Supplemental Digital Content is available in the text.
Abstract
Background.
It has been suggested that hospitalized patients may get suboptimal care in nights or on weekends or summer holidays due to sleep deprivation, physician fatigue, or reduced medical staffing. Our objective was to determine whether there were differences in outcomes when surgery was performed in the night (10 pm–6 am), on weekends (Saturday or Sunday), or during summer months (June–August).
Methods.
We used United Network for Organ Sharing (UNOS) data sets of adults transplanted between February 27, 2002, and September 30, 2016. We estimated the start time of liver transplant surgery by utilizing the cross-clamp time and cold ischemia time (cross-clamp time + cold ischemia time – 2 h). The survival outcomes were estimated by Kaplan-Meier survival analysis. Patients with hepatocellular carcinoma (HCC) were analyzed separately. The independent effect of time of transplant on outcomes was analyzed after adjusting for common confounders, including Model for End-stage Liver Diseases scores and transplant center volume.
Results.
During the study period, 4 434 (9.6%) were done in the night, 12 147 (26.4%) over weekends, and 11 976 (26%) during summer months. The graft and patient survival and complications were not influenced by the time of transplant for both HCC and non-HCC population. Cox regression analysis after adjusting for risk factors, including Model for End-stage Liver Diseases, donor risk index, and liver center volume, confirmed that there were no significant differences in outcomes.
Conclusions.
Our study showed that the time of transplant surgery whether done during nights, weekends, or summer months had no effect on graft or patient survival irrespective of center volume, patient, or donor risk factors.
It has been suggested that hospitalized patients may get suboptimal care from physician during nights, weekends, or summer holidays due to sleep deprivation, fatigue, or reduced medical staffing. Many studies have shown that patients hospitalized outside regular working hours with myocardial infarction,1 pulmonary embolism,2 stroke,3 ruptured abdominal aortic aneurysm,4 heart failure,5 or gastrointestinal bleeding6 have worse outcomes, but there are few conflicting reports.7-10 Except for emergency surgical procedures, most complex surgical procedures are done electively. However, when such surgeries are performed at night, a higher incidence of serious complication rates has been reported with colorectal, laparoscopic, and orthopedic surgeries.11-15 Similarly, percutaneous coronary interventional procedures done during off hours are associated with serious adverse events, including myocardial infarction and mortality.14
Successful outcome of liver transplantation (LT) depends on the active and optimal participation of a multidisciplinary team of surgeons, anesthesiologists, nurses, and technicians. Although many LT are done semielectively, organ availability and procurement determine the start time of liver transplant surgery for a significant number of patients. The impact of nighttime or weekend surgeries on survival had been previously examined in thoracic organs and kidney transplants with discordant results.16-20 One possible explanation for this discrepancy, especially from single-center reports, could be related to differences in center experience (center volume). A large study using United Network for Organ Sharing (UNOS) data, however, showed that patient survival after heart and lung transplantations was not influenced by nighttime surgery.16 Two studies that examined nighttime renal transplantation came with different results. While the report from the United Kingdom did not see any increased complications, a German study showed significantly higher reoperation rates (16.8% vs 6.4%) and graft loss when renal transplantation was performed at night.17,18 However, 2 large studies, one from the United Kingdom and one from the United States, showed that weekend renal transplant had minimal impact on graft and patient survival.19,20 Similarly, 2 previous studies on LT reported conflicting outcomes.2,21 A single-center study that examined LT outcomes stratified by day and night showed longer operating time and greater risk of early death (hazard ratios [HR], 2.8; 95% confidence interval [CI], 1.2–7.0; P = 0.023) rates when liver transplants were done at night.22 Another study that examined outcomes based on UNOS data from 1987 to 2010 showed that both nighttime and weekend LT had no effect on posttransplant survival.21 Liver allocation by UNOS has gone through many changes in the last 16 years, including the use of Model for End-stage Liver Diseases (MELD) scores for organ allocation in 2002, implementation of share 15 Regional in 2005, share 15 National and share 35 Regional in 2013.23 Moreover, indication for LT, age, comorbidities, and severity of liver disease of LT recipients have changed over the years, and these changes could have an influence on the complexity of LT surgery.24
We hypothesized that patients who are transplanted off hours, weekends, and summer months will have a lower survival after adjusting for disease severity (MELD), donor risk factors (donor risk index [DRI]), and transplant center volume. To examine our hypothesis, we performed a retrospective cohort analysis using recent UNOS data sets from the MELD era. We compared the graft and patient survival outcomes of LT done at night and weekends with regular working hours and weekdays, respectively, after adjusting for known recipient and donor risk factors and center volume. In addition, we compared the outcomes of patients transplanted during summer months (June–August), when hospital staffing is often suboptimal, with those transplanted during other months (Fall–Spring).
PATIENTS AND METHODS
All adult patients listed for LT with the UNOS between February 27, 2002, and September 30, 2016 were included in the study (Figure 1). We excluded children (younger than 18 y old), multiple organ transplantations, and hepatocellular carcinoma (HCC). Patients with HCC were analyzed separately as they have a variable outcome. We estimated the start time of liver transplant surgery by utilizing the cross-clamp and cold ischemia times (cross-clamp time + cold ischemia time – 2 h). We stratified patients into 3 groups: LT done in the night (10 pm–6 am), on weekends (Saturday or Sunday), or during summer months (June–August). We also examined the outcomes during extended, major holiday weekends (December 23–January 1 for Christmas and day before Thanksgiving until next Sunday) when hospitals had suboptimal staffing.
FIGURE 1.
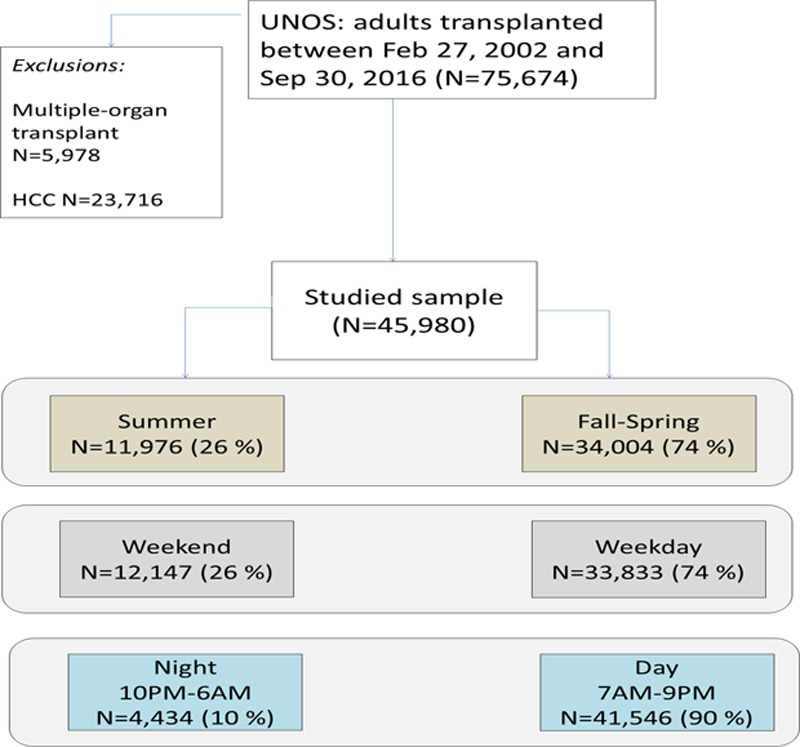
Flowchart showing patient population. HCC, hepatocellular carcinoma; UNOS, United Network for Organ Sharing.
We collected data, including age, sex, ethnicity, body mass index, serum creatinine, presence of diabetes mellitus, MELD score, presence of hepatic encephalopathy, cause of liver disease, and DRI. We calculated DRI for all patients as described by Feng et al.25 We determined complication rates that resulted in graft loss and grouped them as hepatic artery or biliary complications and primary graft nonfunction.
The study was exempt from IRB approval since deidentified data were utilized.
Statistical Methods
The baseline characteristics of patients in the 3 groups were compared using t-tests for continuous variables or Chi-squared tests for categorical variables. We used Kaplan-Meier curves to estimate a probability of graft and patient survival, and the differences between the groups were assessed by log-rank test. The strength of the associations with the risk factors, including demographic, clinical, and graft quality characteristics, was estimated via HR using Cox proportional hazard regressions. For this analysis, those variables that were significant at P ≤0.1 by univariate analysis were included in a multivariate model. The variables included in univariate analysis were age, sex, race, MELD score, presence of morbid obesity (body mass index ≥ 40) or hepatic encephalopathy, etiology of liver disease, DRI, and liver transplantation (LT) center volume stratified into 3 groups (<20, 20–50, and >50 per y). The relative risk of graft and patient failure was adjusted for the differences in distributions of the risk factors between the 3 groups and is expressed as HR with 95% CIs.
RESULTS
Demographic and Clinical Characteristics
During the study period, 75 674 adult liver transplants were performed. After excluding HCC (n = 23 716) and 5 978 with multiorgan transplants, 45 980 were available for the analysis. Of these, 11 976 (26%) were performed during summer, 12 147 (26%) during weekends, and 434 (10%) at nights (Figure 1). During Christmas and Thanksgiving weekends, 1 347 liver transplants were done. Overall 23 716 patients with HCC were transplanted during the same period; of these, 2 440 had LT surgery at night, 6 352 over weekends, and 6 332 during summer months.
There were few differences in patient characteristics between the groups as shown in Table 1. Although some of the differences were statistically significant (mainly because of the power of the study due to large sample size), the differences between the study groups were not clinically significant. Prevalence of type 2 diabetes mellitus was marginally higher in patients undergoing liver transplant at night (16.9% vs 15.5%, P = 0.02) as compared with those done during regular working hours. Dialysis (11.7% vs 10.3%, P = <0.0001) and grade 3–4 encephalopathy (16.6% vs 14.4, P = <0.0001) were more common in weekend transplants when compared with regular working hours. The most common indication for the transplant was viral hepatitis followed by alcoholic cirrhosis, nonalcoholic steatohepatitis, cryptogenic cirrhosis, primary biliary cirrhosis, and primary sclerosing cholangitis.
TABLE 1.
Clinical characteristics of the study population
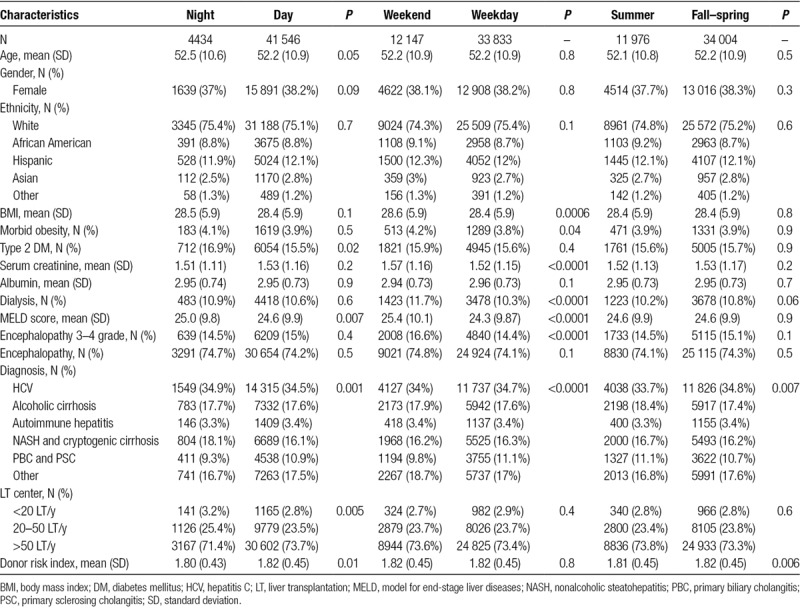
The MELD scores were marginally higher in patients who received LT at night or on a weekend. The DRI was minimally lower for nights and summer LT and similar for weekdays and weekends. While comparatively more liver transplants were done at night in transplant centers that performed either <20 or 20–50 LT/y, more transplants were done during regular working hours in transplant centers that performed >50 LT/y. Otherwise, there were no differences in the proportion of transplantation done during summer months or weekends based on transplant center volume.
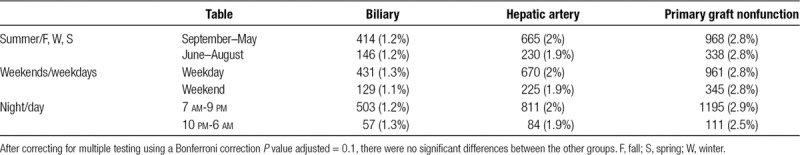
During the study period, there were 895 (2%) hepatic artery complications, 560 (1.2%) biliary complications, and 1306 (2.8%) primary graft nonfunction that resulted in graft failure. There were no differences in the above complication rates at night, on weekends, or during summer months (Table 2).
TABLE 2.
Major complications
Graft and Patient Survival Based on the Time of Transplant Surgery
The graft and patient survival rates were similar irrespective of whether surgery was done at night (Figure 2A and B), on weekends (Figures 2B and 3B), or during summer months (Figures 2C and 3C). When the above analysis was repeated for patients with MELD score 35 or more, the overall mortality rates at night (26.3% vs 27.0% during day), on weekends (26.8% vs 27.0% weekdays), and during summer months (27.2% vs 26.9% during other mo) were similar, suggesting that the survival was unaffected when liver transplant surgeries were performed at night, on weekends, or during summer months in sicker patients.
FIGURE 2.
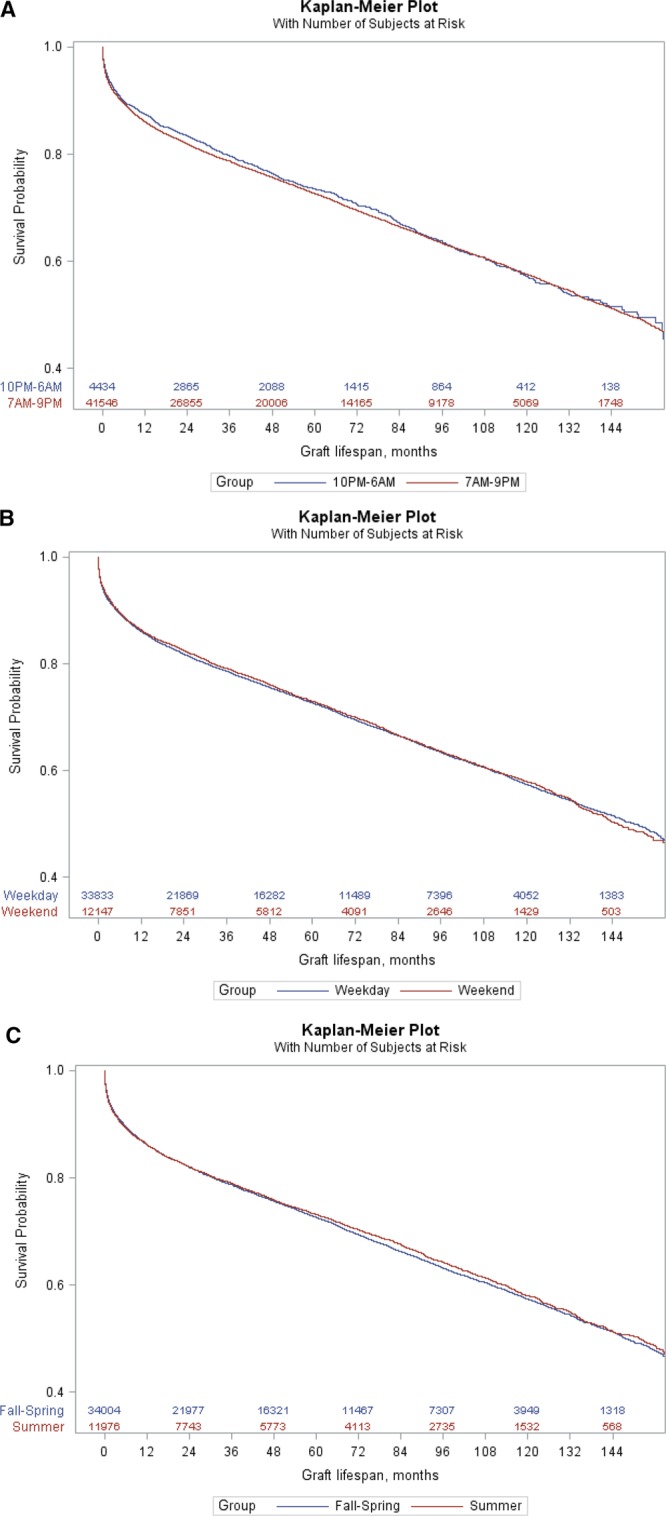
Graft survival probabilities. A, Graft survival stratified by the start time (night vs day) of the procedure (P = 0.26 using a log-rank test). B, Graft survival probability stratified by weekends and weekdays LT (P = 0.57 using a log-rank test). C, Graft survival probability stratified by LT done in summer or fall-spring (P = 0.30 using a log-rank test). LT, liver transplantation. Continued on next page.
FIGURE 3.
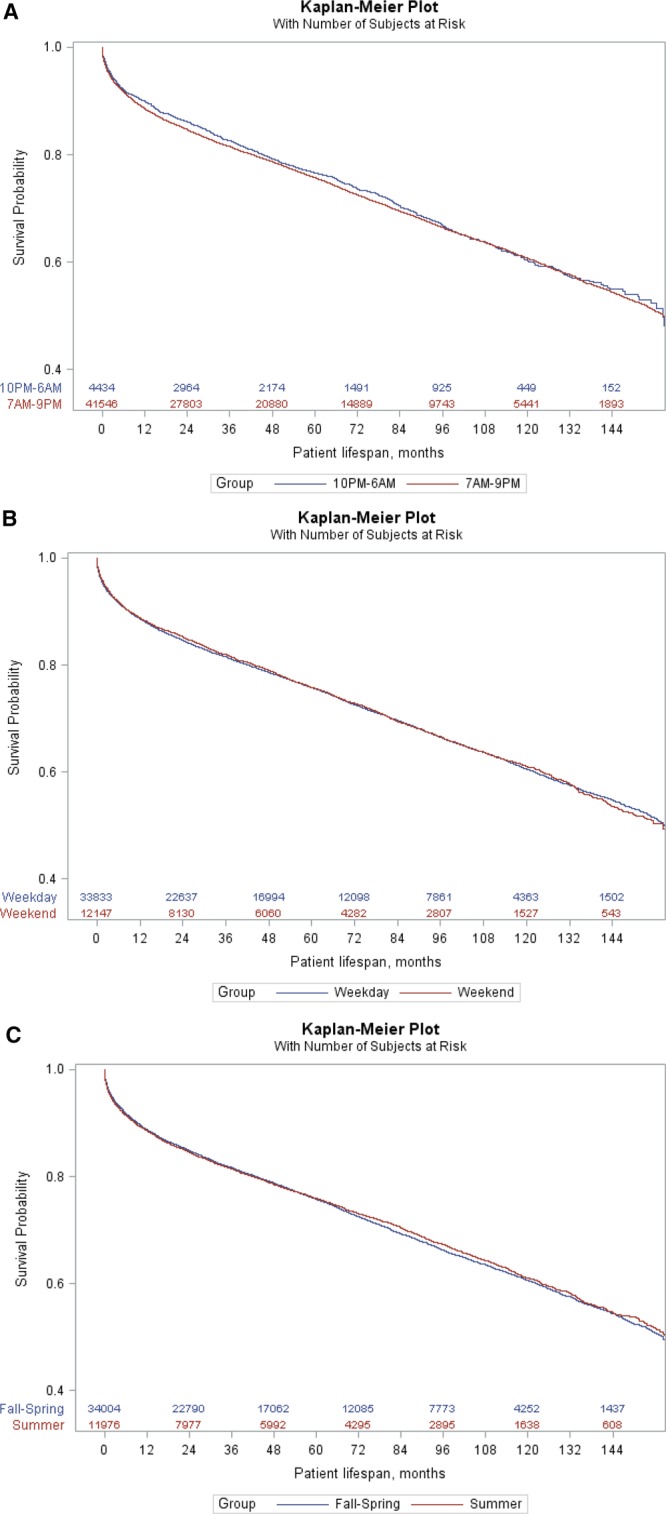
Patient survival probabilities. A, Patient survival stratified by the start time (night vs day) of the procedure (P = 0.23 using a log-rank test). B, Patient survival probability stratified by weekends and weekdays LT (P = 0.78 using a log-rank test). C, Patient survival probability stratified by LT done in summer or fall-spring (P = 0.52 using a log-rank test). LT, liver transplantation. Continued on next page.
When we combined LT surgeries done during extended Christmas or Thanksgiving weekends and compared with other weekends or weekdays, there were no differences in patient survival (Figure S1, SDC, http://links.lww.com/TXD/A206). When HCC patients were analyzed separately, there were no differences in survival when surgeries are done night, weekends, or summer months (Figure S2A–C, SDC, http://links.lww.com/TXD/A206).
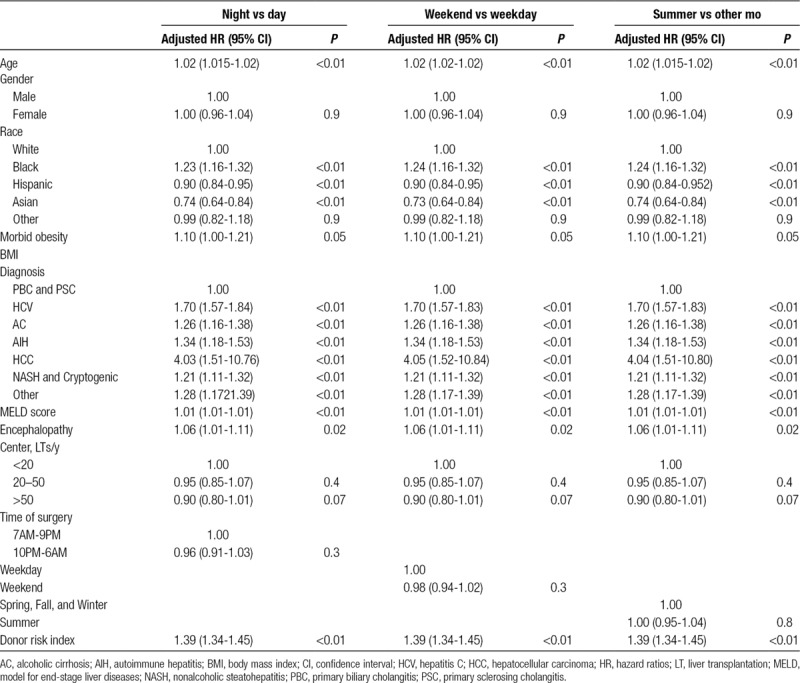
The results of Cox regression analysis (HR with 95% CIs), after adjusting for confounding variables, for graft and patient failure are shown in Tables 3 and 4. The same analysis before adjusting for risk factors is provided in Table S1 (SDC, http://links.lww.com/TXD/A206). After adjustment for confounding risk factors, including MELD score, DRI, and transplant center volume, there were no differences in survival when transplant surgeries were performed at night, on weekends, or during summer months as compared with daytime, weekdays, or nonsummer months, respectively. The adjusted HR for patient mortality was 0.96 (95% CI, 0.91-1.03; P = 0.3) for nighttime, 0.98 (95% CI, 0.98-1.02; P = 0.3) for weekend, and 1.0 (95% CI, 0.95-1.04; P = 0.8) for summer LT. The adjusted HR for graft mortality was 0.98 (95% CI, 0.93-1.04; P = 0.5) for nighttime, 0.99 (95% CI, 0.95-1.03; P = 0.6) for weekend, and 0.99 (95% CI, 0.95-1.03; P = 0.5) for summer LT, suggesting that study groups had identical outcomes.
TABLE 3.
The hazard rate ratios for the graft loss for 3 groups (night, weekend, and summer)
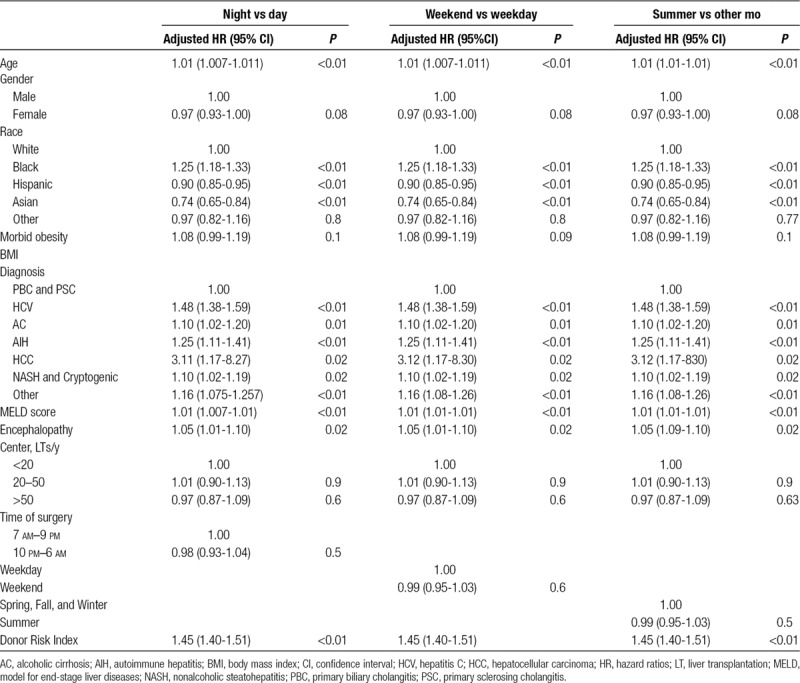
TABLE 4.
The hazard rate ratios for the patient mortality for 3 groups (night, weekend, and summer)
DISCUSSION
In this study, contrary to our hypothesis, the outcomes of liver transplant surgeries were not affected whether they were performed at night, on weekends, or during summer months. The Cox regression analysis after adjusting for known patient risk factors including MELD, DRI, and liver center volume also confirmed that there were no differences in outcomes based on the time, day, or month. There were also no differences during extended major holiday weekends. Moreover, there were no differences when data were analyzed in patients with MELD scores ≥35, suggesting that even sicker patients had the same outcomes. The results were similar for HCC and non-HCC patients. These results are very reassuring and may suggest that transplant centers, irrespective of center volume, have adequate resources throughout the year to perform surgery safely. One potential explanation for this could be that the surgical, anesthetic, and postoperative intensive care may have become very standardized and protocolized. Additionally, unlike other emergency surgical procedures, LT are almost always performed under the close supervision of a senior LT surgeon, supported by a specialized anesthetic and support staff who are experienced in working at night and on weekends.
A previous single-center study had shown increased operating time and greater risk of early death (HR, 2.8; 95% CI, 1.2-7.0; P = 0.023) when LT were performed at night.22 Although their observations were disturbing, it is more likely a center-specific effect that needs to be addressed at the center level and need not be generalized based on our observations. A previous UNOS study20 had reached similar conclusion, but we have confirmed their observations with more recent data and also after adjusting for MELD score, DRI, and center volume. There were few differences between our study and previous UNOS study.21 We analyzed data of those who were transplanted in the MELD era between 2002 and 2016, while the previous study analyzed the data from 1987 to 2010. Additionally, we examined the impact of summer months on outcome. While the previous study defined nighttime as 7 pm–7 am, we used nighttime as 10 pm–6 am. Moreover, we estimated the start time of surgery by adding cross-clamp time + cold ischemia time – 2 hours after discussing with our liver transplant surgeons whereas other studies just added cross-clamp time with cold ischemia time. Both cross-clamp time and cold ischemia time are clearly recorded in UNOS data sets. We also included DRI in our multivariate analysis. Despite these differences, we also found similar outcomes when LT were performed on weekends, and this observation is consistent with previous studies in heart, lung, kidney, and liver transplantations.16,19,20,21,23 We did not find significant differences in disease severity, donor quality, or center differences for weekend LT in our analysis, and adjusted HR was 0.98 (95% CI, 0.94-1.02; P = 0.3). To our knowledge, there have been no previous studies that have compared outcome during summer months when hospitals in the United States have less man power, but ours showed the survival is similar in summer months.
Despite a large unbiased recipient population who were transplanted more recently with more granular data on disease severity, comorbidities, and donor risk factors, our study has few limitations. In this study, we did not examine the impact of organ allocation changes over the years on the outcome for following reasons. Our study corroborated the observations made in a previous study from another era, including pre-MELD years.21 In addition, we adjusted our outcomes for recipient disease severity, DRI, and center volume, and we believe that these variables would capture any impact of organ allocation policy changes on outcomes. Another limitation of our study was that we did not know whether some of the surgeons who performed the LT were also the ones who performed the procurement, which could have an effect on surgeons’ fatigue. The weekday group in our study included public holidays when most hospitals function like weekends. Therefore, we analyzed outcomes for major holidays like Christmas and Thanksgiving separately, but our conclusions remained unchanged. Another confounder in our study could be higher organ discard rates outside regular working hours as has been shown in a previous study on kidney discard rates.26 It is also plausible that marginal organs were not considered on weekends, but the identical DRI during weekdays and weekends argues against the above possibilities. Another possibility is that centers could have prioritized sicker and more complex LT for daytime or weekday LT. The mean MELD scores, however, were higher in recipients who were transplanted at night and on weekends. Moreover, in the MELD era, transplant centers have limited ability to allot organs preferentially based on the time of the day or day of the week. Although we were not able to determine all complication rates, including reoperation rates (data not available), we did not find any differences in hepatic artery or biliary complications or primary graft nonfunction rates that resulted in graft loss between the groups.
In summary, we believe that our findings are robust enough to conclude that outcomes of LTs performed in the US hospital are unaffected when surgeries are performed at night, on weekends, and during summer months. These observations will be very reassuring for patients and their families.
Supplementary Material
Footnotes
Published online 25 April, 2019.
P.J.T. contributed to the study concept, design, analysis, and interpretation of data. P.J.T. and W.A. drafted the manuscript. Y.S. did the statistical analysis. J.L. contributed to interpretation of data and critical revision of manuscript.
The authors declare no funding or conflicts of interest.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantationdirect.com).
REFERENCES
- 1.Kostis WJ, Demissie K, Marcella SW, et al. ; Myocardial Infarction Data Acquisition System (MIDAS 10) Study Group. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356:1099. [DOI] [PubMed] [Google Scholar]
- 2.Coleman CI, Brunault RD, Saulsberry WJ. Association between weekend admission and in-hospital mortality for pulmonary embolism: an observational study and meta-analysis. Int J Cardiol. 2015;194:72. [DOI] [PubMed] [Google Scholar]
- 3.Saposnik G, Baibergenova A, Bayer N, et al. Weekends: a dangerous time for having a stroke? Stroke. 2007;38:1211. [DOI] [PubMed] [Google Scholar]
- 4.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663. [DOI] [PubMed] [Google Scholar]
- 5.Horwich TB, Hernandez AF, Liang L, et al. ; Get With Guidelines Steering Committee and Hospitals. Weekend hospital admission and discharge for heart failure: association with quality of care and clinical outcomes. Am Heart J. 2009;158:451. [DOI] [PubMed] [Google Scholar]
- 6.Peberdy MA, Ornato JP, Larkin GL, et al. ; National Registry of Cardiopulmonary Resuscitation Investigators. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299:785. [DOI] [PubMed] [Google Scholar]
- 7.Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clin Gastroenterol Hepatol. 2009;7:303. [DOI] [PubMed] [Google Scholar]
- 8.Brunot V, Landreau L, Corne P, et al. Mortality associated with night and weekend admissions to ICU with on-site intensivist coverage: results of a nine-year cohort study (2006-2014). Plos One. 2016;11:e0168548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barnett MJ, Kaboli PJ, Sirio CA, et al. Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40:530. [DOI] [PubMed] [Google Scholar]
- 10.Cortes MB, Fernandes SR, Aranha P, et al. Association between weekend and holiday admission with pneumonia and mortality in a tertiary center in Portugal: a cross-sectional study. Acta Med Port. 2017;30:361. [DOI] [PubMed] [Google Scholar]
- 11.Komen N, Dijk JW, Lalmahomed Z, et al. After-hours colorectal surgery: a risk factor for anastomotic leakage. Int J Colorectal Dis. 2009;24:789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ricci WM, Gallagher B, Brandt A, et al. Is after-hours orthopaedic surgery associated with adverse outcomes? A prospective comparative study. J Bone Joint Surg Am. 2009;91:2067. [DOI] [PubMed] [Google Scholar]
- 13.Grantcharov TP, Bardram L, Funch-Jensen P, et al. Laparoscopic performance after one night on call in a surgical department: prospective study. BMJ. 2001;323:1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glaser R, Naidu SS, Selzer F, et al. Factors associated with poorer prognosis for patients undergoing primary percutaneous coronary intervention during off-hours: biology or systems failure? JACC Cardiovasc Interv. 2008;1:681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taffinder NJ, McManus IC, Gul Y, et al. Effect of sleep deprivation on surgeons’ dexterity on laparoscopy simulator. Lancet. 1998;352:1191. [DOI] [PubMed] [Google Scholar]
- 16.George TJ, Arnaoutakis GJ, Merlo CA, et al. Association of operative time of day with outcomes after thoracic organ transplant. JAMA. 2011;305:2193. [DOI] [PubMed] [Google Scholar]
- 17.Seow YY, Alkari B, Dyer P, et al. Cold ischemia time, surgeon, time of day, and surgical complications. Transplantation. 2004;77:1386. [DOI] [PubMed] [Google Scholar]
- 18.Fechner G, Pezold C, Hauser S, et al. Kidney’s nightshift, kidney’s nightmare? Comparison of daylight and nighttime kidney transplantation: impact on complications and graft survival. Transplant Proc. 2008;40:1341. [DOI] [PubMed] [Google Scholar]
- 19.Baid-Agrawal S, Martus P, Feldman H, et al. Weekend versus weekday transplant surgery and outcomes after kidney transplantation in the USA: a retrospective national database analysis. BMJ Open. 2016;6:e010482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson BM, Mytton JL, Evison F, et al. Outcomes after weekend admission for deceased donor kidney transplantation: a population cohort study. Transplantation. 2017;101:2244. [DOI] [PubMed] [Google Scholar]
- 21.Orman ES, Hayashi PH, Dellon ES, et al. Impact of nighttime and weekend liver transplants on graft and patient outcomes. Liver Transpl. 2012;18:558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lonze BE, Parsikia A, Feyssa EL, et al. Operative start times and complications after liver transplantation. Am J Transplant. 2010;10:1842. [DOI] [PubMed] [Google Scholar]
- 23.Becker F, Vogel T, Voß T, et al. The weekend effect in liver transplantation. Plos One. 2018;13:e0198035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wedd JP, Harper AM, Biggine SW. MELD score, allocation, and distribution in the United States. Clin Liver Dis. 2013;2:148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feng S, Goodrich NP, Bragg-Gresham JL, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006;6:783. [DOI] [PubMed] [Google Scholar]
- 26.Mohan S, Foley K, Chiles MC, et al. The weekend effect alters the procurement and discard rates of deceased donor kidneys in the United States. Kidney Int. 2016;90:157. [DOI] [PMC free article] [PubMed] [Google Scholar]


