Abstract
OBJECTIVE
This study examines the prevalence of disordered eating behaviors (DEB) and its associations with glycemic control, insulin sensitivity (IS), and psychosocial functioning in a large, diverse cohort of youth and young adults with type 1 or type 2 diabetes.
RESEARCH DESIGN AND METHODS
In the SEARCH for Diabetes in Youth study, 2,156 youth and young adults with type 1 diabetes (mean ± SD age 17.7 ± 4.3 years; 50.0% female) and 149 youth and young adults with type 2 diabetes (age 21.8 years ± 3.5; 64.4% female) who were receiving insulin therapy completed the Diabetes Eating Problem Survey–Revised (DEPS-R), a self-reported measure for identifying disordered eating. DEB were defined as a DEPS-R score ≥20. Demographic characteristics, clinical measures, and health behaviors of participants with DEB and those without DEB were compared by using t tests.
RESULTS
DEB were observed in 21.2% of participants with type 1 diabetes and 50.3% of participants with type 2 diabetes. Participants encountered challenges in maintaining a healthy weight while controlling their diabetes. For both types of diabetes, individuals with DEB had a significantly higher BMI z score, lower insulin sensitivity, more depressive symptoms, and poorer quality of life than those without DEB. Diabetic ketoacidosis episodes occurred more frequently in youth with type 1 diabetes with DEB compared to those without DEB.
CONCLUSIONS
These findings highlight that DEB are prevalent among youth and young adults with type 1 and type 2 diabetes and who are receiving insulin therapy, and DEB are associated with poorer clinical outcomes and psychosocial well-being. Heightened awareness and early interventions are needed to address DEB for this at-risk population, as are longitudinal studies evaluating the course of DEB and diabetes outcomes.
Introduction
Individuals with diabetes may encounter multiple complex medical and psychosocial issues. The American Diabetes Association recently released a position statement emphasizing the importance of psychosocial care for people with diabetes (1). Adults with type 1 diabetes are reported to be at a higher risk for clinical eating disorders and other disordered eating behaviors (DEB) than are their peers who do not have diabetes (2,3). DEB generally refer to maladaptive behaviors such as restricting food intake, binge eating, using laxatives, or performing intense physical exercise in order to reduce body weight (4). The etiology of DEB in diabetes seems to be multifactorial. Behaviors and attitudes that are important components of diabetes management, such as dietary restraint and counting carbohydrates, may place an unhealthy emphasis on food intake that results in dysregulated eating patterns. Moreover, individuals with diabetes may engage in DEB specific to diabetes, including omitting insulin (5–9). In adults with type 1 diabetes, DEB are associated with a higher BMI z score (BMIz), younger age, and shorter duration of diabetes (10,11).
Children and adolescents with diabetes are also vulnerable to DEB, as shown by previous studies in youth with type 1 diabetes (10–12). By contrast, DEB have not been well studied in youth with type 2 diabetes. In the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) study of 678 youth with type 2 diabetes, 26% of youth reported binge-eating symptoms (12). Compared with those who did not report binge-eating symptoms, these youth also reported significantly higher rates of extreme obesity, depressive symptoms, and impaired quality of life. More research is needed to understand other potential behaviors, such as skipping meals or self-induced vomiting, among youth with type 1 or type 2 diabetes.
The aims of our study were to investigate the prevalence of DEB in youth and young adults with type 1 or type 2 diabetes from the SEARCH for Diabetes in Youth study; to assess individual characteristics, including insulin sensitivity, according to DEB status; and to evaluate clinical and psychosocial outcomes among participants with and without DEB.
Research Design and Methods
SEARCH for Diabetes in Youth Study
The SEARCH for Diabetes in Youth study is a population-based prospective cohort study following children, adolescents, and young adults from diverse racial and ethnic backgrounds who were diagnosed with diabetes at <20 years of age. SEARCH for Diabetes in Youth study participants are identified at sites in five states: Ohio, Washington, South Carolina, Colorado, and California. Details of the study methods are described elsewhere (13,14).
Study Participants
Participants who received a diagnosis of type 1 or type 2 diabetes in 2002–2008 and completed a baseline research visit near the time of diabetes diagnosis were recruited into the SEARCH Cohort Study, which took place in the third phase of the SEARCH for Diabetes in Youth Study, at which time diabetes duration was at least 5 years. At the cohort study visit, standardized outcomes were measured and complete risk factor assessments were performed. The SEARCH Cohort Study enrolled 2,777 individuals. For this analysis, we included participants with type 1 or type 2 diabetes, on the basis of a health care provider’s assessment of diabetes type, who were diagnosed at an age of 10 years or older, reported receiving insulin therapy at the time of their cohort study visit, and completed the Diabetes Eating Problem Survey–Revised (DEPS-R), the Center for Epidemiological Studies Depression Scale (CES-D), and the Pediatric Quality of Life (PedsQL) scale (15–19). Individuals with type 2 diabetes who did not report insulin therapy were excluded because the DEPS-R includes questions about insulin use. Before implementing the protocol, we obtained approval from the local institutional review board(s) at each center. Written informed consent was obtained from participants aged ≥18 years, whereas participant assent and parental written informed consent were obtained for participants <18 years old.
Anthropometric Measurements and Insulin Sensitivity
During the SEARCH cohort visit, surveys were completed, anthropometric measurements were taken, and blood and urine were collected. Participants completed standardized questionnaires for medical history and medications. BMI was calculated as weight (kilograms)/height (meters squared), and age- and sex-specific BMIz were derived (20). Waist circumference was measured using the National Health and Nutrition Examination Survey (NHANES) protocol (21). Hemoglobin A1c (HbA1c) was measured at the central laboratory by using ion-exchange high-performance liquid chromatography (TOSOH Biosciences Inc., South San Francisco, CA) (22). Insulin sensitivity (IS) score is a surrogate marker to determine the degree of IS and is based on clinical measures including waist circumference, plasma triacylglycerol level, and HbA1c. It is estimated by using the following formula: logIS = 4.64725 − 0.02032(waist circumference, cm) − 0.09779(HbA1c, %) − 0.00235(triacylglycerol, mg/dL). The estimated IS score was validated in previous studies that used a euglycemic-hyperinsulinemic clamp in a subset of 12- to 19-year-old youth with diabetes (23,24).
Assessment for DEB and Health Outcomes Including Depression and Quality of Life
DEB were assessed by using the DEPS-R, a validated self-reported screening tool comprising 16 diabetes-specific items. The DEPS-R has demonstrated good psychometric properties and reliability (Cronbach α coefficient = 0.9) for screening for DEB in children and adolescents with type 1 diabetes (15–17). It includes questions regarding adjusting insulin specifically for the purposes of reducing weight. One sample question is, “After I overeat, I skip my next insulin dose.” Responses are scored on a six-point Likert scale (0 = never, 1 = rarely, 2 = sometimes, 3 = often, 4 = usually, 5 = always) and are to consider behaviors within the preceding month. Higher scores indicate a higher frequency of maladaptive behaviors around eating, which may warrant further clinical interview and assessment. A recommended cutoff score of 20 has been empirically established as a threshold that indicates the need for further clinical assessment (15). This cutoff was determined by examining a general population of youth with type 1 diabetes who have no known diagnosis of an eating disorder, and external validity was confirmed against reports by medical providers. In our study, we used the recommended threshold, defining DEB as a DEPS-R score ≥20. In addition, on the basis of the response to each question, we analyzed individual behaviors including self-induced vomiting, binge eating, and skipping meals. Responses could range from 0 to 5; scores ≥2 (i.e., responses of “sometimes,” “often,” “usually,” or “always”) were considered clinically significant.
Health outcomes were assessed by considering glycemic control, the presence of depressive symptoms, and overall quality of life. Glycemic control was measured by using HbA1c. Depressive symptoms were measured by using the CES-D, which is a 20-item scale that measures depressive symptoms and has good sensitivity and high internal consistency (Cronbach α coefficient = 0.9) (18,25). A cut point of 16 was suggested for adolescents in order to stratify depression severity as minimal (scores 0–15), mild (scores 16–23), or moderate/severe (score 24–60).
Perceived quality of life was measured by using the PedsQL scale, which is a measure based on a model defining quality of life through the evaluation of major categories of fundamental life needs (Cronbach α coefficient = 0.8). The items are categorized into four scales including physical, emotional, social, and school functioning. As an example, one question asks how much of a problem paying attention in class has been for the individual during the past 1 month. Items on the PedsQL scale are reverse-scored and transformed to a scale of 0–100. Higher scores indicate better perceived health-related quality of life (19).
Statistical Analysis
Demographic characteristics of individuals in the study sample were summarized by using descriptive statistics. Sociodemographic characteristics and health outcomes were compared across DEB statuses by using the χ2 test for categorical variables and the t test for continuous variables for each diabetes type. We used three age categories: 10–14 years, 15–19 years, and ≥20 years. Individual DEB were assessed by counting the frequency of responses for each question. Differences in BMIz and IS scores between those who did and those who did not exhibit DEB were examined by using the t test. All analyses were performed separately for type 1 and type 2 diabetes, with a significance level of α < 0.05. All analyses were performed in SAS version 9.4 (SAS Institute, Cary, NC).
Results
Participant Characteristics
We analyzed a total of 2,156 youth and young adults with type 1 diabetes and 149 participants with type 2 diabetes who use insulin and were 10–25 years old. The mean ± SD age was 17.7 ± 4.3 years for participants with type 1 diabetes and 21.8 ± 3.5 years for participants with type 2 diabetes. Females accounted for 50% of participants with type 1 diabetes and 64% of those with type 2 diabetes. The predominant racial/ethnic group was non-Hispanic white (75.6%) for individuals with type 1 diabetes and African American (51.0%) for those with type 2 diabetes (Table 1). Participants with type 1 diabetes had higher socioeconomic status and higher household income, and their parent(s) had more education, than participants with type 2 diabetes. The mean ± SD HbA1c was 9.2 ± 1.8% for individuals with type 1 diabetes and 10.4 ± 2.5% for those with type 2 diabetes. Approximately 55% of participants with type 1 diabetes receive insulin through a pump and 18.5% use a continuous glucose monitoring (CGM) system, compared with 18.5% and 34.5% with type 2 diabetes, respectively. Overall, participants with type 1 diabetes had higher IS scores (mean ± SD 6.7 ± 2.5) than participants with type 2 diabetes (3.2 ± 1.8) (Table 1).
Table 1.
Characteristics of cohort study participants stratified by diabetes type and DEB status*
| Characteristics | Type 1 diabetes (n = 2,156) |
Type 2 diabetes (n = 149) |
||||
|---|---|---|---|---|---|---|
| DEB (n = 458) | No DEB (n = 1,698) | P value | DEB (n = 75) | No DEB (n = 74) | P value | |
| Age, years | 18.2 ± 3.8 | 17.6 ± 4.4 | <0.01 | 21.1 ± 3.3 | 22.6 ± 3.6 | <0.01 |
| Male sex (%) | 28.8 | 55.2 | <0.01 | 32.0 | 39.2 | 0.36 |
| Race/ethnicity (%) | ||||||
| Non-Hispanic black | 18.1 | 8.6 | <0.01 | 56.0 | 45.9 | 0.58 |
| Hispanic | 13.5 | 11.0 | 18.7 | 25.6 | ||
| White | 66.4 | 78.0 | 21.3 | 21.7 | ||
| Other | 2.0 | 2.4 | 4.0 | 6.8 | ||
| BMI, kg/m2 | 26.1 ± 5.3 | 23.2 ± 4.8 | <0.01 | 37.8 ± 9.4 | 31.8 ± 8.7 | <0.01 |
| BMIz | 1.0 ± 0.9 | 0.5 ± 0.9 | <0.01 | 2.0 ± 0.6 | 1.3 ± 1.1 | <0.01 |
| Glycemic control | ||||||
| HbA1c, % | 10.2 ± 2.0 | 8.9 ± 1.7 | <0.01 | 11.0 ± 2.3 | 9.8 ± 2.5 | <0.01 |
| Total daily insulin, units/kg/day | 0.9 ± 0.4 | 0.8 ± 0.4 | 0.55 | 0.7 ± 0.4 | 0.8 ± 0.5 | 0.22 |
| CGM use (%) | 4.1 | 14.9 | 0.38 | 14.8 | 16.1 | 0.76 |
| Self-monitoring of blood glucose (%) | ||||||
| Less than once a week | 15.2 | 0.0 | <0.01 | 37.9 | 25.4 | 0.15 |
| Less than once a day | 0.0 | 10.0 | 0.0 | 0.0 | ||
| 1–2 times/day | 17.2 | 14.9 | 34.9 | 26.9 | ||
| 3 times/day | 17.9 | 54.2 | 15.2 | 26.9 | ||
| 4–6 times/day | 43.7 | 9.9 | 10.6 | 19.4 | ||
| ≥7 times/day | 6.0 | 1.4 | 1.4 | |||
| IS score | 5.2 ± 2.0 | 7.1 ± 2.5 | <0.01 | 2.5 ± 1.3 | 3.8 ± 1.9 | <0.01 |
| DKA (≥1 episode) in preceding 6 months (%) | 12.0 | 4.7 | <0.01 | 5.3 | 4.1 | NS |
| CES-D score | 16.7 ± 10.3 | 8.3 ± 7.5 | <0.01 | 20.9 ± 11.0 | 11.9 ± 10.5 | <0.01 |
| PedsQL score | 72.4 ± 14.6 | 84.8 ± 11.8 | <0.01 | 68.7 ± 17.4 | 80.8 ± 16.7 | <0.01 |
Data are mean ± SD unless otherwise indicated.
*DEB status is based on DEPS-R category.
Characteristics of Individuals With DEB
DEB (i.e., DEPS-R score ≥20, with all questions analyzed) were observed in 21.2% of participants with type 1 diabetes and 50.3% of those with type 2 diabetes. Mean ± SD DEPS-R score was 12.7 ± 10.3 for youth with type 1 diabetes and 21.9 ± 12.6 for youth with type 2 diabetes. The prevalence of DEB among both those with type 1 and those with type 2 diabetes was highest in the 15- to 19-year-old age group: 24.9% of adolescents aged 15–19 years and 16% of those aged 10–14 years with type 1 diabetes reported DEB. Among those with type 2 diabetes, ∼67.8% of adolescents aged 15–19 years reported DEB. Among those who had DEB, approximately two-thirds were female (71.2% of those with type 1 diabetes and 68.0% of those with type 2 diabetes). For youth and young adults with type 1 diabetes, individuals with DEB comprised a higher proportion of nonwhite youth and are characterized by having parents with less education, lower household income, and a lack of private health insurance. For youth with type 2 diabetes, we found no significant associations between DEB status and sociodemographic characteristics.
DEB were significantly associated with higher BMIz in participants with type 1 and participants with type 2 diabetes (Table 2). Participants with DEB had lower IS scores (type 1 diabetes: 5.2 vs. 7.1 in those without DEB; type 2 diabetes: 2.5 vs. 3.8 in those without DEB; P < 0.01). We found no significant association of total daily insulin dose with DEB for either type of diabetes. Participants with type 1 diabetes who had DEB were less likely to use an insulin pump, but we observed no difference in CGM use between those with and those without DEB. Blood glucose was self-monitored less frequently in participants with DEB; half of the participants (those with type 1 and those with type 2 diabetes) reported checking blood glucose values three times or fewer per day.
Table 2.
BMI, HBA1c, and IS scores associated with the presence of individual DEB in participants with type 1 diabetes*
| DEB | BMI (kg/m2) | P value | HbA1c (%) | P value | IS score | P value |
|---|---|---|---|---|---|---|
| Insulin restriction# | ||||||
| Yes | 24.3 ± 4.9 | 0.03 | 10.5 | <0.01 | 5.4 ± 2.0 | <0.01 |
| No | 23.7 ± 5.0 | 8.9 | 7.0 ± 2.5 | |||
| Skipping meals## | ||||||
| Yes | 25.5 ± 5.4 | <0.01 | 9.5 | <0.01 | 5.9 ± 2.3 | <0.01 |
| No | 22.9 ± 4.5 | 9.1 | 7.2 ± 2.5 | |||
| Binge eating### | ||||||
| Yes | 24.5 ± 5.1 | <0.01 | 9.6 | <0.01 | 6.1 ± 2.3 | <0.01 |
| No | 23.1 ± 4.8 | 8.8 | 7.3 ± 2.5 | |||
| Self-induced vomiting#### | ||||||
| Yes | 25.7 ± 5.4 | 0.04 | 10.2 | <0.01 | 5.0 ± 2.0 | <0.01 |
| No | 23.8 ± 5.0 | 9.2 | 6.8 ± 2.5 |
*Significant differences were not found in reported behaviors of participants with type 2 diabetes.
#Behavior derived from the survey question regarding insulin restriction: “I take less insulin than I should.”
##Behavior derived from the survey question regarding skipping meals: “I skip meals and/or snacks.”
###Behavior derived from the survey question regarding binge eating: “I alternate between eating very little and eating huge amounts.”
####Behavior derived from the survey question regarding self-induced vomiting: “I make myself vomit.”
Health Outcomes
Youth with DEB had higher HbA1c than individuals without DEB (type 1 diabetes: mean ± SD 10.2 ± 2% vs. 8.9 ± 1.7%; type 2 diabetes: 11.0 ± 2.2% vs. 9.8 ± 2.5%; P < 0.001). Participants with type 1 diabetes who had DEB reported more frequent hospitalizations for diabetic ketoacidosis (DKA) in the 6 months before the study visit than did their counterparts without DEB. The frequency of hypoglycemia episodes was not significantly different between the two groups. For both types of diabetes, participants with DEB had significantly higher CES-D scores than those who did not have DEB (16.7 vs. 8.3 in type 1 diabetes; 20.9 vs. 11.9 in type 2 diabetes; P < 0.01), indicating more depressive symptoms among those with DEB. They also had lower PedsQL scores than their counterparts, reflecting the overall poorer quality of life (Table 1).
Specific Behaviors Related to DEB
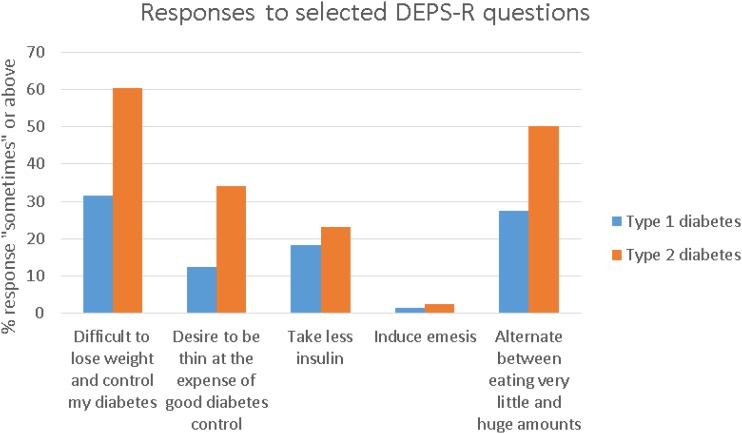
Regarding specific behaviors queried by individual items on the DEPS-R survey, 31.5% of participants with type 1 diabetes and 60.3% of participants with type 2 diabetes reported challenges in maintaining a healthy weight while controlling their diabetes in the preceding month (Fig. 1). Among the participants, 20% of those with type 1 diabetes and 34.2% of those with type 2 diabetes reported concern that their eating is out of control. Approximately 12% of youth with type 1 diabetes and ∼33% with type 2 diabetes reported a desire to be thin even at the expense of good diabetes control. Approximately 18.2% of participants with type 1 diabetes and 23.1% with type 2 diabetes reported taking less insulin than they should. Among the obese subjects with type 1 diabetes, 60.9% reported binge eating, whereas 47.2% of participants with a normal or low weight reported this behavior (Table 3). Skipping meals was more common among obese participants with type 1 diabetes.
Figure 1.
Responses to DEPS-R questions scored ≥2 (“sometimes,” “often,” “usually,” or “always”) by study participants with type 1 diabetes and participants with type 2 diabetes.
Table 3.
Prevalence of each behavior per weight categories in type 1 diabetes
| Insulin restriction | Skipping meals | Binge eating | Self-induced vomiting | |
|---|---|---|---|---|
| Normal weight or underweight (n = 1,309) | 18.3% | 30.3% | 47.2% | 1.1% |
| Overweight (n = 408) | 16.2% | 39.9% | 57.5% | 1.0% |
| Obese (n = 258) | 18.2% | 55.2% | 60.9% | 3.1% |
| P value | 0.6213 | <0.001 | <0.001 | 0.0632 |
Sample sizes by weight do not include all participants because of missing data for participants in each weight category.
Participants with type 1 diabetes who skipped meals had a higher frequency of reported severe hypoglycemic episodes (data not shown; P = 0.03). We also analyzed individual behaviors with respect to BMI and IS scores for participants in both diabetes groups. Significantly higher BMI and lower IS scores were observed in participants with type 1 diabetes who restricted insulin, skipped meals, or binged, but this finding did not reach statistical significance in individuals with type 2 diabetes (Table 2).
Conclusions
In our study, which is to our knowledge one of the largest to include adolescents and young adults with type 1 or type 2 diabetes, DEB were observed in more than one in five of all participants with type 1 diabetes and in approximately half of participants with type 2 diabetes. The frequency of DEB in females with type 1 diabetes was 30% in our study, similar to previous reports that ∼35–40% of females aged 10–19 years old who have type 1 diabetes have DEB (26). DEB were more prevalent in our cohort of youth and young adults with type 2 diabetes than is indicated by findings in adults with type 2 diabetes (6.5–20.0%) (11). Insulin omission was reported in 18% of participants with type 1 diabetes and in 23% of individuals with type 2 diabetes. The frequency of insulin restriction in our study was less than that reported among adults with type 1 diabetes (30–35%) (27); this perhaps is attributable, at least in part, to parents’ involvement in youths’ diabetes management.
Given the focus on planning meals, portioning food, and monitoring carbohydrate intake that is recommended for those managing diabetes, it is not surprising that individuals with diabetes are susceptible to unhealthy behaviors around food. The prevalence of subclinical eating disorders is estimated at 3.6% among the adult population, increasing up to 15–20% among the obese population (10). Similarly, our study demonstrated that DEB are associated with higher BMIz in both types of diabetes. Youth and young adults who are overweight or obese may desire to lose weight, which may result in a negative body image, dieting, and DEB (11,26,28). Overweight and obese youth and young adults with diabetes are commonly counseled to reduce their weight, at which time health care professionals should query for, identify, and address DEB. Specific eating habits, such as binge-eating behaviors, are common among obese individuals. We corroborated this in our study using responses about alternating eating very small and very large food portions. It was surprising that, in our cohort, those who restricted insulin had a higher BMI than those who did not restrict insulin, given the catabolic effects of insulin deficiency (29). This association may reflect concomitant maladaptive behaviors such as binge eating that co-occur with insulin restriction. In the subset of participants with type 1 diabetes who have low BMI (z score 1 SD below the mean), ∼10% had features of DEB, suggesting that components of dieting or restricting meals in order to lose weight can occur along the weight spectrum. We observed no significant associations related to insulin restriction in our population with type 2 diabetes, likely because of the small sample size.
Recent evidence suggests that the age at onset of DEB decreases over time, with a current median age at onset estimated at 14–19 years (30). In our study, among those with type 1 diabetes, 16% of children aged 10–14 years and 24.9% of adolescents aged 15–19 years had some form of maladaptive behavior, such as binge eating and omitting insulin. Adolescence is a developmental stage in which risky behaviors such as alcohol use, unsafe sexual behaviors, and unhealthy dietary behaviors are increased. Furthermore, social media and peers influence many adolescents’ body image, and genetic risk for DEB is moderated by the onset of puberty (31,32). Thus, adolescence is a critical period of risk for the onset of DEB.
In our study, we found that youth with type 1 diabetes who reported DEB were more likely to be female. The development of type 1 diabetes during preadolescence seems to place already susceptible girls at an even greater risk for the subsequent development of eating disorders (33). We found no significant difference in DEB between females and males with type 2 diabetes in our study; both are susceptible to DEB. Thus, health care providers should be aware of the increased risk in both sexes (34).
In addition, we observed that DEB occur more often in those with lower household income and whose parents have less education. This may reflect less parental attention to their child’s diabetes, food insecurity (including challenges in purchasing healthy food and a paucity of structured meals), or both (35,36).
To our knowledge, this study is the first to look at the association between insulin sensitivity and DEB in individuals with diabetes by using IS scores estimated from clinical measures including waist circumference, HbA1c, and triglyceride levels (23). In both participants with type 1 and those with type 2 diabetes, DEB were associated with lower IS scores and hence more insulin resistance. It may be that those with DEB had a higher BMIz and thus are more likely to have an unhealthy weight, leading to increased insulin resistance. This is in contrast to a previous study of individuals with anorexia nervosa but without diabetes, in which IS had a strong, positive genetic correlation with anorexia nervosa, related to the effect of leptin on regulating food intake and energy expenditure (37).
In our study, DEB were associated with worse glycemic control in participants with either type of diabetes. In particular, participants who reported skipping meals or binge eating had higher HbA1c values. Although not examined in this report, hyperglycemia and elevated HbA1c can lead to long-term diabetes-related complications including retinopathy, nephropathy, and neuropathy, which may be accelerated by DEB (38). DEB were also associated with a twofold increase in the number of DKA episodes in the past 6 months among participants with type 1 diabetes. Insulin omission is a unique but maladaptive strategy to promote weight loss in individuals with diabetes, and this places those individuals at increased risk for developing DKA (38). DKA is less often observed in people with type 2 diabetes despite poor glycemic control, largely because of relatively sufficient insulin to block lipolysis and ketoacid formation.
Participants with DEB were more likely than those without DEB to have more depressive symptoms and lower perceived quality of life, which may further compromise their diabetes management. Our study focused only on DEB; however, factors including adherence to the medical regimen, resilience against stress, and family/peer support also play important roles in diabetes management that can affect health outcomes. Declining diabetes control is common as children progress toward adolescence and is due to behavioral and health-related challenges in diabetes (39).
One limitation of our study is that the DEPS-R has not been validated in individuals with type 2 diabetes. Most questions are relevant to individuals with type 2 diabetes who take insulin, including those regarding binge-eating behaviors, insulin omission, and efforts to control weight. However, one question asks whether weight loss is an important goal. We conducted additional analyses to explore the validity of the DEPS-R for youth with type 2 diabetes in our sample by excluding the item, “Losing weight is an important goal to me.” We considered that this might be too general a question for youth and young adults with type 2 diabetes, as weight loss is recommended often. We maintained the same scoring system for individuals with type 2 diabetes. The majority of youth with type 2 diabetes scored high for this question, which might overestimate the overall scores. When this question was excluded, ∼39% of participants screened positive for DEB; this did not change our results for youth with type 2 diabetes (Supplementary Table 1). The Youth Eating Disorder Examination Questionnaire was used in the TODAY study in order to measure eating disorder symptoms in young people with type 2 diabetes (12). Existing instruments/tools that are used to assess diabetes-specific eating and treatment behaviors and concerns in type 2 diabetes need to be refined. In addition, dietary intake and amount of exercise are not part of the DEPS-R screening tool.
Another limitation is the relatively small sample size of individuals with type 2 diabetes. Because of the questions related to insulin in the DEPS-R screening tool, we included only participants receiving insulin therapy, which limits the generalizability of our results. Because this was a cross-sectional study, we are unable to delineate the causal relationship between DEB and diabetes outcomes.
Strengths of the study include the diverse population in the cohort included in the SEARCH for Diabetes in Youth study, one of the largest studies of youth-onset type 1 and type 2 diabetes in the U.S. Both females and males with diverse ethnic, racial, and socioeconomic backgrounds were assessed in this study. Furthermore, we used a diabetes-specific tool to evaluate the prevalence of DEB among people with diabetes.
Various treatments exist for eating disorders, including family-based therapy and cognitive-behavioral therapy. Early intervention has been reported to improve long-term outcomes. However, few treatments for DEB have been tested specifically in patients with diabetes, and therapy tends to be less successful in patients with type 1 diabetes than in those without diabetes (40).
In conclusion, our study showed that DEB are common in youth with type 1 diabetes and youth with type 2 diabetes, and they are associated with poorer clinical and psychosocial functioning. Assessment for DEB is an important element of psychosocial care of youth and young adults with diabetes and is recommended to begin during early adolescence. Further studies of effective preventive interventions and treatments are needed.
Supplementary Material
Article Information
Acknowledgments. The SEARCH for Diabetes in Youth study investigators are indebted to the many youth and their families, and their health care providers, whose participation made this study possible. SEARCH 3 and SEARCH 4: The authors acknowledge the involvement of the Clinical Research Center of Kaiser Permanente Southern California (funded by the Kaiser Foundation Health Plan and supported in part by the Southern California Permanente Medical Group), the South Carolina Clinical & Translational Research Institute at the Medical University of South Carolina (National Institutes of Health [NIH]/National Center for Advancing Translational Sciences [NCATS] grant nos. UL1 TR000062 and UL1 TR001450), Seattle Children’s Hospital and the University of Washington (NIH/NCATS grant no. UL1 TR00423), University of Colorado Pediatric Clinical and Translational Research Center (NIH/NCATS grant no. UL1 TR000154), the Barbara Davis Center at the University of Colorado at Denver (NIH Diabetes Endocrinology Research Center grant no. P30 DK57516), the University of Cincinnati (NIH/NCATS grant nos. UL1 TR000077 and UL1 TR001425), and the Children with Medical Handicaps program managed by the Ohio Department of Health. This study includes data provided by the Ohio Department of Health, which should not be considered an endorsement of this study or its conclusions. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institute of Diabetes and Digestive and Kidney Diseases.
Funding. The SEARCH for Diabetes in Youth study (SEARCH 3) is funded by the Centers for Disease Control and Prevention (Program Announcement nos. 00097, DP-05-069, and DP-10-001) and is supported by the National Institute of Diabetes and Digestive and Kidney Diseases. The SEARCH for Diabetes in Youth Cohort Study (SEARCH 4) is funded by the NIH, National Institute of Diabetes and Digestive and Kidney Diseases (grant no. 1UC4DK108173), and is supported by the Centers for Disease Control and Prevention. The Population Based Registry of Diabetes in Youth Study (1U18DP006131, U18DP006133, U18DP006134, U18DP006136, U18DP006138, U18DP006139) is funded by the Centers for Disease Control and Prevention and supported by the NIH, National Institute of Diabetes and Digestive and Kidney Diseases. SEARCH 3/4 sites included Kaiser Permanente Southern California (U18DP006133, U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U18DP006139, U48/CCU819241-3, U01 DP000247, and U18DP000247-06A1), Cincinnati’s Children’s Hospital Medical Center (U18DP006134, U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U18DP006138, U48/CCU419249, U01 DP000254, and U18DP002708), Seattle Children’s Hospital (U18DP006136, U58/CCU019235-4, U01 DP000244, and U18DP002710-01), and Wake Forest University School of Medicine (U18DP006131, U48/CCU919219, U01 DP000250, and 200-2010-35171).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. A.S.Y.N. and C.P. wrote the manuscript, researched data, contributed to the discussion, and reviewed the manuscript. B.A.R. researched the data and reviewed the manuscript. D.D., A.B., E.J.M.-D., A.R.K., J.M.L., C.M.P., and L.D. contributed to the discussion and reviewed and edited the manuscript. A.S.Y.N. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. This study was presented as a moderated poster at the American Diabetes Association’s 77th Scientific Sessions, San Diego, CA, 9–13 June 2017.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc18-2420/-/DC1.
Contributor Information
Collaborators: SEARCH for Diabetes in Youth Study Group, Jean M. Lawrence, Corinna Koebnick, Kristi Reynolds, Xia Li, Peggy Hung, Eva Lustigova, David J. Pettitt, Dana Dabelea, Richard F. Hamman, Lisa Testaverde, Anna Bellatorre, Georgeanna J. Klingensmith, Marian J. Rewers, David Maahs, Paul Wadwa, Stephen Daniels, Greta Wilkening, Michael G. Kahn, Clifford A. Bloch, Jeffrey Powell, Kathy Love-Osborne, Diana C. Hu, Lawrence M. Dolan, Amy S. Shah, Elaine M. Urbina, Debra A. Standiford, Elizabeth J. Mayer-Davis, Amy Mottl, Joan Thomas, Angela D. Liese, Malaka Jackson, Lisa Knight, Deborah Bowlby, James Amrhein, Bryce Nelson, Elaine Apperson, Catherine Pihoker, Irl Hirsch, Lenna L. Liu, Maryam Afkarian, Grace Kim, Craig Taplin, Faisal Malik, Angel Nip, Joyce Yi-Frazier, Lina Merjaneh, Davene Wright, Alissa Roberts, Beth Loots, Natalie Beauregard, Sue Kearns, Mary Klingsheim, Michael Pascual, Cordelia Franklin, Carlo Gangan, Carla Greenbaum, Giuseppina Imperatore, Sharon H. Saydah, Barbara Linder, Santica M. Marcovina, Noemie Clouet, Greg Foraison, Alan Strylewicz, Jessica Chait, Ralph Harting, Lynne E. D’Agostino, Jasmin Wagenknecht, Beth Divers, Elizabeth T. Reboussin, Brian Jensen, Ramon Wells, Leora Casanova, Kristin Henkin, Maureen T. Lenoir, Carrie Goldstein, Scott Williams, Jeanette Isom, Cynthia Stafford, Suerken, and June Pierce
References
- 1.Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association [published corrections appear in Diabetes Care 2017;40:287 and 726]. Diabetes Care 2016;39:2126–214027879358 [Google Scholar]
- 2.Colton PA, Olmsted MP, Daneman D, et al. Eating disorders in girls and women with type 1 diabetes: a longitudinal study of prevalence, onset, remission, and recurrence. Diabetes Care 2015;38:1212–1217 [DOI] [PubMed] [Google Scholar]
- 3.Young V, Eiser C, Johnson B, et al. Eating problems in adolescents with type 1 diabetes: a systematic review with meta-analysis. Diabet Med 2013;30:189–198 [DOI] [PubMed] [Google Scholar]
- 4.Colton P, Olmsted M, Daneman D, Rydall A, Rodin G. Disturbed eating behavior and eating disorders in preteen and early teenage girls with type 1 diabetes: a case-controlled study. Diabetes Care 2004;27:1654–1659 [DOI] [PubMed] [Google Scholar]
- 5.Kahkoska AR, Mayer-Davis EJ, Hood KK, Maahs DM, Burger KS. Behavioural implications of traditional treatment and closed-loop automated insulin delivery systems in type 1 diabetes: applying a cognitive restraint theory framework. Diabet Med 2017;34:1500–1507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawrence JM, Liese AD, Liu L, et al. Weight-loss practices and weight-related issues among youth with type 1 or type 2 diabetes. Diabetes Care 2008;31:2251–2257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wisting L, Frøisland DH, Skrivarhaug T, Dahl-Jørgensen K, Rø O. Disturbed eating behavior and omission of insulin in adolescents receiving intensified insulin treatment: a nationwide population-based study. Diabetes Care 2013;36:3382–3387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinhas-Hamiel O, Hamiel U, Greenfield Y, et al. Detecting intentional insulin omission for weight loss in girls with type 1 diabetes mellitus. Int J Eat Disord 2013;46:819–825 [DOI] [PubMed] [Google Scholar]
- 9.Bryden KS, Neil A, Mayou RA, Peveler RC, Fairburn CG, Dunger DB. Eating habits, body weight, and insulin misuse. A longitudinal study of teenagers and young adults with type 1 diabetes. Diabetes Care 1999;22:1956–1960 [DOI] [PubMed] [Google Scholar]
- 10.Peterson CM, Fischer S, Young-Hyman D. Topical review: a comprehensive risk model for disordered eating in youth with type 1 diabetes. J Pediatr Psychol 2015;40:385–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young-Hyman DL, Davis CL. Disordered eating behavior in individuals with diabetes: importance of context, evaluation, and classification. Diabetes Care 2010;33:683–689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilfley D, Berkowitz R, Goebel-Fabbri A, et al.; TODAY Study Group . Binge eating, mood, and quality of life in youth with type 2 diabetes: baseline data from the TODAY study. Diabetes Care 2011;34:858–860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pettitt DJ, Talton J, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . Prevalence of diabetes in U.S. youth in 2009: the SEARCH for Diabetes in Youth study. Diabetes Care 2014;37:402–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamman RF, Bell RA, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care 2014;37:3336–3344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Markowitz JT, Butler DA, Volkening LK, Antisdel JE, Anderson BJ, Laffel LM. Brief screening tool for disordered eating in diabetes: internal consistency and external validity in a contemporary sample of pediatric patients with type 1 diabetes. Diabetes Care 2010;33:495–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wisting L, Frøisland DH, Skrivarhaug T, Dahl-Jørgensen K, Rø O. Psychometric properties, norms, and factor structure of the Diabetes Eating Problem Survey-Revised in a large sample of children and adolescents with type 1 diabetes. Diabetes Care 2013;36:2198–2202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pinna F, Diana E, Sanna L, et al. Assessment of eating disorders with the Diabetes Eating Problems Survey - Revised (DEPS-R) in a representative sample of insulin-treated diabetic patients: a validation study in Italy. BMC Psychiatry 2017;17:262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401 [Google Scholar]
- 19.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999;37:126–139 [DOI] [PubMed] [Google Scholar]
- 20.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11 2002;246:1–190 [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention National Health and Nutrition Examination Survey (NHANES): Anthropometry Procedures Manual. Atlanta, GA, Centers for Disease Control and Prevention, 2000, p. 3–31 [Google Scholar]
- 22.Shah AS, Dolan LM, Dabelea D, et al.; SEARCH for Diabetes in Youth Study . Change in adiposity minimally affects the lipid profile in youth with recent onset type 1 diabetes. Pediatr Diabetes 2015;16:280–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dabelea D, D’Agostino RB Jr., Mason CC, et al. Development, validation and use of an insulin sensitivity score in youths with diabetes: the SEARCH for Diabetes in Youth study. Diabetologia 2011;54:78–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gayoso-Diz P, Otero-González A, Rodriguez-Alvarez MX, et al. Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study. BMC Endocr Disord 2013;13:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lawrence JM, Standiford DA, Loots B, et al.; SEARCH for Diabetes in Youth Study . Prevalence and correlates of depressed mood among youth with diabetes: the SEARCH for Diabetes in Youth study. Pediatrics 2006;117:1348–1358 [DOI] [PubMed] [Google Scholar]
- 26.Kelly-Weeder S, Phillips K, Leonard K, Veroneau M. Binge eating and weight loss behaviors of overweight and obese college students. J Am Assoc Nurse Pract 2014;26:445–451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goebel-Fabbri AE, Fikkan J, Franko DL, Pearson K, Anderson BJ, Weinger K. Insulin restriction and associated morbidity and mortality in women with type 1 diabetes. Diabetes Care 2008;31:415–419 [DOI] [PubMed] [Google Scholar]
- 28.Sonneville KR, Thurston IB, Milliren CE, Gooding HC, Richmond TK. Weight misperception among young adults with overweight/obesity associated with disordered eating behaviors. Int J Eat Disord 2016;49:937–946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goebel-Fabbri AE, Anderson BJ, Fikkan J, Franko DL, Pearson K, Weinger K. Improvement and emergence of insulin restriction in women with type 1 diabetes. Diabetes Care 2011;34:545–550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Takii M, Uchigata Y, Kishimoto J, et al. The relationship between the age of onset of type 1 diabetes and the subsequent development of a severe eating disorder by female patients. Pediatr Diabetes 2011;12:396–401 [DOI] [PubMed] [Google Scholar]
- 31.Stice E, Gau JM, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: predictive specificity in high-risk adolescent females. J Abnorm Psychol 2017;126:38–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klump KL, Burt SA, McGue M, Iacono WG. Changes in genetic and environmental influences on disordered eating across adolescence: a longitudinal twin study. Arch Gen Psychiatry 2007;64:1409–1415 [DOI] [PubMed] [Google Scholar]
- 33.Neumark-Sztainer D, Patterson J, Mellin A, et al. Weight control practices and disordered eating behaviors among adolescent females and males with type 1 diabetes: associations with sociodemographics, weight concerns, familial factors, and metabolic outcomes. Diabetes Care 2002;25:1289–1296 [DOI] [PubMed] [Google Scholar]
- 34.Doyle EA, Quinn SM, Ambrosino JM, Weyman K, Tamborlane WV, Jastreboff AM. Disordered eating behaviors in emerging adults with type 1 diabetes: a common problem for both men and women. J Pediatr Health Care 2017;31:327–333 [DOI] [PubMed] [Google Scholar]
- 35.Mellin AE, Neumark-Sztainer D, Patterson J, Sockalosky J. Unhealthy weight management behavior among adolescent girls with type 1 diabetes mellitus: the role of familial eating patterns and weight-related concerns. J Adolesc Health 2004;35:278–289 [DOI] [PubMed] [Google Scholar]
- 36.Tester JM, Lang TC, Laraia BA. Disordered eating behaviours and food insecurity: a qualitative study about children with obesity in low-income households. Obes Res Clin Pract 2016;10:544–552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dostálová I, Smitka K, Papezová H, Kvasnicková H, Nedvídková J. Increased insulin sensitivity in patients with anorexia nervosa: the role of adipocytokines. Physiol Res 2007;56:587–594 [DOI] [PubMed] [Google Scholar]
- 38.Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, Daneman D. Disordered eating behavior and microvascular complications in young women with insulin-dependent diabetes mellitus. N Engl J Med 1997;336:1849–1854 [DOI] [PubMed] [Google Scholar]
- 39.Kichler JC, Moss A, Kaugars AS. Behavioral factors influencing health outcomes in youth with type 1 diabetes. US Endocrinol 2012;8:77–83 [Google Scholar]
- 40.Custal N, Arcelus J, Agüera Z, et al. Treatment outcome of patients with comorbid type 1 diabetes and eating disorders. BMC Psychiatry 2014;14:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.