Abstract
Background:
We conducted a cluster-randomized study to determine the effect of an exportable educational intervention for young women with breast cancer (YWI) to improve care.
Methods:
Sites were randomized 1:1 to YWI or a contact-time control physical activity intervention (PAI) stratified by academic or community site; up to 15 women age ≤45 with newly diagnosed breast cancer were enrolled at each of 14 academic sites, 10 at 40 community sites. The primary endpoint, attention to fertility, was ascertained by medical record review. Statistical inferences on the effect of the intervention used general estimating equations for clustered data.
Results:
467 patients across 54 sites enrolled between 7/2012–12/2013. Median age at diagnosis was 40 years (range 22–45). Attention to fertility by 3 months was observed in 55% of YWI and 58% of PAI patients (p=0.88). Rates were strongly correlated with age (p<0.0001), and highest in patients <30 years old. Attention to genetics was similar (80% YWI, 81% PAI); attention to emotional health was higher in YWI patients (87% vs. 76%, estimated odds ratio, 2.63 [95%CI 1.20–5.76, p=0.016]). Patients rated both interventions as valuable in educating them (64% YWI, 63% PAI).
Conclusions:
This study failed to show differences in attention to fertility with an intervention to improve care for women with breast cancer, although attention to fertility was higher than expected in both groups and emotional health was improved with the YWI group. Greater attention to young women with breast cancer in general may promote more comprehensive care for this population.
Keywords: breast cancer, oncology, young women, fertility, exercise, psychosocial distress, patient communication
PRECIS
A multicenter educational and supportive care intervention for young women with breast cancer at community and academic practices across the U.S. did not improve rates of attention to fertility. However, patients and providers reported that the intervention educated them and improved care.
Trial registration:
Background
Each year, approximately 11% of women diagnosed with breast cancer in the United States are 45 years of age or younger.1 These women have issues unique to or accentuated by their age, including fertility-related concerns, and have higher rates of psychosocial distress than women diagnosed at older ages.2, 3 Current guidelines recommend that fertility risks and concerns be considered in all treatment plans for young women.4 However, in practice, risks to fertility and preservation options may not be discussed or, if addressed, may be addressed inadequately.5–8 Several factors may impair attention to fertility: providers may be uncomfortable discussing loss of fertility or may simply forget that this could be an important topic for the patient; providers may lack knowledge about this topic or feel like they do not have the time to adequately assist patients in making fertility-related decisions. Additionally, patients may not be aware or feel empowered to address the issue, or feel overwhelmed.9, 10
Attention to fertility may also be a proxy for other issues relevant to younger women with breast cancer, including genetic risks, psychosocial distress, and body image and sexual functioning. In 2010, the American Society of Clinical Oncology (ASCO) Quality Oncology Practice Initiative (QOPI) Network audit data determined that documentation of attention to fertility among women of childbearing age with cancer was less than 30% among the majority of audited practices and the rate was 0% in more than 50% of the practices (Personal communication, unpublished data obtained by communication with ASCO staff, 2010). High quality care for young women with breast cancer includes discussing these issues in a systematic and consistent manner, both at diagnosis and in follow-up.
Based on our prior experience of designing a unique in-clinic program for young women with breast cancer,11, 12 we developed and piloted “Young & Strong,” an exportable print and web-based educational and supportive care intervention designed for young women with newly diagnosed, early breast cancer and their providers to address issues salient to this population (e.g., genetics, body image, child care, fertility, education and career issues).13 We sought to test this intervention in the Young and Strong study to 1) increase attention to fertility as an important surrogate for other issues facing young women; and 2) educate and support young women and their providers.
Methods
Study design:
The Young & Strong study was a multi-site, two-arm, cluster randomized clinical trial with the practice site being the unit of randomization (see Figure 1). The study compared a young women’s intervention (YWI) arm to a contact-time, physical activity intervention (PAI) arm. Employing a contact-time comparison intervention ensures that study results are not a function of time and attention given to patients due to their involvement in the study. While a control condition of no intervention was considered, the contact-time comparison (otherwise known as “attention” control) method is commonly used in behavioral studies. While it poses challenges of the control intervention effecting outcomes and the difficulty of developing an “inactive” behavioral control arm that is credible and equally preferable to patients, it entails a compromise in which study conditions in the control group are sufficient to retain subjects while not being so involved that it significantly changes participant behavior.14
Figure 1:
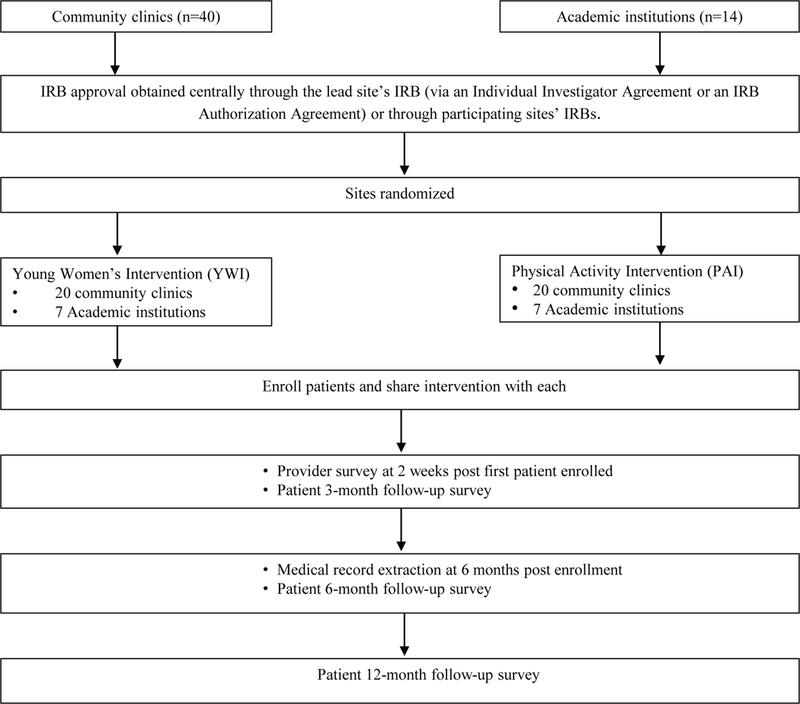
Consort flow diagram of the Young & Strong study
To reach a variety of patients, we implemented the study in both academic institutions and community sites across the United States recruited by advertising to the ASCO QOPI Network and by word of mouth. Sites were asked to commit to approaching all consecutive eligible patients to enroll in the study at that site with a goal of recruiting 10 women at each community site and 15 at each academic site. Patient eligibility included women age 18–45 years at diagnosis with newly diagnosed (within 3 months) stage I-III invasive BC without known recurrence/metastatic disease. Eligible participants had to have had their first appointment with a medical oncologist after the site opened to enrollment and be able to read and write in English.
IRB approval was obtained at Dana-Farber/Harvard Cancer Center (DF/HCC) and then by participating sites or through institutional agreements with DF/HCC. Patient participants signed informed consent for study participation prior to enrollment. Oversight was provided by the Dana-Farber/Harvard Cancer Center Data and Safety Monitoring Board (DF/HCC DSMB), which reviewed the study progress, participant safety, and data collection twice yearly.
Intervention:
After consenting and completing the baseline survey, site coordinators gave the patients an arm-specific booklet (YWI or PAI, depending on site randomization) with accompanying introductory letter, baseline/follow-up doctor visit checklists to encourage discussion with their oncologists, as well as access to an arm-specific website that encompassed all of the information in the booklet plus additional information and resources related to the YWI or PAI content depending on site randomization allocation, including videos and downloadable PDFs.13 (See Supplementary Materials) Intervention materials for oncologists, shared at site initiation, included an introductory letter broadly outlining the study goals, procedures, their role, the arm-specific patient materials, clinical checklists which paralleled the patient checklists, and access to the website, with a special tab only accessible to clinicians including videos and information tailored to them. Provider information was also arm-speciifc, YWI or PAI content focused. The study also provided site oncologists with email access to medical experts at the lead institution for consultation as needed.
Main Outcome Measures:
The primary study outcome, attention to fertility within three months of the initial appointment, was assessed by medical record review. Patients and site providers were not directly informed of the primary outcome: the informed consent document and materials for patients in both arms emphasized that this program was designed to improve patient care as did provider materials. However, providers in both arms were encouraged to document their conversations particularly related to the intervention issues and the IRB-protocol did detail the statistics and primary aims of the study (supplemental material). Medical record extractors were blinded to which intervention arm the site was randomized, and each outcome was double coded. If there was discordance between coders, a third extractor was brought in to adjudicate. Attention to fertility was defined as documentation of at least one of the following: 1) patient’s future childbearing plans or desire for future fertility; 2) receipt of fertility preservation treatments following diagnosis; 3) provider’s attempt to raise the patient’s awareness to the potential interruption/loss of fertility as a consequence of treatment (e.g., discussion of fertility preservation options and/or recommending or initiating a referral to a fertility specialist); 4) evidence of discussion that addressing fertility was not needed (i.e., post-menopausal status or bilateral oophorectomy at baseline), in which case the provider was credited for attention to fertility. Secondary outcomes including attention to genetic issues and psychosocial concerns (e.g., noting emotional health, distress, referral for psychosocial support etc.) as documented in the medical record were also assessed.
Participants also completed baseline, 3, 6, and 12-month surveys via a HIPAA compliant website or by telephone, with participants choosing their preferred modality; respondents were provided a gift card after they completed each follow-up survey ($10 at 3 months, $15 at six months, and $20 at 12 months post-enrollment). At 3 months, patient satisfaction with the intervention was assessed, as was whether patients found the intervention to be valuable, improved care, improved communication and provided educational information.
Providers were asked to complete one five-minute survey, approximately two weeks after his/her first patient enrolled on the study about their views about the YWI or PAI (arm specific). Each participating site received $200 for each enrolled study participant to help cover administrative costs.
Statistical Design:
Participating sites were randomized 1:1 to YWI or PAI using permuted blocks within stratum defined by practice type (community versus academic). Community sites were to enroll 10 participants, and academic sites were to enroll 15 participants to the study. Site number was chosen to detect an expected difference in attention to fertility at three months based on the 2009 data from the 2010 Quality Oncology Practice Initiative Network audit (Personal communition, unpublished data obtained by communication with ASCO staff and Charles Shapiro, 2018). We anticipated that among study participants seen at sites assigned to PAI, the attention to fertility rate at three months would be 10% and the rate among the YWI arm would be at least 40%. The sample size was selected to give adequate power for a range of true, but unknown, levels of within-practice correlation (ρ) in attention among participants. With seven practices per arm from large academic sites and twenty practices per arm from small community sites (total of 54 sites, minimum of 410 participants), there would be 80% power to detect a difference of 28% when within-practice correlation of ρ = 0.50 and 90% power to detect the same difference if ρ = 0.30.15
The primary analysis to compare the attention to fertility between the YWI and PAI arms used general estimating equations (GEE) to evaluate binomial proportions with clustered data.16 GEE models included as a covariate the site-level stratum of practice type. Parameter estimates are reported as odds ratios (OR) with 95% confidence intervals (CI) derived from the robust standard error. Exploratory analysis included additional patient-level factors as covariates and interaction terms in the GEE models. Similar analyses were performed for contrasting the within arm rates of secondary outcomes ascertained by medical record review. All analyses were conducted in the intent-to-treat (ITT) population, defined as all subjects who provided informed consent, according to the randomized assignment of the site. The relationship between attention ascertained by medical record and patient-recorded assessment of the YWI intervention was explored using Fisher exact tests. All inferences used a two-sided alpha = 0.05 to determine statistical significance. Statistical analyses were performed in R version 3.1.1 using the geepack package or general estimating equations.17
Results
A total of 467 women across 54 sites (40 community, 14 academic) were enrolled from July 2012 to December 2013. Community sites enrolled a total of 280 patients (range 1–10, median of 9 and 7 patients per sites on YWI and PAI arms, respectively) and academic sites enrolled 187 patients (range 1–15, all YWI sites enrolled 15 patients, PAI sites enrolled a median of 14 patients), such that 245 and 222 patients are included in the YWI and PAI arms, respectively.
Patient characteristics did not vary by study arm (Table 1). Patient mean age was 38.7 years at enrollment (range 22–45). The majority of women were married (80%) and white (77%), and 12% of the study population was African American. Women reported a range of income levels and education, though a substantial proportion in both study arms were college educated. Two patients (PAI arm) withdrew consent for medical record release and were removed from analysis of primary and secondary outcomes.
TABLE 1.
Demographics of the Study Population by Intervention Arm
| Characteristic | PAI N = 222 |
YWI N = 245 |
Total N = 467 |
Pa | |
|---|---|---|---|---|---|
| Age, y | Mean (SD) | 38.6 (5.4) | 38.8 (4.9) | 38.7 (5.1) | .874 |
| Range | 22−45 | 22−45 | 22−45 | ||
| Married/living with partner, no. | Yes | 178 (80%) | 193 (79%) | 371 (80%) | .732 |
| No | 44 (20%) | 52 (21%) | 96 (21%) | ||
| Hispanic/Latina ethnicity | Yes | 10 (5%) | 20 (8%) | 30 (6%) | .131 |
| No | 212 (95%) | 225 (92%) | 437 (94%) | ||
| Race | White | 173 (78%) | 186 (76%) | 359 (77%) | .805 |
| African American | 25 (11%) | 32 (13%) | 57 (12%) | ||
| Asian | 10 (5%) | 10 (4%) | 20 (4%) | ||
| Native American | 0 (0%) | 1 (<1%) | 1 (<1%) | ||
| Multiracial | 10 (5%) | 8 (3%) | 18 (4%) | ||
| Other | 3 (1%) | 7 (3%) | 10 (2%) | ||
| No response | 1 (<1%) | 1 (<1%) | 2 (<1%) | ||
| Income | <$25,000 | 20 (9%) | 36 (15%) | 56 (12%) | .184 |
| $25,000−$49,999 | 37 (17%) | 37 (15%) | 74 (16%) | ||
| $50,000−$99,999 | 66 (30%) | 73 (30%) | 139 (30%) | ||
| ≥$100,000 | 79 (36%) | 84 (34%) | 163 (35%) | ||
| Do not know | 2 (1%) | 5 (2%) | 7 (2%) | ||
| No response | 18 (8%) | 10 (4%) | 28 (6%) | ||
| Education | Did not graduate from high school | 3 (1%) | 8 (3%) | 11 (2%) | .076 |
| High school graduate/GED | 32 (14%) | 21 (9%) | 53 (11%) | ||
| Some college or 2-y degree | 57 (26%) | 78 (32%) | 135 (29%) | ||
| ≥4−y college degree | 130 (59%) | 138 (56%) | 268 (57%) | ||
| Stage of disease | I | 80 (36%) | 81 (33%) | 161 (34%) | .80 |
| IIA | 66 (30%) | 76 (31%) | 142 (30%) | ||
| IIB | 43 (19%) | 46 (19%) | 89 (19%) | ||
| IIIA | 18 (8%) | 23 (9%) | 41 (9%) | ||
| IIIB | 4 (2%) | 7 (3%) | 11 (2%) | ||
| IIIC | 9 (4%) | 9 (4%) | 18 (4%) | ||
| IV | 0 (0%) | 3 (1%) | 3 (1%) | ||
| Missing data | 2 (1%) | 0 (0%) | 2 (<1%) |
Abbreviations: GED, General Education Development; PAI, physical activity intervention; SD, standard deviation; YWI, young women’s intervention.
P value was derived from a 2−sided Fisher exact test.
For the primary outcome, attention to fertility within 3 months of the initial appointment, rates in both arms exceeded what was anticipated. Attention was recorded in 135 of 245 (55%) YWI patients and in 128 of 220 (58%) PAI patients (Table 2). No significant difference was detected between arms (OR = 0.96, 95% CI: 0.56–1.64, p = 0.88), and the estimated within-practice correlation was 0.13 (s.e. 0.037). We also evaluated whether attention to fertility occurred after 3 months through medical record review: only 8 additional participants were observed to have subsequent attention to fertility. Inclusion of these data did not impact intervention outcomes, indicating that first attention to fertility was predominantly identified within 3 months of the initial visit. Attention to fertility was strongly correlated with age (p < 0.0001), and was highest in patients <30 years old at diagnosis (100% YWI, 94% PAI) compared to women 30–40 years old (68% YWI, 59% PAI) and women age 40–45 years old (42% YWI, 52% PAI). An interaction test between age and the effect of the intervention did not reach statistical significance (p = 0.12). Attention to fertility was highest in patients with stage III/IV disease (62% YWI, 74% PAI) but an interaction test with the effect of the intervention did not reach statistical significance (p = 0.52).
TABLE 2.
Overall Rates of Attention to Fertility and Secondary Endpoints by Intervention Arm
| PAI N = 220a |
YWI N = 245 |
Total N = 465a |
|
|---|---|---|---|
| Overall attention to fertility, no. (%) | |||
| Within 3 mo | 128 (58%) | 135 (55%) | 263 (57%) |
| Between 3−6 mo | 2 (1%) | 4 (2%) | 6 (1%) |
| >6 mo | 1 (<1%) | 1 (<1%) | 2 (<1%) |
| Within stratum by practice type | |||
| Academic sites | 48/80 (60%) | 54/105 (51%) | 102/185 (55%) |
| Community sites | 80/140 (57%) | 81/140 (58%) | 161/280 (58%) |
| Within subgroups by age | |||
| <30 y | 17/18 (94%) | 9/9 (100%) | 26/27 (96%) |
| 30 to <35 y | 18/28 (64%) | 31/40 (78%) | 49/68 (72%) |
| 35 to <40 y | 33/58 (57%) | 39/63 (62%) | 72/121 (60%) |
| 40−45 y | 60/116 (52%) | 56/133 (42%) | 116/249 (47%) |
| Overall attention to genetic issues | 178 (81%) | 195 (80%) | 373 (80%) |
| Overall attention to emotional health | 168 (76%) | 214 (87%) | 382 (82%) |
Abbreviations: PAI, physical activity intervention; YWI, young women’s intervention.
Two participants withdrew consent for medical record review and were excluded from the primary analysis.
For the secondary outcome of attention to genetic issues, rates were high in both arms, with attention recorded in 80% of YWI patients and in 81% PAI patients (Table 2). Rates of attention to emotional health were also generally high, but more attention was reported in YWI patients (87%) as compared to PAI patients (76%), with an estimated OR of 2.63 (95% CI 1.20 – 5.76, p = 0.016).
Three months after study enrollment, patients in the YWI arm were surveyed about their attitude toward the intervention (Table 3). The majority of patients rated the intervention as valuable in educating them (53%). However there was no association between perceived value of the intervention and the primary outcome of attention to fertility in the medical record. Similarly, 67% of patients were satisfied with the intervention, but this did not correlate with attention to fertility. Finally, the majority of patients in the YWI arm agreed that the intervention provided education (56%) but only 14% felt it improved communication; 25% agreed it improved care. In contrast, among providers (response rate 145/171, 85%), most reported that both interventions educated providers (55% YWI; 51% PAI) and patients (79% YWI, 77% PAI), and improved care (79% YWI, 60% PAI).
TABLE 3.
Patient-Reported Responses to the YWI at 3 Months Versus Attention to Fertility at 3 Months as Ascertained From Medical Record Review
| Patient-Reported Response |
Attention to Fertility N = 135 |
No Attention to Fertility N = 110 |
Total on YWI N = 245 |
|
|---|---|---|---|---|
| Value, no. (%) | Low | 44 (33%) | 41 (37%) | 85 (35%) |
| High | 71 (53%) | 59 (54%) | 130 (53%) | |
| Missing data | 20 (15%) | 10 (9%) | 30 (12%) | |
| Satisfaction, no. (%) | Low | 25 (19%) | 23 (21%) | 48 (20%) |
| High | 87 (64%) | 77 (70%) | 164 (67%) | |
| Missing data | 23 (17%) | 10 (9%) | 33 (14%) | |
| Improve care, no. (%) | Disagree | 15 (11%) | 13 (12%) | 28 (11%) |
| Neither | 69 (51%) | 58 (53%) | 127 (52%) | |
| Agree | 32 (24%) | 27 (25%) | 59 (24%) | |
| Missing data | 19 (14%) | 12 (11%) | 31 (13%) | |
| Improve communication, no. (%) | Yes | 21 (16%) | 12 (11%) | 33 (14%) |
| No | 39 (29%) | 33 (30%) | 72 (29%) | |
| Unsure | 57 (42%) | 54 (49%) | 111 (45%) | |
| Missing data | 18 (13%) | 11 (10%) | 29 (12%) | |
| Educated, no. (%) | Disagree | 19 (14%) | 8 (7%) | 27 (11%) |
| Neither | 26 (19%) | 24 (22%) | 50 (20%) | |
| Agree | 70 (52%) | 67 (61%) | 137 (56%) | |
| Missing data | 20 (15%) | 11 (10%) | 31 (13%) |
Abbreviation: YWI, young women’s intervention.
Discussion
Young women with breast cancer have unique issues with which they must contend at diagnosis through survivorship; additional support and education would seem essential to addressing their concerns. However, compared to a contact-time control intervention, an exportable educational and supportive care intervention focused on issues facing young women and their oncologists did not result in a greater attention to fertility, an issue of great import to young survivors. Importantly, attention to fertility was much higher than expected in both intervention arms, especially in women <30. Prior U.S. data used to inform this research had suggested very low rates of attention among young adult women (Personal communication, unpublished data obtained by communication with ASCO staff, 2010). More recent QOPI data has revealed an increase from 2009 to 2014 of documented discussion of fertility and referral for fertility preservation of young patients yet rates of have remained relatively low with with only 35% and 23% of medical records revealing documentation of discussion and referrals, respectively (Personal communication, unpublished data obtained by communication with ASCO staff and Charles Shapiro, 2018).
Other literature has also suggested an increase, though still relatively limited attention to fertility. Among female survivors surveyed as part of a cohort of adolescent and young adult (AYA) survivors identified through a SEER linkage, fewer than half said that strategies to preserve their fertility were discussed prior to starting treatment.18 Other recent reports have found similarly low rates of attention to fertility, although some have found rates as high as 85%.19–22 The study finding the highest rate of attention included only patients seen at NCI-designated comprehensive cancer centers, although our study did not see a difference in attention to fertility between community and academic sites.21
In a representative Swedish population-based study of survivors, diagnosed between the ages of 18–40 (during 2003–2007), 48% reported that they received information about treatment impact on fertility, and 14% reported that they received information about fertility preservation.23 These collective findings could be due to increased awareness of this issue among providers as well as the public. Our findings may also reflect the use a contact time control intervention that provided potentially valuable content and likely focused attention on young women’s issues more than would have occurred in standard care. A study that focused on young women, regardless of intervention content, has the potential to induce a Hawthorne effect, changing the behavior of oncologists and patients, regardless of intervention conditions.24 Importantly, while only the general goals of the study, to improve care for young women with breast cancer, were described in the provider and patient materials, providers were instructed to document their conversations with patients regarding the intervention content in particular and the IRB approved protocol required inclusion of the primary outcome and statistical plan thus it is likely that some of the providers at PAI sites would have been more aware and likely to document fertility discussions.
It is also possible that the sites which signed up to be a part of the study, and patients seen at these practices are not representative. A practice that was able to engage and implement a supportive care study like ours may already deliver comprehensive care in general or they may not see populations of patients who are at high risk for gaps in care, thus their patients would not significantly benefit from such an intervention. The stark difference in our findings compared to those of prior QOPI audits may also reflect differences in what was defined as attention to fertility. On a patient level, while our participation rate was high and our sample relatively diverse both racial/ethnically and geographically, our findings may not be generalizable to all young women with breast cancer and it is likely that women who did not participate may be from more disparate populations in breast cancer care.
Future supportive care research may want to use a risk stratified approach to selecting patients, in order to identify and intervene on those who are most vulnerable to disparities in care and outcomes. The possibility that there were challenges with regard to implementation of this intervention study can also not be excluded. While rigorous and systematic attention was paid to its implementation at sites by the study team, including regular check-ins, fidelity to the intervention as designed was not guaranteed at each practice.
The study also had limited power to detect an age-dependent effect although the youngest women (age ≤ 40 years), for whom fertility would have been most relevant, at sites randomized to the YWI experienced greater attention to fertility numerically when compared to those seen at a PAI site. Future work focused on attention to fertility should specifically target this younger age group, although older women may still be interested in future fertility especially if they have not yet had children, and their concerns in this regard should also be attended.22, 25
Our findings showed that attention to genetics was high in both groups. However, additional attention to psychosocial concerns appeared to be documented more frequently among women at YWI sites. It is possible that the YWI, with content aimed at helping women and their providers recognize the need for, communicate about and get additional emotional support after a diagnosis of breast cancer, prompted more discussion and support around these issues. Evaluation of the effect of both interventions on additional important secondary outcomes, including physical activity, is ongoing to determine whether either intervention yielded differential attention to that salient content.
We believe that this is the first study to prospectively determine the rates of discussion of important care topics between patients and providers while simultaneously intending to increase attention to them. This study is also further distinguished by the expansive reach into a variety of clinics across the country. While the YWI failed to impact on the primary study outcome, given the finding that both patients and providers valued the interventions and reported an increase in education in important, and sometimes unaddressed topics, this work may serve as a novel model to implement programmatic improvements in quality of care in general, and increase education and support to vulnerable patient groups. Future research to evaluate and tailor this intervention to meet the needs of women in a more diverse population is warranted.
Supplementary Material
Acknowledgements
This work was supported by an ASCO Cancer Foundation/Susan G. Komen Improving Cancer Care Grant (PI: Partridge) and by NIH 5K05 CA124415–05 (PI: K. Emmons). Study-related materials were developed in partnership with the DF/HCC Health Communication Core, Boston, MA. We would like to thank all the women who participated in the focus groups, key informant interviews, and in the Young & Strong pilot and parent study as well as the oncologists, providers, site coordinators, and other study staff at the sites.
We would like to thank all the women who participated in the focus groups, key informant interviews, pilot study and this randomized controlled trial, as well as 54 provider site teams who enrolled their patients.
Funding Sources: This work was supported by an ASCO Improving Cancer Care grant (PI: Partridge), Susan G. Komen (PI: Partridge) and by NIH 5K05 CA124415–05 (PI: Emmons).
Footnotes
Disclosures: None
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66: 7–30. [DOI] [PubMed] [Google Scholar]
- 2.Rosenberg SM, Newman LA, Partridge AH. Breast Cancer in Young Women: Rare Disease or Public Health Problem? JAMA Oncol. 2015;1: 877–878. [DOI] [PubMed] [Google Scholar]
- 3.Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104: 386–405. [DOI] [PubMed] [Google Scholar]
- 4.Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24: 2917–2931. [DOI] [PubMed] [Google Scholar]
- 5.Duffy CM, Allen SM, Clark MA. Discussions regarding reproductive health for young women with breast cancer undergoing chemotherapy. J Clin Oncol. 2005;23: 766–773. [DOI] [PubMed] [Google Scholar]
- 6.Gorman JR, Bailey S, Pierce JP, Su HI. How do you feel about fertility and parenthood? The voices of young female cancer survivors. J Cancer Surviv. 2012;6: 200–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruddy KJ, Gelber S, Ginsburg ES, et al. Menopausal symptoms and fertility concerns in premenopausal breast cancer survivors: a comparison to age- and gravidity-matched controls. Menopause. 2011;18: 105–108. [DOI] [PubMed] [Google Scholar]
- 8.Zebrack BJ, Casillas J, Nohr L, Adams H, Zeltzer LK. Fertility issues for young adult survivors of childhood cancer. Psychooncology. 2004;13: 689–699. [DOI] [PubMed] [Google Scholar]
- 9.Quinn GP, Vadaparampil ST, King L, et al. Impact of physicians’ personal discomfort and patient prognosis on discussion of fertility preservation with young cancer patients. Patient Educ Couns. 2009. [DOI] [PubMed] [Google Scholar]
- 10.Goldfarb SB, Dickler MN, McCabe MS, et al. Oncology physician’s knowledge, attitudes, and practices regarding fertility preservation. Journal of Clinical Oncology. 2010;28. [Google Scholar]
- 11.Partridge AH, Ruddy KJ, Kennedy J, Winer EP. Model program to improve care for a unique cancer population: young women with breast cancer. J Oncol Pract. 2012;8: e105–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ruddy KJ, Greaney ML, Sprunck-Harrild K, Meyer ME, Emmons KM, Partridge AH. Young Women with Breast Cancer: A Focus Group Study of Unmet Needs. J Adolesc Young Adult Oncol. 2013;2: 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greaney ML, Sprunck-Harrild K, Ruddy KJ, et al. Study protocol for Young & Strong: a cluster randomized design to increase attention to unique issues faced by young women with newly diagnosed breast cancer. BMC Public Health. 2015;15: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Au DH, Castro M, Krishnan JA. Selection of controls in clinical trials: introduction and conference summary. Proc Am Thorac Soc. 2007;4: 567–569. [DOI] [PubMed] [Google Scholar]
- 15.Donner A, Birkett N, Buck C. Randomization by cluster. Sample size requirements and analysis. Am J Epidemiol. 1981;114: 906–914. [DOI] [PubMed] [Google Scholar]
- 16.Prentice RL, Zhao LP. Estimating equations for parameters in means and covariances of multivariate discrete and continuous responses. Biometrics. 1991;47: 825–839. [PubMed] [Google Scholar]
- 17.Halekoh U, Højsgaard S, Yan J. The R package geepack for generalized estimating equations. Journal of Statistical Software. 2006;15: 1–11. [Google Scholar]
- 18.Shnorhavorian M, Harlan LC, Smith AW, et al. Fertility preservation knowledge, counseling, and actions among adolescent and young adult patients with cancer: A population-based study. Cancer. 2015;121: 3499–3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCray DK, Simpson AB, Flyckt R, et al. Fertility in Women of Reproductive Age After Breast Cancer Treatment: Practice Patterns and Outcomes. Ann Surg Oncol. 2016;23: 3175–3181. [DOI] [PubMed] [Google Scholar]
- 20.Quinn GP, Block RG, Clayman ML, et al. If you did not document it, it did not happen: rates of documentation of discussion of infertility risk in adolescent and young adult oncology patients’ medical records. J Oncol Pract. 2015;11: 137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salsman JM, Yanez B, Smith KN, et al. Documentation of Fertility Preservation Discussions for Young Adults With Cancer: Examining Compliance With Treatment Guidelines. J Natl Compr Canc Netw. 2016;14: 301–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruddy KJ, Gelber SI, Tamimi RM, et al. Prospective study of fertility concerns and preservation strategies in young women with breast cancer. J Clin Oncol. 2014;32: 1151–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Armuand GM, Rodriguez-Wallberg KA, Wettergren L, et al. Sex differences in fertility-related information received by young adult cancer survivors. J Clin Oncol. 2012;30: 2147–2153. [DOI] [PubMed] [Google Scholar]
- 24.McCarney R, Warner J, Iliffe S, van Haselen R, Griffin M, Fisher P. The Hawthorne Effect: a randomised, controlled trial. BMC Med Res Methodol. 2007;7: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Partridge AH, Gelber S, Peppercorn J, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22: 4174–4183. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


