Abstract
Introduction:
Young adults are at high risk for using traditional and novel tobacco products. However, little is known about daily/weekly use patterns or psychosocial triggers for using various tobacco products.
Methods:
This ecological momentary assessment (EMA) study examined timing, tobacco cravings, affect, social context, and other substance use (alcohol, marijuana) in relation to use of cigarettes, electronic nicotine delivery systems (ENDS), and any tobacco product (i.e., cigarettes, ENDS, cigars, hookah), respectively. We also examined interactions between these predictors, sex, and race/ethnicity. From a longitudinal study of 3,418 18-25 year-olds from seven Georgia colleges/universities, we recruited 72 reporting current tobacco use to participate in the 21-day EMA study; 43 participated, of which 31 completed ≥66% assessments and were analyzed. Cravings, affect, social context, and substance use were assessed daily across four four-hour windows.
Results:
Of the 31 participants, average age was 21.10 years (SD=1.95), 45.2% were female, and 71.0% non-Hispanic White; 71.0% used cigarettes, 58.1% ENDS, 38.7% cigars, and 25.8% hookah (25.6% used one product, 46.5% two, 27.9% ≥three). Predictors of cigarette use included higher anxiety, greater odds of marijuana and alcohol use, and higher boredom levels among women. Predictors of ENDS use included being non-White and greater odds of marijuana use, as well as higher tobacco cravings among women and higher boredom among men. Predictors of any tobacco product use included being non-White, higher boredom levels, and greater odds of marijuana and alcohol use.
Conclusions:
Distinct interventions may be needed to address use of differing tobacco products among young adults.
Keywords: Substance use, Tobacco use, Young adults, Risk factors
INTRODUCTION
Tobacco use is the number one preventable cause of death in the US.1 In recent years, alternative tobacco products (ATPs), such as electronic nicotine delivery systems (ENDS; i.e., “e-cigarettes”) and little cigars or cigarillos, have been introduced to the US market, while waterpipes or hookah have increased in popularity.2,3 Beyond some well-documented health risks,4-7 concerns regarding using these products include misperceptions of their relative health risks8-10 and use as a harm-reducing alternative that could delay smoking cessation.11-13 The emergence of ATPs has also increased the occurrence of polytobacco use;14,15 among ATP users, polytobacco use has increased to 40-50%.16,17 This is important, as multiple tobacco product usage may be associated with increased levels of nicotine dependence.14,18
Particularly noteworthy, young adults are now the highest risk group for using ATPs, with the rates continuing to increase19 and roughly 15-30% of young adult smokers currently using more than one tobacco product.20,21 Sex and racial differences in young adult tobacco use exist. Relative to men, women show lower prevalence and greater declines in use during young adulthood.22-24 In addition, Blacks and Whites also demonstrate different tobacco use patterns,24-26 and tobacco use among Whites declines during the decade of the 20s but does not in Blacks.27,28 Indeed, the high rates of use among young adults may be related to marketing strategies, as well as the product flavorings, which may be used to target young adults and distinct segments of this population.29-32
Despite concerns regarding diverse tobacco product use and polytobacco use, little is known about differing patterns of use or factors that trigger or influence use. Research examining profiles and trajectories of tobacco use in young adulthood, mostly focused on cigarette smoking, have commonly found categories including never smokers, experimenters, light or occasional smokers, early established smokers, late escalators, and quitters or decliners.33-37 Project DECOY (Documenting Experiences with Cigarettes and Other Tobacco in Young Adults) aimed to examine the epidemiology of various tobacco product use among young adults over a two-year period.38 Prior analyses from this study documented similar cigarette smoking trajectories identified in the aforementioned research (e.g., dabblers/experimenters, college onset smokers, later onset smokers)39 and also identified distinct use profiles of various tobacco products, including light versus heavy polytobacco users and cigar/hookah/marijuana users.26 These prior studies, as well as others,40-44 suggest that young adults’ tobacco use is a temporally unstable behavior. This is particularly relevant given the current context of diverse tobacco products,45 which are commonly used on an intermittent basis.15,25,26,46
Drawing from a social cognitive perspective,47 a number of environmental (e.g., contextual and social) factors and cognitive factors (e.g., outcome expectancies) may be key influences on tobacco use among young people.48-50 Given the relative paucity of research on such influences related to ATP use relative to cigarette use, a first step in distinguishing influences on and patterns of ATP use among young adults is examining factors shown to be robustly associated with cigarette smoking. As such, the current study focuses on factors encompassed within social cognitive theory47 with substantial empirical support linking them to cigarette smoking.
In terms of contextual factors, trends in substance use vary throughout the day and across days of the week. For example, prior research has documented that morning smoking latency and level is indicative of nicotine dependency.51,52 Relatedly, presence and level of nicotine cravings, an indicator of dependence, have a reciprocal relationship with tobacco use.53,54 Moreover, tobacco is often used with other substances, often consumed in the evening, particularly on the weekends.55-57 As such, time of day and day of the week are important contextual factors related to tobacco and other substance use.
In relation to cognitive factors, different outcome expectancies or motivations for use are also critical influences to understand.58,59 For some users, tobacco use helps them deal with boredom and provides a means for affect regulation, for example using tobacco to reduce negative affect or increase positive affect.60-74 Among others, tobacco use is perceived as mainly linked to social situations or motives.63,75-77 Of particular note, social conformity pressures are robust predictors of substance use and abuse.75-78 Additionally, many young adults identify as “social smokers”; that is, they describe their smoking as almost exclusively in the context of social settings, particularly among other smokers.79-81
Such outcome expectancies also are related to ATP and/or polytobacco use, analyses from Project DECOY found that boredom relief motives were shown to be associated with polytobacco versus cigarette only use.82 Moreover, distinct motives were found to be associated with different product use; for example, cigarette use was related to boredom relief and affect motivation, whereas ATP use was associated with social or self-enhancement motives.82 Additionally, data from Project DECOY examined reasons for polytobacco use (e.g., social context, displacement, experimentation).83 These associations have also varied based on sex and race/ethnicity.26,82,83
Another critically important influence on tobacco use is other substance use. Young adults are at the greatest risk for using various substances, and the use of any one substance is associated with use of other substances.84-87 In addition to tobacco, two of the other most commonly used substances among young adults in the US are marijuana and alcohol.84 Indeed, prior analyses of Project DECOY data indicated a range of reasons for tobacco-marijuana co-use (e.g., instrumentality, social context).88 As such, tobacco use should be examined within the context of other substance use in order to understand use and co-use patterns.
Most research examining influences on tobacco use have relied on data at a crosssection or traditional longitudinal data with large gaps between assessments,89-91 reducing the ability to assess more temporally closely related predictors of tobacco use. Ecological momentary assessment (EMA) studies involve repeated sampling of behaviors and experiences in real time in natural environments, thus minimizing recall bias, maximizing ecological validity, and allowing assessment of micro-processes that influence behavior in real-world contexts.92,93
Attempts to characterize the momentary antecedents of tobacco use are among the earliest and most prominent uses of EMA methodology. For example, a recent systematic review of 91 studies using an ecological momentary approach (ranging from daily diaries to multiple assessments per day prompted electronically) examined cravings and substance use published between 1996 and 2013.94 Of the 91 studies included, 63 published studies focused on tobacco.94 However, applications of EMA in tobacco research have focused almost exclusively on cigarette use.53,54,56,57,94-97 As such, EMA data identifying distinct antecedents of differing and collective tobacco product use are needed and will be directly relevant to interventions.
The current study extends previously published findings regarding patterns and reasons for use.26,82,83 Specifically, this study leveraged Project DECOY25 and analyzed real-time, naturalistic EMA data in order to examine: 1) patterns of use of the various tobacco products and other substances; and 2) the association of timing, cravings, affect, social context, and other substance use to self-reported tobacco use among young adults. Specifically, we examined predictors of three primary outcomes: cigarette use, ENDS use, and any tobacco product use, respectively.
METHODS
This study was conducted in the context of a larger study, Project DECOY, a longitudinal study of 3,418 young adults from seven Georgia colleges/universities. The parent study involved individual online survey assessments every four months for two years, launched in Fall 2014.33 A detailed description of the study is provided elsewhere.38 Inclusion criteria for the parent study were: 1) age ≥18 and ≤25, and 2) able to read English. The currently analyzed EMA study was conducted between Wave 5 (in April 2016) and Wave 6 (in August 2016). The EMA study was approved by Emory University’s Institutional Review Board (IRB00086945).
To determine the appropriate methods for this initial EMA study regarding ATP use in young adults, we referred to the literature. In the aforementioned systematic review,94 after excluding two studies with sample sizes that were outliers (n’s of 1106 and 1504), the average sample size of tobacco EMA studies was 178 (SD=135; range of 15 to 691), and the average number of days of assessment was 21 days (SD=28; range of 2 to 175). Thus, we established a 21-day time period and justified our small sample size, acknowledging that of the 40 independent data sets (excluding the outliers), 49% had sample sizes similar to our recruitment target.
Participants
A subsample of participants who used at least one specific tobacco product ≥15 of the past 30 days at Wave 5 were identified and contacted via email with information about the study, including a link to an eligibility screener. Inclusion criteria for the current EMA study were: 1) use of at least one specific tobacco product ≥15 days of the 30 days prior to the eligibility screener; 2) own an iPhone or Android smartphone (to accommodate EMA technology); 3) willing to receive multiple text messages per day; and 4) no international travel in the next 21 days. The first criteria (i.e., use level) was determined based on the distribution of use level for each tobacco product at Wave 5 and in order to anticipate a sufficient level of use over the 21-day EMA period to provide data regarding contextual factors related to use. The remaining criteria were included in order to ensure that the technology used to conduct the EMA study was compatible with participants’ technology capacity during the EMA study time period. If participants were eligible, they were directed to the online consent form and baseline assessment. They were then sent an email outlining instructions regarding how to enroll in the EMA study (via NYU’s website).
Of 72 participants recruited for this study, 45 consented (62.5%), 2 withdrew (reportedly because of response burden), and 43 (59.7%) participated. After the EMA study was completed, data were screened for missingness. We excluded those who responded to less than two-thirds (66%) of the prompts on tobacco use. In total, 31 of the 43 participants (72.1%) completed ≥66% assessments and were thus included in the multivariate analyses. We established this criteria for inclusion in analyses for several reasons. First, of the 12 participants excluded based on this criteria, 20.8% of prompts resulted in a response (range 1.2% to 57.1%). Thus, the distribution of the data suggested this as a practical cut-point. Second, much of the prior research98-102 has used similar cut-points for inclusion in analyses. Third, in terms of interpretability of the data, large proportions of missing data undermine the meaningfulness of the data. (Note that we also conducted sensitivity analyses to examine differences in study findings 1) if alternative cut-points were selected, e.g., 80%, or 2) if all participants were retained. No significant differences in study findings were documented using these two approaches. As such, we chose to present findings based on those participants with more representative and valid data.)
Data Collection
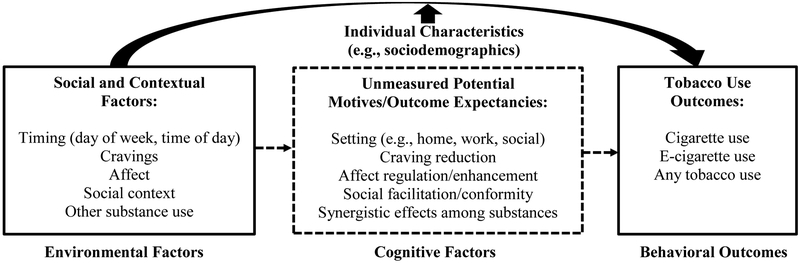
This EMA study was informed by a conceptual framework based on social cognitive perspective47 (see Figure 1). This study assessed environmental (i.e., social and contextual) factors in relation to tobacco use behavioral outcomes. Cognitive factors (i.e., motives and outcome expectancies) were not explicitly examined but indicate some possible mechanisms explaining the association from the objective environmental factors and the tobacco use outcomes. In addition, based on the aforementioned literature, individual characteristics (i.e., sociodemographics) may be potential moderators of the associations between the environmental factors and tobacco use behavioral outcomes.
Figure 1.
Conceptual framework regarding correlates and predictors of tobacco use
Note: Dashed lines indicate unmeasured potentially mediating associations.
Sociodemographics included in these analyses were age, sex, race/ethnicity (operationalized as White vs. other), and highest parental education (operationalized as <bachelor’s degree vs. ≥bachelor’s degree).
For the EMA, each day was broken into four windows – each lasting four hours – and within each four-hour window interval assessments were conducted using text-messaging. Interval assessments were conducted using two approaches: 1) a fixed-interval or “coverage” approach was used to assess tobacco, alcohol, and marijuana use events, and 2) a random-interval approach was used to assess momentary experience surveys. In relation to the former, substance use events were assessed using a dynamic-interval “coverage” survey strategy as this strategy is designed to ensure that all behavioral events of interest are documented with fidelity, as well as ensure that reports for all behaviors are balanced over the course of every day for every participant.103-106 Specifically, participants were asked to report their usual sleep schedule, which anchored the timing of each assessment (i.e., the first assessment was four hours after waking and then three times more every four hours thereafter). At the end of each window, participants were asked, “Since last assessment, how many of each have you used: cigarettes, little cigars or cigarillos, puffs of an e-cigarette or vape pen, puffs of a hookah, puffs of marijuana (vaporized or smoked), a mix of tobacco and marijuana, and servings of alcohol.” (Note that participants were instructed to report e-cigarette use of e-cigarettes containing nicotine and that a separate question assessed marijuana use and mode of use, including vaporized). Combined in succession, these coverage reports produce near-complete and consistent use reports over relatively extended periods, partly because they require only seconds for participants to complete.103-106
Complementing the behavioral use reports collected at the close of each coverage window, randomly prompted momentary assessments, roughly one-to-two minutes each, were used to assess cravings, affect, and social context, within each four-hour window to assess ebbs and flows randomly during the day.104 Cravings for tobacco were assessed on a ten-point scale.56 To assess affect, participants were asked to report how anxious, happy, and bored they felt, respectively, on a ten-point scale.107 To assess social context, participants were asked to report the names of people they were with primarily or if they were alone. Those responses were recoded to Alone/Not Alone. Participants had 20 minutes to complete these assessments.
Participants were able to receive up to $100 via Amazon e-gift cards for completing all components of the study over the 21-day period. This incentive structure included $60 for completing at least 70% of the EMA assessments over the 21-day period and additional incentives for completing end-of-study assessments.
Data Analysis
Generalized hierarchical linear growth models (SAS Proc-Mixed, SAS Institute, Cary, NC) with random intercepts only were used to model cigarette, ENDS, and any tobacco product use, respectively, as binary outcomes. (Frequencies of cigar and hookah use were too low and among too few individuals to allow for this modeling.) These analyses accommodate data with large and variable numbers of observations over time by creating a hierarchical two-level structure and separating variance between subjects and occasions within subjects.108
For each outcome, the models were built sequentially to model time of day, day of the week, tobacco cravings, affect variables (anxiety, happiness, boredom), whether the participant was alone or in company, and marijuana and alcohol use during the last assessment window in relation to tobacco use. First, main effects were entered in batches. Then, interaction effects of sex and race/ethnicity were probed for cravings, affect, social context, and other substance use separately. Only significant interaction effects were retained in the final models. Unstructured covariance structures were used for modeling between- and within-subjects, respectively.109 Model fit was assessed using deviance, AIC, and BIC. ICC was calculated for null and final models. All analyses were conducted using SAS 9.4.
RESULTS
Patterns of Use
Of the 31 participants included in these analyses, participants were an average of 21.10 years (SD=1.95), 14 (45.2%) female, 22 (71.0%) non-Hispanic White, and 18 (58.1%) with highest parental education ≥Bachelor’s degree (Table 1). During the 21-day period, 22 (71.0%) used cigarettes, 18 (58.1%) ENDS, 12 (38.7%) cigars, and 8 (25.8%) hookah. Additionally, 11 (25.6%) participants used one product, 20 (46.5%) used two, and 12 (27.9%) used three or more.
Table 1.
Participant Characteristics
| Variable | Participants included in analyses N=31 N (%) or M (SD) |
Participants excluded from analyses N=12 N (%) or M (SD) |
|---|---|---|
| Sociodemographics | ||
| Age (SD) | 21.10 (1.95) | 21.08 (1.38) |
| Sex (%) | ||
| Male | 17 (54.8) | 6 (50.0) |
| Female | 14 (45.2) | 6 (50.0) |
| Race/Ethnicity (%) | ||
| White (non-Hispanic) | 22 (71.0) | 6 (50.0) |
| Other | 9 (29.0) | 6 (50.0) |
| Parental Education (%) | ||
| < Bachelor’s degree | 14 (45.2) | 5 (41.7) |
| ≥ Bachelor’s degree | 17 (54.8) | 7 (58.3) |
| Substance use * | ||
| Marijuana (%) | 18 (58.1) | -- |
| Alcohol (%) | 27 (87.1) | -- |
| Cigarettes (%) | 22 (71.0) | -- |
| ENDS (%) | 18 (58.1) | -- |
| Cigar products (%) | 12 (38.7) | -- |
| Hookah (%) | 8 (25.8) | -- |
| Number of tobacco products used * | -- | |
| One (%) | 11 (25.6) | -- |
| Two (%) | 20 (46.5) | -- |
| Three or more (%) | 12 (27.9) | -- |
| Engagement with EMA protocol (%) | ||
| Participated in >90% assessments | 12 (38.7) | -- |
| Participated in 81 to 90% | 8 (25.8) | -- |
| Participated in 71 to 80% | 10 (32.3) | -- |
| Participated in 66 to 70% | 1 (3.2) | -- |
| Participated in <66% | -- | 12 (100.0) |
If an occurrence was reported during the 21-day EMA study period.
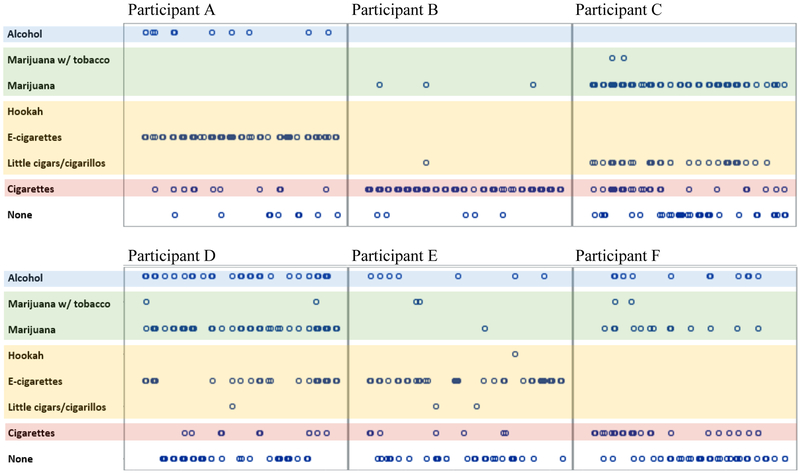
Figure 2 displays example patterns of tobacco and other substance use across the four four-hour windows and across the 21-day period. As shown in the figure, there were vastly different tobacco use patterns, with some participants showing high co-use of ENDS and cigarettes (e.g., Participant A), some showing mainly cigarette use (e.g., Participant B), and some showing high marijuana and tobacco co-use (e.g., Participants C and D). These profiles demonstrate the highly divergent individual patterns of use.
Figure 2.
Example profiles of tobacco and other substance use across 21 days
Note: The x-axis plots the four-hour windows across the 21-day period (a total of 84 windows). The circles indicate an occurrence of use of the product labeled on the left side of the y-axis.
Predictors of Cigarette Use
In the model predicting cigarette use (Table 2), significant main effects were found between higher levels of anxiety (OR=1.17, CI 1.03, 1.34), and greater odds of marijuana use (OR=2.89, CI 1.36, 6.14) and alcohol use (OR=4.13, CI 2.22, 7.69) in relation to cigarette use. An interaction effect was identified such that higher levels of boredom among women was associated with cigarette smoking (OR=1.29, CI 1.08, 1.54), whereas this was not found among men.
Table 2.
Predictors of cigarette use, ENDS use, and any tobacco product use (i.e., cigarettes, ENDS, cigars, hookah)
| Cigarette Use | ENDS Use | Any Tobacco Use | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Effect | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||
| Baseline measures | |||||||||||
| Female (vs. male) | 0.57 | 0.06 | 5.80 | 0.14 | 0.01 | 2.45 | 0.90 | 0.16 | 5.08 | ||
| Age | 0.88 | 0.47 | 1.65 | 0.80 | 0.38 | 1.70 | 0.80 | 0.51 | 1.25 | ||
| Other race (vs. White) | 0.12 | 0.01 | 2.94 | 0.04* | <0.01 | 1.40 | 0.09* | 0.01 | 0.78 | ||
| Parental education | 1.03 | 0.47 | 2.26 | 0.78 | 0.33 | 1.82 | 0.80 | 0.46 | 1.40 | ||
| Timing | |||||||||||
| Weekend (vs. weekday) | 1.25 | 0.79 | 1.98 | 1.30 | 089 | 1.90 | 1.08 | 0.78 | 1.50 | ||
| Time of day (vs. morning) | |||||||||||
| Afternoon | 0.98 | 0.55 | 1.76 | 0.87 | 0.54 | 1.42 | 0.85 | 0.57 | 1.28 | ||
| Early evening | 0.58 | 0.32 | 1.08 | 1.04 | 0.64 | 1.68 | 0.76 | 0.50 | 1.14 | ||
| Late evening | 0.77 | 0.39 | 1.54 | 0.94 | 0.55 | 1.59 | 0.83 | 0.53 | 1.31 | ||
| Momentary variables | |||||||||||
| Tobacco cravings | 1.00 | 0.88 | 1.14 | -- | -- | -- | 1.01 | 0.92 | 1.10 | ||
| x female | -- | -- | -- | 1.32* | 1.08 | 1.60 | -- | -- | -- | ||
| x male | -- | -- | -- | 0.95 | 0.84 | 1.07 | -- | -- | -- | ||
| Momentary moods | |||||||||||
| Anxiety | 1.17* | 1.03 | 1.34 | †-- | †-- | †-- | 1.00 | 0.91 | 1.09 | ||
| Happiness | 1.11 | 0.96 | 1.28 | 1.04 | 0.93 | 1.17 | 1.05 | 0.96 | 1.16 | ||
| Boredom | -- | -- | -- | -- | -- | -- | 1.09* | 1.01 | 1.18 | ||
| x female | 1.29* | 1.08 | 1.54 | 1.00 | 0.84 | 1.18 | -- | -- | -- | ||
| x male | 0.96 | 0.81 | 1.14 | 1.16* | 1.04 | 1.29 | -- | -- | -- | ||
| Social context | |||||||||||
| In company (vs. alone) | 1.08 | 0.68 | 1.73 | 0.90 | 0.63 | 1.29 | 1.07 | 0.78 | 1.46 | ||
| Other substance use | |||||||||||
| Marijuana use | 2.89* | 1.36 | 6.14 | 3.04* | 1.53 | 6.03 | 3.62* | 2.16 | 6.09 | ||
| Alcohol use | 4.13* | 2.22 | 7.69 | -- | -- | -- | 4.46* | 2.60 | 7.63 | ||
| x female | -- | -- | -- | 0.86 | 0.30 | 2.47 | -- | -- | -- | ||
| x male | -- | -- | -- | 3.57* | 1.72 | 7.40 | -- | -- | -- | ||
| Model fit | Null model |
Full model |
Null model |
Full model |
Null model |
Full model |
||
|---|---|---|---|---|---|---|---|---|
| Deviance | 1075.24 | 674.56 | 1220.82 | 910.61 | 1812.69 | 1240.12 | ||
| AIC | 1079.24 | 710.56 | 1224.82 | 948.61 | 1816.69 | 1274.12 | ||
| BIC | 1082.11 | 735.78 | 1227.69 | 975.24 | 1819.55 | 1297.94 | ||
| ICC | 71.7% | 72.2% | 79.9% | 77.6% | 66.1% | 61.2% |
p<.05. AIC = Akaika Information Criterion, BIC = Bayesian Information Criterion, ICC = intraclass correlation.
Anxiety was not significant in a bivariate model predicting ENDS and thus removed for parsimony given the small sample size.
Predictors of ENDS Use
In the model predicting ENDS use (Table 2), main effects were identified indicating that being a racial/ethnic minority (OR=0.04, CI <0.01, 1.40) and greater odds of marijuana use (OR=3.04, CI 1.53, 6.03) were related to ENDS use. Interaction effects were found such that higher tobacco cravings among women (but not men; OR=1.32, CI 1.08, 1.60) and higher levels of boredom among men (but not women; OR=1.16, CI 1.04, 1.29) were associated with ENDS use. (Anxiety was not significant in a bivariate model and thus removed for parsimony given the small sample size.)
Predictors of Any Tobacco Use
In the model predicting use of any tobacco product (i.e., cigarettes, ENDS, cigar products, or hookah; Table 2), main effects were identified such that being non-White (OR=0.09, CI 0.01, 0.78), higher levels of boredom (OR=1.09, CI 1.01, 1.18), and greater odds of marijuana use (OR=3.62, CI 2.16, 6.09) and alcohol use (OR=4.46, CI 2.60, 7.63) predicted any tobacco use. Across models, the final models had significantly better model fit than the null models based on deviance, AIC, and BIC. Null and final models showed that most of the unexplained variance was between participants.
DISCUSSION
This study was among the first to examine, in real world contexts, patterns of various tobacco product and other substance use and distinct cues associated with use of cigarettes, ENDS, and any tobacco products, respectively, guided by a social cognitive perspective.47 In terms of patterns of use, three-fourths of this sample used more than one tobacco product across the 21-day period, with a quarter using three or more. This level of use is higher than found in other samples.16,17,20,21 This might reflect our recruitment of participants who reported at least 15 days of tobacco use in the past 30 days on the longitudinal study survey into the EMA study. As such, our findings should be interpreted with this sample characteristic in mind. However, it is interesting to note the varied and distinct use profiles, with some participants using a single major tobacco product, while others “dabbled” across products. Notable in this sample were instances of co-use of cigarettes and ENDS, highlighting the need for research on the utility of ENDS in helping cigarette smokers switch or otherwise quit using cigarettes completely.12,13
Leveraging a social cognitive perspective,47 we examined a number of momentary influences on tobacco use, including timing, cravings, affect, social context, and other substance use. An important finding is that time of day or week showed no significant effect, which may be due to other factors such as other substance use or social context significantly contributing to the models and also accounting for time of day.
In addition, it is noteworthy that cravings predicted ENDS use among women, but cravings did not predict use of cigarettes or any tobacco product in those models. This may reflect the use of ENDS to reduce cigarette use or in situations where cigarette smoking is not allowed.110,111 In such cases, cravings may be likely to trigger intentional ENDS use behavior,110,111 whereas cigarette smoking might be associated with other contextual factors and/or cravings associated with cigarette smoking may be related to these other factors.60-78 In regards to the specificity of this finding for women, perhaps the women in this sample were specifically using ENDS for cessation or harm reduction. Indeed, women generally are more likely to want to quit smoking112 but have less success doing so.113,114
In terms of affect, while happiness did not show any specific associations with use, anxiety predicted cigarette use, and boredom was shown to be an important factor related to use of cigarettes among women, ENDS use among men, and any tobacco product use. These findings generally align with prior research, including EMA research, indicating the role of negative affect in tobacco use among youth and young adults.53,96,97 Indeed, our prior crosssectional research indicated that affect regulation motives and boredom relief predicted cigarette use (as well as use of cigar products and hookah), but these factors did not predict ENDS use.82 The specificity of the role of boredom relief among the different sexes in use of cigarettes and ENDS is difficult to interpret but may reflect differing functions of cigarettes and ENDS among women and men. For example, women may use cigarettes during leisure time when they may experience boredom and be in circumstances where smoking is more acceptable, while men may use ENDS in various contexts regardless of the circumstance in order to cope with boredom.82
Regarding social context, being alone versus with others did not predict use of cigarettes, ENDS, or any tobacco product. However, we did not assess the tobacco use status of others, thus limiting whether we could identify if tobacco use among others influenced individual tobacco use. In terms of other substance use, as indicated by the literature,84 use of cigarettes, ENDS, and any tobacco product use, respectively, was associated with greater odds of marijuana and alcohol use.
This study has important implications for research and practice. Findings indicated some common predictors (e.g., other substance use) and some specific predictors (e.g., anxiety, boredom) of use of ENDS, cigarettes, and any tobacco product, with some particularly noteworthy sex differences. This study did not explicitly assess reasons for using the various products, but there is some indication that women may have been using ENDS to quit or reduce smoking, whereas men may have been using them more recreationally. Future research is needed to further examine these associations and more explicitly assess use intentions. Moreover, future research should involve larger, more representative samples that would allow for stratified analyses and group comparisons, provide the ability to detect differences in motives for use among ATP and polytobacco users, and allow for generalizability of these findings to the broader young adult population (e.g., including non-college) who may portray more divers tobacco use profiles.2 The replication of these findings might suggest that intervening among women to address cravings may be important in reducing cigarette use, effectively using cessation pharmacotherapy options, and addressing polytobacco use, whereas addressing boredom and anxiety among men may be important factors in reducing tobacco-related health harm. Despite the caveats of this study, it is clear based on our findings and the broader literature84-87 that addressing other substance use is critical in reducing tobacco use.
Limitations
Limitations to this study include limited generalizability of the findings due to its recruitment from colleges and universities in the Southeast region of the US, the small sample size, the exclusion of participants missing more than 30% of the data points, and missing data among the analytic sample. Within this context, possible selection and/or response bias may have affected the data and the conclusions we were able to draw. Other limitations of the EMA data include the nature of self-reported responses and that not all participants included in the analyses responded to 100% of the assessments. Finally, the limited number of assessments (e.g., cravings, affect, social context) and the restricted duration of the study (i.e., 21 days) may only provide partial information regarding patterns and momentary influences on tobacco use. Related to the latter, the study was conducted between April and August 2016. Both circumstantial (e.g., final exams) and seasonal effects (i.e., summer) may have impacted study findings. Despite these limitations, the use of EMA to examine the phenomena of interest is a strength given the ecological validity of EMA, and the novel findings regarding the range of contextual factors in relation to use of cigarettes, ENDS, and any tobacco during this pivotal and dynamic tobacco market are critical.
Conclusions
The use of tobacco products – including cigarettes, ENDS, and any tobacco products – is associated with some common contextual factors (i.e., other substance use) as well as with some distinct momentary influences. As such, current EMA findings suggest that there may be specific intervention targets (e.g., anxiety, boredom, cravings) that may be more important in addressing cigarettes versus ENDS and that these intervention targets may be different for men versus women.
HIGHLIGHTS.
Little is known about daily/weekly use patterns or psychosocial triggers for using various tobacco products.
Ecological momentary assessment (EMA) studies are well-suited to addressing this research gap.
Distinct factors (e.g., timing, cravings, affect, social context) differentially predict use of cigarettes, e-cigarettes, and any tobacco.
Interventions may need to be specifically targeted for use of differing tobacco products among young adults.
ACKNOWLEDGEMENTS
We would like to thank our Campus Advisory Board for their efforts in supporting this research, as well as ICF International for their role in conducting survey assessments over the course of the longitudinal study.
FUNDING
This research was supported by the National Cancer Institute (1R01CA179422-01; PI: Berg) and by pilot funds from Emory University’s Winship Cancer Institute (co-PIs: McBride, Berg). The funders had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
DECLARATION OF INTERESTS
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.U.S. Department of Health and Human Services. Preventing Tobacco Use Among Young People: A Report of the Surgeon General. In: Atlanta GUSDoHaHS, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, ed1994. [Google Scholar]
- 2.Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: an emerging health risk behavior. Pediatrics. 2005;116(1):e113–119. [DOI] [PubMed] [Google Scholar]
- 3.Etter JF. Electronic cigarettes: a survey of users. BMC Public Health. 2010;10:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Lung Association. Hookah Smoking: A Growing Threat to Public Health Issue Brief. Washington, DC: American Lung Association;2011. [Google Scholar]
- 5.Callahan-Lyon P. Electronic cigarettes: human health effects. Tob Control. 2014;23 Suppl 2:ii36–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Cancer Institute. Smokeless Tobacco and Cancer. October 25, 2010. Bethesda, MD: National Cancer Institute;2010. [Google Scholar]
- 7.Chen J, Bullen C, Dirks K. A Comparative Health Risk Assessment of Electronic Cigarettes and Conventional Cigarettes. Int J Environ Res Public Health. 2017;14(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sterling KL, Berg CJ, Thomas AN, Glantz S, Ahluwalia JS. Factors associated with little cigar and cigarillo use among college students. American Journal of Health Behavior. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richter PA, Pederson LL, O'Hegarty MM. Young adult smoker risk perceptions of traditional cigarettes and nontraditional tobacco products. American Journal of Health Behavior. 2006;30(3):302–312. [DOI] [PubMed] [Google Scholar]
- 10.Kozlowski L, Warner K. Adolescents and e-cigarettes. Objects of concern may appear larger than they are. Drug and Alcohol Dependence. 2017. [DOI] [PubMed] [Google Scholar]
- 11.Gartner CE, Hall WD, Chapman S, Freeman B. Should the health community promote smokeless tobacco (snus) as a harm reduction measure? PLoS Med. 2007;4(7):e185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caraballo RS, Shafer PR, Patel D, Davis KC, McAfee TA. Quit Methods Used by US Adult Cigarette Smokers, 2014–2016. Prev Chronic Dis. 2017;14:E32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malas M, van der Tempel J, Schwartz R, et al. Electronic Cigarettes for Smoking Cessation: A Systematic Review. Nicotine Tob Res. 2016;18(10):1926–1936. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Chronic Disease P, Health Promotion Office on S, Health. Reports of the Surgeon General In: The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014. [Google Scholar]
- 15.Richardson A, Williams V, Rath J, Villanti AC, Vallone D. The next generation of users: prevalence and longitudinal patterns of tobacco use among US young adults. Am J Public Health. 2014;104(8):1429–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sung HY, Wang Y, Yao T, Lightwood J, Max W. Polytobacco Use of Cigarettes, Cigars, Chewing Tobacco, and Snuff Among US Adults. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soneji S, Sargent J, Tanski S. Multiple tobacco product use among US adolescents and young adults. Tobacco control. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Etter JF, Eissenberg T. Dependence levels in users of electronic cigarettes, nicotine gums and tobacco cigarettes. Drug Alcohol Depend. 2015;147:68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agaku IT, Alpert HR. Trends in annual sales and current use of cigarettes, cigars, roll-your-own tobacco, pipes, and smokeless tobacco among US adults, 2002–2012. Tob Control. 2015. [DOI] [PubMed] [Google Scholar]
- 20.Lee YO, Hebert CJ, Nonnemaker JM, Kim AE. Youth tobacco product use in the United States. Pediatrics. 2015;135(3):409–415. [DOI] [PubMed] [Google Scholar]
- 21.Lee YO, Hebert CJ, Nonnemaker JM, Kim AE. Multiple tobacco product use among adults in the United States: cigarettes, cigars, electronic cigarettes, hookah, smokeless tobacco, and snus. Preventive medicine. 2014;62:14–19. [DOI] [PubMed] [Google Scholar]
- 22.Chen P, Jacobson KC. Developmental Trajectories of Substance Use From Early Adolescence to Young Adulthood: Gender and Racial/Ethnic Differences. J Adolescent Health. 2012;50(2):154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mendel JR, Berg CJ, Windle RC, Windle M. Predicting young adulthood smoking among adolescent smokers and nonsmokers. Am J Health Behav. 2012;36(4):542–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agaku IT, King BA, Husten CG, et al. Tobacco product use among adults--United States, 2012–2013. MMWR Morb Mortal Wkly Rep. 2014;63(25):542–547. [PMC free article] [PubMed] [Google Scholar]
- 25.Berg CJ, Haardörfer R, Lewis M, et al. DECOY: Documenting Experiences with Cigarettes and Other Tobacco in Young Adults. American Journal of Health Behavior. 2016;40(3):310–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haardörfer R, Berg CJ, Lewis M, et al. Polytobacco, marijuana, and alcohol use patterns in college students: A latent class analysis. Addict Behav. 2016;59:58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Watt TT. The race/ethnic age crossover effect in drug use and heavy drinking. J Ethn Subst Abuse. 2008;7(1):93–114. [DOI] [PubMed] [Google Scholar]
- 28.Keyes KM, Vo T, Wall MM, et al. Racial/ethnic differences in use of alcohol, tobacco, and marijuana: Is there a cross-over from adolescence to adulthood? Soc Sci Med. 2015;124:132–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Latimer LA, Batanova M, Loukas A. Prevalence and harm perceptions of various tobacco products among college students. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2014;16(5):519–526. [DOI] [PubMed] [Google Scholar]
- 30.Mays D, Arrazola RA, Tworek C, Rolle IV, Neff LJ, Portnoy DB. Openness to Using Non-cigarette Tobacco Products Among U.S. Young Adults. American journal of preventive medicine. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Richardson A, Ganz O, Stalgaitis C, Abrams D, Vallone D. Noncombustible tobacco product advertising: how companies are selling the new face of tobacco. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2014;16(5):606–614. [DOI] [PubMed] [Google Scholar]
- 32.Berg CJ, Stratton E, Schauer GL, et al. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Substance use & misuse. 2015;50(1):79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dutra LM, Glantz SA, Lisha NE, Song AV. Beyond experimentation: Five trajectories of cigarette smoking in a longitudinal sample of youth. PLoS One. 2017;12(2):e0171808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bernat DH, Erickson DJ, Widome R, Perry CL, Forster JL. Adolescent smoking trajectories: results from a population-based cohort study. J Adolesc Health. 2008;43(4):334–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Riggs NR, Chou CP, Li C, Pentz MA. Adolescent to emerging adulthood smoking trajectories: when do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine Tob Res. 2007;9(11):1147–1154. [DOI] [PubMed] [Google Scholar]
- 36.Hair E, Bennett M, Williams V, et al. Progression to established patterns of cigarette smoking among young adults. Drug Alcohol Depen. 2017;177:77–83. [DOI] [PubMed] [Google Scholar]
- 37.Schweizer CA, Roesch SC, Khoddam R, Doran N, Myers MG. Examining the stability of young-adult alcohol and tobacco co-use: A latent transition analysis. Addict Res Theory. 2014;22(4):325–335. [Google Scholar]
- 38.Berg CJ, Haardörfer R, Lewis M, et al. DECOY: Documenting Experiences with Cigarettes and Other Tobacco in Young Adults. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berg CJ, Haardörfer R, Vu M, et al. Cigarette use trajectories in young adults: Analyses of multilevel predictors. Drug Alcohol Depen. 2018;188:281–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mays D, Gilman SE, Rende R, Luta G, Tercyak KP, Niaura RS. Parental smoking exposure and adolescent smoking trajectories. Pediatrics. 2014;133(6):983–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rose JS, Lee CT, Dierker LC, Selya AS, Mermelstein RJ. Adolescent nicotine dependence symptom profiles and risk for future daily smoking. Addict Behav. 2012;37(10):1093–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhan W, Dierker LC, Rose JS, Selya A, Mermelstein RJ. The Natural Course of Nicotine Dependence Symptoms Among Adolescent Smokers. Nicotine Tob Res. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nelson SE, Van Ryzin MJ, Dishion TJ. Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: demographic correlates and young adult substance use problems. Dev Psychopathol. 2015;27(1):253–277. [DOI] [PubMed] [Google Scholar]
- 44.Windle M, Windle RC. Early onset problem behaviors and alcohol, tobacco, and other substance use disorders in young adulthood. Drug Alcohol Depend. 2012;121(1–2):152–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McMillen R, Maduka J, Winickoff J. Use of emerging tobacco products in the United States. J Environ Public Health. 2012;2012:989474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Delnevo CD, Giovenco DP, Steinberg MB, et al. Patterns of Electronic Cigarette Use Among Adults in the United States. Nicotine Tob Res. 2016;18(5):715–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. [DOI] [PubMed] [Google Scholar]
- 48.Tyas S, Pederson L. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tobacco Control. 1998;7:409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cengelli S, O'Loughlin J, Lauzon B, Cornuz J. A systematic review of longitudinal population-based studies on the predictors of smoking cessation in adolescent and young adult smokers. Tobacco Control. 2011. [DOI] [PubMed] [Google Scholar]
- 50.Freedman KS, Nelson NM, Feldman LL. Smoking initiation among young adults in the United States and Canada, 1998–2010: a systematic review. Prev Chronic Dis. 2012;9:E05. [PMC free article] [PubMed] [Google Scholar]
- 51.Heatherton T, Kozlowski L, Frecker R, Fagerstrom K. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 52.Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84(7):791–799. [DOI] [PubMed] [Google Scholar]
- 53.Piasecki TM, Hedeker D, Dierker LC, Mermelstein RJ. Progression of nicotine dependence, mood level, and mood variability in adolescent smokers. Psychol Addict Behav. 2016;30(4):484–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Selya AS, Updegrove N, Rose JS, et al. Nicotine-dependence-varying effects of smoking events on momentary mood changes among adolescents. Addict Behav. 2015;41:65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shiffman S. Ecological Momentary Assessment (EMA) in Studies of Substance Use. Psychol Assessment. 2009;21(4):486–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dunbar MS, Scharf D, Kirchner T, Shiffman S. Do smokers crave cigarettes in some smoking situations more than others? Situational correlates of craving when smoking. Nicotine Tob Res. 2010;12(3):226–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shiffman S, Kirchner TR, Ferguson SG, Scharf DM. Patterns of intermittent smoking: An analysis using Ecological Momentary Assessment. Addict Behav. 2009;34(6–7):514–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Carey KB, Correia CJ. Drinking motives predict alcohol-related problems in college students. J Stud Alcohol. 1997;58(1):100–105. [DOI] [PubMed] [Google Scholar]
- 59.Kassel JD, Jackson SI, Unrod M. Generalized expectancies for negative mood regulation and problem drinking among college students. J Stud Alcohol. 2000;61(2):332–340. [DOI] [PubMed] [Google Scholar]
- 60.Piasecki TM, Richardson AE, Smith SM. Self-monitored motives for smoking among college students. Psychol Addict Behav. 2007;21(3):328–337. [DOI] [PubMed] [Google Scholar]
- 61.Budd GM, Preston DB. College student's attidudes and beliefs about the consequences of smoking: development and normative scores of a new scale. J Am Acad Nurse Pract. 2001;13(9):421–427. [DOI] [PubMed] [Google Scholar]
- 62.Piko BF, Wills TA, Walker C. Motives for smoking and drinking: country and gender differences in samples of Hungarian and US high school students. Addict Behav. 2007;32(10):2087–2098. [DOI] [PubMed] [Google Scholar]
- 63.Wills TA, Sandy JM, Shinar O. Cloninger's constructs related to substance use level and problems in late adolescence: a mediational model based on self-control and coping motives. Exp Clin Psychopharmacol. 1999;7(2):122–134. [DOI] [PubMed] [Google Scholar]
- 64.Berg CJ. Reasons for Nondaily Smoking among Young Adults: Scale Development and Validation. Journal of smoking cessation. 2014;9(1):17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khalil GE, Calabro KS, Prokhorov AV. Development and initial testing of the brief adolescent smoking curiosity scale (ASCOS). Addict Behav. 2018;78:67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nodora J, Hartman SJ, Strong DR, et al. Curiosity predicts smoking experimentation independent of susceptibility in a US national sample. Addict Behav. 2014;39(12):1695–1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pierce JP, Distefan JM, Kaplan RM, Gilpin EA. The role of curiosity in smoking initiation. Addict Behav. 2005;30(4):685–696. [DOI] [PubMed] [Google Scholar]
- 68.McCaul KD, Hockemeyer JR, Johnson RJ, Zetocha K, Quinlan K, Glasgow RE. Motivation to quit using cigarettes: a review. Addict Behav. 2006;31(1):42–56. [DOI] [PubMed] [Google Scholar]
- 69.Villanti AC, Bover Manderski MT, Gundersen DA, Steinberg MB, Delnevo CD. Reasons to quit and barriers to quitting smoking in US young adults. Fam Pract. 2016;33(2):133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Berg CJ, Parelkar PP, Lessard L, et al. Defining "smoker": college student attitudes and related smoking characteristics. Nicotine Tob Res. 2010;12(9):963–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wellman RJ, O'Loughlin EK, Dugas EN, Montreuil A, Dutczak H, O'Loughlin J. Reasons for quitting smoking in young adult cigarette smokers. Addict Behav. 2018;77:28–33. [DOI] [PubMed] [Google Scholar]
- 72.Myers MG, MacPherson L. Adolescent reasons for quitting smoking: initial psychometric evaluation. Psychol Addict Behav. 2008;22(1):129–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Turner LR, Mermelstein R. Motivation and reasons to quit: predictive validity among adolescent smokers. Am J Health Behav. 2004;28(6):542–550. [DOI] [PubMed] [Google Scholar]
- 74.Struik LL, O'Loughlin EK, Dugas EN, Bottorff JL, O'Loughlin JL. Gender differences in reasons to quit smoking among adolescents. JSch Nurs. 2014;30(4):303–308. [DOI] [PubMed] [Google Scholar]
- 75.Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011–2013. Nicotine Tob Res. 2015;17(2):228–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gritz ER, Prokhorov AV, Hudmon KS, et al. Predictors of susceptibility to smoking and ever smoking: a longitudinal study in a triethnic sample of adolescents. Nicotine Tob Res. 2003;5(4):493–506. [DOI] [PubMed] [Google Scholar]
- 77.Cronk NJ, Piasecki TM. Contextual and subjective antecedents of smoking in a college student sample. Nicotine Tob Res. 2010;12(10):997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Latane B. The Psychology of Social Impact. Am Psychol. 1981;36(4):343–356. [Google Scholar]
- 79.Moran S, Wechsler H, Rigotti NA. Social smoking among US college students. Pediatrics. 2004;114(4):1028–1034. [DOI] [PubMed] [Google Scholar]
- 80.Hoek J, Maubach N, Stevenson R, Gendall P, Edwards R. Social smokers' management of conflicted identities. Tob Control. 2012. [DOI] [PubMed] [Google Scholar]
- 81.Song AV, Ling PM. Social smoking among young adults: investigation of intentions and attempts to quit. Am J Public Health. 2011;101(7):1291–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wong E, Haardörfer R, Windle M, Berg CJ. Distinct Motives for Use among Polytobacco Versus Cigarette Only Users and among Single Tobacco Product Users. Nicotine and Tobacco Research. 2017;20(1):117–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Berg CJ, Haardörfer R, Schauer GL, et al. Reasons for Polytobacco Use among Young Adults: Scale Development and Validation. Tobacco Prevention & Cessation. 2016;26(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Substance Abuse and Mental Health Services Administration. Results from the 2014 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration;2015. [Google Scholar]
- 85.Bobakova D, Geckova AM, Klein D, Reijneveld SA, van Dijk JP. Protective factors of substance use in youth subcultures. Addict Behav. 2012;37(9):1063–1067. [DOI] [PubMed] [Google Scholar]
- 86.Bobo JK, Husten C. Sociocultural influences on smoking and drinking. Alcohol Res Health. 2000;24(4):225–232. [PMC free article] [PubMed] [Google Scholar]
- 87.Degenhardt L, Hall W. The relationship between tobacco use, substance-use disorders and mental health: results from the National Survey of Mental Health and Well-being. Nicotine Tob Res. 2001;3(3):225–234. [DOI] [PubMed] [Google Scholar]
- 88.Berg CJ, Payne JB, Henriksen LA, et al. Reasons for Marijuana and Tobacco Co-use among Young Adults: A Mixed Methods Scale Development Study. Substance Use and Misuse. 2017;53(3):357–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhu SH, Gamst A, Lee M, Cummins S, Yin L, Zoref L. The Use and Perception of Electronic Cigarettes and Snus among the U.S. Population. PLoS One. 2013;8(10):e79332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Berg CJ, Escoffery C, Bundy L, Haardoerfer R, Zheng P, Kegler MC. Cigarette users interest in using or switching to electronic nicotine delivery systems (ENDS) or smokeless tobacco for harm reduction, cessation, or novelty. Nicotine and Tobacco Research. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sterling KL, Berg CJ, Thomas AN, Glantz S, Ahluwalia JS. Factors associated with little cigar and cigarillo use among college students. American Journal of Health Behavior. 2013;37(3):325–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. [DOI] [PubMed] [Google Scholar]
- 93.Kirchner T, Shiffman S. Spatio-temporal determinants of mental health and well-being: Advances in geographically-explicit ecological momentary assessment. Social Psychiatry and Psychiatric Epidemiology. 2016;51(9):1211–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Serre F, Fatseas M, Swendsen J, Auriacombe M. Ecological momentary assessment in the investigation of craving and substance use in daily life: a systematic review. Drug Alcohol Depend. 2015;148:1–20. [DOI] [PubMed] [Google Scholar]
- 95.Pugach O, Hedeker D, Richmond MJ, Sokolovsky A, Mermelstein R. Modeling mood variation and covariation among adolescent smokers: application of a bivariate location-scale mixed-effects model. Nicotine Tob Res. 2014;16 Suppl 2:S151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kirchner TR, Shiffman S, Wileyto EP. Relapse dynamics during smoking cessation: Recurrent abstinence violation effects and lapse-relapse progression. Journal of Abnormal Psychology. (2011, July 25);Advance online publication. doi: 10.1037/a0024451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shiffman S, Kirchner TR. Cigarette-by-cigarette satisfaction during ad libitum smoking. Journal of Abnormal Psychology. 2009;118(2):348–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Businelle MS, Ma P, Kendzor DE, et al. Predicting Quit Attempts Among Homeless Smokers Seeking Cessation Treatment: An Ecological Momentary Assessment Study. Nicotine & Tobacco Research. 2014;16(10):1371–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yeh VM, McCarthy DE, Baker TB. An Ecological Momentary Assessment Analysis of Prequit Markers for Smoking-Cessation Failure. Exp Clin Psychopharm. 2012;20(6):479–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Shiffman S, Paty J. Smoking patterns and dependence: contrasting chippers and heavy smokers. J Abnorm Psychol. 2006;115(3):509–523. [DOI] [PubMed] [Google Scholar]
- 101.Berkman ET, Dickenson J, Falk EB, Lieberman MD. Using SMS Text Messaging to Assess Moderators of Smoking Reduction: Validating a New Tool for Ecological Measurement of Health Behaviors. Health Psychology. 2011;30(2):186–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Koblitz AR, Magnan RE, McCaul KD, O'Neill HK, Crosby R, Dillard AJ. Smokers' thoughts and worries: a study using ecological momentary assessment. Health Psychol. 2009;28(4):484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tseng TY, Ostroff JS, Campo A, et al. A Randomized Trial Comparing the Effect of Nicotine Versus Placebo Electronic Cigarettes on Smoking Reduction Among Young Adult Smokers. Nicotine & Tobacco Research. 2016;18(10):1937–1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kirchner TR SS-. Ecological Momentary Assessment In: MacKillop J, de Wit H, eds. The Wiley-Blackwell Handbook of Addiction Psychopharmacology. John Wiley & Sons, Ltd; 2013:541–565. [Google Scholar]
- 105.Pearson JL, Smiley SL, Rubin LF, et al. The Moment Study: protocol for a mixed method observational cohort study of the Alternative Nicotine Delivery Systems (ANDS) initiation process among adult cigarette smokers. Bmj Open. 2016;6(4):e011717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mead E, Chen J, Kirchner TR, Butler J, Feldman R. An ecological momentary assessment of cigar dual use among African American young adults. Nicotine and Tobacco Research. 2018;20(S1):S12–S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ferguson SG, Shiffman S, Gwaltney CJ. Does reducing withdrawal severity mediate nicotine patch efficacy? A randomized clinical trial. J Consult Clin Psychol. 2006;74(6):1153–1161. [DOI] [PubMed] [Google Scholar]
- 108.Blackwell E, de Leon CF, Miller GE. Applying mixed regression models to the analysis of repeated-measures data in psychosomatic medicine. Psychosom Med. 2006;68(6):870–878. [DOI] [PubMed] [Google Scholar]
- 109.Schwartz JE, Stone AA. The analysis of real-time momentary data: A practical guide In: Stone AA, Shiffman S, Atienza AA, Nebeling L, eds. The science of real-time data capture: Self-reports in health research. New York: Oxford University Press; 2007. [Google Scholar]
- 110.Berg CJ, Haardoerfer R, Escoffery C, Zheng PP, Kegler M. Cigarette Users' Interest in Using or Switching to Electronic Nicotine Delivery Systems for Smokeless Tobacco for Harm Reduction, Cessation, or Novelty: A Cross-Sectional Survey of US Adults. Nicotine & Tobacco Research. 2015;17(2):245–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Berg CJ. Preferred flavors and reasons for e-cigarette use and discontinued use among never, current, and former smokers. Int J Public Health. 2016;61(2):225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Borland R, Partos TR, Yong HH, Cummings KM, Hyland A. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control Four Country cohort survey. Addiction. 2012;107(3):673–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Smith PH, Bessette AJ, Weinberger AH, Sheffer CE, McKee SA. Sex/gender differences in smoking cessation: A review. Prev Med. 2016;92:135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Allen AM, Scheuermann TS, Nollen N, Hatsukami D, Ahluwalia JS. Gender Differences in Smoking Behavior and Dependence Motives Among Daily and Nondaily Smokers. Nicotine & Tobacco Research. 2016;18(6):1408–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]