Abstract
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), which can be considered a late-onset allergic reaction, can cause serious long-term sequelae. SJS/TEN are considered a spectrum of life-threatening adverse drug reactions. They have the same clinical manifestations and the only difference is in the extent of epidermal detachment. These conditions are associated with high mortality, although incidence of SJS/TEN is rare in children. SJS/TEN is an adverse drug reaction influenced by genes that involve pharmacokinetics, pharmacodynamics and immune response. Infective agents are additional influencing factors. Anticonvulsants and antibiotics, and especially sulphonamides and non-steroidal anti-inflammatory drugs, are among the drugs that were predominantly suspected of triggering SJS/TEN. No evidence-based standardized treatment guidelines for SJS or TEN are currently available. The usual treatment is mainly founded on the withdrawal of the suspected causative agent and supportive therapy. In pediatric patients, the specific therapeutic strategies are controversial and comprise systemic corticosteroids and the use of intravenous immunoglobulin (IVIG). More recently, new therapeutic approaches have been used, such as immunosuppressive therapies, including cyclosporine and TNF-α inhibitors. (www.actabiomedica.it)
Keywords: drug adverse reaction, Stevens-Johnson Syndrome, toxic epidermal necrolysis, hypersensitivity reactions, children, skin test, specific IgE, basophil activation test, drug provocation test
Introduction
Stevens-Johnson Syndrome (SJS) and toxic epidermal necrolysis (TEN) are severe cutaneous adverse reactions (SCAR) that belong to type IV hypersensitivity, mediated by immunological effect (1). SJS and TEN, which were reported for the first time in 1922, are part of the same spectrum of disease and have similar aetiology. There are differences in the extent of detached or detachable skin. SJS affects <10% of the body surface area with, SJS/TEN overlap 10%-30% of the body surface and TEN >30% (2, 3). SJS/TEN is a severe disease, which is often life-threatening and usually drug-induced. Because of its rarity, there is a lack of epidemiologic and prospective studies. The reported incidences of SJS and TEN in adults are 3.96 to 5.3/1,000,000 for SJS and 0.4 to 1.45/1,000,000 for TEN (4, 5). Pediatric data only refer to small case series and retrospective studies (6, 7). Nevertheless, a higher incidence in pediatric age has been recently reported by a US study. The incidence was 6.3/100,000 for SJS, 0.7/100,000 for SJS/TEN overlap syndrome, and 0.5/100,000 for TEN. Children aged 11-15 years recorded the highest incidence (p<0.001). The highest mortality was seen in children aged 0-5 years and in children with TEN (8). The reported mortality rates at 6 weeks are comprised between 7.5% and 23% (7, 9). The increasing incidence of SJS/TEN with age is likely a result of more frequent drug prescriptions and comorbidities that modify the drug effects.
TEN and SJS/TEN overlap syndrome is associated with longer hospitalization, greater mortality, and higher hospital charges compared to SJS. The mortality associated with SJS and TEN in adults is higher than in pediatric populations (5), which are affected by long-term complications in more than half of the cases. Children show a high recurrence rate of SJS, 1 in 5 in the study by Finkelstein et al. (6), suggesting vulnerability and potential genetic predisposition.
How to recognize SJS/TEN
In several studies, prodromal non-specific symptoms lasting 1 to 7 days precede the onset of the SJS/TEN disease. They include discomfort, dysphagia and ocular pruritus, followed by high fever, respiratory symptoms and rashes with blisters or lesions causing mucosal inflammations. Skin lesions are usually preceded by a few days by inflammation and dryness of the mouth and genitalia. The oral, ocular and genital mucous membranes are gradually affected by erythema, erosion, and pseudomembranes. Patients are severely ill and bullous lesions develop fast both on skin and mucous membranes (10), often within 12 hours.
Skin lesions have variable severity and change into vesicles, bullae and extended detachable skin necrosis. When erythema is the main cutaneous finding, the diagnosis may be guided by the Nikolsky sign, in spite of not being exclusive of SJS/TEN. The Nikolsky sign (11) is defined as an epidermal detachment caused by the application of a tangential pressure on erythematous, non-blistering skin. Despite the highest involvement of the skin, multiple organ systems, such as cardiovascular, pulmonary, gastrointestinal, and urinary systems can also be affected. Several different complications are reported in SJS and TEN patients, the most common being secondary skin infection. Bacterial infection is inevitable because of epidermal detachment. Severely ill patients show various complications, such as pneumonia, hepatitis, and septicemia, and they determine the major cause of morbidities and mortalities.
Mucocutaneous complications occur in about 90% of cases and the ocular surface is one of the most frequently affected mucosal surfaces in TEN (50-67%) (12). Patients surviving from the often fatal acute stage of the disease are usually affected by major ocular sequelae, which include bilateral blinding caused by corneal scarring, and vascularization in severe cases. The complications are more severe in TEN than in SJS, except for ocular complications, such as corneal ulcerations, that were equally distributed between SJS and TEN. Furthermore, there is no correlation between the severity of skin detachment and the severity of ocular findings. In view of the persistent ocular complications, prompt eyes examination with appropriate treatment is recommended in all SJS and TEN patients (13, 14).
SJS/TEN is a very severe form of drug-induced reaction. Its differential diagnosis includes various diseases, such as drug induced linear IgA and DRESS. A drug-induced maculo papular exanthema should also be excluded, being the most common cutaneous adverse drug reaction. The Staphylococcal scalded skin syndrome (SSSS) and the erythema multiforme must be also taken into consideration.
Triggers for SJS/TEN
SJS/TEN is induced by drugs in about 60%-90% of children (6, 15, 16). A limited number of drugs are responsible for the majority of cases, especially in children, even if more than 100 drugs have been associated with this disease (6, 7). Anticonvulsants, antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) are the more common triggers. In order to consider SJS/TEN as drug related, the affected patients must be exposed to the suspected drug within 8 weeks prior to the occurrence of the rash. The largest pediatric cohort, which was reported by Levi et al., included 80 patients and 216 matched controls below the age of 15 years. The study shows that the most frequent causative drugs were sulphonamides and anticonvulsants (phenobarbital, lamotrigine, and carbamazepine) (7). In this study, the exposure to the offending agent was reduced to 7 days before the onset of the cutaneous lesions. Because of its longer half-life, this window was extended to 3 weeks for phenobarbital. Techasatian et al. (13) have showed that antiepileptics were the most common cause (60%), followed by antibiotics (26.6%) and other drugs, such as NSAIDs and chemotherapy drugs. The most common drug in the antiepileptic drug group was carbamazepine (26.6%) followed by phenytoin, phenobarbital and levetiracetam. The antibiotic drug group included erythromycin, cefotaxime, trimethoprim-sulfamethoxasone, cloxacillin, and amoxycillin. According to the authors, the latent period from drug exposure to diagnosis was comprised between 1 and 31 days, with a mean of 10.7 days. The longest latent period was recorded for anticonvulsivants in comparison to antibiotics or other drugs (13). In a retrospective study, Egunsola et al. found that valproic acid (VPA) increases the risk of SJS/TEN in pediatric patients receiving lamotrigine (LTG). VPA inhibits hepatic glucuronidation that results in a reduced LTG metabolism and plasma levels (17). Children with SJS/TEN due to azithromicyn (18) and vancomycin (19) have been reported. In children, various pathogens, especially Mycoplasma pneumoniae and Herpes virus have been found to induce SJS (6, 15, 20) in 5%-31% of cases. Infections caused by virus (influenza, Epstein-Barr, cytomegalovirus, coxsakie, human herpes virus 6 and 7, parvovirus), bacteriae (streptococcus β-haemolyticum, group A), mycobacterium, and rickettsia are also associated with pediatric SYS/TEN (16). Infections can also act as potential cofactors. SYS/TEN has been reported to be idiopathic in 5%-18% of children and in 25-50% of adults (6, 16, 21).
Pathogenic mechanisms and genetic aspects
A full understanding of the pathogenesis is still lacking. Drug-induced SJS/TEN may be caused by dysregulation of cellular immunity. Cytotoxic T lymphocytes (CTLs) and natural killer (NK) cells (22, 23) may recognize unmodified drugs or offending drugs or their metabolites (24) presented by human leukocyte antigen (HLA) class I molecules on keratinocytes (24). When these immune cells are activated, various cytotoxic signals, including Fas/Fas ligand, perforin/granzyme B (25) and granulysin (26) are released to mediate keratinocyte apoptosis and detachment of skin and mucous membranes. T lymphocytes, particularly CD8+ lymphocytes, are present in a large amount in blister fluids and exhibit drug specific cytotoxicity in patients affected by TEN (27). Moreover, skin lesions, blister fluids/cells, peripheral blood mononuclear cells, or plasma of patients with SJS/TEN contained an increased number of cytokines that are responsible for proliferation and activation of T cells (25, 28). They include IFN-g, IL-2, IL-5, IL-6, IL-10, and IL-13. Tumor necrosis factor-alpha (TNF-alpha) is released by keratinocytes and macrophages in plasma and blister fluids and it may induce keratinocyte apoptosis (29, 30).
In the last 15 years, associations between drug-induced SJS/TEN (31) and Class I and II HLA alleles of the major histocompatibility complex (MHC) have been demonstrated by pharmacogenomic studies. In order to explain how drugs are recognized by T cells in an MHC-dependent manner, several models have been suggested, including the hapten concept/prohapten model and the p-i model (pharmacological interaction of drugs with immune receptors) (32). Moreover, a major role in the onset of SJS/TEN is played by genetic susceptibility. Carbamazepine-induced SJS is associated with HLA-B15:02 genotyping in a Han Chinese population (33), whereas an association between HLA-B58:01 and allopurinol-induced SJS/TEN has been found in a Japanese population (34). However, such association was not reported in European population. Therefore, the risk of SJS/TEN is related both to the exposure to high-risk drugs and to a genetic predisposition (27). Moreover, many genetic polymorphisms in detoxifying enzymes have been founded, especially in the CYP450 family, that is deeply involved in drug kinetics and toxicity. Furthermore, a low N-acetylating capacity has been identified in some patients with SJS/TEN, and this aspect exposes them to the risk of SCARs (35).
Diagnostic approach
Although the diagnosis of SJS/TEN is mainly based on clinical signs and symptoms. Skin biopsy showing a typical full epidermal thickness necrosis associated with a scarce dermal inflammatory infiltrate is not always required for diagnosis.
It may be difficult to identify the exact causative agent because there is no definitive laboratory test to confirm the role of triggers. In case of a suspected diagnosis of SJS/TEN, it is necessary to obtain a detailed medical history, with a list of all new medications taken during the 8 weeks prior to the onset of the cutaneous lesions. The ALDEN score can be calculated to identify suspected culprit medications (36). The algorithm considers five items, that is to say index day, half-life, prechallenge/rechallenge, dechallenge, and notoriety.
Moreover, different serological tests and polymerase chain reaction (PCR) for diagnosing infections caused by herpes simplex virus 1 and 2, varicella-zoster virus, Epstein-Barr virus, cytomegalovirus, human herpes virus 6 and 7, parvovirus and M pneumoniae (20) should be carried out.
In spite of being useful for diagnostic purposes, a biopsy can prove to be an invasive and time-consuming procedure. Cytokine determination might be a feasible test for diagnosing SJS before performing a skin biopsy. Cytokines may be potentially important for diagnostic purposes, for prognosis and as a possible therapeutic target. Granulysin expression in CD4+ cells by flow cytometry, granzyme B production by ELISpot assay, and IFN-γ levels in cell supernatant by cytokine bead array have been investigated. Several studies have reported that patients with early-stage SJS have a higher level of serum granulysin than patients with other drug-induced skin reactions (37). The granulysin rapid test by immunochromatographic assay is a non-invasive procedure, with the additional advantage of rapid diagnosis within 15 min (19, 38 ,39). Fujita et al. found that the granulysin rapid test was helpful for an early diagnosis of SJS/TEN (38). Lin et al (39) showed that the granulysin rapid test had a sensitivity of 80% and a specificity of 95.8% for SJS/TEN at the very first stages of the disease. It must be pointed out that the prognostic role of cytokines in SJS/TEN has not been completely explained yet. Su et al. demonstrated that the progression and fatality of the illness were correlated with increased levels of IL-15 that may be used to evaluate the prognosis of SJS/TEN (40).
The lymphocyte transformation test (LTT) can be used for identifying the offending drug. It is a safe and reproducible test but its reliability is a controversial issue because it shows many false positive and negative results. In SJS/TEN it has to be performed within the first week after the onset of the rash (41). It has been recently proposed that the T-cell activation assay can be used as an alternative for the LTT to identify the culprit drugs, with a sensitivity of 80% (95%CI: 52-96%) and a specificity of 96% (95%CI: 80-99%) (42). Patch testing (43) are not considered useful in SJS and TEN. It is not indicated to perform drug challenges with suspected drugs in SJS and TEN because second episode can be extremely dangerous (44).
A severity-of-illness score for TEN (SCORTEN) is a clinically predictive score based on 7 prognostic factors and it is used to assess the risk of mortality in TEN patients. In order to obtain a better assessment of the risk of mortality, SCORTEN should be calculated within 24 hours after admission. However, SCORTEN has not received full validation in children (45).
Management and therapy in SJS/TEN children
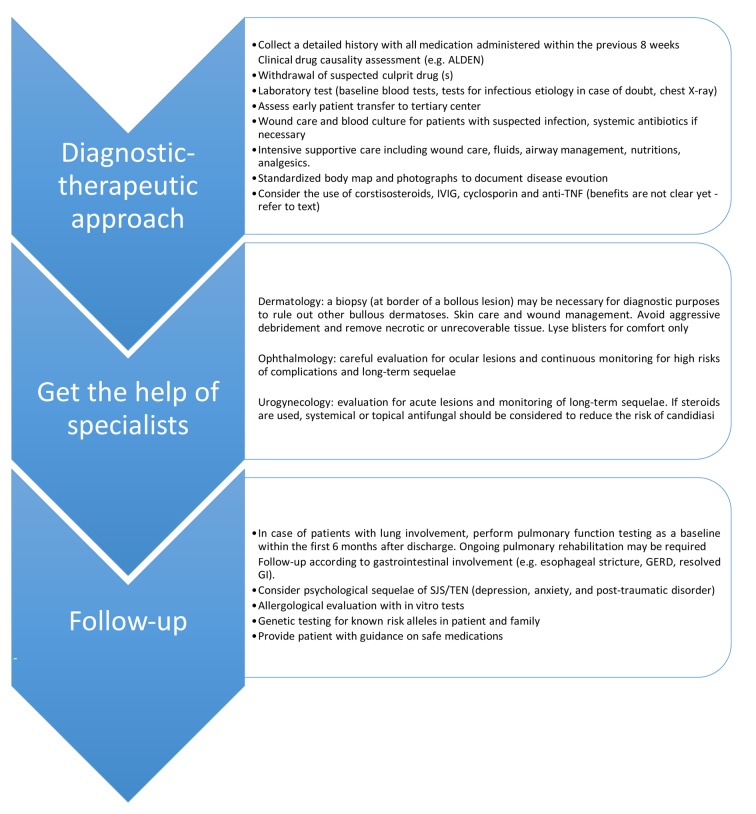
The management of SJS and TEN is mostly conservative and requires multidisciplinary skills (Table 1). It is important to immediately discontinue the causative drug and start supportive care. It comprises monitoring of fluid balance and electrolytes, respiratory and nutritional support. An important aspect is the nutritional needs of children with SJS/TEN. The energy requirements of SJS/TEN pediatric patients are increased, and a 30% factor to resting energy requirements should be applied when calculating nutritional support (46). Pain management includes administration of analgesics and topical anesthetics. With the aim of reducing the complications of the loss of barrier function, wound treatment is necessary and includes debridement of broken blisters, removal of necrotic skin, topical antiseptics or antibiotics, bandages (47, 48) and a warm environment (28°C). Admission to a specialized burn unit when skin involvement is > 25-30% is correlated to decrease morbidity and mortality rates (40). When clinical signs of infection occur, systemic antibiotics should be administered, always guided by systematic cultures of skin, mucosae, catheters and urine (49). An eye visit may be necessary. Psychosocial attention is necessary for a full patient care.
Table 1.
Suggested multidisciplinary approach for the management of SJS/TEN [modified from White KD et al. (71)]
There is insufficient evidence that there is an effective treatment of SJS/TEN. Randomized controlled studies for the treatment of SJS/TEN are lacking because it is a rare disease, often associated with a high rate of mortality. The therapeutic role of intravenous immunoglobulin (IVIG) is related to the direct inhibition of FAS/FAS ligand interaction (50). Many studies showed that patients treated with high dose (2-4 g/kg) in the first 4 days after the beginning ok skin lesions had a better recovery and a higher survival rate (51-53). On the other hand, other studies did not found such an improvement on mortality rates (54). The therapeutic role of corticosteroids (e.g. prednisolone, methylprednisolone and dexamethasone) has also been evaluated. On one side, some studies found that corticosteroids, particularly high doses of dexamethasone were effective, especially when they are used at the beginning of the disease (55). Other studies, underlined a higher risk of complications, such as gastrointestinal hemorrhage and sepsis, and a loss of efficacy (13, 55-58). In fact, the timing for corticosteroid systemic administration, the corticosteroid type, dose and the treatment duration are still not clearly defined.
Studies in adults showed that intensive supportive care was the only therapeutic measure that reduced mortality rates (50). However, a metanalysis did not find any difference between corticosteroid, IVIG and supportive care in reducing mortality (59). Although the literature is poor, patients treated with steroids and IVIG seemed to have a better outcome (54). In recent years it has become widely suggested to administer IVIG at high dose (2-4 g/kg) for 4 days followed by corticosteroids (16), especially in case of TEN or SJS/TEN overlap (60).
Other specific treatments include cyclosporine, plasmapheresis, TNF-α inhibitors or a combination of different drugs.
Recent studies evidenced that the use of immunosuppressive treatment with TNF-α inhibitors can be useful. Infliximab and etanercept have shown to be effective at halting disease progression (61, 63, 64). In moderate-to-severe SJS-TEN patients, a TNF-α antagonist etanercept in a randomized trial showed some advantages towards corticosteroids, including a significant shorter time for skin healing and a lower incidence of gastrointestinal bleeding (65).
Patients with SJS/TEN can be effectively treated with ciclosporine (3mg/kg/die for 7 days followed by 1.5 mg/kg/die) that may improve reepithelization, prevent onset of new lesions, reduce lenght of hospitalization. Both in adults and children cyclosporine reduces mortality (66-68) compared to high dose IVIG (15, 69).
Conclusions
Studies on children with SJS/TEN are scarsely reported and limited to small case series and retrospective studies. Therefore, a definition of SJS/ TEN in children requires further work. Incidence of severe drug reactions including SYS/TEN or anaphylaxis (70) is low in children, but SYS/TEN is associated with high mortality.
Rates of mortality are lower in children in comparison with adults, but a high rate of long-term complications is reported in pediatric population. Important progress has been recently acquired in the immunogenomics and immunopathogenesis of SJS/TEN. Nevertheless, several clinical and research gaps remain (71). Biomarkers for early diagnosis and prognosis are needed. They may be detected not only in serum but also in exhaled breath, a non invasive method for the assessment of inflammation (72-74). Guidelines based on high quality trials or metananalysis (75) for the therapeutic management and genetic predictors for most drugs that cause SJS/TEN are lacking. Furthermore, the reason why only a small percentage of population (<10%) with an HLA risk allele will develop SJS/TEN after exposure to the culprit drugs is still unclear (23). In conclusion, with the aim of ensuring an early diagnosis and an effective treatment, more studies are needed for a deeper understanding of the pathogenesis of SJS/TEN.
Conflict of interest:
None to declare
References
- 1.Pavlos R, White K.D, Wanjalla C, Mallal S.A, Phillips E.J. Severe delayed drug reaction-role of genetics and viral infections. Immunol Allergy Clin N Am. 2017;37:785–815. doi: 10.1016/j.iac.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stevens AM, Johnson FC. A new eruptive fever associated with stomatitis and ophthalmia: report of two cases in children. Am J Dis Child. 1922;24:526–33. [Google Scholar]
- 3.Bastuji-Garin S, Rzany B, Stern RS, Shear NH, Naldi L, Roujeau JC. Clinical classification of cases of toxic epidermal Necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol. 1993;129:92–6. [PubMed] [Google Scholar]
- 4.Yang MS, Lee JY, Kim J, et al. Incidence of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: a nationwide population-based study using National Health Insurance Database in Korea. PLoS One. 2016;11:e0165933. doi: 10.1371/journal.pone.0165933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsu DY, Brieva J, Silverberg NB, Paller AS, Silverberg JI. Pediatric Stevens-Johnson syndrome and toxic epidermal necrolysis in the United States. J Am Acad Dermatol. 2017;76:811–817. doi: 10.1016/j.jaad.2016.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finkelstein Y, Soon GS, Acuna P, et al. Recurrence and outcomes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Pediatrics. 2011;128:723–728. doi: 10.1542/peds.2010-3322. [DOI] [PubMed] [Google Scholar]
- 7.Levi N, Bastuji-Garin S, Mockenhaupt M, et al. Medications as risk factors of Stevens-Johnson syndrome and toxic epidermal necrolysis in children: a pooled analysis. Pediatrics. 2009;123:e297–e304. doi: 10.1542/peds.2008-1923. [DOI] [PubMed] [Google Scholar]
- 8.Antoon JW, Goldman JL, Lee B, Schwartz A. Incidence, outcomes, and resource use in children with Stevens-Johnson syndrome and toxic epidermal necrolysis. Pediatr Dermatol. 2018;35:182–187. doi: 10.1111/pde.13383. [DOI] [PubMed] [Google Scholar]
- 9.Sekula P, Dunant A, Mockenhaupt M, et al. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Invest Dermatol. 2013;133:1197–204. doi: 10.1038/jid.2012.510. [DOI] [PubMed] [Google Scholar]
- 10.Brockow K, Ardern-Jones M, Mockenhaupt M, et al. EAACI position paper on how to classify cutaneous manifestations of drug hypersensitivity. Allergy. 2018 doi: 10.1111/all.13562. doi: 10.1111/all.13562. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz RA, McDonough PH, Lee BW. Toxic epidermal necrolysis: Part I. Introduction, history, classification, clinical features, systemic manifestations, etiology, and immunopathogenesis. J Am Acad Dermatol. 2013;69:173. doi: 10.1016/j.jaad.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 12.López-García JS, Rivas Jara L, García-Lozano CI, Conesa E, de Juan IE, Murube del Castillo J. Ocular features and histopathologic changes during follow-up of toxic epidermal necrolysis. Ophthalmology. 2011;118:265–71. doi: 10.1016/j.ophtha.2010.06.035. [DOI] [PubMed] [Google Scholar]
- 13.Techasatian L, Panombualert S, Uppala R, Jetsrisuparb C. Drug-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in children: 20 years study in a tertiary care hospital. World J Pediatr. 2017;13:255–260. doi: 10.1007/s12519-016-0057-3. [DOI] [PubMed] [Google Scholar]
- 14.Yip LW, Thong BY, Lim J, et al. Ocular manifestations and complications of Stevens-Johnson syndrome and toxic epidermal necrolysis: an Asian series. Allergy. 2007;62:527–531. doi: 10.1111/j.1398-9995.2006.01295.x. [DOI] [PubMed] [Google Scholar]
- 15.Ferrandiz-Pulido C, Garcia-Patos V. A review of causes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Arch Dis Child. 2013;98:998–1003. doi: 10.1136/archdischild-2013-303718. [DOI] [PubMed] [Google Scholar]
- 16.Maverakis E, Wang EA, Shinkai K, et al. Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis standard reporting and evaluation guidelines: results of a National Institutes of Health Working Group. JAMA Dermatol. 2017;153:587–592. doi: 10.1001/jamadermatol.2017.0160. [DOI] [PubMed] [Google Scholar]
- 17.Egunsola O, Star K, Juhlin K, Kardaun SH, Choonara I, Sammons HM. Retrospective review of paediatric case reports of Stevens-Johnson syndrome and toxic epidermal necrolysis with lamotrigine from an international pharmacovigilance database. BMJ Paediatrics Open. 2017 doi: 10.1136/bmjpo-2017-000039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu L, Zhu Y, Yu J, Deng M, Zhu X. Nursing care of a boy seriously infected with Steven-Johnson syndrome after treatment with azithromycin. A case report and literature review. Medicine (Baltimore) 2018;97:e9112. doi: 10.1097/MD.0000000000009112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin Y-C, Sheu J-N, Chung W-H, et al. Vancomycin-induced Stevens-Johnson Syndrome in a boy under 2 years old: an early diagnosis by granulysin rapid test. Front Pediatr. 2018;6:26. doi: 10.3389/fped.2018.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kunimi Y, Hirata Y, Aihara M, Yamane Y Ikezawa. Statistical analysis of Stevens-Johnson syndrome caused by Mycoplasma pneumonia infection in Japan. Allergol Int. 2011;60:525–32. doi: 10.2332/allergolint.11-OA-0309. [DOI] [PubMed] [Google Scholar]
- 21.Tyagi S, Kumar S, Kumar A, Singla M, Singh A. Stevens-Johnson Syndrome - A life threatening skin disorder: A review. Chem Pharm Res. 2010;2:618–626. [Google Scholar]
- 22.Su SC, Chung WH. Update on pathobiology in Stevens-Johnson syndrome and toxic epidermal necrolysis. Dermatol Sin. 2013;31:175e80. [Google Scholar]
- 23.White KD, Chung WH, Hung SI, Mallal S, Phillips EJ. Evolving models of the immunopathogenesis of T cell-mediated drug allergy: the role of host, pathogens, and drug response. J Allergy Clin Immunol. 2015;136:219e34. doi: 10.1016/j.jaci.2015.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chung WH, Wang CW, Dao RL. Severe cutaneous adverse drug reactions. J Dermatol. 2016;43:758–66. doi: 10.1111/1346-8138.13430. [DOI] [PubMed] [Google Scholar]
- 25.Posadas SJ, Padial A, Torres MJ, et al. Delayed reactions to drugs show levels of perforin, granzyme B, and Fas-L to be related to disease severity. J Allergy Clin Immunol. 2002;109:155e61. doi: 10.1067/mai.2002.120563. [DOI] [PubMed] [Google Scholar]
- 26.Chung WH, Hung SI, Yang JY, et al. Granulysin is a key mediator for disseminated keratinocyte death in Stevens-Johnson syndrome and toxic epidermal necrolysis. Nat Med. 2008;14:1343e50. doi: 10.1038/nm.1884. [DOI] [PubMed] [Google Scholar]
- 27.Mockenhaupt M. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis expert review of clinical immunology. Expert Rev Clin Immunol. 2011;7:803–13. doi: 10.1586/eci.11.66. [DOI] [PubMed] [Google Scholar]
- 28.Caproni M, Antiga E, Parodi A, et al. Elevated circulating CD40 ligand in patients with erythema multiforme and Stevens-Johnson syndrome/toxic epidermal necrolysis spectrum. Br J Dermatol. 2006;154:319–324. doi: 10.1111/j.1365-2133.2006.07211.x. [DOI] [PubMed] [Google Scholar]
- 29.Paul C, Wolkenstein P, Adle H, et al. Apoptosis as a mechanism of keratinocyte death in toxic epidermal necrolysis. Br J Dermatol. 1996;134:710–4. doi: 10.1111/j.1365-2133.1996.tb06976.x. [DOI] [PubMed] [Google Scholar]
- 30.Viard-Leveugle I, Gaide O, Jankovic D, et al. TNF-α and IFN-γ are potential inducers of Fas-mediated keratinocyte apoptosis through activation of inducible nitric oxide synthase in toxic epidermal necrolysis. J Invest Dermatol. 2013;133:489–9. doi: 10.1038/jid.2012.330. [DOI] [PubMed] [Google Scholar]
- 31.Bharadwaj M, Illing P, Theodossis A, Purcell AW, Rossjohn J, McCluskey J. Drug hypersensitivity and human leukocyte antigens of the major histo-compatibility complex. Annu Rev Pharmacol Toxicol. 2012;52:401–31. doi: 10.1146/annurev-pharmtox-010611-134701. [DOI] [PubMed] [Google Scholar]
- 32.Pavlos R, Mallal S, Phillips E. HLA and pharmacogenetics of drug hypersensitivity. Pharmacogenomics. 2012;13:1285–306. doi: 10.2217/pgs.12.108. [DOI] [PubMed] [Google Scholar]
- 33.Chung WH, Hung SI. Genetic markers and danger signals in Stevens-Johnson syndrome and toxic epidermal necrolysis. Allergol Int. 2010;59:325–32. doi: 10.2332/allergolint.10-RAI-0261. [DOI] [PubMed] [Google Scholar]
- 34.Kaniwa N, Saito Y, Aihara M, et al. HLA-B locus in Japanese patients with antiepileptics and allopurinol-related Stevens-Johnson syndrome and toxic epidermal necrolysis. Pharmacogenomics. 2008;9:1617–22. doi: 10.2217/14622416.9.11.1617. [DOI] [PubMed] [Google Scholar]
- 35.Pereira FA, Mudgil AV, Rosmarin DM. Toxic epidermal necrolysis. J Am Acad Dermatol. 2007;56:181–200. doi: 10.1016/j.jaad.2006.04.048. [DOI] [PubMed] [Google Scholar]
- 36.Sassolas B, Haddad C, Mockenhaupt M, et al. ALDEN, an algorithm for assessment of drug causality in Stevens-Johnson syndrome and toxic epidermal necrolysis: comparison with case-control analysis. Clin Pharmacol Ther. 2010;88:60–8. doi: 10.1038/clpt.2009.252. [DOI] [PubMed] [Google Scholar]
- 37.Abe R, Yoshioka N, Murata J, Fujita Y, Shimizu H. Granulysin as a marker for early diagnosis of the Stevens-Johnson syndrome. Ann Intern Med. 2009;151:514. doi: 10.7326/0003-4819-151-7-200910060-00016. [DOI] [PubMed] [Google Scholar]
- 38.Fujita Y, Yoshioka N, Abe R, et al. Rapid immunochromatographic test for serum granulysin is useful for the prediction of Stevens-Johnson syndrome and toxic epidermal necrolysis. J Am Acad Dermatol. 2011;65:65–8. doi: 10.1016/j.jaad.2010.04.042. [DOI] [PubMed] [Google Scholar]
- 39.Ezagallaai AA, Rieder MJ. In vitro testing for diagnosis of idiosyncratic adverse drug reactions: Implications for pathophysiology. Br J Clin Pharmacol. 2015;80:889–900. doi: 10.1111/bcp.12505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Su SC, Mockenhaupt M, Wolkenstein P, et al. Interleukin-15 is associated with severity and mortality in Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis. J Invest Dermatol. 2017;137:1065–1073. doi: 10.1016/j.jid.2016.11.034. [DOI] [PubMed] [Google Scholar]
- 41.Kano Y, Hirahara K, Mitsuyama Y, Takahashi R, Shiohara T. Utility of the lymphocyte transformation test in the diagnosis of drug sensitivity: dependence on its timing and the type of drug eruption. Allergy. 2007;62:1439–44. doi: 10.1111/j.1398-9995.2007.01553.x. [DOI] [PubMed] [Google Scholar]
- 42.Porebski G, Pecaric-Petkovic T, Groux-Keller M, Bosak M, Kawabata TT, Pichler WJ. In vitro drug causality assessment in Stevens-Johnson syndrome - alternatives for lymphocyte transformation test. Clin Exp Allergy. 2013;43:1027–37. doi: 10.1111/cea.12145. [DOI] [PubMed] [Google Scholar]
- 43.Caglayan Sozmen S, Povesi Dascola C, Gioia E, Mastrorilli C, Rizzuti L, Caffarelli C. Diagnostic accuracy of patch test in children with food allergy. Pediatr Allergy Immunol. 2015;26:416–22. doi: 10.1111/pai.12377. [DOI] [PubMed] [Google Scholar]
- 44.Caffarelli C, Franceschini F, Caimmi D, et al. SIAIP position paper: provocation challenge to antibiotics and non-steroidal anti-inflammatory drugs in children. Ital J Pediatr. 2018;44:14. doi: 10.1186/s13052-018-0589-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bastuji-Garin S, Fouchard N, Bertocchi M, Roujeau JC, Revuz J, Wolkenstein P. SCORTEN: a severity-of-illness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115:149–153. doi: 10.1046/j.1523-1747.2000.00061.x. [DOI] [PubMed] [Google Scholar]
- 46.Mayes T, Gottschlich M, Khoury J, Warner P, Kagan R. Energy requirements of pediatric patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. Nutr Clin Pract. 2008;23:547–50. doi: 10.1177/0884533608323434. [DOI] [PubMed] [Google Scholar]
- 47.Fernando SL. The management of toxic epidermal necrolysis. Australas J Dermatol. 2012;53:165–71. doi: 10.1111/j.1440-0960.2011.00862.x. [DOI] [PubMed] [Google Scholar]
- 48.Spies M, Sanford AP, Aili Low JF, Wolf SE, Herndon DN. Treatment of extensive toxic epidermal necrolysis in children. Pediatrics. 2001;108:1162–8. doi: 10.1542/peds.108.5.1162. [DOI] [PubMed] [Google Scholar]
- 49.de Prost N, Ingen-Housz-Oro S, Duong Ta, et al. Bacteriemia in Stevens-Johnson síndrome and toxic epidermal necrolysis. Epidemiology, risk factors, and predictive value of skin cultures. Medicine. 2009;89:28–36. doi: 10.1097/MD.0b013e3181ca4290. [DOI] [PubMed] [Google Scholar]
- 50.Schwartz RA, McDonough PH, Lee BW. Toxic epidermal necrolysis: Part II. Prognosis, sequelae, diagnosis, differential diagnosis, prevention, and treatment. J Am Acad Dermatol. 2013;69(187):e1–16. doi: 10.1016/j.jaad.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 51.Stella M, Clemente A, Bollero D, Risso D, Dalmasso P. Toxic epidermal necrolysis and Stevens-Johnson syndrome: experience with high-dose intravenous immunoglobulins and topical conservative approach. A retrospective analysis. Burns. 2007;33:452–9. doi: 10.1016/j.burns.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 52.Mangla K, Rastogi S, Goyal P, Solanki RB, Rawal RC. Efficacy of low dose intravenous immunoglobulins in children with toxic epidermal necrolysis: an open uncontrolled study. Indian J Dermatol Venereol Leprol. 2005;71:398–400. doi: 10.4103/0378-6323.18943. [DOI] [PubMed] [Google Scholar]
- 53.Koh MJ, Tay YK. Stevens-Johnson syndrome and toxic epidermal necrolysis in Asian children. J Am Acad Dermatol. 2010;62:54–60. doi: 10.1016/j.jaad.2009.06.085. [DOI] [PubMed] [Google Scholar]
- 54.Shortt R, Gomez M, Mittman N Cartotto. Intravenous immunoglobulin does not improve outcome in toxic epidermal necrolysis. J Burn Care Rehabil. 2004;25:246–55. doi: 10.1097/01.bcr.0000124746.33279.86. [DOI] [PubMed] [Google Scholar]
- 55.Schneck J, Fagot JP, Sekula P, Sassolas B, Roujeau JC, Mockenhaupt M. Effects of treatments on the mortality of Stevens-Johnson syndrome and toxic epidermal necrolysis: A retrospective study on patients included in the prospective EuroSCAR Study. J Am Acad Dermatol. 2008;58:33–40. doi: 10.1016/j.jaad.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 56.Del Pozzo-Magana BR, Lazo-Langner A, Carleton B, Castro-Pastrana LI, Rieder MJ. A systematic review of treatment of drug-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in children. J Popul Ther Clin Pharmacol. 2011;18:e121–33. [PubMed] [Google Scholar]
- 57.Koh MJ, Tay YK. An update on Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Curr Opin Pediatr. 2009;21:505–10. doi: 10.1097/MOP.0b013e32832d1fef. [DOI] [PubMed] [Google Scholar]
- 58.Corrick F, Anand G. Would systemic steroids be useful in the management of Stevens-Johnson syndrome? Arch Dis Child. 2013;98:828–830. doi: 10.1136/archdischild-2013-304909. [DOI] [PubMed] [Google Scholar]
- 59.Roujeau JC, Bastuji-Garin S. Systematic review of treatments for Stevens-Johnson syndrome and toxic epidermal necrolysis using the SCORTEN score as a tool for evaluating mortality. Ther Adv Drug Saf. 2011;2:87–94. doi: 10.1177/2042098611404094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sato S, Kanbe T, Tamaki Z, et al. Clinical features of Stevens-Johnson syndrome and toxic epidermal necrolysis. Pediatr Int. 2018;60:697–702. doi: 10.1111/ped.13613. [DOI] [PubMed] [Google Scholar]
- 61.Chave TA, Mortimer NJ, Sladden MJ, Hall AP, Hutchinson PE. Toxic epidermal necrolysis: current evidence, practical management and future directions. Br J Dermatol. 2005;153:241–253. doi: 10.1111/j.1365-2133.2005.06721.x. [DOI] [PubMed] [Google Scholar]
- 62.Woolridge K.F, Boler P.L, Lee B.D. Tumor necrosis factor alpha inhibitors in the treatment of toxic epidermal necrolysis. Cutis. 2018;101:e15–e21. [PubMed] [Google Scholar]
- 63.Paradisi A, Abeni D, Bergamo F, Ricci F, Didona D, Didona B. Etanercept therapy for toxic epidermal necrolysis. J Am Acad Dermatol. 2014;71:278–83. doi: 10.1016/j.jaad.2014.04.044. [DOI] [PubMed] [Google Scholar]
- 64.Scott-Lang V1, Tidman M, McKay D. Toxic epidermal necrolysis in a child successfully treated with infliximab. Pediatr Dermatol. 2014;31:532–4. doi: 10.1111/pde.12029. [DOI] [PubMed] [Google Scholar]
- 65.Wang CW, Yang LY, Chen CB, et al. Randomized, controlled trial of TNF-α antagonist in CTL-mediated severe cutaneous adverse reactions. J Clin Invest. 2018;128:985–996. doi: 10.1172/JCI93349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zimmermann S, Sekula P, Venhoffetal M. Systemic immunomodulating therapies for Stevens-Johnson syndrome and toxic epidermal necrolysis: a systematic review and meta-analysis. JAMA Dermatology. 2017;153:514–522. doi: 10.1001/jamadermatol.2016.5668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.St. John J, Ratushny V, Liu KJ, et al. Successful use of cyclosporin A for Stevens-Johnson syndrome and toxic epidermal necrolysis in three children. Pediatr Dermatol. 2017;34:540–546. doi: 10.1111/pde.13236. [DOI] [PubMed] [Google Scholar]
- 68.González-Herrada C, Rodríguez-Martín S, Cachafeiro L, et al. Cyclosporine use in epidermal necrolysis is associated with an important mortality reduction: evidence from three different approaches. J Invest Dermatol. 2017;137:2092–2100. doi: 10.1016/j.jid.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 69.Lee HY, Lim YL, Thirumoorthy T, Pang SM. The role of intravenous immunoglobulin in toxic epidermal necrolysis: a retrospective analysis of 64 patients managed in a specialized centre. Br J Dermatol. 2013;169:1304–9. doi: 10.1111/bjd.12607. [DOI] [PubMed] [Google Scholar]
- 70.Caimmi S, Caimmi D, Bernardini R, et al. Perioperative anaphylaxis: epidemiology. Int J Immunopathol Pharmacol. 2011;24(3):S21–6. doi: 10.1177/03946320110240s304. [DOI] [PubMed] [Google Scholar]
- 71.White KD, Abe R, Arden-Jones M, et al. SJS/TEN 2017: Building Multidisciplinary Networks to Drive Science and Translation. J Allergy Clin Immunol Pract. 2018;6:38–69. doi: 10.1016/j.jaip.2017.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Corradi M, Zinelli C, Caffarelli C. Exhaled breath biomarkers in asthmatic children. Inflamm Allergy Drug Targets. 2007;6:150–9. doi: 10.2174/187152807781696437. [DOI] [PubMed] [Google Scholar]
- 73.Caffarelli C, Dascola CP, Peroni D, et al. Airway acidification in childhood asthma exacerbations. Allergy Asthma Proc. 2014;35:51–6. doi: 10.2500/aap.2014.35.3740. [DOI] [PubMed] [Google Scholar]
- 74.Zinelli C, Caffarelli C, Strid J, Jaffe A, Atherton DJ. Measurement of nitric oxide and 8-isoprostane in exhaled breath of children with atopic eczema. Clin Exp Dermatol. 2009;34:607–12. doi: 10.1111/j.1365-2230.2008.03142.x. [DOI] [PubMed] [Google Scholar]
- 75.Caffarelli C, Bernasconi S. Preventing necrotising enterocolitis with probiotics. Lancet. 2007;369:1578–80. doi: 10.1016/S0140-6736(07)60721-1. [DOI] [PubMed] [Google Scholar]