Abstract
Objectives
Multiple systematic reviews have reported on the impact of rib fracture fixation in the presence of flail chest and multiple rib fractures, however this practice remains controversial. Our aim is to synthesise the effectiveness of surgical rib fracture fixation as evidenced by systematic reviews.
Design
A systematic search identified systematic reviews comparing effectiveness of rib fracture fixation with non-operative management of adults with flail chest or unifocal non-flail rib fractures. MEDLINE, EMBASE, Cochrane Database of Systematic Reviews and Science Citation Index were last searched 17 March 2017. Risk of bias was assessed using the Risk Of Bias In Systematic reviews (ROBIS) tool. The primary outcome was duration of mechanical ventilation.
Results
Twelve systematic reviews were included, consisting of 3 unique randomised controlled trials and 19 non-randomised studies. Length of mechanical ventilation was shorter in the fixation group compared with the non–operative group in flail chest; pooled estimates ranged from −4.52 days, 95% CI (−5.54 to –3.5) to −7.5 days, 95% CI (−9.9 to –5.5). Pneumonia, length of hospital and intensive care unit stay all showed a statistically significant improvement in favour of fixation for flail chest; however, all outcomes in favour of fixation had substantial heterogeneity. There was no statistically significant difference between groups in mortality. Two systematic reviews included one non-randomised studies of unifocal non-flail rib fracture population; due to limited evidence the benefits with surgery are uncertain.
Conclusions
Synthesis of the reviews has shown some potential improvement in patient outcomes with flail chest after fixation. For future review updates, meta-analysis for effectiveness may need to take into account indications and timing of surgery as a subgroup analysis to address clinical heterogeneity between primary studies. Further robust evidence is required before conclusions can be drawn of the effectiveness of surgical fixation for flail chest and in particular, unifocal non-flail rib fractures.
PROSPERO registration number
CRD42016053494.
Keywords: rib fracture, flail chest, multiple rib fractures, internal fixation, systematic review, meta-analysis, mortality, mechanical ventilation, length of hospital stay, pneumonia
Strengths and limitations of this study.
Multiple databases were searched for studies and study selection was undertaken by two researchers, reducing the risk of error.
Risk of bias of studies was assessed using the ROBIS tool by two researchers.
Primary research within the reviews was mapped to identify if the reviews were based on the same primary evidence.
Reviews were included regardless of risk of bias.
Introduction
Multiple rib fractures (adjacent unifocal fractures) and flail chest (three or more adjacent bifocal rib fractures with paradoxical chest wall movement) have high mortality (18.7%) due to the associated complications of acute respiratory distress syndrome, pneumonia and haemorrhage.1 Chest trauma accounts for 15% of all trauma admissions2 most commonly high-energy transfer injury as a result of a road traffic accidents (57.01%) but also from low energy falls (22.96%).1 Flail chest in particular has a high mortality rate as chest wall disruption causes an increase in the work of breathing for patients who are often in significant pain.
Current treatment options for severe chest injury are mainly supportive, including multimodal analgesia and anaesthesia, as well as non-invasive and invasive ventilation.3 Surgical fixation is thought to be beneficial to patients with respiratory failure,4 intractable pain5 or if failing to wean from invasive ventilation secondary to chest trauma.6 7 Fixation has potential to restore chest wall biomechanics and reduce the complications associated with poor ventilation and secretion clearance.7 Due to the rapidly, although heterogeneous, growing evidence base from multiple systematic reviews it is essential to synthesise evidence for this intervention to ascertain safety and efficacy.
This report is part of a wider systematic review to (1) identify and synthesise the evidence of the effectiveness of surgical rib fracture fixation, (2) evaluate the evidence for indications and timing of fixation and (3) identify the outcomes reported in the literature. Systematic reviews and primary studies were eligible for inclusion. This paper maps and synthesises this evidence from systematic reviews assessing the effectiveness of fixation of rib fractures.
Methods
The review was undertaken systematically using the methods described by the Centre for Reviews and Dissemination.8
Eligibility criteria
Population
Adults (over 18 years) who have sustained one or more rib fractures following blunt chest trauma, with or without pulmonary contusion were eligible. Single rib fracture, multiple rib fractures and flail chest injuries were included but treated as separate injuries and therefore reported and analysed separately. Patients with penetrating injuries were excluded. Studies of mixed populations with penetrating and non-penetrating injuries were included only if data were presented separately for the two groups. Surgery for chronic non-union was excluded.
Intervention
Any method of internal surgical fixation such as plate or strut fixation; metal or synthetic material including intramedullary splints and suture fixation were eligible for inclusion.
Comparator
External surgical fixation (traction methods, splints and Hoffman style pin and bar fixation) and non-surgical management (such as supportive ventilation, epidural and regional anaesthesia).
Outcomes
All outcomes were eligible (eg, mortality, pain and pneumonia). The primary outcome of interest was duration of mechanical ventilation due to the close relationship with mortality and morbidity of ventilator associated complications.
Study design
Inclusion
Systematic reviews were included if they specified a search strategy in at least one literature database and included primary research. No restrictions were placed on the study design of the primary studies.
Exclusion
Literature reviews that did not have a defined research question, search strategy or defined process of selecting articles.
Search strategy
MEDLINE including PreMEDLINE, EMBASE, Cochrane Database of Systematic Reviews and Science Citation Index. Clinical guidance, policy documents and relevant databases such as National Institute for Health and Care Excellence (NICE) Evidence, the UK Department of Health policy content, National Clinical Guideline Centre and Scottish Intercollegiate Guidelines Network were searched on 14 December 2016 and updated on 13 March 2017. The Conference Proceedings Citation Index was also searched for unpublished literature.
The start date for the MEDLINE searches was 1976 as that was the year that Advance Trauma Life Support was introduced internationally, incorporating new methods of resuscitation which have significantly improved outcomes.
The search strategy, developed for MEDLINE, is provided in online supplementary file 1 and was adapted to run appropriately on other databases. To identify relevant further reviews reference lists of included studies were assessed for eligibility.
bmjopen-2018-023444supp001.pdf (34.9KB, pdf)
Selection
Searches were downloaded into Endnote X7 (Clarivate Analytics, V.7.1 release date 2 April 2014) and de-duplicated. Two researchers (HI and EC) independently screened titles and abstracts. Any paper classified as potentially eligible by either reviewer was ordered as a full text and independently screened by both reviewers. It was originally planned to have second screening of only 50% but resources allowed for full duplicate screening. A third researcher reviewed disagreements (CM) where a consensus could not be reached between the researchers.
Data extraction
Extracted data included study characteristics, patient characteristics, intervention, comparator, outcome measures, duration of follow-up, effect estimates, SE and CIs as available.
One researcher completed data extraction (HI); a second researcher cross-checked 50% (EC). Discrepancies were cross-checked by both researchers at a second review and a consensus reached.
Risk of bias
Quality assessment with the ROBIS tool9 was undertaken by one researcher (HI) and checked by a second (CM). Discrepancies were resolved by discussion.
Data synthesis
All types of internal surgical fixation were synthesised as one group. Flail chest and multiple rib fractures are considered different injuries and were synthesised separately for each outcome extracted. Each outcome was narratively synthesised including number of reviews using the outcome and effect estimates with 95% CIs from the source review. Important numerical data was presented in tables for all outcomes measured. All outcomes that were reported in the reviews were included in the report to avoid reporting bias.10 Although not fully applicable, reporting was in accordance as much as possible with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.11
Protocol deviations
The registered protocol encompasses a larger body of work which includes synthesis of primary research for effectiveness, indications for surgery, timing of surgery and mapping of outcome measures. Only the synthesis of systematic reviews is reported here. Although all outcomes were extracted and presented in tables only those that were measured in two or more studies were narratively synthesised.
Patient involvement
Patients were not involved in the preparation or conduct of this review.
Results
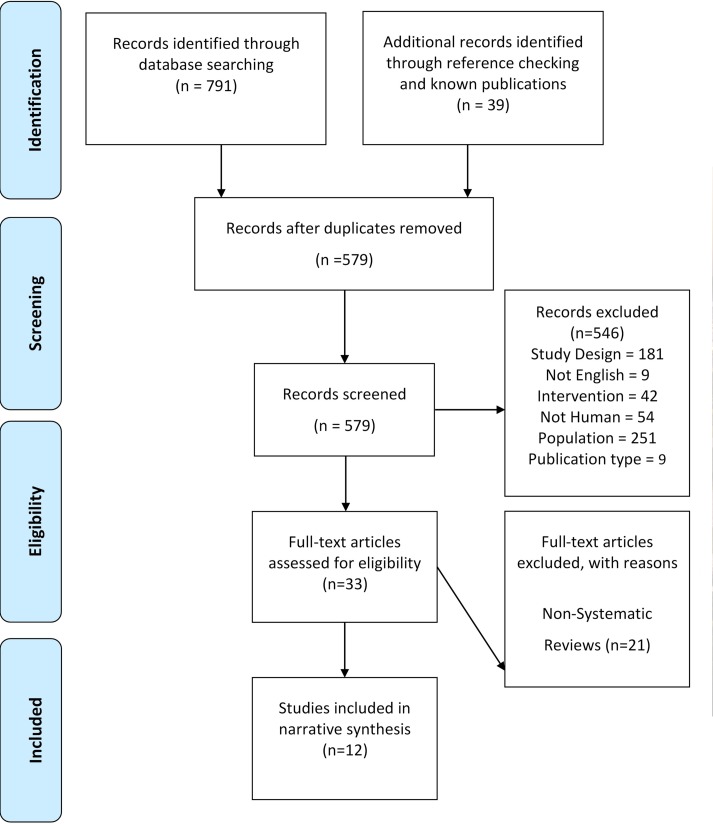
Electronic searches identified 791 records; an additional 39 records were collected following reference checking. The full text screening identified 12 systematic reviews eligible for inclusion, there were 21 papers excluded because they were not classified as systematic reviews (figure 1). See online supplementary file 2 lists the excluded studies.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
bmjopen-2018-023444supp002.pdf (475KB, pdf)
Review characteristics
Eleven systematic reviews and one rapid evidence synthesis,12 published between 2010 and June 2016, met the inclusion criteria. Table 1 provides a summary of review characteristics. Three of the reviews13–15 were presented as best evidence topics16
Table 1.
Review characteristics
| Review Year Country |
Review aim | Search strategy | Studies and participants | Patient, Intervention, Comparator, Outcome and Study type (PICOS) | Risk of bias | Authors’ conclusions |
| Swart et al
17
2017 USA |
To perform a meta-analysis of high quality literature to evaluate both economic and medical benefits of early fixation of rib fractures in severe chest trauma. | PubMed, Embase, Medline and Scopus. No search start date. Last search date 1 June 2016. Search terms defined, No limitations described. Evidence of hand searching. Eligibility criteria: over 18 years of age and studies comparing operative versus non-operative treatment, |
3 RCT n=123 14 Case–control 3 Case series |
Population
Acute flail chest 18 years or older. Intervention Operative fixation. Comparator Non-operative. Studies type All study designs. |
No evidence of quality assessment. | Acute ORIF of rib fractures in patients with flail chest injuries results in reduced mortality and medical complications in conjunction with being cost effective intervention. |
| Schuurmans et al
18
2017 The Netherlands |
Investigate how operative management improves patient care for adults with flail chest. | PubMed, Trip database, Google Scholar. No search start date. Last search date November 2015. Search terms defined, No limitations described. Evidence of reference checking. Eligibility criteria: studies comparing operative versus non-operative treatment, RCT only and English. |
3 RCT n=123 |
Population
Acute flail chest. Intervention Operative fixation. Comparator Non-operative. Studies type RCTs. |
Quality assessment completed but criteria and explanation unclear. | The operative management group showed a significant lower incidence of pneumonia, whereas mortality rate did not differ between treatment groups. |
| Schulte et al
13
2016 UK |
In patients with acute flail chest does surgical rib fixation improve outcomes in terms of morbidity and mortality? | OVID MEDLINE. Search start date 1946. Last search date January 2016. Search terms defined. Search strategy description minimal, no limitations described. No evidence of reference checking. No specific inclusion or exclusion criteria defined. |
1 Meta-analysis by separate author. 1 RCT n=123 (2 further coded as RCT which are non-randomised studies). 3 Retrospective cohort studies. |
Population
Acute flail chest. Intervention Operative fixation. Comparator Non-operative. Studies type Unclear. |
No evidence of quality assessment. | Surgical stabilisation of flail chest in thoracic trauma patients has beneficial effects with respect to reduced ventilatory support, shorter intensive care and hospital stay, reduced incidence of pneumonia and septicaemia, decreased risk of chest deformity and an overall reduced mortality when compared with patients who received non-operative management. |
| Coughlin et al
19
2016 UK |
Compare the efficacy of flail chest surgical stabilisation to non-operative management. | PubMed MEDLINE, Embase, Cochrane Library, clinical trials.gov. No search start date. Last search date February 2015. Search terms defined, No limitations. Evidence of reference checking. Eligibility criteria: studies comparing operative versus non-operative treatment in flail chest and RCT only. |
3 RCT n=123 |
Population
Traumatic flail chest. Intervention Surgical stabilisation of any kind. Comparator Patients treated non-operatively by any other means. Studies type RCTs only. |
Clear quality appraisal of the studies. | Surgical stabilisation for a traumatic flail chest is associated with significant clinical benefits including rate of pneumonia, length of hospital an ICU stay and duration of mechanical ventilation in this meta-analysis of three relatively small RCTs. |
| Unsworth et al
24
2015 Australia |
To review the treatments for blunt chest trauma and their impact on patient and hospital outcomes. Specifically alludes to surgical stabilisation of flail chest. |
Cochrane, Medline, EMBASE and CINAHL databases. Search limited to 1990 onwards. Last search date March 2014. Search terms defined. Limited to humans and adults. Evidence of reference checking. Eligibility criteria: original research, blunt chest trauma, intervention for blunt chest trauma including a comparator and contained measured outcomes. |
3 RCT n=123 5 Retrospective case–controls n=642. 1 Retrospective cohort n=21. |
Population
Adult blunt chest trauma. Flail chest. Intervention Multidisciplinary intervention (models of care, management intervention, care practices, care protocols). Comparator Other intervention not specified. Studies type RCTs. |
Some quality assessment completed but criteria and explanation unclear. | Across the literature there were consistent improvements in patients with flail chest and surgical fixation with fewer days of mechanical ventilation, ICU-LOS and cost savings compared with non-operative techniques. Three out of nine studies were randomised controlled trials, and the level of evidence in all studies was primarily fair or good. |
| de Lesquen et al
15
2015 France |
In flail chest is open reduction and internal fixation needed? | Medline and Science Direct. Search start date limited to 1994 onwards. Last search date January 2014. Search Terms defined. No evidence of hand searching or reference checking. Eligibility criteria: Exclusions of both child and vascular injuries. |
2 Meta-analysis. 3 RCT n=123. 1 Prospective cohort n=60. 5 Retrospective cohort n=238. |
Population
Blunt chest trauma. Flail chest. Intervention Open reduction and internal fixation. Comparator Unclear. Studies type Unclear. |
No evidence of quality assessment. | For flail chest, early surgical stabilisation can be considered in patients who would require mechanical ventilation for >48 hours. |
| Cataneo et al
20
2015 Brazil |
To evaluate the effectiveness and safety of surgical stabilisation compared with clinical management for people with flail chest. | Cochrane Injuries Group Specialised Register, CENTRAL, Medline, Embase, CINAHL, SCI, CPCI-S, Clinical trials.gov, ICTR. No search start date. Last search Date 12 May 2014. Search terms defined, no limitations. Evidence of reference checking. Eligibility criteria: RCTs. |
3 RCTs n=123. |
Population
Adults or children with flail chest. Intervention Surgical stabilisation of any kind. Comparator Clinical management included any type of chest wall stabilisation without surgical intervention such as straps or bags and any type of ventilatory assistance. Studies type RCTs only. |
Clear quality appraisal of the studies. | There was no evidence that surgical intervention reduced mortality in people with FC compared with non-surgical management. There was some evidence that surgical intervention could reduce the risk of developing pneumonia and thoracic deformity; need for tracheostomy; duration of mechanical ventilation, length of ICU stay and hospital stay; and chronic pain, but the trials to date have been small. There is an urgent need for larger high-quality randomised con-trolled trials. |
| de Jong et al
23
2014 The Netherlands |
To specify indications for rib fracture fixation of non-flail chests. | Medline, Cochrane, Embase. Search start date limited to 2010. Last search date December 2013. Search terms defined, limited to year 2000 onwards. Evidence of reference checking. Eligibility criteria: Studies included at least 10 participants who were surgically treated for non-flail chest rib fractures. Reported in English, Dutch or German. Excluded were case reports, biomechanical studies, animal studies and expert opinions. |
1 Case–control n=60. 2 Cohort studies n=47. |
Population
Traumatic non-flail chest. Intervention Surgical treatment of non-flail chest. Comparator Unclear. Studies type All studies with at least 10 surgically treated. |
No evidence of quality assessment. | The evidence for surgical treatment of non-flail chest rib fractures is limited. |
| Slobogean et al
21
2013 Canada |
Compare the critical care outcomes of surgical fixation to non-operative management in patients with flail chest injuries. | Medline, Embase, Cochrane Database of Systematic Reviews and the Cochrane Central, Register of Controlled Trials (CENTRAL). No search start date. Last search date May 2011. No limitations. No evidence of reference checking or hand searching. Eligibility criteria: Comparator studies with more than 10 cases. |
2 RCTs. 1 Case–control n=60. 8 Cohort n=676. |
Population
Acute flail chest. Intervention Operative fixation. Comparator Conservative management. Studies Type RCTs. |
No evidence of quality assessment. | Improved outcomes of multiple critical care outcomes with narrow CIs but based on small retrospective studies. Suggests prospective RCT to overcome potential biases. |
| Leinicke et al
22
2013 USA |
Comparing operative to non-operative therapy in adult flail chest patients. | MEDLINE (1966–2012), Embase (1947–2012), Scopus (all years), Cochrane Databases and ClinicalTrials.gov Last search date February 2012. Search terms defined, limited to English and human studies. Evidence of reference checking. Eligibility criteria: Studies comparing operative versus non-operative treatment in patients with flail chest. Excluded case reports and case series. |
2 RCTs. 3 Case–control n=158. 4 Cohort n=303. |
Population
Flail chest. Intervention Operative fixation. Comparator Non-operative. Studies type RCTs, cohort and case-control trials. |
Clear quality appraisal of the studies. | As compared with non-operative therapy, operative fixation of FC is associated with reductions in DMV, LOS, mortality and complications associated with prolonged MV. These findings support the need for an adequately powered clinical study to further define the role of this intervention. |
| Girsowicz et al
14
2012 France |
In patients over 45 years old with isolated, movable and painful rib fractures without true flail chest is surgical stabilisation superior to non-operative management in improving outcomes? | OVID Medline 1948 –2011. Last search date June 2011. Search terms defined, limited to Human and English language. Evidence of reference checking. Eligibility criteria: Excluded flail chest but inclusions not well described. |
4 Retrospective cohort n=107. 1 Non-systematic review. 1 Case–control=30. 2 Case report n=2. |
Population
Over 45 years old with isolated, movable and painful. Rib fractures without true flail chest. Intervention surgical stabilisation. Comparator Non-operative management. Studies type Unclear. |
Some comments on strengths and weaknesses but no quality or risk of bias assessment. | Surgical stabilisation in the management of isolated multiple non-flail and painful rib fractures improved outcomes (pain, respiratory function, quality of life and reduced socio-professional disability). Studies provided a low level of evidence (small studies with few numbers of patients and short-term follow-up or case reports). Large prospective controlled trials are thus necessary to confirm these encouraging results. |
| NICE Evidence12
2010 UK |
To make recommendations about the safety and efficacy of surgical rib fracture fixation in flail chest. | MEDLINE, PREMEDLINE, EMBASE, Cochrane Library. No search start date. Last search date May 2010. Search terms defined. No limitations. No evidence of reference checking but other searches performed. Eligibility criteria: clinical studies of patients with flail chest operated with metal rib reinforcements and published in English. Excluded conference abstracts and reviews. |
1 RCT. 2 Non-randomised studies. Four case series. Total 225 patients. |
Population
Flail chest. Intervention Insertion of metal rib reinforcements. Comparator Unclear. Studies type Clinical studies were included. Abstracts were excluded where no clinical outcomes were reported or where the paper was a review, editorial or a laboratory or animal study. Conference abstracts were also excluded. |
No evidence of quality assessments. | Surgical rib fracture fixation should be consider in patients with flail chest. |
DMV, duration of mechanical ventilation; FC, flail chest; ICU, Intensive care unit; LOS, length of stay; MV, mechanical ventilation; NICE, National Institute for Health and Care Excellence; ORIF, open reduction internal fixation; RCT, randomised controlled trial.
Nine reviews12 13 15 17–22 evaluated the effectiveness of internal surgical fixation in patients with flail chest, two included patients with multiple rib fractures14 23 and one included all rib fractures but only reported outcomes for flail chest.24
Three reviews18–20 included only RCTs and eight included other study designs12–15 17 21–23 (two systematic reviews, 19 non-randomised studies, 11 case series and two case reports) (table 2). As would be expected, there was overlap across the reviews in the included primary studies. The total number of patients who had internal fixation in primary studies (excluding duplicate studies) was 1036, and there were 1187 controls.
Table 2.
Primary studies included in each review and the number of included patients
| Studies | |||||||||||||||||||||||||||||||||||||
| Review | Leinicke et al 36 | Slobogean et al 21 | Tanaka et al 25 | Granetzny et al 26 | Marasco et al 27 | Paris et al 53 | Kim et al 28 | Karev29 | Ahmed and Mohyuddin37 | Voggenreiter et al 30 | Balci et al 31 | Teng et al 32 | Nirula et al 33 | Althausen et al 54 | De Moya et al 5 | Granhed and Pazooki55 | Doben et al 56 | Jayle et al 57 | Pieracci et al 58 | Zhang et al 59 | Wada et al 60 | Xu et al 61 | Majercik et al 62 | DeFreest et al 63 | Ohresser et al 39 | Hellberg et al 64 | Menard et al 65 | Mouton et al 66 | Cacchione et al 44 | Lardinois et al 67 | Kerr-Valentic et al 68 | Gasparri et al 45 | Borrelly and Aazami38 | Campbell et al 40 | Mayberry et al 41 | Richardson et al 42 | Moreno De La et al 43 |
| Intervention patients | 18 | 20 | 23 | 18 | 18 | 40 | 26 | 20 | 27 | 32 | 30 | 22 | 16 | 60 | 10 | 10 | 35 | 24 | 84 | 17 | 38 | 41 | 14 | 10 | 18 | 23 | 1 | 66 | 40 | 1 | 127 | 32 | 46 | 7 | 22 | ||
| Control patients | 19 | 20 | 23 | 11 | 45 | 93 | 38 | 22 | 37 | 28 | 30 | 28 | 32 | 153 | 11 | 10 | 35 | 15 | 420 | 15 | 57 | 45 | – | – | – | – | – | – | – | – | – | – | – | – | – | ||
| Swart et al 17 | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | |||||||||||||||||
| Schuurmans et al 18 |
● | ● | ● | ||||||||||||||||||||||||||||||||||
| Schulte et al 13 |
● | ● | ● | ● | ● | ● | ● | ● | ● | ● | |||||||||||||||||||||||||||
| Coughlin et al 19 |
● | ● | ● | ||||||||||||||||||||||||||||||||||
| Unsworth et al 24 |
● | ● | ● | ● | ● | ● | ● | ● | ● | ||||||||||||||||||||||||||||
| de Lesquen et al 15 |
● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ||||||||||||||||||||||||||
| Cataneo et al 20 |
|||||||||||||||||||||||||||||||||||||
| de Jong et al 23 |
● | ● | ● | ||||||||||||||||||||||||||||||||||
| Slobogean et al 21 |
● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ||||||||||||||||||||||||||
| Leinicke et al 22 |
● | ● | ● | ● | ● | ● | ● | ● | |||||||||||||||||||||||||||||
| Girsowicz et al 14 |
● | ● | ● | ● | ● | ● | ● | ● | |||||||||||||||||||||||||||||
| NICE12 | ● | ● | ● | ● | ● | ● | ● | ||||||||||||||||||||||||||||||
| Systematic review | Randomised control trial | Non-randomised study | Case series or report | ||||||||||||||||||||||||||||||||||
NICE, National Institute for Health and Care Excellence.
The rapid evidence synthesis by NICE12 was the first review published in 2010, consisting of seven primary studies including one RCT published in 2001.25 Cataneo et al 20 was the first meta-analysis published (in 2015) and included three RCTs.25–27 Two further systematic reviews published since then18 19 identified the same three RCTs and repeated the same meta-analyses for the same review question.
Risk of bias
Seven reviews rated as low risk of bias,12 15 18–22 three as unclear14 17 23 and two as high.13 24 (table 3)The high risk of bias rating was due to lack of detail in the search strategy, no attempts to minimise errors of data extraction and no quality assessment of included studies.
Table 3.
Risk of bias using ROBIS tool
| Studies | Study eligibility criteria | Identification and selection of studies | Data collection and study appraisal | Synthesis and findings | Risk of bias in the review |
| Swart et al 17 | Low | Unclear | High | High | Unclear |
| Schuurmans et al 18 | Low | Unclear | High | Low | Low |
| Schulte et al 13 | High | High | High | High | High |
| Coughlin et al 19 | Low | Low | Low | Low | Low |
| Unsworth et al 24 | Low | Low | Unclear | Unclear | High |
| de Lesquen et al 15 | Unclear | High | Unclear | Unclear | Low |
| Cataneo et al 20 | Low | Low | Low | Low | Low |
| de Jong et al 23 | High | Unclear | High | High | Unclear |
| Slobogean et al 21 | Low | Low | High | Low | Low |
| Leinicke et al 22 | Low | Low | Low | Low | Low |
| Girsowicz et al 14 | High | High | High | High | Unclear |
| NICE12 | Low | Unclear | Unclear | Low | Low |
NICE, National Institute for Health and Care Excellence.
The only review for which a protocol was identified was the Cochrane review undertaken by Cataneo et al.20
Outcome evaluation
All reviews undertook a narrative synthesis with six also including a meta-analysis.17–22 Table 4 summarises the meta-analyses for flail chest, table 5 summarises the narrative syntheses for flail chest and table 6 the narrative syntheses for multiple rib fractures. Across all the reviews, 18 outcomes were reported and 11 outcomes were reported by more than one review.
Table 4.
Results of individual reviews that report a meta-analysis for flail chest
| Total length of invasive mechanical ventilation (days) | ||||||
| Studies reporting outcome | No of studies (no of participants in analysis) | Study types | Details of meta-analysis | Results | I2 | |
| RCT | NR | |||||
| Cataneo et al 20 | 3 (123) | 3 | 0 | MD (IV, fixed, 95% CI) | Results not pooled | – |
| Coughlin et al 19 | 3 (123) | 3 | 0 | MD (IV, random, 95% CI) | −6.30 (−12.16 to –0.43) | 95 |
| Leinicke et al 22 | 8 (474) | 2 | 6 | MD (IV, random 95% CI) | −4.52 (−5.54 to –3.50) | 48.6 |
| Schuurmans et al 18 | 3 (123) | 3 | 0 | MD (IV, random, 95% CI) | −6.53 (−11.88 to –1.18) | 93 |
| Slobogean et al 21 | 8 Studies (563) | 2 | 6 | MD (IV, fixed, 95% CI) | −7.5 (−9.9 to –5.0) | 48 |
| Swart et al 17 | 18 Studies (1150) | 3 | 15 | MD (IV, random, SD) | −4.57 (0.59) | 83 |
| Mortality (frequency) | ||||||
| Cataneo et al 20 | 3 (123) | 3 | 0 | RR (M-H, fixed, 95% CI) | 0.56 (0.13 to 2.42) | 0 |
| Coughlin et al 19 | 2 (86) | 2 | 0 | RR (M-H, random, 95% CI) | 0.57 (0.13 to 2.52) | 0 |
| Leinicke et al 22 | 5 (343) | 1 | 0 | RR (95% CI) | 0.43 (0.28 to 0.69) | 0 |
| Schuurmans et al 18 | 2 (86) | 2 | 0 | RR (M-H, fixed, 95% CI) | 0.56 (0.13 to 2.42) | 0 |
| Slobogean et al 21 | 7 (582) | 2 | 5 | OR (M-H, fixed, 95% CI) | 0.31 (0.20 to 0.48) | – |
| Slobogean et al 21 | 7 (582) | 2 | 5 | RR (M-H, fixed, 95% CI) | 0.19 (0.13 to 0.26) | 0 |
| Swart et al 17 | 13 (1263) | 3 | 10 | RR (M-H, random, SD) | 0.44 (0.09) | 0 |
| Total length of stay in intensive care unit (days) | ||||||
| Cataneo et al 20 | 2 (77) | 2 | 0 | MD (IV, fixed, 95% CI) | Results not pooled | – |
| Coughlin et al 19 | 3 (123) | 3 | 0 | MD (IV, random, 95% CI) | −6.46 (−9.73 to –3.19) | 35 |
| Leinicke et al 22 | 5 (235) | 2 | 3 | MD (IV, random, 95% CI) | −3.4 (−6.01 to –0.80) | 74.9 |
| Schuurmans et al 18 | 3 (123) | 3 | 0 | MD (IV, fixed, 95% CI) | −5.18 (−6.17 to –4.19) | 40 |
| Slobogean et al 21 | 4 (261) | 2 | 2 | MD (IV, fixed, 95% CI) | −4.8 (−7.9 to –1.6) | 0.1 |
| Swart et al 17 | 14 (840) | 3 | 11 | MD (IV, random, SD) | −3.25 (1.29) | 91 |
| Total length of stay in hospital (days) | ||||||
| Coughlin et al 19 | 2 (86) | 2 | 0 | MD (IV, random, 95% CI) | −11.39 (−12.39 to –10.38) | 0 |
| Leinicke et al 22 | 5 (262) | 1 | 4 | MD (IV, random 95% CI) | −3.83 (−7.12 to –0.54) | 68.9 |
| Schuurmans et al 18 | 2 (86) | 2 | 0 | MD (IV, fixed, 95% CI) | −11.39 (−12.39 to –10.38) | 0 |
| Slobogean et al 21 | 4 (404) | 1 | 3 | MD (IV, fixed, 95% CI) | −4.0 (−7.4 to –0.7) | 33 |
| Swart et al 17 | 11(438) | 1 | 10 | MD (IV, random, SD) | −4.48 (1.98) | 89 |
| Pneumonia (frequency) | ||||||
| Cataneo et al 20 | 3 (123) | 3 | 0 | RR (M-H, random, 95% CI) | 0.36 (0.15 to 0.85) | 66 |
| Coughlin et al 19 | 3 (123) | 3 | 0 | RR (M-H, random, 95% CI) | 0.36 (0.15 to 0.85) | 66 |
| Leinicke et al 22 | 4 (260) | 1 | 3 | RR (95% CI) | 0.43 (0.28 to 0.69) | 31 |
| Schuurmans et al 18 | 2 (83) | 2 | 0 | RR (M-H, fixed, 95% CI) | 0.45 (0.29 to 0.7) | 74 |
| Slobogean et al 21 | 8 (816) | 2 | 6 | OR (M-H, fixed, 95% CI) | 0.18 (0.11 to 0.32) | 4 |
| Slobogean et al 21 | 8 (816) | 2 | 6 | RR (M-H, fixed, 95% CI) | 0.31 (0.21 to 0.41) | 4 |
| Swart et al 17 | 15 (1005) | 3 | 12 | RR (M-H, random, SD) | 0.59 (0.10) | 55 |
| Tracheostomy (frequency) | ||||||
| Cataneo et al 20 | 2 (83) | 2 | 0 | RR (M-H, random, 95% CI) | 0.38 (0.14 to 1.02) | 64 |
| Leinicke et al 22 | 4 (215) | 1 | 3 | RR (95% CI) | 0.25 (0.13 to 0.47) | 0 |
| Schuurmans et al 18 | 2 (83) | 2 | 0 | RR (M-H, fixed, 95% CI) | 0.4 (0.2 to 0.7) | Not reported |
| Slobogean et al 21 | 3 (165) | 1 | 2 | OR (M-H, fixed, 95% CI) | 0.12 (0.04 to 0.32) | 0 |
| Slobogean et al 21 | 3 (165) | 1 | 2 | RR (M-H, fixed, 95% CI) | 0.34 (0.10 to 0.57) | 0 |
| Swart et al 17 | 11 (975) | 2 | 9 | RR (M-H, random, SD) | 0.52 (0.07) | 42 |
| Sepsis (frequency) | ||||||
| Slobogean et al 21 | 4 (345) | 0 | 4 | OR (M-H, fixed, 95% CI) | 0.36 (0.19 to 0.71) | 0 |
| Slobogean et al 21 | 4 (345) | 0 | 4 | RR (M-H, fixed, 95% CI) | 0.14 (0.56 to 0.23) | 0 |
| Spirometry (percentage of predicated) | ||||||
| Coughlin et al 19 | – | – | – | – | – | – |
| FVC | 2 (74) | 2 | 0 | MD (IV, random, 95% CI) p value | 1.53 (−13.49 to 16.55) p=0.84 | Not reported |
| FEV1 | 2 (74) | 2 | 0 | MD (IV, random, 95% CI) p value | −0.42 (−4.83 to 3.98) p=0.85 | Not reported |
| TLC | 2 (74) | 2 | 0 | MD (IV, random, 95% CI) p value | 3.69 (−3.08 to 10.46) p=0.29 | Not reported |
| PEFR | 2 (74) | 2 | 0 | MD (IV, random, 95% CI) p value | 0.38 (−0.76 to 1.53) p=0.51 | Not reported |
| Chest deformity (frequency) | ||||||
| Cataneo et al 20 | 2 (86) | 2 | 0 | RR (M-H, fixed, 95% CI) | 0.13 (0.03 to 0.67) | 0 |
| Slobogean et al 21 | 4 (228) | 1 | 3 | OR (M-H, fixed, 95% CI) | 0.11 (0.02 to 0.60) | 2.1 |
| Slobogean et al 21 | 4 (228) | 1 | 3 | RR (M-H, fixed, 95% CI) | 0.30 (0.00 to 0.60) | 2.1 |
| Dyspnoea (frequency) | ||||||
| Slobogean et al 21 | 3 (135) | 1 | 2 | OR (M-H, fixed, 95% CI) | 0.40 (0.16 to 1.01) | 0 |
| Slobogean et al 21 | 3 (135) | 1 | 2 | RR (M-H, fixed, 95% CI) | 0.15 (0.09 to 0.39) | 0 |
| Chest pain (frequency) | ||||||
| Slobogean et al 21 | 2 (71) | 1 | 1 | OR (M-H, fixed, 95% CI) | 0.40 (0.01 to 12.60) | 0 |
| Slobogean et al 21 | 2 (71) | 1 | 1 | RR (M-H, fixed, 95% CI) | 0.18 (-0.46 to 0.83) | 0 |
FEV1, forced expiratory volume; FVC, force vital capacity; IV, inverse variance; M-H, Mantel-Haenszel; MD, mean difference; NR, non-randomised study; PEFR, peak expiratory flow rate; RCT, randomised controlled trial; RR, risk ratio; TLC, total lung capacity.
Table 5.
Results of individual reviews that report a narrative synthesis for flail chest
| Study details | Included studies | Outcomes assessed | Narrative synthesis |
|
Author
Unsworth et al 24 Year 2015 Country Australia |
RCT=2 Granetzny (40) Tanaka (37) Marasco (46) Non-randomised=6 Ahmed (64) Althausen (50) Doben (21) De Moya (48) Nirula (60) Voggenreiter (42) Total number of patients=408 |
|
|
|
Author
de Lesquen et al 15 Year 2015 Country France |
Meta-analysis=2 Leinicke nine studies (538 patients) Slobogean 11 studies (732 patients) RCT=3 Marasco (46) Granetzny (40) Tanaka (37) Non-randomised=6 Ahmed (64) Karev (40) Voggenreiter (20) Balci (64) Nirula (60) Althausen (50) Total number of patients=421 |
|
For flail chest, early surgical stabilisation can be considered in patients who would require mechanical ventilation for >48 hours. (Grade B, extrapolated recommendations from level I evidences.) |
|
Author
NICE12 Year 2010 Country UK |
RCT=1 Tanaka (37) Non-randomised=2 Voggenreiter (42) Paris (29) Case Series=4 Lardinois (66) Mouton (23) Menard (18) Hellberg (10) Total number of patients=225 Intervention group=173 Control group=52 |
|
Surgical stabilisation with metal rib reinforcements aims to allow earlier weaning from mechanical ventilation, reduce acute complications and avoid chronic pain sometimes associated with permanent malformation of the chest wall. Kirschner wire may be used on its own, but this method of rib stabilisation is not covered by this guidance. |
|
Author
Schulte et al 13 Year 2016 Country UK |
Systematic review=1 Slobogean (753) RCT=1 Marasco (23,23) Non-randomised studies=9 Jayle (10,10) Pieracci (35,35) Zhang (24,15) Wada (84,336) Granhed (60,153) Doben (10,11) Xu (17,15) Althausen (22,28) De Moya (16,32) Total number of patients=1712 Intervention group=301 Control group=658 |
|
Surgical stabilisation of flail chest in thoracic trauma patients has beneficial effects with respect to reduced ventilatory support, shorter intensive care and hospital stay, reduced incidence of pneumonia and septicaemia, decreased risk of chest deformity and an overall reduced mortality when compared with patients who received non-operative management. |
ICU, intensive care unit; IMV, invasive mechanical ventilation; LOS, length of stay; NICE, National Institute for Health and Care Excellence; RCT, randomised controlled trial.
Table 6.
Results of individual reviews that report a narrative synthesis for multiple rib fractures
| Study details | Included studies | Outcomes assessed | Narrative synthesis |
|
Author
de Jong et al 23 Year 2014 Country The Netherlands |
RCT=0 Non-randomised=1 Nirula (60) Case series=2 Campbell (32) Mayberry (46, 15 non-flail) Total number of patients=138 Intervention group=108 Control group=30 |
|
Only Nirula et al 33 concluded that rib fracture fixation showed a trend toward fewer total ventilator days. Mayberry et al 41 investigated the quality of life after rib fixation, and they concluded that there was low long-term morbidity and pain. Campbell et al 40 demonstrated low levels of pain and satisfactory rehabilitation. |
|
Author
Girsowicz et al 14 Year 2012 Country France |
Non-systematic review=1 Nirula and Mayberry Case Comparator=1 Nirula (30,30) Case Series=4 Mayberry (46) Richardson (7) Barajas (22) Campbell (32) Case report=3 Gasparri (1) Cacchione (1) Kerr-Valentic (1) Total number of patients=169 Intervention group=139 Control group=30 |
|
In general, of the nine studies presented, all indicated that surgical stabilisation in the management of isolated multiple non-flail and painful rib fractures improved outcomes. Indeed, the interest and benefit was shown not only in terms of pain and respiratory function but also in improved quality of life and reduced socio-professional disability. Hence, the current evidence shows surgical stabilisation to be safe and effective in alleviating post-operative pain and improving patient recovery, thus enhancing the outcome of the procedure. However, retrieved studies provided a low level of evidence (small studies with few numbers of patients and short-term follow-up or case reports). Large prospective controlled trials are thus necessary to confirm these encouraging results. |
IMV, invasive mechanical ventilation; LOS, length of stay; RCT, randomised controlled trial.
Primary outcome: length of mechanical ventilation (days)
Flail chest
Ten systematic reviews reported length of mechanical ventilation; six undertook a meta-analysis17–22 four17–20 of which included the same three RCTs.25–27
There was substantial variation across the reviews in the pooled estimates for this outcome, related to pooling different sets of studies. The largest reduction in duration of mechanical ventilation when surgery is compared with no surgery was reported by Slobogean et al 21 pooling two RCTs25 26 and six non-randomised studies28–33 (mean difference [MD] −7.5 days, 95% CI −9.9 to –5.5) (table 4). The MD was 3 days greater than the pooled estimates from Leinicke et al 22 (–4.52 days, 95% CI −5.54 to −3.50) and Swart et al 17 (–4.57 days, SD 0.59).
There were differences in the data reported across the four meta-analyses17–20 that included the same three RCTs. Schuurmans et al 18 extracted median duration from the Marasco et al RCT,27 producing an estimate MD −6.53 days, 95% CI −11.88 to –1.18. In contrast, Coughlin et al,19 Cataneo et al 20 and Swart et al 17 report the total mean time on mechanical ventilation which they state was obtained directly from the authors producing an estimate MD −6.30 days, 95% CI −12.16 to –0.43.
Variations also arose in relation to the extraction of data from the RCT by Granetzny et al 26 who did not report SDs for mechanical ventilation. Slightly different SD values are found in all six meta-analyses17–22 which may have arisen from different methods of imputation and all give slightly different estimates.
Substantial heterogeneity was seen in all meta-analyses reporting this outcome18 19 21 22 (I2=48% to 95%). Only one study20 did not pool due to heterogeneity.
Narrative synthesis from two reviews concluded that surgery reduces the length of mechanical ventilation compared with no surgery15 24 (table 5).
Multiple rib fractures
Two reviews14 23 included one primary study33 that had matched non-operative controls33 (non-operative treatment not described) and reported a statistically significant reduction in postoperative ventilator days (p=0.02) in favour of the fixation group (table 6) but no statistically significant difference in total ventilator days (p=0.12).
Mortality
Flail chest
Seven reviews reported mortality; six undertook a meta-analysis.15 17–22 Three reviews18–20 which pooled the same three RCTs25–27 showed a non-statistically significant reduction in mortality with surgery compared with no surgery (risk ratio [RR] 0.56, 95% CI [0.13 to 2.42]18 20 and RR 0.57, 95% CI [0.13 to 2.52]19 [table 4]).
Three reviews pooled randomised and non-randomised studies.17 21 22 Estimates were RR 0.19, 95% CI 0.13 to 0.2621; (RR 0.43, 95% CI 0.28 to 0.6922 and RR 0.44, SD 0.09.17 Overall, statistical heterogeneity was low (I2=0%) for this outcome in all studies that presented this data.17–22
Multiple rib fractures
Mortality was not assessed by de Jong et al 23 or Girsowicz et al.14
Length of intensive care unit stay (days)
Flail chest
Eight reviews12 15 17–22 assessed length of intensive care unit (ICU) stay; six undertook a meta-analysis.17–22 Pooled estimates ranged from −3.25 days (SD 1.29)17 to −6.46 days, 95% CI −9.73 to –3.1919 and were all in favour of surgical fixation compared with a variety of comparators (table 4). The range in pooled estimates may be partly explained by the pooling of different sets of studies. However, differences occurred as some pooled median length of ICU stay and others pooled the mean. Furthermore, some used postoperative time spent in ICU and others the total time spent in ICU.17–19
Variation also arose across reviews in the data extracted from a trial that did not report SDs in the primary publication.26 Values were imputed or the raw data obtained from the authors resulting in SD values ranging from 0.7 to 4.4 and 2.2 to 7.3 in the operative and non-operative groups respectively. There was also a substantial difference in the effect estimate for this trial.26 In one review,22 the effect estimate of −10 days, 95% CI −15.41 to –4.59, was 5 days greater than the estimate used from the same trial in other reviews. It is the same as the as length of mechanical ventilation effect estimate reported in the same study26 so is possibly a transcription error.
Statistical heterogeneity ranged from substantial to none34 (I2=74.9%,22 40%,18 35%19 and 0.1%.21 The narrative syntheses concluded that in patients with flail chest undergoing surgical fixation length of ICU stay was reduced compared with non-operative management.15 24
Multiple rib fractures
A single review14 included one non-randomised study reporting no statistically significant difference in ICU days (p=0.51), the MD and 95% CI was not reported.33
Length of hospital stay (days)
Flail chest
Nine reviews12 15 17–22 24 reported length of hospital stay, six undertook a meta-analysis.17–22 Two reviews17 20 pooled the same two trials25 26 and found a significantly shorter hospital length of stay in favour of surgery compared with non-operative management (MD −11.39 days 95% CI −12.39 to –10.38). When non-randomised studies were included in the meta-analysis the pooled effects were smaller −3.83 days, 95% CI −7.12 to –0.5422; –4 days, 95% CI −7.4 to –0.721 and −4.48 days, SD 1.917 in favour of fixation (table 4).
Heterogeneity ranged from low (I2=0,18 19 meta-analyses of RCTs only) to moderate or substantial (I2=89%,17 I2=68.9%22 and I2=33%).21
Multiple rib fractures
Two systematic reviews14 23 (table 6) included a single non-randomised study33 reporting no statistically significant difference in hospital stay with surgery (mean 18.8 days [SD 1.8]) compared with the non-operative management (21.1 days [SD 3.9]), p=0.59).
Pneumonia
Flail chest
Ten reviews,12 15 17–22 35 reported the risk of developing pneumonia, six undertook a meta-analysis.13 17–22 24 Three RCTs25–27 were pooled in two of the reviews15 17 and they found a RR of 0.36, 95% CI 0.15 to 0.85, in favour of fixation compared with non-operative management. When non-randomised studies were combined the RR ranged from 0.31, 95% CI 0.21 to 0.4121 to 0.45, 95% CI 0.29 to 0.7036 in favour of fixation (table 4). Substantial heterogeneity was seen in meta-analyses for this outcome18–20 that included the three RCTs25–27 (I2=66% to 74%). In the reviews that pooled the RCTs alongside the non-randomised studies21 22 there were lower levels of heterogeneity (I2=4% and I2=31%, respectively).
Two narrative syntheses report that among patients with flail chest, risk of pneumonia was reduced in the surgery group compared with the no surgery group (table 5).15 24
Tracheostomy
Flail chest
Five reviews reported a meta-analysis for tracheostomy.17 18 20–22 Pooled RRs ranged from 0.25, 95% CI 0.13 to 0.47 to 0.40, 95% CI 0.2 to 0.7 (table 4). Moderate and substantial heterogeneity was seen in two reviews (I2=42%,17 I2=64%),20 low in two reviews21 22 (I2=0%) and one did not report heterogeneity.18
Sepsis
Flail chest
One review,21 pooling four non-randomised studies28 30 37 38 estimated a RR of 0.14, 95% CI 0.56 to 0.23 with I2=0% in favour of fixation compared with non-operative management for sepsis. The estimate RR reported is not possible given the CI does not include the estimated value, 0.14. The lower interval of 0.56 could possibly be −0.56 creating a wider CI and would suggest that the author’s conclusion was correct and there was a statistically significant difference in favour of fixation.
Spirometry
Flail chest
One review19 reported a meta-analysis of spirometry data which included two RCTs26 27 with spirometry measured at two different time points (three and 2 months respectively). No statistically significant differences in any spirometry data were seen between surgery and no surgery (table 4).
Chest deformity
Flail chest
Two reviews reported a meta-analysis of chest deformity,20 21 both reported a statistically significant difference in favour of surgery compared with no surgery (RR 0.30, 95% CI 0.00 to 0.60, I2=2.1% and RR 0.13, 95% CI 0.03 to 0.67, I2=0%).
Dyspnoea
Flail chest
One review21 pooled an RCT25 and two non-randomised studies.37 39 for dyspnoea (RR 0.15, 95% CI 0.09 to 0.39 in favour of fixation). Duration of follow-up was 1 year for two of the primary studies25 39 and unclear in the third.37 It was unclear how dyspnoea was measured or defined in the three primary studies.
Chest pain
Flail chest
Chest pain was reported in one review21 which pooled one RCT25 and one non-randomised study39 suggesting a benefit in favour of fixation (RR 0.18, CI 95% -0.46 to 0.83).
Other reported outcomes
Several other outcomes were reported within the systematic reviews however no others have been pooled in a meta-analysis. A narrative synthesis was not completed on the outcomes: wound infection, pain-requiring removal of metalwork, return to work, socio-professional disability cost, pulmonary embolism, pneumothorax and haemothorax. In the reviews, data on these additional outcomes was minimal and presented as a narrative synthesis without presenting numerical data (tables 5 and 6).
Discussion
Twelve systematic reviews on the effectiveness of surgery for flail chest and multiple rib fractures published between 2010 and 2016. This is the first systematic review of reviews and highlighted that there are a large number of reviews with same aims and including the same primary studies.
Flail chest
Six17–22 of the 12 systematic reviews presented meta-analyses for flail chest based on overlapping primary studies. They reported reductions in length of mechanical ventilation, length of stay, pneumonia and tracheostomy rates with surgery compared with non-surgical management and inconsistent results for mortality. Across many of the meta-analyses there was moderate to high levels of heterogeneity and variation in the effect estimates.
A single systematic review found reductions in sepsis, dyspnoea, chest deformity and chest pain with surgery compared with no surgery management. Nevertheless, as the outcome measures were not defined it is difficult to know whether the reductions are clinically significant. Reporting of adverse outcomes was infrequent across the reviews, which could reflect lack of measurement and/or reporting of adverse events in the primary studies or the systematic reviews. Therefore, the benefits of surgery could be overestimated in light of the potential risks not being considered. Synthesising multiple meta-analyses data that include overlapping primary studies has the potential to overestimate the strength of the findings therefore it is important to be mindful of the limited evidence on which our conclusions are based. In addition, significant heterogeneity for several of the outcomes that were pooled makes drawing firm conclusions difficult.
Multiple rib fractures
Evidence in support of multiple rib fracture fixation in the absence of flail chest is limited. Two systematic reviews14 23 reported on one non-randomised study33 that recruited between 1996 and 2000, four case series40–43 and two case reports.44 45 Hence, due to limited evidence no conclusive statements on effectiveness can be drawn.
Review quality
A significant amount of effort and time is required to conduct a high quality systematic review and should only be undertaken when there is sufficient cause46 47 (eg, to incorporate the findings of a new RCT or to address an evidence gap). Eight of the systematic reviews were published within 18 months although none were registered on PROSPERO48 so it is possible the authors were unaware of each other’s research. Registering reviews allows transparency of methods and also reduces research waste.49 As similar search strategies and search dates were used in each systematic review, inevitably many of the included studies were the same across reviews.
Only two of the 12 systematic reviews formally appraised the quality of the included studies, therefore 10 of the reviews were not in a position to fully consider the impact of risk of bias on their conclusions. High or unclear risk of bias within reviews have affected the conclusions drawn from this evidence synthesis. In a systematic review of 106 emergency surgery systematic reviews, a low risk of bias was found in 53.8%, identifying a common problem of poor quality reviews conducted in emergency surgery.50
Heterogeneity and meta-analysis errors
The I2 value describes the percentage of total variation across studies that is due to heterogeneity rather than chance.51 Examining the meta-analyses including RCTs highlights moderate to high levels of statistical heterogeneity.
There was also clinical variation in the primary studies in terms of indications and timing of surgery and it is possible that these between study differences could be a source of the substantial heterogeneity. For example, in one RCT25 patients were randomised after 5 days of invasive ventilation, whereas another RCT26 randomised and fixed within 24 to 72 hours regardless of initial intubation state. Also, many reviews define the comparator as usual care or non-operative care but do not elaborate on what encompasses this care. Differences in how outcomes were measured may also have contributed to between study heterogeneity. It was unknown due to lack of reporting whether the outcomes were equivalent in the pooled primary studies or overall between systematic reviews.
In all systematic reviews with meta-analyses, they reported that two reviewers were involved in the data extraction to minimise errors.17 19–22 Despite attempts to minimise errors and therefore an apparent low risk of bias, some errors (up to an MD of 10 days in the measurement of length of intensive care stay) were identified across reviews. It is worth noting that there were no significant changes in the conclusions drawn from these analyses. Although there was substantial statistical and clinical heterogeneity and lack of consideration of risk of bias in many of the reviews, conclusions tended to be similar and in the direction of benefit with fixation suggesting that further high quality RCTs investigating the effectiveness (including adverse effects) of internal surgical fixation over non-operative management are warranted.
Strengths
Multiple databases were searched for studies and study selection was undertaken by two researchers, reducing the risk of error and bias. Although only English language studies were included, some sources of unpublished studies were searched. A mapping of the studies included in the reviews was undertaken to take into account individual studies being included in multiple reviews and hence double counting studies.
Limitations
All systematic reviews were included irrespective of their risk of bias scoring. It could be argued that several reviews were stretching the traditional definition of a systematic review however they did hold to the protocol definition with an electronic database search strategy and included primary evidence. Due to best evidence topics and rapid evidence synthesis being included it was then difficult to apply the ROBIS tool consistently. The ROBIS tool is not designed for rapid evidence synthesis and therefore this type of review showed high risk of bias as they were being assessed against a tool designed for full systematic reviews. Rapid evidence syntheses, by their nature address a trade-off between time and methodological rigour and comprehensiveness.52
Conclusion
The considerable duplication of work across reviews could be mitigated through protocol registration and greater attention to establishing whether a review is necessary by scoping the literature before commencing a new review. Despite this review identifying 12 systematic reviews they only included 37 unique primary studies, only three of which were RCTs. Synthesis of the reviews has shown some potential improvement in patient outcomes with flail chest after surgical intervention. However, there were differences in indications and timing of interventions in the primary studies and moderate to high levels of heterogeneity across reviews. For future review updates, meta-analysis for effectiveness may need to take into account indications and timing of surgery as a subgroup analysis to address clinical heterogeneity between primary studies. Further robust evidence is required before conclusions can be drawn of the effectiveness of surgical fixation for flail chest and in particular, multiple rib fractures.
Supplementary Material
Footnotes
Contributors: HMAI contributed to conceptualisation, methodology, investigation, formal analysis, original draft preparation. EC contributed to investigation, validation, review and editing. WE contributed to conceptualisation, review and editing. AR contributed to funding acquisition, conceptualisation, review and editing. CH contributed to methodology, supervision, conceptualisation, review and editing. CM contributed to methodology, investigation, validation, conceptualisation, supervision, review and editing. All authors approve the final version of the manuscript and are accountable for all aspects of the work.
Funding: This review was completed as part of an MD project which was funded by an educational grant from Orthopaedic Research UK. The research was undertaken at the BOA Orthopaedic Surgery Research Centre (BOSRC) at York Trials Unit.
Competing interests: AR declares receiving research grants from NIHR; research and educational grants from DePuy Ltd outside the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data used for the preparation of this review are reported within the manuscript or its supplementary files.
Patient consent for publication: Not required.
References
- 1. Veysi VT, Nikolaou VS, Paliobeis C, et al. Prevalence of chest trauma, associated injuries and mortality: a level I trauma centre experience. Int Orthop 2009;33:1425–33. 10.1007/s00264-009-0746-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American College of Surgeons. In: Chang MC, ed NTDB ANNUAL REPORT 2016, 2016. [Google Scholar]
- 3. Brasel KJ, Moore EE, Albrecht RA, et al. Western Trauma Association Critical Decisions in Trauma: Management of rib fractures. J Trauma Acute Care Surg 2017;82:200–3. 10.1097/TA.0000000000001301 [DOI] [PubMed] [Google Scholar]
- 4. Vyhnánek F, Jirava D, Očadlík M, et al. [Surgical Stabilisation of Flail Chest Injury: Indications, Technique and Results]. Acta Chir Orthop Traumatol Cech 2015;82:303–7. [PubMed] [Google Scholar]
- 5. de Moya M, Bramos T, Agarwal S, et al. Pain as an indication for rib fixation: a bi-institutional pilot study. J Trauma 2011;71:1750–4. 10.1097/TA.0b013e31823c85e9 [DOI] [PubMed] [Google Scholar]
- 6. Velasquez M, Ordoñez CA, Parra MW, et al. Operative versus Nonoperative Management of Multiple Rib Fractures. Am Surg 2016;82:E103–5. [PubMed] [Google Scholar]
- 7. Bhatnagar A, Mayberry J, Nirula R. Rib fracture fixation for flail chest: what is the benefit? J Am Coll Surg 2012;215:201–5. 10.1016/j.jamcollsurg.2012.02.023 [DOI] [PubMed] [Google Scholar]
- 8. Centre for Reviews and Dissemination. Systematic Reviews - CRD’s guidance for undertaking reviews in health care: York Publishing Services, 2009. [Google Scholar]
- 9. Whiting P, Savović J, Higgins JP, et al. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol 2016;69:225–34. 10.1016/j.jclinepi.2015.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Page MJ, McKenzie JE, Kirkham J, et al. Bias due to selective inclusion and reporting of outcomes and analyses in systematic reviews of randomised trials of healthcare interventions. Cochrane Database Syst Rev 2014;10:MR000035 10.1002/14651858.MR000035.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 12. NICE. Insertion of metal rib reinforcements to stabilise a flail chest wall. Interventional procedures guidance [IPG361]. 2010.
- 13. Schulte K, Whitaker D, Attia R. In patients with acute flail chest does surgical rib fixation improve outcomes in terms of morbidity and mortality? Interact Cardiovasc Thorac Surg 2016;23:314–9. 10.1093/icvts/ivw092 [DOI] [PubMed] [Google Scholar]
- 14. Girsowicz E, Falcoz PE, Santelmo N, et al. Does surgical stabilization improve outcomes in patients with isolated multiple distracted and painful non-flail rib fractures? Interact Cardiovasc Thorac Surg 2012;14:312–5. 10.1093/icvts/ivr028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. de Lesquen H, Avaro JP, Gust L, et al. Surgical management for the first 48 h following blunt chest trauma: state of the art (excluding vascular injuries). Interact Cardiovasc Thorac Surg 2015;20:399–408. 10.1093/icvts/ivu397 [DOI] [PubMed] [Google Scholar]
- 16. Khan OA, Dunning J, Parvaiz AC, et al. Towards evidence-based medicine in surgical practice: best BETs. Int J Surg 2011;9:585–8. 10.1016/j.ijsu.2011.08.001 [DOI] [PubMed] [Google Scholar]
- 17. Swart E, Laratta J, Slobogean G, et al. Operative treatment of rib fractures in flail chest injuries: a meta-analysis and cost-effectiveness analysis. J Orthop Trauma 2017;31:64–70. 10.1097/BOT.0000000000000750 [DOI] [PubMed] [Google Scholar]
- 18. Schuurmans J, Goslings JC, Schepers T. Operative management versus non-operative management of rib fractures in flail chest injuries: a systematic review. Eur J Trauma Emerg Surg 2017;43:1 10.1007/s00068-016-0721-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Coughlin TA, Jwg N, Rollins KE, et al. Management of rib fractures in traumatic flail chest A meta-analysis of randomised control trials. Bone & Joint Journal 2016;98B:1119–25. [DOI] [PubMed] [Google Scholar]
- 20. Cataneo AJ, Cataneo DC, de Oliveira FH, et al. Surgical versus nonsurgical interventions for flail chest. Cochrane Database Syst Rev 2015;7:CD009919 10.1002/14651858.CD009919.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Slobogean GP, MacPherson CA, Sun T, et al. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg 2013;216:302–11. 10.1016/j.jamcollsurg.2012.10.010 [DOI] [PubMed] [Google Scholar]
- 22. Leinicke JA, Elmore L, Freeman BD, et al. Operative management of Rib fractures in the setting of flail chest: A systematic review and meta-analysis. Annals of Surgery 2013;258:914–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. de Jong MB, Kokke MC, Hietbrink F, et al. Surgical Management of Rib Fractures: Strategies and Literature Review. Scand J Surg 2014;103:120–5. 10.1177/1457496914531928 [DOI] [PubMed] [Google Scholar]
- 24. Unsworth A, Curtis K, Asha SE. Treatments for blunt chest trauma and their impact on patient outcomes and health service delivery. Scand J Trauma Resusc Emerg Med 2015;23:17 10.1186/s13049-015-0091-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002;52:727–32. 10.1097/00005373-200204000-00020 [DOI] [PubMed] [Google Scholar]
- 26. Granetzny A, Abd El-Aal M, Emam E, et al. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg 2005;4:583–7. 10.1510/icvts.2005.111807 [DOI] [PubMed] [Google Scholar]
- 27. Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg 2013;216:924–32. 10.1016/j.jamcollsurg.2012.12.024 [DOI] [PubMed] [Google Scholar]
- 28. Kim M, Brutus P, Christides C, et al. [Compared results of flail chests treatments: standard internal pneumatic stabilization, new technics of assisted ventilation, osteosynthesis (author’s transl)]. J Chir 1981;118(8-9):499–503. [PubMed] [Google Scholar]
- 29. Karev DV. Operative management of the flail chest. Wiad Lek 1997;50:205–8. [PubMed] [Google Scholar]
- 30. Voggenreiter G, Neudeck F, Aufmkolk M, et al. Operative chest wall stabilization in flail chest–outcomes of patients with or without pulmonary contusion. J Am Coll Surg 1998;187:130–8. 10.1016/S1072-7515(98)00142-2 [DOI] [PubMed] [Google Scholar]
- 31. Balci AE, Eren S, Cakir O, et al. Open fixation in flail chest: review of 64 patients. Asian Cardiovasc Thorac Ann 2004;12:11–15. 10.1177/021849230401200104 [DOI] [PubMed] [Google Scholar]
- 32. Teng J-P, Cheng Y-G, Da NI, et al. Outcomes of traumatic flail chest treated by operative fixation versus conservative approach. J Shanghai Jiaotong Univ 2009;29:1495. [Google Scholar]
- 33. Nirula R, Allen B, Layman R, et al. Rib fracture stabilization in patients sustaining blunt chest injury. Am Surg 2006;72:307–9. [DOI] [PubMed] [Google Scholar]
- 34. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. 2011. [Google Scholar]
- 35. Nickerson TP, Kim BD, Zielinski MD, et al. Use of a 90° drill and screwdriver for rib fracture stabilization. World J Surg 2015;39:789–93. 10.1007/s00268-014-2862-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Leinicke JA, Elmore L, Freeman BD, et al. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg 2013;258:914–21. 10.1097/SLA.0b013e3182895bb0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. J Thorac Cardiovasc Surg 1995;110:1676–80. 10.1016/S0022-5223(95)70030-7 [DOI] [PubMed] [Google Scholar]
- 38. Borrelly J, Aazami MH. New insights into the pathophysiology of flail segment: the implications of anterior serratus muscle in parietal failure. Eur J Cardiothorac Surg 2005;28:742–9. 10.1016/j.ejcts.2005.08.017 [DOI] [PubMed] [Google Scholar]
- 39. Ohresser P, Amoros JF, Leonardelli M, et al. [The functional sequelae of closed thoracic injuries (apropos of 92 cases)]. Poumon Coeur 1972;28:145–50. [PubMed] [Google Scholar]
- 40. Campbell N, Conaglen P, Martin K, et al. Surgical stabilization of rib fractures using Inion OTPS wraps–techniques and quality of life follow-up. J Trauma 2009;67:596–601. 10.1097/TA.0b013e3181ad8cb7 [DOI] [PubMed] [Google Scholar]
- 41. Mayberry JC, Kroeker AD, Ham LB, et al. Long-term morbidity, pain, and disability after repair of severe chest wall injuries. Am Surg 2009;75:389–94. [PubMed] [Google Scholar]
- 42. Richardson JD, Franklin GA, Heffley S, et al. Operative fixation of chest wall fractures: an underused procedure? Am Surg 2007;73:591–6. [PubMed] [Google Scholar]
- 43. Moreno De La Santa Barajas P, Polo Otero MD, Delgado Sánchez-Gracián C, et al. [Surgical fixation of rib fractures with clips and titanium bars (STRATOS System). Preliminary experience]. Cir Esp 2010;88:180–6. 10.1016/j.ciresp.2010.06.004 [DOI] [PubMed] [Google Scholar]
- 44. Cacchione RN, Richardson JD, Seligson D. Painful nonunion of multiple rib fractures managed by operative stabilization. J Trauma 2000;48:319–21. 10.1097/00005373-200002000-00023 [DOI] [PubMed] [Google Scholar]
- 45. Gasparri MG, Almassi GH, Haasler GB. Surgical management of multiple rib fractures. Chest 2003;124:295S–6. 10.1378/chest.124.4_MeetingAbstracts.295S-a [DOI] [Google Scholar]
- 46. Garner P, Hopewell S, Chandler J, et al. When and how to update systematic reviews: consensus and checklist. BMJ 2016;354:i3507 10.1136/bmj.i3507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lund H, Juhl C, Christensen R. Systematic reviews and research waste. Lancet 2016;387:123–4. 10.1016/S0140-6736(15)01354-9 [DOI] [PubMed] [Google Scholar]
- 48. Booth A, Clarke M, Dooley G, et al. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev 2012;1:2 10.1186/2046-4053-1-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Moher D, Booth A, Stewart L. How to reduce unnecessary duplication: use PROSPERO. BJOG-Int J Obstet Gy 2014;121:784–6. 10.1111/1471-0528.12657 [DOI] [PubMed] [Google Scholar]
- 50. EMSurg Collaborators. Methodological overview of systematic reviews to establish the evidence base for emergency general surgery. Br J Surg 2017;104:513–24. 10.1002/bjs.10476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Featherstone RM, Dryden DM, Foisy M, et al. Advancing knowledge of rapid reviews: an analysis of results, conclusions and recommendations from published review articles examining rapid reviews. Syst Rev 2015;4:50 10.1186/s13643-015-0040-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Paris F, Tarazona V, Blasco E, et al. Surgical stabilization of traumatic flail chest. Thorax 1975;30:521–7. 10.1136/thx.30.5.521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Althausen PL, Shannon S, Watts C, et al. Early surgical stabilization of flail chest with locked plate fixation. J Orthop Trauma 2011;25:641–7. 10.1097/BOT.0b013e318234d479 [DOI] [PubMed] [Google Scholar]
- 55. Granhed HP, Pazooki D. A feasibility study of 60 consecutive patients operated for unstable thoracic cage. J Trauma Manag Outcomes 2014;8:20 10.1186/s13032-014-0020-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Doben AR, Eriksson EA, Denlinger CE, et al. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care 2014;29:139–43. 10.1016/j.jcrc.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 57. Jayle CP, Allain G, Ingrand P, et al. Flail chest in polytraumatized patients: surgical fixation using Stracos reduces ventilator time and hospital stay. Biomed Res Int 2015;2015:1–6. 10.1155/2015/624723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg 2016;80:187–94. 10.1097/TA.0000000000000925 [DOI] [PubMed] [Google Scholar]
- 59. Zhang Y, Tang X, Xie H, et al. Comparison of surgical fixation and nonsurgical management of flail chest and pulmonary contusion. Am J Emerg Med 2015;33:937–40. 10.1016/j.ajem.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 60. Wada T, Yasunaga H, Inokuchi R, et al. Effectiveness of surgical rib fixation on prolonged mechanical ventilation in patients with traumatic rib fractures: A propensity score-matched analysis. J Crit Care 2015;30:1227–31. 10.1016/j.jcrc.2015.07.027 [DOI] [PubMed] [Google Scholar]
- 61. Xu JQ, Qiu PL, Yu RG, et al. Better short-term efficacy of treating severe flail chest with internal fixation surgery compared with conservative treatments. Eur J Med Res 2015;20:55 10.1186/s40001-015-0146-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Majercik S, Vijayakumar S, Olsen G, et al. Surgical stabilization of severe rib fractures decreases incidence of retained hemothorax and empyema. Am J Surg 2015;210:1112–7. 10.1016/j.amjsurg.2015.08.008 [DOI] [PubMed] [Google Scholar]
- 63. DeFreest L, Tafen M, Bhakta A, et al. Open reduction and internal fixation of rib fractures in polytrauma patients with flail chest. Am J Surg 2016;211:761–7. 10.1016/j.amjsurg.2015.11.014 [DOI] [PubMed] [Google Scholar]
- 64. Hellberg K, de Vivie ER, Fuchs K, et al. Stabilization of flail chest by compression osteosynthesis–experimental and clinical results. Thorac Cardiovasc Surg 1981;29:275–81. 10.1055/s-2007-1023495 [DOI] [PubMed] [Google Scholar]
- 65. Menard A, Testart J, Philippe JM, et al. Treatment of flail chest with Judet’s struts. J Thorac Cardiovasc Surg 1983;86:300–5. [PubMed] [Google Scholar]
- 66. Mouton W, Lardinois D, Furrer M, et al. Long-term follow-up of patients with operative stabilisation of a flail chest. Thorac Cardiovasc Surg 1997;45:242–4. 10.1055/s-2007-1013735 [DOI] [PubMed] [Google Scholar]
- 67. Lardinois D, Krueger T, Dusmet M, et al. Pulmonary function testing after operative stabilisation of the chest wall for flail chest. Eur J Cardiothorac Surg 2001;20:496–501. 10.1016/S1010-7940(01)00818-1 [DOI] [PubMed] [Google Scholar]
- 68. Kerr-Valentic MA, Arthur M, Mullins RJ, et al. Rib fracture pain and disability: can we do better? J Trauma 2003;54:1058–63. 10.1097/01.TA.0000060262.76267.EF [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-023444supp001.pdf (34.9KB, pdf)
bmjopen-2018-023444supp002.pdf (475KB, pdf)