This cohort study examines the extent of segregation and inequality of care of very low-birth-weight and very preterm infants across US neonatal intensive care units (NICUs).
Key Points
Question
What is the extent of segregation and inequality in neonatal intensive care units (NICUs)?
Findings
A cohort study of 117 982 very low-birth-weight and very preterm infants found that NICUs were segregated by race and ethnicity. Compared with white infants, black infants were concentrated at lower-quality NICUs and Hispanic and Asian infants at higher-quality NICUs.
Meaning
Segregation explains where infants receive care but not why black infants receive care at lower-quality NICUs and Asian infants receive care at higher-quality NICUs than white infants.
Abstract
Importance
Racial and ethnic minorities receive lower-quality health care than white non-Hispanic individuals in the United States. Where minority infants receive care and the role that may play in the quality of care received is unclear.
Objective
To determine the extent of segregation and inequality of care of very low-birth-weight and very preterm infants across neonatal intensive care units (NICUs) in the United States.
Design, Setting, and Participants
This cohort study of 743 NICUs in the Vermont Oxford Network included 117 982 black, Hispanic, Asian, and white infants born at 401 g to 1500 g or 22 to 29 weeks’ gestation from January 2014 to December 2016. Analysis began January 2018.
Main Outcomes and Measures
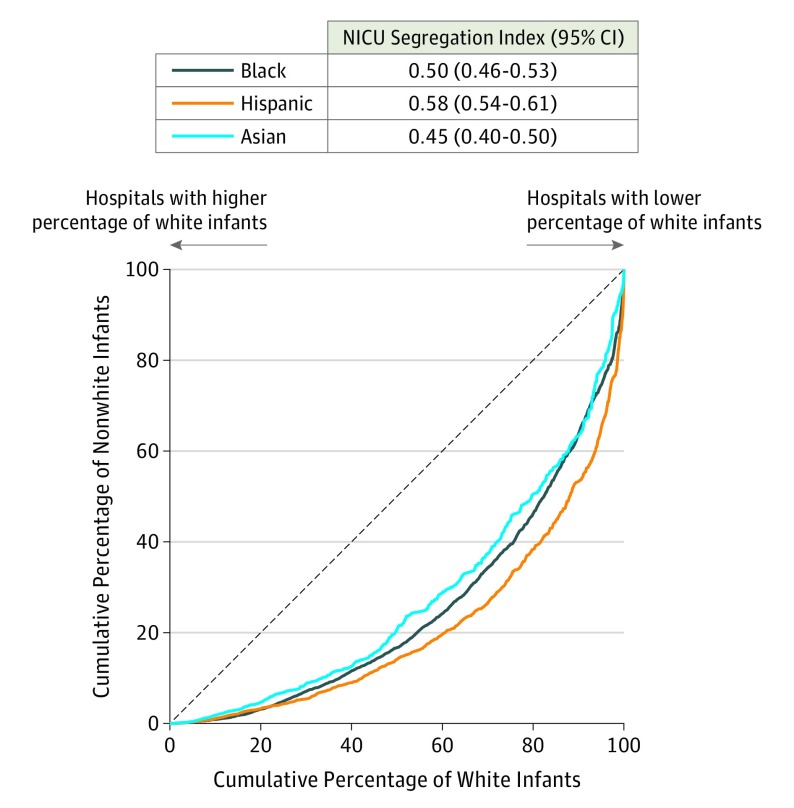
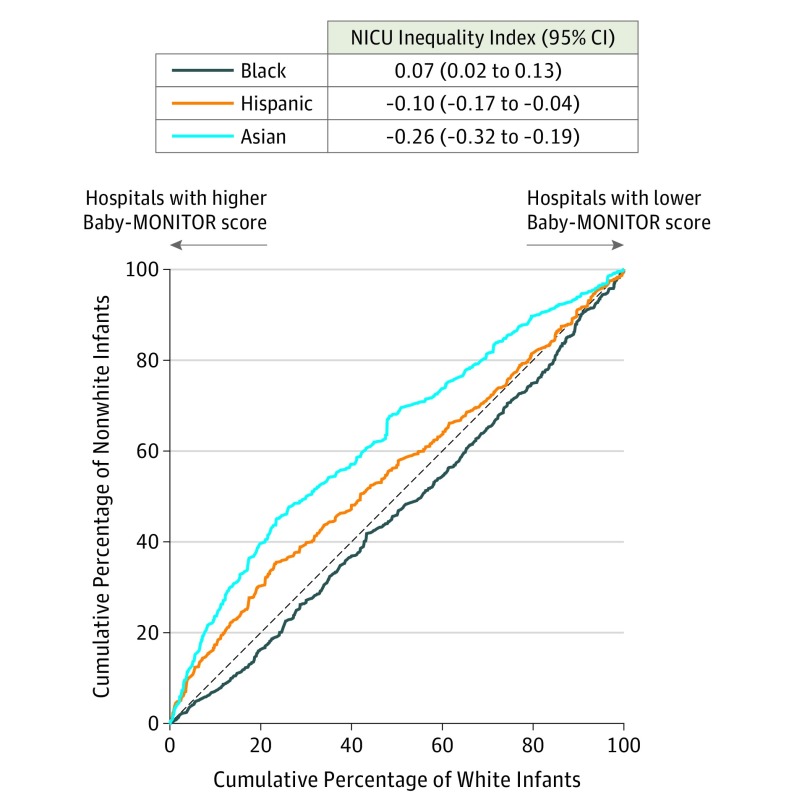
The NICU segregation index and NICU inequality index were calculated at the hospital level as the Gini coefficients associated with the Lorenz curves for black, Hispanic, and Asian infants compared with white infants, with NICUs ranked by proportion of white infants for the NICU segregation index and by composite Baby-MONITOR (Measure of Neonatal Intensive Care Outcomes Research) score for the NICU inequality index.
Results
Infants (36 359 black [31%], 21 808 Hispanic [18%], 5920 Asian [5%], and 53 895 white [46%]) were segregated among the 743 NICUs by race and ethnicity (NICU segregation index: black: 0.50 [95% CI, 0.46-0.53], Hispanic: 0.58 [95% CI, 0.54-0.61], and Asian: 0.45 [95% CI, 0.40-0.50]). Compared with white infants, black infants were concentrated at NICUs with lower-quality scores, and Hispanic and Asian infants were concentrated at NICUs with higher-quality scores (NICU inequality index: black: 0.07 [95% CI, 0.02-0.13], Hispanic: −0.10 [95% CI, −0.17 to −0.04], and Asian: −0.26 [95% CI, −0.32 to −0.19]). There was marked variation among the census regions in weighted mean NICU quality scores (range: −0.69 to 0.85). Region of residence explained the observed inequality for Hispanic infants but not for black or Asian infants.
Conclusions and Relevance
Black, Hispanic, and Asian infants were segregated across NICUs, reflecting the racial segregation of minority populations in the United States. There were large differences between geographic regions in NICU quality. After accounting for these differences, compared with white infants, Asian infants received care at higher-quality NICUs and black infants, at lower-quality NICUs. Explaining these patterns will require understanding the effects of sociodemographic factors and public policies on hospital quality, access, and choice for minority women and their infants.
Introduction
Minority individuals in the United States live in lower-income neighborhoods,1,2,3 attend lower-quality schools,4,5 and receive medical care at lower-quality hospitals than their white counterparts.6,7,8,9,10,11 These inequalities perpetuate the social and economic injustices of structural racism1,12,13,14,15 and contribute to racial and ethnic disparities in health outcomes.16,17,18,19,20 The relationship between segregation and the quality of care received by high-risk infants has not been studied on a national scale, to our knowledge.
The goal of this study was to determine the extent of segregation and inequality in the care of black, Hispanic, and Asian very low-birth-weight and very preterm infants compared with white infants across neonatal intensive care units (NICUs) in the United States. Segregation refers to the uneven distribution of racial or ethnic groups across NICUs. Inequality refers to the concentration of racial or ethnic groups in lower-quality NICUs.
We defined 2 indices, the NICU segregation index and NICU inequality index, based on the Gini coefficients associated with the corresponding Lorenz curves.2,21 These indices quantify the extent of segregation and inequality for black, Hispanic, and Asian infants compared with white infants. Because racial and ethnic minorities reside disproportionately in certain regions of the United States, we also explored differences in NICU quality between regions.
Methods
Population
Vermont Oxford Network is a voluntary worldwide community dedicated to improving the quality, safety, and value of perinatal and neonatal care.22 Member NICUs in the United States contributed standardized data on all infants aged 22 to 29 weeks’ gestation or with 401 g to 1500 g birth weight who were inborn or transferred to the hospital within 28 days of birth.23 We included 134 871 infants born from January 2014 to December 2016. Analysis began January 2018. We excluded Native American infants (n = 915), infants of other races (n = 2499) or unknown race (n = 873), infants with serious congenital anomalies (n = 6220), deaths in the delivery room or within 12 hours of birth (n = 5244), and those transferred more than once (n = 1138), leaving 117 982 eligible infants at 743 hospitals. The University of Vermont institutional review board determined that use of the Vermont Oxford Network repository for this analysis was not human subjects research.
Race and Ethnicity
Definitions of race and ethnicity were derived from the 2010 United States Census.24,25 Abstractors were instructed to obtain the information by personal interview with the mother, review of the birth certificate, or review of the medical record, in that order.25 We combined race and ethnicity to yield non-Hispanic white, non-Hispanic black, Hispanic (any race), and non-Hispanic Asian categories, which we refer to as white, black, Hispanic, and Asian, respectively.
Baby-MONITOR Scores
Baby-MONITOR (Measure of Neonatal Intensive Care Outcomes Research) is a hospital-level composite score of NICU quality based on 9 infant-level measures: antenatal steroid exposure; hypothermia on admission; non–surgically induced pneumothorax; health care–associated bacterial or fungal infection; chronic lung disease; timely retinal examination; discharge on human breast milk; mortality during the birth hospitalization; and growth velocity.26 The measures were designed to attribute events appropriately for infants who were transferred to a NICU from another hospital after birth. The measures were individually risk adjusted and standardized relative to other hospitals in the data set.27,28 The standardized scores for the 9 measures were equally weighted, after placing them on a common scale, and averaged to derive the composite NICU Baby-MONITOR score. A higher Baby-MONITOR score indicates higher quality of care. Baby-MONITOR, which was tested in samples of California NICUs, is a robust discriminator of quality of care delivery.26,29
Lorenz Curves, NICU Segregation Index, and NICU Inequality Index
Lorenz curves for segregation and inequality were generated at the hospital level separately for black, Hispanic, and Asian infants with white infants as the reference group. Gini coefficients associated with the curves were calculated for the NICU segregation index and NICU inequality index for each racial or ethnic group. This approach is based on the method used by Firebaugh and colleagues2 and Farrell and colleagues21 for measuring segregation and inequality of income across residential neighborhoods.
To construct Lorenz curves for segregation, NICUs were ranked by the proportion of white infants from highest to lowest. The cumulative study population percentages of white and minority infants were plotted on the x- and y-axes. If all NICUs had the same racial distribution as the study population, the Lorenz curves would be diagonal lines. When the racial composition at NICUs differs from the study population, the curve falls below the diagonal. The NICU segregation index was defined as the Gini coefficient for the curve, ie, the proportion of the area below the diagonal that is above the curve. The NICU segregation index could range from 0 (no racial segregation) to 1 (complete segregation). Because hospitals were ranked to maximize the difference in cumulative distributions, the Lorenz curve always fell below the diagonal and the NICU segregation index was always positive.
In the Lorenz curves for inequality, NICUs were ranked by Baby-MONITOR scores and the cumulative study population percentages of white and minority infants were plotted on the x- and y-axes. If all NICUs had identical quality scores or if the proportion of each racial group was the same in every NICU as in the study population, the Lorenz curves would be diagonal lines. If minority infants were cared for at lower-quality hospitals, the curve would fall below the diagonal and the NICU inequality index was calculated as above. If minority infants were cared for at higher-quality hospitals, the curve would appear above the diagonal. The NICU inequality index was defined as the proportion of the area above the diagonal that was below the curve and given a negative sign. A negative NICU inequality index indicated that minority infants were treated at higher-quality NICUs than white infants.
Analysis
The NICU segregation and NICU inequality indices were calculated by race. Confidence intervals for the indices were obtained by bootstrap resampling by hospital.30 To investigate regional differences in care, the weighted mean composite Baby-MONITOR score for United States Census divisions31 and the distributions of race/ethnicity by region were determined. Linear regression at the hospital level was used to estimate the associations of racial distribution within hospitals and Baby-MONITOR scores with and without adjusting for region. The reduction in coefficients for races between the 2 models was interpreted to represent the extent that region accounted for NICU-level racial disparities. R version 3.4.3 (R Project for Statistical Computing) was used for all data analyses.32
Results
Of the 743 hospitals in the study, 98 (13%) had restrictions on assisted ventilation, 236 (32%) had no ventilation restrictions and did not perform neonatal surgery, 299 (40%) had no ventilation restrictions and performed neonatal surgery except cardiac surgery requiring bypass, and 110 (15%) had no ventilation restrictions and performed neonatal surgery including cardiac surgery requiring bypass. Overall, 358 (48%) were teaching hospitals. Thirty-eight hospitals (5%) contributed 1 year of data, 28 hospitals (4%) contributed 2 years of data, and 677 hospitals (91%) contributed data for all 3 years. The characteristics of the 117 982 eligible infants (36 359 black [31%], 53 895 white [46%], 21 808 Hispanic [18%], 5920 Asian [5%] infants) are shown in Table 1.
Table 1. Infant Characteristics by Race/Ethnicity, 2014-2016.
| Variable | White Infants (n = 53 895)a | Black Infants (n = 36 359)a | Hispanic Infants (n = 21 808) | Asian Infants (n = 5920)a | Overall (N = 117 982) |
|---|---|---|---|---|---|
| Gestational age, median (IQR), wk | 28 (26-30) | 28 (26-30) | 28 (26-30) | 29 (27-31) | 28 (26-30) |
| Birth weight, median (IQR), g | 1134 (860-1349) | 1035 (760-1290) | 1090 (820-1325) | 1130 (865-1340) | 1100 (820-1330) |
| 1-min Apgar score, median (IQR) | 6 (3-7) | 5 (3-7) | 6 (3-8) | 6 (4-8) | 6 (3-7) |
| Male, No. (%) | 27 283(51) | 17 659 (49) | 11 173 (51) | 3098 (52) | 59 213 (50) |
| Inborn, No. (%) | 46 007 (85) | 31 870 (88) | 18 611 (85) | 5265 (89) | 101 753 (86) |
| Multiple gestation, No. (%) | 17 481 (32) | 7821 (22) | 4675 (21) | 1693 (29) | 31 670 (27) |
| Vaginal delivery, No. (%) | 13 290 (25) | 10 529 (29) | 6064 (28) | 1520 (26) | 31 403 (27) |
Abbreviation: IQR, interquartile range.
Non-Hispanic infants.
The Lorenz curves for segregation are shown in Figure 1. The NICU segregation indices for black, Hispanic, and Asian infants were 0.50 (95% CI, 0.46-0.53), 0.58 (95% CI, 0.54-0.61), and 0.45 (95% CI, 0.40-0.50), respectively, indicating that nonwhite infants were segregated into different hospitals than white infants and demonstrating substantial segregation of minority patients. The average proportions of white, black, Hispanic, and Asian infants by quintiles of the ranked cumulative distribution of white infants are shown in eTable 1 in the Supplement.
Figure 1. Lorenz Curves for Segregation by Race/Ethnicity in US Neonatal Intensive Care Units (NICUs).
Hospitals were ranked by the proportion of white infants from highest to lowest, and the cumulative population percentages of white and minority infants were plotted on the x- and y-axes. If all NICUs had the same racial distribution as the overall population, the curves would fall on the 45° diagonal line. The light blue line (left) represents Asian infants. The dark blue line (middle) represents black infants. The orange line (right) represents Hispanic infants.
The Lorenz curves for inequality are shown in Figure 2. The NICU inequality indices for Hispanic and Asian infants were −0.10 (95% CI, −0.17 to −0.04) and −0.26 (95% CI, −0.32 to −0.19), respectively, and the curves were above the diagonal indicating that these infants were treated at higher-quality NICUs than white infants. The NICU inequality index for black infants was 0.07 (95% CI, 0.02-0.13) and the curve was below the diagonal, indicating that black infants were treated at lower-quality NICUs. The average proportions of white, black, Hispanic, and Asian infants by quintiles of ranked Baby-MONITOR scores are shown in the eFigure in the Supplement.
Figure 2. Lorenz Curves for Inequality of Care by Race/Ethnicity in US Neonatal Intensive Care Units (NICUs).
Hospitals were ranked by their Baby-MONITOR (Measure of Neonatal Intensive Care Outcomes Research) scores, and the cumulative population percentages of white and minority infants were plotted on the x- and y-axes. If all racial/ethnic groups had the same quality distribution as the overall population, the curves would fall on the 45° diagonal line. The light blue line (left) represents Asian infants. The orange line (middle) represents Hispanic infants. The dark blue line (right) represents black infants.
The weighted mean Baby-MONITOR scores for the NICUs and the proportion of all infants in each racial/ethnic group in each Census division are shown in Table 2. Mean Baby-MONITOR scores ranged from 0.85 in the Pacific region to −0.69 in the Mountain region. Thirty-two percent of all Hispanic infants (n = 6877) and 42% of Asian infants (n = 2476) were at NICUs in the Pacific region, which had the highest mean Baby-MONITOR scores of all regions, whereas 31% of Hispanic infants (n = 6846) and 15% of Asian infants (n = 875) were at NICUs in the regions with the lowest Baby-MONITOR scores (East South Central, West South Central, and Mountain). Only 6% of all black infants (n = 2022) were at NICUs in the Pacific region and 76% (n = 9686) were in regions with the lowest Baby-MONITOR scores.
Table 2. Mean Baby-MONITOR Score and Racial Distribution by US Census Region (N = 117 982).
| Region | Weighted Mean Baby-MONITOR Score | No. (%) | |||
|---|---|---|---|---|---|
| White Infantsa | Black Infantsa | Hispanic Infants | Asian Infantsa | ||
| New England | 0.21 | 2514 (5) | 826 (2) | 834 (4) | 244 (4) |
| Middle Atlantic | −0.18 | 5791 (11) | 4283 (12) | 2236 (10) | 852 (14) |
| East North Central | 0.00 | 10 267 (19) | 6025 (17) | 1585 (7) | 546 (9) |
| West North Central | 0.02 | 5653 (10) | 1877 (5) | 599 (3) | 302 (5) |
| South Atlantic | −0.01 | 9626 (18) | 11 640 (32) | 2831 (13) | 625 (11) |
| East South Central | −0.51 | 4597 (9) | 3788 (10) | 356 (2) | 89 (2) |
| West South Central | −0.42 | 5776 (11) | 5226 (14) | 4568 (21) | 547 (9) |
| Mountain | −0.69 | 3629 (7) | 672 (2) | 1922 (9) | 239 (4) |
| Pacific | 0.85 | 6042 (11) | 2022 (6) | 6877 (33) | 2476 (42) |
Abbreviation: MONITOR, Measure of Neonatal Intensive Care Outcomes Research.
Non-Hispanic infants.
The results of linear regression models of Baby-MONITOR scores with and without adjusting for region are shown in Table 3. In the regression model without region, a 10% increase in the percentage of black infants corresponded to an estimated Baby-MONITOR score decrease of 0.05, a 10% increase in the percentage of Hispanic infants corresponded to an increase of 0.04, and a 10% increase in the percentage of Asian infants corresponded to an increase of 0.31. After adjusting for region, the model coefficient for Hispanic ethnicity decreased to 0.02 and the model coefficient for Asian race decreased to 0.14, indicating that the concentration of these infants at higher-quality NICUs may be substantially but not entirely explained by region. The association of a higher proportion of black infants at NICUs with lower Baby-MONITOR scores was not affected by adjusting for region suggesting that the concentration of black infants at lower-quality NICUs cannot be explained by region.
Table 3. Linear Regression Results Comparing Baby-MONITOR Scores With and Without Adjusting for US Census Region.
| Race/Ethnicity | Model Without Region | Model With Region | ||
|---|---|---|---|---|
| Effect of 10% Increase in Population (95% CI) | P Value | Effect of 10% Increase in Population (95% CI) | P Value | |
| Blacka | −0.05 (−0.08 to −0.01) | .01 | −0.05 (−0.09 to −0.01) | .01 |
| Hispanic | 0.04 (0.00 to 0.08) | .06 | 0.02 (−0.03 to 0.06) | .42 |
| Asiana | 0.31 (0.21 to 0.41) | <.001 | 0.14 (0.03 to 0.25) | .01 |
Abbreviation: MONITOR, Measure of Neonatal Intensive Care Outcomes Research.
Non-Hispanic infants.
Discussion
Our results provide evidence for segregation and inequality in the care of very low-birth-weight and very preterm infants. Black, Hispanic, and Asian infants were distributed unevenly across NICUs compared with white infants. Compared with white infants, black infants received care at lower-quality NICUs and Asian infants at higher-quality NICUs after accounting for region of residence.
Residential segregation in the United States is a manifestation of the structural racism inherent in our society.1,2,3,14,15,33,34 It affects opportunities across many dimensions including economic well-being, education, and health care. Previous research has documented the relationship between segregation and access to quality health care. In New York City, New York, black mothers were less likely than white mothers to live in neighborhoods that had hospitals with the lowest risk-adjusted infant mortality rates.9 Adult black patients in New York City were 2 to 3 times less likely than white patients to be treated at academic medical centers, while minority patients in Boston were overrepresented at academic medical centers.35 Jha and colleagues10 found that the lowest-quality, highest-cost hospitals in the United States, primarily located in the south, cared for twice the proportion of elderly black patients compared with the highest-quality, lowest-cost hospitals. Dimick and colleagues11 found that adult black surgical patients who lived in racially segregated health care service areas or markets were significantly more likely to receive care at lower-quality hospitals even if they lived closer to higher-quality hospitals. Although Asian American individuals generally have higher educational and income attainment than other races and ethnicities,36,37 Asian adults, as well as black and Hispanic adults, can experience problems accessing preventive care,38,39 particularly in rural areas.40,41 We found substantial segregation in NICU care nationally for black, Hispanic, and Asian infants as indicated by the NICU segregation indices of 0.50, 0.58, and 0.45, respectively. The role of residential segregation in access to quality health care cannot be overlooked and demands further study at the neighborhood, city, state, and regional levels.
The NICU inequality index for black infants compared with white infants was 0.07 (95% CI, 0.02-0.13), indicating that black infants received care at lower-quality NICUs than white infants, whereas the inequality indices for Hispanic and Asian infants of −0.10 (95% CI, −0.17 to −0.04) and −0.26 (95% CI, −0.32 to −0.19), respectively, indicated they received care at higher-quality NICUs. Because inequality is bounded by segregation, the inequality differences were not as profound as the segregation differences. (Across hospitals, racial inequality is possible only when there is racial segregation.) Black and white infants were spread more evenly across higher-quality and lower-quality hospitals than they were across hospitals in general. Several underlying pathways explain the observed differences, requiring further study.
We found marked, clinically important differences in the mean NICU quality scores among the Census divisions, ranging from −0.69 in the Mountain region to 0.85 in the Pacific region, which helped explain some of these findings. For Hispanic infants, the NICU inequality index may have been explained by higher-quality NICUs in the Pacific region where a large proportion of Hispanic infants resided. The NICU inequality index for Asian infants also may have been partially explained by the regions in which they resided. The concentration of black infants in lower-quality NICUs was not explained by region. Like the regional differences, segregation and inequality in NICU care at the city and state levels likely vary widely around the national mean values that we report.
Other studies have found differences in NICU inequality and outcomes by race and ethnicity, but the directions and magnitudes of the differences have not been consistent. In New York City, 40% of the black-white disparity and 30% of the Hispanic-white disparity in neonatal morbidity and mortality occurred because white pregnant women received care at better-performing hospitals, but there was no evidence of within NICU differences.20 In California, Hispanic infants had significantly lower Baby-MONITOR scores than white infants while black and Asian infants did not; however, in California there were within-NICU disparities by race and ethnicity. White infants appeared to have higher scores than black infants as NICU quality scores increased, and white infants appeared to have higher scores than Hispanic infants in most NICUs irrespective of a NICU’s overall performance. Still, even in low-performing NICUs in California, Asian infants often had higher scores than white infants.29 Whether these patterns will be observed in other states and regions will be the topic of a future Vermont Oxford Network study. Additional research on factors that influence access, referral patterns, and hospital choice is required to fully understand the variation in inequality of NICU care among different cities, health care markets, states, and regions.42
The roles of racism13,14 and bias43 in health care inequalities also deserves further investigation. The Institute of Medicine found that “bias, stereotyping, prejudice, and clinical uncertainty on the part of healthcare providers may contribute to racial and ethnic disparities in healthcare.”44 Sigurdson et al45 summarized provider and family experiences with unequal NICU care and characterized them as neglectful, judgmental, or systems based, targeting families rather than infants. Research is needed to establish the effects of individual or institutional attitudes and behaviors on clinical outcomes. Additionally, the role of nursing cannot be overlooked. Previous research from Vermont Oxford Network has found that nurse-patient ratios and worse nursing work environments,46 higher rates of missed nursing care,47 and recognition for nursing excellence48 play roles in disparities in care.
A further factor that must be considered is the effect of state policies on access and referral patterns for pregnant women and their infants. Approximately 15% of the infants in this analysis required transport to a hospital that could take care of them, but not every state has policies supporting financial reimbursement for neonatal or maternal transport.49 Further, states have widely inconsistent policies on criteria for levels of NICU care, a barrier to monitoring, regulation, and standardized care provision.50 Insufficient policies governing access to and payment for high-quality obstetric, perinatal, and neonatal care may also play a role in quality disparities by race.
Our study makes 3 contributions to the understanding of racial disparities in NICU care. First, there is segregation and inequality in NICU care for very low-birth-weight and very preterm infants, with black infants receiving care at lower-quality NICUs and Asian infants at higher-quality NICUs than white infants. Second, NICU quality varies markedly across regions but does not fully explain the racial disparities in care. Third, 2 new indices, the NICU segregation index and NICU inequality index, may have value in future studies of segregation and inequality within cities, states, regions, and health care markets.
Strengths and Limitations
The strength of our study is the use of a large national data set including nearly 90% of very low-birth-weight and very preterm infants born each year in the United States. A limitation is the classification of race and ethnicity based on abstractors’ identification of maternal race and ethnicity. The possibility of misclassification cannot be excluded. Because race is a social construct contingent on history,51 not an inherent biological characteristic, all studies of race, ethnicity, and health will be subject to this limitation to some extent, regardless of whether they rely on vital records, medical records, or personal interview.52 Our data did not collect information on Asian and Hispanic subethnicities, and other studies have reported significant heterogeneity in health outcomes within these subgroups.53,54,55 Other measures of NICU quality could lead to different results. Black and white infants scored differently on the process and outcome components of Baby-MONITOR.29 A NICU quality score that weighted these components differently might change the quality rankings of NICUs. Finally, there are many unmeasured factors including neighborhood of residence, insurance coverage, immigration status, hospital location and financing, and public policies, among others, that could explain our findings. These will be addressed in future studies.
Conclusions
Black, Hispanic, and Asian very low-birth-weight and very preterm infants are segregated across NICUs reflecting the uneven distribution of minority populations in the United States. Even after accounting for differences in NICU quality among geographic regions, Asian infants received care at higher-quality NICUs and black infants at lower-quality NICUs than white infants. Explaining these patterns will require understanding the effects of sociodemographic factors and public policy on hospital quality, access, and choice for minority women and their infants.
eFigure. Racial Distribution within Quintiles of Baby-MONITOR scores
eTable 1. Quintiles of Proportion of White Infants and Average Proportions of Infants Within Quintiles
eTable 2. Participating Hospitals
References
- 1.Massey DS, Denton NA. American Apartheid: Segregation and Making of the Underclass. Cambridge, MA: Harvard University Press; 1998. [Google Scholar]
- 2.Firebaugh G, Acciai F. For blacks in America, the gap in neighborhood poverty has declined faster than segregation. Proc Natl Acad Sci U S A. 2016;113(47):13372-13377. doi: 10.1073/pnas.1607220113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Firebaugh G, Farrell CR. Still large, but narrowing: the sizable decline in racial neighborhood inequality in metropolitan America, 1980-2010. Demography. 2016;53(1):139-164. doi: 10.1007/s13524-015-0447-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kozol J. Savage Inequalities: Children in America’s Schools. New York, NY: Broadway Paperbacks; 1991. [Google Scholar]
- 5.Rivkin S. Desegregation since the Coleman Report. Educ Next. 2016;16(2):28-37. [Google Scholar]
- 6.Cornely PB. Segregation and discrimination in medical care in the United States. Am J Public Health Nations Health. 1956;46(9):1074-1081. doi: 10.2105/AJPH.46.9.1074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reynolds PP; Cone Memorial Hospital . Hospitals and civil rights, 1945-1963: the case of Simkins v Moses H. Ann Intern Med. 1997;126(11):898-906. doi: 10.7326/0003-4819-126-11-199706010-00009 [DOI] [PubMed] [Google Scholar]
- 8.Smith DB. The racial segregation of hospital care revisited: Medicare discharge patterns and their implications. Am J Public Health. 1998;88(3):461-463. doi: 10.2105/AJPH.88.3.461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hebert PL, Chassin MR, Howell EA. The contribution of geography to black/white differences in the use of low neonatal mortality hospitals in New York City. Med Care. 2011;49(2):200-206. doi: 10.1097/MLR.0b013e3182019144 [DOI] [PubMed] [Google Scholar]
- 10.Jha AK, Orav EJ, Epstein AM. Low-quality, high-cost hospitals, mainly in south, care for sharply higher shares of elderly black, Hispanic, and Medicaid patients. Health Aff (Millwood). 2011;30(10):1904-1911. doi: 10.1377/hlthaff.2011.0027 [DOI] [PubMed] [Google Scholar]
- 11.Dimick J, Ruhter J, Sarrazin MV, Birkmeyer JD. Black patients more likely than whites to undergo surgery at low-quality hospitals in segregated regions. Health Aff (Millwood). 2013;32(6):1046-1053. doi: 10.1377/hlthaff.2011.1365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gee GC, Ford CL. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8(1):115-132. doi: 10.1017/S1742058X11000130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hardeman RR, Medina EM, Kozhimannil KB. Structural racism and supporting black lives: the role of health professionals. N Engl J Med. 2016;375(22):2113-2115. doi: 10.1056/NEJMp1609535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453-1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 15.Rothstein R. The Color of Law. New York, NY: Liveright; 2017. [Google Scholar]
- 16.Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31:178-194. doi: 10.1093/epirev/mxp001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehra R, Boyd LM, Ickovics JR. Racial residential segregation and adverse birth outcomes: a systematic review and meta-analysis. Soc Sci Med. 2017;191:237-250. doi: 10.1016/j.socscimed.2017.09.018 [DOI] [PubMed] [Google Scholar]
- 18.Mutambudzi M, Meyer JD, Reisine S, Warren N. A review of recent literature on materialist and psychosocial models for racial and ethnic disparities in birth outcomes in the US, 2000-2014. Ethn Health. 2017;22(3):311-332. doi: 10.1080/13557858.2016.1247150 [DOI] [PubMed] [Google Scholar]
- 19.Landrine H, Corral I, Lee JGL, Efird JT, Hall MB, Bess JJ. Residential segregation and racial cancer disparities: a systematic review. J Racial Ethn Health Disparities. 2017;4(6):1195-1205. doi: 10.1007/s40615-016-0326-9 [DOI] [PubMed] [Google Scholar]
- 20.Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in morbidity and mortality rates in black, white, and Hispanic very preterm infants among New York City hospitals. JAMA Pediatr. 2018;172(3):269-277. doi: 10.1001/jamapediatrics.2017.4402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farrell CR, Firebaugh G. Is immigrant neighborhood inequality less pronounced in suburban areas? Soc Sci Res. 2016;57:161-176. doi: 10.1016/j.ssresearch.2016.01.001 [DOI] [PubMed] [Google Scholar]
- 22.Horbar JD, Edwards EM, Greenberg LT, et al. . Variation in performance of neonatal intensive care units in the United States. JAMA Pediatr. 2017;171(3):e164396. doi: 10.1001/jamapediatrics.2016.4396 [DOI] [PubMed] [Google Scholar]
- 23.Manual of Operations: Part 1: Guidelines for Database Participation. Burlington, VT: Vermont Oxford Network; 2016. [Google Scholar]
- 24.Humes KR, Jones NA, Ramierez RR. Overview of Race and Hispanic Origin: 2010. Washington, DC: US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2011. [Google Scholar]
- 25.Vermont Oxford Network Manual of Operations: Part 2: Data Definitions and Infant Data Forms. Burlington, VT: Vermont Oxford Network; 2015. [Google Scholar]
- 26.Profit J, Kowalkowski MA, Zupancic JA, et al. . Baby-MONITOR: a composite indicator of NICU quality. Pediatrics. 2014;134(1):74-82. doi: 10.1542/peds.2013-3552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Draper D, Gittoes M. Statistical analysis of performance indicators in U.K. higher education. J R Stat Soc Ser A Stat Soc. 2004;167(3):449-474. doi: 10.1111/j.1467-985X.2004.apm12.x [DOI] [Google Scholar]
- 28.dhelkey/dghrank. GitHub. https://github.com/dhelkey/dghrank. Accessed February 7, 2019.
- 29.Profit J, Gould JB, Bennett M, et al. . Racial/ethnic disparity in NICU quality of care delivery. Pediatrics. 2017;140(3):e20170918. doi: 10.1542/peds.2017-0918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Efron B. Bootstrap methods: another look at the jackknife. Ann Stat. 1979;7(1):1-26. doi: 10.1214/aos/1176344552 [DOI] [Google Scholar]
- 31.US Census Bureau Census Regions and Divisions of the United States. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed February 7, 2019.
- 32.R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 33.Logan JR, Stults B The persistence of segregation in the metropolis: new findings from the 2010 census [census brief prepared for Project US2010 2011].
- 34.Intrator J, Tannen J, Massey DS. Segregation by race and income in the United States 1970-2010. Soc Sci Res. 2016;60:45-60. doi: 10.1016/j.ssresearch.2016.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tikkanen RS, Woolhandler S, Himmelstein DU, et al. . Hospital payer and racial/ethnic mix at private academic medical centers in Boston and New York City. Int J Health Serv. 2017;47(3):460-476. doi: 10.1177/0020731416689549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barringer HR, Takeuchi DT, Xenos P. Education, occupational prestige, and income of Asian Americans. Sociol Educ. 1990;63(1):27-43. doi: 10.2307/2112895 [DOI] [Google Scholar]
- 37.Pew Research Center The Rise of Asian Americans. Washington, DC: Pew Research Center; 2012. [Google Scholar]
- 38.Chan KS, Gaskin DJ, Dinwiddie GY, McCleary R. Do diabetic patients living in racially segregated neighborhoods experience different access and quality of care? Med Care. 2012;50(8):692-699. doi: 10.1097/MLR.0b013e318254a43c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carreon DC, Baumeister SE. Health care access among Asian American subgroups: The role of residential segregation. J Immigr Minor Health. 2015;17(5):1451-1457. doi: 10.1007/s10903-014-0065-0 [DOI] [PubMed] [Google Scholar]
- 40.Caldwell JT, Ford CL, Wallace SP, Wang MC, Takahashi LM. Racial and ethnic residential segregation and access to health care in rural areas. Health Place. 2017;43:104-112. doi: 10.1016/j.healthplace.2016.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Caldwell JT, Ford CL, Wallace SP, Wang MC, Takahashi LM. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. Am J Public Health. 2016;106(8):1463-1469. doi: 10.2105/AJPH.2016.303212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Phibbs CS, Lorch SA. Choice of hospital as a source of racial/ethnic disparities in neonatal mortality and morbidity rates. JAMA Pediatr. 2018;172(3):221-223. doi: 10.1001/jamapediatrics.2017.4917 [DOI] [PubMed] [Google Scholar]
- 43.Hall WJ, Chapman MV, Lee KM, et al. . Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60-e76. doi: 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 45.Sigurdson K, Morton C, Mitchell B, Profit J. Disparities in NICU quality of care: a qualitative study of family and clinician accounts. J Perinatol. 2018;38(5):600-607. doi: 10.1038/s41372-018-0057-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lake ET, Staiger D, Horbar J, Kenny MJ, Patrick T, Rogowski JA. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv Res. 2015;50(2):374-397. doi: 10.1111/1475-6773.12225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lake ET, Staiger D, Edwards EM, Smith JG, Rogowski JA. Nursing Care Disparities in Neonatal Intensive Care Units. Health Serv Res. 2018;53(suppl 1):3007-3026. doi: 10.1111/1475-6773.12762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lake ET, Staiger D, Horbar J, et al. . Association between hospital recognition for nursing excellence and outcomes of very low-birth-weight infants. JAMA. 2012;307(16):1709-1716. doi: 10.1001/jama.2012.504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Okoroh EM, Kroelinger CD, Lasswell SM, Goodman DA, Williams AM, Barfield WD. United States and territory policies supporting maternal and neonatal transfer: review of transport and reimbursement. J Perinatol. 2016;36(1):30-34. doi: 10.1038/jp.2015.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kroelinger CD, Okoroh EM, Goodman DA, Lasswell SM, Barfield WD. Comparison of state risk-appropriate neonatal care policies with the 2012 AAP policy statement. J Perinatol. 2018;38(4):411-420. doi: 10.1038/s41372-017-0006-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bobo LD, Fox C. Race, racism, and discrimination: Bridging problems, methods, and theory in social psychological research. Soc Psychol Q. 2003;66(4):319-332. doi: 10.2307/1519832 [DOI] [Google Scholar]
- 52.Roberts D. Fatal Invention: How Science, Politics, and Big Business Re-create Race in the Twenty-First Century. New York, NY: The New Press; 2011. [Google Scholar]
- 53.Baker LC, Afendulis CC, Chandra A, McConville S, Phibbs CS, Fuentes-Afflick E. Differences in neonatal mortality among whites and Asian American subgroups: evidence from California. Arch Pediatr Adolesc Med. 2007;161(1):69-76. doi: 10.1001/archpedi.161.1.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rossen LM, Schoendorf KC. Trends in racial and ethnic disparities in infant mortality rates in the United States, 1989-2006. Am J Public Health. 2014;104(8):1549-1556. doi: 10.2105/AJPH.2013.301272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rice WS, Goldfarb SS, Brisendine AE, Burrows S, Wingate MS. Disparities in infant mortality by race among Hispanic and non-Hispanic infants. Matern Child Health J. 2017;21(7):1581-1588. doi: 10.1007/s10995-017-2290-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Racial Distribution within Quintiles of Baby-MONITOR scores
eTable 1. Quintiles of Proportion of White Infants and Average Proportions of Infants Within Quintiles
eTable 2. Participating Hospitals