Abstract
Background
Critically ill people may lose fluid because of serious conditions, infections (e.g. sepsis), trauma, or burns, and need additional fluids urgently to prevent dehydration or kidney failure. Colloid or crystalloid solutions may be used for this purpose. Crystalloids have small molecules, are cheap, easy to use, and provide immediate fluid resuscitation, but may increase oedema. Colloids have larger molecules, cost more, and may provide swifter volume expansion in the intravascular space, but may induce allergic reactions, blood clotting disorders, and kidney failure. This is an update of a Cochrane Review last published in 2013.
Objectives
To assess the effect of using colloids versus crystalloids in critically ill people requiring fluid volume replacement on mortality, need for blood transfusion or renal replacement therapy (RRT), and adverse events (specifically: allergic reactions, itching, rashes).
Search methods
We searched CENTRAL, MEDLINE, Embase and two other databases on 23 February 2018. We also searched clinical trials registers.
Selection criteria
We included randomised controlled trials (RCTs) and quasi‐RCTs of critically ill people who required fluid volume replacement in hospital or emergency out‐of‐hospital settings. Participants had trauma, burns, or medical conditions such as sepsis. We excluded neonates, elective surgery and caesarean section. We compared a colloid (suspended in any crystalloid solution) versus a crystalloid (isotonic or hypertonic).
Data collection and analysis
Independently, two review authors assessed studies for inclusion, extracted data, assessed risk of bias, and synthesised findings. We assessed the certainty of evidence with GRADE.
Main results
We included 69 studies (65 RCTs, 4 quasi‐RCTs) with 30,020 participants. Twenty‐eight studied starch solutions, 20 dextrans, seven gelatins, and 22 albumin or fresh frozen plasma (FFP); each type of colloid was compared to crystalloids.
Participants had a range of conditions typical of critical illness. Ten studies were in out‐of‐hospital settings. We noted risk of selection bias in some studies, and, as most studies were not prospectively registered, risk of selective outcome reporting. Fourteen studies included participants in the crystalloid group who received or may have received colloids, which might have influenced results.
We compared four types of colloid (i.e. starches; dextrans; gelatins; and albumin or FFP) versus crystalloids.
Starches versus crystalloids
We found moderate‐certainty evidence that there is probably little or no difference between using starches or crystalloids in mortality at: end of follow‐up (risk ratio (RR) 0.97, 95% confidence interval (CI) 0.86 to 1.09; 11,177 participants; 24 studies); within 90 days (RR 1.01, 95% CI 0.90 to 1.14; 10,415 participants; 15 studies); or within 30 days (RR 0.99, 95% CI 0.90 to 1.09; 10,135 participants; 11 studies).
We found moderate‐certainty evidence that starches probably slightly increase the need for blood transfusion (RR 1.19, 95% CI 1.02 to 1.39; 1917 participants; 8 studies), and RRT (RR 1.30, 95% CI 1.14 to 1.48; 8527 participants; 9 studies). Very low‐certainty evidence means we are uncertain whether either fluid affected adverse events: we found little or no difference in allergic reactions (RR 2.59, 95% CI 0.27 to 24.91; 7757 participants; 3 studies), fewer incidences of itching with crystalloids (RR 1.38, 95% CI 1.05 to 1.82; 6946 participants; 2 studies), and fewer incidences of rashes with crystalloids (RR 1.61, 95% CI 0.90 to 2.89; 7007 participants; 2 studies).
Dextrans versus crystalloids
We found moderate‐certainty evidence that there is probably little or no difference between using dextrans or crystalloids in mortality at: end of follow‐up (RR 0.99, 95% CI 0.88 to 1.11; 4736 participants; 19 studies); or within 90 days or 30 days (RR 0.99, 95% CI 0.87 to 1.12; 3353 participants; 10 studies). We are uncertain whether dextrans or crystalloids reduce the need for blood transfusion, as we found little or no difference in blood transfusions (RR 0.92, 95% CI 0.77 to 1.10; 1272 participants, 3 studies; very low‐certainty evidence). We found little or no difference in allergic reactions (RR 6.00, 95% CI 0.25 to 144.93; 739 participants; 4 studies; very low‐certainty evidence). No studies measured RRT.
Gelatins versus crystalloids
We found low‐certainty evidence that there may be little or no difference between gelatins or crystalloids in mortality: at end of follow‐up (RR 0.89, 95% CI 0.74 to 1.08; 1698 participants; 6 studies); within 90 days (RR 0.89, 95% CI 0.73 to 1.09; 1388 participants; 1 study); or within 30 days (RR 0.92, 95% CI 0.74 to 1.16; 1388 participants; 1 study). Evidence for blood transfusion was very low certainty (3 studies), with a low event rate or data not reported by intervention. Data for RRT were not reported separately for gelatins (1 study). We found little or no difference between groups in allergic reactions (very low‐certainty evidence).
Albumin or FFP versus crystalloids
We found moderate‐certainty evidence that there is probably little or no difference between using albumin or FFP or using crystalloids in mortality at: end of follow‐up (RR 0.98, 95% CI 0.92 to 1.06; 13,047 participants; 20 studies); within 90 days (RR 0.98, 95% CI 0.92 to 1.04; 12,492 participants; 10 studies); or within 30 days (RR 0.99, 95% CI 0.93 to 1.06; 12,506 participants; 10 studies). We are uncertain whether either fluid type reduces need for blood transfusion (RR 1.31, 95% CI 0.95 to 1.80; 290 participants; 3 studies; very low‐certainty evidence). Using albumin or FFP versus crystalloids may make little or no difference to the need for RRT (RR 1.11, 95% CI 0.96 to 1.27; 3028 participants; 2 studies; very low‐certainty evidence), or in allergic reactions (RR 0.75, 95% CI 0.17 to 3.33; 2097 participants, 1 study; very low‐certainty evidence).
Authors' conclusions
Using starches, dextrans, albumin or FFP (moderate‐certainty evidence), or gelatins (low‐certainty evidence), versus crystalloids probably makes little or no difference to mortality. Starches probably slightly increase the need for blood transfusion and RRT (moderate‐certainty evidence), and albumin or FFP may make little or no difference to the need for renal replacement therapy (low‐certainty evidence). Evidence for blood transfusions for dextrans, and albumin or FFP, is uncertain. Similarly, evidence for adverse events is uncertain. Certainty of evidence may improve with inclusion of three ongoing studies and seven studies awaiting classification, in future updates.
Plain language summary
Colloids or crystalloids for fluid replacement in critically people
Background
Critically ill people may lose large amounts of blood (because of trauma or burns), or have serious conditions or infections (e.g. sepsis); they require additional fluids urgently to prevent dehydration or kidney failure. Colloids and crystalloids are types of fluids that are used for fluid replacement, often intravenously (via a tube straight into the blood).
Crystalloids are low‐cost salt solutions (e.g. saline) with small molecules, which can move around easily when injected into the body.
Colloids can be man‐made (e.g. starches, dextrans, or gelatins), or naturally occurring (e.g. albumin or fresh frozen plasma (FFP)), and have bigger molecules, so stay in the blood for longer before passing to other parts of the body. Colloids are more expensive than crystalloids. We are uncertain whether they are better than crystalloids at reducing death, need for blood transfusion or need for renal replacement therapy (filtering the blood, with or without dialysis machines, if kidneys fail) when given to critically ill people who need fluid replacement.
Study characteristics
The evidence is current to February 2018. We searched the medical literature and identified 69 relevant studies with 30,020 critically ill participants who were given fluid replacement in hospital or in an emergency out‐of‐hospital setting. Studies compared colloids (starches; dextrans; gelatins; or albumin or FFP) with crystalloids.
Key results
We found moderate‐certainty evidence that using colloids (starches; dextrans; or albumin or FFP) compared to crystalloids for fluid replacement probably makes little or no difference to the number of critically ill people who die within 30 or 90 days, or by the end of study follow‐up. We also found low‐certainty evidence that using gelatins or crystalloids may make little or no difference to the number of deaths within each of these time points.
We found moderate‐certainty evidence that using starches probably slightly increases the need for blood transfusion. However, we are uncertain whether using other types of colloids, compared to crystalloids, makes a difference to whether people need a blood transfusion because the certainty of the evidence is very low.
We found moderate‐certainty evidence that using starches for fluid replacement probably slightly increases the need for renal replacement therapy. Using albumin or FFP compared to crystalloids may make little or no difference to the need for renal replacement therapy. One study comparing gelatins did not report results for renal replacement therapy according to the type of fluid given, and no studies comparing dextrans assessed renal replacement therapy.
Few studies reported adverse events (specifically, allergic reactions, itching, or rashes), so we are uncertain whether either fluid type causes fewer adverse events (very low‐certainty evidence). We found little or no difference between starches or crystalloids in allergic reactions, but fewer participants given crystalloids reported itching or rashes. We found little or no difference in allergic reactions for the use of dextrans (four studies), gelatins (one study), and albumin or FFP (one study).
Certainty of the evidence
Some study authors did not report study methods clearly and many did not register their studies before they started, so we could not be certain whether the study outcomes were decided before or after they saw the results. Also, we found that some people who were given crystalloids may also have had colloids, which might have affected the results. For some outcomes, we had very few studies, which reduced our confidence in the evidence.
Conclusions
Using colloids (starches; dextrans; or albumin or FFP) compared to crystalloids for fluid replacement probably makes little or no difference to the number of critically ill people who die. It may make little or no difference to the number of people who die if gelatins or crystalloids are used for fluid replacement.
Starches probably increase the need for blood transfusion and renal replacement therapy slightly. Using albumin or FFP may make little or no difference to the need for renal replacement therapy. We are uncertain whether using dextrans, albumin or FFP, or crystalloids affects the need for blood transfusion. Similarly, we are uncertain if colloids or crystalloids increase the number of adverse events. Results from ongoing studies may increase our confidence in the evidence in future.
Summary of findings
Background
Description of the condition
Critically ill people may experience excessive fluid loss, and hypovolaemia, because of haemorrhage from serious injury or burns, or because of critical illnesses, which lead to dehydration, vomiting, or diarrhoea. Fluid loss may lead to mortality and morbidity, for example, haemorrhage accounts for almost half of deaths in the first 24 hours after traumatic injury (Geeraedts 2009; Kauvar 2006), and, worldwide, traumatic injury is a leading cause of death (Peden 2002). Changes in body fluid balance may also lead to acute kidney injury or failure.
Description of the intervention
Fluid resuscitation is one of the most important strategies for early management of critically ill people (Rhodes 2016; Rossaint 2016). Fluids used for this purpose are crystalloids or colloids.
Crystalloids, such as saline and Ringer's lactate, are solutions of salt, water and minerals, and are commonly used in the clinical setting. They have small molecules, and, when used intravenously, they are effective as volume expanders. They may have an isotonic or hypertonic composition, which could affect the distribution of fluid in the body; for example, because hypertonic crystalloids lower plasma osmolality they cause water movement from the intravascular to the extravascular space, and a lower volume may be required for fluid resuscitation (Coppola 2014). They are cheap and easy to use, with few side effects. However, because they move more easily into the extravascular space, their use may increase oedema (Coppola 2014). The composition of the crystalloid may not affect clinical outcomes; recent reviews have examined the possible effect of hypertonic solutions (Shrum 2016), and compared buffered with non‐buffered fluids (Bampoe 2017), but have not found important clinical differences.
Colloids, which are suspended in crystalloid solutions, are similarly given for the purpose of volume expansion. Different types of colloids may be grouped as synthetic or semi‐synthetic, for example: starches, dextrans, gelatins; or naturally occurring, such as human albumin or fresh frozen plasma (FFP). These colloid solutions have different pharmacokinetic properties that may affect plasma expansion in different ways (Orbegozo 2015). All colloids have a larger molecular weight than crystalloids and do not cross the endothelium into the interstitial fluid easily. This means that they stay in the intervascular space for longer than crystalloids, provide the benefit of rapid plasma expansion, and can correct colloidal osmotic pressure (McClelland 1998). Colloids are a more expensive fluid replacement option, and they may have adverse effects such as allergic reactions, blood clotting disorders, and kidney failure (Bailey 2010).
Why it is important to do this review
This is an update of a Cochrane Review that was first published in 1997 and has been updated several times since. The most recent published version of this Cochrane Review looked at the effect of colloids and crystalloids on mortality at the end of study follow‐up (Perel 2013). Meta‐analysis demonstrated no evidence of a difference in mortality when participants were given dextrans, gelatins, albumin or FFP, versus crystalloids. However, the review found evidence of an increase in mortality with the use of starches. Whilst some advise against using starches as a first line of resuscitation (Reinhart 2012), this is not consistent with findings from large randomised trials (Myburgh 2012; Perner 2012), nor with some other systematic reviews (He 2015; Qureshi 2016).
It is possible that results from Perel 2013 could have been confounded by the inclusion of a wider variety of participants in need of fluid resuscitation. In this review, we have sought to reduce heterogeneity in a critically ill population as much as possible by excluding participants who were scheduled for elective surgery; whilst these participants may require fluid replacement during perioperative management to reduce the risk of hypovolaemia, they are less likely to be critically ill at the point of randomisation ‐ even elderly people undergoing semi‐urgent surgery can seldom be seen as critically ill (Lewis 2016).
Also, our aim was to explore other effects of colloids or crystalloids on resuscitation. In particular we aimed to consider whether colloids or crystalloids affect the number of people who require blood transfusion, and the effect on renal function by assessing whether more or fewer critically ill people are likely to need renal replacement therapy after fluid resuscitation interventions, because evidence suggests that use of some types of fluids may increase these risks (Zarychanski 2013). In addition, we considered the effect of type of fluids on adverse events (allergic reactions, itching or pruritis, and rashes) that have been reported in trials (e.g. in Myburgh 2012).
Objectives
To assess the effect of using colloids versus crystalloids in critically ill people requiring fluid volume replacement on mortality, need for blood transfusion or renal replacement therapy, and adverse events (specifically: allergic reactions, itching, rashes).
Methods
Criteria for considering studies for this review
Types of studies
We included parallel‐design randomised controlled trials (RCTs), and quasi‐randomised studies (e.g. studies in which the method of assignment is based on alternation, date of birth or medical record number). We excluded randomised cross‐over trials. We excluded study reports that had been retracted after publication.
Types of participants
We included participants who required fluid volume replacement in hospital or in an emergency out‐of‐hospital setting. We included participants who were described as critically ill, and participants who required fluid volume replacement as a result of trauma, burns, or medical conditions such as sepsis.
We excluded studies of participants undergoing elective surgical procedures. We excluded neonates, and women undergoing caesarean section.
Types of interventions
We included studies that compared a colloid (suspended in any crystalloid solution) versus a crystalloid. We excluded studies in which a colloid was given in both groups of participants.
We included the following colloids: starches; dextrans; gelatins; albumin or fresh frozen plasma (FFP). We included crystalloids of different electrolyte compositions (isotonic or hypertonic).
We considered each colloid type as a separate comparison group. Therefore, we compared:
starches versus crystalloids;
dextrans versus crystalloids;
gelatins versus crystalloids;
albumin or FFP versus crystalloids.
We excluded studies in which the colloid was given to replace a known nutritional deficiency (for example, given for hypoalbuminaemia), or was given as a preloading solution before surgery. We excluded studies in which fluids were given to people with head injury to control intracranial pressure.
Types of outcome measures
We did not exclude studies that did not measure or report review outcomes.
We collected outcome data for mortality from any cause at end‐of‐study follow‐up; we included data for this outcome for which the time point was not reported, and for which the time point was reported as 'before hospital discharge', 'within the ICU', or within 30 days, 60 days, or 90 days. In addition, we collected mortality data that were clearly reported within 90 days, or within 30 days. Our secondary outcomes assessed the effectiveness of the resuscitation fluids and included need for transfusion of any blood product, and need for renal replacement therapy. In addition, we collected data for outcomes of adverse events, specifically: allergic reactions, itching/pruritis, and rashes.
Primary outcomes
All‐cause mortality (at end of follow‐up)
All‐cause mortality (within 90 days)
All‐cause mortality (within 30 days)
Secondary outcomes
Transfusion of blood products
Renal replacement therapy
Adverse events (allergic reactions, itching, and rashes)
Search methods for identification of studies
Electronic searches
We developed subject‐specific search strategies in consultation with the Cochrane Injuries Group Information Specialist. We identified RCTs through literature searching of the following electronic databases:
Cochrane Central Register of Controlled Trials (CENTRAL; 2018, Issue 2) (which contains the Cochrane Injuries Trials Register) in the Cochrane Library (searched 23 February 2018) (Appendix 1);
MEDLINE Ovid (1946 to 23 February 2018) (Appendix 2);
Embase Ovid (1974 to 23 February 2018) (Appendix 3);
PubMed (1948 to 23 February 2018) (Appendix 4);
Web of Science (Core Collection, 1970 to 23 February 2018) (Appendix 5);
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; searched 13 April 2018) (Appendix 6);
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp; searched 13 April 2018) (Appendix 7)
OpenGrey (System for Information on Grey Literature in Europe) (www.opengrey.eu; searched 12 April 2018) (Appendix 8).
This review was an update of a previous Cochrane Review (Perel 2013). However, because we made changes to the inclusion criteria and increased the outcome measures, we ran all the searches from database inception.
Searching other resources
We conducted citation searching of identified included studies published from 2013 onwards in Web of Science (apps.webofknowledge.com) (12 April 2018). We scanned reference lists of relevant systematic reviews (identified during database searches) to search for additional trials.
Data collection and analysis
Two review authors (Sharon Lewis (SL) and either: Michael Pritchard (MP), Andrew Butler (AB), or David Evans (DE)) independently completed all data collection and analyses before comparing results and reaching consensus. We consulted a third review author (Andrew Smith (AS)) to resolve conflicts if necessary.
Selection of studies
We used Endnote reference management software to collate the results of the searches and to remove duplicates. We used Covidence software to screen titles and abstracts and identify potentially relevant studies. We sourced the full texts of all potentially relevant studies and assessed whether the studies met the review inclusion criteria (see Criteria for considering studies for this review). We reviewed abstracts at this stage and included these in the review only if they provided sufficient information to assess eligibility.
We reassessed eligibility of studies included in the last version of the review (Perel 2013), because of changes made to review inclusion criteria.
We recorded the number of papers retrieved at each stage and reported this in a PRISMA flow chart (Liberati 2009; Figure 1). We reported in the review brief details of closely related but excluded papers.
1.
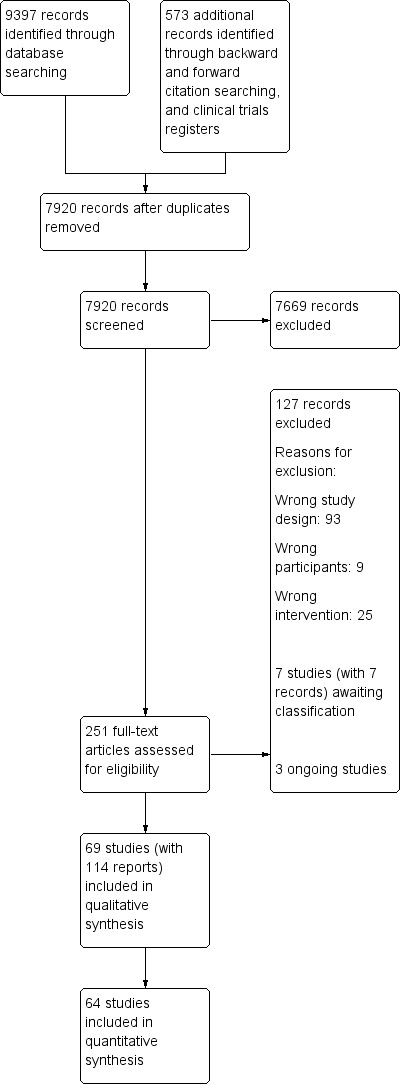
Study flow diagram
Data extraction and management
We used Covidence software to extract data from individual studies. A basic template for data extraction forms is available at www.covidence.org. We adapted this template to include the following information.
Methods ‐ type of study design; setting; country; dates of study; funding sources
Participants ‐ number of participants randomised to each group, number of lost participants, and number of analysed participants, participant condition or reason for fluid resuscitation. Baseline characteristics to include: age, gender, weight or body mass index, blood pressure, prognostic or illness severity scores (American Society of Anaesthesiologists (ASA), Acute Physiology and Chronic Health Evaluation (APACHE) I or II, Simplified Acute Physiology Score (SAPS), Sequential Organ Failure Assessment (SOFA), Glasgow Coma Scale (GCS))
Interventions ‐ details of colloid and crystalloid (concentration of solution, volume, and rate of administration), additional relevant patient management
Outcomes ‐ all outcomes reported by study authors, relevant outcomes (including time of measurement for mortality)
Outcome data ‐ results of outcome data
Because of changes in reporting expectations in Cochrane Reviews ‐ the Methodological Expectations of Cochrane Intervention Reviews (MECIR) (Higgins 2016) ‐ since the last version of the review (Perel 2013), we also used Covidence to re‐conduct data extraction on studies included in the last version of the review.
We considered the applicability of information from individual studies and the generalisability of data to our intended study population (i.e. the potential for indirectness in the review). If we found associated publications from the same study, we created a composite data set based on all eligible publications.
Assessment of risk of bias in included studies
Two review authors (SL and MP, AB, or DE) independently assessed study quality, study limitations, and the extent of potential bias using the Cochrane 'Risk of bias' tool (Higgins 2017). We completed 'Risk of bias' assessment only for studies that reported the review outcomes.
We assessed the following domains.
Sequence generation (selection bias)
Allocation concealment (selection bias)
Blinding of participants, personnel, and outcome assessors (performance bias and detection bias)
Incomplete outcome data (attrition bias)
Selective outcome reporting (reporting bias)
Baseline characteristics
Other bias
We made separate judgements for performance and detection bias for mortality and for blood transfusion/renal replacement therapy/adverse events.
For each domain, we judged whether study authors had made sufficient attempts to minimise bias in their study design. We made judgements using three measures, high, low and unclear risk of bias. We recorded this decision in 'Risk of bias' tables and present a 'Risk of bias' graph and summary figure (Figure 2; Figure 3).
2.
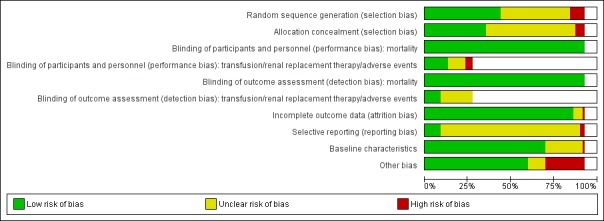
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. We did not make judgements for studies that did not report outcomes of interest in the review, which are indicated by blank spaces
3.
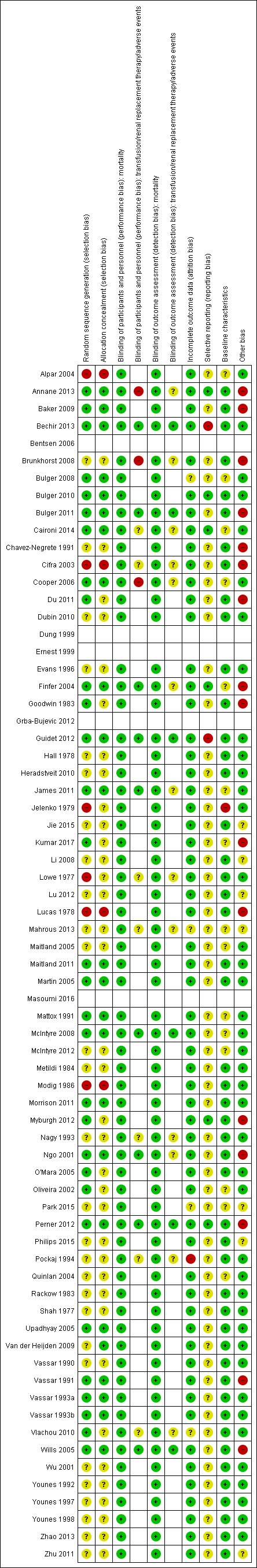
Risk of bias summary: review authors' judgements about each risk of bias item for each included study. We did not make judgements for studies that did not report outcomes of interest in the review, which are indicated by blank spaces
Because of changes in reporting expectations in Cochrane Reviews (MECIR; Higgins 2016) since the last version of the review, we also completed a 'Risk of bias' assessment on all studies included in Perel 2013.
Measures of treatment effect
We collected dichotomous data for each outcome measure (the number of participants who had died, the number of participants who required transfusion of blood products, the number of participants who required renal replacement therapy, and the number of participants who had adverse events).
Unit of analysis issues
We reported data separately according to type of colloid (starches; dextrans; gelatins; albumin or FFP).
For multi‐arm studies that included more than one of the same type of study fluid (e.g. two groups of starches combined with an isotonic or a hypertonic crystalloid), we combined data from study groups in the same analysis only when it was appropriate and when it did not include double‐counting of participants.
In subgroup analysis, in which studies were grouped by different types of crystalloid solution, it was not always appropriate to combine data from multi‐arm study groups. If we had included multi‐arm studies in subgroup analysis, we planned to use the halving method to avoid unit of analysis issues (Deeks 2017).
Dealing with missing data
We assessed whether all measured outcomes had been reported by study authors by comparing, when possible, published reports with protocols or clinical trials register documents that had been prospectively published.
We assessed whether all randomised participants had been included in outcome data. In the absence of an explanation for loss of data, we used the 'Risk of bias' tool to judge whether a study was at high risk of attrition bias.
Assessment of heterogeneity
We assessed whether evidence of inconsistency was apparent in our results by considering heterogeneity. We assessed clinical and methodological heterogeneity by comparing similarities in our included studies between study designs, participants, and interventions, using data collected during data extraction (Data extraction and management). We assessed statistical heterogeneity by calculating the Chi² test and I² statistic (Higgins 2003), and judged any heterogeneity using values of I² greater than 60% and Chi² P value of 0.05 or less to indicate moderate to substantial statistical heterogeneity (Deeks 2017).
As well as looking at statistical results, we considered point estimates and overlap of confidence intervals (CIs). If CIs overlap, then results are more consistent. Combined studies may show a large consistent effect but with significant heterogeneity. Therefore, we planned to interpret heterogeneity with caution (Guyatt 2011a).
Assessment of reporting biases
We attempted to source published protocols for each of our included studies by using clinical trials registers. We compared protocols or clinical trials register documents that had been prospectively published with study results to assess the risk of selective reporting. We generated a funnel plot to assess risk of publication bias in the review, for outcomes in which we identified more than 10 studies (Sterne 2017). An asymmetrical funnel plot may suggest publication of only positive results (Egger 1997). We included funnel plot figures for the primary outcome: all‐cause mortality (at the end of follow‐up) (Figure 4; Figure 5; Figure 6).
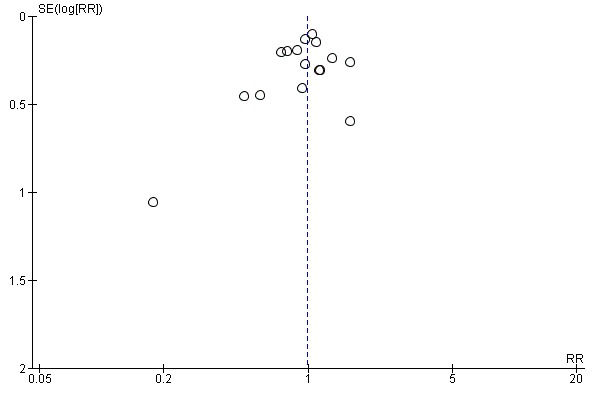
4.
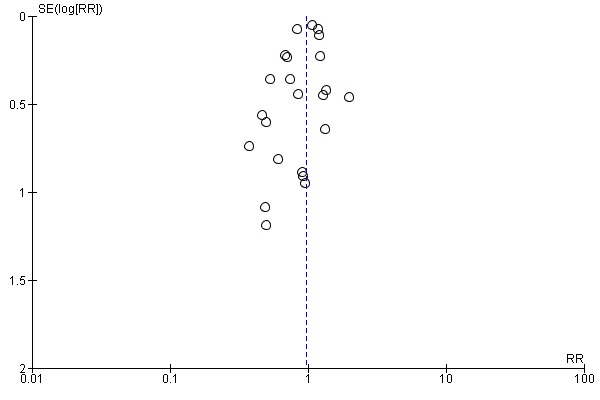
Funnel plot of comparison 1. Starches vs crystalloid, outcome: 1.1 mortality at end of follow‐up
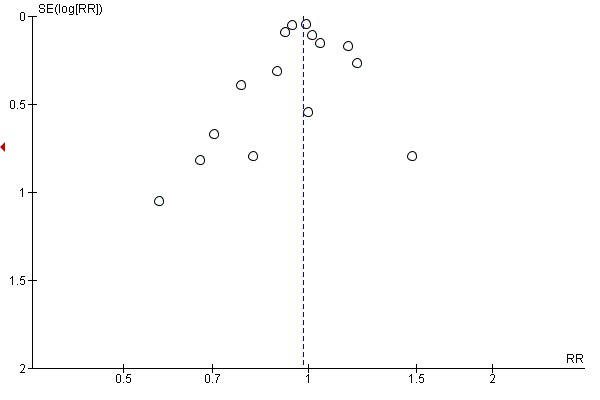
5.
Funnel plot of comparison 2. Dextrans vs crystalloid, outcome: 2.1 mortality at end of follow‐up
6.
Funnel plot of comparison 4. Albumin and FFP vs crystalloid, outcome: 4.1 mortality at end of follow‐up
Data synthesis
We completed meta‐analysis of outcomes in which we had comparable effect measures for more than one study, and when measures of clinical and methodological heterogeneity indicated that pooling was appropriate.
We presented results according to type of colloid (starches; dextrans; gelatins; albumin or FFP) as four separate comparisons (see Types of interventions).
We used the statistical calculator in Review Manager 5 (RevMan 5) to calculate risk ratios (RR) using the Mantel‐Haenszel model (Review Manager 2014). We used a random‐effects statistical model that accounted for the variation amongst participant groups in the review. We calculated CIs at 95% and used a P value of 0.05 or less to judge whether a result was statistically significant. We considered imprecision in the results of analyses by assessing the CI around an effect measure; a wide CI would suggest a higher level of imprecision in our results. A small number of identified studies may also reduce precision (Guyatt 2011b).
Subgroup analysis and investigation of heterogeneity
We explored potential differences in the tonicity of crystalloid solutions that had been used with colloids or used as the comparative crystalloid. This was an a priori subgroup analysis included in the previous version of the review (Perel 2013). We used the calculator in RevMan 5 to perform subgroup analysis, comparing the Chi² and P value for the test for subgroup differences; we interpreted a P value of less than 0.05 as being indicative of a difference between subgroups. We conducted subgroup analysis when data were available for more than 10 studies (Deeks 2017). We considered subgroup analysis only for the primary outcome (all‐cause mortality (at end of follow‐up)) for each of our comparisons (starches; dextrans; gelatins; albumin or FFP). Subgroups were as follows.
-
Tonicity of crystalloid solution:
colloid + isotonic crystalloid versus isotonic crystalloid;
colloid + hypertonic crystalloid versus isotonic crystalloid;
colloid + isotonic crystalloid versus hypertonic crystalloid;
colloid + hypertonic crystalloid versus hypertonic crystalloid.
Sensitivity analysis
We explored the potential effects of decisions made as part of the review process as follows.
We excluded all studies that we judged to be at high or unclear risk of selection bias.
We excluded studies in which we noted that some participants in the crystalloid group were given, or may have been given, additional colloids.
We conducted meta‐analysis using the alternative meta‐analytical effects model (fixed‐effect).
We used alternative data for individual studies in which we noted discrepancies in reported data.
We conducted sensitivity analysis on the primary outcome: all‐cause mortality (at end of follow‐up).
'Summary of findings' table and GRADE
We used the GRADE system to assess the certainty of the body of evidence associated with the following outcomes (Guyatt 2008).
All‐cause mortality (at end of follow‐up)
All‐cause mortality (within 90 days)
All‐cause mortality (within 30 days)
Transfusion of blood products
Renal replacement therapy
Adverse events (allergic reactions, itching, rashes)
The GRADE approach appraises the certainty of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. Evaluation of the certainty of a body of evidence considers within‐study risk of bias, directness of the evidence, heterogeneity of the data, precision of effect estimates, and risk of publication bias.
We constructed four 'Summary of findings' tables using the GRADEpro GDT software to create 'Summary of findings' tables for the following comparisons in this review (GRADEpro GDT 2015).
Starches versus crystalloids
Dextrans versus crystalloids
Gelatins versus crystalloids
Albumin or FFP versus crystalloids
One review author (SL) completed the table in consultation with a second author (MP).
Results
Description of studies
Results of the search
We screened 7920 titles and abstracts from database searches, forward and backward citation searches, and clinical trials register searches. We assessed 248 full‐text reports for eligibility. See Figure 1.
Included studies
See Characteristics of included studies.
We included 69 studies; 42 of these had been included in the previous version of the review (Perel 2013), and 27 were included for the first time in this update.
These 69 studies comprised a total of 114 publications, and included 30,020 participants (Alpar 2004; Annane 2013; Baker 2009; Bechir 2013; Bentsen 2006; Brunkhorst 2008; Bulger 2008; Bulger 2010; Bulger 2011; Caironi 2014; Chavez‐Negrete 1991; Cifra 2003; Cooper 2006; Du 2011; Dubin 2010; Dung 1999; Ernest 1999; Evans 1996; Finfer 2004; Goodwin 1983; Grba‐Bujevic 2012; Guidet 2012; Hall 1978; Heradstveit 2010; James 2011; Jelenko 1979; Jie 2015; Kumar 2017; Li 2008; Lowe 1977; Lu 2012; Lucas 1978; Mahrous 2013; Maitland 2005; Maitland 2011; Martin 2005; Masoumi 2016; Mattox 1991; McIntyre 2008; McIntyre 2012; Metildi 1984; Modig 1986; Morrison 2011; Myburgh 2012; Nagy 1993; Ngo 2001; O'Mara 2005; Oliveira 2002; Park 2015; Perner 2012; Philips 2015; Pockaj 1994; Quinlan 2004; Rackow 1983; Shah 1977; Upadhyay 2005; Van der Heijden 2009; Vassar 1990; Vassar 1991; Vassar 1993a; Vassar 1993b; Vlachou 2010; Wills 2005; Wu 2001; Younes 1992; Younes 1997; Younes 1998; Zhao 2013; Zhu 2011).
Four studies were quasi‐randomised (Alpar 2004; Cifra 2003; Lucas 1978; Modig 1986), and the remaining studies were RCTs.
We included three studies for which we could only source the abstract (Mahrous 2013; Park 2015; Philips 2015); we sourced the full text of all remaining studies.
Study population
Participants had a wide variety of diagnoses for which fluid volume resuscitation was required, including: trauma, burns, and medical conditions such as sepsis and hypovolaemic shock. We have listed each study with the primary participant conditions in Table 5.
1. Summary of participant conditions.
* included for more than one type of condition
ALI: acute lung injury ARDS: acute respiratory distress syndrome ICU: intensive care unit
Seven studies recruited only children (Cifra 2003; Dung 1999; Maitland 2005; Maitland 2011; Ngo 2001; Upadhyay 2005; Wills 2005), and two studies recruited children and adults (Hall 1978; Wu 2001). We noted that some studies reported an inclusion criteria of over 15 years of age (Bulger 2010; Bulger 2011), over 16 years of age (Baker 2009; Bechir 2013; Evans 1996; Masoumi 2016; Mattox 1991; Morrison 2011), or over 17 years of age (Bulger 2008); using mean ages reported by study authors, most participants in these studies were adults over 18 years of age. All remaining studies included only adult participants.
Study setting
Nineteen studies were multicentre studies (Annane 2013; Baker 2009; Brunkhorst 2008; Bulger 2010; Bulger 2011; Caironi 2014; Cooper 2006; Dubin 2010; Finfer 2004; Guidet 2012; Maitland 2011; Martin 2005; Mattox 1991; McIntyre 2008; McIntyre 2012; Morrison 2011; Myburgh 2012; Perner 2012; Quinlan 2004); the remaining studies were single‐centre studies.
Ten studies were based in an out‐of‐hospital setting before transition to an emergency or trauma department within a hospital (Baker 2009; Bulger 2008; Bulger 2010; Caironi 2014; Grba‐Bujevic 2012; Mattox 1991; Morrison 2011; Vassar 1991; Vassar 1993a; Vassar 1993b); the remaining studies were based in a hospital.
Most single‐ or multicentre studies were conducted in one of the following countries: the USA (Bulger 2008; Goodwin 1983; Jelenko 1979; Lowe 1977; Lucas 1978; Martin 2005; Mattox 1991; Metildi 1984; Nagy 1993; O'Mara 2005; Pockaj 1994; Quinlan 2004; Rackow 1983; Shah 1977; Vassar 1990; Vassar 1991; Vassar 1993a; Vassar 1993b); Canada (Baker 2009; Cooper 2006; Ernest 1999; McIntyre 2008; McIntyre 2012; Morrison 2011); China (Du 2011; Jie 2015; Li 2008; Lu 2012; Zhao 2013; Zhu 2011); Brazil (Oliveira 2002; Park 2015; Younes 1992; Younes 1997; Younes 1998); India (Kumar 2017; Philips 2015; Upadhyay 2005); Vietnam (Dung 1999; Ngo 2001; Wills 2005); Norway (Bentsen 2006; Heradstveit 2010); South Africa (Evans 1996; James 2011); the UK (Alpar 2004; Vlachou 2010); Argentina (Dubin 2010); Croatia (Grba‐Bujevic 2012); Denmark (Hall 1978); Germany (Brunkhorst 2008); Iran (Masoumi 2016); Italy (Caironi 2014); Kenya (Maitland 2005); Mexico (Chavez‐Negrete 1991); the Netherlands (Van der Heijden 2009); the Philippines (Cifra 2003); Saudi Arabia (Mahrous 2013); Sweden (Modig 1986); Switzerland (Bechir 2013); Taiwan (Wu 2001).
Eight multicentre studies were conducted in more than one country (Annane 2013: France, Belgium, Canada, Algeria and Tunisia; Perner 2012: Denmark, Finland, Iceland and Norway; Maitland 2011: Kenya, Tanzania and Uganda; Bulger 2010 and Bulger 2011: USA and Canada; Finfer 2004 and Myburgh 2012: Australia and New Zealand; Guidet 2012: France and Germany).
Interventions and comparison
Nine studies were multi‐arm studies that included more than one colloid solution or more than one crystalloid solution or more than one of each type of solution (Dung 1999; Li 2008; Ngo 2001; Rackow 1983; Van der Heijden 2009; Vassar 1993b; Wills 2005; Zhao 2013; Zhu 2011). One study compared colloids with crystalloids and the type of colloid or crystalloid was at the discretion of the physician (Annane 2013); types of colloids in this study were starches, gelatins, and albumin.
Colloids
Twenty‐eight studies used a starch solution (hydroxyethyl starch, hetastarch, or pentastarch) for fluid resuscitation (Annane 2013; Bechir 2013; Bentsen 2006; Brunkhorst 2008; Cifra 2003; Du 2011; Dubin 2010; Grba‐Bujevic 2012; Guidet 2012; Heradstveit 2010; James 2011; Jie 2015; Kumar 2017; Li 2008; Lu 2012; Mahrous 2013; Masoumi 2016; McIntyre 2008; Myburgh 2012; Nagy 1993; Perner 2012; Rackow 1983; Van der Heijden 2009; Vlachou 2010; Wills 2005; Younes 1998; Zhao 2013; Zhu 2011). Of these, sixteen studies did not describe what they used as a suspension solution (Annane 2013; Cifra 2003; Dubin 2010; James 2011; Jie 2015; Li 2008; Lu 2012; Mahrous 2013; Nagy 1993; Perner 2012; Rackow 1983; Van der Heijden 2009; Vlachou 2010; Younes 1998; Zhao 2013; Zhu 2011). Five studies used a starch solution combined with an isotonic crystalloid solution, which was normal saline (Brunkhorst 2008; Masoumi 2016; McIntyre 2008; Myburgh 2012; Wills 2005), and seven studies used a starch solution combined with a hypertonic crystalloid solution, which was hypertonic saline (Bentsen 2006; Grba‐Bujevic 2012; Heradstveit 2010; Li 2008; Zhu 2011), or Ringer's lactate (Bechir 2013; Du 2011). Two studies did not specify the type of crystalloid solution that was combined with a starch (Guidet 2012; Kumar 2017), and one multi‐arm study also included a starch combined with glutamine (Zhao 2013).
Twenty studies used dextrans for fluid resuscitation (Alpar 2004; Baker 2009; Bulger 2008; Bulger 2010; Bulger 2011; Chavez‐Negrete 1991; Dung 1999; Hall 1978; Mattox 1991; Modig 1986; Morrison 2011; Ngo 2001; Oliveira 2002; Vassar 1990; Vassar 1991; Vassar 1993a; Vassar 1993b; Wills 2005; Younes 1992; Younes 1997). Two studies did not describe what they used as a suspension solution in dextran 70 (Modig 1986; Ngo 2001); Ngo 2001 gave Ringer's lactate to all participants after an initial infusion of dextran 70. Three studies used dextran 70 (which has relative molecular mass of 70,000) combined with an isotonic crystalloid solution which was normal saline (Dung 1999; Hall 1978; Wills 2005). Eleven studies used hypertonic saline with 6% dextran 70 solution (HSD 6%) (Baker 2009; Bulger 2008; Bulger 2010; Bulger 2011; Mattox 1991; Morrison 2011; Vassar 1990; Vassar 1993a; Vassar 1993b; Younes 1992; Younes 1997). Three studies used hypertonic saline with dextran 70; Vassar 1993b used it at 12%, while Alpar 2004 used it at 4.2% and Oliveira 2002 used it at 8%. One study used hypertonic saline with dextran 60 (a relative molecular mass of 60,000 (HSD 6%)) (Chavez‐Negrete 1991). One study changed concentration of HSD during the study period; participants were initially given HSD 4.2% with dextran 70 before a protocol change to HSD 6% with dextran 70 (Vassar 1991).
Seven studies used a succinylated gelatin solution (of an isotonic composition) for fluid resuscitation (Annane 2013; Dung 1999; Evans 1996; Ngo 2001Upadhyay 2005; Van der Heijden 2009; Wu 2001).
Twenty‐two studies used albumin or FFP for fluid resuscitation. Thirteen studies used albumin (Annane 2013; Caironi 2014; Ernest 1999; Finfer 2004; Lucas 1978; Maitland 2005; Maitland 2011; Martin 2005; McIntyre 2012; Park 2015; Philips 2015; Quinlan 2004; Rackow 1983). Three studies used albumin combined with an isotonic crystalloid, which was normal saline (Cooper 2006; Pockaj 1994; Van der Heijden 2009), and five studies used albumin combined with a hypertonic crystalloid, which was hypertonic saline (Jelenko 1979), or Ringer's lactate (Goodwin 1983; Lowe 1977; Metildi 1984; Shah 1977). One study used FFP with Ringer's lactate (O'Mara 2005).
Individual study protocols for the concentration, quantity, and timing of administration of each type of study colloid varied. We were not able to establish volume ratios of colloid solutions to crystalloid solutions in most studies; we found that study authors often reported that fluids were provided by the pharmacist and manufacturers in pre‐packaged bags, which we assumed contained fluids in clinically appropriate volume ratios.
Crystalloids
Thirty‐four studies used isotonic solutions as the comparative crystalloid fluid, which was normal saline (Annane 2013; Baker 2009; Bentsen 2006; Bulger 2010; Bulger 2011; Dubin 2010; Dung 1999; Ernest 1999; Finfer 2004; Grba‐Bujevic 2012; Guidet 2012; James 2011; Jie 2015; Maitland 2005; Maitland 2011; Martin 2005; Masoumi 2016; McIntyre 2008; McIntyre 2012; Morrison 2011; Myburgh 2012; Ngo 2001; Oliveira 2002; Philips 2015; Pockaj 1994; Quinlan 2004; Rackow 1983; Upadhyay 2005; Van der Heijden 2009; Vassar 1993a; Younes 1992; Younes 1997; Younes 1998; Zhao 2013).
Forty‐one studies used a hypertonic solution, which was Ringer's lactate (Alpar 2004; Annane 2013; Bechir 2013; Brunkhorst 2008; Bulger 2008; Chavez‐Negrete 1991; Cifra 2003; Cooper 2006; Du 2011; Dung 1999; Evans 1996; Goodwin 1983; Hall 1978; Jelenko 1979; Jie 2015; Kumar 2017; Lowe 1977; Lu 2012; Mahrous 2013; Metildi 1984; Nagy 1993; Ngo 2001; O'Mara 2005; Park 2015; Shah 1977; Vassar 1990; Vassar 1991; Vassar 1993b; Vlachou 2010; Wills 2005; Wu 2001; Zhu 2011), Ringer's acetate (Modig 1986; Perner 2012), or hypertonic saline (Bulger 2010; Bulger 2011; Jelenko 1979; Li 2008; Vassar 1993a; Vassar 1993b; Younes 1992).
One study used Ringer's acetate and normal saline (Heradstveit 2010), and three studies did not specify the type of crystalloid (Caironi 2014; Lucas 1978; Mattox 1991).
Individual study protocols for the quantity and timing of administration of each type of study crystalloid varied.
Outcomes
Only five studies did not report mortality data (Bentsen 2006; Dung 1999; Ernest 1999; Grba‐Bujevic 2012; Masoumi 2016); these five studies did not report any of our review outcomes. Fourteen studies reported number of participants who required transfusion of blood products (Annane 2013; Brunkhorst 2008; Bulger 2011; Cifra 2003; Cooper 2006; Guidet 2012; Lowe 1977; McIntyre 2008; Nagy 1993; Ngo 2001; Perner 2012; Pockaj 1994; Vlachou 2010; Wills 2005). Thirteen studies reported number of participants who required renal replacement therapy (Annane 2013; Bechir 2013; Brunkhorst 2008; Caironi 2014; Finfer 2004; Guidet 2012; James 2011; Mahrous 2013; McIntyre 2008; Myburgh 2012; Park 2015; Perner 2012; Vlachou 2010).
Nine studies reported data for adverse events (Bulger 2008; Guidet 2012; Mattox 1991; Myburgh 2012; Ngo 2001; Perner 2012; Vassar 1990; Vassar 1991; Wills 2005); seven reported incidences of allergic reaction (Bulger 2008; Mattox 1991; Myburgh 2012; Ngo 2001; Perner 2012; Vassar 1990; Vassar 1991), two reported incidences of itching (Guidet 2012; Myburgh 2012), and two reported incidences of rashes (Myburgh 2012; Wills 2005).
Funding sources
Thirty‐nine studies reported funding from departments or other sources that we judged to be independent (Annane 2013; Baker 2009; Brunkhorst 2008; Bulger 2008; Bulger 2010; Bulger 2011; Caironi 2014; Du 2011; Dubin 2010; Dung 1999; Evans 1996; Finfer 2004; Goodwin 1983; Hall 1978; Heradstveit 2010; James 2011; Jelenko 1979; Lowe 1977; Lucas 1978; Maitland 2005; Maitland 2011; Martin 2005; McIntyre 2012; Metildi 1984; Modig 1986; Morrison 2011; Myburgh 2012; Nagy 1993; Oliveira 2002; Perner 2012; Quinlan 2004; Rackow 1983; Shah 1977; Van der Heijden 2009; Vassar 1990; Vassar 1991; Vassar 1993a; Wills 2005; Zhao 2013). Nineteen studies reported funding from pharmaceutical companies, which may have supplied study fluids (Bechir 2013; Brunkhorst 2008; Cooper 2006; Dung 1999; James 2011; Guidet 2012; Maitland 2011; Martin 2005; Mattox 1991; McIntyre 2008; Morrison 2011; Myburgh 2012; Ngo 2001; Perner 2012; Van der Heijden 2009; Vassar 1991; Vassar 1993a; Vassar 1993b; Younes 1992). We noted that one study with pharmaceutical funding reported that funders were involved in the study design, analysis and preparation of the report (Guidet 2012).
The remaining studies did not report funding sources or declare conflicts of interest.
Excluded studies
See Characteristics of excluded studies.
We excluded 127 studies following consideration of the full‐text reports. Ninety‐three reports were of an ineligible study design (studies that were not RCTs, or were commentaries or editorial reports), nine studies had an ineligible participant group, and 25 studies used ineligible interventions (did not compare a colloid versus crystalloid, or fluids given at the wrong time). See Figure 1.
We have not included references and details of all 127 studies excluded during full‐text review, only the 31 that we considered to be key excluded studies (Higgins 2011).
Because of changes to the criteria for considering studies since the last version of the review (Perel 2013), we excluded 31 studies that were previously included and have listed these in the review. Reasons for excluding these studies were: in 28 studies fluid resuscitation was given as part of perioperative management of people undergoing elective surgery (Boutros 1979; Dawidson 1991; Dehne 2001; Eleftheriadis 1995; Evans 2003; Fries 2004; Gallagher 1985; Guo 2003; Hartmann 1993; Hondebrink 1997; Karanko 1987; Lee 2011; Ley 1990; Mazher 1998; McNulty 1993; Moretti 2003; Nielsen 1985; Prien 1990; Shires 1983; Sirieix 1999; Skillman 1975; Tollusfrud 1995; Tollusfrud 1998; Verheij 2006; Virgilio 1979; Wahba 1996; Zetterstorm 1981a; Zetterstorm 1981b); two studies were not RCTs (Bowser‐Wallace 1986; Grundmann 1982); and one study was an abstract of a study protocol where the full study was never published (Rocha e Silva 1994). In addition, we excluded five studies because the publications have been retracted; we have not listed references for these retracted publications.
See Criteria for considering studies for this review and Differences between protocol and review.
Studies awaiting classification
Seven studies are awaiting classification (Halim 2016; Bulanov 2004; Charpentier 2011; NCT00890383; NCT01337934; NCT02064075; Protsenko 2009).
We found three studies during the searches of clinical trials registers (NCT00890383; NCT01337934; NCT02064075). These studies were described as completed but study results were not available; we await publication of the full reports to assess their eligibility for inclusion in the review. One study compared tetrastarch versus an unspecified crystalloid for fluid resuscitation following trauma (NCT00890383); one study compared albumin versus Ringer's lactate for fluid resuscitation for sepsis and septic shock (NCT01337934); and one study compared hydroxyethyl starch versus Ringer's lactate for fluid resuscitation following subarachnoid haemorrhage (NCT02064075). Two studies were published only as abstracts with insufficient information; one compared gelatin versus normal saline for fluid resuscitation for sepsis and septic shock (Halim 2016), and one compared albumin versus normal saline for fluid resuscitation for septic shock (Charpentier 2011). Two studies were published in Russian and require translation to assess eligibility: one compared starches with normal saline (Bulanov 2004), and no details are known about the other study (Protsenko 2009). See Characteristics of studies awaiting classification.
Ongoing studies
We found three ongoing studies during searches of clinical trial registers (NCT01763853; NCT02721238; NCT02782819). One study compares 4% albumin versus an unspecified crystalloid in people with acute respiratory distress syndrome (NCT01763853); one study compares 20% albumin versus plasmalyte in people with cirrhosis‐ and sepsis‐induced hypotension (NCT02721238); and the last study compares 5% albumin or gelatin versus Ringer's lactate or normal saline for treatment of shock (NCT02782819). See Characteristics of ongoing studies.
Risk of bias in included studies
We did not complete 'Risk of bias' assessments for studies that reported none of our review outcomes (Bentsen 2006; Dung 1999; Ernest 1999; Grba‐Bujevic 2012; Masoumi 2016).
We did not seek translation of studies that were published in Chinese (Jie 2015; Li 2008; Lu 2012; Zhu 2011). We made 'Risk of bias' assessments from details available in the English abstracts, and from the baseline characteristics tables.
Allocation
All studies were described as randomised. Thirty studies reported adequate methods of randomisation and we judged these to have a low risk of bias for random sequence generation (Annane 2013; Baker 2009; Bechir 2013; Bulger 2008; Bulger 2010; Bulger 2011; Caironi 2014; Cooper 2006; Du 2011; Finfer 2004; Goodwin 1983; Guidet 2012; James 2011; Kumar 2017; Maitland 2011; Martin 2005; Mattox 1991; McIntyre 2008; Morrison 2011; Myburgh 2012; Ngo 2001; O'Mara 2005; Oliveira 2002; Perner 2012; Upadhyay 2005; Vassar 1991; Vassar 1993a; Vassar 1993b; Vlachou 2010; Wills 2005). Twenty‐four studies reported adequate methods of allocation concealment and we judged these to have a low risk of bias (Annane 2013; Baker 2009; Bechir 2013; Bulger 2008; Bulger 2010; Bulger 2011; Caironi 2014; Cooper 2006; Finfer 2004; Guidet 2012; James 2011; Maitland 2011; Martin 2005; Mattox 1991; McIntyre 2008; Morrison 2011; Ngo 2001; Perner 2012; Upadhyay 2005; Van der Heijden 2009; Vassar 1991; Vassar 1993a; Vassar 1993b; Wills 2005).
Four studies were quasi‐randomised studies, and we believed that methods for random sequence generation and random allocation concealment were at high risk of selection bias (Alpar 2004; Cifra 2003; Lucas 1978; Modig 1986). Two studies were described as randomised but because of differences noted in the baseline characteristics table (Jelenko 1979), and unexplained differences in participant numbers (Lowe 1977), we judged them to be at high risk of bias for random sequence generation. One study described "use of lots" to allocate participants to groups and, without additional details, we were uncertain whether this method was adequate and so assessed risk of bias of random sequence generation as unclear (Hall 1978).
The remaining studies reported insufficient details of random sequence generation (Brunkhorst 2008; Chavez‐Negrete 1991; Dubin 2010; Evans 1996; Hall 1978; Heradstveit 2010; Jie 2015; Li 2008; Lu 2012; Mahrous 2013; Maitland 2005; McIntyre 2012; Metildi 1984; Nagy 1993; Park 2015; Philips 2015; Pockaj 1994; Quinlan 2004; Rackow 1983; Shah 1977; Van der Heijden 2009; Vassar 1990; Wu 2001; Younes 1992; Younes 1997; Younes 1998; Zhao 2013; Zhu 2011), and random allocation concealment (Brunkhorst 2008; Chavez‐Negrete 1991; Du 2011; Dubin 2010; Evans 1996; Goodwin 1983; Hall 1978; Heradstveit 2010; Jelenko 1979; Jie 2015; Kumar 2017; Li 2008; Lowe 1977; Lu 2012; Mahrous 2013; Maitland 2005; McIntyre 2012; Metildi 1984; Myburgh 2012; Nagy 1993; O'Mara 2005; Oliveira 2002; Park 2015; Philips 2015; Pockaj 1994; Quinlan 2004; Rackow 1983; Shah 1977; Vassar 1990; Vlachou 2010; Wu 2001; Younes 1992; Younes 1997; Younes 1998; Zhao 2013; Zhu 2011), and we judged these to have an unclear risk of selection bias.
Blinding
For the mortality outcome, we believed that lack of blinding was unlikely to influence performance, or influence outcome assessment, therefore, we judged all studies that reported mortality data as having a low risk of performance bias and a low risk of detection bias for mortality.
For the remaining outcomes (transfusion of blood products, renal replacement therapy, and adverse events), we assessed whether methods had been used to disguise fluid types from clinicians, and from outcome assessors. Nine studies reported sufficient methods of blinding and we judged these to have low risk of performance bias (Bechir 2013; Bulger 2011; Guidet 2012; Finfer 2004; James 2011; McIntyre 2008; Ngo 2001; Perner 2012; Wills 2005). Two studies described methods of fluid administration as open‐label, in which differences between study fluids would be apparent to personnel; we judged these to have a high risk of performance bias (Brunkhorst 2008; Cooper 2006). Study authors in Annane 2013 reported that clinicians were not blinded because of the immediate need for resuscitation; we judged this study to have a high risk of performance bias. We judged the remaining studies as having an unclear risk of performance bias because methods of blinding were not described (Caironi 2014; Cifra 2003; Lowe 1977; Mahrous 2013; Nagy 1993; Pockaj 1994; Vlachou 2010).
Six studies reported sufficient methods of blinding of outcome assessors and we judged these to have a low risk of detection bias (Bechir 2013; Bulger 2011; Guidet 2012; McIntyre 2008; Perner 2012; Wills 2005). We judged the remaining studies to have an unclear risk of detection bias because study authors reported insufficient methods of blinding of outcome assessors (Brunkhorst 2008; Caironi 2014; Cifra 2003; Cooper 2006; Finfer 2004; James 2011; Lowe 1977; Mahrous 2013; Nagy 1993; Ngo 2001; Pockaj 1994; Vlachou 2010).
Incomplete outcome data
Two studies, published only as abstracts, appeared to have some discrepancies in mortality data and we could not be certain whether this was because of loss of participant data; we judged these studies to have unclear risk of attrition bias (Mahrous 2013; Park 2015).
One study had an apparent loss of analysed participants for mortality, but not for transfusion of blood products, and we could not explain this difference in loss; we judged this study to have a high risk of attrition bias (Pockaj 1994). One study excluded three participants because of protocol deviations; because the study was small this represented a high loss and we judged the study to have an unclear risk of attrition bias (Vlachou 2010). One study noted that approximately 10% of participants did not meet eligibility criteria after randomisation, however these were included in an intention‐to‐treat (ITT) analysis; we judged this study to have an unclear risk of attrition bias because this was a large number of participants in an ITT analysis (Bulger 2008).
The remaining studies had no losses, or few losses that were explained, and we judged them all to have low risk of attrition bias.
Selective reporting
We found prospective clinical trials registration reports for nine studies (Annane 2013; Bechir 2013; Bulger 2008; Bulger 2010; Caironi 2014; Finfer 2004; Guidet 2012; Myburgh 2012; Perner 2012). Outcomes were reported according to these trial registration documents in six studies and we judged these to have a low risk of selective reporting bias (Annane 2013; Bulger 2010; Caironi 2014; Finfer 2004; Myburgh 2012; Perner 2012). In one study, we noted that outcomes were added to the trials register documents after the start of the study, and we could not be certain whether selective reporting bias was introduced because of this (Bulger 2008). In two studies, we noted that outcomes in the study report were not listed as outcomes in the clinical trials registration documents, and we judged these studies to have a high risk of selective reporting bias (Bechir 2013; Guidet 2012).
Three studies were registered retrospectively with clinical trials registers (Dubin 2010; James 2011; Maitland 2011); it was not feasible to use information from these clinical trials documents to assess risk of selective reporting bias.
We could not be certain whether Philips 2015 was prospectively registered because the available abstract report included the clinical trials register identification number but not the study dates; we judged this to have an unclear risk of selective reporting bias.
All other studies did not provide clinical trials registration information, or references for published study protocols, and we were unable to assess risk of selective reporting bias for these studies.
Baseline characteristics
We noted no differences in baseline characteristics that we believed could introduce bias in 46 studies, and we judged these studies to have a low risk of bias (Annane 2013; Baker 2009; Bechir 2013; Brunkhorst 2008; Bulger 2010; Bulger 2011; Chavez‐Negrete 1991; Cifra 2003; Du 2011; Dubin 2010; Evans 1996; Goodwin 1983; Guidet 2012; Hall 1978; Jie 2015; Li 2008; Lowe 1977; Lu 2012; Lucas 1978; Maitland 2011; Martin 2005; Metildi 1984; Modig 1986; Morrison 2011; Myburgh 2012; Nagy 1993; Ngo 2001; O'Mara 2005; Perner 2012; Philips 2015; Pockaj 1994; Rackow 1983; Shah 1977; Upadhyay 2005; Van der Heijden 2009; Vassar 1990; Vassar 1991; Vassar 1993a; Vassar 1993b; Vlachou 2010; Wills 2005; Wu 2001; Younes 1992; Younes 1997; Younes 1998; Zhu 2011).
We noted an imbalance in some baseline characteristics in eleven studies (Alpar 2004; Bulger 2008; Caironi 2014; Cooper 2006; Finfer 2004; James 2011; Kumar 2017; Maitland 2005; McIntyre 2008; Oliveira 2002; Quinlan 2004). We could not be certain whether these imbalances could influence results and we judged these studies to have an unclear risk of bias. We noted differences in several baseline characteristics in one study and judged this to have a high risk of bias (Jelenko 1979).
We could not assess comparability of baseline characteristics in four studies because these were either not reported or not reported by group (Mattox 1991; Mahrous 2013; McIntyre 2012; Park 2015).
Other potential sources of bias
We noted that in 14 studies some participants were given, or may have been given, additional colloids in the crystalloid arm either before or during the study (Annane 2013; Baker 2009; Brunkhorst 2008; Bulger 2011; Chavez‐Negrete 1991; Cifra 2003; Du 2011; Finfer 2004; Goodwin 1983; Myburgh 2012; Ngo 2001; Perner 2012; Vassar 1991; Wills 2005); we judged all these studies to have a high risk of other bias.
We noted that one study was published by a single author, and time between completion of the study and publication of the report was longer than expected (Kumar 2017). We could not be certain whether this study was a primary publication, or a secondary publication of an existing or unknown study, and we judged it to have a high risk of bias. We noted differences in the reported number of deaths in Lucas 1978 according to different study reports, and these differences were unexplained; we judged this study to have a high risk of other bias.
We could not be certain of other risks of bias in the Chinese studies for which we did not seek translation (Jie 2015; Li 2008; Lu 2012; Zhu 2011), nor in studies that were published only as abstracts (Mahrous 2013; Park 2015; Philips 2015); and we assessed these studies to have an unclear risk of other bias.
We noted no other sources of bias in the remaining studies, and judged these all to have a low risk of other bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Summary of findings for the main comparison. Starches compared to crystalloid for fluid resuscitation in critically ill patients.
| Starches compared to crystalloid for fluid resuscitation in critically ill patients | ||||||
| Participants: critically ill people requiring fluid resuscitation Setting: in hospital, in Algeria, Argentina, Belgium, Brazil, Canada, China, France, Germany, India, the Netherlands, Phillipines, South Africa, Switzerland, Tunisia, the UK, USA and Vietnam Intervention: starches to include hydroxyethyl starch, hetastarch, and pentastarch Comparison: crystalloids to include normal saline, hypertonic saline, Ringer's lactate and Ringer's acetate | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with crystalloids | Risk with starches | |||||
| All‐cause mortality (at end of follow‐up) | Study population | RR 0.97 (0.86 to 1.09) | 11,177 (24 studies) | ⊕⊕⊕⊝ Moderatea |
We excluded data from 1 study because we could not be certain whether it accounted for attrition | |
| 233 per 1000 | 226 per 1000 (201 to 254) | |||||
| All‐cause mortality (at 90 days) | Study population | RR 1.01 (0.90 to 1.14) | 10,415 (15 studies) | ⊕⊕⊕⊝ Moderateb |
We excluded data from 1 study because we could not be certain whether it accounted for attrition | |
| 238 per 1000 | 241 per 1000 (214 to 272) | |||||
| All‐cause mortality (within 30 days) | Study population | RR 0.99 (0.90 to 1.09) | 10,135 (11 studies) | ⊕⊕⊕⊝ Moderateb |
We excluded data from 1 study because we could not be certain whether it accounted for attrition | |
| 191 per 1000 | 189 per 1000 (172 to 208) | |||||
| Transfusion of blood products | Study population | RR 1.19 (1.02 to 1.39) | 1917 (8 studies) | ⊕⊕⊕⊝ Moderatea |
1 study included different types of colloids (HES, gelatins, or albumin). We did not include this in analysis because study authors did not report data for only starches; we noted little or no difference between groups in need for transfusion of blood products in this study | |
| 299 per 1000 | 356 per 1000 (305 to 416) | |||||
| Renal replacement therapy | Study population | RR 1.30 (1.14 to 1.48) | 8527 (9 studies) | ⊕⊕⊕⊝ Moderateb |
1 study included different types of colloids (HES, gelatins, or albumin). We did not include this in analysis because study authors did not report data for only starches; we noted little or no difference between groups in need for renal replacement therapy in this study | |
| 82 per 1000 | 106 per 1000 (93 to 121) | |||||
| Adverse events | Allergic reaction | ⊕⊝⊝⊝ Very lowc |
||||
| Study population | RR 2.59 (0.27 to 24.91) | 7757 (3 studies) | ||||
| 0 per 1000 | 0 per 1000 (0 to 0) |
|||||
| Itching | ||||||
| Study population | RR 1.38 (1.05 to 1.82) | 6946 (2 studies) | ||||
| 26 per 1000 | 35 per 1000 (27 to 46) |
|||||
| Rashes | ||||||
| Study population | RR 1.61 (0.90 to 2.89) | 7007 (2 studies) | ||||
| 5 per 1000 | 9 per 1000 (5 to 15) |
|||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWe downgraded by one level for study limitations; some included studies had unclear risk of selection bias, one small study had a high risk of selection bias, and we were often unable to assess risk of selective reporting bias because many included studies did not have prospective clinical trials registration. bWe downgraded by one level for study limitations; some included studies had unclear risk of selection bias, and we were often unable to assess risk of selective reporting bias because many included studies did not have prospective clinical trials registration. cWe downgraded by one level for study limitations; some included studies had unclear risk of selection bias, and we were unable to assess risk of selective reporting bias in some studies because they did not have prospective clinical trials registration. We downgraded by two levels for imprecision; few of our included studies reported data for these outcomes.
Summary of findings 2. Dextrans compared to crystalloid for fluid resuscitation in critically ill patients.
| Dextrans compared to crystalloid for fluid resuscitation in critically ill patients | ||||||
| Participants: critically ill people requiring fluid resuscitation Setting: in hospital, or out of hospital, in Brazil, Canada, Denmark, Mexico, Sweden, UK, USA and Vietnam Intervention: dextrans Comparison: crystalloids to include: normal saline, hypertonic saline, Ringer's lactate, Ringer's acetate, and unspecified types of crystalloids | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with crystalloids | Risk with dextrans | |||||
| All‐cause mortality (at end of follow‐up) | Study population | RR 0.99 (0.88 to 1.11) | 4736 (19 studies) | ⊕⊕⊕⊝ Moderatea |
||
| 237 per 1000 | 235 per 1000 (209 to 263) | |||||
| All‐cause mortality (within 90 days and within 30 days) | Study population | RR 0.99 (0.87 to 1.12) | 3353 (10 studies) | ⊕⊕⊕⊝ Moderatea |
||
| 258 per 1000 | 256 per 1000 (225 to 289) | |||||
| Transfusion of blood products | Study population | RR 0.92 (0.77 to 1.10) |
1272 (3 studies) |
⊕⊝⊝⊝ Very lowb |
||
| 332 per 1000 | 305 per 1000 (255 to 365) |
|||||
| Renal replacement therapy | ‐ | ‐ | ‐ | ‐ | ‐ | Not measured |
| Adverse events | Allergic reactions | |||||
| Study population | RR 6.00 (0.25 to 144.93) |
739 (4 studies) |
⊕⊝⊝⊝ Very lowc |
|||
| 0 per 1000 | 0 per 1000 (0 to 0) |
|||||
| Itching | ||||||
| Study population | Not measured | ‐ | ||||
| ‐ | ‐ | |||||
| Rashes | ||||||
| Study population | Not measured | ‐ | ||||
| ‐ | ‐ | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWe downgraded by one level for study limitations; some included studies had unclear risk of selection bias and we were often unable to assess risk of selective reporting bias because many included studies did not have prospective clinical trials registration. bWe downgraded by two levels for study limitations; we noted in two studies that some participants were given additional colloids in the crystalloid group, and in one study we could not be certain whether some participants in the crystalloids groups also received up to 2000 mL colloid resuscitation prior to randomisation. In addition, we were unable to assess risk of selective reporting bias because of lack of prospective clinical trials registration in each study. We downgraded by one level for imprecision; evidence was from three studies. cWe downgraded by one level for study limitations; one study had an unclear risk of selection bias and we were unable to assess risk of selective outcome reporting bias in all studies. We downgraded by two levels for imprecision because evidence was from few studies with few events.
Summary of findings 3. Gelatins compared to crystalloid for fluid resuscitation in critically ill patients.
| Gelatins compared to crystalloid for fluid resuscitation in critically ill patients | ||||||
| Participants: critically ill people requiring fluid resuscitation Setting: in hospital, in Algeria, France, Germany, India, South Africa, Taiwan, Tunisia and Vietnam Intervention: gelatins Comparison: crystalloids to include normal saline and Ringer's lactate | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with crystalloids | Risk with gelatins | |||||
| All‐cause mortality (at end of follow‐up) | Study population | RR 0.89 (0.74 to 1.08) | 1698 (6 studies) | ⊕⊕⊝⊝ Lowa |
||
| 301 per 1000 | 268 per 1000 (223 to 325) | |||||
| All‐cause mortality (within 90 days) | Study population | RR 0.89 (0.73 to 1.09) | 1388 (1 study) |
⊕⊕⊝⊝ Lowb |
||
| 334 per 1000 | 298 per 1000 (244 to 364) |
|||||
| All‐cause mortality (within 30 days) | Study population | RR 0.92 (0.74 to 1.16) | 1388 (1 study) |
⊕⊕⊝⊝ Lowb |
||
| 266 per 1000 | 244 per 1000 (197 to 308) |
|||||
| Transfusion of blood products | Study population | RR 5.89 (0.24 to 142.41) |
167 (1 study) |
⊕⊝⊝⊝ Very lowc |
We calculated an effect estimate for one small study, with one event in the gelatin group. 1 study reported transfusion of blood products but data were not reported by group. 1 study included different types of colloids (HES, gelatins, or albumin). We did not include this in analysis because study authors did not report data for only gelatins. We noted little or no difference between groups in need for transfusion of blood products |
|
| 0 per 1000 | 0 per 1000 (0 to 0) |
|||||
| Renal replacement therapy | ‐ | ‐ | ‐ | ‐ | ‐ | 1 study included different types of colloids (HES, gelatins, or albumin). We did not include this in analysis because study authors did not report data for only gelatins. We noted little or no difference between groups in need for renal replacement therapy |
| Adverse events | Allergic reaction | ⊕⊝⊝⊝ Very lowc |
We calculated an effect estimate for one small study, with five incidences of allergic reactions in the gelatin group | |||
| 0 per 1000 | 0 per 1000 (0 to 0) |
RR 21.61 (1.22 to 384.05) | 167 (1 study) |
|||
| Itching | ||||||
| ‐ | ‐ | ‐ | ||||
| Rashes | ||||||
| ‐ | ‐ | ‐ | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWe downgraded by one level for study limitations; risk of selection bias was unclear in some studies, and because we were unable to assess risk of selective outcome reporting bias in some studies. We downgraded by one level for imprecision; evidence was from few studies, and we could not be certain of time points for data collection. bWe downgraded by two levels for imprecision; evidence was from a single study. cWe downgraded by one level for study limitations; we were unable to assess risk of selective outcome reporting bias due to lack of prospective clinical trials registration, and some participants in the crystalloid groups also received colloids. We downgraded two levels for imprecision; evidence was from a single small study with very few events.
Summary of findings 4. Albumin and fresh frozen plasma compared to crystalloid for fluid resuscitation in critically ill patients.
| Albumin and fresh frozen plasma compared to crystalloid for fluid resuscitation in critically ill patients | ||||||
| Participants: critically ill people requiring fluid resuscitation Setting: in hospital and out of hospital, in Algeria, Brazil, Canada, France, Germany, Kenya, India, Italy, Tanzania, Tunisia, Uganda and USA Intervention: albumin and fresh frozen plasma Comparison: crystalloids to include: normal saline, hypertonic saline, Ringer's lactate, electrolytes, and unspecified types of crystalloids | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with crystalloids | Risk with albumin and FFP | |||||
| All‐cause mortality (at end of follow‐up) | Study population | RR 0.98 (0.92 to 1.06) | 13,047 (20 studies) | ⊕⊕⊕⊝ Moderatea |
One study also reported mortality but not by group, and so could not be included in analysis | |
| 254 per 1000 | 249 per 1000 (234 to 270) | |||||
| All‐cause mortality (within 90 days) | Study population | RR 0.98 (0.92 to 1.04) | 12,492 (10 studies) | ⊕⊕⊕⊝ Moderatea |
One study also reported mortality but not by group, and so could not be included in analysis | |
| 259 per 1000 | 254 per 1000 (239 to 270) | |||||
| All‐cause mortality (within 30 days) | Study population | RR 0.99 (0.93 to 1.06) | 12,506 (10 studies) | ⊕⊕⊕⊝ Moderatea |
One study also reported mortality but not by group, and so could not be included in analysis | |
| 234 per 1000 | 231 per 1000 (217 to 248) | |||||
| Transfusion of blood products | Study population | RR 1.31 (0.95 to 1.80) | 290 (3 studies) | ⊕⊝⊝⊝ Very lowb |
1 study included different types of colloids (HES, gelatins, or albumin). We did not include this in analysis because study authors did not report data for only albumins or FFP; we noted little or no difference between groups in need for transfusion of blood products | |
| 281 per 1000 | 368 per 1000 (267 to 506) | |||||
| Renal replacement therapy | 201 per 1000 | 223 per 1000 (193 to 255) |
RR 1.11 (0.96 to 1.27) | 3028 (2 studies) |
⊕⊕⊝⊝ Lowc |
One study stated that renal replacement data were measured but it was not reported in the study report (abstract) 1 study included different types of colloids (HES, gelatins, or albumin). We did not include this in analysis because study authors did not report data for only albumin and FFP. We noted little or no difference between groups in need for renal replacement therapy |
| Adverse events | Allergic reactions | ⊕⊝⊝⊝ Very lowd |
||||
| Study population | RR 0.75 (0.17 to 3.33) | 2097 (1 study) |
||||
| 4 per 1000 | 3 per 1000 (1 to 13) |
|||||
| Itching | ||||||
| ‐ | ‐ | ‐ | ‐ | |||
| Rashes | ||||||
| ‐ | ‐ | ‐ | ‐ | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; FFP: fresh frozen plasma RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWe downgraded by one level for study limitations; some included studies had unclear risk of selection bias, and we were often unable to assess risk of selective reporting bias because many included studies did not have prospective clinical trials registration. bWe downgraded by two levels for study limitations; some studies had unclear risk of selection bias, and we noted baseline imbalances in one study. We downgraded by one level for imprecision because analysis included few studies with few participants. cWe downgraded by two levels for study limitations; we noted baseline imbalances and we could not be certain how many participants in the crystalloids group may have received additional colloids. dWe downgraded by one level for study limitations; we were unable to assess risk of selective reporting bias because the included study did not appear to have prospective clinical trials registration. We downgraded by two levels for imprecision; evidence was from a single study with few events.
1. Starches versus crystalloids
All‐cause mortality at end of follow‐up
Twenty‐five studies measured mortality (Annane 2013; Bechir 2013; Brunkhorst 2008; Cifra 2003; Du 2011; Dubin 2010; Guidet 2012; Heradstveit 2010; James 2011; Jie 2015; Kumar 2017; Li 2008; Lu 2012; Mahrous 2013; McIntyre 2008; Myburgh 2012; Nagy 1993; Perner 2012; Rackow 1983; Van der Heijden 2009; Vlachou 2010; Wills 2005; Younes 1998; Zhao 2013; Zhu 2011).
We included 24 in this analysis, in which the time of the assessment point was: within 24 hours (Dubin 2010; Rackow 1983; Younes 1998); within the ICU or hospital stay (Du 2011; Van der Heijden 2009; Vlachou 2010); up to 30 days from hospital discharge (Kumar 2017); within 28 or 30 days (Guidet 2012; Li 2008; McIntyre 2008); within 60 days (Zhao 2013); within 90 days (Annane 2013; Bechir 2013; Brunkhorst 2008; Myburgh 2012; Perner 2012); at 12 months (Heradstveit 2010); and studies in which the time point was unknown (Cifra 2003; James 2011; Jie 2015; Lu 2012; Nagy 1993; Wills 2005; Zhu 2011). We did not include mortality data reported in Mahrous 2013, the data were reported as percentages in the abstract and we could not be certain whether the data were for all randomised participants or whether some participant data were lost.
Three studies were multi‐arm studies. We combined data for both colloid groups in two studies (Zhao 2013; Zhu 2011); and for both colloid groups and both crystalloid groups in Li 2008. One study, which allowed type of colloid or crystalloid to be at the discretion of the clinician, reported mortality outcome data for participants who received only one type of fluid (Annane 2013); we included data for participants who received only hydroxyethyl starch in the colloid group, and combined data for two crystalloid groups (isotonic saline, and Ringer's lactate).
We found little or no difference in the number of participants who died at the end of follow‐up according to whether fluid resuscitation was with a starch or with a crystalloid (RR 0.97 95% CI 0.86 to 1.09; 11,177 participants; 24 studies; I² = 34%; Analysis 1.1).
1.1. Analysis.
Comparison 1 Starches vs crystalloid, Outcome 1 Mortality at end of follow‐up.
We generated a funnel plot to assess risk of publication bias and did not interpret this to indicate high risk (Figure 4).
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had an unclear risk of selection bias, one small study had a high risk of selection bias, and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 1.
All‐cause mortality within 90 days
Sixteen studies measured mortality within 90 days (Annane 2013; Bechir 2013; Brunkhorst 2008; Dubin 2010; Guidet 2012; Kumar 2017; Li 2008; Mahrous 2013; McIntyre 2008; Myburgh 2012; Perner 2012; Rackow 1983; Van der Heijden 2009; Vlachou 2010; Younes 1998; Zhao 2013).
We included mortality data in this analysis in which the time point was: within 24 hours (Dubin 2010; Rackow 1983; Younes 1998); within the ICU or hospital stay (Van der Heijden 2009; Vlachou 2010); up to 30 days from hospital discharge (Kumar 2017); within 28 or 30 days (Guidet 2012; Li 2008; McIntyre 2008); within 60 days (Zhao 2013); or within 90 days (Annane 2013; Bechir 2013; Brunkhorst 2008; Myburgh 2012; Perner 2012). We did not include the mortality data reported in Mahrous 2013, as the data were not clearly reported in the abstract.
Two studies were multi‐arm studies. We combined data for both colloid groups in Zhao 2013, and for both colloid groups and both crystalloid groups in Li 2008. One study, which allowed type of colloid or crystalloid to be at the discretion of the clinician, reported mortality outcome data for participants who received only one type of fluid (Annane 2013). We included data for participants who received only hydroxyethyl starch in the colloid group, and combined data for two crystalloid groups (isotonic saline, and Ringer's lactate).
We found little or no difference in the number of participants who died within 90 days according to whether fluid resuscitation was with a starch or with a crystalloid (RR 1.01, 95% CI 0.90 to 1.14; 10,415 participants; 15 studies; I² = 36%; Analysis 1.2).
1.2. Analysis.
Comparison 1 Starches vs crystalloid, Outcome 2 Mortality within 90 days.
We generated a funnel plot to assess risk of publication bias and did not interpret this as indicating high risk.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had an unclear risk of selection bias and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 1.
All‐cause mortality within 30 days
Twelve studies measured mortality within 30 days (Annane 2013; Bechir 2013; Brunkhorst 2008; Dubin 2010; Guidet 2012; Li 2008; Mahrous 2013; McIntyre 2008; Myburgh 2012; Perner 2012; Rackow 1983; Younes 1998). We did not include mortality data reported in Mahrous 2013, as the data were not clearly reported in the abstract.
One study was a multi‐arm study (Li 2008); we combined data for both colloid groups and both crystalloid groups in this study.
We included mortality data in this analysis in which the time point was: within 24 hours (Dubin 2010; Rackow 1983; Younes 1998); and within 28 or 30 days (Annane 2013; Bechir 2013; Brunkhorst 2008; Guidet 2012; Li 2008; McIntyre 2008; Myburgh 2012; Perner 2012).
We found little or no difference in the number of participants who died within 30 days according to whether fluid resuscitation was with a starch or with a crystalloid (RR 0.99, 95% CI 0.90 to 1.09; 10,135 participants; 11 studies; I² = 12%; Analysis 1.3).
1.3. Analysis.
Comparison 1 Starches vs crystalloid, Outcome 3 Mortality within 30 days.
We generated a funnel plot to assess risk of publication bias and did not interpret this as indicating high risk.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had unclear risk of selection bias and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 1.
Transfusion of blood products
Nine studies reported the number of participants who required transfusion of blood products (Annane 2013; Brunkhorst 2008; Cifra 2003; Guidet 2012; McIntyre 2008; Nagy 1993; Perner 2012; Vlachou 2010; Wills 2005).
One study, which allowed type of colloid or crystalloid to be at the discretion of the clinician, combined data for all types of colloids (hydroxyethyl starch, gelatins, or albumin), and we could not include these data in the analysis of starches (Annane 2013). We reported data for transfusion of blood products for this study in Table 6; we noted little or no difference between groups in the need for blood products according to type of fluid.
2. Data for outcomes with a single study.
| Study ID | Outcome | Events in colloid group: n/N |
Events in crystalloid group: n/N |
Effect estimate |
| Colloids (at the discretion of the clinician: HES, gelatins, or albumin) versus crystalloids | ||||
| Annane 2013 | Transfusion of blood products | 377/1414 | 358/1443 | RR 1.07, 95% CI 0.95 to 1.22; 2857 participants |
| Annane 2013 | Renal replacement therapy | 156/1414 | 181/1443 | RR 0.88, 95% CI 0.72 to 1.08; 2857 participants |
| Gelatin versus crystalloids | ||||
| Annane 2013 | Mortality (within 90 days) | 84/281 | 346/1035 | RR 0.89, 95% CI 0.73 to 1.09; 1388 participants |
| Annane 2013 | Mortality (within 30 days) | 69/281 | 275/1035 | RR 0.92, 95% CI 0.74 to 1.16; 1388 participants |
| Albumin versus crystalloid | ||||
| Maitland 2011 | Adverse events: allergic reactions | 3/1050 | 4/1047 | RR 0.75, 95% CI 0.17 to 3.33; 2097 participants |
CI: confidence interval HES: hydroxyethyl starch n: number of participants with an event N: number of participants randomised to group RR: risk ratio
For the remaining eight studies, we found that more participants required a transfusion of blood product when starches were given (RR 1.19, 95% CI 1.02 to 1.39; 1917 participants; 8 studies; I² = 14%; Analysis 1.4).
1.4. Analysis.
Comparison 1 Starches vs crystalloid, Outcome 4 Transfusion of blood product.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had unclear risk of selection bias, one small study had a high risk of selection bias, and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 1.
Renal replacement therapy
Ten studies reported the number of participants who required renal replacement therapy or dialysis (Annane 2013; Bechir 2013; Brunkhorst 2008; Guidet 2012; James 2011; Mahrous 2013; McIntyre 2008; Myburgh 2012; Perner 2012; Vlachou 2010).
One study, which allowed type of colloid or crystalloid to be at the discretion of the clinician, combined data for all types of colloids (hydroxyethyl starch, gelatins, or albumin), and we could not include these data in analysis of starches (Annane 2013). We reported data for renal replacement therapy for this study in Table 6; we noted little or no difference between groups in the need for renal replacement therapy according to type of fluid.
We found that fewer participants were given renal replacement therapy when fluid resuscitation was with a crystalloid (RR 1.30, 95% CI 1.14 to 1.48; 8527 participants; 9 studies; I² = 0%; Analysis 1.5).
1.5. Analysis.
Comparison 1 Starches vs crystalloid, Outcome 5 Renal replacement therapy.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had unclear risk of selection bias and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 1.
Adverse events (allergic reaction, itching, rashes)
Six studies reported adverse event data for allergic reaction, itching, or rashes (Bulger 2008; Guidet 2012; Myburgh 2012; Ngo 2001; Perner 2012; Wills 2005).
Allergic reaction
We found little or no difference in allergic reaction according to whether starches or crystalloids were used (RR 2.59, 95% CI 0.27 to 24.91; 7757 participants; 3 studies; I² = 0%; Analysis 1.6).
1.6. Analysis.
Comparison 1 Starches vs crystalloid, Outcome 6 Adverse event: allergic reaction.
Itching
We found fewer incidences of itching when participants were given crystalloids (RR 1.38, 95% CI 1.05 to 1.82; 6946 participants; 2 studies; I² = 0%; Analysis 1.7).
1.7. Analysis.
Comparison 1 Starches vs crystalloid, Outcome 7 Adverse event: itching.
Rashes
We found little or no difference in incidences of rashes (RR 1.61, 95% CI 0.90 to 2.89; 7007 participants; 2 studies; I² = 0%; Analysis 1.8).
1.8. Analysis.
Comparison 1 Starches vs crystalloid, Outcome 8 Adverse event: rash.
We used GRADE, and assessed the level of certainty of the evidence for adverse events as very low. We downgraded the evidence by one level for study limitations because some studies had unclear risk of selection bias, and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. We downgraded the evidence by two levels for imprecision because few of our included studies reported data for these outcomes. See Table 1.
Subgroup analysis
Tonicity of crystalloid solution
We found that many studies did not report the solution in which the colloid was suspended. Two studies compared a starch and isotonic crystalloid versus an isotonic crystalloid and reported mortality outcome data (McIntyre 2008; Myburgh 2012), two studies compared a starch and isotonic crystalloid versus a hypertonic crystalloid (Brunkhorst 2008; Wills 2005), and three studies compared a starch and hypertonic crystalloid versus a hypertonic crystalloid (Bechir 2013; Du 2011; Heradstveit 2010). We did not perform subgroup analysis on all‐cause mortality (at end of follow‐up) for this comparison because we had insufficient studies to do so meaningfully.
Sensitivity analysis
Studies at high or unclear risk of selection bias
We excluded 10 studies that we judged to have unclear risk of selection bias (Brunkhorst 2008; Du 2011; Dubin 2010; Jie 2015; Li 2008; Lu 2012; Nagy 1993; Van der Heijden 2009; Younes 1998; Zhu 2011), and one study that we judged to have high risk of selection bias from analysis of the primary outcome (Cifra 2003). This did not alter interpretation of the effect, with little or no difference between groups in all‐cause mortality (at end of follow‐up) when these studies were excluded (RR 1.03, 95% CI 0.91 to 1.17; 10,139 participants; 13 studies; I² = 34%).
Studies in which some participants in the crystalloid group were given, or may have been given, additional colloids
Some studies were at risk of bias because some participants in the crystalloid group were given, or may have been given, additional colloids. We excluded seven studies from analysis of the primary outcome (Annane 2013; Brunkhorst 2008; Cifra 2003; Du 2011; Myburgh 2012; Perner 2012; Wills 2005). Although excluding these studies did not alter interpretation of the effect for analysis of all‐cause mortality (at end of follow‐up), we noted that without these studies statistical heterogeneity was reduced from 34% to 0% (RR 0.84, 95% CI 0.70 to 1.01; 1115 participants; 17 studies; I² = 0%).
Alternative meta‐analytical effects model (fixed‐effect)
Using the alternative meta‐analytical effects model (fixed‐effect), we found no difference in interpretation of the effect, with little or no difference between groups in all‐cause mortality (at end of follow‐up) (RR 1.01, 95% CI 0.95 to 1.08; 11,177 participants; 24 studies; I² = 34%).
Studies with discrepancies in data
In one study we noted discrepancies in mortality data within the study report (Dubin 2010). We removed this study from analysis and found that it made no difference to interpretation of the effect, with little or no difference between groups in all‐cause mortality (at end of follow‐up) (RR 0.98, 95% CI 0.87 to 1.10; 11,152 participants; 23 studies; I² = 33%).
2. Dextrans versus crystalloids
All‐cause mortality at end of follow‐up
Nineteen studies measured outcome data for mortality (Alpar 2004; Baker 2009; Bulger 2008; Bulger 2010; Bulger 2011; Chavez‐Negrete 1991; Hall 1978; Mattox 1991; Modig 1986; Morrison 2011; Ngo 2001; Oliveira 2002; Vassar 1990; Vassar 1991; Vassar 1993a; Vassar 1993b; Wills 2005; Younes 1992; Younes 1997).
Six studies were multi‐arm studies. We combined data in analysis for both crystalloid groups in Bulger 2010, Bulger 2011, Ngo 2001, Vassar 1993b, and Younes 1992, and we combined data in analysis for both colloid groups and both crystalloid groups in Vassar 1993a.
We included mortality data in this analysis in which the time point was: within 24 hours (Chavez‐Negrete 1991); within 48 hours (Hall 1978); until hospital discharge (Vassar 1991; Vassar 1993a; Vassar 1993b; Younes 1992); or was unknown (Alpar 2004; Modig 1986; Ngo 2001; Oliveira 2002; Wills 2005). The remaining studies reported data at 28 or 30 days (Baker 2009; Bulger 2008; Bulger 2010; Bulger 2011; Mattox 1991; Morrison 2011; Vassar 1990; Younes 1997).
We found little or no difference in the number of participants who died at end of follow‐up according to whether fluid resuscitation was with dextran or with a crystalloid (RR 0.99, 95% CI 0.88 to 1.11; 4736 participants; 19 studies; I² = 7%; Analysis 2.1).
2.1. Analysis.
Comparison 2 Dextrans vs crystalloid, Outcome 1 Mortality at end of follow‐up.
We generated a funnel plot to assess risk of publication bias. One study was an outlier in this plot, which we could not explain, but, because the only outlier was a small study from 1991 (Chavez‐Negrete 1991), we did not believe this was evidence of a high risk of publication bias. See Figure 5.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had unclear risk of selection bias and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 2.
All‐cause mortality within 90 days and within 30 days
Ten studies measured mortality within 30 days (Baker 2009; Bulger 2008; Bulger 2010; Bulger 2011; Chavez‐Negrete 1991; Hall 1978; Mattox 1991; Morrison 2011; Vassar 1990; Younes 1997). No studies reported mortality within 90 days, and we included the same data for both outcome time points for this comparison.
Two studies were multi‐arm studies (Bulger 2010; Bulger 2011). We combined the data in analysis for both crystalloid groups.
We included mortality data in this analysis in which the time point was: within 24 hours (Chavez‐Negrete 1991); within 48 hours (Hall 1978); and within 28 or 30 days (Baker 2009; Bulger 2008; Bulger 2010; Bulger 2011; Mattox 1991; Morrison 2011; Vassar 1990; Younes 1997).
We found little or no difference in the number of participants who died within 90 days and within 30 days according to whether fluid resuscitation was with dextran or with a crystalloid (RR 0.99, 95% CI 0.87 to 1.12; 3353 participants; 10 studies; I² = 0%; Analysis 2.2).
2.2. Analysis.
Comparison 2 Dextrans vs crystalloid, Outcome 2 Mortality within 90 days and 30 days.
We generated a funnel plot to assess risk of publication bias. One study was an outlier in this plot, which we could not explain, but, because the only outlier was a small study from 1991 (Chavez‐Negrete 1991), we did not believe this was evidence of a high risk of publication bias.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had unclear risk of selection bias and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 2.
Transfusion of blood products
Three studies reported the number of participants requiring a blood transfusion (Bulger 2011; Ngo 2001; Wills 2005). Bulger 2011, a multi‐arm study, reported blood transfusion of 9 units or fewer of blood, and 10 units or fewer of blood. In analysis, we combined data in the two crystalloids groups in Bulger 2011 for 9 units or fewer of blood.
We found little or no difference in participants requiring a transfusion of blood products according to whether participants were given dextran or a crystalloid (RR 0.92, 95% CI 0.77 to 1.10; 1272 participants; 3 studies; I² = 0%; Analysis 2.3).
2.3. Analysis.
Comparison 2 Dextrans vs crystalloid, Outcome 3 Transfusion of blood products.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as very low. We downgraded the evidence by two levels for study limitations because we noted that in two studies some participants were given additional colloids in the crystalloid group, and in another study we could not be certain whether some participants in the crystalloids groups had also received up to 2000 mL colloid resuscitation prior to randomisation. In addition, we were unable to assess risk of selective reporting bias because, for many studies there was a lack of prospective clinical trials registration. See Table 2.
Renal replacement therapy
No studies reported data for this outcome.
Adverse events (allergic reaction, itching, rashes)
Four studies reported allergic reactions (Mattox 1991; Ngo 2001; Vassar 1990; Vassar 1991), with event data in only one study (Ngo 2001).
We found little or no difference between study fluids in cases of allergic reaction (RR 6.00, 95% CI 0.25 to 144.93; 739 participants; 4 studies; Analysis 2.4).
2.4. Analysis.
Comparison 2 Dextrans vs crystalloid, Outcome 4 Adverse events: allergic reaction.
We used the GRADE approach to downgrade the certainty of the evidence for adverse events to very low. We downgraded by one level for study limitations because one study had an unclear risk of selection bias and we were unable to assess risk of selective outcome reporting bias in all studies. We downgraded by two levels for imprecision because evidence was from few studies with few events.
Subgroup analysis
Tonicity of crystalloid solution
Eight studies used a dextran solution with hypertonic saline (HSD) versus an isotonic crystalloid (which was normal saline) and reported mortality outcome data (Baker 2009; Bulger 2010; Bulger 2011; Morrison 2011; Oliveira 2002; Vassar 1993a; Younes 1992; Younes 1997); two studies used a dextran solution with an isotonic crystalloid versus a hypertonic crystalloid (Ringer's lactate) and reported mortality outcome data (Hall 1978; Wills 2005); and five studies used HSD versus Ringer's lactate and reported mortality outcome data (Alpar 2004; Bulger 2008; Chavez‐Negrete 1991; Vassar 1990; Vassar 1991). One multi‐arm study used two concentrations of HSD that were appropriate to combine in subgroup analysis versus two types of hypertonic crystalloid (hypertonic saline and Ringer's lactate), which were also appropriate to combine in subgroup analysis (Vassar 1993b). We did not include three studies in subgroup analysis because the type of crystalloid in which the dextran was suspended was not reported (Modig 1986; Ngo 2001), or a variety of crystalloids was used in the comparison group (Mattox 1991). We found no evidence of a difference between studies in use of isotonic or hypertonic crystalloid solutions for all‐cause mortality (at end of follow‐up) (P = 0.92). See Analysis 5.1.
5.1. Analysis.
Comparison 5 Dextrans vs crystalloid: subgroup by tonicity of crystalloid, Outcome 1 All‐cause mortality at end of follow‐up.
Sensitivity analysis
Studies at high or unclear risk of selection bias
We judged two studies to have high risk of selection bias (Alpar 2004; Modig 1986), and five studies to have unclear risk of selection bias (Chavez‐Negrete 1991; Hall 1978; Vassar 1990; Younes 1992; Younes 1997), and excluded them from analysis of mortality. This did not alter interpretation of the effect for all‐cause mortality (at the end of follow‐up); there was little or no difference between groups when these studies were excluded (RR 1.03, 95% CI 0.91 to 1.16; 3940 participants; 12 studies; I² = 6%).
Studies in which some participants in the crystalloid group were given, or may have been given, additional colloids
Some studies were at risk of bias because some participants in the crystalloid group were given, or may have been given additional colloids. We excluded six studies from analysis of mortality at end of follow‐up (Baker 2009; Bulger 2011; Chavez‐Negrete 1991; Ngo 2001; Vassar 1991; Wills 2005). This did not alter interpretation of the effect on all‐cause mortality (at end of follow‐up); there was little or no difference between groups when these studies were excluded (RR 1.00, 95% CI 0.88 to 1.15; 3185 participants; 13 studies; I² = 11%).
Alternative meta‐analytical effects model (fixed‐effect)
Using the alternative meta‐analytical effects model (fixed‐effect), did not alter interpretation of the effect on all‐cause mortality (at end of follow‐up); there was little or no difference between groups when we used the fixed‐effect model (RR 0.99, 95% CI 0.89 to 1.10; 4570 participants; 18 studies; I² = 7%).
Studies with discrepancies in data
We included no studies with serious discrepancies in data.
3. Gelatins versus crystalloids
All‐cause mortality at end of follow‐up
Six studies reported outcome data for mortality (Annane 2013; Evans 1996; Ngo 2001; Upadhyay 2005; Van der Heijden 2009; Wu 2001). One study reported the time point as within the ICU or hospital stay (Van der Heijden 2009), one study was at 90 days (Annane 2013), and the remaining time points were unknown.
One study was a multi‐arm study (Ngo 2001); we combined data in analysis for both crystalloid groups.
One study, which allowed type of colloid or crystalloid to be at the discretion of the clinician, reported mortality outcome data for participants who received only one type of fluid (Annane 2013). We included data for participants who received only gelatins in the colloid group, and combined data for two crystalloid groups (isotonic saline and Ringer's lactate).
We found little or no difference in the number of participants who had died from any cause at the end of follow‐up according to whether fluid resuscitation was with gelatins or with a crystalloid (RR 0.89, 95% CI 0.74 to 1.08; 1698 participants; 6 studies; I² = 0%; Analysis 3.1).
3.1. Analysis.
Comparison 3 Gelatins vs crystalloid, Outcome 1 Mortality at end of follow‐up.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as low. We downgraded the evidence by one level for study limitations because risk of selection bias was unclear in some studies and we were unable to assess risk of selective outcome reporting bias in some studies that were not registered with clinical trials registers. We downgraded by one level for imprecision because evidence was from few studies, and we could not be certain of time points for data collection. Table 3.
All‐cause mortality within 90 days
One study reported mortality data at 90 days (Annane 2013). This study allowed the type of colloid or crystalloid to be at the discretion of the clinician and reported mortality outcome data for participants who received only one type of fluid. We combined data for the two crystalloid groups (normal saline and Ringer's lactate) and used RevMan 5 to calculate an effect estimate (Review Manager 2014). Study data are reported in Table 6.
We found little or no difference in the number of participants who died from any cause within 90 days according to whether fluid resuscitation was with gelatins or with a crystalloid (RR 0.89, 95% CI 0.73 to 1.09; 1388 participants; 1 study).
We used GRADE, and assessed the level of certainty of the evidence for this outcome as low. We downgraded by two levels for imprecision because evidence was from a single study.
All‐cause mortality within 30 days
One study reported mortality data at 28 days (Annane 2013). This study allowed type of colloid or crystalloid to be at the discretion of the clinician and reported mortality outcome data for participants who received only one type of fluid. We combined data for the two crystalloid groups (isotonic saline and Ringer's lactate) and used the RevMan 5 to calculate an effect estimate (Review Manager 2014). Study data are reported in Table 6.
We found little or no difference in the number of participants who died from any cause within 30 days according to whether fluid resuscitation was with gelatins or with a crystalloid (RR 0.92, 95% CI 0.74 to 1.16; 1388 participants; 1 study).
We used GRADE, and assessed the level of certainty of the evidence for this outcome as low. We downgraded by two levels for imprecision because evidence was from a single study.
Transfusion of blood products
Three studies measured the number of participants who needed a transfusion of blood products (Annane 2013; Ngo 2001; Wu 2001). However, we could not use the data in Wu 2001, because it was not reported by group (five participants overall required blood transfusion), and we could not report the data in Annane 2013, because it was not reported separately for participants who received only gelatins (we noted little or no difference between people receiving either hydroxyethyl starch, gelatins, or albumin; Table 6).
The remaining study reported one participant in the gelatins group who required a blood transfusion following a severe epistaxis (Ngo 2001). We used the calculator in RevMan 5 (Review Manager 2014), and found little or no difference between groups in need for blood transfusion (RR 5.89, 95% CI 0.24 to 142.41; 167 participants; 1 study).
We used GRADE, and assessed the level of certainty of the evidence for this outcome as very low. We downgraded by one level for study limitations because we were unable to assess risk of selective outcome reporting bias due to lack of prospective clinical trials registration, and some participants in the crystalloid groups also received colloids. We downgraded two levels for imprecision because evidence was from a single small study with very few events.
Renal replacement therapy
One study, which allowed type of colloid or crystalloid to be at the discretion of the clinician, reported number of participants who required renal replacement therapy but did not report these data according to type of colloid received (Annane 2013). We did not include these data in our analysis of gelatins because the types of colloid used were either hydroxyethyl starch, gelatins, or albumin. We included data for renal replacement therapy for Annane 2013 in Table 6; we noted little or no difference between groups in the need for renal replacement therapy according to whether a colloid (hydroxyethyl starch, gelatins, or albumin) or a crystalloid was used.
Adverse events (allergic reaction, itching, rashes)
One study reported that five participants in the gelatins group had an allergic reaction (Ngo 2001). We used the calculator in RevMan 5 (Review Manager 2014), and found little or no difference between groups in incidences of allergic reactions (RR 21.61, 95% CI 1.22 to 384.05; 167 participants; 1 study).
We used GRADE, and assessed the level of certainty of the evidence for this outcome as very low. We downgraded by one level for study limitations because we were unable to assess risk of selective outcome reporting bias due to lack of prospective clinical trials registration, and because some participants in the crystalloid groups also received colloids. We downgraded two levels for imprecision because evidence was from a single small study with very few events.
Subgroup analysis
Tonicity of crystalloid solution
We found insufficient studies to conduct meaningful subgroup analysis. Of the six studies that reported mortality outcome data, five studies reported using a modified gelatin solution suspended in isotonic crystalloid solution. Two studies used Haemaccel (Evans 1996; Upadhyay 2005), two studies used Gelofusine (Van der Heijden 2009; Wu 2001), and one study used Gelafundin (Ngo 2001). The remaining study, in which type of colloid solution was at the discretion of the clinician, did not specify the gelatin solution (Annane 2013).
Sensitivity analysis
Studies at high or unclear risk of selection bias
We excluded one study that we judged to have an unclear risk of selection bias from analysis of mortality (Evans 1996). This did not alter interpretation of the effect for all‐cause mortality (at the end of follow‐up), with little or no difference between groups (RR 0.90, 95% CI 0.74 to 1.08; 1673 participants; 5 studies; I² = 0%).
Studies in which some participants in the crystalloid group were given, or may have been given, additional colloids
Some studies were at risk of bias because some participants in the crystalloid group were given, or may have been given additional colloids. We excluded two studies from analysis of the primary outcome (Annane 2013; Ngo 2001). This did not alter interpretation of the effect for all‐cause mortality (at the end of follow‐up), with little or no difference between groups (RR 0.94, 95% CI 0.52 to 1.72; 143 participants; 4 studies; I² = 0%).
Alternative meta‐analytical effects model (fixed‐effect)
Using the alternative meta‐analytical effects model (fixed‐effect) did not alter interpretation of the effect for all‐cause mortality (at the end of follow‐up), with little or no difference between groups (RR 0.89, 95% CI 0.74 to 1.08; 1689 participants; 6 studies; I² = 0%).
Studies with discrepancies in data
We included no studies with serious discrepancies in data.
4. Albumin or FFP versus crystalloids
All‐cause mortality at end of follow‐up
Twenty‐one studies reported mortality (Annane 2013; Caironi 2014; Cooper 2006; Finfer 2004; Goodwin 1983; Jelenko 1979; Lowe 1977; Lucas 1978; Maitland 2005; Maitland 2011; Martin 2005; McIntyre 2012; Metildi 1984; O'Mara 2005; Park 2015; Philips 2015; Pockaj 1994; Quinlan 2004; Rackow 1983; Shah 1977; Van der Heijden 2009). One study was a multi‐arm study and we combined data in analysis for both crystalloid groups (Jelenko 1979).
We did not include outcome data from one study (McIntyre 2012), as mortality data were reported overall, not by group (12 of 50 participants died).
We included mortality data in this analysis in which the time point was: within 24 hours (Rackow 1983); within seven days (Philips 2015); within the ICU or hospital stay (Van der Heijden 2009); within 90 days (Annane 2013; Caironi 2014); or was unknown (Goodwin 1983; Jelenko 1979; Lowe 1977; Lucas 1978; Maitland 2005; Metildi 1984; O'Mara 2005; Pockaj 1994; Shah 1977). The remaining studies reported data at 28 or 30 days.
We found little or no difference in the number of participants who had died from any cause at the end of follow‐up according to whether fluid resuscitation was with albumin or FFP compared to a crystalloid (RR 0.98, 95% CI 0.92 to 1.06; 13,047 participants; 20 studies; I² = 7%; Analysis 4.1).
4.1. Analysis.
Comparison 4 Albumin or FFP vs crystalloid, Outcome 1 Mortality at end of follow‐up.
We generated a funnel plot to assess risk of publication bias. One study was an outlier in this plot, which we could not explain, but, because the only outlier was a small study from 1978, we did not believe this was evidence of a high risk of publication bias. See Figure 6.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had unclear risk of selection bias, and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 4.
All‐cause mortality within 90 days
Eleven studies measured mortality within 90 days (Annane 2013; Caironi 2014; Cooper 2006; Finfer 2004; Maitland 2011; Martin 2005; McIntyre 2012; Park 2015; Philips 2015; Quinlan 2004; Rackow 1983). We did not include outcome data from one study (McIntyre 2012), as mortality data were reported overall, not by group (12 of 50 participants died).
We included mortality data in this analysis in which the time point was: within 24 hours (Rackow 1983); within seven days (Philips 2015); within 30 days (Cooper 2006; Finfer 2004; Maitland 2011; Martin 2005; Park 2015; Quinlan 2004); and within 90 days (Annane 2013; Caironi 2014).
We found little or no difference in the number of participants who died from any cause within 90 days according to whether fluid resuscitation was with albumin or FFP compared to a crystalloid (RR 0.98, 95% CI 0.92 to 1.04; 12,492 participants; 10 studies; I² = 0%; Analysis 4.2).
4.2. Analysis.
Comparison 4 Albumin or FFP vs crystalloid, Outcome 2 Mortality within 90 days.
We generated a funnel plot to assess risk of publication bias. One study was an outlier in this plot, which we could not explain; we could not be certain whether this indicated risk of publication bias.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had unclear risk of selection bias, and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 4.
All‐cause mortality within 30 days
Eleven studies measured mortality within 30 days (Annane 2013; Caironi 2014; Cooper 2006; Finfer 2004; Maitland 2011; Martin 2005; McIntyre 2012; Park 2015; Philips 2015; Quinlan 2004; Rackow 1983). We did not include outcome data from one study (McIntyre 2012), as mortality data were reported overall, not by group (12 of 50 participants died).
We included mortality data in this analysis in which the time point was: within 24 hours (Rackow 1983); within seven days (Philips 2015); or within 28 or 30 days (Annane 2013; Caironi 2014; Cooper 2006; Finfer 2004; Maitland 2011; Martin 2005; Park 2015; Quinlan 2004).
We found little or no difference in the number of participants who died from any cause within 30 days according to whether fluid resuscitation was with albumin or FFP compared to a crystalloid (RR 0.99, 95% CI 0.93 to 1.06; 12,506 participants; 10 studies; I² = 0%; Analysis 4.3).
4.3. Analysis.
Comparison 4 Albumin or FFP vs crystalloid, Outcome 3 Mortality within 30 days.
We generated a funnel plot to assess risk of publication bias. One study was an outlier in this plot, which we could not explain; we could not be certain whether this indicated risk of publication bias.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as moderate. We downgraded the evidence by one level for study limitations because some studies had unclear risk of selection bias, and because, for many studies, we were unable to assess risk of selective reporting bias due to lack of prospective clinical trials registration. See Table 4.
Transfusion of blood products
Four studies reported outcome data for transfusion of blood products (Annane 2013; Cooper 2006; Lowe 1977; Pockaj 1994).
One study, which allowed type of colloid or crystalloid to be at the discretion of the clinician, reported the number of participants who received a blood product, but these data were not reported according to type of colloid received (Annane 2013). We did not include these data in analysis of albumin or FFP because the types of colloid used were either hydroxyethyl starch, gelatins, or albumin. We included data for transfusion of blood products for Annane 2013 in Table 6; we noted little or no difference between groups in the need for blood products according to whether participants were given a colloid (hydroxyethyl starch, gelatins, or albumin) or a crystalloid.
We found little or no difference in the number of participants who had transfusion of blood products according to whether fluid resuscitation was with albumin or FFP compared to a crystalloid (RR 1.31, 95% CI 0.95 to 1.80; 290 participants; 3 studies; I² = 0%; Analysis 4.4).
4.4. Analysis.
Comparison 4 Albumin or FFP vs crystalloid, Outcome 4 Transfusion of blood product.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as very low. We downgraded the evidence by two levels for study limitations because some studies had unclear risk of selection bias, and we noted baseline imbalances in one study. We downgraded by one level for imprecision because analysis included few studies with few participants. See Table 4.
Renal replacement therapy
Four studies collected outcome data related to renal replacement therapy (Annane 2013; Caironi 2014; Finfer 2004; Park 2015).
One study, which allowed type of colloid or crystalloid to be at the discretion of the clinician, reported the number of participants who required renal replacement therapy, but these data were not reported according to type of colloid received (Annane 2013). We did not include these data in analysis of albumin or FFP because the types of colloid used were either hydroxyethyl starch, gelatins, or albumin. We included data for renal replacement therapy for Annane 2013 in Table 6; we noted little or no difference between groups in the need for renal replacement therapy according to type of fluid. The study report for Park 2015 was an abstract that stated that renal replacement therapy was a secondary outcome, but outcome data were not reported in the abstract. Data in Finfer 2004 were reported for a smaller subgroup of participants who had severe sepsis; we included these data in the analysis.
We noted little or no difference according to type of fluid resuscitation in the number of participants who received renal replacement therapy (RR 1.11, 95% CI 0.96 to 1.27; 3028 participants; 2 studies; I² = 0%; Analysis 4.5).
4.5. Analysis.
Comparison 4 Albumin or FFP vs crystalloid, Outcome 5 Renal replacement therapy.
We used GRADE, and assessed the level of certainty of the evidence for this outcome as low. We downgraded the evidence by two levels for study limitations because we noted baseline imbalances and because we could not be certain whether participants in the crystalloids group in one study may have received colloids. See Table 4.
Adverse events (allergic reaction, itching, rashes)
One study reported incidences of allergic reaction (Maitland 2011). We used RevMan 5 to calculate an effect estimate (Review Manager 2014); we noted little or no difference between groups in allergic reactions (RR 0.75, 95% CI 0.17 to 3.33; 2097 participants; 1 study; Table 6).
We used the GRADE approach to downgrade the certainty of the evidence to very low. We downgraded by one level for study limitations because we were unable to assess the risk of selective outcome reporting bias since the study authors did not report clinical trials registration. We downgraded by two levels because evidence was from one study with few events. See Table 4.
Subgroup analysis
Tonicity of crystalloid solution
We found that many studies did not report the solution in which the colloid was suspended. One study used albumin with an isotonic crystalloid (suspended in normal saline) versus an isotonic crystalloid (normal saline) (Pockaj 1994), and one study used albumin with an isotonic crystalloid (normal saline) versus a hypertonic crystalloid (Ringer's lactate) (Cooper 2006). One study used albumin with a hypertonic crystalloid (hypertonic saline) versus a hypertonic crystalloid (Ringer's lactate) (Jelenko 1979), and five studies used albumin with a hypertonic crystalloid (Ringer's lactate) versus a hypertonic crystalloid (Ringer's lactate) (Goodwin 1983; Lowe 1977; Metildi 1984; O'Mara 2005; Shah 1977). We found insufficient studies to conduct meaningful subgroup analysis.
Sensitivity analysis
Studies at high or unclear risk of selection bias
We excluded two studies that we judged to have high risk of selection bias (Lowe 1977; Lucas 1978), and nine studies that we judged to have unclear risk of selection bias from analysis of mortality (Goodwin 1983; Maitland 2005; Metildi 1984; Park 2015; Philips 2015; Pockaj 1994; Quinlan 2004; Rackow 1983; Shah 1977). This did not alter interpretation of the effect for all‐cause mortality (at end of follow‐up), with little or no difference between groups (RR 0.98, 95% CI 0.91 to 1.04; 12,111 participants; 9 studies; I² = 0%).
Studies in which some participants in the crystalloid group were given, or may have been given, additional colloids
Some studies were at risk of bias because some participants in the crystalloid group were given, or may have been given, additional colloids. We excluded three studies from analysis of mortality (Annane 2013; Finfer 2004; Goodwin 1983). This did not alter interpretation of the effect for all‐cause mortality (at end of follow‐up), with little or no difference between groups (RR 0.96, 95% CI 0.88 to 1.04; 4970 participants; 17 studies; I² = 0%).
Alternative meta‐analytical effects model (fixed‐effect)
Using the alternative meta‐analytical effects model (fixed‐effect) did not alter interpretation of the effect for all‐cause mortality (at end of follow‐up), with little or no difference between groups (RR 0.99, 95% CI 0.93 to 1.05; 13,047 participants; 20 studies; I² = 7%).
Studies with discrepancies in data
We noted a discrepancy in mortality outcome data in different published reports for Lucas 1978. In sensitivity analysis, we used alternative data reported in a later publication, Lucas 1980, which is cited as part of Lucas 1978. This did not alter interpretation of the effect for all‐cause mortality (at end of follow‐up), with little or no difference between groups (RR 0.98, 95% CI 0.92 to 1.04; 13,047 participants; 20 studies; I² = 0%).
Discussion
Summary of main results
We included 69 studies comparing colloids (suspended in any solution) versus crystalloids (isotonic or hypertonic) in critically ill people who required fluid resuscitation. In addition, we identified seven studies that are awaiting classification (two studies were published only as abstracts with insufficient information, three completed studies are listed on clinical trials register sites without publication of full reports, and two studies require translation from Russian), and three ongoing studies.
We reported four comparisons for each type of colloid (starches; dextrans; gelatins; and albumin or FFP) versus crystalloids. We collected outcome data for all‐cause mortality at end of follow‐up, within 90 days, and within 30 days; need for transfusion of blood products; need for renal replacement therapy; and adverse events (allergic reaction, itching, and rashes).
We found moderate‐certainty evidence that there is probably little or no difference in all‐cause mortality at the end of follow‐up, within 90 days, or within 30 days between colloids (which are: starches; dextrans; or albumin or FFP) or crystalloids for fluid resuscitation. We found low‐certainty evidence that there may be little or no difference in all‐cause mortality at the end of follow‐up, within 90 days, or within 30 days between gelatins or crystalloids for fluid resuscitation.
We found moderate‐certainty evidence that using starches probably slightly increases the need for transfusion of blood products. Studies comparing dextrans, gelatins, and albumin or FFP to crystalloids, found little or no difference in the need for transfusion of blood products but certainty of this evidence was very low.
We found moderate‐certainty evidence that using starches probably slightly increases the need for renal replacement therapy. We found low‐certainty evidence from two studies that albumin or FFP versus crystalloids may make little or no difference to the need for renal replacement therapy. We could not use data from renal replacement therapy from one study of gelatins because data were not reported by type of colloid solution, and no studies of dextrans measured this outcome.
Evidence for adverse events (allergic reactions, itching, or rashes) is very low certainty because studies often did not report events. For starches, we found little or no difference between either fluid group in allergic reactions in three studies, but we found more incidences of itching and rashes in two studies. For dextrans, gelatins, and for albumin or FFP, we found little or no difference between groups in allergic reactions.
Overall completeness and applicability of evidence
We identified 69 studies with 30,020 participants who were undergoing fluid resuscitation for conditions that indicated that they were critically ill. The conditions being managed with fluid resuscitation varied, and settings also varied; 10 studies were based in an out‐of‐hospital setting.
All studies compared colloids versus crystalloids. We found 28 studies using starch solutions, 20 studies using dextran solutions, seven studies using gelatins, and 22 studies using albumin or FFP. Some study authors did not report the specific nature of the solution the colloid was suspended in, and other studies reported the use of either an isotonic or hypertonic crystalloid suspension solution. Because of the different use of crystalloid solutions for this purpose, and the different compositions of the comparative crystalloids, we could not be certain whether comparisons by type of colloid were always equivalent. We were unable to perform meaningful subgroup analysis for most types of colloids because of limitations in reporting of suspension solutions. Also, individual study protocols for the concentration, quantity, and timing of administration of fluids varied.
We also noted that studies ranged in date of publication from 1977 to 2016, and, while we did not consider the potential influence of date on our results, it is possible that changes in management of critically ill people may mean that some study data may not be generalisable to the current clinical context.
Quality of the evidence
We used GRADE to consider the effect of study limitations on our outcomes. We found many studies did not report adequate methods of randomisation or allocation concealment, and we could not be certain of the risk of selection bias. We noted that some studies did not report whether clinicians were blinded to the type of study fluids they were giving to participants, or whether outcome assessors were blinded. However, we did not consider risk of performance or detection bias to be likely for mortality, and we did not believe lack of performance or detection bias for our remaining outcomes (transfusion of blood products, renal replacement therapy, or adverse events) were important reasons to downgrade the evidence for this review. We noted that few studies were registered prospectively with clinical trials registers, and although many studies predate the expectation of clinical trials registration, we could not rule out the risk of selective outcome reporting in this review. We included some studies in which some participants in the crystalloid groups were given, or may have been given, additional colloids. Because we could not be certain of the influence of this additional colloid use on the results, we judged these studies to have a high risk of bias and downgraded the certainty of the evidence accordingly. We downgraded the certainty of the evidence for some of our outcomes because of imprecision; for these outcomes, we found evidence from few studies.
Potential biases in the review process
We conducted a thorough search and used two review authors independently to assess study eligibility, extract data, and assess risk of bias in included studies, and believe that this reduced potential bias in the review process. However, we made a post hoc decision to change criteria for considering studies in this review update from the previous version of the review (Perel 2013). This decision led to the exclusion of 36 previously included studies. Our intention was to create a more focused review, with a more comparable participant group, once we had excluded participants scheduled for a wide range of elective surgical procedures; we acknowledge that the exclusion of this large number of studies may also have influenced a change in results since the previous review publication.
We included a number of studies in the review in which participants in the crystalloid group may have received additional colloids. It is possible that our decision to include these studies in our primary analysis may have introduced clinical differences, or bias, between studies, and subsequently influenced our results. We assessed this decision during sensitivity analysis for our primary outcome (all‐cause mortality (at end of follow‐up)) and found that the interpretation of our effect estimates was the same regardless of whether we included these studies. However, we noted that in our comparison of starches versus crystalloids, inclusion of these studies increased statistical heterogeneity (I² = 34%); we did not explore this further in the review.
We included additional outcomes in this review; we intended to explore other effects of colloids and crystalloids for fluid resuscitation. We limited these additional outcomes to need for blood transfusion, need for renal replacement therapy, and three possible adverse events (allergic reactions, itching, and rashes). We acknowledge that our review is limited to only eight outcomes in four types of colloid solutions, and therefore does not explore all the potential risks and benefits of using either colloids or crystalloids in the critically ill setting.
The review does not include seven studies that are awaiting classification (Halim 2016; Bulanov 2004; Charpentier 2011; NCT00890383; NCT01337934; NCT02064075; Protsenko 2009). We did not seek translation of the full study reports for four studies that were reported in Chinese (Jie 2015; Li 2008; Lu 2012; Zhu 2011); our judgements and data were limited to information available in the abstract, or the tables.
Agreements and disagreements with other studies or reviews
The results of this review differ from those of the previous version (Perel 2013), which found an increase in mortality when participants were given starches rather than crystalloids for fluid resuscitation. For this 2018 update, because of changes in the criteria for considering studies in this review, we excluded studies of elective surgical patients. However, because of a decision to include additional outcomes, we re‐ran searches from database inception and included 27 new studies in the review, 13 of which compared starches to crystalloids. Our moderate‐certainty evidence, which demonstrates little or no difference in all‐cause mortality for starches, includes a large number of studies, but we cannot be certain whether the difference in our results is because we excluded elective surgical patients. Results for mortality for dextrans, gelatins, and albumin or FFP were the same as those in Perel 2013.
Whilst other systematic reviews may concentrate on particular types of colloids, or particular participant groups, our findings for mortality appear relatively comparable. He 2015 found no increase in mortality with hydroxyethyl starch for non‐septic patients in the intensive care unit, as did Haase 2013 for patients with sepsis. However, Gattas 2013, which included participants undergoing surgical procedures, reported a non‐statistically significant increase in mortality when starches were used. In reviews of other colloids, de Crescenzo 2017 found no effect on mortality of trauma patients treated in a prehospital setting with dextrans; Qureshi 2016 found no increase in mortality of critically ill, trauma, and surgical patients with any type of colloid; and Eljaiek 2017 found no difference in mortality of burn patients who were given albumin for fluid replacement.
Also, we found some comparable results for renal replacement and blood transfusion. Haase 2013 and Gattas 2013 found that more participants given starches required renal replacement therapy, whilst Haase 2013 also found this effect with starches for transfusion of red blood cells. Similarly, Qureshi 2016 found an increase in acute kidney failure requiring renal replacement that was more pronounced for those who were given fluid resuscitation with starches, but this result was not replicated by He 2015, who found no difference in incidence of renal replacement therapy with use of starches.
Authors' conclusions
Implications for practice.
We found moderate‐certainty evidence that there is probably little or no difference in all‐cause mortality at the end of follow‐up, at 90 days, or at 30 days, between using colloids (starches; dextrans; or albumin or FFP) or crystalloids for fluid resuscitation in critically ill people. We found low‐certainty evidence that there may be little or no difference in all‐cause mortality at these time points between gelatins or crystalloids for fluid resuscitation. Our evidence for all‐cause mortality at the end of follow‐up came from 24 studies of starch solutions, 19 studies of dextrans, six studies of gelatins, and 20 studies of albumin or FFP.
However, we found moderate‐certainty evidence of a slight increase in the need for blood transfusion or renal replacement therapy when starches were used for fluid resuscitation. Whilst evidence for adverse events was very low because most studies did not report these events, we found no evidence of a difference in allergic reactions with starches from three studies, and two studies reported more incidences of itching and rashes when starches were used.
For other colloid solutions, we found little or no difference in the need for blood transfusion for dextrans, gelatins, or for albumin or FFP versus crystalloids but this was very low‐certainty evidence. We found low‐certainty evidence from two studies that albumin or FFP versus crystalloids may make little or no difference to the need for renal replacement therapy. Similarly, evidence for adverse events for dextrans, gelatins, or albumin or FFP was limited to few studies and was very low certainty: we found little or no difference in allergic reactions between dextrans, gelatins, or albumin or FFP compared to crystalloids.
The previous version of this review found that starches might increase mortality, and therefore, differs from the conclusion of this review. However, evidence for this new 2018 version of the review does not include participants who were undergoing elective surgical procedures.
Implications for research.
Whilst this review included a large body of evidence reporting outcome data for mortality, we found that few studies reported the number of participants that required transfusion of blood products, required renal replacement therapy, or experienced other adverse events (allergic reactions, itching, and rashes). Consequently, certainty in our evidence for some comparative colloids was limited because of few studies. We found three ongoing studies, and seven studies awaiting classification (of which three are completed studies without published reports). Inclusion of these studies in future updates may contribute additional evidence to the review.
We would advise future studies of fluid resuscitation of colloids versus crystalloids to consider blood transfusion and renal replacement therapy as relevant outcomes for consideration, and to provide comprehensive reporting of possible adverse events. We would also advise that studies are managed to avoid the risk of additional colloid solutions being given to some participants in the crystalloids study arm. Improved reporting of suspension solutions when colloids are given would allow for beneficial subgroup analysis for the potential effect of isotonic or hypertonic crystalloids.
What's new
| Date | Event | Description |
|---|---|---|
| 1 May 2018 | New citation required and conclusions have changed | We found that there was probably little or no difference in mortality according to whether starches or crystalloids were used for fluid resuscitation. Mortality data for other types of colloids remained the same. |
| 1 May 2018 | New search has been performed | New authors added (Sharon Lewis, Michael Pritchard, Andrew Butler, David Evans, Andrew Smith, Phil Alderson). Two review authors removed (Pablo Perel and Katharine Ker). Edits made to the Background and Methods sections. Change to criteria for considering studies in the review (we excluded elective surgery). Added three new outcomes (transfusion of blood products, need for renal replacement therapy; adverse events ‐ allergic reaction, itching, rashes). We reassessed all studies included in the previous version of the review and excluded studies that did not meet the new inclusion criteria. We completed data extraction and risk of bias on all studies, including those from the previous version of the review. We added a 'Summary of findings' table for each of four comparisons by type of colloid (starches; dextrans; gelatins; and albumin or fresh frozen plasma). |
History
Protocol first published: Issue 4, 1997 Review first published: Issue 4, 1997
| Date | Event | Description |
|---|---|---|
| 25 February 2013 | Amended | Minor corrections made to the results section. |
| 31 January 2013 | New citation required and conclusions have changed | New study data have been included. The conclusions of the review have changed. |
| 17 January 2013 | New search has been performed | Four new studies have been included (Guidet 2012, Lee 2011, Myburgh 2012, and Perner 2012). Mortality data from a reply letter (http://bja.oxfordjournals.org/content/107/5/693/reply) of a previous included study was added (James 2011). |
| 17 October 2012 | Amended | Copy edits made to graph labels. |
| 8 June 2012 | Amended | Copy edits made and citation corrected. |
| 14 May 2012 | New citation required but conclusions have not changed | An updated search was conducted in March 2012. Nine new trials have been included (Bulger 2011; Cooper 2006; Du 2011; Dubin 2010; James 2011; Lu 2012; Maitland 2011; McIntyre 2008; Zhu 2011). The analysis and results sections have been revised accordingly. The conclusions remain unchanged. Three ongoing studies were identified (CHEST Trial; RASP trial; The 6S trial). We plan to update this review once the CHEST Trial (a large phase 3 trial comparing 6% hydroxyethyl starch and saline) is published. |
| 16 March 2012 | New search has been performed | An updated search was conducted in March 2012. |
| 10 February 2011 | New citation required but conclusions have not changed | The editorial group is aware that a clinical trial by Prof. Joachim Boldt has been found to have been fabricated (Boldt 2009). As the editors who revealed this fabrication point out (Reinhart 2011; Shafer 2011), this casts some doubt on the veracity of other studies by the same author. All Cochrane Injuries Group reviews which include studies by this author have therefore been edited to show the results with this author's trials included and excluded. Readers can now judge the potential impact of trials by this author (Boldt 1986, Boldt 1993, Boldt 2001, Lang 2001, Lang 2003) on the conclusions of the review. The authors of the review have changed. |
| 17 April 2009 | New search has been performed | April 2009 An updated search for new trials was conducted in October 2008. One new study was included (Brunkhorst 2008). The analysis, results and discussion sections have been revised accordingly. |
| 16 July 2008 | Amended | Converted to new review format. |
| 1 July 2007 | New search has been performed | August 2007 An updated search for new trials was conducted in December 2006. Ten new studies were included (Evans 2003, Cifra 2003, Fries 2004, Guo 2003, Lang 2003, Maitland 2005, Moretti 2003, Upadhyay 2004, Verheij 2006, Wills 2005). The analysis, results and discussion sections have been revised accordingly. |
Acknowledgements
We acknowledge the contribution of Frances Bunn, Paul Chinnock, Gillian Schierhout, Mia Pearson, Pablo Perel, and Katharine Ker who were authors of earlier versions of this review.
We acknowledge the contribution of those who peer reviewed this 2018 update: Anders Perner and Joseph Ting.
Ian Roberts, an author of this review, is also one of the Co‐ordinating Editors of the Injuries Group. In order to avoid a potential conflict of interest, the editorial base of the Injuries Group requested, and received, editorial assistance from Liz Bickerdike, the Associate Editor of the Cochrane Acute and Emergency Care Network.
This project was supported by the National Institute for Health Research (NIHR) Cochrane Review Incentive Scheme, Department of Health, UK. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor Plasma Volume explode all trees #2 MeSH descriptor Fluid Therapy explode all trees #3 MeSH descriptor Resuscitation explode all trees #4 (fluid* OR volume OR plasma OR rehydrat* OR blood OR oral) next (replac* OR therapy OR substitut* OR restor* OR resuscitat* OR rehydrat*):ti,ab,kw #5 (#1 OR #2 OR #3 or #4) #6 MeSH descriptor Colloids explode all trees #7 MeSH descriptor Hetastarch explode all trees #8 MeSH descriptor Rehydration Solutions explode all trees #9 MeSH descriptor Isotonic Solutions explode all trees #10 MeSH descriptor Serum explode all trees #11 MeSH descriptor Plasma explode all trees #12 MeSH descriptor Plasma Substitutes explode all trees #13 MeSH descriptor Albumins explode all trees #14 MeSH descriptor Serum Albumin explode all trees #15 (colloid* OR hydrocolloid* or crystalloid* OR albumin* OR albumen* OR plasma OR starch* OR dextran* OR gelofus* OR hemaccel* OR haemaccel* OR serum OR hetastarch OR isotonic OR ringer* OR gelatin* OR gentran* OR pentastarch* OR pentaspan* OR hartman OR sodium OR potassium OR saline):ti #16 (Isotonic next saline next solution*) OR (Blood next substitut*) OR (blood next expan*) OR (plasma next volume next expan*) OR (volume next expan*) #17 (#6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16) #18 (#5 AND #17)
Appendix 2. MEDLINE Ovid search strategy
1. exp Plasma Volume/ 2. exp Fluid Therapy/ 3. exp Resuscitation/ 4. ((fluid* or volume or plasma or rehydrat* or blood or oral) adj1 (replac* or therapy or substitut* or restor* or resuscitat* or rehydrat*)).ab,ti. 5. 1 or 2 or 3 or 4 6. exp Colloids/ 7. exp Hetastarch/ 8. exp Rehydration Solutions/ 9. exp Isotonic Solutions/ 10. exp Serum/ 11. exp Plasma/ 12. exp Plasma Substitutes/ 13. exp Albumins/ 14. exp Serum Albumin/ 15. (colloid* or hydrocolloid* or crystalloid* or albumin* or albumen* or plasma or starch* or dextran* or gelofus* or hemaccel* or haemaccel* or serum or hetastarch or isotonic or ringer* or gelatin* or gentran* or pentastarch* or pentaspan* or hartman or sodium or potassium or saline).ti. 16. ((Isotonic adj1 saline adj1 solution*) or (Blood adj1 substitut*) or (blood adj1 expan*) or (plasma adj1 volume adj1 expan*) or (volume adj1 expan*)).ab,ti. 17. or/6‐16 18. 5 and 17 19. randomi?ed.ab,ti. 20. randomized controlled trial.pt. 21. controlled clinical trial.pt. 22. placebo.ab. 23. clinical trials as topic.sh. 24. randomly.ab. 25. trial.ti. 26. 19 or 20 or 21 or 22 or 23 or 24 or 25 27. (animals not (humans and animals)).sh. 28. 26 not 27 29. 18 and 28
Appendix 3. Embase Ovid search strategy
1. exp plasma volume/ 2. exp fluid therapy/ 3. exp fluid resuscitation/ 4. ((fluid* or volume or plasma or rehydrat* or blood or oral) adj1 (replac* or therapy or substitut* or restor* or resuscitat* or rehydrat*)).ab,ti. 5. 1 or 2 or 3 or 4 6. exp colloid/ 7. exp hetastarch/ 8. exp "solution and solubility"/ 9. exp isotonic solution/ 10. exp serum/ 11. exp serum albumin/ 12. exp crystalloid/ 13. exp hetastarch/ 14. exp plasma/ 15. exp plasma substitute/ 16. exp albumin/ 17. exp serum albumin/ 18. or/6‐17 19. (th or ad orIV).fs. 20. 18 and 19 21. (colloid* or hydrocolloid* or crystalloid* or albumin* or albumen* or plasma or starch* or dextran* or gelofus* or hemaccel* or haemaccel* or serum or hetastarch or isotonic or ringer* or gelatin* or gentran* or pentastarch* or pentaspan* or hartman or sodium or potassium or saline).ti. 22. ((Isotonic adj1 saline adj1 solution*) or (Blood adj1 substitut*) or (blood adj1 expan*) or (plasma adj1 volume adj1 expan*) or (volume adj1 expan*)).ab,ti. 23. 20 or 21 or 22 24. exp Randomized Controlled Trial/ 25. exp controlled clinical trial/ 26. randomi?ed.ab,ti. 27. placebo.ab. 28. *Clinical Trial/ 29. randomly.ab. 30. trial.ti. 31. 24 or 25 or 26 or 27 or 28 or 29 or 30 32. exp animal/ not (exp human/ and exp animal/) 33. 31 not 32 34. 5 and 23 and 33
Appendix 4. PubMed search strategy
(((((((colloid* OR hydrocolloid* OR crystalloid* OR albumin* OR albumen* OR plasma OR starch* OR dextran* OR gelofus* OR hemaccel* OR haemaccel* OR serum OR hetastarch OR isotonic OR ringer* OR gelatin* OR gentran* OR pentastarch* OR pentaspan* OR hartman OR sodium OR potassium OR saline) AND title)) OR (colloids[MeSH Terms]))) AND ((((fluid* OR volume OR plasma OR rehydrat* OR blood OR oral) AND (replac* OR therapy OR substitut* OR restor* OR resuscitat* OR rehydrat*))) OR (((plasma volume[MeSH Terms]) OR fluid therapy) OR resuscitation)))) AND ((randomised OR randomized OR randomly OR random order OR random sequence OR random allocation OR randomly allocated OR at random OR randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized controlled trials[mh]) NOT ((models, animal[mh] OR Animals[mh] OR Animal Experimentation[mh] OR Disease Models, Animal[mh] OR Animals, Laboratory[mh]) NOT (Humans[mh])))
Appendix 5. Web of Science search strategy
#1 colloid* OR hydrocolloid* or crystalloid* #2 (Isotonic NEAR/1 saline NEAR/1 solution*) OR (Blood NEAR/1 substitut*) OR (blood NEAR/1 expan*) OR (plasma NEAR/1 volume NEAR/1 expan*) OR (volume NEAR/1 expan*) #3 #1 OR #2 #4 (fluid* OR volume OR plasma OR rehydrat* OR blood OR oral) NEAR/2 (replac* OR therapy OR substitut* OR restor* OR resuscitat* OR rehydrat*) #5 (random*) NEAR/3 (study or trial) #6 (singl* OR doubl* OR trebl* OR tripl*) NEAR/3 (blind* OR mask*) NEAR/3 (study or trial) #7 #6 OR #5 #8 #7 AND #4 AND #3
Appendix 6. ClinicalTrials.gov search strategy
colloid AND crystalloid
Appendix 7. WHO ICTRP search strategy
colloid AND crystalloid
Appendix 8. OpenGrey search strategy
colloid OR crystalloid
Data and analyses
Comparison 1. Starches vs crystalloid.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality at end of follow‐up | 24 | 11177 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.86, 1.09] |
| 2 Mortality within 90 days | 15 | 10415 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.90, 1.14] |
| 3 Mortality within 30 days | 11 | 10135 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.90, 1.09] |
| 4 Transfusion of blood product | 8 | 1917 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [1.02, 1.39] |
| 5 Renal replacement therapy | 9 | 8527 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.14, 1.48] |
| 6 Adverse event: allergic reaction | 3 | 7757 | Risk Ratio (M‐H, Random, 95% CI) | 2.59 [0.27, 24.91] |
| 7 Adverse event: itching | 2 | 6946 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [1.05, 1.82] |
| 8 Adverse event: rash | 2 | 7007 | Risk Ratio (M‐H, Random, 95% CI) | 1.61 [0.90, 2.89] |
Comparison 2. Dextrans vs crystalloid.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality at end of follow‐up | 19 | 4736 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.88, 1.11] |
| 2 Mortality within 90 days and 30 days | 10 | 3353 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.87, 1.12] |
| 3 Transfusion of blood products | 3 | 1272 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.77, 1.10] |
| 4 Adverse events: allergic reaction | 4 | 738 | Risk Ratio (M‐H, Random, 95% CI) | 6.0 [0.25, 144.93] |
Comparison 3. Gelatins vs crystalloid.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality at end of follow‐up | 6 | 1698 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.74, 1.08] |
Comparison 4. Albumin or FFP vs crystalloid.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality at end of follow‐up | 20 | 13047 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.92, 1.06] |
| 2 Mortality within 90 days | 10 | 12492 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.92, 1.04] |
| 3 Mortality within 30 days | 10 | 12506 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.06] |
| 4 Transfusion of blood product | 3 | 290 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.95, 1.80] |
| 5 Renal replacement therapy | 2 | 3028 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.96, 1.27] |
Comparison 5. Dextrans vs crystalloid: subgroup by tonicity of crystalloid.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 All‐cause mortality at end of follow‐up | 16 | 4247 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.90, 1.13] |
| 1.1 colloid + hypertonic crystalloid vs isotonic crystalloid | 8 | 2845 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.87, 1.13] |
| 1.2 colloid + isotonic crystalloid vs hypertonic crystalloid | 2 | 493 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.62, 2.06] |
| 1.3 colloid + hypertonic crystalloid vs hypertonic crystalloid | 6 | 909 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.74, 1.41] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alpar 2004.
| Methods | Quasi‐RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 180 Inclusion criteria: patients admitted to MIU Exclusion criteria: no details Participant condition: head, chest, abdominal injuries Baseline characteristics Colloids group
Crystalloids group
Country: UK Setting: MIU |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic analysis; urine outputs; recovery; LoS Outcomes relevant to the review: mortality (time not reported) |
|
| Notes |
Funding/declarations of interest: none apparent Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate participants added to each group based on odd/even numbers |
| Allocation concealment (selection bias) | High risk | Alternate allocation used and therefore unlikely to be concealed |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; not likely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Unclear risk | The proportion of participants in each arm with chest injuries differed. It is unclear whether this influenced results. |
| Other bias | Low risk | No other sources of bias identified |
Annane 2013.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 2857 Inclusion criteria: no prior fluid resuscitation in ICU; required fluid resuscitation for acute hypovolaemia Exclusion criteria: received fluid resuscitation in ICU; anaesthesia‐related hypotension; advanced chronic liver disease; acute anaphylactic reaction; inherited coagulation disorders; do‐not‐resuscitate order; pregnant; burned > 20% of TBSA; allergy to study drug; refused consent; dehydrated; brain death or organ donor; other (not specified) Participant condition: acute hypovolaemia, sepsis, and trauma Baseline characteristics Colloids group
Crystalloids group
Country: France, Belgium, Canada, Algeria, Tunisia Setting: ICU |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: mortality at 28 days; mortality at 90 days and at ICU and hospital discharge; number of days alive and not receiving renal replacement therapy, mechanical ventilation or vasopressor therapy; days not in ICU or hospital; days without organ failure Outcomes relevant to the review: mortality (at 28 days, 90 days, and at end of follow‐up); renal replacement therapy; requiring blood transfusion |
|
| Notes |
Funding/declarations of interest: funded by French Ministry of Health. Study sponsors not involved in design and conduct of study Study dates: Febuary 2003‐November 2012 Note: study was stopped early because study authors noted no difference in 28‐day mortality rates. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were used at the bedside to allow randomisation of eligible participants without any delay and was done blinded to block size |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Clinicians were not blinded because of immediate need for resuscitation; unlikely to introduce bias for this outcome |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | High risk | Clinicians were not blinded because of immediate need for resuscitation; could introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Quote: "mortality end‐points were collected and assessed by study members blinded to treatment assignment." Unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses |
| Selective reporting (reporting bias) | Low risk | Prospective clinical trials registration (NCT00318942); all outcomes listed on registration site were reported |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | High risk | 47.5% of participants in the crystalloid group were given colloids within 12 h before the start of the study and this may have influenced study results |
Baker 2009.
| Methods | RCT Parallel design Multicentre (2 x level 1 adult trauma centres) |
|
| Participants |
Total number of randomised participants: 64 Inclusion criteria: coma, with a loss of consciousness because of isolated blunt head trauma or a GCS score ≤ 8 Exclusion criteria: primary penetrating injury; previous IV therapy ≥ 50 mL; time of arrival at scene to IV access > 4 h; < 16 years of age; burn or amputation; presumed to be pregnant; vital signs absent prior to randomisation Participant condition: blunt trauma head injury Baseline characteristics Colloids group
Crystalloids group
Country: Canada Setting: ambulatory prior to adult‐designated level 1 trauma centres |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: neurological outcomes at hospital discharge (or 30 days) using various scales; mortality; biomarkers Outcomes relevant to the review: mortality (at 28 days) |
|
| Notes |
Funding/declarations of interest: funded by Defence Research and Development Canada Study dates: September 2004‐January 2006 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Computer randomisation was used to assign sequentially numbered identical IV bags to the ambulance |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Participants and personnel were blinded to treatment allocation |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Paramedics, physicians and study co‐ordinators were blinded to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | High risk | Study authors report that participants could receive additional fluid resuscitation during standard care and this could influence outcome results for this study |
Bechir 2013.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 48 Inclusion criteria: ≥ 16 years of age with second‐ or third‐degree acute burn injuries and > 15% of body surface area burned Exclusion criteria: expected to die within 24‐36 h (i.e. burn victims with whole body burn trauma); in situations of palliative care; pregnancy; lack of informed consent; known allergy to HES; contraindications for balanced 6% HES 130/0.04; intracerebral bleeding; acute renal failure; severe hypernatraemia and other severe electrolyte disorders; severe von Willebrand Syndrome; acute liver failure Participant condition: burns; TBSA > 15% Baseline characteristics Colloids group
Crystalloids group
Country: Switzerland Setting: tertiary burns unit |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: group difference in administration of fluid with 72 h; creatinine levels; urine output; ARDS; LoS in ICU; LoS in hospital; in‐hospital mortality and at 28 days; post‐hoc 90‐day mortality; RRT Outcomes relevant to the review: mortality (28 days; and 90 days); RRT (collected as a 90‐day post‐hoc analysis) |
|
| Notes |
Funding/declarations of interest: funding from manufacturer of HES, which supplied study fluids; 2 of the authors have vocationally been members of advisory board meetings. No competing interests declared. Funders reported as having no input in study design and interpretation of results Study dates: November 2009‐January 2013 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation completed using minimisation technique, conducted by a third party |
| Allocation concealment (selection bias) | Low risk | A third party not involved in conduction of study, performed the randomisation process |
| Blinding of participants and personnel (performance bias): mortality | Low risk | All personnel blinded. Fluids prepared externally, and concealed in bags of black plastic |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Low risk | All personnel blinded. Fluids prepared externally, and concealed in bags of black plastic |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details in study report. However, trial registration report states that outcome assessors were blinded |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Low risk | No details in study report. However, trial registration report states that outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 participants were retrospectively excluded because of meeting exclusion criteria. Data missing from 1 additional participant because of early discharge. Overall, < 10% dropout/exclusion; data reported for 45/48 randomised participants |
| Selective reporting (reporting bias) | High risk | Prospective clinical trials registration (NCT01012648). Only primary outcome (fluid volume administered) was listed on the trial registration site |
| Baseline characteristics | Low risk | Baseline characteristics comparable |
| Other bias | Low risk | No other sources of bias identified |
Bentsen 2006.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 22 Inclusion criteria: ICU patients with an acute, spontaneous subarachnoid haemorrhage, with stable ICP in the range of 10 mmHg‐20 mmHg; > 18 years of age; sedated; mechanically ventilated; stable haemodynamics; serum sodium of < 160 mmol/L Exclusion criteria: no details Participant condition: spontaneous subarachnoid haemorrhage Baseline characteristics Colloids group
Crystalloids group
Country: Norway Setting: ICU |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: ICP; CPP; extravascular lung water; serum sodium levels Outcomes relevant to the review: none |
|
| Notes |
Funding/declarations of interest: not reported Study dates: April 2002‐October 2004 Participant condition not reported by group; "A total of 21 patients had haemorrhaged because of a ruptured aneurysm, and one patient was diagnosed with a fusiform dilation of the left vertebral artery." |
|
Brunkhorst 2008.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 537 Inclusion criteria: patients with severe sepsis or septic shock; ≥ 18 years of age; onset of the syndrome < 24 h before admission to the ICU or < 12 h after admission if the condition developed in the ICU Exclusion criteria: treatment with > 1000 mL of HES within 24 h before study inclusion; pre‐existing renal failure requiring dialysis or a serum creatinine level ≥ 320 μmoL/L (3.6 mg/dL); < 18 years of age; pregnancy; known allergy against HES; intra‐cerebral haemorrhage; heart failure with NYHA IV; requirement of an inspiratory oxygen fraction of at least 0.7; immunosuppression from cytostatic chemotherapy; high dosage of steroids or AIDS; participation in another interventional trial; moribund due to coexisting disease; order to withhold or withdraw therapy Participant condition: severe sepsis or septic shock Baseline characteristics Colloids group
Crystalloids group
Country: Germany Setting: ICU; 18 tertiary hospitals |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: mortality (at 28 days and 90 days); morbidity (according to SOFA scores); need for blood transfusion; renal failure (to include need for RRT); time to haemodynamic stabilisation; frequency of vasopressor therapy; need for red‐cell transfusion; duration of mechanical ventilation, LoS in the ICU; adverse events (worsening of oxygenation, bleeding complications, allergic reaction, any event judged to occur in relation to study fluid) Outcomes relevant to the review: mortality (at 28 days and 90 days; need transfusion of a blood product; need for renal replacement therapy |
|
| Notes |
Funding/declarations of interest: supported by a grant (01 KI 0106) from the German Federal Ministry of Education and Research and by unrestricted grants from B Braun, HemoCue and Novo Nordisk Study dates: April 2003‐June 2005 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Open‐label design; unlikely to introduce bias for this outcome |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | High risk | Open‐label design; could introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | High risk | Note: 26.6% of participants in the crystalloid group were given colloids during the study period and this may have influenced study results |
Bulger 2008.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 209 Inclusion criteria: blunt trauma; > 17 years of age (or adult size if age was unknown); at least 1 prehospital SBP measurement ≤ 90 mmHg; transported directly to a single level 1 trauma centre from the site of injury Exclusion criteria: ongoing cardiopulmonary resuscitation; isolated penetrating trauma; known or suspected pregnancy; receipt of > 2000 mL of crystalloid before availability of study fluid Participant condition: blunt trauma Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: prehospital (ambulatory) prior to admission to a single level 1 trauma centre |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: incidence of ARDS; mortality; multiple organ failure syndrome; nosocomial infections; length of hospital and ICU stay; ventilator‐free days; adverse events; non‐infectious complications Outcomes relevant to the review: mortality (28 days) |
|
| Notes |
Funding/declarations of interest: grant R01 HL073233‐01 from the National Institutes of Health Study dates: October 2003‐August 2005 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | A random number (computer‐generated by pharmacist) was applied to each bag and kept by the pharmacist. Ambulance crew did not have access to allocation sequence |
| Blinding of participants and personnel (performance bias): mortality | Low risk | All contents of fluid bags were blinded by research pharmacists. Therefore, personnel and participants were blinded to treatment assignment |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 21 participants did not meet eligibility criteria once randomisation had taken place but remained in the results using ITT analysis. Three participants lost to follow‐up, explanations reported by study authors |
| Selective reporting (reporting bias) | Unclear risk | Clinical trials registration ID: NCT01012648. All outcomes specified on clinical trials registration site were reported. However, we noted that the outcomes were only added to the trials registration site after the study start date |
| Baseline characteristics | Unclear risk | We noted higher injury severity scores for those in the colloids group, and we could not be certain whether this could influence outcome data |
| Other bias | Low risk | No other sources of bias identified |
Bulger 2010.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 1331 Inclusion criteria: blunt mechanism of injury; ≥ 15 years of age; GCS score ≤ 8; ineligibility for enrolment in the haemorrhagic shock cohort Exclusion criteria: known or suspected pregnancy; < 15 years of age; out‐of‐hospital cardiopulmonary resuscitation; administration of > 2000 mL of crystalloid or any amount of colloid or blood products prior to enrolment; severe hypothermia (28 °C); drowning; asphyxia because of hanging; burns on > 20% of TBSA; isolated penetrating head injury; inability to obtain IV access; > 4 h between receipt of dispatch call to study intervention Participant condition: traumatic brain injury Baseline characteristics Colloids group
Crystalloids group (NS)
Crystalloids group (HS)
Country: USA and Canada Setting: 11 regional clinical centres |
|
| Interventions |
Colloids group
Crystalloids group (NS)
Crystalloids group (HS)
|
|
| Outcomes |
Outcomes measured/reported: 6‐month neurologic status (Glasgow Outcome Score); 28‐day survival; survival to discharge; ICP; interventions required to manage intracranial hypertension; fluid and bolus requirements in first 24 h; physiologic parameters of organ dysfunction; 28‐day ARDS‐free survival; MODS; nosocomial infections Outcomes relevant to the review: mortality (28 days) |
|
| Notes |
Funding/declarations of interest: National Heart, Lung and Blood Institute plus partners Study dates: May 2006‐May 2009 Study terminated after futility criteria met at 6 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly generated numeric code used at central location |
| Allocation concealment (selection bias) | Low risk | Randomisation scheme conducted externally and all personnel unaware of allocation |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Quote: "Study fluids were provided in identical intravenous bags and shipped to a single distribution center, where they were labelled with a randomly generated numeric code" Participants, caregivers, and outcome assessors were blinded to treatment |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Participants, caregivers, and outcome assessors were blinded to treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Mortality data reported for 359/373 (HSD), 341/355 (HS), and 582/603 (NS). < 5% dropout/loss in each group |
| Selective reporting (reporting bias) | Low risk | Prospective clinical trials registration: NCT00316004. All outcomes were prespecified |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | Low risk | No other sources of bias identified |
Bulger 2011.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 895 Inclusion criteria: ≥ 15 years of age; in significant haemorrhagic shock (out‐of‐hospital SBP ≤ 70 mmHg or 71‐90 mmHg with concomitant HR ≤ 108 bpm) Exclusion criteria: known or suspected pregnancy; < 15 years of age; out‐of‐hospital cardiopulmonary resuscitation; administration of > 2000 mL crystalloid, colloid, or blood products before enrolment; severe hypothermia (< 28 °C); drowning; asphyxia because of hanging; burns > 20% TBSA; isolated penetrating head injury; inability to obtain IV access; time of dispatch call received to study intervention > 4 h; known prisoners Participant condition: traumatic hypovolaemic shock Baseline characteristics Colloids group
Crystalloids group (NS)
Crystalloids group (HS)
Country: USA and Canada Setting: out‐of‐hospital |
|
| Interventions |
Colloids group
Crystalloids group (NS)
Crystalloids group (HS)
|
|
| Outcomes |
Outcomes measured/reported: 28‐day survival; physiologic parameters of organ dysfunction; ARDS criteria met in the first 28 days after injury; MODS; presence of nosocomial infection Outcomes relevant to the review: mortality (28 days); participants having transfusion (0‐9 units); participants having transfusion (> 10 units) |
|
| Notes |
Funding/declarations of interest: The National Heart, Lung and Blood Institute. Study authors declare no financial conflicts of interest Study dates: May 2006‐August 2008 Note: the previous version of this review did not include participants in the HS group (Perel 2013). We have included outcome data for these participants, and in analysis we have combined both crystalloid groups. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomly generated numeric code was applied to each bag and a randomization list kept by the Data Co‐ordinating Center" Information taken from study protocol |
| Allocation concealment (selection bias) | Low risk | Randomisation list kept by study investigators (taken from study protocol) |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Care providers, investigators, and participants were blinded to treatment assignment, study fluids concealed |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Low risk | Care providers, investigators, and participants were blinded to treatment assignment, study fluids concealed |
| Blinding of outcome assessment (detection bias): mortality | Low risk | All personnel were blinded |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Low risk | All personnel were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 42/895 participants were not included in analysis but reasons were clearly provided (most of these losses were because of inclusion/exclusion criteria) |
| Selective reporting (reporting bias) | Unclear risk | A protocol was published for this study; publication of protocol was retrospective and it was not feasible to use this to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | High risk | We noted that participants may have received up to 2000 mL of crystalloid or colloid before randomisation (as part of exclusion criteria). Study authors did not report how many participants received fluid resuscitation before randomisation, or which fluid was given, and this may influence outcome data for this study |
Caironi 2014.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 1810 Inclusion criteria: ≥ 18 years of age; severe sepsis within previous 24 h Exclusion criteria: < 18 years of age; terminal state; known adverse reaction to albumin administration; severe sepsis or septic shock after proved or suspected head injury; clinically active; congestive heart failure (NYHA class 3 or 4); pathological conditions in which albumin administration was clinically indicated (hepatic cirrhosis with ascites, intestinal malabsorption syndrome, nephrotic syndrome, burns); > 24 h since inclusion criteria were met; religious objection to the administration of human blood products; inclusion in other experimental studies Participant condition: severe sepsis Baseline characteristics Colloids group
Crystalloids group
Country: Italy Setting: ICU |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: death from any cause (28 days); death from any cause (90 days); number of participants with organ dysfunction; length of ICU and hospital stay Outcomes relevant to the review: mortality (at 28 days, and at 90 days); RRT |
|
| Notes |
Funding/declarations of interest: Italian Medicines Agency Study dates: Aug 2008‐Feb 2012 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed centrally, with the use of the computer‐generated and blinded assignment sequence. Randomization was stratified according to the participating ICU and the interval between the time that the patient met the clinical criteria for severe sepsis and randomization" |
| Allocation concealment (selection bias) | Low risk | Central allocation, blinded |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Open‐label study; lack of blinding unlikely to introduce bias for this outcome |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few losses; unlikely to affect analysis |
| Selective reporting (reporting bias) | Low risk | Prospective clinical trials registration (NCT00707122). All outcomes listed were reported |
| Baseline characteristics | Unclear risk | Quote: "Baseline characteristics were similar between the two study groups, except for a slight imbalance in the number of patients with organ dysfunction and values of central venous oxygen saturation". It was not reported if these differences between groups were at a level of statistical significance. We were uncertain whether these differences might influence the results |
| Other bias | Low risk | No other sources of bias identified |
Chavez‐Negrete 1991.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 49 Inclusion criteria: SBP ≤ 90 mmHg for < 1 h; normal ECG; written consent by participant or first‐degree relative Exclusion criteria: pregnancy; renal, cardiac, or neurological diseases Participant condition: haemorrhagic shock Baseline characteristics Colloids group
Crystalloids group
Country: Mexico Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic variables; urinary output; GCS; mortality (within 24 h) Outcomes relevant to the review: mortality |
|
| Notes |
Funding/declarations of interest: none reported Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were assigned to groups using random numbers but no Additional details provided |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | High risk | Quote: "Dextran 40 was administered to the control group if necessary according to medical judgement." Study authors did not report the number of participants in the crystalloid group who received additional colloids and this may influence outcome data for this study |
Cifra 2003.
| Methods | Quasi‐RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 26 Inclusion criteria: admitted to a children's medical centre; fever lasting 2‐7 days; haemorrhagic manifestations; evidence of consumptive coagulopathy, a fall in platelet count, prolonged bleeding, prolonged prothrombin time, or prolonged partial thromboplastin time; evidence of plasma leakage; evidence of circulatory failure Exclusion criteria: severe infection other than dengue haemorrhagic fever; protein‐deficient abnormalities; bleeding diathesis; given multiple plasma substitutes Participant condition: DSS Baseline characteristics Colloids group
Crystalloids group
Country: Philippines Setting: ICU |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: duration of control of shock, haematocrit level, length of ICU stay, transfusion of blood products, frequency of recurrence of shock, mortality Outcomes relevant to the review: mortality (time point not reported); transfusion of blood products (FFP or packed red blood cells) |
|
| Notes |
Funding/declarations of interest: not reported Study dates: June 2001‐July 2001 Note: 3 out of 16 participants in the crystalloid group (18.75%) also received colloids during the study period and this may have influenced study results |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised method to allocate participants, using alternating allocation to each group |
| Allocation concealment (selection bias) | High risk | Not possible to conceal allocation because of methods used to allocate participants |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Personnel were not blinded; however, unlikely to introduce bias for this outcome |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Four participants were excluded from some analysis. Because mortality data were reported for these participants we included these in analysis. |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | High risk | 3 out of 16 participants in the crystalloid group (18.75%) also received colloids during the study period and this may have influenced study results |
Cooper 2006.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 42 Inclusion criteria: thermal burn of ≥ 20% TBSA; time elapsed since injury ≤ 12 h; written informed consent from the participant or a suitable substitute decision maker; availability of data regarding fluids administered before arrival at the study centre Exclusion criteria: unlikely survival, defined as APACHE II score > 30 or predicted mortality ≥ 90%; ventricular fibrillation; ventricular tachycardia; unstable angina; known congestive heart failure or myocardial infarction within the month before thermal injury; electrical or chemical burn injury; pregnancy Participant condition: burns Baseline characteristics Colloids group
Crystalloids group
Country: Canada Setting: hospital units |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: MODS; mortality; duration of mechanical ventilation; LoS in ICU; local infection events; systemic infection events; percentage of graft take; oxygenation failure (PaO2‐to‐FiO2 ratio) (all evaluated up to and including Day 28) Outcomes relevant to the review: mortality (28 days); blood transfusion |
|
| Notes |
Funding/declarations of interest: funded by Bayer Biologics, Canada Study dates: June 1999‐June 2001 Trial stopped early due to slow enrolment |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | High risk | Quote: "Treatment fluid was given in an open label fashion owing to differences in the physical properties (color, tendency to bubble) and medium of delivery (glass vials vs. polymer bags)" Could introduce bias for blood transfusion outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details; lack of blinding unlikely to influence data for mortality |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Unclear risk | Baseline characteristics and demographics were comparable between groups except for predicted mortality, which was greater in the colloid group (18.6%) compared with the crystalloid group (9.4%) |
| Other bias | Low risk | No other sources of bias |
Du 2011.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 41 Inclusion criteria: adults; male and female; with hospital diagnosis of severe acute pancreatitis Exclusion criteria: history of allergy to HES; history of cardiac dysfunction or renal insufficiency; pregnancy, malignancy or immunoinsufficiency; other colloids within 24 h; serum albumin < 25 g/L; likely death within 48 h. Also excluded those who died within 72 h; received surgery during treatment period; severe adverse effects to HES Participant condition: severe acute pancreatitis Baseline characteristics Colloids group
Crystalloids group
Country: China Setting: university hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: mortality (within‐hospital stay); intra‐abdominal pressure; fluid balance; major organ complications; use of respirator; APACHE II score; serum levels of inflammatory mediators Outcomes relevant to the review: mortality (within‐hospital stay) |
|
| Notes |
Funding/declarations of interest: supported by Sichuan Province of Science and Technology Department Technology Support Project Study dates: January 2008‐November 2009 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐derived random number table |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | We have included 1 participant that was excluded from the study as this participant died therefore providing relevant data for this review |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | High risk | 57.1% of participants in the crystalloid group were given colloids during the study period and we noted that this may have influenced study results |
Dubin 2010.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 25 Inclusion criteria: ≥ 18 years of age; confirmed or suspected infection plus ≥ 2 signs of the systemic inflammatory response syndrome (definition of sepsis by American College of Chest Physicians/Society of Critical Care Medicine criteria), and tissue hypoperfusion (MAP < 65 mmHg despite a crystalloid fluid challenge of 20 mL/kg or blood lactate concentration of ≥ 4 mmol/L) Exclusion criteria: impossible to perform sublingual video‐microscopy; < 18 years of age; pregnancy; stroke; acute coronary syndrome; hydrostatic pulmonary oedema; status asthmaticus; cardiac arrhythmias (as a main diagnosis); contraindication for central venous catheterisation; active gastrointestinal haemorrhage; seizures; drug intoxications; burns; trauma; need of immediate surgery; terminal cancer; immunosuppression (organ transplant or systemic illness); no resuscitation order; delayed admission to the intensive care unit from the emergency department (> 4 h); or previous resuscitation with > 1500 mL of fluids Participant condition: sepsis Baseline characteristics Colloids group
Crystalloids group
Country: Argentina Setting: 2 teaching ICUs |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: heart rate; MAP; CVP; central venous gases and oxygen saturations; microcirculatory variables; mortality Outcomes relevant to the review: mortality (time point not reported) |
|
| Notes |
Funding/declarations of interest: supported by the grant PICT‐2007‐00912, Agencia Nacional de Promoción Científica y Tecnológica, Argentina Study dates: January 2006‐August 2009 Note: data for mortality were not clearly reported in the study report. We have included deaths of participants within 24 h and combined these with deaths reported in the study report outcome table. The previous version of this review did not include mortality outcome data (Perel 2013). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Simple randomization by the use of sealed envelopes" Insufficient details to allow judgement |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes, but no mention of opaqueness, or whether they were numbered sequentially |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study authors reported a small number of losses because of death. We included these as data for the mortality outcome |
| Selective reporting (reporting bias) | Unclear risk | Clinical trials registration occurred after the start of the study (NCT00799916); not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | Low risk | No other sources of bias identified |
Dung 1999.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 50 Inclusion criteria: 5‐15 years of age; DSS; had not received IV fluid therapy during their current illness Exclusion criteria: no details Participant condition: DSS Baseline characteristics Colloids group (dextran)
Colloids group (gelatin)
Crystalloids group (RL)
Crystalloids group (NS)
Country: Vietnam Setting: hospital |
|
| Interventions |
Colloids group (dextran)
Colloids group (gelatin)
Crystalloids group (RL)
Crystalloids group (NS)
|
|
| Outcomes |
Outcomes measured/reported: recovery from shock; duration of shock and number of episodes of shock; improvements in cardiac output and haematocrit values; requirements for further fluid resuscitation Outcomes relevant to the review: none |
|
| Notes |
Funding/declarations of interest: B Braun provided the fluids used in this study. Financial support from The Wellcome Trust of Great Britain Study dates: all participants admitted between July and November 1995 |
|
Ernest 1999.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 18 Inclusion criteria: septic; critically ill; fluid infusion clinically indicated; pulmonary catheter already in place; patient not overtly bleeding Exclusion criteria: no details Participant condition: sepsis Baseline characteristics Colloids group
Crystalloids group
Country: Canada Setting: ICU |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: MAP, PAOP, cardiac index, arterial oxygen content, plasma albumin concentration, PV and ECFV Outcomes relevant to the review: none |
|
| Notes |
Funding/declarations of interest: none reported Study dates: not reported |
|
Evans 1996.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 25 Inclusion criteria: > 16 years of age; blunt or penetrating trauma; requiring IV fluid resuscitation; arrival at trauma unit within 2 h of injury; RL as the only prehospital infusion; no underlying illness or medication that would affect the patient's coagulating system Exclusion criteria: no details Participant condition: trauma Baseline characteristics Colloids group
Crystalloids group
Country: South Africa Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: bleeding times, prothrombin, thrombin, partial thromboplastin times, platelet count, secondary resuscitation Outcomes relevant to the review: mortality (data from personal communication with study authors; time point unknown) |
|
| Notes |
Funding/declarations of interest: "Hoechst SA for their independent grant and sponsorship for this research project" Study dates: not reported Note: we used mortality data reported in the previous version of this review (Perel 2013). These data were collected from personal communication with the study authors |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised but no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | Low risk | No other sources of bias identified |
Finfer 2004.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 6997 Inclusion criteria: ≥ 18 years of age; treating clinician judged to require fluid administration to maintain or increase intravascular volume Exclusion criteria: people admitted to ICU after cardiac surgery; liver transplantation; treatment of burns Participant condition: various ICU admissions (to include trauma, sepsis, ARDS) Baseline characteristics Colloids group
Crystalloids group
Country: Australia and New Zealand Setting: hospital ‐ 16 ICUs |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: all‐cause mortality within 28 days, survival time during first 28 days, proportion of participants with organ failure, duration of mechanical ventilation, duration of renal‐replacement therapy, duration of ICU and hospital stay Outcomes relevant to the review: mortality (28 days), RRT (for subgroup of participants with severe sepsis) |
|
| Notes |
Funding/declarations of interest: Auckland District Health Board and the Health Research Council of New Zealand Study dates: November 2001‐June 2003 Note: in the previous version of the review (Perel 2013), this study was called SAFE 2004. This study reports a subgroup of participants who had severe sepsis (1218 participants; 603 in the albumin group, and 615 in the saline group). Data were available for RRT for these participants and we have included this subgroup of participants in analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was carried out centrally with the use of a minimisation algorithm; service accessed through a secure website |
| Allocation concealment (selection bias) | Low risk | Used central randomisation by a third party |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Blinding was maintained by use of identical 500 mL bottles and cartons designed to mask fluid type and administration sets |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Low risk | Blinding was maintained by use of identical 500 mL bottles and cartons designed to mask fluid type and administration sets |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding provided; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data (on vital status) were missing for 1% of randomised participants at 28 days, which is acceptable. Some discrepancies with reported numbers of participants analysed, but not significant |
| Selective reporting (reporting bias) | Low risk | Prospective clinical trials registration (ISRCTN76588266); all outcomes listed on registration site were reported |
| Baseline characteristics | Unclear risk | We noted that the albumin group had a higher CVP at baseline; we could not be certain whether this imbalance might influence results. No other baseline imbalances were noted |
| Other bias | High risk | Study authors reported that 3.9% of participants in the saline group were given albumin in the previous 72 h; this represents few participants and it is not likely to have introduced significant bias. However, some participants were given additional resuscitation fluids during the study period according to clinician preference, and numbers for this were not reported. This may influence outcome data for this study |
Goodwin 1983.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 79 Inclusion criteria: control of resuscitation obtained within 4 h of injury; all participants admitted within 12 h of injury Exclusion criteria: none stated Participant condition: burns Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: Brooke Army Medical Center |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic responses; mortality at end of follow‐up Outcomes relevant to the review: mortality at end of follow‐up |
|
| Notes |
Funding/declarations of interest: study authors state, "the opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense" Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomised using random numbers table |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses reported |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics are comparable |
| Other bias | High risk | All participants in the crystalloid group received colloids after 24 h and this may have influenced study results |
Grba‐Bujevic 2012.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 50 Inclusion criteria: trauma patients who met the criteria for haemorrhagic‐hypovolaemic shock, with definitive signs of external or internal haemorrhage in a prehospital setting; aged 18‐60 years Exclusion criteria: no details Participant condition: haemorrhagic‐hypovolaemic shock Baseline characteristics Colloids group
Crystalloids group
Country: Croatia Setting: prehospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: BP, pulse rate, peripheral oxygen saturation, and respiration rate Outcomes relevant to the review: none |
|
| Notes |
Funding/declarations of interest: none reported Study dates: not reported |
|
Guidet 2012.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 196 Inclusion criteria: ≥ 18 years of age; required fluid resuscitation; clinically defined severe sepsis Exclusion criteria: serum creatinine > 300 µmol/L; chronic renal failure; anuria lasting > 4 h; requirement for renal support Participant condition: severe sepsis Baseline characteristics Colloids group
Crystalloids group
Country: France and Germany Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: amount of study drug to achieve haemodynamic stabilisation; time to achieve initial haemodynamic stabilisation; quantity of study drug infused over 4 consecutive days; LoS in ICU and hospital; SOFA scores; kidney injury (RIFLE and AKIN scores); mortality (28 days and 90 days); blood transfusion; adverse events (itching) Outcomes relevant to the review: mortality (28 days); blood transfusion (red blood cells); RRT (score of 3 using AKIN); adverse events (itching) |
|
| Notes |
Funding/declarations of interest: supported by grant from Fresenius Kabi, Germany. The pharmaceutical company was involved in the study design, analysis and preparation of the report Study dates: not reported Note: the previous version of this review (Perel 2013) used mortality data at 90 days; in this review we have analysed mortality data at 28 days |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Refers to reference from Myburgh 2012 to describe randomisation technique. Used external web‐based randomisation |
| Allocation concealment (selection bias) | Low risk | Use of web‐based system ensured that allocation code was kept concealed |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Participants and personnel were blinded. Study drugs were kept in identical packaging |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Low risk | Participants and personnel were blinded. Study drugs were kept in identical packaging |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Reference from Myburgh 2012 suggests that all personnel were blinded, including outcome assessors |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Low risk | Reference from Myburgh 2012 suggests that all personnel were blinded, including outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant was unaccounted for in saline group for mortality outcome only, unlikely to influence outcome data overall |
| Selective reporting (reporting bias) | High risk | Prospective clinical trials registration (NCT00464204). Clinical trials registration documents do not list mortality, transfusion of blood products, or RRT as study outcomes. Clinical trials registration documents title of the study is "Effects of voluven on hemodynamics and tolerability of enteral nutrition in patients with severe sepsis" and some outcomes relate to assessment of caloric intake |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | Low risk | No other sources of bias identified |
Hall 1978.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 172 Inclusion criteria: admitted during acute phase, with burns for which treatment for shock was indicated; adults and children Exclusion criteria: no details Participant condition: burns Baseline characteristics Colloids group
Crystalloids group
Country: Denmark Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: fluid input and output, haemoglobin levels, mortality Outcomes relevant to the review: mortality (48 h) |
|
| Notes |
Funding/declarations of interest: supported by grant from Danish Medical Research Council Study dates: not reported, the last participant was recruited in December 1975 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were stratified according to burn severity and type and then lots were used to determine which treatment the first participant in each stratum received |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are reported for all randomised participants |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or pre‐published protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | Low risk | No other sources of bias identified |
Heradstveit 2010.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 19 Inclusion criteria: witnessed cardiac arrest with probable cardiac cause; advanced medical life support within 15 min; return of spontaneous circulation within 60 min; comatose when admitted to the hospital; aged 18‐80 years Exclusion criteria: terminal illness; strongly in need of nursing; primary coagulopathy; prehospital fluid load > 2000 mL Participant condition: postcardiac arrest Baseline characteristics Colloids group
Crystalloids group
Country: Norway Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: fluid volume required to achieve treatment goals; oedema; haemodynamics; adverse events (to include renal failure); survival after 1 year Outcomes relevant to the review: survival after 1 year |
|
| Notes |
Funding/declarations of interest: supported by grant from the Regional Centre for Emergency Medical Research and Development and Development and Section of Emergency Medicine, Dept of Anaesthesia and Intensive Care, Haukeland University Hospital Study dates: September 2005‐March 2007 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study authors report use of stratified randomisation, with allocation generated by study authors. We could not be certain whether this method was sufficient |
| Allocation concealment (selection bias) | Unclear risk | Numbered envelopes were distributed and opened by a physician after participant enrolment. Study authors do not report whether envelopes were sealed or opaque |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding of physician; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics are comparable |
| Other bias | Low risk | No other sources of bias identified |
James 2011.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 115 Inclusion criteria: penetrating or blunt trauma; requiring > 3 L of volume resuscitation; 18‐60 years of age Exlusion criteria: fluid overload pulmonary oedema; known allergy to HES; known pre‐existing renal failure with oliguria or anuria; receiving dialysis treatment before the injury; severe hypernatraemia or hyperchloraemia on admission; severe head injury from which recovery was unlikely; severe intracranial bleeding; severe crush injury; arterial pressure unresponsive to 2 L IV fluid loading which could not be recorded; clinically obvious cardiac tamponade; neurogenic shock (high spinal cord injury); known AIDS or AIDS‐related complex; admitted > 6 h after injury; people who had already received any colloid before randomisation; taking part in another clinical trial at the same time; refused consent Participant condition: penetrating or blunt trauma Baseline characteristics Colloids group (penetrating trauma HES)
Crystalloids group (penetrating trauma saline)
Colloids group (blunt trauma HES)
Crystalloids group (blunt trauma saline)
Country: South Africa Setting: hospital, level 1 trauma centre |
|
| Interventions |
Colloids group (penetrating trauma HES + blunt trauma HES)
Crystalloids group (penetrating trauma saline + blunt trauma saline)
|
|
| Outcomes |
Outcomes measured/reported: volumes of study fluid in first 24 h; number of participants achieving normal gastrointestinal function by day 5; mortality; serious adverse events; acute renal injury; dialysis; use of blood products; biochemical abnormalities; days in ICU; days on ventilator support, SOFA scores, TEG measurements, skin itching Outcomes relevant to the review: mortality (time point unknown), dialysis |
|
| Notes |
Funding/declarations of interest: funding from Fresenius‐Kabi, who also supplied study fluids. Funders had no input into study design, analysis, interpretation etc. Also funds from TEG and laboratory investigations derived from Dept of Anaesthesia, UCT, research funds Study dates: not reported Study authors stratified data according to whether participants had penetrating or blunt trauma injuries. We have combined both types of injuries in analysis Note: we used mortality data reported in the previous version of this review (Perel 2013). These data were collected from personal communication with the study authors |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used random numbers in blocks of 8 for each category of trauma |
| Allocation concealment (selection bias) | Low risk | Fluids prepacked by pharmacy, and we have assumed that, therefore, allocation was concealed from personnel |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Study fluids were presented in identical black bags |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Low risk | Study fluids were presented in identical black bags |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few losses, and reasons were reported by study authors |
| Selective reporting (reporting bias) | Unclear risk | Retrospective clinical trials registration (ISRCTN 42061860); so not feasible to assess risk of selective reporting bias from these documents |
| Baseline characteristics | Unclear risk | Injury severity scores were higher in the colloids group. We could not be certain whether this could influence outcome data |
| Other bias | Low risk | No other sources of bias identified |
Jelenko 1979.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 19 Inclusion criteria: 20%‐98% TBSA; selected when, within 15 min, precise time of burn injury and intake and output experienced by patient from time of injury to time of admission was known Exclusion criteria: no details Participant condition: burns Baseline characteristics Colloids group
Crystalloids group (RL)
Crystalloids group (HS)
Country: USA Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group (RL)
Crystalloids group (HS)
|
|
| Outcomes |
Outcomes measured/reported: fluid volume; clinical results; laboratory results; urine variables (including renal failure); serum osmolality; sodium and potassium levels; cardiorespiratory and haemodynamic variables Outcomes relevant to the review: mortality (time point not reported) |
|
| Notes |
Funding/declarations of interest: supported in part by National Institutes of Health Grant Study dates: January 1977‐March 1978 In the previous version of the review (Perel 2013), the study ID was Jelenko 1978 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Described as randomised. No additional details but significant details in baseline demographics which would suggest an insufficient method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details; lack of blinding unlikely to influence data for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details; lack of blinding unlikely to influence data for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | High risk | Statistically significant differences between groups for baseline characteristics |
| Other bias | Low risk | No other sources of bias identified |
Jie 2015.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 84 Inclusion criteria: 18‐85 years of age; meet criteria for septic shock; resuscitation within 6 h with crystalloid or HES ≥ 30 mL/kg; within 24 h no packed red blood cells, plasma or other blood products that would affect coagulation and fibrinolysis significantly; no unauthorised drugs; no previous coagulation disorders Exclusion criteria: severe heart failure; bleeding occurring during resuscitation and requiring the use of blood products; serious renal insufficiency Participant condition: septic shock Baseline characteristics Colloids group
Crystalloids group
Country: China Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: prothrombin time, tissue factor, tissue factor pathway inhibitor, active protein C, LoS in ICU, mortality Outcomes relevant to the review: mortality (time point unknown) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: November 2009‐October 2014 Article in Chinese. Data for study characteristics taken from English abstract, and from study report tables, with translation using Google Translate |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised. Data for 'Risk of bias' assessment taken from English abstract only |
| Allocation concealment (selection bias) | Unclear risk | No details. Data for 'Risk of bias' assessment taken from English abstract only |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Data for 'Risk of bias' assessment taken from English abstract only. No details of clinical trials registration in English abstract |
| Baseline characteristics | Low risk | Baseline characteristics appeared largely comparable |
| Other bias | Unclear risk | We could not be certain of other risks of bias because 'Risk of bias' assessments were made from the English abstract only |
Kumar 2017.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 105 Inclusion criteria: perforation peritonitis; 18‐60 years of age Exclusion criteria: pregnancy; known allergies or manifesting symptoms of possible anaphylaxis with test dose of HES; major coagulation disorders; renal failure because of medical renal disease; severe hepatic insufficiency; congestive cardiac failure at admission; traumatic perforation cases; < 18 years of age or > 60 years of age; people who had been resuscitated before reaching emergency surgical unit; denied consent Participant condition: perforation peritonitis Baseline characteristics Colloids group
Crystalloids group
Country: India Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: time to achieve goals of fluid resuscitation, morbidity, mortality, length of hospital stay, complications attributable to type of fluid administration Outcomes relevant to the review: mortality (up to 30 days from hospital discharge) |
|
| Notes |
Funding/declarations of interest: no funding and no conflicts of interest Study dates: October 2006‐April 2009 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised with the help of computer‐generated random table" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Quote: "Administered the fluid therapy according to randomisation without knowledge of the observer" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Unclear risk | We noted differences in physiological scores between groups. We could not be certain whether this difference could influence the outcome data |
| Other bias | High risk | Note the length of time since completion of trial, and publication of full study report. Also, note that the study was reported by a single author |
Li 2008.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 60 Inclusion criteria: not reported in abstract Exclusion criteria: not reported in abstract Participant condition: patients with septic shock Baseline characteristics Colloids group (HES)
Colloids group (HES with HS)
Crystalloids group (NS)
Crystalloids group (HS)
Country: China Setting: hospital |
|
| Interventions |
Colloids group (HES)
Colloids group (HES with HS)
Crystalloids group (NS)
Crystalloids group (HS)
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic parameters, blood lactate clearance, mortality (at 28 days) Outcomes relevant to the review: mortality |
|
| Notes |
Funding/declarations of interest: not reported in abstract Study dates: not reported in abstract Article in Chinese. Data for study characteristics taken from English abstract, and from study report tables, with translation using Google Translate |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Risk of bias' assessment made using English abstract only. Described as randomised, no additional detail |
| Allocation concealment (selection bias) | Unclear risk | No details. 'Risk of bias' assessment made using English abstract only |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details. 'Risk of bias' assessment made using English abstract only. However, lack of blinding unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details. 'Risk of bias' assessment made using English abstract only. However, lack of blinding unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias. 'Risk of bias' assessment made using English abstract only |
| Baseline characteristics | Low risk | Baseline characteristics appeared largely comparable |
| Other bias | Unclear risk | We could not be certain about other risks of bias because 'Risk of bias' assessment were made using English abstract only |
Lowe 1977.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 141 Inclusion criteria: people undergoing laparotomy for acute abdominal trauma Exclusion criteria: associated chest injury Participant condition: laparotomy for acute abdominal trauma Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: hospital, trauma unit |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: red blood cell transfusions, urine output, mortality, ventilator support, pulmonary function test variables Outcomes relevant to the review: mortality (at 28 days); blood transfusion (0‐9 units) |
|
| Notes |
Funding/declarations of interest: supported by a grant form US Army Medical Research and Development Command Study dates: not reported Note: we edited the number of randomised participants in each group as reported in the previous version of this review (Perel 2013); we did not include participants who were excluded because of chest injury. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The use of cards in sealed envelopes is an appropriate method of randomisation but additional details are required. It is unclear why there was a difference in participant numbers between groups once those with chest injuries were excluded. The study author provided an explanation following the discussion but it is possible that the study was not truly randomised |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study authors reported exclusion of 30 participants because of chest injury, and the reported results are for the remaining 141 participants. We have assumed that these 30 participants were not 'lost' but were excluded because of prespecified exclusion criteria, We noted missing data in the baseline characteristics for 4 participants; this loss was not explained, but we did not expect it to influence outcome data |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or a prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Lu 2012.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 42 Inclusion criteria: septic shock; admitted to ICU Exclusion criteria: no details Participant condition: septic shock Baseline characteristics Colloids group
Crystalloids group
Country: China Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: prothrombin time, activated partial thromboplastin time, plasma tissue plasminogen activator, plasminogen activator inhibitor, length of ICU stay, mortality, fluid volume, vasoactive drugs Outcomes relevant to the review: mortality (time point not reported) |
|
| Notes |
Funding/declarations of interest: not reported in abstract Study dates: September 2009‐June 2011 Article in Chinese. Data for study characteristics taken from English abstract, and from study report tables, with translation using Google Translate. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no additional details. 'Risk of bias' assessment made using English abstract only |
| Allocation concealment (selection bias) | Unclear risk | No details. 'Risk of bias' assessment made using English abstract only |
| Blinding of participants and personnel (performance bias): mortality | Low risk | 'Risk of bias' assessment made using English abstract only. No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | 'Risk of bias' assessment made using English abstract only. No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or a prepublished protocol; not feasible to assess risk of selective outcome reporting bias. 'Risk of bias' assessment made using English abstract only |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Unclear risk | We could not be certain about other risks of bias because 'Risk of bias' assessment made using English abstract only |
Lucas 1978.
| Methods | Quasi‐RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 52 Inclusion criteria: serious injuries requiring multiple transfusions Exclusion criteria: no details Participant condition: hypovolaemic shock Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: fluid volumes ‐ input and output, protein variables, serum protein variables Outcomes relevant to the review: mortality (time point not reported) |
|
| Notes |
Funding/declarations of interest: supported by the Detroit General Hospital Research Corporation Study dates: November 1975‐February 1977 Note: We found a discrepancy between the study reports for Lucas 1978. A later published report (Lucas 1980) covers a longer time period, with a larger number of randomised participants. Lucas 1980 reports 5 deaths (3 in the albumin group and 2 in the crystalloid group). The earlier report, Lucas 1978, is for fewer participants and reports 7 deaths in the albumin group, and no deaths in the crystalloid group. We have used data from the earlier report because this was used in the previous published version of the review (Perel 2013). We assessed this decision in sensitivity analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation decision was based on last digit of each participant's case number |
| Allocation concealment (selection bias) | High risk | Randomisation decision was based on last digit of each participant's case number |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | High risk | We were concerned by differences in the reported number of deaths in the associated publications for this study |
Mahrous 2013.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 56 Inclusion criteria: febrile neutropenic patients with severe sepsis and septic shock Exclusion criteria: no details Participant condition: severe sepsis; septic shock Baseline characteristics Colloids group
Crystalloids group
Country: Saudi Arabia Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: acute renal failure, need for RRT, 28‐day mortality Outcomes relevant to the review: mortality (at 28 days), RRT |
|
| Notes |
Funding/declarations of interest: none reported Study dates: not reported Abstract only. We did not include mortality data from this report, which were reported as percentages; we could not be certain whether the data were for all randomised participants or whether some participant data were lost (crystalloid group: 63.4%; colloid group: 73.3%). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned, no additional details. Abstract only |
| Allocation concealment (selection bias) | Unclear risk | No details. Abstract only |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Abstract only. However, lack of blinding unlikely to introduce bias for mortality |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details. Abstract only |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Abstract only. However, lack of blinding unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details. Abstract only |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Abstract only. We could not be certain whether this study had participant losses for mortality because of apparent discrepancies in reported data in the abstract |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Unclear risk | Not possible to assess baseline characteristics from abstract |
| Other bias | Unclear risk | Not feasible to assess other risks of bias from abstract only |
Maitland 2005.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 117 Inclusion criteria: children with clinical feature of severe malaria; Plasmodium falciparum parasitaemia; metabolic acidosis with base deficit of > 8 mmol/L; haemoglobin concentration of > 50 g/L Exclusion criteria: pulmonary oedema; oedematous malnutrition; papilledema; parental refusal of consent Participant condition: severe malaria Baseline characteristics Colloids group
Crystalloids group
Country: Kenya Setting: hospital (paediatric high‐dependency unit) |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: percentage reduction in base deficit (8 h); requirement for rescue therapies; neurological sequelae; mortality Outcomes relevant to the review: mortality (time point not reported) |
|
| Notes |
Funding/declarations of interest: supported by a grant from the Wellcome Trust, and from senior fellowship funding Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised but no additional details |
| Allocation concealment (selection bias) | Unclear risk | Use of sealed cards, but insufficient details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nine losses of 159 randomised participants. Losses because of early requirement of randomisation prior to complete diagnoses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Unclear risk | Baseline characteristics reported in moderate and severe acidosis groups. There were no significant clinical differences at the time of hospital admission, although among children in the severe acidosis group who received albumin, seizures, hypotension and hypoglycaemia were more common than among children assigned to the saline group. We could not be certain whether these differences would influence the data |
| Other bias | Low risk | No other sources of bias identified |
Maitland 2011.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 2126 (2097 in group A; 29 in group B) Inclusion criteria: between 60 days and 12 years of age; severe febrile illness complicated by impaired consciousness or respiratory distress; impaired perfusion Exclusion criteria: severe malnutrition; gastroenteritis; non‐infectious causes of shock and conditions for which volume expansion is contraindicated Participant condition group A: severe febrile illness, without hypotension Participant condition group B: severe febrile illness with hypotension Baseline characteristics group A Colloids group
Crystalloids group
Baseline characteristics group B Colloids group
Crystalloids group
Country: Kenya, Tanzania, Uganda Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: mortality at 48 h, mortality at 4 weeks, neurologic sequelae at 4 and 24 weeks, episodes of hypertensive shock within 48 h, adverse events Outcomes relevant to the review: mortality (4 weeks) |
|
| Notes |
Funding/declarations of interest: supported by a grant from Medical Research Council UK; resuscitation fluids donated by Baxter Healthcare. Neither had involvement in study Study dates: January 2009‐January 2011 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed in permuted blocks of random sizes and was stratified according to clinical center" |
| Allocation concealment (selection bias) | Low risk | Quote: "Trial numbers were kept inside opaque, sealed envelopes, which were numbered consecutively and opened in numerical order by a study clinician" |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few losses, which are clearly reported |
| Selective reporting (reporting bias) | Unclear risk | Retrospective clinical trials registration (ISRCTN69856593); not feasible to assess risk of selective outcome reporting |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Martin 2005.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 40 Inclusion criteria: American‐European Consensus Conference definition of ALI; serum protein level < 6.0 g/dL; ongoing nutritional support; mechanical ventilation ≥ 24 h Exclusion criteria: haemodynamic instability; renal disease; clinically documented cirrhosis; allergy to albumin or furosemide; < 18 years of age; pregnancy; serum sodium level > 155 mEq/L or potassium level < 2.5 mEq/L Participant condition: ALI; acute respiratory distress syndrome Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: need for mechanical ventilation, shock, documented nosocomial infections, mortality Outcomes relevant to the review: mortality (30 days) |
|
| Notes |
Funding/declarations of interest: supported in part by the National Institutes of Health and Bayer Healthcare, Inc. (provision of study drug and an unrestricted grant) Study dates: February 1999‐December 2002 Study also included study of furosemide, given in each group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer‐generated four‐subject‐block randomization list held by the investigational pharmacy at each hospital" |
| Allocation concealment (selection bias) | Low risk | Quote: "List held by the investigational pharmacy at each hospital, which was also responsible for study drug preparation, camouflaged, blinding, and dispensation" |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Quote: "Albumin study drug was concealed within a sterile plastic container and infused in opaque intravenous tubing to obscure visual detail" |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Outcome assessors blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Masoumi 2016.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 100 Inclusion criteria: traumatic haemorrhagic shock Exclusion criteria: heart failure; people who received blood before study was completed; death; sensitivity to serum; transfer to operating room before study completed; hepatic insufficiency; respiratory failure; renal impairment; sepsis; severe anaemia; non‐haemorrhagic shock; history of sensitivity to intervention fluids; < 16 years of age Participant condition: traumatic haemorrhagic shock Baseline characteristics Colloids group
Crystalloids group
Country: Iran Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: base excess (using measures of arterial blood gas); shock index Outcomes relevant to the review: none (see note below) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: not reported Note: study authors report, "Five subjects (10% in HES group (Voluven) and seven (14%) in NS group were excluded from the study due to death, blood transfusion, and transfer to the operating room and their info was not included in the final analysis". Number of participants was not reported for each outcome and we were unable to include these data in our analysis |
|
Mattox 1991.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 422 Inclusion criteria: ≥ 16 years of age; victim of penetrating or blunt trauma within last hour before randomisation; initial field SBP ≤ 90 mmHg Exclusion criteria: initial trauma score ≤ 2; revised trauma score ≤ 1; pregnancy; history of seizures; coagulopathy; liver or renal disease; application of medical anti‐shock trousers Participant condition: victims of penetrating or blunt trauma Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: out‐of‐hospital. Ambulance paramedic service |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: mortality, change in revised trauma score, complication (to include acute renal failure), fluid and urine output, laboratory variables, adverse events (allergic reaction) Outcomes relevant to the review: mortality (30 days; study authors report that most deaths were within 24 h), adverse events (allergic reaction) |
|
| Notes |
Funding/declarations of interest: supported by grant from Pharmacia AB, Sweden and Pharmacia, Inc., New Jersey Study dates: October 1987‐November 1988 Note: for mortality data we used data reported for participants that were analysed by study investigators (for 184 participants in colloids group, and 175 participants in the crystalloid group). In the previous version of the review (Perel 2013), review authors used total number randomised (211 in each group) for analysis of mortality data. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | No details of randomisation method, but completed externally. We have assumed low risk. Fluid bags labelled with consecutive numbers |
| Allocation concealment (selection bias) | Low risk | Randomisation sequence generated externally. Personnel involved in treatment of participants were unlikely to be aware of code |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Blinded. Use of identical, coded treatment bags |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Personnel blinded until end of study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High number of losses postrandomisation. 63 or 424 participants, reasons given were because of eligibility criteria, and being given < 250 mL of allocated fluid. Data reported as per‐protocol data. Study authors reported analysis was performed to compare ITT with per‐protocol, with no difference in results |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Unclear risk | Study authors did not report baseline characteristics |
| Other bias | Low risk | No other sources of bias identified |
McIntyre 2008.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 40 Inclusion criteria: early septic shock; hypotension; systemic inflammatory response syndrome; a suspected or confirmed infectious source Exclusion criteria: people who received > 500 mL of colloid (5% albumin or pentastarch) or 2000 mL of crystalloid fluid; other forms of shock (haemorrhagic, cardiogenic or obstructive shock); acute myocardial infarction or cardiogenic pulmonary oedema; von Willebrand's disease; previous severe reaction to HES; chronic renal failure requiring dialysis; immediate need for surgery; a contraindication to internal jugular or subclavian line insertion; projected life expectancy < 3 months; < 18 years of age; pregnant or lactating; previous ICU admission with septic shock during the present hospitalisation Participant condition: septic shock Baseline characteristics Colloids group
Crystalloids group
Country: Canada Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: feasibility measure, clinical events such as hospital, 28‐day and 90‐day mortality, ICU and hospital LoS, organ failure Outcomes relevant to the review: mortality (28 days); blood transfusion (any volume); RRT |
|
| Notes |
Funding/declarations of interest: lead author received unrestricted funds from Bristol Myers Squibb and Edwards Life Sciences to conduct trial. Also unrestricted funds from Abbott Laboratories Study dates: not reported Trial was terminated early because of lower than anticipated recruitment and the results from another similar trial (Brunkhorst 2008). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Central randomisation using a computerised permuted four‐block randomisation scheme (generated by an independent bio‐statistician) |
| Allocation concealment (selection bias) | Low risk | Quote: "Only the designated research pharmacist at each institution was aware of the treatment allocation for individual patients" |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Quote: "Study fluids were prepared and blinded ahead of time by the site research pharmacist" |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Low risk | Quote: "Study fluids were prepared and blinded ahead of time by the site research pharmacist" |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Only pharmacist aware of group allocation, therefore assume that outcome assessors were blinded |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Low risk | Only pharmacist aware of group allocation, therefore assume that outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data reported for all randomised participants. One participant was excluded post‐randomisation because of meeting exclusion criteria |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias. We noted that 90‐day mortality was listed as an outcome in the methods section of the published report but not included in the results |
| Baseline characteristics | Unclear risk | Baseline characteristics were similar between groups with the exception of the need for organ support at baseline. Fewer patients in the saline group (versus pentastarch group) were on a vasopressor at baseline. We could not be certain whether these differences would influence outcome data |
| Other bias | Low risk | No other sources of bias identified |
McIntyre 2012.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 50 Inclusion criteria: ≥ 18 years of age; suspected septic shock (refractory hypotension plus ≥ 2 criteria for systemic inflammatory response syndrome) Exclusion criteria: > 8 h passed from the first hypotensive episode; received > 250 mL of colloid fluid (albumin or HES); shock (e.g. haemorrhagic, obstructive, or cardiogenic); previous ICU admission with severe sepsis or septic shock during the current hospitalisation; burn or traumatic brain injury before the current hospitalisation; history of chronic liver disease; religious objection to use of albumin; known previous severe reaction to albumin; lack of commitment of the patient, family, or clinical team to full therapeutic management; pregnant; enrolled in another related interventional trial Participant condition: septic shock Overall baseline characteristics
Country: Canada Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: related to study feasibility; overall mortality (at 28 days) Outcomes relevant to the review: mortality (but number randomised to each group not reported and therefore no available data for the review) |
|
| Notes |
Funding/declarations of interest: supported by funding from Canadian Institute of Health Research and CSL Behring. Also partial funding from SAFE trial, and unlimited grant from Univerisity of Alberta Study dates: April 2009‐December 2009 Mortality was reported overall, but not by group; 12 out of 50 participants died. This was a feasibility pilot study. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Used randomisation lists but no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Identical glass containers with opaque coverings were used to conceal study fluids from all participants and personnel |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Identical glass containers with opaque coverings were used to conceal study fluids from outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few losses, which were reported and explained |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Unclear risk | Not reported for each group |
| Other bias | Low risk | No other sources of bias identified |
Metildi 1984.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 46 Inclusion criteria: established pulmonary failure; intrapulmonary shunt > 20% and a roentgenogram of the chest demonstrating interstitial and intra‐alveolar oedema Exclusion criteria: no details Participant condition: severe pulmonary insufficiency Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: hospital, surgical ICU |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: colloid osmotic pressure, PCWP, cardiac index, stroke work, intrapulmonary shunt, fluid volume, mortality, length of ICU stay Outcomes relevant to the review: mortality (time point not reported, some deaths were within 48 h) |
|
| Notes |
Funding/declarations of interest: supported by ONR Contract (definition of ONR not provided in study report) Study dates: June 1978‐May 1979 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Assigned by random number. No additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Modig 1986.
| Methods | Quasi‐RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 31 Inclusion criteria: severe traumatic shock with a SBP < 70 mmHg Exclusion criteria: < 18 years of age; > 75 years of age; considered to be in a terminal stage; associated major cerebral, thoracic or abdominal injuries; long‐bone fractures requiring major primary anaesthetic and surgical intervention Participant condition: severe traumatic shock Baseline characteristics Colloids group
Crystalloids group
Country: Sweden Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: development of ARDS, complications to include mortality Outcomes relevant to the review: mortality (during study period) |
|
| Notes |
Funding/declarations of interest: supported by grants from Swedish National Defense Research Institute, Swedish Association against Heart and Chest Diseases, and the Laerdal Foundation Study dates: February 1980‐February 1983 Note: only one author for this study report. In previous version of the review (Perel 2013), the study ID was Modig 1983. Some discrepancies between reports of Modig 1983 and Modig 1986, however they appear to be reports of the same study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation based on even/uneven data of admission to emergency department |
| Allocation concealment (selection bias) | High risk | No concealment. No randomisation sequence |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias. |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Morrison 2011.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 107 Inclusion criteria: ≥ 16 years of age; initial assessment of GCS ≤ 8; blunt traumatic mechanism of injury Exclusion criteria: known pregnancy; primary penetrating injury; vital signs absent before randomisation; previous IV therapy ≥ 50 mL; time interval between arrival at scene and IV access > 4 h; amputation above wrist or ankle; any burn (thermal, chemical, electrical, radiation); suspected environmental hypothermia; asphyxia (strangulation, hanging, choking, suffocation, drowning); fall from height ≤ 1 m or ≤ 5 stairs Participant condition: blunt trauma Baseline characteristics Colloids group
Crystalloids group
Country: Canada Setting: out‐of‐hospital, paramedic service, air and land |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: survival at 30 days, 48‐h survival, cerebral performance at discharge, Functional Independence Measure, Disability Rating Scale, Glasgow Outcome Scale, Extended Glasgow Outcome Scale, neuropsychological assessments Outcomes relevant to the review: mortality (30 days) |
|
| Notes |
Funding/declarations of interest: Defence Research and Development Canada (DRDC) and Biophausia Sweden provided the study fluid (RescueFlow) free of charge without obligation to the investigators for the duration of the trial Study dates: unclearly reported. Completion date December 2008 (from clinical trials registration documents). Study dates in an associated publication with a subset of participants were September 2004‐January 2006. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation used (from Morrison 2009 (see Morrison 2011) ‐ use of computer‐generated random table or block randomisation) |
| Allocation concealment (selection bias) | Low risk | Concealment with use of sealed opaque envelopes |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Personnel remained blinded until after opening of envelopes. Lack of blinding unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Lack of blinding unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Study dates are not clearly reported. However, study appears to have retrospective clinical trials registration (NCT00878631), and publication of retrospective protocols. Not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | We noted a higher number of male participants in the crystalloid group, but we did not expect this to influence outcome data |
| Other bias | Low risk | No other sources of bias identified |
Myburgh 2012.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 7000 Inclusion criteria: requiring fluid resuscitation in the ICU; > 18 years of age Exclusion criteria: > 1000 mL HES before screening; impending or current dialysis‐dependent renal failure; evidence of intracranial haemorrhage on cranial computed tomography Participant condition: requiring fluid resuscitation in the ICU (to include trauma, sepsis, brain injury) Baseline characteristics Colloids group
Crystalloids group
Country: Australia and New Zealand Setting: ICU, 32 hospitals |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: all cause mortality (at 90 days, in the ICU, in hospital, and within 28 days); acute kidney injury (using RIFLE); need for RRT; new organ failure for cardiovascular; respiratory; coagulation; liver systems that were not present at baseline; duration of mechanical ventilation; adverse events (to include allergic reaction, itching, rashes), cause‐specific mortality; duration of ICU and hospital stay; rate of death in the ICU, hospital, and at 28 days Outcomes relevant to the review: mortality (within 28 days, within 90 days); need for RRT (dialysis); adverse events (to include allergic reaction, itching, rashes) |
|
| Notes |
Funding/declarations of interest: supported by a grant from the National Health and Medical Research Council of Australia, and by unrestricted grants from New South Wales Ministry of Health, and Fresenius Kabi (supplied study fluids and distributed them to sites). Funding agencies had no input into the design, conduct, data collection, statistical analysis, or writing of the manuscript Study dates: December 2009‐January 2012 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used web‐based randomisation program |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There are an inconsistent number of losses between flow chart and data tables. However, loss of participants is < 10% |
| Selective reporting (reporting bias) | Low risk | Prospective clinical trials registration (NCT00935168). Most outcomes (all review outcomes) were reported according to clinical trials registration |
| Baseline characteristics | Low risk | Baseline characteristics appeared balanced between groups |
| Other bias | High risk | 15% of participants in each group had HES before start of study; this may introduce bias in the crystalloid group |
Nagy 1993.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 41 Inclusion criteria: adults with measurable SBP < 90 mmHg because of haemorrhage Exclusion criteria: no details Participant condition: haemorrhagic shock Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic parameters, arterial blood gases, blood product requirement (transfusion) respiratory measurements Outcomes relevant to the review: mortality (during study), blood transfusion (packed red blood cells) |
|
| Notes |
Funding/declarations of interest: supported by a grant from American Critical Care, McGaw Park, Illinois Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants described as randomised, but no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics not reported. Study authors state "There was no difference between groups with regard to race, age, sex or weight" |
| Other bias | Low risk | No other sources of bias identified |
Ngo 2001.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 222 Inclusion criteria: children from 1‐15 years of age; dengue haemorrhagic fever (grade III or IV); had not received any IV fluid therapy; with a parent or guardian who gave consent Exclusion criteria: severe haemorrhagic manifestations for whom transfusion seemed likely; children with chronic disorders Participant condition: DSS Baseline characteristics Colloids group (dextran 70)
Colloids group (gelatins)
Crystalloids group (RL)
Crystalloids group (NS)
Country: Vietnam Setting: ICU, paediatric hospital |
|
| Interventions |
Colloids group (dextran 70)
Colloids group (gelatins)
Crystalloids group (RL)
Crystalloids group (NS)
|
|
| Outcomes |
Outcomes measured/reported: initial pulse pressure recovery time, occurrence and timing of subsequent episodes of shock, drop in haematocrit and pulse rate after the first hour, total volume of dextran 70 required after first hour, mortality (time point not reported), adverse events (allergic reactions, severe epistaxis requiring blood transfusion) Outcomes relevant to the review: mortality (time point not reported), transfusion of blood products, adverse events (allergic reactions) |
|
| Notes |
Funding/declarations of interest: study drugs all supplied by manufacturer (B Braun) Study dates: September 1996‐September 1997 Note: study authors report that 222 children had dengue haemorrhagic fever that was grade III, and 8 children had dengue haemorrhagic fever that was grade IV. Because of the small number of grade IV children, the study authors decided to exclude these from the report. Therefore, analysis is for 222 participants. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation done externally in blocks of 10 |
| Allocation concealment (selection bias) | Low risk | Use of opaque envelopes containing only a treatment pack number |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Fluid solutions were in bottles covered in opaque black insulating tape to ensure blinding |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Low risk | Fluid solutions were in bottles covered in opaque black insulating tape to ensure blinding |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details; lack of blinding unlikely to influence outcome data |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Appear comparable |
| Other bias | High risk | 36.4% participants in the RL group also received dextran 70 after the first hour; 30.4% participants in the NS group also received dextran 70 after the first hour |
O'Mara 2005.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 31 Inclusion criteria: 25% or > TBSA burn with smoke inhalation, or > 40% TBSA burn if inhalation injury was not present Exclusion criteria: patients who had withdrawal of support without efforts of resuscitation; ≤ 16 years of age Participant condition: burns Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: fluid volumes; intra‐abdominal pressure; urine output; renal function; peak airway pressure; mortality Outcomes relevant to the review: mortality (time point not reported) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used predetermined randomisation code which was maintained by primary investigator |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Oliveira 2002.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 29 Inclusion criteria: newly admitted to ICU; clinically suspected infection; fulfilled ≥ 2 criteria of systemic inflammatory response syndrome; presence of perfusion abnormalities Exclusion criteria: adjustment of catecholamine doses or aggressive volume resuscitation (fluid administration > 200 mL within 30 min) during 180‐min study period; coma after pulmonary cardiocerebral resuscitation; renal failure; hypernatraemia; pregnant Participant condition: severe sepsis Baseline characteristics Colloids group
Crystalloids group
Country: Brazil Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic parameters; PAOP; cardiac index; systemic vascular resistance; stroke volume; metabolic variables; mortality rate Outcomes relevant to the review: mortality (time point not reported) |
|
| Notes |
Funding/declarations of interest: supported by The Wellcome Trust Study dates: study was completed over 23 months, dates not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used random number table |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Unclear risk | We noted that participants in the colloids group were younger, with statistically significantly lower APACHE II scores. We could not be certain whether these differences would influence outcome data |
| Other bias | Low risk | No other sources of bias identified |
Park 2015.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 110 Inclusion criteria: patients with cancer and septic shock Exclusion criteria: no details Participant condition: patients with cancer and septic shock Baseline characteristics Colloids group
Crystalloids group
Country: Brazil Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: mortality (30 days, 90 days, in the ICU), ICU and hospital LoS, daily SOFA scores, rates and duration of mechanical ventilation, renal replacement, need for vasopressor drugs, status performance, fluid balance Outcomes relevant to the review: mortality (30 days), RRT (outcome data not reported in the abstract) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: start date not reported, recruitment up to November 2014 Available report is from an abstract only |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised. No additional details in abstract |
| Allocation concealment (selection bias) | Unclear risk | No details in abstract |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Described as double‐blind but no additional details. However, lack of blinding unlikely to influence outcome data for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details. Assume all participants were accounted for (although the percentage data for mortality, which did not give whole numbers, suggests some loss of participants) |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Unclear risk | Baseline characteristics not reported in abstract |
| Other bias | Unclear risk | Insufficient details in abstract to assess other sources of bias |
Perner 2012.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 800 Inclusion criteria: adults who needed fluid resuscitation in the ICU and who had fulfilled criteria for severe sepsis within the previous 24 h according to the SCCM/ACCP and where informed consent was obtainable either from the patient or by proxy (in Denmark, 2 physicians followed by delayed consent from next of kin and the patient’s general practitioner. In Iceland, Finland and Norway, next of kin) Exclusion criteria: < 18 years of age; previously randomised in the 6S trial; allergy towards HES or malic acid; treatment with > 1000 mL of any synthetic colloid within the last 24 h prior to randomisation; any form of RRT; acute burn injury > 10% TBSA; severe hyperkalaemia, pK > 6 mM; liver or kidney transplantation during current hospital admission; intracranial bleeding within current hospitalisation; enrolment into another ICU trial of drugs with potential action on circulation, renal function or coagulation; withdrawal of active therapy Participant condition: severe sepsis Baseline characteristics Colloids group
Crystalloids group
Country: Denmark, Norway, Finland and Iceland Setting: 26 ICUs |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic parameters; PAOP; cardiac index; systemic vascular resistance; stroke volume; metabolic variables; mortality (at 28 days, at 90 days); transfusion of blood products (packed red blood cells, FFP, platelets; at day 1, day 2, day 3, and cumulative); adverse events (allergic reactions) Outcomes relevant to the review: mortality (at 28 days, and at 90 days); RRT; transfusion of blood products (packed red blood cells at day 1); adverse events (allergic reactions) Note: in order to avoid double of counting of participants we only included transfusion of one type of blood products (red blood cells) and on the first day |
|
| Notes |
Funding/declarations of interest: Danish Research Council. Study fluids supplied free of charge by B Braun. Neither funders nor B Braun had influence on protocol, trial conduct, data analyses and reporting. Study dates: December 2009‐November 2011 Note: the previous version of this review used mortality data at 90 days (Perel 2013); in this review we have analysed mortality data at 28 days. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated allocation concealment |
| Allocation concealment (selection bias) | Low risk | Centralised, blinded randomisation |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Used identical fluid bags, covered in black opaque plastic |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Low risk | Used identical fluid bags, covered in black opaque plastic |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Outcome assessors were blinded to treatment groups |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Low risk | Outcome assessors were blinded to treatment groups |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Very few losses, which were explained in flow chart (804 participants randomised, but ITT data for only 798) |
| Selective reporting (reporting bias) | Low risk | Prospective clinical trials registration (NCT00962156). Generally all 90‐day outcomes listed in the protocol were well reported in the primary manuscript. Length of hospital stay was not reported in primary publication but was in the long‐term outcomes paper |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | High risk | Most participants in each group received other fluids (study authors listed other fluids as crystalloids, nutrition, water, fluid with medications, synthetic colloids, and albumin); because some participants received additional colloids in both groups, this may influence study results |
Philips 2015.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 308 Inclusion criteria: patients with cirrhosis and who had sepsis‐induced hypotension Exclusion criteria: no details Participant condition: cirrhosis and sepsis‐induced hypotension Baseline characteristics Colloids group
Crystalloids group
Country: India Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: MAP; HR; lactate; lactate clearance; urine output; survival at 1 week Outcomes relevant to the review: mortality (7 days) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: not reported Abstract only |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Abstract only with limited detail on randomisation methods |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Clinical trials registration (NCT02462902). We do not know if this was prospectively registered; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Unclear risk | Insufficient information in abstract to assess risk of other bias |
Pockaj 1994.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 107 Inclusion criteria: adults with metastatic cancer whose standard treatment had failed and had expected survivals of > 3 months Exclusion criteria: no details Participant condition: vascular leak syndrome Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: volume of fluid; number of doses of interleukin‐2; weight gain; pulse; SBP; days in ICU; time to discharge; laboratory changes (haematocrit etc.); blood transfusion; mortality Outcomes relevant to the review: mortality (time point not reported); blood transfusion (any volume) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: March 1990‐August 1990 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised but no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Some participants did not complete the full course of treatment and reasons were explained. Outcome data for participants requiring blood transfusion were for all randomised participants, but data for mortality were for 76 participants (loss of 18 participants in colloid group, and loss of 13 participants in crystalloid group) |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Quinlan 2004.
| Methods | RCT Parallel design Multicentre |
|
| Participants |
Total number of randomised participants: 20 Inclusion criteria: people fulfilling American‐European Consensus criteria for ALI (including ARDS) Exclusion criteria: no details Participant condition: ALI/ARDS Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: hospital ICU |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: fluid volume; total protein; thiols; antioxidant; iron‐binding anti‐oxidant protection; iron‐oxidising antioxidant protection; mortality Outcomes relevant to the review: mortality (28 days) |
|
| Notes |
Funding/declarations of interest: supported by grants from the Dunhill Medical Trust, British Lung Foundation, and the Plasma Protein Therapeutics Association Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised, but no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Unclear risk | We noted that participants in the crystalloid group were younger. We could not be certain whether this might influence outcome data |
| Other bias | Low risk | No other sources of bias identified |
Rackow 1983.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 26 Inclusion criteria: included if pretreatment determinations revealed: systolic intra‐arterial pressure of < 90 mmHg; CI < 2.2 L/min/m²; serum arterial lactate > 18 mg/dL; WP < 15 mmHg Exclusion criteria: < 18 years of age; considered to be in a terminal state; manifesting a significant coagulopathy Participant condition: septic or hypovolaemic shock Baseline characteristics Colloids group (HES)
Colloids group (albumin)
Crystalloids group
Country: USA Setting: hospital |
|
| Interventions |
Colloids group (HES)
Colloids group (albumin)
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic variables; respiratory data; survival (during study period and hospital stay) Outcomes relevant to the review: mortality (within 24 h) |
|
| Notes |
Funding/declarations of interest: supported by a grant from American Critical Care Study dates: October 1979‐June 1981 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned but no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | We noted a larger number of male participants in the colloids group. However, overall numbers of participants were few and we assumed that gender differences would not influence outcome data |
| Other bias | Low risk | No other sources of bias identified |
Shah 1977.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 20 Inclusion criteria: severe multiple trauma and shock; SBP < 90 mmHg Exclusion criteria: no details Participant condition: severe multiple trauma and shock Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: mortality; respiratory and haemodynamic variables Outcomes relevant to the review: mortality (during study period) |
|
| Notes |
Funding/declarations of interest: supported by grants from National Institute of General Medical Sciences Study dates: not reported Data in baseline characteristics only given for 8 participants in crystalloid group (3 had died because it was not possible to resuscitate them) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised using a sealed envelope technique. Insufficient details |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelope containing fluid group. Insufficient details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 participants were excluded from all analyses because of death. However, we have included these mortality data for this review |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Upadhyay 2005.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 60 Inclusion criteria: 1 month‐12 years of age; septic shock Exclusion criteria: features of multiorgan failure such as disseminated intravascular coagulation with bleeding manifestation; jaundice; acute renal failure; adult respiratory distress syndrome; coma; < 1 month old; underlying immunodeficiency status such as leukaemia; lymphoma; long‐term immunosuppressive therapy Participant condition: paediatric septic shock Baseline characteristics Colloids group
Crystalloids group
Country: India Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: fluid volumes; haemodynamic stability; organ failure; acute respiratory distress syndrome; acute renal failure; mortality Outcomes relevant to the review: mortality (time point not reported) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: March 1999‐April 2000 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables |
| Allocation concealment (selection bias) | Low risk | Random number generation kept in sealed envelopes by one investigator |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Van der Heijden 2009.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 48 Inclusion criteria: mechanically ventilated and critically ill people with clinical hypovolaemia and at risk for, or with, ALI/ARDS Exclusion criteria: > 78 years of age; pregnant; known anaphylactoid reaction to colloid fluids; life expectancy < 24 h Participant condition: clinical hypovolaemia Baseline characteristics Colloids group (HES)
Colloids group (albumin)
Colloids group (gelatin)
Crystalloids group
Country: the Netherlands Setting: hospital |
|
| Interventions |
Colloids group (HES)
Colloids group (albumin)
Colloids group (gelatin)
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic variables; respiratory variables; mortality Outcomes relevant to the review: mortality (until discharge from the ICU) |
|
| Notes |
Funding/declarations of interest: supported in part by B Braun Medical, Melsungen, Germany and the Netherlands Heart Foundation, The Hague Study dates: not reported Patients stratified into septic and non‐septic. We combined these groups. Use of online supplementary information for some data |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation performed by pharmacist; no additional detail on methods used to generate codes |
| Allocation concealment (selection bias) | Low risk | Used sealed envelopes prepared by pharmacist |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Vassar 1990.
| Methods | RCT Parallel design Single centre (assumed, but not reported by study authors) |
|
| Participants |
Total number of randomised participants: 47 Inclusion criteria: people attending the emergency department with ≤ SBP 90 mmHg Exclusion criteria: people who appeared to be < 18 years of age; pregnant women; known severe pre‐existing cardiac, hepatic, or renal disease Participant condition: SBP ≤ 80 mmHg Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: emergency department |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic variables; blood chemistry; mortality; adverse events (allergic reactions) Outcomes relevant to the review: mortality (28 days); adverse events (allergic reactions) |
|
| Notes |
Funding/declarations of interest: supported in part from the National Institutes of Health Study dates: April 1987‐May 1988 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Identical bottles used to conceal study fluids from participants and personnel |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration; not feasible to assess risk of selective reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias detected |
Vassar 1991.
| Methods | RCT Parallel design Single centre (assumed, but not reported by study authors) |
|
| Participants |
Total number of randomised participants: 166 Inclusion criteria: trauma patients being transported to hospital by helicopter; SBP ≤ 100 mmHg; palpable peripheral pulse or a sinus complex on ECG; ≥ 18 years of age Exclusion criteria: women who appeared to be pregnant; chronically debilitated people with severe hepatic, renal, cardiac, or neurologic disease; peripheral oedema Participant condition: hypovolaemic Baseline characteristics Colloids group
Crystalloids group
Country: USA Setting: out‐of‐hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: survival (to hospital discharge, and in emergency department); haemodynamic parameters; HR; volume of fluid given; volume of surgical blood loss and blood replacement in first 24 h; intracranial bleed in those with head injury; survival in patients with head injury; complications; adverse events (allergic reactions) Outcomes relevant to the review: mortality; adverse events (allergic reactions) |
|
| Notes |
Funding/declarations of interest: supported in part by a grant from National Institutes of Health and by pharmacia. HSD provided by pharmaceutical company Study dates: June 1986‐February 1988 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used random number tables |
| Allocation concealment (selection bias) | Low risk | Bags were identical and placed in order by a code established by hospital pharmacy team to be used by helicopter paramedics |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Study solutions were prepared by pharmacist in identical 250 mL bags with codes determined by random number tables |
| Blinding of outcome assessment (detection bias): mortality | Low risk | All personnel involved in participant care were blinded to study groups for at least one month after participants were entered into trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | High risk | Study authors changed concentration of HSD during study period. It is unclear whether this could have influenced outcome data. 14 of the 83 participants in the crystalloids group and 15 of the 83 participants in the colloids group were given unspecified resuscitation before flight nurses arrived and this could influence study results |
Vassar 1993a.
| Methods | RCT Parallel design Single centre (assumed, but not reported by study authors) |
|
| Participants |
Total number of randomised participants: 258 Inclusion criteria: SBP < 90 mmHg Exclusion criteria: asystolic or undergoing cardiopulmonary resuscitation; lacked a sinus complex on ECG; appeared to be < 18 years of age; seen > 2 h from time of injury; pregnant; known to have a history of seizures or a bleeding disorder; appeared to have a pre‐existing hepatic cardiac, or renal disease, as indicated by ascites or peripheral oedema; injured as a result of a burn; BP > 90 mmHg by time that IV access was established; lacked IV access Participant condition: trauma Baseline characteristics Colloids group (HSD)
Crystalloids group (NS)
Crystalloids group (HS)
Country: USA Setting: out‐of‐hospital, ambulance service |
|
| Interventions |
Colloids group (HSD)
Crystalloids group (NS)
Crystalloids group (HS)
|
|
| Outcomes |
Outcomes measured/reported: BP response; mortality (at hospital discharge); survival compared with that predicted by norms from the MTOS Outcomes relevant to the review: mortality |
|
| Notes |
Funding/declarations of interest: supported by a grant from national Institutes of Health, and Kabi Pharmaceuticals, Inc. Study dates: September 1988‐July 1991 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number list |
| Allocation concealment (selection bias) | Low risk | Assignment made at pharmacy level, and fluid bag contents concealed from paramedic personnel |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Study fluids were prepared in identical bags, and personnel were blinded to group allocation |
| Blinding of outcome assessment (detection bias): mortality | Low risk | All investigators and personnel were blinded throughout the trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Large number of exclusions post‐randomisation (36 participants) because these participants did not meet the eligibility. Acceptable loss of participants recruited in a trauma setting (minimal inclusion criteria but large exclusion criteria established once in hospital) |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Vassar 1993b.
| Methods | RCT Parallel design Single centre (assumed, but not reported by study authors) |
|
| Participants |
Total number of randomised participants: 194 Inclusion criteria: SBP < 90 mmHg Exclusion criteria: asystolic or undergoing cardiopulmonary resuscitation; lacked a sinus complex on ECG; appeared to be < 18 years of age; > 2 h from the time of injury; thought to be pregnant; known to have a history of seizures or a bleeding disorder; appeared to have pre‐existing hepatic, cardiac, or renal disease, as indicated by ascites or peripheral oedema; were injured as a result of a burn; or lacked IV access Participant condition: various Baseline characteristics Colloids group (HSD)
Colloids group (HSD 12% dextran)
Crystalloids group (RL)
Crystalloids group (HS)
Country: USA Setting: out‐of‐hospital |
|
| Interventions |
Colloids group (HSD)
Colloids group (HSD 12% dextran)
Crystalloids group (RL)
Crystalloids group (HS)
|
|
| Outcomes |
Outcomes measured/reported: mortality (until hospital discharge) Outcomes relevant to the review: mortality |
|
| Notes |
Funding/declarations of interest: supported in part by grant from Kabi‐Pharmacia Study dates: March 1990‐June 1991 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used computer‐generated random number tables |
| Allocation concealment (selection bias) | Low risk | Bags were coded, and allocated sequentially to helicopters |
| Blinding of participants and personnel (performance bias): mortality | Low risk | All personnel were blinded. Used sealed bags with coded identification label |
| Blinding of outcome assessment (detection bias): mortality | Low risk | All investigators kept blinded throughout trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High number of exclusions after study fluids administered because of late assessment of inclusion/exclusion criteria, but inevitable because of the out‐of‐hospital setting. No additional apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared largely comparable |
| Other bias | Low risk | No other sources of bias identified |
Vlachou 2010.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 26 Inclusion criteria: adult acute burns admission with injury > 15% TBSA Exclusion criteria: < 16 years of age or > 80 years of age; burn > 80% TBSA; pregnant; transfer delay > 6 h from time of injury; history or biochemical evidence of renal impairment on admission; history or haematological evidence of a bleeding diathesis; failure to obtain consent Participant condition: burns > 15% TBSA Baseline characteristics Colloids group
Crystalloids group
Country: UK Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: fluid intake and balance; weight; urinary albumin; respiratory function; serum C‐reactive protein; mortality; RRT Outcomes relevant to the review: mortality (during hospital stay); RRT; blood transfusion (any volume) |
|
| Notes |
Funding/declarations of interest: none Study dates: May 2004‐May 2006 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation in blocks of 10 participants |
| Allocation concealment (selection bias) | Unclear risk | Used sealed envelopes, but no additional details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 3 participants excluded from crystalloid group because they were given colloid. Small study, so this represents a large percentage of losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Wills 2005.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 383 Inclusion criteria: 2‐15 years of age; presenting directly to the hospital with clinical DSS; parent or guardian provided consent Exclusion criteria: not reported Participant condition: DSS Baseline characteristics Colloids group (dextran)
Colloids group (HES)
Crystalloids group
Country: Vietnam Setting: paediatric ICU |
|
| Interventions |
Colloids group (dextran)
Colloids group (HES)
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: requirement for supplemental intervention with rescue colloid; time taken to achieve initial and sustained cardiovascular stability; pattern of change in haematocrit; days in hospital; adverse effects (including need for blood transfusion, rashes), mortality Outcomes relevant to the review: need for transfusion of a blood product; mortality (time point not reported); adverse events (rashes) |
|
| Notes |
Funding/declarations of interest: supported by the Wellcome Trust Study dates: August 1999‐March 2004 Note: this study included a separate arm comparing two colloids for participants with severe shock (pulse pressure, ≤ 10 mm Hg); we did not include these participants because colloids were not compared with a crystalloid |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of computer‐generated random numbers completed by independent research staff |
| Allocation concealment (selection bias) | Low risk | Allocation concealed through treatment packs of fluid prepared in advance, in cardboard containers, and only identifiable by a study number |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Treatment packs of fluid were prepared in advance, in cardboard containers, and only identifiable by a study number |
| Blinding of participants and personnel (performance bias): transfusion/renal replacement therapy/adverse events | Low risk | Treatment packs of fluid were prepared in advance, in cardboard containers, and only identifiable by a study number |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding for assessment of mortality; lack of blinding unlikely to influence data for this outcome |
| Blinding of outcome assessment (detection bias): transfusion/renal replacement therapy/adverse events | Low risk | Blinding reported for assessment of other outcomes, and we assumed that assessment of transfusion data was also blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | High risk | 31% participants in the crystalloid group were also given colloids and this may have influenced study results |
Wu 2001.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 34 Inclusion criteria: ≥ 16 years of age; MAP < 80 mmHg or SBP < 100 mmHg; impression of haemorrhagic or spinal shock Exclusion criteria: pregnant; history of congestive heart disease; intubated mechanically ventilated patients; refractory to initial fluid challenge Participant condition: hypovolaemic shock Baseline characteristics Colloids group
Crystalloids group
Country: Taiwan Setting: hospital, emergency department |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: haemodynamic variables; haemoglobin and haematocrit levels; survival rates Outcomes relevant to the review: mortality (time point not reported), also reported blood transfusion (although not by group) but these participants were excluded from the study |
|
| Notes |
Funding/declarations of interest: none reported Study dates: July 1997‐February 1998 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants described as randomly allocated to groups, but no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses of participants for reporting of mortality data |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | We noted some differences in gender balance between groups; we did not anticipate that these differences would influence outcome data |
| Other bias | Low risk | No other sources of bias identified |
Younes 1992.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 105 Inclusion criteria: > 18 years of age; admitted with haemorrhagic hypovolaemia (SBP < 80 mmHg) with a palpable pulse or positive ECG; not pregnant, and with a previous history of cardiac or metabolic diseases Exclusion criteria: no details Participant condition: hypovolaemic shock Baseline characteristics Colloids group
Crystalloids group (NS)
Crystalloids group (HS)
Country: Brazil Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group (NS)
Crystalloids group (HS)
|
|
| Outcomes |
Outcomes measured/reported: pulmonary complications; renal complications; cardiac complications; infectious complications; haemodynamic variables; mortality Outcomes relevant to the review: mortality (until hospital discharge) |
|
| Notes |
Funding/declarations of interest: supported by Laboratorios B Braun Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants randomised, but no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Solutions prepared in similar and unmarked bottles to ensure blinding |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Younes 1997.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 212 Inclusion criteria: people being treated for haemorrhagic hypovolaemia and requiring blood transfusion Exclusion criteria: < 16 years of age; pregnant; having cardiac or renal failure previous to their acute haemorrhagic episode; arriving with cardiac arrest Participant condition: hypovolaemia Baseline characteristics Colloids group
Crystalloids group
Country: Brazil Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: fluid volumes; survival at 24 h and 30 days; complications (renal failure, cardiac, pulmonary, infectious, and neurologic complications) Outcomes relevant to the review: mortality (30 days) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: February 1991‐November 1992 Study ID was Younes 1994 in previous version of the review (Perel 2013) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised, but no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | Fluids in "coded, externally identical vials". Quote: "Neither the investigators nor the ER team had any control or knowledge of the infused solution during the entire study period" |
| Blinding of outcome assessment (detection bias): mortality | Low risk | Quote: "Neither the investigators nor the ER team had any control or knowledge of the infused solution during the entire study period" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Four losses in HSD and 3 in NS group. Explanations for losses given. Few losses; unlikely to introduce significant risk of bias |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Younes 1998.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 23 Inclusion criteria: people with SBP < 90 mmHg; admitted to emergency department with no previous treatment Exclusion criteria: no details Participant condition: hypovolaemia Baseline characteristics Colloids group
Crystalloids group
Country: Brazil Setting: hospital |
|
| Interventions |
Colloids group
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: MAP; fluid volumes; transfusion (by volume); complications (not specified); survival (24 h) Outcomes relevant to the review: mortality (24 h) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised by closed envelopes. Insufficient details provided |
| Allocation concealment (selection bias) | Unclear risk | Used closed envelopes. Insufficient details provided |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details of blinding; unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Low risk | No other sources of bias identified |
Zhao 2013.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 120 Inclusion criteria: 18‐60 years of age; diagnosed with severe acute pancreatitis Exclusion criteria: heart disease; severe renal and hepatic dysfunction; coagulation disturbances; allergy to HES or glutamine; manifestation for > 48 h, or received resuscitation from another hospital Participant condition: severe acute pancreatitis Baseline characteristics Colloids group (HES)
Colloids group (HES and glutamine)
Crystalloids group (NS)
Country: China Setting: hospital |
|
| Interventions |
Colloids group (HES)
Colloids group (HES and glutamine)
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: respiratory infection; abdominal infection; sepsis; abdominal haemorrhage; intra‐abdominal hypertension; abdominal compartment syndrome; renal failure; acute respiratory distress syndrome; multiple organ dysfunction syndrome; operation intervention; length of ICU and hospital stay; laboratory variables Outcomes relevant to the review: mortality (day 60) |
|
| Notes |
Funding/declarations of interest: supported by grants from National Science Foundation Committee of China, and Fundamental Research Funds of Central Universities of China Study dates: January 2007‐March 2010 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were described as randomly divided into group; no additional details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias): mortality | Low risk | No details; lack of blinding unlikely to influence data for this outcome |
| Blinding of outcome assessment (detection bias): mortality | Low risk | No details; lack of blinding unlikely to influence data for this outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | No details of clinical trials registration or prepublished protocol; not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appear comparable |
| Other bias | Low risk | No other sources of bias identified |
Zhu 2011.
| Methods | RCT Parallel design Single centre |
|
| Participants |
Total number of randomised participants: 135 Inclusion criteria: people with severe sepsis Exclusion criteria: no details Participant condition: severe sepsis Baseline characteristics Colloids group (HES)
Colloids group (HES + HS)
Crystalloids group
Country: China Setting: ICU |
|
| Interventions |
Colloids group (HES)
Colloids group (HES + HS)
Crystalloids group
|
|
| Outcomes |
Outcomes measured/reported: MAP; oxygenation; arterial lactate; lactate clearance rate; APACHE I score; fluid infusion volume; urine output; MODS; mortality Outcomes relevant to the review: mortality (time point not reported) |
|
| Notes |
Funding/declarations of interest: none reported Study dates: not reported in English abstract Note: article in Chinese. Data for study characteristics taken from English abstract, and from study report tables, with translation using Google Translate |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Risk of bias' assessment made using English abstract. No details provided |
| Allocation concealment (selection bias) | Unclear risk | 'Risk of bias' assessment made using English abstract. No details provided |
| Blinding of participants and personnel (performance bias): mortality | Low risk | 'Risk of bias' assessment made using English abstract. Lack of blinding unlikely to introduce bias for mortality |
| Blinding of outcome assessment (detection bias): mortality | Low risk | 'Risk of bias' assessment made using English abstract. Lack of blinding unlikely to introduce bias for mortality |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | 'Risk of bias' assessment made using English abstract. Not feasible to assess risk of selective outcome reporting bias |
| Baseline characteristics | Low risk | Baseline characteristics appeared comparable |
| Other bias | Unclear risk | We could not be certain of other risks of bias because 'Risk of bias' assessment made using English abstract only |
ACCP: American College of Chest Physicians AFR: additional fluid rate AIDS: Acquired Immune Deficiency Syndrome AKIN: Acute Kidney Injury Network ALI: acute lung injury ANH: acute normovolaemic haemodilution APACHE II: Acute Physiology and Chronic Health Evaluation II ARDS: acute respiratory deficiency syndrome ASA: American Society of Anaesthesiologists ATLSG: Advanced Trauma Life Support Guidelines BMI: body mass index BP: blood pressure bpm: beats per minute BR: basal rate CO: cardiac output CPP: cerebral perfusion pressure CSL: Central Science Laboratory CVP: central venous pressure Da: dalton(s) DBP: diastolic blood pressure DSS: Dengue Shock Syndrome FFP: fresh frozen plasma ECG: electrocardiogram EMS: emergency medical services ER: emergency room GCS: Glasgow Coma Scale GDT: goal‐directed therapy h: hour(s) HES: hydroxyethyl starch HR: heart rate HS: hypertonic saline HSD: dextran solution with hypertonic saline ICP: intracranial pressure ICU: intensive care unit IQR: interquartile range ITT: intention‐to‐treat IV: intravenous infusion LoS: length of stay MAP: mean arterial BP M:F: male:female MIU: major injuries unit MMP‐9: matrix metalloproteinase‐9 MMSE: Mini‐Mental State Exam MODS: Multiple Organ Dysfunction Syndrome MPA: mega pascal(s) MTOS: Major Trauma Outcome Study NS: normal saline NYHA: New York Heart Association classification PAOP: pulmonary artery occlusion pressure PCWP: pulmonary capillary wedge pressure POCD: postoperative cognitive disorder RCT: randomised control trial RL: Ringer's lactate RRT: renal replacement therapy SAG M: saline‐adenine‐glucose‐mannitol SAPS II: Simplified Acute Physiology Score II SBP: systolic blood pressure SCCM: Society of Critical Care Medicine SD: standard deviation SE: standard error SEM: standard error of the mean SOFA: Sequential Organ Failure Assessment TBSA: total body surface area TEG: thromboelastography TFV: tidal flow volume TIMP‐1: tissue inhibitor of metalloproteinases‐1 TRISS: Trauma Injury Severity Score WHO: World Health Organization WP: wedge pressure
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Boutros 1979 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for major abdominal aortic surgery |
| Bowser‐Wallace 1986 | Included in previous version of review (Perel 2013). Excluded because study was not an RCT |
| Dawidson 1991 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for abdominal aortic surgery |
| Dehne 2001 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for middle ear surgery |
| Eleftheriadis 1995 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Evans 2003 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for hip replacement |
| Fries 2004 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for knee replacement |
| Gallagher 1985 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Grundmann 1982 | Included in previous version of the review (Perel 2013). Does not appear to be an RCT, and associated reference does not include crystalloid group; therefore, we have excluded this study from the review |
| Guo 2003 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for cytoreductive surgery |
| Hartmann 1993 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for major abdominal surgery |
| Hondebrink 1997 | Included in previous version of review (Perel 2013); hypoalbuminaemia after major surgery. Study ID was Woittiez 1997 in previous version of the review |
| Karanko 1987 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Lee 2011 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Ley 1990 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Mazher 1998 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| McNulty 1993 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Moretti 2003 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for general, gynaecological, orthopaedic, or urological procedures |
| Nielsen 1985 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for abdominal aortic surgery |
| Prien 1990 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for modified Whipple's operation |
| Rocha e Silva 1994 | Abstract only. Included in previous version of review (Perel 2013). Protocol for a study that has not been published. We have excluded this study because we no longer expect that results for this study will be published |
| Shires 1983 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for aortic reconstruction surgery |
| Sirieix 1999 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Skillman 1975 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for abdominal reconstructive surgery |
| Tollusfrud 1995 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Tollusfrud 1998 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Verheij 2006 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Virgilio 1979 | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for abdominal aortic surgery |
| Wahba 1996 | Included in previous version of review (Perel 2013). Excluded because participants were elective cardiac surgical patients |
| Zetterstorm 1981a | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for abdominal surgery |
| Zetterstorm 1981b | Included in previous version of review (Perel 2013). Excluded because participants were elective surgical patients scheduled for abdominal aortic surgery |
RCT: randomised control trial
Characteristics of studies awaiting assessment [ordered by study ID]
Bulanov 2004.
| Methods | RCT Parallel design |
| Participants |
Number of randomised participants: no details Inclusion criteria: no details Exclusion criteria: no details Participant condition: no details Country: Russia Setting: no details |
| Interventions |
Colloids group 1 Details: 6% HES 200/0.5 Colloids group 2 Details: 6% HES 130/0.4 Crystalloids group Details: NS |
| Outcomes |
Outcomes measured/reported: no details Outcomes relevant to the review: no details |
| Notes |
Funding/declarations of interest: no details Study dates: no details Study report requires translation from Russian to assess eligibility |
Charpentier 2011.
| Methods | RCT Parallel design Multicentre |
| Participants |
Number of randomised participants: 798 Inclusion criteria: informed consent; any patient with septic shock 6 h after catecholamine introduction Exclusion criteria: overweight; previous severe heart failure; neutropenia; cirrhosis and primary peritonitis and severe burns Participant condition: septic shock Country: France Setting: 29 hospitals |
| Interventions |
Colloids group Details: 20% albumin; 100 mL Crystalloids group Details: 0.9% NaCl; 100 mL |
| Outcomes |
Outcomes measured/reported: all‐cause mortality (at day 28); SOFA score; LoS in ICU and in hospital Outcomes relevant to the review: mortality |
| Notes |
Funding/declarations of interest: none reported Study dates: July 2006 to March 2010 Abstract only. Awaiting publication of the full text for more information to assess eligibility |
Halim 2016.
| Methods | RCT Parallel design |
| Participants |
Number of randomised participants: no details Inclusion criteria: no details Exclusion criteria: no details Participant condition: severe sepsis and septic shock Country: no details Setting: no details |
| Interventions |
Colloids group Details: 4% gelatin; 500 mL every 30 min Crystalloids group Details: 0.9% saline; 500 mL every 30 min |
| Outcomes |
Outcomes measured/reported: haemodynamic variables Outcomes relevant to the review: no details |
| Notes |
Funding/declarations of interest: no details Study dates: no details Report is from a conference abstract only. Awaiting publication of the full text for more information to assess eligibility |
NCT00890383.
| Methods | RCT Parallel design Multicentre |
| Participants |
Estimated number of randomised participants: 50 Inclusion criteria: between 18 and 65 years of age; > 40 kg; onset of trauma ≤ 48 h prior to assessment; clinically judged to be in haemorrhagic shock by the attending surgeon; 2 or more of the following characteristics: penetrating or blunt etiology with haemodynamic instability at ER or intra‐operatively; ISS > 15; hypotension defined as either ≥ 10 mmHg change in SBP or MAP ≤ 65 mmHg or needing vasopressors (dopamine ≥ 5 µg/kg/min or norepinephrine at any dose) at the time of admission; hypoperfusion defined as base deficit ≥ 4 mmol/L Exclusion criteria: known severe congestive heart failure (EF ≤ 35%); chronic renal, liver or pancreatic disease; TB, COPD, asthma; coagulopathy or bleeding tendency; allergy to HES; participation in a clinical drug trial within the last 2 months; pregnancy or lactation; GCS < 9; advanced cancer (stage IV or metastatic disease); receiving immunosuppressive drugs; do‐not‐resuscitate status; advanced directives restricting implementation of the protocol; skeletal deformity, scarring, infection, gross contamination or previous surgery at the CVP insertion site; severe hypoxaemia if the CVP is to be inserted in the subclavian area; active gastrointestinal haemorrhage; concomitant drug poisoning Participant condition: trauma Country: Philippines Setting: 2 × medical centres |
| Interventions |
Colloids group Details: tetrastarch (Voluven); goal directed volume therapy for severe trauma resuscitation Crystalloids group Details: crystalloid only; participants will receive crystalloid fluids only for volume therapy for severe trauma |
| Outcomes |
Outcomes measured/reported: intra‐abdominal hypertension; abdominal compartment syndrome Outcomes relevant to the review: none |
| Notes |
Funding/declarations of interest: sponsored by University of the Philippines and Fresenius Kabi Study dates: May 2009 to December 2009 Study described as completed in clinical trials record. Study results not posted. Awaiting publication of completed study to assess eligibility |
NCT01337934.
| Methods | RCT Parallel design Single centre |
| Participants |
Estimated number of randomised participants: 360 Inclusion criteria: ≥ 18 years of age; severe sepsis or septic shock into 6 h of evolution; written informed consent Exclusion criteria: shock from other causes; adverse reactions to human albumin; previous fluid resuscitation during current disease; previous use of albumin in the last 72 h; religion objection; enrolment in another study; traumatic brain injury; hepatic cirrhosis; end stage renal disease; plasmapheresis; patients receiving end‐of‐life care Participant condition: severe sepsis and septic shock Country: Brazil Setting: medical centre |
| Interventions |
Colloids group Details: albumin Crystalloids group Details: RL |
| Outcomes |
Outcomes measured/reported: mortality (at 7 days); SOFA score; ICU LoS; hospital LoS; ventilator‐free days; need for RRT (at 28 days); days free of vasopressor; mortality (at 28 days) Outcomes relevant to the review: mortality; need of RRT |
| Notes |
Funding/declarations of interest: sponsored by University of Sao Paulo Study dates: October 2013 to December 2017 Study described as completed in clinical trials record. Study results not posted. Awaiting publication of completed study to assess eligibility |
NCT02064075.
| Methods | RCT Parallel design Single centre |
| Participants |
Estimated number of randomised participants: 96 Inclusion criteria: between 18 and 80 years of age; subarachnoid haemorrhage; Hunt‐Hess grade I to III Exclusion criteria: patients with Hunt‐Hess grade IV to V Participant condition: subarachnoid haemorrhage Country: Hungary Setting: medical centre |
| Interventions |
Colloids group Details: 15 mL/kg RL and 15 to 50 mL/kg HES Crystalloids group Details: 15 mL/kg to 50 mL/kg RL |
| Outcomes |
Outcomes measured/reported: incidence rate of vasospasm; 30‐day survival; neurological status; GOS scores Outcomes relevant to the review: mortality |
| Notes |
Funding/declarations of interest: sponsored by University of Debrecen Study dates: February 2013 to October 2013 Study described as completed in clinical trials record. Study results not posted. Awaiting publication of completed study to assess eligibility |
Protsenko 2009.
| Methods | RCT Parallel design Multicentre |
| Participants |
Number of randomised participants: no details Inclusion criteria: no details Exclusion criteria: no details Participant condition: severe sepsis Country: Russia Setting: no details |
| Interventions |
Colloids group Details: no details Crystalloids group Details: no details |
| Outcomes |
Outcomes measured/reported: correction of hypovolaemia, and stabilising haemodynamics Outcomes relevant to the review: no details |
| Notes |
Funding/declarations of interest: no details Study dates: no details Study report requires translation from Russian to assess eligibility |
COPD: chronic obstructive pulmonary disease CVP: central venous pressure EF: ejection fraction ER: emergency room GCS: Glasgow Coma Scale HES: hydroxyethyl starch ISS: Injury Severity Score MAP: mean arterial blood pressure NS: normal saline RCT: randomised control trial RL: Ringer's lactate RRT: renal replacement therapy SBP: systolic blood pressure SOFA: Sequential Organ Failure Assessment TB: tuberculosis
Characteristics of ongoing studies [ordered by study ID]
NCT01763853.
| Trial name or title | Impact of fluid resuscitation therapy on pulmonary edema as measured by alveolar fluid clearance in patients with acute respiratory distress syndrome (ARDS) |
| Methods | RCT Parallel design Single centre |
| Participants |
Estimated number of randomised participants: 70 Inclusion criteria: ≥ 18 years of age; ICU patients under mechanical ventilation; within the first 24 h after onset of moderate or severe ARDS; hypovolaemia requiring fluid resuscitation therapy Exclusion criteria: pregnancy; < 18 years of age; refusal of the protocol; contraindications for the use of Voluven or RL; contraindications for femoral artery catheterisation or subclavian venous catheterisation Participant condition: ARDS; hypovolaemia; pulmonary oedema Country: France Setting: university hospital |
| Interventions |
Colloids group Details: 4% albumin Crystalloids group Details: no details |
| Outcomes |
Outcomes measured/reported: rate of alveolar fluid clearance; alveolar oedema fluid resorption; mortality (at 20 days) Outcomes relevant to the review: mortality |
| Starting date | December 2012 |
| Contact information | Patrick LACARIN; email: placarin@chu‐clermontferrand.fr |
| Notes | Funding/declarations of interest: sponsored by University Hospital, Clermont‐Ferrand |
NCT02721238.
| Trial name or title | Comparison of colloid (20% albumin) versus crystalloid (Plasmalyte) for fluid resuscitation in cirrhotics with sepsis induced hypotension |
| Methods | RCT Parallel design Single centre |
| Participants |
Estimated number of randomised participants: 90 Inclusion criteria: between 18 and 75 years of age; cirrhosis with suspected or documented sepsis with MAP < 65 mm Hg Exclusion criteria: already received colloid or 2 L of fluid within the first 12 h of presentation; already on vasopressors and/or inotropes; spontaneous bacterial peritonitis and serum albumin less then 1.5 g/dL; structural heart disease; on maintenance haemodialysis; other causes of hypotension; pregnant or lactating women; in need of emergent surgical interventions; chronic obstructive lung disease and congestive heart failure; previous adverse reaction to human albumin solution Participant condition: cirrhosis with sepsis Country: India Setting: medical centre |
| Interventions |
Colloids group Details: 20% albumin Crystalloids group Details: Plasmalyte |
| Outcomes |
Outcomes measured/reported: reversal of hypotension; mortality (at 7 and 28 days); proportion of patients with new organ failures; duration of mechanical ventilation; requirement of RRT; length of ICU stay Outcomes relevant to the review: mortality; requirement of RRT |
| Starting date | March 31, 2016 |
| Contact information | Dr Abhinav Verma; email: abhinav.3183@gmail.com |
| Notes | Funding/declarations of interest: sponsored by Institute of Liver and Biliary Sciences, India |
NCT02782819.
| Trial name or title | A comparison of crystalloid alone versus crystalloid plus colloid in shock resuscitation |
| Methods | RCT Parallel design Single centre |
| Participants |
Estimated number of randomised participants: 320 Inclusion criteria: ≥ 18 years of age; new onset of shock within 24 h; MAP < 65 mmHg or SBP < 60% of baseline BP; evidence of poor tissue perfusion including: urine output < 0.5 mL/kg/h, lactate > 2 mmol/L, alteration of consciousness without other explanation; evidence of fluid inadequacy (CVP < 12 mmHg, PCWP < 18 mmHg) or evidence of fluid responsive (IVC diameter variation > 15%, pulse pressure variation > 15%, positive fluid challenge test) Exclusion criteria: prolonged shock > 24 h; received colloid solution > 1000 mL in previous 72 h; do‐not‐resuscitate order; contraindication for fluid therapy including: suspected cardiogenic shock, evidence of pulmonary oedema, history of anaphylaxis after fluid therapy Participant condition: shock Country: Thailand Setting: hospital |
| Interventions |
Colloids group Details: colloid solution resuscitation Crystalloids group Details: isotonic crystalloid solution resuscitation |
| Outcomes |
Outcomes measured/reported: proportion of patients who had shock reversal; mortality (at 28 and 90 days); total fluid resuscitation within 24 h; need of RRT Outcomes relevant to the review: mortality; need of RRT |
| Starting date | September 2014 |
| Contact information | Surat Tongyoo, MD; email: surat_Ty@yahoo.co.uk; Prapan Laophannarai, MD; email: praphan113@hotmail.com |
| Notes | Funding/declarations of interest: sponsored by Mahidol University |
ARDS: Acute Respiratory Distress Syndrome CVP: central venous pressure HES: hydroxyethyl starch ICU: intensive care unit IVC: inferior vena cava MAP: mean arterial blood pressure PCWP: pulmonary capillary wedge pressure RCT: randomised control trial RRT: renal replacement therapy SBP: systolic blood pressure
Differences between protocol and review
We have made the following changes to the review since its last publication (Perel 2013).
We added six new review authors (Sharon Lewis, Michael Pritchard, Andrew Butler, David Evans, Andrew Smith, Phil Alderson) and removed two review authors from the author list (Pablo Perel and Katharine Ker).
Background: we rewrote the background section using current Cochrane headings. We used more recent references to substantiate statements.
Methods: we rewrote the methods section using current Cochrane headings, and following the Methodological Expectations of Cochrane Intervention Reviews (MECIR) standards (Higgins 2016). We edited the criteria for considering studies in the review in order to improve clarity.
Types of studies: we excluded study reports that had been retracted after publication, following current guidance from Cochrane.
Types of participants: we excluded people who were scheduled for elective surgery because, although they may have required fluid resuscitation as part of standard perioperative clinical management, we believed that these people were not critically ill at the point of randomisation.
Types of outcome measures: we added additional outcomes to the review (mortality within 90 days, mortality within 30 days, transfusion of blood products, renal replacement therapy, and adverse events, specifically, allergic reactions, itching, or rashes) in order to give consideration to other potential benefits of colloid or crystalloid fluid resuscitation.
Data collection and analysis: we specified subgroup analyses (tonicity of crystalloid solution ‐ this was considered in analysis in the last review publication but was not reported as subgroup analysis), and sensitivity analyses (we added consideration of additional use of colloids in the crystalloid group, analysis using the alternative effect estimate, and decisions made for individual studies in which we noted serious discrepancies).
Results: we wrote these sections using current Cochrane headings, and following MECIR standards.
Excluded studies: because of changes made to the criteria for considering studies in the review, we excluded some studies that were included in the previous version of the review.
Risk of bias in included studies: we re‐assessed risk of bias for studies that were in the previous version of the review, following MECIR standards.
We added a 'Summary of findings' table for each comparison (organised by type of colloid).
Contributions of authors
July 2007: PP and IR examined trials for inclusion or exclusion, reaching agreement by discussion. PP and IR extracted data from the new studies. PP, IR and KK amended the text of the review.
April 2009: IR and MP examined trials for inclusion or exclusion, reaching agreement by discussion. IR and MP extracted data from the new study. MP amended the text of the review. PP edited the final version.
February 2011: the Cochrane Injuries Group amended the text (Emma Sydenham, Managing Editor). Both authors agreed with the changes to the manuscript.
November 2012: PP and IR examined trials for inclusion or exclusion, reaching agreement by discussion. PP and KK extracted data from the new studies. PP amended the text of the review. All the review authors agreed with the changes in the manuscript.
April 2018: SL, MP, DE, AB examined trials for inclusion or exclusion, reaching agreement by discussion with AS and PA. SL, MP, DE and AB extracted data from all studies. SL and MP conducted the analysis and wrote the review. All review authors (SL, MP, AB, DE, PA, AS, IR) agreed with changes in the manuscript.
Sources of support
Internal sources
Institute of Child Health, University of London, UK.
UK Cochrane Centre, NHS R&D Programme, UK.
External sources
NHS R&D Programme: Mother and Child Health, UK.
-
National Institute for Health Research (NIHR) Cochrane Review Incentive Scheme, Department of Health, UK.
The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Declarations of interest
Sharon R Lewis: none known Michael W Pritchard: none known Andrew R Butler: none known Phil Alderson: none known Andrew F Smith: none known Ian Roberts: none known
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Alpar 2004 {published data only}
- Alpar EK, Killampalli VV. Effects of hypertonic dextran in hypovolaemic shock: a prospective clinical trial. Injury 2004;35(5):500‐6. [PUBMED: 15081328] [DOI] [PubMed] [Google Scholar]
Annane 2013 {published data only}
- Annane D, Siami S, Jaber S, Martin C, Elatrous S, Declere AD, et al. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA 2013;310(17):1809‐17. [PUBMED: 24108515] [DOI] [PubMed] [Google Scholar]
- Heming N, Elatrous S, Jaber S, Dumenil AS, Cousson J, Forceville X, et al. Haemodynamic response to crystalloids or colloids in shock: an exploratory subgroup analysis of a randomised controlled trial. BMJ Open 2017;7(10):e016736. [PUBMED: 28988172] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heming N, Elatrous S, Jaber S, Dumenil AS, Cousson J, Forceville X, et al. Hemodynamic effects of crystalloids vs colloids: a subgroup analysis of the CRISTAL trial. Anaesthesiology Intensive Therapy 2014;2:115‐6. [PUBMED: 28988172]28988172 [Google Scholar]
Baker 2009 {published data only}
- Baker AJ, Rhind SG, Morrison LJ, Black S, Crnko NT, Shek PN, et al. Resuscitation with hypertonic saline‐dextran reduces serum biomarker levels and correlates with outcome in severe traumatic brain injury patients. Journal of Neurotrauma 2009;26(8):1227‐40. [PUBMED: 19637968] [DOI] [PubMed] [Google Scholar]
Bechir 2013 {published data only}
- Bechir M, Puhan MA, Fasshauer M, Schuepbach RA, Stocker R, Neff TA. Early fluid resuscitation with hydroxyethyl starch 130/0.4 (6%) in severe burn injury: a randomized, controlled, double‐blind clinical trial. Critical Care 2013;17(6):R299. [PUBMED: 24365167] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bentsen 2006 {published data only}
- Bentsen G, Breivik H, Lundar T, Stubhaug A. Hypertonic saline (7.2%) in 6% hydroxyethyl starch reduces intracranial pressure and improves hemodynamics in a placebo‐controlled study involving stable patients with subarachnoid hemorrhage. Critical Care Medicine 2006;34(12):2912‐7. [17075367] [DOI] [PubMed] [Google Scholar]
Brunkhorst 2008 {published data only}
- Brunkhorst FM, Engel C, Bloos F, Meier‐Hellmann A, Ragaller M, Weiler N, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. New England Journal of Medicine 2008;358(2):125‐39. [PUBMED: 351096686] [DOI] [PubMed] [Google Scholar]
Bulger 2008 {published data only}
- Bulger EM, Cuschieri J, Warner K, Maier RV. Hypertonic resuscitation modulates the inflammatory response in patients with traumatic hemorrhagic shock. Annals of Surgery 2007;245(4):635‐41. [PUBMED: 17414614] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulger EM, Jurkovich GJ, Nathens AB, Copass MK, Hanson S, Cooper C, et al. Hypertonic resuscitation of hypovolemic shock after blunt trauma: a randomized controlled trial. Archives of Surgery 2008;143(2):139‐48. [18283138] [DOI] [PubMed] [Google Scholar]
Bulger 2010 {published data only}
- Bulger EM, May S, Brasel KJ, Schreiber M, Kerby JD, Tisherman SA, et al. Out‐of‐hospital hypertonic resuscitation following severe traumatic brain injury: a randomized controlled trial. JAMA 2010;304(13):1455‐64. [PUBMED: 20924011] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bulger 2011 {published data only}
- Bulger EM, May S, Kerby JD, Emerson S, Stiell IG, Schreiber MA, et al. Out‐of‐hospital hypertonic resuscitation after traumatic hypovolemic shock: a randomized, placebo controlled trial. Annals of Surgery 2011;253(3):431‐41. [PUBMED: 21178763] [DOI] [PMC free article] [PubMed] [Google Scholar]
Caironi 2014 {published data only}
- Caironi P, Masson S, Tommaso M, Bottazzi B, Roberto L, Michela M, et al. Pentraxin 3 in patients with severe sepsis or shock: the ALBIOS trial. European Journal of Clinical Investigation 2017;47(1):73‐83. [PUBMED: 27864924] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, et al. Albumin replacement in patients with severe sepsis or septic shock. New England Journal of Medicine 2014;370(15):1412‐21. [PUBMED: 24635772] [DOI] [PubMed] [Google Scholar]
Chavez‐Negrete 1991 {published data only}
- Chavez‐Negrete A, Majluf Cruz S, Frati Munari A, Perches A, Arguero R. Treatment of hemorrhagic shock with intraosseous or intravenous infusion of hypertonic saline dextran solution. European Surgical Research 1991;23(2):123‐9. [PUBMED: 1718756] [DOI] [PubMed] [Google Scholar]
Cifra 2003 {published data only}
- Cifra HL, Velasco JN. A comparative study of the efficacy of 6% Haes‐Steril and Ringer's lactate in the management of dengue shock syndrome 555. Critical Care and Shock 2003;2:95‐100. [Google Scholar]
Cooper 2006 {published data only}
- Cooper AB, Cohn SM, Zhang HS, Hanna K, Stewart TE, Slutsky AS. Five percent albumin for adult burn shock resuscitation: lack of effect on daily multiple organ dysfunction score. Transfusion 2006;46(1):80‐9. [PUBMED: 16398734] [DOI] [PubMed] [Google Scholar]
Du 2011 {published data only}
- Du XJ, Hu WM, Xia Q, Huang ZW, Chen GY, Jin XD, et al. Hydroxyethyl starch resuscitation reduces the risk of intra‐abdominal hypertension in severe acute pancreatitis. Pancreas 2011;40(8):1220‐5. [PUBMED: 21775917] [DOI] [PubMed] [Google Scholar]
Dubin 2010 {published data only}
- Dubin A, Pozo MO, Casabella CA, Murias G, Palizas F Jr, Moseinco MC, et al. Comparison of 6% hydroxyethyl starch 130/0.4 and saline solution for resuscitation of the microcirculation during the early goal‐directed therapy of septic patients. Journal of Critical Care 2010;25(4):659.e1‐8. [PUBMED: 20813485] [DOI] [PubMed] [Google Scholar]
Dung 1999 {published data only}
- Dung NM, Day NP, Tam DT, Loan HT, Chau HT, Minh LN, et al. Fluid replacement in dengue shock syndrome: a randomized, double‐blind comparison of four intravenous‐fluid regimens. Clinical Infectious Diseases 1999;29(4):787‐94. [PUBMED: 10589889] [DOI] [PubMed] [Google Scholar]
Ernest 1999 {published data only}
- Ernest D, Belzberg AS, Dodek PM. Distribution of normal saline and 5% albumin infusions in septic patients. Critical Care Medicine 1999;27(1):46‐50. [PUBMED: 9934892] [DOI] [PubMed] [Google Scholar]
Evans 1996 {published data only}
- Evans PA, Garnett M, Boffard K, Kirkman E, Jacobson BF. Evaluation of the effect of colloid (Haemaccel) on the bleeding time in the trauma patient. Journal of the Royal Society of Medicine 1996;89(2):101P. [PUBMED: 8683491] [DOI] [PMC free article] [PubMed] [Google Scholar]
Finfer 2004 {published data only}
- Bellomo R, Morimatsu H, Presneill J, French C, Cole L, Story D, et al. Effects of saline or albumin resuscitation on standard coagulation tests. Critical Care and Resuscitation 2009;11(4):250‐6. [PUBMED: 20001872] [PubMed] [Google Scholar]
- Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. New England Journal of Medicine 2004;350(22):2247‐56. [15163774] [DOI] [PubMed] [Google Scholar]
- Finfer S, Bellomo R, McEvoy S, Lo SK, Myburgh J, Neal B, et al. Effect of baseline serum albumin concentration on outcome of resuscitation with albumin or saline in patients in intensive care units: analysis of data from the saline versus albumin fluid evaluation (SAFE) study. BMJ 2006;7577:1044. [PUBMED: 17040925] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finfer S, Myburgh J, Norton R, Cooper DJ, MacMahon S, Peto R, et al. Impact of albumin compared to saline on organ function and mortality of patients with severe sepsis. Intensive Care Medicine 2011;37(1):86‐96. [PUBMED: 20924555] [DOI] [PubMed] [Google Scholar]
- Myburgh J, Cooper DJ, Finfer S, Bellomo R, Norton R, Bishop N, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. New England Journal of Medicine 2007;357(9):874‐84. [PUBMED: 17761591] [DOI] [PubMed] [Google Scholar]
- Myburgh J, Neal B, Norton R, McEvoy S, Hayek M, Sandercock P, et al. Effect of baseline serum albumin concentration on outcome of resuscitation with albumin or saline in patients in intensive care units: analysis of data from the saline versus albumin fluid evaluation (SAFE) study. BMJ 2006;333(7577):1044‐6. [PUBMED: 17040925] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodwin 1983 {published data only}
- Goodwin CW, Dorethy J, Lam V, Pruitt BA Jr. Randomized trial of efficacy of crystalloid and colloid resuscitation on hemodynamic response and lung water following thermal injury. Annals of Surgery 1983;197(5):520‐31. [PUBMED: 6342554] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grba‐Bujevic 2012 {published data only}
- Grba‐Bujevic M, Bosan‐Kilibarda I, Strikic N. The use of hypertonic‐hyperoncotic solution for hypovolemic shock in trauma patients in prehospital setting. Neurologia Croatica 2012;61(Suppl 2):21‐4. [Google Scholar]
Guidet 2012 {published data only}
- Guidet B, Martinet O, Boulain T, Philippart F, Poussel JF, Maizel J, et al. Assessment of hemodynamic efficacy and safety of 6% hydroxyethyl starch 130/0.4 vs. 0.9% NaCl fluid replacement in patients with severe sepsis: the CRYSTMAS study. Critical Care 2012;16(3):R94. [PUBMED: 22624531] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hall 1978 {published data only}
- Hall K, Sorenson B. The treatment of burn shock: results of a 5‐year randomized, controlled clinical trial of dextran 70 v Ringer lactate solution. Burns 1978;5(1):107‐12. [Google Scholar]
- Hall KV, Sorensen B. The treatment of burn shock. A comparative controlled trial of treatment by colloid infusion (Dextran saline), and by exclusively electrolyte infusion (Ringer lactate). Scandinavian Journal of Plastic and Reconstructive Surgery 173;7(1):67‐73. [PUBMED: 4752572] [DOI] [PubMed] [Google Scholar]
Heradstveit 2010 {published data only}
- Heradstveit BE, Guttormsen AB, Langorgen J, Hammersborg S‐M, Wentzel‐Larsen T, Fanebust R, et al. Capillary leakage in post‐cardiac arrest survivors during therapeutic hypothermia ‐ a prospective, randomised study. Scandinavian Journal of Trauma, Resuscitation & Emergency Medicine 2010;18:29. [PUBMED: 20500876] [DOI] [PMC free article] [PubMed] [Google Scholar]
James 2011 {published data only}
- James MF, Michell WL, Joubert IA, Nicol AJ, Navsaria PH, Gillespie RS. Resuscitation with hydroxyethyl starch improves renal function and lactate clearance in penetrating trauma in a randomized controlled study: the FIRST trial (Fluids in Resuscitation of Severe Trauma). British Journal of Anaesthesia 2011;107(5):693‐702. [PUBMED: 21857015] [DOI] [PubMed] [Google Scholar]
Jelenko 1979 {published data only}
- Jelenko C 3rd, Solenberger RI, Wheeler ML, Callaway BD. Shock and resuscitation. III. Accurate refractometric COP determinations in hypovolemia treated with HALFD. JACEP 1979;8(7):253‐6. [PUBMED: 449157] [DOI] [PubMed] [Google Scholar]
- Jelenko C 3rd, Wheeler ML, Callaway BD, Divilio LT, Bucklen KR, Holdredge TD. Shock and resuscitation. II: volume repletion with minimal edema using the "HALFD" (Hypertonic Albuminated Fluid Demand) regimen. JACEP 1978;7(9):326‐33. [PUBMED: 45702] [DOI] [PubMed] [Google Scholar]
- Jelenko C 3rd, Williams JB, Wheeler ML, Callaway BD, Fackler VK, Albers CA, et al. Studies in shock and resuscitation, I: use of a hypertonic, albumin‐containing, fluid demand regimen (HALFD) in resuscitation. Critical Care Medicine 1979;7(4):157‐67. [PUBMED: 446052] [PubMed] [Google Scholar]
Jie 2015 {published data only}
- Jie L, Tong L, Fang L, Youzhong A. The influence of hydroxyethyl starch on exogenous coagulation and active protein C in patients with septic shock. Chinese Critical Care Medicine 2015;27(1):28‐32. [PUBMED: 25591433] [DOI] [PubMed] [Google Scholar]
Kumar 2017 {published data only}
- Kumar S. Audit of preoperative fluid resuscitation in perforation peritonitis patients using physiological and operative severity score for enumeration of mortality and morbidity. Journal of Emergencies, Trauma and Shock 2017;10(1):7‐12. [PUBMED: 28243006] [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2008 {published data only}
- Li F, Sun H, Han XD. The effect of different fluids on early fluid resuscitation in septic shock. Chinese Critical Care Medicine 2008;20(8):472‐5. [PUBMED: 18687174] [PubMed] [Google Scholar]
Lowe 1977 {published data only}
- Lowe RJ, Moss GS, Jilek J, Levine HD. Crystalloid versus colloid in the etiology of pulmonary failure after trauma ‐ a randomized trial in man. Critical Care Medicine 1979;7(3):107‐12. [PUBMED: 436425] [DOI] [PubMed] [Google Scholar]
- Lowe RJ, Moss GS, Jilek J, Levine HD. Crystalloid vs colloid in the etiology of pulmonary failure after trauma: a randomized trial in man. Surgery 1977;81(6):676‐83. [PUBMED: 860200] [PubMed] [Google Scholar]
- Moss GS, Lowe RJ, Jilek J, Levine HD. Colloid or crystalloid in the resuscitation of hemorrhagic shock: a controlled clinical trial. Surgery 1981;89(4):434‐8. [PUBMED: 7010650] [PubMed] [Google Scholar]
Lu 2012 {published data only}
- Lu J, Zhao HY, Liu F, An YZ. The influence of lactate Ringer solution versus hydroxyethyl starch on coagulation and fibrinolytic system in patients with septic shock. Chinese Critical Care Medicine 2012;24(1):38‐41. [PUBMED: 22248750] [PubMed] [Google Scholar]
Lucas 1978 {published data only}
- Clift DR, Lucas CE, Ledgerwood AM, Sardesai V, Kithier K, Grabow D. The effect of albumin resuscitation for shock on the immune response to tetanus toxoid. Journal of Surgical Research 1982;32(5):449‐52. [PUBMED: 7087432] [DOI] [PubMed] [Google Scholar]
- Johnson SD, Lucas CE, Gerrick SJ, Ledgerwood AM, Higgins RF. Altered coagulation after albumin supplements for treatment of oligemic shock. Archives of Surgery 1979;114(4):379‐83. [PUBMED: 435053] [DOI] [PubMed] [Google Scholar]
- Lucas CE, Bouwman DL, Ledgerwood AM, Higgins R. Differential serum protein changes following supplemental albumin resuscitation for hypovolemic shock. Journal of Trauma‐Injury Infection & Critical Care 1980;20(1):47‐51. [PUBMED: 7351677] [PubMed] [Google Scholar]
- Lucas CE, Weaver D, Higgins RF, Ledgerwood AM, Johnson SD, Bouwman DL. Effects of albumin versus non‐albumin resuscitation on plasma volume and renal excretory function. Journal of Trauma‐Injury Infection & Critical Care 1978;18(8):564‐70. [PUBMED: 682218] [DOI] [PubMed] [Google Scholar]
- Weaver DW, Ledgerwood AM, Lucas CE, Higgins R, Bouwman DL, Johnson SD. Pulmonary effects of albumin resuscitation for severe hypovolemic shock. Archives of Surgery 1978;113(4):387‐92. [PUBMED: 637709] [DOI] [PubMed] [Google Scholar]
Mahrous 2013 {published data only}
- Mahrous A, Elsammk M, Megahed M, Zytoun T. Renal effect of colloid versus crystalloid in septic neutropenic patients. Critical Care Medicine 2013;1:A250. [PUBMED: 71534173] [Google Scholar]
Maitland 2005 {published data only}
- Maitland K, Pamba A, English M, Peshu N, Marsh K, Newton C, et al. Randomized trial of volume expansion with albumin or saline in children with severe malaria: preliminary evidence of albumin benefit. Clinical Infectious Diseases 2005;40(4):538‐45. [PUBMED: 15712076 ] [DOI] [PubMed] [Google Scholar]
Maitland 2011 {published data only}
- Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot‐Olupot P, Akech SO, et al. Mortality after fluid bolus in African children with severe infection. New England Journal of Medicine 2011;364(26):2483‐95. [PUBMED: 21615299] [DOI] [PubMed] [Google Scholar]
Martin 2005 {published data only}
- Martin GS, Moss M, Wheeler AP, Mealer M, Morris JA, Bernard GR. A randomized, controlled trial of furosemide with or without albumin in hypoproteinemic patients with acute lung injury. Critical Care Medicine 2005;33(8):1681‐7. [PUBMED: 16096441] [DOI] [PubMed] [Google Scholar]
Masoumi 2016 {published data only}
- Masoumi K, Forouzan A, Darian AA, Rafaty Navaii A. Comparison of the effectiveness of hydroxyethyl starch (Voluven) solution with normal saline in hemorrhagic shock treatment in trauma. Journal of Clinical Medicine Research 2016;8(11):815‐8. [PUBMED: 27738483] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mattox 1991 {published data only}
- Mattox KL, Maningas PA, Moore EE, Mateer JR, Marx JA, Aprahamian C, et al. Prehospital hypertonic saline/dextran infusion for post‐traumatic hypotension. The U.S.A. Multicenter Trial. Annals of Surgery 1991;213(5):482‐91. [PUBMED: 1708984] [DOI] [PMC free article] [PubMed] [Google Scholar]
McIntyre 2008 {published data only}
- McIntyre LA, Fergusson D, Cook DJ, Rankin N, Dhingra V, Granton J, et al. Fluid resuscitation in the management of early septic shock (FINESS): a randomized controlled feasibility trial. Canadian Journal of Anaesthesia 2008;55(12):819‐26. [PUBMED: 19050085] [DOI] [PubMed] [Google Scholar]
McIntyre 2012 {published data only}
- McIntyre LA, Fergusson DA, Cook DJ, Rowe BH, Bagshaw SM, Easton D, et al. Fluid resuscitation with 5% albumin versus normal saline in early septic shock: a pilot randomized, controlled trial. Journal of Critical Care 2012;27(3):317.e1‐6. [PUBMED: 22176806] [DOI] [PubMed] [Google Scholar]
Metildi 1984 {published data only}
- Metildi LA, Shackford SR, Virgilio RW, Peters RM. Crystalloid versus colloid in fluid resuscitation of patients with severe pulmonary insufficiency. Surgery, Gynecology & Obstetrics 1984;158(3):207‐12. [PUBMED: 6701732] [PubMed] [Google Scholar]
Modig 1986 {published data only}
- Modig J. Advantages of dextran 70 over Ringer acetate solution in shock treatment and in prevention of adult respiratory distress syndrome. A randomized study in man after traumatic‐haemorrhagic shock. Resuscitation 1983;10(4):219‐26. [PUBMED: 6196822] [DOI] [PubMed] [Google Scholar]
- Modig J. Effectiveness of dextran 70 versus Ringer's acetate in traumatic shock and adult respiratory distress syndrome. Critical Care Medicine 1986;14(5):454‐7. [PUBMED: 16081356] [DOI] [PubMed] [Google Scholar]
Morrison 2011 {published data only}
- Morrison LJ, Baker AJ, Rhind SG, Kiss A, MacDonald RD, Schwartz B, et al. The Toronto prehospital hypertonic resuscitation‐head injury and multiorgan dysfunction trial: feasibility study of a randomized controlled trial. Journal of Critical Care 2011;26(4):363‐72. [PUBMED: 51162409] [DOI] [PubMed] [Google Scholar]
- Morrison LJ, Rizoli SB, Schwartz B, Rhind SG, Simitcui M, Perreira T, et al. The Toronto prehospital hypertonic resuscitation‐head injury and multiorgan dysfunction trial (TOPHR‐HIT) ‐ methods and data collection tools. Trials 2009;10:105. [DOI: 10.1186/1745-6215-10-105] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhind SG, Crnko NT, Baker AJ, Morrison LJ, Shek PN, Scarpelini S, et al. Prehospital resuscitation with hypertonic saline‐dextran modulates inflammatory, coagulation and endothelial activation marker profiles in severe traumatic brain injured patients. Journal of Neuroinflammation 2010;7:5. [PUBMED: 20082712] [DOI] [PMC free article] [PubMed] [Google Scholar]
Myburgh 2012 {published data only}
- Myburgh J, Bellomo R, Cass A, French J, Finfer S, Gattas D, et al. The crystalloid versus hydroxyethyl starch trial: protocol for a multi‐centre randomised controlled trial of fluid resuscitation with 6% hydroxyethyl starch (130/0.4) compared to 0.9% sodium chloride (saline) in intensive care patients on mortality. Intensive Care Medicine 2011;37(5):816‐23. [PUBMED: 21308360] [DOI] [PubMed] [Google Scholar]
- Myburgh J, Li Q, Heritier S, Dan A, Glass P. Statistical analysis plan for the crystalloid versus hydroxyethyl starch trial (CHEST). Critical Care & Resuscitation 2012;14(1):44‐52. Erratum appears in Critical Care & Resuscitation 2012; 14(2):164. [PUBMED: 22404061] [PubMed] [Google Scholar]
- Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. New England Journal of Medicine 2012;367(20):1901‐11. [PUBMED: 23075127] [DOI] [PubMed] [Google Scholar]
- NCT00935168. A multicentre randomized controlled trial of fluid resuscitation with starch (6% hydroxyethyl starch 130/0.4) compared to saline (0.9% sodium chloride) in intensive care patients on mortality. clinicaltrials.gov/ct2/show/NCT00935168 (first received 1 July 2009). [PUBMED: 23604905]23604905
- Patel A, Pieper K, Myburgh JA, Perkovic V, Finfer S, Yang Q, et al. Reanalysis of the crystalloid versus hydroxyethyl starch trial (CHEST). New England Journal of Medicine 2017;377(3):298‐300. [PUBMED: 28723325] [DOI] [PubMed] [Google Scholar]
- Taylor C, Thompson K, Finfer S, Higgins A, Jan S, Li Q, et al. Hydroxyethyl starch versus saline for resuscitation of patients in intensive care: long‐term outcomes and cost‐effectiveness analysis of a cohort from CHEST. Lancet Respiratory Medicine 2016;4(10):818‐25. [PUBMED: 27324967] [DOI] [PubMed] [Google Scholar]
Nagy 1993 {published data only}
- Nagy KK, Davis J, Duda J, Fildes J, Roberts R, Barrett J. A comparison of pentastarch and lactated Ringer's solution in the resuscitation of patients with hemorrhagic shock. Circulatory Shock 1993;40(4):289‐94. [PUBMED: 7690689] [PubMed] [Google Scholar]
Ngo 2001 {published data only}
- Ngo NT, Cao XT, Kneen R, Wills B, Nguyen VM, Nguyen TQ, et al. Acute management of dengue shock syndrome: a randomized double‐blind comparison of 4 intravenous fluid regimens in the first hour. Clinical Infectious Diseases 2001;32(2):204‐13. [PUBMED: 11170909] [DOI] [PubMed] [Google Scholar]
O'Mara 2005 {published data only}
- O'Mara MS, Slater H, Goldfarb IW, Caushaj PF. A prospective, randomized evaluation of intra‐abdominal pressures with crystalloid and colloid resuscitation in burn patients. Journal of Trauma 2005;58(5):1011‐8. [PUBMED: 15920417] [DOI] [PubMed] [Google Scholar]
Oliveira 2002 {published data only}
- Oliveira RP, Weingartner R, Ribas EO, Moraes RS, Friedman G. Acute haemodynamic effects of a hypertonic saline/dextran solution in stable patients with severe sepsis. Intensive Care Medicine 2002;28(11):1574‐81. [PUBMED: 12415443] [DOI] [PubMed] [Google Scholar]
Park 2015 {published data only}
- Park C, Osawa E, Almeida J, Nakamura R, Duayer I, Fukushima J, et al. Lactated Ringer versus albumin in early sepsis therapy (RASP) study: preliminary data of a randomized controlled trial. Critical Care 2015;1:S125. [PUBMED: 71938758] [Google Scholar]
Perner 2012 {published data only}
- Anthon CT, Muller RB, Haase N, Hjortrup PB, Moller K, Lange T, et al. Effects of hydroxyethyl starch 130/0.42 vs. Ringer's acetate on cytokine levels in severe sepsis. Acta Anaesthesiologica Scandinavica 2017;61(8):904‐13. [PUBMED: 28653377] [DOI] [PubMed] [Google Scholar]
- Haase N, Wetterslev J, Winkel P, Perner A. Bleeding and risk of death with hydroxyethyl starch in severe sepsis: post hoc analyses of a randomized clinical trial. Intensive Care Medicine 2013;39(12):2126‐34. [PUBMED: 24081433] [DOI] [PubMed] [Google Scholar]
- Haase N, Wetterslev J, Winkel P, Perner A. Hydroxyethyl starch 130/0.42 versus Ringer's acetate in severe sepsis: post‐hoc analyses of coagulation, bleeding and transfusion in a randomised trial. Intensive Care Medicine 2013;39(2):S213. [DOI: ] [DOI] [PubMed] [Google Scholar]
- Haase NR. Hydroxyethyl starch in sepsis. Danish Medical Journal 2014;61(1):B4764. [PUBMED: 24393593] [PubMed] [Google Scholar]
- Hjortrup PB, Haase N, Wetterslev J, Perner A. Associations of hospital and patient characteristics with fluid resuscitation volumes in patients with severe sepsis: post hoc analyses of data from a multicentre randomised clinical trial. PLOS One 2016;11(5):e0155767. [PUBMED: 27196104] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller RB, Haase N, Lange T, Wetterslev J, Perner A. Acute kidney injury with hydroxyethyl starch 130/0.42 in severe sepsis. Acta Anaesthesiologica Scandinavica 2015;59(3):329‐36. [PUBMED: 25524831] [DOI] [PubMed] [Google Scholar]
- Muller RB, Ostrowski SR, Haase N, Wetterslev J, Perner A, Johansson PI. Markers of endothelial damage and coagulation impairment in patients with severe sepsis resuscitated with hydroxyethyl starch 130/0.42 vs Ringer acetate. Journal of Critical Care 2016;32:16‐20. [PUBMED: 26810483] [DOI] [PubMed] [Google Scholar]
- Muller RG, Haase N, Wetterslev J, Perner A. Effects of hydroxyethyl starch in subgroups of patients with severe sepsis: exploratory post‐hoc analyses of a randomised trial. Intensive Care Medicine 2013;39(11):1963‐71. [PUBMED: 24037226] [DOI] [PubMed] [Google Scholar]
- Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, et al. Hydroxyethyl starch 130/0.42 versus Ringer's acetate in severe sepsis. New England Journal of Medicine 2012;367(2):124‐34. [PUBMED: 365216118] [DOI] [PubMed] [Google Scholar]
- Perner A, Haase N, Wetterslev J, Aneman A, Tenhunen J, Guttormsen AB, et al. Comparing the effect of hydroxyethyl starch 130/0.4 with balanced crystalloid solution on mortality and kidney failure in patients with severe sepsis (6S‐‐Scandinavian Starch for Severe Sepsis/Septic Shock trial): study protocol, design and rationale for a double‐blinded, randomised clinical trial. Trials 2011;12:24. [PUBMED: 21269526] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perner A, Haase N, Winkel P, Guttormsen AB, Tenhunen J, Klemenzson G, et al. Long‐term outcomes in patients with severe sepsis randomised to resuscitation with hydroxyethyl starch 130/0.42 or Ringer's acetate. Intensive Care Medicine 2014;40(7):927‐34. [PUBMED: 24807084] [DOI] [PubMed] [Google Scholar]
Philips 2015 {published data only}
- Philips CA, Choudhury AK, Sahney A, Maiwall R, Mitra LG, Sarin SK. Comparison and outcomes of 5% albumin vs 0.9% normal saline fluid resuscitation in cirrhotics presenting with sepsis induced hypotension‐a randomized controlled trial‐fluid resuscitation in septic shock in cirrhosis (FRISC Protocol). Hepatology 2015;62:261a. [Issn Print: 0270‐9139] [Google Scholar]
Pockaj 1994 {published data only}
- Pockaj BA, Yang JC, Lotze MT, Lange JR, Spencer WF, Steinberg SM, et al. A prospective randomized trial evaluating colloid versus crystalloid resuscitation in the treatment of the vascular leak syndrome associated with interleukin‐2 therapy. Journal of Immunotherapy with Emphasis on Tumor Immunology 1994;15(1):22‐8. [PUBMED: 8110727] [DOI] [PubMed] [Google Scholar]
Quinlan 2004 {published data only}
- Quinlan GJ, Mumby S, Martin GS, Bernard GR, Gutteridge JM, Evans TW. Albumin influences total plasma antioxidant capacity favorably in patients with acute lung injury. Critical Care Medicine 2004;32(3):755‐9. [PUBMED: 15090958] [DOI] [PubMed] [Google Scholar]
Rackow 1983 {published data only}
- Haupt MT, Rackow EC. Colloid osmotic pressure and fluid resuscitation with hetastarch, albumin, and saline solutions. Critical Care Medicine 1982;10(3):159‐62. [PUBMED: 6174274] [DOI] [PubMed] [Google Scholar]
- Kaufman BS, Rackow EC, Falk JL. Fluid resuscitation in circulatory shock. Colloids versus crystalloids. Current Studies in Hematology & Blood Transfusion 1986;53:186‐98. [PUBMED: 3536330] [DOI] [PubMed] [Google Scholar]
- Rackow EC, Falk JL, Fein IA, Siegel JS, Packman MI, Haupt MT, et al. Fluid resuscitation in circulatory shock: a comparison of the cardiorespiratory effects of albumin, hetastarch, and saline solutions in patients with hypovolemic and septic shock. Critical Care Medicine 1983;11(11):839‐50. [PUBMED: 14245570] [PubMed] [Google Scholar]
Shah 1977 {published data only}
- Shah DM, Browner BD, Dutton RE, Newell JC, Powers JC Jr. Cardiac output and pulmonary wedge pressure. Use for evaluation of fluid replacement in trauma patients. Archives of Surgery 1977;112(10):1161‐8. [PUBMED: 907460] [DOI] [PubMed] [Google Scholar]
Upadhyay 2005 {published data only}
- Upadhyay M, Singhi S, Murlidharan J, Kaur N, Majumdar S. Randomized evaluation of fluid resuscitation with crystalloid (saline) and colloid (polymer from degraded gelatin in saline) in pediatric septic shock. Indian Pediatrics 2005;42(3):223‐31. [PUBMED: 40461538] [PubMed] [Google Scholar]
Van der Heijden 2009 {published data only}
- Smorenberg A, Groeneveld AB. Diuretic response to colloid and crystalloid fluid loading in critically ill patients. Journal of Nephrology 2015;28(1):89‐95. [PUBMED: 24828327] [DOI] [PubMed] [Google Scholar]
- Spoelstra‐de Man AM, Smorenberg A, Groeneveld AB. Different effects of fluid loading with saline, gelatine, hydroxyethyl starch or albumin solutions on acid‐base status in the critically ill. PLOS One 2017;12(4):e0174507. [PUBMED: 28380062] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trof RJ, Sukul SP, Twisk JW, Girbes AR, Groeneveld AB. Greater cardiac response of colloid than saline fluid loading in septic and non‐septic critically ill patients with clinical hypovolaemia. Intensive Care Medicine 2010;36(4):697‐701. [PUBMED: 20165941] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heijden M, Verheij J, Nieuw Amerongen GP, Groeneveld AB. Crystalloid or colloid fluid loading and pulmonary permeability, edema, and injury in septic and nonseptic critically ill patients with hypovolemia. Critical Care Medicine 2009;37(4):1275‐81. [PUBMED: 19242338] [DOI] [PubMed] [Google Scholar]
Vassar 1990 {published data only}
- Holcroft JW, Vassar MJ, Perry CA, Gannaway WL, Kramer GC. Use of a 7.5% NaCl/6% dextran 70 solution in the resuscitation of injured patients in the emergency room. Progress in Clinical and Biological Research 1989;299:331‐8. [PUBMED: 2471213] [PubMed] [Google Scholar]
- Vassar MJ, Perry CA, Holcroft JW. Analysis of potential risks associated with 7.5% sodium chloride resuscitation of traumatic shock. Archives of Surgery 1990;125(10):1309‐15. Erratum in Archives of Surgery 1991; 126(1):43. [PUBMED: 1699508] [DOI] [PubMed] [Google Scholar]
Vassar 1991 {published data only}
- Holcroft JW, Vassar MJ, Perry CA, Gannaway WL, Kramer GC. Perspectives on clinical trials for hypertonic saline/dextran solutions for the treatment of traumatic shock. Brazilian Journal of Medical & Biological Research 1989;22(2):291‐3. [PUBMED: 2477096] [PubMed] [Google Scholar]
- Holcroft JW, Vassar MJ, Turner JE, Derlet RW, Kramer GC. 3% NaCl and 7.5% NaCl/dextran 70 in the resuscitation of severely injured patients. Annals of Surgery 1987;206(3):279‐88. [PUBMED: 2443087] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vassar MJ, Perry CA, Gannaway WL, Holcroft JW. 7.5% sodium chloride/dextran for resuscitation of trauma patients undergoing helicopter transport. Archives of Surgery 1991;126(9):1065‐72. [PUBMED: 1718243] [DOI] [PubMed] [Google Scholar]
Vassar 1993a {published data only}
- Vassar MJ, Fischer RP, O'Brien PE, Bachulis BL, Chambers JA, Hoyt DB, et al. A multicenter trial for resuscitation of injured patients with 7.5% sodium chloride. The effect of added dextran 70. The Multicenter Group for the Study of Hypertonic Saline in Trauma Patients. Archives of Surgery 1993;128(9):1003‐11; discussion 1011‐3. [PUBMED: 7690225] [DOI] [PubMed] [Google Scholar]
Vassar 1993b {published data only}
- Vassar MJ, Perry CA, Holcroft JW. Prehospital resuscitation of hypotensive trauma patients with 7.5% NaCl versus 7.5% NaCl with added dextran: a controlled trial. Journal of Trauma 1993;34(5):622‐32; discussion 632‐3. [PUBMED: 7684457] [PubMed] [Google Scholar]
Vlachou 2010 {published data only}
- Vlachou E, Gosling P, Moiemen NS. Hydroxyethylstarch supplementation in burn resuscitation ‐ a prospective randomised controlled trial. Burns 2010;36(7):984‐91. [PUBMED: 20558004] [DOI] [PubMed] [Google Scholar]
Wills 2005 {published data only}
- Wills BA, Dung NM, Loan HT, Tam DT, Thuy TT, Minh LT, et al. Comparison of three fluid solutions for resuscitation in dengue shock syndrome. New England Journal of Medicine 2005;353(9):877‐89. [PUBMED: 16135832] [DOI] [PubMed] [Google Scholar]
Wu 2001 {published data only}
- Wu JJ, Huang MS, Tang GJ, Kao WF, Shih HC, Su CH, et al. Hemodynamic response of modified fluid gelatin compared with lactated Ringer's solution for volume expansion in emergency resuscitation of hypovolemic shock patients: preliminary report of a prospective, randomized trial. World Journal of Surgery 2001;25(5):598‐602. [PUBMED: 11369986] [DOI] [PubMed] [Google Scholar]
Younes 1992 {published data only}
- Younes RN, Aun F, Accioly CQ, Casale LP, Szajnbok I, Birolini D. Hypertonic solutions in the treatment of hypovolemic shock: a prospective, randomized study in patients admitted to the emergency room. Surgery 1992;111(4):380‐5. [PUBMED: 1373007] [PubMed] [Google Scholar]
Younes 1997 {published data only}
- Younes RN, Aun F, Ching C, Goldenberg D, Franco M, Miura F, Santos S, et al. Prognosis following the administration of hypertonic/hyperoncotic solutions in hypovolemic patients. Program and abstracts. International Conference on Hypertonic Resuscitation (6th) (SALT 6); 1994 Jun 2‐3; Teton Village (WY). 1994.
- Younes RN, Aun F, Ching CT, Goldenberg DC, Franco MH, Miura FK, et al. Prognostic factors to predict outcome following the administration of hypertonic/hyperoncotic solution in hypovolemic patients. Shock (Augusta, Ga.) 1997;7(2):79‐83. [PUBMED: 9035281] [DOI] [PubMed] [Google Scholar]
Younes 1998 {published data only}
- Younes RN, Yin KC, Amino CJ, Itinoshe M, Rocha e Silva M, Birolini D. Use of pentastarch solution in the treatment of patients with hemorrhagic hypovolemia: randomized phase II study in the emergency room. World Journal of Surgery 1998;22(1):2‐5. [PUBMED: 9465753] [DOI] [PubMed] [Google Scholar]
Zhao 2013 {published data only}
- Zhao G, Zhang J‐G, Wu H‐S, Tao J, Qin Q, Deng S‐C, et al. Effects of different resuscitation fluid on severe acute pancreatitis. World Journal of Gastroenterology 2013;19(13):2044‐52. [PUBMED: 23599623] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhu 2011 {published data only}
- Zhu GC, Quan ZY, Shao YS, Zhao JG, Zhang YT. The study of hypertonic saline and hydroxyethyl starch treating severe sepsis. Chinese Critical Care Medicine 2011;23(3):150‐3. [PUBMED: 361547296] [PubMed] [Google Scholar]
References to studies excluded from this review
Boutros 1979 {published data only}
- Boutros AR, Ruess R, Olson L, Hoyt JL, Baker WH. Comparison of hemodynamic, pulmonary, and renal effects of use of three types of fluids after major surgical procedures on the abdominal aorta. Critical Care Medicine 1979;7(1):9‐13. [PUBMED: 367709] [DOI] [PubMed] [Google Scholar]
Bowser‐Wallace 1986 {published data only}
- Bowser‐Wallace BH, Caldwell FT Jr. Fluid requirements of severely burned children up to 3 years old: hypertonic lactated saline vs. Ringer's lactate‐colloid. Burns 1986;12(8):549‐55. [PUBMED: 3454687] [DOI] [PubMed] [Google Scholar]
Dawidson 1991 {published data only}
- Dawidson IJ, Willms CD, Sandor ZF, Coorpender LL, Reisch JS, Fry WJ. Ringer's lactate with or without 3% dextran‐60 as volume expanders during abdominal aortic surgery. Critical Care Medicine 1991;19(1):36‐42. [PUBMED: 1702696] [DOI] [PubMed] [Google Scholar]
Dehne 2001 {published data only}
- Dehne MG, Mühling J, Sablotzki A, Dehne K, Sucke N, Hempelmann G. Hydroxyethyl starch (HES) does not directly affect renal function in patients with no prior renal impairment. Journal of Clinical Anesthesia 2001;13(2):103‐11. [PUBMED: 11331169] [DOI] [PubMed] [Google Scholar]
Eleftheriadis 1995 {published data only}
- Eleftheriadis S, Sedemund Adib B, Klotz KF, Hubner N, Kuppe H. Volume replacement after cardiac surgery: comparison of Ringer, HES 6% and gelatine 3.5%. Intensive Care Medicine 1995;21(Suppl 1):S216. [Google Scholar]
Evans 2003 {published data only}
- Evans PA, Heptinstall S, Crowhurst EC, Davies T, Glenn JR, Madira W, et al. Prospective double‐blind randomized study of the effects of four intravenous fluids on platelet function and hemostasis in elective hip surgery. Journal of Thrombosis and Haemostasis 2003;10(1):2140‐8. [PUBMED: 14521596] [DOI] [PubMed] [Google Scholar]
Fries 2004 {published data only}
- Fries D, Streif W, Margreiter J, Klingler A, Kuhbacher G, Schobersberger W, et al. The effects of perioperatively administered crystalloids and colloids on concentrations of molecular markers of activated coagulation and fibrinolysis. Blood Coagulation and Fibrinolysis 2004;15(3):213‐9. [PUBMED: 15060416] [DOI] [PubMed] [Google Scholar]
Gallagher 1985 {published data only}
- Gallagher JD, Moore RA, Kerns D, Jose AB, Botros SB, Flicker S, et al. Effects of colloid or crystalloid administration on pulmonary extravascular water in the postoperative period after coronary artery bypass grafting. Anesthesia and Analgesia 1985;64(8):753‐8. [PUBMED: 2409845] [PubMed] [Google Scholar]
Grundmann 1982 {published data only}
- Grundmann R, Heistermann S. Postoperative albumin infusion therapy based on colloid osmotic pressure. A prospectively randomized trial. Archives of Surgery 1985;120(8):911‐5. [PUBMED: 3893389] [DOI] [PubMed] [Google Scholar]
- Grundmann R, Meyer H. The significance of colloid osmotic pressure measurement after crystalloid and colloid infusions. Intensive Care Medicine 1982;8(4):179‐86. [PUBMED: 7119271] [DOI] [PubMed] [Google Scholar]
Guo 2003 {published data only}
- Guo XY, Xu ZH, Ren HZ, Luo AL, Huang YG, Ye TH. Effect of volume replacement with hydroxyethyl starch solution for blood loss on splanchnic oxygenation in patients undergoing cytoreductive surgery for ovarian carcinoma. Zhonghua Yi Xue Za Zhi 2003;83(2):114‐7. [PUBMED: 12812678] [PubMed] [Google Scholar]
Hartmann 1993 {published data only}
- Hartmann M, Jonsson K, Zederfeldt B. Effects of dextran and crystalloids on subcutaneous oxygen tension and collagen accumulation. A randomized study in surgical patients. European Surgical Research 1993;25(5):270‐7. [PUBMED: 7691604] [DOI] [PubMed] [Google Scholar]
Hondebrink 1997 {published data only}
- Hondebrink Y, Jeekel L, Nijhuis JO, Woittiez AJ. Restoration of colloid osmotic pressure in hypoalbuminaemic patients. Intensive Care Medicine 1997;23(Suppl 1):S184. [Google Scholar]
- Timmer B, Hondebrink J, Oude Nijhuis J, Woittiez AJ. Restoration of colloid osmotic pressure in hypoalbuminaemic patients. Netherlands Journal of Medicine 1998;52:A42. [Google Scholar]
Karanko 1987 {published data only}
- Karanko MS, Klossner JA, Laaksonen VO. Restoration of volume by crystalloid versus colloid after coronary artery bypass: hemodynamics, lung water, oxygenation, and outcome. Critical Care Medicine 1987;15(6):559‐66. [PUBMED: 2436856] [DOI] [PubMed] [Google Scholar]
Lee 2011 {published data only}
- Lee JS, Ahn SW, Song JW, Shim JK, Yoo KJ, Kwak YL. Effect of hydroxyethyl starch 130/0.4 on blood loss and coagulation in patients with recent exposure to dual antiplatelet therapy undergoing off‐pump coronary artery bypass graft surgery. Circulation Journal 2011;75(10):2397‐402. [PUBMED: 21817820] [DOI] [PubMed] [Google Scholar]
Ley 1990 {published data only}
- Ley SJ, Miller K, Skov P, Preisig P. Crystalloid versus colloid fluid therapy after cardiac surgery. Heart and Lung: Journal of Critical Care 1990;19(1):31‐40. [PUBMED: 20045823] [PubMed] [Google Scholar]
Mazher 1998 {published data only}
- Mazhar R, Samenesco A, Royston D, Rees A. Cardiopulmonary effects of 7.2% saline solution compared with gelatin infusion in the early postoperative period after coronary artery bypass grafting. Journal of Thoracic & Cardiovascular Surgery 1998;115(1):178‐89. [PUBMED: 9451062 ] [DOI] [PubMed] [Google Scholar]
McNulty 1993 {published data only}
- McNulty SE, Sharkey SJ, Asam B, Lee JH. Evaluation of STAT‐CRIT hematocrit determination in comparison to Coulter and centrifuge: the effects of isotonic hemodilution and albumin administration. Anesthesia and Analgesia 1993;76(4):830‐4. [PUBMED: 23107606] [DOI] [PubMed] [Google Scholar]
Moretti 2003 {published data only}
- Moretti EW, Robertson KM, El‐Moalem H, Gan TJ. Intraoperative colloid administration reduces postoperative nausea and vomiting and improves postoperative outcomes compared with crystalloid administration. Anesthesia and Analgesia 2003;96(2):611‐7. [PUBMED: 12538221] [DOI] [PubMed] [Google Scholar]
Nielsen 1985 {published data only}
- Nielsen OM, Engell HC. Extracellular fluid volume and distribution in relation to changes in plasma colloid osmotic pressure after major surgery. A randomized study. Acta Chirurgica Scandinavica 1985;151(3):221‐5. [PUBMED: 3892993] [PubMed] [Google Scholar]
Prien 1990 {published data only}
- Prien T, Backhaus N, Pelster F, Pircher W, Bunte H, Lawin P. Effect of intraoperative fluid administration and colloid osmotic pressure on the formation of intestinal edema during gastrointestinal surgery. Journal of Clinical Anesthesia 1990;2(5):317‐23. [PUBMED: 1702977 ] [DOI] [PubMed] [Google Scholar]
Rocha e Silva 1994 {published data only}
- Rocha e Silva M, Poli de Figueiredo LF. Hypertonic‐hyperoncotic saline solution for the treatment of post‐traumatic hypotension in the emergency room. The Brazilian multi‐center trial. Program and abstracts. International Conference on Hypertonic Resuscitation (6th) (SALT 6); 1994 Jun 2‐3; Teton Village (WY). 1994.
Shires 1983 {published data only}
- Shires GT 3rd, Peitzman AB, Albert SA, Illner H, Silane MF, Perry MO, et al. Response of extravascular lung water to intraoperative fluids. Annals of Surgery 1983;197(5):515‐9. [PUBMED: 6847271] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sirieix 1999 {published data only}
- Sirieix D, Hongnat JM, Delayance S, D'Attellis N, Vicaut E, Berrebi A, et al. Comparison of the acute hemodynamic effects of hypertonic or colloid infusions immediately after mitral valve repair. Critical Care Medicine 1999;27(10):2159‐65. [PUBMED: 10548199 ] [DOI] [PubMed] [Google Scholar]
Skillman 1975 {published data only}
- Skillman JJ, Restall DS, Salzman EW. Randomized trial of albumin vs. electrolyte solutions during abdominal aortic operations. Surgery 1975;78(3):291‐303. [PUBMED: 1154272 ] [PubMed] [Google Scholar]
Tollusfrud 1995 {published data only}
- Tollofsrud S, Svennevig JL, Breivik H, Kongsgaard U, Ozer M, Hysing E, et al. Fluid balance and pulmonary functions during and after coronary artery bypass surgery: Ringer's acetate compared with dextran, polygeline, or albumin. Acta Anaesthesiologica Scandinavica 1995;39(5):671‐7. [PUBMED: 7572019] [DOI] [PubMed] [Google Scholar]
Tollusfrud 1998 {published data only}
- Tollofsrud S, Noddeland H. Hypertonic saline and dextran after coronary artery surgery mobilises fluid excess and improves cardiorespiratory functions. Acta Anaesthesiologica Scandinavica 1998;42(2):154‐61. [PUBMED: 9509195] [DOI] [PubMed] [Google Scholar]
Verheij 2006 {published data only}
- Verheij J, Lingen A, Beishuizen A, Christiaans HM, Jong JR, Girbes AR, et al. Cardiac response is greater for colloid than saline fluid loading after cardiac or vascular surgery. Intensive Care Medicine 2006;32(7):1030‐8. [PUBMED: 16791665] [DOI] [PubMed] [Google Scholar]
Virgilio 1979 {published data only}
- Virgilio RW, Rice CL, Smith DE, James DR, Zarins CK, Hobelmann CF, et al. Crystalloid vs. colloid resuscitation: is one better? A randomized clinical study. Surgery 1979;85(2):129‐39. [PUBMED: 419454] [PubMed] [Google Scholar]
Wahba 1996 {published data only}
- Wahba A, Sendtner E, Strotzer M, Wild K, Birnbaum DE. Fluid therapy with Ringer's solution versus Haemaccel following coronary artery bypass surgery. Acta Anaesthesiologica Scandinavica 1996;40(10):1227‐33. [PUBMED: 8986187] [DOI] [PubMed] [Google Scholar]
Zetterstorm 1981a {published data only}
- Zetterstrom H, Hedstrand U. Albumin treatment following major surgery. I. Effects on plasma oncotic pressure, renal function and peripheral oedema. Acta Anaesthesioligica Scandinavica 1981;25(2):125‐32. [PUBMED: 7324819 ] [DOI] [PubMed] [Google Scholar]
Zetterstorm 1981b {published data only}
- Zetterstrom H. Albumin treatment following major surgery. II. Effects on postoperative lung function and circulatory adaptation. Acta Anaesthesiologica Scandinavica 1981;25(2):133‐41. [PUBMED: 7324820 ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Bulanov 2004 {published data only}
- Bulanov AI, Gorodetskii VM, Shulutko EM, Vasil'ev SA, Orel EB, Malofeev VN, et al. Effect of different colloid volume‐replacing solutions on a changed hemostasis system. Anesteziologiia i Reanimatologiia 2004;2:25‐30. [PUBMED: 15206272] [PubMed] [Google Scholar]
Charpentier 2011 {published data only}
- Charpentier J, Mira J‐P. Efficacy and tolerance of hyperoncotic albumin administration in septic shock patients: the EARSS study. Intensive Care Medicine 2011;37(Suppl 1):S115. [Google Scholar]
Halim 2016 {published data only}
- Abd El Halim MA, Elsaid Hafez MH, Moktar AM, Eladawy A, Elazizy HM. Impact of gelatins on perfusion of microcirculatory blood flow in patient with septic shock. In: 29th Annual Congress of the European Society of Intensive Care Medicine (ESICM), 2016 Oct 1‐5; Milan (Italy). Intensive Care Medicine Experimental 2016.
NCT00890383 {published data only}
- NCT00890383. Colloids in severe trauma [Colloids in severe trauma: a multi‐center pilot study of "crystalloid only" or "crystalloid + colloid" volume resuscitation in trauma patients (CIST)]. clinicaltrials.gov/ct2/show/record/NCT00890383 (first received 29 April 2009).
NCT01337934 {published data only}
- NCT01337934. Ringer versus albumin in septic patients: a randomized controlled clinical trial [Lactated Ringer versus albumin in early sepsis therapy (RASP)]. clinicaltrials.gov/ct2/show/NCT01337934 (first received 13 April 2011).
NCT02064075 {published data only}
- NCT02064075. The mortality and changes in quality of life of patients suffering from SAH with different hydration strategies [Phase 4 prospective, randomized, blinded study on the effect of different hydration strategies on mortality and changes in quality of life of patients suffering from subarachnoid haemorrhage]. clinicaltrials.gov/ct2/show/record/NCT02064075 (first received 17 February 2014).
Protsenko 2009 {published data only}
- Protsenko DN, Leiderman IN, Grigor'ev EV, Kokarev EA, Levit AL, Gel'fand BR. Evaluation of the effectiveness and safety of synthetic colloid solutions in the treatment of severe abdominal sepsis: a randomized comparative study. Anesteziologiia i Reanimatologiia 2009;5:9‐13. [PUBMED: 19938709] [PubMed] [Google Scholar]
References to ongoing studies
NCT01763853 {published data only}
- NCT01763853. Impact of fluid resuscitation therapy on pulmonary edema as measured by alveolar fluid clearance in patients with acute respiratory distress syndrome (ARDS). clinicaltrials.gov/ct2/show/record/NCT01763853 (first received 9 January 2013).
NCT02721238 {published data only}
- NCT02721238. Comparison of colloid (20% albumin) versus crystalloid (Plasmalyte) for fluid resuscitation in cirrhotics with sepsis induced hypotension. clinicaltrials.gov/ct2/show/record/NCT02721238 (first received 29 March 2016).
NCT02782819 {published data only}
- NCT02782819. A comparison of crystalloid alone versus crystalloid plus colloid in shock resuscitation [A randomized controlled trial of crystalloid alone versus crystalloid plus colloid in shock resuscitation]. clinicaltrials.gov/ct2/show/record/NCT02782819 (first received 16 May 2016).
Additional references
Bailey 2010
- Bailey AG, McNaull PP, Jooste E, Tuchman JB. Perioperative crystalloid and colloid fluid management in children: where are we and how did we get here?. Anesthesia and Analgesia 2010;110(2):375‐90. [PUBMED: 19955503] [DOI] [PubMed] [Google Scholar]
Bampoe 2017
- Bampoe S, Odor PM, Dushianthan A, Bennett‐Guerrero E, Cro S, Gan TJ, et al. Perioperative administration of buffered versus non‐buffered crystalloid intravenous fluid to improve outcomes following adult surgical procedures. Cochrane Database of Systematic Reviews 2017, Issue 9. [DOI: 10.1002/14651858.CD004089.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Coppola 2014
- Coppola S, Froio S, Chiumello D. Fluid resuscitation in trauma patients: what should we know?. Current Opinion in Critical Care 2014;20(4):444‐50. [PUBMED: 24927043] [DOI] [PubMed] [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation. Covidence. Melbourne (Australia): Veritas Health Innovation, (accessed 23 February 2018).
de Crescenzo 2017
- Crescenzo C, Gorouhi F, Salcedo ES, Galante JM. Prehospital hypertonic fluid resuscitation for trauma patients: a systematic review and meta‐analysis. The Journal of Trauma and Acute Care Surgery 2017;82(5):956‐62. [PUBMED: 28257392] [DOI] [PubMed] [Google Scholar]
Deeks 2017
- Deeks JJ, Higgins JP, Altman DG, editor(s) on behalf of the Cochrane Statistical Methods Group. Chapter 9: Analysing data and undertaking meta‐analyses.In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017). The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook.
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ (Clinical Research Ed.) 1997;315(7109):629‐34. [PUBMED: 9310563] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eljaiek 2017
- Eljaiek R, Heylbroeck C, Dubois MJ. Albumin administration for fluid resuscitation in burn patients: a systematic review and meta‐analysis. Burns 2017;43(1):17‐24. [PUBMED: 27613476] [DOI] [PubMed] [Google Scholar]
Endnote [Computer program]
- Thomson Reuters. Endnote X5. Philadelphia (PA): Thomson Reuters, 2011.
Gattas 2013
- Gattas DJ, Dan A, Myburgh J, Billot L, Lo S, Finfer S. Fluid resuscitation with 6% hydroxyethyl starch (130/0.4 and 130/0.42) in acutely ill patients: systematic review of effects on mortality and treatment with renal replacement therapy. Intensive Care Medicine 2013;39(4):558‐68. [PUBMED: 23407978] [DOI] [PubMed] [Google Scholar]
Geeraedts 2009
- Geeraedts LM Jr, Kaasjager HA, Vugt AB, Frolke JP. Exsanguination in trauma: a review of diagnostics and treatment options. Injury 2009;40(1):11‐20. [PUBMED: 19135193] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed 23 February 2018. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Guyatt 2008
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schunemann HJ. What is "quality of evidence" and why is it important to clinicians?. BMJ (Clinical Research Ed.) 2008;336(7651):995‐8. [PUBMED: 18456631] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence ‐ inconsistency. Journal of Clinical Epidemiology 2011;64(12):1294‐302. [PUBMED: 21803546] [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso‐Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence ‐ imprecision. Journal of Clinical Epidemiology 2011;64(12):1283‐93. [PUBMED: 21839614] [DOI] [PubMed] [Google Scholar]
Haase 2013
- Haase N, Perner A, Hennings LI, Siegemund M, Lauridsen B, Wetterslev M, et al. Hydroxyethyl starch 130/0.38‐0.45 versus crystalloid or albumin in patients with sepsis: systematic review with meta‐analysis and trial sequential analysis. BMJ (Clinical Research Ed.) 2013;346:f839. [PUBMED: 23418281] [DOI] [PMC free article] [PubMed] [Google Scholar]
He 2015
- He B, Xu B, Xu X, Li L, Ren R, Chen Z, et al. Hydroxyethyl starch versus other fluids for non‐septic patients in the intensive care unit: a meta‐analysis of randomized controlled trials. Critical Care 2015;19:92. [PUBMED: 25886952] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Deeks J, editor(s). Chapter 7: Selecting studies and collecting data. In: Higgins JP, Green S, editor(s), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2016
- Higgins JP, Lasserson T, Chandler J, Tovey D, Churchill R. Methodological Expectations of Cochrane Intervention Reviews. Cochrane: London, Version 1.02, 2016. Available from community.cochrane.org/sites/default/files/uploads/MECIR%20PRINTED%20BOOKLET%20FINAL%20v1.02.pdf.
Higgins 2017
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017). The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook.
Kauvar 2006
- Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. The Journal of Trauma 2006;60(6 Suppl):S3‐11. [PUBMED: 16763478] [DOI] [PubMed] [Google Scholar]
Lewis 2016
- Lewis SR, Butler AR, Brammar A, Nicholson A, Smith AF. Perioperative fluid volume optimization following proximal femoral fracture. Cochrane Database of Systematic Reviews 2016, Issue 3. [DOI: 10.1002/14651858.CD003004.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology 2009;62(10):e1‐34. [PUBMED: 19631507] [DOI] [PubMed] [Google Scholar]
McClelland 1998
- McClelland DB. Safety of human albumin as a constituent of biologic therapeutic products. Transfusion 1998;38(7):690‐9. [PUBMED: 9683109] [DOI] [PubMed] [Google Scholar]
Orbegozo 2015
- Orbegozo Cortes D, Gamarano Barros T, Njimi H, Vincent JL. Crystalloids versus colloids: exploring differences in fluid requirements by systematic review and meta‐regression. Anesthesia and Analgesia 2015;120(2):389‐402. [PUBMED: 25565318] [DOI] [PubMed] [Google Scholar]
Peden 2002
- Peden M, Hyder A. Road traffic injuries are a global public health problem. BMJ 2002; Vol. 324, issue 7346:1153. [PUBMED: 12003892] [DOI] [PMC free article] [PubMed]
Qureshi 2016
- Qureshi SH, Rizvi SI, Patel NN, Murphy GJ. Meta‐analysis of colloids versus crystalloids in critically ill, trauma and surgical patients. The British Journal of Surgery 2016;103(1):14‐26. [PUBMED: 26522616] [DOI] [PubMed] [Google Scholar]
Reinhart 2012
- Reinhart K, Perner A, Sprung CL, Jaeschke R, Schortgen F, Johan Groeneveld AB, et al. Consensus statement of the ESICM task force on colloid volume therapy in critically ill patients. Intensive Care Medicine 2012;38(3):368‐83. [PUBMED: 22323076] [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rhodes 2016
- Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Critical Care Medicine 2016;45(3):486‐552. [PUBMED: 28098591] [DOI] [PubMed] [Google Scholar]
Rossaint 2016
- Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernandez‐Mondejar E, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Critical Care 2016;20:100. [PUBMED: 27072503] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shrum 2016
- Shrum B, Church B, McArthur E, Burns KEA, Znajda T, McAlister V. Hypertonic salt solution for peri‐operative fluid management. Cochrane Database of Systematic Reviews 2016, Issue 6. [DOI: 10.1002/14651858.CD005576.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2017
- Sterne JA, Egger M, Moher D, Boutron I, editor(s). Chapter 10: Addressing reporting biases. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017). The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook.
Zarychanski 2013
- Zarychanski R, Abou‐Setta AM, Turgeon AF, Houston BL, McIntyre L, Marshall JC, et al. Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation: a systematic review and meta‐analysis. JAMA 2013;309(7):678‐88. [PUBMED: 23423413] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Perel 2013
- Perel P, Roberts I, Ker K. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database of Systematic Reviews 2013, Issue 2. [DOI: 10.1002/14651858.CD000567.pub6] [DOI] [PubMed] [Google Scholar]
Schierhout 1998
- Schierhout G, Roberts I. Fluid resuscitation with colloids or crystalloid solutions in critically ill patients: a systematic review of randomised controlled trials. BMJ 1998;316:961‐4. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]


