Abstract
Background
Ulcerative colitis (UC) is a chronic inflammatory bowel disease. Corticosteroids and 5‐aminosalicylates are the most commonly used therapies. However, many patients require immunosuppressive therapy for steroid‐refractory and steroid‐dependent disease. Methotrexate is a medication that is effective for treating a variety of inflammatory diseases, including Crohn's disease. This review was performed to determine the effectiveness of methotrexate treatment in UC patients. This review is an update of a previously published Cochrane review.
Objectives
To assess the efficacy and safety of methotrexate for induction of remission in patients with UC.
Search methods
MEDLINE, EMBASE, CENTRAL and the Cochrane IBD/FBD group specialized trials register were searched from from inception to June 26, 2014. Study references and review papers were also searched for additional trials. Abstracts from major gastroenterological meetings were searched to identify research published in abstract form only.
Selection criteria
Randomized controlled trials comparing methotrexate with placebo or an active comparator in patients with active ulcerative colitis were considered for inclusion.
Data collection and analysis
Two authors independently reviewed studies for eligibility, extracted data and assessed study quality using the Cochrane risk of bias tool. The primary outcome measure was the proportion of patients who achieved clinical remission and withdrawal from steroids as defined by the studies and expressed as a percentage of the total number of patients randomized (intention‐to‐treat analysis). We calculated the risk ratio (RR) and corresponding 95% confidence intervals (95% CI) for dichotomous outcomes. The overall quality of the evidence supporting the primary outcome was assessed using the GRADE criteria.
Main results
Two studies (n = 101 patients) were included in the review. One study (n = 67) compared oral methotrexate 12.5 mg/week) to placebo. The other study (n = 34) compared oral methotrexate (15 mg/week) to 6‐mercaptopurine (1.5 mg/kg/day) and 5‐aminosalicylic acid (3 g/day). The placebo‐controlled study was judged to be at low risk of bias. The other study was judged to be at high risk of bias due to an open‐label design. There was no statistically significant difference in clinical remission rates between methotrexate and placebo patients. Forty‐seven per cent (14/30) of methotrexate patients achieved clinical remission and complete withdrawal from steroids during the study period compared to 49% (18/37) of placebo patients (RR 0.96, 95% CI 0.58 to 1.59. A GRADE analysis indicated that the overall quality of the evidence supporting this outcome was low due to very sparse data (32 events). There were no statistically significant differences in the proportion of patients who achieved clinical remission and withdrawal from steroids in the study comparing oral methotrexate to 6‐mercaptopurine and 5‐aminosalicylic acid. At 30 weeks, 58% (7/12) of methotrexate patients achieved clinical remission and withdrawal from steroids compared to 79% (11/14) of 6‐mercaptopurine patients (RR 0.74, 95% CI 0.43 to 1.29) and 25% of 5‐aminosalicylic acid patients (RR 2.33, 95% CI 0.64 to 8.49). GRADE analyses indicated that the overall quality of the evidence was very low due to very sparse data (18 and 9 events respectively) and and high risk of bias. In the placebo‐controlled trial two patients (7%) were withdrawn from the methotrexate group due to adverse events (leucopenia, migraine) compared to one patient (3%) who had a rash in the placebo group (RR 2.47, 95% CI 0.23 to 25.91). Adverse events experienced by methotrexate patients in the active comparator study included nausea and dyspepsia, mild alopecia, mild increase in aspartate aminotransferase levels, peritoneal abscess, hypoalbuminemia, severe rash and atypical pneumonia.
Authors' conclusions
Although methotrexate was well‐tolerated, the studies showed no benefit for methotrexate over placebo or active comparators. The results for efficacy outcomes between methotrexate and placebo, methotrexate and 6‐mercaptopurine and methotrexate and 5‐aminosalicylic acid were uncertain. Whether a higher dose or parenteral administration would be effective for induction therapy is unknown. At present there is no evidence supporting the use of methotrexate for induction of remission in active ulcerative colitis. A trial in which larger numbers of patients receive a higher dose of oral methotrexate should be considered. Currently there are two large ongoing placebo‐controlled trials (METEOR and MERIT‐UC) assessing the efficacy and safety of intramuscular or subcutaneous methotrexate in patients with active UC which may help resolve the evidence supporting the use of methotrexate as therapy for active of ulcerative colitis.
Keywords: Humans; Administration, Oral; Anti‐Inflammatory Agents; Anti‐Inflammatory Agents/administration & dosage; Anti‐Inflammatory Agents/adverse effects; Colitis, Ulcerative; Colitis, Ulcerative/drug therapy; Immunosuppressive Agents; Immunosuppressive Agents/administration & dosage; Immunosuppressive Agents/adverse effects; Induction Chemotherapy; Induction Chemotherapy/methods; Mercaptopurine; Mercaptopurine/administration & dosage; Mesalamine; Mesalamine/administration & dosage; Methotrexate; Methotrexate/administration & dosage; Methotrexate/adverse effects; Randomized Controlled Trials as Topic
Plain language summary
Methotrexate for treatment of chronic active ulcerative colitis
What is ulcerative colitis?
Ulcerative colitis is a long‐term (chronic) inflammatory bowel disease characterized by pains (abdominal cramping), a need to rush to the toilet to pass feces (fecal urgency) and bloody diarrhea.
What is methotrexate?
Methotrexate is a medicine that reduces the body's natural immune responses and may reduce the inflammation associated with ulcerative colitis. When people with ulcerative colitis are experiencing the symptoms of the disease it is said to be ‘active’; periods when the symptoms stop are called ‘remission’.
What did the researchers investigate?
The researchers investigated whether methotrexate produces remission in people with active ulcerative colitis, and whether it causes any harms (side effects). The researchers searched the medical literature extensively up to June 26, 2014.
What did the researchers find?
The researchers identified two studies that included a total of 101 participants. One was a high quality study (67 participants) that compared oral methotrexate (12.5 mg/week) to a placebo (a sugar pill or fake medicine). The other study (34 participants) compared oral methotrexate (15 mg/week) against 6‐mercaptopurine (an immunosuppressive drug at a dose of 1.5 mg/kg/day) and against 5‐aminosalicylic acid (an anti‐inflammatory drug at a dose of 3 g/day).
In the high quality study, there was no difference between the methotrexate and placebo treatment groups for the number of people who achieved remission and were able to stop taking steroids. This suggests that, when used at this low dose (12.5 mg/week), methotrexate does not produce remission from ulcerative colitis. However, this result is uncertain because of the small number of people who were assessed.
The other, smaller study showed no differences between methotrexate and the other treatments in the proportion of participants who experienced remission and were able to stop taking steroids. This result is also uncertain due to poor study design and the low number of participants.
The side effects reported in the two studies included leucopenia (a decrease in the number of white blood cells), migraine, rash, nausea and dyspepsia (indigestion), mild alopecia (hair loss), mild increase in levels of an enzyme found in the liver (aspartate aminotransferase), a collection of pus in the abdominal tissue (peritoneal abscess), abnormally low levels of the protein albumin in the blood (hypoalbuminemia), and pneumonia.
At present, the results from medical trials do not support the use of low dose oral methotrexate (12.5 mg to 15 mg/week) for the production of remission in active ulcerative colitis. It is not known whether a higher dose of oral methotrexate, or giving methotrexate by a different route (e.g. by injection), would increase the likelihood of remission.
In future, researchers should consider organising a study with a larger number of participants who receive a higher dose of oral methotrexate. Currently, there are two large studies being run that compare a higher dose of methotrexate – given by injection – with placebo in people with active ulcerative colitis (the METEOR and MERIT‐UC studies). The results of these studies may resolve the uncertainty surrounding the use of methotrexate for the treatment of active ulcerative colitis.
Summary of findings
Summary of findings for the main comparison. Methotrexate compared to placebo for induction of remission in ulcerative colitis.
| Methotrexate compared to Placebo for induction of remission in ulcerative colitis | ||||||
| Patient or population: patients with induction of remission in ulcerative colitis Settings: Outpatient Intervention: Methotrexate Comparison: Placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Methotrexate | |||||
| Remission and complete withdrawal from steroids Follow‐up: mean 36 weeks | 486 per 10001 | 467 per 1000 (282 to 774) | RR 0.96 (0.58 to 1.59) | 67 (1 study) | ⊕⊕⊝⊝ low2 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Control group risk comes from control arm of study 2 Very sparse data (32 events)
Summary of findings 2. Methotrexate compared to 6‐mercaptopurine for induction of remission in ulcerative colitis.
| Methotrexate compared to 6‐Mercaptopurine for induction of remission in ulcerative colitis | ||||||
| Patient or population: patients with induction of remission in ulcerative colitis Settings: Outpatient Intervention: Methotrexate Comparison: 6‐Mercaptopurine | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| 6‐Mercaptopurine | Methotrexate | |||||
| Proportion of patients achieved clinical remission Follow‐up: mean 30 weeks | 786 per 10001 | 581 per 1000 (338 to 1000) | RR 0.74 (0.43 to 1.29) | 26 (1 study) | ⊕⊝⊝⊝ very low2,3 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Control group risk comes from control arm of study 2 Details regarding randomization, allocation concealment, and blinding were not described in the study 3 Very sparse data (18 events)
Summary of findings 3. Methotrexate compared to 5‐aminosalicylic acid (5‐ASA) for induction of remission in ulcerative colitis.
| Methotrexate compared to 5‐ASA for induction of remission in ulcerative colitis | ||||||
| Patient or population: patients with induction of remission in ulcerative colitis Settings: Outpatient Intervention: Methotrexate Comparison: 5‐ASA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| 5‐ASA | Methotrexate | |||||
| Proportion of patients achieved clinical remission Follow‐up: mean 30 weeks | 250 per 1000 | 582 per 1000 (165 to 910) | RR 2.33 (0.66 to 3.64) | 20 (1 study) | ⊕⊝⊝⊝ very low1,2 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Details of randomization, allocation concealment, and blinding were not described in the study 2 Very sparse data (9 events)
Background
Ulcerative colitis is a chronic inflammatory bowel disease characterized by abdominal cramping, fecal urgency and bloody diarrhea. The most commonly used therapies for patients with ulcerative colitis are 5‐aminosalicylates and corticosteroids. However, many patients require immunosuppressive agents when their disease becomes steroid‐refractory or dependent. Azathioprine, while modestly effective at maintaining remission in patients with quiescent ulcerative colitis (Hawthorne 1992; Jewell 1974; Timmer 2012), has shown mixed results when studied for remission induction in active disease (Ardizzone 2006; Jewell 1974). Cyclosporine may be effective in treating patients with severe disease, but with potentially significant toxicity (Shibolet 2005). More recently, infliximab has been proven to be beneficial for inducing and maintaining remission in patients who have failed other therapies (Lawson 2006; Rutgeerts 2005). However, despite these treatment advances, a proportion of ulcerative colitis patients still require colectomy for refractory disease (Bach 2006), and the identification of other effective therapies is an important area of research.
Methotrexate, a dihydrofolate reductase inhibitor, has been shown to be effective for both induction and maintenance of remission in patients with Crohn's disease (Feagan 1995; Feagan 2000; McDonald 2012; Patel 2014). Although ulcerative colitis shares some clinical and pathological features with Crohn's disease, and some treatments are similar, therapies effective for one type of inflammatory bowel disease are not necessarily effective for the other, and data regarding efficacy of interventions cannot be extrapolated from studies of one disease to the other. This systematic review is an update of a previously published Cochrane review (Chande 2007).
Objectives
To assess the efficacy and safety of methotrexate for induction of remission in patients with ulcerative colitis.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials comparing methotrexate with placebo or an active comparator were considered for inclusion. For future updates, studies published as abstracts only will be included if the authors can be contacted for further information.
Types of participants
Adult patients with active ulcerative colitis defined by a combination of clinical, radiographic, endoscopic and histological criteria were included.
Types of interventions
Methotrexate given by any route.
Types of outcome measures
The primary outcome measure was the number of patients achieving clinical remission and complete withdrawal from steroids as defined by the studies and expressed as a percentage of the number of patients randomized (intention to treat analysis). Secondary outcomes measures included: a) Endoscopic remission as defined by the authors; b) Clinical, histological or endoscopic improvement as defined by the authors; c) The occurrence of adverse events; and d) Improvements in quality of life as measured by a validated instrument.
Search methods for identification of studies
See: Inflammatory Bowel Disease and Functional Bowel Disorders Group search strategy.
MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials, and the Cochrane IBD/FBD group specialized trials register were searched from inception to June 26, 2014 to identify relevant publications. The search strategies are reported in Appendix 1. Review papers on ulcerative colitis, and references from identified papers were also searched in an effort to identify additional studies. Abstracts from major gastroenterological meetings were searched to identify research published in abstract form only.
Data collection and analysis
Study selection Two authors (YW and JKM) independently reviewed the studies identified by the literature search to determine eligibility for inclusion based on the criteria identified above. Studies published in abstract form only were to be included only if the authors could be contacted for further information.
Data collection A data extraction form was developed and used to extract data from included studies. Two authors (YW, JKM) independently extracted data. Any disagreements were resolved by consensus.
Statistical analysis Data were analyzed using Review Manager (RevMan 5.3.3). Data were analyzed on an intention‐to‐treat basis, and treated dichotomously. In the future if any cross‐over studies are identified, only data from the first arm will be included. The primary endpoint was induction of remission, as defined by the studies. Data were to be combined for analysis if they assessed the same treatments (methotrexate versus placebo or other therapy). If a comparison was only assessed in a single trial, the risk ratio (RR) and corresponding 95% confidence interval (95% CI) were calculated and P‐values were derived using the Chi2 test. If the comparison is assessed in more than one trial, summary test statistics were to be derived using the pooled RR and corresponding 95% CI. The presence of heterogeneity among studies was to be assessed using the Chi2 test (a P value of 0.10 was to be regarded as statistically significant). If statistically significant heterogeneity was identified the RR and 95% CI were to be calculated using a random‐effects model.
Quality assessment The methodological quality of the included studies was evaluated using the Cochrane risk of bias tool (Higgins 2011). This tool involves rating trials as high, low or unclear risk for each of the following criteria:
Randomization sequence generation;
Allocation concealment;
Blinding;
Missing data and attrition;
Outcome reporting; and
Other sources of bias.
The overall quality of the evidence was evaluated using the GRADE approach (Guyatt 2008; Schünemann 2011). Outcome data are rated as being of high, moderate, low or very low quality evidence. Data from randomized controlled trials begin as high quality but can be downgraded based on the following criteria:
Risk of bias in the included trials;
Indirect evidence;
Inconsistent findings (including unexplained heterogeneity);
Imprecision (i.e. sparse data or wide confidence interval or both); and
Reporting bias.
The different quality ratings are interpreted as the likelihood that future research would affect the estimate of effect. An estimate of effect based on high quality evidence is unlikely to change with further research. If the overall evidence is of moderate quality further research may have an impact on our confidence in the estimate and may change the estimate. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate when the evidence is rated as low quality. Very low quality research means that we are very uncertain about the finding (Guyatt 2008; Schünemann 2011).
Results
Description of studies
A literature search conducted on June 26, 2014 identified 2776 records. After duplicates were removed, a total of 2481 records remained for review of titles and abstracts. Two authors (YW and JKM) independently reviewed the titles and abstracts of these trials and 30 records were selected for full text review (see Figure 1). Twenty‐eight reports of 24 studies were excluded (See: Characteristics of excluded studies). Egan 1999a was a randomized study but was excluded because there was no placebo or active comparator group. The study compared two doses of subcutaneous methotrexate (15 mg/week versus 25 mg/week). Twenty‐three studies were excluded because they were not randomized controlled trials (Baron 1993; Cummings 2005; Dejica 1998; Egan 1999b; Egan 2000; Fraser 2002; Fraser 2003; Gibson 2006; González‐Lama 2012; Hayes 2014; Herrlinger 2005; Houben 1994; Khan 2013; Kozarek 1989; Kozarek 1992; Mañosa 2011; Paoluzi 2002; Richter 2012; Saibeni 2012; Siveke 2003; Soon 2004; Te 2000; Wahed 2009; see characteristics of excluded studies table and Additional Table 4 ‐ Results from excluded studies). Two studies (total of 101 patients) met the pre‐defined inclusion criteria and were included in the review (Maté‐Jiménez 2000; Oren 1996). The two included studies were sufficiently heterogeneic in terms of comparators, treatment duration, and study design that it was not valid to pool the data. The GRADE analyses were performed on individual studies for each outcome.
1.
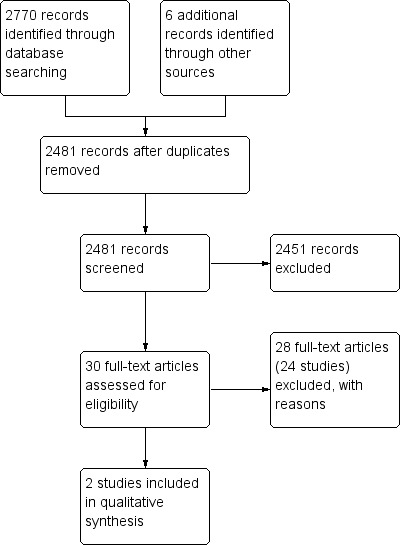
Study flow diagram.
1. Results from excluded studies.
| Study ID | Description | Results |
| Baron 1993 | Open label clinical trial enrolling patients with steroid dependent or steroid refractory IBD (Crohn's n = 10, UC n = 8) Patients received oral methotrexate 15 mg/wk and prednisone The primary outcomes were complete or partial withdrawal from steroids and mean steroid use |
UC patients: mean prednisone dose dropped from 26.3 +/‐ 3.2 mg/day to 12.7 +/‐ 2.0 mg/day (P < 0.001) Three patients had a partial response Adverse events were mild |
| Cummings 2005 | Retrospective chart review at two hospitals Steroid dependent or steroid refractory UC patients (n=50) were treated with oral methotrexate (mean dose 19.9 mg/wk for a median of 30 weeks) The primary outcome was remission defined as lack of treatment with steroids for 3 months or more Secondary outcomes: response defined as good, partial or nil, and proportionate reduction of steroids |
Remission occurred in 42% of patients The response was good in 54% and partial in 18% Adverse events occurred in 23%; 10% stopped treatment due to adverse events |
| Dejica 1998 | Unrandomized, open label, preliminary trial enrolled twenty‐two patients with chronic active ulcerative colitis, refractory to steroids or sulfasalazine or both for at least 3 months The patients were treated with 25 mg weekly intramuscular injection for 20 weeks The primary outcome was clinical remission with Mayo Clinic Socre ≤ 3, including endoscopy |
Clinical remission were obtained in 50% of patients (n=11) Fifteen of 22 patients (68%) had significant clinical improvement in Mayo Clinic score Five patients developed side effects, but the drug‐related adverse effects were not severe enough to warrant discontinuation of therapy |
| Egan 1999a | Randomized, single‐blind trial comparing two doses of subcutaneous methotrexate (15 mg/wk, n=18, versus 25 mg/wk, n=14) in patients with steroid dependent or refractory IBD The primary outcome was remission at 16 weeks defined as the presence of quiescent disease (IBDQ score > or = 170) and discontinuation of prednisone The secondary outcome was partial response defined as ability to discontinue prednisone without a decrease in IBDQ or a clinically significant improvement in disease activity. |
After 16 weeks 17% (3/18) of patients in the 15 mg group achieved remission compared to 17% (2/12) of patients in the 25 mg group (P = N.S.) Improvement occurred in 39% (7/18) of the 15 mg group compared to 33% (4/12) of the 25 mg group (P = N.S.) Adverse events occurred in 11% (2/18) of patients in the 15 mg group compared to 17% (2/12) of patients in the 25 mg group (P = N.S.) |
| Egan 1999b | Adenosine was thought to play a major role in anti‐inflammatory mechanism of action of methotrexate in animal models The non‐randomized, open‐label pharmacokinetic study investigating the effects of methotrexate on adenosine concentrations in plasma and at the site of the disease in patients with inflammatory bowel disease In 10 patients with Crohn's disease or ulcerative colitis, rectal adenosine and plasma adenosine concentrations were measured before and immediately after a subcutaneous injection of methotrexate at 15 or 25 mg |
There were no significant differences between pre‐injection and post‐injection values in both plasma and rectal adenosine concentrations The mean pre‐dose and post‐dose mean rectal adenosine concentrations were 2.4 µmol/L and 2.1 µmol/L, respectively (P = 0.17) The mean pre‐dose and post ‐dose plasma adenosine concentrations were 3.4 µmol/L and 3.4 µmol/L, respectively (P = 0.95) Therefore, the evidence does not support adenosine as the anti‐inflammatory mediator of methotrexate |
| Egan 2000 | Case series Three patients with steroid refractory UC and 2 patients with steroid refractory Crohn's disease who failed monotherapy with subcutaneous methotrexate 25 mg/week for 16 weeks were treated with the combination of methotrexate and low‐dose oral cyclosporine (3 mg/kg/day) for an additional 16 weeks The primary outcome was remission at 16 weeks defined as the presence of quiescent disease (IBDQ score > or = 170) and discontinuation of prednisone The secondary outcome was partial response defined as ability to discontinue prednisone without a decrease in IBDQ or a clinically significant improvement in disease activity |
The three patients with UC experienced clinical improvement with a mean increase in IBDQ score from 164 to 190 points (P = 0.01) One patient developed hypertension |
| Fraser 2002 | Retrospective chart review at two hospitals Seventy patients were reviewed (Crohn's n = 48, UC n = 22) Patients were treated with oral methotrexate (n = 62) or intramuscular methotrexate (n=8) at a mean dose of 20 mg/week for a mean duration of 17.1 months Remission was defined as the lack of a need for oral steroids (either prednisolone or budesonide) for at least 3 months Patients who were well on low doses of prednisolone or budesonide steroids were recorded as ‘remission not achieved’ The continued use of oral 5‐aminosalicylic acid compounds and steroids or 5‐aminosalicylic acid enemas was allowed within the definition of remission Relapse was defined as the need for re‐introduction of steroids, the need for a surgical procedure or the use of infliximab |
Remission was achieved in 34 of 55 (62%) of patients who completed more than 3 months of treatment Life‐table analysis showed that the chances of remaining in remission at 12, 24 and 36 months, if treatment was continued, were 90%, 73% and 51% respectively The chances of remaining in remission after stopping treatment at 6, 12 and 18 months were 42%, 21% and 16% respectively |
| Fraser 2003 | Open label clinical trial Eight patients with chronically active moderate to severe UC refractory to corticosteroids and azathioprine or 6‐mercaptopurine were treated with intramuscular methotrexate 25 mg/week (and folic acid) for 16 weeks Efficacy was assessed with the Mayo clinic score |
Six of eight patients completed 16 weeks of treatment One patient withdrew due to severe exacerbation and one withdrew due to failure to improve Two patients developed anemia and one patient developed hypertransaminasemia The median Mayo clinic score at 16 weeks was 8 (range 6 to 11) Two patients were referred for colectomy at the end of the study |
| Gibson 2006 | Retrospective chart review at a single IBD clinic including 65 patients (Crohn's n=45, UC n=20) The initial weekly dose was 25 mg in 29 patients, 20 mg in 16 patients, 15 mg in 7 patients or 10 mg in 3 Eighty‐four percent received methotrexate by subcutaneous injection All patients received folate supplementation Response was defined as improvement in bowel symptoms or ability to reduce the dose of steroids Remission was defined as improvement in symptoms with no requirement for steroids for 3 months, or ability to wean off steroids |
Remission was achieved by 12 of 19 (63%) patients with UC ‐ an additional patient with UC had a response to treatment The median duration of treatment was 11 months (range 3 to 36) in responders and 6 months (range 1.5 to 10) in non‐responders Fifteen per cent of patients experienced adverse events |
| González‐Lama 2012 | Retrospective chart review of IBD patients treated with methotrexate in eight hospitals in Madrid, Spain Seventy‐seven patients were included (Crohn's disease n = 62, ulcerative colitis n = 15) Methotrexate was initiated at a mean dose of 21 mg/week (range: 15‐30), using parenteral administration in 67% of cases and oral route in 33% of patients Partial response was defined as a decrease in the Harvey‐Bradshaw index of more than three points Remission was defined as a Harvey‐Bradshaw index without steroid treatment below or equal to four |
Fourteen out of 15 UC patients received parenteral methotrexate Two patients achieved clinical remission with induction therapy, and 12 (71%) patients gained some response and started maintenance treatment Among the twelve patients, five required dose modification during the follow‐up, three showed loss of response after a mean of 28 weeks, and three more patients achieved clinical remission Adverse events led to methotrexate withdrawal in 5% (4/77) of patients |
| Hayes 2014 | Retrospective chart review of UC patients treated with infliximab (IFX) at a regional referral center Eighty‐five patients with UC were included in the analysis Duration of efficacious IFX therapy, and serum IFX and antibody‐to‐IFX (ATI) levels were compared between patients, who received IFX as monotherapy (n = 39) and in combination with an immunosuppressant (n = 46) Immunosuppressants included azathioprine (65.2% of combination group), mercaptopurine (28.3%), and methotrexate (6.5%) |
Concomitant immunosuppressant use was associated with increased duration of IFX therapy (90% in combination group vs. 61% of patients in monotherapy group at 1 year, P = 0.016); greater IFX levels (20.4 mg/L vs. 10.5 mg/L, P = 0.025); and less frequent ATI formation (4.5% vs. 33.3%, P = 0.031) |
| Herrlinger 2005 | Case control study of pharmacogenetics of Mtx therapy in IBD Allele frequencies were assessed in 102 IBD patients treated with methotrexate, 202 patients with Crohn's disease, 205 patients with UC and 189 healthy volunteers All subjects were genotyped for four polymorphisms |
No significant difference in allele frequencies were detected between Crohn's disease, UC and healthy volunteers Twenty‐one per cent of methotrexate treated patients experienced adverse events |
| Houben 1994 | Case series of 15 IBD patients (Crohn's disease n=13, UC n=2) treated with intramuscular methotrexate 25 mg/week for 12 weeks, followed by a tapering oral dose One patient was treated twice Disease activity was determined after 1, 2 and 3 months of treatment |
The mean defecation frequency went down from 7 to 2 times daily after 12 weeks and prednisone dose could be lowered from 22 mg to 15 mg after 3 months Subjective and objective improvement was noted in 12/15 patients No serious adverse events were reported |
| Khan 2013 | Retrospective cohort study using the nationwide Veterans Affairs database to describe the efficacy of methotrexate in achieving steroid‐free remission Ninety‐one patients with UC were included and they were followed for 15 months after methotrexate initiation by tracking prednisone, methotrexate, thiopurines, and infliximab dispensing records Endpoints were: 1) successful remission (cessation of prednisone filling activity while continuing methotrexate); 2) failure with continuance, failure to be weaned off steroids while continuing methotrexate; 3) failure with discontinuance, cessation of methotrexate while continuing steroids |
The average weekly prescription dose for oral and parenteral methotrexate was 14 mg/week (range: 2.3‐31.25) and 25 mg/week (range: 5.8‐70), respectively The mean daily prescription dose for oral prednisone within the oral methotrexate group was 12 mg/day (range 0.7‐68 mg/day) and 25 mg/day (range: 5‐113 mg/day) in the parenteral methotrexate group At the twelfth month, 37% of patients on oral methotrexate and 30% of patients on parenteral methotrexate were able to discontinue steroids |
| Kozarek 1989 | Open label clinical trial including 21 patients with refractory IBD (Crohn's n=14, UC n=7) Patients received intramuscular methotrexate 25 mg/week for 12 weeks After 12 weeks, patients were switched to a tapering oral dose if clinical and objective improvement was noted |
Five of 7 UC patients had an objective response as measured by the Ulcerative Colitis Activity Index (13.3 to 6.3, P=0.007) Prednisone dosage decreased from 38.6 mg +/‐ 6.35 (SEM) to 12.9 mg +/‐ 3.4, P=0.01 Five of 7 had histological improvement. None of the UC patients had normal flexible sigmoidoscopy results. Adverse events included mild rises in transaminase levels in 2 patients, transient leukopenia in 1, self‐limited diarrhea and nausea in 2 patients, brittle nails (1 case) and atypical pneumonitis (1 case). |
| Kozarek 1992 | Retrospective chart review, over a 4 year period (1987 to 1991) 86 patients with refractory IBD (Crohn's n=37, UC n=30) were started on 25 mg/week parenteral methotrexate Those patients who responded clinically at 12 weeks were offered weekly oral methotrexate therapy (7.5 to 15 mg) Outcomes included the DAI (scored 0 to 15), prednisone dose, and Mtx toxicity |
Seventy per cent of UC patients had a symptomatic and objective response At a mean follow‐up of 59 weeks, only 40% of UC patients continued to respond to Mtx (DAI 5.0 +/‐ 0.9; prednisone 12 +/‐ 3.9 mg), 15 of 30 UC patients required colectomy and one patient stopped methotrexate due to hypersensitivity pneumonitis |
| Mañosa 2011 | Retrospective chart review to evaluate the efficacy and safety of methotrexate in UC patients Patients were included in the study if they received methotrexate for steroid dependency or steroid refractoriness and for maintenance of remission Forty patients were identified from databases of 8 Spanish IBD referral hospitals and followed for at least 6 months Therapeutic success was defined as the absence of UC‐related symptoms, complete steroid withdrawal and no‐requirement of rescue therapies within the first 6 months after starting methotrexate |
At 6 months, 45% (18/40) achieved therapeutic success Treatment failure were mainly due to inefficacy (11/22, 50%) or intolerance (8/22, 36%) After a median follow‐up of 28 months. 38% (7) of patients with initial therapeutic success required new steroid courses, 22% (4) started biological therapy and 1 of them required colectomy The cumulative probability of maintaining steroid‐free clinical remission was 60%, 48%, and 35% at 6, 12, 24 months after starting methotrexate, respectively In all, 11 out of 40 patients (27.5%) experienced adverse effects, leading to methotrexate discontinuation in 8 patients |
| Paoluzi 2002 | Open label clinical trial including 42 patients with steroid dependent or steroid resistant active UC Patients were treated with a daily dose of azathioprine (2 mg/kg) and, if intolerant or not responding, with intramuscular methotrexate (12.5 mg/week) Efficacy was assessed by clinical, endoscopic and histological examinations at 6 months Patients achieving clinical remission continued with treatment and were followed up Ten patients received methotrexate The achievement of complete remission with the ability to discontinue oral steroids was defined as the primary outcome Response to treatment was defined as follows: complete remission equals achievement of clinical, endoscopic and histological remission; improvement equals disappearance of symptoms (clinical remission) with endoscopic and histological improvement of inflammatory changes; failure equals worsening, no benefit or clinical improvement with the persistence of unmodified inflammatory changes of the mucosa |
Methotrexate induced complete remission in six patients (60%) and improvement in four (40%) During follow‐up, a larger number of patients on azathioprine relapsed in comparison with patients on methotrexate [16/28 (57%) vs. 2/10 (20%), respectively; P < 0.05] |
| Richter 2012 | Retrospective study using a large U.S. health insurance database to document treatment of new‐onset ulcerative colitis (UC) and ulcerative proctitis (UP) in routine clinical practice One thousand five hundred and sixteen UC patients and 636 UP patients were included in the analysis New‐onset UC or UP were identified based on: 1) initial receipt of an oral 5‐ASA, mesalazine suppository, 5‐ASA enema, steroid, antimetabolite, budesonide or TNF inhibitor; 2) sigmoidoscopy/colonoscopy in prior 30 days resulting in a new diagnosis of UC or UP and 3) no prior encounters for Crohn's disease |
In UC, initial therapies most frequently used were oral 5‐ASAs (53%), oral 5‐ASAs and systemic steroids (12%), systemic steroids (8%) and mesalazine suppositories (6%); in UP, mesalazine suppositories (42%) and oral 5‐ASAs (19%), combination therapy (14%), mesalazine enema (11%) and rectal steroids (10%) were the mostly frequently used therapies Few patients received maintenance therapy, and there was a limited use of antimetabolites (0.3% in UC, and lower in UP ‐ no specific figures were provided) and biological agents (0.1% in UC) |
| Saibeni 2012 | Retrospective, observational study using 5420 case histories from 8 referral centres in Italy, to evaluate frequency, indications, efficacy and safety of methotrexate in IBD patients One hundred and twelve patients received methotrexate (2.1%, 89 Crohn's disease, 23 ulcerative colitis) |
Indications: first‐line immunosuppressant in 32 (28.6%), alternative (second‐line) to thiopurines in 80 (71.4%) Efficacy: optimal in 39/112 (34.8%), partial in 29/112 (25.9%), absent in 22/112 (19.6%), not assessable in 22/122 (19.6%) Side effects happened in 49/112 patients (43.7%, 39 Crohn's disease, 10 ulcerative colitis), leading to drug discontinuation in 38 patients (33.9%) Folic acid use was related to the lower side effects (35/93, 37.6% in those who received folic acid vs. 14/19, 73.7% in those who did not) |
| Siveke 2003 | Case series of 3 patients with steroid dependent or steroid resistant UC Patients were treated with intramuscular methotrexate 25 mg/week These patients received 10 mg of folate orally on the day after injection An additional patient received 15 mg of methotrexate, with the dose being adjusted to 25 mg following increased activity of colitis |
Three of 4 patients achieved remission One patient had to discontinue methotrexate due to an increase in aspartate aminotransferase and alanine aminotransferase levels despite dose reduction and prophylactic supplementation of folate |
| Soon 2004 | Retrospective chart review including 72 patients (Crohn's n=66, UC n=6) Patients were treated with mean dose of 18.2 mg/week of methotrexate for six months Methotrexate was given orally in 64 patients and intramuscularly in eight patients Clinical response was defined as sustained withdrawal of oral steroids within 3 months of starting treatment and sustained for a further 3 months or fistula improvement New episodes of steroid therapy, infliximab or surgery during the first 6 months were considered as failure to achieve clinical response |
Fifty‐four patients completed six months of treatment Clinical response was achieved in 22 (40.7%) patients [19 of 48 (39.6%) with CD and three of six (50%) with UC] |
| Te 2000 | Retrospective chart review looking at hepatotoxicity among IBD patients who had received a minimum cumulative dose of 1500 mg of methotrexate | In 20 patients who had liver biopsies, the mean cumulative methotrexate dose was 2633 mg (range, 1500–5410 mg), given for a mean of 131.7 wk (range, 66–281 weeks) Nineteen of 20 patients (95%) had mild histological abnormalities (Roenigk’s grade I and II), and one patient had hepatic fibrosis (Roenigk’s grade IIIB) |
| Wahed 2009 | Retrospective chart review to examine the efficacy and safety profile of methotrexate in patients with CD or UC who were either intolerant or non‐responsive to azathioprine/mercaptopurine (AZA/MP) One hundred and thirty‐one patients with IBD treated with MTX were included (99 CD, 32 UC) Clinical response was assessed at 6 months and it was defined as steroid withdrawal, normalization of previously raised CRP or physician's clinical assessment of improvements |
In CD, clinical response occurred in 18/29 patients (62%) refractory to AZA/MP and 42/70 patients (60%) intolerant to AZA/MP (P = 1.0) In UC, clinical response occurred in 7/9 patients (78%) refractory to AZA/MP and 15/23 (65%) intolerant to AZA/MP Side effects were seen in 23 (17.4%) patients and led to discontinuation in 11 (8.3%) patients |
Methotrexate versus placebo
Oren 1996 This trial included 67 patients (35 male, 32 female) with chronic active steroid‐dependent ulcerative colitis (defined by typical clinical, radiographic, endoscopic, and pathological criteria). Disease chronicity was defined by the requirement of steroid therapy (minimum 7.5 mg/day) for 4 months of the preceding 12 months. Current use of mesalamine or steroids was permitted. Steroid therapy was to be tapered and discontinued within 2 to 3 months of study entry, but could be restarted or the dose increased as clinically indicated. No immunosuppressive agents could be used in the three months prior to entry . Active disease was defined by a Mayo clinic score of > 7 at study entry. The patients were randomized to oral methotrexate 12.5 mg/week (n = 30) or identical placebo (n = 37) for 9 months. The patients were seen at regular intervals during the nine months. At each visit, the Mayo clinic score was calculated, and a sigmoidoscopy was also performed every three months. The primary outcomes were the proportion of patients who achieved their first remission as well as the maintenance of remission in those patients. The definition of remission was a Mayo clinic score of < 3 (or < 2 without sigmoidoscopy results), and complete withdrawal from steroid therapy.
Methotrexate versus active comparators
Maté‐Jiménez 2000 This study enrolled 34 patients with ulcerative colitis (and 38 patients with Crohn's disease). All patients had steroid‐dependent disease (Mayo clinic score of > 7 despite prednisone > 20 mg/day), but all other therapies were stopped at least 6 months before study entry. The patients were randomized in a 2:2:1 ratio to 6‐mercaptopurine 1.5 mg/kg/day (n = 14), methotrexate 15 mg weekly (n = 12), or 5‐aminosalicylic acid 3 g/day (n = 8) for 30 weeks. There was no placebo comparator. All medications were given orally, and prednisone was tapered by 8 mg/week if clinically appropriate. If remission was achieved the methotrexate dose was reduced to 10 mg/week and the 6‐mercaptopurine dose to 1 mg/kg/day. Patients in the 5‐aminosalicylic acid group who achieved remission continued to receive the same dose (3 g/day) as maintenance therapy. Follow‐up occurred regularly over the study period, and the Mayo clinic score was calculated at weeks 12 and 30. Patients in remission and off steroids at the end of 30 weeks then entered a 76 week maintenance phase. The primary outcome measure was the proportion of patients in remission at 30 weeks, defined by a Mayo clinic score of < 3 and withdrawal from steroid therapy.
Risk of bias in included studies
The risk of bias results are summarized in Figure 2. Oren 1996 used adequate methods of randomization, blinding, and allocation concealment and was rated as low risk of bias for these items. Maté‐Jiménez 2000 was an open‐label study and was rated as high risk of bias for blinding. Moreover, Maté‐Jiménez 2000 did not report the methods used for randomization and allocation concealment and these items were rated as unclear risk of bias. Both of the included trials were rated as low risk of bias for incomplete outcome data (Maté‐Jiménez 2000; Oren 1996). No other issues were found with the trials and they were rated as low risk of bias for the other bias item (Maté‐Jiménez 2000; Oren 1996).
2.
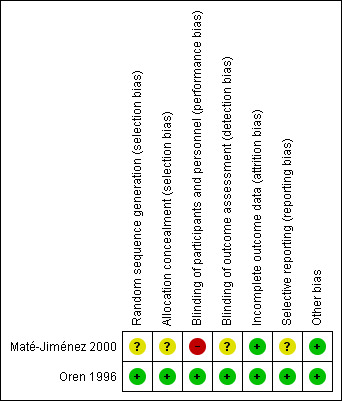
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
See: Table 1; Table 2; Table 3
Methotrexate versus placebo One study (N = 67) compared methotrexate to placebo (Oren 1996). There was no statistically significant difference in clinical remission rates between methotrexate and placebo patients. Forty‐seven per cent (14/30) of methotrexate patients achieved clinical remission and complete withdrawal from steroids during the study period compared to 49% (18/37) of placebo patients (RR 0.96, 95% CI 0.58 to 1.59; See Figure 3). A GRADE analysis indicated that the overall quality of the evidence supporting this outcome was low due to very sparse data (32 events; See Table 1). The mean time to remission was 4.1 months in the methotrexate group compared to 3.4 months in the placebo group. There was no statistically significant difference in withdrawals due to adverse events (RR 2.47, 95% CI 0.23 to 25.91). Two patients (7%) were withdrawn from the methotrexate group due to adverse events (leucopenia, migraine) compared to one patient (3%) from the placebo group (rash). The Oren 1996 study did not report on any of the other secondary outcomes including endoscopic remission, clinical, histological or endoscopic improvement or improvements in quality of life.
3.
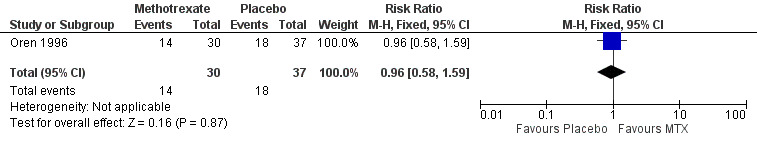
Forest plot of comparison: 1 Methotrexate versus placebo, outcome: 1.1 Remission and complete withdrawal from steroids.
Methotrexate versus active comparators One study (N = 34) compared methotrexate to 6‐mercaptopurine and 5‐aminosalicylic acid (Maté‐Jiménez 2000). There were no statistically significant differences in the proportion of patients who achieved clinical remission and withdrawal from steroids. At 30 weeks 58% (7/12) of methotrexate patients achieved clinical remission and withdrawal from steroids compared to 79% (11/14) of 6‐mercaptopurine patients (RR 0.74, 95% CI 0.43 to 1.29; See Figure 4). Twenty‐five per cent (2/8) of 5‐aminosalicylic acid patients achieved remission and withdrawal of steroids after completing 30 weeks of induction treatment compared to 58% (7/12) of methotrexate patients (RR 2.33, 95% CI 0.64 to 8.49; See Figure 5). GRADE analyses indicated that the overall quality of the evidence was very low due to very sparse data and high risk of bias (see Table 2; Table 3). Adverse events experienced by methotrexate patients included nausea and dyspepsia, mild alopecia, mild increase in aspartate aminotransferase levels, peritoneal abscess, hypoalbuminemia, severe rash and atypical pneumonia. Three of 26 patients treated with methotrexate withdrew due to adverse events compared to 4 of 30 patients treated with 6‐mercaptopurine.
4.
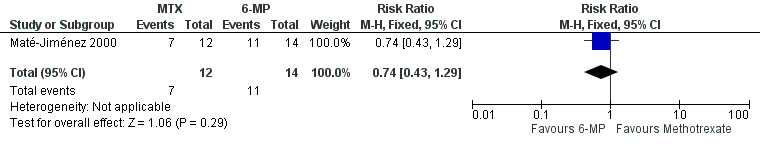
Forest plot of comparison: 2 Methotrexate versus 6‐Mercaptopurine, outcome: 2.1 Proportion of patients achieved clinical remission.
5.
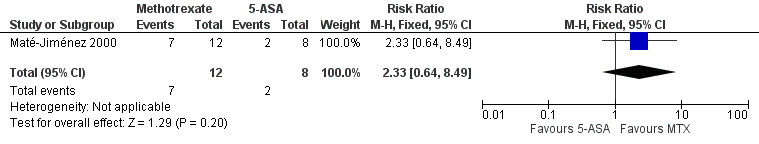
Forest plot of comparison: 3 Methotrexate versus 5‐ASA, outcome: 3.1 Proportion of patients achieved clinical remission.
Discussion
The treatment of patients with ulcerative colitis often involves 5‐aminosalicylic acid and corticosteroids. However, some patients require immunosuppressive therapy when their disease becomes dependent on or refractory to steroid therapy. Unfortunately, there are a limited number of therapeutic options for these patients. Azathioprine has traditionally been the next choice of therapy for these patients, and although it may be effective for maintenance of remission (Timmer 2012), it does not appear to provide any benefit for induction of remission in these patients (Hawthorne 1992; Jewell 1974; Ardizzone 2006). Infliximab has recently been shown to be effective for induction of remission in patients with active ulcerative colitis who have failed steroid therapy (Lawson 2006; Rutgeerts 2005). Cyclosporine may be effective for treating some patients with severe disease (Shibolet 2005). Failing these medications, surgery is usually considered the next therapeutic option for these patients.
Methotrexate has been shown to be effective for both induction of remission (at a dose of 25 mg intramuscular weekly) and maintenance of remission (15 mg intramuscular weekly) in patients with Crohn's disease (Feagan 1995; Feagan 2000; McDonald 2012; Patel 2014). There has only been one well‐designed, placebo‐controlled, randomized trial assessing methotrexate for induction of remission in ulcerative colitis.
Oren 1996 was designed to assess the utility of methotrexate for induction of remission in patients with active steroid‐dependent ulcerative colitis. In this study, no benefit for methotrexate over placebo was found. The dose of methotrexate used (12.5 mg orally weekly) was lower than the dose used in the trial assessing methotrexate for induction of remission in Crohn's disease (Feagan 1995), and was administered orally rather than parenterally. The low dose oral regimen utilized by Oren 1996 is effective in patients with rheumatoid arthritis (Lopez‐Olivo 2014). Since methotrexate is absorbed in the small bowel, oral administration should be appropriate in ulcerative colitis. A parenteral route is preferred in Crohn's disease, where drug absorption may be affected by disease activity. However, whether or not a higher dose or parenteral administration of methotrexate in ulcerative colitis patients would be more effective is unknown.
One other small (N =34), poor quality randomized trial assessing methotrexate, 6‐mercaptopurine and 5‐aminosalicylic acid in ulcerative colitis has been published (Maté‐Jiménez 2000). No statistically significant differences in clinical remission rates were found. The results for efficacy outcomes between methotrexate and 6‐mercaptopurine and methotrexate and 5‐aminosalicylic acid were uncertain as GRADE analyses rated the overall quality of evidence from this study as very low. Thus no firm conclusions can be drawn from this study.
Authors' conclusions
Implications for practice.
Although methotrexate was well‐tolerated, the studies showed no benefit for methotrexate over placebo or active comparators. The results for efficacy outcomes between methotrexate and placebo, methotrexate and 6‐mercaptopurine and methotrexate and 5‐aminosalicylic acid were uncertain. Whether a higher dose or parenteral administration would be effective is unknown. At present there is no evidence supporting the use of methotrexate for induction of remission in active ulcerative colitis.
Implications for research.
There are a limited number of therapeutic options for treating patients with ulcerative colitis. Methotrexate has been shown to be effective in both remission induction and maintenance in Crohn's disease (Feagan 1995; Feagan 2000;McDonald 2012; Patel 2014). The randomized, controlled trials of methotrexate in ulcerative colitis used a lower dose and different route of administration than that used in Crohn's disease patients, and no significant benefits were found. Another study with similar dosing to that used in Crohn's patients is warranted, and should definitively determine whether or not methotrexate is effective for remission induction in ulcerative colitis. Such a trial could be coupled with a study to determine whether the drug is effective for maintenance of remission. MERIT‐UC and METEOR are two large, ongoing multi‐center, placebo‐controlled clinical trials evaluating the efficacy and safety of methotrexate for induction and maintenance of remission in ulcerative colitis (NCT00498589; NCT01393405).
What's new
| Date | Event | Description |
|---|---|---|
| 3 October 2014 | Amended | Revised plain language summary |
History
Protocol first published: Issue 3, 2007 Review first published: Issue 4, 2007
| Date | Event | Description |
|---|---|---|
| 19 August 2014 | New search has been performed | New literature search conducted on June 26, 2014 |
| 19 August 2014 | New citation required and conclusions have changed | Updated review with one new author. One new study added |
Acknowledgements
Funding for the IBD/FBD Review Group (September 1, 2010 ‐ August 31, 2015) has been provided by the Canadian Institutes of Health Research (CIHR) Knowledge Translation Branch (CON ‐ 105529) and the CIHR Institutes of Nutrition, Metabolism and Diabetes (INMD); and Infection and Immunity (III) and the Ontario Ministry of Health and Long Term Care (HLTC3968FL‐2010‐2235).
Miss Ila Stewart has provided support for the IBD/FBD Review Group through the Olive Stewart Fund.
Appendices
Appendix 1. Search strategies
MEDLINE search strategy
1. ulcerative colitis.mp. or exp ulcerative colitis/
2. (proctocolitis or proctosigmoiditis or rectocolitis or rectosigmoiditis or proctitis).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
3. 1 or 2
4. methotrexate.mp. or exp methotrexate derivative/ or exp methotrexate/ or exp methotrexate gamma aspartic acid/ or exp methotrexate polyglutamate/
5. 3 and 4
EMBASE search strategy
1. ulcerative colitis.mp. or exp ulcerative colitis/
2. (proctocolitis or proctosigmoiditis or rectocolitis or rectosigmoiditis or proctitis).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
3. 1 or 2
4. methotrexate.mp. or exp methotrexate derivative/ or exp methotrexate/ or exp methotrexate gamma aspartic acid/ or exp methotrexate polyglutamate/
5. 3 and 4
CENTRAL search strategy
1. ulcerative colitis
2. methotrexate
3. 1 and 2
SR‐IBD
colitis AND methotrexate
Data and analyses
Comparison 1. Methotrexate versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission and complete withdrawal from steroids | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.58, 1.59] |
| 2 Withdrawal due adverse events | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.47 [0.23, 25.91] |
1.1. Analysis.
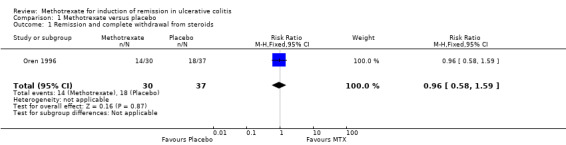
Comparison 1 Methotrexate versus placebo, Outcome 1 Remission and complete withdrawal from steroids.
1.2. Analysis.
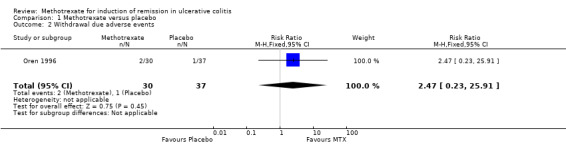
Comparison 1 Methotrexate versus placebo, Outcome 2 Withdrawal due adverse events.
Comparison 2. Methotrexate versus 6‐Mercaptopurine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion of patients achieved clinical remission | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.43, 1.29] |
2.1. Analysis.
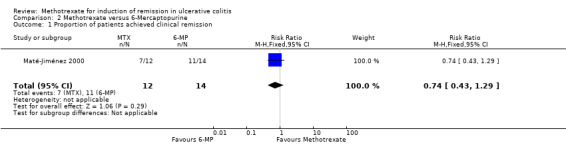
Comparison 2 Methotrexate versus 6‐Mercaptopurine, Outcome 1 Proportion of patients achieved clinical remission.
Comparison 3. Methotrexate versus 5‐ASA.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion of patients achieved clinical remission | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.33 [0.64, 8.49] |
3.1. Analysis.
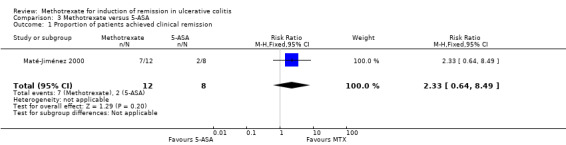
Comparison 3 Methotrexate versus 5‐ASA, Outcome 1 Proportion of patients achieved clinical remission.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Maté‐Jiménez 2000.
| Methods | Randomized (in 2:2:1 ratio to methotrexate, 6‐MP, and 5‐ASA), single‐center, controlled clinical trial | |
| Participants | Radiological or endoscopic diagnosis of CD or UC and steroid dependent (N = 72) Steroid dependent was defined as those patients whose prednisone could not be lowered to 20 mg/day without presenting inflammatory activity determined by a Mayo Clinic Score of 7 or more or having presented more than two episodes in the last 6 months or more than 3 in the last 12 months None of the patients had received 6‐MP or methotrexate prior to entry Numbers for ulcerative colitis participants: Methotrexate n = 12, 6‐mercaptopurine n = 14, 5‐aminosalicylic acid n = 8 |
|
| Interventions | Oral methotrexate 15 mg/wk or 6‐mercaptopurine 1.5 mg/kg/day or 5‐aminosalicylic acid 3 g/day for 30 weeks For 2 weeks after randomization no attempt was made to decrease prednisone dose, thereafter prednisone was decreased by 8 mg/week Prednisone was reduced if the condition of the patient remained stable or improved and discontinued if clinical remission was achieved Methotrexate was reduced to 10 mg/week and the 6‐mercaptopurine dose to 1 mg/kg/day if clinical remission was achieved Patients in the 5‐aminosalicylic acid group continued to receive 3 g/day after achieving remission and stopping prednisone |
|
| Outcomes | Remission: prednisone stopped and Mayo Clinic Score < 7 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described in published study |
| Allocation concealment (selection bias) | Unclear risk | Not described in published study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not mentioned in published study Authors assumed the study was unblinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described in published study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 24/72 patients dropped out in the first 30 weeks of the trial (worst outcome assumed) |
| Selective reporting (reporting bias) | Unclear risk | Primary outcomes were reported Some post hoc outcomes were also reported |
| Other bias | Low risk | No other issues |
Oren 1996.
| Methods | Randomized, double‐blind, placebo‐controlled Duration of treatment and study was 9 months Prepackaged coded sets (equal number of methotrextae or placebo tablets) were delivered to each centre If all of these were used up subsequent randomization was performed by a central pharmacy |
|
| Participants | Patients with definite, chronic active ulcerative colitis (Mayo clinic score of > or = 7 at entry). Chronicity was defined as steroid therapy at > or = 7.5 mg/day for at least 4 months of the proceeding year. Ulcerative colitis was diagnosed by clinical, radiographic, endoscopic, and pathological criteria.(N = 67) | |
| Interventions | Oral methotrexate (n=30; 12.5 mg/wk ‐ 2.5 mg/day) or identical placebo (n=37) for 9 months | |
| Outcomes | Remission: a Mayo clinic score of < or = 3 (or Mayo score of < or = 2 without sigmoidoscopy results) Relapse: an increase of 3 or more points in the Mayo clinic score (not including sigmoidoscopy) and or reintroduction of steroids at a dose of > or = 300 mg/month. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | At the start of the study, each center received 4‐6 prepackaged code sets containing an equal number of methotrexate or placebo tablets sufficient for 9 months of therapy. Subsequent randomization was performed by the central pharmacy. |
| Allocation concealment (selection bias) | Low risk | Centralized pharmacy randomization |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double blind. The investigators were blinded to treatment assignment. An unblinded independent observer was the only person who had access to the "drug key" in cases in which there was a compelling medical reason to break the code (and discontinue the trial) Methotrexate and placebo were in the same dosage form and quantities, and the tablets were administered in the similar fashion |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double blind trial design |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | A total of 11/67 patients withdrew from the study (methotrexate n = 2; placebo n = 9 , P < 0.052) All analyses were performed on an intention to treat basis |
| Selective reporting (reporting bias) | Low risk | All outcome were reported |
| Other bias | Low risk | No other issues |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Baron 1993 | Not a RCT ‐ open label clinical trial |
| Cummings 2005 | Not a RCT ‐ retrospective chart review |
| Dejica 1998 | Not a RCT ‐ non‐randomized, open label clinical trial |
| Egan 1999a | No placebo or active comparator ‐ trial compared two doses of subcutaneous methotrexate (15 mg/week versus 25 mg/week) |
| Egan 1999b | Not a RCT ‐ non‐randomized, pharmacokinetic study |
| Egan 2000 | Not a RCT ‐ case series |
| Fraser 2002 | Not a RCT ‐ retrospective chart review looking at maintenance treatment with methotrexate |
| Fraser 2003 | Not a RCT ‐ open label clinical trial |
| Gibson 2006 | Not a RCT ‐ retrospective chart review |
| González‐Lama 2012 | Not a RCT ‐ retrospective chart review |
| Hayes 2014 | Not a RCT ‐ retrospective chart review |
| Herrlinger 2005 | Not a RCT ‐ case control study of pharmacogenetics of methotrexate therapy in IBD |
| Houben 1994 | Not a RCT ‐ case series |
| Khan 2013 | Not a RCT ‐ retrospective cohort study |
| Kozarek 1989 | Not a RCT ‐ open label clinical trial |
| Kozarek 1992 | Not a RCT ‐ retrospective chart review |
| Mañosa 2011 | Not a RCT ‐ retrospective chart review |
| Paoluzi 2002 | Not a RCT ‐ open label clinical trial |
| Richter 2012 | Not a RCT ‐ retrospective chart review |
| Saibeni 2012 | Not a RCT ‐ retrospective chart review |
| Siveke 2003 | Not a RCT ‐ case series |
| Soon 2004 | Not a RCT ‐ retrospective chart review |
| Te 2000 | Not a RCT ‐ retrospective chart review |
| Wahed 2009 | Not a RCT ‐ retrospective chart review |
Characteristics of ongoing studies [ordered by study ID]
NCT00498589.
| Trial name or title | A controlled, randomized, double‐blind, multicenter study, comparing methotrexate versus placebo in steroid‐refractory ulcerative colitis (METEOR) |
| Methods | Multicenter, randomized, double‐blind study |
| Participants | Patients with steroid‐dependent ulcerative colitis (n=110) |
| Interventions | Methotrexate 25 mg (n=55) or placebo (n=55) given once weekly by intramuscular injection |
| Outcomes | Remission without steroids at week 16 and 24 weeks of treatment |
| Starting date | September, 2007 |
| Contact information | Franck Carbonnel, Tel: 00 33 3 81 66 82 53, Email: fcarbonnel@chu‐besancon.fr |
| Notes | NCT00498589, study is ongoing |
NCT01393405.
| Trial name or title | Randomized, double blind, prospective trial investigating the efficacy of methotrexate in induction and maintenance of steroid free remission in ulcerative colitis (MEthotrexate Response In Treatment of UC ‐ MERIT‐UC) |
| Methods | Double‐blind, placebo controlled, randomized, multicenter, parallel group trial |
| Participants | Active ulcerative colitis (n = 220) |
| Interventions | Methotrexate: induction period (week 1‐16) (open label): 25 mg MTX subcutaneous (sq) once weekly + steroid taper + 1 mg folic acid daily; maintenance period (week 17‐48) (randomization):25 mg MTX sq once weekly + 1 mg folic acid daily + 2.4 g mesalamine Placebo: sq once weekly + 1 mg folic acid daily + 2.4 g mesalamine |
| Outcomes | Primary outcome: relapse free survival Secondary outcome: mucosal healing and relapse of disease Aims of the study: i) the safety and tolerability MTX over 48 weeks; ii) the relapse‐free survival of MTX maintenance therapy compared to placebo over 32 weeks; iii) the efficacy of MTX to induce steroid free remission over 16 weeks; iv) the evaluation of clinical and pharmacogenomic models to predict the response to MTX therapy in patients with UC |
| Starting date | February 2012 |
| Contact information | Hans Herfarth, Tel: 919‐966‐6806, Email: hherf@med.unc.edu |
| Notes | NCT01393405, estimated completion date is June 2016 |
Declarations of interest
Nilesh Chande has received fees for consultancy from Abbott/AbbVie and Ferring, fees for lectures from Abbott and Janssen, travel expenses from Merck and has stock/stock options in Pfizer, Glaxo Smith Kline, Proctor and Gamble and Johnson and Johnson. All of these financial activities are outside the submitted work.
The other authors have no known declarations of interest.
Edited (no change to conclusions)
References
References to studies included in this review
Maté‐Jiménez 2000 {published data only}
- Maté‐Jiménez J, Hermida C, Cantero‐Perona J, Moreno‐Otero R. 6‐Mercaptopurine or methotrexate added to prednisone induces and maintains remission in steroid‐dependent inflammatory bowel disease. European Journal of Gastroenterology and Hepatology 2000;12(11):1227‐33. [DOI] [PubMed] [Google Scholar]
Oren 1996 {published data only}
- Oren R, Arber N, Odes S, Moshkowitz M, Keter D, Pomeranz I, et al. Methotrexate in chronic active ulcerative colitis: a double‐blind, randomized, Israeli multicenter trial. Gastroenterology 1996;110(5):1416‐21. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Baron 1993 {published data only}
- Baron TH, Truss CD, Elson CO. Low‐dose oral methotrexate in refractory inflammatory bowel disease. Digesdtive Diseases and Sciences 1993;38(10):1851‐6. [DOI] [PubMed] [Google Scholar]
Cummings 2005 {published data only}
- Cummings JR, Herrlinger KR, Travis SP, Gorard DA, McIntyre AS, Jewell DP. Oral methotrexate in ulcerative colitis. Alimentary Pharmacology and Therapeutics 2005;21(4):385‐9. [DOI] [PubMed] [Google Scholar]
Dejica 1998 {published data only}
- Dejica D, Porr PJ. Long‐term parenteral therapy with methotrexate in refractory ulcerative colitis. Preliminary results. Romanian Journal of Gastroenterology 1998;7(3):175‐8. [Google Scholar]
Egan 1999a {published data only}
- Egan L, Sandborn W, Tremaine W, Leighton J, Mays D, Pike M, et al. A randomized, single‐blind, pharmacokinetic and dose response study of subcutaneous methotrexate, 15 and 25 mg/week, for refractory ulcerative colitis and Crohn's disease. Gastroenterology 1998;14(4 Pt 2):A227. [Google Scholar]
- Egan LJ, Sandborn WJ, Tremaine WJ, Leighton JA, Mays DC, Pike MG, et al. A randomized dose‐response and pharmacokinetic study of methotrexate for refractory inflammatory Crohn's disease and ulcerative colitis. Alimentary Pharmacology and Therapeutics 1999;13(12):1597‐604. [DOI] [PubMed] [Google Scholar]
Egan 1999b {published data only}
- Egan LJ, Sandborn WJ, Mays DC, Tremaine WJ, Lipsky JJ. Plasma and rectal adenosine in inflammatory bowel disease: effect of methotrexate. Inflammatory Bowel Diseases 1999;5(3):167‐73. [DOI] [PubMed] [Google Scholar]
Egan 2000 {published data only}
- Egan LJ, Tremaine WJ, Mays DC, Lipsky JJ, Sandborn WJ. Clinical outcome and pharmacokinetics after addition of low‐dose cyclosporine to methotrexate: a case study of five patients with treatment‐resistant inflammatory bowel disease. Inflammatory Bowel Diseases 2000;6(4):286‐9. [DOI] [PubMed] [Google Scholar]
Fraser 2002 {published data only}
- Fraser AG, Morton D, McGovern D, Travis S, Jewell DP. The efficacy of methotrexate for maintaining remission in inflammatory bowel disease. Alimentary Pharmacology and Therapeutics 2002;16(4):693‐7. [DOI] [PubMed] [Google Scholar]
Fraser 2003 {published data only}
- Fraser GM, Ben‐Bassat O, Segal N, Fishman‐Mor M, Niv Y. Parenteral methotrexate is not effective treatment for refractory ulcerative colitis. Gastroenterology 2003;124(4 Suppl 1):A525. [Google Scholar]
Gibson 2006 {published data only}
- Gibson P, Nathan D, John I. Subcutaneous methotrexate: a safe and effective therapy in IBD. Gastroenterology 2006;130(4 Suppl 2):A661. [Google Scholar]
González‐Lama 2012 {published data only}
- González‐Lama Y. Efficacy and safety of methotrexate therapy in inflammatory bowel disease. The Madrid experience. Gastroenterology 2009;136(5 Suppl 1):A662. [Google Scholar]
- González‐Lama Y, Taxonera C, López‐Sanromán A, Pérez‐Calle JL, Bermejo F, Pajares R, et al. Methotrexate in inflammatory bowel disease: a multicenter retrospective study focused on long‐term efficacy and safety. The Madrid experience. European Journal of Gastroenterology and Hepatology 2012;24(9):1086‐91. [DOI] [PubMed] [Google Scholar]
Hayes 2014 {published data only}
- Hayes MJ, Sakuraba A, Stein AC, Hanauer SB. A comparison of efficacy, pharmacokinetics and immunogenicity in patients with ulcerative colitis receiving infliximab monotherapy versus combination therapy. Gastroenterology 2013;144(5 Suppl 1):S430. [DOI] [PubMed] [Google Scholar]
- Hayes MJ, Stein AC, Sakuraba A. Comparison of efficacy, pharmacokinetics, and immunogenicity between infliximab mono‐ versus combination therapy in ulcerative colitis. Journal of Gastroenterology and Hepatology 2014;29(6):1177‐85. [DOI] [PubMed] [Google Scholar]
Herrlinger 2005 {published data only}
- Herrlinger KR, Cummings JR, Barnardo MC, Schwab M, Ahmad T, Jewell DP. The pharmacogenetics of methotrexate in inflammatory bowel disease. Pharmacogenetics and Genomics 2005;15(10):705‐11. [DOI] [PubMed] [Google Scholar]
Houben 1994 {published data only}
- Houben MH, Wijk HJ, Driessen WM, Spreeuwel JP. Methotrexate as possible treatment in refractory chronic inflammatory intestinal disease [Methotrexaat Als Mogelijke Behandeling Bij Refractaire Chronische Inflammatoire Darmziekte]. Nederlands Tijdschrift voor Geneeskunde 1994;138(51):2552‐6. [PubMed] [Google Scholar]
Khan 2013 {published data only}
- Khan N, Abbas A, Moehlen M, Balart L. Methotrexate in ulcerative colitis: a nationwide retrospective cohort from the Veteran Affairs Healthcare System. American Journal of Gastroenterology 2012;107:S690‐1. [Google Scholar]
- Khan N, Abbas AM, Moehlen M, Balart L. Methotrexate in ulcerative colitis: a nationwide retrospective cohort from the Veteran Affairs Health Care System. Inflammatory Bowel Diseases 2013;19(7):1379‐83. [DOI] [PubMed] [Google Scholar]
Kozarek 1989 {published data only}
- Kozarek RA, Patterson DJ, Gelfand MD, Botoman VA, Ball TJ, Wilske KR. Methotrexate induces clinical and histologic remission in patients with refractory inflammatory bowel disease. Annals of Internal Medicine 1989;110(5):353‐6. [DOI] [PubMed] [Google Scholar]
Kozarek 1992 {published data only}
- Kozarek RA, Patterson OJ, Gelfand MD, Ball TJ, Botoman VA. Long‐term use of methotrexate in inflammatory bowel disease: severe disease 3, drug therapy 2. Seventh inning stretch. Gastroenterology 1992;102(Suppl):A648. [Google Scholar]
Mañosa 2011 {published data only}
- Mañosa M, García V, Castro L, García‐Bosch O, Chaparro M, Barreiro‐de Acosta M, et al. Methotrexate in ulcerative colitis: a Spanish multicentric study on clinical use and efficacy. Journal of Crohn's and Colitis 2011;5(5):397‐401. [DOI] [PubMed] [Google Scholar]
Paoluzi 2002 {published data only}
- Paoluzi OA, Pica R, Marcheggiano A, Crispino P, Iacopini F, Iannoni C, et al. Azathioprine or methotrexate in the treatment of patients with steroid‐dependent or steroid‐resistant ulcerative colitis: results of an open‐label study on efficacy and tolerability in inducing and maintaining remission. Alimentary Pharmacology and Therapeutics 2002;16(10):1751‐9. [DOI] [PubMed] [Google Scholar]
Richter 2012 {published data only}
- Richter JM, Kushkuley S, Barrett JA, Oster G. Treatment of new‐onset ulcerative colitis and ulcerative proctitis: a retrospective study. Alimentary Pharmacology and Therapeutics 2012;36(3):248‐56. [DOI] [PubMed] [Google Scholar]
Saibeni 2012 {published data only}
- Saibeni S, Bollani S, Losco A, Michielan A, Sostegni R, Devani M, et al. The use of methotrexate for treatment of inflammatory bowel disease in clinical practice. Digestive and Liver Disease 2012;44(2):123‐7. [DOI] [PubMed] [Google Scholar]
Siveke 2003 {published data only}
- Siveke JT, Folwaczny C. Methotrexate in ulcerative colitis. Alimentary Pharmacology and Therapeutics 2003;17(3):479‐80. [DOI] [PubMed] [Google Scholar]
Soon 2004 {published data only}
- Soon SY, Ansari A, Yaneza M, Raoof S, Hirst J, Sanderson JD. Experience with the use of low‐dose methotrexate for inflammatory bowel disease. European Journal of Gastroenterology and Hepatology 2004;16(9):921‐6. [DOI] [PubMed] [Google Scholar]
Te 2000 {published data only}
- Te HS, Schiano TD, Kuan SF, Hanauer SB, Conjeevaram HS, Baker AL. Hepatic effects of long‐term methotrexate use in the treatment of inflammatory bowel disease. American Journal of Gastroenterology 2000;95(11):3150‐6. [DOI] [PubMed] [Google Scholar]
Wahed 2009 {published data only}
- Wahed M, Louis‐Auguste JR, Baxter LM, Limdi JK, McCartney SA, Lindsay JO, et al. Efficacy of methotrexate in Crohn's disease and ulcerative colitis patients unresponsive or intolerant to azathioprine /mercaptopurine. Alimentary Pharmacology and Therapeutics 2009;30(6):614‐20. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT00498589 {published data only}
- A controlled, randomized, double‐blind, multicenter study, comparing methotrexate versus placebo in steroid‐refractory ulcerative colitis (METEOR). Ongoing study September, 2007.
NCT01393405 {published data only}
- Randomized, double blind, prospective trial investigating the efficacy of methotrexate in induction and maintenance of steroid free remission in ulcerative colitis (MEthotrexate Response In Treatment of UC ‐ MERIT‐UC). Ongoing study February 2012.
Additional references
Ardizzone 2006
- Ardizzone S, Maconi G, Russo A, Imbesi V, Colombo E, Bianchi Porro G. Randomised controlled trial of azathioprine and 5‐aminosalicylic acid for treatment of steroid dependent ulcerative colitis. Gut 2006;55(1):47‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bach 2006
- Bach SP, Mortensen NJ. Revolution and evolution: 30 years of ileoanal pouch surgery. Inflammatory Bowel Diseases 2006;12(2):131‐45. [DOI] [PubMed] [Google Scholar]
Feagan 1995
- Feagan BG, Rochon J, Fedorak RN, Irvine EJ, Wild G, Sutherland L, et al. Methotrexate for the treatment of Crohn's disease. The North American Crohn's Study Group Investigators. New England Journal of Medicine 1995;332(5):292‐7. [DOI] [PubMed] [Google Scholar]
Feagan 2000
- Feagan BG, Fedorak RN, Irvine EJ, Wild G, Sutherland L, Steinhart AH, et al. A comparison of methotrexate with placebo for the maintenance of remission in Crohn's disease. North American Crohn's Study Group Investigators. New England Journal of Medicine 2000;342(22):1627‐32. [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawthorne 1992
- Hawthorne AB, Logan RF, Hawkey CJ, Foster PN, Axon AT, Swarbrick ET, et al. Randomised controlled trial of azathioprine withdrawal in ulcerative colitis. BMJ 1992;305(6844):20‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Jewell 1974
- Jewell DP, Truelove SC. Azathioprine in ulcerative colitis: final report on controlled therapeutic trial. British Medical Journal 1974;4(5945):627‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lawson 2006
- Lawson MM, Thomas AG, Akobeng AK. Tumour necrosis factor alpha blocking agents for induction of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD005112.pub2] [DOI] [PubMed] [Google Scholar]
Lopez‐Olivo 2014
- Lopez‐Olivo MA, Siddhanamatha HR, Shea B, Tugwell P, Wells GA, Suarez‐Almazor ME. Methotrexate for treating rheumatoid arthritis. Cochrane Database of Systematic Reviews 2014, Issue 6. [DOI: 10.1002/14651858.CD000957.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
McDonald 2012
- McDonald JWD, Tsoulis DJ, MacDonald JK, Feagan BG. Methotrexate for induction of remission in refractory Crohn's disease. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD003459.pub3] [DOI] [PubMed] [Google Scholar]
Patel 2014
- Patel V, Wang Y, MacDonald JK, McDonald JW, Chande N. Methotrexate for maintenance of remission in Crohn's disease. Cochrane Database of Systematic Reviews 2014, Issue 8. [DOI: 10.1002/14651858.CD006884.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rutgeerts 2005
- Rutgeerts P, Sandborn WJ, Feagan BG, Reinisch W, Olson A, Johanns J, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. New England Journal of Medicine 2005;353(23):2462‐76. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Shibolet 2005
- Shibolet O, Regushevskaya E, Brezis M, Soares‐Weiser K. Cyclosproine A for induction of remission in severe ulcerative colitis. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI: 10.1002/14651858.CD004277.pub2] [DOI] [PubMed] [Google Scholar]
Timmer 2012
- Timmer A, McDonald JWD, Tsoulis DJ, MacDonald JK. Azathioprine and 6‐mercaptopurine for maintenance of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD000478.pub3] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Chande 2007
- Chande N, MacDonald JK, McDonald JW. Methotrexate for induction of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD006618.pub2] [DOI] [PubMed] [Google Scholar]


