Summary
Background
Suicidal thoughts and non-suicidal self-harm are common in adolescents and are strongly associated with suicide attempts. We aimed to identify predictors of future suicide attempts in these high-risk groups.
Methods
Participants were from the Avon Longitudinal Study of Parents and Children, a population-based birth cohort study in the UK. The sample included 456 adolescents who reported suicidal thoughts and 569 who reported non-suicidal self-harm at 16 years of age. Logistic regression analyses were used to explore associations between a wide range of prospectively recorded risk factors and future suicide attempts, assessed at the age of 21 years.
Findings
38 (12%) of 310 participants with suicidal thoughts and 46 (12%) of 380 participants who had engaged in non-suicidal self-harm reported having attempted suicide for the first time by the follow-up at 21 years of age. Among participants with suicidal thoughts, the strongest predictors of transition to attempts were non-suicidal self-harm (odds ratio [OR] 2·78, 95% CI 1·35–5·74; p=0·0059), cannabis use (2·61, 1·11–6·14; p=0·029), other illicit drug use (2·47, 1·02–5·96; p=0·045), exposure to self-harm (family 2·03, 0·93–4·44, p=0·076; friend 1·85, 0·93–3·69, p=0·081), and higher levels of the personality type intellect/openness (1·62, 1·06–2·46; p=0·025). Among participants with non-suicidal self-harm at baseline, the strongest predictors were cannabis use (OR 2·14, 95% CI 1·04–4·41; p=0·038), other illicit drug use (2·17, 1·10–4·27; p=0·025), sleep problems (waking in the night 1·91, 0·95–3·84, p=0·069; insufficient sleep 1·97, 1·02–3·81, p=0·043), and lower levels of the personality type extraversion (0·71, 0·49–1·03; p=0·068).
Interpretation
Most adolescents who think about suicide or engage in non-suicidal self-harm will not make an attempt on their life. Many commonly cited risk factors were not associated with transition to suicide attempt among these high-risk groups. Our findings suggest that asking about substance use, non-suicidal self-harm, sleep, personality traits, and exposure to self-harm could inform risk assessments, and might help clinicians to identify which adolescents are at greatest risk of attempting suicide in the future.
Funding
American Foundation for Suicide Prevention, National Institute for Health Research Biomedical Research Centre at the University Hospitals Bristol National Health Service Foundation Trust, and the University of Bristol.
Introduction
Suicidal behaviour is a major public health concern in adolescents. Although suicidal thoughts and non-suicidal self-harm are strong predictors of suicide attempts, little is known about the factors that predict attempts in these high-risk groups. A better understanding of these factors is crucial for improved suicide prediction and prevention.
Only a third of adolescents who have suicidal thoughts are estimated to go on to make a suicide attempt.1 Theoretical models of suicide, including the interpersonal theory,2 the integrated motivational–volitional model,3 and the three-step theory,4 are consistent with an ideation-to-action framework. This framework proposes that the factors involved in the development of suicidal thoughts are distinct from those involved in the transition from thoughts to attempts. Several large epidemiological and meta-analytical studies provide empirical support for this framework and have found that many well established risk factors for suicide (such as depression, impulsivity, and hopelessness) do not meaningfully differentiate individuals with suicidal thoughts from those who have made an attempt.1, 5, 6, 7 According to a recent review,8 the factors that most consistently predict suicide attempts among people with ideation relate to suicide capability (ie, the degree to which an individual feels able to make a suicide attempt). In a previous study of more than 4500 adolescents,9 we explored a wide range of risk factors and found that exposure to self-harm in others, psychiatric disorders, and substance use most strongly distinguished between adolescents with suicidal thoughts and those who acted on those thoughts. However, like most previous studies exploring this issue,1, 10, 11, 12, 13, 14 the analyses were cross-sectional, and the extent to which these factors would predict future suicide attempts is currently unknown.
Much of the scientific literature and theory exploring transitions to suicide attempts has focused on suicidal thoughts. However, investigation of predictors of attempts among people who engage in non-suicidal self-harm is also important, because this factor is strongly associated with suicide attempt history and predicts future attempts in longitudinal studies.15, 16, 17, 18, 19 A meta-analysis of 52 studies (all using retrospective self-report) found that the strongest correlates of suicide attempts among adolescents who engaged in non-suicidal self-harm were suicidal ideation, hopelessness, and non-suicidal self-harm characteristics (frequency and number of methods).20 As found for suicidal thoughts, many often-cited risk factors for suicide were generally poor at distinguishing between adolescents with suicidal and non-suicidal self-harm. The only previous longitudinal study21 also found self-harm frequency to be an important predictor of suicidal behaviour among adolescents who engage in non-suicidal self-harm. Other factors identified were reduced social connectedness and sense of meaning in life, and increased levels of mental health treatment.
Research in context.
Evidence before this study
Suicidal thoughts and non-suicidal self-harm are strongly associated with suicide attempts. However, the majority of adolescents who think about suicide or engage in non-suicidal self-harm will not make an attempt on their life. We searched PubMed for studies published in English before Dec 13, 2018, investigating risk factors for suicide attempts among these high-risk groups. We did two separate searches of the scientific literature. One search was for suicidal thoughts using the query (“suicidal thoughts” OR “suicidal ideation”) AND (“suicide attempt” OR “suicidal behaviour” OR “ideation to action”). The other search was for non-suicidal self-harm using the query (“non-suicidal self-harm” OR “non-suicidal self-injury” OR “NSSI”) AND (“suicide attempt” OR “suicidal behaviour”). We also checked citations of relevant publications and searched the reference lists of selected articles. Existing research suggests that many well established risk factors for suicide (such as depression, hopelessness, and impulsivity) do not predict suicide attempts among adolescents who have suicidal thoughts or engage in non-suicidal self-harm. Longitudinal studies investigating predictors of future suicide attempts in these high-risk groups are extremely scarce.
Added value of this study
This is the first population-based birth cohort study to explore predictors of future suicide attempts among adolescents who have suicidal thoughts or engage in non-suicidal self-harm. We were able to explore associations with a wide range of prospectively recorded risk factors from different domains. Previous studies have used either cross-sectional study designs (thereby limiting causal inference because they rely on recall of both risk factors and suicidal behaviour) or clinical (or atypical) cohorts with small sample sizes and few risk factor data. Among participants with suicidal thoughts, we found that the strongest predictors of transition to attempts were non-suicidal self-harm, cannabis use, other illicit drug use, exposure to self-harm, and higher levels of the personality type intellect/openness. Among participants with non-suicidal self-harm at baseline, the strongest predictors were cannabis use, other illicit drug use, sleep problems, and lower levels of the personality type extraversion.
Implications of all the available evidence
Our findings could help practitioners to identify which adolescents are at greatest risk of attempting suicide in the future, which could lead to improved targeting of prevention and intervention strategies.
An important limitation of previous research is a reliance on cross-sectional studies and the retrospective reporting of both risk factors and suicide-related outcomes. Such studies can be subject to recall bias, and the temporal direction of associations is often unclear. Longitudinal studies adopting an ideation-to-action framework are extremely scarce,8, 22 and the few existing studies have been done in clinical or atypical samples (university students).21, 23, 24 We aimed to extend previous work by using longitudinal data to explore associations between a comprehensive range of prospectively recorded risk factors and first-time suicide attempts among adolescents with suicidal thoughts and non-suicidal self-harm. Associations were explored in a community-based sample that was more than twice as large as those used in previous longitudinal investigations.
Methods
Participants
The Avon Longitudinal Study of Parents And Children (ALSPAC) is an ongoing population-based birth cohort study examining influences on health and development across the life course. The ALSPAC core enrolled sample consists of 14 541 pregnant women resident in the former county of Avon in southwest England (UK), with expected delivery dates between April 1, 1991, and Dec 31, 1992.25, 26 Of the 14 062 livebirths, 13 798 were singletons or first-born of twins and were alive at 1 year of age. Participants have been followed up regularly since recruitment through questionnaires and research clinics. The study website contains details of all the data that are available through a fully searchable data dictionary. Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees.
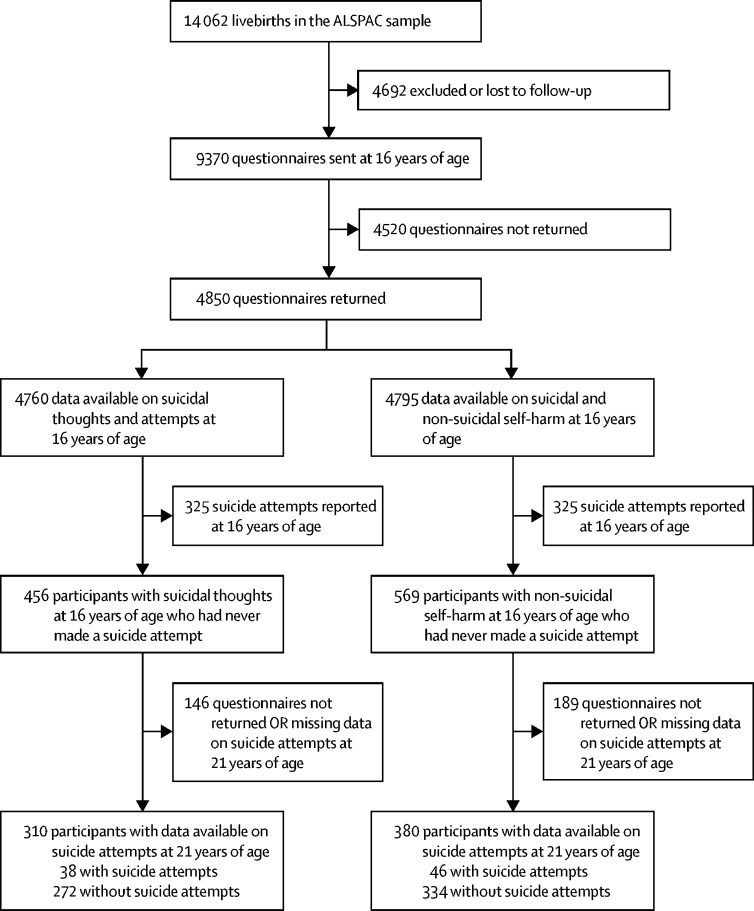
This investigation is based on the subsample of participants who completed a detailed self-report questionnaire on suicidal thoughts and self-harm at 16 and 21 years of age. Two samples were used for analysis. The first sample included adolescents who reported suicidal thoughts at baseline (n=456), assessed with the question, “Have you ever thought of killing yourself, even if you would not really do it?”. The second sample included adolescents who reported non-suicidal self-harm at baseline (n=569), assessed with the question, “Have you ever hurt yourself on purpose in any way (eg, by taking an overdose of pills, or by cutting yourself)?”. Participants who reported having attempted suicide at the age of 16 years (n=325) were excluded to focus on predictors of first-time suicide attempts.
Measures
Participants were classified according to whether they reported having ever attempted suicide at 21 years of age. Individuals who indicated having self-harmed, which was assessed by answering “yes” to the question “have you ever hurt yourself on purpose in any way (eg, by taking an overdose of pills or by cutting yourself)?”, were then asked a series of follow-up questions to establish suicidal intent. Participants were classified as having self-harmed with suicidal intent if they either gave the answer “I wanted to die” when asked to give reasons for self-harming or answered “yes” to: “On any of the occasions when you have hurt yourself on purpose, have you ever seriously wanted to kill yourself?”. Suicide attempts were assessed in the same way at 16 years of age.
A description of the risk factors examined in this study is provided in table 1. These risk factors are all known to be associated with self-harm, and their selection was informed by psychological models of suicide and by previous scientific literature. The risk factors included sex, intelligence quotient, executive function, impulsivity, sensation seeking, personality traits, exposure to self-harm in others, life events, early adversity, body dissatisfaction, sleep problems, psychiatric disorders, hopelessness, symptoms of depression, substance use, suicidal plans, and non-suicidal self-harm characteristics. All risk factors were assessed at or before the assessment at 16 years of age.
Table 1.
Risk factors
| Age at assessment | Measure used | Rater | Additional information | ||
|---|---|---|---|---|---|
| Demographic variables | |||||
| Sex | Birth | Questionnaire item | Mother | None | |
| Psychosocial variables | |||||
| Intelligence quotient | 8 years | Wechsler Intelligence Test for Children, third edition | Child | None | |
| Executive function | |||||
| Updating | 8 years | Wechsler Intelligence Test for Children, third edition | Child | Digit span task | |
| Attentional switching | 8 years | The adapted Test-of-Everyday-Attention-for-Children | Child | The dual-attention task of the Sky-Search subtest | |
| Attentional control | 8 years | The adapted Test-of-Everyday-Attention-for-Children | Child | The inhibition aspect of the Opposite Worlds task | |
| Impulsivity | 10 years | Stop-signal task | Child | Number of correct trials (lower scores indicate higher impulsivity) | |
| Sensation seeking | 16 years | Arnett inventory of sensation-seeking scale | Child | Novelty and intensity subscales | |
| Big five personality dimensions | 14 years | International personality item pool | Child | Five subscales (extraversion, agreeableness, conscientiousness, emotional stability, and intellect/openness) | |
| Family self-harm | |||||
| Parent suicide attempt | Repeated eight times from birth to 11 years | Questionnaire item | Mother | Lifetime rating | |
| Self-harm in family member | 16 years | Questionnaire item | Child | Lifetime rating | |
| Friend self-harm | 16 years | Questionnaire item | Child | Lifetime rating | |
| Number of life events | 16 years | Life events questionnaire | Child | Since age of 12 years | |
| Early adversity* | |||||
| Childhood sexual abuse | Repeated seven times from birth to eight years | Questionnaire item | Mother | None | |
| Cruelty to children in household | Repeated eight times from birth to 11 years | Questionnaire item | Mother | None | |
| Being bullied | 12 years | Modified version of the bullying and friendship interview schedule | Child | Overt or relational bullying at least once a week over the previous 6 months | |
| Body dissatisfaction | 13 years | Questionnaire item | Unhappy or happy over the past year | ||
| Sleep problems | |||||
| Waking in the night | 15 years | Questionnaire item | Child | Usually wakes at least once a night | |
| Insufficient sleep | 15 years | Questionnaire item | Child | Feels as though usually has too little sleep | |
| Psychiatric or mental health variables | |||||
| Psychiatric disorder | 15 years | DAWBA | Child | None | |
| Depression symptoms | 16 years | Short Mood and Feelings Questionnaire | Child | None | |
| Hopelessness | 16 years | Community Assessment of Psychic Experience | Child | Two items used: “Have you felt pessimistic about everything?” and “Have you felt as if there is no future for you?” | |
| Substance use | |||||
| Alcohol | 15 years | Questionnaire items | Child | Consuming at least four drinks on a typical occasion in the previous 6 months | |
| Cannabis | 15 years | Questionnaire items | Child | At least occasional use | |
| Smoking | 15 years | Questionnaire items | Child | Regular smoking (at least weekly) | |
| Illicit drugs (other than cannabis) | 15 years | Questionnaire items | Child | Past year | |
| Suicidal plans | 16 years | Questionnaire item | Child | Lifetime history | |
| Non-suicidal self-harm | 16 years | Questionnaire item | Child | Lifetime history | |
| Features of non-suicidal self-harm | |||||
| Frequency | 16 years | Questionnaire item | Child | Frequency of self-harm over the past year, coded as no history of self-harm, not in past year, 1–5 times, and ≥6 times. Because of small numbers, we combined together the original categories “once” and “2–5” and the categories “6–10” and “10+”. | |
| Method of self-harm | 16 years | Questionnaire item | Child | Method used on most recent episode. Coded as no history of self-harm, cutting, other, and more than one method. | |
DAWBA=Development and Well-Being Assessment.
A composite variable was created because of the low prevalence of individual adversities. This binary (yes or no) measure was derived from responses to questions on sexual abuse, parental cruelty to children in the household, and being bullied.
Additional analyses controlled for the possible confounding effects of child sex and socioeconomic position. Socioeconomic position was assessed by a maternal questionnaire and included average weekly household disposable income recorded at the ages of 3 and 4 years; highest maternal or paternal social class, assessed during pregnancy (professional or managerial, or other); and highest maternal educational attainment, assessed during pregnancy (less than O level, O level, A level, or university degree).
Statistical analysis
We used logistic regression analyses to examine associations between prospectively recorded risk factors and suicide attempts reported at the age of 21 years. We adjusted for potentially confounding effects of sex and socioeconomic position, but we did not adjust for additional confounders because our aim was to identify potential risk factors for the transition to suicide attempts, rather than to build the most parsimonious prediction model. Continuous risk factors were standardised before analysis to create Z scores with a mean of 0 and an SD of 1.
Our analyses were done on an imputed dataset based on participants who reported suicidal thoughts (n=456) and non-suicidal self-harm (n=569) at baseline. We used multiple imputation by chained equations27, 28 to generate 50 imputed datasets for each exposure of interest. This method assumes that data are missing at random, whereby any systematic differences between the missing and the observed values can be explained by differences in observed data. Comparison of the estimates from the complete case and imputed data analysis are presented in the appendix. For the non-suicidal group, we did a sensitivity analysis excluding individuals who reported having self-poisoned on the most recent self-harm occasion (appendix). We did all analyses using Stata, version 15.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Complete outcome data at 21 years of age were available for 310 participants with suicidal thoughts and 380 participants who had engaged in non-suicidal self-harm (figure). However, by use of the wealth of auxiliary data available in ALSPAC, we were able to impute up to the sample of adolescents with complete data on suicidal thoughts or non-suicidal self-harm at baseline. Participants with and without missing outcome data were found to be similar across a range of demographic variables (appendix); however, several differences were found between responders and non-responders to the self-harm questionnaire completed at 16 years of age (appendix). Participants who responded were more likely to be female and from more highly educated, affluent backgrounds. Findings were broadly consistent in the imputed and complete case analysis. 38 (12%) of 310 participants with suicidal thoughts and 46 (12%) of 380 participants who had engaged in non-suicidal self-harm reported having attempted suicide for the first time by the follow-up at 21 years of age. 107 participants reported both suicidal thoughts and non-suicidal self-harm at 16 years of age. Of these, 22 (21%) reported having attempted suicide by the follow-up at 21 years of age, compared with 32 (1%) of 2283 participants in the subsample who did not report either suicidal thoughts or non-suicidal self-harm at baseline (see the appendix for the prevalence of risk factors in this subgroup). Demographic information for the samples is shown in table 2.
Figure.
Flow-chart of attrition and self-harm outcomes in the Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort
Table 2.
Descriptive information for the complete case sample
|
Sample with suicidal thoughts at baseline |
Sample with non-suicidal self-harm at baseline |
|||
|---|---|---|---|---|
| No transition to attempts (n=272) | Transition to attempts (n=38) | No transition to attempts (n=334) | Transition to attempts (n=46) | |
| Child sex | ||||
| Male | 70 (26%) | 10 (26%) | 59 (18%) | 10 (22%) |
| Female | 202 (74%) | 28 (74%) | 275 (82%) | 36 (70%) |
| Maternal education | ||||
| A level or degree | 142 (52%) | 16 (42%) | 161 (49%) | 21 (46%) |
| O level | 85 (31%) | 15 (40%) | 117 (36%) | 17 (37%) |
| <O level | 44 (16%) | 7 (18%) | 51 (16%) | 8 (17%) |
| Parental social class | ||||
| Professional or managerial | 174 (66%) | 23 (66%) | 213 (67%) | 26 (59%) |
| Other | 88 (34%) | 12 (34%) | 106 (33%) | 18 (41%) |
Data are n (%). Numbers vary because of missing data.
Table 3 shows associations between each risk factor and future suicide attempts among the subsample with suicidal thoughts at baseline. In both unadjusted and adjusted analyses, the strongest evidence for an association was found for cannabis use (adjusted odds ratio [OR] 2·61, 95% CI 1·11–6·14; p=0·029), other illicit drug use (2·47, 1·02–5·96; p=0·045), non-suicidal self-harm (2·78, 1·35–5·74; p=0·0059), and higher levels of the personality type intellect/openness (1·62, 1·06–2·46; p=0·025). There was also weak evidence of an association with exposure to self-harm in others (family member self-harm adjusted OR 2·03, 95% CI 0·93–4·44, p=0·076; friend self-harm 1·85, 0·93–3·69, p=0·081).
Table 3.
Predictors of incident suicide attempts among adolescents with suicidal thoughts at baseline
| Total sample | No transition to attempts | Transition to attempts | Unadjusted odds ratio (95% CI) | p value | Adjusted odds ratio*(95% CI) | p value | ||
|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||
| Male | 27% | 27% | 26% | 1 (ref) | .. | 1 (ref) | .. | |
| Female | 73% | 73% | 74% | 1·09 (0·51–2·31) | 0·822 | 1·01 (0·47–2·18) | 0·975 | |
| Psychosocial variables | ||||||||
| Intelligence quotient | 108·1 (16·4) | 108·7 (16·09) | 105·8 (16·96) | 0·84 (0·58–1·21) | 0·347 | 0·92 (0·60–1·42) | 0·716 | |
| Executive function | ||||||||
| Updating | 13·2 (2·81) | 13·2 (2·81) | 12·9 (2·56) | 0·89 (0·62–1·26) | 0·504 | 0·94 (0·64–1·37) | 0·742 | |
| Attentional switching | 11·3 (14·48) | 11·5 (15·19) | 12·2 (15·7) | 1·03 (0·72–1·47) | 0·880 | 0·99 (0·68–1·45) | 0·968 | |
| Attentional control | 17·9 (15·61) | 17·1 (4·33) | 17·7 (3·78) | 1·13 (0·84–1·52) | 0·418 | 1·11 (0·81–1·51) | 0·528 | |
| Impulsivity | 13·9 (2·38) | 14·0 (2·23) | 13·4 (3·03) | 0·80 (0·57–1·14) | 0·221 | 0·80 (0·56–1·15) | 0·228 | |
| Sensation seeking | ||||||||
| Arnett intensity subscale | 26·0 (4·76) | 25·9 (4·73) | 26·5 (4·90) | 1·15 (0·83–1·60) | 0·412 | 1·20 (0·85–1·70) | 0·290 | |
| Arnett novelty subscale | 26·1 (4·50) | 26·0 (4·51) | 26·8 (4·34) | 1·21 (0·86–1·73) | 0·275 | 1·27 (0·88–1·82) | 0·201 | |
| Big five personality dimensions | ||||||||
| Extraversion | 33·2 (7·81) | 33·2 (7·93) | 33·2 (7·18) | 1·00 (0·69–1·45) | 0·990 | 1·00 (0·68–1·47) | 0·992 | |
| Agreeableness | 39·3 (4·91) | 39·3 (4·92) | 39·5 (4·87) | 1·05 (0·74–1·47) | 0·795 | 1·08 (0·73–1·59) | 0·693 | |
| Conscientiousness | 31·2 (5·93) | 31·3 (5·88) | 30·8 (6·19) | 0·93 (0·62–1·40) | 0·717 | 0·90 (0·59–1·38) | 0·639 | |
| Emotional stability | 28·0 (6·44) | 28·1 (6·44) | 27·5 (6·40) | 0·90 (0·61–1·32) | 0·588 | 0·91 (0·60–1·38) | 0·657 | |
| Intellect/openness | 36·8 (5·62) | 36·5 (5·58) | 38·5 (5·52) | 1·47 (0·98–2·19) | 0·061 | 1·62 (1·06–2·46) | 0·025 | |
| Family self-harm | 19% | 17% | 29% | 2·04 (0·94–4·41) | 0·070 | 2·03 (0·93–4·44) | 0·076 | |
| Friend self-harm | 61% | 59% | 72% | 1·82 (0·93–3·55) | 0·079 | 1·85 (0·93–3·69) | 0·081 | |
| Life events | 3·9 (2·28) | 3·9 (2·31) | 3·8 (2·07) | 0·92 (0·67–1·28) | 0·629 | 0·90 (0·65–1·24) | 0·511 | |
| Early adversity | 44% | 45% | 38% | 0·73 (0·30–1·74) | 0·473 | 0·75 (0·31–1·81) | 0·513 | |
| Body dissatisfaction | 44% | 44% | 43% | 0·95 (0·47–1·91) | 0·874 | 0·95 (0·45–1·98) | 0·883 | |
| Sleep problems | ||||||||
| Waking in the night | 55% | 55% | 58% | 1·14 (0·56–2·31) | 0·710 | 1·05 (0·51–2·18) | 0·895 | |
| Insufficient sleep | 50% | 52% | 40% | 0·62 (0·27–1·41) | 0·250 | 0·59 (0·25–1·39) | 0·224 | |
| Psychiatric or mental health variables | ||||||||
| Any DAWBA diagnosis | 12% | 11% | 14% | 1·26 (0·41–3·81) | 0·685 | 1·12 (0·35–3·63) | 0·844 | |
| Hopelessness | 42% | 39% | 56% | 1·61 (0·85–3·07) | 0·144 | 1·65 (0·85–3·18) | 0·137 | |
| Depression symptoms | 11·1 (6·25) | 11·1 (6·19) | 11·5 (6·62) | 1·07 (0·76–1·51) | 0·702 | 1·06 (0·74–1·51) | 0·754 | |
| Substance use | ||||||||
| Alcohol, heavy drinking | 25% | 25% | 28% | 1·16 (0·46–2·92) | 0·749 | 1·11 (0·43–2·83) | 0·830 | |
| Cannabis, at least occasional use | 18% | 16% | 32% | 2·46 (1·08–5·62) | 0·033 | 2·61 (1·11–6·14) | 0·029 | |
| Smoking, at least weekly | 17% | 16% | 26% | 1·78 (0·63–5·00) | 0·271 | 1·70 (0·58–4·97) | 0·333 | |
| Other illicit drug use, past year | 18% | 16% | 33% | 2·50 (1·06–5·92) | 0·037 | 2·47 (1·02–5·96) | 0·045 | |
| Suicidal plans | 12% | 12% | 14% | 1·17 (0·41–3·37) | 0·771 | 1·15 (0·39–3·41) | 0·800 | |
| Non-suicidal self-harm | 35% | 32% | 54% | 2·47 (1·24–4·90) | 0·010 | 2·78 (1·35–5·74) | 0·006 | |
| Frequency (percentage of those with non-suicidal self-harm) | ||||||||
| Not in the last year | 42% | 39% | 51% | 1 (ref) | 0·401 | 1 (ref) | 0·517 | |
| 1–5 times | 36% | 39% | 26% | 0·49 (0·17–1·39) | .. | 0·53 (0·18–1·58) | .. | |
| ≥6 times | 22% | 22% | 23% | 0·81 (0·27–2·49) | .. | 0·92 (0·26–3·26) | .. | |
| Method used during most recent self-harm episode (percentage of those with non-suicidal self-harm) | ||||||||
| Cutting | 64% | 59% | 82% | 1 (ref) | 0·129 | 1 (ref) | 0·107 | |
| Other | 14% | Not shown† | Not shown† | 0·57 (0·16–2·08) | .. | 0·44 (0·11–1·83) | .. | |
| Multiple methods | 23% | Not shown† | Not shown† | 0·16 (0·02–1·18) | .. | 0·15 (0·02–1·16) | .. | |
Data are percentages or mean (SD). Sample numbers not shown because percentages are based on imputed data (n=456). DAWBA=Development and Well-Being Assessment.
Adjusted for sex and socioeconomic position.
Data censored to prevent disclosure due to small cell counts; continuous variables were standardised before analysis.
Table 4 shows associations between each risk factor and future suicide attempts among the subsample with non-suicidal self-harm at baseline. In both unadjusted and adjusted analyses, the strongest evidence predicting the transition to suicide attempts was found for cannabis use (adjusted OR 2·14, 95% CI 1·04–4·41; p=0·038), other illicit drug use (2·17, 1·10–4·27; p=0·025), and insufficient sleep (1·97, 1·02–3·81; p=0·043). There was also weak evidence of an association with waking in the night (adjusted OR 1·91, 95% CI 0·93–4·44; p=0·069) and lower levels of the personality type extraversion (0·71, 0·49–1·03; p=0·068).
Table 4.
Predictors of incident suicide attempts among adolescents with non-suicidal self-harm at baseline
| Total sample | No transition to attempts | Transition to attempts | Unadjusted odd ratio (95% CI) | p value | Adjusted odds ratio*(95% CI) | p value | ||
|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||
| Male | 20% | 20% | 22% | 1 (ref) | .. | 1 (ref) | .. | |
| Female | 80% | 80% | 78% | 0·87 (0·42–1·80) | 0·711 | 0·82 (0·39–1·72) | 0·596 | |
| Psychosocial variables | ||||||||
| Total intelligence quotient (age 8 years) | 109·3 (14·79) | 109·4 (14·66) | 108·4 (15·47) | 0·94 (0·67–1·32) | 0·711 | 0·99 (0·67–1·46) | 0·944 | |
| Executive function | ||||||||
| Updating | 13·4 (2·74) | 13·5 (2·77) | 13·2 (2·52) | 0·88 (0·64–1·20) | 0·421 | 0·90 (0·64–1·27) | 0·552 | |
| Attentional switching | 10·8 (11·74) | 10·7 (11·82) | 11·1 (11·23) | 0·99 (0·67–1·46) | 0·959 | 0·98 (0·65–1·48) | 0·931 | |
| Attentional control | 16·9 (3·71) | 16·9 (3·67) | 17·1 (3·89) | 1·06 (0·77–1·45) | 0·725 | 1·02 (0·74–1·42) | 0·886 | |
| Impulsivity | 13·7 (2·59) | 13·8 (2·54) | 13·5 (2·81) | 0·93 (0·64–1·33) | 0·672 | 0·92 (0·64–1·34) | 0·670 | |
| Sensation seeking | ||||||||
| Arnett intensity subscale | 26·2 (4·81) | 26·2 (4·78) | 26·2 (4·97) | 1·01 (0·77–1·34) | 0·938 | 0·97 (0·72–1·31) | 0·848 | |
| Arnett novelty subscale | 26·6 (4·35) | 26·6 (4·30) | 26·9 (4·66) | 1·07 (0·81–1·41) | 0·625 | 1·06 (0·79–1·40) | 0·711 | |
| Big five personality dimensions | ||||||||
| Extraversion | 35·3 (6·99) | 35·6 (6·83) | 33·4 (7·53) | 0·73 (0·52–1·03) | 0·072 | 0·71 (0·49–1·03) | 0·068 | |
| Agreeableness | 39·1 (4·89) | 39·1 (4·90) | 39·1 (4·82) | 0·99 (0·72–1·37) | 0·965 | 1·04 (0·73–1·47) | 0·837 | |
| Conscientiousness | 30·4 (6·11) | 30·5 (6·18) | 30·3 (5·70) | 0·97 (0·71–1·32) | 0·826 | 0·95 (0·70–1·31) | 0·773 | |
| Emotional stability | 28·9 (6·52) | 29·1 (6·49) | 27·7 (6·52) | 0·80 (0·55–1·17) | 0·254 | 0·79 (0·53–1·17) | 0·237 | |
| Intellect/openness | 36·9 (5·83) | 36·7 (5·83) | 37·9 (5·73) | 1·24 (0·88–1·75) | 0·222 | 1·25 (0·87–1·81) | 0·221 | |
| Family self-harm | 18% | 18% | 23% | 1·38 (0·66–2·89) | 0·390 | 1·42 (0·66–3·05) | 0·364 | |
| Friend self-harm | 76% | 76% | 75% | 0·94 (0·49–1·79) | 0·851 | 0·97 (0·50–1·89) | 0·936 | |
| Life events | 3·7 (2·28) | 3·7 (2·30) | 3·8 (2·13) | 1·07 (0·79–1·45) | 0·680 | 1·09 (0·80–1·49) | 0·573 | |
| Early adversity | 35% | 33% | 36% | 1·13 (0·56 2·30) | 0·727 | 1·14 (0·56–2·35) | 0·712 | |
| Body dissatisfaction | 48% | 49% | 38% | 0·63 (0·33–1·20) | 0·160 | 0·63 (0·33–1·23) | 0·176 | |
| Sleep problems | ||||||||
| Waking in the night | 55% | 52% | 67% | 1·94 (1·01–3·73) | 0·047 | 1·91 (0·95–3·84) | 0·069 | |
| Insufficient sleep | 41% | 39% | 55% | 1·90 (1·00–3·59) | 0·049 | 1·97 (1·02–3·81) | 0·043 | |
| Psychiatric or mental health variables | ||||||||
| Any DAWBA diagnosis | 9% | Not shown† | Not shown† | 0·56 (0·13–2·35) | 0·428 | 0·54 (0·13–2·30) | 0·403 | |
| Hopelessness | 29% | 28% | 32% | 1·15 (0·58–2·26) | 0·691 | 1·20 (0·60–2·40) | 0·603 | |
| Depressive symptoms | 8·7 (5·94) | 8·7 (5·89) | 8·8 (6·27) | 1·01 (0·73–1·38) | 0·975 | 1·00 (0·73–1·38) | 0·996 | |
| Substance use | ||||||||
| Alcohol, heavy drinking | 29% | 32% | 27% | 0·79 (0·40–1·58) | 0·510 | 0·77 (0·38–1·54) | 0·452 | |
| Cannabis, at least occasional use | 20% | 18% | 32% | 2·15 (1·07–4·32) | 0·032 | 2·14 (1·04–4·41) | 0·038 | |
| Smoking, at least weekly | 16% | 14% | 26% | 2·09 (0·86–5·05) | 0·101 | 2·07 (0·83–5·13) | 0·116 | |
| Other illicit drug use, past year | 26% | 24% | 40% | 2·15 (1·10–4·19) | 0·025 | 2·17 (1·10–4·27) | 0·025 | |
| Suicidal plans | 4% | 4% | 8% | 2·17 (0·63–7·48) | 0·218 | 2·25 (0·62–8·12) | 0·215 | |
| Non-suicidal self-harm frequency | ||||||||
| Not in the last year | 48% | 48% | 51% | 1 (ref) | 0·622 | 1 (ref) | 0·599 | |
| 1–5 times | 39% | 40% | 34% | 0·80 (0·42–1·51) | .. | 0·83 (0·44–1·58) | .. | |
| ≥6 times | 13% | 13% | 16% | 1·19 (0·53–2·65) | .. | 1·29 (0·57–2·92) | .. | |
| Non-suicidal self-harm method used during most recent self-harm episode | ||||||||
| Cutting | 72% | 71% | 79% | 1 (ref) | 0·529 | 1 (ref) | 0·554 | |
| Other | 16% | 16% | 13% | 0·70 (0·29–1·69) | .. | 0·67 (0·27–1·65) | .. | |
| Multiple methods | 12% | 13% | 9% | 0·62 (0·21–1·83) | .. | 0·66 (0·22–1·99) | .. | |
Data are percentages or mean (SD). Sample numbers not shown because percentages are based on imputed data (n=569). DAWBA=Development and Well-Being Assessment.
Adjusted for sex and socioeconomic position.
Data censored to prevent disclosure because of small cell counts; continuous variables were standardised before analysis.
A small proportion (15 [4%] of 380) of adolescents in the non-suicidal self-harm group reported having self-poisoned on the most recent self-harm occasion; however, sensitivity analysis excluding these individuals did not change the pattern of results (appendix).
Discussion
To our knowledge, this is the largest longitudinal study to explore the transition to suicide attempts among adolescents with suicidal thoughts or non-suicidal self-harm. We identified several risk factors that predicted future suicide attempts in these high-risk groups. Among participants with suicidal thoughts at 16 years of age, future risk of suicide attempt was associated with non-suicidal self-harm history, cannabis use, other illicit drug use, higher intellect/openness score, and exposure to self-harm in others. This finding is consistent with a cross-sectional analysis of this cohort,9 which found substance use and exposure to self-harm differentiated between adolescents with suicidal thoughts and those who had attempted suicide at age 16 years. Both cannabis and other illicit drug use also predicted the transition to attempts among participants with non-suicidal self-harm at baseline, along with a lower extraversion score and sleep difficulties.
Although some differences were found in the predictors of transition for participants with suicidal thoughts and those with non-suicidal self-harm at baseline, other illicit drug use and cannabis use were identified in both samples, suggesting that these factors might be particularly robust predictors of future suicide attempt risk. Consistent with our findings, a previous meta-analysis5 found drug use moderately distinguished between adolescents with suicidal thoughts and attempts. However, a separate meta-analysis20 did not find an association with attempts among adolescents with non-suicidal self-harm. It is possible that substances such as cannabis and other illicit drugs increase suicide capability by lowering inhibitions and impairing decision making. It is also possible that drug use leads to mental illness over time, and this mental illness leads to suicide attempts. Alternatively, substance use might be a proxy for particular types of coping in response to stress that are maladaptive. There is also evidence to suggest that there might be a bidirectional relationship; several longitudinal studies29, 30, 31, 32, 33 have reported an association between adolescent self-harm and substance use problems in adulthood. Notably, we did not find evidence for an association with alcohol use or smoking in either sample, which highlights the importance of exploring relationships with different substances independently. Future research should explore whether associations differ for different forms of illicit drug use (eg, injection drug use).
Previous research suggests that non-suicidal self-harm is a robust predictor of future suicide attempts;15, 16, 17, 18, 19 however, non-suicidal self-harm has rarely been considered within an ideation-to-action framework. Our study extends previous work by demonstrating that non-suicidal self-harm is specifically associated with the transition from suicidal thinking to action. Several explanations for this association are possible, including shared neurobiological vulnerability to self-harm, an increased risk of social exclusion or mental illness as a result of non-suicidal self-harm,34 or a direct effect on reducing the inhibition to attempt suicide in the face of suicidal thoughts.2 Our findings are in line with those of a previous prospective community study of adolescents35 and indicate that those individuals who report both suicidal thoughts and non-suicidal self-harm might be an especially high-risk group. We found that approximately 1 in 5 (21%) of the adolescents who reported both suicidal thoughts and non-suicidal self-harm at baseline went on to make a suicide attempt, which compares with only 1% of those who did not report either of these behaviours. Despite the low prevalence, it is notable that this group accounted for approximately a quarter of participants who attempted suicide over the follow-up. In contrast to some previous studies,20, 21 we did not find characteristics of non-suicidal self-harm (such as method and frequency) to be strong predictors of future suicide attempts. This difference could be due to methodological differences in sample or definition of non-suicidal self-harm: for example, the timeframe of assessment (past year vs lifetime) or method choice (lifetime vs most recent). Alternatively, we might have been underpowered to detect effects; however, our sample size is more than twice as large as the only other longitudinal study21 exploring predictors of concurrent and future suicide attempts among adolescents with non-suicidal self-harm.
Other factors that were associated with future suicide attempts among participants with non-suicidal self-harm included sleep problems and a lower extraversion score. Both of these factors have been associated with suicidal behaviour in previous research;36, 37, 38, 39 however, our study is the first to explore prospectively the role of sleep difficulties and personality traits in the transition to suicide attempts over time. It might be that individuals who are less extraverted are more socially disconnected, which has been shown to predict future suicide attempts in a sample of university students with non-suicidal self-harm.21 Sleep problems could affect feelings of social connection by impairing an individual's ability and motivation to interact with others.40, 41 They might also have a more direct effect on suicide risk, leading to increased distress at a time when fewer social supports are available.
A growing number of cross-sectional studies have found that exposure to self-harm in others differentiates between adolescents with suicidal ideation and attempts.9, 10, 12, 13, 42 In this study, we found weak evidence to suggest that exposure to self-harm also predicts future suicide attempts in adolescents who have thought about suicide, but not among those who have been engaged in non-suicidal self-harm. One explanation is that self-harm exposure might increase the capability of suicide among adolescents with suicidal thoughts by increasing the salience and acceptability of self-harm (eg, increased awareness of self-harm as an option, its functional utility, and knowledge of methods),43 whereas those who have engaged in non-suicidal self-harm are already aware of self-harm methods. Further research will need to investigate the mechanisms by which exposure to self-harm in others increases the risk of suicide attempts. Potential candidate mechanisms include genetic influences, social transmission, imitation, and assortative relating among people at high risk.
It might appear surprising that we did not find evidence of an association for several well established suicide risk factors, including depression symptoms, psychiatric disorder, suicidal plans, and impulsivity. However, our results are consistent with previous research5, 20 that has suggested that these factors appear to be associated with suicide attempts because they are associated with the development of suicidal thoughts or non-suicidal self-harm, but are not involved in the transition. An alternative methodological explanation for this negative finding could be that we (in common with other large epidemiological studies) did not measure symptoms immediately before the suicide attempt, when there might have been a stronger association than at 16 years of age. The CIs for some predictors are also wide, and it is possible there is an association that we were underpowered to detect.
This study has many strengths, including the large population-based sample, longitudinal design, and ability to explore a wide range of prospectively recorded risk factors. The vast majority of research in this area has been cross-sectional, and therefore limited by retrospective reporting of both risk factors and outcomes. We also excluded people with a previous suicide attempt at baseline, which enabled us to establish the direction of effects between our measures and ensure that we were not modelling risk for repeat suicide attempts.
There are also several limitations to consider. First, it cannot be assumed that the associations identified in this study are causal. We adjusted only for two confounding variables (sex and socioeconomic position); however, it was not our aim to identify independent predictors, and to examine this adequately would require a separate theory-driven analytical model for each exposure. This analysis was beyond the scope of the current paper, but is an important area for future research. Second, information was not available on the date of the first suicide attempt. We therefore focused on risk factors that occurred at or before the age 16 years' assessment to ensure that they preceded the outcome. 5 years is a relatively long follow-up period, and risk factors that predict the transition to suicide attempts over the short term might differ from those that predict over the long term. Newly emerging methods of data collection, such as Ecological Momentary Assessment, could be used in future studies to explore predictors of transitions over a shorter timeframe (ie, hours, days, or weeks). Third, we excluded individuals who had attempted suicide before the age of 16 years so that we could examine predictors of incident suicide attempts. Although we consider this approach to be a strength of the study, it is possible that it weakened associations with some of our risk factors. For example, if a particular risk factor is strongly associated with suicide attempts (eg, suicidal plans), then it is more likely that individuals with that risk factor would have already attempted suicide, and therefore been excluded from the analyses. This means that our findings might not be applicable to individuals who have already attempted suicide by the age of 16 years. However, identifying individuals who will make a first attempt in late adolescence or young adulthood is important, because this is the age at which hospital presentations for self-harm are at their highest.44 Further longitudinal research is needed to explore whether there are differences in the risk factors for incident and repeat suicide attempts among individuals with current suicidal ideation. Fourth, we did not correct for multiple testing as analyses were exploratory. Our results are therefore in need of replication, given the large number of tests done. Finally, as with all longitudinal studies, there was some attrition over time that might have biased our complete case analyses. However, findings were similar using imputed data, suggesting that the effects of this potential bias were not substantial. Although we cannot say with certainty that our data are missing at random, ALSPAC contains a wealth of auxiliary data, which increases the plausibility of this assumption. There were also some differences between those individuals who did and did not respond to the age 16 years' self-harm questionnaire and this non-random response might limit the generalisability of our results.
Identification of factors that predict the transition from suicidal thoughts or non-suicidal self-harm to suicide attempts is crucial for improved suicide prediction and prevention. Although results of existing cross-sectional research have provided important information about the factors that differentiate between individuals with suicidal thoughts or non-suicidal self-harm and those with attempts, longitudinal studies such as this are required to investigate whether the identified factors predict the transition to attempts over time. Our findings suggest that asking about factors such as substance use, non-suicidal self-harm, sleep, personality traits, and exposure to self-harm might help clinicians to identify which adolescents are at greatest risk of attempting suicide in the future.
Acknowledgments
Acknowledgments
BM was supported by a grant from the American Foundation for Suicide Prevention (PDF-0-091-14) between January, 2016, and December, 2017, and has been supported by the National Institute for Health Research (NIHR) Biomedical Research Centre at the University Hospitals Bristol National Health Service Foundation Trust and the University of Bristol (Bristol, UK) since January, 2018. The UK Medical Research Council and Wellcome Trust (grant reference 102215/2/13/2) and the University of Bristol provide core support for the Avon Longitudinal Study of Parents and Children. The data used in this research were specifically funded by the Wellcome Trust (grant reference GR067797MA), Norwegian University of Science and Technology, and the NIHR (grant reference PR-RS-0912-11023). The views expressed in this publication are those of the authors and not necessarily those of the American Foundation for Suicide Prevention, the National Health Service, NIHR, or UK Department of Health. We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole Avon Longitudinal Study of Parents and Children team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses.
Contributors
BM, JH, EDK, PM, RCO'C, PW, KT, and DG contributed to conception and design of the study. BM, JH, and DG contributed to the organisation of the conduct of the study. BM carried out the study (including acquisition of data), analysed data, and drafted the output. BM, JH, EDK, PM, RCO'C, PW, KT, and DG contributed to interpretation of data. JH, EDK, PM, RCO'C, PW, KT, and DG critiqued the output for important intellectual content. All authors have read and approved the final version of the manuscript. BM serves as guarantor for the contents of this paper.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Nock MK, Green JG, Hwang I. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Connor RC, Kirtley OJ. The integrated motivational–volitional model of suicidal behaviour. Phil Trans R Soc B. 2018;373:20170268. doi: 10.1098/rstb.2017.0268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klonsky ED, May AM. The three-step theory (3ST): a new theory of suicide rooted in the “ideation-to-action” framework. Int J Cogn Ther. 2015;8:114–129. [Google Scholar]
- 5.May AM, Klonsky ED. What distinguishes suicide attempters from suicide ideators? A meta–analysis of potential factors. Clin Psychol. 2016;23:5–20. [Google Scholar]
- 6.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 7.Nock MK, Hwang I, Sampson N. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6:e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klonsky ED, Qiu T, Saffer BY. Recent advances in differentiating suicide attempters from suicide ideators. Curr Opin Psychiatry. 2017;30:15–20. doi: 10.1097/YCO.0000000000000294. [DOI] [PubMed] [Google Scholar]
- 9.Mars B, Heron J, Klonsky ED. What distinguishes adolescents with suicidal thoughts from those who have attempted suicide? A population-based birth cohort study. J Child Psychol Psychiatry. 2019;60:91–99. doi: 10.1111/jcpp.12878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asarnow JR, Baraff LJ, Berk M. Pediatric emergency department suicidal patients: two-site evaluation of suicide ideators, single attempters, and repeat attempters. J Am Acad Child Adolesc Psychiatry. 2008;47:958–966. doi: 10.1097/CHI.0b013e3181799ee8. [DOI] [PubMed] [Google Scholar]
- 11.Borges G, Benjet C, Medina-Mora ME, Orozco R, Nock M. Suicide ideation, plan, and attempt in the Mexican adolescent mental health survey. J Am Acad Child Adolesc Psychiatry. 2008;47:41–52. doi: 10.1097/chi.0b013e31815896ad. [DOI] [PubMed] [Google Scholar]
- 12.Dhingra K, Boduszek D, O'Connor RC. Differentiating suicide attempters from suicide ideators using the Integrated Motivational–Volitional model of suicidal behaviour. J Affect Disord. 2015;186:211–218. doi: 10.1016/j.jad.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 13.O'Connor RC, Rasmussen S, Hawton K. Distinguishing adolescents who think about self-harm from those who engage in self-harm. Br J Psychiatry. 2012;200:330–335. doi: 10.1192/bjp.bp.111.097808. [DOI] [PubMed] [Google Scholar]
- 14.Taliaferro LA, Muehlenkamp JJ. Risk and protective factors that distinguish adolescents who attempt suicide from those who only consider suicide in the past year. Suicide Life Threat Behav. 2014;44:6–22. doi: 10.1111/sltb.12046. [DOI] [PubMed] [Google Scholar]
- 15.Hamza CA, Stewart SL, Willoughby T. Examining the link between nonsuicidal self-injury and suicidal behavior: a review of the literature and an integrated model. Clin Psychol Rev. 2012;32:482–495. doi: 10.1016/j.cpr.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT) Am J Psychiatry. 2011;168:495–501. doi: 10.1176/appi.ajp.2010.10050718. [DOI] [PubMed] [Google Scholar]
- 17.Guan K, Fox KR, Prinstein MJ. Nonsuicidal self-injury as a time-invariant predictor of adolescent suicide ideation and attempts in a diverse community sample. J Consult Clin Psychol. 2012;80:842–849. doi: 10.1037/a0029429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asarnow JR, Porta G, Spirito A. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: findings from the TORDIA study. J Am Acad Child Adolesc Psychiatry. 2011;50:772–781. doi: 10.1016/j.jaac.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klonsky ED, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. J Abnorm Psychol. 2013;122:231–237. doi: 10.1037/a0030278. [DOI] [PubMed] [Google Scholar]
- 20.Victor SE, Klonsky ED. Correlates of suicide attempts among self-injurers: a meta-analysis. Clin Psychol Rev. 2014;34:282–297. doi: 10.1016/j.cpr.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 21.Whitlock J, Muehlenkamp J, Eckenrode J. Nonsuicidal self-injury as a gateway to suicide in young adults. J Adolesc Health. 2013;52:486–492. doi: 10.1016/j.jadohealth.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Burke TA, Alloy LB. Moving toward an ideation-to-action framework in suicide research: a commentary on May and Klonsky (2016) Clin Psychol. 2016;23:26–30. doi: 10.1111/cpsp.12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.May AM, Klonsky ED, Klein DN. Predicting future suicide attempts among depressed suicide ideators: a 10-year longitudinal study. J Psychiatr Res. 2012;46:946–952. doi: 10.1016/j.jpsychires.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qiu T, Klonsky ED, Klein DN. Hopelessness predicts suicide ideation but not attempts: a 10-year longitudinal study. Suicide Life Threat Behav. 2017;47:718–722. doi: 10.1111/sltb.12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boyd A, Golding J, Macleod J. Cohort profile: the ‘children of the 90s’—the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42:111–127. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fraser A, Macdonald-Wallis C, Tilling K. Cohort profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int J Epidemiol. 2013;42:97–110. doi: 10.1093/ije/dys066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Royston P, White IR. Multiple imputation by chained equations (MICE): implementation in Stata. J Stat Softw. 2011;45:1–20. [Google Scholar]
- 28.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20:40–49. doi: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moran P, Coffey C, Romaniuk H, Degenhardt L, Borschmann R, Patton G. Substance use in adulthood following adolescent self-harm: a population-based cohort study. Acta Psychiatr Scand. 2015;131:61–68. doi: 10.1111/acps.12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Borschmann R, Becker D, Coffey C. 20-year outcomes in adolescents who self-harm: a population-based cohort study. Lancet Child Adolesc Health. 2017;1:195–202. doi: 10.1016/S2352-4642(17)30007-X. [DOI] [PubMed] [Google Scholar]
- 31.Mars B, Heron J, Crane C. Clinical and social outcomes of adolescent self harm: population based birth cohort study. BMJ. 2014;349:g5954. doi: 10.1136/bmj.g5954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldman-Mellor S, Caspi A, Harrington H. Suicide attempt in young people: a signal for long-term healthcare and social needs. JAMA Psychiatry. 2014;71:119–127. doi: 10.1001/jamapsychiatry.2013.2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Suicidal behaviour in adolescence and subsequent mental health outcomes in young adulthood. Psychol Med. 2005;35:983–994. doi: 10.1017/s0033291704004167. [DOI] [PubMed] [Google Scholar]
- 34.Wilkinson PO, Qiu T, Neufeld S, Jones PB, Goodyer IM. Sporadic and recurrent non-suicidal self-injury before age 14 and incident onset of psychiatric disorders by 17 years: prospective cohort study. Br J Psychiatry. 2018;212:222–226. doi: 10.1192/bjp.2017.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scott LN, Pilkonis PA, Hipwell AE, Keenan K, Stepp SD. Non-suicidal self-injury and suicidal ideation as predictors of suicide attempts in adolescent girls: a multi-wave prospective study. Compr Psychiatry. 2015;58:1–10. doi: 10.1016/j.comppsych.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O'Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1:73–85. doi: 10.1016/S2215-0366(14)70222-6. [DOI] [PubMed] [Google Scholar]
- 37.Hysing M, Stormark KM, O'Connor RC. Sleep problems and self-harm in adolescence. Br J Psychiatry. 2015;207:306–312. doi: 10.1192/bjp.bp.114.146514. [DOI] [PubMed] [Google Scholar]
- 38.Wong MM, Brower KJ, Craun EA. Insomnia symptoms and suicidality in the national comorbidity survey–adolescent supplement. J Psychiatr Res. 2016;81:1–8. doi: 10.1016/j.jpsychires.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73:e1160–e1167. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- 40.Roberts RE, Roberts CR, Chen IG. Functioning of adolescents with symptoms of disturbed sleep. J Youth Adolesc. 2001;30:1–18. [Google Scholar]
- 41.Beattie L, Kyle SD, Espie CA, Biello SM. Social interactions, emotion and sleep: a systematic review and research agenda. Sleep Med Rev. 2015;24:83–100. doi: 10.1016/j.smrv.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 42.Wetherall K, Cleare S, Eschle S. From ideation to action: differentiating between those who think about suicide and those who attempt suicide in a national study of young adults. J Affect Disord. 2018;241:475–483. doi: 10.1016/j.jad.2018.07.074. [DOI] [PubMed] [Google Scholar]
- 43.Rasmussen S, Hawton K. Adolescent self-harm: a school-based study in Northern Ireland. J Affect Disord. 2014;159:46–52. doi: 10.1016/j.jad.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 44.Hawton K, Bergen H, Casey D. Self-harm in England: a tale of three cities. Soc Psychiatry Psychiatr Epidemiol. 2007;42:513–521. doi: 10.1007/s00127-007-0199-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.