Abstract
Introduction: One of the major complains after surgery is pain. Recent advances in the prevention and reduction of postoperative pain have provided several modalities. One of them is the use of laser irradiation on the surgical area.
Objectives: To evaluate the effects of low level laser therapy (LLLT) on pain and side effects after surgery.
Methods: In this research, databases such as: PubMed, Science Direct, Google Scholar, Springer and Cochrane were used and the words of laser therapy, photobiomodulation, therapeutic laser, low level laser therapy, surgery and pain were searched. Articles, including systematic reviews, original articles, case series, and clinical intervention studies related to these words, were studied. The language of all articles was English and consists of papers from 2009 until 2017.
Results: A total of 370 papers were studied and 10 articles that met inclusion criteria were selected for this review. Few of these articles were followed up. Surgery included a wide range of surgeries including mastectomy, breast augment post-fracture, episiotomy, tonsillectomy and hernia. The methodological quality score on the PEDro scale was between 5 and 11. 8 trials reported positive effects and 2 trials reported negative effects. In order to study clinical effect size of laser therapy after surgery, only 4 papers met entry criteria and the mean effect sizes were 0.13 to 2.77. Accordingly, the best treatment protocol included a red laser dose of 4 J/cm2 for the post-operative pain of tonsillectomy, which was irradiated through the infra mandibular angle on the tonsils.
Conclusion: LLLT may be an appropriate modality for reducing pain after surgery, nevertheless the effect size of this modality is variable. Therefore, further research based on proper protocols for these patients and follow-up of therapeutic course should be designed and implemented.
Keywords: Photobiomodulation, Low level laser therapy, Surgery, Pain
Introduction
Postoperative pain is an unpleasant complaint of surgeries and insufficient attention to pain relief may delay and change the recovery cycles and leads to enormous costs which society has to bear.1 Unfavorable effects of postoperative pain can involve other parts of the body that may not be related to the surgical cut. These impairments include deep vein thrombosis, impaired function of pulmonary and cardiovascular systems, inappropriate wound healing, insomnia and weakening morale1,2 which might result in increasing rate of mortality and morbidity.1 Pain that lasts for a long time can become chronic.3
There are different ways to reduce postoperative pain such as surgical blockage of pain transmitted neurons, non-opioid drugs or non-steroidal anti-inflammatory drugs (NSAIDs), opioid analgesic or patients controlled analgesia (PCA) and epidural analgesia.2,4-6 Surgical blockage effects on reducing pain is temporary and pain will come back after a while.7 Also, because of the side effects of above drugs, the use of adequate dosage is limited.4,5-8
Recently, new methods have been proposed to reduce pain after surgery. One of these novel methods is low-level laser therapy (LLLT).9 LLLT means the use of low-power radiations which is between 5-500 mW. Its effects are non-thermal9,10 that are used for different goals such as healing, pain relief and reducing inflammation.10-14
It was suggested that analgesic effects of LLLT are probably related to increased secretion of endorphin in inflammation sites and enhanced circulation.15 In addition, it was believed LLLT can help the release of neurotransmitters, for example serotonin that improves endorphin’s performance.16 Furhtermore, LLLT decreases the level of pain-related factors such as prostaglandin E2 and cyclooxygenase-2.17 Other mechanisms for reducing pain of LLLT are caused by declining in nociceptor signal transduction.18
LLLT evidently degraded pain in chronic and acute status19,20 like carpal tunnel syndrome (CTS),21 osteoarthritis, rheumatoid arthritis,22 fibromyalgia,23 temporomandibular disorders.19 As well as LLLT has been used to relieve pain in postoperative pain.24 But, there was not any systematic review that studies the role of LLLT in improving postoperative pain. So, the aim of this study was to systematically review of evidence regarding the effects of LLLT on postoperative pain.
Methods
Search Strategy
A systematic search was performed using the following databases: PubMed, Science Direct, Google Scholar, Springer and Cochrane. Two reviewers accomplished the search. The language of all articles was English and consists of papers from 2009 until 2017. The keywords included laser therapy, photobiomodulation, therapeutic laser, low-level laser therapy, surgery and pain. Also, we used Medical Subjects Heading in PubMed that included: laser therapy, pain, surgery, low-level therapy and postoperation. References of all full-text of papers were manually searched to recognize additional related studies. All articles, including systematic reviews, original article, case series, and clinical intervention studies related to these words, were studied.
Inclusion and Exclusion Criteria
1) Papers should be randomized control trial.
2) The effect of laser on postoperative pain was investigated.
3) The severity of pain was evaluated as outcome measures.
4) The language was English.
As well the exclusion criteria were: (1) Trials not having control groups (2) Trials that compare laser therapy with other types of therapeutic modalities such as ultrasound.
Data Collection
Data were obtained by two independent reviewers. Each reviewer, individually evaluate the abstracts of the articles. If they were related to the topic of the present study, read the full-text of them. Then, the factors related to the articles, including the type of paper, subjects, interventions, the method of evaluation and results were recorded. If there were any differences among 2 reviewers, the third reviewer was consulted.
Qualitative Evaluation of Clinical Trials
The PEDro scale was used to evaluate the quality of the articles. The PEDro scale is introduced by the PEDro database and includes 11 criteria for evaluating clinical trial’s validity. Articles with less than 5 entries were deleted.
Effect Size
At first, the difference between the mean pain intensity (visual analogue scale, VAS) before the intervention and the mean pain intensity after the intervention were calculated separately in each group and then we divided the obtained values into standard deviation (SD) of one of the means in the same group. The numerical value obtained represents the size of the effect in that group.
Results
Literature Search
A total of 1194 papers were found. After removing duplicated 370 articles remain. By studying their titles and abstracts, 349 studies were excluded and full-text of 21 remained papers was assessed for eligibility. Seven of them were eliminated due to lack of eligible subjects and 4 of them were eliminated due to lack of eligible method. Finally, 10 articles that met the desired inclusion criteria were selected for this study (Figure 1 and Table 1). Few of these articles were followed up. The evidence obtained from the papers is shown in the tables 1 and 2. These tables contain information about (1) author, (year) (2) subjects, (3) inclusion criteria, (4) method and (5) results. Also the parameters of laser therapy including wavelength, dosage, duration of irradiation per point and location of irradiation about these 10 articles is shown in Table 2).
Figure 1.
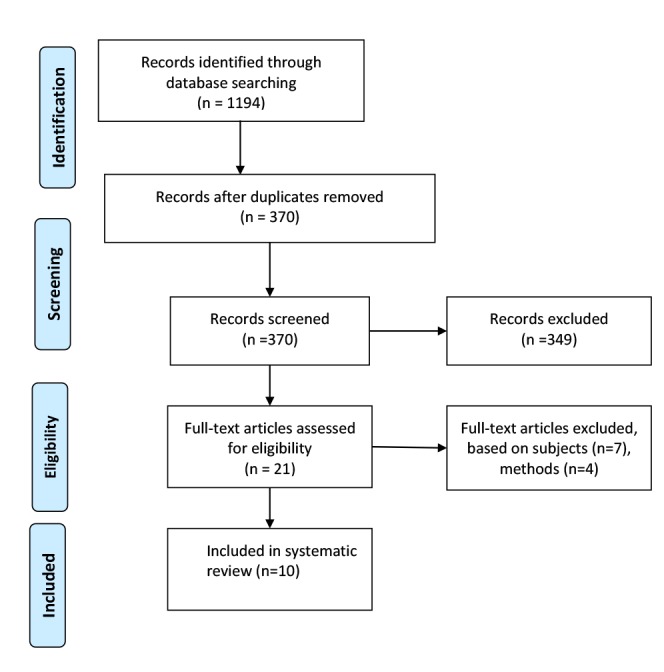
Chart of Screening and Search History.
Table 1. Characteristics of Papers Used in This Review .
| Author (Y) | Subjects | Main Inclusion Criteria | Method | Result |
| Kozanoglu25 (2009) |
n= 47 Mean age = 45-51 y |
Patients with history of postmastectomy arm lymphoedema for at least 3 months. |
Group I - pneumatic compression group (n=24): Intermittent pneumatic compression therapy was applied for 2 hours, 3 times a week for 4 weeks. Group II - LLLT group (n=23): LLLT was applied for 20 min, 3 times a week for 4 weeks. |
There was no significant difference in pain severity between the 2 groups. |
| Jackson26 (2009) |
n= 104 Age=18-55 y |
Patient who were nominated for breast augmentation surgery. |
Group I – LLLT group (n=50): LLLT was applied after 10 minutes of the start of surgery, 10 min, 24 h and 1 week after surgery. Group II – control group (n=54) a sham red light was applied. |
The pain was significantly reduced following the use of the LLLT, and the dose of medication was reduced at 1 day and 1 week in LLLT group compared to other group. |
| Carvalho27 (2009) |
n=28 Mean age=47 y |
Patients who had surgery for an inguinal hernia. |
Group I – LLLT group (n=14): LLLT was applied on the first day after surgery and then on days 3, 5, and 7. Group II – control group (n=14): No treatment was used. |
The average of severity of pain in the placebo group is much greater than that of the LLLT group. |
| Neiva28 (2009) |
n=18 Age = 5-15 y |
- Patients who had underwent tonsillectomy. - Aged 5-15 years. |
Group I – LLLT group (n=9): LLLT was applied intraoperatively, immediately after the surgery, on the first day and 24 h after surgery. Group II – control group (n=9) LLLT was applied 24 h after surgery. |
LLLT reduced postoperative pain significantly and deceased dose of medication was. |
| Santos29 (2012) |
n=52 Age ≥18 y |
- Postpartum women with mediolateral episiotomies. - Age ≥18 y - Do not have any vaginal delivery. |
Group I – LLLT group (n=26): LLLT was used in 3 sessions: up to 2 h, between 20-24 and between 40-48 h after delivery. Group II – control group (n=26): placebo laser was applied. |
Postoperative pain was reduced in LLLT group. |
| Santos30 (2012) |
n=114 Age ≥18 y |
-Women who had right mediolateral episiotomies during vaginal delivery. - Having pain ≥3 on VAS. - Age ≥18 y. |
Group I – inferred LLLT group (n=38) Group II – red LLLT group (n=38): Both LLLT groups were received laser in one session between 6–56 h after delivery. Group III – control group (n=38): placebo laser was applied. |
LLLT was not effective in reduction of pain. |
|
Aghamohammadi31
(2013) |
n=60 Age=20-40 y |
- Patients underwent tonsillectomy. - Age between 20-40. |
Group I – LLLT group (n=30): The tonsils’ bed treated by infrared laser. Group II – control group (n=30): The tonsils’ bed treated by placebo laser. |
The use of LLLT decreased postoperative pain significantly and decreased using analgesics. |
|
Nesioonpour24
(2014) |
n=54 Age=18-60 y |
- Patients who had tibial fracture surgery. - Age between 18-60. |
Group I – LLLT group (n=27): After operation and before the terminal bandage, combination of 2 lasers were used . Group II – control group (n=27): Placebo laser was used. |
Postoperative pain reduced in LLLT group and had longer effect. |
|
Karlekar32
(2015) |
n=100 Age ≥18 y |
- Patients who had candidate for coronary artery bypass graft through sternotomy. - Aged 18 years or older. |
Group I – LLLT group (n=40): LLLT was applied 1, 30 min after surgery and following tracheal extubation for once a day. Group II – (n=60): LLT was applied 1, 30 min after surgery and following tracheal extubation for once a day, this process was repeated after 2 days if VRS was greater than 5. |
Postoperative pain significantly reduced after LLLT. |
|
Fernandes33
(2017) |
n=90 Age=18-75 who |
Patients who had candidate for coronary artery bypass surgery with a longitudinal sternotomy incision and extracorporeal circulation. - Ages 18-75 years. - Having stable hemodynamic system. - Having BMI lesser than 29.9 kg/m2. |
Group I: control group (n=30): No treatment was used. Group II: placebo group (n=30): placebo laser was used 6–56 h after delivery. Group III: LLLT group (n=30): LLLT was used instantly after surgery and on days of 2, 4, 6, and 8. |
LLLT could effectively decrease pain after coronary-?arterial bypass grafting. |
Table 2. Parameters of Laser Irradiations in Trials .
| Author (Year) | Laser Wave Length | Laser Dosage | Duration of Irradiation Per Point | Location of Irradiation |
| Kozanoglu25 (2009) | 904 nm | 1.5 J/cm2 | 20 min | 3 points at the antecubital fossa and 7 points on the axilla. |
| Jackson26 (2009) | 630–640 nm | 4 min | Scanned laser above each breast. | |
| Carvalho27 (2009) | 830 nm | 10.4 J/cm2 | 26 s/point | 10 points in each scar. |
| Neiva28 (2009) | 685 nm | 4 J/cm2 | 3 min and 20 s | Surgical wounds. |
| Santos29 (2012) | 660 nm | 3.8 j/ cm2 | 10 s/point | 3 points of the episiotomy (upper, central and lower). |
| Santos30 (2012) |
Red light irradiation beams: 660 nm Infrared laser diode: 780 nm |
8.8 j/ cm2 | 10 s/point | 3 points of the episiotomy (upper, central and lower). |
| Aghamohammadi31 (2013) | 980 nm | 4 J/cm2 | From mandibular angle irradiated to the tonsils’ bed. | |
| Nesioonpour24 (2014) | Combination of 2 lasers: 808 nm; and 650 nm | 9 J/cm2 | 20 s/point | Anterior, posterior, medial and lateral sides of fracture area and popliteal fossa |
| Karlekar32 (2015) | 980 nm | 10 J/cm2 | 150 s/point | Around the sternum. |
| Fernandes33 (2017) | 660 nm | 6 J/cm2 | 60 s/point | 8 points around the incision. |
Qualitative Evaluation of Clinical Trials
The quality assessment of the 10 trials used in this study is shown in Table 3. The magnitude of this scale was between 5 and 11, with an average score of 9/1. In 8 articles, the random allocation of samples was done and only in 2 articles was not observed. In 7 articles the subjects, in 6 articles the therapist and in 6 articles the examiner were blinded, respectively.
Table 3. Results of Assessment of Quality of Studies by PEDro Scale .
| Author | Cri1 | Cri2 | Cri3 | Cri4 | Cri5 | Cri6 | Cri7 | Cri8 | Cri9 | Cri10 | Cri11 | Sum |
| Kozanoglu25 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 8 |
| Nesioonpour24 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 |
| Santos29 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 10 |
| Aghamohammadi31 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| Neiva28 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 9 |
| Carvalho 27 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Jackson26 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 9 |
| Karlekar32 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Fernandes33 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 |
| Santos30 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 |
Cri=criteria, Sum= summation.
Effect Size of Studies
The effect size of laser therapy has been reported in Table 4. The effect size was only calculated in 4 papers,24,25,29,31 and in other articles due to the absence of SD or VAS, was not calculated.26-28,30,32,33 As well, in Santos et al29 VAS measurement was performed twice; more than 2 hours after surgery, and after 40-48 hours after surgery. Therefore, one of these measurements was used to determine the treatment effect size.
Table 4. Results of Effect Size Evaluation .
| Author | Parameters | ||||||
| LLLT Group | Control Group | ||||||
| M1 (SD) | M2 (SD) | ES | M1 (SD) | M2 (SD) | ES | ||
| Kozanoglu25 | 32.9 (21.8) | 8.4 (15.5) | 1.12 | 23.9 (22.1) | 13.5 (21.3) | 0.47 | |
| Nesioonpour24 | 5.46 (1.79) | 2.88 (1.36) | 1.44 | 6.69 (1.87) | 4.15 (1.53) | 1.35 | |
| Santos29 | Up to 2 h | 2.2 (2.4) | 1.7 (2.3) | 0.33 | 2.4 (2.4) | 1.6 (2.3) | 0.13 |
| 40–48 h | 2.3 (2.4) | 1.5 (1.9) | 2.8 (2.3) | 2.5 (2.3) | |||
| Aghamohammadi31 | 1.84 (0.80) | 1.00 (0.00) | 1.05 | 2.77 (0.57) | 1.19 (0.40) | 2.77 | |
| Neiva28 | 3 | 0 | - | 5 | 1 | - | |
| Carvalho27 | - | 0.35(1.33) | - | - | 0.92 (1.32) | - | |
| Jackson26 | 21.4 | 3.32 | - | 36.7 | 6.70 | - | |
| Karlekar32 | - | - | - | - | - | - | |
| Fernandes33 | - | - | - | - | - | - | |
| Santos30 | R→4.4 | R→2.4 | - | 4.7 | 2.6 | - | |
| IR→4.3 | IR→2.1 | - | |||||
Discussion
Pain is one of the major complaints after surgery. Because of the adverse effects of using pain medications,4,5,8 the new methods for reducing pain are in progress. One of these methods is LLLT.9 LLLT is a non-invasive method with approximately no side effects and its cost is more reasonable. Previous studies have documented various mechanisms for the efficacy of laser on pain relief, including photobiomodulation, which caused certain reactions such as increased production of ATP, prostaglandins34,35 and beta-endorphins, decreased bradykinin levels, inhibition signal transduction from type C fibers,32 and increased secretion of pain relief neurotransmitters such as serotonin.36 In addition, LLLT can increases blood circulation, thus increases oxygen available for tissues and the pain-causing factors are diverted.37-39 Therefore, according to the above findings, it can be concluded that laser therapy can reduce inflammation and pain.
The effects of LLLT depends on various parameters such as wavelength, energy density, duration of radiation, power density, pulse status, Location of irradiation and the number of therapeutic sessions.12,40-42 Hence if the duration, energy density (up to 10.4 J/cm2), the number of therapeutic sessions of LLLT are increased (laser wavelength between 600-1000), it will have a greater effect on pain relief.43-45
Methodological quality of the trials in this review based on Pedro’s scale was high. Ten articles were studied in this review, of which 8 papers reported that LLLT significantly reduced postoperative pain and only the results of 2 articles contradicted others. Kozanoglu et al25 compared the effect of pneumatic compression and LLLT on lymphoedema and pain after breast surgery. They observed that pain was decreased after using both of the above-mentioned modalities, but there was no significant difference between the two groups in reducing postmastectomy pain.25 The laser dosage in this study was 1/5 J/cm2. Santos et al examined the effect of LLLT on postoperative pain after episiotomy and found that LLLT did not have a significant effect on pain relief in these patients. They expressed that the dosage of the laser was probably not enough, and the location of the surgical cut of the participant was different in terms of length and depth.30 The depth of laser penetration varies depending on the anatomical features of the tissue. There is still no complete information about the wavelength needed to penetrate a specific depth in the body. Therefore, most researchers considered the depth of laser penetration hypothetically.46 However, laser was not effective in 2 mentioned trials due to the use of inadequate dosage according to the depth of penetration.
The results of 8 other studies that were studied in this review showed that LLLT was effective in reducing postoperative pain in patients with breast augmentation surgery,26 inguinal hernia surgery,27 tonsillectomy,28,31 episiotomies,29 tibial fracture surgery24 and coronary artery bypass surgery.32,33 In addition, the laser can reduce the use of pain relief medication, thus protecting the patient from the complications of these drugs.
Examining of effect size of LLLT showed that it was variable in the above papers and only 4 papers had entry criteria, with a range of effect sizes ranging from 0.13 to 2.77. Accordingly, the best treatment protocol was an infrared laser dose of 4 J/cm2 for the postoperative pain of tonsillectomy, which was irradiated through the infra mandibular angle on the tonsils. The infrared laser has a greater penetration depth, so it may affect nociceptors.39 Consequently, it can be argued that LLLT is a suitable modality for the treatment of postoperative pain, although the effect size of this modality was variable.
In vitro studies have shown that photobiomodulation can be effective in reducing pain and inflammation, but there is a great ambiguity about applying this method in in vivo studies due to various factors that causes pain and inflammation, various intervention and differences in the choice of parameters. Therefore, selecting proper subjects and parameters for LLLT is important.47 This review had some limitations, including heterogeneity in the results. One of them was that in some articles, along with laser therapy, pain reliever had been used, so it was difficult to distinguish between them. Another discrepancy for the results of this study was because of the differences in the number of therapeutic sessions, laser wavelength, and radiation duration in the trials. As a result, we failed to introduce certain parameters as the most appropriate parameters for pain relief. However, according to the results of existing studies, we have introduced the most appropriate parameters in these articles to reduce postoperative pain. But there is a need for further investigation in this regard. It is also recommended that a specific approach should be developed for future systematic reviews and guidelines of photobiomodulation so that a standard method is used in all parts of the world to obtain more accurate and verifiable results.
Conclusion
According to the findings of the present study, it appears that, LLLT may be an appropriate modality with no side effects for reducing postoperative pain, but its effectiveness depends on the use of suitable parameters especially adequate dosage. However, there is a lack of sufficient evidence supporting the effect of laser on pain reduction after surgery. Hence, further research should be designed and implemented based on proper protocols for these patients and follow-up of therapeutic course.
Ethical Considerations
Not applicable.
Conflict of Interests
The authors declare no conflict of interest.
Acknowledgments
The authors of this review would like to appreciate all who collaborated on the development of this study.
Please cite this article as follows: Ezzati K, Fekrazad R, Raoufi Z. The effects of photobiomodulation therapy on post-surgical pain. J Lasers Med Sci. 2019;10(2):79-85. doi:10.15171/jlms.2019.13.
References
- 1.Carr DB, Goudas LC. Acute pain. Lancet. 1999;353(9169):2051–2058. doi: 10.1016/S0140-6736(99)03313-9. [DOI] [PubMed] [Google Scholar]
- 2.Breivik H. Postoperative pain management: why is it difficult to show that it improves outcome? Eur J Anaesthesiol. 1998;15(6):748–751. doi: 10.1097/00003643-199811000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Imani F, Rahimzadeh P. Gabapentinoids: gabapentin and pregabalin for postoperative pain management. Anesth Pain Med. 2012;2(2):52–3. doi: 10.5812/aapm.7743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nayman J. Measurement and control of postoperative pain. Ann R Coll Surg Engl. 1979;61(6):419. [PMC free article] [PubMed] [Google Scholar]
- 5.Sieber FE, Mears S, Lee H, Gottschalk A. Postoperative opioid consumption and its relationship to cognitive function in older adults with hip fracture. J Am Geriatr Soc. 2011;59(12):2256–62. doi: 10.1111/j.1532-5415.2011.03729.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breivik H, Högström H, Niemi G. et al. 2 Safe and effective post-operative pain relief: introduction and continuous quality-improvement of comprehensive post-operative pain management programmes. Baillieres Clin Anaesthesiol. 1995;9(3):423–460. doi: 10.1016/S0950-3501(95)80015-8. [DOI] [Google Scholar]
- 7.McDonald GJ, Lord SM, Bogduk N. Long-term follow-up of patients treated with cervical radiofrequency neurotomy for chronic neck pain. Neurosurgery. 1999;45(1):61–68. doi: 10.1097/00006123-199907000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Chaney MA. Side effects of intrathecal and epidural opioids. Can J Anaesth. 1995;42(10):891–903. doi: 10.1007/BF03011037. [DOI] [PubMed] [Google Scholar]
- 9.Asnaashari M, Safavi N. Application of low level lasers in dentistry (endodontic) J Lasers Med Sci. 2013;4(2):57–66. [PMC free article] [PubMed] [Google Scholar]
- 10.Prabhu V, Rao S, Chandra S. et al. Spectroscopic and histological evaluation of wound healing progression following low level laser therapy (LLLT) J Biophotonics. 2012;5(2):168–184. doi: 10.1002/jbio.201100089. [DOI] [PubMed] [Google Scholar]
- 11.Fernando S, Hill C, Walker R. A randomised double blind comparative study of low level laser therapy following surgical extraction of lower third molar teeth. Br J Oral Maxillofac Surg. 1993;31(3):170–2. doi: 10.1016/0266-4356(93)90118-G. [DOI] [PubMed] [Google Scholar]
- 12.Enwemeka CS, Parker JC, Dowdy DS, Harkness EE, Harkness LE, Woodruff LD. The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg. 2004;22(4):323–329. doi: 10.1089/pho.2004.22.323. [DOI] [PubMed] [Google Scholar]
- 13.Albertini R, Villaverde A, Aimbire F. et al. Anti-inflammatory effects of low-level laser therapy (LLLT) with two different red wavelengths (660nm and 684nm) in carrageenan-induced rat paw edema. J Photochem Photobiol B. 2007;89(1):50–55. doi: 10.1016/j.jphotobiol.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Medrado AR, Pugliese LS, Reis SRA, Andrade ZA. Influence of low level laser therapy on wound healing and its biological action upon myofibroblasts. Lasers Surg Med. 2003;32(3):239–244. doi: 10.1002/lsm.10126. [DOI] [PubMed] [Google Scholar]
- 15.Aras MH, Ömezli MM, Güngörmüş M. Does low-level laser therapy have an antianesthetic effect? A review. Photomed Laser Surg. 2010;28(6):719–722. doi: 10.1089/pho.2008.2430. [DOI] [PubMed] [Google Scholar]
- 16.Mizutani K, Musya Y, Wakae K. et al. A clinical study on serum prostaglandin E2 with low-level laser therapy. Photomedicine and Laser Therapy. 2004;22(6):537–539. doi: 10.1089/pho.2004.22.537. [DOI] [PubMed] [Google Scholar]
- 17.Bjordal JM, Johnson MI, Iversen V, Aimbire F, Lopes-Martins RAB. Low-level laser therapy in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomedicine and Laser Therapy. 2006;24(2):158–68. doi: 10.1089/pho.2006.24.158. [DOI] [PubMed] [Google Scholar]
- 18. Brugnera Júnior A, Santos AEC, Bologna ED, Ladalardo TCC. Atlas de laserterapia aplicada à clínica odontológica. Santos; 2003.
- 19.Fikácková H, Dostálová T, Navrátil L, Klaschka J. Effectiveness of low-level laser therapy in temporomandibular joint disorders: a placebo-controlled study. Photomed Laser Surg. 2007;25(4):297–303. doi: 10.1089/pho.2007.2053. [DOI] [PubMed] [Google Scholar]
- 20.Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003;49(2):107–116. doi: 10.1016/s0004-9514(14)60127-6. [DOI] [PubMed] [Google Scholar]
- 21. Rankin IA, Sargeant H, Rehman H, Gurusamy KS. Low‐level laser therapy for carpal tunnel syndrome. The Cochrane Library; 2017. [DOI] [PMC free article] [PubMed]
- 22.Brosseau L, Welch V, Wells G. et al. Low level laser therapy for osteoarthritis and rheumatoid arthritis: a metaanalysis. J Rheumatol. 2000;27(8):1961–1969. [PubMed] [Google Scholar]
- 23.Gür A, Karakoc M, Nas K, Cevik R, Sarac J, Demir E. Efficacy of low power laser therapy in fibromyalgia: a single-blind, placebo-controlled trial. Lasers Med Sci. 2002;17(1):57–61. doi: 10.1007/s10103-002-8267-4. [DOI] [PubMed] [Google Scholar]
- 24.Nesioonpour S, Mokmeli S, Vojdani S. et al. The effect of low-level laser on postoperative pain after tibial fracture surgery: a double-blind controlled randomized clinical trial. Anesth Pain Med. 2014;4(3):e17350. doi: 10.5812/aapm.17350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kozanoglu E, Basaran S, Paydas S, Sarpel T. Efficacy of pneumatic compression and low-level laser therapy in the treatment of postmastectomy lymphoedema: a randomized controlled trial. Clin Rehabil. 2009;23(2):117–124. doi: 10.1177/0269215508096173. [DOI] [PubMed] [Google Scholar]
- 26.Jackson RF, Roche G, Mangione T. Low-level laser therapy effectiveness for reducing pain after breast augmentation. The American Journal of Cosmetic Surgery. 2009;26(3):144–8. [Google Scholar]
- 27.Carvalho RL, Alcântara PS, Kamamoto F, Cressoni MD, Casarotto RA. Effects of low-level laser therapy on pain and scar formation after inguinal herniation surgery: a randomized controlled single-blind study. Photomed Laser Surg. 2010;28(3):417–422. doi: 10.1089/pho.2009.2548. [DOI] [PubMed] [Google Scholar]
- 28.Neiva FC, Vieira FMJ, Figueiredo CR, Stamm AEC, Weckx LLM, Pignatari SSN. Therapeutic laser for pain relief after tonsillectomy. Rev Paul Pediatr. 2010;28(3):322–328. doi: 10.1590/S0103-05822010000300011. [DOI] [Google Scholar]
- 29.Santos Jde O1, Oliveira SM, Nobre MR, Aranha AC, Alvarenga MB. A randomised clinical trial of the effect of low-level laser therapy for perineal pain and healing after episiotomy: A pilot study. Midwifery. 2012;28(5):e653–e659. doi: 10.1016/j.midw.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 30.Santos JdO, de Oliveira SM, da Silva F, Nobre MR, Osava RH, Riesco ML. Low‐level laser therapy for pain relief after episiotomy: a double‐blind randomised clinical trial. J Clin Nurs. 2012;21(23-24):3513–3522. doi: 10.1111/j.1365-2702.2011.04019.x. [DOI] [PubMed] [Google Scholar]
- 31.Aghamohammadi D, Eidi M, Lotfi A. et al. Effect of low level laser application at the end of surgery to reduce pain after tonsillectomy in adults. J Lasers Med Sci. 2013;4(2):79–85. [PMC free article] [PubMed] [Google Scholar]
- 32.Karlekar A, Bharati S, Saxena R, Mehta K. Assessment of feasibility and efficacy of Class IV laser therapy for postoperative pain relief in off-pump coronary artery bypass surgery patients: A pilot study. Ann Card Anaesth. 2015;18(3):317–322. doi: 10.4103/0971-9784.159800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fernandes GA, Araújo Júnior RB, Lima AC, Gonzaga IC, de Oliveira RA, Nicolau RA. Low-intensity laser (660 NM) has analgesic effects on sternotomy of patients who underwent coronary artery bypass grafts. Ann Card Anaesth. 2017;20(1):52–56. doi: 10.4103/0971-9784.197836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Colombo F, Neto Ade A, Sousa AP, Marchionni AM, Pinheiro AL, Reis SR. Effect of low-level laser therapy (660 nm) on angiogenesis in wound healing: a immunohistochemical study in a rodent model. Braz Dent J. 2013;24(4):308–312. doi: 10.1590/0103-6440201301867. [DOI] [PubMed] [Google Scholar]
- 35.Dos Santos SA, Alves ACA, Leal-Junior ECP. et al. Comparative analysis of two low-level laser doses on the expression of inflammatory mediators and on neutrophils and macrophages in acute joint inflammation. Lasers Med Sci. 2014;29(3):1051–1058. doi: 10.1007/s10103-013-1467-2. [DOI] [PubMed] [Google Scholar]
- 36.Brosseau L, Welch V, Wells G. et al. Low level laser therapy for osteoarthritis and rheumatoid arthritis: a metaanalysis. J Rheumatol. 2000;27(8):1961–1969. [PubMed] [Google Scholar]
- 37.Schindl A, Schindl M, Schön H, Knobler R, Havelec L, Schindl L. Low-intensity laser irradiation improves skin circulation in patients with diabetic microangiopathy. Diabetes Care. 1998;21(4):580–5804. doi: 10.2337/diacare.21.4.580. [DOI] [PubMed] [Google Scholar]
- 38.Yu W, Naim JO, McGowan M, Ippolito K, Lanzafame RJ. Photomodulation of oxidative metabolism and electron chain enzymes in rat liver mitochondria. Photochem Photobiol. 1997;66(6):866–871. doi: 10.1111/j.1751-1097.1997.tb03239.x. [DOI] [PubMed] [Google Scholar]
- 39.Fekrazad R. The effect of 810-nm low-level laser therapy on pain caused by orthodontic elastomeric separators. Lasers Med Sci. 2014;29(2):559–564. doi: 10.1007/s10103-012-1258-1. [DOI] [PubMed] [Google Scholar]
- 40.Fulop AM, Dhimmer S, Deluca JR. et al. A meta-analysis of the efficacy of laser phototherapy on pain relief. Clin J Pain. 2010;26(8):729–736. doi: 10.1097/AJP.0b013e3181f09713. [DOI] [PubMed] [Google Scholar]
- 41. Hamblin MR, Demidova TN, eds. Mechanisms of low level light therapy. Mechanisms for low-light therapy. International Society for Optics and Photonics; 2006.
- 42.Rastgar Koutenaei F, Mosallanezhad Z, Naghikhani M. et al. The effect of low level laser therapy on pain and range of motion of patients with knee osteoarthritis. Physical Treatments. 2017;7(1):13–28. [Google Scholar]
- 43.Alghadir A, Omar MTA, Al-Askar AB, Al-Muteri NK. Effect of low-level laser therapy in patients with chronic knee osteoarthritis: a single-blinded randomized clinical study. Lasers Med Sci. 2014;29(2):749–755. doi: 10.1007/s10103-013-1393-3. [DOI] [PubMed] [Google Scholar]
- 44.Fukuda VO, Fukuda TY, Guimarães M. et al. Short-term efficacy of low-level laser therapy in patients with knee osteoarthritis: a randomized placebo-controlled, double-blind clinical trial. Rev Bras Ortop. 2011;46(5):526–533. doi: 10.1016/S2255-4971(15)30407-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwon K, Son T, Lee K-J, Jung B. Enhancement of light propagation depth in skin: cross-validation of mathematical modeling methods. Lasers Med Sci. 2009;24(4):605–615. doi: 10.1007/s10103-008-0625-4. [DOI] [PubMed] [Google Scholar]
- 46.Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003;49(2):107–116. doi: 10.1016/s0004-9514(14)60127-6. [DOI] [PubMed] [Google Scholar]
- 47.Fekrazad R, Chiniforush N, Bouraima SA, Valipour M, Aslani M, Zare M. et al. Low level laser therapy in management of complications after intra oral surgeries. J Lasers Med Sci. 2012;3(4):135. [Google Scholar]


