Abstract
Background
Office work has changed considerably over the previous couple of decades and has become sedentary in nature. Physical inactivity at workplaces and particularly increased sitting has been linked to increase in cardiovascular disease, obesity and overall mortality.
Objectives
To evaluate the effects of workplace interventions to reduce sitting at work compared to no intervention or alternative interventions.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, CINAHL, OSH UPDATE, PsycINFO, Clinical trials.gov and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal up to 2 June, 2015. We also screened reference lists of articles and contacted authors to find more studies to include.
Selection criteria
We included randomised controlled trials (RCTs), cluster‐randomised controlled trials (cRCTs), and quasi‐randomised controlled trials of interventions to reduce sitting at work. For changes of workplace arrangements, we also included controlled before‐and‐after studies (CBAs) with a concurrent control group. The primary outcome was time spent sitting at work per day, either self‐reported or objectively measured by means of an accelerometer‐inclinometer. We considered energy expenditure, duration and number of sitting episodes lasting 30 minutes or more, work productivity and adverse events as secondary outcomes.
Data collection and analysis
Two review authors independently screened titles, abstracts and full‐text articles for study eligibility. Two review authors independently extracted data and assessed risk of bias. We contacted authors for additional data where required.
Main results
We included 20 studies, two cross‐over RCTs, 11 RCTs, three cRCTs and four CBAs, with a total of 2180 participants from high income nations. The studies evaluated physical workplace changes (nine studies), policy changes (two studies), information and counselling (seven studies) and interventions from multiple categories (two studies). One study had both physical workplace changes and information and counselling components. We did not find any studies that had investigated the effect of periodic breaks or standing or walking meetings.
Physical workplace changes
A sit‐stand desk alone compared to no intervention reduced sitting time at work per workday with between thirty minutes to two hours at short term (up to three months) follow‐up (six studies, 218 participants, very low quality evidence). In two studies, sit‐stand desks with additional counselling reduced sitting time at work in the same range at short‐term follow‐up (61 participants, very low quality evidence). One study found a reduction at six months' follow‐up of ‐56 minutes (95% CI ‐101 to ‐12, very low quality evidence) compared to no intervention. Also total sitting time at work and outside work decreased with sit‐stand desks compared to no intervention (MD ‐78 minutes, 95% CI ‐125 to ‐31, one study) as did the duration of sitting episodes lasting 30 minutes or more (MD ‐52 minutes, 95% CI ‐79 to ‐26, two studies). This is considerably less than the two to four hours recommended by experts. Sit‐stand desks did not have a considerable effect on work performance, musculoskeletal symptoms or sick leave. It remains unclear if standing can repair the harms of sitting because there is hardly any extra energy expenditure.
The effects of active workstations were inconsistent. Treadmill desks combined with counselling reduced sitting time at work (MD ‐29 minutes, 95% CI ‐55 to ‐2, one study) compared to no intervention at 12 weeks' follow‐up. Pedalling workstations combined with information did not reduce inactive sitting at work considerably (MD ‐12 minutes, 95% CI ‐24 to 1, one study) compared to information alone at 16 weeks' follow‐up. The quality of evidence was low for active workstations.
Policy changes
Two studies with 443 participants provided low quality evidence that walking strategies did not have a considerable effect on workplace sitting time at 10 weeks' (MD ‐16 minutes, 95% CI ‐54 to 23) or 21 weeks' (MD ‐17 minutes, 95% CI ‐58 to 25) follow‐up respectively.
Information and counselling
Counselling reduced sitting time at work (MD ‐28 minutes, 95% CI ‐52 to ‐5, two studies, low quality evidence) at medium term (three months to 12 months) follow‐up. Mindfulness training did not considerably reduce workplace sitting time (MD ‐2 minutes, 95% CI ‐22 to 18) at six months' follow‐up and at 12 months' follow‐up (MD ‐16 minutes, 95% CI ‐45 to 12, one study, low quality evidence). There was no considerable increase in work engagement with counselling.
There was an inconsistent effect of computer prompting on sitting time at work. One study found no considerable effect on sitting at work (MD ‐17 minutes, 95% CI ‐48 to 14, low quality evidence) at 10 days' follow‐up, while another study reported a significant reduction in sitting at work (MD ‐55 minutes, 95% CI ‐96 to ‐14, low quality evidence) at 13 weeks' follow‐up. Computer prompts to stand reduced sitting at work by 14 minutes more (95% CI 10 to 19, one study) compared to computer prompts to step at six days' follow‐up. Computer prompts did not change the number of sitting episodes that last 30 minutes or longer.
Interventions from multiple categories
Interventions combining multiple categories had an inconsistent effect on sitting time at work, with a reduction in sitting time at 12 weeks' (25 participants, very low quality evidence) and six months' (294 participants, low quality evidence) follow‐up in two studies but no considerable effect at 12 months' follow‐up in one study (MD ‐47.98, 95% CI ‐103 to 7, 294 participants, low quality evidence).
Authors' conclusions
At present there is very low to low quality evidence that sit‐stand desks may decrease workplace sitting between thirty minutes to two hours per day without having adverse effects at the short or medium term. There is no evidence on the effects in the long term. There were no considerable or inconsistent effects of other interventions such as changing work organisation or information and counselling. There is a need for cluster‐randomised trials with a sufficient sample size and long term follow‐up to determine the effectiveness of different types of interventions to reduce objectively measured sitting time at work.
Keywords: Humans, Ergonomics, Posture, Accelerometry, Controlled Before‐After Studies, Energy Metabolism, Randomized Controlled Trials as Topic, Time Factors, Workplace, Workplace/statistics & numerical data
Workplace interventions for reducing sitting time at work
Why is the amount of time spent sitting at work important?
Physical inactivity at work, particularly sitting has increased in recent years. Long periods of sitting increase the risk for obesity, heart disease, and overall mortality. It is unclear whether interventions that aim to reduce sitting at workplaces are effective at reducing the amount of time spent sitting.
The purpose of this review
We wanted to find out the effects of interventions aimed at reducing sitting time at work. We searched the literature in various databases up to 2 June 2015.
What trials did the review find?
We found twenty studies with a total of 2174 participants from high income nations. Nine studies evaluated physical changes in the workplace, four evaluated changes in workplace policy, seven studies evaluated information and counselling interventions and one study evaluated both physical workplace changes and information and counselling components.
Effect of sit‐stand desks
Sit‐stand desks alone decreased workplace sitting with about half an hour to two hours per day. When combined with information and counselling sit‐stand desks reduced sitting at work in the same range. Sit‐stand desks also reduced total sitting time (both at work and outside work) and the duration of sitting episodes that last 30 minutes or longer.
Effect of active workstations
Treadmill desks combined with counselling reduced sitting time at work compared to no intervention. Pedalling workstations combined with information did not reduce sitting at work compared to information alone.
Effect of walking during breaks
The introduction of walking during breaks in two studies with 443 participants did not change sitting time.
Effect of information and counselling
In two studies counselling decreased sitting time with 28 minutes and in another study mindfulness training did not have any effect on sitting at work. There was no considerable increase in work engagement with counselling.
Computer prompting software did not reduce sitting time in two studies. In another study computer prompts reduced sitting time with 55 minutes compared to no intervention. One study found that prompts to stand reduced sitting 14 minutes more than prompts to step. Computer prompts did not change the number of sitting episodes that last 30 minutes or longer.
Interventions from multiple categories
When multiple categories of interventions were combined to decrease sitting, there was reduction in workplace sitting time at 12 weeks' and six months' follow‐up but there was no considerable difference between intervention and control group at 12 months' follow‐up.
Conclusions
The quality of evidence was very low to low for most interventions mainly because studies were very poorly designed and because they had very few participants. We conclude that at present there is very low quality evidence that sit‐stand desks can reduce sitting at work at the short term. There is no evidence for other types of interventions. We need research to assess the effectiveness of different types of interventions for decreasing sitting at workplaces in the long term.
Summary of findings
Summary of findings for the main comparison.
Sit‐stand desks with or without counselling for reducing sitting at work: CBAs
| Sit‐stand desks with or without counselling versus no intervention for reducing sitting at work | ||||||
|
Patient or population: employees who sit at work Settings: workplace Intervention: sit‐stand desk with or without counselling Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No intervention | Sit‐stand desk | |||||
| Time spent sitting at work /8‐hour workday Accelerometer‐inclinometer Follow‐up: median 3 months | The mean time spent sitting at work in the control groups was 346 minutes4 | The mean time spent sitting at work in the intervention groups was 113 minutes less (143 to 84 less) | 61 (2 studies) | ⊕⊝⊝⊝ very low1,2 | ||
| Work performance (1‐10 scale) Self‐reported Follow‐up: median 3 months | The median work performance (1‐10 scale) in the control groups was 8.15 | The mean change in work performance (1‐10) in the intervention groups was 0.35 higher (0.1 lower to 0.79 higher) | 109 (3 studies) | ⊕⊝⊝⊝ very low1,2 | ||
| Time spent sitting at work /8‐hour workday Accelerometer‐inclinometer Follow‐up: median 6 months | The mean time spent sitting at work in the control group was 389 minutes3 | The mean time spent sitting at work in the intervention group was 56 minutes less (101 to 12 less) | 45 (1 study) |
⊕⊝⊝⊝ very low1, 2 |
||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Non‐randomised controlled before‐after study/studies with high risk of bias, downgraded one level
2 Small sample size, no further downgrading possible
3 Value from the control group
4 Mean value from control groups
5 Median of the scores in the three control groups
Summary of findings 2.
Sit‐stand desks for reducing sitting at work: RCTs
| Sit‐stand desks versus no intervention for reducing sitting at work | ||||||
|
Patient or population: employees who sit at work Settings: workplace Intervention: sit‐stand desk Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Sit‐stand desk | no intervention | |||||
|
Time spent sitting at work /8‐hour workday Accelerometer‐inclinometer Follow‐up: short term |
The mean time spent sitting at work in the control group was 343 minutes 4 | The mean time spent sitting at work in the intervention group was 96 minutes less (110 to 83 less) | 70 (2 studies) | ⊕⊕⊝⊝ low1,2 | ||
|
Time spent sitting at work /8‐hour workday Self‐reported questionnaires Follow‐up: median 8 weeks |
The mean time spent sitting at work in the control group was 387 minutes5 | The mean time spent sitting at work in the intervention group was 80 minutes less (129 to 31 less) |
44 (1 study) |
⊕⊕⊝⊝ low1,3 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Risk of bias high due to unconcealed allocation and lack of blinding of participants and personnel, downgraded one level
2 Unrealistic confidence interval, downgraded one level
3 Imprecision with wide confidence intervals, small sample size, downgraded one level
4 Mean value from control groups
5 Sitting time in the control group
Summary of findings 3.
Treadmill desks plus counselling for reducing sitting at work: RCT
| Treadmill desks plus counselling versus no intervention for reducing sitting at work | ||||||
|
Patient or population: employees who sit at work Settings: workplace Intervention: Treadmill desk + counselling Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| no intervention | Treadmill desk | |||||
| Time spent sitting at work /8‐hour workday Accelerometer‐inclinometer Follow‐up: median 3 months | The mean time spent sitting at work in the control group was 342 minutes 3 | The mean time spent sitting at work in the intervention group was 29 minutes less (55 to 2 less) | 31 (1 study) | ⊕⊕⊝⊝ low1,2 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 lack of blinding of participants and personnel, downgraded one level
2 Imprecision with wide confidence intervals, small sample size, downgraded one level
3 Sitting time in the control group
Summary of findings 4.
Cycling workstations + information and counselling compared to information and counselling alone for reducing sitting at work: RCT
| Cycling workstations + information and counselling compared with information and counselling for reducing sitting at work | ||||||
|
Patient or population: employees who sit at work Settings: workplace Intervention: Cycling workstation + information and counselling Comparison: Information and counselling | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Information and counselling | Pedalling workstation + information and counselling | |||||
|
Time spent sitting at work /8‐hour workday Accelerometer‐inclinometer Follow‐up: median 16 weeks |
The mean time spent in sitting at work in the control group was 413 minutes3 | The mean time spent in sitting at work in the intervention groups was 12 minutes less (24 less to 1 more) | 54 (1 study) |
⊕⊕⊝⊝ low1,2 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Imprecision with wide confidence intervals, small sample size, downgraded with one level
2 Lack of blinding of participants and attrition bias, downgraded with one level
3 Sitting time in the control group
Summary of findings 5.
Walking strategies for reducing sitting at work: RCT
| Walking strategies for reducing sitting at work | ||||||
|
Patient or population: employees who sit at work Settings: workplace Intervention: walking strategies Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No intervention | Walking strategies | |||||
| Time spent sitting at work Log book Follow‐up: median 10 weeks | The mean time spent sitting at work in the control group was 344 minutes/day 4 | The mean time spent sitting at work in the intervention group was 16 minutes less (54 less to 23 more) | 179 (1 study) | ⊕⊕⊝⊝ low1,2 | ||
| Time spent sitting at work Self‐reported questionnaires Follow‐up: median 21 weeks | The mean time spent sitting at work in the control group was 389 minutes/day 4 | The mean time spent sitting at work in the intervention group was 17 minutes less (65 less to 32 more) | 190 (1 study) |
⊕⊕⊝⊝ low2,3 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate | ||||||
1 Risk of bias high due to unblinded outcome assessment and lack of allocation concealment, downgraded with one level 2 Imprecision with wide confidence intervals, downgraded with one level
3 Lack of blinding of participants and personnel and attrition bias, downgraded with one level
4 Sitting time in the control group
Summary of findings 6.
Computer prompts + information compared to information alone for reducing sitting at work
| Computer prompts + information compared to information alone for reducing sitting at work | ||||||
| Patient or population: employees who sit at work Settings: workplace Intervention: computer prompt + information Comparison: information alone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Information alone | Computer prompt + information | |||||
| Time spent sitting at work Accelerometer‐inclinometer Follow‐up: short term | The mean time spent sitting at work in the control group was 289 minutes/day4 | The mean time spent sitting at work in the intervention group was 17 minutes less (48 less to 14 more) | 59 (2 studies) | ⊕⊕⊕⊝ low1,2 | ||
| Time spent sitting at work Self‐reported Follow‐up: median 13 weeks | The mean time spent sitting at work in the control group was 362 minutes/day4 | The mean time spent sitting at work in the intervention group was 55 minutes less (96 to 14 less) | 34 (1 study) | ⊕⊕⊝⊝ low2,3 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: we are very uncertain about the estimate | ||||||
1 Risk of bias high due to selective reporting and attrition bias, downgraded with one level 2 Small sample size, downgraded with one level 3 Risk of bias high due to unblinded outcome assessment, downgraded with one level
4 Sitting time in the control group
Summary of findings 7.
Counselling for reducing sitting at work
| Counselling for reducing sitting at work | ||||||
| Patient or population: employees who sit at work Settings: workplace Intervention: counselling Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Usual care | Counselling | |||||
| Time spent sitting at work Self‐reported questionnaires Follow‐up: medium term | The mean time spent in sitting at work in the control group was 462 minutes/day3 | The mean time spent in sitting at work in the intervention groups was 28 minutes less (52 to 5 less) | 747 (2 studies) | ⊕⊕⊝⊝ low1,2 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: we are very uncertain about the estimate | ||||||
1 Risk of bias, allocation not concealed, lack of blinding, high attrition rate, downgraded with one level
2 Imprecision with wide confidence intervals, small sample size, downgraded with one level
3 Mean value from control groups
Summary of findings 8.
Mindfulness training for reducing sitting at work
| Mindfulness training versus no intervention for reducing sitting at work | ||||||
|
Patient or population: employees who sit at work Settings: workplace Intervention: mindfulness training Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No intervention | Mindful training | |||||
| Time spent sitting at work /day Self‐reported questionnaires Follow‐up: median 6 months | The mean time spent in sitting at work in the control group was 295 minutes2 | The mean time spent in sitting at work in the intervention groups was 2 minutes less (22 less to 18 more) | 257 (1 study) | ⊕⊕⊝⊝ low1 | ||
| Time spent sitting at work /day Self‐reported questionnaires Follow‐up: median 12 months | The mean time spent in sitting at work in the control groups was 316 minutes2 | The mean time spent in sitting at work in the intervention groups was 16 minutes less (45 less to 12 more) | 257 (1 study) | ⊕⊕⊝⊝ low1 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: we are very uncertain about the estimate | ||||||
1 Risk of bias high due to unconcealed allocation and unblinded outcome assessment, downgraded with two levels
2 Sitting time in the control group
Summary of findings 9.
Multiple interventions for reducing sitting at work
| Multiple interventions versus no intervention for reducing sitting at work | ||||||
|
Patient or population: employees who sit at work Settings: workplace Intervention: multiple interventions Comparison: no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No intervention | Multiple environment interventions with or without counselling | |||||
| Time spent sitting at work Self‐reported questionnaires Follow‐up: median six months | The mean time spent sitting at work in the control group was 415 minutes/day5 | The mean time spent sitting at work in the intervention group was 61 minutes less (115 to 7 less) | 294 (1 study) |
⊕⊕⊝⊝ low1,2 | ||
| Time spent sitting at work Self‐reported questionnaires Follow‐up: median 12 months | The mean time spent sitting at work in the control group was 415 minutes/day5 | The mean time spent sitting at work in the intervention group was 48 minutes less (103 less to 8 more) | 294 (1 study) |
⊕⊕⊝⊝ low1,2 | ||
|
Time spent sitting at work /8‐hour workday Activity log and accelerometer‐inclinometer Follow‐up: median 12 weeks |
The mean time spent in sitting at work in the control group was 370 minutes5 | The mean time spent in sitting at work in the intervention groups was 117 minutes less (168 to 67 less) | 25 (1 study) |
⊕⊕⊝⊝ very low3,4 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Risk of bias high due to un blinded outcome assessment and attrition bias, downgraded with one level
2 Imprecision with wide confidence intervals, downgraded with one level
3 Imprecision with wide confidence intervals, small sample size, downgraded with two levels
4 Lack of blinding of personnel, downgraded with one level
5 Sitting time in the control group
Background
Description of the condition
The nature of office work has changed considerably over the last couple of decades such that workers do not have to move from their work stations even for simple activities like communicating with colleagues or storing information in files (VicHealth 2012). Advancement in technology (e.g. robotics, computers) has made work easier and more efficient than before, and it has led to a decrease in physical strain at workplaces (Craig 2002). Consequently workers have become less physically active at their workplace compared to their leisure time (Franklin 2011; McCrady 2009; Parry 2013; Thorp 2012; van Uffelen 2010). According to a study by McCrady 2009, office employees sit on average 100 minutes more on workdays than on leisure days.
Sitting at work and conducting one's assigned work tasks whilst seated involves energy expenditure of 1.5 METs or less. Energy expenditure involved in various tasks is measured in metabolic equivalents (METs). One MET is the resting energy, i.e. energy cost of resting quietly, defined as an oxygen uptake of 3.5 mL kg‐1 min‐1(Ainsworth 2000). Reduction in sitting usually results in an increase in physical activity of light to moderate intensity like standing or walking (Mansoubi 2014).
In high‐income countries like the USA and the UK, since 2000, the average amount of occupational physical activity has declined from 125 MET hours per week to 75 MET hours per week. If a person works 40 hours per week and his estimated energy expenditure is three METs per hour, then his or her total estimated expenditure is 120 MET hours per week. However, in low‐ and middle‐income countries average occupational physical activity declined from round 220 MET hours per week to 180 MET hours per week over the same period. The largest decline in occupational physical activity has been seen in China where it has declined from 240 MET hours per week to 160 MET hours per week since 2000 (Ng 2012). This decline in occupational physical activity can largely be attributed to an increase in physical inactivity, especially sitting at the workplace.
Ryan 2011 found that office‐based employees spent 66% of their total time spent at work sitting, of which 5% of sitting events and 25% of sitting time was in single duration events that lasted longer than 55 minutes.
Increase in time spent sitting at work has increased the risk of cardiovascular disease, obesity, diabetes and total mortality, even if one is engaged in recommended levels of physical activity during leisure (Chau 2014a; Craft 2012; Dunstan 2011). There is a 5% increase in risk of obesity and 7% increase in risk of diabetes with each two‐hour per day increase in sitting time at work (Hu 2003). Those who sit for eight to 11 hours per day are at a 15% increased risk of death in the next three years than those who sit for less than four hours per day. This risk increases to 40% for those who sit for more than 11 hours per day (Van der Ploeg 2012). So employees should be encouraged not only to do exercise during commuting to work and during leisure, but also to maintain their intermittent levels of non‐exercise daily activities.
Replacing sitting with physical activity of light (from 1.6 METs to 2.9 METs) to moderate (3 METs to 5.9 METs; Ainsworth 2011) intensity improves insulin sensitivity of tissues, and results in improved metabolism of glucose. It also increases lipoprotein lipase activity that breaks down triglycerides and enhances their uptake into cells (Franklin 2011; Healy 2008). These benefits are seen especially when sitting is replaced with activity of light to moderate intensity like standing and walking, instead of vigorous activity of fixed duration of equal energy expenditure (Duvivier 2013). Reducing and breaking up the time that people spend sitting while at work will improve health (Gilson ND 2011; Hamilton 2008; Healy 2008; Rutten 2013).
Description of the intervention
Globally, it is estimated that 60% of world's population is part of the workforce and spends 60% of their waking hours at work. Thus it is possible to influence the health behaviour of a large proportion of the adult population through workplace interventions (WHO/WEF 2008). Interventions for reducing sitting time at work can involve various types of physical activity of light to moderate intensity.
Workplaces have the advantage of in‐built social support, meaning active collaboration of employees in making sustainable changes to attain a healthy life‐style, and do not require a high degree of individual effort and motivation. Therefore, the changes in lifestyle achieved at work are thought to be sustainable in the long term (Plotnikoff 2012).
Workers can be encouraged to be more physically active through changes in the workplace environment and design. An ordinary office desk can be replaced with a sit‐stand desk or a so‐called hot desk, which is height adjustable and allows the user to alternate posture between sitting and standing (Alkhajah 2012; Gilson ND 2012; Straker 2013), or a vertical workstation that allows the use of a personal computer while walking on a treadmill at a self‐selected velocity (Levine 2007), or a stepping/pedalling/desk cycle device placed under the desk that allows the user to pedal while being seated at work (McAlpine 2007), or an inflated balloon chair or a therapy ball (Beers 2008; USPTO 2000). Replacing ordinary office chairs with inflated balloon chairs makes the act of sitting more physically active by increasing the need to use the abdominal, back, leg and thigh muscles to remain upright and maintain balance. Sitting can also be decreased by changing the layout of workplaces, for example placing printers further away from desks. Office work can also be made more physically demanding by forming walking or other exercise groups like dance or gym groups during work time (Ogilvie 2007; Thogersen‐Ntoumani 2013), by encouraging employees to walk around office buildings during breaks or to take a walk to communicate with fellow employees instead of using the telephone or email. The practice and policy of the workplace can be changed to incorporate periodic breaks within the organisational schedule for short bouts of activity (e.g. of five to 15 minutes' duration) in workplace settings or for conducting walking or standing meetings (Commissaris 2007). Meeting rooms can be equipped with sit‐stand workstations so that employees can choose to stand during meetings if they wish (Atkinson 2014). These changes in workplace practice and policy have the potential of providing an opportunity to a large number of people, who mostly sit at work, to reduce their sitting time.
Workers can also be made aware of the need to change their sitting behaviour by the provision of information, such as motivational prompts to sit less at the workstation, via an e‐health intervention that encourages and reminds the worker to move from a sitting position (Cooley 2013; Evans 2012; Pedersen 2013), or by distributing leaflets with messages like "Sit less, move more" that highlight the risks associated with sitting. An e‐health intervention consists of information that is delivered electronically like emails, point of choice prompts or any message displayed on a computer screen periodically. The same information can also be delivered by a trained counsellor in an interactive manner when he or she listens to workers, finds out their interests and offers them some choices on how to reduce or replace their sitting behaviour (Opdenacker 2008).
There are also some drawbacks to these interventions. The performance and productivity of workers at sitting jobs may be decreased when walking at the workplace is encouraged and the employees leave their desks. Workers on a treadmill desk need to be careful not to trip or fall, and thus divide their attention between work and safety, which might compromise their productivity (Tudor‐Locke 2013). In addition, fine motor skills like mouse handling accuracy, maths problem solving skills and perceived work performance decreases with treadmill and cycling workstations (Commissaris 2014; John 2009). This decrease in efficiency may be due to learning effects, that is becoming acquainted with new modes of work.
How the intervention might work
We envisage three different ways (in isolation or conjunction with each other) that these interventions could work to decrease sitting at workplaces.
Physical changes in the workplace design and environment
If employees are using an ordinary desk or chair in the workplace, provision of new types of work desks or chairs can make them aware of the possibilities these new facilities offer to decrease sitting, and they may be tempted to try them. This would replace sitting with some other activity, while allowing the usual tasks to be carried out with the same efficiency. Changing the layout of the workplace by, for example, placing printers away from desks forces employees to stand up and walk to obtain their printouts.
A policy to change the organisation of work
Organisational policies should support social environments that favour the formation of walking or exercise groups at the workplace, or walking meetings. Formation of walking or exercise groups, or a policy for walking meetings, will help individuals to encourage each other to adapt to new behaviours. The provision of purposive short breaks (with the aim of reducing sitting) will help workers to engage in such activities more frequently. The breaks would also encourage employees to take a walk to communicate with colleagues instead of using the telephone or email. Standing meeting rooms would provide an opportunity for every office employee to reduce his or her sitting time.
Provision of information or counselling
Since people are inclined to expend the least possible energy, workers should be made aware of the need to decrease their sitting behaviour. They should be informed about health risks and the benefits of reducing or replacing sitting with more active behaviour. Wilks 2006 found that employees who had received information regarding the health risks of sitting were more likely to use a sit‐stand desk more frequently than those who had not. Even if people are aware of the adverse effects of sitting, and have access to facilities and programs to decrease sitting, they will still find difficulties in adapting to new behaviour. It requires conscious effort for a person to interrupt their normal sitting behaviour and engage briefly in physical activity of light to moderate intensity while at work. To facilitate behaviour change, people may be provided with point of choice prompts or counselling, which enable individuals to evaluate behavioural choices. Prompts at points of decision can be delivered through various means such as signs, emails, text messages, or telephone calls to create a new daily routine. A prompting software can be installed in an employee's personal computer so that a one‐minute reminder to take a break appears on their screen every 30 minutes (Evans 2012).
Why it is important to do this review
Interventions to decrease sitting at work are increasingly popular, however it is unclear whether they are effective in the long term (Healy 2013). Therefore there is a need to evaluate whether sitting at work can be reduced by interventions, and to compare the effectiveness of various means of achieving reductions.
Although some studies show that sit‐stand desks and walking have been useful in reducing sitting, Straker 2013 found no significant difference in the length of each episode of sitting. Also, Gilson 2009 did not find a significant effect of strategies to increase walking on sitting behaviour, while Evans 2012 found that point‐of‐choice prompting software along with education was superior to education alone. So it is still unclear whether these interventions actually work, and if one is better than the others for decreasing sitting at work.
Possibly because of the variation in results across studies, recommendations for reducing sitting at work vary. One recommendation says prolonged sitting should be limited to no more than two hours over an eight‐hour workday (Commissaris 2007; ISO 11226:2000). Another recommends that a 30‐minute period of moderate intensity physical activity, or its equivalent, should be incorporated into an eight‐hour workday (Commissaris 2007), and a third one recommends a five‐minute exercise break, such as walking, for every 40 to 50 minutes of sitting (CCOHS 2010). In 2015, an international group of experts recommended that desk based employees should aim towards accumulating two hours per day of standing and light activity (light walking) during working hours, eventually progressing to a total accumulation of four hours per day. To achieve this, they recommended to break up sitting time with standing work with the use of sit–stand desks, or by taking short active standing breaks (Buckley 2015). While all these guidelines stress the evidence of the adverse effects of sitting on health, there is little evidence that different interventions that aim to reduce sitting can achieve any of these recommendations. Furthermore, since this topic is of increasing interest, it is likely that the availability of evidence will increase in the near future. A Cochrane systematic review will ensure timely updating of this information for decision makers.
Objectives
To evaluate the effects of workplace interventions to reduce sitting at work compared to no intervention or alternative interventions.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), cluster‐RCTs and also quasi‐RCTs. Quasi‐RCTs are trials that randomise participants to the intervention or control group using a method of randomisation that is not actually random, such as date of birth. At workplaces, interventions operate at group level and are difficult to deliver to individuals (Ijaz 2014). Since it is more difficult to randomise units when the intervention is implemented at a higher aggregate level, we also included controlled before‐and‐after studies (CBAs) that used a concurrent control group for the interventions that aimed to change workplace arrangements.
Types of participants
We included all studies conducted with participants who were 18 years or older, whose occupations involved spending the majority of their working time sitting at a desk, such as in administrative jobs, customer service, help‐desk professionals, call‐centre representatives and receptionists (Pronk 2012).
We excluded studies that addressed transportation work. People working in the transportation industry (such as taxi drivers, truck drivers, bus drivers, airline pilots) and who operate heavy equipment (such as crane operators, bulldozer operators) are also exposed to prolonged sitting, but it is difficult to plan an intervention to decrease sitting in such occupations. Reducing sitting in people who work in the transportation industry and operate heavy machinery requires different interventions that could be the scope of another review.
Types of interventions
Intervention
Physical changes in workplace environment
Changes in the layout of the workplace such as printers situated further away from desks.
Changes in desks enabling more activity, such as the use of a sit‐stand desk, a vertical workstation on a treadmill, desk cycle/cycling workstation or a stepping device.
Changes in chairs enabling more activity, such as inflated balloon chairs or therapy balls.
A policy to change the organisation of work
Multiple environmental interventions.
Supporting the social environment by the introduction of walking meetings, walking or other exercise groups during work time.
Breaks (periodic, frequent, or purposive) to sit less, stand up and take an exercise break.
Sitting diaries.
Information and counselling to encourage workers to sit less
Signs or prompts at the workplace (e.g. posters) or at the workstation (computer).
E‐health intervention.
Distribution of leaflets.
Counselling (face to face, email, or telephone).
Multiple category interventions
Interventions composed of multiple elements that include more than one of the above categories.
Comparison
We compared the interventions described above with no intervention or with other active interventions.
Types of outcome measures
Primary outcomes
We included studies that evaluated sitting at work measured either as:
self‐reported time spent seated at work by questionnaires; or
objectively measured sitting by means of an accelerometer‐inclinometer, which assesses intensity of physical activity and body posture (Kanoun 2009; Kim 2015); or
self‐reported or objectively measured time spent in episodes of prolonged sitting at work (30 minutes or more) and number of such episodes.
Secondary outcomes
Estimated energy expenditure in MET hours per workday as a proxy measure to detect changes in sitting time.
Self‐reported or objectively measured total time spent in sitting at and outside work.
Work productivity.
Adverse events including any reported musculoskeletal symptoms due to prolonged standing as a possible side effect of using a sit‐stand desk.
Search methods for identification of studies
Electronic searches
We searched for all eligible published and unpublished trials in all languages. We were prepared to translate non‐English language abstracts for potential inclusion. Our search strategy was based on concepts of types of study population, types of study design, work‐related aspects and outcomes related to sitting, and it consisted of words generated with the help of a thesaurus such as 'seated posture'.
We searched the following electronic databases from inception to 2 June 2015 for identifying potential studies:
Cochrane Central Register of Controlled Trials (CENTRAL; Appendix 1);
MEDLINE (PubMed; Appendix 2);
CINAHL (Cumulative Index to Nursing & Allied Health Literature; Appendix 3);
OSH UPDATE (Occupational Safety and Health Database; Appendix 4);
EMBASE (embase.com; Appendix 5);
PsycINFO (ProQuest; Appendix 6);
ClinicalTrials.gov (http://clinicaltrials.gov/; Appendix 7); and
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal (http://apps.who.int/trialsearch/; Appendix 8).
Searching other resources
We checked reference lists of all included studies and systematic reviews for additional references. We contacted experts in the field and authors of included studies to identify additional unpublished or ongoing studies.
Data collection and analysis
Selection of studies
Two review authors (NS, KKH) independently screened titles and abstracts of studies that we found in our systematic search, to identify studies for inclusion. The same authors marked citations as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. We retrieved full‐text study reports or publications for all citations considered potentially relevant. Two review authors (NS, KKH) independently assessed the full text of these to identify eligible studies for inclusion. We recorded reasons for exclusion of ineligible studies. We resolved disagreements through discussion or, if required, we consulted a third author (SI). We identified and excluded duplicates and collated multiple reports of the same study so that each study rather than each report was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram (Moher 2009).
Data extraction and management
We used a piloted data collection form for study characteristics and outcome data. We extracted the following study characteristics.
Methods: study location, date of publication, type of study design, study setting.
Participants: number randomised, mean age or age range, gender, inclusion and exclusion criteria of the trial, occupation, number of withdrawals, similarity of study groups in age, gender, occupation and sitting time at baseline.
Interventions: description of intervention methods and randomised groups, duration of active intervention, duration of follow‐up, and description of comparisons interventions and co‐interventions.
Outcomes: description of primary and secondary outcomes and their assessment methods.
Notes: funding for trial and notable conflicts of interest of trial authors.
Two review authors (NS and either VH or SB) independently extracted outcome data from included studies. We noted in the 'Characteristics of included studies' table when trial authors did not report outcome data in a usable way. We resolved disagreements by consensus or by involving a third author (SI). One review author (NS) transferred data into the Cochrane Collaboration's statistical software, Review Manager 2013 (RevMan). We double‐checked that we had entered the data correctly. For this purpose we tabulated extracted information about studies in a spreadsheet before entry into RevMan. A second review author (JV) spot‐checked a random 20% of extracted data for accuracy against the trial report.
Assessment of risk of bias in included studies
Two review authors (NS and either SK or CN in the previous version and VH or SB in this update) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements by discussion or by involving another author (SI). We assessed the included studies' risk of bias according to the following domains.
Random sequence generation
Allocation concealment
Blinding of participants and personnel
Blinding of outcome assessment
Incomplete outcome data
Selective outcome reporting
Validity of outcome measure
Baseline comparability/imbalance for age, gender and occupation of study groups
We graded each potential source of bias as high, low or unclear and provided a quote from the study report together with a justification for our judgment in the 'Risk of bias' tables. We summarised the risk of bias judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes where necessary (e.g. the risk of bias for objectively measured sitting by means of an accelerometer‐inclinometer may be very different from a self‐reported reduction in sitting time). Where information on risk of bias relates to unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' tables.
We judged studies that used an accelerometer‐inclinometer to assess sitting as being at low risk, even if the outcome assessor was not blinded, as participants were unlikely to misreport sitting time. Conversely we judged studies assessing sitting time with self‐reported questionnaires as being at high risk of bias, as participants receiving the intervention would have been aware of the goals set and the purpose of the intervention, and there was potential for misreporting sitting times.
We judged studies as being at low risk for selective outcome reporting if the final publications of the trial followed what had been planned and registered in international databases (trial registries), e.g. ClinicalTrials.gov, ANZCTR.org.au (Australia and New Zealand), or NTR (Netherland’s Trial Registry). We judged those studies that were not registered in trial registries as being at low risk for selective outcome reporting if they had reported all the outcomes mentioned in the methods section.
We judged a study to be at low risk of bias overall when the study reported a sufficiently detailed description of its random sequence generation, allocation concealment, blinding of outcome assessment (only for studies that assessed sitting objectively by using an accelerometer‐inclinometer, but not for self‐reported sitting time), complete outcome data, no selective outcome reporting and valid outcome measure, that is, all domains had a low risk of bias. Conversely we judged a study to have a high risk of bias when it reported a feature that would be judged as having a high risk of bias in any one of these eight domains. We did not assess blinding of participants or personnel for risk of bias as it is not possible to blind either in studies that are trying to modify activity behaviour.
Measures of treatment effect
We entered the outcome data for each study into the data tables in RevMan to calculate the treatment effects. We used risk ratios (RRs) for dichotomous outcomes and mean differences (MDs) for continuous outcomes. Where only effect estimates and their 95% confidence intervals (CIs) or standard errors were reported in studies, we entered these data into RevMan using the generic inverse variance method. We ensured that higher scores for continuous outcomes had the same meaning for the particular outcome, explained the direction to the reader and reported where we reversed the directions, if this was necessary.
If in future updates of this review we include studies that report results in such a way that we cannot enter them in RevMan in either of the two ways outlined above, we will describe them in the Characteristics of included studies tables, or we will enter the data into Additional tables.
Unit of analysis issues
With studies that employed a cluster‐randomised design and that reported sufficient data to be included in the meta‐analyses, but did not make an allowance for the design effect, we planned to calculate the design effect based on a fairly large assumed intra cluster correlation coefficient of 0.10. We based this assumption on a realistic estimate by analogy on studies about implementation research (Campbell 2001). The three cluster‐RCTs we included (Coffeng 2014; Puig‐Ribera 2015; Verweij 2012) all accounted for the clustering, so we did not need to adjust for the design effect. If we need to do this in future updates of this review we will follow the methods stated in the Section 16.3 of the Cochrane Handbook for Systematic Reviews of Interventions for the calculations (Higgins 2011).
Where study authors reported multiple trial arms in a single trial, we included only the relevant arms. In studies where two comparisons (e.g. educational classes compared to no intervention or to educational classes plus software for point of choice prompting) need to be combined in the same meta‐analysis, we halved the control group to avoid double‐counting.
Dealing with missing data
None of the studies we included in this review had omitted reporting data.
When we did not find a full study report even after contacting authors listed in an abstract, we categorised the references as Studies awaiting classification.
We contacted researchers or study sponsors in order to verify key study characteristics and obtain missing information or full text reports.
If in future updates of this review we find numerical outcome data missing, such as standard deviations (SDs) or correlation coefficients and we cannot obtain them from the authors, we will calculate them from other available statistics such as P values according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Where this is not possible, and the missing data are thought to introduce serious bias, we will explore the impact of including such studies in the overall assessment of results by a sensitivity analysis.
Assessment of heterogeneity
We assessed clinical homogeneity of the results of included studies based on similarity of populations, interventions, outcomes and follow‐up times. We considered populations to be similar when the participants were 18 years or older and their occupations involved sitting for a major part of their working time. We considered interventions to be similar when their working mechanisms were similar, for example, all interventions with changes in desks (see Description of the intervention). We regarded follow‐up times of three months or less as short‐term, between three months and one year as medium‐term and more than one year as long‐term.
We used the I² statistic to measure heterogeneity among the trials in each analysis. If we identified substantial heterogeneity we reported it and explored possible causes by pre‐specified subgroup analysis. Moreover, we quantified the degree of heterogeneity using the I² statistic, where an I² value of 25% to 50% indicates a low degree of heterogeneity, 50% to 75% a moderate degree of heterogeneity and more than 75% a high degree of heterogeneity.
Assessment of reporting biases
Since we could not pool more than three studies for any single outcome, we could not test for the effect of small studies using a funnel plot or with Egger's test (Egger 1997).
Data synthesis
We pooled data from studies we judged to be clinically homogeneous using RevMan (Review Manager 2013). Where studies were statistically heterogeneous we used a random‐effects model, otherwise we used a fixed‐effect model. When using the random‐effects model, we conducted a sensitivity check by using the fixed‐effect model to reveal differences in results.
We avoided decimals that are not meaningful with respect to the original measurement while reporting the outcomes.
We analysed the effects of interventions according to the categories of intervention defined above in Types of interventions: physical changes in the workplace design and environment (changes in desks; changes in chairs); policy to change the organisation of work (supporting social environment and policies for breaks); or information and counselling.
'Summary of findings' table
We created a 'Summary of findings' table using the outcome self‐reported time spent sitting, and objectively measured time spent sitting by means of an accelerometer‐inclinometer, at the workplace measured in minutes per workday. We used the five Grading of Recommendations Assessment, Development and Evaluation (GRADE) considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence as it relates to the studies that contributed data to the meta‐analyses for the pre‐specified outcomes. We used methods and recommendations described in the Section 11.5 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We justified all decisions to down‐ or up‐grade the quality of evidence using footnotes and we made comments to aid readers' understanding of the review where necessary.
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following subgroup analyses using the outcomes self‐reported time spent sitting and objectively measured time spent sitting by means of an accelerometer‐inclinometer at the workplace measured in minutes per workday.
Age: as the probability of maintaining good health and fitness diminishes as an individual gets older (AIHW 2008), there may be differing motivations for participation in workplace interventions depending on age and also because older employees might expect a larger health benefit due to a reduction in sitting (Manini 2015). We planned to compare studies conducted in participants aged 18 to 40 years with studies where all participants were aged 41 years or older.
Types of outcome measure used: we planned to carry out subgroup analysis by type of outcome measure used i.e. self‐reported questionnaire, log book, accelerometer‐inclinometer, or ecological momentary assessment for each intervention.
We were unable to conduct subgroup analysis because we could not find a sufficient number of suitable studies.
Sensitivity analysis
We planned to assess the robustness of our conclusions by excluding studies judged to have a high risk of bias from our meta‐analyses. However, there were not enough studies with a low risk of bias to perform a meaningful sensitivity analysis.
Reaching conclusions
We based our conclusions only on the findings of our review. Our implications for research suggest priorities for future research and outline the uncertainties in this domain of research.
Results
Description of studies
See: Figure 1, Characteristics of included studies, Characteristics of excluded studies, Characteristics of studies awaiting classification, and Characteristics of ongoing studies.
Figure 1.
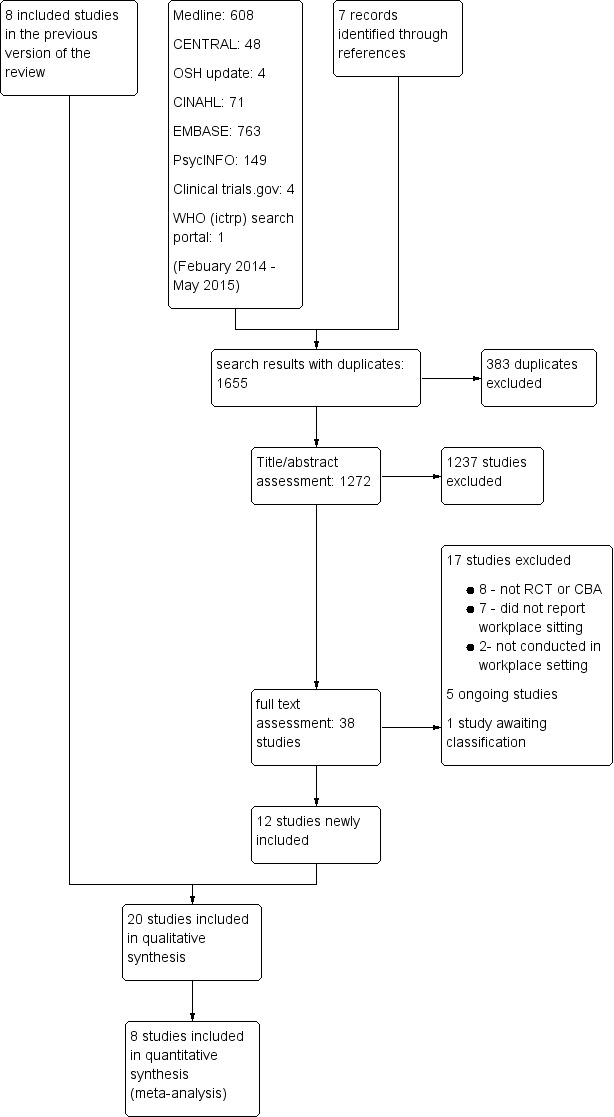
PRISMA Study flow diagram
Results of the search
We conducted searches in various electronic databases (CENTRAL, MEDLINE, CINAHL, OSH UPDATE, EMBASE, and PsycINFO, Clinical trials.gov and WHO search trial portal) and we also searched for grey literature. We present a detailed search strategy for all the electronic databases we used in the Appendices. We identified 10713 references from the initial electronic literature search (run up to December 2013), retrieving 54 references for full‐text scrutiny. After further examination we excluded 46 articles and included eight studies in the first published version of this review.
As outlined in Figure 1, the electronic searches yielded a total of 1655 references for this update. These break down as follows: CENTRAL 48 (Appendix 1, 2 June 2015): MEDLINE 608 (Appendix 2, 2 June 2015): CINAHL 71 (Appendix 3, 2 June 2015): OSH UPDATE 4 (Appendix 4, 2 June 2015): EMBASE 763 (Appendix 5, 2 June 2015): PsycINFO 149 (Appendix 6, 2 June 2015): Clinical trials.gov 3 (Appendix 7, 2 June 2015): WHO search trial portal 1 (Appendix 8, 2 June 2015). We also identified seven references through checking reference lists and update alerts by Google scholar for newly published articles on the topic. Removal of duplicates reduced the total to 1272 references. Based on the title and abstract, we selected 38 references for full text reading. Out of these, we excluded those that did not fulfil our inclusion criteria. When the article did not provide enough data we contacted the authors for the missing information. If we did not receive sufficient information to judge whether the study should be included we classified the study as awaiting classification. This resulted in 12 studies being included in this review update in addition to the eight studies already included in the previous version of this review.
Included studies
Study design
Eleven of the 20 included studies were randomised controlled trials, two were cross‐over randomised control trials, four were controlled before‐and‐after studies with concurrent controls and three were cluster‐randomised trials. See Characteristics of included studies for further details. Although the authors described their studies as quasi‐RCTs, we categorised Alkhajah 2012 and Neuhaus 2014a as controlled before‐and‐after studies, because the risk of baseline differences for studies with only two clusters is very high.
For meta‐analyses that included two arms of the same study, we halved the number of participants in the control group in Coffeng 2014. To be able to do this we had to use the unadjusted results at twelve months follow‐up. In other comparisons we used the adjusted values with the generic inverse variance method. One included study (Neuhaus 2014a) reported only mean differences and standard errors and the authors could not provide raw data, so we could not adjust the number of participants. In this case we modelled the means and standard deviations from the intervention and the control group in RevMan as closely to the real data as possible to achieve the same mean difference and standard error. Then we halved the number of participants in the control group and entered the resulting standard errors into RevMan.
Participants
In total, the included studies analysed 2180 employees. van Berkel 2014 analysed 257 employees; Gilson 2009 179 employees; Verweij 2012 16 occupational physicians, and 523 employees; Alkhajah 2012 30 employees; Carr 2015; 44 employees; Chau 2014 42 employees; Coffeng 2014 412 employees; Donath 2015 31 employees; Dutta 2014 29 employees; Ellegast 2012 25 employees; Evans 2012 28 employees; Gao 2015 45 employees; Graves 2015 44 employees; Healy 2013 36 employees; Pedersen 2013 34 employees; Neuhaus 2014a 44 employees; Gordon 2013 22 employees; Puig‐Ribera 2015 264 employees; Schuna 2014 31 employees and Swartz 2014 60 employees.
Gender
Participants in nine studies were predominantly women (Carr 2015; Donath 2015; Dutta 2014; Evans 2012; Gao 2015; Gilson 2009; Graves 2015; Schuna 2014; Swartz 2014). In the remaining 11 studies the proportions of women and men did not differ significantly.
Country
Studies were conducted in Australia, USA and high income nations in Europe.
Interventions
1. Physical changes in workplace environment
Nine studies evaluated the effectiveness of individual workspace modifications on workplace sitting time (Alkhajah 2012; Carr 2015; Chau 2014; Dutta 2014; Gao 2015; Graves 2015; Healy 2013; Neuhaus 2014a; Schuna 2014).
Sit‐stand desk
Seven studies assessed the effect of a sit‐stand desk. The intervention was assessed alone (Alkhajah 2012; Chau 2014; Dutta 2014; Gao 2015; Graves 2015; Neuhaus 2014a), as well as in combination with information and counselling (Healy 2013; Neuhaus 2014a).
Neuhaus 2014a also assessed the effectiveness of a sit‐stand desk plus information and counselling compared to a sit‐stand desk only.
Treadmill workstation
One study (Schuna 2014) assessed the effectiveness of a treadmill workstation.
Cycle workstation
One study (Carr 2015) assessed the effectiveness of a cycle workstation.
2. A policy to change the organisation of work
Two studies evaluated the effect of walking strategies (Gilson 2009; Puig‐Ribera 2015). Gilson 2009 evaluated the effectiveness of route and incidental walking on office employees' sitting time at work. The route‐based walking was intended to increase brisk sustained walking during work breaks. The incidental walking targeted walking and talking to colleagues, rather than sending emails or making telephone calls, and standing and walking in meetings, instead of sitting at desks. Puig‐Ribera 2015 evaluated the effect of incidental movement and short (5–10 minutes) and longer (10+ minute) walks on office employees' sitting time at work.
3. Information and counselling
Computer prompts
Three studies evaluated the effectiveness of computer prompts plus information compared to information alone in decreasing sitting time in office employees (Donath 2015; Evans 2012; Pedersen 2013). Computer prompts offer an opportunity to employees to choose and engage in a short‐burst of physical activity such as standing or walking. One study (Swartz 2014) assessed the effect of hourly prompts (computer based and wrist worn) to stand up or to step on reducing sitting time in office employees.
Counselling
Verweij 2012 evaluated the effectiveness of counselling by occupational physicians compared to usual care in decreasing sitting time in office employees. Occupational physicians are highly trained specialists who provide health services to employees and employers (AFOEM 2014). Coffeng 2014 evaluated the effectiveness of group motivational interviewing by occupational physicians on office employees' sitting time. Group motivational interviewing is a counselling style that stimulates behavioral change by focusing on exploring and resolving ambivalence in a group.
van Berkel 2014 evaluated the effectiveness of mindfulness training in decreasing sitting time in office employees. The mindfulness intervention consisted of homework exercises and information through emails.
4. Multiple interventions
Two studies evaluated the effect of multiple interventions on sitting at work (Coffeng 2014; Ellegast 2012).
Coffeng 2014 assessed the effect of multiple environmental interventions. The multiple environmental interventions consisted of (1) the Vitality in Practice (VIP) Coffee Corner Zone – a workplace coffee corner was modified by adding a bar with bar chairs, a large plant and a giant wall poster (a poster visualizing a relaxing environment, e.g. wood, water and mountains); (2) the VIP Open Office Zone – an office was modified by introducing exercise balls and curtains to divide desks in order to reduce background noise; (3) the VIP Meeting Zone – conference rooms were modified by placing a standing table and a giant wall poster; and (4) the VIP Hall Zone ‐ table tennis tables were placed and lounge chairs were introduced in the hall for informal meetings. In addition, footsteps were placed on the floor in the entrance hall to promote stair walking.
Ellegast 2012 assessed the effectiveness of multiple environment interventions in combination with a walking strategy. The intervention consisted of measures aiming to change working conditions (e.g. sit‐stand tables) and behaviour (e.g. pedometers as activity feedback and face‐to‐face motivation for lunch walks and an incentive system for bicycle commuting or sports activities).
Type of control group
No intervention
Fifteen of the included studies used a no intervention control group (Alkhajah 2012; Chau 2014; Coffeng 2014; Dutta 2014; Ellegast 2012; Gao 2015; Gilson 2009; Graves 2015; Healy 2013; Neuhaus 2014a; Puig‐Ribera 2015; Schuna 2014; van Berkel 2014; Verweij 2012).
Other controls
Neuhaus 2014a also compared sit‐stand desks plus information and counselling with sit‐stand desks only resulting in the net effect of information and counselling. Carr 2015 compared a cycle workstation in combination with information and counselling with information and counselling only resulting in the net effect of a cycle workstation.
Donath 2015, Evans 2012 and Pedersen 2013 compared point‐of‐choice prompts plus information with information only resulting in the net effect of point‐of‐choice prompts.
Gordon 2013 compared a cognitive‐based e‐newsletter with cognitive‐based health education.
Swartz 2014 compared computer‐based and wrist‐worn prompts with instruction to stand versus instruction to step.
Outcome
Total time spent sitting at work
Sitting was reported as total time spent sitting at work in 14 studies (Alkhajah 2012; Chau 2014; Donath 2015; Dutta 2014; Ellegast 2012; Evans 2012; Gilson 2009; Gordon 2013; Graves 2015; Healy 2013; Neuhaus 2014a; Pedersen 2013; Puig‐Ribera 2015; Schuna 2014). Carr 2015, Coffeng 2014, Gao 2015, Schuna 2014, Verweij 2012 and van Berkel 2014 reported sitting time at work as occupational sedentary time which is equivalent to time spent sitting at work.
Prolonged sitting episodes at work
Three studies reported time spent in prolonged sitting at work (Evans 2012; Healy 2013; Neuhaus 2014a). Two studies reported number of prolonged sitting events at work (Evans 2012, Swartz 2014).
Total time spent sitting at and outside work
Alkhajah 2012, Dutta 2014 and Verweij 2012 also reported total time spent sitting.
Energy expenditure
Only one study reported estimated energy expenditure based on information about sitting time at work (Pedersen 2013). They chose 1.5 MET to represent sitting and 2.3 MET to represent standing which is actually an unrealistically big difference. They reported calories but this must be kilocalories. Júdice 2015b measured energy costs calorimetrically for sitting and standing and found that there was only a 0.07 Kcal difference.
Work productivity
Three studies reported work performance on a scale of 1 to 10 (Alkhajah 2012; Healy 2013; Neuhaus 2014a). Carr 2015 also reported having measured work productivity but the authors present no data.
Two studies reported work engagement on a scale of 0 to 6 (Coffeng 2014; van Berkel 2014) using the Utrecht Work Engagement Scale (UWES). The Utrecht Work Engagement Scale is a self‐report questionnaire that measures three aspects of engagement: vigour (6 items), dedication (5 items), and absorption (6 items).
Adverse events
Three studies reported musculoskeletal symptoms by anatomical regions (Alkhajah 2012; Healy 2013; Neuhaus 2014a). Two studies (Gao 2015; Graves 2015) reported musculoskeletal discomfort or pain at three sites: lower back, upper back, neck and shoulders. Gao 2015 used a scale ranging from 1 (very comfortable) to 5 (very uncomfortable) and Graves 2015 used a scale ranging from 0 (no discomfort) to 10 (extremely uncomfortable). Carr 2015 also reported having measured musculoskeletal discomfort but present no data in their article.
One study reported more than one sick day for the last three months (Alkhajah 2012), whereas two studies reported more than one sick day in the last month of intervention (Healy 2013; Neuhaus 2014a).
Only one study reported adverse events in general defined as overall body pain (Neuhaus 2014a).
Follow‐up times
In three studies the longest follow‐up was one month or less (Evans 2012; Healy 2013; Swartz 2014) and in ten studies the follow‐up was three months or less (Alkhajah 2012; Chau 2014; Donath 2015; Dutta 2014; Ellegast 2012; Gilson 2009; Gordon 2013; Graves 2015; Neuhaus 2014a; Schuna 2014). We defined all of these as short term follow‐up.
The remaining five studies followed participants between three to 12 months (Carr 2015; Coffeng 2014; Gao 2015; Pedersen 2013; Puig‐Ribera 2015; van Berkel 2014; Verweij 2012) which we defined as medium term follow‐up.
No studies had a follow‐up longer than 12 months which we defined as long term follow‐up.
Excluded studies
Of the 87 papers assessed as full text, we found that 47 did not meet our inclusion criteria and that we summarily excluded. Twenty one studies were not randomised controlled trials or controlled before‐and‐after studies with concurrent controls. Three studies were not conducted in workplace setting, three studies reported sedentary time, which also included activities like standing and reclining. 10 studies reported sitting time but no distinction between sitting at work and leisure time, and another 11 studies did not report sitting time at all. See the Characteristics of excluded studies table for further details.
Risk of bias in included studies
Risk of bias varied considerably across studies (Figure 2).
Figure 2.
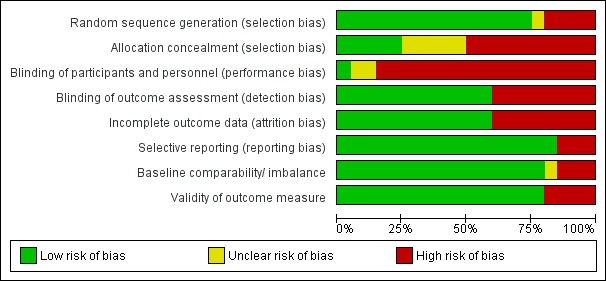
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
Except Alkhajah 2012, Gao 2015, Healy 2013 and Neuhaus 2014a, all the studies described the method of randomisation they had used, so we judged these studies to have a low risk of bias for the domain of sequence generation. Donath 2015 used the minimization method which is considered equivalent to randomisation (Chapter 8; Assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions, Higgins 2011). Only Carr 2015, Ellegast 2012, Evans 2012, Schuna 2014 and Swartz 2014 reported concealing intervention versus control group allocation, so we judged all the other studies to have a high risk of bias for the domain of allocation concealment.
Blinding
In all but a single included study (Verweij 2012), the blinding of participants to the interventions they were receiving would have been impossible due to the nature and aims of interventions being self‐evident, so we judged that these seven studies had a high risk of bias in the performance bias domain. Verweij 2012 reported asking randomised occupational physicians not to reveal their allocation to participating employees who were their patients.
For outcome assessment Alkhajah 2012, Carr 2015, Chau 2014, Donath 2015, Dutta 2014, Ellegast 2012, Evans 2012, Gordon 2013, Healy 2013, Neuhaus 2014a, Schuna 2014 and Swartz 2014 used an accelerometer‐inclinometer to assess sitting time, so we judged these studies to have a low risk of detection bias. Conversely Coffeng 2014,Gao 2015, Gilson 2009, Graves 2015, Pedersen 2013, Puig‐Ribera 2015, van Berkel 2014 and Verweij 2012 assessed sitting time with self‐reported questionnaires or paper‐based diary or ecological momentary assessment, and so we judged these studies to have a high risk of detection bias.
Incomplete outcome data
We judged Dutta 2014, Gao 2015, Gilson 2009, Neuhaus 2014a, Puig‐Ribera 2015, Swartz 2014, Verweij 2012 to have a high risk of bias for incomplete outcome data. Dutta 2014 did not report 14% of working hours and the remaining studies lost more than 10% of participants to follow‐up. We judged all other studies to have a low risk of bias for incomplete outcome data. Gordon 2013, Graves 2015 and van Berkel 2014 conducted intention‐to‐treat analysis. Coffeng 2014 conducted multilevel analysis to account for missing data. Chau 2014 reported that imputing values for missing covariate values did not influence the effect of the intervention on the adjusted estimates for the outcomes. Evans 2012 and Healy 2013 lost the same proportion of participants from both intervention and control groups, so we believe that the missing data did not have a significant impact on outcomes (Cochrane Handbook for Systematic Reviews of Interventions, section 8.13.2,Higgins 2011).
Selective reporting
We judged three studies (Evans 2012; Neuhaus 2014a; Schuna 2014) to have a high risk of bias due to discordance between outcomes in available protocols and the ones reported in study results. We judged the remaining 17 studies to have a low risk of bias as they reported results for all the outcome measures mentioned either in the protocol or methods section for studies where a protocol was not available (Alkhajah 2012; Chau 2014; Coffeng 2014; Donath 2015; Dutta 2014; Gao 2015; Gilson 2009; Gordon 2013; Healy 2013; Pedersen 2013; Puig‐Ribera 2015; Schuna 2014; Swartz 2014; van Berkel 2014; Verweij 2012).
Other potential sources of bias
This domain had two parts as decided a priori:
Validity of outcome measure
Baseline comparability/imbalance for age, gender and occupation of study groups
Coffeng 2014, Gao 2015, Pedersen 2013, Verweij 2012 and van Berkel 2014 assessed sitting time at work with questionnaires. Self‐report questionnaires are cost‐effective and readily accessible to the majority of the population however participants receiving the intervention might be aware of the goals set and the purpose of the intervention and may therefore misreport outcomes (Healy 2011). The questionnaire used by Coffeng 2014, Gao 2015, Verweij 2012 and van Berkel 2014 has not been tested for its validity in assessing time spent sitting at work. Pedersen 2013 used the Occupational Sedentary and Physical Activity Questionnaire (OSPAQ) which has moderate validity for assessing time spent sitting at work (Chau 2012). Gilson 2009 and Puig‐Ribera 2015 assessed sitting time with paper‐based diary (log book). There is a lack of validity and reliability data for assessing sitting through logbooks. However, they are less dependent on long‐term recall and therefore might provide a more accurate measurement of sitting time at work. In any case log data are subject to reporting bias as it is not possible to determine if the log has been filled in at the required intervals or if it was, for example, completed on the final day (Clark 2009). Graves 2015 assessed sitting time at work with ecological momentary assessment (EMA) diaries. Ecological momentary assessment is a valid, reliable, and feasible approach to evaluate activity and sedentary behavior. The benefit of EMA is its ability to collect data in real‐time and real‐world circumstances hence there is no recall bias (Marszalek 2014).
Alkhajah 2012, Carr 2015, Chau 2014, Donath 2015, Dutta 2014, Ellegast 2012, Evans 2012, Gordon 2013, Healy 2013, Neuhaus 2014a, Schuna 2014 and Swartz 2014 assessed sitting time at work with an accelerometer‐inclinometer. Such objective measurements also have some limitations such as outcomes being likely affected by methodological decisions made before and after data collection (i.e. type of accelerometer, cut‐off point and non‐wear time definitions) (Janssen 2015). Self‐reported sedentary time has shown to have low to moderate correlation with accelerometer‐derived sedentary time, with improved validity when specific domains of sedentary time are recalled (e.g. time spent watching TV, computer use, sitting at work) (Healy 2011). We therefore judged Coffeng 2014, Gao 2015, Verweij 2012 and van Berkel 2014 to have a high risk of bias based on validity of outcome measure.
We judged two studies to be at high risk of other bias: in Alkhajah 2012, participants in the intervention group were academics involved with sedentary behaviour research, whereas participants in the control group had never been involved in sedentary behaviour or physical activity research. In Gordon 2013, the intervention group had more official and managerial level individuals as well as more people with significantly higher BMI in the intervention group. We judged all other studies to have a low risk for other bias, as neither baselines nor outcome validity was questionable.
Overall Risk of Bias
Overall, we judged all twenty included studies to have a high risk of bias overall based on: inadequate randomisation (Alkhajah 2012; Gao 2015; Healy 2013; Neuhaus 2014a), allocation concealment (Alkhajah 2012; Chau 2014; Dutta 2014; Gao 2015; Graves 2015; Healy 2013; Neuhaus 2014a; Pedersen 2013; van Berkel 2014; Verweij 2012), blinding of outcome assessment (Coffeng 2014; Gao 2015; Gilson 2009; Graves 2015; Pedersen 2013; Puig‐Ribera 2015; van Berkel 2014; Verweij 2012), incomplete outcome data (Donath 2015; Dutta 2014; Gao 2015; Gilson 2009; Neuhaus 2014a; Puig‐Ribera 2015; Swartz 2014; Verweij 2012), and selective reporting (Evans 2012; Neuhaus 2014a; Schuna 2014). See Figure 3 for a summary of our judgements about each risk of bias item for each included study.
Figure 3.
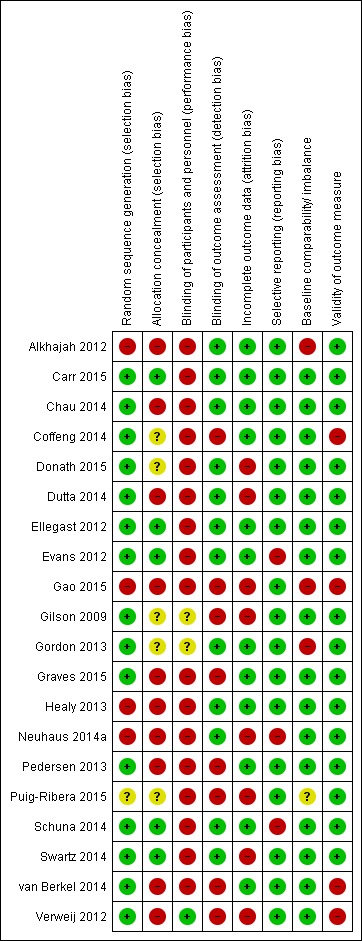
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9
Physical changes in the workplace environment
Sit‐stand desks with or without counselling versus no intervention: CBA
Outcome: sitting time at work
Measured as time spent in sitting at work: follow‐up at three months
One CBA involving employees in a public health research institute (Alkhajah 2012) showed a decrease in sitting of 137 minutes per eight‐hour workday (95% CI ‐179 to ‐95) in the sit‐stand desk group compared to no intervention. However, another other CBA involved regular office workers and showed a much smaller decrease in sitting of 33 minutes per eight‐hour workday (95% CI ‐84 to 17) with sit‐stand desks (Neuhaus 2014a), which was not significantly different from no intervention. Therefore, we did not pool the results of these two studies comparing the effect of a sit‐stand desk alone versus no intervention due to substantial heterogeneity (I² = 89%).
Two different studies also compared a sit‐stand desk plus information and counselling to no intervention (Healy 2013; Neuhaus 2014a). The pooled analysis showed that after three months the sit‐stand desk plus information and counselling intervention reduced sitting time at work by 113 minutes per eight‐hour workday (95% CI ‐143 to ‐84; Analysis 1.1).
Analysis 1.1.
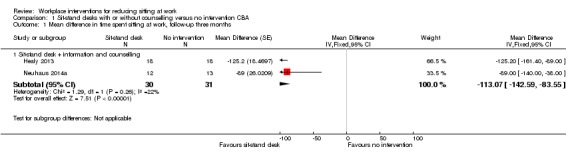
Comparison 1 Sit‐stand desks with or without counselling versus no intervention CBA, Outcome 1 Mean difference in time spent sitting at work, follow‐up three months.
Measured as time spent in sitting at work: follow‐up at six months
Also at medium‐term follow‐up (six months), in one CBA, (Gao 2015) providing workers with sit‐stand desks reduced sitting time at work with 56 minutes per eight‐hour workday (95% CI ‐101 to ‐12) compared to no intervention (Analysis 1.2).
Analysis 1.2.
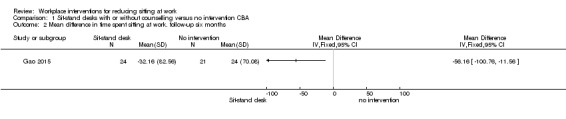
Comparison 1 Sit‐stand desks with or without counselling versus no intervention CBA, Outcome 2 Mean difference in time spent sitting at work. follow‐up six months.
Measured as duration of sitting in episodes lasting 30 minutes or more: follow‐up at three months
Two studies containing three study arms measured the intervention effect on duration of sitting in episodes lasting 30 minutes or more (Healy 2013; Neuhaus 2014a).
Neuhaus 2014a compared a sit‐stand desk only with a sit‐stand desk plus counselling and with no intervention. Healy 2013 compared a sit‐stand desk plus counselling with no intervention.The pooled effect estimate of those three study arms showed a reduction of 52 minutes per eight‐hour workday (95% CI ‐79 to ‐26) in sitting episodes lasting 30 minutes or more in the intervention group, with moderate heterogeneity (I² = 45%).
Analysis of the subgroup of sit‐stand desks combined with counselling resulted in a mean reduction of 63 minutes per eight‐hour workday (95% CI ‐93 to ‐33) with moderate heterogeneity (I² = 31%; Analysis 1.3).
Analysis 1.3.
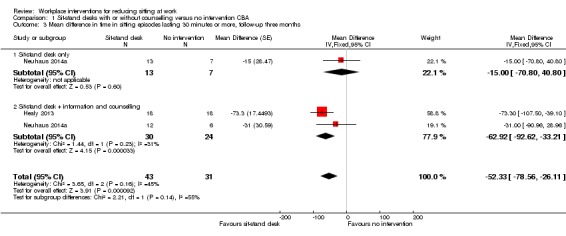
Comparison 1 Sit‐stand desks with or without counselling versus no intervention CBA, Outcome 3 Mean difference in time in sitting episodes lasting 30 minutes or more, follow‐up three months.
Measured as total time spent in sitting at and outside work: follow‐up at three months
Alkhajah 2012 also reported a reduction of 78 minutes per 16‐hour day (95% CI ‐125 to ‐31) in total sitting time at work and outside work with a sit‐stand desk compared to no intervention at three months' follow‐up (Analysis 1.4).
Analysis 1.4.
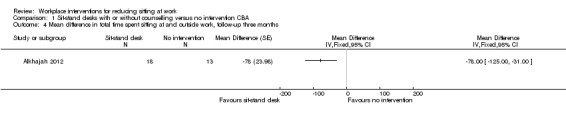
Comparison 1 Sit‐stand desks with or without counselling versus no intervention CBA, Outcome 4 Mean difference in total time spent sitting at and outside work, follow‐up three months.
Outcome: adverse events
Overall body pain
In the Neuhaus 2014a CBA study one participant out of the 13 in the sit‐stand workstation group withdrew from the trial because of overall body pain.
Musculoskeletal symptoms: follow‐up at three months
Alkhajah 2012, Healy 2013 and Neuhaus 2014a reported musculoskeletal symptoms by anatomic regions. We did not combine their results in a meta‐analysis because of substantial heterogeneity in the results (I² = 98%). Musculoskeletal symptoms were measured as the percentage (number) of each group who answered 'yes' to a question about musculoskeletal symptoms.
Alkhajah 2012 and Neuhaus 2014a found a decrease in percentage of participants with musculoskeletal symptoms using a sit‐stand desk compared to no intervention at three months. However the magnitude of effect was much larger in the study by Neuhaus 2014a (MD ‐16.5, 95% CI ‐17.8 to ‐15.3) than in the study by Alkhajah 2012 (MD ‐6, 95% CI ‐6.9 to ‐5.1).
Healy 2013 found a non‐significant increase in percentage of participants with musculoskeletal symptoms in the sit‐stand desk plus counselling group (MD 4, 95% CI 2.6 to 5.5) while Neuhaus 2014a found a slight decrease in percentage of participants with musculoskeletal symptoms (MD ‐11.5, 95% CI ‐12.6 to ‐10.5) in the sit‐stand desk plus counselling group compared to no intervention at three months' follow‐up.
Musculoskeletal symptoms: follow‐up at six months
Gao 2015 assessed mean perceived musculoskeletal comfort for different body parts (neck and shoulders, upper limbs, back and lower limbs) rated at the end of a normal workday on a scale from 1 (very comfortable) to 5 (very uncomfortable). The study found no change in musculoskeletal symptoms with a sit‐stand desk compared to no intervention at six months' follow‐up (MD ‐0.54 95% CI ‐0.89 to ‐0.19).
Outcome: work performance
Measured as: self‐reported work performance: follow‐up at three months
In three studies (Alkhajah 2012; Healy 2013; Neuhaus 2014a) the introduction of sit‐stand desks did not lead to an increase work performance (on a scale of 1 to 10; MD 0.35 score points; 95% CI ‐0.1 to 0.8; Analysis 1.5). Work performance was assessed with a 10 item scale ranging from 1 to 10 relating to the past week with higher scores indicating better performance.
Analysis 1.5.
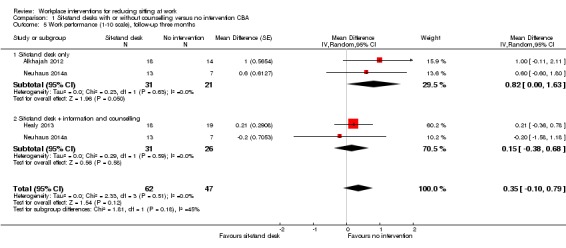
Comparison 1 Sit‐stand desks with or without counselling versus no intervention CBA, Outcome 5 Work performance (1‐10 scale), follow‐up three months.
Measured as: more than one sick day in last three months; follow‐up at three months
One study showed a significant increase by 120% in the proportion of employees having more than one sick day in the sit‐stand desk group compared to no intervention in the last three months after installation of a sit‐stand desk (RR 2.2, 95% CI 0.9 to 5.2; Analysis 1.6; Alkhajah 2012).
Analysis 1.6.
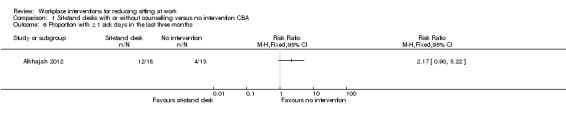
Comparison 1 Sit‐stand desks with or without counselling versus no intervention CBA, Outcome 6 Proportion with ≥ 1 sick days in the last three months.
Two studies measured the proportion of people with more than one sick day in the last month at three months' follow‐up (Healy 2013; Neuhaus 2014a). The introduction of sit‐stand desks reduced the risk of having had more than one sick day in the last month by 23% (RR 0.8, 95% CI 0.5 to 1.2). There was difference between subgroups that had an intervention that included information and counselling along with a sit‐stand desk (reduction in risk by 30%, RR 0.7, 95% CI 0.4 to 1.2) and those that had the sit‐stand desk only (reduction in risk by 10%, RR 0.9, 95% CI 0.4, 2.1; Analysis 1.7).
Analysis 1.7.
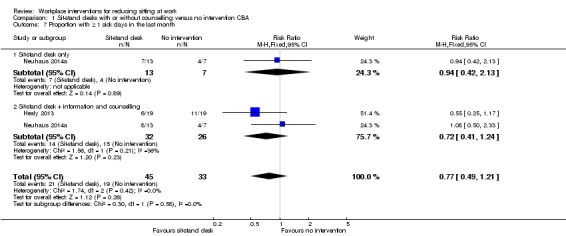
Comparison 1 Sit‐stand desks with or without counselling versus no intervention CBA, Outcome 7 Proportion with ≥ 1 sick days in the last month.
Sit‐stand desks plus information and counselling versus sit‐stands desk only: CBA
Outcome: sitting time
Measured as time spent sitting at work: follow‐up at three months
Neuhaus 2014a found that providing information and counselling to the employees along with the installation of a sit‐stand desk was more effective in reducing sitting at work (MD ‐56 minutes per eight‐hour workday, 95% CI ‐107 to ‐5) than just the installation of a sit‐stand desk (Analysis 2.1).
Analysis 2.1.
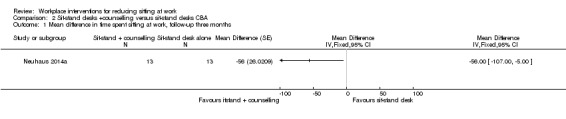
Comparison 2 Sit‐stand desks +counselling versus sit‐stand desks CBA, Outcome 1 Mean difference in time spent sitting at work, follow‐up three months.
Measured as duration of sitting episodes lasting 30 minutes or more: follow‐up at three months
In the same study Neuhaus 2014a found a non‐significant reduction in duration of sitting episodes lasting 30 minutes or more (MD ‐17 minutes per eight‐hour workday, 95% CI ‐63 to 29) with sit‐stand desk plus information and counselling when compared to sit‐stand desk only (Analysis 2.2).
Analysis 2.2.
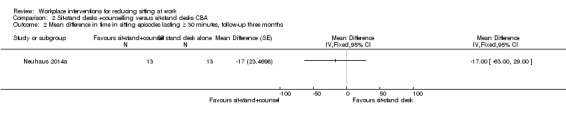
Comparison 2 Sit‐stand desks +counselling versus sit‐stand desks CBA, Outcome 2 Mean difference in time in sitting episodes lasting ≥ 30 minutes, follow‐up three months.
Outcome: adverse events
Measured as: self‐reported work performance: follow‐up at three months
Neuhaus 2014a also found a non‐significant reduction in work performance score by 0.8 points (on a scale of 1 to 10; 95% CI ‐2.1 to 0.5) with sit‐stand desk plus information and counselling when compared to sit‐stand desk alone (Analysis 2.3).
Analysis 2.3.
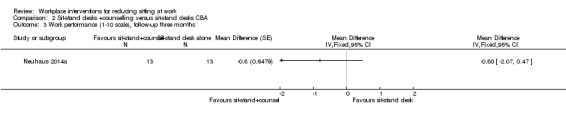
Comparison 2 Sit‐stand desks +counselling versus sit‐stand desks CBA, Outcome 3 Work performance (1‐10 scale), follow‐up three months.
Measured as more than one sick day in the last month: follow‐up at three months
In the same study Neuhaus 2014a found a non‐significant increase in the proportion of employees with more than one sick day in the last month using the sit‐stand desk plus information and counselling compared to sit‐stand desk alone, with a risk ratio of 1.1 (95% CI 0.6 to 2.2; Analysis 2.4).
Analysis 2.4.
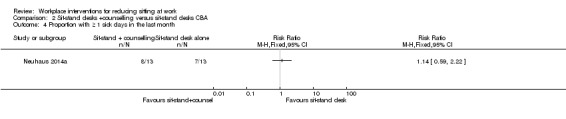
Comparison 2 Sit‐stand desks +counselling versus sit‐stand desks CBA, Outcome 4 Proportion with ≥ 1 sick days in the last month.
Sit‐stand desks versus no intervention: RCT
Outcome: Sitting time
Measured as time spent sitting at work (cross‐over RCT): follow‐up at short term
Two studies compared a sit‐stand desk to no intervention (Chau 2014; Dutta 2014). The pooled analysis showed that the sit‐stand desk intervention reduced sitting time at work by 96 minutes per eight‐hour workday (95% CI ‐110 to ‐83; I² = 56%; Analysis 3.1). However, the data from the Dutta 2014 study carried 84% of the weight in the meta‐analysis due to the unrealistically narrow confidence interval of the outcome reported by the study. The Dutta 2014 study reported percentage reduction in time spent sitting at work, which we converted into minutes per eight‐hour workday.
Analysis 3.1.
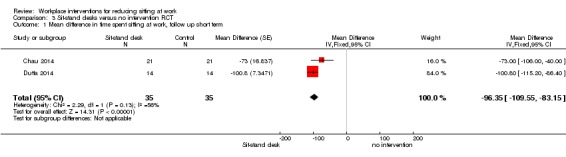
Comparison 3 Sit‐stand desks versus no intervention RCT, Outcome 1 Mean difference in time spent sitting at work, follow up short term.
Measured as time spent sitting at work: follow‐up at eight weeks
In one RCT, Graves 2015 found that sit‐stand desks reduced sitting time at work by 80 minutes per eight‐hour workday (95% CI ‐129 to ‐31) at eight weeks' follow‐up (Analysis 3.2) .
Analysis 3.2.
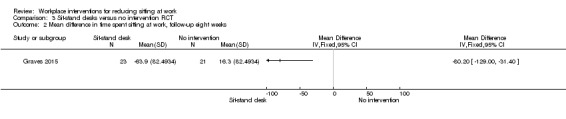
Comparison 3 Sit‐stand desks versus no intervention RCT, Outcome 2 Mean difference in time spent sitting at work, follow‐up eight weeks.
Outcome: adverse events
Measured as musculoskeletal symptoms: follow‐up at eight weeks
Graves 2015 found no change in rating of musculoskeletal discomfort by participants using a sit‐stand desk compared to no intervention at eight weeks' follow‐up (MD ‐0.51, 95% CI ‐1.03 to 0, Analysis 3.3). Participants rated musculoskeletal discomfort or pain at three sites (lower back, upper back, neck and shoulders) on a Likert scale ranging from 0 (no discomfort) to 10 (extremely uncomfortable).
Analysis 3.3.
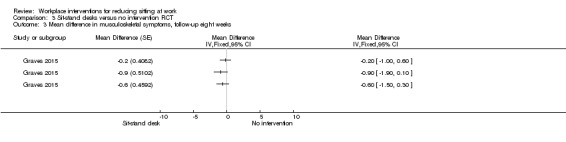
Comparison 3 Sit‐stand desks versus no intervention RCT, Outcome 3 Mean difference in musculoskeletal symptoms, follow‐up eight weeks.
Treadmill desks plus counselling versus no intervention
Outcome: Sitting time
Measured as time spent sitting at work: follow‐up at 12 weeks
In one RCT, Schuna 2014 found that a treadmill desk plus counselling reduced sitting time at work by 29 minutes per eight‐hour workday (95% CI ‐55 to ‐2) compared to no intervention at 12 weeks' follow‐up (Analysis 4.1).
Analysis 4.1.
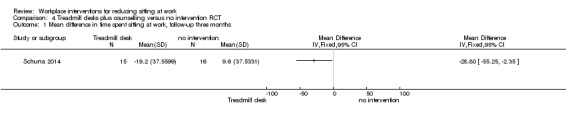
Comparison 4 Treadmill desks plus counselling versus no intervention RCT, Outcome 1 Mean difference in time spent sitting at work, follow‐up three months.
Pedalling workstations plus information and counselling versus information and counselling only
Outcome: Sitting time
Measured as time spent in inactive sitting at work: follow‐up at 16 weeks
Carr 2015 found an non‐significant decrease in inactive sitting at work by 12 minutes (95% CI ‐24 to 1) with a pedalling workstation plus information and counselling compared to information and counselling only at 16 weeks' follow‐up Analysis 5.1
Analysis 5.1.
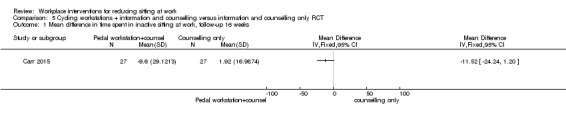
Comparison 5 Cycling workstations + information and counselling versus information and counselling only RCT, Outcome 1 Mean difference in time spent in inactive sitting at work, follow‐up 16 weeks.
Outcome: adverse events
Carr 2015 found no change in musculoskeletal discomfort over the past seven days and work productivity with a pedalling workstation plus information and counselling compared to information and counselling only at 16 weeks' follow‐up. However, the study did not report any data for these outcomes.
A policy to change organisation of work
Walking strategies versus no intervention
Outcome: sitting time
Measured as time spent sitting at work: follow‐up at 10 weeks
In a three‐armed randomised controlled trial, Gilson 2009 found a non‐significant decrease in mean sitting time at work per day (MD ‐16 minutes per day, 95% CI ‐54 to 23) in both route and incidental walking groups compared to a control group (Analysis 6.1).
Analysis 6.1.
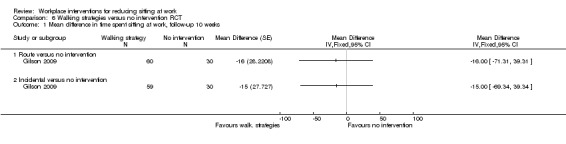
Comparison 6 Walking strategies versus no intervention RCT, Outcome 1 Mean difference in time spent sitting at work, follow‐up 10 weeks.
Measured as time spent sitting at work: follow‐up at 21 weeks
In a cluster‐randomised controlled trial, Puig‐Ribera 2015 found a non‐significant decrease in mean sitting time at work per day (MD ‐17 minutes per day, 95% Cl ‐65 to 32) following a web‐based intervention encouraging incidental walking and short walks during the working day compared to a control group at 21 weeks' follow‐up (Analysis 6.2).
Analysis 6.2.
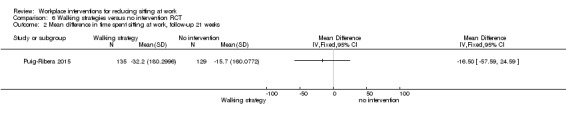
Comparison 6 Walking strategies versus no intervention RCT, Outcome 2 Mean difference in time spent sitting at work, follow‐up 21 weeks.
Information and counselling
Computer prompts plus information versus information alone
Outcome: Sitting time
Measured as time spent sitting at work: follow‐up at short term
Two studies compared point of choice prompts plus information to information only (Donath 2015; Evans 2012). Both the studies were randomised controlled trials. The pooled analysis showed that the point of choice prompt with information resulted in a non‐significant decrease of 17 minutes per workday in time spent sitting at work (95% CI ‐48 to 14) compared to information alone (Analysis 7.1).
Analysis 7.1.
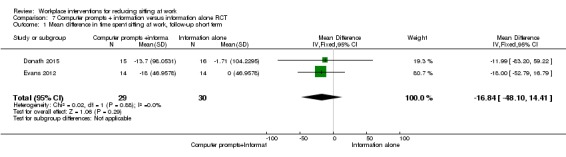
Comparison 7 Computer prompts + information versus information alone RCT, Outcome 1 Mean difference in time spent sitting at work, follow‐up short term.
Measured as time spent sitting at work: follow‐up at 13 weeks
In another randomised controlled trial, Pedersen 2013 reported a decrease in mean sitting time at work of 55 minutes per day (95% CI ‐96 to ‐14) with computer prompting plus information compared to information alone (Analysis 7.2).
Analysis 7.2.
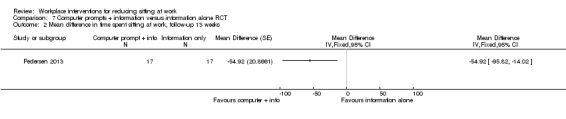
Comparison 7 Computer prompts + information versus information alone RCT, Outcome 2 Mean difference in time spent sitting at work, follow‐up 13 weeks.
Measured as number and duration of sitting episodes lasting 30 minutes or more: follow‐up at 10 days
Evans 2012 also found a small decrease of 1.1 events per day (95% CI ‐1.9 to ‐0.3) in the number of sitting episodes lasting 30 minutes or more with computer prompting plus information compared to information alone (Analysis 7.3).
Analysis 7.3.
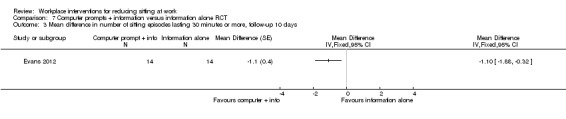
Comparison 7 Computer prompts + information versus information alone RCT, Outcome 3 Mean difference in number of sitting episodes lasting 30 minutes or more, follow‐up 10 days.
In the same randomised controlled trial, Evans 2012 also found a reduction of 60 minutes per day in duration of sitting episodes lasting 30 minutes or more (95% CI ‐107 to ‐13) in those using computer prompts plus information compared to those given information alone (Analysis 7.4).
Analysis 7.4.
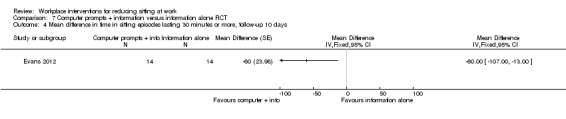
Comparison 7 Computer prompts + information versus information alone RCT, Outcome 4 Mean difference in time in sitting episodes lasting 30 minutes or more, follow‐up 10 days.
Outcome: energy expenditure at workplace
Estimated as calories: follow‐up at 13 weeks
Pedersen 2013 estimated energy expenditure at the workplace based on reported activities and found that the intervention computer prompts plus information increased energy expenditure with a non‐significant 278 kilocalories per workday (95% CI ‐556 to 0.01) compared to information alone (Analysis 7.5).
Analysis 7.5.
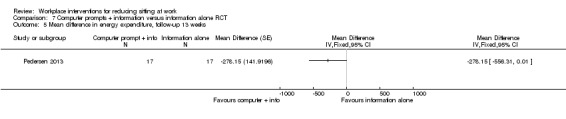
Comparison 7 Computer prompts + information versus information alone RCT, Outcome 5 Mean difference in energy expenditure, follow‐up 13 weeks.
Computer prompts to step versus computer prompts to stand
Outcome: sitting time
Measured as time spent sitting at work: follow‐up six days
Swartz 2014 found that employees receiving computer prompts to step sat 14 minutes per eight‐hour workday more at work (95% CI 10 to 19) compared to employees receiving computer prompts to stand (Analysis 8.1).
Analysis 8.1.
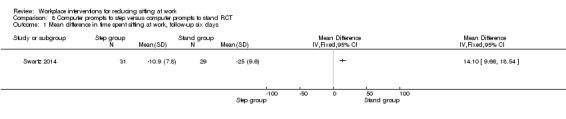
Comparison 8 Computer prompts to step versus computer prompts to stand RCT, Outcome 1 Mean difference in time spent sitting at work, follow‐up six days.
Measured as number of sitting episodes lasting 30 minutes or more: follow‐up at 6 days
In the same study Swartz 2014 found that employees in the step group had 0.4 events per day more sitting events lasting 30 minutes or more (95% CI 0.3 to 0.5) compared to employees in the stand group (Analysis 8.2).
Analysis 8.2.
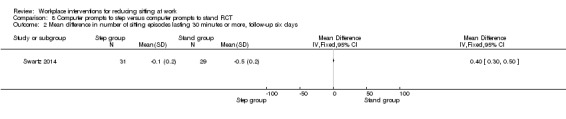
Comparison 8 Computer prompts to step versus computer prompts to stand RCT, Outcome 2 Mean difference in number of sitting episodes lasting 30 minutes or more, follow‐up six days.
E‐newsletters on workplace sitting versus e‐newsletters on health education
Outcome: sitting time
Measured as time spent sitting at work: follow‐up 10 weeks
In a randomised controlled trial, Gordon 2013 reported a non‐significant decrease in workplace sitting of six minutes per eight‐hour workday (95% Cl ‐70 to 59) following an e‐newsletter on workplace sitting compared to those receiving an e‐newsletter on health education (Analysis 9.1).
Analysis 9.1.
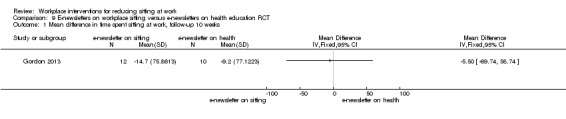
Comparison 9 E‐newsletters on workplace sitting versus e‐newsletters on health education RCT, Outcome 1 Mean difference in time spent sitting at work, follow‐up 10 weeks.
Counselling versus no intervention
Outcome: sitting time
Measured as time spent sitting at work: follow‐up at medium term
Two studies compared counselling to no intervention (Coffeng 2014; Verweij 2012). Both the studies were cluster‐randomised controlled trials. The pooled analysis showed that counselling reduced sitting time at work by 28 minutes per day (CI ‐52 to ‐5, Analysis 10.1).
Analysis 10.1.
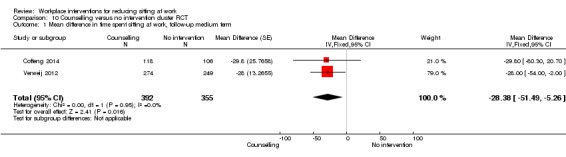
Comparison 10 Counselling versus no intervention cluster RCT, Outcome 1 Mean difference in time spent sitting at work, follow‐up medium term.
Measured as total time spent in sitting at and outside work: follow‐up at six months
Verweij 2012 also reported a non‐significant decrease of 20 minutes per day (95% CI ‐85 to 45) in total sitting time with guideline‐based counselling by an occupational physician compared to usual care by an occupational physician (Analysis 10.2).
Analysis 10.2.
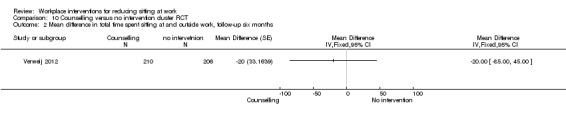
Comparison 10 Counselling versus no intervention cluster RCT, Outcome 2 Mean difference in total time spent sitting at and outside work, follow‐up six months.
Outcome: adverse events
The Coffeng 2014 study reported no difference in work engagement (0.1 score points; 95% CI ‐0.1 to 0.3; on a scale of 0 to 6) at 12 months' follow‐up (Analysis 10.3).
Analysis 10.3.
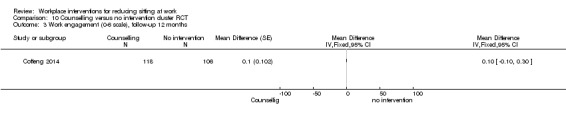
Comparison 10 Counselling versus no intervention cluster RCT, Outcome 3 Work engagement (0‐6 scale), follow‐up 12 months.
Mindfulness training versus no intervention
Outcome: sitting time
Measured as time spent sitting at work: follow‐up at six months
In a randomised controlled trial, van Berkel 2014 found that mindfulness training did not reduce sitting time at work (MD ‐2 minutes per day 95% CI ‐22 to 18) compared to no intervention at six‐month follow‐up (Analysis 12.1).
Measured as time spent sitting at work: follow‐up at 12 months
In the same study, van Berkel 2014 observed that the reduction was still non‐significant at 12 months' follow‐up (MD ‐16 minutes per day, 95% CI ‐45 to 12; Analysis 11.2).
Analysis 11.2.
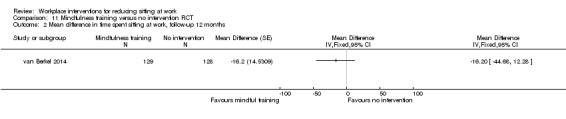
Comparison 11 Mindfulness training versus no intervention RCT, Outcome 2 Mean difference in time spent sitting at work, follow‐up 12 months.
Outcome: adverse events
The van Berkel 2014 study reported no difference in work engagement (on a scale of 0 to 6) at the six‐month follow‐up (0.1 score points; 95% CI ‐0.2 to 0.4; Analysis 11.3), and at 12 months' follow‐up (0.2 score points; 95% CI ‐0.1 to 0.5; Analysis 11.4). Work engagement was assessed using the Utrecht Work Engagement Scale, which is a self‐reported questionnaire that measures three aspects of engagement: vigour, dedication and absorption.
Analysis 11.3.
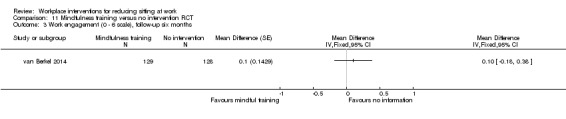
Comparison 11 Mindfulness training versus no intervention RCT, Outcome 3 Work engagement (0 ‐ 6 scale), follow‐up six months.
Analysis 11.4.
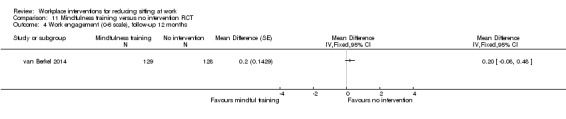
Comparison 11 Mindfulness training versus no intervention RCT, Outcome 4 Work engagement (0‐6 scale), follow‐up 12 months.
Multiple category interventions
Multiple interventions versus no intervention
Outcome: Sitting time
Measured as time spent sitting at work: follow‐up at 12 weeks
Ellegast 2012 found a significant decrease of 117 minutes per eight‐hour workday in workplace sitting (95% CI ‐168 to ‐67) with multiple interventions compared to no intervention at 12 weeks' follow‐up (Analysis 12.3). The Ellegast 2012 study reported percentage reduction in time spent sitting at work which we converted into minutes per eight‐hour workday.
Analysis 12.3.
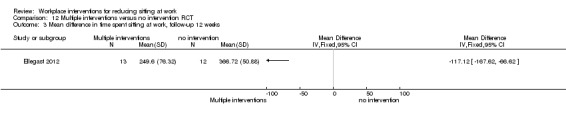
Comparison 12 Multiple interventions versus no intervention RCT, Outcome 3 Mean difference in time spent sitting at work, follow‐up 12 weeks.
Measured as time spent sitting at work: follow‐up at six months
Coffeng 2014 found a significant decrease of 61 minutes per day in workplace sitting (95% CI ‐115 to ‐7) with multiple environmental interventions with or without counselling compared to no intervention at six months' follow‐up (Analysis 12.1).
Analysis 12.1.
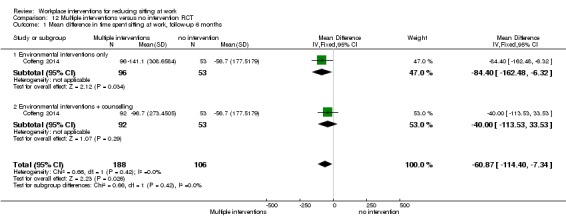
Comparison 12 Multiple interventions versus no intervention RCT, Outcome 1 Mean difference in time spent sitting at work, follow‐up 6 months.
Measured as time spent sitting at work: follow‐up at 12 months
Coffeng 2014 found a non‐significant decrease of 48 minutes per day in workplace sitting (95% CI ‐103 to 7) following multiple environmental interventions with or without counselling compared to no intervention at 12 months' follow‐up (Analysis 12.2).
Analysis 12.2.
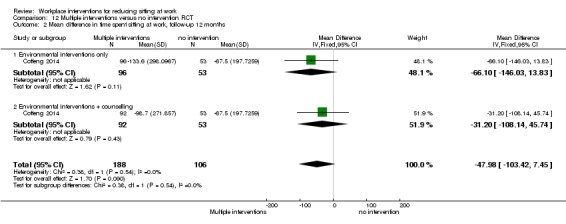
Comparison 12 Multiple interventions versus no intervention RCT, Outcome 2 Mean difference in time spent sitting at work, follow‐up 12 months.
Outcome: adverse events
The Coffeng 2014 study reported no change in score points (95% CI ‐0.14 to 0.14) in work engagement (on a scale of 0 to 6) with multiple environmental interventions with or without counselling compared to no intervention at 12 months' follow‐up (Analysis 12.4).
Analysis 12.4.
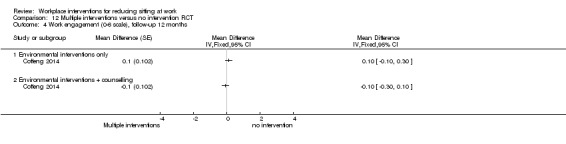
Comparison 12 Multiple interventions versus no intervention RCT, Outcome 4 Work engagement (0‐6 scale), follow‐up 12 months.
Discussion
Summary of main results
We included 20 studies, two cross‐over RCTs, 11 RCTs, three cRCTs and four CBAs, with a total of 2174 participants. All studies had been conducted in high income countries (Australia, USA, and various European countries). Nine studies evaluated physical workplace changes, two policy changes, seven information and counselling and two multiple category interventions for decreasing workplace sitting.
Physical workplace changes
Sit‐stand desks
According to six studies, providing workers with sit‐stand desks alone reduces workplace sitting at short‐term (three months' follow‐up) from at least 33 minutes up to 137 minutes per eight‐hour workday compared to no intervention but the magnitude of the effect is inconsistent and the quality of evidence is very low. In two studies, providing workers with both sit‐stand desks and counselling reduced sitting during an eight‐hour workday in the same range (MD ‐113 minutes, 95% CI ‐143 to ‐84, very low quality evidence) at short‐term follow‐up. In one study the reduction in sitting time was 56 minutes (95% CI ‐101 to ‐12, very low quality evidence) at six months' follow‐up. In one study also total sitting time at work and outside work decreased with sit‐stand desks compared to no intervention (MD ‐78 minutes, 95% CI ‐125 to ‐31). Acording to two studies, sit‐stand desks also reduced the amount of time in episodes of prolonged sitting by 52 minutes (95% CI ‐79 to ‐26). This is still less than the two to four hours of standing promoted by a group of experts.
As to the secondary outcomes, none of the included studies measured energy expenditure with sit‐stand desks. There was no evidence of a significant increase in musculoskeletal symptoms in four studies that evaluated sit‐stand desks even though the magnitude of the effect was variable and there was a decrease in some studies. There was neither evidence of an increase or a decrease in work productivity as a result of using sit‐stand desks.
Active workstations
There was inconsistent evidence for active workstations. In one study a cycle workstation did not have a considerable effect on inactive sitting time at work at 16 weeks' follow‐up (MD ‐12 minutes, 95% CI ‐24 to 1, low quality evidence). In another study a treadmill workstation led to a 28‐minute reduction (95% CI ‐55 to ‐2, low quality evidence) in workplace sitting at three months' follow‐up.
Policies to change organisation of work
Two studies with 443 participants provided low quality evidence that walking strategies did not have a considerable effect on workplace sitting time at 10 weeks' (MD ‐16 minutes, 95% CI ‐54 to 23) or 21 weeks' (MD ‐17 minutes, 95% CI ‐58 to 25) follow‐up respectively.
Information and counselling
In two studies, counselling alone reduced sitting time at work by 28 minutes per day (CI ‐52 to ‐5, low quality evidence) at medium term follow‐up. Another study yielded low quality evidence that mindfulness training did not change workplace sitting time significantly at either the six‐month (MD ‐2 minutes, 95% CI ‐22 to 18) or 12‐month follow‐up (MD ‐16 minutes, 95%CI ‐45 to 12). In the counselling studies, there was no considerable increase in work engagement in two studies.
In one study, an e‐newsletter on workplace sitting did not show a considerable reduction in sitting time at work (MD ‐6 minutes 95% CI ‐70 to 59, low quality evidence) compared to those who received an e‐newsletter on health education.
Computer prompting plus information had no significant effect on time spent sitting at work (MD ‐17 minutes, 95% CI ‐48 to 14, two studies) at short term follow‐up. Another study showed that computer prompting plus information significantly reduced sitting time at work by 55 minutes per day (95% CI ‐96 to ‐14) at 13 weeks' follow‐up. However the quality of evidence was low for computer prompting plus information.
Yet another study reported that prompts to stand reduced sitting time at work more than prompts to step (MD 14 minutes, 95% CI 10 to 19).
Interventions from multiple categories
When interventions from multiple categories were combined to reduce sitting, there was a significant reduction in sitting time at 12 weeks' (MD ‐117 minutes, 95% CI ‐168 to ‐67, very low quality evidence) and six months' (MD ‐61 minutes, 95% CI ‐115 to ‐7, low quality evidence) follow‐up in two studies but not at 12 months' follow‐up in one study (MD ‐48 minutes, 95% CI ‐103 to 8, low quality evidence).
Overall completeness and applicability of evidence
In total we included 20 studies assessing various kind of interventions for decreasing sitting at the workplace. Most studies assessed sit‐stand desks, and the results of our review largely concern them. There were no RCTs or CBA studies that assessed the effects of interventions such as periodic breaks or standing or walking meetings to reduce sitting at work.
The included studies were all from Australia, Europe and USA. We could not find any studies to include from other continents, or from low‐ and middle‐income countries. So it is difficult to generalise the findings of this review beyond the settings in which these interventions have been evaluated. This is partly because work environments and norms vary greatly across the globe, and the acceptability and feasibility of workplace interventions pertaining to sitting work may differ accordingly. Since obesity and other lifestyle diseases are common in high income countries of the west, most studies were from these regions. However since these diseases are now becoming more prevalent in some regions of Asia too (Tan 2011; Wang 2011), it is important that the effectiveness of these interventions is tested on office employees also in these regions.
Almost all studies had a very short to short term follow‐up. There were no studies with a long‐term follow‐up of more than one year. It is important to demonstrate that behaviour change from sitting to a more active behaviour is sustainable in the long‐term. The investment in sit‐stand desks can be considerable but is much less if the effects can be sustained in the long‐term.
The population of participants in the included studies consisted of office workers of a research institution, an academic institution, a government agency, a police organisation and private organisations. We believe that the population is largely representative of office workers who spend a large proportion of their working time seated and who are in need of interventions to decrease sitting at the workplace.
Although individually focused interventions such as sit‐stand workstations are very popular, they are considerably more expensive than standard workstations, so their deployment may not be feasible in many workplaces particularly in small offices or resource constrained settings. Standing meetings can be an alternative low cost option that provides an opportunity to every employee to use these sit‐stand workstations during meetings and so to reduce their sitting time (Atkinson 2014). Posters or prompting to stand up or engage in light to moderate intensity physical activity, or placing printers or dust‐bins away from desks could also be feasible lower cost interventions for larger populations of employees. There is some evidence available for breaking up sitting time with intermittent brief bouts of light‐intensity or moderate‐intensity physical activity (Bailey 2015; Larsen 2014), but mainly from experiments with obese and non obese adults. We still do not know if this is applicable to workplaces, So there is a need for these low cost interventions to be evaluated in future trials.
Interventions should also take advantage of changes in the built and social environments, in the use of social networks, and the promotion of relevant public policy changes. Traditional strategies of behaviour change that require cognitive awareness might need to be complemented with interventions that address automatic habitual action (or inaction). Health messaging can play an important role when it matches the individual’s characteristics, emphasizing the benefits and target self‐efficacy beliefs that encourage participation (Manini 2015).
Quality of the evidence
Most included studies were randomised controlled trials or cluster‐randomised trials but the risk of bias was high in most of these and therefore the quality of evidence is low to very low. In an occupational health setting with complex interventions, the random allocation and its concealment is known to be more difficult than for a trial in a hospital setting. And yet three of the included studies managed to achieve it. Unless sample sizes are large enough, the random allocation does not spread the confounders equally across groups, and therefore randomisation is not very effective in studies as small as those included in our review. Similarly the self‐evident nature of the intervention makes it difficult to blind personnel and participants in these scenarios.
Risk of bias for objectively measured sitting time by inclinometer differs from self‐reported sitting time. It is not possible to misreport the outcomes when sitting time is measured by an accelerometer coupled with an inclinometer, whereas with self‐reported sitting time, participants may be aware of the goals of intervention and overestimate or underestimate the effect.
Alkhajah 2012 and Neuhaus 2014a were not RCTs as stated a priori because they randomised only two groups. The trial authors described them as quasi‐RCTs. The risk of baseline differences is much higher for such studies with only two clusters, so we believe that it is fairer to categorise these studies as CBA studies rather than RCTs. We addressed the baseline imbalances for both studies in our risk of bias assessment.
Although studies performed poorly on the allocation concealment and blinding of participants and personnel domains, most studies assessed the outcomes in a way that we judged to have a low risk of bias. Therefore, we rated the overall quality of the evidence as very low to low.
Potential biases in the review process
We did not exclude articles published in languages other than English. Therefore, we avoided language bias in our review.
We searched sources of grey literature and sought unpublished studies and data to avoid publication bias. We had planned to assess publication bias using funnel plots, but we found too few studies per outcome. However, as most included studies were small and all reported positive outcomes, it is conceivable that there may be publication bias in this area. If more studies are included in a future update, we will assess the extent of publication bias by means of funnel plots and Egger's test (Egger 1997).
Agreements and disagreements with other studies or reviews
Recently, many systematic reviews have been published on interventions for reducing sedentary behaviour (Chau 2010; Commissaris 2015; Gardner 2015; Karakolis 2014; MacEwen 2015; Martin 2015; Neuhaus 2014b; Prince 2014; Tew 2015; Torbeyns 2014; Tudor‐Locke 2013 and VicHealth 2012).
Chau 2010 found studies that used e‐health interventions, walking groups and educational counselling. The review included six studies, but only one specifically measured sitting time at work, which is our primary outcome, and concluded that there is a dearth of evidence on the effectiveness of workplace interventions for reducing sitting. Since Chau 2010 was published, the number of studies that measured effects of interventions to reduce sitting at work has increased. VicHealth 2012 included 13 studies that reported various outcomes relating to workplace sitting, such as number of breaks in sedentary time, musculoskeletal symptoms, eye strain and work productivity, but no studies that measured reduction in sitting time at work. Therefore, it is not possible to compare our findings with this review. We performed a formal risk of bias assessment of the included studies and incorporated these assessments into the analysis and the conclusions we drew, whereas Chau 2010 and VicHealth 2012 did neither. We consider this very important, as the quality of the included studies is known to affect the effect size. Risk of bias especially in the outcome assessment domain was the major factor in drawing clear conclusions in this Cochrane review.
Neuhaus 2014b (38 included studies), Torbeyns 2014 (30 included studies) and Tew 2015 (five included studies) evaluated the effectiveness of active workstations on sedentary time at work. Neuhaus 2014b included laboratory based studies whereas Torbeyns 2014 included studies that evaluated outcomes other than sitting at work and both studies also included non‐randomised and uncontrolled studies. Neuhaus 2014b and Torbeyns 2014 concluded that installation of active workstations at offices is a feasible means to reduce time spent sitting at work, whereas Tew 2015 concluded that most studies conducted on height adjustable workstations had methodological shortcomings so high quality randomised controlled trials are needed to help determine the impact of height‐adjustable workstation interventions on occupational sedentary behaviour, both in the short and long term. In Neuhaus 2014b and Torbeyns 2014, even the non‐randomised studies received a moderate to high quality score which is not possible with the Cochrane risk of bias tool. Overall, Tew 2015 and our Cochrane review yielded findings that were considerably different from the other two reviews. Martin 2015 (51 included studies) and Prince 2014 (65 included studies) assessed the effectiveness of interventions to reduce sedentary behaviour in adults at the workplace as well as at other settings. Both reviews concluded that it was possible to reduce sedentary behaviour in adults by interventions that aim to reduce sedentary behaviour. A recent systematic review by Commissaris 2015 (40 studies) assessed the effectiveness of workplace interventions to change employees’ sedentary behaviour or physical activity or both. This review found strong evidence for a decrease in sedentary behaviour with the use of alternative workstations and does not resemble our findings of very low to low quality evidence for alternative workstations.
Another recent systematic review by Gardner 2015 (26 included studies) looked into the behavior change strategies adopted by sedentary behaviour interventions using the Behavior Change Wheel. It found that using more techniques made the interventions more promising in terms of an effect. The most frequently observed behaviour change techniques were setting behavioural goals, providing social support, and environmental interventions. Gardner 2015 found two workplace interventions to be promising: environmental intervention and education. Only the first finding is in line with the finding of our Cochrane review. Karakolis 2014 concluded that sit‐stand desks are effective in reducing perceived discomfort and do not decrease productivity. Similarly MacEwen 2015 concluded that there is a substantial evidence gap on health benefits of sit‐stand desks and tread‐mill desks and Tudor‐Locke 2013 concluded that workstation alternatives have potential in mitigating diminished energy expenditure in desk‐based employees. However these three reviews did not evaluate reduction in sitting time, which is our main outcome.
The differences in energy expenditure between sitting and standing are minor. Mansoubi 2015 found that sitting typing tasks reached an energy expenditure of 1.45 MET (SD 0.32), whereas standing only reached 1.59 MET (SD 0.37). On the other hand, more active sitting tasks such as playing on the Wii reached 2.06 METS (SD 0.5). And walking MET values increased incrementally with speed from 2.17 MET (SD 0.5) at 0.2 miles/hour to 3.22 (SD 0.69) at 1.6 miles/hour. It is also clear that using more dynamic workstations increases energy costs considerably.For example, using a desk bike type workstation at light intensity reaches 2.4 MET (Botter 2015). Mansoubi 2015 therefore questions if the perceived positive benefits of reduced sedentary behavior are primarily driven by increases in energy expenditure that accompany the transition into light activity (e.g. playing on the Wii), or to differences in postural allocation (e.g. standing), or a combination of both (e.g. walking and cycling). This should be further investigated.
Aiming to reduce obesity or overweight by standing up at work is not however realistic. Júdice 2015b found only a marginally higher additional metabolic cost for standing. In theory if an average man and woman spent 50% of an eight‐hour working day standing, he would spend an additional 20 kcal and she would spend an additional 12 kcal per working day. However, in this Cochrane review, we calculated that after three months a sit‐stand desk combined with counselling reduced sitting time only by 113 minutes, so the additional energy expenditure is negligible. Also Chaput 2015 mentions that greater occupational standing time is not sufficient to prevent the development of overweight, obesity, an impaired glucose tolerance or type 2 diabetes.
Katzmarzyk 2014 suggests that standing may not be a hazardous form of behaviour. Given that mortality rates decline at higher levels of standing, standing may be a healthier alternative to excessive periods of sitting. However, promoting sustained standing is also not the solution. Andersen 2007 reports musculoskeletal symptoms with prolonged standing. Furthermore, Coenen 2015 mentions that an intervention with increased standing and reduced sitting was less effective for people with low back pain. When standing becomes a burden is not yet known, but promoting four hours of standing per day during work hours could have negative consequences for specific groups. For instance, elderly workers complain when performing standing work, even if it is less than 50% of their working time (Graf 2015).
Authors' conclusions
For changes in the physical environment, there was very low quality evidence that the use of sit‐stand desks can reduce workplace sitting time with about 30 minutes to two hours at short term follow‐up. This is considerably less than the two to four hours recommended by experts.There was no considerable effect on musculoskeletal symptoms or on work performance neither in a harmful nor in a beneficial way. There is no evidence on longer term effects. It is unclear if standing can repair the harms of sitting because there is hardly any extra energy expenditure. The effects of active workstations were inconsistent: a treadmill workstation reduced inactive sitting time but a cycle workstation did not.
For policies to change the organisation of work there were no effects or they were inconsistent. Walking strategies had no effect on workplace sitting, while computer prompting plus information had an inconsistent effect on workplace sitting. There was low quality evidence for a small reduction in workplace sitting with counselling and no considerable effect of mindfulness training on sitting time.
For interventions combining multiple approaches, there was inconsistent effect on sitting time with a significant reduction at 12 weeks' and six months' follow‐up but not at 12 months' follow‐up.
For physical changes of the workplace, we need studies on sit‐stand desks with larger sample sizes and longer duration of follow‐up and studies on active workstations. To prevent contamination, we recommend randomising employees in a cluster‐randomised design with at least two intervention sites and two control sites, but preferably many more, to minimise confounding by workplace‐specific variables (EPOC). Even when employees are not explicitly told which group they are in, true blinding is not possible, as intervention activities will be noticeable at intervention work sites (McEachan 2011).
We recommend conducting trials aimed at reducing sitting at work also in low and middle income nations where the burden of non‐communicable diseases is increasing slowly. All participants, irrespective of the nature of intervention, should receive information regarding the adverse effects of prolonged sitting.
For policies to change the organisation of work, there is a need to conduct trials on low cost interventions (standing meetings, posters or prompts for standing, printers or dust‐bins placed further) for decreasing sitting, which would be very useful particularly in small offices and resource scarce settings. It would be helpful to first better understand the ideas that workers and employers have about sitting and means to decrease sitting. This could help to develop better interventions. There is qualitative research available that should be summarised in a systematic review.
Future studies should measure the time spent sitting at work by means of a thigh mounted accelerometer‐inclinometer with a data reduction approach that estimates inclination from triaxial data. This is because the thigh is the segment of the body that changes position when shifting from sitting to standing (Janssen 2015). We do not recommend the use of self‐reported measures alone, as the validity of these measures is unclear (Aadahl 2003; Lagersted‐Olsen 2014). Moreover, participants receiving the intervention would be aware of the goals set and the intention of the intervention, and would be therefore likely to underestimate or overestimate sitting time when reporting it themselves (Rzewnicki 2003; Shephard 2003). Furthermore, if the intervention is found to be effective at reducing sitting, future studies should try to examine what replaced sitting time (i.e. standing, light intensity physical activity, or moderate to vigorous intensity physical activity). Reducing sitting time at work is important, but compensatory mechanisms outside work, for example more sitting during leisure, might result in no net change in total sitting time (Mansoubi 2015b). Hence, it is important that intervention studies also assess total sitting time at work and outside work. We recommend including outcome measures that will be of interest to employers, such as valid and reliable measures of productivity, job stress and absenteeism as well as cardio‐metabolic health benefits. Future studies should also include cost‐effectiveness analyses to help stakeholders and decision makers to determine whether the cost of these interventions to reduce sitting at work is justified by improvements in health and work‐related outcomes.
The effect of the intervention could then be measured as the mean difference in the time spent sitting at work in the intervention group compared to the control group. The effect should be statistically adjusted for the clustering effect. The overall sample size, and also the number of clusters should be taken into account while recruiting participants in order to calculate the statistical power and the size of study groups.
The ongoing studies that we found studied sit‐stand desks, treadmill desks, walking strategies, motivational prompts, information and counselling. There are still no randomised trials set in ordinary workplaces for other interventions such as sitting diaries, stepping devices, periodic breaks to interrupt sitting, or standing or walking meetings.
Three ongoing studies have been designed according to our recommendations (Dunstan 2014; NCT01996176, O’Connell 2015). All three are cluster‐randomised controlled trials and will have at least two intervention and two control sites. Dunstan 2014 and O’Connell 2015 have planned to assess the effectiveness of sit‐stand or height adjustable workstations while the NCT01996176 study will assess the effectiveness of an intervention consisting of walking strategies, standing meetings and motivational prompts. All three studies have planned to measure sitting at work with an accelerometer‐inclinometer.
Acknowledgements
We thank Jani Ruotsalainen, Managing Editor, Cochrane Work Group for providing administrative and logistical support for the conduct of the current review, and Kaisa Neuvonen, Trials Search Co‐ordinator, Cochrane Work Group for developing and executing the search strategies.
We would also like to thank the Cochrane Work Group's Editors Esa‐Pekka Takala and Anneli Ojajärvi and external peer referees Kimi Sawada, Kristel King, Rintaro Mori and Hidde van der Ploeg for their comments. We thank Joey Kwong, Elizabeth Royle and Jani Ruotsalainen for copy editing the text.
We also like to thank Suresh Kumar and Chukwudi P Nwankwo for their contribution in the previous version of this review.
We would also like to thank all who donated in the crowdfunding campaign to support the review.
Appendices
Appendix 1. CENTRAL search strategy
#1 work*
#2 sedentary
#3 sitting
#4 #2 or #3
#5 office
#6 inactiv*
#7 #5 and #6
#8 #4 or #7
#9 #1 and #8
#10 #9 AND trials
Appendix 2. MEDLINE (PubMed) search strategy
#1 (work[tw] OR works*[tw] OR work'*[tw] OR worka*[tw] OR worke*[tw] OR workg*[tw] OR worki*[tw] OR workl*[tw] OR workp*[tw] OR occupation*[tw] OR employe*[tw])
#2 (effect*[tw] OR control[tw] OR controls*[tw] OR controla*[tw] OR controle*[tw] OR controli*[tw] OR controll*[tw] OR evaluat*[tw] OR intervention*[tw] OR program*[tw] OR compare*[tw])
#3 (sedentary OR sitting) OR seated posture OR chair[tiab] OR desk[tiab] OR (office AND inactiv*)
#4 (animals [mh] NOT humans [mh])
#5 #1 AND #2 AND #3 NOT #4
Appendix 3. CINAHL search strategy
S10 S1 AND S2 AND S9 Limiters ‐ Exclude MEDLINE records Search modes ‐ Boolean/Phrase
S9 S3 OR S4 OR S5 OR S6 OR S7 OR S8
S8 (office AND inactive*) or TX (office AND inactive*) or MW (office AND inactive*)
S7 Desk or TX desk or MW desk
S6 Sedentary or TX sedentary or MW sedentary
S5 Seated posture or TX seated posture or MW seated posture
S4 Sitting or TX sitting or MW sitting
S3 Chair or TX chair or MW chair
S2 TX randomised controlled trial or TX controlled clinical trial or AB placebo or TX clinical trials or AB randomly or TI trial or TX intervent* or control* or evaluation* or program*
S1 work* OR (offic* OR busines*) OR occupat*
Appendix 4. OSH update search strategy
#1 DC{OUCISD OR OUHSEL OR OUNIOC OR OUNIOS OR OURILO}
#2 GW{office AND inactiv*}
#3 GW{sitting OR sedentary}
#4 TW{work*}
#5 #2 OR #3
#6 #4 AND #5
#7 #1 AND #6
Appendix 5. EMBASE search strategy
#1 sedentary
#2 'sitting'/de
#3 'seated posture'
#4 seated NEAR/1 posture
#5 chair:ab,ti OR desk:ab,ti
#6 chair:ab,ti
#7 desk:ab,ti
#8 office AND inactiv*
#9 #1 OR #2 OR #4 OR #6 OR #7 OR #8
#10 'work'/de OR work
#11 work*
#12 'occupation'/de OR occupation
#13 employe*
#14 #10 OR #12 OR #13
#15 effect
#16 control
#17 evaluat*
#18 intervention*
#19 program
#20 compare
#21 #15 OR #16 OR #17 OR #18 OR #19 OR #20
#22 #9 AND #14 AND #21
#23 #22 AND [embase]/lim
#24 #23 AND [humans]/lim AND [embase]/lim
Appendix 6. PsycINFO (ProQuest)
S25 S13 AND S17 AND S24
S24 S18 OR S19 OR S20 OR S21 OR S22 OR S23
S23 compare
S22 program
S21 intervention*
S20 evaluat*
S19 control
S18 effect
S17 S14 OR S15 OR S16
S16 employe*
S15 occupation
S14 work
S13 S1 OR S2 OR S4 OR S8 OR S11 OR S12
S12 office AND inactive*
S11 S9 OR S10
S10 ab(desk)
S9 ti(desk)
S8 S6 OR S7
S7 ti(chair)
S6 ab(chair)
S5 ab(chair) OR ti(chair)
S4 seated NEAR/1 posture
S3 seated posture
S2 sitting
S1 sedentary
Appendix 7. ClinicalTrials.gov
Sitting AND Workplace
Appendix 8. World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal
Sitting AND Workplace
Data and analyses
Comparison 1.
Sit‐stand desks with or without counselling versus no intervention CBA
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up three months | 2 | Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 1.1 Sit‐stand desk + information and counselling | 2 | 61 | Mean Difference (Fixed, 95% CI) | ‐113.07 [‐142.59, ‐83.55] |
| 2 Mean difference in time spent sitting at work. follow‐up six months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Mean difference in time in sitting episodes lasting 30 minutes or more, follow‐up three months | 2 | 74 | Mean Difference (Fixed, 95% CI) | ‐52.33 [‐78.56, ‐26.11] |
| 3.1 Sit‐stand desk only | 1 | 20 | Mean Difference (Fixed, 95% CI) | ‐13.00 [‐70.80, 40.80] |
| 3.2 Sit‐stand desk + information and counselling | 2 | 54 | Mean Difference (Fixed, 95% CI) | ‐62.92 [‐92.62, ‐33.21] |
| 4 Mean difference in total time spent sitting at and outside work, follow‐up three months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 5 Work performance (1‐10 scale), follow‐up three months | 3 | 109 | Mean Difference (Random, 95% CI) | 0.35 [‐0.10, 0.79] |
| 5.1 Sit‐stand desk only | 2 | 52 | Mean Difference (Random, 95% CI) | 0.82 [0.00, 1.63] |
| 5.2 Sit‐stand desk + information and counselling | 2 | 57 | Mean Difference (Random, 95% CI) | 0.15 [‐0.38, 0.68] |
| 6 Proportion with ≥ 1 sick days in the last three months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Proportion with ≥ 1 sick days in the last month | 2 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.49, 1.21] |
| 7.1 Sit‐stand desk only | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.42, 2.13] |
| 7.2 Sit‐stand desk + information and counselling | 2 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.41, 1.24] |
| 8 Musculoskeletal symptoms | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected |
Analysis 1.8.
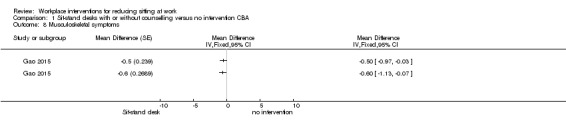
Comparison 1 Sit‐stand desks with or without counselling versus no intervention CBA, Outcome 8 Musculoskeletal symptoms.
Comparison 2.
Sit‐stand desks +counselling versus sit‐stand desks CBA
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up three months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 2 Mean difference in time in sitting episodes lasting ≥ 30 minutes, follow‐up three months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 3 Work performance (1‐10 scale), follow‐up three months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 4 Proportion with ≥ 1 sick days in the last month | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3.
Sit‐stand desks versus no intervention RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow up short term | 2 | 70 | Mean Difference (Fixed, 95% CI) | ‐96.35 [‐109.55, ‐83.15] |
| 2 Mean difference in time spent sitting at work, follow‐up eight weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Mean difference in musculoskeletal symptoms, follow‐up eight weeks | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected |
Comparison 4.
Treadmill desks plus counselling versus no intervention RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up three months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 5.
Cycling workstations + information and counselling versus information and counselling only RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent in inactive sitting at work, follow‐up 16 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 6.
Walking strategies versus no intervention RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up 10 weeks | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 1.1 Route versus no intervention | 1 | Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Incidental versus no intervention | 1 | Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Mean difference in time spent sitting at work, follow‐up 21 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 7.
Computer prompts + information versus information alone RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up short term | 2 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐16.84 [‐48.10, 14.41] |
| 2 Mean difference in time spent sitting at work, follow‐up 13 weeks | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 3 Mean difference in number of sitting episodes lasting 30 minutes or more, follow‐up 10 days | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 4 Mean difference in time in sitting episodes lasting 30 minutes or more, follow‐up 10 days | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 5 Mean difference in energy expenditure, follow‐up 13 weeks | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected |
Comparison 8.
Computer prompts to step versus computer prompts to stand RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up six days | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Mean difference in number of sitting episodes lasting 30 minutes or more, follow‐up six days | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 9.
E‐newsletters on workplace sitting versus e‐newsletters on health education RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up 10 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 10.
Counselling versus no intervention cluster RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up medium term | 2 | 747 | Mean Difference (Fixed, 95% CI) | ‐28.38 [‐51.49, ‐5.26] |
| 2 Mean difference in total time spent sitting at and outside work, follow‐up six months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 3 Work engagement (0‐6 scale), follow‐up 12 months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected |
Comparison 11.
Mindfulness training versus no intervention RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up six months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 2 Mean difference in time spent sitting at work, follow‐up 12 months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 3 Work engagement (0 ‐ 6 scale), follow‐up six months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 4 Work engagement (0‐6 scale), follow‐up 12 months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected |
Analysis 11.1.
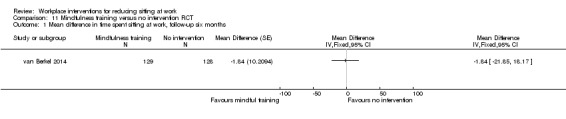
Comparison 11 Mindfulness training versus no intervention RCT, Outcome 1 Mean difference in time spent sitting at work, follow‐up six months.
Comparison 12.
Multiple interventions versus no intervention RCT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up 6 months | 1 | 294 | Mean Difference (IV, Fixed, 95% CI) | ‐60.87 [‐114.40, ‐7.34] |
| 1.1 Environmental interventions only | 1 | 149 | Mean Difference (IV, Fixed, 95% CI) | ‐84.40 [‐162.48, ‐6.32] |
| 1.2 Environmental interventions + counselling | 1 | 145 | Mean Difference (IV, Fixed, 95% CI) | ‐40.0 [‐113.53, 33.53] |
| 2 Mean difference in time spent sitting at work, follow‐up 12 months | 1 | 294 | Mean Difference (IV, Fixed, 95% CI) | ‐47.98 [‐103.42, 7.45] |
| 2.1 Environmental interventions only | 1 | 149 | Mean Difference (IV, Fixed, 95% CI) | ‐66.1 [‐146.03, 13.83] |
| 2.2 Environmental interventions + counselling | 1 | 145 | Mean Difference (IV, Fixed, 95% CI) | ‐31.20 [‐108.14, 45.74] |
| 3 Mean difference in time spent sitting at work, follow‐up 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Work engagement (0‐6 scale), follow‐up 12 months | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 4.1 Environmental interventions only | 1 | Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Environmental interventions + counselling | 1 | Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
What's new
| Date | Event | Description |
|---|---|---|
| 18 February 2016 | New citation required and conclusions have changed | New studies incorporated into review |
| 2 June 2015 | New search has been performed | Searches updated |
Differences between protocol and review
Even though in the protocol we stated that in cases where we would include more than one comparison from a trial with multiple arms in the same meta‐analysis, we would halve the numbers of control group participants to prevent them from being included twice, this does not work for the inverse variance input method. Neuhaus 2014a reported only the results from Ancova and could not provide us with the raw data. For this trial we modelled the means and standard deviations from the intervention and the control group in RevMan as closely to the real data as possible to achieve the same mean difference and standard error. Then we halved the number of participants in the control group and entered the resulting standard errors into RevMan.
We judged studies to be at low risk for selective outcome reporting if the final publications of the trial reported what had been planned and registered in international databases (trial registries), such as ClinicalTrials.gov, ANZCTR.org.au (Australia and New Zealand), NTR (Netherland’s Trial Registry). We judged those studies that were not registered in trial registries as being at low risk for selective outcome reporting if they reported all the outcomes mentioned in the methods section.
Initially we planned to pool interventions that were categorised under broad headings like physical changes in workplace environment, policy changes and information and counselling, but later we found that the interventions were quite different from one another and decided not to combine them under these broad headings. We also added a new category consisting of approaches that used multiple categories of interventions at the same time.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Non‐random allocation by clusters: CBA Single‐blind Study duration: 3 months Drop out: 9% Location: Australia Recruitment: control group participants were recruited from locations separated from the intervention group participants by at least 1 building level |
|
| Participants |
Population: employees in public health research centres within 2 academic institutions, aged 20‐65 years Intervention group: 18 participants Control group: 12 participants Demographics: BMI: Intervention group 22.6 (SD 2.6) kg/m², Control group 21.5 (SD 2.6) kg/m² |
|
| Interventions |
Duration: 3 months Intervention: sit‐stand workstation Control: no sit‐stand workstation |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This study was funded by a University of Queensland Major Equipment and Infrastructure grant. Alkhajah was supported by a United Arab Emirates Ministry of Higher Education and Scientifıc Research Scholarship; Reeves was supported by a National Health and Medical Research Council (NHMRC) Early Career Fellowship; Eakin was supported by an NHMRC Senior Research Fellowship; Owen was supported by an NHMRC Senior Principal Research Fellowship; and Healy was supported by an NHMRC Early Career Fellowship. Authors reported no financial disclosures | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation was not done as participants in intervention and control groups were selected from different building locations |
| Allocation concealment (selection bias) | High risk | Intervention and control groups were selected from two separate locations. However no information on allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The intervention group had sit‐stand workstations installed at their workplace and received verbal instruction on their use, as well as written instructions on the correct ergonomic posture for both sitting and standing and the importance of regular postural change throughout the day. The control group had no change in workstation and participants were advised to maintain usual day‐to‐day activity. The participants were probably aware of their allocation. The authors do not report who gave the instructions to the intervention and control groups. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Sitting, standing and stepping time and sit‐to‐stand transitions were measured using a thigh‐mounted accelerometer‐inclinometer, so misreporting of these activities was not possible. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Virtually no attrition: only one participant was missing from the control group because of a malfunctioning accelerometer‐inclinometer. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. Study protocol was not available. |
| Baseline comparability/ imbalance | High risk | Baseline data for age and gender were similar. It seems probable that there were baseline imbalances in awareness and physical activity levels between intervention and control groups as participants to the intervention group were selected from an academic institution focused on sedentary behaviour research whereas participants in the control group were never involved in physical activity research. |
| Validity of outcome measure | Low risk | The accelerometer‐inclinometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation single‐blind Study duration: 8 months Drop out: 10% (Five participants were lost to follow‐up and one discontinued the intervention). Location: USA Recruitment: Participants were recruited via an electronic advertisement on the company’s wellbeing website. The advertisement included a link to an online eligibility survey. Research staff contacted interested and eligible employees via telephone to schedule a baseline testing session. |
|
| Participants |
Population: Healthy adults working in full‐time sedentary jobs at a large private company were invited to participate via an electronic advertisement on the company’s wellbeing website. They were physically inactive, overweight/obese. Intervention group: 27 participants Control group: 27 participants Demographics: Mean age: Intervention: 45.2 (SD 10.9), Control 45 (SD 10.7), 70% participants were females in both intervention and control groups BMI: Intervention 34.5 (SD 6.8) kg/m², control 33 (SD 5.6)kg/m² |
|
| Interventions |
Duration of intervention: 16 weeks Intervention: Ergonomic workstation intervention; three activity‐promoting e‐mails/week and access to a seated active workstation (elliptical machine, activeLife Trainer). Control: Ergonomic intervention and e‐mails only. |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | The second author, Dr. Christoph Leonhard owns propriety rights to the activeLife Trainer. No other financial disclosures were reported by the authors of this paper. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A 1:1 randomisation scheme was generated by the principal investigator using an online random sequence generator. |
| Allocation concealment (selection bias) | Low risk | Based on the randomisation scheme, participants were provided a sealed envelope indicating their treatment assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The envelope was provided by a research assistant who was previously unaware of the randomisation schedule. But the participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Sitting and physical activity were measured using an ankle‐worn accelerometer (GENEActiv). Participants were asked to track monitor wear time and time spent at work using an activity log. It is unlikely that results were influenced by the lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 54 of the 60 participants completed all assessments. Five were lost to follow‐up and one discontinued the intervention thus yielding a total attrition of 10%. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. |
| Baseline comparability/ imbalance | Low risk | Mean age: Intervention: 45.2 (10.9), Control 45 (10.7), 70% participants were females in both intervention and control groups, BMI: Intervention 34.5 (6.8) kg/m², control 33 (5.6)kg/m² |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation with cross‐over and wait‐list control Participants were allocated randomly by drawing from the ballot four at a time. The first four were allocated to intervention group and next four to control group for four weeks. The remaining participants were assigned to the wait‐list control condition and were placed on the waiting list in seven groups (four to five people per group). After the initial four weeks, the previous control group received the intervention with the next group from the ballot draw serving as their controls. This was repeated until all nine groups had received the intervention. Unblinded Study duration: 9 weeks Drop out: 7% Location: Australia Recruitment: project was advertised to staff as part of their workplace wellness program via internal mail, staff meetings and information fliers in the office. Staff members who were interested in participating contacted the research team and received additional project information and an expression of interest form. They could then join the study ballot by returning the expression of interest form. |
|
| Participants |
Population: staff from a non‐government health agency in New South Wales, Australia Demographics: Body mass index (kg/m²) : Underweight (<18.5): 13%, Normal range (18.5 – 24.9): 50%, Overweight (25 – 29.9): 25%, Obese (≥30): 13% |
|
| Interventions |
Duration of intervention: 9 weeks Intervention: sit‐stand workstation Control: no sit‐stand workstation |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This research was supported by funding from Heart Foundation New South Wales, and Australian National Health and Medical Research Council Program Grant (#569940). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly drawn from a ballot by a researcher in the presence of potential participants and other researchers. Participants were allocated to the intervention group, control group and wait‐list control condition. |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not possible due to the open plan nature of the study office environment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Research staff, participants, and assessors were not blinded to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As outcomes were measured with accelerometer‐inclinometers and self‐administered questionnaires, it is unlikely that results were influenced by the lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Three participants who were missing age or BMI values were not included in the analyses. Imputing values for these missing covariate values did not influence the effect of the intervention on the adjusted estimates for the outcomes, nor did it change the effects age or BMI had on the outcome. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | Since the trial used a cross‐over design, all the participants would receive the interventions at some point. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation in clusters Location: Amsterdam, the Netherlands Recruitment: a top‐down communication approach was used, starting with the management • An explanatory meeting with team leaders • Invitation to all employees from the department to participate in the study • Data on sick leave, salary and the duration of employment was obtained through the Human Resource Management department | |
| Participants |
Population description: office employees (18 years or above), working at the Dutch financial service provider Demographics: Age in years: GMI 43.6 (SD 10.3); Environmental modification 42.2 (SD 10.5); GMI + Environmental modification 38.0 (SD 10.5); no intervention 40.7 (SD 9.2) Male [n (%)]: GMI 73 (SD 61.9); Environmental modification 60 (SD 62.5); GMI + Environmental modification 51 (SD 55.4); no intervention 65 (SD 61.3) |
|
| Interventions |
Duration of intervention: Environmental modification: 12 months and GMI: 3.5 months The Be Active & Relax program was evaluated using 4 arms: • GMI (group motivational interviewing) and environmental modifications (3 clusters 92 employees); Group Motivational Interviewing (GMI) derived from Motivational Interviewing (MI). Motivational interviewing (MI) is a counselling style that stimulates behavioural change by focusing on exploring and resolving ambivalence. A group setting has several benefits, e.g. sharing experiences, providing feedback and giving support. • Environmental modifications (3 clusters; 96 employees); (1) the VIP Coffee Corner Zone – the coffee corner was modified by adding a bar with bar chairs, a large plant and a giant wall poster (a poster visualizing a relaxing environment, e.g. wood, water and mountains); (2) the VIP Open Office Zone – the office was modified by introducing exercise balls and curtains to divide desks in order to reduce background noise; (3) the VIP Meeting Zone – conference rooms were modified by placing a standing table (a table that allows you to stand while working) and a giant wall poster (as before); and (4) the VIP Hall Zone ‐ table tennis tables were placed and lounge chairs were introduced in the hall for informal meetings. In addition, footsteps were placed on the floor in the entrance hall to promote stair walking. • GMI (7 cluster; 118 employees); • No intervention or control group (6 cluster; 106 employees) |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Primary outcome: need for recovery Secondary outcomes: daily physical activity, sedentary behaviour at work, detachment and relaxation, exhaustion, absenteeism, work performance, work engagement |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was executed by an independent researcher by using a computer generated list from SPSS. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of the participants and intervention providers for the social environmental intervention was impossible. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Sitting time at work was assessed by questionnaires. Participants receiving the intervention would have been aware of the goals set and the purpose of the intervention, and may have therefore misreported outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incompleteness of the data is taken into account with the multilevel analysis. Loss‐to‐follow‐up at 6 months was considerable (>20%). However, there were no significant differences at baseline between responders and non‐responders. |
| Selective reporting (reporting bias) | Low risk | All mentioned outcomes in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | No differences regarding age, gender, education, marital status, ethnicity, working hours, general health, job demands, supervisor support. Males were slightly over‐represented. |
| Validity of outcome measure | High risk | Validity of the questionnaire used in the study has not been tested. |
| Methods | Random allocation by minimization Single‐blinded Study duration: 12 weeks Drop out: 8% Location: Switzerland |
|
| Participants |
Population: staff from the confederate Swiss health insurance company EGK Intervention: 15 participants Control: 16 participants Demographics: Age: Intervention: 45 (SD 12), control: 40 (SD10) Sex (m/f): intervention 4/11, control 4/12 BMI (kg/m²): Intervention: 23.7 (SD 3.7), control: 24.7 (SD 5) |
|
| Interventions |
Duration of intervention: 12 weeks Intervention: Point of choice prompt + information Control: information only |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | no conflict of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group assignment was randomly conducted according to the minimization method: age, gender, BMI, physical activity and working time served as strata criteria in order to minimize group differences in demographical variables. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Testing personnel were blinded to group allocation. Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Sitting and standing were measured using accelerometer‐inclinometers, so misreporting of these activities was not possible. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3 participants in the control group and 4 participants in the intervention group withdrew due to job changes and illness (8% of participants). They were not included in the analysis (i.e. no intention‐to‐treat analysis). |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. Study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | Group differences were minimized. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation with cross‐over Unblinded Study duration: 10 weeks Drop out: 1231 working hours data were missing Location: USA Recruitment: a word‐of‐mouth search was performed for finding interested companies to host the study and Caldrea Inc. volunteered. A recruitment presentation was made at an all‐employee meeting (n ˜ 50) and was followed a few days later by enrolment interviews. |
|
| Participants |
Population: employees of Caldrea Inc. company, USA Demographics: average age: 40.4 years, Out of 28 participants, 19 were female |
|
| Interventions |
Duration of intervention: 4 weeks Intervention: sit‐stand workstation Three different models of desks were used: Workfit‐S, a setup that attaches to the front of one’s existing desk that can hold the computer monitor, keyboard and mouse; Workfit‐A, a setup that is identical to Workfit‐S but attaches to the back of one’s existing desk; and Workfit‐D, a whole desk that is easily moved up and down. The Workfit‐A and S also came with an added work‐surface and all three types of desks came with anti‐fatigue floor mats for comfort during standing. Control: no sit‐stand desk |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Sitting time, standing time, and light activity at work self‐reported and objectively assessed with accelerometer‐inclinometer Self‐reported energy and relaxation levels |
|
| Notes | James A. Levine has patents in accelerometer algorithms with Gruve Technologies Inc. but he did not access or analyse the raw the data from the Gruve device. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned to receive the intervention during period 1 or period 2, using a 1:1 allocation in 1 block of 35, using Microsoft Excel 2007. |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not possible due to the nature of the intervention. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel was not possible due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | By accelerometer‐inclinometer and self‐administered questionnaire, it is unlikely that results were influenced by the lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | If we assume a person works for 40 hours per week, then for 28 participants the working hours will be 8960 hours for 8 weeks (4 weeks intervention and 4 weeks control period). However the study reported only 7,729 working hours based on accelerometer data. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | There were no significant differences in age or BMI between interventions and control groups. Most of the participants were female. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation Unblinded Study duration: 12 weeks No dropouts Location: Germany only part of the study was presented as all the data has not been analysed. |
|
| Participants |
Population: Desk based employees at VDU workplaces Demographics: Mean age (years): 40.7 (range 24 to 58), Control 42.1 (range 25 to 61) 4 female participants in both intervention and control groups Mean BMI: 26.3 (SD 3.2) kg/m² |
|
| Interventions |
Duration of intervention: 12 weeks Intervention: The intervention consisted of:
Control: Ususal office work |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This project was initiated and funded by the German Social Accident Insurance (DGUV). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Following correspondence with the authors, they replied: "Randomization by computer generated list". |
| Allocation concealment (selection bias) | Low risk | Following correspondence with the authors, they replied: "our secretary, who was not involved in the project, generated the allocation list." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Following correspondence with the authors, they replied: "The participants were blinded, the personnel was not blinded (they knew according to the subject code, who belongs to the Intervention group and to the Control group)". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The measurements were recorded by activity log and accelerometer‐inclinometer, so misreporting of activity was not possible. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. |
| Baseline comparability/ imbalance | Low risk | Participants were recruited from different VDU workplaces. No significant difference in age of participants between intervention and control groups. 4 female participants in both intervention and control groups. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation: RCT Single‐blind Study duration: 10 days Drop out: 7% Location: United Kingdom Recruitment: healthy working adults who could stand unassisted recruited via poster and email |
|
| Participants |
Population: healthy adults working in an office at Glasgow Caledonian University in Scotland Intervention group: 14 participants (point of choice prompts (PoC) Control group: 14 participants (education) Demographics: PoC group (mean age 49 (SD 8 years) were older than the education group (mean age 39 (SD 10) years), predominantly female (11 in PoC group and 11 in education group), worked as administrators (4 in PoC group and 3 in education group), researchers (5 in PoC group and 7 in education group), lecturers (5 in PoC group and 4 in education group) BMI: PoC group 23.7 (SD 3.5) vs. education group 23.6 (SD 2.8) |
|
| Interventions |
Duration of intervention: 5 days but the participants were followed up for 10 days. Intervention: PoC prompting software + information Control: information only (a short educational talk) All participants received a short educational talk regarding the health risks of prolonged sitting stating that standing every 30 minutes could be beneficial, and a short information leaflet was also provided. Then participants in the intervention group had a prompting software installed in their personal computer to remind them to take a break for 1 min every 30 minutes. |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Assessed with thigh‐mounted accelerometer‐inclinometer
|
|
| Notes | This study was funded by the School of Health, Glasgow Caledonian University and formed the dissertation project for Masters of Rehabilitation Science of Rhian Evans, Henrietta Fawole, and Stephanie Sheriff. No financial support was received from any commercial company. No financial disclosures were reported by the authors of this publication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generation was used. |
| Allocation concealment (selection bias) | Low risk | Information on the group assignment was placed into sequentially numbered sealed opaque envelopes. The researcher was involved in opening the envelope immediately after the education. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Both the researcher and participants were aware of the allocation. Awareness of the purpose of the study may have led the education group participants to behave differently during the study, which may have affected the outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Data treatment was conducted by a researcher blinded to the allocation of the participants. The measurements were recorded by thigh‐mounted activPAL accelerometer‐inclinometers, so misreporting of activity was not possible. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 participants were excluded from analyses due to incomplete data: 1 from the PoC group and 1 from the education group. As the same proportion of participants were excluded from both groups, the missing data did not have much impact on outcomes. |
| Selective reporting (reporting bias) | High risk | Not all outcomes mentioned in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | PoC group (mean age 49 (SD 8) years) was older than the education group (mean age 39 (SD 10) years), participants worked as administrators (4 in PoC group, 3 in education group), researchers (5 in PoC group, 7 in education group), or lecturers (5 in PoC group, 4 in education group) and were predominantly female (11 in PoC group, 11 in education group) |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | non‐random allocation unblinded Study duration: 6 months Drop outs: 49% Location: University of Jyväskylä, Finland Recruitment: All faculty employees (n = 170) were invited to fill out a questionnaire between August and September 2012 and again in February 2013. |
|
| Participants |
Population: Healthy adults working in a university setting: researchers, teachers, administrative workers, assistants, professors and technical workers. Intervention group: 24 participants Control group: 21 participants Demographics: Mean age: Intervention 47.8 (SD 10.8) years, control 39 (SD 8.5) years. 70.8% were females in the intervention group and 81% were females in the control group. BMI (kg/m²): Intervention: 24.8 (SD 3.9), control: 23.3 (SD 3.8) |
|
| Interventions |
Duration of intervention: 6 months Intervention: sit‐stand desk Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | The study was funded by the China Scholarship Council (201206320092). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The study did not employ randomisation. Part of the personnel moved to a renovated building with sit‐stand workstations. |
| Allocation concealment (selection bias) | High risk | Allocation was not concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Sitting time was self‐reported by the participants. Participants receiving the intervention would have been aware of the goals set and the purpose of the intervention, and may have misreported outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The questionnaire was returned by 92 employees at baseline, before working at sit–stand workstations, and 61 employees after 6 months. Those who completed the questionnaire only once were excluded, leaving 45 individuals who were included in the analysis. The study lost 49% participants during follow‐up. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the protocol were reported. |
| Baseline comparability/ imbalance | High risk | In the intervention group participants were older and had more experience of office work. 70.8% were females in the intervention group and 81% were females in the control group. BMI (kg/m²): Intervention: 24.8 (3.9), control: 23.3 (3.8) |
| Validity of outcome measure | High risk | Validity of the questionnaire used in the study has not been tested. |
| Methods | Random allocation Unblinded Study duration: 10 weeks Drop out: 16% Location: UK, Australia and Spain Recruitment: Participants came from 3 major regional universities in 3 countries, represented by a lead investigator in each university, who had expressed an interest in running an employee intervention at their respective university as part of an evolving, international project. |
|
| Participants |
Population: white‐collar (i.e. professional, managerial, or administrative) university staff from the UK (n = 64), Australia (n = 70) and Spain (n = 80) Intervention groups:
Control group: 60 participants Demographics: mean age (years): route walking group 42.1 (SD 9.2); incidental walking group 41 (SD 9.7), control group 40.8 (SD 11.4) Women were predominant in all 3 groups Mean BMI (kg/m²): route walking group 25.1 (SD 4), incidental walking group 25.4 (SD 4.3), control group 24.2 (SD 3.8) |
|
| Interventions |
Duration of intervention: 10 weeks Interventions: walking strategies (route and incidental walking) Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | Authors declared that they had no competing interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pre‐intervention workday step counts and block stratification were used to assign participants at each site randomly and equally to a waiting list control or one of two intervention groups. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Sitting time was self‐reported by the participants. Participants receiving the intervention would have been aware of the goals set and the intention of the intervention, and may have misreported outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | From a potential sample size of 214 participants, 16% (n = 35) had missing data at pre‐intervention or 2 or more intervention measurement points. These data were removed prior to analyses, resulting in a final sample size of n = 179. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | Age was not significantly different between groups: 42.1 (SD 9.2) years in the route walking group group; 41 (SD 9.7) years in the incidental walking group and 40.8 (SD 11.4) years in the control group. Study participants were predominantly women. All participants were white collar workers (i.e. professional, managerial, or administrative). |
| Validity of outcome measure | Low risk | Paper‐based diaries were used to report sitting time at work. |
| Methods | Random allocation Unblinded Study duration: 10 weeks Drop out: 14% Location: USA Recruitment: strategically placed fliers posted around the Arizona State University Downtown Phoenix Campus, email advertisements delivered to employees through the Employee Wellness Committee, and word of mouth. |
|
| Participants |
Population: currently employed adults with predominantly sedentary occupations working in the Greater Phoenix area in 2012‐2013 Intervention group: 12 participants Control group: 10 participants Demographics: Mean age: Intervention 44.2 (SD 12.5), Control 47.2 (SD 13.5), 50% females in both groups, BMI: Intervention 24.1 (SD 3) kg/m², control 30.6 (SD 5) kg/m² Intervention group composed of significantly more “official and managerial level” individuals. |
|
| Interventions |
Duration of intervention: 10 weeks Intervention: one orientation to walking workstation, 5 bi‐weekly newsletters, specifically targeting workplace sitting behaviours, 5 bi‐weekly FAQ’s and access to study website for intervention content, latest sedentary behaviour research and links for tools for decreasing sitting time at work. Control: health education |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Sitting time/workday (minutes/8‐hour workday) measured by accelerometer‐inclinometer. Participants were also asked to complete a daily log to determine work schedule and verify obtained inclinometer and accelerometer data |
|
| Notes | Thesis presented in partial fulfilment of the requirements for the degree Master of Science. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation was decided by tossing a coin. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Sitting time was measured using accelerometer‐inclinometer, so misreporting of these activities was not possible. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant from both groups withdrew, due to busy schedule, 1 participant from both groups was excluded due to device malfunction and 1 participant from the control group was excluded due to refusal to wear accelerometer. Intention‐to‐treat analysis was followed for data analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. Study protocol was not available. |
| Baseline comparability/ imbalance | High risk | Intervention group composed of significantly more “official and managerial level” individuals. Age of participants in the control group was 47.2 (SD 13.5) and in the intervention group was 44.2 (SD 12.5). There were 50% females in both groups. There was significant difference in BMI of participants between intervention and control groups. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation Unblinded Study duration: 8 weeks Drop out: 4% Location: UK Recruitment: Consent was sought from 11 departmental managers for employee recruitment. All employees in consenting departments received an overview of the study and participant information sheet, and were invited to a study information session via an email from the research team. |
|
| Participants |
Population: Office workers from one organisation (Liverpool John Moores University, Liverpool, UK). Employees within the approached departments were predominantly administrative staff. Intervention group: 26 participants Control group: 21 participants Demographics: Mean age: Intervention 38.8 (SD 9.8) years, Control 38.4 (SD 9.3) years 89% in intervention group and 67% in control group were females BMI: Intervention (kg/m²): Intervention 67.4 (SD 13.8), control 70.5 (SD 16.4) |
|
| Interventions |
Duration of intervention: 8 weeks Intervention: Sit‐stand desk combined with face‐to‐face training and ergonomic information. Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | Ergotron Ltd provided the sit‐stand workstation but had no involvement on the provenance, commissioning, conduct or findings of the study. No other financial disclosures were reported by the authors of this paper. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised using a randomised block design and random number table. |
| Allocation concealment (selection bias) | High risk | One member of the research team assigned the participants to a treatment arm, based on a design and table with alternating scheme. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Reaserchers were aware of the allocation and participants may have also been aware of the allocation due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Sitting and other activities were assessed via ecological momentary assessment diaries (EMA). Participants receiving the intervention would have been aware of the goals set and the intention of the intervention and may have misreported outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The authors conducted a per‐protocol analysis and excluded participants from analyses for outcomes to which they did not contribute data. For workplace sitting, standing and walking, the per‐protocol analysis was compared with an intention‐to‐treat analysis, as a sensitivity analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. |
| Baseline comparability/ imbalance | Low risk | Groups were comparable at baseline except for a higher proportion of women in the intervention group (89% versus 67% in the control group). |
| Validity of outcome measure | Low risk | Ecological Momentary Assessment (EMA) diaries were used to report sitting time at work. |
| Methods | Non‐random allocation by clusters (floor): CBA Unblinded Study duration: 3 months Drop out:14% Location: Melbourne, Australia Recruitment: an invitation email was sent to all potential participants to attend one of two 30‐minute study information sessions delivered by research staff. Participants who subsequently expressed interest were screened via telephone for eligibility. |
|
| Participants |
Population: from a single workplace (Comcare: the government agency responsible for workplace safety, rehabilitation and compensation for Australian government workplaces) in metropolitan Melbourne, Australia Intervention group: 19 participants Control group: 19 participants Demographics: mean age 42.4 (SD 10.6) years in the intervention group and 42.9 (SD 10.3) years in the control group Women were predominant in the intervention group and men were predominant in the control group. Mean BMI (kg/m²): intervention group 27.5 (SD 6.1); control group 26.2 (SD 4.6) |
|
| Interventions |
Duration of intervention: 4 weeks Intervention: the intervention communicated 3 key messages: “Stand Up, Sit Less, Move More” and had the following components:
Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This study was funded by an NHMRC project grant and the Victorian Health Promotion Foundation. Ergotron provided the height‐adjustable workstations (www.ergotron.com). No financial disclosures were reported by the authors and the authors declared that there were no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation was not done. |
| Allocation concealment (selection bias) | High risk | Allocation into groups was by floor, with intervention participants (primarily administrative staff) working on the floor above the control participants (predominantly senior administrative staff). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Research staff, participants, and assessors were not blinded to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As outcomes were assessed by accelerometer‐inclinometers and self‐administered questionnaires, it is unlikely that results were influenced by the lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 participants, 2 each from the intervention and control groups withdrew and 2 further participants, 1 each from the intervention and control groups were lost during follow‐up. As the same proportion of participants were excluded from both groups, the missing data did not have much impact on outcomes. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | There were more women in the intervention group than in the control group. The mean age of both groups was similar. All participants were recruited from a single workplace in metropolitan Melbourne, Australia. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Allocation by clusters, 2 groups randomly and 2 group non‐randomly: CBA Unblinded Study duration: 3 months Drop out: 13.6% Location: University of Queensland, Brisbane, Australia Recruitment: a recruitment email explaining the study's purpose and procedures was sent to all staff from consenting units. Interested employees emailed the project manager and were interviewed via telephone to assess eligibility. |
|
| Participants |
Population: desk‐based office workers located on the same office floor, aged between 20–65 years from 3 different campuses Intervention group:
Control group: 13 participants Demographics: mean age in the multi component group was 37.3 (SD 10.7) years, 43 (SD 10.2) years in the workstation only group, and 48 (SD 11.6) years in the control group. There were no men in the multi component group, 3 in the workstation only group, and 4 in the control group. |
|
| Interventions |
Duration of intervention: 3 months Interventions:
Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) All outcomes were assessed at 3‐month follow‐up
|
|
| Notes | Funding source: Australian Postgraduate Award Scholarship, UQ School of Population Health Top‐Up Scholarship and research student funding, Queensland Health Core Infrastructure Funding, and UQ Major Equipment and Infrastructure and NHMRC Equipment Grant. Height‐adjustable workstations were provided by Ergotron. No other financial disclosures were reported by the authors. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The 2 units that were located closer to the research centre were randomised to the intervention arms and the more distant unit was allocated to the control arm. No further information provided on the method used to generate the random sequence. |
| Allocation concealment (selection bias) | High risk | The faculty staff were allocated to the multi component group, department staff were allocated to the workstation only group and campus staff were allocated to the control group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The participants and personnel knew the group to which they had been allocated. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Since the measurements for sitting were recorded by accelerometer‐inclinometer, it is unlikely that results were influenced by the lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 25% participants were lost in the sit‐stand desk plus counselling group, and one participant i.e. 7% each in of the other two groups. The high attrition of participants from the sit‐stand desk plus counselling group will have affected the outcome. |
| Selective reporting (reporting bias) | High risk | Not all the outcomes mentioned in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | All the participants had desk‐based jobs at the University of Queensland in Brisbane, Australia. The mean age in the multi component group was 37.3 (SD 10.7) years, in the workstation only group it was 43 (SD 10.2) years, and 48 (SD 11.6) years in the control group. There were no men in the multi component group, 3 in the workstation only group, and 4 in the control group. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation Unblinded Study duration: 13 weeks No drop outs Location: Tasmania, Australia |
|
| Participants |
Population: chosen from 460 desk‐based Tasmania Police employees across several metropolitan sectors Intervention group: 17 participants Control group: 17 participants Demographics: mean age: intervention group 41.5 (SD 12.39) years, control group 43.88 (SD 9.65) years |
|
| Interventions |
Duration of intervention:13 weeks Intervention: computer prompts Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Published: daily workplace energy expenditure (calories/workday) for different activities estimated from occupational physical activity questionnaire at 13 weeks vs. baseline Unpublished: self‐reported time spent sitting at work (minutes/day) at 13 weeks |
|
| Notes | This research was launched through a research partnership between the Tasmania State Police Department and the University of Tasmania; funded by the Tasmanian government’s Healthy@Work grant scheme. The authors report no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Following correspondence with the authors, they replied: "We used a random numbers generation software through the web." |
| Allocation concealment (selection bias) | High risk | Following correspondence with the authors, they replied: "The researchers did randomisation, so we were not blind to the allocation." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Following correspondence with the authors, they replied: "Since it was field based, participants were not blind to the treatment groups." |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Sitting time was self‐reported by the participants. Participants receiving the intervention would have been aware of the goals set and the purpose of the intervention and may have misreported outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no drop outs or exclusion of data. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. A study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | All participants were employees of the Tasmania police department. Age was not significantly different between groups: 41.5 (12.4) years in the intervention group, and 43.88 (9.6) years in the control group. |
| Validity of outcome measure | Low risk | Occupational Sedentary and Physical Activity Questionnaire (OSPAQ) which had moderate validity was used for assessing time spent sitting at work. |
| Methods | Random allocation by cluster Single blind Study duration: 27 weeks Drop outs: 28% Location: Spain Recruitment: Office workers were first invited to participate in an on‐line survey to identify those with low and moderate PA levels. Then they were were invited to participate in the intervention by email or phone calls. |
|
| Participants |
Population: administrative and academic staff working at six campuses in four Spanish Universities in Galicia, the Basque Country and Catalonia Intervention group: 135 participants (3 clusters) Control group: 129 participants (3 clusters) |
|
| Interventions |
Duration of intervention: 8 weeks Intervention: Automated web‐based intervention (W@WS) to encourage incidental walking and short walks during the working day. The walking strategies focused on breaking occupational sitting time by incidental walking into work tasks such as moving rather than sitting during lectures and seminars, not sitting to take phone calls, short walks (5–10 minutes) within University campuses, active transport (e.g. walking to work whenever possible) or active lunch breaks. Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Self‐reported occupational sitting time (minutes/day) measured by paper dairy log Daily step counts measured by Pedometer, Yamax‐200 and physical risk factors (waist circumference, BMI, blood pressure) |
|
| Notes | The study was funded by the Spanish Ministry of Science and Innovation (MICCIN) (project reference DEP 2009‐1147). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Campuses were randomly assigned by worksite to an Intervention (n = 3; deployed W@WS) or Comparative group (n = 3; maintained normal behaviour). In each region, one university campus was randomly assigned to the program (intervention group; IG) and another campus acted as a comparison group (CG). Authors replied to our request for further information but their reasoning was unclear. |
| Allocation concealment (selection bias) | Unclear risk | Authors replied to our request for further information but their reasoning was unclear. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Following correspondence with authors, they replied: “In the "big universities": the comparison and the intervention campuses were located in different cities and therefore, participants from each campus were not aware that another campus was doing the intervention. In the "small universities": Each university was located in a different city (Barcelona and Vic). Thus, participants did not know there was another university doing the intervention.” However because of the self‐evident nature of the intervention awareness of their own exposure to a certain changed environment or intervention might have changed their behaviour. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Sitting time was self‐reported by the participants. Participants receiving the intervention would have been aware of the goals set and the intention of the intervention and may have misreported outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Number of withdrawals was unbalanced in two groups, with more in the intervention group. There were 33 (24%) in the intervention and 41 (32%) in the control group. |
| Selective reporting (reporting bias) | Low risk | All the outcomes mentioned in the protocol were reported. |
| Baseline comparability/ imbalance | Unclear risk | No information provided. |
| Validity of outcome measure | Low risk | Paper‐based diary was used to report sitting time at work. |
| Methods | Random allocation Single blind Study duration: 3 months Drop outs: 24% Location: USA Recruitment: in‐house distribution of print and electronic media. Potential participants received an e‐mail providing a link to an online survey that included a series of screening questions designed to assess participant eligibility. |
|
| Participants |
Population: pool of 728 Overweight/obese and sedentary employees at a single office Intervention group: 15 participants Control group: 16 participants Demographics: mean age: Intervention 40 (SD 9.5) years Control 40.3 (SD 10.9) years only one male participant and 40 female participants BMI: Intervention 36.1 (SD 8.7) kg/m², control 35.6 (SD 8.2) kg/m² |
|
| Interventions |
Duration of intervention: 3 months Intervention: Treadmill desk plus counselling Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Physical activity (minutes/hour) and sedentary behavior (minutes/hour) measured by accelerometer‐inclinometer, body mass, body fat percentage, and BMI |
|
| Notes | This research was supported by Blue Cross and Blue Shield of Louisiana. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Following correspondence with authors, they replied: "Statisticians generated a random list." |
| Allocation concealment (selection bias) | Low risk | Following correspondence with authors, they replied: “The randomisation codes were sealed in envelopes with randomisation numbers.” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Following correspondence with authors, they replied: “Participants were not blinded. Intervention personnel and Project Manager were not blinded.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Sitting, step counts, Physical activity and sit‐to‐stand transitions were measured using thigh‐mounted accelerometer‐inclinometers, so misreporting of these activities was not possible. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Does not appear to have attrition bias. |
| Selective reporting (reporting bias) | High risk | The trial registry mentions a follow‐up of 6 months but the study reports only 3 months' follow‐up. |
| Baseline comparability/ imbalance | Low risk | Age, sex and occupation were similar in both the intervention group and the control group at baseline. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation by cluster Unblinded Study duration: 6 days Drop outs: 23% Location: USA Recruitment: employees with clerical positions were identified through University directory. |
|
| Participants |
Population: full time employees (employed >20 yrs) engaged in a sedentary occupation Intervention: stand group: 29 participants step group: 31 participants Demographics: mean age: stand: 42.3 (SD 11.6) years, step: 46.1 (SD 10.5) years 60% were females in stand group and 75% were females in step group BMI: Stand: 29.3 (SD 7.3) kg/m², step: 27.7 (SD 7.4) kg/m² |
|
| Interventions |
Duration of intervention: 3 days Intervention: computer‐based versus wrist worn prompts |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Total sitting time (minutes/workday), duration of longest sitting bout (minutes/workday), number of sitting bouts/workday of 30 min or more, standing time (minutes/workday), stepping time, sit/stand transitions measured by accelerometer‐inclinometers. |
|
| Notes | The Clinical and Translational Science Institute of Southeastern Wisconsin supported this research. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generation was used to assign participants to either the stand group or step group. |
| Allocation concealment (selection bias) | Low risk | Assignments were written out and placed in sealed numbered envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The envelopes were opened sequentially by a researcher, participants were informed of group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Since the measurements for sitting were recorded by accelerometer‐inclinometers, it is unlikely that results were influenced by the lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 18 participants were excluded, 9 each from stand group and step group. Reasons were drop out, equipment malfunction and not wearing monitor properly. The authors did not conduct intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | No baseline differences were found between the two groups for age, body mass, height or BMI. There was however difference in gender with the Stand group having 60% females and the Step group having 75%. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation Unblinded Study duration: 12 months Drop out: 11% Location: Amsterdam, the Netherlands |
|
| Participants |
Population: all employees from 2 Dutch research institutes were invited to participate, between April‐November 2010 Intervention group: 129 participants Control group: 128 participants Demographics: mean age of the study population was 46 years. 67% of participants were women. About 60% of the study population had a healthy weight (BMI 18.5‐25). |
|
| Interventions |
Duration of intervention: 6 months but the participants were followed up for 12 months. Intervention: the Mindful VIP intervention consists of 8 weeks of in‐company mindfulness training with homework exercises, followed by 8 sessions of e–coaching. The homework exercises comprised a variety of formal (“body scan” meditation, sitting meditation) and informal exercises (small exercises, such as breathing exercises when starting up the computer, and grocery shopping mindfully). Additionally, free fruit and snack vegetables were provided during the 6 months. In addition, lunch walking routes, and a buddy‐system were offered as supportive tools. Control: received information on existing lifestyle behaviour‐related facilities that were already available at the worksite. |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | The authors report no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were individually randomised to either the intervention or control group, using a computer‐generated randomisation sequence. |
| Allocation concealment (selection bias) | High risk | After randomisation, the research assistant notified each participant by e‐mail about the group to which he or she was allocated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of the participants and the trainers was not possible. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Sitting time at work was assessed by questionnaires. Participants receiving the intervention would have been aware of the goals set and the purpose of the intervention and may have misreported outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8 participants were lost to follow‐up from the intervention group and 17 from the control group. The loss to follow‐up in the control group was twice that in the intervention group. The authors conducted intention‐to‐treat analysis by linear mixed‐effect models. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | Mean age was similar between the intervention group and control group. There were 63.6% women in the intervention group and 71% in the control group. All participants were from two Dutch research institutes. |
| Validity of outcome measure | High risk | Validity of the questionnaire used in the study has not been tested. |
| Methods | Allocation randomly by cluster Double‐blind Study duration: 6 months Drop out: 43% in occupational physicians (OPs) and 10% in employees Location: Amsterdam, the Netherlands Recruitment: OPs were recruited by the Netherlands Society of Occupational Medicine via a direct mailing to their members' registry (> 2100 OPs). OPs were asked to recruit 1 or more companies of medium or large size (> 100 workers). Next, OPs recruited employees via a health risk appraisal consisting of anthropometric measurements and subsequent health advice. |
|
| Participants |
Population: OPs from the Netherlands Society of Occupational Medicine and employees from medium or large sized companies in the Netherlands Intervention group: OPs (n = 7), employees (n = 274) Control group: OPs (n = 9), employees (n = 249) Demographics: mean age of employees in the intervention group was 46 (SD 8) years, mean age in the control group was 48 (SD 9) years. Percentages of men were 62% and 65% in the intervention and control groups respectively. 33% of employees in the intervention group and 27% of employees in the control group had a normal BMI. Type of worker Intervention group: blue collar (manual labour) 15%; white collar 70%; client contact 15% Control group: blue collar 17%; white collar 73%; client contact 10% |
|
| Interventions |
Duration of intervention: 6 months Intervention: guideline‐based counselling by OP providing advice to employers on how to assess and intervene on the obesogenic work environment. Conducted by OPs as 5 face‐to‐face behavioural change counselling sessions for employees to improve their lifestyle to prevent weight gain. Control: usual care by physician |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This study was funded by the Netherlands Organisation for Health Research and Development. The authors report no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | OPs who consented to participate were randomly assigned to the intervention or control group by an independent researcher using Random Allocation Software (V.1.0; Isfahan University of Medical Sciences) |
| Allocation concealment (selection bias) | High risk | After randomisation, the principal researcher notified OPs of the group to which they had been allocated. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | As OPs themselves were the intervention providers, they could not be blinded for allocation. OPs were asked not to reveal their group to participating employees or assistants performing measurements. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Behavioural outcomes (i.e. physical activity, sedentary behaviour and dietary behaviour) were assessed by questionnaire. Waist circumference, body weight and height were measured by unblinded OPs or by blinded clinic employees. Participants receiving the intervention would have been aware of goals set and the purpose of the intervention and may have misreported behavioural outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 28 OPs were randomised, but 12 (43%) did not participate in the study at all. However, the remaining OPs recruited employees well, matching the number of planned employees. During the 6‐month intervention period, employees from both groups were lost to follow‐up (n = 7 from the intervention group and n = 16 from the control group). These subjects (n = 53) were significantly younger, women, and had a lower income than study completers. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | Age, sex and occupation were similar in both the intervention group and the control group at baseline. |
| Validity of outcome measure | High risk | Validity of the questionnaire used in the study has not been tested. |
Abbreviations
BMI: body‐mass index CBA: controlled before‐and‐after study h: hour(s) OP: occupational physician PoC: point of contact RCT: randomised controlled trial SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aadahl 2015 | Not conducted in a workplace setting. Did not report workplace sitting, only total sitting. |
| Adams 2012 | Not all the participants were working. Did not report workplace sitting as a separate outcome. Total sitting time reported. |
| Aittasalo 2004 | Did not report workplace sitting as a separate outcome. Sitting time reported separately for working days and non‐working days but the working days included both work and leisure time. |
| Alderman 2014 | Not RCT or CBA. Did not report workplace sitting. |
| Ben‐Ner 2014 | Did not report data on sitting time at work separately. Daily sitting time (during waking hours) was measured with an accelerometer but it included both work and leisure time. |
| Bird 2014 | Not RCT or CBA. |
| Boreham 2005 | This was a stair‐climbing training study that took place during working hours, but sitting time was not assessed. |
| Bouchard 2015 | Not RCT or CBA. |
| Brown 2012 | Did not report workplace sitting. |
| Carr 2013 | No data reported for sitting time at work. Daily sedentary time (criterion: 0 steps/minute) was measured with StepWatch (accelerometer attached on ankle), but it included both work and leisure time (the monitor was kept during all wakeful hours for 7 consecutive days). Correspondence with the author was unclear regarding the distinction between work and leisure in sitting time. It is also not clear what the StepWatch measures as an accelerometer. |
| Carter 2015 | Not RCT or CBA. Does not describe a full working day. |
| Chae 2015 | Not RCT or CBA (pre‐post design). All the participants did not complete the program. |
| Cheema 2013 | Did not report workplace sitting. |
| Chia 2015 | Did not report workplace sitting. Following correspondence with authors they replied: "We did not specifically measure sitting time but had an indication of the time spent in the office (these are desk bound participants‐ when they filled in the questionnaire of alertness by the hour (0900‐1700hrs)". |
| Clemes 2014 | Not RCT or CBA. Pedometers were used to record sitting time and step counts. |
| Dewa 2009 | Did not report workplace sitting. Sitting time was assessed (IPAQ) but it included both work and leisure time. |
| Elmer 2014 | Not RCT or CBA. Outcome is energy expenditure not time spent sitting at work. |
| Freak‐Poli 2011 | Not an RCT or CBA. Workplace sitting not reported. Sitting time was questioned separately for weekdays and weekend days but it included both work and leisure. |
| Gilson 2012 | Not an RCT or CBA. Did not report workplace sitting. |
| Gilson ND 2012 | Not an RCT or CBA. |
| Gorman 2013 | Not an RCT or CBA. |
| Grunseit 2012 | Not an RCT or CBA. |
| Hedge 2004 | Sitting time was not reported in hours (only %). The length of intervention was not the same for everybody (no detailed information, stated “4‐6 wks”). |
| Irvine 2011 | Not an RCT or CBA. No quantitative data on sitting time at work. |
| John 2011 | Not an RCT or CBA. Did not report workplace sitting. Daily sitting time (waking hours) was measured with an accelerometer, but it included both work and leisure time. |
| Júdice 2015 | Did not report workplace sitting, only total sitting time. |
| Kennedy 2007 | Did not report workplace sitting. |
| Koepp 2013 | Not an RCT or CBA. |
| Lara 2008 | Not an RCT or CBA. Did not report workplace sitting. |
| Maeda 2014 | Not RCT or CBA. Participants were university students. |
| Mainsbridge 2014 | Did not report workplace sitting. |
| Mair 2014 | Did not report workplace sitting. |
| Marshall 2003 | Did not report workplace sitting. Sitting time was assessed (IPAQ, short version) but it included both work and leisure time (reported as ‘weekday sitting time’). |
| McAlpine 2007 | Not a normal working day, but an experimental office facility. Not an RCT or CBA. |
| Miyachi 2015 | Did not report workplace sitting. |
| NCT01221363 | Following correspondence with the authors, they replied: "Ours is not a work place intervention study, but a 'total sitting time' community‐based intervention study where the individual behavioural intervention addresses all domains of life, i.e. leisure time, work, transportation etc. Approximately 1/3 of participants are not working (retired or unemployed) and those who do work, do not necessarily have sedentary work, since our main inclusion criterion was minimum 3.5 hours of leisure time sitting/day. Consequently our primary outcome measure is objectively measured total daily sitting time (activPAL), and we only have rather crude self‐report measures on sitting time at work." |
| Opdenacker 2008 | Did not report workplace sitting. Sitting time was assessed (IPAQ) but it included both work and leisure time. |
| Ouyang 2015 | Not conducted in a workplace setting. Participants were sedentary overweight females. |
| Parry S 2013 | Did not report workplace sitting. Reported sedentary time measured by accelerometer. Sedentary time was defined as an activity having less than 100 counts on an accelerometer. |
| Pronk 2012 | Not an RCT or CBA. |
| Slootmaker 2009 | Did not report workplace sitting. Daily sitting time (waking hours) was measured with an accelerometer, but it included both work and leisure time. |
| Sternfeld 2009 | Did not report workplace sitting. Sedentary time assessed during leisure. |
| Straker 2013 | Not an RCT or CBA. |
| Thogersen‐Ntoumani 2013 | Did not report workplace sitting. |
| Thompson 2014 | Did not report workplace sitting. The authors used accelerometers, but converted their results into energy expenditure/day (no separation between work and leisure time). |
| Thorp 2015 | Outcome is energy expenditure not time spent sitting at work. |
| Yancey 2004 | Did not report workplace sitting. |
| Østerås 2005 | Not an RCT or CBA. |
Abbreviations
CBA: controlled before‐and‐after study IPAQ: International physical activity questionnaire RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised controlled trial |
| Participants | Sedentary office workers (n=127; ages 22‐64; BMI=28.5±6.1 kg/m²) were recruited from three Minnesota employers. |
| Interventions | The intervention consisted of 4 groups for 6 months: 1) Control, 2) Move (30 min of light activity during the workday), 3) Stand (standing 50% of the workday using a sit‐stand workstation), or 4) Stand+Move (combined Stand and Move). |
| Outcomes | Outcomes were assessed at baseline and at 6 months' follow‐up using the following cardiometabolic risk factors: blood pressure, fasting blood glucose, log of fasting triglycerides, and HDL‐cholesterol. |
| Notes | We could not find the full text article. |
| Methods | No information available. |
| Participants | No information available. |
| Interventions | No information available. |
| Outcomes | No information available. |
| Notes | We could not find the full text article. |
| Methods | Pre‐post design |
| Participants | Scottish working adults |
| Interventions | a 30‐minute individual discussion incorporating cognitive behavioural strategies (e.g. decisional balance, goal setting) to encourage individuals to think about their current sedentary behaviour and strategies to change. Duration of intervention: 2 weeks |
| Outcomes | Time spent sitting/lying, standing, stepping, step counts and sit‐to‐stand transitions. |
| Notes | We could not find the full text article. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | |
| Methods | Random allocation in clusters Location: Australia Recruitment: not yet recruiting |
| Participants | Population: male and female employees of Rockhampton Regional Council working either full‐time or part‐time, aged 18‐65 years |
| Interventions | Participants will be asked to wear a pedometer during the 6‐week challenge and to record the number of steps they have taken each day on the Central Queensland University 10,000 Steps website. Control: no intervention |
| Outcomes |
Primary outcome: total steps of physical activity measured using the Yamax Digiwalker DW‐150 pedometer Secondary outcomes
|
| Starting date | It is unclear whether the study has started at all. The study was promised to take place in 2013 and the study registration has not been updated. |
| Contact information | Mitch Duncan, email: m.duncan@cqu.edu.au |
| Notes | Primary sponsor: Government funding body Central Queensland Hospital and Health Service |
| Trial name or title | |
| Methods | Random allocation Recruitment: not yet recruiting |
| Participants | Population: office‐based workers aged 18 years and over, working at least 0.6 full time equivalent |
| Interventions | The organisational plus technology support intervention lasts for 8 weeks and consists of the following components:
Control: will receive all the elements of the intervention except PLUS technology support. |
| Outcomes |
Primary outcome
Secondary outcomes
|
| Starting date | It is unclear whether the study has started despite mentioning anticipated date of first participant enrolment 17/03/2014. The study registration has not been updated. |
| Contact information | Genevieve Healy, email: g.healy@uq.edu.au |
| Notes | Primary sponsor: University Cancer Prevention Research Centre, The University of Queensland, Australia |
| Trial name or title | The Inphact treadmill study |
| Methods | Random allocation Location: Sweden Recruitment: Recruitment and screening of participants has been completed. |
| Participants | Population description: Healthy overweight and obese office workers (n = 80) with mainly sedentary tasks will be recruited from office workplaces in Umeå, Sweden. |
| Interventions | The intervention group will receive a health consultation and a treadmill desk, which they will use for at least one hour per day for 13 months. Control: The control group will receive the same health consultation, but continue to work at their regular workstations. |
| Outcomes |
Primary outcome: Physical activity and sedentary time during workdays and non‐workdays as well as during working and non‐working hours on workdays will be measured objectively using accelerometers (Actigraph and activPAL) at baseline and after 2, 6, 10, and 13 months of follow‐up. Secondary outcome: Food intake will be recorded and metabolic and anthropometric variables, body composition, stress, pain, depression, anxiety, cognitive function, and functional magnetic resonance imaging will be measured at 3–5 time points during the study period. |
| Starting date | November 2013 |
| Contact information | Tommy Olsson, email: tommy.g.olsson@umu.se |
| Notes | Sponsors: Not reported |
| Trial name or title | Stand Up Victoria |
| Methods | Random allocation Location: Australia Recruitment: not yet recruiting |
| Participants | Population description: employees aged 18‐65 years, from 16 work sites located in Victoria, Australia |
| Interventions | The intervention consists of four distinct components:
Control: no intervention |
| Outcomes |
Primary outcome
Secondary outcomes Examine the effect of the intervention on cardiometabolic markers of health and disease including:
Explore workplace and individual‐level mediators (how did the intervention work?) and moderators (for whom did it work?) of change using a specially formulated questionnaire. |
| Starting date | July 2011 |
| Contact information | David Dunstan, email: David.Dunstan@bakeridi.edu.au |
| Notes | Sponsors: National Health and Medical Research Council and Vic Health |
| Trial name or title | |
| Methods | Random allocation Location: Finland Recruitment: recruitment is performed in the city of Jyväskylä, Finland, by delivering advertisements to parents via kindergartens and primary schools that have been pre‐randomised to control and intervention groups after balancing different environmental and socioeconomic regions within the city. |
| Participants | Population description: families from Jyväskylä region, Finland |
| Interventions | Tailored counselling targeted to decrease sitting time by focusing on commuting and work time. Control: no intervention |
| Outcomes | Changes in physical activity, health‐related indices and maintenance of the behavioural change |
| Starting date | December 2011 |
| Contact information | Taija Juutinen, email: taija.m.juutinen@jyu.fi |
| Notes | Study sponsors: Ministry of Education and Culture, Finland |
| Trial name or title | Take A Stand for Workplace Health: A Sit‐stand Workstation Project Evaluation |
| Methods | Random allocation Recruitment: active, not recruiting |
| Participants | Population: office employees primarily engaged in desk‐based work at one of the two worksites involved in the study (Macmillan Cancer Support, Public Health England) |
| Interventions |
Duration of intervention: 12 months Three arm trial Intervention: a sit‐stand workstation only and a multi‐component sit‐stand workstation intervention including individual and organisation‐level approaches Control: Usual practice (seated workstation) |
| Outcomes | Objective measures of sitting, standing, and physical activity using ActivPAL3™ and ActiGraph (GT3X+) understanding of the influence of organisational culture on sitting, standing and physical activity behaviour in the workplace using qualitative methods |
| Starting date | May 2014 |
| Contact information | Jenifer Hall, email: Jennifer.Hall@brunel.ac.uk |
| Notes | Sponsors and collaborators: Brunel University, Macmillan Cancer Support, Ergotron, Public Health England |
| Trial name or title | Booster breaks: health promoting work breaks |
| Methods | Random allocation |
| Participants | Population: Employees with sedentary office jobs from four workplaces in a large, urban southwestern U.S. city. |
| Interventions | Three arm trial Intervention: Computer Prompt (individualized PA work breaks) group and Booster Break group Control: Usual break group |
| Outcomes |
Primary outcomes: Lipid profile, Blood pressure, Height, Weight, International Physical Activity Questionnaire (IPAQ), Pedometer readings Secondary outcomes: Physical activity mediators and employee and organizational psychosocial constructs: self‐report assessments. |
| Starting date | January 2009 |
| Contact information | Wendell Taylor, email: Wendell.C.Taylor@uth.tmc.edu |
| Notes | Sponsor: National Institutes of Health (USA) |
| Trial name or title | |
| Methods | Random allocation Location: Australia |
| Participants | Population: employees of 1 of 3 of the university’s campuses located in Sydney and Melbourne, working on a part‐time or full‐time basis in either a job with an academic or administrative designation. |
| Interventions |
Duration of intervention: 12 weeks The intervention will comprise 2 distinct treatment phases targeting behaviour adoption (weeks 1‐4) and adherence (weeks 5‐12) using 'stages of behaviour change' principles
Control: no intervention |
| Outcomes |
Primary outcome: Average workday step count: measured by pedometer (Yamax SW‐200) and averaged over 5 working days at each time point Secondary outcomes
|
| Starting date | March 2010 |
| Contact information | Martin Mackey, email: martin.mackey@sydney.edu.au |
| Notes |
Study sponsors: Australian Research Council: ARC (Industry) Linkage Grant Professor Philip Taylor |
| Trial name or title | SedestActiv Project |
| Methods | Random allocation Location: Spain Recruitment: a total of 232 subjects will be randomly allocated to an intervention and control group (116 individuals each group). In addition, 50 subjects with fibromyalgia will be included. |
| Participants | Population description: professionals from 13 primary health care centres will randomly invite mildly obese or overweight patients of both genders, aged 25‐65 years, to participate. |
| Interventions | 6‐month primary care intervention Control: no intervention |
| Outcomes |
Duration of intervention: 6 months Primary outcome: to assess the effectiveness of a 6‐month primary care intervention to reduce diary hours of sitting time in overweight and obese patients, as well as to increase their weekly energy expenditure Secondary outcomes
|
| Starting date | June 2012 |
| Contact information | Carme Martín‐Borràs Email: sedestactiv@gmail.com |
| Notes | Study sponsor: Jordi Gol i Gurina Foundation |
| Trial name or title | |
| Methods | Random allocation Recruitment: active, not recruiting |
| Participants | Population: sedentary office employees |
| Interventions | Height adjustable desk installation in office |
| Outcomes |
Primary outcome: workplace sitting time Secondary outcomes
|
| Starting date | January 2013 |
| Contact information | |
| Notes | Study sponsor: USDA (United States Department of Agriculture) Grand Forks Human Nutrition Research Center |
| Trial name or title | |
| Methods | Random allocation Recruitment: active, not recruiting |
| Participants | Population: sedentary employees who use a single computer workstation for the majority of their workday |
| Interventions | Sit‐stand workstation with three arms
|
| Outcomes |
|
| Starting date | November 2013 |
| Contact information | |
| Notes | Study sponsor: University of Minnesota ‐ Clinical and Translational Science Institute |
| Trial name or title | Take a Stand! |
| Methods | Random allocation in clusters Location: Denmark Recruitment: enrolling by invitation |
| Participants | Population: 400 adults with sedentary office‐based work. Subjects should understand Danish and be without disabilities or diseases affecting their ability to stand or walk. |
| Interventions |
Duration of intervention: 3 months Intervention The intervention consists of four components:
Control: no intervention |
| Outcomes |
Primary outcomes: assessed by ActiGraph accelerometer
Secondary outcomes
|
| Starting date | November 2013 |
| Contact information | |
| Notes | Study sponsor: University of Southern Denmark |
| Trial name or title | Modifying the workplace to decrease sedentary behavior and improve health |
| Methods | Random allocation |
| Participants | Healthy volunteers employed in a full time sedentary job |
| Interventions |
Duration of intervention: 12 months Three arm trial Intervention: Treadmill workstation and Sit‐stand workstation Control: Participants will be asked to engage in three 10 min walking bouts each work day |
| Outcomes | Change in weight |
| Starting date | April 2014 |
| Contact information | Anne Thorndike, email: ATHORNDIKE@mgh.harvard.edu |
| Notes | Study sponsor: Northeastern University |
| Trial name or title | SMArT Work: Stand More AT Work |
| Methods | Random allocation in clusters Location: UK Recruitment: Participant recruitment will be coordinated via the research team at the Leicester Diabetes Centre. The study team currently hold a database of office units within the University Hospitals of Leicester NHS Trust and will promote this study to them initially through the use of the Trust’s intranet and emails to department managers. This will be followed up with a face‐to‐face presentation/meeting if necessary. |
| Participants | Desk‐based office workers (n = 238) from a stratified sample of NHS staff (e.g. employees, managers, gender, job role) |
| Interventions | height‐adjustable workstations at the environmental, organisational and individual level that support less occupational sitting. |
| Outcomes |
|
| Starting date | October 2014 |
| Contact information | Dr Ben Jackson, email: b.r.jackson@lboro.ac.uk |
| Notes |
| Trial name or title | The Healthier Office Study |
| Methods | Quasi‐random allocation Location: Australia Recruitment: "Posters will be placed in staff tearooms and common areas, inviting staff to participate. The advertisements will contain general information informing participants that we are testing simple occupational health interventions and that participants will be provided with an ergonomic device or advice about improving healthy work practices. The study will also be advertised at Faculty staff meetings to improve potential participants’ awareness of the study" |
| Participants | Population description: participants will be recruited from academic and administrative staff of The University of Sydney, Sydney, Australia |
| Interventions |
Intervention: 3 groups (1 control group and 2 intervention groups) will be conducted in an office workplace setting. The education intervention group will receive an education package that encourages reduction in sitting behaviours. The sit‐stand desk intervention group will receive the same education package along with an adjustable sit‐stand desk. The control group will receive no information or advice about postural change and no modification to their office desk set‐up. |
| Outcomes | Average daily sedentary time during work hours, measured by an accelerometer |
| Starting date | March 2013 |
| Contact information | |
| Notes | Study sponsors: this research is supported by funding from the Heart Foundation, Sydney, NSW, Australia, and by Australian National Health and Medical Research Council Program Grant (number: 569940; AB). Sit‐stand workstations were donated by Sit Back and Relax, Alexandria, NSW, Australia. |
| Trial name or title | |
| Methods | Random allocation Location: Belgium Recruitment: all participants were recruited from working places in Flanders (Belgium) through flyers, emails, pharmacists, and word of mouth |
| Participants | Population: employees (male and female) aged 19‐67 years who mentioned not being physically active during the last year |
| Interventions |
Interventions: Participants were randomised into one of the following four intervention groups:
|
| Outcomes |
Primary outcome: physical activity level Secondary outcomes
|
| Starting date | |
| Contact information | |
| Notes | No conflict of interest |
Abbreviation
BMI: body‐mass index
Contributions of authors
Jos Verbeek, Sharea Ijaz and Nipun Shrestha conceptualised the review.
Nipun Shrestha took the lead in writing the protocol.
Kaisa Neuvonen (Trials Search Co‐ordinator, Cochrane Work Review Group) and Nipun Shrestha designed the systematic search strategies.
Nipun Shrestha and Katriina Kukkonen‐Harjula conducted the study selection.
Nipun Shrestha, Suresh Kumar and Chukwudi Nwankwo did the data extraction and risk of bias assessment for the previous version.
Nipun Shrestha, Veerle Hermans and Soumyadeep Bhaumik did the data extraction and risk of bias assessment for the current update.
Nipun Shrestha and Jos Verbeek conducted the data analysis.
Nipun Shrestha wrote the manuscript collaborating with Jos Verbeek, Katriina Kukkonen‐Harjula, Sharea Ijaz, Veerle Hermans and Soumyadeep Bhaumik.
Sources of support
Internal sources
-
Cochrane Work Review Group, Finland.
Nipun Shrestha attended a three‐month internship to learn about Cochrane systematic review methodology.
-
Cochrane, UK.
Nipun Shrestha received a developing country stipend for attending the 22nd Cochrane Colloquium in 2014 in Hyderabad India.
-
Mesenaatti.me, Finland.
The author team collected EUR 1600 through the Mesenaatti.me crowdfunding platform to support Nipun Shrestha complete the review
External sources
No sources of support supplied
Declarations of interest
Nipun Shrestha: None known.
Jos Verbeek: I am employed by the Finnish Institute of Occupational Health to coordinate the Cochrane Work Review Group.
Sharea Ijaz: None known.
Katriina T Kukkonen‐Harjula: None known.
Veerle Hermans: None known.
Soumyadeep Bhaumik: None known.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
- Alkhajah TA, Reeves MM, Eakin EG, Winkler EA, Owen N, Healy GN. Sit‐stand workstations: a pilot intervention to reduce office sitting time. American Journal of Preventive Medicine 2012;43(3):298‐303. [DOI] [PubMed] [Google Scholar]; Healy G, Alkhajah T, Winkler E, Owen N, Eakin E. Reducing sitting time in office workers: Efficacy and acceptability of sit‐stand workstations. Journal of Science and Medicine in Sport 2012;15:S196. [Google Scholar]
- Carr LJ, Leonhard C, Tucker S, Fethke N, Benzo R, Gerr F. Total worker health intervention increases activity of sedentary workers. American Journal of Preventive Medicine 2015;49:[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]; NCT02071420. Efficacy of a combined ergonomic health promotion intervention on employee health. https://clinicaltrials.gov/ct2/show/NCT02071420 (accessed 28 November 2015).
- ACTRN12612000072819. The Stand@Work Pilot Study. A randomised controlled trial to see if using sit‐stand workstations reduces sitting time in office workers. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12612000072819 (accessed 3 June 2015). ; Chau JY, Daley M, Dunn S, Srinivasan A, Do A, Bauman AE, et al. The effectiveness of sit‐stand workstations for changing office workers' sitting time: results from the Stand@Work randomized controlled trial pilot. International Journal of Behavioral Nutrition and Physical Activity 2014;11:127. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chau JY, Daley M, Srinivasan A, Dunn S, Bauman AE, Ploeg HP. Desk‐based workers’ perspectives on using sit‐stand workstations: a qualitative analysis of the Stand@Work study. BMC Public Health 2014;14:752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffeng JK, Boot CR, Duijts SF, Twisk JW, Mechelen W, Hendriksen IJ. Effectiveness of a worksite social & physical environment intervention on need for recovery, physical activity and relaxation; results of a randomized controlled trial. PLoS ONE 2014;9(12):e114860. [DOI] [PMC free article] [PubMed] [Google Scholar]; Coffeng JK, Hendriksen IJ, Duijts SF, Proper KI, Mechelen WV, Boot CRL. The development of the Be Active & Relax "Vitality in Practice" (VIP) project and design of an RCT to reduce the need for recovery in office employees. BMC Public Health 2012;12:592. [DOI] [PMC free article] [PubMed] [Google Scholar]; Coffeng JK, Hendriksen IJ, Mechelen W, Boot CR. Process evaluation of a worksite social and physical environmental intervention. Journal of Occupational and Environmental Medicine 2013;55(12):1409‐20. [DOI] [PubMed] [Google Scholar]; Coffeng JK, Hendriksen IJM, Duijts SFA, Twisk JWR, Mechelen W, Boot CRL. Effectiveness of a combined social and physical environmental intervention on presenteeism, absenteeism, work performance and work engagement in office employees. Journal of Occupational Environment Medicine in press; Vol. 56, issue 3:258‐65. [DOI] [PubMed]; NTR2553. The cost‐effectiveness of an intervention to increase physical activity and relaxation amongst office workers. http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=2553 (accessed 3 June 2014).
- Donath L, Faude O, Schefer Y, Roth R, Zahner L. Repetitive daily point of choice prompts and occupational sit‐stand transfers, concentration and neuromuscular performance in office workers: an RCT. International Journal of Environmental Research and Public Health 2015;12(4):4340‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta N, Koepp GA, Stovitz SD, Levine JA, Pereira MA. Using sit‐stand workstations to decrease sedentary time in office workers: a randomized crossover trial. International Journal of Environmental Research and Public Health 2014;11(7):6653‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]; Dutta N, Walton T, Pereira MA. Experience of switching from a traditional sitting workstation to a sit‐stand workstation in sedentary office workers. Work 2014;52(1):83‐9. [DOI] [PubMed] [Google Scholar]
- Ellegast R, Weber B, Mahlberg R. Method inventory for assessment of physical activity at VDU workplaces. Work. 2012; Vol. 41, issue suppl 1:2355‐9. [DOI] [PubMed] [Google Scholar]; Mahlberg R. Entwicklung und Erprobung eines arbeitsmedizinischen Methodeninventars zur Effektivitätsanalyse von Präventionsmassnahmen zur Vermeidung von Muskel‐Skelett Erkrankungen an bewegungsarmen Arbeitsplätzen. Hohen Medizinischen Fakultät der Ruhr‐Universität Bochum. PhD dissertation2011.
- Evans RE, Fawole HO, Sheriff SA, Dall PM, Grant PM, Ryan CG. Point‐of‐choice prompts to reduce sitting time at work: a randomised trial. American Journal of Preventive Medicine 2012 Sep;43(3):293‐7. [DOI] [PubMed] [Google Scholar]; NCT01628861. Point‐of‐Choice Prompts to Reduce Prolonged Sitting Time at Work. http://clinicaltrials.gov/ct2/show/NCT01628861 (accessed 15 March 2014).
- Gao Y, Nevala N, Cronin NJ, Finni T. Effects of environmental intervention on sedentary time, musculoskeletal comfort and work ability in office workers. European Journal of Sport Science 2015;(Epub ahead of print):1‐8. [DOI] [PubMed] [Google Scholar]; ISRCTN43848163. Can an adjustable workstation reduce occupational sedentary time?. http://www.isrctn.com/ISRCTN43848163 (accessed 3 June 2015).
- Gilson ND, Puig‐Ribera A, McKenna J, Brown WJ, Burton NW, Cooke CB. Do walking strategies to increase physical activity reduce reported sitting in workplaces: a randomised control trial. International Journal of Behavioral Nutrition and Physical Activity 2009;6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon A. A theory‐based pilot study to decrease sitting time in the workplace. A theory‐based pilot study to decrease sitting time in the workplace (Msc Thesis). Arizona: Arizona State University, 2013. [Google Scholar]
- Graves LEF, Murphy RC, Shepherd SO, Cabot J, Hopkins ND. Evaluation of sit‐stand workstations in an office setting: a randomised controlled trial. BMC Public Health 2015;15(1):1145. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT02496507. A mixed‐methods evaluation of sit‐stand workstations in an office setting. https://clinicaltrials.gov/ct2/show/NCT02496507 (accessed 1 December 2015). [DOI] [PMC free article] [PubMed]
- Healy GN, Eakin EG, Lamontagne AD, Owen N, Winkler EA, Wiesner G, et al. Reducing sitting time in office workers: short‐term efficacy of a multi component intervention. Preventive Medicine 2013;57(1):43‐8. [DOI] [PubMed] [Google Scholar]; Neuhaus M, Healy G, Eakin E, FJeldsoe B, Lamontagne A, Owen N, et al. Efficacy of an integrated approach to reduce sitting time in office workers. Journal of Science and Medicine in Sport 2012;15:S197. [Google Scholar]; Stephens SK, Winkler EA, Trost SG, Dunstan DW, Eakin EG, Chastin SF, et al. Intervening to reduce workplace sitting time: how and when do changes to sitting time occur?. British Journal of Sports Medicine 2014;48(13):1037‐42. [DOI] [PubMed] [Google Scholar]
- ACTRN12612001246875. Reducing sitting time in office workers: comparison of a multifaceted workplace approach vs. installation of height‐adjustable desks only using a three‐armed controlled trial. http://www.anzctr.org.au/ACTRN12612001246875.aspx (accessed 15 March 2014). ; Neuhaus M, Healy GN, Dunstan DW, Owen N, Eakin EG. Workplace sitting and height‐adjustable workstations: a randomised controlled trial. American Journal of Preventive Medicine 2014;46(1):30‐40. [DOI] [PubMed] [Google Scholar]
- Cooley D, Pedersen S, Mainsbridge C. Assessment of the impact of a workplace intervention to reduce prolonged occupational sitting time. Qualitative Health Research 2014;24(1):90‐101. [DOI] [PubMed] [Google Scholar]; Pedersen SJ, Cooley PD, Mainsbridge C. An e‐health intervention designed to increase workday energy expenditure by reducing prolonged occupational sitting habits. Work 2014;49(2):289‐95. [DOI] [PubMed] [Google Scholar]
- Puig‐Ribera A, Bort‐Roig J, González‐Suárez AM, Martínez‐Lemos I, Giné‐Garriga M, Fortuño J, et al. Patterns of impact resulting from a 'sit less, move more' web‐based program in sedentary office employees. PLoS One 2015;10(4):e01224. [DOI] [PMC free article] [PubMed] [Google Scholar]; Roig JB, Horcajo MM, Ribera AP, Gonzalez Á, Lemos IM. Walk and Work Spain: Participants’ perspectives and experiences on reducing occupational sitting time. Journal of Science and Medicine in Sport 2012;15(Supplement 1):S303. [Google Scholar]; Roig JB, Ribera AP, Gilson N, Gonzalez Á, Lemos IM, Garriga MG, Fortuño J. A 5‐months workplace pedometer‐based intervention: Did it change employees’ sedentary behaviour 2 months after removal?. Journal of Science and Medicine in Sport 2012;15(1):S197. [Google Scholar]
- NCT01587092. Workstation Pilot Study. https://clinicaltrials.gov/ct2/show/NCT01587092 (accessed 3 June 2014). ; Schuna JM Jr, Swift DL, Hendrick CA, Duet MT, Johnson WD, Martin CK, et al. Evaluation of a workplace treadmill desk intervention: a randomized controlled trial. Journal of Occupational and Environmental Medicine 2014;56(12):1266‐76. [DOI] [PubMed] [Google Scholar]; Tudor‐Locke C, Hendrick CA, Duet MT, Swift DL, Schuna JM Jr, Martin CK, et al. Implementation and adherence issues in a workplace treadmill desk intervention. Applied Physiology, Nutrition, and Metabolism 2014;39(10):1104‐11. [DOI] [PubMed] [Google Scholar]
- Swartz AM, Rote AE, Welch WA, Maeda H, Hart TL, Cho YI, et al. Prompts to disrupt sitting time and increase physical activity at work. Centers for Disease Control and Prevention, Preventing Chronic Disease 2014;11:E73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkel J, Boot CR, Proper KI, Bongers PM, Beek AJ. Effectiveness of a worksite mindfulness‐related multi‐component health promotion intervention on work engagement and mental health: results of a randomised controlled trial. PLoS ONE 2014;9(1):e84118. [DOI] [PMC free article] [PubMed] [Google Scholar]; Berkel J, Boot CR, Proper KI, Bongers PM, Beek AJ. Mindful "Vitality in Practice": an intervention to improve the work engagement and energy balance among workers; the development and design of the randomised controlled trial. BMC Public Health 2011;11:736. [DOI] [PMC free article] [PubMed] [Google Scholar]; Berkel J, Boot CR, Proper KI, et al. Effectiveness of a worksite mindfulness‐based multi‐component intervention on lifestyle behaviours. International Journal of Behavioral Nutrition and Physical Activity2014; Vol. 11. [DOI] [PMC free article] [PubMed]
- ISRCTN73545254. Balance@Work: the cost effectiveness of an occupational health guideline to improve physical activity and dietary behaviour among workers in order to prevent weight gain. http://www.isrctn.com/ISRCTN73545254 2009 (accessed 28 November 2015). ; Verweij LM, Proper KI, Weel AN, Hulshof CT, Mechelen W. Design of the Balance@Work project: systematic development, evaluation and implementation of an occupational health guideline aimed at the prevention of weight gain among employees. BMC Public Health 2009;9:461. [DOI] [PMC free article] [PubMed] [Google Scholar]; Verweij LM, Proper KI, Weel AN, Hulshof CT, Mechelen W. Long‐term effects of an occupational health guideline on employees' body weight‐related outcomes, cardiovascular disease risk factors, and quality of life: results from a randomised controlled trial. Scandinavian Journal of Work, Environment & Health 2013;39(3):284‐94. [DOI] [PubMed] [Google Scholar]; Verweij LM, Proper KI, Weel AN, Hulshof CT, Mechelen W. The application of an occupational health guideline reduces sedentary behaviour and increases fruit intake at work: results from an RCT. Occupational and Environmental Medicine 2012;69(7):500‐7. [DOI] [PubMed] [Google Scholar]; Wier MF, Verweij LM, Proper KI, Hulshof CT, Tulder MW, Mechelen W. Economic evaluation of an occupational health care guideline for prevention of weight gain among employees. Journal of occupational and environmental medicine 2013;55(9):1100. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Aadahl M, Linneberg A, Møller TC, Rosenørn S, Dunstan DW, Witte DR, et al. Motivational counselling to reduce sitting time: a community‐based randomized controlled trial in adults. American Journal of Preventive Medicine 2015;47(5):576‐86. [DOI] [PubMed] [Google Scholar]; NCT00289237. Lifestyle intervention in a general population for prevention of ischaemic heart disease. https://clinicaltrials.gov/show/NCT00289237 2012 (accessed 1 December 2015).
- Adams 2012. On our feet: Feasibility trial of an intervention to reduce sedentary behavior and increase physical activity (PhD Thesis). Greensboro: The University of North Carolina, 2012. [Google Scholar]; Melanie M. Adams MM, Davis PG, Gill DL. A hybrid online intervention for reducing sedentary behavior in obese women. Frontiers in Public Health 2013;1:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aittasalo M, Miilunpalo S, Suni J. The effectiveness of physical activity counselling in a work‐site setting. A randomised, controlled trial. Patient Education and Counselling 2004;55(2):193‐202. [DOI] [PubMed] [Google Scholar]
- Alderman BL, Olson RL, Mattina DM. Cognitive function during low‐intensity walking: a test of the treadmill workstation. Journal of Physical Activity and Health 2014;11(4):752‐8. [DOI] [PubMed] [Google Scholar]
- Ben‐Ner A, Hamann DJ, Koepp G, Manohar CU, Levine J. Treadmill workstations: the effects of walking while working on physical activity and work performance. PLoS ONE 2014;9(2):e88620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird ML, Shing C, Mainsbridge C, Cooley D, Pederson S. Activity behaviours of University staff in the workplace: A pilot study. Journal of Physical Activity and Health 2014 [Epub ahead of print];12(8):1128‐32. [DOI] [PubMed] [Google Scholar]
- Boreham CA, Kennedy RA, Murphy MH, Tully M, Wallace WF, Young I. Training effects of short bouts of stair climbing on cardiorespiratory fitness, blood lipids, and homocysteine in sedentary young women. British Journal of Sports Medicine 2005;39(9):590‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchard DR, Strachan S, Johnson L, Moola F, Chitkara R, McMillan D, et al. Using shared treadmill workstations to promote less time spent in daily low intensity physical activities: A pilot study. Journal of Physical Activity and Health 2015;8:[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Brown DK, Barton JL, Pretty J, Gladwell VF. Walks4work: rationale and study design to investigate walking at lunchtime in the workplace setting. BMC Public Health 2012;12:550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr LJ, Karvinen K, Peavler M, Smith R, Cangelosi K. Multicomponent intervention to reduce daily sedentary time: a randomised controlled trial. BMJ 2013;3(10):e003261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter SE, Jones M, Gladwell VF. Energy expenditure and heart rate response to breaking up sedentary time with three different physical activity interventions. Nutrition Metabolism and Cardiovascular Diseases 2015;25(5):503‐9. [DOI] [PubMed] [Google Scholar]
- Chae D, Kim S, Park Y, Hwang Y. The effects of an academic‐workplace partnership intervention to promote physical activity in sedentary office workers. Workplace Health & Safety 2015;63(6):259‐66. [DOI] [PubMed] [Google Scholar]
- Cheema BS, Houridis A, Busch L, Raschke‐Cheema V, Melville GW, Marshall PW, et al. Effect of an office worksite‐based yoga program on heart rate variability: outcomes of a randomised controlled trial. BMC Complementary and Alternative Medicine 2013;13:82. [DOI] [PMC free article] [PubMed] [Google Scholar]; Cheema BS, Marshall PW, Chang D, Colagiuri B, Machliss B. Effect of an office worksite‐based yoga program on heart rate variability: a randomised controlled trial. BMC Public Health 2011;11:578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia M, Chen B, Suppiah H. Office sitting made less sedentary – A future‐forward approach to reducing physical inactivity at work. Montenegrin Journal of Sports Science and Medicine 2015;4(2):5‐10. [Google Scholar]
- Clemes SA, Patel R, Mahon C, Griffiths PL. Sitting time and step counts in office workers. Occupational Medicine 2014;64(3):188‐92. [DOI] [PubMed] [Google Scholar]
- Dewa CS, Ruiter W, Chau N, Karioja K. Walking for wellness: using pedometers to decrease sedentary behaviour and promote mental health. International Journal of Mental Health Promotion 2009;11(2):24‐8. [Google Scholar]
- Elmer SJ, Martin JC. A cycling workstation to facilitate physical activity in office settings. Applied Ergonomics 2014;45(4):1240‐6. [DOI] [PubMed] [Google Scholar]
- Freak‐Poli R, Wolfe R, Backholer K, Courten M, Peeters A. Impact of a pedometer‐based workplace health program on cardiovascular and diabetes risk profile. Preventive Medicine 2011;53(3):162‐71. [DOI] [PubMed] [Google Scholar]
- Gilson N, Faulker G, Murphy M, Umstattd Meyer M, Ryde G, McCarthy K, et al. An international study of an automated web‐based walking program (Walk@Work) to increase workday step counts in lower active office workers. Journal of Science and Medicine in Sport 2012;15:S235‐6. [Google Scholar]
- Gilson N, Suppini A, Ryde G, Brown H, Brown W. Do height adjustable 'hot' desks change sedentary work behaviour in an open plan office?. Journal of Science and Medicine in Sport 2011;14:e24‐5. [Google Scholar]; Gilson ND, Suppini A, Ryde GC, Brown HE, Brown WJ. Does the use of standing 'hot' desks change sedentary work time in an open plan office?. Preventive Medicine 2012;54(1):65‐7. [DOI] [PubMed] [Google Scholar]
- Gorman E, Ashe MC, Dunstan DW, Hanson HM, Madden K, Winkler EA, et al. Does an 'activity‐permissive' workplace change office workers' sitting and activity time?. PLoS One 2013;8(10):e76723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunseit A, Chau J, Ploeg H, Bauman A. Thinking on your feet: a qualitative evaluation of an installation of sit‐stand desks in a medium‐sized workplace. Journal of Science and Medicine in Sport 2012;15:S195‐6. [Google Scholar]
- Hedge A, Ray EJ. Effect of an electronic height‐adjustable work surface on computer worker musculoskeletal discomfort and productivity. Proceedings of Human Factors & Ergonomic Society, 48th Annual Meeting 2004. SAGE publications, 2004. [Google Scholar]
- Irvine AB, Philips L, Seeley J, Wyant S, Duncan S, Moore RW. Get moving: a web site that increases physical activity of sedentary employees. American Journal of Health Promotion 2011;25(3):199‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John D, Thompson DL, Raynor H, Bielak K, Rider B, Bassett DR. Treadmill workstations: a worksite physical activity intervention in overweight and obese office workers. Journal of Physical Activity and Health 2011;8(8):1034‐43. [DOI] [PubMed] [Google Scholar]
- Júdice PB, Hamilton MT, Sardinha LB, Silva AM. Randomized controlled pilot of an intervention to reduce and break‐up overweight/obese adults’ overall sitting‐time. Trials 2015;16(1):490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy RA, Boreham CA, Murphy MH, Young IS, Mutrie N. Evaluating the effects of a low volume stair climbing programme on measures of health‐related fitness in sedentary office workers. Journal of Sports Science and Medicine 2007;6(4):448‐54. [PMC free article] [PubMed] [Google Scholar]
- Koepp GA, Manohar CU, McCrady‐Spitzer SK, Ben‐Ner A, Hamann DJ, Runge CF, et al. Treadmill desks: a 1‐year prospective trial. Obesity (Silver Spring) 2013;21(4):705‐11. [DOI] [PubMed] [Google Scholar]
- Lara A, Yancey AK, Tapia‐Conye R, Flores Y, Kuri‐Morales P, Mistry R, et al. Pausa para tu Salud: reduction of weight and waistlines by integrating exercise breaks into workplace organizational routine. Preventing Chronic DiseaseEpub 2008; Vol. 5, issue 1:A12. [PMC free article] [PubMed]
- Maeda H, Quartiroli A, Vos PW, Carr LJ, Mahar MT. Feasibility of retrofitting a university library with active workstations to reduce sedentary behavior. American Journal of Preventive Medicine 2014;46(5):525‐8. [DOI] [PubMed] [Google Scholar]
- Mainsbridge CP, Cooley PD, Fraser SP, Pedersen SJ. The effect of an e‐health intervention designed to reduce prolonged occupational sitting on mean arterial pressure. Journal of Occupational and Environmental Medicine 2014;56(11):1189‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair JL, Boreham CA, Ditroilo M, McKeown D, Lowery MM, Caulfield B, et al. Benefits of a worksite or home‐based bench stepping intervention for sedentary middle‐aged adults ‐ a pilot study. Clinical Physiology and Functional Imaging 2014;34(1):10‐7. [DOI] [PubMed] [Google Scholar]
- Marshall AL, Leslie ER, Bauman AE, Marcus BH, Owen N. Print versus web site physical activity programs: a randomised trial. American Journal of Preventive Medicine 2003;25(2):88‐94. [DOI] [PubMed] [Google Scholar]
- McAlpine DA, Manohar CU, McCrady SK, Hensrud D, Levine JA. An office‐place stepping device to promote workplace physical activity. British Journal of Sports Medicine 2007;41(12):903‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyachi M, Kurita S, Tripette J, Takahara R, Yagi Y, Murakami H. Installation of a stationary high desk in the workplace: effect of a 6‐week intervention on physical activity. BMC Public Health 2015;15:368. [DOI] [PMC free article] [PubMed] [Google Scholar]; UMIN000016731. Installation of a stationary high desk in the workplace: effect of a 6‐week intervention on physical activity. UMIN‐CTR Clinical Trial (accessed 3 June 2015). [DOI] [PMC free article] [PubMed]
- NCT01221363. Reduction of sitting time ‐ a randomised controlled intervention study. http://clinicaltrials.gov/ct2/show/NCT01221363 (accessed 15 March 2014).
- Opdenacker J, Boen F. Effectiveness of face‐to‐face versus telephone support in increasing physical activity and mental health among university employees. Journal of Physical Activity and Health 2008;5(6):830‐43. [DOI] [PubMed] [Google Scholar]
- Ouyang P, Stewart KJ, Bedra ME, York S, Valdiviezo C, Finkelstein J. Text messaging to reduce inactivity using real‐time step count monitoring in sedentary overweight females. Circulation 2015;131:AMP10. [Google Scholar]
- ACTRN12612000743864. Can a participatory workplace intervention improve sedentary behaviour and physical activity in office workers?. http://www.anzctr.org.au/ACTRN12612000743864.aspx (accessed 14 March 2014). ; Parry S, Straker L, Gilson ND, Smith AJ. Participatory workplace interventions can reduce sedentary time for office workers ‐ a randomised controlled trial. PLoS One 2013;8(11):e78957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk NP, Katz AS, Lowry M, Payfer JR. Reducing occupational sitting time and improving worker health: the Take‐a‐Stand Project. Preventing Chronic Disease 2012;9:e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slootmaker SM, Chinapaw MJ, Schuit AJ, Seidell JC, Mechelen W. Feasibility and effectiveness of online physical activity advice based on a personal activity monitor: randomised controlled trial. Journal of Medical Internet Research 2009;11(3):e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternfeld B, Block C, Quesenberry CP Jr, Block TJ, Husson G, Norris JC, et al. Improving diet and physical activity with ALIVE: a worksite randomised trial. American Journal of Preventive Medicine 2009;36(6):475‐83. [DOI] [PubMed] [Google Scholar]
- Straker L, Abbott R, Heiden M, Mathiassen S, Toomingas A. Sit‐stand desks and sedentary behavior in Swedish call centre workers. Journal of Science and Medicine in Sport 2012;15:S194. [Google Scholar]; Straker L, Abbott RA, Heiden M, Mathiassen SE, Toomingas A. Sit‐stand desks in call centres: associations of use and ergonomics awareness with sedentary behavior. Applied Ergonomics 2013;44(4):517‐22. [DOI] [PubMed] [Google Scholar]
- NCT01150084. Step by Step: A Feasibility Study of the Promotion of Lunchtime Walking to Increase Physical Activity and Improve Mental Well‐being in Sedentary Employees. http://clinicaltrials.gov/ct2/show/NCT01150084 (accessed 15 March 2014). ; Thogersen‐Ntoumani C, Loughren E, Duda J, Fox KR. "Step by Step": A feasibility study of a lunchtime walking intervention designed to increase walking, improve mental well‐being and work performance in sedentary employees: rationale and study design. BMC Public Health 2010;10:578. [DOI] [PMC free article] [PubMed] [Google Scholar]; Thogersen‐Ntoumani C, Loughren E, Duda J, Fox KR. Step by Step: The feasibility of a 16‐week workplace lunchtime walking intervention for physically inactive employees. Journal of Physical Activity And Health 2013;10:Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Thompson WG, Koepp GA, Levine JA. Increasing physician activity with treadmill desks. Work2014; Vol. 48, issue 1:47‐51. [DOI] [PubMed]
- Thorp AA, Kingwell BA, English C, Hammond L, Sethi P, Owen N. Alternating sitting and standing increases the workplace energy expenditure of overweight adults. Journal of Physical Activity and Health 2015;8:[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Yancey AK, McCarthy WJ, Taylor WC, Merlo A, Gewa C, Weber MD, et al. The Los Angeles Lift Off: a sociocultural environmental change intervention to integrate physical activity into the workplace. Preventive Medicine 2004;38(6):848‐56. [DOI] [PubMed] [Google Scholar]
- Østerås H, Sigbjørn H. The effectiveness of a pragmatic worksite physical activity program on maximal oxygen consumption and the physical activity level in healthy people. Journal of Bodywork and Movement Therapies 2006;10(1):51‐7. [Google Scholar]
References to studies awaiting assessment
- Carpenter K, Feltes L, Vuing B, Kalbes A, Koepp G, Dutta N, et al. Effect of sit‐stand workstations on metabolic risk in sedentary workers: A randomized controlled trial. The Journal of the Federation of American societies for Experimental Biology 2015;29:supplement 1. [Google Scholar]
- Dutta N, Koepp G, Schmitz C, Stovitz SD, Levine JA, Pereira MA. Impact of adjustable sit‐stand workstations on physical activity in sedentary office workers. Diabetes 2013;62:A186. [Google Scholar]
- Kirk A, Fitzsimons C, Murphy M, Mutrie N. Effect of a person centred consultation intervention to reduce the sedentary behaviour of working Scottish adults. Journal of Science and Medicine in Sport 2012;15:S314. [Google Scholar]
References to ongoing studies
- ACTRN12612001290886. The effectiveness of the 10,000 Steps workplace challenge in increasing health outcomes for employees at Rockhampton Regional Council. http://www.anzctr.org.au/ACTRN12612001290886.aspx (accessed 15 March 2014).
- ACTRN12614000252617. Comparison of organisational support vs. organisational plus technology support for reducing prolonged sitting in the office workplace. http://www.anzctr.org.au/ACTRN12614000252617.aspx (accessed 15 March 2014).
- Bergman F, Boraxbekk CJ, Wennberg P, Sörlin A Olsson T. Increasing physical activity in office workers – the Inphact Treadmill study; a study protocol for a 13‐month randomized controlled trial of treadmill workstations. BMC Public Health 2015;15(1):632. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT01997970. NEAT ‐ Prevention and treatment of overweight and obesity. (InphactUm). https://clinicaltrials.gov/ct2/show/NCT01997970 (accessed 3 June 2015).
- ACTRN12611000742976. Stand Up Victoria: a trial to determine whether environmental modification and behavioural counselling can lead to reductions in workplace sitting time in office workers. http://www.anzctr.org.au/ACTRN12611000742976.aspx (accessed 15 March 2014). ; Dunstan DW, Wiesner G, Eakin EG, Neuhaus M, Owen N, LaMontagne AD, et al. Reducing office workers' sitting time: rationale and study design for the Stand Up Victoria cluster randomised trial. BMC Public Health 2013;13:1057. [DOI] [PMC free article] [PubMed] [Google Scholar]; Neuhaus M, Healy GN, Fjeldsoe BS, Lawler S, Owen N, Dunstan DW, et al. Iterative development of Stand Up Australia: a multi‐component intervention to reduce workplace sitting. International Journal of Behavioral Nutrition and Physical Activity 2014;11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finni T, Saakslahti A, Laukkanen A, Pesola A, Sipilä S. A family based tailored counselling to increase non‐exercise physical activity in adults with a sedentary job and physical activity in their young children: design and methods of a year‐long randomised controlled trial. BMC Public Health2011; Vol. 11. [DOI] [PMC free article] [PubMed]; ISRCTN28668090. Actions to reduce sedentary time in parents and their young children. http://www.isrctn.com/ISRCTN28668090 (accessed 15 March 2014).
- Hall J, Mansfield L, Kay T, McConnell AK. The effect of a sit‐stand workstation intervention on daily sitting, standing and physical activity: protocol for a12 month workplace randomised control trial. BMC Public Health 2015;15:152. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT02172599. Take a stand for workplace health: A sit‐stand workstation project evaluation. https://clinicaltrials.gov/ct2/show/NCT02172599?term=workplace+and+sitting&rank=1 (accessed 3 June 2015).
- ISRCTN25767399. Impact of Booster Breaks on physical activity among sedentary employees: a cluster randomized controlled trial. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN25767399 (accessed 3 June 2015).
- ACTRN12610000301066. Walking to Wellness in an ageing sedentary university community. http://www.anzctr.org.au/ACTRN12610000301066.aspx (accessed 15 March 2014). ; Mackey M, Bohle P, Taylor P, Biase T, McLoughlin C, Purnell K. 'Walking to wellness' in an ageing sedentary university community‐a randomised controlled feasibility study. Physiotherapy. 2011; Vol. 97:eS733‐eS4. [Google Scholar]; Mackey MG, Bohle P, Taylor P, Biase T, McLoughlin C, Purnell K. Walking to wellness in an ageing sedentary university community: design, method and protocol. Contemporary Clinical Trials 2011;32(2):273‐9. [DOI] [PubMed] [Google Scholar]
- Borras CM, Garriga MG, Martinez E, Cantera CM, Puigdoménech E, Solà M, et al. Effectiveness of a primary care‐based intervention to reduce sitting time in overweight and obese patients (SEDESTACTIV): a randomised controlled trial; rationale and study design. BMC Public Health2014; Vol. 14. [DOI] [PMC free article] [PubMed]; NCT01729936. SedestActiv Project: intervention to reduce diary hours of sitting time in overweight and obese patients. http://clinicaltrials.gov/ct2/show/NCT01729936 (accessed 15 March 2014).
- NCT01787643. Standing behavior after installation of height‐adjustable desks. http://clinicaltrials.gov/ct2/show/NCT01787643 (accessed 15 March 2014).
- NCT01846013. Increasing workplace physical activity in sedentary office workers. http://clinicaltrials.gov/ct2/show/NCT01846013 (accessed 15 March 2014).
- NCT01996176. Take a Stand! ‐ a cluster randomised controlled intervention study at four office‐based workplaces aiming to reduce occupational sitting time. http://clinicaltrials.gov/ct2/show/NCT01996176 (accessed 15 March 2014).
- NCT02376504. Modifying the Workplace to Decrease Sedentary Behavior and Improve Health. https://clinicaltrials.gov/ct2/show/NCT02376504?term=workplace+and+sitting&rank=3 (accessed 3 June 2015).
- ISRCTN10967042. SMArT Work: Stand More AT Work. http://www.isrctn.com/ISRCTN10967042 (accessed 25 December 2015). ; O’Connell SE, Jackson BR, Edwardson CL, Yates T, Biddle SJH, Davies MJ, et al. Providing NHS staff with height‐adjustable workstations and behaviour change strategies to reduce workplace sitting time:protocol for the Stand More AT (SMArT)Work cluster randomised controlled trial. BMC Public Health 2015;15:1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ACTRN12613000366752. Reducing sedentary behaviour in office workers. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=363960 (accessed 15 March 2014). ; Radas A, Mackey M, Leaver A, Bouvier AL, Chau JY, Shirley D, et al. Evaluation of ergonomic and education interventions to reduce occupational sitting in office‐based university workers: study protocol for a randomised controlled trial. Trials2013; Vol. 14. [DOI] [PMC free article] [PubMed]
- Hoye K, Boen F, Lefevre J. The effects of physical activity feedback on behavior and awareness in employees: study protocol for a randomised controlled trial. International Journal of Telemedicine and Applications 2012;2012:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
- Aadahl M, Jorgensen T. Validation of a new self‐report instrument for measuring physical activity. Medicine and Science in Sports and Exercise 2003;35(7):1196‐202. [DOI] [PubMed] [Google Scholar]
- The Royal Australasian College of Physicians. Australasian Faculty of Occupational and Environmental Medicine. https://www.racp.edu.au/page/about‐afoem (accessed 12 December 2014).
- Australian Institute of Health and Welfare. Australia's health 2008. http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=6442453674 (accessed 15 September 2013).
- Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Medicine and Science in Sports and Exercise 2000;32(9 Suppl):S498‐504. [DOI] [PubMed] [Google Scholar]
- Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DRJ, Tudor‐Locke C, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Medicine and Science in Sports and Exercise 2011;43(8):1575‐81. [DOI] [PubMed] [Google Scholar]
- Andersen JH, Haahr JP, Frost P. Risk factors for more severe regional musculoskeletal symptoms: a two‐year prospective study of a general working population. Arthritis and rheumatism 2007;56(4):1355‐64. [DOI] [PubMed] [Google Scholar]
- Atkinson J, Haynes K. Standing meeting rooms – exploring enablers and barriers of interventions to reduce sitting time in the workplace. Australian and New Zealand Journal of Public Health June 2014;38(3):291‐2. [DOI] [PubMed] [Google Scholar]
- Bailey DP, Locke CD. Breaking up prolonged sitting with light‐intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. Journal of Science and Medicine in Sport 2015;18(3):294‐8. [DOI] [PubMed] [Google Scholar]
- Beers EA, Roemmich JN, Epstein LH, Horvath PJ. Increasing passive energy expenditure during clerical work. European Journal of Applied Physiology 2008;103(3):353‐60. [DOI] [PubMed] [Google Scholar]
- Botter J, Ellegast RP, Burford EM, Weber B, Könemann R, Commissaris DA. Comparison of the postural and physiological effects of two dynamic workstations to conventional sitting and standing workstations. Ergonomics 2015;(Epub ahead of print):1‐15. [DOI] [PubMed] [Google Scholar]
- Buckley JP, Hedge A, Yates T, Copeland RJ, Loosemore M, Hamer M, et al. The sedentary office: an expert statement on the growing case for change towards better health and productivity. British Journal of Sports Medicine 2015;49(21):1357‐62. [DOI] [PubMed] [Google Scholar]
- Campbell MK, Mollison J, Grimshaw JM. Cluster trials in implementation research: estimation of intracluster correlation coefficients and sample size. Statistics in Medicine 2001;20(3):391‐9. [DOI] [PubMed] [Google Scholar]
- Canadian Center for Occupational Health and Safety (CCOHS). Downside of sitting on our backsides. Health and safety report 2010. http://www.ccohs.ca/newsletters/hsreport/issues/2010/03/ezine.html (accessed 10 Nov 2013); Vol. 8, issue 3.
- Chaput JP, Saunders TJ, Tremblay MS, Katzmarzyk PT, Tremblay A, Bouchard C. Workplace standing time and the incidence of obesity and type 2 diabetes: a longitudinal study in adults. BMC Public Health 2015;10(15):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau JY, Ploeg HP, Uffelen JG, Wong J, Riphagen I, Healy GN, et al. Are workplace interventions to reduce sitting effective? A systematic review. Preventive Medicine 2010;51(5):352‐6. [DOI] [PubMed] [Google Scholar]
- Chau JY, Ploeg HP, Dunn S, Kurko J, Bauman AE. Validity of the occupational sitting and physical activity questionnaire. Medicine and Science in Sports and Excercise 2012;44(1):118‐25. [DOI] [PubMed] [Google Scholar]
- Chaua JY, Grunseita A, Midthjellb K, Holmen J, Holmenabb TL, Baumana AE, et al. Cross‐sectional associations of total sitting and leisure screen time with cardio metabolic risk in adults. Results from the HUNT study, Norway. Journal of Science and Medicine in Sport 2014;17:78‐84. [DOI] [PubMed] [Google Scholar]
- Clark BK, Sugiyama T, Healy GN, Salmon J, Dunstan DW, Owen N. Validity and reliability of measures of television viewing time and other non‐occupational sedentary behaviour of adults: a review. Obesity Reviews 2009;10(1):7‐16. [DOI] [PubMed] [Google Scholar]
- Coenen P, Healy GN, Winkler E, Dunstan DW, Straker L. Musucloskeletal pain is a barrier for sedentary behavior interventions. Proceedings 19th triennial congress of the IEA. Melbourne, 2015. [Google Scholar]
- Commissaris DACM, Douwes M, Schoenmaker N, Korte EM. Recommendations for sufficient physical activity at work. 2007. http://www.nordiskergonomi.org/nes2007/CD_NES_2007/papers/A79_Commissaris.pdf. Elsevier, Oxford, (accessed 25 November 2013).
- Commissaris DACM, Konemann R, Mastrigt SH, Burford EM, Botter J, Douwes M, et al. Effects of a standing and three dynamic workstations on computer task performance and cognitive function tests. Applied Ergonomics 2014;45:1570‐8. [DOI] [PubMed] [Google Scholar]
- Commissaris DACM, Huysmans MA, Mathiassen SE, Srinivasan D, Koppes LLJ, Hendriksen IJM. Interventions to reduce sedentary behavior and increase physical activity during productive work: a systematic review. Scandinavian Journal of Work Environment and Health 2015;41:[epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Cooley D, Pedersen S, Mainsbridge C. Assessment of the impact of a workplace intervention to reduce prolonged occupational sitting time. Qualitative Health Research [Epub ahead of print] 14 November 2013. [DOI] [PubMed]
- Craft LL, Zderic TW, Gapstur SM, Vaniterson EH, Thomas DM, Siddique J, et al. Evidence that women meeting physical activity guidelines do not sit less: an observational inclinometry study. International Journal of Behavioral Nutrition and Physical Activity 2012;9:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig CL, Brownson RC, Cragg SE, Dunn AL. Exploring the effect of the environment on physical activity: a study examining walking to work. American Journal of Preventive Medicine 2002;23(2 Suppl):36‐43. [DOI] [PubMed] [Google Scholar]
- Dunstan DW, Thorp AA, Healy N. Prolonged sitting: is it a distinct coronary heart disease risk factor?. Current Opinion in Cardiology 2011;26(5):412‐9. [DOI] [PubMed] [Google Scholar]
- Duvivier BM, Schaper NC, Bremers MA, Crombrugge G, Menheere PP, Kars M, et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS ONE 2013;8(2):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test.. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochrane Effective Practice and Organisation of Care Group. EPOC resources for review authors. http://epoc.cochrane.org/epoc‐resources‐review‐authors (accessed 10 June 2014).
- Franklin BA. Health implications of low cardiorespiratory fitness, too little exercise, and too much sitting time: changing paradigms and perceptions. American Journal of Health Promotion 2011;25(4):exi‐v. [DOI] [PubMed] [Google Scholar]
- Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJH. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychology Review 2015;16:1‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson ND, Burton NW, Uffelen JG, Brown WJ. Occupational sitting time: employees' perceptions of health risks and intervention strategies. Health Promotion Journal of Australia 2011;22(1):38‐43. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist G, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. Rating quality of evidence and strength of recommendations GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graf M, Krieger R, Läubli T, Martin B. Should we recommend people to stand more than sit at work?. Proceedings 19th triennial congress of the IEA. Melbourne, 2015. [Google Scholar]
- Hamilton MT, Healy GN, Dunstan DW, Zderic TW, Owen N. Too little exercise and too much sitting: Inactivity physiology and the need for new recommendations on sedentary behavior. Current Cardiovascular Risk Reports 2008;2(4):292‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care 2008;31(2):369‐71. [DOI] [PubMed] [Google Scholar]
- Healy GN, Clark BK, Winkler EA, Gardiner PA, Brown WJ, Matthews CE. Measurement of adults’ sedentary time in population‐based studies. American Journal of Preventive Medicine 2011;41:216‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
- Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviours in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 2003;289(14):1785‐91. [DOI] [PubMed] [Google Scholar]
- Ijaz S, Verbeek JH, Mischke C, Ruotsalainen J. Inclusion of non randomized studies in Cochrane systematic reviews was found to be in need of improvement. Journal of Clinical Epidemiology 2014;67(6):645‐53. [DOI: 10.1016/j.jclinepi.2014.01.001; PUBMED: 24725644] [DOI] [PubMed] [Google Scholar]
- ISO 11226:2000. Ergonomics ‐ Evaluation of static working postures. http://www.iso.org/iso/catalogue_detail.htm?csnumber=25573 (accessed 13 November 2013).
- Janssen X, Cliff DP. Issues related to measuring and interpreting objectively measured sedentary behavior data. Measurement in Physical Education and Exercise Science 2015;19(3):116‐24. [Google Scholar]
- John D, Bassett D, Thompson D, Fairbrother J, Baldwin D. Effect of using a treadmill workstation on performance of simulated office work tasks. Journal of Physical Activity and Health 2009;6(5):617‐24. [DOI] [PubMed] [Google Scholar]
- Júdice PB, Hamilton MT, Sardinha LB, Zderic TW, Silva AM. What is the metabolic and energy cost of sitting, standing and sit/stand transitions?. European Journal of Applied Physiology 2015;115:[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Kanoun N. Validation of the ActivPAL activity monitor as a measure of walking at pre‐determined slow walking speeds in a healthy population in a controlled setting. Reinvention: a Journal of Undergraduate Research 2009, http://www.warwick.ac.uk/go/reinventionjournal/issues/volume2issue2/kanoun (accessed 13 November 2013).
- Karakolis T, Callaghan JP. The impact of sit‐stand office workstations on worker discomfort and productivity: A review. Applied Ergonomics 2014;45(3):799‐806. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT. Standing and mortality in a prospective cohort of Canadian adults. Medicine and Science in Sports and Exercise 2014;46(5):940‐6. [DOI] [PubMed] [Google Scholar]
- Kim Y, Barry VW, Kang M. Validation of the ActiGraph GT3X and activPAL Accelerometers for the Assessment of Sedentary Behavior. Measurement in Physical Education and Exercise Science 2015;19(3):125‐37. [Google Scholar]
- Lagersted‐Olsen J, Korshøj M, Skotte J, Carneiro IG, Søgaard K, Holtermann A. Comparison of objectively measured and self‐reported time spent sitting. International Journal of Sports Medicine 2014;35(6):534‐40. [DOI] [PubMed] [Google Scholar]
- Larsen RN, Kingwell BA, Sethi P, Cerin E, Owen N, Dunstan DW. Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutrition Metabolism and Cardiovascular Diseases 2014;24(9):976‐82. [DOI] [PubMed] [Google Scholar]
- Levine JA, Miller JM. The energy expenditure of using a "walk‐and‐work" desk for office workers with obesity. British Journal of Sports Medicine 2007;41(9):558‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacEwen BT, MacDonald DJ, Burr JF. A systematic review of standing and treadmill desks in the workplace. Preventive Medicine 2015;70C:50‐8. [DOI] [PubMed] [Google Scholar]
- Manini TM, Carr LJ, King AC, Marshall S, Robinson TN, Rejeski WJ. Interventions to reduce sedentary behavior. Medicine and Science in Sports and Exercise 2015;47(6):1306‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansoubi M, Pearson N, Biddle SJ, Clemes S. The relationship between sedentary behaviour and physical activity in adults: a systematic review. Preventive Medicine 2014;69C:28. [DOI] [PubMed] [Google Scholar]
- Mansoubi M, Pearson N, Clemes SA, Biddle SJH, Bodicoat DH, Tolfrey K, et al. Energy expenditure during common sitting and standing tasks: examining the 1.5 MET definition of sedentary behaviour. BMC Public Health 2015;15:516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansoubi M, Pearson N, Biddle SJH, Clemes SA. Using sit‐to‐stand workstations in offices: Is there a compensation effect?. Medicine & Science in Sports & Excercise 2015;47:(epub ahead of print). [DOI] [PubMed] [Google Scholar]
- Marszalek J, Morgulec‐Adamowicz N, Rutkowska I, Kosmol A. Using ecological momentary assessment to evaluate current physical activity. BioMed Research International 2014;Article ID 915172:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin A, Fitzsimons C, Jepson R, Saunders DH, Ploeg HP, Teixeira PJ, et al. Interventions with potential to reduce sedentary time in adults: systematic review and meta‐analysis. British Journal of Sports Medicine 2015;49(16):1056‐63. [DOI] [PubMed] [Google Scholar]
- McCrady SK, Levine JA. Sedentariness at work: how much do we really sit?. Obesity (Silver Spring, Md) 2009;17(11):2103‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEachan RR, Lawton RJ, Jackson C, Conner M, Meads DM, West RM. Testing a workplace physical activity intervention: a cluster randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2011;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuhaus M, Eakin EG, Straker L, Owen N, Dunstan DW, Reid N, et al. Reducing occupational sedentary time: a systematic review and meta‐analysis of evidence on activity‐permissive workstations. Obesity Reviews 2014;15(10):822‐38. [DOI] [PubMed] [Google Scholar]
- Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obesity Reviews 2012;13(8):659‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogilvie D, Foster CE, Rothnie H, Cavill N, Hamilton V, Fitzsimons CF, et al. Interventions to promote walking: systematic review. BMJ 2007;334(7605):1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry S, Straker L. The contribution of office work to sedentary behaviour associated risk. BMC Public Health 2013;13(1):296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plotnikoff R, Karunamuni N. Reducing sitting time: the new workplace health priority. Archives of Environmental and Occupational Health 2012;67(3):125‐7. [DOI] [PubMed] [Google Scholar]
- Prince SA, Saunders TJ, Gresty K, Reid RD. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta‐analysis of controlled trials. Obesity Reviews 2014;15(11):905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2013.
- Rutten GM, Savelberg HH, Biddle SJ, Kremers SP. Interrupting long periods of sitting: good STUFF. International Journal of Behavioral Nutrition and Physical Activity 2013;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan CG, Dall PM, Granat MH, Grant PM. Sitting patterns at work: objective measurement of adherence to current recommendations. Ergonomics 2011;54(6):531‐8. [Google Scholar]
- Rzewnicki R, Yves VA, Ilse DB. Addressing over reporting on the International Physical Activity Questionnaire (IPAQ) telephone survey with a population sample. Public Health Nutrition 2003;6(3):299‐305. [DOI] [PubMed] [Google Scholar]
- Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. British Journal of Sports Medicine 2003;37(3):197‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan DA. Changing disease trends in the Asia‐Pacific. Climacteric 2011;14(5):529‐34. [DOI] [PubMed] [Google Scholar]
- Tew GA, Posso MC, Arundel CE, McDaid CM. Systematic review: height‐adjustable workstations to reduce sedentary behaviour in office‐based workers. Occupational Medicine 2015;65(5):357‐66. [DOI] [PubMed] [Google Scholar]
- Thorp AA, Healy GN, Winkler E, Clark BK, Gardiner PA, Owen N, et al. Prolonged sedentary time and physical activity in workplace and non‐work contexts: a cross‐sectional study of office, customer service and call centre employees. International Journal of Behavioral Nutrition and Physical Activity 2012;9:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torbeyns T, Meeusen R, Bailey S, Bos I. Active workstations to fight sedentary behaviour. Sports Medicine 2014;44(9):1261. [DOI] [PubMed] [Google Scholar]
- Tudor‐Locke C, Schuna JM Jr, Frensham LJ, Proenca M. Changing the way we work: elevating energy expenditure with workstation alternatives. International Journal of Obesity 2013;38(6):755‐6. [DOI] [PubMed] [Google Scholar]
- United States Patent and Trademark Office (USPTO). United States Patent 6,070,943. Guery‐Strahm R. Ergonomic seating unit. June 6, 2000. http://patft.uspto.gov/netacgi/nph‐Parser?Sect2=PTO1&Sect2=HITOFF&p=1&u=/netahtml/PTO/search‐bool.html&r=1&f=G&l=50&d=PALL&RefSrch=yes&Query=PN/6070943 (accessed 2 December 2013).
- Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all‐cause mortality risk in 222 497 Australian adults. Archives of Internal Medicine 2012;172(6):494‐500. [DOI] [PubMed] [Google Scholar]
- Uffelen JG, Wong J, Chau JY, Ploeg HP, Riphagen I, Gilson ND, et al. Occupational sitting and health risks: a systematic review. American Journal of Preventive Medicine 2010;39(4):379‐88. [DOI] [PubMed] [Google Scholar]
- Victorian Health Promotion Foundation. Reducing prolonged sitting in the workplace. An evidence review: summary report. 2012. http://www.vichealth.vic.gov.au/˜/media/ResourceCentre/PublicationsandResources/Economic%20participation/2012%20workplace/VH_Reducing_prolonged_sitting_07.ashx (accessed 4 December 2013).
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378(9793):815‐25. [DOI] [PubMed] [Google Scholar]
- World Health Organization/World Economic Forum. Preventing non communicable diseases in the workplace through diet and physical activity. http://www.weforum.org/pdf/Wellness/WHOWEF_report.pdf 2008, (accessed 10 June 2014).
- Wilks S, Mortimer M, Nylén P. The introduction of sit‐stand worktables; aspects of attitudes, compliance and satisfaction. Applied Ergonomics 2006;37(3):359‐65. [DOI] [PubMed] [Google Scholar]


