Supplemental Digital Content is available in the text
Keywords: general anesthesia, meta-analysis, spinal anesthesia, total-hip arthroplasty
Abstract
Background:
The optimal anesthetic technique remains debated in patients undergoing total-hip arthroplasty (THA). The purpose of this meta-analysis was to test the efficacy of general and spinal anesthesia for patients undergoing THA.
Methods:
In January 2018, we searched PubMed, Embase, Web of Science, Cochrane Database of Systematic Reviews, and the Google database. Data from randomized controlled trials (RCTs) that compared the use of general and spinal anesthesia for patients undergoing THA were retrieved. The primary outcome was to compare the total blood loss. The secondary outcomes were the occurrence of deep venous thrombosis (DVT), the occurrence of nausea, and the length of hospital stay. Software Stata 12.0 was used for meta-analysis.
Results:
Five RCTs with 487 THAs were finally included for meta-analysis. There was no significant difference between the general anesthesia and spinal anesthesia in terms of the total blood loss (weighted mean difference [WMD] = −20.72, 95% confidence interval [CI] −84.50 to 43.05, P = .524; I2 = 87.8%) and the occurrence of DVT (risk ratio (RR) = 0.85, 95% CI 0.24–3.01, P = .805; I2 = 70.5%). Compared with general anesthesia, spinal anesthesia was a significant reduction in the occurrence of nausea (RR = 3.04, 95% CI 1.69–5.50, P = .000; I2 = 0.0%) and the length of hospital stay (WMD = 1.00, 95% CI 0.59–1.41, P = .000; I2 = 94.7%).
Conclusion:
Spinal anesthesia was superior than general anesthesia in terms of the occurrence of nausea and shorten the length of hospital stay. The quality and number of included studies was limited; thus, a greater number of high-quality RCTs is still needed to further identify the effects of spinal anesthesia on reducing the blood loss after THA.
1. Introduction
Total-hip arthroplasty (THA) is a frequently performed and painful procedure.[1,2] Patients undergoing THA may be offered either spinal anesthesia or general anesthesia.[3] Among the various regional techniques, spinal anesthesia is not only common, but also recommended.[4] Recent years, many studies has been published and compared spinal anesthesia and general anesthesia for clinical outcomes of THA. Harsten et al[5] reported that general anesthesia resulted in a more favorable recovery profile compared with spinal anesthesia after THA. However, Maurer et al's[6] spinal anesthesia appears superior to general anesthesia for THA. With more evidence appears, we want to identify whether spinal anesthesia was superior than general anesthesia in terms of the perioperative blood loss, the occurrence of deep venous thrombosis (DVT) and nausea.
2. Materials and methods
This meta-analysis was conducted in accordance with the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions[7] and was written in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) checklist.[8] There was no registered protocol.
2.1. Search strategy and study selection
The following electronic databases were systematically searched from their inception through January 2018: PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science and the Google database. The detailed PubMed search strategy was as follows: (((spinal anesthesia) AND general anesthesia)) AND (((((“Arthroplasty, Replacement, Hip”[Mesh]) OR THR) OR THA) OR total-hip arthroplasty) OR total-hip replacement). No language restriction was applied. We manually searched relevant meta-analysis to find any omitting study.
2.2. Eligibility criteria
-
1.
Participants: Patients who underwent THA (including primary THA and THA revisions).
-
2.
Interventions: General anesthesia was used preoperatively for the intervention group.
-
3.
Comparisons: Spinal anesthesia was used preoperatively for the comparison group.
-
4.
Outcomes: Total blood loss, the occurrence of DVT, the occurrence of nausea, and the length of hospital stay.
-
5.
Study design: Only randomized controlled trials (RCTs) were included.
2.3. Data extraction and outcome measures
For each published study included in the meta-analysis, 2 authors (XP and JS) independently extracted the following data: author, publication year, country, cases of spinal anesthesia and general anesthesia, mean age, dose and drugs of general anesthesia and spinal anesthesia, outcomes, duration of the follow-up period, and study type. Any disagreement was resolved by discussion. The outcome measures were total blood loss, the occurrence of DVT, the occurrence of nausea, and the length of hospital stay. If the data were not available and presented in figures or other forms, we extracted the mean and standard deviation values using GetData Graph Digitizer software as needed.[7] If there was any missing data, we contact with authors for missing data.
2.4. Risk of bias assessment
Two reviewers independently evaluated the risk of bias in RCTs according to the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions.[7] There were a total of 7 items need to identify for the risk of bias of the RCTs (random sequence generation, allocation concealment, blinding of the participant and outcome assessment and other bias). Each items were assessed as “low risk of bias,” “unclear risk of bias,” and “high risk of bias.”
2.5. Quality of evidence assessment
To assess the quality of evidence, 2 authors (XP and JS) used the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) methodology.[9] For each outcome, 5 separate factors were rated for quality: risk of bias, inconsistency, indirectness, imprecision, and publication bias.[9,10] And GRADE Profiler (GRADEpro, version 3.6, McMaster University and Evidence Prime Inc, Hamilton) was used to construct summary table.
2.6. Statistical analysis
For dichotomous outcomes (the occurrence of DVT and the occurrence of nausea), we calculated the risk ratio (RR) and the 95% confidence interval (CI). For continuous outcomes (total blood loss and the length of hospital stay), we calculated the weighted mean difference (WMD) and corresponding CIs. Heterogeneity was considered to be statistically significant if the I2-value was >50%. A fixed-effects model was applied if the I2-value was <50%. All statistical analyses were conducted using Stata 12.0 (Stata Corp., College Station, TX). A P-value <.05 was considered statistically significant. We used kappa values to assess the degree of agreement between the 2 reviewers. The criteria was as follows: fair, 0.40 to 0.59; good, 0.60 to 0.74; and excellent, 0.75 or higher.[11] In addition, we calculated numbers needed to treat (NNT) to examine the risk vs benefit of general anesthesia and spinal anesthesia for some endpoints.[12] We used DerSimonian–Laird method to synthesis outcomes with large heterogeneity.[13]
3. Results
3.1. Search results
The literature search and selection process are illustrated in Figure 1. The initial search yielded 158 articles (PubMed = 92, Embase = 18, Web of Science = 32, Cochrane Library = 6, Google database = 10). After excluding duplications, 132 studies were examined. Next, 127 of the 132 studies were excluded based on the inclusion criteria. Finally, a total of 5 studies were finally included in this meta-analysis.[5–17] Kappa value between the 2 reviewers was 0.713 and indicated that degree of agreement was good. There was no missing data for the outcomes.
Figure 1.
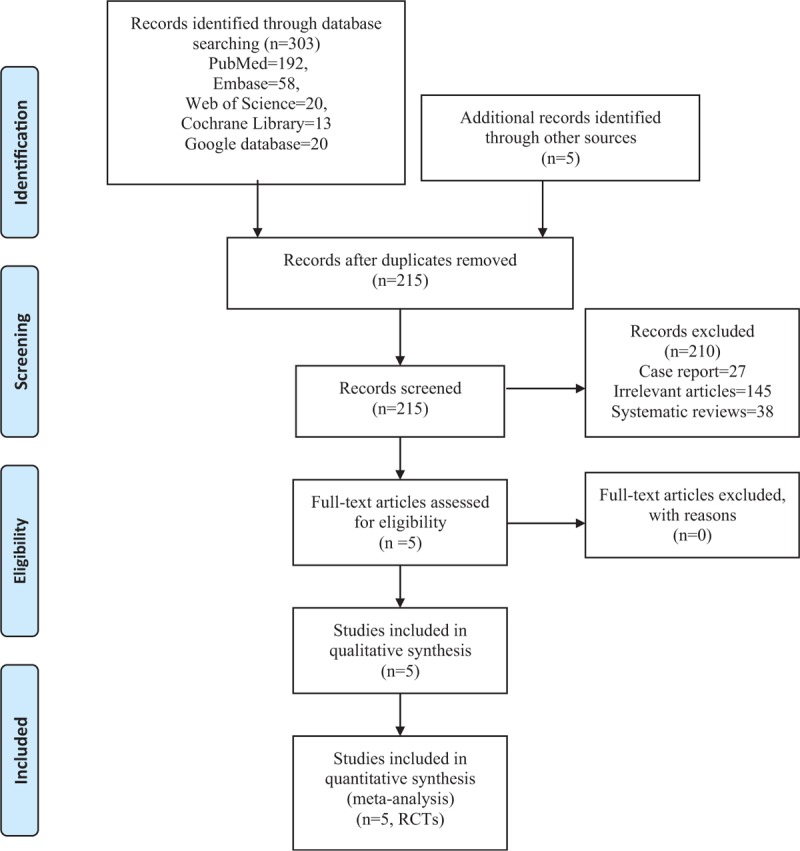
Flowchart of the included studies.
3.2. Study characteristics
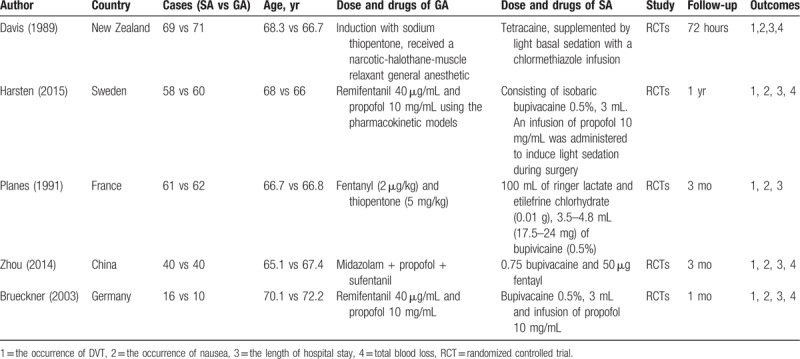
Detailed baseline characteristics of the included studies are presented in Table 1. Four studies were included in the meta-analysis. All articles were published in English between 2011 and 2016. The sample sizes ranged from 10 to 71 (total = 487, SA = 244, GA = 243), and the mean ages ranged from 65.1 to 72.2. The follow-up period was ranged from 72 hours to 1 year.
Table 1.
General characteristics of the included studies.
3.3. Risk of bias among the included studies
Risk of bias can be obtained in Figures 2 and 3. Three studies reported the random sequence generation and only 1 study did not describe the random sequence generation. Three studies were with low risk of bias for the allocation concealment, and 2 studies were with unclear risk of bias. Blinding of the participant and outcome assessment were with low risk of bias in 3 studies. Attrition bias, reporting bias, and other bias were all with low risk of bias.
Figure 2.
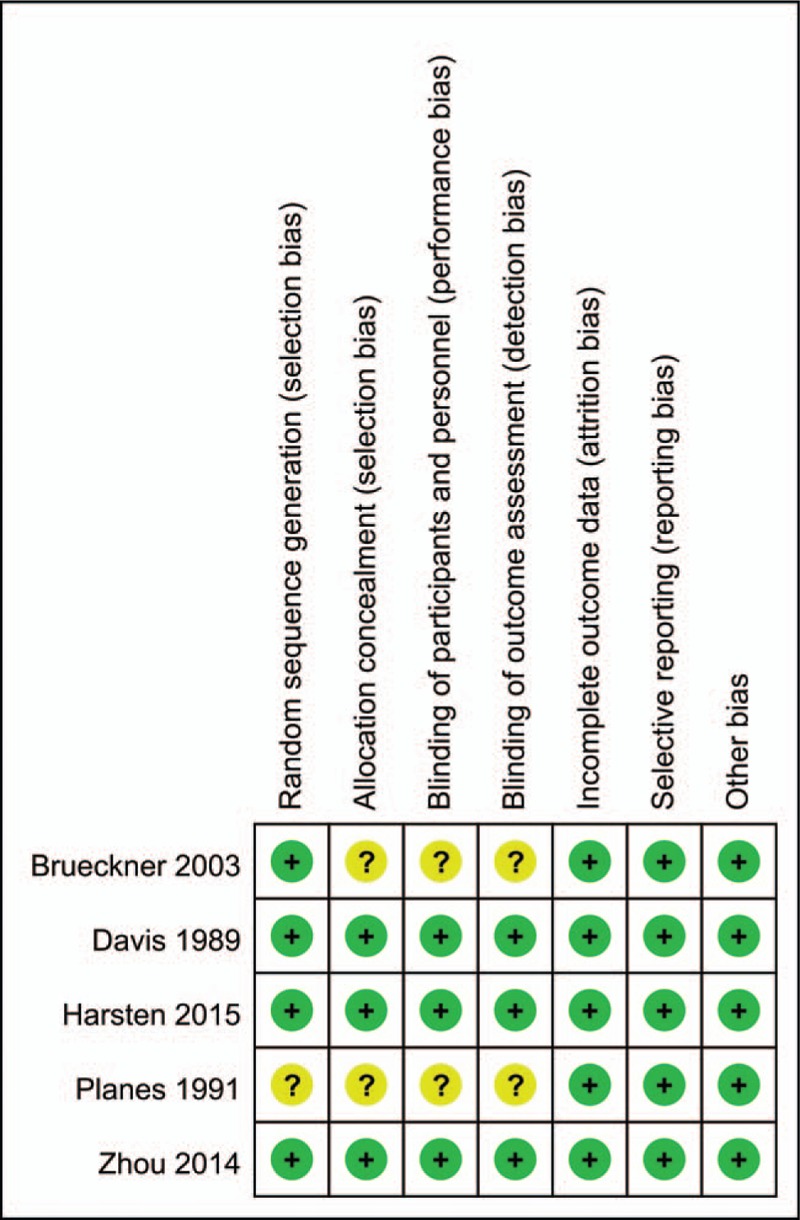
Risk of bias summary of the included studies. “+” low risk of bias, “−” high risk of bias, “?” unclear risk of bias.
Figure 3.
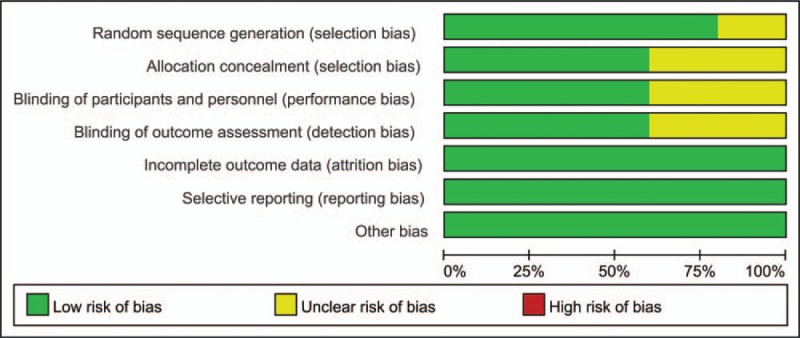
Risk of bias graph.
3.4. Results of meta-analysis
3.4.1. Total blood loss
Three studies, including 381 patients with THA, tested the effect of general anesthesia and spinal anesthesia on the total blood loss. There was no significant difference between the general anesthesia and spinal anesthesia in terms of the total blood loss (WMD = −20.72, 95% CI −84.50 to 43.05, P = .524; I2 = 87.8%, moderate evidence, Fig. 4). We use a random-effects model to pool the relevant data.
Figure 4.
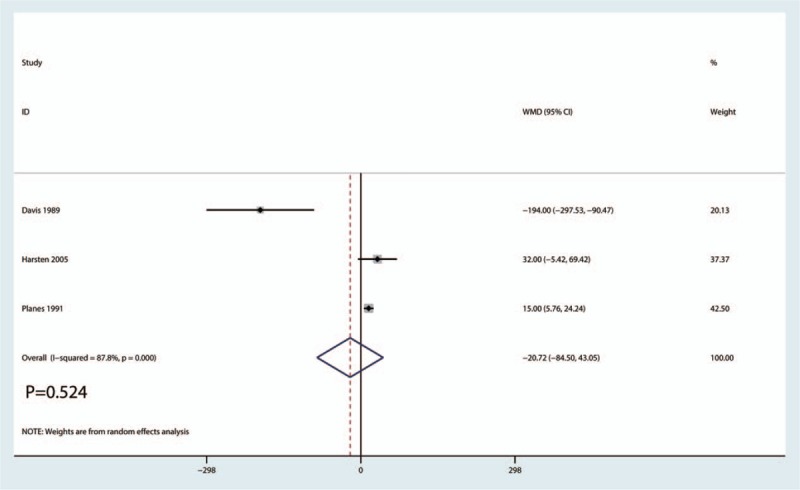
Forest plot of the total blood loss between the 2 groups.
3.4.2. Occurrence of DVT
Three studies including 289 patients with THA tested the effect of general anesthesia and spinal anesthesia in terms of the occurrence of DVT. There was no significant difference between the occurrence of DVT between the 2 groups (RR = 0.85, 95% CI 0.24–3.01, P = .805; I2 = 70.5%, low evidence; Fig. 5) with NNT value is 19.51.
Figure 5.
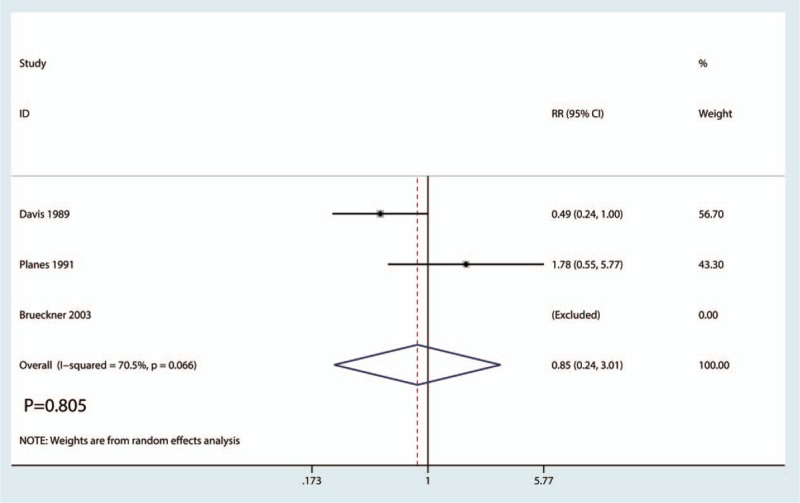
Forest plot of the occurrence of deep venous thrombosis between the 2 groups.
3.4.3. Occurrence of nausea
Four studies including 369 patients tested the effect of general anesthesia and spinal anesthesia on the occurrence of nausea. Compared with general anesthesia, spinal anesthesia was associated with a significant reduction in the occurrence of nausea (RR = 3.04, 95% CI 1.69–5.50, P = .000; I2 = 0.0%, high evidence; Fig. 6) with NNT value is 6.69.
Figure 6.
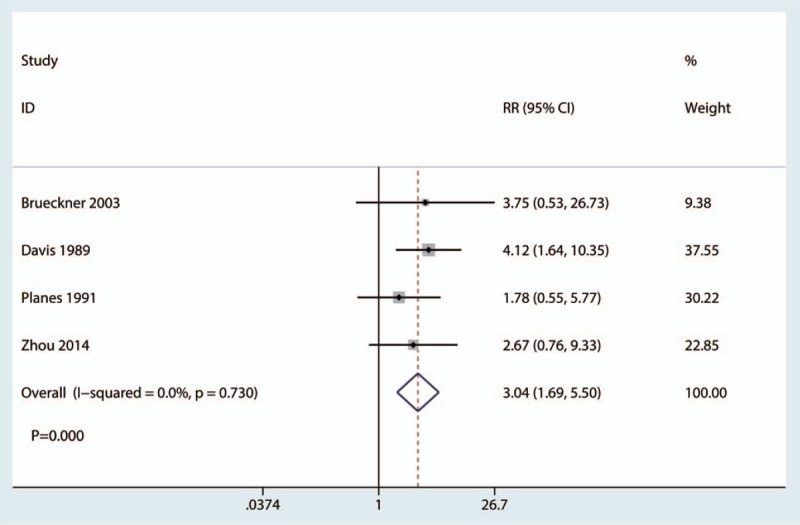
Forest plot of the occurrence of nausea between the 2 groups.
3.4.4. Length of hospital stay
Four studies including 369 patients tested the effect of general anesthesia and spinal anesthesia on the length of hospital stay. Compared with the general anesthesia, spinal anesthesia was associated with a significant reduction in the length of hospital stay (WMD = 1.00, 95% CI 0.59–1.41, P = .000; I2 = 94.7%, low evidence; Fig. 7).
Figure 7.
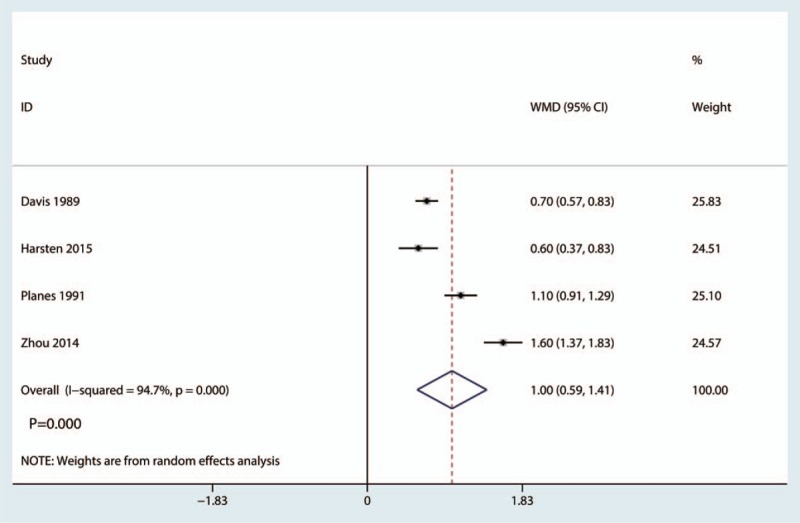
Forest plot of the length of hospital stay between the 2 groups.
3.4.5. Sensitivity analyses, publication bias, and GRADE evidence
Figure 8 shows the result of sensitivity analyses for total blood loss. Results shown that after omitting each study, the final results did not alter. Since the number of included studies was <10 and thus it was not necessary to perform funnel plot or Begg test. Grade evidences for outcomes were presented in Supplement S1.
Figure 8.
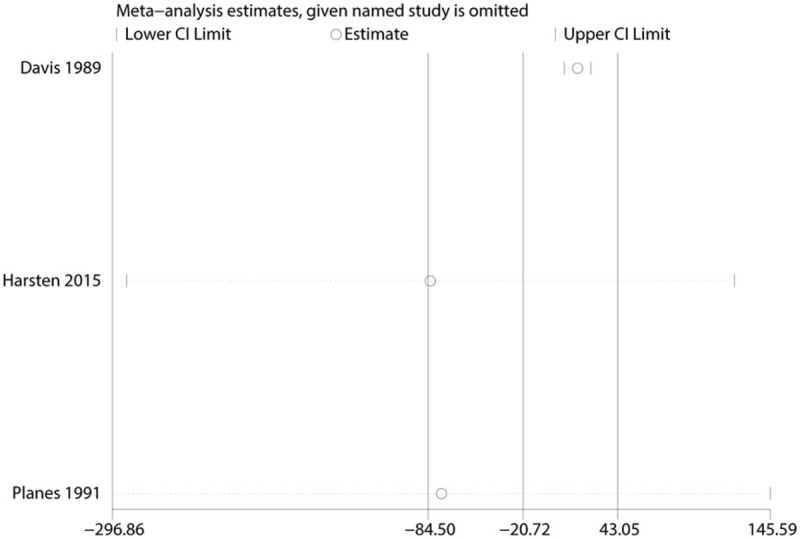
Sensitivity analysis of the total blood loss.
4. Discussion
This is the 1st systematic review and meta-analysis that comparing general anesthesia and spinal anesthesia after THA. Current meta-analysis indicated that there was no significant difference between the general anesthesia vs spinal anesthesia in terms of the total blood loss, the occurrence of DVT. Spinal anesthesia was associated with a reduction of the occurrence of nausea and the length of hospital stay.
General and spinal anesthesia are both commonly used during THA. However, the effects of general and spinal anesthesia for perioperative blood loss and the occurrence of DVT was unknown. Current meta-analysis demonstrated that general anesthesia had no benefit effect on the total blood loss and the occurrence of DVT. There is a high heterogeneity for these outcomes. We performed sensitivity analysis by omitting each study in turn, the final results did not alter. The reason may be as the clinical heterogeneity such as different surgical approach, prosthesis, and surgeons.
Maurer et al[6] reported that spinal anesthesia was associated with a significantly reduction in blood loss and subsequently blood transfusion. However, Harsten et al[5] reported that there was no significant difference between the hemoglobin level after THA between general anesthesia and spinal anesthesia. Gonano et al[18] compared spinal anesthesia and general anesthesia in terms of the occurrence of DVT and found that spinal anesthesia was associated with a reduction of the occurrence of DVT. Lončarić-Katušin et al[19] revealed that the mode of anesthesia (general vs spinal) has no effect on postoperative mortality, and that the mode of anesthesia should be applied on an individual basis in correlation with associated comorbidities. Accepted benefits of spinal anesthesia include the avoidance of airway management, decreased perioperative blood loss, and reduction of DVT risk, whereas general anesthesia is recommended for hemodynamically unstable patients.[20,21]
For the occurrence of nausea, we found that spinal anesthesia was associated with a reduction of the occurrence of nausea. Brueckner et al[14] drawn a similar conclusion with our results that spinal anesthesia was associated with a significantly reduction of the occurrence of nausea (P < .05). Finsterwald et al[22] reported that the spinal surgery patients in the spinal anesthesia group has lower postoperative nausea and vomiting than general anesthesia group. What's more, lumbar spine surgery in cardiovascular high risk patients with spinal anesthesia is safe.
In addition, we then draw a conclusion that spinal anesthesia was associated with a reduction of the length of hospital stay and further reduce the hospital-related costs. Gonano et al[18] reported that spinal anesthesia was associated with a reduction of the economic costs in THA patients. Kuju et al[23] compared the effectiveness of spinal anesthesia and general anesthesia for open cholecystectomy and results shown that spinal anesthesia is safe and more effective than general anesthesia.
For costs of spinal anesthesia and general anesthesia, many studies shown that spinal anesthesia lead to lower health care costs.[22–24] Since there was no direct comparison between the costs of these 2 approaches. Thus, more studies were needed to identify the economic costs of the 2 methods.
There were a total of 4 main limitations in this meta-analysis: only 5 RCTs with small sample size and overestimation of the intervention effect is more likely compared with larger sample studies; the drug used for spinal anesthesia and general anesthesia were different in the included studies and may cause the heterogeneity for the final outcomes; included studies selected reporting the diagnosis method of DVT and the use of venous thrombosis prophylaxis; perioperative pain management was different in the included studies and thus may cause the heterogeneity.
5. Conclusion
In conclusion, we found that spinal anesthesia was superior than general anesthesia in terms of the occurrence of nausea and shorten the length of hospital stay. There was no significant difference between the perioperative blood loss and the occurrence of DVT. Future research should be aimed at the optimal drug and dose for spinal anesthesia. In addition, more well-designed RCTs should be performed to confirm these results.
Author contributions
Formal analysis: Jian-ming Sun.
Software: Xiang Pu.
Writing – review & editing: Xiang Pu, Jian-ming Sun.
Supplementary Material
Footnotes
Abbreviations: CENTRAL = Cochrane Central Register of Controlled Trials, CI = confidence interval, DVT = deep venous thrombosis, GRADE = Grading of Recommendations, Assessment, Development and Evaluation, PRISMA = preferred reporting items for systematic reviews and meta-analyses, RCTs = randomized controlled trials, RR = risk ratio, SD = standard deviation, THA = total-hip arthroplasty, WMD = weighted mean differences.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Yang Q, Zhang Z, Xin W, et al. Preoperative intravenous glucocorticoids can decrease acute pain and postoperative nausea and vomiting after total hip arthroplasty: a PRISMA-compliant meta-analysis. Medicine (Baltimore) 2017;96:e8804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Zhang X, Yang Q, Zhang Z. The efficiency and safety of local liposomal bupivacaine infiltration for pain control in total hip arthroplasty: a systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e8433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Liang C, Wei J, Cai X, et al. Efficacy and safety of 3 different anesthesia techniques used in total hip arthroplasty. Med Sci Monit 2017;23:3752–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kearns R, Macfarlane A, Grant A, et al. A randomised, controlled, double blind, non-inferiority trial of ultrasound-guided fascia iliaca block vs. spinal morphine for analgesia after primary hip arthroplasty. Anaesthesia 2016;71:1431–40. [DOI] [PubMed] [Google Scholar]
- [5].Harsten A, Kehlet H, Ljung P, et al. Total intravenous general anaesthesia vs. spinal anaesthesia for total hip arthroplasty: a randomised, controlled trial. Acta Anaesthesiol Scand 2015;59:298–309. [DOI] [PubMed] [Google Scholar]
- [6].Maurer SG, Chen AL, Hiebert R, et al. Comparison of outcomes of using spinal versus general anesthesia in total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2007;36:E101–6. [PubMed] [Google Scholar]
- [7].Higgins JPT GS. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. 2011. [Google Scholar]
- [8].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Guyatt GH, Oxman AD, Kunz R, et al. What is “quality of evidence” and why is it important to clinicians? BMJ 2008;336:995–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Laupacis A, Sackett DL, Roberts RS. An assessment of clinically useful measures of the consequences of treatment. N Engl J Med 1988;318:1728–33. [DOI] [PubMed] [Google Scholar]
- [13].IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol 2014;14:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Brueckner S, Reinke U, Roth-Isigkeit A, et al. Comparison of general and spinal anesthesia and their influence on hemostatic markers in patients undergoing total hip arthroplasty. J Clin Anesth 2003;15:433–40. [DOI] [PubMed] [Google Scholar]
- [15].Davis FM, Laurenson VG, Gillespie WJ, et al. Deep vein thrombosis after total hip replacement. A comparison between spinal and general anaesthesia. J Bone Joint Surg Br 1989;71:181–5. [DOI] [PubMed] [Google Scholar]
- [16].Planes A, Vochelle N, Fagola M, et al. Prevention of deep vein thrombosis after total hip replacement. The effect of low-molecular-weight heparin with spinal and general anaesthesia. J Bone Joint Surg Br 1991;73:418–22. [DOI] [PubMed] [Google Scholar]
- [17].Zhou X, Jiang H, Li J, et al. The comparison of complications between general anesthesia and isobaric spinal anesthesia for total hip arthroplasty in elderly patients. Ningxia Med J 2014;36:521–3. [Google Scholar]
- [18].Gonano C, Leitgeb U, Sitzwohl C, et al. Spinal versus general anesthesia for orthopedic surgery: anesthesia drug and supply costs. Anesth Analg 2006;102:524–9. [DOI] [PubMed] [Google Scholar]
- [19].Lončarić-Katušin M, Miskovic P, Lavrnja-Skolan V, et al. General versus spinal anaesthesia in proximal femoral fracture surgery - treatment outcomes. Injury 2017;48Suppl 5:S51–5. [DOI] [PubMed] [Google Scholar]
- [20].Neuman MD, Silber JH, Elkassabany NM, et al. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. Anesthesiology 2012;117:72–92. [DOI] [PubMed] [Google Scholar]
- [21].Guay J, Parker MJ, Gajendragadkar PR, et al. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev 2016;2:Cd000521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Finsterwald M, Muster M, Farshad M, et al. Spinal versus general anesthesia for lumbar spine surgery in high risk patients: perioperative hemodynamic stability, complications and costs. J Clin Anesth 2018;46:3–7. [DOI] [PubMed] [Google Scholar]
- [23].Kuju RB, Dongol Y, Verma R. Effectiveness of spinal anaesthesia versus general anaesthesia for open cholecystectomy. J Nepal Health Res Counc 2016;14:93–8. [PubMed] [Google Scholar]
- [24].Pierce JT, Kositratna G, Attiah MA, et al. Efficiency of spinal anesthesia versus general anesthesia for lumbar spinal surgery: a retrospective analysis of 544 patients. Local Reg Anesth 2017;10:91–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


