Abstract
Background
Bilateral symptomatic femoroacetabular impingement (FAI) is common. However, the fate of asymptomatic hip in patients with the radiographic diagnosis of bilateral FAI and unilateral symptoms remains unknown.
Questions/purposes
(1) What is the likelihood of the asymptomatic hip becoming painful in patients with unilateral symptoms but with radiographic evidence of bilateral femoroacetabular impingement? (2) What radiological and clinical factors are associated with the development of symptoms in an asymptomatic hip diagnosed with FAI?
Methods
A longitudinally maintained institutional FAI database was queried to collect relevant data for this retrospective study. To answer our research questions, we created a cohort of patients with bilateral radiographic signs of FAI but only unilateral symptoms at the time of initial presentation. Between 2004 and 2016, a senior surgeon (JP) at one institution treated 652 patients for hip pain determined to be from FAI, a diagnosis we made based on clinical symptoms, physical exam, and diagnostic imaging. We excluded 95 patients (15%) because of inadequate data or other diagnoses, which left 557 patients. Of those, 170 patients (31%) had bilateral radiological diagnosis of FAI, and 88 (52%) of them had bilateral hip symptoms, and so were excluded. Of the remaining 82 patients, eight (10%) underwent bilateral FAI surgery under the same anesthetic despite having only unilateral symptoms, leaving 74 for analysis in this study. Patients were followed with annual clinic visits, or contacted by phone and electronically. We defined onset of symptoms using a modified Harris Hip Score (mHHS) or the University of California at Los Angeles (UCLA) activity scale, and used a logistic regression model to identify factors associated with the development of symptoms.
Results
Of the 74 patients with bilateral FAI and an asymptomatic hip at initial presentation, 60 (81%) became symptomatic at a mean 2 years (range, 0.3–11 years) followup. Of these 60 patients, 43 (72%) eventually underwent subsequent surgical intervention. After controlling for potential confounding variables such as sex, age, BMI, history of trauma we identified that reduced neck-shaft angle (r = -0.243, p = 0.009), increased lateral center-edge angle (r = 0.123, p = 0.049), increased alpha angle (r = 0.069, p = 0.025), and younger age (r = -0.071, p = 0.046) were associated with the development of symptoms in the contralateral hip. With the numbers available, none of the other examined variables such as sex, BMI, history of trauma, psychiatric condition, employment, Tönnis grade, Tönnis angle, crossover sign, type of impingement, and joint congruency were found to be associated with symptom progression.
Conclusions
Bilateral FAI may be observed about one-third of patients. Most patients with unilateral symptomatic FAI and radiographic diagnosis of bilateral FAI in this cohort became symptomatic relatively quickly and most of them underwent subsequent surgical intervention in the contralateral hip. Reduced neck-shaft angle, increased lateral center-edge angle, increased alpha angle, and younger age were associated with symptom development in the contralateral hip. Hip preservation surgeons may use the finding of this study to counsel patients who present with bilateral FAI but only unilateral symptoms about the natural history of their condition.
Level of Evidence
Level III, therapeutic study.
Introduction
FAI affects 7% to 23% of the population [7, 8]. Although most patients present with symptoms in only one hip, bilateral FAI is common. The proportion of bilateral symptomatic FAI has been reported as 21% in a study of 641 patients who underwent surgical treatment for FAI [12]. In addition, many patients demonstrate radiographic signs and findings consistent with FAI even in the asymptomatic hip [12, 2]. Allen et al. [2] reported radiographic evidence of FAI in up to 78% of the contralateral hips in patients presenting with a painful hip, of whom only 26% experienced bilateral symptoms. The situation is further clouded by the uncertainty regarding the reproducibility of many of the standard radiographic parameters [6].
However, to our knowledge, there are no studies evaluating the fate of the asymptomatic hip in patients with the radiographic diagnosis of bilateral FAI and unilateral symptoms. Thus, the fate of the contralateral asymptomatic hip and the factors that may lead to generation of symptoms is largely unknown. We have been treating patients with FAI since 2004 at our institution and have observed that many patients with unilateral hip pain secondary to FAI have radiographic evidence of FAI in the contralateral hip, but because we lack good natural history data on this scenario, it can be hard to help the patients understand what to expect.
Therefore, we asked: (1) What is the likelihood of the asymptomatic hip becoming painful in patients with unilateral symptoms but with radiographic evidence of bilateral femoroacetabular impingement? (2) What radiological and clinical factors are associated with the development of symptoms in an asymptomatic hip diagnosed with FAI?
Patients and Methods
Between 2004 to 2016, the senior author saw 4000 patients with a diagnosis of femoroacetabular impingement, of whom 652 patients underwent surgical management. Institutional review board approval was obtained before study commencement. All patients underwent mini-open femoroacetabular osteoplasty. We queried a retrospectively maintained institutional FAI database to obtain relevant data on all patients, including detailed demographic and radiological data. Patients who undergo joint preservation are followed regularly as part of our database at our institution. These patients are given an appointment to return annually for evaluation. Those who miss their appointments are contacted electronically or via phone. Of the 652 patients, there was inadequate data regarding symptoms in the contralateral hip in 55 patients (60 hips), and we excluded these patients. We also excluded 17 patients (20 hips) with slipped capital femoral epiphysis (SCFE), eight patients with Legg-Calvé Perthes disease (LCPD), four patients who underwent periacetabular osteotomy (PAO) at the same session with femoroacetabular osteoplasty, four patients with a history of previous PAO before index femoroacetabular osteoplasty, four patients who underwent synovectomy and biopsy performed during femoroacetabular osteoplasty, two patients with a history of avascular necrosis (AVN), and one patient with a history of ankylosing spondylitis. The remaining 557 patients (646 hips) were included for analyses. Of these, 387 patients presented with unilateral hip pain with no evidence of FAI in the contralateral hip. In all, 170 patients (31%) had radiographic evidence of bilateral FAI, of which 88 (52%) presented with bilateral hip symptoms. The remaining 82 patients (48%) had unilateral hip symptoms, eight (10%) of whom underwent surgery on both hips simultaneously. The other 74 patients (90%) opted for observation of the contralateral asymptomatic hip with FAI (Fig. 1), and these patients form the final cohort for our analysis. Of the 74 patients, 14 (19%) did not become symptomatic (Group A), and 60 patients (81%) become symptomatic (Group B) and at minimum 1-year followup. We defined symptomatic as a worsening modified Harris Hip score (mHHS) or a decrease in function as measured by the UCLA Activity score. Conservative treatment was implemented for mild symptoms, and surgery was offered to patients if symptoms did not respond.
Fig. 1.
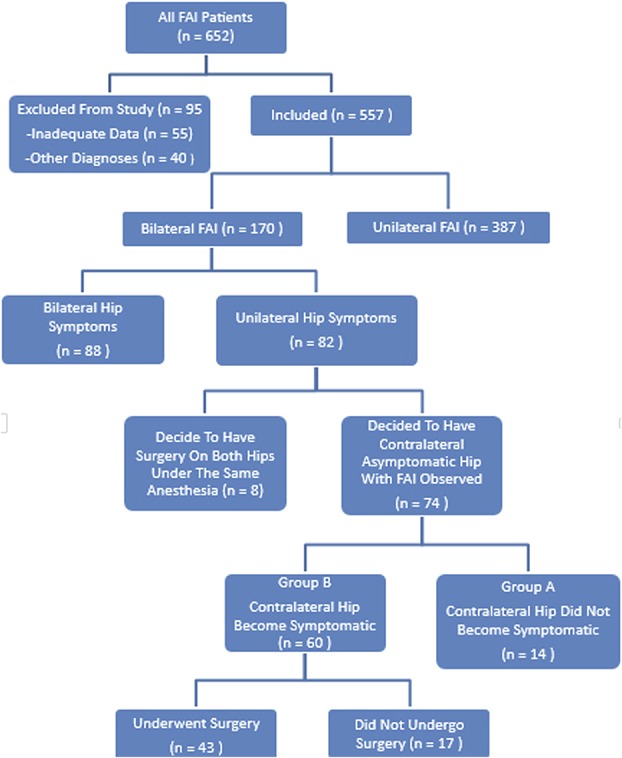
The flow diagram depicts the study sample.
The FAI diagnosis was made based on clinical symptoms, examination, and radiographic imaging. We scrutinized the insidious onset of symptoms, groin pain associated with activity, inability to perform activities, such as high hip flexion or prolonged sitting, painful clicking, locking, or instability. We used the impingement sign (pain on adduction of a flexed, internally rotated hip with the patient supine) and Stinchfield test for clinical diagnosis of FAI.
Radiographs, including an AP view of the pelvis, and lateral (Dunn 90°, crosstable lateral, and/or frog-leg lateral) hip radiographs were made. The largest alpha angle measured on lateral view was used. Cam-type FAI was diagnosed in the presence of abnormal alpha angle on lateral view (> 55°). The radiological diagnosis of pincer type FAI was made with the presence of deep acetabulum (coxa profunda and or protrusion acetabuli where the relative depth of the acetabulum is increased) or acetabular retroversion where the anterolateral acetabular edge obstructs flexion and increased lateral center-edge angle. In addition, the femoral neck shaft angle, lateral center-edge angle, and Tönnis angle were measured using x-rays. Tönnis grade, congruency, deep acetabular socket (coxa profunda and or protrusion acetabuli), crossover sign, and posterior wall sign were noted. We recorded job type, which was classified as light work, such as a desk job; and hard work, including gym teachers, policemen, martial arts trainers, or farmers; as well as a history of trauma, psychiatric conditions, and initiation of symptoms. Before they could be recommended for surgical intervention, all patients had to have undergone and failed a trial of nonoperative therapy, including NSAIDs and/or physical therapy.
Patients with abnormalities on the femoral head/neck side were thought to have cam-type FAI (49%), while those with abnormalities on the acetabular side were believed to suffer from pincer-type FAI (11.2%). Division of the FAI to cam- or pincer-type FAI was not possible in 40% of patients who exhibited signs of both pincer and cam FAI. We excluded patients with Tönnis 3 osteoarthritis from study.
Statistical Analysis
We used the Shapiro-Wilk test to confirm that data was within the ranges of normal distribution in both groups. We used the chi-square test for categorical variables and the Mann-Whitney U test for continuous variables. Correlations between symptomatic and asymptomatic patients regarding their contralateral hip were investigated with the help of Spearman’s correlation. By using a binary logistic regression analysis, a multivariate analysis was performed to detect the associated factors for the occurrence of a symptomatic hip. An enter method was used to construct multivariate logistic regression models in relation to various dependent variables. P value < 0.05 with a 95% confidence interval (CI) was accepted as significant.
Results
Of 74 patients with bilateral FAI and unilateral hip symptoms, 60 patients (81%) became symptomatic, as defined by worsening mHHS and UCLA activity scores, at a mean 2 years (range, 0.3–11 years) followup. The remaining 14 patients (19%) stayed asymptomatic at a mean followup of 3 years (range, 1–6 years). Of 60 patients who become symptomatic, 43 (72%) underwent surgical intervention within a mean of 2 years (range, 0.3–5 years) after the initial onset of symptoms. The remaining 17 patients (28%) who developed mild symptoms have been offered conservative treatment. The mean preoperative and postoperative mHHS was 49 ± 9 and 74 ± 21, respectively (p < 0.001). The mean preoperative and postoperative UCLA score was 5.3 ± 2.5 and 6.8 ± 2.4 respectively (p < 0.001).
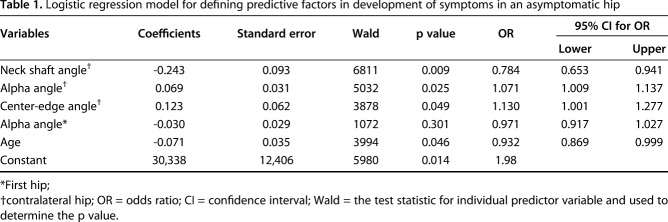
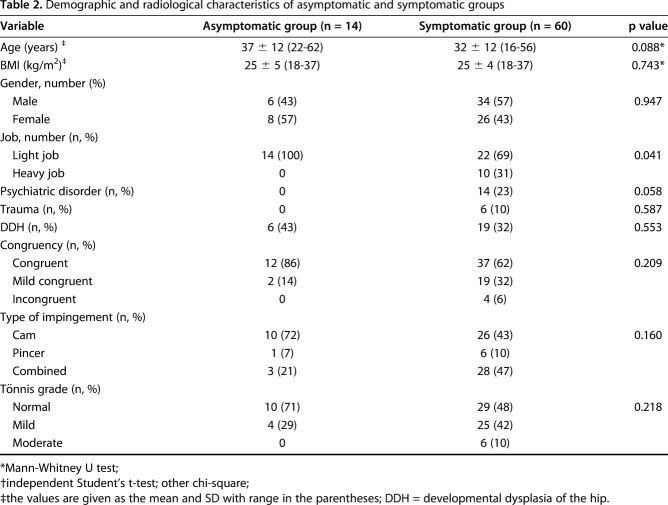
After controlling for potential confounding variables, we identified that a reduced neck-shaft angle (r = -0.243, p = 0.009), increased lateral center-edge angle (r = 0.123, p = 0.049), increased alpha angle (r = 0.069, p = 0.025), and younger age (r = -0.071, p = 0.046) were associated with developing symptoms in the contralateral hip (Table 1). With the numbers available, none of the other examined variables such as sex, BMI, history of trauma, psychiatric condition, employment, Tönnis grade, Tönnis angle, crossover sign, type of impingement, and joint congruency were found to be associated with symptom progression (Table 2).
Table 1.
Logistic regression model for defining predictive factors in development of symptoms in an asymptomatic hip
Table 2.
Demographic and radiological characteristics of asymptomatic and symptomatic groups
Discussion
FAI affects 7% to 23% of the population [7, 8]. Although most patients present with symptoms in only one hip, bilateral FAI is common. The course of the asymptomatic contralateral hip is an important concern for both orthopaedic surgeons and their patients. Patients almost always inquire about the fate of the asymptomatic hip after radiological diagnosis of FAI. However, the fate of asymptomatic hip in patients with the radiographic diagnosis of bilateral FAI and a unilateral symptom is unclear. We therefore aimed to investigate the chance that a contralateral hip becomes symptomatic in patients who undergo unilateral surgery for impingement but who show radiographic evidence of bilateral involvement. Also we tried to identify factors that are associated with symptom development. To the best of our knowledge, this is the first study investigating the fate of asymptomatic hip with FAI. Based on the results of this study, it appears that the incidence of bilateral FAI is relatively common at 31%. Most patients with unilateral symptomatic FAI and radiographic evidence of bilateral FAI eventually underwent surgical intervention in the contralateral hip (72%). After controlling for potential confounding variables such as age, sex, BMI, alpha angle, we identified that a reduced neck-shaft angle, increased lateral center-edge angle, increased alpha angle, and younger age are associated with developing symptoms in the contralateral hip.
This study has several limitations. First, we could not include 55 of 652 (8%) patients who had inadequate data about their symptoms, which may have biased our results and underestimated the likelihood that patients will become symptomatic over time. In addition, we excluded patients with FAI secondary to other diagnoses such as LCPD, SCFE, AVN. The latter was in an attempt to improve cohort homogeneity. Though a relatively large cohort, the number of patients with asymptomatic hip was relatively small, which may have resulted in type II error, causing us to fail to identify some factors that might be associated with an increased risk of symptom development in a hip with radiographic signs of FAI. Based on our data, we would suggest that future studies focus on the Tönnis grade, retroversion, race, and congruency. Also, we did not evaluate femoral version, which may play role in FAI. Although the minimum followup duration was 1 year in our study, we acknowledge that this relatively short followup duration may have underestimated the likelihood that patients will become symptomatic over time. In this study, the senior surgeon assessed all patients in terms of their symptoms, recommended conservative treatment for mild symptoms and surgery when conservative treatment was unsuccessful. Although this may reduce bias regarding recommending treatment choices, we acknowledge the indications for recommending surgery may differ depending on surgeon judgment. We note that other clinicians, or other patients, might exercise different treatment options.
Most patients who underwent surgery for unilateral, symptomatic FAI who had radiographic evidence of bilateral hip disease had a high likelihood of presenting soon after with pain and loss of function in the previously asymptomatic contralateral hip and most of them underwent surgical intervention. A study by Klingenstein et al. [12], has investigated risk factors that lead to bilateral hip preservation surgery for FAI, in which the prevalence of bilateral surgery was found to be 20.4%. This study found that younger patients, males, higher alpha angles, and reduced acetabular anteversion at initial presentation of the first hip were associated with an increased likelihood of undergoing surgery on the contralateral hip bilateral surgery; however, they compared unilateral hips with bilateral hips. Also, they did not report the time it took for asymptomatic hips to become symptomatic. In our study, the incidence of bilateral FAI was 31%. We investigated the chance that a contralateral hip becomes symptomatic in patients who underwent unilateral surgery for impingement but who showed radiographic evidence of bilateral involvement. We found that 81% of patients became symptomatic at a mean 2 years (range, 0.3–11 years) followup. Of those who become symptomatic, 72% underwent surgical intervention within a mean of 2 years (range, 0.3–5 years) after the initial onset of symptoms.
We found only a few identifiable factors associated with symptom progression in the previously asymptomatic hip, such as younger age, alpha angle, increased lateral center-edge angle, reduced femoral neck shaft angle. This study found that patients who became subsequently symptomatic were approximately 5 years younger than patients who remained asymptomatic. The exact reason for the latter finding is also not clear. Perhaps the high intensity of activity in the younger patients may account for this finding. However, Chládek et al. [5] found that patients younger than 30 years old with FAI had greater postoperative improvement compared with patients older than 30 years. Among the numerous factors studied, a higher alpha angle was found to be an independent predictor in developing symptoms in the contralateral hip. The latter may relate to the radiographic severity of the disease. Prior studies have shown that severe cam deformity, as defined by larger alpha angles, could indicate which individuals may be at risk for developing early hip pain and arthritis [1, 11, 12]. However, the association between cam morphology, hip pain, and subsequent hip osteoarthritis needs to be firmly established. Beaulé et al. [3] demonstrated that an alpha angle greater than 65° was associated with the development of more severe cartilage damage. In addition, a biomechanical investigation performed by Kapron et al. [10] also demonstrated the consequences of cam morphology on the anterolateral hip region. The investigators demonstrated that radiographically observed impingement contact points correlated with areas of anterolateral labral and chondral damage visualized during surgery [10]. Another study by McGuffin et al. [15] assessed the profile of the weightbearing cartilage of hips with a cam deformity using T1r magnetic resonance imaging (MRI) and evaluated for a side-to-side difference in the T1r profile of patients with bilateral cam morphology but only unilateral hip pain. The cartilage bilayer of the hip was evaluated and the mean T1r relaxation time calculated for each quadrant of the weightbearing surface. They concluded that the presence of a cam deformity, regardless of symptoms, is suggestive of early, preclinical cartilage degradation, and thus patients with asymptomatic cam morphology may be at increased risk for the development of hip osteoarthritis [15]. Thus, it is important to fully evaluate and consider the alpha angle and identify any cam morphology when providing a medical and surgical treatment plan. We also found that increased center-edge angle is associated with developing symptoms in the contralateral hip. Previous studies have demonstrated that a center edge angle of > 39° is associated with the development of symptomatic pincer FAI caused by acetabular over-coverage [13, 20]. In this study, the mean center-edge angle of the contralateral hip in symptomatic patients was 28.1 ± 7.7° (11–54°). Using the center-edge angle can help anticipate which patients with bilateral radiographic signs of FAI but only unilateral symptoms at presentation will develop symptoms in the contralateral hip. Reduced femoral neck shaft angle was found to be associated with developing symptoms in the contralateral hip. A decreased femoral neck shaft angle may be indicative of early symptoms [9, 14, 16, 17]. Neck shaft angle in patients with FAI have been reported to be between 123-140° [4, 14, 19]. Individuals with a cam morphology and decreased femoral neck-shaft angle are likely to experience severe hip stresses and earlier impingement [4]. Although asymptomatic participants with cam morphology have elevated stresses, a higher femoral neck-shaft angle has been associated with lower stresses [18]. Considering the femoral neck-shaft angle in patients may be useful in identifying those who may be at risk for FAI.
In conclusion, this study demonstrated that most patients with unilateral symptomatic FAI and radiographic evidence of bilateral FAI become symptomatic relatively quickly and undergo surgical intervention in the contralateral hip. This information will allow surgeons to have an informative discussion with patients with bilateral radiographic signs of FAI when only one hip is asymptomatic at initial presentation.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
One of the authors certifies that he (JP) has received or may receive personal fees during the study period, an amount of USD 100,001 to USD 1,000,000 from Corentec (Morristown, NJ, USA); less than USD 10,000 from MicroGen DX (Orlando, FL, USA); less than USD 10,000 from DataTrace (Towson, MD, USA); less than USD 10,000 from Elsevier (Philadelphia, PA, USA); less than USD 10,000 from Jaypee Publishers (London, UK); less than USD 10,000 from Slack Incorporated (Thorofare, NJ, USA); and less than USD 10,000 from Wolters Kluwer (Alphen aan den Rijn, Netherlands). One of the authors certifies that he (JP) has stock ownership in Parvizi Surgical Innovations (Philadelphia, PA, USA); Hip Innovation Technology (Boca Raton, FL, USA); Cross Current Business Intelligence (Newtown, PA, USA); Alphaeon (Irvine, CA, USA); Joint Purification Systems (Solana Beach, CA, USA); Ceribell (Mountain View, CA, USA); MedAp, Physician Recommended Nutriceuticals (Blue Bell, PA, USA); PRN Veterinary (Blue Bell, PA, USA); MDValuate (Centennial, CO, USA); Intellijoint (Waterloo, Ontario, Canada); and MicroGenDx (Orlando, FL, USA). One of the authors certifies that he (JP) he is a consultant to Zimmer Biomet (Warsaw, IN, USA), ConvaTec (Deeside, UK), CeramTec (Plochingen, Germany), Corentec (Morristown, NJ, USA), Ethicon (Somerville, NJ, USA), and Tenor (San Francisco, CA, USA).
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Agricola R, Heijboer MP, Bierma-Zeinstra SMA, Verhaar JAN, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: A nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72:918-923. [DOI] [PubMed] [Google Scholar]
- 2.Allen D, Beaulé PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91:589-594. [DOI] [PubMed] [Google Scholar]
- 3.Beaulé P, Hynes K, Parker G, Kemp K. Can the alpha angle assessment of cam impingement predict acetabular cartilage delamination? Clin Orthop Relat Res. 2012;470:3361-3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouma HW, Hogervorst T, Audenaert E, Krekel P, van Kampen PM. Can combining femoral and acetabular morphology parameters improve the characterization of femoroacetabular impingement? Clin Orthop Relat Res. 2015;473:1396-1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chládek P, Musálek M, Trč T, Zahradník P, Kos P. Femoroacetabular impingement syndrome--efficacy of surgical treatment with regards to age and basic diagnosis. Int Orthop. 2015;39:417-422. [DOI] [PubMed] [Google Scholar]
- 6.Clohisy JC, Carlisle JC, Trousdale R, et al. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467:666-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fukushima K, Uchiyama K, Takahira N, Moriya M, Yamamoto T, Itoman M, Takaso M. Prevalence of radiographic findings of femoroacetabular impingement in the Japanese population. J Orthop Surg Res. 2014;9:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436-2444. [DOI] [PubMed] [Google Scholar]
- 9.Hartofilakidis G, Bardakos NV, Babis GC, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br. 2011;93:580-586. [DOI] [PubMed] [Google Scholar]
- 10.Kapron AL, Aoki SK, Peters CL, Anderson AE. Subject-specific patterns of femur-labrum contact are complex and vary in asymptomatic hips and hips with femoroacetabular impingement. Clin Orthop Relat Res. 2014;472:3912-3922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khanna V, Caragianis A, Diprimio G, Rakhra K, Beaulé PE. Incidence of hip pain in a prospective cohort of asymptomatic volunteers: Is the cam deformity a risk factor for hip pain? Am J Sports Med. 2014;42:793-797. [DOI] [PubMed] [Google Scholar]
- 12.Klingenstein GG, Zbeda RM, Bedi A, Magennis E, Kelly BT. Prevalence and preoperative demographic and radiographic predictors of bilateral femoroacetabular impingement. Am J Sports Med. 2013;41:762-768. [DOI] [PubMed] [Google Scholar]
- 13.Kutty S, Schneider P, Faris P, Kiefer G, Frizzell B, Park R, Powell JN. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. International Orthopaedics (SICOT). 2012;36:505-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leunig M, Maffiuletti N. CORR insights®: Patient-specific anatomical and functional parameters provide new insights into the pathomechanism of cam FAI. Clin Orthop Relat Res. 2015;473:1297-1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGuffin WS, Melkus G, Rakhra KS, Beaulé PE. Is the contralateral hip at risk in patients with unilateral symptomatic cam femoroacetabular impingement? A quantitative T1ρ MRI study. Osteoarthritis Cartilage. 2015;23:1337-1342. [DOI] [PubMed] [Google Scholar]
- 16.Ng KCG, Lamontagne M, Labrosse MR, Beaulé PE. Comparison of anatomical parameters of cam femoroacetabular impingement to evaluate hip joint models segmented from CT data. Comput Methods Biomech Biomed Eng Imaging Vis. 2018;6:293-302. [Google Scholar]
- 17.Ng KCG, Lamontagne M, Beaulé PE. Differences in anatomical parameters between the affected and unaffected hip in patients with bilateral cam-type deformities. Clin Biomech (Bristol, Avon). 2016;33:13-19. [DOI] [PubMed] [Google Scholar]
- 18.Ng KCG, Mantovani G, Lamontagne M, Labrosse MR, Beaulé PE. Increased hip stresses resulting from a cam deformity and decreased femoral neck-shaft angle during level walking. Clin Orthop Relat Res. 2017;475:998-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Streit J, Gebhart J, Bedi A, Bush-Joseph C, Nho S, Salata M. Femoral neck-shaft angle differs but femoral anteversion is constant in osteological specimens with and without a cam deformity of the proximal femur. Arthroscopy . 2013;29:e207. [Google Scholar]
- 20.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: Radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540-1552. [DOI] [PubMed] [Google Scholar]