Abstract
Background
A large number of people are employed in sedentary occupations. Physical inactivity and excessive sitting at workplaces have been linked to increased risk of cardiovascular disease, obesity, and all‐cause mortality.
Objectives
To evaluate the effectiveness of workplace interventions to reduce sitting at work compared to no intervention or alternative interventions.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, CINAHL, OSH UPDATE, PsycINFO, ClinicalTrials.gov, and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal up to 9 August 2017. We also screened reference lists of articles and contacted authors to find more studies.
Selection criteria
We included randomised controlled trials (RCTs), cross‐over RCTs, cluster‐randomised controlled trials (cluster‐RCTs), and quasi‐RCTs of interventions to reduce sitting at work. For changes of workplace arrangements, we also included controlled before‐and‐after studies. The primary outcome was time spent sitting at work per day, either self‐reported or measured using devices such as an accelerometer‐inclinometer and duration and number of sitting bouts lasting 30 minutes or more. We considered energy expenditure, total time spent sitting (including sitting at and outside work), time spent standing at work, work productivity and adverse events as secondary outcomes.
Data collection and analysis
Two review authors independently screened titles, abstracts and full‐text articles for study eligibility. Two review authors independently extracted data and assessed risk of bias. We contacted authors for additional data where required.
Main results
We found 34 studies — including two cross‐over RCTs, 17 RCTs, seven cluster‐RCTs, and eight controlled before‐and‐after studies — with a total of 3,397 participants, all from high‐income countries. The studies evaluated physical workplace changes (16 studies), workplace policy changes (four studies), information and counselling (11 studies), and multi‐component interventions (four studies). One study included both physical workplace changes and information and counselling components. We did not find any studies that specifically investigated the effects of standing meetings or walking meetings on sitting time.
Physical workplace changes
Interventions using sit‐stand desks, either alone or in combination with information and counselling, reduced sitting time at work on average by 100 minutes per workday at short‐term follow‐up (up to three months) compared to sit‐desks (95% confidence interval (CI) −116 to −84, 10 studies, low‐quality evidence). The pooled effect of two studies showed sit‐stand desks reduced sitting time at medium‐term follow‐up (3 to 12 months) by an average of 57 minutes per day (95% CI −99 to −15) compared to sit‐desks. Total sitting time (including sitting at and outside work) also decreased with sit‐stand desks compared to sit‐desks (mean difference (MD) −82 minutes/day, 95% CI −124 to −39, two studies) as did the duration of sitting bouts lasting 30 minutes or more (MD −53 minutes/day, 95% CI −79 to −26, two studies, very low‐quality evidence).
We found no significant difference between the effects of standing desks and sit‐stand desks on reducing sitting at work. Active workstations, such as treadmill desks or cycling desks, had unclear or inconsistent effects on sitting time.
Workplace policy changes
We found no significant effects for implementing walking strategies on workplace sitting time at short‐term (MD −15 minutes per day, 95% CI −50 to 19, low‐quality evidence, one study) and medium‐term (MD −17 minutes/day, 95% CI −61 to 28, one study) follow‐up. Short breaks (one to two minutes every half hour) reduced time spent sitting at work on average by 40 minutes per day (95% CI −66 to −15, one study, low‐quality evidence) compared to long breaks (two 15‐minute breaks per workday) at short‐term follow‐up.
Information and counselling
Providing information, feedback, counselling, or all of these resulted in no significant change in time spent sitting at work at short‐term follow‐up (MD −19 minutes per day, 95% CI −57 to 19, two studies, low‐quality evidence). However, the reduction was significant at medium‐term follow‐up (MD −28 minutes per day, 95% CI −51 to −5, two studies, low‐quality evidence).
Computer prompts combined with information resulted in no significant change in sitting time at work at short‐term follow‐up (MD −10 minutes per day, 95% CI −45 to 24, two studies, low‐quality evidence), but at medium‐term follow‐up they produced a significant reduction (MD −55 minutes per day, 95% CI −96 to −14, one study). Furthermore, computer prompting resulted in a significant decrease in the average number (MD −1.1, 95% CI −1.9 to −0.3, one study) and duration (MD ‐74 minutes per day, 95% CI −124 to −24, one study) of sitting bouts lasting 30 minutes or more.
Computer prompts with instruction to stand reduced sitting at work on average by 14 minutes per day (95% CI 10 to 19, one study) more than computer prompts with instruction to walk at least 100 steps at short‐term follow‐up.
We found no significant reduction in workplace sitting time at medium‐term follow‐up following mindfulness training (MD −23 minutes per day, 95% CI −63 to 17, one study, low‐quality evidence). Similarly a single study reported no change in sitting time at work following provision of highly personalised or contextualised information and less personalised or contextualised information. One study found no significant effects of activity trackers on sitting time at work.
Multi‐component interventions
Combining multiple interventions had significant but heterogeneous effects on sitting time at work (573 participants, three studies, very low‐quality evidence) and on time spent in prolonged sitting bouts (two studies, very low‐quality evidence) at short‐term follow‐up.
Authors' conclusions
At present there is low‐quality evidence that the use of sit‐stand desks reduce workplace sitting at short‐term and medium‐term follow‐ups. However, there is no evidence on their effects on sitting over longer follow‐up periods. Effects of other types of interventions, including workplace policy changes, provision of information and counselling, and multi‐component interventions, are mostly inconsistent. The quality of evidence is low to very low for most interventions, mainly because of limitations in study protocols and small sample sizes. There is a need for larger cluster‐RCTs with longer‐term follow‐ups to determine the effectiveness of different types of interventions to reduce sitting time at work.
Keywords: Humans, Ergonomics, Posture, Accelerometry, Controlled Before‐After Studies, Energy Metabolism, Randomized Controlled Trials as Topic, Time Factors, Workplace, Workplace/statistics & numerical data
Workplace interventions (methods) for reducing time spent sitting at work
Why is the amount of time spent sitting at work important?
Time spent sitting and being physically inactive at work has increased in recent decades. Long periods of sitting may increase the risk of obesity, heart disease, and premature death. It is unclear whether interventions that aim to reduce sitting at workplaces are effective.
The purpose of this review
We wanted to find out the effects of interventions aimed at reducing sitting time at work. We searched the literature in various databases up to 9 August 2017.
What trials did the review find?
We found 34 studies conducted with a total of 3,397 employees from high‐income countries. Sixteen studies evaluated physical changes in the workplace design and environment, four studies evaluated changes in workplace policies, 10 studies evaluated information and counselling interventions, and four studies evaluated multi‐category interventions.
Effect of sit‐stand desks
The use of sit‐stand desks seems to reduce workplace sitting on average by 84 to 116 minutes per day. When combined with the provision of information and counselling, the use of sit‐stand desks seems to result in similar reductions in sitting at work. Sit‐stand desks also seem to reduce total sitting time (including sitting at work and outside work) and the duration of workplace sitting bouts that last 30 minutes or longer. One study compared standing desks and sit‐stand desks but due to the small number of employees included, it does not provide enough evidence to determine which type of desk is more effective at reducing sitting time.
Effect of active workstations
Treadmill desks combined with counselling seem to reduce sitting time at work, while the available evidence is insufficient to conclude whether cycling desks combined with the provision of information reduce sitting at work more than the provision of information alone.
Effect of walking during breaks or length of breaks
The available evidence is insufficient to draw conclusions about the effectiveness of walking during breaks in reducing sitting time. Taking short breaks (one to two minutes every half hour) seems to reduce time spent sitting at work by 15 to 66 minutes per day more than taking long breaks (two 15‐minute breaks per workday).
Effect of information and counselling
Providing information, feedback, counselling, or all of these reduces sitting time at medium‐term follow‐up (3 to 12 months after the intervention) on average by 5 to 51 minutes per day. The available evidence is insufficient to draw conclusions about the effects at short‐term follow‐up (up to three months after the intervention). The use of computer prompts combined with providing information reduces sitting time in the medium‐term on average by 14 to 96 minutes per day. The available evidence is insufficient to draw conclusions about the effects in the short‐term.
One study found that prompts to stand reduce sitting time more than prompts to step, on average by 10 to 19 minutes per day.
The available evidence is insufficient to conclude whether providing highly personalised or contextualised information is more or less effective than providing less personalised or contextualised information in reducing siting time at work. The available evidence is also insufficient to draw conclusions about the effect of mindfulness training and the use of activity trackers on sitting at work.
Effect of combining multiple interventions
Combining multiple interventions seems to be effective in reducing sitting time and time spent in prolonged sitting bouts in the short‐term and the medium‐term. However, this evidence comes from only a small number of studies and the effects were very different across the studies.
Conclusions
The quality of evidence is low to very low for most interventions, mainly because of limitations in study protocols and small sample sizes. At present there is low‐quality evidence that sit‐stand desks may reduce sitting at work in the first year of their use. However, the effects are likely to reduce with time. There is generally insufficient evidence to draw conclusions about such effects for other types of interventions and for the effectiveness of reducing workplace sitting over periods longer than one year. More research is needed to assess the effectiveness of different types of interventions for reducing sitting at workplaces, particularly over longer periods.
Summary of findings
Summary of findings for the main comparison.
Alternative desks and workstations compared to sit‐desks for reducing sitting at work
| Alternative desks and workstations compared to sit‐desks for reducing sitting at work | |||||
| Patient or population: employees who sit at work Setting: workplace Intervention: alternative desks and workstations Comparison: sit‐desks | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with sit‐desk | Risk with changes in desk | ||||
| Comparison: sit‐stand desk with or without information and counselling versus sit‐desk | |||||
| Mean difference in time spent sitting at work, short‐term follow‐up (up to 3 months) | The mean difference in time spent sitting at work (short‐term follow‐up) was 364 minutes | MD 100 minutes lower (116 lower to 84 lower) | 323 (10 studies: 4 RCTs, 2 cross‐over RCTs, 4 CBAs) | ⊕⊕⊝⊝ LOW 1 2 | Subgroup analysis showed no difference in effect between sit‐stand desks used alone or in combination with information and counselling. Restricting the analysis to RCTs only did not show any difference in effect either. |
| Mean difference in time in sitting bouts lasting 30 minutes or more, short‐term follow‐up | The mean difference in time in sitting bouts lasting 30 minutes or more (short‐term follow‐up) was 167 minutes | MD 53 minutes lower (79 lower to 26 lower) | 74 (2 CBAs) | ⊕⊝⊝⊝ VERY LOW 2 3 | |
| Comparison: treadmill desk combined with counselling versus sit‐desk | |||||
| Mean difference in time spent sitting at work, short‐term follow‐up (up to 3 months) | The mean difference in time spent sitting at work (short‐term follow‐up) was 342 minutes | MD 29 minutes lower (55 lower to 2 lower) | 31 (1 RCT) | ⊕⊕⊝⊝ LOW 2 4 | |
| Mean difference in time in sitting bouts lasting 30 minutes or more, short‐term follow‐up — not reported | ‐ | ‐ | ‐ | ‐ | |
| Comparison: cycling desk + information and counselling versus sit‐desk + information and counselling | |||||
| Mean difference in time spent in inactive sitting at work, medium‐term follow‐up (from 3 to 12 months) | The mean difference in time spent in inactive sitting at work (medium‐term follow‐up) was 413 minutes | MD 12 minutes lower (24 lower to 1 higher) | 54 (1 RCT) | ⊕⊕⊝⊝ LOW 2 5 | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; RCT: randomised controlled trial CBA: controlled before‐and‐after study; MD: mean difference | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Of the six RCTs, five were at high risk of bias. The non‐randomised controlled before‐and‐after study/studies were also at high risk of bias; downgraded one level
2 Imprecision with wide confidence intervals, small sample size; downgraded one level
3 Unconcealed allocation, unblinded outcome assessment and attrition bias; downgraded two levels
4 Unblinded outcome assessment; downgraded one level
5 Unblinded outcome assessment and attrition bias; downgraded one level
Summary of findings 2.
Workplace policy changes compared to no intervention or alternate intervention for reducing sitting at work
| Workplace policy changes compared to no intervention for reducing sitting at work | |||||
| Patient or population: employees who sit at work Setting: workplace Intervention: policy changes Comparison: no intervention | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with Policy changes | ||||
| Comparision: walking strategies versus no intervention | |||||
| Mean difference in time spent sitting at work, short‐term follow‐up | The mean difference in time spent sitting at work (short‐term follow‐up) was 344 minutes | MD 15 minutes lower (50 lower to 19 higher) | 179 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | |
| Mean difference in time in sitting bouts lasting 30 minutes or more, short‐term follow‐up — not reported | ‐ | ‐ | ‐ | ‐ | |
| Comparision: short break versus long break | |||||
| Mean difference in time spent sitting at work, short‐term follow‐up | The mean difference in time spent sitting at work (short term follow‐up) was 131 minutes | MD 40 minutes lower (66 lower to 15 lower) | 49 (1 RCT) | ⊕⊕⊝⊝ LOW 2 3 | |
| Mean difference in time in sitting bouts lasting 30 minutes or more, short‐term follow‐up — not reported | ‐ | ‐ | ‐ | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; RCT: randomised controlled trial; MD: mean difference | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Risk of bias high due to unblinded outcome assessment and lack of allocation concealment; downgraded with one level
2 Imprecision with wide confidence intervals; downgraded with one level
3 Unconcealed allocation and attrition bias
Summary of findings 3.
Information, feedback, and/or counselling compared to information only or no intervention for reducing sitting at work
| Information and counselling compared to information only or no intervention for reducing sitting at work | |||||
| Patient or population: employees who sit at work Setting: workplace Intervention: information and counselling Comparison: information only or no intervention | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with information only or no intervention | Risk with Information and counselling | ||||
| Information, feedback and counselling versus no intervention | |||||
| Mean difference in time spent sitting at work, short‐term follow‐up — information and feedback versus no intervention | The mean difference in time spent sitting at work (short‐term follow‐up) was 550 minutes | MD 19 minutes lower (57 lower to 19 higher) | 63 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | |
| Mean difference in time spent sitting at work, medium‐term follow‐up — counselling versus no intervention | The mean difference in time spent sitting at work (medium‐term follow‐up) was 462 minutes | MD 28 minutes lower (51 lower to 5 lower) | 747 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 3 | |
| Mean difference in time in sitting bouts lasting 30 minutes or more, short‐term follow‐up ‐ not reported | ‐ | ‐ | ‐ | ‐ | |
| Prompts combined with information versus information alone | |||||
| Mean difference in time spent sitting at work, short‐term follow‐up | The mean difference in time spent sitting at work (short‐term follow‐up) was 349 minutes | MD 10 minutes lower (45 lower to 24 higher) | 75 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | |
| Mean difference in time in sitting bouts lasting 30 minutes or more, short‐term follow‐up | The mean difference in time in sitting bouts lasting 30 minutes or more (short‐term follow‐up) was 286 minutes | MD 74 minutes lower (124 lower to 24 lower) | 28 (1 RCT) | ⊕⊕⊝⊝ LOW 1 4 | |
| Mindfulness training versus no intervention | |||||
| Mean difference in time spent sitting at work, medium‐term follow‐up | The mean difference in time spent sitting at work (medium‐term follow‐up) was 316 minutes | MD 23 minutes lower (63 lower to 17 higher) | 257 (1 RCT) | ⊕⊕⊝⊝ LOW 1 6 | |
| Mean difference in time in sitting bouts lasting 30 minutes or more, medium‐term follow‐up — not reported | ‐ | ‐ | ‐ | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; RCT: randomised controlled trial; MD: mean difference | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Imprecision with wide confidence intervals, small sample size; downgraded with one level
2 Unblinded outcome assessment and attrition bas
3 Risk of bias, allocation not concealed, lack of blinding, high attrition rate; downgraded with one level
4 Lack of blinding of participants and selective reporting
5 Lack of blinding of participants and attrition bias
6 Risk of bias high due to unconcealed allocation and unblinded outcome assessment; downgraded with one level
7 Lack of blinding of participants
Summary of findings 4.
Multi‐component intervention compared to no intervention for reducing sitting at work
| Multi‐component intervention compared to no intervention for reducing sitting at work | |||||
| Patient or population: employees who sit at work Setting: workplace Intervention: multi‐component intervention Comparison: no intervention | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with Multi‐component intervention | ||||
| Mean difference in time spent sitting at work, short‐term follow‐up | See comment | see comment | 573 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | Not pooled |
| Mean difference in time in sitting bouts lasting 30 minutes or more, short‐term follow‐up | See comment | See comment | 518 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | Not pooled |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; RCT: randomised controlled trial | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Unconcealed allocation and unblinded outcome assessment
2 Imprecision with wide confidence interval, small sample size
3 Not pooled due to high heterogeneity
3 Small sample size
Background
Description of the condition
Sedentary behaviour, especially sitting, has attracted great interest from media, government agencies and researchers in recent years. Energy expenditure in various tasks can be expressed in metabolic equivalents (METs). One MET is equivalent to resting energy expenditure, i.e. the energy cost of resting quietly, defined as an oxygen uptake of 3.5 mL kg‐1 min‐1(Ainsworth 2000). Sitting at work and conducting work tasks whilst seated usually involves energy expenditure of 1.5 METs or less. Reduction in time spent sitting usually results in increased levels of physical activity of light to moderate intensity, such as standing or walking (Mansoubi 2014).
The nature of office work has changed since the year 2000 in such a way that workers do not have to move often from their work stations (VicHealth 2012). Advancement in technology (e.g. robotics, computers) has led to a decrease in physical strain at workplaces (Craig 2002). Consequently, workers in some settings have become less physically active at their workplace compared to their leisure time (Franklin 2011; McCrady 2009; Parry 2013; Thorp 2012; van Uffelen 2010). Since the 1960s, in the USA and the UK for example, population levels of occupational physical activity have declined by more than 30% (Ng 2012). A large decline in occupational physical activity has been also found in low‐ and middle‐income countries, such as Brazil and China (Ng 2012). This decline in occupational physical activity can largely be attributed to an increase in time spent sitting at the workplace. It has been found that office‐based employees spent 66% of their total working time sitting, with 5% of all sitting events and 25% of total sitting time spent in bouts longer than 55 minutes (Ryan 2011).
Studies have shown that excessive time spent sitting at work may increase the risk of cardiovascular disease, obesity, diabetes, and all‐cause mortality, even if one is engaged in recommended levels of physical activity during their leisure time (Chau 2014a; Craft 2012; Dunstan 2011). Estimates show a 5% increase in the risk of obesity and 7% increase in the risk of diabetes associated with every two‐hour per day increase in sitting time at work (Hu 2003). It has also been estimated that those who sit for eight to 11 hours per day are at a 15% increased risk of death in the next three years than those who sit for less than four hours per day, whilst the risk increases to 40% for those who sit for more than 11 hours per day (Van der Ploeg 2012). In Bey 2003, it is hypothesised that replacing sitting with physical activity of light (from 1.5 METs to 3 METs) to moderate (3 METs to 6 METs; Ainsworth 2011) intensity improves glucose and lipid metabolism. Another study, Duvivier 2013, has also suggested that benefits may be greater when sitting is replaced with activity of light to moderate intensity, such as standing and walking, than when it is replaced with vigorous cycling of equal energy expenditure. This may indicate that, in interventions to reduce sedentary behaviour, changing posture may be equally or even more important than increasing energy expenditure.
Description of the intervention
It is estimated that 60% of the world's population is part of the workforce and spends on average 60% of their waking hours at work (WHO/WEF 2008). Thus, it is possible to influence health behaviour of a large proportion of the adult population worldwide through workplace interventions.
Workplaces have the advantage of having the potential for creating in‐built social support, that is, active collaboration of employees in making sustainable changes to attain a healthy lifestyle, which may reduce the degree of individual effort and motivation needed to make behavioural changes. Therefore, the changes in lifestyle achieved at work are thought to be sustainable in the long term (Plotnikoff 2012).
Workers can be encouraged to be more physically active through changes in the workplace environment and design. A conventional sitting desk can be replaced or supplemented with: a sit‐stand desk; a so‐called 'hot desk' that is height‐adjustable and allows its user to alternate posture between sitting and standing (Alkhajah 2012; Gilson ND 2012; Straker 2013); a vertical workstation that allows the use of a personal computer while walking on a treadmill at a self‐selected velocity (Levine 2007); a stepping/pedalling desk exercise machine placed under the desk that allows the user to step or pedal while being seated (McAlpine 2007); an inflated balloon chair; or a therapy ball (Beers 2008; USPTO 2000). Replacing conventional office chairs with inflated balloon chairs makes the act of sitting more physically demanding by increasing the need to use the abdominal, back, leg and thigh muscles to remain upright and maintain balance.
Time spent in sedentary behaviour can theoretically also be reduced by changing the layout of workplaces, for example by placing printers further away from desks. Office work can also be made more physically demanding by forming walking or other exercise groups like dance or gym groups during work time (Ogilvie 2007; Thogersen‐Ntoumani 2013), and by encouraging employees to walk around office buildings during breaks or to take a walk to communicate with fellow employees instead of using the telephone or email. The practices and policies of workplaces can be changed by incorporating periodic breaks within the organisational schedule including short bouts of physical activity (e.g. five to 15‐minute activity bouts) or by conducting walking or standing meetings (Commissaris 2007). Meeting rooms can be equipped with sit‐stand desks so that employees can choose to stand during meetings, if they wish (Atkinson 2014). These changes in workplace practice and policy have the potential of providing an opportunity to a large number of people, who mostly sit at work, to reduce their sitting time.
Workers can also be made aware of the importance of changing their sitting behaviour by the provision of information, such as by motivational prompts to sit less at the workstation, via e‐health interventions that encourage and remind workers to sit less or interrupt prolonged periods of sitting (Cooley 2014; Evans 2012; Pedersen 2013), or by distributing leaflets with messages like "Sit less, move more" that highlight the risks associated with sitting. An e‐health intervention consists of information that is delivered electronically like emails, point‐of‐choice prompts, or any message periodically displayed on the computer screen. Informational interventions can also be delivered by trained counsellors in an interactive manner, where, as part of counselling sessions, they find out about worker's interests and provide the worker different options on how to reduce sedentary behaviour (Opdenacker 2008).
There are some potential drawbacks to these interventions. The performance and productivity of workers at sitting jobs might be decreased when walking at the workplace is encouraged and the employees more frequently leave their desks. Workers using a treadmill desk need to be careful not to trip or fall, and thus divide their attention between work and safety, which might compromise their productivity (Tudor‐Locke 2013). In addition, fine motor skills like mouse handling accuracy, math problem solving skills, and perceived work performance seem to decrease with treadmill and cycling desks (Commissaris 2014; John 2009). This decrease in efficiency might be due to learning effects, that is, becoming acquainted with new modes of work.
How the intervention might work
According to ecological models, successful strategies for reducing sedentary behaviour include:
providing access to infrastructures for reducing sedentary behaviour;
increasing awareness and understanding of the importance of and methods for reducing sedentary behaviour; or
using social networks and organisational support to inform and encourage changes in policies and norms related to sedentary behaviour (Sallis 2006).
Based on this definition, we envisage three different ways (in isolation or conjunction with each other) in which interventions could work to decrease sitting at workplaces.
Physical changes in the workplace design and environment
If employees are using a conventional desk or chair in the workplace, provision of new types of work desks or chairs can make them aware of the possibilities such new equipment offers to decrease sitting, and they may be tempted to try them. This would hypothetically replace sitting with some other activity, while allowing the usual tasks to be carried out with the same efficiency. Changing the layout of the workplace by, for example, placing printers away from desks would force employees to stand up and walk to obtain their printouts.
Policies to change the organisation of work
Organisational policies could support the formation of walking or exercise groups at the workplace or conducting walking meetings. Formation of walking or exercise groups or conducting walking meetings, might help individuals to reduce sitting and might also help them encourage each other to adapt new behaviours. The provision of purposive short breaks (with the aim of reducing sitting) might help workers engage in such activities more frequently. The breaks might also encourage employees to take a walk to communicate with colleagues instead of using the telephone or email. Standing meeting rooms would provide an opportunity for office employees to reduce their sitting time.
Provision of information and counselling
Sedentary workers could be made aware of the importance of reducing their time spent in sedentary behaviour. They could be informed about health risks and the benefits of reducing time spent sitting and replacing it with time spent in a more physically demanding behaviour. In Wilks 2006, it was found that employees who had received information regarding the health risks of sitting were more likely to use a sit‐stand desk more frequently than those who had not. Even if people are aware of the adverse effects of excessive sitting, and have access to facilities and programs to decrease sitting, they might still find difficulties in adapting to new behaviour. It requires conscious effort for a person to interrupt their normal sitting behaviour and engage in physical activity while at work. To facilitate behaviour change, people could be provided with point‐of‐choice prompts or counselling, which might enable individuals to evaluate their behavioural choices and motivate them to adopt healthy ones. Points‐of‐choice prompts can be delivered through various means such as signs, emails, text messages, or telephone calls, to motivate change of behaviour. A prompting software can be installed on an employee's personal computer, so that a one‐minute reminder to take a break appears on their screen every 30 minutes (Evans 2012).
Why it is important to do this review
Interventions to decrease sitting at work are becoming increasingly popular, but it is unclear whether they are effective in the long term or not (Healy 2013). Therefore, there is a need to evaluate whether sitting at work can be reduced by interventions, and to compare the effectiveness of various types of such interventions.
Although some studies have shown that sit‐stand desks and walking strategies have been useful in reducing sitting, no significant difference in the duration of individual bouts of sitting was found in Straker 2013. Another study did not find a significant effect of strategies to increase walking on sitting behaviour (Gilson 2009), while in Evans 2012, it was found that point‐of‐choice prompting software along with education was superior to education alone. Such inconsistency in the findings from individual studies means it is unclear whether workplace interventions for reducing sitting are effective, and whether different types of interventions differ in their effectiveness.
Possibly because of the variation in results across studies, recommendations for reducing sitting at work vary. In recent years, several countries, such as the UK and Australia (Australian Government 2014; Department of Health 2011), have incorporated sedentary behaviour recommendations as part of their physical activity guidelines. These guidelines, however, only propose potential strategies for reducing sitting time without quantifying the recommended total duration of sitting time. In 2015, an international group of experts recommended that desk‐based employees should aim towards accumulating two hours of standing and light activity (light walking) per day during working hours, eventually progressing to a total accumulation of four hours per day. To achieve this, they recommended breaking up sitting time with standing by using sit–stand desks or by taking short active standing breaks (Buckley 2015). While all these guidelines stress the evidence of the adverse effects of sitting on health, there is little evidence that different interventions aiming to reduce sitting can help individuals meet any of these recommendations. Furthermore, since this topic is of increasing interest, it is likely that the availability of evidence will increase in the near future. A Cochrane systematic review will ensure timely updating of this information for decision makers.
Objectives
To evaluate the effectiveness of workplace interventions for reducing sitting at work compared to no intervention or alternative interventions.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), cross‐over RCTs, cluster‐RCTs, and quasi‐RCTs. Quasi‐RCTs are trials that allocate participants to the intervention or control group using a method of randomisation that is not actually random. At workplaces, interventions operate at group level and may therefore be difficult to deliver to individuals (Ijaz 2014). Since it is more difficult to randomise units when the intervention is implemented at a higher aggregate level, we also included controlled before‐and‐after studies (CBAs) that used a concurrent control group for the interventions that aimed to change workplace arrangements.
Types of participants
We included all studies conducted with participants aged 18 years or more, whose occupations involved spending the majority of their working time sitting at a desk, such as administrative workers, customer service operators, help‐desk professionals, call‐centre representatives, and receptionists.
We excluded studies that addressed transportation work. People working in the transportation industry (such as taxi drivers, truck drivers, bus drivers, and airline pilots) and who operate heavy equipment (such as crane operators and bulldozer operators) are also exposed to prolonged sitting, but current technology provides very limited options for implementing interventions to decrease sitting in such occupations. Reducing sitting in people who work in the transportation industry and operate heavy machinery would require specific interventions that could be the scope of another review.
Types of interventions
Intervention
Physical changes in the workplace design and environment
Changes in the layout of the workplace, such as placing printers away from office desks.
Changes in desks enabling more physical activity, such as the use of sit‐stand desks, vertical workstations on treadmills, desk cycle/cycling desks, or stepping devices.
Changes in chairs enabling more physical activity, such as inflated balloon chairs or therapy balls.
Policies to change the organisation of work
Walking meetings and walking or other exercise groups during work time.
Breaks (periodic, frequent, or purposive) to sit less, stand up, and take an exercise break.
Sitting diaries.
Provision of information and counselling
Signs or prompts at the workplace (e.g. posters) or at the workstation (computer).
E‐health intervention.
Distribution of leaflets.
Counselling (face to face, by email, or by telephone).
Multi‐component interventions
Interventions that included elements from all the three above‐mentioned categories.
Comparison
We compared the interventions described above with no intervention or with other interventions.
Types of outcome measures
Primary outcomes
We included studies that evaluated sitting at work measured either as:
self‐reported time spent sitting at work by questionnaires; or
device‐based measures of sitting assessed by means of an accelerometer‐inclinometer, which assesses intensity of physical activity and body posture (Kanoun 2009; Kim 2015); or
self‐reported or device‐based measures of time spent in prolonged sitting bouts (e.g. 30 minutes or more) and number of such bouts.
Secondary outcomes
Estimated energy expenditure in metabolic equivalent (MET) hours per workday as a proxy measure to detect changes in sitting time.
Self‐reported or device‐measured total time spent sitting, including sitting at and outside work.
Self‐reported or device‐measured time spent standing and stepping at work.
Work productivity.
Adverse events including any reported musculoskeletal symptoms due to prolonged standing as a possible side‐effect of using a sit‐stand desk.
Search methods for identification of studies
Electronic searches
We searched for all eligible published and unpublished trials in any language. We were prepared to translate non‐English language abstracts for potential inclusion. Our search strategy was based on types of study population, types of study design, work‐related aspects, and outcomes related to sitting, and it consisted of keywords generated with the help of a thesaurus, such as 'seated posture'.
We searched the following electronic databases from inception to 9 August 2017 for identifying potential studies:
Cochrane Central Register of Controlled Trials (CENTRAL; Appendix 1);
MEDLINE (searched through Ovid; Appendix 2);
Cumulative Index to Nursing & Allied Health Literature (CINAHL; Appendix 3);
Occupational Safety and Health Database (OSH UPDATE; Appendix 4);
Excerpta Medica dataBASE (Embase; Appendix 5);
PsycINFO (searched through Ovid; Appendix 6);
ClinicalTrials.gov (http://clinicaltrials.gov/; Appendix 7); and
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal (http://apps.who.int/trialsearch/; Appendix 8).
Searching other resources
We checked reference lists of all included studies and systematic reviews for additional trials. We contacted experts in the field and authors of included studies to identify additional unpublished or ongoing studies.
Data collection and analysis
Selection of studies
Two review authors (NS, KKH) independently screened titles and abstracts of the documents found in our systematic search, to identify potential studies for inclusion. The same authors marked citations as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. We retrieved full‐text study reports or publications for all citations considered potentially relevant. Two authors (NS, KKH) independently assessed the retrieved full‐texts to identify eligible studies for inclusion. We recorded reasons for exclusion of ineligible studies. We resolved disagreements through discussion or, if required, we consulted a third author (SI). We identified and excluded duplicates and collated multiple reports of the same study so that each study rather than each report was the unit of interest in the review. We recorded the selection process in sufficient detail to create a Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram (Moher 2009).
Data extraction and management
We used a data collection template to extract study characteristics and outcome data. We extracted the following information.
Methods: study location, date of publication, type of study design, study setting.
Participants: number randomised or recruited, mean age or age range, gender, inclusion and exclusion criteria of the trial, occupation, number of withdrawals, similarity of study groups in age, gender, occupation, and sitting time at baseline.
Interventions: description of intervention methods and randomised groups, duration of active intervention, duration of follow‐up, and description of comparisons, interventions and co‐interventions.
Outcomes: description of primary and secondary outcomes and their assessment methods.
Notes: source of funding for the trial and potential conflicts of interest of trial authors.
Two review authors (NS and either VH or SI) independently extracted outcome data from the included studies. We noted in the Characteristics of included studies table when trial authors did not report outcome data in a usable way. We resolved disagreements by consensus or by involving a third author (either SI or VH). One review author (NS) transferred data into Cochrane's statistical software, Review Manager 5 (Review Manager 2014). We double‐checked that we had entered the data correctly. For this purpose we tabulated extracted information about studies in a spreadsheet before entry into Review Manager. A review author (JV) spot‐checked a random 20% of extracted data for accuracy against the trial report.
Assessment of risk of bias in included studies
Two review authors (NS and either VH or SI) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements by discussion or by involving another author (ZP). We assessed the included studies' risk of bias according to the following domains.
Random sequence generation
Allocation concealment
Blinding of participants and personnel
Blinding of outcome assessment
Incomplete outcome data
Selective outcome reporting
Validity of outcome measure
Baseline comparability/imbalance for age, gender and occupation of study groups
We graded each potential source of bias as high, low, or unclear and provided a quote from the study report together with a justification for our judgment in the 'Risk of bias' tables. We summarised the risk of bias judgements across different studies for each of the domains. Where information on risk of bias related to unpublished data or correspondence with a trialist, we noted it as such in the 'Risk of bias' tables.
We judged studies as being at low risk for selective outcome reporting, if the publications of the trial followed what had been planned and had been registered in international databases (trial registries), such as ClinicalTrials.gov, Australia and New Zealand Clinical Trials Registry (anzctr.org.au/), or Netherlands Trial Registry (trialregister.nl). We judged the studies that were not registered in trial registries as being at low risk for selective outcome reporting if they had reported all the outcomes mentioned in their methods section.
We judged a study to be at low risk of bias overall when the study included a sufficiently detailed description of its random sequence generation, allocation concealment, blinding of outcome assessment, complete outcome data, no selective outcome reporting, and valid outcome measures, that is, all the domains had a low risk of bias. We judged a study to have a high risk of bias when it reported a feature that would be judged as having a high risk of bias in any one of the eight domains. We did not assess blinding of participants or study personnel for risk of bias, as it is very difficult to blind either of them in studies that are trying to modify sedentary behaviour.
Measures of treatment effect
We entered the outcome data for each study into the data tables in Review Manager to calculate the pooled treatment effects. We used risk ratios (RRs) for dichotomous outcomes and mean differences (MDs) for continuous outcomes. Where only effect estimates and their 95% confidence intervals (CIs) or standard errors were reported in studies, we entered these data into Review Manager using the generic inverse variance method.
Unit of analysis issues
For cluster‐RCTs that did not present results accounting for clustering effect, we calculated these assuming a large intra‐cluster correlation coefficient of 0.10. We based this assumption on a realistic estimate by analogy on studies about implementation research (Campbell 2001). We transformed all measurement units for sitting at work into minutes per eight‐hour workday where needed and possible, and assumed the data referred to a five‐day work week, if this was not reported.
Dealing with missing data
We contacted researchers or study sponsors to verify key study characteristics and obtain missing information or full‐text reports. When we did not find a full study report even after contacting authors listed in the respective abstract, we categorised the references as Studies awaiting classification.
For missing data not obtained from authors, such as standard deviations, we calculated these following the advice in the Cochrane Handbook section 16.1.2 (Higgins 2011). We tested the inclusion of studies with missing data and any imputations in sensitivity analyses.
Assessment of heterogeneity
We assessed clinical homogeneity of the results of included studies based on similarity of populations, interventions, outcomes, and follow‐up times. We considered populations to be similar when the participants were 18 years or older and their occupations involved sitting for a major part of their working time. We considered interventions to be similar when their working mechanisms were similar, for example, replacing sit‐desks with sit‐stand desks (see Types of interventions). We regarded follow‐up times of three months or less as short‐term, between three months and one year as medium‐term, and more than one year as long‐term.
We quantified the degree of heterogeneity using the I² statistic, where an I² value of 25% to 50% indicates a low degree of heterogeneity, 50% to 75% a moderate degree of heterogeneity, and more than 75% a high degree of heterogeneity. If we identified moderate to high heterogeneity, we reported it and explored possible causes by pre‐specified subgroup analyses.
Assessment of reporting biases
When ten or more studies were included in a meta‐analysis, we tested for the effect of small studies using a funnel plot.
Data synthesis
We analysed the effects of interventions in the categories defined in Types of interventions: physical changes in the workplace design and environment (changes in desks; changes in chairs); policies to change the organisation of work (supporting social environment and policies for breaks); or provision of information and counselling. We pooled effect size estimates from individual studies using Review Manager 5 (Review Manager 2014). We considered studies to be heterogeneous, and therefore used a random‐effects model to calculate pooled effect sizes.
We calculated the prediction interval for the outcome sitting time at work for sit‐stand desks compared to sit‐desks. Prediction intervals give an estimate of the effect of a new study based on the heterogeneity of effects of studies included in the meta‐analysis (Higgins 2009; IntHout 2016).
'Summary of findings' table
We reported time spent sitting at work and time spent in sitting bouts of 30 minutes or more at short‐term follow‐up in the 'Summary of findings' table. Where study authors did not report effects in the short‐term follow‐up for the outcomes mentioned above, we presented results at medium‐term follow‐up. We only reported the most relevant comparisons. We used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of the body of evidence that contributed data to the meta‐analyses for these outcomes (Higgins 2011). We justified all decisions to downgrade or upgrade the quality of evidence using footnotes and we made comments to aid readers’ understanding of the review where necessary.
Subgroup analysis and investigation of heterogeneity
If sufficient data become available in future updates of this review we will conduct the following subgroup analyses for the primary outcome of time spent sitting at work.
Age: we will compare studies conducted in participants aged 18 to 40 years with studies where all participants were aged 41 years or older, as the probability of maintaining good health and fitness diminishes with older age (AIHW 2008). Older employees might also expect a larger health benefit due to a reduction in sitting (Manini 2015).
Types of outcome measure: we will carry out a subgroup analysis by type of outcome measure, that is, self‐reported (e.g. questionnaire, log book) versus accelerometer/inclinometer versus Ecological Momentary Assessment.
Types of intervention: we will carry out a subgroup analysis for different interventions that have been pooled under a broader category of intervention.
Similarly, we will assess the robustness of our results by excluding studies we judge to have a high risk of bias from all meta‐analyses.
Results
Description of studies
See: Figure 1, Characteristics of included studies, Characteristics of excluded studies, Characteristics of studies awaiting classification, and Characteristics of ongoing studies.
Figure 1.
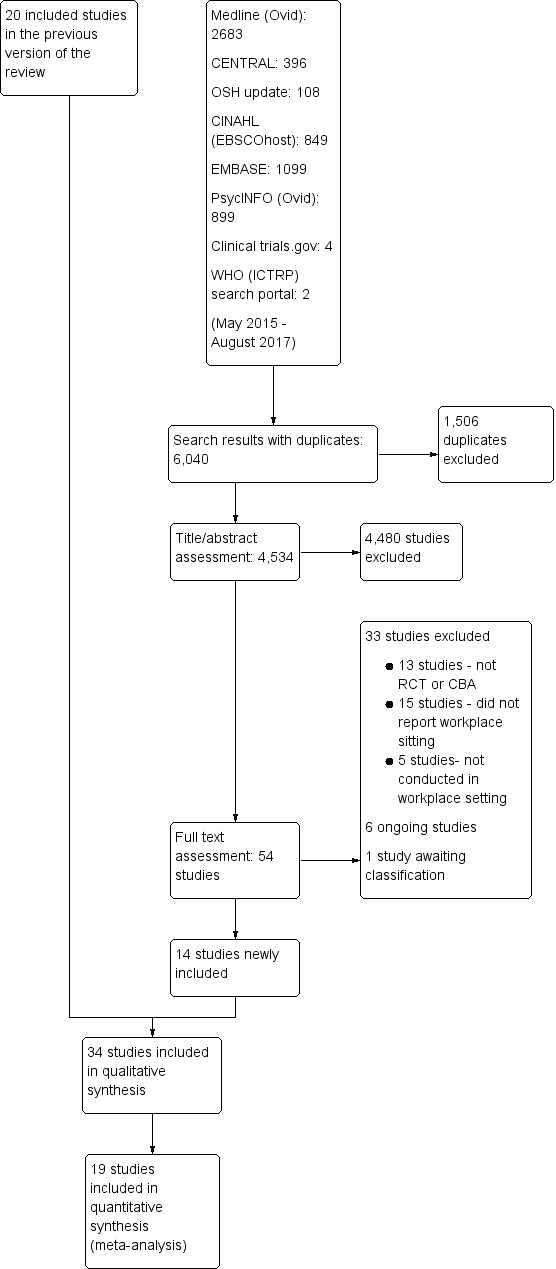
PRISMA study flow diagram
Results of the search
We conducted systematic searches in selected electronic databases and grey literature sources. We identified altogether 12,368 references in the initial search (December 2013) and the first search update (June 2015), and retrieved a total of 92 references for full‐text scrutiny. Of these, we excluded 72 articles and included 20 studies in the previous published version of this review. For this update, we searched the electronic databases from June 2015 until 9 August 2017. The updated search identified a total of 6,040 references, as outlined in Figure 1: 396 from CENTRAL (Appendix 1; 9 August 2017); 2683 from MEDLINE (searched through Ovid, Appendix 2; 9 August 2017); 849 from CINAHL (Appendix 3; 9 August 2017); 108 from OSH UPDATE (Appendix 4; 9 August 2017); 1099 from Embase (Appendix 5; 9 August 2017); 899 from PsycINFO (Appendix 6; 9 August 2017); 4 from ClinicalTrials.gov (Appendix 7; 9 August 2017); and 2 from the WHO trials search portal (Appendix 8; 9 August 2017). Removal of duplicates reduced the total number of references to 4,534. Based on their titles and abstracts, we selected 54 of these references for full‐text reading. Out of these, we excluded 33 studies. Six studies are ongoing and one study was not available in full text so we classified it as a study awaiting classification. This resulted in 14 studies being included in this review update in addition to the 20 studies already included in the previous version of the review.
Included studies
Study design
Out of the 34 included studies, 17 are RCTs, two are cross‐over RCTs, seven are cluster‐RCTs, and eight are controlled before‐and‐after studies with concurrent controls. See Characteristics of included studies for further details. Although the authors described their studies as quasi‐RCTs, we categorised Alkhajah 2012, and Neuhaus 2014a, as controlled before‐and‐after studies because the risk of baseline differences for studies with only two clusters is very high. Only one cluster trial reported unadjusted results (De Cocker 2016). Therefore we adjusted their results for the design effect following the methods stated in Section 16.3 of the Cochrane Handbook for Systematic Reviews of Interventions for the calculations (Higgins 2011).
We considered randomised and non‐randomised studies as similar if there were no considerable differences in their effect estimates (Alkhajah 2012; Chau 2014; Chau 2016; Dutta 2014; Graves 2015; Healy 2013; Li 2017; MacEwen 2017; Neuhaus 2014a; Tobin 2016), but explored any potential differences in a subgroup analysis.
For meta‐analyses that included two arms of the same study, we halved the number of participants in the control group (Coffeng 2014; De Cocker 2016; Neuhaus 2014a). For Coffeng 2014, we used the unadjusted results at twelve months follow‐up. In other comparisons we used the adjusted values with the generic inverse variance method. One included study (Neuhaus 2014a) reported only MDs and standard errors and the authors could not provide raw data, so we could not adjust the number of participants. In this case we modelled the means and standard deviations from the intervention and the control group in Review Manager as closely to the real data as possible to achieve the same MD and standard error. Then we halved the number of participants in the control group and entered the resulting standard errors into Review Manager.
Participants
The included studies were conducted with a total of 3,397 employees. The sample sizes of included trials ranged from 16 in the smallest study (Chau 2016), to 523 in the largest one (Verweij 2012), with a median of 44. Studies included workers from the public and private sectors, with nine studies including researchers and other academic staff, two studies including health workers, and 23 including employees in private companies.
Gender
Participants in 20 studies were predominantly women (Carr 2015; Danquah 2017; De Cocker 2016; Donath 2015; Dutta 2014; Evans 2012; Gao 2015; Gilson 2009; Graves 2015; Healy 2016; Kress 2014; Li 2017; MacEwen 2017; Mailey 2016; Pickens 2016; Priebe 2015; Schuna 2014; Swartz 2014; Tobin 2016; Urda 2016). In the remaining 14 studies the proportions of women and men did not differ significantly.
Country
The studies were conducted in Australia, the USA, Canada, and several high‐income countries in Europe.
Interventions
1. Physical changes in the workplace design and environment
Sixteen studies evaluated the effectiveness of individual workspace modifications on workplace sitting time (Alkhajah 2012; Carr 2015; Chau 2014; Chau 2016; Dutta 2014; Gao 2015; Graves 2015; Healy 2013; Kress 2014; Pickens 2016; Li 2017; MacEwen 2017; Neuhaus 2014a; Schuna 2014; Sandy 2016; Tobin 2016)
Sit‐stand desk
Twelve studies assessed the effectiveness of interventions using sit‐stand desks. The interventions using a sit‐stand desk were assessed independently (Alkhajah 2012; Chau 2014; Dutta 2014; Gao 2015; MacEwen 2017; Neuhaus 2014a), and in combination with information and counselling (Chau 2016; Graves 2015; Healy 2013; Li 2017; Neuhaus 2014a; Tobin 2016).
One study compared the effectiveness of multiple types of interventions, including: 1) sit‐stand desk; 2) ergonomic training; 3) sit‐stand desk combined with ergonomic training; and 4) standard sit‐desk (Sandy 2016).
Standing desk
Two studies compared the effectiveness of a standing desk intervention and a sit‐stand desk intervention (Kress 2014; Pickens 2016).
Active workstation
Two studies evaluated the effectiveness of interventions using active workstations (i.e. desks that cause significant increase in energy expenditure compared to conventional sit‐desks). One study assessed the effectiveness of a treadmill desk (Schuna 2014), while another assessed the effectiveness of a cycle desk (Carr 2015).
2. Policy to change the organisation of work
Two studies evaluated the effectiveness of walking strategies (Gilson 2009; Puig‐Ribera 2015). The first evaluated the effectiveness of route and incidental walking on office employees' sitting time at work (Gilson 2009). The route‐based walking intervention was intended to increase the amount of brisk, sustained walking during work breaks. The incidental walking intervention aimed to increase walking and talking to colleagues, instead of sending emails or making telephone calls, and standing and walking during meetings, instead of sitting at desks. The other study evaluated the effectiveness of incidental movement and short (5 to 10 minutes) and longer (10+ minute) walks on office employees' sitting time at work (Puig‐Ribera 2015).
One study evaluated the effectiveness of planned daily breaks from sitting (Mailey 2016). They compared taking short breaks (one to two minutes every half hour) to taking long breaks (two 15‐minute breaks per workday).
3. Provision of information and counselling
Information and feedback
One study evaluated the effectiveness of personalised computer‐tailored feedback and generic feedback intervention in reducing sitting time in office employees (De Cocker 2016). Another compared the effectiveness of delivering emails containing psychosocial materials and other available resources that were based on constructs of Social Cognitive Theory relating to decreasing sedentary behaviours at work, to delivering emails concerning general health topics (Gordon 2013). In Priebe 2015, the effectiveness of providing highly personalised or contextualised information was compared with the effectiveness of providing less personalised or contextualised information.
Counselling
In Verweij 2012, the effectiveness of counselling by occupational physicians (highly trained specialists who provide health services to employees and employers (AFOEM 2014)) was compared with usual care in decreasing sitting time in office employees. Another study evaluated the effectiveness of group motivational interviewing (i.e. a counselling style that stimulates behavioural change by focusing on exploring and resolving ambivalence in a group) by occupational physicians on office employees' sitting time (Coffeng 2014).
Computer prompts
Four studies evaluated the effectiveness of computer prompts combined with information, compared to information alone, for decreasing sitting time in office employees (Donath 2015; Evans 2012; Pedersen 2013; Urda 2016). Computer prompts offer an opportunity to employees to choose and engage in a short 'burst' of physical activity such as standing or walking. One study, Swartz 2014, assessed the effect of hourly prompts (computer‐based and wrist worn) to stand up or to step on reducing sitting time in office employees.
One study, Brakenridge 2016, assessed the effectiveness of activity tracker combined with organisational support compared to organisational support only.
One study, van Berkel 2014, evaluated the effectiveness of mindfulness training in decreasing sitting time in office employees. The mindfulness intervention consisted of homework exercises and information through emails.
4. Multi‐component interventions
Four studies evaluated the effectiveness of combining multiple interventions on sitting at work (Coffeng 2014; Danquah 2017; Ellegast 2012; Healy 2016).
In Coffeng 2014, the effectiveness of combining multiple environmental interventions with Group Motivational Interviewing (GMI) was assessed. The multi‐component environmental intervention consisted of: 1) the Vitality in Practice (VIP) Coffee Corner Zone, where a workplace coffee corner was modified by adding a bar with bar chairs, a large plant, and a giant wall poster (a poster visualizing a relaxing environment, e.g. wood, water, and mountains); 2) the VIP Open Office Zone, where an office was modified by introducing exercise balls and curtains to divide desks in order to reduce background noise; 3) the VIP Meeting Zone, where conference rooms were modified by placing a standing table and a giant wall poster; and 4) the VIP Hall Zone, where table tennis tables were placed and lounge chairs were introduced in the hall for informal meetings. In addition, footsteps were placed on the floor in the entrance hall to promote stair walking.
In Ellegast 2012, the effectiveness of multiple environmental interventions in combination with a walking strategy were assessed. The intervention consisted of measures aiming to change workplace environment (e.g. sit‐stand tables) and behaviour (e.g. using pedometers to provide activity feedback, face‐to‐face motivation for lunch walks, and an incentive system for bicycle commuting or sports activities).
The study by Danquah and colleagues evaluated the effectiveness of a multi‐component intervention comprising of organisational strategies (support from management), environmental strategies (installation of standing meeting tables), and individual strategies (a lecture and email or text messages) (Danquah 2017).
The fourth study evaluated the effectiveness of a multi‐component intervention comprising of organisational strategies (consultation and support from the management), environmental strategies (sit‐stand desk), and individual strategies (coaching and goal setting) (Healy 2016).
Type of control group
No intervention
Twenty‐three included studies used a 'no intervention' control group (Alkhajah 2012; Chau 2014; Chau 2016; Coffeng 2014; Danquah 2017; De Cocker 2016; Dutta 2014; Ellegast 2012; Gao 2015; Gilson 2009; Graves 2015; Healy 2013; Healy 2016; Li 2017; MacEwen 2017; Neuhaus 2014a; Puig‐Ribera 2015; Sandy 2016; Schuna 2014; Tobin 2016; Urda 2016; van Berkel 2014; Verweij 2012).
Other controls
In Carr 2015, a cycle desk in combination with information and counselling was compared with information and counselling only, resulting in the net effect of a cycle desk. In Kress 2014, and Pickens 2016, the effectiveness of standing desks was compared with the effectiveness of sit‐stand desks. Three studies compared computer prompts combined with information with information only, resulting in the net effect of computer prompts (Donath 2015; Evans 2012; Pedersen 2013). In Gordon 2013, the effectiveness of delivering emails concerning general health topics was compared with delivering emails containing psychosocial materials and other available resources based on constructs of the Social Cognitive Theory relating to decreasing sedentary behaviours at work. In Swartz 2014, computer‐based and wrist‐worn prompts, combined with instruction to stand, were compared with the same prompts combined with instruction to walk at least 100 steps. In Priebe 2015, highly personalised information was compared with less personalised information. One study evaluated the effectiveness of short breaks compared to long breaks (Mailey 2016). Another study compared the effectiveness of activity trackers combined with organisational support with organisational support only (Brakenridge 2016).
Outcomes
Total time spent sitting at work
Total time spent sitting at work was used as an outcome variable in 24 studies (Alkhajah 2012; Brakenridge 2016; Chau 2014; Chau 2016; Danquah 2017; De Cocker 2016; Donath 2015; Dutta 2014; Ellegast 2012; Gilson 2009; Gordon 2013; Graves 2015; Healy 2013; Healy 2016; Kress 2014; Li 2017; MacEwen 2017; Neuhaus 2014a; Pedersen 2013; Puig‐Ribera 2015; Sandy 2016; Swartz 2014; Tobin 2016; Urda 2016).
Eight studies reported time spent in occupational sedentary behaviour, which we considered to be equivalent to time spent sitting at work (Carr 2015; Coffeng 2014; Gao 2015; Mailey 2016; Pickens 2016; Schuna 2014; Verweij 2012; van Berkel 2014).
Number of prolonged sitting bouts at work
Three studies reported number of prolonged sitting bouts at work (Evans 2012; Danquah 2017; Swartz 2014).
Total duration of prolonged sitting bouts at work
Six studies reported time spent in prolonged periods of sitting at work (Brakenridge 2016; Danquah 2017; Evans 2012; Healy 2013; Neuhaus 2014a; Priebe 2015).
Total time spent sitting, including sitting at and outside work
Eight studies reported total time spent sitting, including sitting at and outside work (Alkhajah 2012; Brakenridge 2016; De Cocker 2016; Dutta 2014; Ellegast 2012; Healy 2016; MacEwen 2017; Verweij 2012).
Time spent standing and stepping at work
Sixteen studies reported time spent standing at work (Alkhajah 2012; Brakenridge 2016; Chau 2014; Chau 2016; Danquah 2017; De Cocker 2016; Donath 2015; Gao 2015; Graves 2015; Healy 2013; Healy 2016; Li 2017; MacEwen 2017; Neuhaus 2014a; Swartz 2014; Tobin 2016).
Eleven studies reported time spent stepping at work (Alkhajah 2012; Brakenridge 2016; Chau 2014; Chau 2016; Graves 2015; Healy 2013; Healy 2016; Li 2017; Neuhaus 2014a; Swartz 2014; Tobin 2016).
Energy expenditure
Only one study reported estimated energy expenditure based on information about sitting time at work (Pedersen 2013). They used 1.5 METs to represent energy expenditure of sitting and 2.3 METs to represent energy expenditure of quiet standing.
Work productivity
Three studies assessed work performance on a scale from 1 to 10 (Alkhajah 2012; Healy 2013; Neuhaus 2014a). One study, Carr 2015, also reported they had assessed work productivity, but the authors did not report the results.
Two studies assessed work engagement on a scale from 0 to 6 (Coffeng 2014; van Berkel 2014), using the Utrecht Work Engagement Scale, a questionnaire that measures three aspects of engagement: vigour (six items); dedication (five items); and absorption (six items).
One study, Puig‐Ribera 2015, reported the percentage of lost work productivity in terms of Work Limitation Questionnaire Index (WLQ Index) Score. WLQ Index Score is a weighted sum of the scores from the WLQ scales. The Work Limitation Questionnaire consists of 25 items which require employees to rate their level of difficulty to perform 25 specific job demands in the last two weeks. The individual items form four scales: Time management; Physical demands; Mental or Interpersonal, and Output demands scale.
Adverse events
Three studies reported musculoskeletal symptoms by anatomical regions (Alkhajah 2012; Healy 2013; Neuhaus 2014a). Two studies reported musculoskeletal discomfort or pain at three sites: lower back, upper back, and neck and shoulders (Gao 2015; Graves 2015). The first study, Gao 2015, used a scale ranging from 1 (very comfortable) to 5 (very uncomfortable); and in Graves 2015, a scale ranging from 0 (no discomfort) to 10 (extremely uncomfortable) was used. Another study, Carr 2015, also reported having measured musculoskeletal discomfort but they presented no respective data in their article. One study, Danquah 2017, reported musculoskeletal symptoms at all sites on the scale from 0 to 6.
One study measured adverse events as 'one sick day in the last three months' (Alkhajah 2012), whilst two studies used 'more than one sick day in the last month of intervention' (Healy 2013; Neuhaus 2014a).
In Neuhaus 2014a, adverse events were defined as overall body pain.
Follow‐up times
In six studies the longest follow‐up was one month or less (Evans 2012; Healy 2013; Li 2017; Priebe 2015; Swartz 2014; Urda 2016), and in 20 studies the longest follow‐up was between one and three months (Alkhajah 2012; Brakenridge 2016; Chau 2014; Chau 2016; Danquah 2017; De Cocker 2016; Donath 2015; Dutta 2014; Ellegast 2012; Gilson 2009; Gordon 2013; Graves 2015; Healy 2016; Kress 2014; MacEwen 2017; Mailey 2016; Neuhaus 2014a; Pickens 2016; Schuna 2014; Tobin 2016). We categorised all these as short‐term follow‐up.
The remaining eight studies followed participants between three and 12 months (Carr 2015; Coffeng 2014; Gao 2015; Pedersen 2013; Puig‐Ribera 2015; Sandy 2016; van Berkel 2014; Verweij 2012), which we categorised as medium‐term follow‐up.
No studies had a follow‐up longer than 12 months, which we defined as long‐term follow‐up.
Excluded studies
Of the 54 papers we assessed as full‐text, 33 did not meet our inclusion criteria and we summarily excluded them. Thirteen studies were not RCTs or controlled before‐and‐after studies with concurrent controls. Five studies were not conducted in a workplace setting and another 15 studies did not report sitting time at work. See the Characteristics of excluded studies table for further details.
Risk of bias in included studies
Risk of bias varied considerably across the studies (Figure 2).
Figure 2.
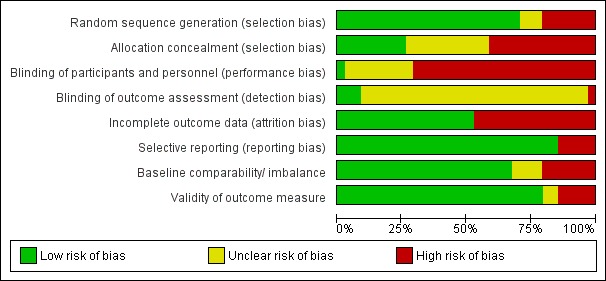
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Seven studies, Alkhajah 2012, Chau 2016, Gao 2015, Healy 2013, Kress 2014, Neuhaus 2014a, Pickens 2016, did not randomise participants and we judged these studies to be at high risk of bias for the domain of random sequence generation. Except for De Cocker 2016, Puig‐Ribera 2015, and Tobin 2016, all the studies described the method of randomisation they had used, so we judged them as having a low risk of bias for the domain of sequence generation. Although these studies mentioned in their publication they conducted randomised trials (De Cocker 2016; Puig‐Ribera 2015; Tobin 2016), they did not describe the method of randomisation and so we judged them to have an unclear risk of bias. One study, Donath 2015, used the minimisation method which is considered equivalent to randomisation (Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions, Higgins 2011).
Only nine studies reported concealing intervention versus control group allocation, so we judged these studies to be at low risk of bias (Brakenridge 2016; Carr 2015; Danquah 2017; Ellegast 2012; Evans 2012; Li 2017; Mailey 2016; Schuna 2014; Swartz 2014). Eleven studies provided no information on allocation concealment, thus we judged these studies to be at unclear risk of bias (Coffeng 2014; De Cocker 2016; Donath 2015; Gilson 2009; Gordon 2013; MacEwen 2017; Priebe 2015; Puig‐Ribera 2015; Sandy 2016; Tobin 2016; Urda 2016). Allocation was not concealed in the remaining studies (Alkhajah 2012; Chau 2014; Chau 2016; Dutta 2014; Gao 2015; Graves 2015; Healy 2013; Healy 2016; Kress 2014; Neuhaus 2014a; Pedersen 2013; Pickens 2016; van Berkel 2014; Verweij 2012) and thus we judged them to be at high risk of bias.
Blinding
In all but a single study (Verweij 2012), the blinding of participants to the interventions they were receiving was not done due to the nature and aims of interventions being self‐evident, so we judged that these 33 studies had a high risk of bias in the performance bias domain. The single study, Verweij 2012, reported asking randomised occupational physicians not to reveal their allocation to participating employees who were their patients.
With regard to outcome assessment, only three studies reported blinding of outcome assessor to group allocation and thus we judged them to have a low risk of bias (Danquah 2017; Evans 2012; Li 2017). One study, Healy 2013, reported that outcome assessors were not blinded to group allocation and we judged their study to have a high risk of bias. The remaining studies did not report on blinding of outcome assessors and thus we judged them to have an unclear risk of detection bias.
Incomplete outcome data
We judged 16 studies to have a high risk of bias due to incomplete outcome data (Chau 2016; De Cocker 2016; Donath 2015; Dutta 2014; Gao 2015; Gilson 2009; Kress 2014; Li 2017; MacEwen 2017; Mailey 2016; Neuhaus 2014a; Pickens 2016; Priebe 2015; Puig‐Ribera 2015; Swartz 2014; Verweij 2012). One study, Dutta 2014, did not report 14% of working hours; the remaining studies lost more than 10% of participants during the follow‐up period. We judged all the remaining 18 studies to have a low risk of bias for incomplete outcome data because of the following reasons. Three studies, Gordon 2013, Graves 2015, and van Berkel 2014, conducted an intention‐to‐treat analysis. One study, Coffeng 2014, conducted multilevel analysis to account for missing data. Another, Chau 2014, reported that imputing values for missing covariate data did not influence the estimated adjusted effects of the intervention on the outcomes. Three studies, Brakenridge 2016, Danquah 2017, and Healy 2016, reported assessing sensitivity of results by multiple imputation using chained equations. Another three studies, Evans 2012, Healy 2013, and Tobin 2016, lost the same proportion of participants from both the intervention groups and the control groups, so we assumed that the missing data was unlikely to have had a significant impact on outcomes (Cochrane Handbook for Systematic Reviews of Interventions, section 8.13.2,Higgins 2011).
Selective reporting
We judged five studies to have a high risk of bias due to discordance between outcomes in available protocols and the ones reported in study results (De Cocker 2016; Evans 2012; Li 2017; Neuhaus 2014a; Schuna 2014). We judged the remaining 17 studies to have a low risk of bias as they reported results for all the outcome measures mentioned either in the protocol or in the methods section of studies where a protocol was not available (Alkhajah 2012; Chau 2014; Coffeng 2014; Donath 2015; Dutta 2014; Gao 2015; Gilson 2009; Gordon 2013; Healy 2013; Pedersen 2013; Puig‐Ribera 2015; Schuna 2014; Swartz 2014; van Berkel 2014; Verweij 2012).
Other potential sources of bias
This domain had the following two parts of assessment, as decided a priori:
validity of outcome measure;
baseline comparability or imbalance for age, gender and occupation of study groups.
Eight studies assessed sitting time at work using questionnaires (Coffeng 2014; Gao 2015; Pedersen 2013; Pickens 2016; Priebe 2015; Sandy 2016; Verweij 2012; van Berkel 2014). Questionnaires are cost‐effective and readily accessible to the majority of the population, but participants receiving the intervention might be aware of the goals and the purpose of the intervention and may, therefore, misreport outcomes (Healy 2011). In six studies (Coffeng 2014; Gao 2015; Priebe 2015; Sandy 2016; Verweij 2012; van Berkel 2014), the questionnaire used has not been tested for validity in assessing time spent sitting at work. Two studies, Pedersen 2013, and Pickens 2016 used the Occupational Sitting and Physical Activity Questionnaire (OSPAQ) which has moderate validity for assessing time spent sitting at work (Chau 2012). Another two studies, Gilson 2009, and Puig‐Ribera 2015, assessed sitting time using a paper‐based diary (log book). The validity and reliability of assessing sitting time using log‐books has not been established. However, they are less dependent on long‐term recall and therefore might provide a more accurate measurement of sitting time at work. In any case log data are subject to reporting bias, as it is not possible to determine whether the log has been filled in at the required intervals or if it was, for example, completed in whole on the final day of assessment (Clark 2009). In Graves 2015, sitting time at work was assessed with Ecological Momentary Assessment diaries. This is a valid, reliable, and feasible approach to assess physical activity and sedentary behaviour. The benefit of Ecological Momentary Assessment is its ability to collect data in real‐time and real‐world circumstances; hence there is no recall bias (Marszalek 2014).
Twenty‐three studies assessed sitting time at work with an accelerometer‐inclinometer (Alkhajah 2012; Brakenridge 2016; Carr 2015; Chau 2014; Chau 2016; Danquah 2017; De Cocker 2016; Donath 2015; Dutta 2014; Ellegast 2012; Evans 2012; Gordon 2013; Healy 2013; Healy 2016; Kress 2014; Li 2017; MacEwen 2017; Mailey 2016; Neuhaus 2014a; Schuna 2014; Swartz 2014; Tobin 2016; Urda 2016. Such device‐based measurements also have some limitations, as outcomes may be affected by methodological decisions made before and after the data collection (e.g. type of accelerometer, cut‐off points, and non‐wear time definitions) (Janssen 2015; Pedišić 2015). Self‐reported sedentary time has shown to have low to moderate correlation with accelerometer‐derived sedentary time, with improved validity when specific domains of sedentary time are recalled (e.g. time spent watching television, computer use, sitting at work; Healy 2011). We therefore judged six studies to have a high risk of bias based on validity of outcome measure (Coffeng 2014; Gao 2015; Priebe 2015; Sandy 2016; Verweij 2012; van Berkel 2014).
We judged two studies to have a high risk of other bias. In Alkhajah 2012, participants in the intervention group were academics involved in sedentary behaviour research, whilst participants in the control group had never been involved in sedentary behaviour or physical activity research. In Gao 2015, Gordon 2013, MacEwen 2017, Mailey 2016, and Pickens 2016, a significant difference was reported between the intervention group and the control group in baseline characteristics and thus we judged these studies to have a high risk of bias. Four studies did not report characteristics of participants at baseline and thus we judged them to have an unclear risk of bias (Priebe 2015; Puig‐Ribera 2015; Sandy 2016; Urda 2016). We judged all other studies to have a low risk of other bias, as neither baselines nor outcome validity was questionable.
Overall Risk of Bias
Overall, we judged only three studies to have a low risk of bias (Carr 2015; Danquah 2017; Ellegast 2012). The remaining studies were judged to have a high risk of bias overall based on: inadequate randomisation (Alkhajah 2012; Chau 2016; Gao 2015; Healy 2013; Kress 2014; Neuhaus 2014a; Pickens 2016); allocation concealment (Alkhajah 2012; Chau 2014; Chau 2016; Dutta 2014; Gao 2015; Graves 2015; Healy 2013; Healy 2016; Kress 2014; Neuhaus 2014a; Pedersen 2013; Pickens 2016; van Berkel 2014; Verweij 2012); blinding of outcome assessment (Healy 2013); incomplete outcome data (Chau 2016; De Cocker 2016; Donath 2015; Dutta 2014; Gao 2015; Gilson 2009; Kress 2014; Li 2017; MacEwen 2017; Mailey 2016; Neuhaus 2014a; Pickens 2016; Priebe 2015; Puig‐Ribera 2015; Swartz 2014; Verweij 2012); selective reporting (De Cocker 2016; Evans 2012; Li 2017; Neuhaus 2014a; Schuna 2014); and other bias (Alkhajah 2012; Brakenridge 2016; Coffeng 2014; Gao 2015; Gordon 2013; MacEwen 2017; Mailey 2016; Pickens 2016; Sandy 2016; van Berkel 2014; Verweij 2012). See Figure 3 for a summary of our judgements about each risk of bias item for each included study.
Figure 3.
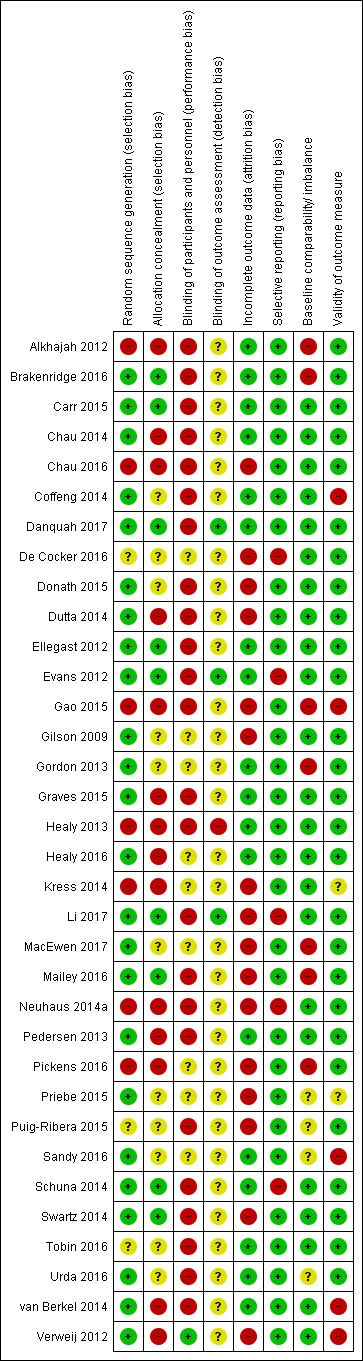
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
We present results using only outcomes for which data were available.
Physical changes in the workplace design and environment
Sit‐stand desk with or without information and counselling versus sit‐desk
Outcome: sitting time
Time spent sitting at work: follow‐up at short term
Ten studies compared the effects of using a sit‐stand desk with or without information and counselling to the effects of using a sit‐desk (Chau 2014; Chau 2016; Dutta 2014; Gao 2015; Graves 2015; Healy 2013; Li 2017; MacEwen 2017; Neuhaus 2014a; Tobin 2016). The pooled analysis showed that the sit‐stand desk with or without information and counselling intervention reduced sitting time at work by on average 100 minutes per eight‐hour workday (95% CI −116 to −84, I² = 37%; Analysis 1.1). In a subgroup analysis, there was no difference in effectiveness between sit‐stand desks with information and counselling and sit‐stand desks only in reducing sitting time at work.
Analysis 1.1.
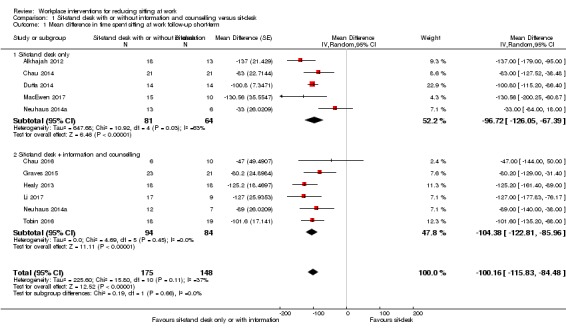
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 1 Mean difference in time spent sitting at work follow‐up short‐term.
In a subgroup analysis including only RCTs, (four studies, Graves 2015; Li 2017; MacEwen 2017; Tobin 2016), a sit‐stand desk with information and counselling reduced sitting time at work on average by 105 minutes (95% CI −128 to −82, I² = 0%; Analysis 1.2). Data presented by one study, Sandy 2016, did not allow for calculation of time spent in sitting time at work and therefore we did not include the study in the quantitative synthesis.
Analysis 1.2.
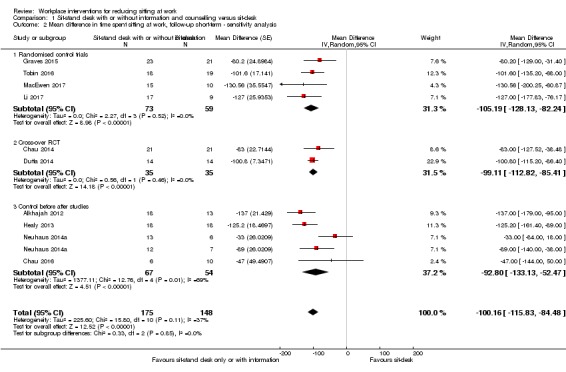
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 2 Mean difference in time spent sitting at work, follow‐up short‐term ‐ sensitivity analysis.
The prediction interval for sitting time ranged from −146 to −54 minutes a day, indicating that in 95% of cases the true effect of a new unique intervention will fall within these values.
Time spent sitting at work: follow‐up at medium‐term
At medium‐term follow‐up, two controlled before‐and‐after studies (Chau 2016; Gao 2015), that provided workers with sit‐stand desks, reduced sitting time at work on average by 57 minutes per eight‐hour workday (95% CI −99 to −15, I² = 0%) compared to sit‐desks (Analysis 1.3).
Analysis 1.3.
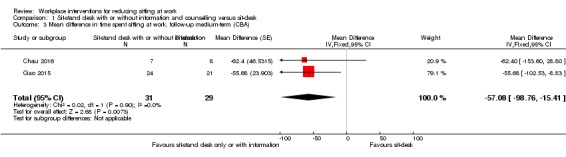
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 3 Mean difference in time spent sitting at work. follow‐up medium‐term (CBA).
Total duration of sitting bouts lasting 30 minutes or more: follow‐up at short‐term
Two controlled before‐and‐after studies containing three study arms measured the intervention effect on the total duration of sitting bouts lasting 30 minutes or more (Healy 2013; Neuhaus 2014a).
In Neuhaus 2014a, they compared the effects of using a sit‐stand desk only with a sit‐stand desk combined with counselling and with a sit‐desk. In Healy 2013, they compared a sit‐stand desk combined with counselling with a sit‐desk. The pooled effect estimate combining sit‐stand desk and sit‐stand desk combined with counselling showed a reduction of 53 minutes, on average, per eight‐hour workday (95% CI −79 to −26) in the total duration of sitting bouts lasting 30 minutes or more in the intervention group, with moderate heterogeneity (I² = 45%; Analysis 1.4). Analysis of the subgroup of interventions combining sit‐stand desks with counselling resulted in a mean reduction of 63 minutes per eight‐hour workday (95% CI −93 to −34), with moderate heterogeneity (I² = 31%; Analysis 1.4).
Analysis 1.4.
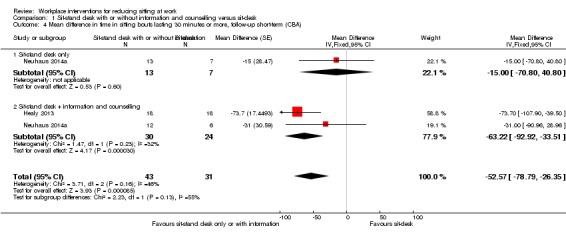
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 4 Mean difference in time in sitting bouts lasting 30 minutes or more, follow‐up short‐term (CBA).
Total time spent sitting, including sitting at and outside work: follow‐up at short‐term
The pooled analysis of two studies (Alkhajah 2012; MacEwen 2017), which compared the effects of sit‐stand desks and sit‐desks on total sitting time, including sitting at work and outside work, at short‐term follow‐up showed a reduction of 82 minutes, on average, per day (95% CI −124 to −39, I² = 0%; Analysis 1.5).
Analysis 1.5.
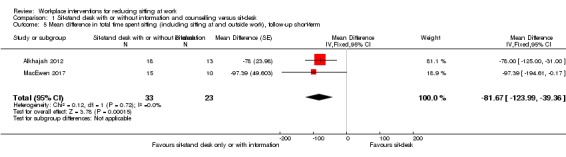
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 5 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up short‐term.
Outcome: standing and stepping time
Time spent standing at work: follow‐up at short‐term
Nine studies reported time spent standing at work at short‐term follow‐up (Alkhajah 2012; Chau 2014; Chau 2016; Graves 2015; Healy 2013; Li 2017; MacEwen 2017; Neuhaus 2014a; Tobin 2016). The pooled analysis showed that sit‐stand desks with or without information and counselling increased standing time at work on average by 89 minutes per eight‐hour workday (95% CI 76 to 102, I² = 58%; Analysis 1.6). However, in a subgroup analysis, sit‐stand desks combined with information and counselling were more effective in increasing standing time at work than sit‐stand desks only (test for subgroup differences: Chi² = 4.31, df = 1 (P = 0.04), I² = 76.8%). Sit‐stand desks only increased standing time at work on average by 76 minutes per eight‐hour workday (95% CI 58 to 94), but there was substantial heterogeneity (I² = 78%) in effect sizes. Sit‐stand desks combined with information and counselling increased standing time at work on average by 103 minutes per eight‐hour workday (95% CI 85 to 122, I² = 0%; Analysis 1.6.2).
Analysis 1.6.
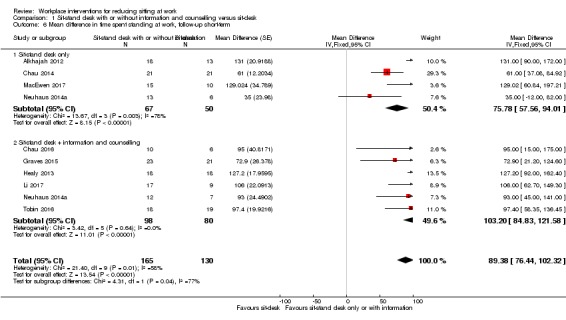
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 6 Mean difference in time spent standing at work, follow‐up short‐term.
In a sensitivity analysis, including only RCTs (four studies, Graves 2015; Li 2017; MacEwen 2017; Tobin 2016), a sit‐stand desk combined with information and counselling increased standing at work on average by 99 minutes per eight‐hour workday (95% CI 75 to 122, I² = 0%; Analysis 1.7).
Analysis 1.7.
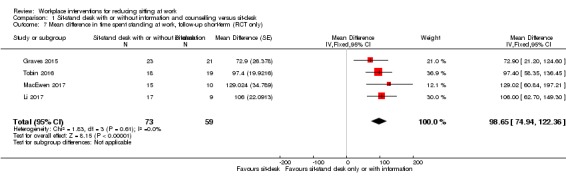
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 7 Mean difference in time spent standing at work, follow‐up short‐term (RCT only).
Time spent stepping at work: follow‐up at short‐term
In the pooled analysis of eight studies (Alkhajah 2012; Chau 2014; Chau 2016; Graves 2015; Healy 2013; Li 2017; Neuhaus 2014a; Tobin 2016), we found no significant difference between the effects of sit‐stand desks and sit‐desks on time spent stepping at work at short‐term follow‐up (MD −1 minute per eight hour workday, 95% CI −4 to 3, I² = 0%; Analysis 1.8).
Analysis 1.8.
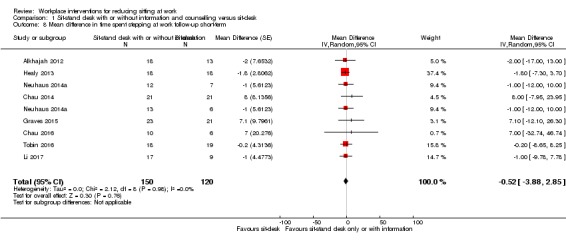
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 8 Mean difference in time spent stepping at work follow‐up short‐term.
Time spent standing at work: follow‐up at medium‐term
At medium‐term follow‐up, two controlled before‐and‐after studies (Chau 2016; Gao 2015), found that providing workers with sit‐stand desks increased standing time at work on average by 53 minutes per eight‐hour workday (95% CI 17 to 90, I² = 0%) compared to sit‐desks (Analysis 1.9).
Analysis 1.9.
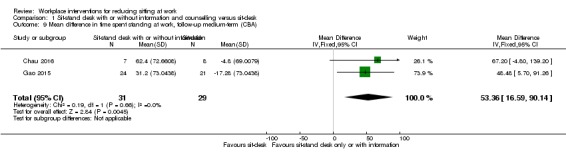
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 9 Mean difference in time spent standng at work, follow‐up medium‐term (CBA).
Outcome: work performance
Self‐reported work performance: follow‐up at short‐term
In three studies (Alkhajah 2012; Healy 2013; Neuhaus 2014a), interventions with sit‐stand desks produced a non‐significant pooled effect on work performance (on a scale from 1 to 10; MD 0.35 score points; 95% CI −0.1 to 0.8; Analysis 1.10). In these studies, work performance was assessed with a 10‐item scale ranging from 1 to 10 relating to the past week, with higher values on the scale indicating better performance.
Analysis 1.10.
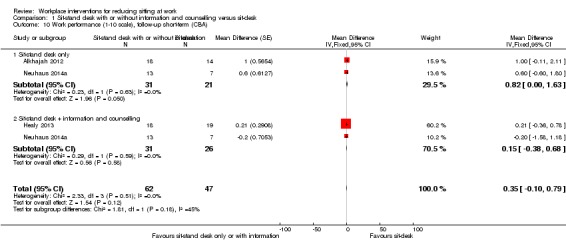
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 10 Work performance (1‐10 scale), follow‐up short‐term (CBA).
Number of sick days: follow‐up at short‐term
One study found no significant change in the proportion of employees having more than one sick day in the sit‐stand desk group compared to sit‐desk in the three months following the installation of sit‐stand desks (risk ratio (RR) 2.2, 95% CI 0.9 to 5.2; Analysis 1.11; Alkhajah 2012).
Analysis 1.11.
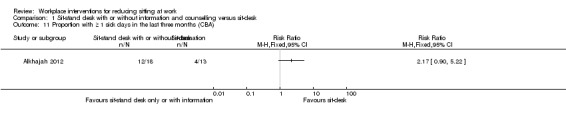
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 11 Proportion with ≥ 1 sick days in the last three months (CBA).
Two studies assessed the proportion of people with more than one sick day in the last month at three months follow‐up (Healy 2013; Neuhaus 2014a). We found no significant pooled effect of the introduction of sit‐stand desks on the risk of having more than one sick day in the last month (RR 0.8, 95% CI 0.5 to 1.2). Accordingly, we found no significant effects for interventions that included information and counselling along with a sit‐stand desk (RR 0.7, 95% CI 0.4 to 1.2) and for those that included sit‐stand desks only (RR 0.9, 95% CI 0.4 to 2.1; Analysis 1.12).
Analysis 1.12.
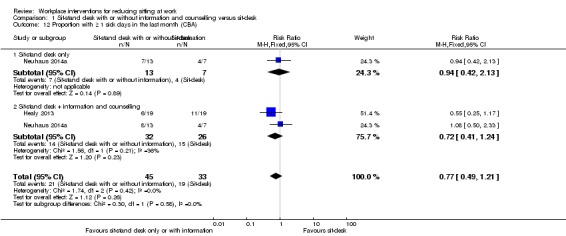
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 12 Proportion with ≥ 1 sick days in the last month (CBA).
Outcome: adverse events
Overall body pain
In one controlled before‐and‐after study, Neuhaus 2014a, one out of 13 participants in the sit‐stand desk group withdrew from the trial because of overall body pain.
Musculoskeletal symptoms: follow‐up at short‐term
Three studies, Alkhajah 2012, Healy 2013, and Neuhaus 2014a, reported musculoskeletal symptoms, assessed using questions with a binary response scale (yes/no), by anatomic regions. We did not combine their results in a meta‐analysis because of substantial heterogeneity in the results (I² = 98%).
Two studies found a lower prevalence of musculoskeletal symptoms among participants using sit‐stand desks compared to those using sit‐desks at three months follow‐up (Alkhajah 2012; Neuhaus 2014a). In the study by Neuhaus 2014a, the magnitude of the effect was significantly larger (MD −16.5, 95% CI −17.8 to −15.3) than in the study by Alkhajah 2012 (MD −6, 95% CI −6.9 to −5.1).
In Healy 2013, a significant but relatively small increase was found in the percentage of participants with musculoskeletal symptoms in the sit‐stand desk combined with counselling group (MD 4, 95% CI 2.6 to 5.5), while in Neuhaus 2014a, a slight decrease was found in the percentage of participants with musculoskeletal symptoms (MD −11.5, 95% CI −12.6 to −10.5) in the sit‐stand desk combined with counselling group compared to the sit‐desk group at three‐month follow‐up.
In Graves 2015, a non‐significant change was found in the ratings of musculoskeletal discomfort by participants using sit‐stand desks compared to participants using sit‐desk at short‐term follow‐up (MD −0.5, 95% CI −1 to 0; Analysis 1.13). Participants rated musculoskeletal discomfort or pain at three sites (lower back, upper back, and neck and shoulders) on a Likert scale ranging from 0 (no discomfort) to 10 (extremely uncomfortable).
Analysis 1.13.
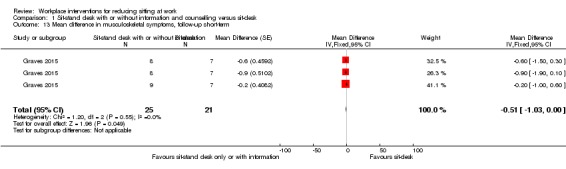
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 13 Mean difference in musculoskeletal symptoms, follow‐up short‐term.
Musculoskeletal symptoms: follow‐up at medium‐term
One study, Gao 2015, assessed perceived musculoskeletal comfort for different body parts (neck and shoulders, upper limbs, back, and lower limbs) rated at the end of a normal workday on a scale from 1 (very comfortable) to 5 (very uncomfortable). The study found a significant but relatively small change in musculoskeletal symptoms with a sit‐stand desk compared to a sit‐desk at six‐month follow‐up (MD −0.5, 95% CI −0.9 to −0.2; Analysis 1.14).
Analysis 1.14.
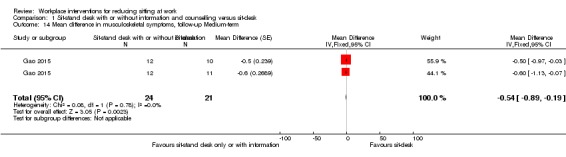
Comparison 1 Sit‐stand desk with or without information and counselling versus sit‐desk, Outcome 14 Mean difference in musculoskeletal symptoms, follow‐up Medium‐term.
Standing desk versus sit‐stand desk
Outcome: sitting time
Time spent sitting at work
One controlled before‐and‐after study, Kress 2014, found that using a standing desk reduced sitting time at work in their sample on average by 10 minutes per eight‐hour workday (95% CI −62 to 43) at short‐term follow‐up (Analysis 2.1) and by 19 minutes per eight‐hour workday (95% CI −64 to 26) at medium‐term follow‐up, but these effects were not statistically significant (Analysis 2.2). Data presented by another study, Pickens 2016, did not allow for calculation of time spent sitting at work and the study was therefore not included in the quantitative synthesis.
Analysis 2.1.
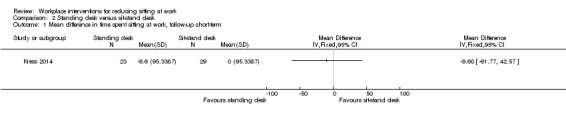
Comparison 2 Standing desk versus sit‐stand desk, Outcome 1 Mean difference in time spent sitting at work, follow‐up short‐term.
Analysis 2.2.
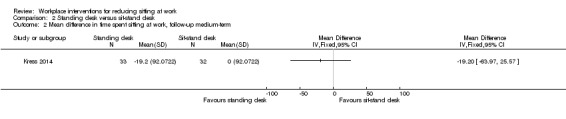
Comparison 2 Standing desk versus sit‐stand desk, Outcome 2 Mean difference in time spent sitting at work, follow‐up medium‐term.
Active workstation versus sit‐desk
Outcome: sitting time
Time spent sitting at work: follow‐up at short‐term
Treadmill desk combined with counselling versus sit‐desk
One RCT, Schuna 2014, found that a treadmill desk combined with counselling reduced sitting time at work by 29 minutes on average per eight‐hour workday (95% CI −55 to −2) compared to no intervention at short‐term follow‐up (Analysis 3.1).
Analysis 3.1.
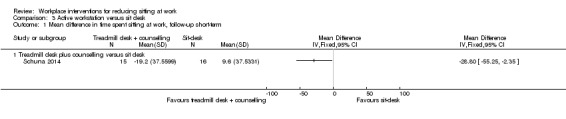
Comparison 3 Active workstation versus sit desk, Outcome 1 Mean difference in time spent sitting at work, follow‐up short‐term.
Time spent in inactive sitting at work: follow‐up at medium‐term
Cycling desks + information and counselling versus information and counselling only
One RCT, Carr 2015, found a non‐significant decrease in inactive sitting at work (MD −12 minutes per day, 95% CI −24 to 1) with a cycling desk combined with information and counselling compared to information and counselling only at medium‐term follow‐up (Analysis 3.2).
Analysis 3.2.
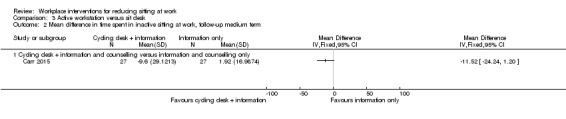
Comparison 3 Active workstation versus sit desk, Outcome 2 Mean difference in time spent in inactive sitting at work, follow‐up medium term.
Outcome: work productivity
One RCT, Carr 2015, found no significant change in musculoskeletal discomfort over the past seven days and work productivity with a cycling desk combined with information and counselling compared to information and counselling only at medium‐term follow‐up. The study did not report any quantitative data for these outcomes.
Policies to change organisation of work
Walking strategies versus no intervention
Outcome: sitting time
Time spent sitting at work: follow‐up at short‐term
A three‐armed RCT, Gilson 2009, found a non‐significant decrease in mean sitting time at work per day (MD −15 minutes per day, 95% CI −50 to 19) in route and incidental walking groups compared to a control group (Analysis 4.1).
Analysis 4.1.
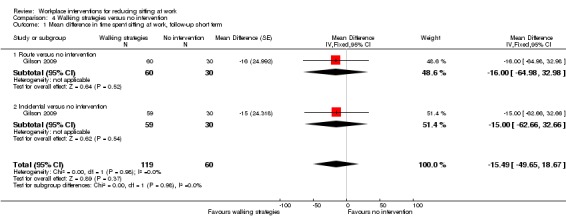
Comparison 4 Walking strategies versus no intervention, Outcome 1 Mean difference in time spent sitting at work, follow‐up short term.
Time spent sitting at work: follow‐up at medium‐term
A cluster‐RCT, Puig‐Ribera 2015, found a non‐significant decrease in sitting time at work (MD −17 minutes per day, 95% Cl −61 to 28) following a web‐based intervention encouraging incidental walking and short walks during the working day compared to a control group at 21‐week follow‐up (Analysis 4.2).
Analysis 4.2.
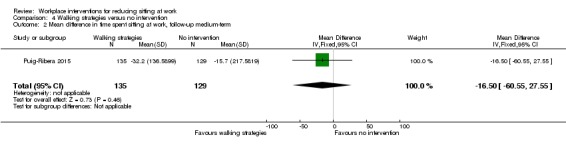
Comparison 4 Walking strategies versus no intervention, Outcome 2 Mean difference in time spent sitting at work, follow‐up medium‐term.
Outcome: work productivity
Percentage of lost work productivity: follow‐up at medium‐term
One cluster‐RCT, Puig‐Ribera 2015, found walking strategies resulted in an average decrease in Work Limitation Questionnaire Index Score of −2.6% (95% CI −4 to −1.3) when compared to no intervention (Analysis 4.3).
Analysis 4.3.
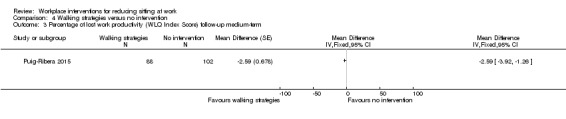
Comparison 4 Walking strategies versus no intervention, Outcome 3 Percentage of lost work productivity (WLQ Index Score) follow‐up medium‐term.
Short break versus long break
Time spent sitting at work: follow‐up at short‐term
One RCT, Mailey 2016, reported that short breaks reduced time spent sitting at work by 40 minutes per eight‐hour workday (95% CI −66 to −15) when compared to long breaks at short‐term follow‐up (Analysis 5.1).
Analysis 5.1.
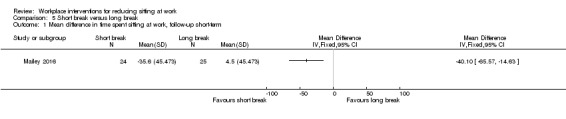
Comparison 5 Short break versus long break, Outcome 1 Mean difference in time spent sitting at work, follow‐up short‐term.
Information and counselling
Information, counselling, and feedback versus no intervention
Outcome: sitting time
Time spent sitting at work: follow‐up at short‐term
Two RCTs compared the effects of information and feedback to no intervention on time spent sitting a work at short‐term follow‐up (De Cocker 2016; Gordon 2013). The pooled effect size for information, feedback, reminder, or all of the above was not significantly different from no intervention (MD −19 minutes per eight‐hour workday, 95% CI −57 to 19, I² = 0%; Analysis 6.1).
Analysis 6.1.
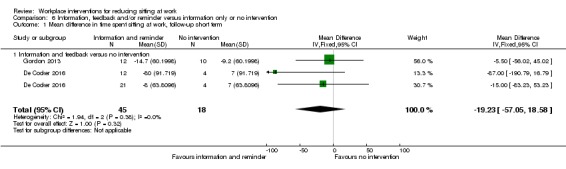
Comparison 6 Information, feedback and/or reminder versus information only or no intervention, Outcome 1 Mean difference in time spent sitting at work, follow‐up short term.
Time spent sitting at work: follow‐up at medium‐term
The pooled analysis of two RCTs comparing counselling to no intervention, Coffeng 2014, and Verweij 2012, showed that counselling reduced sitting time at work on average by 28 minutes per eight‐hour workday (95% CI −51 to −5; I² =0%; Analysis 6.2).
Analysis 6.2.
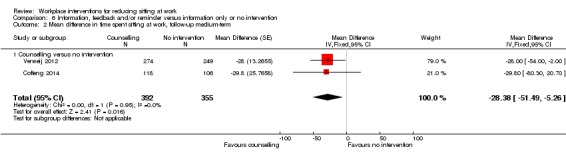
Comparison 6 Information, feedback and/or reminder versus information only or no intervention, Outcome 2 Mean difference in time spent sitting at work, follow‐up medium‐term.
Total time spent sitting, including sitting at and outside work: follow‐up at short‐term
One RCT, De Cocker 2016 found a non‐significant decrease in total time spent sitting with information and feedback compared to no intervention at short‐term follow‐up (MD −16 minutes per day, 95% CI −97 to 64; Analysis 6.3).
Analysis 6.3.
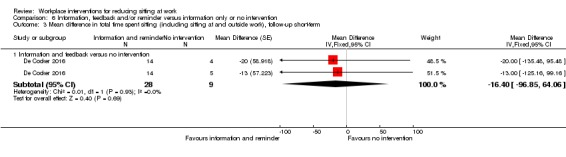
Comparison 6 Information, feedback and/or reminder versus information only or no intervention, Outcome 3 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up short‐term.
Total time spent sitting, including sitting at and outside work: follow‐up at medium‐term
One RCT, Verweij 2012, found a non‐significant decrease in total sitting time with guideline‐based counselling by an occupational physician compared to usual care by an occupational physician (MD −20 minutes per day, 95% CI −85 to 45; Analysis 6.4).
Analysis 6.4.
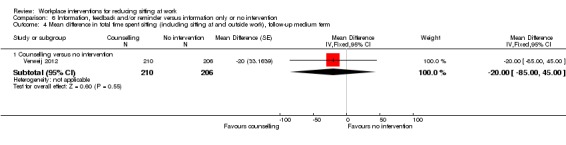
Comparison 6 Information, feedback and/or reminder versus information only or no intervention, Outcome 4 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up medium term.
Outcome: standing time at work
Time spent standing at work: follow‐up at short‐term
One RCT, De Cocker 2016, found a non‐significant effect of information and feedback compared to no intervention on time spent standing at work at short‐term follow‐up (MD 10 minutes per eight‐hour workday, 95% CI −17 to 38; Analysis 6.5).
Analysis 6.5.
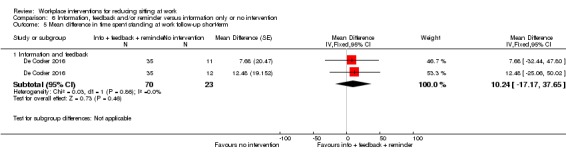
Comparison 6 Information, feedback and/or reminder versus information only or no intervention, Outcome 5 Mean difference in time spent standing at work follow‐up short‐term.
Outcome: work engagement
One RCT, Coffeng 2014, found a non‐significant difference in work engagement (MD 0.1 score points, 95% CI −0.1 to 0.3; on a scale of 0 to 6) at medium‐term follow‐up (Analysis 6.6).
Analysis 6.6.
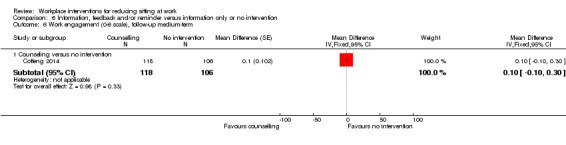
Comparison 6 Information, feedback and/or reminder versus information only or no intervention, Outcome 6 Work engagement (0‐6 scale), follow‐up medium‐term.
Prompts combined with information versus information alone
Outcome: sitting time
Time spent sitting at work: follow‐up at short‐term
Two RCTs compared the effects of computer prompts combined with information to information only on time spent sitting at work (Donath 2015; Urda 2016). The pooled effect size for the computer prompts combined with information compared to information alone was not significant (−10 minutes per eight‐hour workday, 95% CI −45 to 24; I² =0%) (Analysis 7.1).
Analysis 7.1.
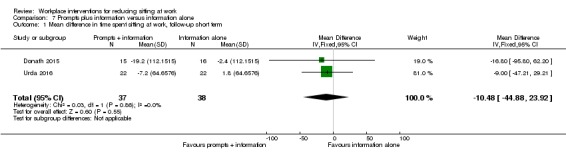
Comparison 7 Prompts plus information versus information alone, Outcome 1 Mean difference in time spent sitting at work, follow‐up short term.
Time spent sitting at work: follow‐up at medium‐term
One RCT, Pedersen 2013, reported a mean decrease in sitting time at work of 55 minutes per eight‐hour workday (95% CI −96 to −14) when computer prompting combined with information was compared to information alone (Analysis 7.2).
Analysis 7.2.
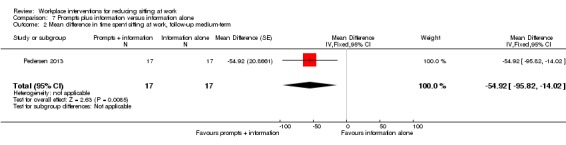
Comparison 7 Prompts plus information versus information alone, Outcome 2 Mean difference in time spent sitting at work, follow‐up medium‐term.
Number of sitting bouts lasting 30 minutes or more: follow‐up at short‐term
One RCT, Evans 2012, found a significant but small decrease of on average 1.1 sitting bouts lasting 30 minutes or more per day (95% CI −1.9 to −0.3) when computer prompting combined with information was compared to information alone (Analysis 7.3).
Analysis 7.3.
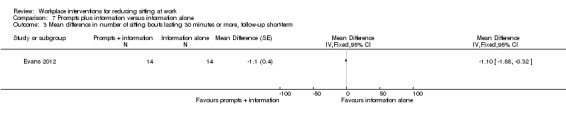
Comparison 7 Prompts plus information versus information alone, Outcome 3 Mean difference in number of sitting bouts lasting 30 minutes or more, follow‐up short‐term.
Total duration of sitting bouts lasting 30 minutes or more: follow‐up at short‐term
One RCT, Evans 2012, also found a reduction of on average 74 minutes per day in the total duration of sitting bouts lasting 30 minutes or more (95% CI −124 to −24) when computer prompts combined with information was compared to information alone (Analysis 7.4).
Analysis 7.4.
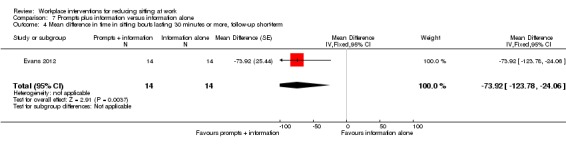
Comparison 7 Prompts plus information versus information alone, Outcome 4 Mean difference in time in sitting bouts lasting 30 minutes or more, follow‐up short‐term.
Total time spent sitting, including sitting at and outside work: follow‐up at short‐term
One RCT, Evans 2012, found a non‐significant decrease in total time spent sitting, including sitting at and outside work, with information and feedback compared to no intervention at short‐term follow‐up (MD −18 minutes per day, 95% CI −53 to 17) (Analysis 7.5).
Analysis 7.5.
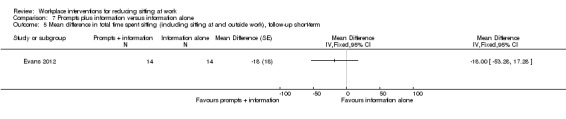
Comparison 7 Prompts plus information versus information alone, Outcome 5 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up short‐term.
Outcome: standing time at work
Time spent standing at work: follow‐up at short‐term
One RCT, Donath 2015, found a non‐significant increase in time spent standing at work with information and feedback compared to no intervention at short‐term follow‐up (MD 32 minutes per eight‐hour workday, 95% CI −7 to 72; Analysis 7.6).
Analysis 7.6.
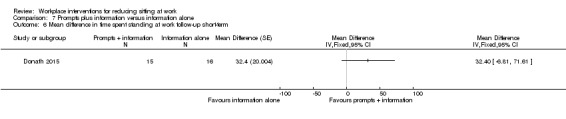
Comparison 7 Prompts plus information versus information alone, Outcome 6 Mean difference in time spent standing at work follow‐up short‐term.
Outcome: energy expenditure at workplace
Calories: follow‐up at medium‐term
One RCT, Pedersen 2013, found a non‐significant difference between the effects of an intervention using computer prompts combined with information and computer prompts alone on estimated energy expenditure at the workplace based on reported activities (MD −278 kilocalories per workday, 95% CI −556 to 0.01; Analysis 7.7).
Analysis 7.7.
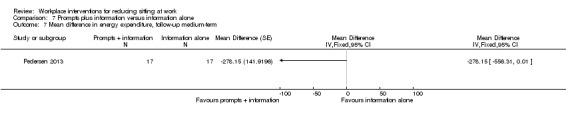
Comparison 7 Prompts plus information versus information alone, Outcome 7 Mean difference in energy expenditure, follow‐up medium‐term.
Computer prompts with instruction to walk 100 steps versus computer prompts with instruction to stand
Outcome: sitting time
Time spent sitting at work: follow‐up at short‐term
One RCT, Swartz 2014, found that employees who received computer prompts to step, sat on average 14 minutes per eight‐hour workday more (95% CI 10 to 19) than employees who received computer prompts to stand (Analysis 8.1).
Analysis 8.1.
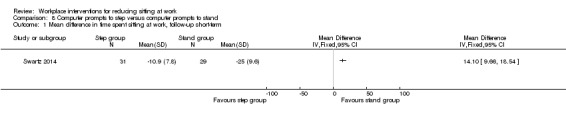
Comparison 8 Computer prompts to step versus computer prompts to stand, Outcome 1 Mean difference in time spent sitting at work, follow‐up short‐term.
Number of sitting bouts lasting 30 minutes or more: follow‐up at short‐term
In the same study, Swartz 2014, the number of sitting events lasting 30 minutes or more was on average 0.4 (95% CI 0.3 to 0.5) higher among the employees in the step group than among the employees in the stand group (Analysis 8.2).
Analysis 8.2.
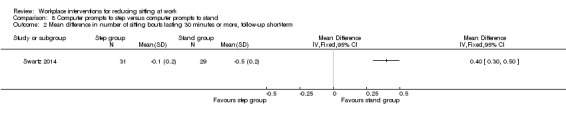
Comparison 8 Computer prompts to step versus computer prompts to stand, Outcome 2 Mean difference in number of sitting bouts lasting 30 minutes or more, follow‐up short‐term.
Outcome: standing and stepping time
Time spent standing and stepping at work: follow‐up at short‐term
One RCT, Swartz 2014, found that employees who received computer prompts to step stood on average 12 minutes less (95% CI −15 to −8; Analysis 8.3) and stepped on average 7 minutes more (95% CI 5 to 8; Analysis 8.4) compared to employees who received computer prompts to stand.
Analysis 8.3.
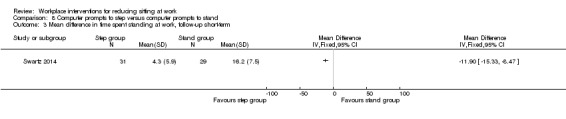
Comparison 8 Computer prompts to step versus computer prompts to stand, Outcome 3 Mean difference in time spent standing at work, follow‐up short‐term.
Analysis 8.4.
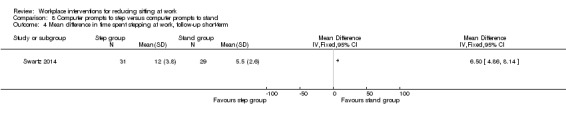
Comparison 8 Computer prompts to step versus computer prompts to stand, Outcome 4 Mean difference in time spent stepping at work, follow‐up short‐term.
Highly personalised information versus less personalised information
Total duration of sitting bouts lasting 30 minutes or more: follow‐up at short‐term
One RCT, Priebe 2015, found a non‐significant increase in the total duration of sitting bouts lasting 30 minutes or more at short‐term follow‐up (MD 14 minutes per eight‐hour workday, 95% CI −37 to 65; Analysis 9.1).
Analysis 9.1.
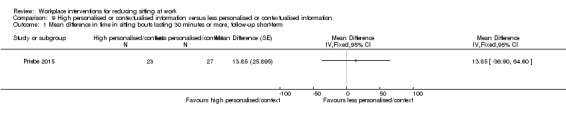
Comparison 9 High personalised or contextualised information versus less personalised or contextualised information, Outcome 1 Mean difference in time in sitting bouts lasting 30 minutes or more, follow‐up short‐term.
Mindfulness training versus no intervention
Outcome: sitting time
Time spent sitting at work: follow‐up at medium‐term
One RCT, van Berkel 2014, found a non‐significant reduction in sitting time at work with mindfulness training compared to no intervention at medium‐term follow‐up (MD −23 minutes per day, 95% CI −63 to 17; Analysis 10.1).
Analysis 10.1.
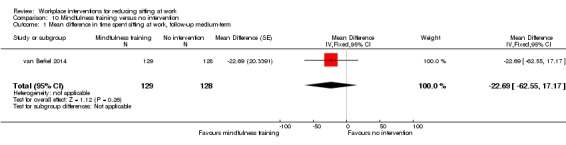
Comparison 10 Mindfulness training versus no intervention, Outcome 1 Mean difference in time spent sitting at work, follow‐up medium‐term.
Outcome: work engagement
One study, van Berkel 2014, reported no significant difference in work engagement (on a scale of 0 to 6) at medium‐term follow‐up (0.2 score points; 95% CI −0.1 to 0.5; Analysis 10.2). The authors assessed work engagement using the Utrecht Work Engagement Scale, which is a self‐reported questionnaire that measures three aspects of engagement: vigour, dedication and absorption.
Analysis 10.2.
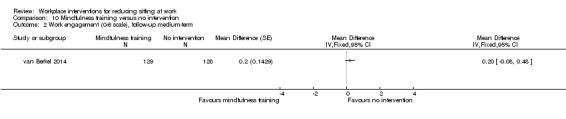
Comparison 10 Mindfulness training versus no intervention, Outcome 2 Work engagement (0‐6 scale), follow‐up medium‐term.
Activity tracker combined with organisational support versus organisational support only
Time spent sitting at work: follow‐up at short‐term
One RCT, Brakenridge 2016, found a non‐significant difference in the effectiveness of an activity tracker combined with organisational support and organisational support only in reducing time spent sitting at work at short‐term follow‐up (MD −6.60 minutes per eight‐hour workday, 95% CI −35 to 22; Analysis 11.1).
Analysis 11.1.
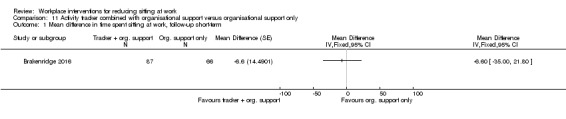
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 1 Mean difference in time spent sitting at work, follow‐up short‐term.
Time spent sitting at work: follow‐up at medium‐term
One RCT, Brakenridge 2016, found a non‐significant difference in the effectiveness of an activity tracker combined with organisational support and organisational support only in reducing time spent sitting at work at medium‐term follow‐up (MD −4.40 minutes per eight‐hour workday, 95% CI −33 to 42; Analysis 11.2).
Analysis 11.2.
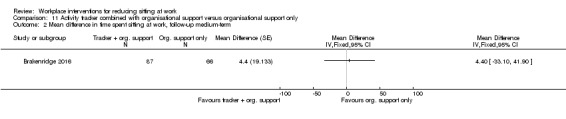
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 2 Mean difference in time spent sitting at work, follow‐up medium‐term.
Total duration of sitting bouts lasting 30 minutes or more: follow‐up at short‐term
One RCT, Brakenridge 2016, found a non‐significant increase in the duration of sitting bouts lasting 30 minutes or more at short‐term follow‐up with an activity tracker combined with organisational support compared to organisational support only (MD 11 minutes per eight‐hour workday, 95% CI −28 to 50; Analysis 11.3).
Analysis 11.3.
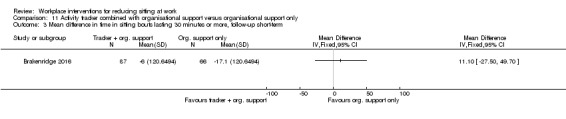
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 3 Mean difference in time in sitting bouts lasting 30 minutes or more, follow‐up short‐term.
Total duration of sitting bouts lasting 30 minutes or more: follow‐up at medium‐term
One RCT, Brakenridge 2016, found a non‐significant difference in the effectiveness of an activity tracker combined with organisational support and organisational support only in reducing duration of sitting bouts lasting 30 minutes or more at medium‐term follow‐up (MD −1 minute per eight‐hour workday, 95% CI −51 to 48; Analysis 11.4).
Analysis 11.4.
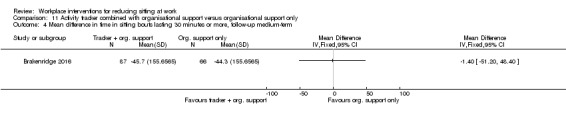
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 4 Mean difference in time in sitting bouts lasting 30 minutes or more, follow‐up medium‐term.
Total time spent sitting, including sitting at and outside work: follow‐up at short‐term
One RCT, Brakenridge 2016, found a non‐significant difference in the effectiveness of an activity tracker combined with organisational support and organisational support only in reducing total time spent sitting, including sitting at and outside work, at short‐term follow‐up (MD 2 minutes per eight‐hour workday, 95% CI −42 to 46; Analysis 11.5).
Analysis 11.5.
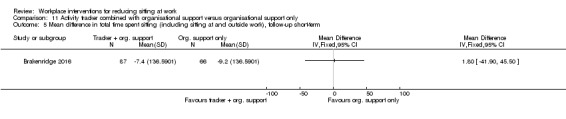
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 5 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up short‐term.
Total time spent sitting, including sitting at and outside work: follow‐up at medium‐term
One RCT, Brakenridge 2016, found a non‐significant decrease in total time spent sitting, including sitting at and outside work, at medium‐term follow‐up with an activity tracker combined with organisational support compared to organisational support only (MD −8 minutes per eight‐hour workday, 95% CI −57 to 40; Analysis 11.6).
Analysis 11.6.
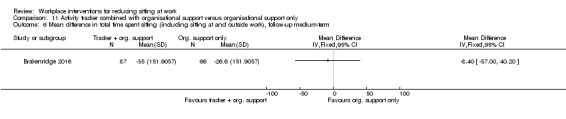
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 6 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up medium‐term.
Outcome: standing and stepping time
Time spent standing and stepping at work: follow‐up at short‐term
One RCT, Brakenridge 2016, found a non‐significant change in time spent standing (MD 3 minutes per eight‐hour workday, 95% CI −20 to 26 minutes per eight‐hour workday; Analysis 11.7) and stepping at work (MD 4 minutes per eight‐hour workday, 95% CI −6 to 14 minutes per eight‐hour workday; Analysis 11.8) with an activity tracker combined with organisational support compared to organisational support only at short‐term follow‐up.
Analysis 11.7.
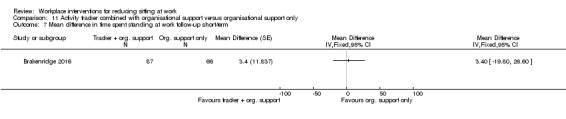
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 7 Mean difference in time spent standing at work follow‐up short‐term.
Analysis 11.8.
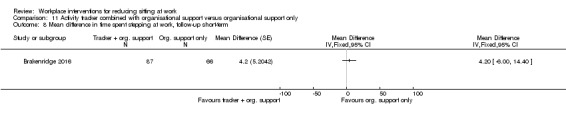
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 8 Mean difference in time spent stepping at work, follow‐up short‐term.
Time spent standing and stepping at work: follow‐up at medium‐term
One RCT, Brakenridge 2016, found a non‐significant change in time spent standing (MD −12 minutes per eight‐hour workday, 95% CI −45 to 20 minutes per eight‐hour workday; Analysis 11.9) and stepping at work (MD 8 minutes per eight‐hour workday, 95% CI −4 to 19 minutes per eight‐hour workday; Analysis 11.10) with an activity tracker combined with organisational support compared to organisational support only at medium‐term follow‐up.
Analysis 11.9.
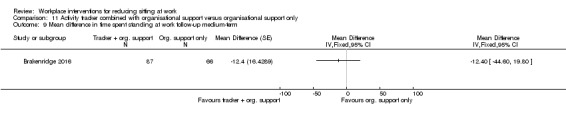
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 9 Mean difference in time spent standing at work follow‐up medium‐term.
Analysis 11.10.
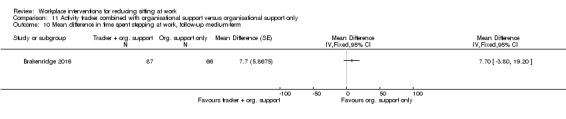
Comparison 11 Activity tracker combined with organisational support versus organisational support only, Outcome 10 Mean difference in time spent stepping at work, follow‐up medium‐term.
Multi‐component intervention versus no intervention
Outcome: sitting time
Time spent sitting at work: follow‐up at short‐term
Three RCTs reported effects on time spent sitting at work at short‐term follow‐up (Ellegast 2012; Danquah 2017; Healy 2016). The pooled analysis of two studies (Ellegast 2012; Healy 2016), showed a significant reduction of on average 101 minutes per eight‐hour workday (95% CI −117.27 to −84, I² =0%; Analysis 12.1) in time spent sitting at work at short‐term follow‐up. However, the third study, Danquah 2017, reported a much smaller reduction in sitting of on average 48 minutes per eight‐hour workday (95% CI −62 to −34). Therefore, we did not pool this study with the other two studies comparing the effect of multi‐component intervention versus no intervention, due to substantial heterogeneity (I² = 92%).
Analysis 12.1.
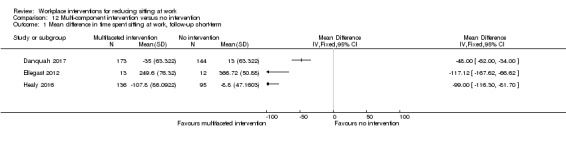
Comparison 12 Multi‐component intervention versus no intervention, Outcome 1 Mean difference in time spent sitting at work, follow‐up short‐term.
Time spent sitting at work: follow‐up at medium‐term
The pooled analysis of two RCTs (Coffeng 2014; Healy 2016), showed a significant decrease of on average 46 minutes per eight‐hour workday in workplace sitting (95% CI −63 to −29, I² = 0%) following multi‐component intervention compared to no intervention at medium‐term follow‐up (Analysis 12.2).
Analysis 12.2.
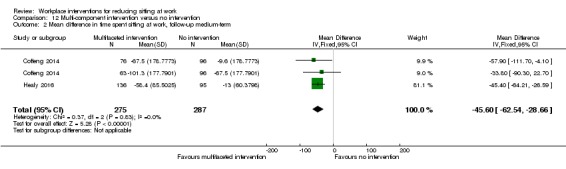
Comparison 12 Multi‐component intervention versus no intervention, Outcome 2 Mean difference in time spent sitting at work, follow‐up medium‐term.
Number of sitting bouts lasting 30 minutes or more: follow‐up at short‐term
One RCT, Danquah 2017, found a small decrease in the number of sitting bouts lasting 30 minutes or more with multi‐component intervention compared to no intervention at short‐term follow‐up (MD −0.4 bouts per day, 95% CI −0.7 to −0.12; Analysis 12.3).
Analysis 12.3.
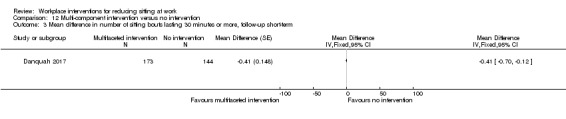
Comparison 12 Multi‐component intervention versus no intervention, Outcome 3 Mean difference in number of sitting bouts lasting 30 minutes or more, follow‐up short‐term.
Total duration of sitting bouts lasting 30 minutes or more: follow‐up at short‐term
One RCT, Healy 2016, found a decrease of 73 minutes, on average, per eight‐hour workday (95% CI −94 to −51) in the total duration of sitting bouts lasting 30 minutes or more following multi‐component intervention compared to no intervention at short‐term follow‐up. However, in the study by Danquah 2017, a much smaller decrease was found in the total duration of sitting bouts lasting 30 minutes or more of on average 16 minutes per eight‐hour workday (95% CI −31 to −1) following multi‐component intervention. Therefore, we did not pool the results of these two studies due to substantial heterogeneity (Analysis 12.4, I² = 95%).
Analysis 12.4.
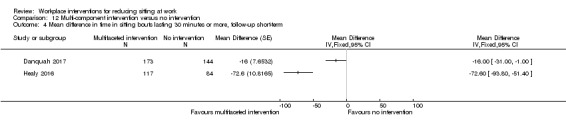
Comparison 12 Multi‐component intervention versus no intervention, Outcome 4 Mean difference in time in sitting bouts lasting 30 minutes or more, follow‐up short‐term.
Total duration of sitting bouts lasting 30 minutes or more: follow‐up at medium‐term
One RCT, Healy 2016, reported a non‐significant decrease of on average 18 minutes per eight‐hour workday (95% CI −46 to 10) in the total duration of sitting bouts lasting 30 minutes or more at medium‐term follow‐up (Analysis 12.5).
Analysis 12.5.
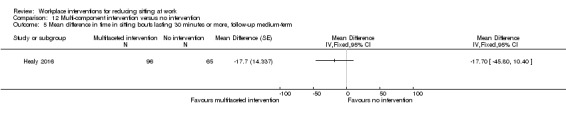
Comparison 12 Multi‐component intervention versus no intervention, Outcome 5 Mean difference in time in sitting bouts lasting 30 minutes or more, follow‐up medium‐term.
Total time spent sitting, including sitting at and outside work: follow‐up at short‐term
Two RCTs reported total time spent sitting, including sitting at and outside work, at short‐term follow‐up (Ellegast 2012; Healy 2016). The pooled analysis showed a significant reduction of on average 73 minutes per day (95% CI −92 to −54) in total time spent sitting, including sitting at and outside work with multi‐component intervention compared to no intervention (Analysis 12.6).
Analysis 12.6.
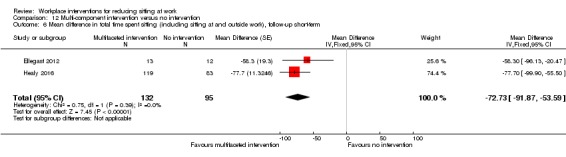
Comparison 12 Multi‐component intervention versus no intervention, Outcome 6 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up short‐term.
Total time spent sitting, including sitting at and outside work: follow‐up at medium‐term
One RCT, Healy 2016, reported a reduction of on average 36 minutes per day (95% CI −62 to −11) in total time spent sitting, including sitting at and outside work, at medium‐term follow‐up (Analysis 12.7).
Analysis 12.7.
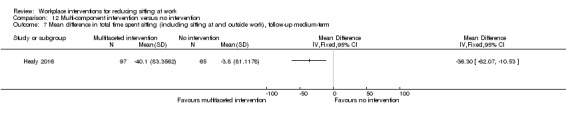
Comparison 12 Multi‐component intervention versus no intervention, Outcome 7 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up medium‐term.
Outcome: standing and stepping time
Time spent standing and stepping at work: follow‐up at short‐term
Two RCTs reported effects on time spent standing at work at short‐term follow‐up (Danquah 2017; Healy 2016). In Healy 2016, an increase was reported of on average 95 minutes per eight‐hour workday (95% CI 79 to 112) in time spent standing at work with multi‐component intervention compared to no intervention (Analysis 12.8). Danquah 2017, however, reported a significantly smaller increase of 43 minutes, on average, per eight‐hour workday (95% CI 30 to 56; Analysis 12.8). We did not pool the results of these two studies due to high heterogeneity (I ² = 96%).
Analysis 12.8.
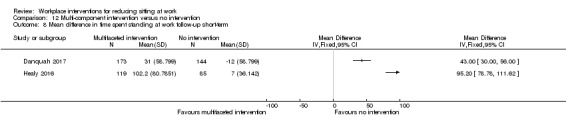
Comparison 12 Multi‐component intervention versus no intervention, Outcome 8 Mean difference in time spent standing at work follow‐up short‐term.
One RCT, Healy 2016, found no significant change in time spent stepping at work (MD 1 minute per eight‐hour workday, 95% CI −4 to 5; Analysis 12.9) following multi‐component intervention compared to no intervention at short‐term follow‐up.
Analysis 12.9.
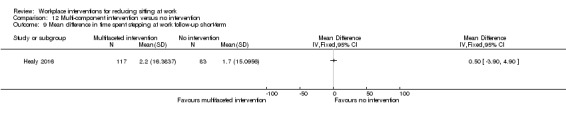
Comparison 12 Multi‐component intervention versus no intervention, Outcome 9 Mean difference in time spent stepping at work follow‐up short‐term.
Time spent standing and stepping at work: follow‐up at medium‐term
One RCT, Healy 2016, reported an average increase of 43 minutes per eight‐hour workday (95% CI 26 to 60; Analysis 12.10) in standing time, whilst they found no significant change in stepping time at work (MD 0 minutes per eight‐hour workday, 95% CI −5 to 4; Analysis 12.11) at medium‐term follow‐up.
Analysis 12.10.
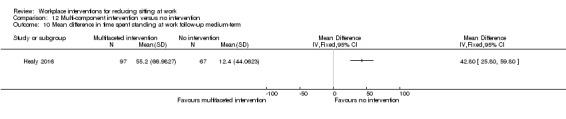
Comparison 12 Multi‐component intervention versus no intervention, Outcome 10 Mean difference in time spent standing at work follow‐up medium‐term.
Analysis 12.11.
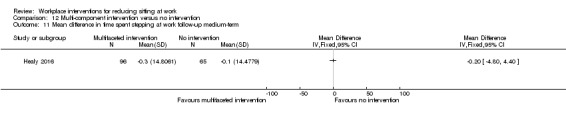
Comparison 12 Multi‐component intervention versus no intervention, Outcome 11 Mean difference in time spent stepping at work follow‐up medium‐term.
Outcome: work engagement
Work engagement: follow‐up at medium‐term
One study, Coffeng 2014, reported no change in work engagement scale score (MD 0 points, 95% CI −0.1 to 0.1, on a scale from 0 to 6) following multi‐component intervention compared to no intervention at medium‐term follow‐up (Analysis 12.12).
Analysis 12.12.
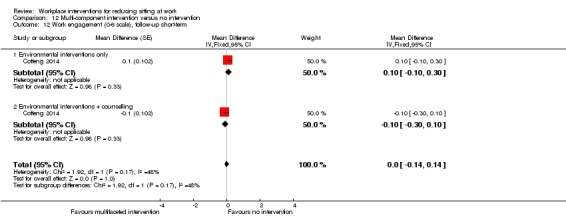
Comparison 12 Multi‐component intervention versus no intervention, Outcome 12 Work engagement (0‐6 scale), follow‐up short‐term.
Outcome: adverse events
Musculoskeletal symptoms: follow‐up at short‐term
One study, Danquah 2017, reported no change in musculoskeletal symptom score (MD −0.2 points, 95% CI −0.32 to −0.02, on a scale from 0 to 6) following multi‐component intervention compared to no intervention at short‐term follow‐up (Analysis 12.13).
Analysis 12.13.
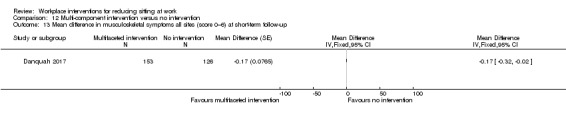
Comparison 12 Multi‐component intervention versus no intervention, Outcome 13 Mean difference in musculoskeletal symptoms all sites (score 0–6) at short‐term follow‐up.
Discussion
Summary of main results
We identified 34 studies which evaluated interventions for reducing sitting at work. These studies investigated physical workplace changes in workplace design and environment, workplace policy changes, information and counselling, and multi‐component interventions for reducing sitting at work.
Physical workplace changes
According to ten studies, providing workers with sit‐stand desks either alone or in combination with information and counselling reduces workplace sitting at short‐term by on average 100 minutes per eight‐hour workday (95% CI −116 to −84, low‐quality evidence) compared to sit‐desks. This finding shows that sit‐stand desk interventions may contribute to achieving the two to four hours of standing at work promoted by a group of experts, in the short term (Buckley 2015). The prediction interval for sitting time at work resulting from interventions comparing sit‐stand desks to sit‐desks ranges from −146 to −54, indicating that in 95% of cases the effect a new unique intervention will fall within these values. It is important to know which activity replaced sitting with the implementation of intervention. The sit‐stand desk intervention seems to replace sitting primarily with standing at short‐term follow‐up (MD 89 minutes, 95% CI 76 to 102). The effectiveness of sit‐stand desk seems to decrease with the length of follow up, with two studies showing an average reduction of 57 minutes per day (95% CI −99 to −15) at medium‐term follow‐up. In two studies that had a follow‐up at short‐term, providing workers with sit‐stand desks reduced the total amount of time spent in bouts of prolonged sitting by 53 minutes a day (95% CI −79 to −26, very low‐quality evidence). Similarly, total sitting time (including sitting at and outside work) also decreased at short‐term follow‐up on average by 82 minutes per day (95% CI −124 to −39, two studies). A single study found a non‐significant difference between standing desks and sit‐stand desks in their effects on reducing the total amount of time spent in bouts of prolonged sitting. The effects of active workstations, such as treadmill desks or cycling desks, on sitting time were unclear or inconsistent.
Policies to change organisation of work
One study showed that implementing walking strategies had no significant effect on workplace sitting time at short‐term (MD −15 minutes per day, 95% CI −50 to 19, low‐quality evidence) and medium‐term follow‐up (MD −17 minutes per day, 95% CI −61 to 28). Furthermore, a single study found that short breaks (one to two minutes every half hour) reduced time spent sitting at work on average by 40 minutes per day (95% CI 66 to 15, low‐quality evidence) more than long breaks (two 15‐minute breaks per workday) at short‐term follow‐up.
Information and counselling
The pooled effect size from two studies which evaluated provision of information and feedback found a non‐significant reduction in time spent sitting at work at short‐term follow‐up (MD −19 minutes per day, 95% CI −57 to 19, low‐quality evidence). A pooled analysis of two studies comparing counselling to no intervention, showed a significant reduction in time spent sitting at work at medium‐term follow‐up (MD −28 minutes per day, 95% CI −51 to −5, low‐quality evidence). Computer prompting led to a nonsignificant reduction in sitting time at work in the short term (MD −10 minutes per day, 95% CI −45 to 24, 2 studies, low‐quality evidence). However, their effect at medium‐term follow‐up was significant (MD −55 minutes per day, 95% CI −96 to −15, one study). Furthermore, computer prompting resulted in a significant decrease in the average number (−1.1, 95% CI −1.9 to −0.3, one study). and duration (MD ‐74 minutes per day, 95% CI −124 to −24) of sitting bouts lasting 30 minutes or more. A single study found that, in the short term, employees receiving computer prompts to step sat on average 14 minutes more per eight‐hour workday (95% CI 10 to 19) than employees receiving computer prompts to stand. One study found no significant added benefit of providing highly personalised information compared to less personalised information in terms of reducing sitting time at work. A single study did not find a significant change in workplace sitting time at medium‐term follow‐up with mindfulness training (MD −16 minutes, 95% CI −45 to 12, low‐quality evidence). Similarly, a single study found no significant effects of activity trackers on reducing sitting at work in short and medium terms.
Interventions from multiple categories
Multi‐component interventions consisting of physical workplace changes, workplace policy changes, and informational components resulted in significant reductions of time spent sitting at work (three studies, very low‐quality evidence) and time spent in prolonged sitting bouts (two studies, very low‐quality evidence) in the short term. However, there was significant heterogeneity in effect sizes between different studies. At medium‐term follow‐up, the pooled effects of two studies showed a reduction of 46 minutes, on average, per eight‐hour workday (95% CI −63 to −29) with multi‐component intervention.
Overall completeness and applicability of evidence
In total, we included 34 studies assessing various kinds of interventions for reducing time spent sitting at work. Most studies assessed the effectiveness of sit‐stand desks, and the results of our review largely concern this particular intervention. There are no RCTs or controlled before‐and‐after studies that have specifically assessed the effects of standing meetings or walking meetings to reduce sitting at work.
The included studies are all from Australia, Europe, Canada, and the USA. We not find any studies from other countries or continents. None of the included studies had been conducted in low‐ and middle‐income countries. This potentially limits the generalisability of the findings of this review beyond the settings in which the included studies have been conducted. This is partly because work environments and normal practices vary greatly across the globe, and the acceptability and feasibility of workplace interventions pertaining to sitting at work may differ accordingly. Since obesity and other lifestyle‐related diseases are common in high‐income countries, it is not surprising that most studies were from such countries. However, since these diseases are now becoming increasingly prevalent in other countries, for example, in some parts of Asia (Tan 2011; Wang 2011), it would be important to test the effectiveness of these interventions among office employees in a more diverse range of countries.
Almost all studies included in this Cochrane Review have used only short‐term follow‐up. There are no studies with a follow‐up period longer than one year. It is important to demonstrate that behaviour change from sitting to a more active behaviour is sustainable in the long term. The cost of interventions, such as implementation of sit‐stand desks, may be considerable; but if the effects can be sustained in the long‐term, potential benefits are more likely to outweigh the costs.
The population of participants in the included studies consists of office workers of academic institutions, a government agency, a police organisation, and private organisations. We believe that the overall population is largely representative of office workers who spend a large part of their working time sitting and who are in need of interventions to reduce their workplace sitting time.
Although individually focused interventions, such as sit‐stand desks, seem to be very popular, they are considerably more expensive than standard desks and so their use may not be feasible in many workplaces with limited financial resources. In some settings, standing meetings may be an alternative, low‐cost option for reducing sitting time at work (Atkinson 2014). Motivational posters or prompting to stand up or engage in light‐ to moderate‐intensity physical activity, or placing printers or dust‐bins away from desks, could also be feasible low‐cost interventions for larger groups of employees. There is some evidence of health benefits available for breaking up sitting time with intermittent brief bouts of light‐intensity or moderate‐intensity physical activity (Bailey 2015; Larsen 2014) but, as for now, no definite conclusions can be drawn about applicability of such findings to workplaces. There is a need for evaluating the effectiveness of low‐cost interventions that would enable workers to break up sitting time by engaging in brief bouts of physical activity. Only some of the included studies assessed outcomes like standing or stepping to identify where the sitting time was reallocated. It would be important to assess this in future studies, as reallocation of time spent sitting at work to walking or other physical activities would potentially be a more healthy substitute than reallocation to standing.
Quality of the evidence
Even though 26 of 34 studies included in this Cochrane Review are RCTs or cluster‐RCTs, we considered the majority of them to be at high risk of bias and therefore the quality of evidence they yield is low to very low. With complex interventions in the occupational health setting, the random allocation and its concealment is known to be more difficult than in clinical trials. Nevertheless, nine of the included studies managed to achieve it. Unless sample size is large enough, random allocation does not distribute the potential confounders equally across groups; therefore, randomisation is not very effective in studies as small as those included in our review. Further, the self‐evident nature of the interventions makes it very difficult to blind personnel and participants.
Risk of bias for device‐based measures of sitting time by accelerometer‐inclinometer differs from self‐reported sitting time. Participants may be aware of the goals of intervention and overestimate or underestimate sitting time, if it is assessed by self‐reports. Using accelerometer‐inclinometers may make it less likely for participants to interfere with outcome measurement. Consequently the use of device‐measured sedentary behaviour has been recommended for intervention trials (Pedišić 2015).
Two studies are not RCTs as stated a priori in their publication, because they randomised only two groups (Alkhajah 2012; Neuhaus 2014a). The trial authors described them as quasi‐RCTs. The risk of baseline differences is much higher for such studies with only two clusters, so we categorised these two studies as controlled before‐and‐after studies, rather than RCTs. We addressed the baseline imbalances for both studies in our 'Risk of bias' assessment.
Although studies performed poorly on the allocation concealment and blinding of participants and personnel domains, most studies assessed the outcomes in a way that we judged to have a low risk of bias. Taking all this into consideration, we rated the overall quality of the evidence as low to very low.
Potential biases in the review process
We did not exclude articles published in languages other than English. In this way, we avoided language bias in our review.
We could not assess the robustness of our results, as there were not enough studies with a low risk of bias to perform a meaningful sensitivity analysis.
To avoid publication bias, we searched sources of grey literature and unpublished studies and data. We noted no obvious asymmetry (which would indicate publication bias) in the funnel plots of studies comparing sit‐stand desks with or without information and counselling with sit‐desks for time spent sitting at work as an outcome (Figure 4). For other comparisons and outcomes, there were too few studies per outcome (less than 10 studies) to assess publication bias using funnel plots. However, the fact that most included studies were small and all reported positive outcomes is indicative that there may be publication bias in this area. If more studies are included in a future update of this review, we will assess the extent of publication bias by means of funnel plots and Egger's test (Egger 1997).
Figure 4.
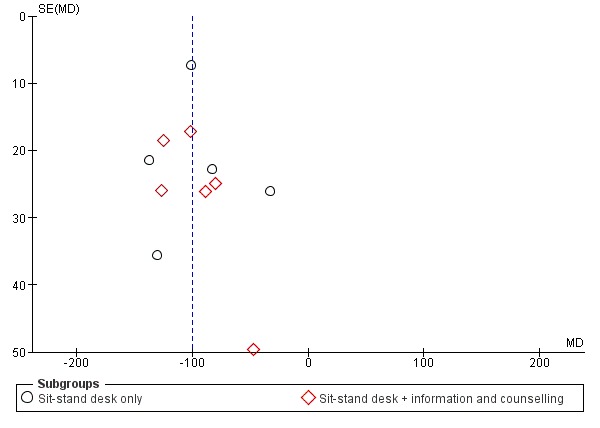
Funnel plot of comparison: 1 Sit‐stand desk with or without information and counselling versus sit‐desk, outcome: 1.1 Mean difference in time spent sitting at work: short‐term follow‐up.
Agreements and disagreements with other studies or reviews
Recently, several systematic reviews have been published on interventions for reducing sedentary behaviour (Commissaris 2016; Gardner 2015a; Martin 2015; Prince 2014). Two of these assessed the effectiveness of interventions for reducing sedentary behaviour in adults at the workplace as well as in other settings; they included 51 studies (Martin 2015), and 65 studies (Prince 2014). Both reviews concluded that sedentary behaviour interventions in adults may be effective for reducing sedentary behaviour. A recent systematic review by Commissaris 2016, containing 40 studies, assessed the effectiveness of workplace interventions to change employees’ sedentary behaviour or physical activity, or both. This systematic review found strong evidence for a decrease in sedentary behaviour with the use of alternative desks, and this differs considerably from our finding of very‐low to low‐quality evidence for alternative desks.
Another recent systematic review with 26 included studies, Gardner 2015a, looked into the behaviour change strategies adopted by sedentary behaviour interventions using the Behaviour Change Wheel. It found that using more techniques made the interventions more promising in terms of their effectiveness. The most frequently observed behaviour change techniques were: setting behavioural goals, providing social support, and environmental interventions. In Gardner 2015a, they found two workplace interventions to be promising: education and environmental interventions. Only the finding about the latter type of interventions is in line with the findings of our review.
The differences in energy expenditure between sitting and standing seem to be minor. In Mansoubi 2015, it was found that sitting typing tasks resulted in energy expenditure of 1.45 METs (standard deviation (SD) 0.32), whereas the energy cost of standing equated to 1.59 METs (SD 0.37). By contrast, there was a considerable difference between energy costs of sitting and physical activity; for example, walking MET values increased incrementally with speed from 2.17 METs (SD 0.5) at 0.2 miles/hour to 3.22 METs (SD 0.69) at 1.6 miles/hour. It is therefore clear that the use of more dynamic workstations has the potential to considerably increase energy costs. For example, energy expenditure of using a desk‐bike type workstation at light intensity reaches 2.4 METs (Botter 2015). Mansoubi 2015, in line with this, questions if the health benefits of reduced sedentary behaviour are primarily driven by increases in energy expenditure that accompany the transition to light activity (e.g. cycling), differences in postural allocation (e.g. standing), or a combination of both (e.g. walking and cycling). This should be further investigated, to inform future interventions.
Although obesity in employees might incur a significant loss for the workplace (Shrestha 2016), aiming to reduce obesity or overweight by standing up at work may, however, not be pragmatic. One study found only a marginally higher additional metabolic cost for quiet standing compared to sitting (Júdice 2015b). In theory, if an average man and woman spent 50% of an eight‐hour workday standing, they would spend approximately an additional 20 kilocalories (kcal) and 12 kcal, respectively. Our findings show that after three months, a sit‐stand desk combined with counselling increased time spent standing on average by 89 minutes (95% CI 76 to 102), so the additional energy expenditure that can be expected from standing in such interventions is negligible. In accordance with our finding, the authors of a longitudinal study suggested that increasing occupational standing time may not be sufficient to prevent the development of overweight, obesity, impaired glucose tolerance, and type 2 diabetes (Chaput 2015).
One study has suggested that higher amounts of time spent standing may be associated with reduced risk of all‐cause and cardiovascular‐disease mortality (Katzmarzyk 2014). Given that mortality rates decline at higher levels of standing, regardless of insignificant increase in energy expenditure, it may be that standing is generally a healthier behaviour than sitting. However, promoting sustained standing over longer periods of time also does not seem a reasonable solution; for example, Andersen 2007, reported increased musculoskeletal symptoms associated with prolonged standing. Coenen and colleagues have mentioned that an intervention with increased standing and reduced sitting was less effective for people with low back pain than those without low back pain (Coenen 2015). It is not yet known at which amount of standing we may expect adverse health effects, but it is possible that promoting four hours of standing per day during work hours could have negative consequences for some population groups. For instance, elderly workers complain when performing standing work, even if it constitutes less than 50% of their working time (Graf 2015). Pedišić and colleagues have suggested that exploring the effectiveness of interventions promoting an optimal balance between physical activity, quiet standing, sedentary behaviour, and sleep may be an important avenue for future research (Pedišić 2017).
Authors' conclusions
Regarding interventions in the category 'physical changes in workplace design and environment', there is low‐quality evidence that a sit‐stand desk reduces workplace sitting time at short‐term and medium‐term follow‐up. The expected reduction in sitting time with this type of intervention is a little less than two hours per day in short term, which is nearly sufficient on its own to meet expert recommendations on reducing occupational sedentary behaviour. However, the sustainability of these effects over longer periods still remains to be examined. Sit‐stand desks do not have significant effects on work performance, whilst their effects on musculoskeletal symptoms are unclear. The effects of active workstations are inconsistent; treadmill desks seem to reduce inactive sitting time, but we found no significant effects for a cycle desk intervention.
Regarding interventions in the category 'policies to change the organisation of work', studies found that implementing walking strategies had no significant effects on workplace sitting. A single study found taking short breaks to be more effective than taking long breaks for reducing time spent sitting at work. However, it should be noted that the total durations of short breaks (approximately eight breaks of one to two minutes) and long breaks (two breaks of 15 minutes) in this study were not equal; hence the finding about the difference in their effectiveness is vague.
Regarding interventions in the category 'provision of information and counselling', a single study found no significant effects for mindfulness training, while the provision of information, feedback or counselling (or both) and computer prompting showed inconsistent effects on workplace sitting.
Multi‐component interventions consisting of physical workplace changes, workplace policy changes, and informational components resulted in significant reductions of time spent sitting at work, but significant heterogeneity in their effects across studies prevent estimation of a pooled effect size.
Regarding physical changes of the workplace design and environment, we need studies on sit‐stand desks with larger sample sizes and longer duration of follow‐up and more studies testing the effectiveness of active workstations. To prevent possible contamination, we recommend randomising employees using a cluster‐randomised design with at least two intervention sites and two control sites but preferably many more, to minimise confounding by workplace‐specific variables (EPOC). Even when employees are not explicitly told which group they are in, true blinding is not possible as intervention activities will be noticeable at work sites (McEachan 2011). We recommend conducting trials aimed at reducing sitting at work in low‐ and middle‐income countries, where the burden of non‐communicable diseases is also increasing.
Regarding policies to change the organisation of work, there is a need to conduct trials evaluating low‐cost interventions (e.g. standing meetings or walking meetings, posters or prompts for standing, printers or dust‐bins placed away from the workstation), as they might be the only feasible options in settings with limited financial resources. To develop more effective interventions, it might be important to first better understand the ideas that workers and employers have about health effects of excessive sitting and means to reduce it. There is qualitative research on this topic available that should be summarised in a systematic review.
Future studies should consider measuring the time spent sitting using wearable devices, because of their superior measurement properties compared to self‐reports. Thigh‐mounted accelerometer‐inclinometers may be useful for this purpose, because the thigh changes its angle when shifting from sitting to standing (Janssen 2015). We do not recommend only employing self‐reported measures as their validity may not be adequate for intervention trials (Aadahl 2003; Lagersted‐Olsen 2014). Moreover, participants receiving the intervention are aware of the goals set and the intention of the intervention, and are therefore susceptible to recall bias when reporting their sitting time (Rzewnicki 2003; Shephard 2003). Furthermore, if the intervention is found to reduce sitting, future studies should try to examine what behaviour replaces sitting (e.g. standing, light‐intensity physical activity, or moderate‐ to vigorous‐intensity physical activity). Mansoubi and colleagues argued that reducing sitting time at work might result in more sitting during leisure (Mansoubi 2016). However, a recent systematic review found that interventions aimed at reducing sitting at work also reduced sitting during leisure time (Shrestha 2018). Hence, it is important that workplace intervention studies assess time spent sitting not only in the work domain but also, if possible, in non‐occupational domains.
We recommend including outcome measures that will be of interest to employers, such as valid and reliable measures of productivity, job stress, absenteeism, and cardio‐metabolic health. Future studies should also consider including cost‐effectiveness analyses to help stakeholders and decision makers determine whether the cost of interventions to reduce sitting at work is justified by improvements in health and work‐related outcomes.
Where applicable, the effect should be statistically adjusted for the clustering effect. The overall sample size and the number of clusters should be taken into account when recruiting participants, in order to calculate the required sample size for achieving adequate statistical power.
The ongoing studies that we identified study effectiveness of sit‐stand desks, treadmill desks, cycle desks, walking strategies, computer prompts, provision of information, and counselling. There are still no workplace RCTs evaluating other types of interventions, such as sitting diaries, stepping devices and assessing specifically standing meetings or walking meetings.
Two ongoing studies have been designed according to our recommendations (Dunstan 2014; O’Connell 2015). Both studies are cluster‐RCTs and will have at least two intervention and two control sites. These studies have planned to assess the effectiveness of sit‐stand or height adjustable desks. Both studies have planned to measure sitting at work with an accelerometer‐inclinometer.
Acknowledgements
We thank Jani Ruotsalainen, Managing Editor of the Cochrane Work Group, for providing administrative and logistical support for the conduct of the current review; and Kaisa Neuvonen, Information Specialist of the Cochrane Work Group, for developing the search strategies; and Heikki Laitinen for executing the search strategies for this current update.
We would also like to thank the Cochrane Work Group's Editors, Esa‐Pekka Takala and Anneli Ojajärvi; and external peer referees, Kimi Sawada, Kristel King, Rintaro Mori and Hidde van der Ploeg, for their comments. We thank Joey Kwong, Elizabeth Royle, Jessica Sharp and Jani Ruotsalainen for copy editing the text.
We also wish to thank Suresh Kumar, Chukwudi P Nwankwo and Soumyadeep Bhaumik for their contribution to the previous version of this review.
Sharea Ijaz's time is supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care West (CLAHRC West) at University Hospitals Bristol NHS Foundation Trust.
This review update is a part of the PhD project of the first author, Nipun Shrestha, supervised by Professor Alexandra Parker, Professor Stuart JH Biddle, and Dr Zeljko Pedisic (principal supervisor).
Appendices
Appendix 1. CENTRAL search strategy
#1 work*
#2 sedentary
#3 sitting
#4 #2 or #3
#5 office
#6 inactiv*
#7 #5 and #6
#8 #4 or #7
#9 #1 and #8
#10 #9 AND trials
Appendix 2. MEDLINE search strategy
#1 (work[tw] OR works*[tw] OR work'*[tw] OR worka*[tw] OR worke*[tw] OR workg*[tw] OR worki*[tw] OR workl*[tw] OR workp*[tw] OR occupation*[tw] OR employe*[tw])
#2 (effect*[tw] OR control[tw] OR controls*[tw] OR controla*[tw] OR controle*[tw] OR controli*[tw] OR controll*[tw] OR evaluat*[tw] OR intervention*[tw] OR program*[tw] OR compare*[tw])
#3 (sedentary OR sitting) OR seated posture OR chair[tiab] OR desk[tiab] OR (office AND inactiv*)
#4 (animals [mh] NOT humans [mh])
#5 #1 AND #2 AND #3 NOT #4
Appendix 3. CINAHL search strategy
S10 S1 AND S2 AND S9 Limiters ‐ Exclude MEDLINE records Search modes ‐ Boolean/Phrase
S9 S3 OR S4 OR S5 OR S6 OR S7 OR S8
S8 (office AND inactive*) or TX (office AND inactive*) or MW (office AND inactive*)
S7 Desk or TX desk or MW desk
S6 Sedentary or TX sedentary or MW sedentary
S5 Seated posture or TX seated posture or MW seated posture
S4 Sitting or TX sitting or MW sitting
S3 Chair or TX chair or MW chair
S2 TX randomised controlled trial or TX controlled clinical trial or AB placebo or TX clinical trials or AB randomly or TI trial or TX intervent* or control* or evaluation* or program*
S1 work* OR (offic* OR busines*) OR occupat*
Appendix 4. OSH update search strategy
#1 DC{OUCISD OR OUHSEL OR OUNIOC OR OUNIOS OR OURILO}
#2 GW{office AND inactiv*}
#3 GW{sitting OR sedentary}
#4 TW{work*}
#5 #2 OR #3
#6 #4 AND #5
#7 #1 AND #6
Appendix 5. EMBASE search strategy
#1 sedentary
#2 'sitting'/de
#3 'seated posture'
#4 seated NEAR/1 posture
#5 chair:ab,ti OR desk:ab,ti
#6 chair:ab,ti
#7 desk:ab,ti
#8 office AND inactiv*
#9 #1 OR #2 OR #4 OR #6 OR #7 OR #8
#10 'work'/de OR work
#11 work*
#12 'occupation'/de OR occupation
#13 employe*
#14 #10 OR #12 OR #13
#15 effect
#16 control
#17 evaluat*
#18 intervention*
#19 program
#20 compare
#21 #15 OR #16 OR #17 OR #18 OR #19 OR #20
#22 #9 AND #14 AND #21
#23 #22 AND [embase]/lim
#24 #23 AND [humans]/lim AND [embase]/lim
Appendix 6. PsycINFO (ProQuest)
S25 S13 AND S17 AND S24
S24 S18 OR S19 OR S20 OR S21 OR S22 OR S23
S23 compare
S22 program
S21 intervention*
S20 evaluat*
S19 control
S18 effect
S17 S14 OR S15 OR S16
S16 employe*
S15 occupation
S14 work
S13 S1 OR S2 OR S4 OR S8 OR S11 OR S12
S12 office AND inactive*
S11 S9 OR S10
S10 ab(desk)
S9 ti(desk)
S8 S6 OR S7
S7 ti(chair)
S6 ab(chair)
S5 ab(chair) OR ti(chair)
S4 seated NEAR/1 posture
S3 seated posture
S2 sitting
S1 sedentary
Appendix 7. ClinicalTrials.gov
Sitting AND Workplace
Appendix 8. World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal
Sitting AND Workplace
Data and analyses
Comparison 1.
Sit‐stand desk with or without information and counselling versus sit‐desk
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work follow‐up short‐term | 10 | 323 | Mean Difference (Random, 95% CI) | ‐100.16 [‐115.83, ‐84.48] |
| 1.1 Sit‐stand desk only | 5 | 145 | Mean Difference (Random, 95% CI) | ‐96.72 [‐126.05, ‐67.39] |
| 1.2 Sit‐stand desk + information and counselling | 6 | 178 | Mean Difference (Random, 95% CI) | ‐104.38 [‐122.81, ‐85.96] |
| 2 Mean difference in time spent sitting at work, follow‐up short‐term ‐ sensitivity analysis | 10 | 323 | Mean Difference (Random, 95% CI) | ‐100.16 [‐115.83, ‐84.48] |
| 2.1 Randomised control trials | 4 | 132 | Mean Difference (Random, 95% CI) | ‐105.19 [‐128.13, ‐82.24] |
| 2.2 Cross‐over RCT | 2 | 70 | Mean Difference (Random, 95% CI) | ‐99.11 [‐112.82, ‐85.41] |
| 2.3 Control before after studies | 4 | 121 | Mean Difference (Random, 95% CI) | ‐92.80 [‐133.13, ‐52.47] |
| 3 Mean difference in time spent sitting at work. follow‐up medium‐term (CBA) | 2 | 60 | Mean Difference (Fixed, 95% CI) | ‐57.08 [‐98.76, ‐15.41] |
| 4 Mean difference in time in sitting bouts lasting 30 minutes or more, follow‐up short‐term (CBA) | 2 | 74 | Mean Difference (Fixed, 95% CI) | ‐52.57 [‐78.79, ‐26.35] |
| 4.1 Sit‐stand desk only | 1 | 20 | Mean Difference (Fixed, 95% CI) | ‐13.00 [‐70.80, 40.80] |
| 4.2 Sit‐stand desk + information and counselling | 2 | 54 | Mean Difference (Fixed, 95% CI) | ‐63.22 [‐92.92, ‐33.51] |
| 5 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up short‐term | 2 | 56 | Mean Difference (Fixed, 95% CI) | ‐81.67 [‐123.99, ‐39.36] |
| 6 Mean difference in time spent standing at work, follow‐up short‐term | 9 | 295 | Mean Difference (Fixed, 95% CI) | 89.38 [76.44, 102.32] |
| 6.1 Sit‐stand desk only | 4 | 117 | Mean Difference (Fixed, 95% CI) | 75.78 [57.56, 94.01] |
| 6.2 Sit‐stand desk + information and counselling | 6 | 178 | Mean Difference (Fixed, 95% CI) | 103.20 [84.83, 121.58] |
| 7 Mean difference in time spent standing at work, follow‐up short‐term (RCT only) | 4 | 132 | Mean Difference (Fixed, 95% CI) | 98.65 [74.94, 122.36] |
| 8 Mean difference in time spent stepping at work follow‐up short‐term | 8 | 270 | Mean Difference (Random, 95% CI) | ‐0.52 [‐3.88, 2.85] |
| 9 Mean difference in time spent standng at work, follow‐up medium‐term (CBA) | 2 | 60 | Mean Difference (IV, Fixed, 95% CI) | 53.36 [16.59, 90.14] |
| 10 Work performance (1‐10 scale), follow‐up short‐term (CBA) | 3 | 109 | Mean Difference (Fixed, 95% CI) | 0.35 [‐0.10, 0.79] |
| 10.1 Sit‐stand desk only | 2 | 52 | Mean Difference (Fixed, 95% CI) | 0.82 [0.00, 1.63] |
| 10.2 Sit‐stand desk + information and counselling | 2 | 57 | Mean Difference (Fixed, 95% CI) | 0.15 [‐0.38, 0.68] |
| 11 Proportion with ≥ 1 sick days in the last three months (CBA) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 12 Proportion with ≥ 1 sick days in the last month (CBA) | 2 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.49, 1.21] |
| 12.1 Sit‐stand desk only | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.42, 2.13] |
| 12.2 Sit‐stand desk + information and counselling | 2 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.41, 1.24] |
| 13 Mean difference in musculoskeletal symptoms, follow‐up short‐term | 1 | 46 | Mean Difference (Fixed, 95% CI) | ‐0.51 [‐1.03, ‐0.00] |
| 14 Mean difference in musculoskeletal symptoms, follow‐up Medium‐term | 1 | 45 | Mean Difference (Fixed, 95% CI) | ‐0.54 [‐0.89, ‐0.19] |
Comparison 2.
Standing desk versus sit‐stand desk
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up short‐term | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Mean difference in time spent sitting at work, follow‐up medium‐term | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 3.
Active workstation versus sit desk
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up short‐term | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Treadmill desk plus counselling versus sit desk | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Mean difference in time spent in inactive sitting at work, follow‐up medium term | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Cycling desk + information and counselling versus information and counselling only | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4.
Walking strategies versus no intervention
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up short term | 1 | 179 | Mean Difference (Fixed, 95% CI) | ‐15.49 [‐49.65, 18.67] |
| 1.1 Route versus no intervention | 1 | 90 | Mean Difference (Fixed, 95% CI) | ‐16.0 [‐64.98, 32.98] |
| 1.2 Incidental versus no intervention | 1 | 89 | Mean Difference (Fixed, 95% CI) | ‐15.0 [‐62.66, 32.66] |
| 2 Mean difference in time spent sitting at work, follow‐up medium‐term | 1 | 264 | Mean Difference (IV, Fixed, 95% CI) | ‐16.50 [‐60.55, 27.55] |
| 3 Percentage of lost work productivity (WLQ Index Score) follow‐up medium‐term | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected |
Comparison 5.
Short break versus long break
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up short‐term | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 6.
Information, feedback and/or reminder versus information only or no intervention
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up short term | 2 | 63 | Mean Difference (IV, Fixed, 95% CI) | ‐19.23 [‐57.05, 18.58] |
| 1.1 Information and feedback versus no intervention | 2 | 63 | Mean Difference (IV, Fixed, 95% CI) | ‐19.23 [‐57.05, 18.58] |
| 2 Mean difference in time spent sitting at work, follow‐up medium‐term | 2 | 747 | Mean Difference (Fixed, 95% CI) | ‐28.38 [‐51.49, ‐5.26] |
| 2.1 Counselling versus no intervention | 2 | 747 | Mean Difference (Fixed, 95% CI) | ‐28.38 [‐51.49, ‐5.26] |
| 3 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up short‐term | 1 | Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 3.1 Information and feedback versus no intervention | 1 | 37 | Mean Difference (Fixed, 95% CI) | ‐16.40 [‐96.85, 64.06] |
| 4 Mean difference in total time spent sitting (including sitting at and outside work), follow‐up medium term | 1 | Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 4.1 Counselling versus no intervention | 1 | 416 | Mean Difference (Fixed, 95% CI) | ‐20.0 [‐85.00, 45.00] |
| 5 Mean difference in time spent standing at work follow‐up short‐term | 1 | Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 5.1 Information and feedback | 1 | 93 | Mean Difference (Fixed, 95% CI) | 10.24 [‐17.17, 37.65] |
| 6 Work engagement (0‐6 scale), follow‐up medium‐term | 1 | Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 6.1 Counseling versus no intervention | 1 | 224 | Mean Difference (Fixed, 95% CI) | 0.1 [‐0.10, 0.30] |
Comparison 7.
Prompts plus information versus information alone
Comparison 8.
Computer prompts to step versus computer prompts to stand
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up short‐term | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Mean difference in number of sitting bouts lasting 30 minutes or more, follow‐up short‐term | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Mean difference in time spent standing at work, follow‐up short‐term | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Mean difference in time spent stepping at work, follow‐up short‐term | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 9.
High personalised or contextualised information versus less personalised or contextualised information
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time in sitting bouts lasting 30 minutes or more, follow‐up short‐term | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected |
Comparison 10.
Mindfulness training versus no intervention
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean difference in time spent sitting at work, follow‐up medium‐term | 1 | 257 | Mean Difference (Fixed, 95% CI) | ‐22.69 [‐62.55, 17.17] |
| 2 Work engagement (0‐6 scale), follow‐up medium‐term | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected |
Comparison 11.
Activity tracker combined with organisational support versus organisational support only
Comparison 12.
Multi‐component intervention versus no intervention
What's new
Last assessed as up‐to‐date: 9 August 2017.
| Date | Event | Description |
|---|---|---|
| 4 April 2018 | New citation required and conclusions have changed | 'Summary of findings' tables updated |
| 4 April 2018 | New search has been performed | New studies have been incorporated into review, and new analyses have been added. |
| 9 August 2017 | New search has been performed | Searches updated |
Differences between protocol and review
We added time spent in prolonged sitting bouts (e.g. 30 minutes or more) and number of such bouts, total time spent sitting, including sitting at and outside work, time spent standing and stepping at work as new outcomes in the review. We added the number and duration of prolonged sitting bouts as outcomes because research has suggested that breaking up sitting time may be beneficial to health (Dunstan 2011). We added the total time spent sitting, including sitting at and outside work, as an outcome because reducing occupational sitting time may lead to an increase of time spent sitting in non‐occupational domains. The possibility of such compensatory effects has been described in previous papers (Gomersall 2013; Pedišić 2017). We added the amounts of time spent standing and stepping at work as outcomes because the amount of time in a 24‐hour day is fixed and every reduction of time spent sitting has to necessarily result in a proportional increase of time spent in one or more other time‐use components (Pedišić 2017). From the public health perspective it may be important to know whether time spent sitting is replaced with quiet standing, physical activity or some other movement or non‐movement related behaviour.
In the protocol we stated that in cases where we would include more than one comparison from a trial with multiple arms in the same meta‐analysis, we would halve the numbers of control group participants to prevent them from being included twice, however this does not work for the inverse variance input method. One study, Neuhaus 2014a, reported only the results from ANCOVA and could not provide us with the raw data. For this trial we modelled the means and standard deviations from the intervention and the control group in Review Manager as closely to the real data as possible to achieve the same MD and standard error. Then we halved the number of participants in the control group and entered the resulting standard errors into Review Manager.
We judged studies to be at low risk of selective outcome reporting if the final publications of the trial reported what had been planned and registered in international databases (trial registries), such as ClinicalTrials.gov, Australia New Zealand Clinical Trials Registry (ANZCTR.org.au), Netherland’s Trial Registry (NTR). We judged the studies that were not registered in trial registries as being at low risk for selective outcome reporting if they reported all the outcomes mentioned in the methods section.
Initially, we planned to pool interventions that were categorised under broad headings like physical changes in workplace environment, workplace policy changes and information and counselling, but later we found that the interventions were quite different from one another and decided not to combine them under these broad headings. We also added a new category consisting of approaches that used multiple types of interventions at the same time. Due to the large number of outcomes it was not practical to incorporate a GRADE rating of the quality of the evidence of every single result. Hence we report time spent sitting at work and time spent in sitting bouts lasting 30 minutes or more for short‐term follow‐up in the 'Summary of findings' table. Where studies reporting effects at short‐term follow‐up for the above‐mentioned outcomes were not available, we present medium‐term follow‐up. We only report the most relevant comparisons.
We also calculated a prediction interval for the outcome 'sitting time at work' for interventions comparing the effectiveness of sit‐stand desks and sit‐desks.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Non‐random allocation by clusters: CBA Single‐blind Study duration: 3 months Dropout: 9% Location: Australia Recruitment: control group participants were recruited from locations separated from the intervention group participants by at least 1 building level |
|
| Participants |
Population: employees in public health research centres within 2 academic institutions, aged 20‐65 years Intervention group: 18 participants Control group: 12 participants Demographics: BMI: intervention group 22.6 (SD 2.6) kg/m², control group 21.5 (SD 2.6) kg/m² |
|
| Interventions |
Duration: 3 months Intervention: sit‐stand desk Control: sit‐desk |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This study was funded by a University of Queensland Major Equipment and Infrastructure grant. Alkhajah was supported by a United Arab Emirates Ministry of Higher Education and Scientifıc Research Scholarship; Reeves was supported by a National Health and Medical Research Council (NHMRC) Early Career Fellowship; Eakin was supported by an NHMRC Senior Research Fellowship; Owen was supported by an NHMRC Senior Principal Research Fellowship; and Healy was supported by an NHMRC Early Career Fellowship. Authors reported no financial disclosures. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation was not done as participants in intervention and control groups were selected from different building locations. |
| Allocation concealment (selection bias) | High risk | Intervention and control groups were selected from two separate locations. However no information on allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The intervention group had sit‐stand desks installed at their workplace and received verbal instruction on their use, as well as written instructions on the correct ergonomic posture for both sitting and standing and the importance of regular postural change throughout the day. The control group had no change in desks and participants were advised to maintain usual day‐to‐day activity. The participants were probably aware of their allocation. The authors do not report who gave the instructions to the intervention and control groups. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Virtually no attrition: only one participant was missing from the control group because of a malfunctioning accelerometer‐inclinometer. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. Study protocol was not available. |
| Baseline comparability/ imbalance | High risk | Baseline data for age and gender were similar. It seems probable that there were baseline imbalances in awareness and physical activity levels between intervention and control groups as participants to the intervention group were selected from an academic institution focused on sedentary behaviour research whereas participants in the control group were never involved in physical activity research. |
| Validity of outcome measure | Low risk | The accelerometer‐inclinometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation by clusters Single‐blind Study duration: 12 months Dropout: more than 45% in both groups. Location: Australia Recruitment: participants were invited to attend an information session, during which eligibility was confirmed and informed written consent was obtained. |
|
| Participants |
Population: employees from an international property and infrastructure group, located at two cities: Sydney and Brisbane. Organisational‐support intervention (ORG) group: 9 teams with 117 employees ORG + tracker group: 9 teams with 93 employees Demographics: Mean age: ORG group: 40.0 (SD 8.0), ORG + tracker group: 37.6 (SD 7.8) % of males: ORG group 60 %, ORG+ tracker group 47 % BMI: ORG group 25.0 (SD 3.4) kg/m², ORG + tracker group 24.1 (SD 3.4) kg/m² |
|
| Interventions |
Duration: 12 months Organisational‐support intervention (ORG group): information booklet, five fortnightly emails consisting of chosen activity‐promoting tips, comments from participants or managers, images of participants taking part in the ‘Stand Up, Sit Less, Move More’ message and the organisation’s branding. ORG + tracker group: organisational support combined with activity tracker |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | The authors declared that they have no competing interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation sequence was generated using randomisation website. |
| Allocation concealment (selection bias) | Low risk | A university staff member not involved in the study randomised teams by strata (location B/small location A teams/large location A teams) to either Group ORG or Group ORG + tracker. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither the research team nor participants were blinded to participants’ randomisation status. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data were imputed by chained equations. |
| Selective reporting (reporting bias) | Low risk | All the outcomes mentioned in the protocol were reported. |
| Baseline comparability/ imbalance | High risk | Group ORG had a higher proportion of males, senior leaders and overweight participants, had fewer managers and reported more lower‐extremity musculoskeletal problems than Group ORG + tracker. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation Single‐blind Study duration: 8 months Drop out: 10% (five participants were lost to follow‐up and one discontinued the intervention). Location: USA Recruitment: participants were recruited via an electronic advertisement on the company’s well‐being website. The advertisement included a link to an online eligibility survey. Research staff contacted interested and eligible employees via telephone to schedule a baseline testing session. |
|
| Participants |
Population: healthy adults working in full‐time sedentary jobs at a large private company were invited to participate via an electronic advertisement on the company’s well‐being website. They were physically inactive, overweight/obese. Intervention group: 27 participants Control group: 27 participants Demographics: Mean age: intervention: 45.2 (SD 10.9), control 45 (SD 10.7), 70% participants were females in both intervention and control groups BMI: intervention 34.5 (SD 6.8) kg/m², control 33 (SD 5.6)kg/m² |
|
| Interventions |
Duration of intervention: 16 weeks Intervention: ergonomic workstation intervention; three activity‐promoting emails/week and access to a seated active workstation (elliptical machine, activeLife Trainer). Control: ergonomic intervention and emails only. |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | The second author, Dr Christoph Leonhard, owns propriety rights to the activeLife Trainer. No other financial disclosures were reported by the authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A 1:1 randomisation scheme was generated by the principal investigator using an online random sequence generator. |
| Allocation concealment (selection bias) | Low risk | Based on the randomisation scheme, participants were provided a sealed envelope indicating their treatment assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The envelope was provided by a research assistant who was previously unaware of the randomisation schedule, but the participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 54 of the 60 participants completed all assessments. Five were lost to follow‐up and one discontinued the intervention thus yielding a total attrition of 10%. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. |
| Baseline comparability/ imbalance | Low risk | Mean age: intervention: 45.2 (10.9), control 45 (10.7), 70% participants were females in both intervention and control groups, BMI: intervention 34.5 (6.8) kg/m², control 33 (5.6)kg/m² |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation with cross‐over and wait‐list control Participants were allocated randomly by drawing from the ballot four at a time. The first four were allocated to intervention group and next four to control group for four weeks. The remaining participants were assigned to the wait‐list control condition and were placed on the waiting list in seven groups (four to five people per group). After the initial four weeks, the previous control group received the intervention with the next group from the ballot draw serving as their controls. This was repeated until all nine groups had received the intervention. Unblinded Study duration: 9 weeks Dropout: 7% Location: Australia Recruitment: project was advertised to staff as part of their workplace wellness program via internal mail, staff meetings and information fliers in the office. Staff members who were interested in participating contacted the research team and received additional project information and an expression of interest form. They could then join the study ballot by returning the expression of interest form. |
|
| Participants |
Population: staff from a non‐government health agency in New South Wales, Australia Demographics: BMI (kg/m²): underweight (< 18.5): 13%, normal range (18.5–24.9): 50%, overweight (25–29.9): 25%, obese (≥ 30): 13% |
|
| Interventions |
Duration of intervention: 9 weeks Intervention: sit‐stand desk Control: no sit‐stand desk |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This research was supported by funding from Heart Foundation New South Wales, and Australian National Health and Medical Research Council Program Grant (#569940). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly drawn from a ballot by a researcher in the presence of potential participants and other researchers. Participants were allocated to the intervention group, control group and wait‐list control condition. |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not possible due to the open plan nature of the study office environment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Research staff, participants, and assessors were not blinded to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Three participants who were missing age or BMI values were not included in the analyses. Imputing values for these missing covariate values did not influence the effect of the intervention on the adjusted estimates for the outcomes, nor did it change the effects age or BMI had on the outcome. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | Since the trial used a cross‐over design, all the participants would receive the interventions at some point. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Non‐random allocation: CBA Single‐blind Study duration: 20 weeks Dropout: 22% Location: Australia Recruitment: the research team gave a presentation about the study to team leaders and managers, who then discussed the study with their staff. Participants joined the study by returning a signed consent form to the researchers. |
|
| Participants |
Population: customer care (call centre) staff from two teams working at one worksite of a large telecommunications company in Sydney, Australia. Intervention group: 16 participants Control group: 15 participants Demographics: Mean age: control 35.1 (SD 11.5), intervention 31.0 (SD 10.0) The intervention group had higher BMI than control group. |
|
| Interventions |
Duration: 19 weeks Intervention: sit‐stand desk + email reminders Control: no sit‐stand desk |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | A co‐author, Amanda Sainsbury has received payment from Eli Lilly, the Pharmacy Guild of Australia, Novo Nordisk, and the Dietitians Association of Australia for seminar presentations at conferences. She is also the author of The Don’t Go Hungry Diet (Bantam, Australia, and New Zealand, 2007) and Don’t Go Hungry For Life (Bantam, Australia, and New Zealand, 2011). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation was not performed. |
| Allocation concealment (selection bias) | High risk | Allocation was not concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither the research team nor participants were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Low participant adherence to activity monitor use and device malfunction resulted in high attrition rates. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. Study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | Both groups were comparable at baseline for age, sex and BMI. |
| Validity of outcome measure | Low risk | The accelerometer and Occupational Sitting and Physical Activity Questionnaire (OSPAQ) are valid tools for the measurement of sitting time. |
| Methods | Random allocation by clusters Single‐blind Location: Amsterdam, the Netherlands Recruitment: a top‐down communication approach was used, starting with the management • An explanatory meeting with team leaders • Invitation to all employees from the department to participate in the study • Data on sick leave, salary and the duration of employment was obtained through the Human Resource Management department |
|
| Participants |
Population description: office employees (18 years or above), working at the Dutch financial service provider Demographics: Age in years: group motivational interviewing (GMI) 43.6 (SD 10.3); environmental modification 42.2 (SD 10.5); GMI + environmental modification 38.0 (SD 10.5); no intervention 40.7 (SD 9.2) Male [n (%)]: GMI 73 (SD 61.9); Environmental modification 60 (SD 62.5); GMI + Environmental modification 51 (SD 55.4); no intervention 65 (SD 61.3) |
|
| Interventions |
Duration of intervention: environmental modification: 12 months and GMI: 3.5 months The Be Active & Relax program was evaluated using 4 arms: • GMI (group motivational interviewing) and environmental modifications (3 clusters 92 employees); GMI derived from Motivational Interviewing (MI). MI is a counselling style that stimulates behavioural change by focusing on exploring and resolving ambivalence. A group setting has several benefits, e.g. sharing experiences, providing feedback and giving support. • Environmental modifications (3 clusters; 96 employees): 1) the VIP Coffee Corner Zone – the coffee corner was modified by adding a bar with bar chairs, a large plant and a giant wall poster (a poster visualizing a relaxing environment, e.g. wood, water and mountains); 2) the VIP Open Office Zone – the office was modified by introducing exercise balls and curtains to divide desks in order to reduce background noise; 3) the VIP Meeting Zone – conference rooms were modified by placing a standing table (a table that allows you to stand while working) and a giant wall poster (as before); and 4) the VIP Hall Zone ‐ table tennis tables were placed and lounge chairs were introduced in the hall for informal meetings. In addition, footsteps were placed on the floor in the entrance hall to promote stair walking. • GMI (7 cluster; 118 employees); • No intervention or control group (6 cluster; 106 employees) |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was executed by an independent researcher by using a computer generated list from SPSS. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of the participants and intervention providers for the social environmental intervention was impossible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incompleteness of the data is taken into account with the multilevel analysis. Loss to follow‐up at 6 months was considerable (> 20%). However, there were no significant differences at baseline between responders and non‐responders. |
| Selective reporting (reporting bias) | Low risk | All mentioned outcomes in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | No differences regarding age, gender, education, marital status, ethnicity, working hours, general health, job demands, supervisor support. Males were slightly over‐represented. |
| Validity of outcome measure | High risk | Validity of the questionnaire used in the study has not been tested. |
| Methods | Random allocation by clusters Single‐blind Study duration: 3 months Dropout: Location: Denmark Recruitment: recruited through a press release and an open invitation in an electronic newsletter aimed at practitioners and health workers in municipalities and private workplaces all over Denmark |
|
| Participants |
Population: practitioners and health workers in municipalities and private workplaces all over Denmark Intervention group: 173 participants in 10 offices Control group: 144 participants in 9 offices Demographics: Mean age: intervention 46 (SD 10), control 45 (SD 11) % of females: intervention 61%, control 73% BMI: intervention group 26 (SD 5.0) kg/m², control group 27 (SD 4.8) kg/m² |
|
| Interventions |
Duration: 3 months Intervention: a multi‐component work‐based intervention (ambassadors, environmental changes, lecture, workshop, emails and texts). Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | Funded by Tryg Fonden, Denmark. The funders had no role in study design, data collection or analysis, decision to publish or preparation of the manuscript. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A senior researcher carried out the randomisation, using random number sequence in Stata |
| Allocation concealment (selection bias) | Low risk | Randomisation took place before baseline measurements were recorded, but allocation was not disclosed to participants, researchers or data collectors until the baseline assessments had been completed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The researchers were not blinded at follow‐up. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A blinded version of the data was used for data management and analysis. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Final levels of missing data on primary outcomes were 9% at baseline, 15% at 1‐month follow‐up and 20% at 3‐ months follow‐up. however missing data were imputed by multiple imputations using chained equations. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the study protocol has been reported. |
| Baseline comparability/ imbalance | Low risk | Both groups were comparable at baseline for age, sex and BMI. |
| Validity of outcome measure | Low risk | ActiGraph GT3X accelerometer is a valid instrument for assessing physical activity and sedentary behaviour |
| Methods | Random allocation by clusters Single‐blind Study duration: 3 months Dropout: Location: Belgium Recruitment: employees were invited to participate by email |
|
| Participants |
Population: employees of 2 companies (a university and an environmental agency) in Flanders Intervention group: tailored group: 78 participants (2 departments), Generic group: 84 participants (2 departments) Control group: 51 participants (2 departments) Demographics: Age in years: tailored 40.5 (SD 8.6), generic 40.7 (SD 9.7), control 39.3 (SD 9.0) % of males: tailored 32%, generic 27%, control 15% % of participants with high school/university education: tailored 58%, generic 70%, control 46% BMI: tailored 24.2 (3.1) kg/m², generic 23.6 (SD 3.5) kg/m², control group 23.7 (SD 3.5) kg/m² |
|
| Interventions |
Duration: 3 months Intervention: tailored group: personalised computer‐tailored feedback about sitting time, including tips and suggestions on how to interrupt (taking short standing breaks) and reduce (replacing sitting by periods of standing) sitting, and in the end motivated participants were invited to create an action plan to convert intentions into specific actions. Generic group: generic information on the importance of reducing and interrupting sitting Control: usual lifestyle |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Self‐reported changes in sitting (total sitting, sitting at work, domains of leisure sitting) measured at 3 months |
|
| Notes | The first author is supported by the Research Foundation Flanders (FWO) (postdoctoral research fellowship: FWO11/PDO/097). Authors declared no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 10% participants were lost to follow‐up in each comparison groups. |
| Selective reporting (reporting bias) | High risk | Not every outcome mentioned in the study protocol has been reported. |
| Baseline comparability/ imbalance | Low risk | The comparison groups did not differ in sociodemographic, work‐related, and health‐related variables. |
| Validity of outcome measure | Low risk | The WSQ has acceptable reliability (interclass correlation coefficient = .63) and validity against objectively accelerometer‐measured sitting time (r = .34 to r = .45). |
| Methods | Random allocation by minimization Single‐blind Study duration: 12 weeks Drop out: 8% Location: Switzerland |
|
| Participants |
Population: staff from the confederate Swiss health insurance company EGK Intervention: 15 participants Control: 16 participants Demographics: Age: intervention: 45 (SD 12), control: 40 (SD10) Sex (m/f): intervention 4/11, control 4/12 BMI (kg/m²): Intervention: 23.7 (SD 3.7), control: 24.7 (SD 5) |
|
| Interventions |
Duration of intervention: 12 weeks Intervention: computer prompt + information Control: information only |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | Authors reported no conflict of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group assignment was randomly conducted according to the minimization method: age, gender, BMI, physical activity and working time served as strata criteria in order to minimize group differences in demographical variables. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Testing personnel were blinded to group allocation. Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3 participants in the control group and 4 participants in the intervention group withdrew due to job changes and illness (8% of participants). They were not included in the analysis (i.e. no intention‐to‐treat analysis). |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. Study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | Group differences were minimized. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation with cross‐over Unblinded Study duration: 10 weeks Dropout: 1231 working hours data were missing Location: USA Recruitment: a word‐of‐mouth search was performed for finding interested companies to host the study and Caldrea Inc. volunteered. A recruitment presentation was made at an all‐employee meeting (n ˜ 50) and was followed a few days later by enrolment interviews. |
|
| Participants |
Population: employees of Caldrea Inc. company, USA Demographics: average age: 40.4 years; out of 28 participants, 19 were female |
|
| Interventions |
Duration of intervention: 4 weeks Intervention: sit‐stand desk Three different models of desks were used: Workfit‐S, a setup that attaches to the front of one’s existing desk that can hold the computer monitor, keyboard and mouse; Workfit‐A, a setup that is identical to Workfit‐S but attaches to the back of one’s existing desk; and Workfit‐D, a whole desk that is easily moved up and down. The Workfit‐A and S also came with an added work‐surface and all three types of desks came with anti‐fatigue floor mats for comfort during standing. Control: no sit‐stand desk |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Sitting time, standing time, and light activity at work self‐reported and objectively assessed with accelerometer‐inclinometer Self‐reported energy and relaxation levels |
|
| Notes | James A. Levine has patents in accelerometer algorithms with Gruve Technologies Inc. but he did not access or analyse the raw the data from the Gruve device. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned to receive the intervention during period 1 or period 2, using a 1:1 allocation in 1 block of 35, using Microsoft Excel 2007. |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not possible due to the nature of the intervention. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel was not possible due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | If we assume a person works for 40 hours per week, then for 28 participants the working hours will be 8960 hours for 8 weeks (4 weeks intervention and 4 weeks control period). However the study reported only 7,729 working hours based on accelerometer data. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | There were no significant differences in age or BMI between interventions and control groups. Most of the participants were female. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation Unblinded Study duration: 12 weeks No dropouts Location: Germany Only part of the study was presented as all the data have not been analysed. |
|
| Participants |
Population: desk‐based employees at VDU workplaces Demographics: mean age (years): 40.7 (range 24 to 58), control 42.1 (range 25 to 61) 4 female participants in both intervention and control groups Mean BMI: 26.3 (SD 3.2) kg/m² |
|
| Interventions |
Duration of intervention: 12 weeks Intervention
Control: usual office work |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This project was initiated and funded by the German Social Accident Insurance (DGUV). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Following correspondence with the authors, they replied: "Randomization by computer generated list". |
| Allocation concealment (selection bias) | Low risk | Following correspondence with the authors, they replied: "our secretary, who was not involved in the project, generated the allocation list". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Following correspondence with the authors, they replied: "The participants were blinded, the personnel was not blinded (they knew according to the subject code, who belongs to the Intervention group and to the Control group)". |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. |
| Baseline comparability/ imbalance | Low risk | Participants were recruited from different VDU workplaces. No significant difference in age of participants between intervention and control groups. 4 female participants in both intervention and control groups. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation: RCT Single‐blind Study duration: 10 days Dropout: 7% Location: United Kingdom Recruitment: healthy working adults who could stand unassisted recruited via poster and email |
|
| Participants |
Population: healthy adults working in an office at Glasgow Caledonian University in Scotland Intervention group: 14 participants (computer prompts (CP)) Control group: 14 participants (education) Demographics: CP group (mean age 49 (SD 8 years) were older than the education group (mean age 39 (SD 10) years), predominantly female (11 in CP group and 11 in education group), worked as administrators (4 in CP group and 3 in education group), researchers (5 in CP group and 7 in education group), lecturers (5 in CP group and 4 in education group) BMI: CP group 23.7 (SD 3.5) vs. education group 23.6 (SD 2.8) |
|
| Interventions |
Duration of intervention: 5 days but the participants were followed up for 10 days. Intervention: CP + information Control: information only (a short educational talk) All participants received a short educational talk regarding the health risks of prolonged sitting stating that standing every 30 minutes could be beneficial, and a short information leaflet was also provided. Then participants in the intervention group had a prompting software installed in their personal computer to remind them to take a break for 1 min every 30 minutes. |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Assessed with thigh‐mounted accelerometer‐inclinometer
|
|
| Notes | This study was funded by the School of Health, Glasgow Caledonian University and formed the dissertation project for Masters of Rehabilitation Science of Rhian Evans, Henrietta Fawole, and Stephanie Sheriff. No financial support was received from any commercial company. No financial disclosures were reported by the authors of this publication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generation was used. |
| Allocation concealment (selection bias) | Low risk | Information on the group assignment was placed into sequentially numbered sealed opaque envelopes. The researcher was involved in opening the envelope immediately after the education. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Both the researcher and participants were aware of the allocation. Awareness of the purpose of the study may have led the education group participants to behave differently during the study, which may have affected the outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Data treatment was conducted by a researcher blinded to the allocation of the participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 participants were excluded from analyses due to incomplete data: 1 from the CP group and 1 from the education group. As the same proportion of participants were excluded from both groups, the missing data did not have much impact on outcomes. |
| Selective reporting (reporting bias) | High risk | Not all outcomes mentioned in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | CP group (mean age 49 (SD 8) years) was older than the education group (mean age 39 (SD 10) years), participants worked as administrators (4 in CP group, 3 in education group), researchers (5 in CP group, 7 in education group), or lecturers (5 in CP group, 4 in education group) and were predominantly female (11 in CP group, 11 in education group) |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Non‐random allocation Unblinded Study duration: 6 months Dropouts: 49% Location: University of Jyväskylä, Finland Recruitment: all faculty employees (n = 170) were invited to fill out a questionnaire between August and September 2012 and again in February 2013. |
|
| Participants |
Population: healthy adults working in a university setting: researchers, teachers, administrative workers, assistants, professors and technical workers. Intervention group: 24 participants Control group: 21 participants Demographics: mean age: intervention 47.8 (SD 10.8) years, control 39 (SD 8.5) years. 70.8% were females in the intervention group and 81% were females in the control group. BMI (kg/m²): intervention: 24.8 (SD 3.9), control: 23.3 (SD 3.8) |
|
| Interventions |
Duration of intervention: 6 months Intervention: sit‐stand desk Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | The study was funded by the China Scholarship Council (201206320092). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The study did not employ randomisation. Part of the personnel moved to a renovated building with sit‐stand desks. |
| Allocation concealment (selection bias) | High risk | Allocation was not concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The questionnaire was returned by 92 employees at baseline, before working at sit–stand desks, and 61 employees after 6 months. Those who completed the questionnaire only once were excluded, leaving 45 individuals who were included in the analysis. The study lost 49% participants during follow‐up. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the protocol were reported. |
| Baseline comparability/ imbalance | High risk | In the intervention group participants were older and had more experience of office work. 70.8% were females in the intervention group and 81% were females in the control group. BMI (kg/m²): intervention: 24.8 (3.9), control: 23.3 (3.8) |
| Validity of outcome measure | High risk | Validity of the questionnaire used in the study has not been tested. |
| Methods | Random allocation Unblinded Study duration: 10 weeks Dropout: 16% Location: UK, Australia and Spain Recruitment: participants came from 3 major regional universities in 3 countries, represented by a lead investigator in each university, who had expressed an interest in running an employee intervention at their respective university as part of an evolving, international project. |
|
| Participants |
Population: white‐collar (i.e. professional, managerial, or administrative) university staff from the UK (n = 64), Australia (n = 70) and Spain (n = 80) Intervention groups:
Control group: 60 participants Demographics: mean age (years): route walking group 42.1 (SD 9.2); incidental walking group 41 (SD 9.7), control group 40.8 (SD 11.4) Women were predominant in all 3 groups Mean BMI (kg/m²): route walking group 25.1 (SD 4), incidental walking group 25.4 (SD 4.3), control group 24.2 (SD 3.8) |
|
| Interventions |
Duration of intervention: 10 weeks Interventions: walking strategies (route and incidental walking) Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | Authors declared that they had no competing interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pre‐intervention workday step counts and block stratification were used to assign participants at each site randomly and equally to a waiting list control or one of two intervention groups. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | From a potential sample size of 214 participants, 16% (n = 35) had missing data at pre‐intervention or 2 or more intervention measurement points. These data were removed prior to analyses, resulting in a final sample size of n = 179. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | Age was not significantly different between groups: 42.1 (SD 9.2) years in the route walking group; 41 (SD 9.7) years in the incidental walking group and 40.8 (SD 11.4) years in the control group. Study participants were predominantly women. All participants were white collar workers (i.e. professional, managerial, or administrative). |
| Validity of outcome measure | Low risk | Paper‐based diaries were used to report sitting time at work. |
| Methods | Random allocation Unblinded Study duration: 10 weeks Dropout: 14% Location: USA Recruitment: strategically placed fliers posted around the Arizona State University Downtown Phoenix Campus, email advertisements delivered to employees through the Employee Wellness Committee, and word of mouth. |
|
| Participants |
Population: currently employed adults with predominantly sedentary occupations working in the Greater Phoenix area in 2012‐2013 Intervention group: 12 participants Control group: 10 participants Demographics: Mean age: intervention 44.2 (SD 12.5), control 47.2 (SD 13.5) 50% females in both groups BMI: intervention 24.1 (SD 3) kg/m², control 30.6 (SD 5) kg/m² Intervention group composed of significantly more “official and managerial level” individuals. |
|
| Interventions |
Duration of intervention: 10 weeks Intervention: one orientation to walking workstation, 5 bi‐weekly newsletters, specifically targeting workplace sitting behaviours, 5 bi‐weekly FAQ’s and access to study website for intervention content, latest sedentary behaviour research and links for tools for decreasing sitting time at work. Control: health education |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Sitting time/workday (minutes/8‐hour workday) measured by accelerometer‐inclinometer. Participants were also asked to complete a daily log to determine work schedule and verify obtained inclinometer and accelerometer data |
|
| Notes | Thesis presented in partial fulfilment of the requirements for the degree Master of Science. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation was decided by tossing a coin. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant from both groups withdrew, due to busy schedule; 1 participant from both groups was excluded due to device malfunction; and 1 participant from the control group was excluded due to refusal to wear accelerometer. Intention‐to‐treat analysis was followed for data analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. Study protocol was not available. |
| Baseline comparability/ imbalance | High risk | Intervention group composed of significantly more “official and managerial level” individuals. Age of participants in the control group was 47.2 (SD 13.5) and in the intervention group was 44.2 (SD 12.5). There were 50% females in both groups. There was significant difference in BMI of participants between intervention and control groups. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation Unblinded Study duration: 8 weeks Dropout: 4% Location: UK Recruitment: consent was sought from 11 departmental managers for employee recruitment. All employees in consenting departments received an overview of the study and participant information sheet, and were invited to a study information session via an email from the research team. |
|
| Participants |
Population: office workers from one organisation (Liverpool John Moores University, Liverpool, UK). Employees within the approached departments were predominantly administrative staff. Intervention group: 26 participants Control group: 21 participants Demographics: Mean age: intervention 38.8 (SD 9.8) years, control 38.4 (SD 9.3) years 89% in intervention group and 67% in control group were females BMI (kg/m²): intervention 67.4 (SD 13.8), control 70.5 (SD 16.4) |
|
| Interventions |
Duration of intervention: 8 weeks Intervention: sit‐stand desk combined with face‐to‐face training and ergonomic information. Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | Ergotron Ltd provided the sit‐stand desks but had no involvement on the provenance, commissioning, conduct or findings of the study. No other financial disclosures were reported by the authors of this paper. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised using a randomised block design and random number table. |
| Allocation concealment (selection bias) | High risk | One member of the research team assigned the participants to a treatment arm, based on a design and table with alternating scheme. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Researchers were aware of the allocation and participants may have also been aware of the allocation due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The authors conducted a per‐protocol analysis and excluded participants from analyses for outcomes to which they did not contribute data. For workplace sitting, standing and walking, the per‐protocol analysis was compared with an intention‐to‐treat analysis, as a sensitivity analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. |
| Baseline comparability/ imbalance | Low risk | Groups were comparable at baseline except for a higher proportion of women in the intervention group (89% versus 67% in the control group). |
| Validity of outcome measure | Low risk | Ecological Momentary Assessment diaries were used to report sitting time at work. |
| Methods | Non‐random allocation by clusters (floor): CBA Unblinded Study duration: 3 months Dropout: 14% Location: Melbourne, Australia Recruitment: an invitation email was sent to all potential participants to attend one of two 30‐minute study information sessions delivered by research staff. Participants who subsequently expressed interest were screened via telephone for eligibility. |
|
| Participants |
Population: from a single workplace (Comcare: the government agency responsible for workplace safety, rehabilitation and compensation for Australian government workplaces) in metropolitan Melbourne, Australia Intervention group: 19 participants Control group: 19 participants Demographics: mean age 42.4 (SD 10.6) years in the intervention group and 42.9 (SD 10.3) years in the control group Women were predominant in the intervention group and men were predominant in the control group. Mean BMI (kg/m²): intervention group 27.5 (SD 6.1); control group 26.2 (SD 4.6) |
|
| Interventions |
Duration of intervention: 4 weeks Intervention: the intervention communicated 3 key messages: “Stand Up, Sit Less, Move More” and had the following components:
Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This study was funded by an NHMRC project grant and the Victorian Health Promotion Foundation. Ergotron provided the height‐adjustable desks (www.ergotron.com). No financial disclosures were reported by the authors and the authors declared that there were no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation was not done. |
| Allocation concealment (selection bias) | High risk | Allocation into groups was by floor, with intervention participants (primarily administrative staff) working on the floor above the control participants (predominantly senior administrative staff). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Research staff, participants, and assessors were not blinded to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Assessors were not blinded to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 participants, 2 each from the intervention and control groups withdrew and 2 further participants, 1 each from the intervention and control groups were lost during follow‐up. As the same proportion of participants were excluded from both groups, the missing data did not have much impact on outcomes. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | There were more women in the intervention group than in the control group. The mean age of both groups was similar. All participants were recruited from a single workplace in metropolitan Melbourne, Australia. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation by clusters Single‐blind Study duration: 3 months Dropout: 12 months Location: Australia Recruitment: an information session about the study was presented for consenting teams within each site, with summary material also provided via e‐mail. Employees within these participating teams were then screened by telephone for eligibility. |
|
| Participants |
Population: staff from the department of human services (a large Australian Government organisation), desk‐based office workers Intervention group: 7 worksites, 164 participants Control group: 7 worksites, 144 participants Demographics: Mean age in years: intervention 44.6 (SD 9.1), control 47.0 (SD 9.7) % females: intervention 65.4%, control 72.6% BMI: intervention group 28.61 (SD 6.46) kg/m², control group 28.61 (SD 5.48) kg/m² |
|
| Interventions |
Duration: 3 months Intervention: multicomponent intervention composed of organisational (Consultation workshop, tailored email messages to promote organisational strategies by team champions) environmental (dual screen sit‐stand desk), and individual‐level strategies and targeted change at both the individual and the cluster levels (face to face coaching and telephone calls by study‐trained health coaches). Control: usual practice |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done by generating a randomisation plan for up to 24 clusters in one block |
| Allocation concealment (selection bias) | High risk | Participants and study staff were unblinded to group allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Randomisation was performed by a research staff member not involved in recruitment or data collection. However no information on blinding of participants. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The sensitivity of results were assessed by using multiple imputation by chained equations. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the protocol section were reported. |
| Baseline comparability/ imbalance | Low risk | There were more females in the intervention group compared to control group. Both groups were comparable in terms of age and BMI. |
| Validity of outcome measure | Low risk | activPal accelerometer is a valid instrument for assessing physical activity and sedentary behaviour. |
| Methods | Non‐random allocation Study duration: 6 months Drop outs: 47% Location: United States Recruitment: participants were contacted by email with an invitation to participate in the study |
|
| Participants |
Population: call centre workers in a company (healthways) in USA. Healthways Inc., a well‐being improvement company with headquarters in Franklin, Tennessee, has multiple call centres in which their Health Coaches, Clinicians (Nurses and Dieticians), and Customer Service Representatives work. Intervention: sit‐stand desks (45 participants0, standing desks(46 participants) Control: seated (47 participants) Demographics: mean age in years: sit‐stand 34.8 (SD 11.5), standing 28.9 (6.8), seated 35 (SD 13.2) % female participants: sit‐stand 71%, standing 59%, seated 70% BMI: sit‐stand 29 (SD 9.13), standing 26.8 (SD 5.5), seated 27.8 (SD 5.7) |
|
| Interventions |
Duration of intervention: 6 months Sit‐stand desk vs. standing desk |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | Data for seated group not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Likely not random and it may be that people swapped desks because of open design of call centre. |
| Allocation concealment (selection bias) | High risk | Assignment to the workstation type was dependent on Healthways, and it made assignments as random as possible. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout (47% attrition) |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | Mean age of participants was higher for sit‐desk (control) group. Both groups were comparable at baseline for gender and BMI. |
| Validity of outcome measure | Unclear risk | The armband accelerometer (SenseWear model) is a valid instrument for assessing physical activity and sedentary behaviour |
| Methods | Random allocation Single‐blind Study duration: 5 weeks Dropout: 18% Location: Australia Recruitment: employees were invited to participate through internal email communication. |
|
| Participants |
Population: employees from the Health Promotion Unit (HPU) of a local health district in the Sydney metropolitan region. Control group: Group 1 (10 participants) Intervention group: Group 2 with 8 participants, Group 3 with 7 participants, Group 4 with 7 participants Demographics: BMI: intervention group 22.6 (SD 2.6) kg/m², control group 21.5 (SD 2.6) kg/m² |
|
| Interventions |
Duration: 4 weeks Control: Group 1 usual seated work Intervention: sit‐stand desk: Group 2 alternated between 40 minutes sitting and 20 minutes standing, Group 3 alternated between 30 minutes sitting and 30 minutes standing, Group 4 alternated between 20 minutes sitting and 40 minutes standing; in addition all intervention group received email reminders |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | Authors reported no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were assigned identification codes that were randomised using permuted blocks with block size 8 and 4. |
| Allocation concealment (selection bias) | Low risk | Group allocation sequence was generated by a study investigator who was not involved in data analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding participants or all members of the research team to group allocation was not possible due to the nature of the trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The researcher conducting the data analysis was blinded to the group allocation of participants until analyses were completed. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7 participants in intervention and 1 in control group lost to follow‐up (25% attrition rate). |
| Selective reporting (reporting bias) | High risk | All outcomes mentioned in the study protocol were not reported. |
| Baseline comparability/ imbalance | Low risk | Intervention and control group were comparable for age, sex and BMI at baseline. |
| Validity of outcome measure | Low risk | activPal accelerometer is a valid instrument for assessing physical activity and sedentary behaviour |
| Methods | Random allocation Single‐blind Study duration: 3 months Dropout: 11% Location: Australia Recruitment: through posters and word‐of‐mouth |
|
| Participants |
Population: full‐time desk‐based employees in the Charlottetown area. Intervention group: 16 participants Control group: 12 participants Demographics: Mean age in years: intervention 43.2 (SD 9.7), control 48.9 (SD 11.4) BMI: intervention group 36.5 (SD 9) kg/m², control group 34.6 (SD 7) kg/m² |
|
| Interventions |
Duration: 3 months Intervention: sit‐stand desk Control: no sit‐stand desk |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | The project was supported by StepsCount, Inc | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned via coin flip to intervention and control group. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Four participants were excluded from analysis (14% attrition). |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the study protocol were reported. |
| Baseline comparability/ imbalance | High risk | Participants in the control group were older (48.9 years, SD 11.4) than the intervention group (43.2 years, SD 9.7) and the intervention group had higher BMI (36.5 kg/m2, SD 9) than the control group (34.6 kg/m2 SD 7). |
| Validity of outcome measure | Low risk | activPal accelerometer is a valid instrument for assessing physical activity and sedentary behaviour |
| Methods | Random allocation Single‐blind Study duration: 9 weeks Dropout: 22% Location: United States Recruitment: university email lists and flyers distributed at local businesses. |
|
| Participants |
Population: university employees in office settings with set hours (8:00 a.m.‐5:00 p.m.) but not set break schedules Long break group: 25 participants Short break group: 24 participants Demographics: Mean age in years: long break: 38.92 (SD 7.88), short break: 38.50 (SD8.67) All participants were females and 60% of them were obese |
|
| Interventions |
Duration: 8 weeks Long break (LB) vs. short break (SB) |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised to the SB or LB group using a random digit generation Microsoft Excel. |
| Allocation concealment (selection bias) | Low risk | Participants were randomised to the SB or LB group, by an investigator not involved with testing. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded to their treatment group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Total 11 employees (22.4%) dropped out over 8 weeks. No ITT analysis |
| Selective reporting (reporting bias) | Low risk | All the outcomes mentioned in the protocol were reported. |
| Baseline comparability/ imbalance | High risk | Participants assigned to the LB group had higher total cholesterol (P = 0.02) and fewer minutes of sedentary time per workday (P = 0.05) at baseline than participants assigned to the SB group |
| Validity of outcome measure | Low risk | Actigraph GT3X accelerometer is a valid instrument for assessing physical activity and sedentary behaviour. |
| Methods | Allocation by clusters, 2 groups randomly and 2 group non‐randomly: CBA Unblinded Study duration: 3 months Dropout: 13.6% Location: University of Queensland, Brisbane, Australia Recruitment: a recruitment email explaining the study's purpose and procedures was sent to all staff from consenting units. Interested employees emailed the project manager and were interviewed via telephone to assess eligibility. |
|
| Participants |
Population: desk‐based office workers located on the same office floor, aged between 20–65 years from 3 different campuses Intervention group:
Control group: 13 participants Demographics: mean age in the multi component group was 37.3 (SD 10.7) years, 43 (SD 10.2) years in the workstation only group, and 48 (SD 11.6) years in the control group. There were no men in the multi component group, 3 in the workstation only group, and 4 in the control group. |
|
| Interventions |
Duration of intervention: 3 months Interventions:
Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) All outcomes were assessed at 3‐month follow‐up
|
|
| Notes | Funding source: Australian Postgraduate Award Scholarship, UQ School of Population Health Top‐Up Scholarship and research student funding, Queensland Health Core Infrastructure Funding, and UQ Major Equipment and Infrastructure and NHMRC Equipment Grant. Height‐adjustable workstations were provided by Ergotron. No other financial disclosures were reported by the authors. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The 2 units that were located closer to the research centre were randomised to the intervention arms and the more distant unit was allocated to the control arm. No further information provided on the method used to generate the random sequence. |
| Allocation concealment (selection bias) | High risk | The faculty staff were allocated to the multi component group, department staff were allocated to the workstation only group and campus staff were allocated to the control group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The participants and personnel knew the group to which they had been allocated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 25% of participants were lost in the sit‐stand desk plus counselling group, and one participant, i.e. 7% each, in of the other two groups. The high attrition of participants from the sit‐stand desk plus counselling group will have affected the outcome. |
| Selective reporting (reporting bias) | High risk | Not all the outcomes mentioned in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | All the participants had desk‐based jobs at the University of Queensland in Brisbane, Australia. The mean age in the multi component group was 37.3 (SD 10.7) years, in the workstation only group it was 43 (SD 10.2) years, and 48 (SD 11.6) years in the control group. There were no men in the multi component group, 3 in the workstation only group, and 4 in the control group. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation Unblinded Study duration: 13 weeks No dropouts Location: Tasmania, Australia |
|
| Participants |
Population: chosen from 460 desk‐based Tasmania Police employees across several metropolitan sectors Intervention group: 17 participants Control group: 17 participants Demographics: mean age: intervention group 41.5 (SD 12.39) years, control group 43.88 (SD 9.65) years |
|
| Interventions |
Duration of intervention:13 weeks Intervention: computer prompts Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Published: daily workplace energy expenditure (calories/workday) for different activities estimated from occupational physical activity questionnaire at 13 weeks vs. baseline Unpublished: self‐reported time spent sitting at work (minutes/day) at 13 weeks |
|
| Notes | This research was launched through a research partnership between the Tasmania State Police Department and the University of Tasmania; funded by the Tasmanian government’s Healthy@Work grant scheme. The authors report no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Following correspondence with the authors, they replied: "We used a random numbers generation software through the web". |
| Allocation concealment (selection bias) | High risk | Following correspondence with the authors, they replied: "The researchers did randomisation, so we did not blind to the allocation". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Following correspondence with the authors, they replied: "Since it was field based, participants were not blind to the treatment groups". |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no drop outs or exclusion of data. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. A study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | All participants were employees of the Tasmania police department. Age was not significantly different between groups: 41.5 (12.4) years in the intervention group, and 43.88 (9.6) years in the control group. |
| Validity of outcome measure | Low risk | Occupational Sedentary and Physical Activity Questionnaire (OSPAQ) which had moderate validity was used for assessing time spent sitting at work. |
| Methods | Non‐random allocation: CBA Study duration: 6 months Dropout: 45% Location: United States Recruitment: email from human resource department of company |
|
| Participants |
Population: employees of a call centre company in the Eastern United States. Intervention group: sit‐to‐stand (45 participants) and standing (46 participants) Control group: seated (47 participants) Demographics: Mean age in years: sit‐stand group: 34.8 (SD 11.5), stand group: 28.9 (SD 6.8), seated group: 35.0 (SD 13.2) % of females: sit‐stand group 71.1%, stand group 58.7%, seated group 70.2% BMI: sit‐stand group 29.0 (SD 9.13) kg/m², stand group 26.8 (SD 5.5) kg/m², seated group 27.8 (SD 5.7) kg/m² |
|
| Interventions |
Duration: 3 months Sit‐to‐stand vs. standing vs. seated workstation |
|
| Outcomes |
Outcome name, measurement time (units of measurement)
|
|
| Notes | Authors have not reported post intervention values for seated control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | While not completely random, management did their best to randomise employees between the workstation conditions. The call centre layout and team make‐ups consisted of groups of four to eight workstations. Because of this, and the arrangement within the facility, management kept the type of workstation within each group constant. |
| Allocation concealment (selection bias) | High risk | Not reported but based on above quote, unlikely the allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout rate at three months (30%) and six months (45%) follow‐up times. No ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All the outcomes mentioned in the methods section were reported |
| Baseline comparability/ imbalance | High risk | Age and sex is significantly different where persons using a standing workstation were 5 years younger and had more men. Also many more in this group were ‘health coaches’ and fewer were in customer services. |
| Validity of outcome measure | Low risk | The questionnaire used to assess activity outcomes in this study were based on the International Physical Activity Questionnaire (IPAQ), and the Modified Occupational Sitting and Physical Activity Questionnaire (OSPAQ) |
| Methods | Random allocation Study duration: 13 days Dropout: 32% Location: Canada Recruitment: email sent by human resource personnel on the researchers' behalf to potential participants. |
|
| Participants |
Population: office workers employed in the head office of one large private company in Canada High personal/high contextual norm (n = 35), high personal/low contextual norm (n = 36), low personal/high contextual norm (n = 35) and low personal/low contextual norm (n = 36) Demographics: Mean age in years: 40.30 (SD 12.02) 66% of participants were females |
|
| Interventions |
Duration: 10 days High personal/high contextual norm vs. high personal/ ow contextual norm vs. low personal/high contextual norm vs. low personal/low contextual norm |
|
| Outcomes |
Outcome name, measurement time (units of measurement)
|
|
| Notes | This work was supported by a Vanier Canada Graduate Scholarship (first author) from the Social Sciences and Humanities Research Council of Canada. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were manually randomly assigned using random number tables to one of four conditions. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Very high dropout (32% attrition) |
| Selective reporting (reporting bias) | Low risk | No protocol. All the outcomes mentioned in the method section were reported. |
| Baseline comparability/ imbalance | Unclear risk | Not reported |
| Validity of outcome measure | Unclear risk | Not reported |
| Methods | Random allocation by cluster Single blind Study duration: 27 weeks Dropouts: 28% Location: Spain Recruitment: office workers were first invited to participate in an on‐line survey to identify those with low and moderate PA levels. Then they were invited to participate in the intervention by email or phone calls. |
|
| Participants |
Population: administrative and academic staff working at six campuses in four Spanish Universities in Galicia, the Basque Country and Catalonia Intervention group: 135 participants (3 clusters) Control group: 129 participants (3 clusters) |
|
| Interventions |
Duration of intervention: 8 weeks Intervention: automated web‐based intervention (W@WS) to encourage incidental walking and short walks during the workday. The walking strategies focused on breaking occupational sitting time by incidental walking into work tasks such as moving rather than sitting during lectures and seminars, not sitting to take phone calls, short walks (5–10 minutes) within University campuses, active transport (e.g. walking to work whenever possible) or active lunch breaks. Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Self‐reported occupational sitting time (minutes/day) measured by paper dairy log Daily step counts measured by Pedometer, Yamax‐200 Physical risk factors (waist circumference, BMI, blood pressure) |
|
| Notes | The study was funded by the Spanish Ministry of Science and Innovation (MICCIN) (project reference DEP 2009‐1147). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Campuses were randomly assigned by worksite to an intervention (n = 3; deployed W@WS) or comparative group (n = 3; maintained normal behaviour). In each region, one university campus was randomly assigned to the program (intervention group; IG) and another campus acted as a comparison group (CG). Authors replied to our request for further information but their reasoning was unclear. |
| Allocation concealment (selection bias) | Unclear risk | Authors replied to our request for further information but their reasoning was unclear. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Following correspondence with authors, they replied: “In the "big universities": the comparison and the intervention campuses were located in different cities and therefore, participants from each campus were not aware that another campus was doing the intervention. In the "small universities": Each university was located in a different city (Barcelona and Vic). Thus, participants did not know there was another university doing the intervention.” However because of the self‐evident nature of the intervention awareness of their own exposure to a certain changed environment or intervention might have changed their behaviour. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Number of withdrawals was unbalanced in two groups, with more in the intervention group. There were 33 (24%) in the intervention and 41 (32%) in the control group. |
| Selective reporting (reporting bias) | Low risk | All the outcomes mentioned in the protocol were reported. |
| Baseline comparability/ imbalance | Unclear risk | Not reported |
| Validity of outcome measure | Low risk | Paper‐based diary was used to report sitting time at work. |
| Methods | Random allocation Single‐blind Study duration: 14 weeks Dropouts: 14% Location: Australia Recruitment: participants were recruited via an email |
|
| Participants |
Population: employees of Lockheed Martin Mission System and Training business unit: primarily develops software solutions and training/simulation technologies for both civil and commercial markets. 2500 full‐time employees of whom 90% in sedentary computer work for a large percentage of their workday Intervention group: ergonomic training (16 participants), adjustable desks (23 participants), training and desks (20 participants) Control group: 13 participants Demographics: mean age in years: 37.2 (SD 9.4) BMI: 26.9 (SD 4.4) kg/m2 |
|
| Interventions |
Duration of intervention: 14 weeks Intervention: Training vs. adjustable desks vs. training and desks Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | No conflict of interest reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were listed out in Excel and randomly placed into one of the four groups. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | < 10% attrition rate |
| Selective reporting (reporting bias) | Low risk | No protocol; all the outcomes mentioned in the methods section are reported. |
| Baseline comparability/ imbalance | Unclear risk | Baseline characteristics of participants not reported |
| Validity of outcome measure | High risk | Only mentioned self report. No information on validity of questionnaires used. |
| Methods | Random allocation Single‐blind Study duration: 3 months Dropouts: 24% Location: USA Recruitment: in‐house distribution of print and electronic media. Potential participants received an email providing a link to an online survey that included a series of screening questions designed to assess participant eligibility. |
|
| Participants |
Population: pool of 728 overweight/obese and sedentary employees at a single office Intervention group: 15 participants Control group: 16 participants Demographics: mean age: intervention 40 (SD 9.5) years, control 40.3 (SD 10.9) years One male participant and 40 female participants BMI: intervention 36.1 (SD 8.7) kg/m², control 35.6 (SD 8.2) kg/m² |
|
| Interventions |
Duration of intervention: 3 months Intervention: treadmill desk plus counselling Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Physical activity (minutes/hour) and sedentary behaviour (minutes/hour) measured by accelerometer‐inclinometer. Body mass, body fat percentage, and BMI |
|
| Notes | This research was supported by Blue Cross and Blue Shield of Louisiana. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Following correspondence with authors, they replied: "Statisticians generated a random list". |
| Allocation concealment (selection bias) | Low risk | Following correspondence with authors, they replied: “The randomisation codes were sealed in envelopes with randomisation numbers”. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Following correspondence with authors, they replied: “Participants were not blinded. Intervention personnel and Project Manager were not blinded”. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Does not appear to have attrition bias |
| Selective reporting (reporting bias) | High risk | The trial registry mentions a follow‐up of 6 months but the study reports only 3 months' follow‐up. |
| Baseline comparability/ imbalance | Low risk | Age, sex and occupation were similar in both the intervention group and the control group at baseline. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation by cluster Unblinded Study duration: 6 days Dropouts: 23% Location: USA Recruitment: employees with clerical positions were identified through University directory. |
|
| Participants |
Population: full‐time employees (employed > 20 years) engaged in a sedentary occupation Intervention: stand group: 29 participants; step group: 31 participants Demographics: mean age: stand: 42.3 (SD 11.6) years, step: 46.1 (SD 10.5) years 60% were females in stand group and 75% were females in step group BMI: stand: 29.3 (SD 7.3) kg/m², step: 27.7 (SD 7.4) kg/m² |
|
| Interventions |
Duration of intervention: 3 days Intervention: computer‐based versus wrist worn prompts |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement) Total sitting time (minutes/workday), duration of longest sitting bout (minutes/workday), number of sitting bouts/workday of 30 min or more, standing time (minutes/workday), stepping time, sit/stand transitions measured by accelerometer‐inclinometers. |
|
| Notes | The Clinical and Translational Science Institute of Southeastern Wisconsin supported this research. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generation was used to assign participants to either the stand group or step group. |
| Allocation concealment (selection bias) | Low risk | Assignments were written out and placed in sealed numbered envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The envelopes were opened sequentially by a researcher; participants were informed of group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 18 participants were excluded, 9 each from stand group and step group. Reasons were dropout, equipment malfunction and not wearing monitor properly. The authors did not conduct intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section were reported. The study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | No baseline differences were found between the two groups for age, body mass, height or BMI. There was however difference in gender with the Stand group having 60% females and the Step group having 75%. |
| Validity of outcome measure | Low risk | The accelerometer is a valid instrument for the measurement of sitting time. |
| Methods | Random allocation Single‐blind Study duration: 5 weeks Dropouts: 29% Location: Australia Recruitment: participants were recruited via an email sent to all staff working in the study locations |
|
| Participants |
Population: participants were recruited from four locations across two organisations. The organisations were a non‐government organisation and a university. All locations were office‐based environments. Intervention group: 26 participants Control group: 26 participants Demographics: mean age in years: intervention 34.8 (SD 10.5), control 34.3 (SD 8.9) % female participants: intervention 89%, control 84% |
|
| Interventions |
Duration of intervention: 5 weeks Intervention: sit‐stand desk + instructions/ergonomic assessment Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This study was funded by Healthway (File No: Healthway Promotion Research Agreement 24008). The sit‐stand workstations were supplied by Ergotron (www.ergotron.com). Authors had no conflicts of interest to report |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported (only use the word randomised, no protocol to check) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were probably aware of allocation because of self evident nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar proportions of participants were missing from final analysis in both groups. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. Study protocol was not available. |
| Baseline comparability/ imbalance | Low risk | Participants in control and intervention groups were comparable in age, sex, BMI and education at baseline. |
| Validity of outcome measure | Low risk | activPAL is a valid instrument for assessment of physical activity and sedentary behaviour |
| Methods | Random allocation Single‐blind Study duration: 2 weeks Dropouts: 8% Location: United States Recruitment: not reported |
|
| Participants |
Population: staff at a United States university in desk jobs Intervention group: 26 participants Control group: 22 participants Demographics: mean age in years: 48 (SD 10) All participants were females Mean BMI: 30.5 (SD 8.2) kg/m2 |
|
| Interventions |
Duration of intervention: 1 week Intervention: audible alert and text message every hour and information on behavioural choices and health risks associated with prolonged sitting Control: no intervention |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | No conflict of interest reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment included assigning participants by table of random numbers to 1 of 2 groups. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Group assignment was doubly blinded until the end of week 1, at which time both the participants and the investigator were aware of group assignment. However, Its not for the duration of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (8%) |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the method section were reported. Study protocol was not available. |
| Baseline comparability/ imbalance | Unclear risk | Participants characteristics at baseline not reported |
| Validity of outcome measure | Low risk | activPAL is a valid instrument for assessing physical activity and sedentary behaviour. |
| Methods | Random allocation Unblinded Study duration: 12 months Dropout: 11% Location: Amsterdam, the Netherlands |
|
| Participants |
Population: all employees from 2 Dutch research institutes were invited to participate, between April and November 2010 Intervention group: 129 participants Control group: 128 participants Demographics: mean age of the study population was 46 years 67% of participants were women About 60% of the study population had a healthy weight (BMI 18.5‐25). |
|
| Interventions |
Duration of intervention: 6 months but the participants were followed up for 12 months. Intervention: the Mindful VIP intervention consists of 8 weeks of in‐company mindfulness training with homework exercises, followed by 8 sessions of e–coaching. The homework exercises comprised a variety of formal (“body scan” meditation, sitting meditation) and informal exercises (small exercises, such as breathing exercises when starting up the computer, and grocery shopping mindfully). Additionally, free fruit and snack vegetables were provided during the 6 months. In addition, lunch walking routes, and a buddy‐system were offered as supportive tools. Control: received information on existing lifestyle behaviour‐related facilities that were already available at the worksite. |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | The authors report no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were individually randomised to either the intervention or control group, using a computer‐generated randomisation sequence. |
| Allocation concealment (selection bias) | High risk | After randomisation, the research assistant notified each participant by email about the group to which he or she was allocated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of the participants and the trainers was not possible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8 participants were lost to follow‐up from the intervention group and 17 from the control group. The authors conducted intention‐to‐treat analysis by linear mixed‐effect models. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | Mean age was similar between the intervention group and control group. There were 63.6% women in the intervention group and 71% in the control group. All participants were from two Dutch research institutes. |
| Validity of outcome measure | High risk | Validity of the questionnaire used in the study has not been tested. |
| Methods | Allocation randomly by cluster Double‐blind Study duration: 6 months Dropout: 43% in occupational physicians (OPs) and 10% in employees Location: Amsterdam, the Netherlands Recruitment: OPs were recruited by the Netherlands Society of Occupational Medicine via a direct mailing to their members' registry (> 2100 OPs). OPs were asked to recruit 1 or more companies of medium or large size (> 100 workers). Next, OPs recruited employees via a health risk appraisal consisting of anthropometric measurements and subsequent health advice. |
|
| Participants |
Population: OPs from the Netherlands Society of Occupational Medicine and employees from medium or large sized companies in the Netherlands Intervention group: OPs (n = 7), employees (n = 274) Control group: OPs (n = 9), employees (n = 249) Demographics: mean age of employees in the intervention group was 46 (SD 8) years, mean age in the control group was 48 (SD 9) years. Percentages of men were 62% and 65% in the intervention and control groups respectively. 33% of employees in the intervention group and 27% of employees in the control group had a normal BMI. Type of worker Intervention group: blue collar (manual labour) 15%; white collar 70%; client contact 15% Control group: blue collar 17%; white collar 73%; client contact 10% |
|
| Interventions |
Duration of intervention: 6 months Intervention: guideline‐based counselling by OP providing advice to employers on how to assess and intervene on the obesogenic work environment. Conducted by OPs as 5 face‐to‐face behavioural change counselling sessions for employees to improve their lifestyle to prevent weight gain. Control: usual care by physician |
|
| Outcomes |
Outcome name, measurement time/tool (units of measurement)
|
|
| Notes | This study was funded by the Netherlands Organisation for Health Research and Development. The authors report no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | OPs who consented to participate were randomly assigned to the intervention or control group by an independent researcher using Random Allocation Software (V.1.0; Isfahan University of Medical Sciences) |
| Allocation concealment (selection bias) | High risk | After randomisation, the principal researcher notified OPs of the group to which they had been allocated. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | As OPs themselves were the intervention providers, they could not be blinded for allocation. OPs were asked not to reveal their group to participating employees or assistants performing measurements. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Waist circumference, body weight and height were measured by unblinded OPs or by blinded clinic employees. However blinding for assessment of sitting was not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 28 OPs were randomised, but 12 (43%) did not participate in the study at all. However, the remaining OPs recruited employees well, matching the number of planned employees. During the 6‐month intervention period, employees from both groups were lost to follow‐up (7 from the intervention group and 16 from the control group). These subjects (n = 53) were significantly younger, women, and had a lower income than study completers. |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the study protocol were reported. |
| Baseline comparability/ imbalance | Low risk | Age, sex and occupation were similar in both the intervention group and the control group at baseline. |
| Validity of outcome measure | High risk | Validity of the questionnaire used in the study has not been tested. |
Abbreviations
BMI: body‐mass index CBA: controlled before‐and‐after study h: hour(s) OP: occupational physician CP: computer prompts RCT: randomised controlled trial SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aadahl 2015 | Not conducted in a workplace setting. Did not report workplace sitting, only total sitting. |
| Adams 2012 | Not all the participants were working. Did not report workplace sitting as a separate outcome. Total sitting time reported. |
| Aittasalo 2004 | Did not report workplace sitting as a separate outcome. Sitting time reported separately for working days and non‐working days but the working days included both work and leisure time. |
| Alderman 2014 | Not RCT or CBA. Did not report workplace sitting. |
| Arrogi 2017 | Did not report workplace sitting |
| Audrey 2015 | Not conducted in a workplace setting. |
| Barbieri 2017 | Did not report workplace sitting |
| Ben‐Ner 2014 | Did not report data on sitting time at work separately. Daily sitting time (during waking hours) was measured with an accelerometer but it included both work and leisure time. |
| Berberien 2016 | Not RCT or CBA. |
| Biddle 2015 | Not conducted in a workplace setting. |
| Bird 2014 | Not RCT or CBA. |
| Bjorklund 2015 | Did not report workplace sitting |
| Boreham 2005 | This was a stair‐climbing training study that took place during working hours, but sitting time was not assessed. |
| Bouchard 2015 | Not RCT or CBA. |
| Brown 2012 | Did not report workplace sitting. |
| Buchholz 2016 | Not RCT or CBA. |
| Carr 2013 | No data reported for sitting time at work. Daily sedentary time (criterion: 0 steps/minute) was measured with StepWatch (accelerometer attached on ankle), but it included both work and leisure time (the monitor was kept during all wakeful hours for 7 consecutive days). Correspondence with the author was unclear regarding the distinction between work and leisure in sitting time. It is also not clear what the StepWatch measures as an accelerometer. |
| Carter 2015 | Not RCT or CBA. Does not describe a full working day. |
| Chae 2015 | Not RCT or CBA (pre‐post design). All the participants did not complete the program. |
| Cheema 2013 | Did not report workplace sitting. |
| Chia 2015 | Did not report workplace sitting. Following correspondence with authors they replied: "We did not specifically measure sitting time but had an indication of the time spent in the office (these are desk bound participants‐ when they filled in the questionnaire of alertness by the hour (0900‐1700hrs)". |
| Cifuentes 2015 | Not RCT or CBA. |
| Clemes 2014 | Not RCT or CBA. Pedometers were used to record sitting time and step counts. |
| DeCocker 2015 | Not RCT or CBA. |
| Dewa 2009 | Did not report workplace sitting. Sitting time was assessed (IPAQ) but it included both work and leisure time. |
| Elmer 2014 | Not RCT or CBA. Outcome is energy expenditure not time spent sitting at work. |
| Engelen 2017 | Not RCT or CBA. |
| Fennell 2017 | Did not report workplace sitting |
| Foley 2016 | Not RCT or CBA. |
| Freak‐Poli 2011 | Not an RCT or CBA. Workplace sitting not reported. Sitting time was questioned separately for weekdays and weekend days but it included both work and leisure. |
| Ganesan 2016 | Did not report workplace sitting |
| Gardner 2015 | Not conducted in a workplace setting. |
| Gilson 2012 | Not an RCT or CBA. Did not report workplace sitting. |
| Gilson 2015 | Not RCT or CBA. |
| Gilson ND 2012 | Not an RCT or CBA. |
| Gorman 2013 | Not an RCT or CBA. |
| Green 2016 | Not RCT or CBA. |
| Grunseit 2012 | Not an RCT or CBA. |
| Hadgraft 2017 | Did not report workplace sitting |
| Hedge 2004 | Sitting time was not reported in hours (only %). The length of intervention was not the same for everybody (no detailed information, stated “4‐6 wks”). |
| Irvine 2011 | Not an RCT or CBA. No quantitative data on sitting time at work. |
| Jancey 2016 | Not RCT or CBA. |
| John 2011 | Not an RCT or CBA. Did not report workplace sitting. Daily sitting time (waking hours) was measured with an accelerometer, but it included both work and leisure time. |
| Jones 2017 | Did not report workplace sitting |
| Júdice 2015 | Did not report workplace sitting, only total sitting time. |
| Kennedy 2007 | Did not report workplace sitting. |
| Kerr 2016 | Not conducted in a workplace setting. |
| Koepp 2013 | Not an RCT or CBA. |
| Lara 2008 | Not an RCT or CBA. Did not report workplace sitting. |
| Liu 2016 | Not RCT or CBA. |
| Maeda 2014 | Not RCT or CBA. Participants were university students. |
| Mahmud 2015 | Did not report workplace sitting |
| Mainsbridge 2014 | Did not report workplace sitting. |
| Mair 2014 | Did not report workplace sitting. |
| Marshall 2003 | Did not report workplace sitting. Sitting time was assessed (IPAQ, short version) but it included both work and leisure time (reported as ‘weekday sitting time’). |
| McAlpine 2007 | Not a normal working day, but an experimental office facility. Not an RCT or CBA. |
| Miyachi 2015 | Did not report workplace sitting. |
| NCT01221363 | Following correspondence with the authors, they replied: "Ours is not a work place intervention study, but a 'total sitting time' community‐based intervention study where the individual behavioural intervention addresses all domains of life, i.e. leisure time, work, transportation etc. Approximately 1/3 of participants are not working (retired or unemployed) and those who do work, do not necessarily have sedentary work, since our main inclusion criterion was minimum 3.5 hours of leisure time sitting/day. Consequently our primary outcome measure is objectively measured total daily sitting time (activPAL), and we only have rather crude self‐report measures on sitting time at work." |
| Ognibene 2016 | Did not report workplace sitting |
| Opdenacker 2008 | Did not report workplace sitting. Sitting time was assessed (IPAQ) but it included both work and leisure time. |
| Ouyang 2015 | Not conducted in a workplace setting. Participants were sedentary overweight females. |
| Parry S 2013 | Did not report workplace sitting. Reported sedentary time measured by accelerometer. Sedentary time was defined as an activity having less than 100 counts on an accelerometer. |
| Pilcher 2017 | Did not report workplace sitting |
| Poirier 2016 | Did not report workplace sitting |
| Pronk 2012 | Not an RCT or CBA. |
| Roossien 2017 | Not RCT or CBA. |
| Schwartz 2016 | Did not report workplace sitting |
| Slootmaker 2009 | Did not report workplace sitting. Daily sitting time (waking hours) was measured with an accelerometer, but it included both work and leisure time. |
| Sternfeld 2009 | Did not report workplace sitting. Sedentary time assessed during leisure. |
| Straker 2013 | Not an RCT or CBA. |
| Taylor 2016 | Did not report workplace sitting |
| Thogersen‐Ntoumani 2013 | Did not report workplace sitting. |
| Thompson 2014 | Did not report workplace sitting. The authors used accelerometers, but converted their results into energy expenditure/day (no separation between work and leisure time). |
| Thorp 2015 | Outcome is energy expenditure not time spent sitting at work. |
| Torbeyns 2016 | Did not report workplace sitting |
| Torbeyns 2017 | Not RCT or CBA. |
| Tucker 2016 | Did not report workplace sitting |
| vanNassau 2015 | Not RCT or CBA. |
| Wirick 2016 | Not conducted in a workplace setting. |
| Yancey 2004 | Did not report workplace sitting. |
| Østerås 2005 | Not an RCT or CBA. |
Abbreviations
CBA: controlled before‐and‐after study IPAQ: International physical activity questionnaire RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised controlled trial |
| Participants | Sedentary office workers (n = 127; ages 22‐64; BMI = 28.5±6.1 kg/m²) were recruited from three Minnesota employers. |
| Interventions | The intervention consisted of 4 groups for 6 months: 1) Control, 2) Move (30 minutes of light activity during the workday), 3) Stand (standing 50% of the workday using a sit‐stand workstation), or 4) Stand + Move (combined Stand and Move). |
| Outcomes | Outcomes were assessed at baseline and at 6 months' follow‐up using the following cardiometabolic risk factors: blood pressure, fasting blood glucose, log of fasting triglycerides, and HDL‐cholesterol. |
| Notes | We could not find the full‐text article. |
| Methods | No information available |
| Participants | No information available |
| Interventions | No information available |
| Outcomes | No information available |
| Notes | We could not find the full‐text article. |
| Methods | Pre‐post design |
| Participants | Scottish working adults |
| Interventions | A 30‐minute individual discussion incorporating cognitive behavioural strategies (e.g. decisional balance, goal setting) to encourage individuals to think about their current sedentary behaviour and strategies to change. Duration of intervention: 2 weeks |
| Outcomes | Time spent sitting/lying, standing, stepping, step counts and sit‐to‐stand transitions. |
| Notes | We could not find the full‐text article. |
| Methods | Random allocation |
| Participants | Desk‐based employees |
| Interventions | Intervention: height‐adjustable workstation Control: no intervention |
| Outcomes | Change in workplace sedentary time assessed at 4 weeks after installation of height‐adjustable workstations, and 4 weeks after removal of height‐adjustable workstations Change in workplace absenteeism using the World Health Organization Health and Work Performance Questionnaire Change in workplace presenteeism using the World Health Organization Health and Work Performance Questionnaire |
| Notes | Principal Investigator: Simon H Till, Sheffield Hallam University |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | |
| Methods | Random allocation in clusters Location: Australia Recruitment: not yet recruiting |
| Participants | Population: male and female employees of Rockhampton Regional Council working either full‐time or part‐time, aged 18‐65 years |
| Interventions | Participants will be asked to wear a pedometer during the 6‐week challenge and to record the number of steps they have taken each day on the Central Queensland University 10,000 Steps website. Control: no intervention |
| Outcomes |
Primary outcome: total steps of physical activity measured using the Yamax Digiwalker DW‐150 pedometer Secondary outcomes
|
| Starting date | It is unclear whether the study has started at all. The study was promised to take place in 2013 and the study registration has not been updated. |
| Contact information | Mitch Duncan, email: m.duncan@cqu.edu.au |
| Notes | Primary sponsor: Government funding body Central Queensland Hospital and Health Service |
| Trial name or title | |
| Methods | Random allocation Recruitment: not yet recruiting |
| Participants | Population: office‐based workers aged 18 years and over, working at least 0.6 full‐time equivalent |
| Interventions | The organisational plus technology support intervention lasts for 8 weeks and consists of the following components:
Control: will receive all the elements of the intervention except PLUS technology support. |
| Outcomes |
Primary outcome
Secondary outcomes
|
| Starting date | It is unclear whether the study has started despite mentioning anticipated date of first participant enrolment 17/03/2014. The study registration has not been updated. |
| Contact information | Genevieve Healy, email: g.healy@uq.edu.au |
| Notes | Primary sponsor: University Cancer Prevention Research Centre, The University of Queensland, Australia |
| Trial name or title | The Inphact treadmill study |
| Methods | Random allocation Location: Sweden Recruitment: recruitment and screening of participants has been completed. |
| Participants | Population description: healthy overweight and obese office workers (n = 80) with mainly sedentary tasks will be recruited from office workplaces in Umeå, Sweden. |
| Interventions | The intervention group will receive a health consultation and a treadmill desk, which they will use for at least one hour per day for 13 months. Control: the control group will receive the same health consultation, but continue to work at their regular workstations. |
| Outcomes |
Primary outcome: Physical activity and sedentary time during workdays and non‐workdays as well as during working and non‐working hours on workdays will be measured objectively using accelerometers (Actigraph and activPAL) at baseline and after 2, 6, 10, and 13 months of follow‐up. Secondary outcome: Food intake will be recorded and metabolic and anthropometric variables, body composition, stress, pain, depression, anxiety, cognitive function, and functional magnetic resonance imaging will be measured at 3–5 time points during the study period. |
| Starting date | November 2013 |
| Contact information | Tommy Olsson, email: tommy.g.olsson@umu.se |
| Notes | Sponsors: Not reported |
| Trial name or title | Stand & Move at Work |
| Methods | Random allocation by clusters Location: United States Recruitment: not yet recruiting |
| Participants | Population description: worksites will be enrolled in the greater Phoenix, AZ, USA and Minneapolis, MN, USA metropolitan regions. Selected worksites will be drawn from three distinct work sectors: higher education, industry/healthcare (e.g., law firms, health insurance providers), and government (e.g. state departments). |
| Interventions | Multicomponent interventions comprising of sit‐stand workstation, e‐newsletter, individualised coaching, prompts and engagement of worksite administrators and managers to enact policy‐level workplace modifications |
| Outcomes |
Primary outcomes: time spent sitting and LPA at work, will be assessed with the activPAL3 accelerometer‐inclinometer Secondary outcomes: cardiometabolic risk, workplace productivity, work engagement, and workplace satisfaction |
| Starting date | |
| Contact information | Matthew P. Buman, email address: matthew.buman@asu.edu |
| Notes | Study supported by the National Institutes of Health [R01CA198971]. |
| Trial name or title | Stand Up Victoria |
| Methods | Random allocation Location: Australia Recruitment: not yet recruiting |
| Participants | Population description: employees aged 18‐65 years, from 16 work sites located in Victoria, Australia |
| Interventions | The intervention consists of four distinct components:
Control: no intervention |
| Outcomes |
Primary outcome
Secondary outcomes Examine the effect of the intervention on cardiometabolic markers of health and disease including:
Explore workplace and individual‐level mediators (how did the intervention work?) and moderators (for whom did it work?) of change using a specially formulated questionnaire. |
| Starting date | July 2011 |
| Contact information | David Dunstan, email: David.Dunstan@bakeridi.edu.au |
| Notes | Sponsors: National Health and Medical Research Council and Vic Health |
| Trial name or title | TRial of Economic Incentives to Promote Physical Activity (TRIPPA) |
| Methods | Random allocation Location: Singapore Recruitment: on a rolling basis, and in two steps. In the first step, companies were engaged through existing contacts and “cold calls”. If companies responded positively, a study briefing was conducted to apprise the management of study details. Once we received confirmation of participation from the management team, we proceeded to step two of the recruitment process. Recruitment materials (e.g., electronic direct mails, posters, and newsletters) communicating the nature of the research study were disseminated to employees through internal channels unique to each company. The materials directed potential participants to the study website for additional information. Employees were also invited to attend a presentation conducted by the study team at each participating worksite. |
| Participants | Population description: employees from 13 companies spanning 15 worksites in Singapore |
| Interventions | 4 arms: “basic package” comprising two educational booklets, Fitbit arm, two incentive arms (cash or charity) |
| Outcomes | Primary outcome: MVPA bout minutes/week as measured via accelerometry Secondary outcomes:
|
| Starting date | |
| Contact information | Eric A. Finkelstein, e‐mail address: eric.finkelstein@duke‐nus.edu.sg |
| Notes | This study is supported by the Singapore Ministry of Health's Health Services Research Competitive Research Grant (HSRG/022/2012). |
| Trial name or title | |
| Methods | Random allocation Location: Finland Recruitment: recruitment is performed in the city of Jyväskylä, Finland, by delivering advertisements to parents via kindergartens and primary schools that have been pre‐randomised to control and intervention groups after balancing different environmental and socioeconomic regions within the city. |
| Participants | Population description: families from Jyväskylä region, Finland |
| Interventions | Tailored counselling targeted to decrease sitting time by focusing on commuting and work time. Control: no intervention |
| Outcomes | Changes in physical activity, health‐related indices and maintenance of the behavioural change |
| Starting date | December 2011 |
| Contact information | Taija Juutinen, email: taija.m.juutinen@jyu.fi |
| Notes | Study sponsors: Ministry of Education and Culture, Finland |
| Trial name or title | Take A Stand for Workplace Health: A Sit‐stand Workstation Project Evaluation |
| Methods | Random allocation Recruitment: active, not recruiting |
| Participants | Population: office employees primarily engaged in desk‐based work at one of the two worksites involved in the study (Macmillan Cancer Support, Public Health England) |
| Interventions |
Duration of intervention: 12 months Three‐arm trial Intervention: a sit‐stand workstation only and a multi‐component sit‐stand workstation intervention including individual and organisation‐level approaches Control: usual practice (seated workstation) |
| Outcomes |
|
| Starting date | May 2014 |
| Contact information | Jenifer Hall, email: Jennifer.Hall@brunel.ac.uk |
| Notes | Sponsors and collaborators: Brunel University, Macmillan Cancer Support, Ergotron, Public Health England |
| Trial name or title | Booster breaks: health promoting work breaks |
| Methods | Random allocation |
| Participants | Population: employees with sedentary office jobs from four workplaces in a large, urban southwestern U.S. city. |
| Interventions | Three‐arm trial Intervention: Computer Prompt (individualized PA work breaks) group and Booster Break group Control: usual break group |
| Outcomes |
Primary outcomes: lipid profile, blood pressure, height, weight, International Physical Activity Questionnaire (IPAQ), pedometer readings Secondary outcomes: physical activity mediators and employee and organisational psychosocial constructs: self‐report assessments. |
| Starting date | January 2009 |
| Contact information | Wendell Taylor, email: Wendell.C.Taylor@uth.tmc.edu |
| Notes | Sponsor: National Institutes of Health (USA) |
| Trial name or title | |
| Methods | Random allocation Location: Australia |
| Participants | Population: employees of 1 of 3 of the university’s campuses located in Sydney and Melbourne, working on a part‐time or full‐time basis in either a job with an academic or administrative designation. |
| Interventions |
Duration of intervention: 12 weeks The intervention will comprise 2 distinct treatment phases targeting behaviour adoption (weeks 1‐4) and adherence (weeks 5‐12) using 'stages of behaviour change' principles
Control: no intervention |
| Outcomes |
Primary outcome: Average workday step count: measured by pedometer (Yamax SW‐200) and averaged over 5 workdays at each time point Secondary outcomes
|
| Starting date | March 2010 |
| Contact information | Martin Mackey, email: martin.mackey@sydney.edu.au |
| Notes |
Study sponsors: Australian Research Council: ARC (Industry) Linkage Grant Professor Philip Taylor |
| Trial name or title | |
| Methods | Random allocation Location: United Kingdom Recruitment: will be recruited through: 1) employment databases and invited via letter/email, and 2) adverts in local newsletters and flyers posted within the buildings of target organisations. |
| Participants | Population description: office‐based employees from two companies in Cambridge, UK |
| Interventions | Intervention: sit‐stand desks Control: no intervention |
| Outcomes |
|
| Starting date | |
| Contact information | Correspondence: tm388@medschl.cam.ac.uk |
| Notes | The study is supported by a grant from the Department of Health Policy Research Program (Policy Research Unit in Behaviour and Health [PR‐UN‐0409‐10109]), the Medical Research Council (Unit Programme number MC_UU_12015/3) and the British Heart Foundation (Intermediate Basic Science Research Fellowship grant FS/12/58/29709 to KW) |
| Trial name or title | SedestActiv Project |
| Methods | Random allocation Location: Spain Recruitment: a total of 232 subjects will be randomly allocated to an intervention and control group (116 individuals each group). In addition, 50 subjects with fibromyalgia will be included. |
| Participants | Population description: professionals from 13 primary health care centres will randomly invite mildly obese or overweight patients of both genders, aged 25‐65 years, to participate. |
| Interventions | 6‐month primary care intervention Control: no intervention |
| Outcomes |
Duration of intervention: 6 months Primary outcome: to assess the effectiveness of a 6‐month primary care intervention to reduce diary hours of sitting time in overweight and obese patients, as well as to increase their weekly energy expenditure Secondary outcomes
|
| Starting date | June 2012 |
| Contact information | Carme Martín‐Borràs Email: sedestactiv@gmail.com |
| Notes | Study sponsor: Jordi Gol i Gurina Foundation |
| Trial name or title | |
| Methods | Random allocation Recruitment: active, not recruiting |
| Participants | Population: sedentary office employees |
| Interventions | Height‐adjustable desk installation in office |
| Outcomes |
Primary outcome: workplace sitting time Secondary outcomes
|
| Starting date | January 2013 |
| Contact information | |
| Notes | Study sponsor: USDA (United States Department of Agriculture) Grand Forks Human Nutrition Research Center |
| Trial name or title | |
| Methods | Random allocation Recruitment: active, not recruiting |
| Participants | Population: sedentary employees who use a single computer workstation for the majority of their workday |
| Interventions | Sit‐stand workstation with three arms
|
| Outcomes |
|
| Starting date | November 2013 |
| Contact information | |
| Notes | Study sponsor: University of Minnesota ‐ Clinical and Translational Science Institute |
| Trial name or title | Modifying the workplace to decrease sedentary behaviour and improve health |
| Methods | Random allocation |
| Participants | Healthy volunteers employed in a full‐time sedentary job |
| Interventions |
Duration of intervention: 12 months Three‐arm trial Intervention: treadmill workstation and sit‐stand workstation Control: participants will be asked to engage in three 10 min walking bouts each workday |
| Outcomes | Change in weight |
| Starting date | April 2014 |
| Contact information | Anne Thorndike, email: ATHORNDIKE@mgh.harvard.edu |
| Notes | Study sponsor: Northeastern University |
| Trial name or title | |
| Methods | Random allocation |
| Participants | Employees from 10 organisations involved with the Healthy Working Lives initiative |
| Interventions |
Duration of intervention: 12 weeks Intervention: hourly prompts to stand for a period of 10 weeks plus education on why and how to reduce prolonged sitting Control: education on why and how to reduce prolonged sitting |
| Outcomes | Total time spent sitting at work, accessed by 7 day ActivPal and diary measurement Time spent sitting in prolonged sedentary bouts at work Number of sitting events at work Number of prolonged sitting events at work |
| Starting date | 1 February 2015 |
| Contact information | |
| Notes | Pricinpal Investigator: Philippa Dall, PhD |
| Trial name or title | |
| Methods | Random allocation |
| Participants | Desk‐based office employees |
| Interventions |
Duration: 12 weeks Intervention: an education session on the health benefits of breaking prolonged sitting and feedback on baseline sitting behaviour followed by hourly prompts to stand delivered by Microsoft Outlook for a period of 10 weeks. The messages will be short in length, varied and centre around the key message of breaking prolonged sitting by standing. Control: same education session as the prompt group, as well as feedback on their baseline sitting behaviour. |
| Outcomes | Total time spent sitting at work will be objectively measured using a tri‐axial accelerometer Total time spent sitting at work in continuous bouts of at least 30 minutes Number of sitting events at work Number of prolonged sitting events at work Time after prompt to stand |
| Starting date | March 2016 |
| Contact information | Philippa Dall, PhD |
| Notes |
| Trial name or title | |
| Methods | Random allocation |
| Participants | Desk‐based employees |
| Interventions | Treadmill workstation versus sit‐stand workstation |
| Outcomes |
|
| Starting date | August 2017 |
| Contact information | Mark Pereira, perei004@umn.edu |
| Notes |
| Trial name or title | SMArT Work: Stand More AT Work |
| Methods | Random allocation in clusters Location: UK Recruitment: participant recruitment will be coordinated via the research team at the Leicester Diabetes Centre. The study team currently hold a database of office units within the University Hospitals of Leicester NHS Trust and will promote this study to them initially through the use of the Trust’s intranet and emails to department managers. This will be followed up with a face‐to‐face presentation/meeting if necessary. |
| Participants | Desk‐based office workers (n = 238) from a stratified sample of NHS staff (e.g. employees, managers, gender, job role) |
| Interventions | Height‐adjustable workstations at the environmental, organisational and individual level that support less occupational sitting. |
| Outcomes |
|
| Starting date | October 2014 |
| Contact information | Dr Ben Jackson, email: b.r.jackson@lboro.ac.uk |
| Notes |
| Trial name or title | The Healthier Office Study |
| Methods | Quasi‐random allocation Location: Australia Recruitment: "Posters will be placed in staff tearooms and common areas, inviting staff to participate. The advertisements will contain general information informing participants that we are testing simple occupational health interventions and that participants will be provided with an ergonomic device or advice about improving healthy work practices. The study will also be advertised at Faculty staff meetings to improve potential participants’ awareness of the study" |
| Participants | Population description: participants will be recruited from academic and administrative staff of The University of Sydney, Sydney, Australia |
| Interventions |
Intervention: 3 groups (1 control group and 2 intervention groups) will be conducted in an office workplace setting. The education intervention group will receive an education package that encourages reduction in sitting behaviours. The sit‐stand desk intervention group will receive the same education package along with an adjustable sit‐stand desk. The control group will receive no information or advice about postural change and no modification to their office desk set‐up. |
| Outcomes | Average daily sedentary time during work hours, measured by an accelerometer |
| Starting date | March 2013 |
| Contact information | |
| Notes | Study sponsors: this research is supported by funding from the Heart Foundation, Sydney, NSW, Australia, and by Australian National Health and Medical Research Council Program Grant (number: 569940; AB). Sit‐stand workstations were donated by Sit Back and Relax, Alexandria, NSW, Australia. |
| Trial name or title | |
| Methods | Random allocation Location: Belgium Recruitment: all participants were recruited from working places in Flanders (Belgium) through flyers, emails, pharmacists, and word of mouth |
| Participants | Population: employees (male and female) aged 19‐67 years who mentioned not being physically active during the last year |
| Interventions |
Interventions: Participants were randomised into one of the following four intervention groups.
|
| Outcomes |
Primary outcome: physical activity level Secondary outcomes
|
| Starting date | |
| Contact information | |
| Notes | No conflict of interest |
Abbreviation
BMI: body mass index
Contributions of authors
Jos Verbeek, Sharea Ijaz, and Nipun Shrestha conceptualised the review.
Nipun Shrestha took the lead in writing the protocol.
Kaisa Neuvonen (Information Specialist, Cochrane Work Group) and Nipun Shrestha designed the systematic search strategies.
Nipun Shrestha and Katriina Kukkonen‐Harjula conducted the study selection.
Nipun Shrestha, Suresh Kumar, Chukwudi Nwankwo, Veerle Hermans, and Soumyadeep Bhaumik did the data extraction and 'Risk of bias' assessment for the previous versions.
Nipun Shrestha, Veerle Hermans, and Sharea Ijaz did the data extraction and 'Risk of bias' assessment for the current update.
Nipun Shrestha, Jos Verbeek, and Zeljko Pedisic conducted the data analysis.
Nipun Shrestha wrote the manuscript collaborating with Jos Verbeek, Katriina Kukkonen‐Harjula, Sharea Ijaz, Veerle Hermans, and Zeljko Pedisic.
Sources of support
Internal sources
-
Cochrane Work Review Group, Finland.
Nipun Shrestha attended a three‐month internship to learn about Cochrane systematic review methodology.
External sources
-
NIHR CLAHRC West, UK.
S Ijaz's time for this update was supported by National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care West (CLAHRC West) at University Hospitals Bristol NHS Foundation Trust.
-
Victoria University, Australia.
Nipun Shrestha has received financial support through a VU Research Scholarship 2016 from Victoria University.
Declarations of interest
Nipun Shrestha: None known.
Jos Verbeek: I am employed by the Finnish Institute of Occupational Health to co‐ordinate the Cochrane Work Group.
Sharea Ijaz: None known.
Katriina T Kukkonen‐Harjula: None known.
Veerle Hermans: None known.
Zeljko Pedisic: None known.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
- Alkhajah TA, Reeves MM, Eakin EG, Winkler EA, Owen N, Healy GN. Sit‐stand workstations: a pilot intervention to reduce office sitting time. American Journal of Preventive Medicine 2012;43(3):298‐303. [DOI] [PubMed] [Google Scholar]; Healy G, Alkhajah T, Winkler E, Owen N, Eakin E. Reducing sitting time in office workers: efficacy and acceptability of sit‐stand workstations. Journal of Science and Medicine in Sport 2012;15:S196. [Google Scholar]
- ACTRN12614000252617. Comparison of organisational support vs. organisational plus technology support for reducing prolonged sitting in office workers. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=365886 (accessed 12 September 2017). ; Brakenridge CL, Fjeldsoe BS, Young DC, Winkler EA, Dunstan DW, Straker LM. Evaluating the effectiveness of organisational‐level strategies with or without an activity tracker to reduce office workers' sitting time: a cluster‐randomised trial. International Journal of Behavioural Nutrition and Physical Activity 2016;13(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]; Brakenridge CL, Fjeldsoe BS, Young DC, Winkler EA, Dunstan DW, Straker LM. Organizational level strategies with or without an activity tracker to reduce office workers' sitting time: rationale and study design of a pilot cluster‐randomized trial. JMIR research protocols 2016;5(2):e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr LJ, Leonhard C, Tucker S, Fethke N, Benzo R, Gerr F. Total worker health intervention increases activity of sedentary workers. American Journal of Preventive Medicine 2015;49:[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]; NCT02071420. Efficacy of a combined ergonomic health promotion intervention on employee health. https://clinicaltrials.gov/ct2/show/NCT02071420 (accessed 28 November 2015).
- ACTRN12612000072819. The Stand@Work Pilot Study. A randomised controlled trial to see if using sit‐stand workstations reduces sitting time in office workers. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12612000072819 (accessed 3 June 2015). ; Chau JY, Daley M, Dunn S, Srinivasan A, Do A, Bauman AE, et al. The effectiveness of sit‐stand workstations for changing office workers' sitting time: results from the Stand@Work randomized controlled trial pilot. International Journal of Behavioral Nutrition and Physical Activity 2014;11:127. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chau JY, Daley M, Srinivasan A, Dunn S, Bauman AE, Ploeg HP. Desk‐based workers’ perspectives on using sit‐stand workstations: a qualitative analysis of the Stand@Work study. BMC Public Health 2014;14:752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau JY, Sukala W, Fedel K, Do A, Engelen L, Kingham M, et al. More standing and just as productive: effects of a sit‐stand desk intervention on callcenter workers’ sitting, standing, and productivity at work in the Opt to Standpilot study. Preventive Medicine Reports 2016;3:68‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffeng JK, Boot CR, Duijts SF, Twisk JW, Mechelen W, Hendriksen IJ. Effectiveness of a worksite social & physical environment intervention on need for recovery, physical activity and relaxation; results of a randomized controlled trial. PLoS ONE 2014;9(12):e114860. [DOI] [PMC free article] [PubMed] [Google Scholar]; Coffeng JK, Hendriksen IJ, Duijts SF, Proper KI, Mechelen WV, Boot CRL. The development of the Be Active & Relax "Vitality in Practice" (VIP) project and design of an RCT to reduce the need for recovery in office employees. BMC Public Health 2012;12:592. [DOI] [PMC free article] [PubMed] [Google Scholar]; Coffeng JK, Hendriksen IJ, Mechelen W, Boot CR. Process evaluation of a worksite social and physical environmental intervention. Journal of Occupational and Environmental Medicine 2013;55(12):1409‐20. [DOI] [PubMed] [Google Scholar]; Coffeng JK, Hendriksen IJM, Duijts SFA, Twisk JWR, Mechelen W, Boot CRL. Effectiveness of a combined social and physical environmental intervention on presenteeism, absenteeism, work performance and work engagement in office employees. Journal of Occupational Environment Medicine in press; Vol. 56, issue 3:258‐65. [DOI] [PubMed]; NTR2553. The cost‐effectiveness of an intervention to increase physical activity and relaxation amongst office workers. http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=2553 (accessed 3 June 2014).
- Danquah IH, Kloster S, Holtermann A, Aadahl M, Bauman A, Ersbøll AK, et al. Take a Stand!‐a multi‐component intervention aimed at reducing sitting time among office workers‐a cluster randomized trial. International Journal of Epidemiology 2017;46(1):128–40. [DOI] [PubMed] [Google Scholar]; Danquah IH, Kloster S, Holtermann A, Aadahl M, Tolstrup JS. Effects on musculoskeletal pain from “Take a stand!” – A cluster‐randomized controlled trial reducing sitting time among office workers. Scandinavian Journal of Work, Environment and Health. 2017;43(4):350‐7. [DOI] [PubMed] [Google Scholar]; NCT01996176. Take a Stand! ‐ an intervention to reduce occupational sitting time. https://clinicaltrials.gov/ct2/show/NCT01996176 (accessed 12 September 2017).
- Cocker K, Bourdeaudhuij I, Cardon G, Vandelanotte C. The effectiveness of a web‐based computer‐tailored intervention on workplace sitting: a randomized controlled trial. Journal of Medical Internet Research 2016;18(5):e96. [DOI] [PMC free article] [PubMed] [Google Scholar]; Cocker Katrien, Bourdeaudhuij I, Cardon G, Vandelanotte C. What are the working mechanisms of a web‐based workplace sitting intervention targeting psychosocial factors and action planning?. BMC Public Health 2017;1:382. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT02672215. RCT Computer‐tailored intervention on workplace sitting (StartToStand). https://clinicaltrials.gov/ct2/show/NCT02672215 (accessed 12 September 2017).
- Donath L, Faude O, Schefer Y, Roth R, Zahner L. Repetitive daily point of choice prompts and occupational sit‐stand transfers, concentration and neuromuscular performance in office workers: an RCT. International Journal of Environmental Research and Public Health 2015;12(4):4340‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta N, Koepp GA, Stovitz SD, Levine JA, Pereira MA. Using sit‐stand workstations to decrease sedentary time in office workers: a randomized crossover trial. International Journal of Environmental Research and Public Health 2014;11(7):6653‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]; Dutta N, Walton T, Pereira MA. Experience of switching from a traditional sitting workstation to a sit‐stand workstation in sedentary office workers. Work 2014;52(1):83‐9. [DOI] [PubMed] [Google Scholar]
- Ellegast R, Weber B, Mahlberg R. Method inventory for assessment of physical activity at VDU workplaces. Work. 2012; Vol. 41, issue suppl 1:2355‐9. [DOI] [PubMed] [Google Scholar]; Mahlberg R. Entwicklung und Erprobung eines arbeitsmedizinischen Methodeninventars zur Effektivitätsanalyse von Präventionsmassnahmen zur Vermeidung von Muskel‐Skelett Erkrankungen an bewegungsarmen Arbeitsplätzen. Hohen Medizinischen Fakultät der Ruhr‐Universität Bochum. PhD dissertation2011.
- Evans RE, Fawole HO, Sheriff SA, Dall PM, Grant PM, Ryan CG. Point‐of‐choice prompts to reduce sitting time at work: a randomised trial. American Journal of Preventive Medicine 2012 Sep;43(3):293‐7. [DOI] [PubMed] [Google Scholar]; NCT01628861. Point‐of‐choice prompts to reduce prolonged sitting time at work. http://clinicaltrials.gov/ct2/show/NCT01628861 (accessed 15 March 2014).
- Gao Y, Nevala N, Cronin NJ, Finni T. Effects of environmental intervention on sedentary time, musculoskeletal comfort and work ability in office workers. European Journal of Sport Science 2015;(Epub ahead of print):1‐8. [DOI] [PubMed] [Google Scholar]; ISRCTN43848163. Can an adjustable workstation reduce occupational sedentary time?. http://www.isrctn.com/ISRCTN43848163 (accessed 3 June 2015).
- Gilson ND, Puig‐Ribera A, McKenna J, Brown WJ, Burton NW, Cooke CB. Do walking strategies to increase physical activity reduce reported sitting in workplaces: a randomised control trial. International Journal of Behavioral Nutrition and Physical Activity 2009;6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon A. A theory‐based pilot study to decrease sitting time in the workplace. A theory‐based pilot study to decrease sitting time in the workplace (Msc Thesis). Arizona: Arizona State University, 2013. [Google Scholar]
- Graves LEF, Murphy RC, Shepherd SO, Cabot J, Hopkins ND. Evaluation of sit‐stand workstations in an office setting: a randomised controlled trial. BMC Public Health 2015;15(1):1145. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT02496507. A mixed‐methods evaluation of sit‐stand workstations in an office setting. https://clinicaltrials.gov/ct2/show/NCT02496507 (accessed 1 December 2015). [DOI] [PMC free article] [PubMed]
- Healy GN, Eakin EG, Lamontagne AD, Owen N, Winkler EA, Wiesner G, et al. Reducing sitting time in office workers: short‐term efficacy of a multi component intervention. Preventive Medicine 2013;57(1):43‐8. [DOI] [PubMed] [Google Scholar]; Neuhaus M, Healy G, Eakin E, FJeldsoe B, Lamontagne A, Owen N, et al. Efficacy of an integrated approach to reduce sitting time in office workers. Journal of Science and Medicine in Sport 2012;15:S197. [Google Scholar]; Stephens SK, Winkler EA, Trost SG, Dunstan DW, Eakin EG, Chastin SF, et al. Intervening to reduce workplace sitting time: how and when do changes to sitting time occur?. British Journal of Sports Medicine 2014;48(13):1037‐42. [DOI] [PubMed] [Google Scholar]
- ACTRN12611000742976. In office workers, does environmental modification combined with behavioural counselling, compared to no change, lead to reductions in workplace sitting time. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12611000742976 (accessed 12 September 2017). ; Healy GN, Eakin EG, Owen N, Lamontagne AD, Moodie M, Winkler EA. A cluster randomized controlled trial to reduce office workers' sitting time: effect on activity outcomes. Medicine and Science in Sports and Exercise 2016;48(9):1787‐97. [DOI] [PubMed] [Google Scholar]; Winkler EA, Chastin S, Eakin EG, Owen N, LaMontagne AD, Moodie M. Cardiometabolic impact of changing sitting, standing, and stepping in the workplace. Medicine and Science in Sports and Exercise 2017;50(3):516‐24. [DOI] [PubMed] [Google Scholar]
- Kress MM. The use of stand‐capable workstations for reducing sedentary time in office employees. Dissertation Abstracts International: Section B: The Sciences and Engineering 2015;76:6‐B(E). [Google Scholar]; Kress MM. The use of stand‐capable workstations for reducing sedentary time in office employees. Doctoral dissertation, Texas A & M University.2014.
- ACTRN12615001018505. Examining different sit‐stand protocols in terms of health and behavioural outcomes: an office‐based pilot study. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=369210 (accessed 12 September 2017). ; Li I, Mackey MG, Foley B, Pappas E, Edwards K, Chau JY, et al. Reducing office workers' sitting time at work using sit‐stand protocols: results from a pilot randomized controlled trial. Journal of Occupational Environmental Medicine 2016;59(6):543‐9. [DOI] [PubMed] [Google Scholar]
- MacEwen BT, Saunders TJ, MacDonald DJ, Burr JF. Sit‐stand desks to reduce workplace sitting time In office workers with abdominal obesity: a randomized controlled trial. Journal of Physical Activity and Health 2017;17:1‐18. [DOI] [PubMed] [Google Scholar]; NCT02342301. Cardiometabolic Response to Sit‐stand Workstations. https://clinicaltrials.gov/ct2/show/NCT02342301 (accessed 12 September 2017).
- Mailey EL, Rosenkranz SK, Casey K, Swank A. Comparing the effects of two different break strategies on occupational sedentary behavior in a real world setting. Preventive Medicine Reports 2016;4:423‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT02609438. An intervention to reduce sitting time at work: effects on metabolic health and inactivity (Up4Health). https://clinicaltrials.gov/ct2/show/NCT02609438 (accessed 12 September 2017).
- ACTRN12612001246875. Reducing sitting time in office workers: comparison of a multifaceted workplace approach vs. installation of height‐adjustable desks only using a three‐armed controlled trial. http://www.anzctr.org.au/ACTRN12612001246875.aspx (accessed 15 March 2014). ; Neuhaus M, Healy GN, Dunstan DW, Owen N, Eakin EG. Workplace sitting and height‐adjustable workstations: a randomised controlled trial. American Journal of Preventive Medicine 2014;46(1):30‐40. [DOI] [PubMed] [Google Scholar]
- Cooley D, Pedersen S, Mainsbridge C. Assessment of the impact of a workplace intervention to reduce prolonged occupational sitting time. Qualitative Health Research 2014;24(1):90‐101. [DOI] [PubMed] [Google Scholar]; Pedersen SJ, Cooley PD, Mainsbridge C. An e‐health intervention designed to increase workday energy expenditure by reducing prolonged occupational sitting habits. Work 2014;49(2):289‐95. [DOI] [PubMed] [Google Scholar]
- Pickens AW, Kress MM, Benden ME, Zhao H, Wendel M, Congleton JJ. Stand‐capable desk use in a call center:a six‐month follow‐up pilot study. Public Health 2016;135:131‐4. [DOI] [PubMed] [Google Scholar]
- Priebe CS, Spink KS. Less sitting and more moving in the office: using descriptive norm messages to decrease sedentary behavior and increase light physical activity at work. Psychology of Sport and Exercise 2015;19:76‐84. [Google Scholar]
- NCT02960750. Effectiveness of a workplace "Sit Less and Move More" web‐based program (Walk@WorkSpain) on occupational sedentary behavior, habitual physical activity, physical risk factors for chronic disease and efficiency‐related outcomes in Spanish office employees. https://clinicaltrials.gov/ct2/show/NCT02960750 (accessed 12 September 2017). ; Puig‐Ribera A, Bort‐Roig J, Gine‐Garriga M, Gonzalez‐Suarez AM, Martinez‐Lemos I, Fortuno J, et al. Impact of a workplace 'sit less, move more' program on efficiency‐related outcomes of office employees. BMC Public Health 2017;17(1):455. [DOI] [PMC free article] [PubMed] [Google Scholar]; Puig‐Ribera A, Bort‐Roig J, González‐Suárez AM, Martínez‐Lemos I, Giné‐Garriga M, Fortuño J, et al. Patterns of impact resulting from a 'sit less, move more' web‐based program in sedentary office employees. PLoS One 2015;10(4):e01224. [DOI] [PMC free article] [PubMed] [Google Scholar]; Roig JB, Horcajo MM, Ribera AP, Gonzalez Á, Lemos IM. Walk and Work Spain: Participants’ perspectives and experiences on reducing occupational sitting time. Journal of Science and Medicine in Sport 2012;15(Supplement 1):S303. [Google Scholar]
- Sandy ME. Longitudinal Study of Adjustable Workstations. Graduate Theses and Dissertations2016.
- NCT01587092. Workstation Pilot Study. https://clinicaltrials.gov/ct2/show/NCT01587092 (accessed 3 June 2014). ; Schuna JM Jr, Swift DL, Hendrick CA, Duet MT, Johnson WD, Martin CK, et al. Evaluation of a workplace treadmill desk intervention: a randomized controlled trial. Journal of Occupational and Environmental Medicine 2014;56(12):1266‐76. [DOI] [PubMed] [Google Scholar]; Tudor‐Locke C, Hendrick CA, Duet MT, Swift DL, Schuna JM Jr, Martin CK, et al. Implementation and adherence issues in a workplace treadmill desk intervention. Applied Physiology, Nutrition, and Metabolism 2014;39(10):1104‐11. [DOI] [PubMed] [Google Scholar]
- Swartz AM, Rote AE, Welch WA, Maeda H, Hart TL, Cho YI, et al. Prompts to disrupt sitting time and increase physical activity at work. Centers for Disease Control and Prevention, Preventing Chronic Disease 2014;11:E73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin R, Leavy J, Jancey J. Uprising: An examination of sit‐stand workstations, mental health and work ability in sedentary office workers, in Western Australia. Work 2016;55(2):359‐71. [DOI] [PubMed] [Google Scholar]
- Urda JL, Lynn JS, Gorman A, Larouere B. Effects of a minimal workplace intervention to reduce sedentary behaviors and improve perceived wellness in middle‐aged women office workers. Journal of Physical Activity and Health 2016;13:838‐44. [DOI] [PubMed] [Google Scholar]
- Berkel J, Boot CR, Proper KI, Bongers PM, Beek AJ. Effectiveness of a worksite mindfulness‐related multi‐component health promotion intervention on work engagement and mental health: results of a randomised controlled trial. PLoS ONE 2014;9(1):e84118. [DOI] [PMC free article] [PubMed] [Google Scholar]; Berkel J, Boot CR, Proper KI, Bongers PM, Beek AJ. Mindful "Vitality in Practice": an intervention to improve the work engagement and energy balance among workers; the development and design of the randomised controlled trial. BMC Public Health 2011;11:736. [DOI] [PMC free article] [PubMed] [Google Scholar]; Berkel J, Boot CR, Proper KI, et al. Effectiveness of a worksite mindfulness‐based multi‐component intervention on lifestyle behaviours. International Journal of Behavioral Nutrition and Physical Activity2014; Vol. 11. [DOI] [PMC free article] [PubMed]
- ISRCTN73545254. Balance@Work: the cost effectiveness of an occupational health guideline to improve physical activity and dietary behaviour among workers in order to prevent weight gain. http://www.isrctn.com/ISRCTN73545254 2009 (accessed 28 November 2015). ; Verweij LM, Proper KI, Weel AN, Hulshof CT, Mechelen W. Design of the Balance@Work project: systematic development, evaluation and implementation of an occupational health guideline aimed at the prevention of weight gain among employees. BMC Public Health 2009;9:461. [DOI] [PMC free article] [PubMed] [Google Scholar]; Verweij LM, Proper KI, Weel AN, Hulshof CT, Mechelen W. Long‐term effects of an occupational health guideline on employees' body weight‐related outcomes, cardiovascular disease risk factors, and quality of life: results from a randomised controlled trial. Scandinavian Journal of Work, Environment & Health 2013;39(3):284‐94. [DOI] [PubMed] [Google Scholar]; Verweij LM, Proper KI, Weel AN, Hulshof CT, Mechelen W. The application of an occupational health guideline reduces sedentary behaviour and increases fruit intake at work: results from an RCT. Occupational and Environmental Medicine 2012;69(7):500‐7. [DOI] [PubMed] [Google Scholar]; Wier MF, Verweij LM, Proper KI, Hulshof CT, Tulder MW, Mechelen W. Economic evaluation of an occupational health care guideline for prevention of weight gain among employees. Journal of occupational and environmental medicine 2013;55(9):1100. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Aadahl M, Linneberg A, Møller TC, Rosenørn S, Dunstan DW, Witte DR, et al. Motivational counselling to reduce sitting time: a community‐based randomized controlled trial in adults. American Journal of Preventive Medicine 2015;47(5):576‐86. [DOI] [PubMed] [Google Scholar]; NCT00289237. Lifestyle intervention in a general population for prevention of ischaemic heart disease. https://clinicaltrials.gov/show/NCT00289237 2012 (accessed 1 December 2015).
- Adams 2012. On our feet: Feasibility trial of an intervention to reduce sedentary behavior and increase physical activity (PhD Thesis). Greensboro: The University of North Carolina, 2012. [Google Scholar]; Melanie M. Adams MM, Davis PG, Gill DL. A hybrid online intervention for reducing sedentary behavior in obese women. Frontiers in Public Health 2013;1:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aittasalo M, Miilunpalo S, Suni J. The effectiveness of physical activity counselling in a work‐site setting. A randomised, controlled trial. Patient Education and Counselling 2004;55(2):193‐202. [DOI] [PubMed] [Google Scholar]
- Alderman BL, Olson RL, Mattina DM. Cognitive function during low‐intensity walking: a test of the treadmill workstation. Journal of Physical Activity and Health 2014;11(4):752‐8. [DOI] [PubMed] [Google Scholar]
- Arrogi A, Schotte A, Bogaerts A, Boen F, Seghers J. Short‐ and long‐term effectiveness of a three‐month individualized need‐supportive physical activity counseling intervention at the workplace.. BMC Public Health 2017;17(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrey S, Cooper AR, Hollingworth W, Metcalfe C, Procter S, Davis A, et al. Study protocol: the effectiveness and cost effectiveness of an employer‐led intervention to increase walking during the daily commute: the Travel to Work randomised controlled trial. BMC public Health 2015;15:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbieri DF, Srinivasan D, Mathiassen SE, Oliveira AB. Comparison of sedentary behaviors in office workers using sit‐stand tables with and without semiautomated position changes. Human Factors 2017;59(5):782‐95. [DOI] [PubMed] [Google Scholar]
- Ben‐Ner A, Hamann DJ, Koepp G, Manohar CU, Levine J. Treadmill workstations: the effects of walking while working on physical activity and work performance. PLoS ONE 2014;9(2):e88620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berberien V, Lowensteyn I. Evaluating the impact of a workplace wellness program on women: the experience at Merck Canada after one year. Canadian Journal of Cardiology 2016;32(4):S1‐S2. [Google Scholar]
- Biddle SJ, Edwardson CL, Wilmot EG, Yates T, Gorely T, Bodicoat DH, et al. A randomised controlled trial to reduce sedentary time in young adults at risk of Type 2 Diabetes Mellitus: project STAND (Sedentary Time ANd Diabetes). PloS One 2015;10(12):e0143398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird ML, Shing C, Mainsbridge C, Cooley D, Pederson S. Activity behaviours of University staff in the workplace: A pilot study. Journal of Physical Activity and Health 2014 [Epub ahead of print];12(8):1128‐32. [DOI] [PubMed] [Google Scholar]
- Bjorklund M, Tronarp R, Granas M, Dahlgren G, McDonough S, Nyberg A, et al. Office‐cycling while working: an innovative concept to prevent and reduce musculoskeletal pain in office workers‐a controlled feasibility study. Physiotherapy 2015;101:eS155‐6. [Google Scholar]
- Boreham CA, Kennedy RA, Murphy MH, Tully M, Wallace WF, Young I. Training effects of short bouts of stair climbing on cardiorespiratory fitness, blood lipids, and homocysteine in sedentary young women. British Journal of Sports Medicine 2005;39(9):590‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchard DR, Strachan S, Johnson L, Moola F, Chitkara R, McMillan D, et al. Using shared treadmill workstations to promote less time spent in daily low intensity physical activities: A pilot study. Journal of Physical Activity and Health 2015;8:[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Brown DK, Barton JL, Pretty J, Gladwell VF. Walks4work: rationale and study design to investigate walking at lunchtime in the workplace setting. BMC Public Health 2012;12:550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchholz SW, Ingram D, Wilbur J, Fogg L, Sandi G, Moss A, et al. Bilingual Text4Walking food service employee intervention pilot study. JMIR mHealth and uHealth 2016;4(2):e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr LJ, Karvinen K, Peavler M, Smith R, Cangelosi K. Multicomponent intervention to reduce daily sedentary time: a randomised controlled trial. BMJ 2013;3(10):e003261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter SE, Jones M, Gladwell VF. Energy expenditure and heart rate response to breaking up sedentary time with three different physical activity interventions. Nutrition Metabolism and Cardiovascular Diseases 2015;25(5):503‐9. [DOI] [PubMed] [Google Scholar]
- Chae D, Kim S, Park Y, Hwang Y. The effects of an academic‐workplace partnership intervention to promote physical activity in sedentary office workers. Workplace Health & Safety 2015;63(6):259‐66. [DOI] [PubMed] [Google Scholar]
- Cheema BS, Houridis A, Busch L, Raschke‐Cheema V, Melville GW, Marshall PW, et al. Effect of an office worksite‐based yoga program on heart rate variability: outcomes of a randomised controlled trial. BMC Complementary and Alternative Medicine 2013;13:82. [DOI] [PMC free article] [PubMed] [Google Scholar]; Cheema BS, Marshall PW, Chang D, Colagiuri B, Machliss B. Effect of an office worksite‐based yoga program on heart rate variability: a randomised controlled trial. BMC Public Health 2011;11:578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia M, Chen B, Suppiah H. Office sitting made less sedentary – A future‐forward approach to reducing physical inactivity at work. Montenegrin Journal of Sports Science and Medicine 2015;4(2):5‐10. [Google Scholar]
- Cifuentes M, Jin Q, Fulmer S, Bello A. Facilitators and barriers to using treadmill workstations under real working conditions: a qualitative study in female office workers. American Journal of Health Promotion 2015;30(2):93‐100. [DOI] [PubMed] [Google Scholar]
- Clemes SA, Patel R, Mahon C, Griffiths PL. Sitting time and step counts in office workers. Occupational Medicine 2014;64(3):188‐92. [DOI] [PubMed] [Google Scholar]
- Cocker K, Bourdeaudhuij I, Cardon G, Vandelanotte C. Theory‐driven, web‐based, computer‐tailored advice to reduce and interrupt sitting at work: development, feasibility and acceptability testing among employee. BMC Public Health 2015;15(100968562):959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewa CS, Ruiter W, Chau N, Karioja K. Walking for wellness: using pedometers to decrease sedentary behaviour and promote mental health. International Journal of Mental Health Promotion 2009;11(2):24‐8. [Google Scholar]
- Elmer SJ, Martin JC. A cycling workstation to facilitate physical activity in office settings. Applied Ergonomics 2014;45(4):1240‐6. [DOI] [PubMed] [Google Scholar]
- Engelen L, Chau J, Bohn‐Goldbaum E, Young S, Hespe D, Bauman A. Is Active Design changing the workplace? ‐ a natural pre‐post experiment looking at health behaviour and workplace perceptions. Work 2017;56(2):229‐37. [DOI] [PubMed] [Google Scholar]
- Fennell C. The effects of a 16‐week exercise program and cell phone use on physical activity, sedentary behavior, and health‐related outcomes. Dissertation Abstracts International: Section B: The Sciences and Engineering 2017;78:3‐B(E). [Google Scholar]
- Foley B, Engelen L, Gale J, Bauman A, Mackey M. Sedentary behavior and musculoskeletal discomfort are reduced when office workers trial an activity based work environment. Journal of Occupational & Environmental Medicine 2016;58(9):924‐31. [DOI] [PubMed] [Google Scholar]
- Freak‐Poli R, Wolfe R, Backholer K, Courten M, Peeters A. Impact of a pedometer‐based workplace health program on cardiovascular and diabetes risk profile. Preventive Medicine 2011;53(3):162‐71. [DOI] [PubMed] [Google Scholar]
- Ganesan AN, Louise J, Horsfall M, Bilsborough SA, Hendriks J, McGavigan AD, et al. International mobile‐health intervention on physical activity, sitting, and weight: the Stepathlon cardiovascular health study. Journal of the American College of Cardiology 2016;67(21):2453‐63. [DOI] [PubMed] [Google Scholar]
- Gardner B, Smith L, Aggio D, Iliffe S, Fox KR, Jefferis BJ, et al. 'On Your Feet to Earn Your Seat': update to randomised controlled trial protocol. Trials 2015;16:330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson N, Faulker G, Murphy M, Umstattd Meyer M, Ryde G, McCarthy K, et al. An international study of an automated web‐based walking program (Walk@Work) to increase workday step counts in lower active office workers. Journal of Science and Medicine in Sport 2012;15:S235‐6. [Google Scholar]
- Gilson N, Ng N, Pavey T, Ryde G, Straker L, Brown W. Project energise: the impact of real‐time prompts on sedentary and physically active work time in Australian office workers. Journal of Science and Medicine in Sport 2015;19:e10. [DOI] [PubMed] [Google Scholar]
- Gilson N, Suppini A, Ryde G, Brown H, Brown W. Do height adjustable 'hot' desks change sedentary work behaviour in an open plan office?. Journal of Science and Medicine in Sport 2011;14:e24‐5. [Google Scholar]; Gilson ND, Suppini A, Ryde GC, Brown HE, Brown WJ. Does the use of standing 'hot' desks change sedentary work time in an open plan office?. Preventive Medicine 2012;54(1):65‐7. [DOI] [PubMed] [Google Scholar]
- Gorman E, Ashe MC, Dunstan DW, Hanson HM, Madden K, Winkler EA, et al. Does an 'activity‐permissive' workplace change office workers' sitting and activity time?. PLoS One 2013;8(10):e76723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green N, Sigurdsson S, Wilder DA. Decreasing bouts of prolonged sitting among office workers. Journal of Applied Behavior Analysis 2016;49(3):717‐22. [DOI] [PubMed] [Google Scholar]
- Grunseit A, Chau J, Ploeg H, Bauman A. Thinking on your feet: a qualitative evaluation of an installation of sit‐stand desks in a medium‐sized workplace. Journal of Science and Medicine in Sport 2012;15:S195‐6. [Google Scholar]
- Hadgraft NT, Winkler EA, Healy GN, Lynch BM, Neuhaus, M, Eakin EG, et al. Intervening to reduce workplace sitting: mediating role of social‐cognitive constructs during a cluster randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2017;14(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedge A, Ray EJ. Effect of an electronic height‐adjustable work surface on computer worker musculoskeletal discomfort and productivity. Proceedings of Human Factors & Ergonomic Society, 48th Annual Meeting 2004. SAGE publications, 2004. [Google Scholar]
- Irvine AB, Philips L, Seeley J, Wyant S, Duncan S, Moore RW. Get moving: a web site that increases physical activity of sedentary employees. American Journal of Health Promotion 2011;25(3):199‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jancey JM, McGann S, Creagh R, Blackford KD, Howat P, Tye M. Workplace building design and office‐based workers' activity: a study of a natural experiment. Australian & New Zealand Journal of Public Health 2016;40(1):78‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John D, Thompson DL, Raynor H, Bielak K, Rider B, Bassett DR. Treadmill workstations: a worksite physical activity intervention in overweight and obese office workers. Journal of Physical Activity and Health 2011;8(8):1034‐43. [DOI] [PubMed] [Google Scholar]
- Jones CA. Examining the efficacy and feasibility of digital activity monitors and shared active desks to reduce employee sedentary behavior. Dissertation Abstracts International: Section B: The Sciences and Engineering 2017;77:11‐B(E). [Google Scholar]
- Júdice PB, Hamilton MT, Sardinha LB, Silva AM. Randomized controlled pilot of an intervention to reduce and break‐up overweight/obese adults’ overall sitting‐time. Trials 2015;16(1):490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy RA, Boreham CA, Murphy MH, Young IS, Mutrie N. Evaluating the effects of a low volume stair climbing programme on measures of health‐related fitness in sedentary office workers. Journal of Sports Science and Medicine 2007;6(4):448‐54. [PMC free article] [PubMed] [Google Scholar]
- Kerr J, Takemoto M, Bolling K, Atkin A, Carlson J, Rosenberg D, et al. Two‐arm randomized pilot intervention trial to decrease sitting time and increase sit‐to‐stand transitions in working and non‐working older adults. Plos one 2016;11(1):e0145427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koepp GA, Manohar CU, McCrady‐Spitzer SK, Ben‐Ner A, Hamann DJ, Runge CF, et al. Treadmill desks: a 1‐year prospective trial. Obesity (Silver Spring) 2013;21(4):705‐11. [DOI] [PubMed] [Google Scholar]
- Lara A, Yancey AK, Tapia‐Conye R, Flores Y, Kuri‐Morales P, Mistry R, et al. Pausa para tu Salud: reduction of weight and waistlines by integrating exercise breaks into workplace organizational routine. Preventing Chronic DiseaseEpub 2008; Vol. 5, issue 1:A12. [PMC free article] [PubMed]
- Liu Y. Supporting working time interruption management through persuasive design. Dissertation Abstracts International: Section B: The Sciences and Engineering 2016;77:3‐B(E). [Google Scholar]
- Maeda H, Quartiroli A, Vos PW, Carr LJ, Mahar MT. Feasibility of retrofitting a university library with active workstations to reduce sedentary behavior. American Journal of Preventive Medicine 2014;46(5):525‐8. [DOI] [PubMed] [Google Scholar]
- Mahmud N, Kenny DT, Md Zein R, Hassan SN. The effects of office ergonomic training on musculoskeletal complaints, sickness absence, and psychological well‐being: a cluster randomized control trial. Asia‐Pacific Journal of Public Health 2015;27(2):NP1652‐68. [DOI] [PubMed] [Google Scholar]
- Mainsbridge CP, Cooley PD, Fraser SP, Pedersen SJ. The effect of an e‐health intervention designed to reduce prolonged occupational sitting on mean arterial pressure. Journal of Occupational and Environmental Medicine 2014;56(11):1189‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair JL, Boreham CA, Ditroilo M, McKeown D, Lowery MM, Caulfield B, et al. Benefits of a worksite or home‐based bench stepping intervention for sedentary middle‐aged adults ‐ a pilot study. Clinical Physiology and Functional Imaging 2014;34(1):10‐7. [DOI] [PubMed] [Google Scholar]
- Marshall AL, Leslie ER, Bauman AE, Marcus BH, Owen N. Print versus web site physical activity programs: a randomised trial. American Journal of Preventive Medicine 2003;25(2):88‐94. [DOI] [PubMed] [Google Scholar]
- McAlpine DA, Manohar CU, McCrady SK, Hensrud D, Levine JA. An office‐place stepping device to promote workplace physical activity. British Journal of Sports Medicine 2007;41(12):903‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyachi M, Kurita S, Tripette J, Takahara R, Yagi Y, Murakami H. Installation of a stationary high desk in the workplace: effect of a 6‐week intervention on physical activity. BMC Public Health 2015;15:368. [DOI] [PMC free article] [PubMed] [Google Scholar]; UMIN000016731. Installation of a stationary high desk in the workplace: effect of a 6‐week intervention on physical activity. UMIN‐CTR Clinical Trial (accessed 3 June 2015). [DOI] [PMC free article] [PubMed]
- NCT01221363. Reduction of sitting time ‐ a randomised controlled intervention study. http://clinicaltrials.gov/ct2/show/NCT01221363 (accessed 15 March 2014).
- Ognibene GT, Torres W, Eyben R, Horst KC. Impact of a sit‐stand workstation on chronic low back pain: results of a randomized trial. Journal of Occupational and Environmental Medicine 2016;58(3):287‐93. [DOI] [PubMed] [Google Scholar]
- Opdenacker J, Boen F. Effectiveness of face‐to‐face versus telephone support in increasing physical activity and mental health among university employees. Journal of Physical Activity and Health 2008;5(6):830‐43. [DOI] [PubMed] [Google Scholar]
- Ouyang P, Stewart KJ, Bedra ME, York S, Valdiviezo C, Finkelstein J. Text messaging to reduce inactivity using real‐time step count monitoring in sedentary overweight females. Circulation 2015;131:AMP10. [Google Scholar]
- ACTRN12612000743864. Can a participatory workplace intervention improve sedentary behaviour and physical activity in office workers?. http://www.anzctr.org.au/ACTRN12612000743864.aspx (accessed 14 March 2014). ; Parry S, Straker L, Gilson ND, Smith AJ. Participatory workplace interventions can reduce sedentary time for office workers ‐ a randomised controlled trial. PLoS One 2013;8(11):e78957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilcher JJ, Morris DM, Bryant SA, Merritt PA, Feigl HB. Decreasing sedentary behavior: effects on academic performance, meta‐cognition, and sleep. Frontiers in Neuroscience 2017;11(101478481):219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poirier J, Bennett WL, Jerome GJ, Shah NG, Lazo M, Yeh HC, et al. Effectiveness of an activity tracker‐ and internet‐based adaptive walking program for adults: a randomized controlled trial. Journal of Medical Internet Research 2016;18(2):e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk NP, Katz AS, Lowry M, Payfer JR. Reducing occupational sitting time and improving worker health: the Take‐a‐Stand Project. Preventing Chronic Disease 2012;9:e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roossien CC, Stegenga J, Hodselmans AP, Spook SM, Koolhaas W, Brouwer S, et al. Can a smart chair improve the sitting behavior of office workers?. Applied Ergonomics 2017;65:355‐61. [DOI] [PubMed] [Google Scholar]
- Schwartz B, Kapellusch JM, Schrempf A, Probst K, Haller M, Baca A. Effect of a novel two‐desk sit‐to‐stand workplace (ACTIVE OFFICE) on sitting time, performance and physiological parameters: protocol for a randomized control trial. BMC Public Health 2016;16(100968652):578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slootmaker SM, Chinapaw MJ, Schuit AJ, Seidell JC, Mechelen W. Feasibility and effectiveness of online physical activity advice based on a personal activity monitor: randomised controlled trial. Journal of Medical Internet Research 2009;11(3):e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternfeld B, Block C, Quesenberry CP Jr, Block TJ, Husson G, Norris JC, et al. Improving diet and physical activity with ALIVE: a worksite randomised trial. American Journal of Preventive Medicine 2009;36(6):475‐83. [DOI] [PubMed] [Google Scholar]
- Straker L, Abbott R, Heiden M, Mathiassen S, Toomingas A. Sit‐stand desks and sedentary behavior in Swedish call centre workers. Journal of Science and Medicine in Sport 2012;15:S194. [Google Scholar]; Straker L, Abbott RA, Heiden M, Mathiassen SE, Toomingas A. Sit‐stand desks in call centres: associations of use and ergonomics awareness with sedentary behavior. Applied Ergonomics 2013;44(4):517‐22. [DOI] [PubMed] [Google Scholar]
- Taylor WC, Paxton RJ, Shegog R, Coan SP, Dubin A, Page T, et al. Impact of booster breaks and computer prompts on physical activity and sedentary behavior among desk‐based workers: a cluster‐randomized controlled trial. Preventing Chronic Disease 2016;13(101205018):E155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01150084. Step by Step: a feasibility study of the promotion of lunchtime walking to increase physical activity and improve mental well‐being in sedentary employees. http://clinicaltrials.gov/ct2/show/NCT01150084 (accessed 15 March 2014). ; Thogersen‐Ntoumani C, Loughren E, Duda J, Fox KR. "Step by Step": a feasibility study of a lunchtime walking intervention designed to increase walking, improve mental well‐being and work performance in sedentary employees: rationale and study design. BMC Public Health 2010;10:578. [DOI] [PMC free article] [PubMed] [Google Scholar]; Thogersen‐Ntoumani C, Loughren E, Duda J, Fox KR. Step by Step: the feasibility of a 16‐week workplace lunchtime walking intervention for physically inactive employees. Journal of Physical Activity And Health 2013;10:Epub ahead of print. [DOI] [PubMed] [Google Scholar]; Thogersen‐Ntoumani C, Loughren EA, Kinnafick F‐E, Taylor IM, Duda JL, Fox KR. Changes in work affect in response to lunchtime walking in previously physically inactive employees: a randomized trial. Scandinavian Journal of Medicine & Science in Sports 2015;25(6):778‐87. [DOI] [PubMed] [Google Scholar]
- Thompson WG, Koepp GA, Levine JA. Increasing physician activity with treadmill desks. Work2014; Vol. 48, issue 1:47‐51. [DOI] [PubMed]
- Thorp AA, Kingwell BA, English C, Hammond L, Sethi P, Owen N. Alternating sitting and standing increases the workplace energy expenditure of overweight adults. Journal of Physical Activity and Health 2015;8:[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Torbeyns T, Geus B, Bailey S, Pauw K, Decroix L, Cutsem J, et al. Bike desks in the office: Physical health, cognitive function, work engagement, and work performance. Journal of Occupational & Environmental Medicine 2016;58(12):1257‐63. [DOI] [PubMed] [Google Scholar]
- Torbeyns T, Geus B, Bailey S, Decroix L, Meeusen R. The potential of bike desks to reduce sedentary time in the office: a mixed‐method study. Public Health 2017;144:16‐22. [DOI] [PubMed] [Google Scholar]
- Tucker S, Farrington M, Lanningham‐Foster LM, Clark MK, Dawson C, Quinn GJ. Worksite physical activity intervention for ambulatory clinic nursing staff. Workplace Health & Safety 2016;64(7):313‐25. [DOI] [PubMed] [Google Scholar]
- Nassau F, Chau JY, Lakerveld J, Bauman AE, Ploeg HP. Validity and responsiveness of four measures of occupational sitting and standing. The International Journal of Behavioral Nutrition and Physical Activity 2015;12:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirick SE. The promotion of regular exercise behavior among sedentary emerging adults based on social cognitive theory. Dissertation Abstracts International: Section B: The Sciences and Engineering 2016;76:7‐B(E). [Google Scholar]
- Yancey AK, McCarthy WJ, Taylor WC, Merlo A, Gewa C, Weber MD, et al. The Los Angeles Lift Off: a sociocultural environmental change intervention to integrate physical activity into the workplace. Preventive Medicine 2004;38(6):848‐56. [DOI] [PubMed] [Google Scholar]
- Østerås H, Sigbjørn H. The effectiveness of a pragmatic worksite physical activity program on maximal oxygen consumption and the physical activity level in healthy people. Journal of Bodywork and Movement Therapies 2006;10(1):51‐7. [Google Scholar]
References to studies awaiting assessment
- Carpenter K, Feltes L, Vuing B, Kalbes A, Koepp G, Dutta N, et al. Effect of sit‐stand workstations on metabolic risk in sedentary workers: a randomized controlled trial. The Journal of the Federation of American societies for Experimental Biology 2015;29:supplement 1. [Google Scholar]
- Dutta N, Koepp G, Schmitz C, Stovitz SD, Levine JA, Pereira MA. Impact of adjustable sit‐stand workstations on physical activity in sedentary office workers. Diabetes 2013;62:A186. [Google Scholar]
- Kirk A, Fitzsimons C, Murphy M, Mutrie N. Effect of a person centred consultation intervention to reduce the sedentary behaviour of working Scottish adults. Journal of Science and Medicine in Sport 2012;15:S314. [Google Scholar]
- NCT02932787. Effects of installing height‐adjustable workstations on office workers workplace sitting time and productivity. https://clinicaltrials.gov/show/NCT02932787 (accessed 12 September 2017).
References to ongoing studies
- ACTRN12612001290886. The effectiveness of the 10,000 Steps workplace challenge in increasing health outcomes for employees at Rockhampton Regional Council. http://www.anzctr.org.au/ACTRN12612001290886.aspx (accessed 15 March 2014).
- ACTRN12614000252617. Comparison of organisational support vs. organisational plus technology support for reducing prolonged sitting in the office workplace. http://www.anzctr.org.au/ACTRN12614000252617.aspx (accessed 15 March 2014).
- Bergman F, Boraxbekk CJ, Wennberg P, Sörlin A Olsson T. Increasing physical activity in office workers – the Inphact Treadmill study; a study protocol for a 13‐month randomized controlled trial of treadmill workstations. BMC Public Health 2015;15(1):632. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT01997970. NEAT ‐ Prevention and treatment of overweight and obesity. (InphactUm). https://clinicaltrials.gov/ct2/show/NCT01997970 (accessed 3 June 2015).
- Buman MP, Mullane SL, Toledo MJ, Rydell SA, Gaesser GA, Crespo NC, et al. An intervention to reduce sitting and increase light‐intensity physical activity at work: design and rationale of the 'Stand & Move at Work' group randomized trial. Contemporary Clinical Trials 2017;53:11‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT02566317. Stand & Move at Work. https://clinicaltrials.gov/ct2/show/NCT02566317 (accessed 12 September 2017).
- ACTRN12611000742976. Stand Up Victoria: a trial to determine whether environmental modification and behavioural counselling can lead to reductions in workplace sitting time in office workers. http://www.anzctr.org.au/ACTRN12611000742976.aspx (accessed 15 March 2014). ; Dunstan DW, Wiesner G, Eakin EG, Neuhaus M, Owen N, LaMontagne AD, et al. Reducing office workers' sitting time: rationale and study design for the Stand Up Victoria cluster randomised trial. BMC Public Health 2013;13:1057. [DOI] [PMC free article] [PubMed] [Google Scholar]; Neuhaus M, Healy GN, Fjeldsoe BS, Lawler S, Owen N, Dunstan DW, et al. Iterative development of Stand Up Australia: a multi‐component intervention to reduce workplace sitting. International Journal of Behavioral Nutrition and Physical Activity 2014;11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein EA, Sahasranaman A, John G, Haaland, BA, Bilger M, Sloan RA, et al. Design and baseline characteristics of participants in the TRial of Economic Incentives to Promote Physical Activity (TRIPPA): a randomized controlled trial of a six month pedometer program with financial incentives. Contemporary Clinical Trials 2015;41:238‐47. [DOI] [PubMed] [Google Scholar]; NCT01855776. A randomized trial of economic incentives to promote walking among full time employees. https://clinicaltrials.gov/ct2/show/NCT01855776 (accessed 12 September 2017).
- Finni T, Saakslahti A, Laukkanen A, Pesola A, Sipilä S. A family based tailored counselling to increase non‐exercise physical activity in adults with a sedentary job and physical activity in their young children: design and methods of a year‐long randomised controlled trial. BMC Public Health2011; Vol. 11. [DOI] [PMC free article] [PubMed]; ISRCTN28668090. Actions to reduce sedentary time in parents and their young children. http://www.isrctn.com/ISRCTN28668090 (accessed 15 March 2014).
- Hall J, Mansfield L, Kay T, McConnell AK. The effect of a sit‐stand workstation intervention on daily sitting, standing and physical activity: protocol for a12 month workplace randomised control trial. BMC Public Health 2015;15:152. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT02172599. Take a stand for workplace health: A sit‐stand workstation project evaluation. https://clinicaltrials.gov/ct2/show/NCT02172599?term=workplace+and+sitting&rank=1 (accessed 3 June 2015).
- ISRCTN25767399. Impact of Booster Breaks on physical activity among sedentary employees: a cluster randomized controlled trial. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN25767399 (accessed 3 June 2015).
- ACTRN12610000301066. Walking to Wellness in an ageing sedentary university community. http://www.anzctr.org.au/ACTRN12610000301066.aspx (accessed 15 March 2014). ; Mackey M, Bohle P, Taylor P, Biase T, McLoughlin C, Purnell K. 'Walking to wellness' in an ageing sedentary university community‐a randomised controlled feasibility study. Physiotherapy. 2011; Vol. 97:eS733‐eS4. [Google Scholar]; Mackey MG, Bohle P, Taylor P, Biase T, McLoughlin C, Purnell K. Walking to wellness in an ageing sedentary university community: design, method and protocol. Contemporary Clinical Trials 2011;32(2):273‐9. [DOI] [PubMed] [Google Scholar]
- ISRCTN44827407. Does using sit‐stand desks at work affect how many calories people burn and how much time they spend sitting over the entire day? A feasibility study. http://www.isrctn.com/ISRCTN44827407 (accessed 12 September 2017). ; Mantzari E, Wijndaele K, Brage S, Griffin SJ, Marteau TM. Impact of sit‐stand desks at work on energy expenditure and sedentary time: protocol for a feasibility study. Pilot and Feasibility Studies 2016;2(30):eCollection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borras CM, Garriga MG, Martinez E, Cantera CM, Puigdoménech E, Solà M, et al. Effectiveness of a primary care‐based intervention to reduce sitting time in overweight and obese patients (SEDESTACTIV): a randomised controlled trial; rationale and study design. BMC Public Health2014; Vol. 14. [DOI] [PMC free article] [PubMed]; NCT01729936. SedestActiv Project: intervention to reduce diary hours of sitting time in overweight and obese patients. http://clinicaltrials.gov/ct2/show/NCT01729936 (accessed 15 March 2014).
- NCT01787643. Standing behavior after installation of height‐adjustable desks. http://clinicaltrials.gov/ct2/show/NCT01787643 (accessed 15 March 2014).
- NCT01846013. Increasing workplace physical activity in sedentary office workers. http://clinicaltrials.gov/ct2/show/NCT01846013 (accessed 15 March 2014).
- NCT02376504. Modifying the workplace to decrease sedentary behavior and improve health. https://clinicaltrials.gov/ct2/show/NCT02376504?term=workplace+and+sitting&rank=3 (accessed 3 June 2015).
- NCT02609282. The impact of hourly prompts on reducing prolonged sitting at work. https://clinicaltrials.gov/show/NCT02609282 (accessed 12 September 2017).
- NCT02785640. A study to assess the impact of a multicomponent intervention to reduce prolonged sitting in the workplace. https://clinicaltrials.gov/show/NCT02785640 (accessed 12 September 2017).
- NCT03236597. Assessing the effects of treadmill and sit‐to‐stand desks on light physical activity, sitting time, and cardio‐metabolic risk. https://clinicaltrials.gov/show/NCT03236597 (accessed 12 September 2017).
- ISRCTN10967042. SMArT Work: Stand More AT Work. http://www.isrctn.com/ISRCTN10967042 (accessed 25 December 2015). ; O’Connell SE, Jackson BR, Edwardson CL, Yates T, Biddle SJH, Davies MJ, et al. Providing NHS staff with height‐adjustable workstations and behaviour change strategies to reduce workplace sitting time:protocol for the Stand More AT (SMArT)Work cluster randomised controlled trial. BMC Public Health 2015;15:1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ACTRN12613000366752. Reducing sedentary behaviour in office workers. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=363960 (accessed 15 March 2014). ; Radas A, Mackey M, Leaver A, Bouvier AL, Chau JY, Shirley D, et al. Evaluation of ergonomic and education interventions to reduce occupational sitting in office‐based university workers: study protocol for a randomised controlled trial. Trials2013; Vol. 14. [DOI] [PMC free article] [PubMed]
- Hoye K, Boen F, Lefevre J. The effects of physical activity feedback on behavior and awareness in employees: study protocol for a randomised controlled trial. International Journal of Telemedicine and Applications 2012;2012:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
- Aadahl M, Jorgensen T. Validation of a new self‐report instrument for measuring physical activity. Medicine and Science in Sports and Exercise 2003;35(7):1196‐202. [DOI] [PubMed] [Google Scholar]
- The Royal Australasian College of Physicians. Australasian Faculty of Occupational and Environmental Medicine. https://www.racp.edu.au/page/about‐afoem (accessed 12 December 2014).
- Australian Institute of Health and Welfare. Australia's health 2008. http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=6442453674 (accessed 15 September 2013).
- Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Medicine and Science in Sports and Exercise 2000;32(9 Suppl):S498‐504. [DOI] [PubMed] [Google Scholar]
- Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DRJ, Tudor‐Locke C, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Medicine and Science in Sports and Exercise 2011;43(8):1575‐81. [DOI] [PubMed] [Google Scholar]
- Andersen JH, Haahr JP, Frost P. Risk factors for more severe regional musculoskeletal symptoms: a two‐year prospective study of a general working population. Arthritis and rheumatism 2007;56(4):1355‐64. [DOI] [PubMed] [Google Scholar]
- Atkinson J, Haynes K. Standing meeting rooms – exploring enablers and barriers of interventions to reduce sitting time in the workplace. Australian and New Zealand Journal of Public Health June 2014;38(3):291‐2. [DOI] [PubMed] [Google Scholar]
- Australian Government, Department of Health and Aging. Make your Move – sit less. Be active for life! Australia's physical activity and sedentary behaviour guidelines. Canberra: Commonwealth of Australia. http://www.health.gov.au/internet/main/publishing.nsf/content/health‐pubhlth‐strateg‐phys‐act‐guidelines#npa052014.
- Bailey DP, Locke CD. Breaking up prolonged sitting with light‐intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. Journal of Science and Medicine in Sport 2015;18(3):294‐8. [DOI] [PubMed] [Google Scholar]
- Beers EA, Roemmich JN, Epstein LH, Horvath PJ. Increasing passive energy expenditure during clerical work. European Journal of Applied Physiology 2008;103(3):353‐60. [DOI] [PubMed] [Google Scholar]
- Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low‐intensity activity. The Journal of Physiology 2003;1(551):673‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botter J, Ellegast RP, Burford EM, Weber B, Könemann R, Commissaris DA. Comparison of the postural and physiological effects of two dynamic workstations to conventional sitting and standing workstations. Ergonomics 2015;(Epub ahead of print):1‐15. [DOI] [PubMed] [Google Scholar]
- Buckley JP, Hedge A, Yates T, Copeland RJ, Loosemore M, Hamer M, et al. The sedentary office: an expert statement on the growing case for change towards better health and productivity. British Journal of Sports Medicine 2015;49(21):1357‐62. [DOI] [PubMed] [Google Scholar]
- Campbell MK, Mollison J, Grimshaw JM. Cluster trials in implementation research: estimation of intracluster correlation coefficients and sample size. Statistics in Medicine 2001;20(3):391‐9. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Saunders TJ, Tremblay MS, Katzmarzyk PT, Tremblay A, Bouchard C. Workplace standing time and the incidence of obesity and type 2 diabetes: a longitudinal study in adults. BMC Public Health 2015;10(15):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau JY, Ploeg HP, Dunn S, Kurko J, Bauman AE. Validity of the occupational sitting and physical activity questionnaire. Medicine and Science in Sports and Excercise 2012;44(1):118‐25. [DOI] [PubMed] [Google Scholar]
- Chaua JY, Grunseita A, Midthjellb K, Holmen J, Holmenabb TL, Baumana AE, et al. Cross‐sectional associations of total sitting and leisure screen time with cardio metabolic risk in adults. Results from the HUNT study, Norway. Journal of Science and Medicine in Sport 2014;17:78‐84. [DOI] [PubMed] [Google Scholar]
- Clark BK, Sugiyama T, Healy GN, Salmon J, Dunstan DW, Owen N. Validity and reliability of measures of television viewing time and other non‐occupational sedentary behaviour of adults: a review. Obesity Reviews 2009;10(1):7‐16. [DOI] [PubMed] [Google Scholar]
- Coenen P, Healy GN, Winkler E, Dunstan DW, Straker L. Musucloskeletal pain is a barrier for sedentary behavior interventions. Proceedings 19th triennial congress of the IEA. Melbourne, 2015. [Google Scholar]
- Commissaris DACM, Douwes M, Schoenmaker N, Korte EM. Recommendations for sufficient physical activity at work. 2007. http://www.nordiskergonomi.org/nes2007/CD_NES_2007/papers/A79_Commissaris.pdf. Elsevier, Oxford, (accessed 25 November 2013).
- Commissaris DACM, Konemann R, Mastrigt SH, Burford EM, Botter J, Douwes M, et al. Effects of a standing and three dynamic workstations on computer task performance and cognitive function tests. Applied Ergonomics 2014;45:1570‐8. [DOI] [PubMed] [Google Scholar]
- Commissaris DACM, Huysmans MA, Mathiassen SE, Srinivasan D, Koppes LLJ, Hendriksen IJM. Interventions to reduce sedentary behavior and increase physical activity during productive work: a systematic review. Scandinavian Journal of Work Environment and Health 2016;42:181‐91. [DOI] [PubMed] [Google Scholar]
- Cooley D, Pedersen S, Mainsbridge C. Assessment of the impact of a workplace intervention to reduce prolonged occupational sitting time. Qualitative Health Research2014; Vol. 24:90‐101. [DOI] [PubMed]
- Craft LL, Zderic TW, Gapstur SM, Vaniterson EH, Thomas DM, Siddique J, et al. Evidence that women meeting physical activity guidelines do not sit less: an observational inclinometry study. International Journal of Behavioral Nutrition and Physical Activity 2012;9:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig CL, Brownson RC, Cragg SE, Dunn AL. Exploring the effect of the environment on physical activity: a study examining walking to work. American Journal of Preventive Medicine 2002;23(2 Suppl):36‐43. [DOI] [PubMed] [Google Scholar]
- Department of Health. Start active, stay active: a report on physical activity for health from the Four Home Countries' Chief Medical Officers. London, UK: Department of Health. https://www.gov.uk/government/publications/start‐active‐stay‐active‐a‐report‐on‐physical‐activity‐from‐the‐four‐home‐countries‐chief‐medical‐officers2011.
- Dunstan DW, Thorp AA, Healy N. Prolonged sitting: is it a distinct coronary heart disease risk factor?. Current Opinion in Cardiology 2011;26(5):412‐9. [DOI] [PubMed] [Google Scholar]
- Duvivier BM, Schaper NC, Bremers MA, Crombrugge G, Menheere PP, Kars M, et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS ONE 2013;8(2):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochrane Effective Practice and Organisation of Care Group. EPOC resources for review authors. http://epoc.cochrane.org/epoc‐resources‐review‐authors (accessed 10 June 2014).
- Franklin BA. Health implications of low cardiorespiratory fitness, too little exercise, and too much sitting time: changing paradigms and perceptions. American Journal of Health Promotion 2011;25(4):exi‐v. [DOI] [PubMed] [Google Scholar]
- Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJH. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychology Review 2015;16:1‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomersall SR, Rowlands AV, English C, Maher C, Olds TS. The Activitystat hypothesis: The concept,the evidence and the methodologies. Sports Medicine 2013;43(2):135‐49. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist G, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. Rating quality of evidence and strength of recommendations GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graf M, Krieger R, Läubli T, Martin B. Should we recommend people to stand more than sit at work?. Proceedings 19th triennial congress of the IEA. Melbourne, 2015. [Google Scholar]
- Healy GN, Clark BK, Winkler EA, Gardiner PA, Brown WJ, Matthews CE. Measurement of adults’ sedentary time in population‐based studies. American Journal of Preventive Medicine 2011;41:216‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Spiegelhalter DJ. A re‐evaluation of random‐effects meta‐analysis. Journal of Royal Statistical Society. Series A, (Statistics in Society) 2009;172(1):137‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
- Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviours in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 2003;289(14):1785‐91. [DOI] [PubMed] [Google Scholar]
- Ijaz S, Verbeek JH, Mischke C, Ruotsalainen J. Inclusion of non randomized studies in Cochrane systematic reviews was found to be in need of improvement. Journal of Clinical Epidemiology 2014;67(6):645‐53. [DOI: 10.1016/j.jclinepi.2014.01.001; PUBMED: 24725644] [DOI] [PubMed] [Google Scholar]
- IntHout J, Ioannidis JPA, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta‐analysis. BMJ Open 2016;6:e010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen X, Cliff DP. Issues related to measuring and interpreting objectively measured sedentary behavior data. Measurement in Physical Education and Exercise Science 2015;19(3):116‐24. [Google Scholar]
- John D, Bassett D, Thompson D, Fairbrother J, Baldwin D. Effect of using a treadmill workstation on performance of simulated office work tasks. Journal of Physical Activity and Health 2009;6(5):617‐24. [DOI] [PubMed] [Google Scholar]
- Júdice PB, Hamilton MT, Sardinha LB, Zderic TW, Silva AM. What is the metabolic and energy cost of sitting, standing and sit/stand transitions?. European Journal of Applied Physiology 2015;116(2):263‐73. [DOI] [PubMed] [Google Scholar]
- Kanoun N. Validation of the ActivPAL activity monitor as a measure of walking at pre‐determined slow walking speeds in a healthy population in a controlled setting. Reinvention: a Journal of Undergraduate Research 2009, http://www.warwick.ac.uk/go/reinventionjournal/issues/volume2issue2/kanoun (accessed 13 November 2013).
- Katzmarzyk PT. Standing and mortality in a prospective cohort of Canadian adults. Medicine and Science in Sports and Exercise 2014;46(5):940‐6. [DOI] [PubMed] [Google Scholar]
- Kim Y, Barry VW, Kang M. Validation of the ActiGraph GT3X and activPAL accelerometers for the assessment of sedentary behavior. Measurement in Physical Education and Exercise Science 2015;19(3):125‐37. [Google Scholar]
- Lagersted‐Olsen J, Korshøj M, Skotte J, Carneiro IG, Søgaard K, Holtermann A. Comparison of objectively measured and self‐reported time spent sitting. International Journal of Sports Medicine 2014;35(6):534‐40. [DOI] [PubMed] [Google Scholar]
- Larsen RN, Kingwell BA, Sethi P, Cerin E, Owen N, Dunstan DW. Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutrition Metabolism and Cardiovascular Diseases 2014;24(9):976‐82. [DOI] [PubMed] [Google Scholar]
- Levine JA, Miller JM. The energy expenditure of using a "walk‐and‐work" desk for office workers with obesity. British Journal of Sports Medicine 2007;41(9):558‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manini TM, Carr LJ, King AC, Marshall S, Robinson TN, Rejeski WJ. Interventions to reduce sedentary behavior. Medicine and Science in Sports and Exercise 2015;47(6):1306‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansoubi M, Pearson N, Biddle SJ, Clemes S. The relationship between sedentary behaviour and physical activity in adults: a systematic review. Preventive Medicine 2014;69C:28. [DOI] [PubMed] [Google Scholar]
- Mansoubi M, Pearson N, Clemes SA, Biddle SJH, Bodicoat DH, Tolfrey K, et al. Energy expenditure during common sitting and standing tasks: examining the 1.5 MET definition of sedentary behaviour. BMC Public Health 2015;15:516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansoubi M, Pearson N, Biddle SJH, Clemes SA. Using sit‐to‐stand workstations in offices: is there a compensation effect?. Medicine & Science in Sports & Excercise 2016;48:720‐5. [DOI] [PubMed] [Google Scholar]
- Marszalek J, Morgulec‐Adamowicz N, Rutkowska I, Kosmol A. Using ecological momentary assessment to evaluate current physical activity. BioMed Research International 2014;Article ID 915172:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin A, Fitzsimons C, Jepson R, Saunders DH, Ploeg HP, Teixeira PJ, et al. Interventions with potential to reduce sedentary time in adults: systematic review and meta‐analysis. British Journal of Sports Medicine 2015;49(16):1056‐63. [DOI] [PubMed] [Google Scholar]
- McCrady SK, Levine JA. Sedentariness at work: how much do we really sit?. Obesity (Silver Spring, Md) 2009;17(11):2103‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEachan RR, Lawton RJ, Jackson C, Conner M, Meads DM, West RM. Testing a workplace physical activity intervention: a cluster randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2011;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obesity Reviews 2012;13(8):659‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogilvie D, Foster CE, Rothnie H, Cavill N, Hamilton V, Fitzsimons CF, et al. Interventions to promote walking: systematic review. BMJ 2007;334(7605):1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry S, Straker L. The contribution of office work to sedentary behaviour associated risk. BMC Public Health 2013;13(1):296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedišić Ž, Bauman A. Accelerometer‐based measures in physical activity surveillance: current practices and issues. British Journal of Sports Medicine 2015;49(4):219‐23. [DOI] [PubMed] [Google Scholar]
- Pedišić Z, Dumuid D, Olds TS. Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time‐use epidemiology: definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiology2017; Vol. 49, issue 2.
- Plotnikoff R, Karunamuni N. Reducing sitting time: the new workplace health priority. Archives of Environmental and Occupational Health 2012;67(3):125‐7. [DOI] [PubMed] [Google Scholar]
- Prince SA, Saunders TJ, Gresty K, Reid RD. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta‐analysis of controlled trials. Obesity Reviews 2014;15(11):905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- Ryan CG, Dall PM, Granat MH, Grant PM. Sitting patterns at work: objective measurement of adherence to current recommendations. Ergonomics 2011;54(6):531‐8. [Google Scholar]
- Rzewnicki R, Yves VA, Ilse DB. Addressing over reporting on the International Physical Activity Questionnaire (IPAQ) telephone survey with a population sample. Public Health Nutrition 2003;6(3):299‐305. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. An ecological approach to creating active living communities. Annual Review of Public Health 2006;27:297‐322. [DOI] [PubMed] [Google Scholar]
- Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. British Journal of Sports Medicine 2003;37(3):197‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha N, Pedisic Z, Neil‐Sztramko S, Kukkonen‐Harjula KT, Hermans V. The impact of obesity in the workplace: a review of contributing factors, consequences and potential solutions. Current Obesity Reports 2016;5(3):344‐60. [DOI] [PubMed] [Google Scholar]
- Shrestha N, Grgic J, Wiesner G, Parker A, Podnar H, Bennie JA, et al. Effectiveness of interventions for reducing non‐occupational sedentary behaviour in adults and older adults: a systematic review and meta‐analysis. British Journal of Sports Medicine2018; Vol. Epub ahead of print. [DOI] [PubMed]
- Tan DA. Changing disease trends in the Asia‐Pacific. Climacteric 2011;14(5):529‐34. [DOI] [PubMed] [Google Scholar]
- Thorp AA, Healy GN, Winkler E, Clark BK, Gardiner PA, Owen N, et al. Prolonged sedentary time and physical activity in workplace and non‐work contexts: a cross‐sectional study of office, customer service and call centre employees. International Journal of Behavioral Nutrition and Physical Activity 2012;9:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor‐Locke C, Schuna JM Jr, Frensham LJ, Proenca M. Changing the way we work: elevating energy expenditure with workstation alternatives. International Journal of Obesity 2013;38(6):755‐6. [DOI] [PubMed] [Google Scholar]
- United States Patent and Trademark Office (USPTO). United States Patent 6,070,943. Guery‐Strahm R. Ergonomic seating unit. June 6, 2000. http://patft.uspto.gov/netacgi/nph‐Parser?Sect2=PTO1&Sect2=HITOFF&p=1&u=/netahtml/PTO/search‐bool.html&r=1&f=G&l=50&d=PALL&RefSrch=yes&Query=PN/6070943 (accessed 2 December 2013).
- Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all‐cause mortality risk in 222 497 Australian adults. Archives of Internal Medicine 2012;172(6):494‐500. [DOI] [PubMed] [Google Scholar]
- Uffelen JG, Wong J, Chau JY, Ploeg HP, Riphagen I, Gilson ND, et al. Occupational sitting and health risks: a systematic review. American Journal of Preventive Medicine 2010;39(4):379‐88. [DOI] [PubMed] [Google Scholar]
- Victorian Health Promotion Foundation. Reducing prolonged sitting in the workplace. An evidence review: summary report. 2012. http://www.vichealth.vic.gov.au/˜/media/ResourceCentre/PublicationsandResources/Economic%20participation/2012%20workplace/VH_Reducing_prolonged_sitting_07.ashx (accessed 4 December 2013).
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378(9793):815‐25. [DOI] [PubMed] [Google Scholar]
- World Health Organization/World Economic Forum. Preventing non communicable diseases in the workplace through diet and physical activity. http://www.weforum.org/pdf/Wellness/WHOWEF_report.pdf 2008, (accessed 10 June 2014).
- Wilks S, Mortimer M, Nylén P. The introduction of sit‐stand worktables; aspects of attitudes, compliance and satisfaction. Applied Ergonomics 2006;37(3):359‐65. [DOI] [PubMed] [Google Scholar]


