ABSTRACT
Background: Trauma adjustment varies in children and adolescents. Studies on objective risk factors of posttraumatic stress symptoms (PTSS) yielded inconsistent results. Dysfunctional posttraumatic cognitions (PTCs) might play a mediating role between risk factors and posttraumatic symptomatology.
Objective: To investigate the interplay of the characteristics of the trauma (e.g. trauma type), the characteristics of the individual (e.g. age, sex), and the characteristics of the social environment (e.g. parental distress, marital status) on PTSS and depression, taking the child’s dysfunctional PTCs into account as a possible mediator.
Method: Structural equation modelling was used to better understand trauma adjustment in two heterogeneous samples of children and adolescents: a sample of 114 participants aged 7–16 after accidental trauma and a sample of 113 participants aged 6–17 after interpersonal trauma.
Results: In the accidental trauma sample, dysfunctional PTCs mediated the positive associations of younger age and lower parental educational level on child PTSS, but not on depression. In the interpersonal trauma sample, being female positively predicted child depression. Furthermore, parental dysfunctional PTCs positively predicted both child PTSS and depression. No mediation effect of child dysfunctional PTCs was found in the interpersonal trauma sample. Child dysfunctional PTCs moderately to strongly predicted child PTSS and depression in both trauma samples.
Conclusions: The impact of the characteristics of the individual and the characteristics of the social environment on child PTSS and depression might depend on the type of trauma experienced. Dysfunctional PTCs mediated between the characteristics of the individual and the characteristics of the social environment and the severity of PTSS in the aftermath of accidental trauma, but not of interpersonal trauma.
KEYWORDS: Accidental trauma, adolescents, children, depression, dysfunctional posttraumatic cognitions, interpersonal trauma, mediation, posttraumatic stress symptoms, structural equation modelling, trauma adjustment
HIGHLIGHTS
• Dysfunctional posttraumatic cognitions (PTCs) were associated with posttraumatic stress symptoms (PTSS) and depression.• In accidentally injured children, dysfunctional PTCs mediated between the characteristics of the individual and the characteristics of the social environment and the severity of PTSS.
Abstract
El ajuste del trauma varía en niños y adolescentes. Estudios sobre los factores de riesgo objetivos de los síntomas de estrés postraumático (PTSS) han arrojado resultados inconsistentes. Las cogniciones postraumáticas disfuncionales (PTCs) pueden desempeñar un rol mediador entre los factores de riesgo y la sintomatología postraumática.
Objetivo: Para investigar la interacción de las características del trauma (por ejemplo, tipo de trauma), las características del individuo (por ejemplo, edad, sexo) y las características del entorno social (por ejemplo, angustia de los padres, estado civil) en los PTSS y depresión, tomando en cuenta las PTCs disfuncionales del niño como un posible mediador.
Método: Se utilizó un modelo de ecuación estructural para una mejor comprensión del ajuste del trauma en dos muestras heterogéneas de niños y adolescentes: una muestra de 114 participantes de 7 a 16 años de edad después de un trauma accidental y una muestra de 113 participantes de 6 a 17 años de edad después de un trauma interpersonal.
Resultados: En la muestra de trauma accidental, las PTCs disfuncionales mediaron las asociaciones positivas de edades más jóvenes y más bajos niveles educacionales parentales en los PTSS infantiles, pero no en depresión. En la muestra de trauma interpersonal, ser mujer predijo positivamente la depresión infantil. Además, las PTCs disfuncionales de los padres predijeron positivamente tanto los PTSS infantiles como la depresión. No se encontró ningún efecto de mediación de las PTCs disfuncionales de los niños en la muestra de trauma interpersonal. Las PTCs disfuncionales infantiles predijeron, de manera moderada a robusta, los PTSS infantiles y la depresión en ambas muestras.
Conclusiones: El impacto de las características individuales y las características del entorno social en los PTSS infantiles y la depresión pueden depender del tipo de trauma experimentado. Las PTCs disfuncionales mediaron entre las características individuales y las características del entorno social y la severidad de los PTSS después de un trauma accidental, pero no tras un trauma interpersonal.
PALABRAS CLAVE: trauma accidental, adolescentes, niños, depresión, cogniciones postraumáticas disfuncionales, trauma interpersonal, mediación, síntomas de estrés postraumático, modelado de ecuaciones estructurales, ajuste de trauma
背景
背景:儿童和青少年的创伤适应过程不同。对创伤后应激症状(PTSS)的客观危险因素的研究得到不一致的结论。功能失调的创伤后认知(PTCs)可能在风险因素和创伤后症状学之间起中介作用。
目的:调查创伤特征(例如创伤类型),个体特征(例如年龄、性别)和社交环境特征(例如父母痛苦、婚姻状况)的交互作用对PTSS和抑郁的影响,将儿童功能失调的PTCs作为可能的中介变量。
方法:我们使用结构方程模型以便更好地理解两个儿童和青少年的异质样本中的创伤适应:114名年龄在7-16岁被试经历了意外创伤和113名年龄在6-17岁的被试经历了人际创伤。
结果:在意外创伤样本中,功能失调的PTCs中介了较小年轻和较低父母教育水平和儿童PTSS的正相关,但没有在抑郁症上发现。在人际创伤样本中,女性性别积极预测儿童抑郁症。此外,父母功能失调性PTCs正向预测儿童PTSS和抑郁症。在人际创伤样本中未发现儿童功能失调性PTCs的中介作用。儿童功能失调的PTCs中度到强烈地预测儿童PTSS和两种创伤样本中的抑郁症。
结论:个体特征和社会环境特征对儿童PTSS和抑郁的影响可能取决于所经历的创伤类型。功能失调的PTCs中介了个体的特征和社会环境的特征以及意外创伤后PTSS的严重程度,而在人际创伤中没有发现。
关键词: 意外创伤, 青少年, 儿童, 抑郁, 功能失调的创伤后认知, 人际创伤, 中介, 创伤后应激症状, 结构方程模型, 创伤适应
1. Background
A significant number of children and adolescents experience traumatic events (Copeland, Keeler, Angold, & Costello, 2007; Landolt, Schnyder, Maier, Schoenbucher, & Mohler-Kuo, 2013). Their trauma adjustment, however, varies greatly. Trauma models developed specifically for children and adolescents, such as the Developmental Psychopathology Model of Childhood Traumatic Stress by Pynoos, Steinberg, and Piacentini (1999) and the Transactional Model of Coping with Trauma by Landolt (2012), highlight the interplay of the characteristics of the trauma (e.g. trauma type), the characteristics of the individual (e.g. age, sex), and the characteristics of the social environment (e.g. parental distress, marital status) and include subjective appraisals and coping behaviour as mediators and/or direct predictors of posttraumatic symptomatology (see Figure 1).
Figure 1.
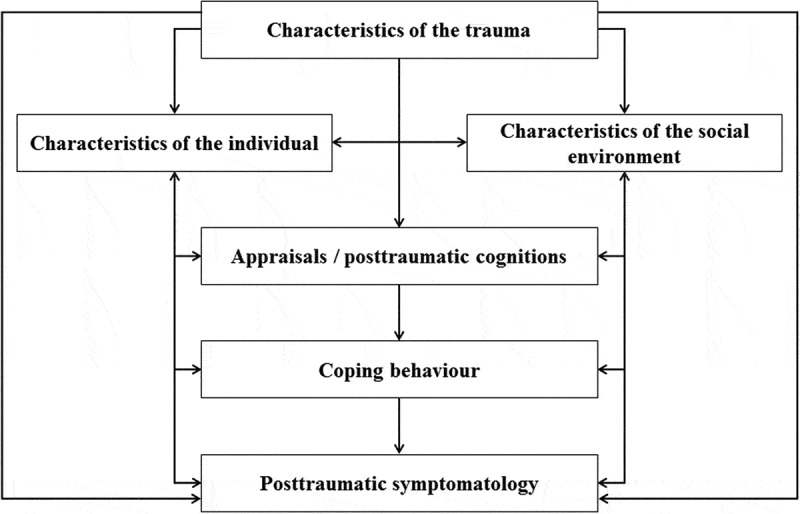
Transactional Model of Coping with Trauma Adapted from Landolt, 2012, p. 81.
Research studies have investigated a variety of possible predictors of trauma adjustment in children and adolescents. Characteristics of the trauma seem to play a role, including trauma type (Alisic et al., 2014, meta-analysis; Landolt et al., 2013), the dose–response relationship (Neuner et al., 2004), and the type of perpetrator (Milan, Zona, Acker, & Turcios-Cotto, 2013). Mixed results have been reported for trauma-related factors such as the objective severity of the traumatic event (Alisic, Jongmans, van Wesel, & Kleber, 2011, meta-analysis; Lavi, Green, & Dekel, 2013) and the child’s role in the traumatic event (Bayarri Fernàndez, Ezpeleta, Granero, de la Osa, & Domènech, 2011; Tierens et al., 2012). Characteristics of the individual have also been investigated. Female sex (Alisic et al., 2014, meta-analysis; Landolt et al., 2013; Trickey, Siddaway, Meiser-Stedman, Serpell, & Field, 2012, meta-analysis), previous traumatic events (Langley et al., 2013; Salazar, Keller, Gowen, & Courtney, 2013), and prior psychopathology have all emerged as risk factors (Alisic et al., 2011, meta-analysis; Cox, Kenardy, & Hendrikz, 2008, meta-analysis). Findings regarding age are inconsistent (Gunaratnam & Alisic, 2017; overview in book chapter). Characteristics of the social environment also play an important role. For example, the impact of parental psychological problems such as parental posttraumatic stress symptoms (PTSS) and depression yielded small to moderate effect sizes (Alisic et al., 2011, meta-analysis; Cox et al., 2008, meta-analysis; Landolt, Ystrom, Sennhauser, Gnehm, & Vollrath, 2012; Morris, Gabert-Quillen, & Delahanty, 2012, meta-analysis). Furthermore, parenting behaviours (Williamson et al., 2017, meta-analysis), parental dysfunctional posttraumatic cognitions (PTCs) (Hiller et al., 2018), poor family functioning, and low socio-economic status (SES; Trickey et al., 2012, meta-analysis) were found to be risk factors for child stress. However, social support might act as a protective factor (Langley et al., 2013).
Since objective trauma variables cannot satisfactorily explain differences in trauma adjustment, the role of subjective appraisals has become more central. Studies have found that subjective parameters may be more important in trauma adjustment than their objective counterparts (Trickey et al., 2012, meta-analysis). Variables that seem important include perceived control (Zhang, Liu, Jiang, Wu, & Tian, 2014), feelings of guilt (Haag, Zehnder, & Landolt, 2015; Kletter, Weems, & Carrion, 2009), and dysfunctional PTCs regarding one’s ongoing vulnerability (Bryant, Salmon, Sinclair, & Davidson, 2007; Mitchell, Brennan, Curran, Hanna, & Dyer, 2017, meta-analysis). Furthermore, dysfunctional PTCs regarding the traumatic event and its consequences might mediate between objective factors and psychological symptoms (Leeson & Nixon, 2011; Palosaari, Punamäki, Peltonen, Diab, & Qouta, 2016). This finding is in line with the Transactional Model of Coping with Trauma (Landolt, 2012), in which trauma-related appraisals and PTCs mediate between the characteristics of the trauma, the characteristics of the individual, and characteristics of the social environment on the one hand and the posttraumatic symptomatology on the other (see Figure 1).
Based on Landolt’s (2012) trauma model, we investigated whether characteristics of the individual and characteristics of the social environment impact child PTSS and depression, either directly or indirectly via the child’s dysfunctional PTCs, in two different trauma samples: one of children and adolescents after accidental trauma and the other of children and adolescents after interpersonal trauma. Coping with accidental trauma compared to interpersonal trauma might differ considerably. Furthermore, treating them as separate data sets provided us with the opportunity to compare the strength of associations across these different trauma types. In line with the Transactional Model of Coping with Trauma by Landolt (2012), we chose the following variables. Characteristics of the individual were represented by age at assessment, child sex, and trauma history. Characteristics of the social environment included demographic variables such as marital status and parental educational levels. Based on previous research that showed that parental dysfunctional PTCs (Hiller et al., 2018) and parental PTSS (Morris et al., 2012) played a role in their child’s trauma adjustment, we addressed these variables as characteristics of the social environment.
2. Methods
2.1. Procedure
Inclusion criteria for the current study were age between 6 and 17, exposure to a traumatic event meeting the posttraumatic stress disorder (PTSD). A criteria of DSM-IV or DSM-5, child’s and caregiver’s willingness to participate, and the informed consent of a legal guardian. Two samples were used. The Swiss sample consisted of 114 children and adolescents aged 7 to 16 years who had experienced accidental trauma such as a road traffic accident or burn injury. They participated in a longitudinal study called Dysfunctional Posttraumatic Cognitions in Children and Adolescents (PTC; NCT02693249). The assessment used in the current study took place three months after the incident. The German sample included 113 children and adolescents aged 6 to 17 years who had experienced interpersonal trauma, such as sexual abuse, sexual assault, physical violence, or witnessing domestic violence, at least three months before the study admission. They participated in the TreatChildTrauma study (TCT; NCT01516827). The data we used from the TCT study had all been collected pre-treatment (see Goldbeck, Muche, Sachser, Tutus, & Rosner, 2016, for more details of the study design). From the TCT study sample, we included only children and adolescents who reported the interpersonal trauma as index event. Nine of 122 participants were excluded, because their trauma experience did not meet DSM PTSD A criteria.
2.2. Measures
2.2.1. Child measures
The Child Posttraumatic Cognitions Inventory (CPTCI; Meiser-Stedman et al., 2009; German version de Haan, Petermann, Meiser-Stedman, & Goldbeck, 2016; accidental sample Cronbach’s α = .83; interpersonal sample Cronbach’s α = .92) consists of 25 items divided into two subscales: the Permanent and disturbing change subscale (CPTCI-PC) and the Fragile person in a scary world subscale (CPTCI-SW). Items are rated from 1 (don’t agree at all) to 4 (agree a lot). Examples are ‘My reactions since the frightening event mean I have changed for the worse’ (CPTCI-PC item) or ‘I can’t stop bad things from happening to me’ (CPTCI-SW item).
PTSS and trauma history were assessed with the University of California at Los Angeles Post-Traumatic Stress Disorder Reaction Index for Children/Adolescents (UCLA-RI; Steinberg, Brymer, Decker, & Pynoos, 2004; interpersonal sample Cronbach’s α = 0.80). We administered the DSM-5 version to the accidental sample (Pynoos & Steinberg, 2013; authorized German version by Landolt, 2014; Cronbach’s α = 0.84). The items are rated on a 5-point scale from 0 (none of the time) to 4 (most of the time). In the interpersonal sample, trauma history was assessed with the DSM-IV Clinician-Administered PTSD Scale for Children and Adolescents (CAPS-CA; Nader et al., 1996; German version Füchsel & Steil, 2006). If more than one traumatic event was reported, the child was asked to identify the ‘worst’ or most upsetting event. This event was referred to when assessing dysfunctional PTCs and PTSS.
The Children’s Depression Inventory (CDI; Kovacs, 1985) was applied to assess the presence and severity of depression symptoms. We used the third German edition (Stiensmeier-Pelster, Braune-Krickau, Schürmann, & Duda, 2014; Cronbach’s α = .85) for the accidental sample and the second German edition (Stiensmeier-Pelster, Schürmann, & Duda, 2000; Cronbach’s α = .90) for the interpersonal sample.
2.2.2. Caregiver questionnaires
The Post-Traumatic Cognitions Inventory (PTCI; Foa, Ehlers, Clark, Tolin, & Orsillo, 1999; accidental sample Cronbach’s α = .89; interpersonal sample Cronbach’s α = .95) was administered to the caregiver to rate his or her own dysfunctional PTCs related to the child’s trauma, as in Nixon, Sterk, and Pearce (2012). Furthermore, the caregiver’s PTSS were assessed with German version of the Posttraumatic Diagnostic Scale (PDS; Ehlers, Steil, Winter, & Foa, 1996; interpersonal sample Cronbach’s α = .92). We used the DSM-5 version for the accidental sample (Foa et al., 2016; Cronbach’s α = .88), translated into German.
2.3. Caregiver characteristics and missing data
Values were missing from caregiver questionnaires predominantly due to non-German speaking parents or because the children were accompanied by foster parents or child welfare service staff. Questionnaire respondents were biological parents, predominately mothers (accidental trauma sample n = 78, 91.8%; interpersonal trauma sample n = 65, 87.8%). In one case it was a female relative. Therefore, the terms parental PTCs and parental PTSS were used in the result section. A negligible number of child questionnaires was missing (see Table 2 and Supplementary Table S1 for specific information).
Table 2.
Comparison of measures (mean, SD, range) between the Swiss accidental and German interpersonal trauma samples.
| Accidental N = 114 |
Interpersonal N = 113 |
|||||
|---|---|---|---|---|---|---|
| Item range | M (SD) | n | M (SD) | n | Statistics | |
| CPTCI item mean | 1–4 | 1.36 (0.33) | 109 | 2.35 (0.63) | 111 |
t(166.5) = −14.56, p < .001 |
| UCLA-RI item mean | 0–4 | 0.59 (0.51) | 110 | 2.20 (0.64) | 110 |
t(206.8) = −20.62, p < .001 |
| CDI item mean | 0–2 | 0.21 (0.18) | 105 | 0.78 (0.37) | 111 |
t(162.4) = −14.41, p < .001 |
| PTCI item mean | 1–7 | 1.47 (0.53) | 85 | 2.74 (1.07) | 74 |
t(103.0) = −9.21, p < .001 |
| PDS item mean | 0–3 | 0.17 (0.26) | 76 | 0.88 (0.66) | 67 |
t(83.7) = −8.28, p < .001 |
Note. CPTCI = Child Post-Traumatic Cognitions Inventory; UCLA-RI = University of California at Los Angeles Post-Traumatic Stress Disorder Reaction Index; CDI = Child Depression Inventory; PTCI = Post-Traumatic Cognitions Inventory; PDS = Posttraumatic Diagnostic Scale.
2.4. Data analyses
Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS, version 22.0; IBM-Corp, 2013) and Mplus (version 8.1; Muthén & Muthén, 1998–2018). Statistical significance was established at an alpha level of .05. To compare PTSS and depression scores resulting from different versions of the same measures, the item means were calculated and used in the analyses. For every questionnaire, data were imputed at item level up to 20% missing values per questionnaire using the subscale mean. Data missing from total scores in the structural equation modelling (SEM) were handled with Full Information Maximum Likelihood (FIML). We used the Maximum Likelihood estimator (ML) with bootstrapping. The predictor variables were either obtained from demographic data (age at assessment, child sex, marital status, parental education) or via questionnaires (trauma load, parental PTCs, parental PTSS). Correlation paths were defined between (a) the characteristics of the individual and characteristics of the social environment and (b) between the dependent variables child PTSS and depression. Indirect and direct effects were calculated to investigate the potential mediation effect of child dysfunctional PTCs. SEMs were calculated for both subsamples separately. We calculated z-tests to test whether significant parameters in both samples were equal to each other using the model constraint command in Mplus. Since we calculated a saturated model, no model fit indices could be reported or compared.
3. Results
3.1. Sample characteristics
Both samples differed significantly from each other with regard to demographic and trauma-related characteristics (see Table 1). Participants from the interpersonal trauma sample reported a significantly higher amount of trauma types experienced and a predominately multi-type trauma history. Descriptive information about the measures and clinically relevant cut-offs as well as the percentage of each sample who met a PTSD diagnosis can be found in Supplementary Table S1. Table 2 describes item means and standard deviations for the child and parental dysfunctional PTCs and psychological symptoms included in the SEMs. Supplementary Tables S2 and S3 display the pairwise bivariate Spearman correlations for all variables, separated into the accidental and the interpersonal trauma sample.
Table 1.
Sociodemographic data and trauma-related information of the Swiss accidental and German interpersonal trauma samples.
| Accidental N = 114 |
Interpersonal N = 113 |
||||
|---|---|---|---|---|---|
| Characteristics | M or n | SD or % | M or n | SD or % | Statistics |
| Age, years at assessment | 10.75 | 2.55 | 12.98 | 2.77 | t(225) = −6.31, |
| p < .001 | |||||
| Sex | |||||
| Male | 64 | 56.1 | 33 | 29.2 | χ2(1) = 16.83, |
| Female | 50 | 43.9 | 80 | 70.8 | p < .001 |
| Living situation | |||||
| With both | 84 | 73.7 | 25 | 22.1 | χ2(2) = 79.75, |
| biological parents | p < .0 01 | ||||
| With one biological parent | 19 | 16.7 | 57 | 50.4 | |
| Other relatives, foster care etc. | – | – | 29 | 25.7 | |
| Not determineda | 11 | 9.6 | 2 | 1.8 | |
| Educational level mother | |||||
| No obligatory | 3 | 2.6 | 8 | 7.1 | χ2(3) = 62.20, |
| Obligatory | 4 | 3.5 | 32 | 28.3 | p < .001 |
| Medium | 25 | 21.9 | 30 | 26.5 | |
| Higher | 72 | 63.2 | 14 | 12.4 | |
| Not determineda | 10 | 8.8 | 29 | 25.7 | |
| Educational level father | |||||
| No obligatory | – | – | 3 | 2.7 | χ2(3) = 52.75, |
| Obligatory | 5 | 4.4 | 25 | 22.1 | p < .001 |
| Medium | 16 | 14.0 | 25 | 22.1 | |
| Higher | 76 | 66.7 | 17 | 15.0 | |
| Not determineda | 17 | 14.9 | 43 | 38.1 | |
| Trauma history | |||||
| Single trauma type | 81 | 71.1 | 13 | 11.5 | χ2(1) = 85.53, |
| Multiple trauma types | 31 | 27.2 | 100 | 88.5 | p < .001 |
| Not determineda | 2 | 1.8 | – | – | |
| Number of trauma types | 1.53 | 1.11 | 3.65 | 1.85 | t(184.1) = −10.41, |
| p < .001 | |||||
Note. aNot determined: these participants could not be reliably classified in any category due to insufficient information.
3.2. Structural equation modelling
In the accidental trauma sample, the indirect path from age at assessment via child dysfunctional PTCs to child PTSS was significant (b = −.261, p < .001). The direct path between age at assessment and child PTSS was not (b = .017, p = .800), which confirmed a mediation effect of child dysfunctional PTCs. The same pattern emerged for parental education: The indirect paths from parental education via child PTCs to child PTSS was significant (b = −.181, p = .013), but the direct path from parental education to child PTSS was not (b = −.013, p = .847). Since neither age at assessment nor parental education predicted child depression, a mediation effect was not investigated (see Baron & Kenny, 1986). Figure 2 displays the significant paths in the accidental trauma sample.
Figure 2.
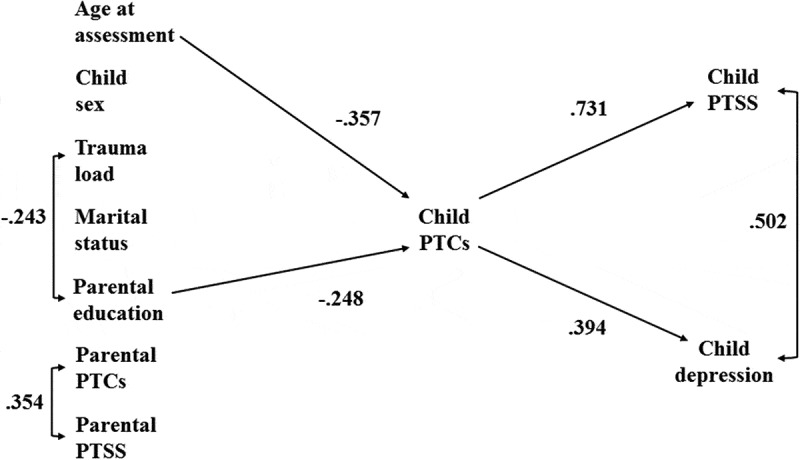
Cross-sectional associations for the accidental trauma sample.
PTCs = dysfunctional posttraumatic cognitions. PTSS = posttraumatic stress symptoms. Trauma load displays the number of trauma types experienced. The parental educational level is the mean of the individual maternal and paternal educational levels. If this information was only available for one parent, his or her value was used as the parental educational level. Standardized coefficients are reported. Only significant paths are displayed. The model accounted for 56.9% (R2 = .569, p < .001) of the variance in child PTSS, 26.5% (R2 = .265, p = .003) of the variance in child depression, and 22.9% (R2 = .229, p = .010) of the variance in child dysfunctional PTCs.
In the interpersonal trauma sample, none of the child or social characteristics predicted child dysfunctional PTCs. However, direct paths to PTSS and depression were found (see Figure 3).
Figure 3.
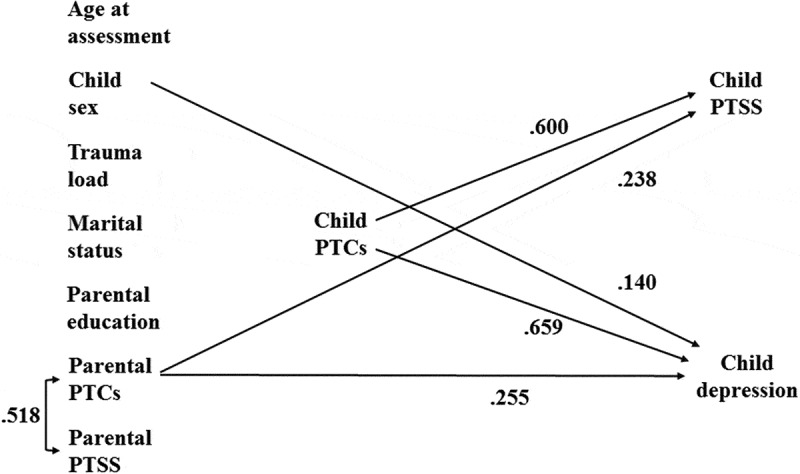
Cross-sectional associations for the interpersonal trauma sample.
PTCs = dysfunctional posttraumatic cognitions. PTSS = posttraumatic stress symptoms. Trauma load displays the number of trauma types experienced. The parental educational level is the mean of the individual maternal and paternal educational levels. If this information was only available for one parent, his or her value was used as the parental educational level. Standardized coefficients are reported. Only significant paths are displayed. The model accounted for 47.2% (R2 = .472, p < .001) of the variance in child PTSS, 60.2% (R2 = .602, p < .001) of the variance in child depression, and 12.3% (R2 = .123, p = .093) of the variance in child dysfunctional PTCs.
3.3. Group comparison
We compared the groups in regard to the paths that had emerged as significant in one or both samples. A significant difference between the samples emerged for the regressive paths of age at assessment on child dysfunctional PTCs (unstandardized b = −0.080, p = .002). In the accidental trauma sample, younger age was associated with more dysfunctional PTCs of the child. In the interpersonal trauma sample, age emerged as nonsignificant (b = .146, p = .129). Furthermore, the regressive paths from child dysfunctional PTCs to child PTSS and child depression differed significantly in both samples (PTCs to PTSS: unstandardized b = 0.517, p = .005; PTCs to depression: unstandardized b = −0.166, p = .031). This means that child dysfunctional PTCs predicted PTSS significantly more strongly in the accidental trauma sample, while child dysfunctional PTCs predicted depression significantly more strongly in the interpersonal trauma sample. The correlation between parental PTCs and parental PTSS differed significantly between samples (unstandardized r = −0.316, p = .001). In the interpersonal trauma sample, parental PTCs and PTSS correlated significantly more strongly than in the accidental trauma sample.
4. Discussion
We investigated the role of the characteristics of the trauma, the characteristics of the individual, and the characteristics of the social environment, and dysfunctional PTCs on trauma adjustment in two international trauma samples of children and adolescents representing frequent types of trauma exposure, accidental injuries and interpersonal violence, using SEM. In line with the current state of research, we found mixed results. In the accidental trauma sample, dysfunctional PTCs mediated the positive associations of younger age and lower parental educational level on child PTSS but not on depression. In the interpersonal trauma sample, being female positively predicted child depression. Furthermore, parental dysfunctional PTCs positively predicted both child PTSS and depression. Child dysfunctional PTCs positively predicted child PTSS and depression moderately to strongly in both trauma samples. Notably, differences between samples might be due not only to trauma type but also to variables such as time since trauma, presence of acute or chronic PTSD, and complexity of trauma history.
The significant difference between samples in association between age at assessment and dysfunctional PTCs has several possible explanations. (1) The role of age might be confounded with trauma type. Trickey et al. (2012) found a significantly stronger relationship between younger age in children and adolescents and PTSD when the index trauma was unintentional than when it was intentional. (2) Trauma history might play a role. For younger participants, the trauma event they reported might have been their first traumatic experience ever. Janoff-Bulman (1985) suggests that such trauma might shatter positive pre-trauma schemata about the self (the self is worthy) and about the world (the world is benevolent; the world is meaningful). Furthermore, younger children often have a more self-centred perspective. Experiencing loss of control might encourage misconceptions about their own abilities and the world around them. (3) A methodological reason might also explain these findings. The samples differed in the time since the index event had occurred. In the Swiss sample, the accident had happened three months before the assessment. Therefore, age at accident and age at assessment were broadly the same. In the German sample, the interpersonal trauma had happened at least three months before the study admission; in some cases, then, the traumatic event might have happened years ago.
The impact of child sex on PTSS and depression also differed between samples. The divergent findings might be explained by differences in age between the samples. The participants of the interpersonal trauma sample had a mean age of 13 years. Being female positively predicted child depression in this sample, in line with studies showing depression to be more frequent in females than males from 12 years and peaking between 13 and 15 years (Salk, Hyde, & Abramson, 2017). Notably, although significant, the effect was weak. The younger mean age of the accidental trauma sample might explain why they exhibited no sex differences in depression. Surprisingly, we did not find a sex effect for PTSS in either of the samples, which contradicts findings from recent meta-analyses (Alisic et al., 2014; Trickey et al., 2012). However, our finding might support Tolin and Foa’s (2002) assumption that trauma type needs to be considered when assessing the impact of sex. However, Landolt et al. (2013) controlled for trauma types and still found higher prevalence in females.
Characteristics of the social environment emerged as predictors for child PTSS and depression. Mediated by child dysfunctional PTCs, lower parental education was associated with more child PTSS after accidental trauma. This finding is in line with Trickey et al.’s (2012) finding that low SES is a general risk factor for child PTSD. Furthermore, Landolt et al. (2013) reported that children from families with lower parental education had a higher risk of PTSD; they concluded that children from families with lower educational level or SES might have fewer resources for dealing with traumatic events.
In line with the Transactional Model of Coping with Trauma (Landolt, 2012) and previous research that has shown that parental responses to trauma play a role in their child`s trauma adjustment, we included them as characteristics of the social environment: More parental dysfunctional PTCs were associated with a higher level of PTSS and depression in their children after interpersonal trauma. The same pattern was reported in two longitudinal studies with children after acute severe injuries (Hiller et al., 2018) and mixed trauma experiences (Nixon et al., 2012). Dysfunctional PTCs in parents might lead to a more overprotective parenting style, less child autonomy, and more communication about current threat possibilities (Cobham & McDermott, 2014), which might hinder child trauma adjustment. Conversely, parental PTSS did not impact child dysfunctional PTCs, PTSS, or depression in either of the samples. The same cross-sectional finding was reported by Landolt et al. (2012) and Palosaari et al. (2016), but it contrasts with de Vries et al. (1999) and Egberts, van de Schoot, Geenen, and Van Loey (2018), who found significant parental–child associations. Methodological considerations might explain these differing findings (self- vs. proxy-report; interview vs. questionnaire). However, we found parental dysfunctional PTCs regarding their child’s traumatic experience and parental PTSS to be significantly correlated in both trauma types, in line with Hiller et al. (2018). Two explanations are possible: (1) Witnessing a traumatic event and learning that a relative or close friend was exposed to a trauma both meet the PTSD A criteria (APA, 2013). Thus, parents may also develop PTSS related to their child’s trauma; (2) The dose–response relationship implies that current trauma may re-activate, trigger, or strengthen past trauma experience. Thus, parents with a trauma history might be at higher risk of developing dysfunctional PTCs regarding their child’s traumatic experience, which then impact the child’s psychological symptoms.
Child dysfunctional PTCs were a moderate to strong predictor of child PTSS and depression after controlling for characteristics of the individual and characteristics of the social environment in both trauma samples; this confirms their overarching importance in trauma adjustment. Their minor role in mediating between child and social environmental factors and PTSS and depression may indicate that dysfunctional PTCs are important in children and adolescents, irrespective of specific characteristics of the trauma, characteristics of the individual, and characteristics of the social environment. However, the impact of child’s dysfunctional PTCs on PTSS and depression differed between the two samples; it predicted PTSS significantly more strongly in the accidental sample and depression significantly more strongly in the interpersonal trauma sample. Note that in the accidental trauma sample, PTSS was assessed according to DSM-5 criteria, which include items regarding negative alternations in cognitions and mood. The specificity of dysfunctional PTCs’ effects on PTSS or depression has been investigated before (Ehring, Ehlers, & Glucksman, 2006; Meiser-Stedman et al., 2009). Our findings contribute the novel finding that the specificity might actually depend on the trauma type. The CPTCI assesses dysfunctional PTCs regarding being permanently and disturbingly changed and feeling like a fragile person in a scary world. This content might be more closely related to PTSS following accidental trauma. In interpersonal trauma, cognitions linked to humiliation, shame, and self-blame seem also to be of high importance for PTSS (Beck et al., 2015; Kletter et al., 2009), however, these latter are not assessed by the CPTCI.
Surprisingly, child PTSS and child depression were not significantly correlated in the interpersonal sample. However, this finding is in line with Palosaari et al. (2016), who did not find a significant association between child depression and PTSS in their mediation model either. They assumed that the association between child depression and PTSS might be explained by their common connection to child dysfunctional PTCs.
In sum, differences emerged between the trauma samples in the variables that impact the child’s PTSS and depression symptoms and, related to this, in the mediating role of the child’s dysfunctional PTCs. These mixed findings support the Transactional Model of Coping with Trauma (Landolt, 2012), which highlights the fact that individual and social environmental factors in various combinations impact the posttraumatic symptomatology of the child both directly and mediated by dysfunctional PTCs. This includes the interaction of diverse risk and protective factors. Indeed, the number of trauma types experienced by the child correlated significantly with parental educational level in the accidental trauma sample. Several studies have described the same finding (e.g. Perkonigg, Kessler, Storz, & Wittchen, 2000). Morrongiello and House (2004), for example, suggest that young children in lower SES households are at higher risk of traumatic injuries due to less supervision.
Our findings have several implications for practice and research. The mixed findings regarding the role of the characteristics of the individual and the characteristics of the social environment in two different trauma samples make clear that screening for PTSS and depression should be common practice in every psychological assessment, irrespectively of specific trauma, child, or social environmental characteristics. Child dysfunctional PTCs emerged as an important predictor of child PTSS and depression and thus may be a good starting point for assessing and monitoring posttraumatic symptomatology. Studies showed that they are malleable through therapy and constitute an important target for change (e.g. Meiser-Stedman et al., 2017). Younger age should not be neglected as a risk factor after accidental trauma. Furthermore, parental distress in the form of dysfunctional PTCs and PTSS should be considered, whether the parents were directly involved in the trauma or not (Hiller et al., 2016). Future research should use longitudinal studies focusing on the causal relationships between dysfunctional PTCs and posttraumatic symptomatology to further validate the Transactional Model of Coping with Trauma (Landolt, 2012).
4.1. Limitations
Strengths of our study included using two international trauma samples and advanced statistical methods. Nevertheless, several limitations warrant note when interpreting our findings. Although the studies differed in index event (accidental vs interpersonal trauma), individual trauma histories might overlap. For example, one-quarter of the accidental trauma sample had previously experienced another type of trauma, thus perhaps influencing PTSS, depression, and dysfunctional PTCs. As discussed above, time since trauma also differed between samples. The participants of the accidental trauma sample were assessed around three months after the accident, but the interpersonal trauma sample varied regarding this variable, so in some cases the traumatic event might have happened years ago. This could mean that the differences we found were not mainly due to the trauma types but to time since trauma and/or chronic exposure to trauma and the presence of chronic PTSD symptoms in the interpersonal trauma sample. Furthermore, the participants in the interpersonal trauma sample were all treatment-seeking, whereas the accidental trauma sample took part in an observational study. It is therefore possible that participants differed in expectancies regarding both studies, which might have led to differences in their answering behaviour.
Child posttraumatic symptomatology is often assessed by parental report, but parents might over- or underestimate their children’s symptoms. We therefore used child self-reports. However, each study conducted its child assessments differently: in the Swiss accidental trauma sample, the child was interviewed; in the German interpersonal trauma sample, the child completed a written questionnaire. Furthermore, the caregiver reports were mainly given by biological mothers. Including both maternal and paternal distress might have given a broader insight into the social environment of the child.
Moreover, it is important to keep in mind that our study had a cross-sectional design. Conclusions concerning causal directions can therefore not be drawn from our findings. Although the sample size for each group was adequate for SEM, the samples were not very large and it is therefore still possible that some pathways were non-significant because analyses were under-powered. Furthermore, due to a saturated model, no model fit indices could be reported or compared. Lastly, widely established requirements for calculating mediator analyses were applied (see Baron & Kenny, 1986). However, newer studies also suggest drawing conclusions from inconsistent mediation models or suppressor effects (e.g. MacKinnon, Fairchild, & Fritz, 2007; Paulhus, Robins, Trzesniewski, & Tracy, 2004).
5. Conclusions
The impact of the characteristics of the individual and the characteristics of the social environment on child PTSS and depression might depend on the type of trauma experienced. Risk factors should not be seen as independent but as intertwined with each other. Child dysfunctional PTCs may mediate the association between risk factors and child posttraumatic symptomatology. Parental dysfunctional PTCs regarding their child’s traumatic event need to be considered when assessing and treating families after child trauma (see Hiller et al., 2016).
Supplementary Material
Acknowledgments
The authors want to thank the participating children and their caregivers. Furthermore, we are thankful to everyone who was involved in data collection.
Data availability statement
Given that the ethical committees agree, the datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Alisic E., Jongmans M. J., van Wesel F., & Kleber R. J. (2011). Building child trauma theory from longitudinal studies: A meta-analysis. Clinical Psychology Review, 31, 736–11. [DOI] [PubMed] [Google Scholar]
- Alisic E., Zalta A. K., van Wesel F., Larsen S. E., Hafstad G. S., Hassanpour K., & Smid G. E. (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. British Journal of Psychiatry, 204, 335–340. [DOI] [PubMed] [Google Scholar]
- APA (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Baron R. M., & Kenny D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Bayarri Fernàndez E., Ezpeleta L., Granero R., de la Osa N., & Domènech J. M. (2011). Degree of exposure to domestic violence, psychopathology, and functional impairment in children and adolescents. Journal of Interpersonal Violence, 26, 1215–1231. [DOI] [PubMed] [Google Scholar]
- Beck J. G., Reich C. M., Woodward M. J., Olsen S. A., Jones J. M., & Patton S. C. (2015). How do negative emotions relate to dysfunctional posttrauma cognitions? An examination of interpersonal trauma survivors. Psychological Trauma: Theory, Research, Practice, and Policy, 7, 3–10. [DOI] [PubMed] [Google Scholar]
- Bryant R. A., Salmon K., Sinclair E., & Davidson P. (2007). A prospective study of appraisals in childhood posttraumatic stress disorder. Behaviour Research and Therapy, 45, 2502–2507. [DOI] [PubMed] [Google Scholar]
- Cobham V. E., & McDermott B. (2014). Perceived parenting change and child posttraumatic stress following a natural disaster. Journal of Child and Adolescent Psychopharmacology, 24, 18–23. [DOI] [PubMed] [Google Scholar]
- Copeland W. E., Keeler G., Angold A., & Costello E. J. (2007). Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry, 64, 577–584. [DOI] [PubMed] [Google Scholar]
- Cox C. M., Kenardy J. A., & Hendrikz J. K. (2008). A meta-analysis of risk factors that predict psychopathology following accidental trauma. Journal for Specialists in Pediatric Nursing, 13, 98–110. [DOI] [PubMed] [Google Scholar]
- de Haan A., Petermann F., Meiser-Stedman R., & Goldbeck L. (2016). Psychometric properties of the German version of the Child Post-Traumatic Cognitions Inventory (CPTCI-GER). Child Psychiatry & Human Development, 47, 151–158. [DOI] [PubMed] [Google Scholar]
- de Vries A. P., Kassam-Adams N., Cnaan A., Sherman-Slate E., Gallagher P. R., & Winston F. K. (1999). Looking beyond the physical injury: Posttraumatic stress disorder in children and parents after pediatric traffic injury. Pediatrics, 104, 1293–1299. [DOI] [PubMed] [Google Scholar]
- Egberts M. R., van de Schoot R., Geenen R., & Van Loey N. E. E. (2018). Mother, father and child traumatic stress reactions after paediatric burn: Within-family co-occurrence and parent-child discrepancies in appraisals of child stress. Burns, 44, 861–869. [DOI] [PubMed] [Google Scholar]
- Ehlers A., Steil R., Winter H., & Foa E. B. (1996). Deutschsprachige Übersetzung der Posttraumatic Diagnostic Scale von Foa (1995). Oxford: Department of Psychiatry, Warneford Hospital. [Google Scholar]
- Ehring T., Ehlers A., & Glucksman E. (2006). Contribution of cognitive factors to the prediction of post-traumatic stress disorder, phobia and depression after motor vehicle accidents. Behaviour Research and Therapy, 44, 1699–1716. [DOI] [PubMed] [Google Scholar]
- Foa E. B., Ehlers A., Clark D., Tolin D., & Orsillo S. (1999). The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment, 11, 303–314. [Google Scholar]
- Foa E. B., McLean C. P., Zang Y., Zhong J., Powers M. B., Kauffman B. Y., … Knowles K. (2016). Psychometric properties of the posttraumatic diagnostic scale for DSM-5 (PDS-5). Psychological Assessment, 28(10), 1166–1171. [DOI] [PubMed] [Google Scholar]
- Füchsel G., & Steil R. (2006). Interviews zu Belastungsstörungen bei Kindern und Jugendlichen: IBS-KJ; Diagnostik der akuten und der posttraumatischen Belastungsstörung; Manual. Göttingen: Hogrefe. [Google Scholar]
- Goldbeck L., Muche R., Sachser C., Tutus D., & Rosner R. (2016). Effectiveness of trauma-focused cognitive behavioral therapy for children and adolescents: A randomized controlled trial in eight German mental health clinics. Psychotherapy and Psychosomatics, 85, 159–170. [DOI] [PubMed] [Google Scholar]
- Gunaratnam S., & Alisic E. (2017). Epidemiology of trauma and trauma-related disorders in children and adolescents In Landolt M. A., Cloitre M., & Schnyder U. (Eds.), Evidence-based treatments for trauma related disorders in children and adolescents (pp. 29–47). Cham: Springer International Publishing. [Google Scholar]
- Haag A.-C., Zehnder D., & Landolt M. A. (2015). Guilt is associated with acute stress symptoms in children after road traffic accidents. European Journal of Psychotraumatology, 6, 29074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiller R. M., Halligan S. L., Ariyanayagam R., Dalgleish T., Smith P., Yule W., … Meiser-Stedman R. (2016). Predictors of posttraumatic stress symptom trajectories in parents of children exposed to motor vehicle collisions. Journal of Pediatric Psychology, 41, 108–116. [DOI] [PubMed] [Google Scholar]
- Hiller R. M., Meiser-Stedman R., Lobo S., Creswell C., Fearon P., Ehlers A., … Halligan S. L. (2018). A longitudinal investigation of the role of parental responses in predicting children’s post-traumatic distress. Journal of Child Psychology and Psychiatry, 59, 781–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM-Corp (2013). IBM SPSS statistics for windows, version 22.0. Armonk, NY: IBM Corp. [Google Scholar]
- Janoff-Bulman R. (1985). The aftermath of victimization: Rebuilding shattered assumptions In Figley C. R. (Ed.), Trauma and its wake: The study and treatment of post-traumatic stress disorder (pp. 15–35). New York, NY: Brunner/Mazel. [Google Scholar]
- Kletter H., Weems C. F., & Carrion V. G. (2009). Guilt and posttraumatic stress symptoms in child victims of interpersonal violence. Clinical Child Psychology and Psychiatry, 14, 71–83. [DOI] [PubMed] [Google Scholar]
- Kovacs M. (1985). The children’s depression inventory (CDI). Psychopharmacology Bulletin, 21, 995–998. [PubMed] [Google Scholar]
- Landolt M. A. (2012). Psychotraumatologie des Kindesalters: Grundlagen, Diagnostik und Interventionen (2nd ed.). Göttingen: Hogrefe. [Google Scholar]
- Landolt M. A. (2014). UCLA PTSD Reaction Index for Children/Adolescents: DSM-5 (German version). Zurich: University Childrens Hospital Zurich. [Google Scholar]
- Landolt M. A., Schnyder U., Maier T., Schoenbucher V., & Mohler-Kuo M. (2013). Trauma exposure and posttraumatic stress disorder in adolescents: A national survey in Switzerland. Journal of Traumatic Stress, 26, 209–216. [DOI] [PubMed] [Google Scholar]
- Landolt M. A., Ystrom E., Sennhauser F. H., Gnehm H. E., & Vollrath M. E. (2012). The mutual prospective influence of child and parental post-traumatic stress symptoms in pediatric patients. Journal of Child Psychology and Psychiatry, 53, 767–774. [DOI] [PubMed] [Google Scholar]
- Langley A. K., Cohen J. A., Mannarino A. P., Jaycox L. H., Schonlau M., Scott M., … Gegenheimer K. L. (2013). Trauma exposure and mental health problems among school children 15 months post-hurricane Katrina. Journal of Child & Adolescent Trauma, 6, 143–156. [Google Scholar]
- Lavi T., Green O., & Dekel R. (2013). The contribution of personal and exposure characteristics to the adjustment of adolescents following war. Journal of Adolescence, 36, 21–30. [DOI] [PubMed] [Google Scholar]
- Leeson F. J., & Nixon R. D. V. (2011). The role of children’s appraisals on adjustment following psychological maltreatment: A pilot study. Journal of Abnormal Child Psychology, 39, 759–771. [DOI] [PubMed] [Google Scholar]
- MacKinnon D. P., Fairchild A. J., & Fritz M. S. (2007). Mediation analysis. Annual Review of Psychology, 58, 593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiser-Stedman R., Smith P., Bryant R., Salmon K., Yule W., Dalgleish T., & Nixon R. D. V. (2009). Development and validation of the child post-traumatic cognitions inventory (CPTCI). Journal of Child Psychology and Psychiatry, 50, 432–440. [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman R., Smith P., McKinnon A., Dixon C., Trickey D., Ehlers A., … Dalgleish T. (2017). Cognitive therapy as an early treatment for post-traumatic stress disorder in children and adolescents: A randomized controlled trial addressing preliminary efficacy and mechanisms of action. Journal of Child Psychology and Psychiatry, 58(5), 623–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milan S., Zona K., Acker J., & Turcios-Cotto V. (2013). Prospective risk factors for adolescent PTSD: Sources of differential exposure and differential vulnerability. Journal of Abnormal Child Psychology, 41, 339–353. [DOI] [PubMed] [Google Scholar]
- Mitchell R., Brennan K., Curran D., Hanna D., & Dyer K. F. (2017). A meta‐analysis of the association between appraisals of trauma and posttraumatic stress in children and adolescents. Journal of Traumatic Stress, 30, 88–93. [DOI] [PubMed] [Google Scholar]
- Morris A., Gabert-Quillen C., & Delahanty D. (2012). The association between parent PTSD/depression symptoms and child PTSD symptoms: A meta-analysis. Journal of Pediatric Psychology, 37, 1076–1088. [DOI] [PubMed] [Google Scholar]
- Morrongiello B. A., & House K. (2004). Measuring parent attributes and supervision behaviors relevant to child injury risk: Examining the usefulness of questionnaire measures. Injury Prevention, 10, 114–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., & Muthén B. O. (1998–2018). Mplus user’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nader K., Kriegler J. A., Blake D. D., Pynoos R. S., Newman E., & Weathers F. W. (1996). Clinician-administered PTSD scale, child and adolescent version. White River Junction, VT: National Center for PTSD. [Google Scholar]
- Neuner F., Schauer M., Karunakara U., Klaschik C., Robert C., & Elbert T. (2004). Psychological trauma and evidence for enhanced vulnerability for posttraumatic stress disorder through previous trauma among West Nile refugees. BMC Psychiatry, 4, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nixon R. D. V., Sterk J., & Pearce A. (2012). A randomized trial of cognitive behaviour therapy and cognitive therapy for children with posttraumatic stress disorder following single-incident trauma. Journal of Abnormal Child Psychology, 40, 327–337. [DOI] [PubMed] [Google Scholar]
- Palosaari E., Punamäki R.-L., Peltonen K., Diab M., & Qouta S. R. (2016). Negative social relationships predict posttraumatic stress symptoms among war-affected children via posttraumatic cognitions. Journal of Abnormal Child Psychology, 44, 845–857. [DOI] [PubMed] [Google Scholar]
- Paulhus D. L., Robins R. W., Trzesniewski K. H., & Tracy J. L. (2004). Two replicable suppressor situations in personality research. Multivariate Behavioral Research, 39, 303–328. [DOI] [PubMed] [Google Scholar]
- Perkonigg A., Kessler R. C., Storz S., & Wittchen H. U. (2000). Traumatic events and post-traumatic stress disorder in the community: Prevalence, risk factors and comorbidity. Acta Psychiatrica Scandinavica, 101, 46–59. [DOI] [PubMed] [Google Scholar]
- Pynoos R. S., & Steinberg A. M. (2013). UCLA PTSD reaction index for children/adolescents – DSM-5. Los Angeles, CA: University of California. [Google Scholar]
- Pynoos R. S., Steinberg A. M., & Piacentini J. C. (1999). A developmental psychopathology model of childhood traumatic stress and intersection with anxiety disorders. Biological Psychiatry, 46, 1542–1554. [DOI] [PubMed] [Google Scholar]
- Salazar A. M., Keller T. E., Gowen L. K., & Courtney M. E. (2013). Trauma exposure and PTSD among older adolescents in foster care. Social Psychiatry and Psychiatric Epidemiology, 48, 545–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk R. H., Hyde J. S., & Abramson L. Y. (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin, 143, 783–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg A. M., Brymer M. J., Decker K. B., & Pynoos R. S. (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports, 6, 96–100. [DOI] [PubMed] [Google Scholar]
- Stiensmeier-Pelster J., Braune-Krickau M., Schürmann M., & Duda K. (2014). Depressionsinventar für Kinder und Jugendliche (3rd ed.). Göttingen: Hogrefe. [Google Scholar]
- Stiensmeier-Pelster J., Schürmann M., & Duda K. (2000). Depressionsinventar für Kinder und Jugendliche (2nd ed.). Göttingen: Hogrefe. [Google Scholar]
- Tierens M., Bal S., Crombez G., Loeys T., Antrop I., & Deboutte D. (2012). Differences in posttraumatic stress reactions between witnesses and direct victims of motor vehicle accidents. Journal of Traumatic Stress, 25, 280–287. [DOI] [PubMed] [Google Scholar]
- Tolin D. F., & Foa E. B. (2002). Gender and PTSD: A cognitive model In Kimerling R., Ouimette P., & Wolfe J. (Eds.), Gender and PTSD (pp. 76–97). New York, NY: Guilford Press. [Google Scholar]
- Trickey D., Siddaway A. P., Meiser-Stedman R., Serpell L., & Field A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32, 122–138. [DOI] [PubMed] [Google Scholar]
- Williamson V., Creswell C., Fearon P., Hiller R. M., Walker J., & Halligan S. L. (2017). The role of parenting behaviors in childhood post-traumatic stress disorder: A meta-analytic review. Clinical Psychology Review, 53, 1–13. [DOI] [PubMed] [Google Scholar]
- Zhang W., Liu H., Jiang X., Wu D., & Tian Y. (2014). A longitudinal study of posttraumatic stress disorder symptoms and its relationship with coping skill and locus of control in adolescents after an earthquake in China. Plos One, 9. doi: 10.1371/journal.pone.0088263 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Given that the ethical committees agree, the datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


