met the inclusion criteria, we contacted the study authors for further details.
Data extraction and management
We extracted the following data from the included studies, using a modified version of the Cochrane Consumers and Communication Review Group's data extraction template:
General information: title, authors, source, publication status, date published, language, review author information, date reviewed.
Setting: Geographic location, type of health care setting, type of healthcare providers
Study methods: study design, objectives, aims of intervention, methods of participant recruitment, inclusion/exclusion criteria, informed consent and ethical approval, funding, statistical methods, consumer involvement.
Risk of bias: see 'Assessment of risk of bias in included studies'.
Participants: description, number, age, gender, ethnicity, socioeconomic status distribution. If relevant: principal health problem or diagnosis, stage of illness, treatment received.
Interventions: description including technical specifications on SMS and handset provider, duration of intervention, frequency of delivery, message content, details of control/usual or routine care, co‐interventions.
Outcomes: primary and secondary outcomes as specified above, methods of assessing outcomes, follow up for non‐respondents, adverse events.
Results: all reported measurements for the primary and secondary outcomes, including multiple timings for measurements, subgroup analyses or results in different measurement scales if applicable.
TdJ and VVJ independently extracted the above data onto a standard form. The forms were then assessed by one review author (IGU) who checked these descriptive data. Any discrepancies between the two data extraction sheets were discussed by two review authors (TdJ and VVJ), and resolved jointly with the two other review authors (IGU and JC).
Assessment of risk of bias in included studies
We assessed the risk of bias of included studies in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) which recommends the explicit reporting of sequence generation, allocation concealment, blinding of participants, providers and outcome assessors, incomplete outcome data, selective outcome reporting and other sources of bias for RCTs.
Two review authors (TdJ and VVJ) independently assessed the risk of bias in the included studies, with any disagreements resolved by discussion and consensus of the team. We used a template to guide the assessment of risk of bias, and judged each domain as low risk, high risk or unclear risk of bias. We have presented the results of the 'Risk of bias' assessment in tables and a summary figure, and provided a narrative discussion of the risk of bias in individual domains.
We assessed the overall quality of the evidence using GRADEprofiler (GRADEpro) software. We considered study limitations, inconsistency of results, the indirectness of the evidence, imprecision or other considerations, and downgraded the quality where appropriate (Guyatt 2008).
Measures of treatment effect
We used risk ratios (RRs) as effect measures for dichotomous outcomes and standardised mean differences (SMDs) for continuous outcomes. RRs and SMDs have been derived from Manzel‐Haenszel and inverse variance methods respectively. We used a random‐effects model, where possible, to pool the results and reported confidence intervals with all measures of effect.
Unit of analysis issues
We noted the method of randomisation in each included trial, and considered additional issues regarding the assessment of risk of bias of cluster randomised trials as discussed in Chapter 16 of the Cochrane Handbook (Higgins 2011). In the case of repeated measurements, we defined several outcomes based on different periods of follow‐up and performed separate analyses for each outcome. In studies with more than two treatment groups, we made multiple pair‐wise comparisons between all possible pairs of intervention groups.
Dealing with missing data
We contacted the original investigators to request missing data. With incomplete outcome data (such as drop‐outs, loss to follow‐up and withdrawn study participants), we assessed and reported the risk of bias as high/unclear/low risk as guided by the Cochrane Handbook (Higgins 2011) and identified the numbers as well as the reasons for incomplete data. As the numbers and reasons for incomplete outcome data in included studies suggested that data were missing at random, we used only available data in the review and did not use imputation methods.
Assessment of heterogeneity
Statistical heterogeneity was examined by visual inspection of the forest plots as well as using the I2 statistic. We interpreted the amount of heterogeneity as low, moderate and high using I2 values of 25%, 50% and 75%, respectively (Higgins 2003). If there was high heterogeneity, we attempted to determine potential reasons for it by examining individual study characteristics. We combined the study results in a meta‐analysis only if there was no substantial clinical or methodological heterogeneity.
Assessment of reporting biases
We assessed reporting bias using funnel plots. The funnel plots, however, were not very informative due to the small number of studies included. Selective outcome reporting was assessed using the Cochrane 'Risk of bias' assessment tool.
Data synthesis
We conducted a meta‐analysis using Cochrane Review Manager (RevMan) software to calculate an overall effect size, comparing text message reminders with alternative modes of communicating reminders. We used a random‐effects model in the meta‐analysis of the calculated measures of effect as described in Measures of treatment effect.
Subgroup analysis and investigation of heterogeneity
No subgroup analyses were specified in the updated review methodology.
Sensitivity analysis
We undertook a sensitivity analysis to explore whether our main findings are robust to exclusion of outlying studies identified though assessment of heterogeneity.
We did not conduct the following sensitivity analyses due to the small number of studies included. We had aimed to explore the influence of the following factors on effect size:
excluding unpublished studies;
taking account of risk of bias of included studies, as specified above;
excluding any large studies to establish how they impact on the results.
Consumer participation
The draft review was circulated to consumers in The Cochrane Collaboration for comment. The original version of this review received comments from two consumers through the Cochrane Consumers and Communication Review Group's standard editorial process. We then also examined whether consumers were involved in the design and implementation of each included study. No additional consumer participation was sought during the update of this review.
Results
Description of studies
Results of the search
Our search (across both this review and de Jongh in preparation) identified 2876 unique citations. After initial screening of the titles for basic relevance to the reviews we retained 660 citations. We subsequently excluded 355 citations that, based on the abstract, showed insufficient relevance to the suite of reviews or evidently did not meet the stated study design criteria. After review of the full text of the remaining 129 citations (note: we were unable to retrieve 12 citations), plus an additional 25 citations that were identified through follow‐up on trial protocols and conference abstracts, we subsequently rejected a further 94 papers for failing to meet the inclusion criteria. After allocation of the selected papers across the two parallel reviews, we selected eight individual studies for inclusion in this review (Figure 1).
Figure 1.
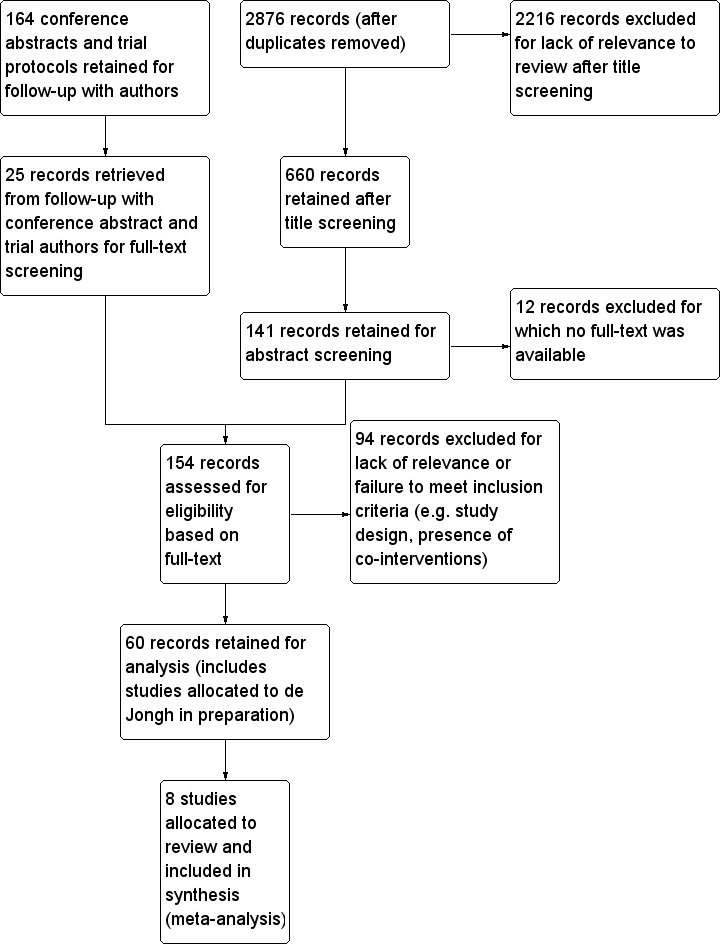
Study flow diagram. (Note: search strategy and screening selection is common for this review and for de Jongh in preparation until the final allocation stage).
Included studies
We included eight studies involving 6615 people in this review (Chen 2008; Fairhurst 2008; Koury 2005; Leong 2006; Liew 2009; Lin 2012; Odeny 2012; Taylor 2012). Four of these studies (Liew 2009; Lin 2012; Odeny 2012; Taylor 2012) were newly‐identified during this update. We present key characteristics of the included studies below and in the Characteristics of included studies table.
Of the 94 papers excluded in the final selection stage, only 4 had potential relevance to this particular review (the other 90 are potentially relevant to de Jongh in preparation). These have been listed in Characteristics of excluded studies, specifying the reasons for their exclusion. Six studies (Car 2008; Downer 2005; Geraghty 2008; Koshy 2008; Kruse 2009; Milne 2006) that were listed as excluded in the earlier version of this review (Car 2012) now do not appear in the List of Excluded Studies as the search and selection were repeated using a narrower study design criteria (see Differences between protocol and review). These studies were either not included in the search results or excluded from the review at an earlier stage of selection.
Methods
All of the eight included studies were RCTs. In seven studies the unit of randomisation was the individual participant (Chen 2008; Koury 2005; Leong 2006; Liew 2009; Lin 2012; Odeny 2012; Taylor 2012). In one study the unit of randomisation was the healthcare appointment (Fairhurst 2008)
All studies compared the effects of the text messaging intervention to usual practice. In seven studies the usual practice was no reminders (Chen 2008; Fairhurst 2008; Leong 2006; Liew 2009; Lin 2012; Odeny 2012; Taylor 2012). In one study (Koury 2005), the usual practice was to send postal reminders two weeks before appointments. Chen 2008, Leong 2006 and Liew 2009 had a second intervention arm and compared the effects of the text messaging intervention to phone call reminders. The sample sizes for the included studies ranged from 291 (Koury 2005) to 1848 participants (Chen 2008).
Participants
The studies were set in Australia (Taylor 2012), China (Chen 2008; Lin 2012), Scotland (Fairhurst 2008), England (Koury 2005), Kenya (Odeny 2012) and Malaysia (Leong 2006; Liew 2009). The settings were one hospital health promotion centre (Chen 2008), one inner‐city general practice (Fairhurst 2008), one ophthalmic centre (Lin 2012), two physical therapy departments (Taylor 2012), six ear, nose and throat (ENT) clinics within a hospital (Koury 2005), nine primary care clinics (seven in Leong 2006; two in Liew 2009) and 12 governmental health clinics (Odeny 2012).
The target group for the intervention varied. In seven of the studies, all the patients that required an appointment in the clinic or practice were eligible for the study, provided they had access to a mobile phone capable of receiving text messages and were able to read and understand those messages. In Fairhurst 2008, however, only participants with a history of two or more failed appointments within one year were eligible.
The participants' mean age ranged from 29 years in Odeny 2012 to 59 years in Liew 2009. Seven studies included both men and women, with the proportion of males ranging from 35% (Leong 2006) to 62% (Lin 2012). The study by Odeny 2012, however, targeted only men due to the nature of the appointment. Koury 2005 did not provide any information on the age and gender distribution of the participants.
Interventions
Purpose
The purpose of all interventions in the eight studies was to remind the participant of their upcoming healthcare appointment.
Specifications
The text messaging interventions were delivered using different platforms. In Fairhurst 2008, Koury 2005 and Odeny 2012 texts were sent using various web‐based platforms, and in Chen 2008 texts were sent automatically via a Global System for Mobile (GSM) modem linked to an electronic health records system. No information on the text messaging specifications was provided in Leong 2006,Liew 2009 and Lin 2012. In the study by Taylor 2012 one of the study sites sent messages manually, whereas the second site used an automated delivery system.
Six studies mention that the delivery of the messages was verified by 'message sent' prompts; in the study by Odeny 2012 the SMS software was not programmed to request delivery notifications, whereas Taylor 2012 does not specify whether any notification system was in place. Chen 2008 notes that as mobile phone numbers are changed frequently in China, the authors could not verify whether the message was delivered to the correct recipient.
Message content
Chen 2008 and Leong 2006 state that the text message reminders included the participant's name and appointment details, but do not provide the exact wording of the messages. The reminder in Fairhurst 2008 was "You have an appointment at (name of practice) (today/tomorrow) at (time). Please call (number) if you can't make it." Similarly, in Taylor 2012 the content read "Reminder: Physical therapy appointment at [site] on [day], [date] at [time]. Please call [number] ONLY if you cannot attend." The messages in Lin 2012 and Odeny 2012 elaborate on this form in that, in addition to a basic appointment reminder, they emphasise the importance of the appointment (Lin 2012: "Rigorous and regular follow‐up is essential to timely and successful management of childhood cataract.") or contain post‐operative instructions (Odeny 2012). It should be noted that in the latter study there was no fixed appointment; participants were simply asked to come to the clinic seven days after their procedure. Koury 2005 and Liew 2009 provided no information on message content.
Timing of the reminder
The text reminder was sent 24 hours before the appointment in Koury 2005, 24 to 48 hours before the appointment in Leong 2006 and Liew 2009, and 72 hours before the appointment in Chen 2008. In Fairhurst 2008, reminders were sent between 08:00 and 09:00 on the morning preceding afternoon appointments, and between 16:00 and 17:00 on the afternoon preceding morning appointments. Reminders for Monday morning appointments were sent in the afternoon of the preceding Friday. In Lin 2012 a total of four reminders per appointment was sent, namely at 10am and 4pm on one and four days before the date of the appointment. The reminder in Taylor 2012 was sent two days before the appointment, if it was booked more than three days in advance; otherwise it was sent on the day before the appointment. Participants in the study by Odeny 2012 received daily text messages. However, only the messages sent on days six and seven after the procedure contained the appointment reminder, corresponding to the day before the intended check‐up visit and the day of the visit itself respectively.
Outcomes
All studies reported (non‐)attendance rates at healthcare appointments as the primary outcome. Two studies (Chen 2008; Leong 2006) reported on the costs of the intervention. None of the included studies reported health outcomes, user perceptions of safety, or potential harms of the intervention.
Funding
Three studies were mainly funded by research funding from universities (Leong 2006; Liew 2009; Odeny 2012), and three by the participating hospital or healthcare organisations (Fairhurst 2008; Lin 2012; Taylor 2012). Two studies had additional research program support by governmental organisations including the National Institutes of Health (Odeny 2012) and the Chinese Ministry of Health (Lin 2012). Two studies did not specify their funding source (Chen 2008; Koury 2005).
Risk of bias in included studies
We have summarised the risk of bias in included studies in Figure 2 and in the Characteristics of included studies.
Figure 2.
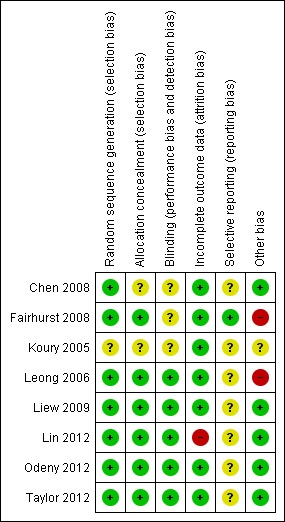
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Seven studies reported the use of adequate sequence generation methods (computer‐generated random allocation sequences or random number tables); one study did not specify the method of randomisation (Koury 2005). Six studies had adequate methods for concealing the allocation sequence (through use of sealed opaque envelopes or masked computer files, or because the person performing the allocation was not involved in recruitment of patients or delivery of the intervention); in two studies the method of allocation concealment was unclear (Chen 2008; Koury 2005).
In none of the studies was there blinding of participants, due to the nature of the intervention which requires overt interaction with the intervention. In the studies by Lin 2012 and Taylor 2012 it is explicitly stated that the outcome assessors and/or the researchers conducting the analysis were masked to allocation. In Leong 2006, the person who conducted the randomisation was not involved in participant recruitment and intervention delivery. No mention is made in other studies of blinding of outcome assessors or researchers and this could have potentially introduced a source of bias.
Because we did not have access to the original study protocols, we cannot fully judge whether there may have been any selective reporting of outcomes. In addition, only one included study reported adverse effects as an outcome (Fairhurst 2008). In all studies it was reported that the intervention and control groups were sufficiently comparable at baseline, although Koury 2005 does not provide any supporting data.
Although the time lapse between the reminder and the appointment could have had an effect on the outcome, none of the studies assessed this variable. In Fairhurst 2008, as the unit of analysis is the appointment rather than individual patient who may have more than one appointment in the study period, there is clustering of data. In Leong 2006, the effect size is likely to be underestimated as the definition of 'attendance' is restricted to attendance at the clinics on scheduled days. However, participants in this study were accustomed to walk‐in visits rather than scheduled visits and 48% of the participants actually attended the clinic, but on days other than the appointment dates.
Effects of interventions
See: Table 1; Table 2; Table 3
Attendance at healthcare appointments
Text message reminders improved the rate of attendance at healthcare appointments compared with no reminders (risk ratio (RR) 1.14; 95% confidence interval (CI) 1.03 to 1.26) (7 studies, 5841 participants) (Table 1; Analysis 1.1; Figure 3) and postal reminders (RR 1.10, 95% CI 1.02 to 1.19) (1 study, 291 participants) (Table 2; Analysis 2.1; Figure 4). It should be noted that the potential underestimation of the effect size in Leong 2006 (Risk of bias in included studies) could mean that also the overall effect may also be larger than apparent from the meta‐analysis result. Text messages and phone reminders, on the other hand, had similar effects on attendance (RR 0.99, 95% CI 0.95 to 1.02) (3 studies, 2509 participants) (Table 3; Analysis 3.1; Figure 5).
Analysis 1.1.
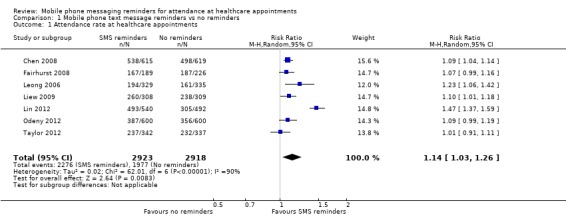
Comparison 1 Mobile phone text message reminders vs no reminders, Outcome 1 Attendance rate at healthcare appointments.
Figure 3.
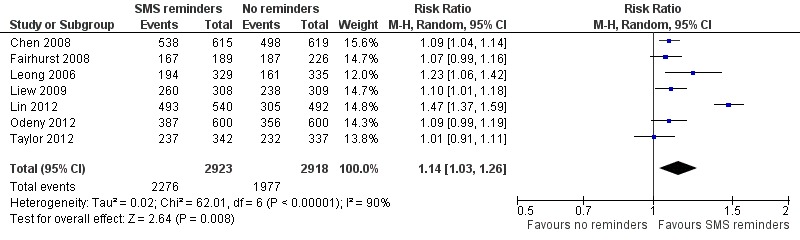
Forest plot of comparison: 1 Mobile phone text message reminders vs no reminders, outcome: 1.1 Attendance rate at healthcare appointments.
Analysis 2.1.
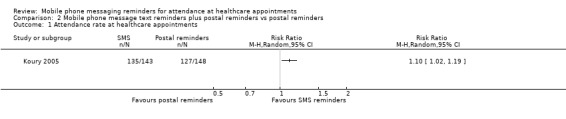
Comparison 2 Mobile phone message text reminders plus postal reminders vs postal reminders, Outcome 1 Attendance rate at healthcare appointments.
Figure 4.
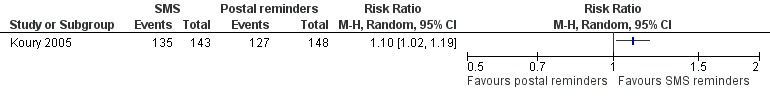
Forest plot of comparison: 2 Mobile phone message text reminders plus postal reminders vs postal reminders, outcome: 2.1 attendance rate of scheduled healthcare appointments.
Analysis 3.1.
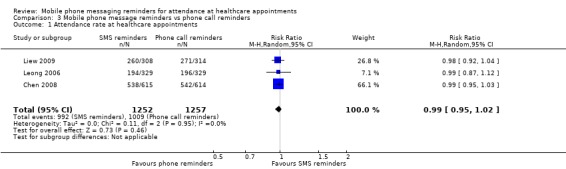
Comparison 3 Mobile phone message reminders vs phone call reminders, Outcome 1 Attendance rate at healthcare appointments.
Figure 5.
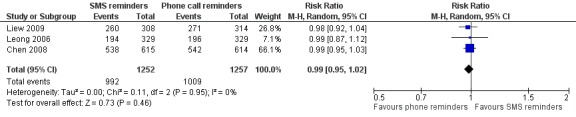
Forest plot of comparison: 3 Mobile phone message reminders vs phone call reminders, outcome: 3.1 Attendance rate at healthcare appointments.
There was high heterogeneity (I2 = 90%) in the comparison of text messaging and no reminders (Analysis 1.1; Figure 3). Investigation of the source of the heterogeneity revealed that the effect estimate of one study (Lin 2012) is clearly much larger than the other six studies. This might have been due to study characteristics, such as the higher number of reminders sent, message content and the involvement of parent‐child dyads. However, these differences were not sufficiently critical to justify the exclusion of the study from the main analysis. A sensitivity analysis without Lin 2012 also concluded that the text messages improved the attendance rate compared with no reminders, although the overall effect was smaller (RR 1.08, 95% CI 1.05 to 1.12, I2 = 5%) (Analysis 1.2).
Analysis 1.2.
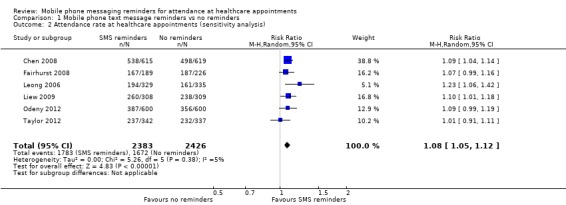
Comparison 1 Mobile phone text message reminders vs no reminders, Outcome 2 Attendance rate at healthcare appointments (sensitivity analysis).
Costs and cost‐effectiveness
Two studies measured the cost per unit of effective intervention of text message versus telephone reminder (Chen 2008; Leong 2006). While the attendance rates after text messages versus phone reminders were similar, the costs per text message were lower than costs per phone call reminder in both studies. The relative cost of the text message reminders per attendance was 55% and 65% of the cost of phone call reminders in Leong 2006 and Chen 2008, respectively (Table 8; Table 2).
Table 2.
Secondary outcomes data
| Study |
Costs and cost effectiveness (monetary unit as specified in the study) |
Participant evaluation of the intervention (as reported in the study) |
Potential harms or adverse effects of the intervention (as reported in the study) |
| Chen 2008 |
Cost per attendance: SMS group: 0.31 Yuan (4.7 GBP) Telephone group: 0.48 Yuan (7.3 GBP) Ratio of total cost per attendance: SMS group: 0.65 (relative to telephone group) |
Not reported | Not reported |
| Koury 2005 | Not reported | 98% willing to receive routine reminders of their appointments. Usefulness of the intervention:
|
Not reported |
| Leong 2006 |
Cost per attendance: SMS group: 0.45 RM (0.67 GBP) Mobile phone group: 0.82 RM (0.123 GBP) Ratio of total cost per attendance: SMS group: 0.55 (relative to mobile phone group) |
Not reported | No adverse events reported during the study period. |
| Lin 2012 | Not reported | 132 out of 135 (97.8%) reported they would like the intervention to continue | Not reported |
User evaluation of the intervention
One study reported the pre‐intervention acceptability of the intervention and found that 98% of patients were willing to receive routine mobile phone text message reminders of their outpatient appointments (Koury 2005; Table 8). One study reported on the post‐intervention acceptability of the intervention: 132 out of 135 patients (97.8%) reported that they would like the SMS programme to continue (Lin 2012).
Potential harms or adverse effects of the intervention
One study comparing the effects of mobile phone text message reminders to phone call reminders reported that there were no adverse effects during the study period (Fairhurst 2008), although there was no indication of what adverse events were considered in this study. None of the studies specifically reported events such as misreading or misinterpretation of data, transmission of inaccurate data, loss of verbal and non‐verbal communication cues, issues of privacy and disclosure, or failure or delay in the message delivery.
Other outcomes
None of the included studies reported health outcomes, or user perceptions of safety.
Discussion
Summary of main results
There is moderate and low quality evidence showing that mobile phone text message reminders increase healthcare appointment attendance rates when compared to no reminders and postal reminders, respectively (Table 1; Table 2). Further, we found moderate quality evidence that mobile phone text message reminders are as effective as phone call reminders (Table 3).
In the main analysis of seven studies of mobile phone text messaging reminders compared with no reminders, one of the studies included four reminder messages rather than one reminder, as in the other six studies. We therefore carried out a sensitivity analysis without this one study. Here the overall effect of the intervention was more robust (with significantly less heterogeneity) but was smaller than the overall effect of the seven included studies.
Two studies reported that mobile phone text message reminders are more cost‐effective than phone call reminders. We found very limited evidence about the potential adverse effects, or user evaluation. None of the included studies reported health outcomes, user perceptions of safety, or harms of the intervention. Overall, there is a need for more high‐quality research about the effects of mobile phone message reminders.
Overall completeness and applicability of evidence
We identified one study from Australia, one from Africa, two from Europe and three from Asia, thus covering low‐income (Kenya), middle‐income (China) and high‐income countries (UK, Australia). Overall, we found some, albeit limited, evidence in favour of text messaging for healthcare appointment reminders. However, as our review contains only a relatively small number of studies, it is difficult to assess to what extent these findings can be generalised.
None of the studies included in this review evaluated potential complications from text messaging such as loss or misinterpretation of data. No consideration was given to issues of security and confidentiality. Particularly in low‐income countries where mobile phones are frequently shared between family members, these are important confidentiality issues that need to be taken into account when designing interventions using SMS.
Quality of the evidence
The included studies were of varying methodological quality; most of them provided insufficient information to enable us to accurately assess the risk of bias. On the whole, sequence generation for randomisation was considered adequate (although the randomisation method was unclear in one study) but in two studies it was not clear whether, and how, the allocation was concealed. The lack of blinding of participants in all studies can be explained by the interactive nature of the text message interventions and is unavoidable. There is, however, a potential for bias due to the apparent lack of blinding of outcome assessors in most studies.
The overall quality of evidence in the comparison of text messaging with no reminders or phone call reminders was assessed as moderate as there was unclear risk of bias for several categories in the included studies and possible unit of analysis issues in one study. The overall quality of evidence in the comparison of text messaging plus postal reminders versus postal reminders only was low, as only one study was included and this study had a small number or participants and unclear risk of bias in all but one items.
Potential biases in the review process
We believe that we have identified all the studies concerning the use of mobile phone messaging reminders for attendance at healthcare appointments that met our study design criteria up to August 2012, as we utilised a comprehensive search strategy, independent assessment of study eligibility , and risk of bias, and independent data extraction. However, by excluding studies which had possible confounding from other communication and/or data transmission methods, we may have introduced selection bias towards less successful interventions, as it is conceivable that more complex interventions are more effective at improving attendance rates.
Agreements and disagreements with other studies or reviews
This review follows on from several other reviews that have analysed mobile phone messaging interventions. Fjeldsoe 2009 reviewed the evidence for behaviour change interventions delivered by SMS, whereas Krishna 2009 looked more broadly at healthcare delivery via mobile phones in the management and prevention of disease. However, neither of these studies looked at the effects of mobile phone messaging reminders for attendance at healthcare appointments.
Furthermore, two recent reviews focussed on mobile phone messaging reminders, either exclusively or in the context of a wider set of applications, both of which align closely with our review. The first, Guy 2012, looked at the effects of SMS reminders on clinic attendance. The authors identified 18 relevant studies, comprising eight RCTs and 10 controlled observational studies. After stratification for study design, Guy and colleagues found a summary effect from the RCTs of 1.48 (95% CI 1.23 to 1.72) in favour of SMS reminders compared to the controls. The second review, Free 2013b, looked more generally at mobile health technologies to improve healthcare service delivery processes. Free 2013b included four of the same studies as our review (Chen 2008; Fairhurst 2008; Leong 2006; Liew 2009), together with four studies that did not meet our inclusion criteria. Across these eight studies, an increased pooled effect was observed on appointment attendance from text message reminders versus no reminders, with an RR of 1.06 (95% CI 1.05 to 1.07), and a non‐significant increase was found in the pooled effect on the number of cancelled appointments (RR 1.08, 95% CI 0.89 to 1.30). There was no difference in attendance using SMS reminders versus other reminders (RR 0.98, 95% CI 0.94 to 1.02). The findings of both of these reviews are consistent with those presented here. This is largely due to the fact that all three reviews base most of their findings on the same small set of studies, although in our review we have applied more stringent inclusion criteria than the other two reviews. Nonetheless, our review indicates that the three most recent studies that we have included (Lin 2012; Odeny 2012; Taylor 2012), which were published after the study selections by Guy 2012 and Free 2013b were completed, have further strengthened the evidence of a positive effect from mobile phone messaging reminders on appointment attendance.
Authors' conclusions
This review identified eight randomised controlled trials involving 6615 people. The studies reported attendance rates (or non‐attendance in one case) and in two studies cost as the end point measures.
This review shows that mobile phone messaging reminders increase attendance at healthcare appointments when compared to no reminders or postal reminders. Text messaging reminders were similar to telephone reminders in terms of their effect on attendance rates, and were more cost‐effective than telephone reminders. However, the included studies were heterogeneous and the quality of the evidence therein is low to moderate, which makes the findings difficult to generalise. Further, there is a lack of information about health effects, adverse effects and harms, user evaluation of the intervention and user perceptions of its safety. The current evidence therefore still remains insufficient to conclusively inform policy decisions.
There is a need for more high‐quality randomised trials of mobile phone messaging reminders, that measure not only patients’ attendance rates, but also focus on the cost‐effectiveness of these interventions. Postal reminders are used rarely, therefore research could focus on the comparisons of no reminder or phone reminders with text messaging reminders. Health outcomes, patients’ and healthcare providers’ evaluation and perceptions of the safety of the interventions, potential harms, and adverse effects of mobile phone messaging reminders should be assessed. Studies should report message content and timing in relation to the appointment.
Acknowledgements
We acknowledge the very helpful support of the Cochrane Consumers and Communication Review Group editorial base in different stages of this review.
Appendices
Appendix 1. MEDLINE (Ovid) search strategy
cellular phone/
((cell* or mobile or wireless) adj (phone* or telephon*)).tw.
(cellphone* or mobiles or mhealth or m‐health).tw.
((mobile or handheld or hand‐held) adj2 (device* or technolog* or app* or health*)).tw.
(smart phone* or smartphone* or blackberry or iphone* or android phone* or google android or ipod touch or personal digital assistant* or pda or pdas).tw.
or/1‐5
(text* or messag* or multimedia or multi‐media or imag* or mms or data or input* or application* or app?).tw.
6 and 7
text messaging/
((text or short or multimedia or multi‐media) adj1 messag*).tw.
sms.tw.
(texting* or texted or texter*).tw.
(mms and (multimedia or multi‐media or messag*)).mp.
or/8‐13
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized.ab.
placebo.ab.
drug therapy.fs.
randomly.ab.
trial.ab.
groups.ab.
or/15‐22
exp animals/ not humans.sh.
23 not 24
14 and 25
limit 26 to yr="1993 ‐ 2012"
Appendix 2. EMBASE (Ovid) search strategy
mobile phone/
((cell* or mobile or wireless) adj (phone* or telephon*)).ti,ab,kw
(cellphone* or mobiles or mhealth or m‐health).ti,ab,kw
((mobile or handheld or hand‐held) adj2 (device* or technolog* or app* or health*)).ti,ab,kw
personal digital assistant/
(smart phone* or smartphone* or blackberry or iphone* or android phone* or google android or ipod touch or personal digital assistant* or pda or pdas).ti,ab,kw.
or/1‐6
(text* or messag* or multimedia or multi‐media or imag* or mms or data or input* or application* or app?).ti,ab,kw.
7 and 8
text messaging/
((text or short or multimedia or multi‐media) adj1 messag*).ti,ab,kw.
sms.ti,ab,kw.
(texting* or texted or texter*).ti,ab,kw.
(mms and (multimedia or multi‐media or messag*)).mp.
or/9‐14
randomized controlled trial/
controlled clinical trial/
single blind procedure/ or double blind procedure/
crossover procedure/
random*.tw.
placebo*.tw.
((singl* or doubl*) adj (blind* or mask*)).tw.
(crossover or cross over or factorial* or latin square).tw.
(assign* or allocat* or volunteer*).tw.
or/16‐24
15 and 25
limit 26 to yr="1993 ‐ 2012"
Appendix 3. PsycINFO (Ovid) search strategy
cellular phones/
((cell* or mobile or wireless) adj (phone* or telephon*)).ti,ab,id.
(cellphone* or mobiles or mhealth or m‐health).ti,ab,hw,id.
((mobile or handheld or hand‐held) adj2 (device* or technolog* or app* or health*)).ti,ab,hw,id.
mobile devices/
(smart phone* or smartphone* or blackberry or iphone* or android phone* or google android or ipod touch or personal digital assistant* or pda or pdas).ti,ab,hw,id.
or/1‐6
(text* or messag* or multimedia or multi‐media or imag* or mms or data or input* or application* or app?).ti,ab,hw,id.
7 and 8
((text or short or multimedia or multi‐media) adj1 messag*).ti,ab,id.
sms.ti,ab,id.
(texting* or texted or texter*).ti,ab,id.
(mms and (multimedia or multi‐media or messag*)).ti,ab,hw,id.
or/9‐13
random*.ti,ab,hw,id.
trial*.ti,ab,hw,id.
controlled stud*.ti,ab,hw,id.
placebo*.ti,ab,hw,id.
((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)).ti,ab,hw,id.
(cross over or crossover or factorial* or latin square).ti,ab,hw,id.
(assign* or allocat* or volunteer*).ti,ab,hw,id.
treatment effectiveness evaluation/
mental health program evaluation/
exp experimental design/
"2000".md.
or/15‐25
14 and 26
limit 27 to yr="1993 ‐ 2012"
Appendix 4. CENTRAL search strategy
#1 ((cell* or mobile or wireless) next (phone* or telephon* or communication)):ti,ab,kw
#2 ((mobile or handheld or hand‐held) near/2 (device or technology or app or apps or health*)):ti,ab,kw
#3 (cellphone or mhealth or m‐health or smart‐phone or smartphone or blackberry or iphone or android‐phone or google‐android or ipod‐touch or personal‐digital‐assistant or pda or pdas):ti,ab,kw
#4 ((text or short or multimedia or multi‐media) next messag*):ti,ab,kw
#5 (texting* or texted or texter or sms or mms):ti,ab,kw
#6 (#1 OR #2 OR #3 OR #4 OR #5)
Appendix 5. CINAHL (EBSCO) search strategy
| S19 | S17 and S18 |
| S18 | EM 199301‐ |
| S17 | S6 and S16 |
| S16 | S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 |
| S15 | TI (singl* or doubl* or tripl* or trebl*) and TI (blind* or mask*) |
| S14 | AB (singl* or doubl* or tripl* or trebl*) and AB (blind* or mask*) |
| S13 | AB (random* or trial or placebo*) or TI (random* or trial or placebo*) |
| S12 | MH Quantitative Studies |
| S11 | MH Placebos |
| S10 | MH Random Assignment |
| S9 | MH Clinical Trials+ |
| S8 | PT Clinical Trial |
| S7 | PT randomized controlled trial |
| S6 | S1 or S2 or S3 or S4 or S5 |
| S5 | ((text or short or multimedia or "multi‐media") N1 messag*) or texting* or texted or texter* or sms or mms |
| S4 | cellphone* or mobiles or mhealth or "m‐health" or "smart phone*" or smartphone* or blackberry or iphone* or "android phone*" or "google android" or "ipod touch" or "personal digital assistant*" or pda or pdas |
| S3 | (mobile or handheld or "hand‐held") N1 (device* or technolog* or app or apps or health*) |
| S2 | (cell* or mobile or wireless) N1 (phone* or telephon*) |
| S1 | MH Wireless Communications |
Appendix 6. Search Strategy for Trial portals
“cellular phone” OR “mobile phone” OR cellular telephone* OR mobile telephone* OR text messag* OR texting OR texted OR short messag* OR multimedia messag* OR sms OR mms
Data and analyses
Comparison 1.
Mobile phone text message reminders vs no reminders
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Attendance rate at healthcare appointments | 7 | 5841 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.03, 1.26] |
| 2 Attendance rate at healthcare appointments (sensitivity analysis) | 6 | 4809 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [1.05, 1.12] |
Comparison 2.
Mobile phone message text reminders plus postal reminders vs postal reminders
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Attendance rate at healthcare appointments | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 3.
Mobile phone message reminders vs phone call reminders
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Attendance rate at healthcare appointments | 3 | 2509 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.95, 1.02] |
What's new
| Date | Event | Description |
|---|---|---|
| 28 February 2013 | New citation required but conclusions have not changed | Four new studies were added to the review (Liew 2009; Lin 2012; Odeny 2012; Taylor 2012), increasing the total number of included trials from four to eight (from 3547 to 6615 participants). The overall conclusions were, however, unaffected by this expansion of the evidence base. |
| 28 February 2013 | Amended | The author order was revised to better reflect respective contributions to the updated version of the review. |
| 23 August 2012 | New search has been performed | Searches were updated in August 2012. Minor changes were made to the search strategies and review methods, with agreement from the Cochrane Consumers and Communication Review Group. Specifically, these were:
|
Differences between protocol and review
Changes between the protocol (Car 2008b) and the original review (Car 2012):
We were not able to search the following databases we had listed in the protocol (Car 2008b):
Proceedings from the MEDNET Congresses: We could not access the proceedings.
TrialsCentralTM (www.trialscentral.org): The website for the database was not functional and did not allow for the search of clinical trials.
African Trials Register: The trials in the African Trials Register are collected with a search strategy using the Cochrane Controlled Trials Register and the African Health Anthology (AHA). As we searched both original sources, it was not necessary to access the African Trials Register separately.
Health Star: The database ceased to exist as of December 2000, with all peer‐reviewed journal articles transferred to PubMed.
Changes between the original (Car 2012) and the updated review:
Compared to the first version of this review (Car 2012) several changes have been made to the methodology. These changes were approved by the editors of the Cochrane Consumers and Communication Review Group before the update was conducted. Specifically, we have made the following changes:
We excluded the LILACS and African Health Anthology databases from our search, as these proved very difficult to search and produced no studies of interest to the initial review that were not also retrieved from other, included databases;
We no longer included the following study designs: quasi‐randomised controlled trials (QRCTs), controlled before and after studies (CBAs), and interrupted time series (ITS) with at least three time points before and after the intervention, because the original review found no such studies that met the criteria for inclusion;
We reorganised the data extraction sheet to group specific data under different headings, but maintaining all relevant fields, to enable a better overview;
We no longer aimed to conduct subgroup analysis for different age categories as the original review indicated that very few studies stratified outcomes by age;
We no longer aimed to conduct sensitivity analysis to check for the effects of publication language or source of funding as the original review found only a few studies published in languages other than English and source of funding did not appear to be relevant factor;
In the original review, study results were not combined in a meta‐analysis if there was substantial clinical, methodological or statistical heterogeneity. In the updated review, however, we have conducted a meta‐analysis of all combined results, despite significant statistical heterogeneity. Instead, we have addressed the issue of heterogeneity by also performing a sensitivity analysis of the results, with exclusion of the outlying study.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: randomised controlled trial (from April to May 2007) | |
| Participants | China, Hospital Health Promotion Centre. 1891 adults (mean age 50.6 years, 57.6% male) who had scheduled appointments within 72 hours to 2 months from recruitment. 32 adults who failed to provide telephone numbers were excluded. | |
| Interventions | SMS group: Participants received text message reminders delivered through a mobile phone SMS, 72 hrs before appointment. The SMS was automatically sent through GSM model linked to the electronic health record system. The text message included participant's name and appointment details. Telephone group: Participants were called by the office medical assistants from the health promotion centre, 72 hrs before appointment. A maximum of three reminders were attempted in the telephone group. If the phone was unanswered, the participant would be called on their mobile phone number. Call content was the same as the SMS content. Control group: No reminders. |
|
| Outcomes | Attendance rate at the healthcare appointment. Costs of reminders. |
|
| Funding | Not specified | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information of blinding of researchers was provided. Blinding of participants was not possible due to the nature of the intervention, but this is unlikely to have influenced outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 11 participants could not be contacted by telephone or SMS as they changed their numbers or there was incorrect recording of the phone numbers by the medical assistant. The numbers of those lost‐to‐follow up are small in comparison to sample size. |
| Selective reporting (reporting bias) | Unclear risk | Protocol is not available, however, the number of possible outcomes seems restricted to those reported. |
| Other bias | Low risk | Control and intervention groups were similar at baseline for age and gender. No other apparent source of bias was identified. |
| Methods | Study design: randomised controlled trial (from August 2004 to February 2005). | |
| Participants | Scotland. Inner city general practice. 415 appointments made by 173 participants who had failed to attend two or more routine appointments in the preceding year. Same day appointments and participants with no mobile phones numbers were excluded. | |
| Interventions | SMS group: Participants received text message reminders delivered through a mobile phone SMS. The text message was sent between 8:00‐9:00 on the morning preceding afternoon appointments, and between 16:00‐17:00 on the afternoon preceding morning appointments. Texts were sent from a PC using www.vodafone.net. Control group: No reminders. |
|
| Outcomes | Non‐attendance rate. | |
| Funding | This study was funded by the Lothian and Borders Primary Care Research Network. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random sequence of labels. The randomisation sequence was based on a table of random numbers. |
| Allocation concealment (selection bias) | Low risk | "[S]ealed opaque numbered envelopes. One of two trained designated receptionists randomised each appointment by sequentially opening the sealed envelopes and allocating the appointment to the intervention group or the control group as indicated. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information of blinding of researchers was provided. Blinding of participants was not possible due to the nature of the intervention, but this is unlikely to have influenced outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Three appointments had to be excluded due to incorrect recording of the appointment date. 25 out of 191 text messages in the intervention group were not successfully delivered. |
| Selective reporting (reporting bias) | Low risk | Protocol is available and the study's pre‐specified outcomes have been reported. |
| Other bias | High risk | Groups were comparable at baseline for age and gender. However, as the unit of analysis is the appointment rather than the individual participant, who may have more than one appointment in the study period, there is potential clustering of data. |
| Methods | Study design: randomised controlled trial (from November 2003 to June 2004). | |
| Participants | UK. Six randomly‐selected ear, nose and throat (ENT) clinics in one district general hospital. 441 participants who were scheduled to attend the selected clinics were eligible. Participants who could not be contacted by telephone, who were not familiar with SMS and those not wishing to participate in the study were excluded. 291 participants were included in the study. | |
| Interventions | SMS group: All participants received postal reminders two weeks before appointment. Intervention group also received text message reminders 24 hours before appointment. Texts were sent through a web‐based provider. Control group: Postal reminder two weeks before appointment only. |
|
| Outcomes | Attendance rate; Proportion of participants willing to be contacted by SMS (before the intervention). | |
| Funding | Not specified. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on the method of randomisation was provided. |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment was provided. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information of blinding of researchers was provided. Blinding of participants was not possible due to the nature of the intervention, but this is unlikely to have influenced outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no loss to follow up. |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available, however the number of possible outcomes seems restricted to those reported. |
| Other bias | Unclear risk | The authors state that the groups were comparable at baseline on age and gender, although no data are provided to support this. |
| Methods | Study design: randomised controlled trial (between April and October 2005). | |
| Participants | Malaysia. Seven primary care clinics. 993 participants whose follow‐up appointments fell between 48 hours to 3 months from recruitment date. Either the patients or their caregivers had to have a mobile phone with text messaging function. | |
| Interventions | SMS group: Participants received text message reminders delivered through a mobile phone SMS, 24 to 48 hrs before appointment. The text message included participant's name and appointment details. Mobile phone group: Participants were called 24 to 48 hrs before appointment. A maximum of three reminders was attempted in the intervention groups. Call content was the same as the SMS content. Control group: No reminders. |
|
| Outcomes | Attendance rate at the healthcare appointment. Costs of reminders. |
|
| Funding | This research was funded via an unrestricted grant from the International Medical University, Malaysia. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation method using software. |
| Allocation concealment (selection bias) | Low risk | The researcher who did the randomisation was said to be not involved in patient recruitment or delivery of the intervention. The method of allocation concealment is not stated. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Research assistants were blinded to the intervention. Participants could not be blinded due to the nature of the intervention, but this is unlikely to have influenced outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Between 9 to 11 participants in each group did not receive the allocated intervention due to incorrect assignments by researchers. They were included in the intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Unclear risk | Protocol is not available, however, the number of possible outcomes seems restricted to those reported. |
| Other bias | High risk | The groups are comparable on age, gender, income, reason for follow‐up, and whether the participant is the patient or the caregiver. However, the definition of 'attendance' is strict, being attendance at the clinics on scheduled days, whereas participants in the study were not accustomed to healthcare appointments but rather walk‐in visits; Consequently, 48% of the participants actually visited the clinic on days other than the appointment dates. |
| Methods | Study design: randomised controlled trial (study dates not reported). | |
| Participants | Malaysia. Two primary care clinics. 931 participants with chronic diseases such as diabetes, asthma, hypertension, dyslipidaemia, and coronary artery disease with a scheduled return appointment between 1 and 6 months. Ownership of a mobile phone by the patient or an accompanying person who would be able to contact the patient was required. | |
| Interventions | SMS group: Participants received a standard text message reminder 24 to 48 hours before the scheduled appointment. Telephone reminder: Participants received a reminder call 24 to 48 hours before the scheduled appointment. If the contact was unsuccessful, up to three further attempts were made at 4‐hourly intervals. Control group: No reminders. |
|
| Outcomes | Non‐attendance rate, defined as the rate of those who did not attend, attended early, or attended late without rescheduling their appointment. | |
| Funding | This study was made possible with research funding from University of Malaya (reference F0381/2005C) and University Kebangsaan Malaysia (reference FF‐225‐2005). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation by computer, using a block size of three units. |
| Allocation concealment (selection bias) | Low risk | Assignment of participants was done by computer using a list of anonymous identification codes. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | The recruiters who enrolled the research subjects were blinded to the intervention at the time of recruitment. Study subjects could not be blinded due to the nature of the intervention, but this is unlikely to have influenced outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attendance rates were calculated based on intention‐to‐treat principle. |
| Selective reporting (reporting bias) | Unclear risk | Protocol is not available. However, the number of possible outcomes seems restricted to those reported. |
| Other bias | Low risk | Control and intervention groups were similar at baseline for age, gender, chronic disease, mobile phone ownership. However, in the control group more patients (78.0%) owned a mobile telephone than in the intervention groups (telephone 67.2%; text messaging 68.5%). No other apparent sources of bias were identified. |
| Methods | Study design: randomised controlled trial (from December 2010 until end of 2011). | |
| Participants | China. Zhongshan Ophthalmic Center, Guangzhou. 258 parent–child pairs involved in the Childhood Cataract Programme of the Chinese Ministry of Health. Parent–child pairs were eligible if: 1) the child was diagnosed as having congenital or development cataract, regardless of treatment status; and 2) the parents owned a mobile phone and could use the free mobile service used in this study. Children with as‐yet‐unoperated cataract and with previous cataract surgery with or without placement of intraocular lenses were all eligible to take part. Illiterate parents were eligible if assisted by a literate partner. Children were ineligible if they showed other ocular abnormalities. If intraocular pressure could not be controlled within 1 week after surgery, children were withdrawn from the study and referred to the Center's glaucoma department. | |
| Interventions | SMS group: Participants received 4 SMS reminders per appointment, i.e. at 10am and 4pm on 1 and 4 days before the date of the appointment. Appointments were once every month before surgery and at 1 week, 1 month, 2 months and 3 months post surgery (then every 3 months). The reminder read (in Chinese): "This is a reminder of the appointment for routine ophthalmic examination of your child at Zhongshan Ophthalmic Center at [time] on [date]. Rigorous and regular follow‐up is essential to timely and successful management of childhood cataract. Please make your preparations in advance and be on time." Control group: Participants in the control group received standard care, without any appointment reminders. |
|
| Outcomes | Primary outcome: Attendance rate. Secondary outcomes: Additional procedures (surgeries, laser treatments, or changes in eyeglass prescription); occurrence of secondary ocular hypertension. |
|
| Funding | Funded by the Key Projects for Hospital Clinical Disciplines of Ministry of Health of China in 2010‐2012 and partly by Fundamental Research Funds of State Key Laboratory of Ophthalmology. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Written allocation assignments were sealed in individual opaque envelopes marked only with study identification numbers. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Regular ocular examinations and analyses were performed by investigators and clinical staff, both masked to group allocation. Study participants and the study personnel in charge of randomization and sending the SMS could not be masked, because the intervention required overt participation. However, this is unlikely to have influenced outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The rate of non‐attendance at the visit at 3 months after surgery, and thus the percentage of patients lost to follow‐up, was high in both the intervention (17%) and control (67%) group. This percentage is particularly high in the control group, therefore it was not possible to state whether the intervention improved outcomes significantly. |
| Selective reporting (reporting bias) | Unclear risk | Protocol is not available. However, the number of possible primary outcomes seems restricted to those reported. Some secondary outcomes were reported, for which it could not be judged whether these were subject to undue selection. |
| Other bias | Low risk | Treatment and control groups were comparable at baseline for gender, residence status, parent's education, travel cost, number of children per household, and cataract history. No other sources of bias were identified. |
| Methods | Study design: randomised controlled trial (from September 2010 until April 2011). | |
| Participants | Kenya. 12 public health clinics. Participants were 1200 adult men who were in need of follow‐up care after circumcision. Included were men aged 18 or older who had undergone circumcision on the day of screening. Participants needed to be in possession of a mobile phone at the time of enrolment, and be able and willing to respond to a questionnaire administered by phone 42 days after circumcision. | |
| Interventions | SMS group: For the first seven days after circumcision, participants in the intervention group were sent daily text messages with post‐operative instructions and asking them to visit the clinic at seven days post‐procedure. Control group: Participants in the control group received standard care, but no text messages. |
|
| Outcomes | Attendance at the seven‐day post‐operative clinic visit, that is: within 3 days before or after the scheduled 7‐day visit. | |
| Funding | Funded by the University of Washington International AIDS Research and Training Program, which is supported by the Fogarty International Center (NIH 5D43‐TW000007). Additional support for the trial was provided by the Department of Epidemiology and Biostatistics at the University of Illinois at Chicago; and the Biostatistics and International Cores of the University of Washington Center for AIDS Research, an NIH funded program (P30 AI027757) which is supported by the following NIH Institutes and Centers (NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NIA). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done using a computer‐generated block randomisation scheme with variable blocks of size 4 to16. Randomisation was stratified by clinic. |
| Allocation concealment (selection bias) | Low risk | "A biostatistician in Seattle, who was not involved in any other aspect of study implementation, developed the randomization sequence [...] Investigators and study staff were blinded to the block number, block size, and sequence in the block. Individual participant randomization envelopes were shipped from Seattle to Kisumu, while the key to intervention assignments was retained in Seattle. Participants were assigned to intervention arms using pre‐prepared sequentially numbered, sealed, opaque envelopes containing group assignment. Study staff issued the next envelope in the series." |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Because of the nature of the intervention, it was not possible to mask participants to group assignments. However, clinicians and nurses performing the circumcision procedure and follow‐up were not aware of study group assignment." It is unlikely that the lack of blinding of participants would have influenced outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The primary analysis followed the intention‐to‐treat principle and was unadjusted. 12 (1%) participants whose clinic records could not be located after an extensive search were considered lost to follow‐up. Sensitivity analyses were performed in which the 12 men with missing clinic records were considered as failures to return. |
| Selective reporting (reporting bias) | Unclear risk | Protocol is not available. However, the number of possible outcomes seems restricted to those reported. |
| Other bias | Low risk | There were minor differences in the proportions of men reporting zero versus one partner in the past month in the intervention versus control arms. However, the proportion reporting multiple partners was similar. Other baseline characteristics were similar in both study arms. |
| Methods | Study design: randomised controlled trial (study dates not reported). | |
| Participants | Australia. 2 physical therapy outpatient departments. 679 patients in need of physical therapy. Participants were included if they had an appointment in a physical therapy outpatient clinic at 1 of the participating clinics and provided a mobile telephone number on which they could be contacted. Participants were excluded if they had an appointment scheduled on the same day on which they made the appointment or if they already had participated in the project by being allocated for a previous appointment during the trial. | |
| Interventions | SMS group: Participants were sent an SMS reminder 2 days before their appointment if it was made more than 3 days in advance, or the day before the appointment if it was made within 2 days. The content of the SMS reminder was “Reminder: Physical therapy appointment at [site] on [day], [date] at [time]. Please call [number] ONLY if you cannot attend.” Control group: Participants received no appointment reminders. |
|
| Outcomes | Non‐attendance rate, defined as the number of scheduled appointments not attended as a proportion of the total number of scheduled appointments. | |
| Funding | The trial was funded by the participating hospitals. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was prepared by an independent researcher using random number tables stratified for site in permuted blocks of 10. |
| Allocation concealment (selection bias) | Low risk | Group allocation was concealed in a computer file. An administration assistant opened the pre‐prepared computer file and selected the next participant in sequence, revealing their allocation by changing the text colour in the cell from white to black. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Data were retrieved in a blinded manner (i.e. without reference to group allocation) by a member of the research team by using the hospital’s data management system or were recorded manually by outpatient physical therapists at the time of the next scheduled appointment. Treating physical therapists were blinded to group allocation." Participants could not be blinded due to the nature of the intervention, but this is unlikely to have influenced outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Numbers of those lost to follow‐up or excluded from analysis were comparable across the different study arms. All data were analysed according to intention‐to‐treat principles. |
| Selective reporting (reporting bias) | Unclear risk | Protocol is not available. However, the list of reported outcomes seems comprehensive. |
| Other bias | Low risk | Intervention and control groups were comparable on all assessed demographic variables. No other sources of bias were identified. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bos 2005 | Study design: cohort study. |
| Bourne 2011 | Study design: no randomisation. |
| Fischer 2012 | Study design: cohort study. |
| Fung 2012 | Study underpowered: intervention group of n = 2. |
| Steenhoff 2012 | Outcome data for visit adherence not presented. |
Contributions of authors
Ipek Gurol‐Urganci developed the protocols and was involved in both the original version of this review and the 2013 update. She has led the updated search process and participated in screening the papers. She collected, analysed, interpreted the data and participated in writing the review.
Thyra de Jongh was involved in the original version of this review and has led the 2013 update. This includes the screening and quality appraisal processes for the studies, as well as the data extraction and management. She has collected, analysed and interpreted the data and participated in writing the review.
Vlasta Vodopivec Jamsek helped develop the protocols. For the 2013 update of this review she has been involved in data extraction and has contributed to writing the review.
Rifat Atun provided strategic guidance in all stages of the study and contributed to writing of the review.
Josip Car conceived the review together with Rifat Atun and has played a coordinating role in all stages of the study. He contributed to writing the review.
Sources of support
Internal sources
-
eHealth Unit, Department of Primary Care and Social Medicine, Imperial College, UK.
salaries, office space
-
Centre for Health Management, Tanaka Business School, Imperial College, UK.
salaries, office space
-
Department of Family Medicine, Faculty of Medicine, University of Ljubljana, Slovenia.
salaries, office space
-
London School of Hygiene and Tropical Medicine, UK.
salaries, office space
External sources
No sources of support supplied
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
- Chen ZW, Fang LZ, Chen LY, Dai HL. Comparison of an SMS text messaging and phone reminder to improve attendance at a health promotion center: A randomized controlled trial. Journal of Zhejiang University: Science B 2008;9(1):34‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairhurst K, Sheikh A. Texting appointment reminders to repeated non‐attenders in primary care: randomised controlled study. Quality and Safety in Health Care 2008;17(5):373‐6. [DOI] [PubMed] [Google Scholar]
- Koury E, Faris C. Mobile phones and clinic appointments: the start of a beautiful new friendship?. British Journal of Healthcare Computing & Information Management 2005;22(8):18‐20. [Google Scholar]
- Leong KC, Chen WS, Leong KW, Mastura I, Mimi O, Sheikh MA, et al. The use of text messaging to improve attendance in primary care: a randomized controlled trial. Family Practice 2006;23(6):699‐705. [DOI] [PubMed] [Google Scholar]
- Liew SM, Tong SF, Lee VK, Ng CJ, Leong KC, Teng CL. Text messaging reminders to reduce non‐attendance in chronic disease follow‐up: a clinical trial. The British Journal of General Practice 2009;59(569):916‐20. [PUBMED: 19712544] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H, Chen W, Luo L, Congdon N, Zhang X, Zhong X, et al. Effectiveness of a short message reminder in increasing compliance with pediatric cataract treatment: a randomized trial. Ophthalmology 2012;119(12):2463‐70. [PUBMED: 22921386] [DOI] [PubMed] [Google Scholar]
- Odeny TA, Bailey RC, Bukusi EA, Simoni JM, Tapia KA, Yuhas K, et al. Text messaging to improve attendance at post‐operative clinic visits after adult male circumcision for HIV prevention: a randomized controlled trial. PloS One 2012;7(9):e43832. [PUBMED: 22957034] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor NF, Bottrell J, Lawler K, Benjamin D. Mobile telephone short message service reminders can reduce nonattendance in physical therapy outpatient clinics: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2012;93(1):21‐6. [PUBMED: 22000821] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Bos A, Hoogstraten J, Prahl‐Andersen B. Failed appointments in an orthodontic clinic. American Journal of Orthodontics and Dentofacial Orthopedics 2005;127(3):355‐7. [DOI] [PubMed] [Google Scholar]
- Bourne C, Knight V, Guy R, Wand H, Lu H, McNulty A. Short message service reminder intervention doubles sexually transmitted infection/HIV re‐testing rates among men who have sex with men. Sexually Transmitted Infections 2011;87(3):229‐31. [DOI: 10.1136; PUBMED: 21296796] [DOI] [PubMed] [Google Scholar]
- Fischer HH, Moore SL, Ginosar D, Davidson AJ, Rice‐Peterson CM, Durfee MJ, et al. Care by cell phone: text messaging for chronic disease management. American Journal of Managed Care 2012;18(2):e42‐e57. [PubMed] [Google Scholar]
- Fung MK, Briggs B, Frascoia A, Petrov‐Kondatov V, Rivard S, Thai P, et al. The effects of text message reminder on blood donor show rate. The University of Vermont College of Medicine (Poster)2012.
- Steenhoff AP, Thompson J, Gabaitiri L, Cary MS, Steele KT, Mayisela S, et al. A pilot study of cellular phone SMS reminders to improve HIV visit and medication adherence at Independence Surgery Clinic, Gaborone, Botswana. Botswana‐UPenn Partnership (poster)2012.
Additional references
- Adler R. Health Care Unplugged: The Evolving Role of Wireless Technology. Oakland: California Health Care Foundation, 2007. [Google Scholar]
- Al Faris EA, Abdulghani HM, Mahdi AH, Salih MA, Al Kordi AG. Compliance with appointments and medications in a pediatric neurology clinic at a University Hospital in Riyadh, Saudi Arabia. Saudi Medical Journal 2002;23(8):969‐74. [PubMed] [Google Scholar]
- Atun RA, Sittampalam S. A review of the characteristics and benefits of SMS in delivering healthcare. In: Atun RA editor(s). The role of mobile phones in increasing accessibility and efficiency in healthcare. Vodafone Group Plc, 2006. [Google Scholar]
- Atun RA, Gurol‐Urganci I. Analysis of calls to NHS Direct. In: Atun RA editor(s). The role of mobile phones in increasing accessibility and efficiency in healthcare. Vodafone Group Plc., 2006. [Google Scholar]
- Bauer S, Percevic R, Okon E, Meermann R, Kordy H. Use of text messaging in the aftercare of patients with bulimia nervosa. European Eating Disorders Review 2003;11(3):279‐90. [Google Scholar]
- Bech M. The economics of non‐attendance and the expected effect of charging a fine on non‐attendees. Health Policy 2005;74(2):181‐91. [DOI] [PubMed] [Google Scholar]
- Bottomley WW, Cotterill JA. An audit of the factors involved in new patient non‐attendance in a dermatology out‐patient department. Clinical and Experimental Dermatology 1994;19(5):399‐400. [DOI] [PubMed] [Google Scholar]
- Brown KA, Shetty V, Delrahim S, Belin T, Leathers R. Correlates of missed appointments in orofacial injury patients. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 1999;87(4):405‐10. [DOI] [PubMed] [Google Scholar]
- Campbell JD, Chez RA, Queen T, Barcelo A, Patron E. The no‐show rate in a high‐risk obstetric clinic. Journal of Women's Health & Gender‐Based Medicine 2000;9(8):891‐5. [DOI] [PubMed] [Google Scholar]
- Can S, Macfarlane T, O'Brien KD. The use of postal reminders to reduce non‐attendance at an orthodontic clinic: A randomised controlled trial. British Dental Journal 2003;195(4):199‐201. [DOI] [PubMed] [Google Scholar]
- Canizares MJ, Penneys NS. The incidence of nonattendance at an urgent care dermatology clinic. Journal of the American Academy of Dermatology 2002;46(3):457‐9. [DOI] [PubMed] [Google Scholar]
- Car J, Ng C, Atun R, Card A. SMS text message healthcare appointment reminders in England. Journal of Ambulatory Care Management 2008;31(3):216‐9. [DOI] [PubMed] [Google Scholar]
- Carrion PG, Swann A, Kellert‐Cecil H, Barber M. Compliance with clinic attendance by outpatients with schizophrenia. Hospital and Community Psychiatry 1993;44(8):764‐7. [DOI] [PubMed] [Google Scholar]
- Cashman SB, Savageau JA, Lemay CA, Ferguson W. Patient health status and appointment keeping in an urban community health center. Journal of Healthcare for the Poor and Underserved 2004;15(3):474‐88. [DOI] [PubMed] [Google Scholar]
- Catz SL, McClure JB, Jones GN, Brantley PJ. Predictors of outpatient medical appointment attendance among persons with HIV. AIDS Care 1999;11(3):361‐73. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Chung JW, Wong TK, Yeung AC. Non‐attendance at an orthopaedic and trauma specialist outpatient department of a regional hospital. Journal of Nursing Management 2004;12(5):362‐7. [DOI] [PubMed] [Google Scholar]
- Clarke EA, Notghi A, Harding LK. Counting the cost of patients who do not attend nuclear medicine departments. Nuclear Medicine Communications 1998;19(3):193‐7. [DOI] [PubMed] [Google Scholar]
- Collins J, Santamaria N, Clayton L. Why outpatients fail to attend their scheduled appointments: a prospective comparison of differences between attenders and non‐attenders. Australian Health Review 2003;26(1):52‐63. [DOI] [PubMed] [Google Scholar]
- Coodin S, Staley D, Cortens B, Desrochers R, McLandress S. Patient factors associated with missed appointments in persons with schizophrenia. Canadian Journal of Psychiatry 2004;49(2):145‐8. [DOI] [PubMed] [Google Scholar]
- Jongh T, Gurol‐Urganci I, Vodopivec‐Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self‐management of long‐term illnesses. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD007459] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongh T, Gurol‐Urganci I, Vodopivec‐Jamsek V, Car J, Atun R, Javad S. Mobile phone messaging for preventing and managing disease. Cochrane Database of Systematic Reviews 2013, Issue [in preparation]. [Google Scholar]
- Deyo RA, Inui TS. Dropouts and broken appointments. A literature review and agenda for future research. Medical Care 1980;18(11):1146‐57. [DOI] [PubMed] [Google Scholar]
- Dini EF, Linkins RW, Chaney M. Effectiveness of computer‐generated telephone messages in increasing clinic visits. Archives of Pediatrics and Adolescent Medicine 1995;149(8):902‐5. [DOI] [PubMed] [Google Scholar]
- Department of Health. Missed appointments guidance. GP Bulletin2004, issue 33.
- Downer SR, Meara JG, Costa AC. Use of SMS text messaging to improve outpatient attendance. Medical Journal of Australia 2005;183(7):366‐8. [PUBMED: 16201955] [DOI] [PubMed] [Google Scholar]
- Downer SR, Meara JG, Costa AC, Sethuraman K. SMS text messaging improves outpatient attendance. Australian Health Review 2006;30(3):389‐96. [PUBMED: 16879098] [DOI] [PubMed] [Google Scholar]
- DPP. DPP: Developing Patient Partnerships. www.dpp.org.uk2003.
- Ellenbogen J. Preference for text message reminders may be greatest in lower socio‐economic groups. BMJ 2003;327:564‐e. [Google Scholar]
- Fahey D. Reminding patients by text message: text reminders could lead to increased health inequalities. BMJ 2003;327(7414):564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairley CK, Levy R, Rayner CR, Allardice K, Costello K, Thomas C. Randomized trial of an adherence programme for clients with HIV. International Journal of STD & AIDS 2003;14(12):805‐9. [DOI] [PubMed] [Google Scholar]
- Ferrer‐Roca O, Cardenas A, Diaz‐Cardama A, Pulido P. Mobile phone text messaging in the management of diabetes. Journal of Telemedicine and Telecare 2004;10(5):282‐5. [DOI] [PubMed] [Google Scholar]
- Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short‐message service. American Journal of Preventive Medicine 2009;36(2):165‐73. [DOI] [PubMed] [Google Scholar]
- Franklin V, Waller A, Pagliari C, Greene S. "Sweet Talk": text messaging support for intensive insulin therapy for young people with diabetes. Diabetes Technology & Therapeutics 2003;5(6):991‐6. [DOI] [PubMed] [Google Scholar]
- Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The effectiveness of mobile‐health technology‐based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Medicine 2013;10(1):e1001362. [DOI: 10.1371/journal.pmed.1001362] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile‐health technologies to improve health care service delivery processes: a systematic review and meta‐analysis. PLoS Medicine 2013;10(1):e1001363. [DOI: 10.1371/journal.pmed.1001363] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatrad AR. Comparison of Asian and English non‐attenders at a hospital outpatient department. Archives of Disease in Childhood 1997;77(5):423‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatrad AR. A completed audit to reduce hospital outpatients non‐attendance rates. Archives of Disease in Childhood 2000;82(1):59‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George A, Rubin G. Non‐attendance in general practice: a systematic review and its implications for access to primary health care. Family Practice 2003;20(2):178‐84. [DOI] [PubMed] [Google Scholar]
- Geraghty M, Glynn F, Amin M, Kinsella J. Patient mobile telephone 'text' reminder: A novel way to reduce non‐attendance at the ENT out‐patient clinic. Journal of Laryngology and Otology 2008;122(3):296‐8. [DOI] [PubMed] [Google Scholar]
- Grunebaum M, Luber P, Callahan M, Leon AC, Olfson M, Portera L. Predictors of missed appointments for psychiatric consultations in a primary care clinic. Psychiatric Services 1996;47(8):848‐52. [DOI] [PubMed] [Google Scholar]
- McVeigh, T. Text messaging turns 20. http://www.guardian.co.uk/technology/2012/dec/01/text‐messaging‐20‐years?CMP=twt_gu. The Guardian, 1 December 2012.
- Gurol‐Urganci I, Jongh T, Vodopivec‐Jamsek V, Car J, Atun R. Mobile phone messaging for communicating results of medical investigations. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD007456.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy R, Hocking J, Wand H, Stott S, Ali H, Kaldor J. How effective are short message service reminders at increasing clinic attendance? A meta‐analysis and systematic review. Health Services Research 2012;47(2):614‐32. [DOI: 10.1111/j.1475-6773.2011.01342.x] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y. Rating quality of evidence and strength of recommendations GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton W, Round A, Sharp D. Patient, hospital, and general practitioner characteristics associated with non‐attendance: a cohort study. British Journal of General Practice 2002;52(477):317‐9. [PMC free article] [PubMed] [Google Scholar]
- Hashim MJ, Franks P, Fiscella K. Effectiveness of telephone reminders in improving rate of appointments kept at an outpatient clinic: a randomized controlled trial. Journal of the American Board of Family Medicine 2001;14(3):193‐6. [PubMed] [Google Scholar]
- Herrick J, Gilhooly ML, Geddes DA. Non‐attendance at periodontal clinics: forgetting and administrative failure. Journal of Dentistry 1994;22(5):307‐9. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 [updated March 2011]. The Cochrane Collaboration. Available from www.cochrane‐handbook.org, 2011. [Google Scholar]
- Hon KL, Leung TF, Ma KC. Issues regarding nonattendance at a paediatric dermatology centre. Clinical and Experimental Dermatology 2002;27(8):711‐3. [DOI] [PubMed] [Google Scholar]
- Hon KL, Leung TF, Wong Y, Ma KC, Fok TF. Reasons for new referral non‐attendance at a pediatric dermatology center: a telephone survey. Journal of Dermatological Treatment 2005;16(2):113‐6. [DOI] [PubMed] [Google Scholar]
- Hull AM, Alexander DA, Morrison F, McKinnon JS. A waste of time: non‐attendance at out‐patient clinics in a Scottish NHS Trust. Health Bulletin 2002;60(1):62‐9. [PubMed] [Google Scholar]
- Husain‐Gambles M, Neal RD, Dempsey O, Lawlor DA, Hodgson J. Missed appointments in primary care: questionnaire and focus group study of health professionals. British Journal of General Practice 2004;54(499):108‐13. [PMC free article] [PubMed] [Google Scholar]
- Iben P, Kanellis MJ, Warren J. Appointment‐keeping behavior of Medicaid‐enrolled pediatric dental patients in eastern Iowa. Pediatric Dentistry 2000;22(4):325‐9. [PubMed] [Google Scholar]
- International Telecommunications Union. Key statistical highlights: ITU data release June 2012. http://www.itu.int/ITU‐D/ict/statistics/material/pdf/2011%20Statistical%20highlights_June_2012.pdf2012.
- ITU. Key Global Telecom Indicators for the World Telecommunication Service Sector. http://www.itu.int/ITU‐D/ict/statistics/at_glance/keytelecom.html Accessed 18 Jan 2013.
- Kane K. Non‐attendance for appointments in an out‐patients' x‐ray department. Radiography Today 1991;57(653):15‐9. [PubMed] [Google Scholar]
- Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries?. Global Health 2006 May 23;2:9. [PUBMED: 16719925] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly H. OMG, the text message turns 20. But has SMS peaked?. http://edition.cnn.com/2012/12/03/tech/mobile/sms‐text‐message‐20/index.html Accessed 18 Jan 2013.
- Killaspy H, Banerjee S, King M, Lloyd M. Prospective controlled study of psychiatric out‐patient non‐attendance. Characteristics and outcome. British Journal of Psychiatry 2000;176:160‐5. [DOI] [PubMed] [Google Scholar]
- King A, David D, Jones HS, O'Brien C. Factors affecting non‐attendance in an ophthalmic outpatient department. Journal of the Royal Society of Medicine 1995;88(2):88‐90. [PMC free article] [PubMed] [Google Scholar]
- Koshy E, Car J, Majeed A. Effectiveness of mobile‐phone short message service (SMS) reminders for ophthalmology outpatient appointments: Observational study. BMC Ophthalmology 2008;8(9):‐. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemedicine and e‐Health 2009;15(3):231‐40. [PUBMED: 19382860] [DOI] [PubMed] [Google Scholar]
- Kruse LV, Hansen LG, Olesen C. [Non‐attendance at a pediatric outpatient clinic. SMS text messaging improves attendance]. Ugeskr Laeger 2009;171(17):1372‐5. [PubMed] [Google Scholar]
- Kwon HS, Cho JH, Kim HS, Lee JH, Song BR, Oh JA, et al. Development of web‐based diabetic patient management system using short message service (SMS). Diabetes Research and Clinical Practice 2004;66 Suppl 1:S133‐7. [DOI] [PubMed] [Google Scholar]
- Lasser KE, Mintzer IL, Lambert A, Cabral H, Bor DH. Missed appointment rates in primary care: the importance of site of care. Journal of Health Care for the Poor and Underserved 2005;16(3):475‐86. [DOI] [PubMed] [Google Scholar]
- Livianos‐Aldana L, Vila‐Gomez M, Rojo‐Moreno L, Luengo‐Lopez MA. Patients who miss initial appointments in community psychiatry? A Spanish community analysis. International Journal of Social Psychiatry 1999;45(3):198‐206. [DOI] [PubMed] [Google Scholar]
- Lloyd M, Bradford C, Webb S. Non‐attendance at outpatient clinics: is it related to the referral process?. Family Practice 1993;10(2):111‐7. [DOI] [PubMed] [Google Scholar]
- Majeroni BA, Cowan T, Osborne J, Graham RP. Missed appointments and Medicaid managed care. Archives of Family Medicine 1996;5(9):507‐11. [DOI] [PubMed] [Google Scholar]
- Mantyjarvi M. No‐show patients in an ophthalmological out‐patient department. Acta Ophthalmologica Scandinavica 1994;72(3):284‐9. [DOI] [PubMed] [Google Scholar]
- Marquez Contreras E, Figuera von Wichmann M, Gil‐Guillen V, Ylla‐Catala A, Figueras M, Balana M, et al. [Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA‐Alert)]. Atencion Primaria 2004;34(8):399‐405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin C, Perfect T, Mantle G. Non‐attendance in primary care: the views of patients and practices on its causes, impact and solutions. Family Practice 2005;22(6):638‐43. [DOI] [PubMed] [Google Scholar]
- Milne RG, Horne M, Torsney B. SMS reminders in the UK national health service: an evaluation of its impact on "no‐shows" at hospital out‐patient clinics. Health Care Management Review 2006;31(2):130‐6. [DOI] [PubMed] [Google Scholar]
- Mirotznik J, Ginzler E, Zagon G, Baptiste A. Using the health belief model to explain clinic appointment‐keeping for the management of a chronic disease condition. Journal of Community Health 1998;23(3):195‐210. [DOI] [PubMed] [Google Scholar]
- Mohamed BA, Al Doghaither AH. Missed appointments at public hospitals in Riyadh, Saudi Arabia. Saudi Medical Journal 2002;23(4):388‐92. [PubMed] [Google Scholar]
- Moore CG, Wilson‐Witherspoon P, Probst JC. Time and money: effects of no‐shows at a family practice residency clinic. Family Medicine 2001;33(7):522‐7. [PubMed] [Google Scholar]
- Murdock A, Rodgers C, Lindsay H, Tham TC. Why do patients not keep their appointments? Prospective study in a gastroenterology outpatient clinic. Journal of the Royal Society of Medicine 2002;95(6):284‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neal RD, Lawlor DA, Allgar V, Colledge M, Ali S, Hassey A, et al. Missed appointments in general practice: retrospective data analysis from four practices. British Journal of General Practice 2001;51(471):830‐2. [PMC free article] [PubMed] [Google Scholar]
- Neal RD, Hussain‐Gambles M, Allgar VL, Lawlor DA, Dempsey O. Reasons for and consequences of missed appointments in general practice in the UK: questionnaire survey and prospective review of medical records. BMC Family Practice 2005;6:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norwell N. Text messaging raises medicolegal issues. BMJ 2003;326(7399):1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obermayer JL, Riley WT, Jean‐Mary J. College smoking‐cessation using cell phone text messaging. Journal of American College Health 2004;53(2):71‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Ofcom. The Communications Market 2012. http://stakeholders.ofcom.org.uk/market‐data‐research/market‐data/communications‐market‐reports/cmr12/ 18 July 2012.
- Ostojic V, Cvoriscec B, Ostojic SB, Reznikoff D, Stipic‐Markovic A, Tudjman Z. Improving asthma control through telemedicine: a study of short‐message service. Telemedicine Journal and e‐Health 2005;11(1):28‐35. [DOI] [PubMed] [Google Scholar]
- Owens JM, McLaughlin SB, Sudweeks J. Driver performance while text messaging using handheld and in‐vehicle systems. Accident; Analysis and Prevention 2011;43(3):939‐47. [PUBMED: 21376886] [DOI] [PubMed] [Google Scholar]
- Pal B, Taberner DA, Readman LP, Jones P. Why do outpatients fail to keep their clinic appointments? Results from a survey and recommended remedial actions. International Journal of Clinical Practice 1998;52(6):436‐7. [PubMed] [Google Scholar]
- Paul J, Hanna JB. Applying the marketing concept in health care: the no‐show problem. Health Marketing Quarterly 1997;14(3):3‐17. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Pesata V, Pallija G, Webb AA. A descriptive study of missed appointments: families' perceptions of barriers to care. Journal of Pediatric Health Care 1999;13(4):178‐82. [DOI] [PubMed] [Google Scholar]
- Potamitis T, Chell PB, Jones HS, Murray PI. Non‐attendance at ophthalmology outpatient clinics. Journal of the Royal Society of Medicine 1994;87(10):591‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramm C, Robinson S, Sharpe N. Factors determining non‐attendance at a cardiac rehabilitation programme following myocardial infarction. The New Zealand Medical Journal 2001;114(1132):227‐9. [PubMed] [Google Scholar]
- Reda S, Makhoul S. Prompts to encourage appointment attendance for people with serious mental illness. Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD002085] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reekie D, Devlin H. Preventing failed appointments in general dental practice: a comparison of reminder methods. British Dental Journal 1998;185(9):472‐4. [DOI] [PubMed] [Google Scholar]
- Richardson A. Failed appointments in an academic orthodontic clinic. British Dental Journal 1998;184(12):612‐5. [DOI] [PubMed] [Google Scholar]
- Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin RB, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tobacco Control 2005;14(4):255‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross JD, McIver A, Blakely A, Dalrymple J, Peacock W, Wallis C. Why do patients default from follow‐up at a genitourinary clinic?: a multivariate analysis. Genitourinary Medicine 1995;71(6):393‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer SM, Zalan A, Bond LM. Telephone reminders improve adolescent clinic attendance: a randomized controlled trial. Journal of Paediatrics and Child Health 2002;38(1):79‐83. [DOI] [PubMed] [Google Scholar]
- Sharp DJ, Hamilton W. Non‐attendance at general practices and outpatient clinics. BMJ 2001;323(7321):1081‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons AV, Atkinson K, Atkinson P, Crosse B. Failure of patients to attend a medical outpatient clinic. Journal of the Royal College of Physicians of London 1997;31(1):70‐3. [PMC free article] [PubMed] [Google Scholar]
- Skaret E, Raadal M, Kvale G, Berg E. Missed and cancelled appointments among 12‐18‐year‐olds in the Norwegian Public Dental Service. European Journal of Oral Sciences 1998;106(6):1006‐12. [DOI] [PubMed] [Google Scholar]
- Skaret E, Raadal M, Kvale G, Berg E. Factors related to missed and cancelled dental appointments among adolescents in Norway. European Journal of Oral Sciences 2000;108(3):175‐83. [DOI] [PubMed] [Google Scholar]
- Specht EM, Powell KR, Dormo CA. Factors affecting missed appointment rates for pediatric patients insured by medicaid in a traditional hospital‐based resident clinic and hospital‐owned practice settings. Clinical Pediatrics 2004;43(8):749‐52. [DOI] [PubMed] [Google Scholar]
- Thomas D. Postal reminders can improve attendance at orthodontic clinics. Evidence‐Based Dentistry 2004;5(1):14. [DOI] [PubMed] [Google Scholar]
- Baar JD, Joosten H, Car J, Freeman GK, Partridge MR, Weel C, et al. Understanding reasons for asthma outpatient (non)‐attendance and exploring the role of telephone and e‐consulting in facilitating access to care: exploratory qualitative study. Quality and Safety in Health Care 2006;15(3):191‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernon S. Families in poor socio‐economic areas and mobile phones. BMJ 2003;327:564. [Google Scholar]
- Vilella A, Bayas JM, Diaz MT, Guinovart C, Diez C, Simo D, et al. The role of mobile phones in improving vaccination rates in travelers. Preventive Medicine 2004;38(4):503‐9. [DOI] [PubMed] [Google Scholar]
- Vodafone text message pilot evaluation. Homerton University Hospital, NHS Foundation Trust.2004.
- Vodopivec‐Jamsek V, Jongh T, Gurol‐Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD007457] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller J, Hodgkin P. Defaulters in general practice: who are they and what can be done about them?. Family Practice 2000;17(3):252‐3. [DOI] [PubMed] [Google Scholar]
- Weingarten N, Meyer DL, Schneid JA. Failed appointments in residency practices: who misses them and what providers are most affected?. Journal of the American Board of Family Practice 1997;10(6):407‐11. [PubMed] [Google Scholar]
- Wikipedia. Short Message Service. http://en.wikipedia.org/wiki/Short_message_service(accessed February 2007).
- Wogelius P, Poulsen S. Associations between dental anxiety, dental treatment due to toothache, and missed dental appointments among six to eight‐year‐old Danish children: a cross‐sectional study. Acta Odontologica Scandinavica 2005;63(3):179‐82. [DOI] [PubMed] [Google Scholar]
- Yoon EY, Davis MM, Cleave J, Maheshwari S, Cabana MD. Factors associated with non‐attendance at pediatric subspecialty asthma clinics. Journal of Asthma 2005;42(7):555‐9. [DOI] [PubMed] [Google Scholar]
- Zailinawati AH, Ng CJ, Nik‐Sherina H. Why do patients with chronic illnesses fail to keep their appointments? A telephone interview. Asia‐Pacific Journal of Public Health 2006;18(1):10‐5. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Car J, Gurol‐Urganci I, Jongh T, Vodopivec‐Jamsek V, Atun R. Mobile phone messaging reminders for attendance at scheduled healthcare appointments. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD007458] [DOI] [Google Scholar]
- Car J, Gurol‐Urganci I, Jongh T, Vodopivec‐Jamsek V, Atun R. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD007458.pub2] [DOI] [PubMed] [Google Scholar]


