Abstract
B cell superantigens, also called immunoglobulin superantigens, bind to the variable regions of either the heavy or light chain of immunoglobulins mirroring the lymphocyte-activating properties of classical T cell superantigens. Protein A of Staphylococcus aureus, protein L of Peptostreptococcus magnus, and gp120 of HIV are typical immunoglobulin superantigens. Mast cells are immune cells expressing the high-affinity receptor for IgE (FcεRI) and are strategically located in the human heart, where they play a role in several cardiometabolic diseases. Here, we investigated whether immunoglobulin superantigens induced the activation of human heart mast cells (HHMCs). Protein A induced the de novo synthesis of cysteinyl leukotriene C4 (LTC4) from HHMCs through the interaction with IgE VH3+ bound to FcεRI. Protein L stimulated the production of prostaglandin D2 (PGD2) from HHMCs through the interaction with κ light chains of IgE. HIV glycoprotein gp120 induced the release of preformed (histamine) and de novo synthesized mediators, such as cysteinyl leukotriene C4 (LTC4), angiogenic (VEGF-A), and lymphangiogenic (VEGF-C) factors by interacting with the VH3 region of IgE. Collectively, our data indicate that bacterial and viral immunoglobulin superantigens can interact with different regions of IgE bound to FcεRI to induce the release of proinflammatory, angiogenic, and lymphangiogenic factors from human cardiac mast cells.
Keywords: angiogenesis, heart, histamine, IgE, leukotriene C4, lymphangiogenesis, mast cells, myocardial infarction, prostaglandin D2, superantigens
1. Introduction
The term “superantigen” (SAg) refers to several proteins synthesized by a variety of bacteria and viruses that not only mimic, but also exceed the activity of conventional antigens in activating T and B cells [1,2,3,4,5]. Typical antigens are processed by antigen-presenting cells (APCs) into small peptides that bind a distal groove in the molecules of the major histocompatibility complex (MHC) [6]. The peptide: MHC (p:MHC) complex on the APC surface acts as a ligand of both T cell receptor (TCR) α and TCR β variable domains on a few specific T cell clones. By contrast, SAgs bind directly to the lateral surfaces of the MHC class II molecules and to the Vβ domain of the TCR and thus bypass the processing and presentation of conventional antigens by APCs [7,8,9,10]. As a result, conventional antigens stimulate less than 1 in 10,000–100,000 T cells, while SAgs can stimulate up to 20% of all T cells [1,3]. A wide range of diseases from autoimmune and allergic disorders, neoplasia, and immunodeficiencies can be associated with SAgs [11,12,13,14,15].
In addition to classical T cell Sags, there are also B cell SAgs endowed with immunoglobulin (Ig)-binding capacity. In contrast to conventional antigens, which bind to both the heavy and light chain variable (V)-domains of Igs, B cell SAgs bind to the conserved sides of either the heavy (H)- or light (L)-chain [16,17,18], resulting in a massive proliferation of B cells. Staphylococcus aureus (S. aureus) is a source of several T cell SAgs (S. aureus enterotoxins: SE) [19]. Two staphylococcal B cell SAgs, S. aureus protein A and SEA, bind specifically to VH3 domain of human Igs, whereas SED, which is also a T cell SAg, binds to VH4 [11]. VH3 is the largest of human Ig germline VH families; thereby, protein A can stimulate almost half of the B cells in the circulation [17]. Protein A is the archetypal B cell SAg and contains five homologous repeated domains, each of which can bind to all or most of the VH3+ Igs. S. aureus is a common pathogen causing toxic shock syndrome and endocarditis [20,21]. Most of clinical isolates of S.aureus synthesize protein A, which can be released from the cell wall [22]. Protein A has two binding sites for human Igs: the classical site binds Fcγ, a constant region of IgG [23] and an alternative site that binds the Fab portion of 15% to 50% of human polyclonal IgG, IgM, IgA, and IgE [24].
Similarly, glycoprotein 120 (gp120) of HIV-1 is a viral B cell SAg, because it interacts with Ig VH3+ [25,26]. The entry of HIV into host cells is mediated the interaction of viral glycoprotein [27] gp120 with CD4 [28] and chemokine receptors on the cell surface [29,30]. HIV gp120 is a member of the Ig SAg family [31,32,33]. Emergence of cardiovascular disease has become a leading concern for patients with HIV infection [34,35].
Protein L is a cell wall protein synthesized by Peptostreptococcus magnus (P. magnus) [36]. Protein L is a multi-domain protein that binds to some κ light chain variable domain without interfering with the antigen-binding site [37,38]. Protein L binds to the V domain of the κ light chains of Igs [39,40,41]. In particular, protein L binds with high affinity (~1010 M−1) only human Vk I, Vk III and Vk IV subtypes, but does not interact with Vk II subtype [42].
Mast cells are tissue resident immune cells present in most connective tissues including murine [43,44,45], canine [46,47], and human heart [48,49,50,51]. Mast cells are canonically considered key effectors of allergic responses [52,53,54,55,56] and are critical sentinels in immunity [57,58]. Mast cells and their mediators participate in a variety of pathophysiological processes including response to infections [58,59,60], angiogenesis [61,62,63,64,65], lymphangiogenesis [61,66], autoimmune disorders [67,68,69], cancer [70,71,72,73], and cardiometabolic diseases [49,74,75,76,77,78].
Human mast cells express the high-affinity receptor (FcεRI) for immunoglobulin E (IgE) and cross-linking of the IgE-FcεRI network induces the release of preformed (e.g., histamine, tryptase, chymase) and de novo synthesized lipid mediators (e.g., prostaglandin D2 (PGD2), cysteinyl leukotriene C4 (LTC4)). We have previously shown that several immune cells, such as human lung mast cells [61], basophils [79], macrophages [80,81], and neutrophils [82], produce angiogenic (e.g., vascular endothelial growth factor A:VEGF-A) and/or lymphangiogenic factors (e.g., vascular endothelial growth factor C: VEGF-C) [52,61,81]. However, there is a marked heterogeneity of human mast cells with respect to the mediators released from cells isolated from different anatomic sites [83,84,85].
This study has been undertaken to evaluate whether bacterial (protein A and protein L) and viral (gp120) superantigens induce the release of proinflammatory, angiogenic, and lymphangiogenic factors from human cardiac mast cells.
2. Results
2.1. Effect of Human IgG Anti-IgE on Mediator Release from HHMCs
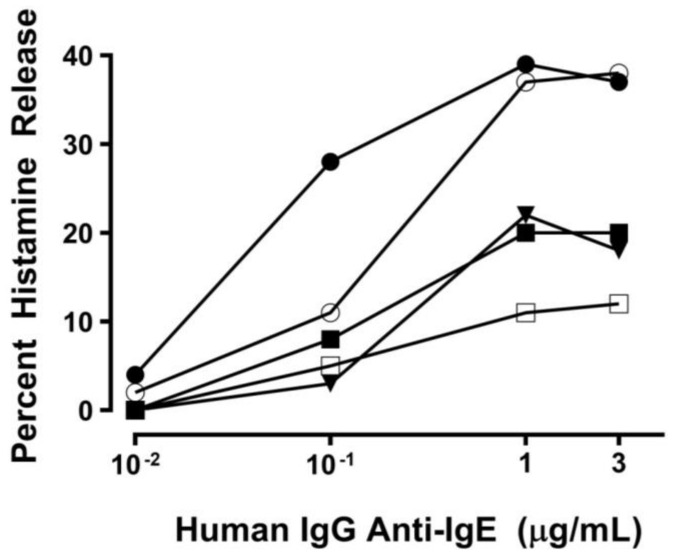
We have previously reported that IgG anti-IgE purified from the serum of a small percentage of atopic dermatitis patients can induce histamine and LTC4 release from human basophils [86]. The activating property of human IgG anti-IgE (H-aIgE) is mediated by the interaction with membrane-bound IgE on human basophils. Therefore, we used this human autoantibody to activate human heart mast cells (HHMCs) in vitro. Figure 1 shows that H-aIgE (10−2 to 3 μg/mL) induced a concentration-dependent histamine release from five different preparations of HHMCs. Four preparations of IgG (10−2 to 3 μg/mL) purified from the serum of normal donors did not cause histamine release (data not shown). These results suggest that mast cells isolated from human heart express IgE bound to FcεRI.
Figure 1.
Effect of increasing concentrations of human IgG anti-IgE purified from the serum of a patient with atopic dermatitis [86] on histamine release from five different preparations of human heart mast cells (HHMCs). HHMCs were incubated (45 min at 37 °C) with the indicated concentrations of human IgG anti-IgE. Each point shows the mean of duplicate determinations. Each symbol represents the results from an individual donor.
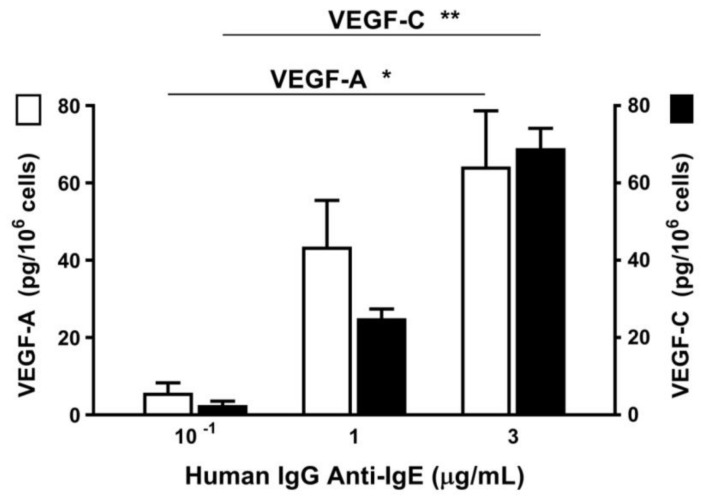
Vascular endothelial growth factors (VEGFs) are involved in new vessel formation and play a central role in cardiac pathophysiology [87]. Therefore, we evaluated the release of angiogenic (VEGF-A) and lymphangiogenic factors (VEGF-C) induced by H-aIgE from HHMCs. Figure 2 shows that H-aIgE induced a concentration-dependent release of both VEGF-A and VEGF-C from four different preparations of HHMCs.
Figure 2.
Effect of increasing concentrations of human IgG anti-IgE on the release of vascular endothelial growth factor-A (VEGF-A) and vascular endothelial growth factor-C (VEGF-C) from HHMCs from four donors. HHMCs were incubated (6 h at 37 °C) in the presence of the indicated concentrations of human IgG anti-IgE. Each bar is the mean ± SEM. * p < 0.05; ** p < 0.01.
2.2. Effect of Bacterial Superantigens on Mediator Release from HHMCs
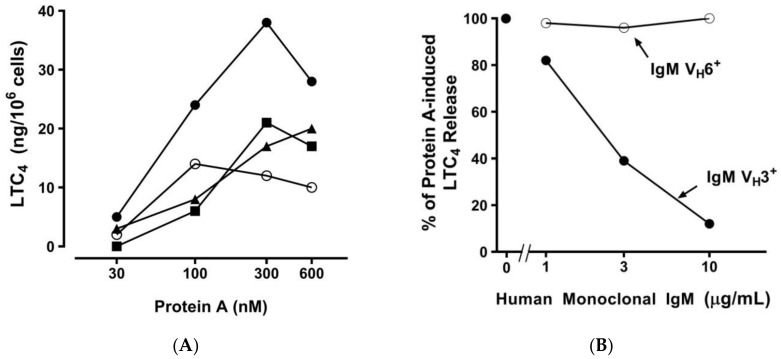
Figure 3A shows that protein A induced a concentration-dependent release of LTC4 from four different preparations of HHMC. To evaluate the mechanism by which protein A activates HHMCs, it was preincubated with human monoclonal IgM possessing different VH domains. Figure 3B shows that human monoclonal IgM VH3+ dose-dependently inhibited the LTC4-releasing activity of protein A. By contrast, human monoclonal IgM VH6+ had no inhibitory effect. These findings are compatible with the hypothesis that protein A activates HHMCs through the binding to IgE VH3+ bound on FcεRI.
Figure 3.
(A) Effect of increasing concentrations of protein A on the de novo synthesis of cysteinyl leukotriene C4 (LTC4) from four different preparations of HHMCs. HHMCs were incubated (45 min at 37 °C) with the indicated concentrations of protein A. Each point shows the mean of duplicate determinations. Each symbol represents the results from an individual donor. (B) Effect of preincubation of protein A with human monoclonal IgM on the activation of HHMCs. Protein A (300 nM) was preincubated (15 min at 37 °C) with increasing concentrations (1 to 10 μg/mL) of human monoclonal IgM VH3+ or IgM VH6+. HHMCs were then added and incubation continued for another 45 min at 37 °C. Each point shows the mean of duplicate determinations of a representative experiment. Similar results were obtained in two other experiments.
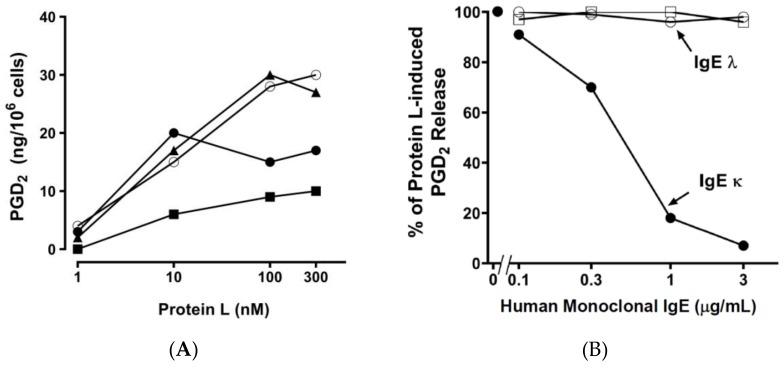
We have previously found that P. magnus and protein L activate human basophils and mast cells [39,41]. Figure 4A shows that increasing concentrations of protein L induced de novo synthesis of PGD2 from HHMCs. The activating property of protein L (100 nM) was inhibited by preincubation with increasing concentrations (0.1 to 3 μg/mL) of human monoclonal IgE k, but not by two human monoclonal IgE λ (Figure 4B). These results are compatible with the hypothesis that protein L activates HHMCs through the interaction with the k light chain of IgE on cardiac mast cells.
Figure 4.
(A) Effect of increasing concentrations of protein L on the de novo synthesis of prostaglandin D2 (PGD2) from four different preparations of HHMCs. HHMCs were incubated (45 min at 37 °C) with the indicated concentrations of protein L. Each point shows the mean of duplicate determinations. Each symbol represents the results from an individual donor. (B) Effect of preincubation of protein L with human monoclonal IgE on the activation of HHMCs. Protein L (100 nM) was preincubated (15 min at 37 °C) with increasing concentrations (0.1 to 3 μg/mL) of two human monoclonal IgE λ light chain and one human monoclonal IgE κ light chain and incubation continued for another 45 min at 37 °C. Each point shows the mean of duplicate determinations of PGD2 of a representative experiment. Similar results were obtained in two other experiments.
2.3. Effect of Viral Superantigens on Mediator Release from HHMCs
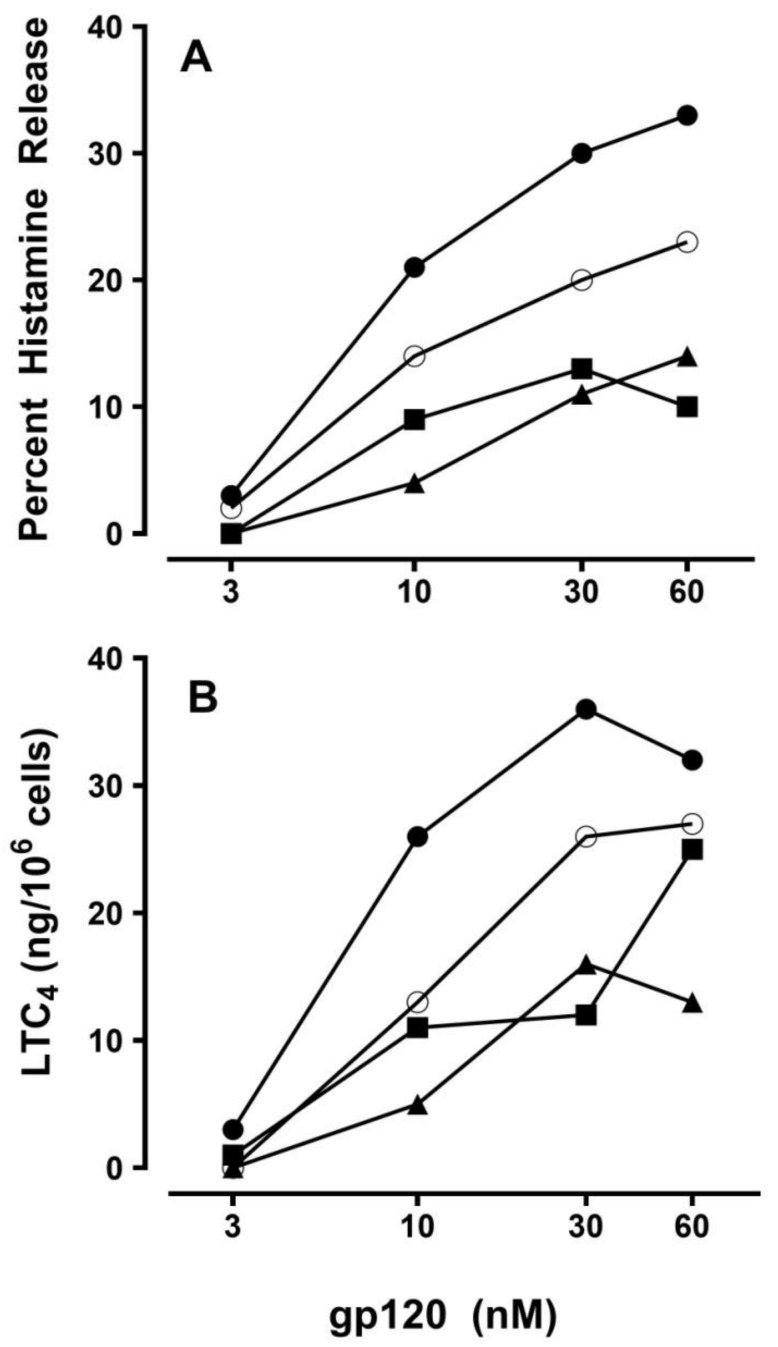
Figure 5 shows the results of four independent experiments in which we incubated HHMCs with recombinant gp120. These experiments demonstrated that increasing concentrations of gp120 stimulated the release of histamine (Figure 5A) and the de novo synthesis of LTC4 from HHMCs (Figure 5B). Preincubation of gp120 (30 nM) with increasing concentrations (0.1 to 3 μg/mL) of human monoclonal IgE VH3+ inhibited the releasing activity of gp120 (data not shown). These results indicate that gp120 activates HHMCs by interacting with IgE VH3+ bound to FcεRI.
Figure 5.
Effect of increasing concentrations of human immunodeficiency virus (HIV) gp120 on mediator release from four different preparations of HHMCs. HHMCs were incubated (45 min at 37 °C) with the indicated concentrations of gp120. At the end of incubation, the concentrations of histamine (A) and LTC4 (B) were measured in the four supernatants. Each point shows the mean of duplicate determinations. Each symbol represents the results from an individual donor.
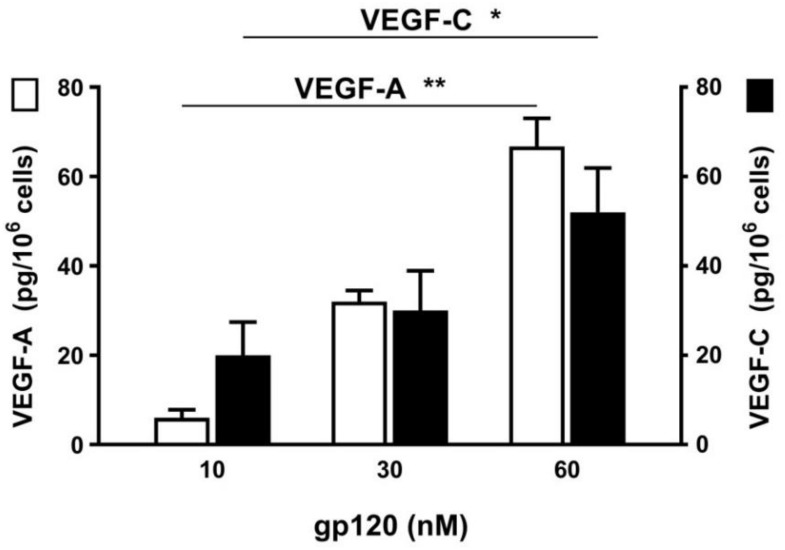
We then cultured HHMCs with increasing concentrations of recombinant gp120 (10 to 60 nM) for 6 h at 37 °C. At the end of this incubation the release of VEGF-A and VEGF-C was assayed in the supernatants of mast cells. Figure 6 shows the results of three preparations of HHMCs, indicating that gp120 induced the release of angiogenic (VEGF-A) and lymphangiogenic (VEGF-C) factors from HHMCs.
Figure 6.
Effect of increasing concentrations of HIV gp120 on the release of VEGF-A (open bars) and VEGF-C (black bars) from four different preparations of HHMCs. HHMCs were incubated (6 h at 37 °C) in the presence of the indicated concentrations of gp120. Each bar shows the mean ± SEM. * p < 0.05; ** p < 0.01.
3. Discussion
This study shows that primary mast cells isolated from human myocardial tissue can be activated by a human IgG anti-IgE isolated from the serum of a patient with atopic dermatitis. These results are compatible with the hypothesis that HHMCs bind IgE, which has a role not only in allergic diseases [53,88] but also in several cardiovascular disorders [89,90,91]. Bacterial (protein A and protein L) and viral (gp120) superantigens can activate HHMCs to release a variety of proinflammatory (histamine, LTC4, PGD2), angiogenic (VEGF-A), and lymphangiogenic (VEGF-C) mediators. The releasing activity of protein A and gp120 appears to be mediated by interaction with the VH3 region of IgE on HHMCs. By contrast, protein L of P. magnus activates HHMCs by interaction with the κ light chains of IgE on cardiac mast cells. Our findings provide evidence, to our knowledge for the first time, that the immunologic (human IgG anti-IgE) and superantigenic activation of human myocardial mast cells can induce the release of angiogenic and lymphangiogenic factors.
Mast cells are present in strategically important locations of murine [43,92] and human heart [48,49,51,77]. Mast cells are present in atherosclerotic lesions [50,93] and promote atherogenesis [89]. These cells and their mediators are also involved in cardiometabolic diseases [78], myocardial infarction [76] and remodeling [94], atrial fibrillation [95], thromboembolism [45,51,96], and myocarditis [74,97,98]. Therefore, understanding how cardiac mast cells participate in these inflammatory disorders could help in the development of targeted therapies for these common diseases.
Serum IgE levels are elevated in patients with myocardial infarction [90,91] and coronary artery disease compared to controls [89]. Moreover, IgE and FcεRI are overexpressed in human atherosclerotic lesions. These findings suggest that mast cells and perhaps other immune cells expressing FcεRI (e.g., dendritic cells, macrophages, basophils, platelets) [89,99,100] could play a role in the pathogenesis of human atherosclerosis. Previous studies have demonstrated that autoantibodies anti-IgE and anti-FcεRI can occur in several immunologic disorders [86,101,102,103,104]. In this study we found that a human IgG anti-IgE induced the release of histamine, VEGF-A, and VEGF-C from HHMCs. To our knowledge this is the first evidence that cross-linking of IgE on human myocardial mast cells can induce the release of angiogenic factors. Angiogenesis, the process by which new capillaries develop from the pre-existing vasculature [105], plays a central role in cardiac pathophysiology [87,106]. VEGF-A is a pivotal mediator in angiogenesis and is synthesized by several immune cells [61,79,81,82,107,108,109,110]. The possibility that human cardiac mast cells can contribute to myocardial angiogenesis, a process of major relevance in cardiac pathophysiology [106], requires further investigations.
The mammalian heart is rich of lymphatic vessels [111,112] and their number is increased in human heart following myocardial infarction, in atherosclerosis lesions, and in endocarditis [113,114]. The involvement of VEGF-C in salt-sensitive hypertension [115,116] and in coronary artery development [117] further add to the implications of lymphangiogenic factors in cardiovascular diseases [112]. Our results provide the first indication to our knowledge that immunologic and superantigenic activation of HHMCs leads to the production of VEGF-C, a major selective mediator of lymphangiogenesis [112].
S. aureus is an important human pathogen implicated in sepsis and endocarditis [118], and sepsis is a risk factor for cardiac arrhythmias [119]. This study demonstrates that protein A induces the release of LTC4 from HHMCs through the interaction of the VH3 region of IgE. These results extend on the previous observation that protein A induces the in vitro release of histamine from HHMCs [40]. Recently, it has been reported that in vivo challenge with protein A resulted in fatal anaphylaxis involving VH3+ immunoglobulin interaction on mast cells and basophils [120]. Given the relevance of histamine and cysteinyl leukotrienes in heart pathophysiology [121,122,123], our results might explain, at least in part, how S. aureus can cause heart damage in patients with sepsis.
Protein L synthesized by P. magnus induces the de novo synthesis of PGD2 from HHMCs, by interacting with the κ light chains of IgE on HHMCs. These results extend previous findings indicating that protein L induces the release of preformed histamine from HHMC [40]. Therefore, protein L is a complete secretagogue capable of releasing preformed and de novo synthesized mediators implicated in cardiovascular pathophysiology [121,122,123,124].
Our results provide the first indication that HIV gp120 activates HHMCs, thus acting as Ig SAg. Previous studies from our group have shown that gp120 induces the release of cytokines (IL-4 and IL-13) from human basophils [26]. Collectively, these findings support the hypothesis that virus-bound or shed gp120 [125] can function as a viral superantigen activating HMMCs and basophils to release proinflammatory mediators (histamine, LTC4), cytokines (IL-4 and IL-13), and angiogenic/lymphangiogenic factors (VEGF-A and VEGF-C), thus contributing to the dysregulation of immune system in HIV infection. The successful rollout of anti-viral therapy ensured that HIV infection is managed as a chronic condition. Persistent inflammation and immune dysregulation associated with HIV leads to accelerated aging and cardiovascular diseases [34,35,126,127]. HIV-positive persons are, therefore, exhibiting increasing cardiovascular complications [34,35]. Our results, indicating that gp120 can induce the release of potent proinflammatory (histamine and LTC4) mediators that exert cardiovascular effects [121,122,123] from myocardial mast cells, might explain, at least in part, how HIV can cause heart damage.
In this study we have identified several immunological, bacterial, and viral products that activate human cardiac mast cells through the interaction with IgE bound to FcεRI. However, mast cells can be activated by non-IgE- mediated stimuli such as cytokines (e.g., IL-33, SCF) [65,77,128], TLR ligands [60,129], and neuropeptides [52,130]. Additional studies are necessary to evaluate the effects of non-IgE-mediated stimuli on the release of proinflammatory mediators, angiogenic and lymphangiogenic factors from human cardiac mast cells.
Our study has a limitation which has to be pointed out. It was performed using primary mast cells isolated from myocardial tissue obtained from patients undergoing heart transplantation. Thus, these mast cells might have different characteristics from cells obtained from healthy donors. We have previously had the opportunity to address this important issue by comparing the release of mediators from mast cells isolated from failing hearts and from subjects who died in accidents without cardiovascular diseases [77]. We found quantitative, but not qualitative differences in the release of mediators from “normal” cardiac mast cells when compared with those from explanted hearts.
In conclusion, our results demonstrate that bacterial and viral immunoglobulin superantigens can activate primary human cardiac mast cells to release vasoactive and proinflammatory mediators and angiogenic and lymphangiogenic factors.
4. Materials and Methods
4.1. Reagents
HClO4 (Baker Chemical Co., Deventer, The Netherlands), BSA, piperazine-N,N′-bis (2-ethanesulfonic acid), L-glutamine, antibiotic-antimycotic solution (10,000 IU penicillin, 10 mg/mL streptomycin, and 25 μg/mL amphotericin B), hyaluronidase, chymopapain, elastase type I, LTC4, and PGD2 (Sigma-Aldrich, St. Louis, MO, USA), collagenase (Worthington Biochemical Co., Freehold, NJ, USA), Hanks’ balanced salt solution and fetal calf serum (FCS) (GIBCO, Grand Island, NY, USA), deoxyribonuclease I and pronase (Calbiochem, La Jolla, CA, USA), RPMI 1640 with 25 mM HEPES buffer, Eagle’s minimum essential medium (Flow Laboratories, Irvine, UK), Percoll (Pharmacia Fine Chemicals, Uppsala, Sweden), (3H)-LCT4 and (3H)-PGD2 (New England Nuclear, Boston, MA, USA) were commercially purchased. CD117 MicroBead kit was purchased from Miltenyi Biotech (Bologna, Italy). The rabbit anti-LTC4 and anti-PGD2 antibodies were a gift of Dr. Lawrence M. Lichtenstein (The Johns Hopkins University, Baltimore, MD, USA). Human IgG anti-IgE was purified from the serum of a patient with atopic dermatitis as described elsewhere [86].
4.2. Buffers
The Pipes (P) buffer used in these experiments was a mixture of 25 mM Pipes, 110 mM NaCl, 5 mM KCl, pH 7.37, referred to as P. P2CG, contains, in addition to P, 2 mM CaCl2 and 1 g/L dextrose [49]; pH was titrated to 7.4 with sodium bicarbonate. PGMD contains 0.25 g/L MgCl2·6H2O, 10 mg/L DNase, and 1 g/L gelatin in addition to P, pH 7.37.
4.3. Human Monoclonal IgM and IgE and Human Polyclonal IgG
Monoclonal IgM were purified from the serum of patients with Waldenström’s macroglobulinemia as described elsewhere [77]. IgE myeloma proteins were purified from the serum of three patients described elsewhere [131,132]. Variable regions of these monoclonal IgM were determined using a panel of primary sequence-dependent VH and VK family specific reagents that identify framework regions [133]. Human polyclonal IgG were purified from the serum of healthy donors as described elsewhere [132].
4.4. Isolation of HHMCs
The study was approved by the Ethics Committee of the University of Naples Federico II (Protocol: Human MC No 7/19, 05/03/2009). The heart tissue was obtained from patients undergoing heart transplantation at the Deutsches Herzzentrum, Berlin, mostly for cardiomyopathy [77]. The explanted heart was immediately immersed in cold (4 °C) cardioplegic solution and was processed within 5 to 18 h of removal. Fat tissue, large vessels, and pericardium were removed. The tissue was finely minced into 2–5 mm fragments, suspended in P buffer (10 mL/g of wet tissue), and washed by centrifugation 3 times. After each centrifugation, the heart fragments were filtered through a 150 μm pore Nytex cloth (Tetko, Elmsford, NY, USA). Fragments were incubated (15 min, 37 °C) under constant stirring in P buffer containing 10 mg collagenase/g of wet tissue. At the end of the incubation the cell suspension was filtered through a 150 μm pore Nytex cloth and three additional cycles of enzymatic digestion were performed. After the last procedure, the cells were centrifuged (150× g, 22 °C, 8 min) and filtered through a 60 μm pore Nytex cloth to remove large particles and large cells (mostly myocytes). Lastly, cells were washed twice in PGMD by centrifugation (150× g, 22 °C, 8 min). Cell pellets were resuspended in P buffer containing 2% BSA and centrifuged (25× g, 22 °C, 2 min) to remove sedimented myocytes (>100 μm long). Supernatants containing endothelial cells, fibroblasts, and mast cells were then collected and centrifuged (150× g, 22 °C, 8 min). HHMC were partially purified by flotation through a discontinuous Percoll gradient [77]. The purity of these populations ranged from 0.1% to 18%. The enzymatic dispersion tissue yields ≈ 5 × 104 mast cells per gram of heart tissue. HHMCs were further purified using a CD117 MicroBead kit sorting system (Miltenyi Biotec, Bologna, Italy). Mast cell purities using these techniques ranged from 26% to 58% and was assessed by toluidine blue staining.
4.5. Histamine Release Assay
HHMCs (≈ 3 × 104 mast cells per tube) were resuspended in P2CG, and 0.3 mL of the cell suspension were placed in 12 × 75 mm polyethylene tubes and warmed to 37 °C; 0.2 mL of each prewarmed releasing stimulus was added, and incubation was continued at 37 °C for 45 min [39]. The reaction was stopped by centrifugation (1000× g, 22 °C, 2 min), and the supernatants were stored at −80 °C for subsequent assay of histamine, LTC4, and PGD2 content. The cell-free supernatants were assayed for histamine with an automated fluorometric technique [134]. To calculate histamine release as a percentage of total cellular histamine, the “spontaneous” release from mast cells was subtracted from both numerator and denominator. All values are based on means of duplicate determinations which differed by less than 10%.
4.6. Immunoassay of LTC4 and PGD2
LTC4 and PGD2 were measured in duplicate determinations by radioimmunoassay [39,135]. The anti-LTC4 and anti-PGD2 antibodies are highly selective, with less than 1% cross-reactivity to other eicosanoids [39,135].
4.7. VEGF-A and VEGF-C Release
HHMCs (≈ 4 × 104 mast cells/per tube) were incubated (37 °C, 6 h) in RPMI 1640 containing 5% FCS, 2 mM L-glutamine, and 1% antibiotic-antimycotic solution, and activated with various concentrations of stimuli. At the end of incubation, cells were centrifuged (1000× g, 4 °C, 5 min) and the supernatants were stored at −80 °C for subsequent determination of mediator release. VEGF-A and VEGF-C were measured in duplicate determinations using commercially available ELISA kits (R&D System, Minneapolis, MN, USA) as previously described [136]. The ELISA sensitivity is 31.1–2000 pg/mL for VEGF-A and 62–4000 pg/mL for VEGF-C.
4.8. Statistical Analysis
Values were expressed as means ± SEM (standard error of the mean). The one-way repeated measures analysis of variance (ANOVA) with Greenhouse–Geisser corrections was used to examine the variations of continuous variables at different experimental conditions. Results were analyzed with GraphPad Prism software (version 8.01; GraphPad Software, La Jolla, CA, USA), and p values of less than 0.05 were considered significant.
Acknowledgments
Gjada Criscuolo for critical reading of the manuscript.
Abbreviations
| S. aureus | Staphylococcus aureus |
| P. magnus | Peptostreptococcus magnus |
| LTC4 | Cysteinyl leukotriene C4 |
| HHMCs | Human heart mast cells |
| Ig | Immunoglobulin |
| FcεRI | High-affinity receptor for IgE |
| PGD2 | Prostaglandin D2 |
| gp120 | Glycoprotein 120 |
| VEGF | Vascular endothelial growth factor |
| SAg | Superantigen |
| APCs | Antigen-presenting cells |
| MHC | Major histocompatibility complex |
| TCR | T cell receptor |
| V | Variable |
| H | Heavy |
| L | Light |
| SE | Staphylococcus aureus enterotoxins |
| IL | Interleukin |
| HIV | Human immunodeficiency virus |
| FCS | Fetal calf serum |
| BSA | Bovine serum albumin |
| H-aIgE | Human IgG anti-IgE |
Author Contributions
G.V., S.L., A.P., A.G., G.S., and G.M. conceived and designed the study. G.V., S.L., F.R., and F.B. performed the experiments. A.P. performed the statistical analysis of the results. A.P. and G.M. elaborated the figures. All the authors contributed intellectually and to the writing of the submitted version of the manuscript.
Funding
This work was supported in part by grants from Regione Campania CISI-Lab Project, CRèME Project, and TIMING Project.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.White J., Herman A., Pullen A.M., Kubo R., Kappler J.W., Marrack P. The V beta-specific superantigen staphylococcal enterotoxin B: Stimulation of mature T cells and clonal deletion in neonatal mice. Cell. 1989;56:27–35. doi: 10.1016/0092-8674(89)90980-X. [DOI] [PubMed] [Google Scholar]
- 2.Kotzin B.L., Leung D.Y., Kappler J., Marrack P. Superantigens and their potential role in human disease. Adv. Immunol. 1993;54:99–166. doi: 10.1016/s0065-2776(08)60534-9. [DOI] [PubMed] [Google Scholar]
- 3.Marone G. Superantigens and superallergens. Chem. Immunol. Allergy. 2007;93 doi: 10.1159/isbn.978-3-318-01451-8. [DOI] [PubMed] [Google Scholar]
- 4.Marrack P., Kappler J. The staphylococcal enterotoxins and their relatives. Science. 1990;248:705–711. doi: 10.1126/science.2185544. [DOI] [PubMed] [Google Scholar]
- 5.Bouvet J.P., Pires R., Lunel-Fabiani F., Crescenzo-Chaigne B., Maillard P., Valla D., Opolon P., Pillot J. Protein F. A novel F(ab)-binding factor, present in normal liver, and largely released in the digestive tract during hepatitis. J. Immunol. 1990;145:1176–1180. [PubMed] [Google Scholar]
- 6.Germain R.N. Antigen presentation. The second class story. Nature. 1991;353:605–607. doi: 10.1038/353605a0. [DOI] [PubMed] [Google Scholar]
- 7.Fields B.A., Ober B., Malchiodi E.L., Lebedeva M.I., Braden B.C., Ysern X., Kim J.K., Shao X., Ward E.S., Mariuzza R.A. Crystal structure of the V alpha domain of a T cell antigen receptor. Science. 1995;270:1821–1824. doi: 10.1126/science.270.5243.1821. [DOI] [PubMed] [Google Scholar]
- 8.Li H., Llera A., Tsuchiya D., Leder L., Ysern X., Schlievert P.M., Karjalainen K., Mariuzza R.A. Three-dimensional structure of the complex between a T cell receptor beta chain and the superantigen staphylococcal enterotoxin B. Immunity. 1998;9:807–816. doi: 10.1016/S1074-7613(00)80646-9. [DOI] [PubMed] [Google Scholar]
- 9.Malchiodi E.L., Eisenstein E., Fields B.A., Ohlendorf D.H., Schlievert P.M., Karjalainen K., Mariuzza R.A. Superantigen binding to a T cell receptor beta chain of known three-dimensional structure. J. Exp. Med. 1995;182:1833–1845. doi: 10.1084/jem.182.6.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sundberg E.J., Li H., Llera A.S., McCormick J.K., Tormo J., Schlievert P.M., Karjalainen K., Mariuzza R.A. Structures of two streptococcal superantigens bound to TCR beta chains reveal diversity in the architecture of T cell signaling complexes. Structure. 2002;10:687–699. doi: 10.1016/S0969-2126(02)00759-1. [DOI] [PubMed] [Google Scholar]
- 11.Goodyear C.S., Silverman G.J. B cell superantigens: A microbe’s answer to innate-like B cells and natural antibodies. Springer Semin. Immunopathol. 2005;26:463–484. doi: 10.1007/s00281-004-0190-2. [DOI] [PubMed] [Google Scholar]
- 12.Viau M., Zouali M. B-lymphocytes, innate immunity, and autoimmunity. Clin. Immunol. 2005;114:17–26. doi: 10.1016/j.clim.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 13.Bachert C., Gevaert P., Zhang N., van Zele T., Perez-Novo C. Role of staphylococcal superantigens in airway disease. Chem. Immunol. Allergy. 2007;93:214–236. doi: 10.1159/000100897. [DOI] [PubMed] [Google Scholar]
- 14.Marone G., Rossi F.W., Detoraki A., Granata F., Genovese A., Spadaro G. Role of superallergens in allergic disorders. Chem. Immunol. Allergy. 2007;93:195–213. doi: 10.1159/000100896. [DOI] [PubMed] [Google Scholar]
- 15.Pastacaldi C., Lewis P., Howarth P. Staphylococci and staphylococcal superantigens in asthma and rhinitis: A systematic review and meta-analysis. Allergy. 2011;66:549–555. doi: 10.1111/j.1398-9995.2010.02502.x. [DOI] [PubMed] [Google Scholar]
- 16.Pascual V., Capra J.D. B-cell superantigens? Curr. Biol. 1991;1:315–317. doi: 10.1016/0960-9822(91)90097-G. [DOI] [PubMed] [Google Scholar]
- 17.Silverman G.J., Goodyear C.S. A model B-cell superantigen and the immunobiology of B lymphocytes. Clin. Immunol. 2002;102:117–134. doi: 10.1006/clim.2001.5143. [DOI] [PubMed] [Google Scholar]
- 18.Zouali M. B-cell superantigens: Implications for selection of the human antibody repertoire. Immunol. Today. 1995;16:399–405. doi: 10.1016/0167-5699(95)80009-3. [DOI] [PubMed] [Google Scholar]
- 19.Thomas D., Chou S., Dauwalder O., Lina G. Diversity in Staphylococcus aureus enterotoxins. Chem. Immunol. Allergy. 2007;93:24–41. doi: 10.1159/000100856. [DOI] [PubMed] [Google Scholar]
- 20.Friedrich R., Panizzi P., Fuentes-Prior P., Richter K., Verhamme I., Anderson P.J., Kawabata S., Huber R., Bode W., Bock P.E. Staphylocoagulase is a prototype for the mechanism of cofactor-induced zymogen activation. Nature. 2003;425:535–539. doi: 10.1038/nature01962. [DOI] [PubMed] [Google Scholar]
- 21.Lowy F.D. Staphylococcus aureus infections. N. Engl. J. Med. 1998;339:520–532. doi: 10.1056/NEJM199808203390806. [DOI] [PubMed] [Google Scholar]
- 22.Becker S., Frankel M.B., Schneewind O., Missiakas D. Release of protein A from the cell wall of Staphylococcus aureus. Proc. Natl. Acad. Sci. USA. 2014;111:1574–1579. doi: 10.1073/pnas.1317181111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Forsgren A., Sjoquist J. “Protein A” from S. aureus. I. Pseudo-immune reaction with human gamma-globulin. J. Immunol. 1966;97:822–827. [PubMed] [Google Scholar]
- 24.Inganäs M. Comparison of mechanisms of interaction between protein A from Staphylococcus aureus and human monoclonal IgG, IgA and IgM in relation to the classical FC gamma and the alternative F(ab’)2 epsilon protein A interactions. Scand. J. Immunol. 1981;13:343–352. doi: 10.1111/j.1365-3083.1981.tb00143.x. [DOI] [PubMed] [Google Scholar]
- 25.Florio G., Petraroli A., Patella V., Triggiani M., Marone G. The immunoglobulin superantigen-binding site of HIV-1 gp120 activates human basophils. AIDS. 2000;14:931–938. doi: 10.1097/00002030-200005260-00004. [DOI] [PubMed] [Google Scholar]
- 26.Patella V., Florio G., Petraroli A., Marone G. HIV-1 gp120 induces IL-4 and IL-13 release from human Fc epsilon RI+ cells through interaction with the VH3 region of IgE. J. Immunol. 2000;164:589–595. doi: 10.4049/jimmunol.164.2.589. [DOI] [PubMed] [Google Scholar]
- 27.Killelea B.K., Chagpar A.B., Horowitz N.R., Lannin D.R. Characteristics and treatment of human epidermal growth factor receptor 2 positive breast cancer: 43,485 cases from the National Cancer Database treated in 2010 and 2011. Am. J. Surg. 2017;213:426–432. doi: 10.1016/j.amjsurg.2016.05.018. [DOI] [PubMed] [Google Scholar]
- 28.Kwong P.D., Wyatt R., Robinson J., Sweet R.W., Sodroski J., Hendrickson W.A. Structure of an HIV gp120 envelope glycoprotein in complex with the CD4 receptor and a neutralizing human antibody. Nature. 1998;393:648–659. doi: 10.1038/31405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feng Y., Broder C.C., Kennedy P.E., Berger E.A. HIV-1 entry cofactor: functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science. 1996;272:872–877. doi: 10.1126/science.272.5263.872. [DOI] [PubMed] [Google Scholar]
- 30.Dragic T., Litwin V., Allaway G.P., Martin S.R., Huang Y., Nagashima K.A., Cayanan C., Maddon P.J., Koup R.A., Moore J.P., et al. HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5. Nature. 1996;381:667–673. doi: 10.1038/381667a0. [DOI] [PubMed] [Google Scholar]
- 31.Karray S., Zouali M. Identification of the B cell superantigen-binding site of HIV-1 gp120. Proc. Natl. Acad. Sci. USA. 1997;94:1356–1360. doi: 10.1073/pnas.94.4.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Silverman G.J. B-cell superantigens. Immunol. Today. 1997;18:379–386. doi: 10.1016/S0167-5699(97)01101-8. [DOI] [PubMed] [Google Scholar]
- 33.Zouali M. B cell superantigens subvert innate functions of B cells. Chem. Immunol. Allergy. 2007;93:92–105. doi: 10.1159/000100860. [DOI] [PubMed] [Google Scholar]
- 34.Durand M., Chartrand-Lefebvre C., Baril J.G., Trottier S., Trottier B., Harris M., Walmsley S., Conway B., Wong A., Routy J.P., et al. The Canadian HIV and aging cohort study—Determinants of increased risk of cardio-vascular diseases in HIV-infected individuals: rationale and study protocol. BMC Infect. Dis. 2017;17:611. doi: 10.1186/s12879-017-2692-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Teer E., Essop M.F. HIV and cardiovascular disease: Role of immunometabolic perturbations. Physiology (Bethesda) 2018;33:74–82. doi: 10.1152/physiol.00028.2017. [DOI] [PubMed] [Google Scholar]
- 36.Lakhrif Z., Pugniere M., Henriquet C., di Tommaso A., Dimier-Poisson I., Billiald P., Juste M.O., Aubrey N. A method to confer Protein L binding ability to any antibody fragment. mAbs. 2016;8:379–388. doi: 10.1080/19420862.2015.1116657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bjorck L. Protein L. A novel bacterial cell wall protein with affinity for Ig L chains. J. Immunol. 1988;140:1194–1197. [PubMed] [Google Scholar]
- 38.Myhre E.B., Erntell M. A non-immune interaction between the light chain of human immunoglobulin and a surface component of a Peptococcus magnus strain. Mol. Immunol. 1985;22:879–885. doi: 10.1016/0161-5890(85)90073-2. [DOI] [PubMed] [Google Scholar]
- 39.Patella V., Casolaro V., Bjorck L., Marone G. Protein L. A bacterial Ig-binding protein that activates human basophils and mast cells. J. Immunol. 1990;145:3054–3061. [PubMed] [Google Scholar]
- 40.Genovese A., Bouvet J.P., Florio G., Lamparter-Schummert B., Bjorck L., Marone G. Bacterial immunoglobulin superantigen proteins A and L activate human heart mast cells by interacting with immunoglobulin E. Infect. Immun. 2000;68:5517–5524. doi: 10.1128/IAI.68.10.5517-5524.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Genovese A., Borgia G., Bjorck L., Petraroli A., de Paulis A., Piazza M., Marone G. Immunoglobulin superantigen protein L induces IL-4 and IL-13 secretion from human Fc epsilon RI+ cells through interaction with the kappa light chains of IgE. J. Immunol. 2003;170:1854–1861. doi: 10.4049/jimmunol.170.4.1854. [DOI] [PubMed] [Google Scholar]
- 42.Nilson B.H., Solomon A., Bjorck L., Akerstrom B. Protein L from Peptostreptococcus magnus binds to the kappa light chain variable domain. J. Biol. Chem. 1992;267:2234–2239. [PubMed] [Google Scholar]
- 43.Ingason A.B., Mechmet F., Atacho D.A.M., Steingrimsson E., Petersen P.H. Distribution of mast cells within the mouse heart and its dependency on Mitf. Mol. Immunol. 2018;105:9–15. doi: 10.1016/j.molimm.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 44.Aldi S., Robador P.A., Tomita K., Di Lorenzo A., Levi R. IgE receptor-mediated mast-cell renin release. Am. J. Pathol. 2014;184:376–381. doi: 10.1016/j.ajpath.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ponomaryov T., Payne H., Fabritz L., Wagner D.D., Brill A. Mast cells granular contents are crucial for deep vein thrombosis in mice. Circ. Res. 2017;121:941–950. doi: 10.1161/CIRCRESAHA.117.311185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Somasundaram P., Ren G., Nagar H., Kraemer D., Mendoza L., Michael L.H., Caughey G.H., Entman M.L., Frangogiannis N.G. Mast cell tryptase may modulate endothelial cell phenotype in healing myocardial infarcts. J. Pathol. 2005;205:102–111. doi: 10.1002/path.1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frangogiannis N.G., Mendoza L.H., Lindsey M.L., Ballantyne C.M., Michael L.H., Smith C.W., Entman M.L. IL-10 is induced in the reperfused myocardium and may modulate the reaction to injury. J. Immunol. 2000;165:2798–2808. doi: 10.4049/jimmunol.165.5.2798. [DOI] [PubMed] [Google Scholar]
- 48.Patella V., Marino I., Lamparter B., Arbustini E., Adt M., Marone G. Human heart mast cells. Isolation, purification, ultrastructure, and immunologic characterization. J. Immunol. 1995;154:2855–2865. [PubMed] [Google Scholar]
- 49.Patella V., de Crescenzo G., Marino I., Genovese A., Adt M., Gleich G.J., Marone G. Eosinophil granule proteins activate human heart mast cells. J. Immunol. 1996;157:1219–1225. [PubMed] [Google Scholar]
- 50.Kaartinen M., Penttila A., Kovanen P.T. Mast cells accompany microvessels in human coronary atheromas: Implications for intimal neovascularization and hemorrhage. Atherosclerosis. 1996;123:123–131. doi: 10.1016/0021-9150(95)05794-3. [DOI] [PubMed] [Google Scholar]
- 51.Bankl H.C., Radaszkiewicz T., Klappacher G.W., Glogar D., Sperr W.R., Grossschmidt K., Bankl H., Lechner K., Valent P. Increase and redistribution of cardiac mast cells in auricular thrombosis. Possible role of kit ligand. Circulation. 1995;91:275–283. doi: 10.1161/01.CIR.91.2.275. [DOI] [PubMed] [Google Scholar]
- 52.Varricchi G., Raap U., Rivellese F., Marone G., Gibbs B.F. Human mast cells and basophils-How are they similar how are they different? Immunol. Rev. 2018;282:8–34. doi: 10.1111/imr.12627. [DOI] [PubMed] [Google Scholar]
- 53.Borriello F., Granata F., Varricchi G., Genovese A., Triggiani M., Marone G. Immunopharmacological modulation of mast cells. Curr. Opin. Pharmacol. 2014;17:45–57. doi: 10.1016/j.coph.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 54.Mukai K., Tsai M., Saito H., Galli S.J. Mast cells as sources of cytokines, chemokines, and growth factors. Immunol. Rev. 2018;282:121–150. doi: 10.1111/imr.12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Galli S.J. The mast cell-IgE paradox: From homeostasis to anaphylaxis. Am. J. Pathol. 2016;186:212–224. doi: 10.1016/j.ajpath.2015.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bradding P., Arthur G. Mast cells in asthma—State of the art. Clin. Exp. Allergy. 2016;46:194–263. doi: 10.1111/cea.12675. [DOI] [PubMed] [Google Scholar]
- 57.Olivera A., Beaven M.A., Metcalfe D.D. Mast cells signal their importance in health and disease. J. Allergy Clin. Immunol. 2018;142:381–393. doi: 10.1016/j.jaci.2018.01.034. [DOI] [PubMed] [Google Scholar]
- 58.Piliponsky A.M., Romani L. The contribution of mast cells to bacterial and fungal infection immunity. Immunol. Rev. 2018;282:188–197. doi: 10.1111/imr.12623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Marone G., Varricchi G., Loffredo S., Galdiero M.R., Rivellese F., de Paulis A. Are basophils and mast cells masters in HIV Infection? Int. Arch. Allergy Immunol. 2016;171:158–165. doi: 10.1159/000452889. [DOI] [PubMed] [Google Scholar]
- 60.Suurmond J., Rivellese F., Dorjee A.L., Bakker A.M., Rombouts Y.J., Rispens T., Wolbink G., Zaldumbide A., Hoeben R.C., Huizinga T.W., et al. Toll-like receptor triggering augments activation of human mast cells by anti-citrullinated protein antibodies. Ann. Rheum. Dis. 2015;74:1915–1923. doi: 10.1136/annrheumdis-2014-205562. [DOI] [PubMed] [Google Scholar]
- 61.Detoraki A., Staiano R.I., Granata F., Giannattasio G., Prevete N., de Paulis A., Ribatti D., Genovese A., Triggiani M., Marone G. Vascular endothelial growth factors synthesized by human lung mast cells exert angiogenic effects. J. Allergy Clin. Immunol. 2009;123:1142–1149. doi: 10.1016/j.jaci.2009.01.044. [DOI] [PubMed] [Google Scholar]
- 62.Varricchi G., Loffredo S., Galdiero M.R., Marone G., Cristinziano L., Granata F. Innate effector cells in angiogenesis and lymphangiogenesis. Curr. Opin. Immunol. 2018;53:152–160. doi: 10.1016/j.coi.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 63.Marone G., Varricchi G., Loffredo S., Granata F. Mast cells and basophils in inflammatory and tumor angiogenesis and lymphangiogenesis. Eur. J. Pharmacol. 2016;778:146–151. doi: 10.1016/j.ejphar.2015.03.088. [DOI] [PubMed] [Google Scholar]
- 64.Abdel-Majid R.M., Marshall J.S. Prostaglandin E2 induces degranulation-independent production of vascular endothelial growth factor by human mast cells. J. Immunol. 2004;172:1227–1236. doi: 10.4049/jimmunol.172.2.1227. [DOI] [PubMed] [Google Scholar]
- 65.Theoharides T.C., Zhang B., Kempuraj D., Tagen M., Vasiadi M., Angelidou A., Alysandratos K.D., Kalogeromitros D., Asadi S., Stavrianeas N., et al. IL-33 augments substance P-induced VEGF secretion from human mast cells and is increased in psoriatic skin. Proc. Natl. Acad. Sci. USA. 2010;107:4448–4453. doi: 10.1073/pnas.1000803107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Varricchi G., Granata F., Loffredo S., Genovese A., Marone G. Angiogenesis and lymphangiogenesis in inflammatory skin disorders. J. Am. Acad. Dermatol. 2015;73:144–153. doi: 10.1016/j.jaad.2015.03.041. [DOI] [PubMed] [Google Scholar]
- 67.Rivellese F., Suurmond J., Habets K., Dorjee A.L., Ramamoorthi N., Townsend M.J., de Paulis A., Marone G., Huizinga T.W., Pitzalis C., et al. Ability of interleukin-33- and immune complex-triggered activation of human mast cells to down-regulate monocyte-mediated immune responses. Arthritis Rheumatol. 2015;67:2343–2353. doi: 10.1002/art.39192. [DOI] [PubMed] [Google Scholar]
- 68.Rivellese F., Nerviani A., Rossi F.W., Marone G., Matucci-Cerinic M., de Paulis A., Pitzalis C. Mast cells in rheumatoid arthritis: friends or foes? Autoimmun. Rev. 2017;16:557–563. doi: 10.1016/j.autrev.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 69.Rivellese F., Mauro D., Nerviani A., Pagani S., Fossati-Jimack L., Messemaker T., Kurreeman F.A.S., Toes R.E.M., Ramming A., Rauber S., et al. Mast cells in early rheumatoid arthritis associate with disease severity and support B cell autoantibody production. Ann. Rheum. Dis. 2018;77:1773–1781. doi: 10.1136/annrheumdis-2018-213418. [DOI] [PubMed] [Google Scholar]
- 70.Visciano C., Liotti F., Prevete N., Cali G., Franco R., Collina F., de Paulis A., Marone G., Santoro M., Melillo R.M. Mast cells induce epithelial-to-mesenchymal transition and stem cell features in human thyroid cancer cells through an IL-8-Akt-Slug pathway. Oncogene. 2015;34:5175–5186. doi: 10.1038/onc.2014.441. [DOI] [PubMed] [Google Scholar]
- 71.Galdiero M.R., Varricchi G., Marone G. The immune network in thyroid cancer. Oncoimmunology. 2016;5:e1168556. doi: 10.1080/2162402X.2016.1168556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Varricchi G., Galdiero M.R., Loffredo S., Marone G., Iannone R., Granata F. Are mast cells MASTers in cancer? Front Immunol. 2017;8:424. doi: 10.3389/fimmu.2017.00424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Varricchi G., Galdiero M.R., Marone G., Granata F., Borriello F. Controversial role of mast cells in skin cancers. Exp. Dermatol. 2017;26:11–17. doi: 10.1111/exd.13107. [DOI] [PubMed] [Google Scholar]
- 74.Fairweather D., Frisancho-Kiss S., Gatewood S., Njoku D., Steele R., Barrett M., Rose N.R. Mast cells and innate cytokines are associated with susceptibility to autoimmune heart disease following coxsackievirus B3 infection. Autoimmunity. 2004;37:131–145. doi: 10.1080/0891693042000196200. [DOI] [PubMed] [Google Scholar]
- 75.Varricchi G., Galdiero M.R., Tocchetti C.G. Cardiac toxicity of immune checkpoint inhibitors: Cardio-oncology meets immunology. Circulation. 2017;136:1989–1992. doi: 10.1161/CIRCULATIONAHA.117.029626. [DOI] [PubMed] [Google Scholar]
- 76.Ngkelo A., Richart A., Kirk J.A., Bonnin P., Vilar J., Lemitre M., Marck P., Branchereau M., Le Gall S., Renault N., et al. Mast cells regulate myofilament calcium sensitization and heart function after myocardial infarction. J. Exp. Med. 2016;213:1353–1374. doi: 10.1084/jem.20160081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Patella V., Marino I., Arbustini E., Lamparter-Schummert B., Verga L., Adt M., Marone G. Stem cell factor in mast cells and increased mast cell density in idiopathic and ischemic cardiomyopathy. Circulation. 1998;97:971–978. doi: 10.1161/01.CIR.97.10.971. [DOI] [PubMed] [Google Scholar]
- 78.Shi G.P., Bot I., Kovanen P.T. Mast cells in human and experimental cardiometabolic diseases. Nat. Rev. Cardiol. 2015;12:643–658. doi: 10.1038/nrcardio.2015.117. [DOI] [PubMed] [Google Scholar]
- 79.De Paulis A., Prevete N., Fiorentino I., Rossi F.W., Staibano S., Montuori N., Ragno P., Longobardi A., Liccardo B., Genovese A., et al. Expression and functions of the vascular endothelial growth factors and their receptors in human basophils. J. Immunol. 2006;177:7322–7331. doi: 10.4049/jimmunol.177.10.7322. [DOI] [PubMed] [Google Scholar]
- 80.Granata F., Frattini A., Loffredo S., Staiano R.I., Petraroli A., Ribatti D., Oslund R., Gelb M.H., Lambeau G., Marone G., et al. Production of vascular endothelial growth factors from human lung macrophages induced by group IIA and group X secreted phospholipases A2. J. Immunol. 2010;184:5232–5241. doi: 10.4049/jimmunol.0902501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Staiano R.I., Loffredo S., Borriello F., Iannotti F.A., Piscitelli F., Orlando P., Secondo A., Granata F., Lepore M.T., Fiorelli A., et al. Human lung-resident macrophages express CB1 and CB2 receptors whose activation inhibits the release of angiogenic and lymphangiogenic factors. J. Leukoc. Biol. 2016;99:531–540. doi: 10.1189/jlb.3HI1214-584R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Loffredo S., Borriello F., Iannone R., Ferrara A.L., Galdiero M.R., Gigantino V., Esposito P., Varricchi G., Lambeau G., Cassatella M.A., et al. Group V secreted phospholipase A2 induces the release of proangiogenic and antiangiogenic factors by human neutrophils. Front. Immunol. 2017;8:443. doi: 10.3389/fimmu.2017.00443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Benyon R.C., Lowman M.A., Church M.K. Human skin mast cells: Their dispersion, purification, and secretory characterization. J. Immunol. 1987;138:861–867. [PubMed] [Google Scholar]
- 84.Guhl S., Lee H.H., Babina M., Henz B.M., Zuberbier T. Evidence for a restricted rather than generalized stimulatory response of skin-derived human mast cells to substance P. J. Neuroimmunol. 2005;163:92–101. doi: 10.1016/j.jneuroim.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 85.De Paulis A., Marino I., Ciccarelli A., de Crescenzo G., Concardi M., Verga L., Arbustini E., Marone G. Human synovial mast cells. I. Ultrastructural in situ and in vitro immunologic characterization. Arthritis Rheum. 1996;39:1222–1233. doi: 10.1002/art.1780390723. [DOI] [PubMed] [Google Scholar]
- 86.Marone G., Casolaro V., Paganelli R., Quinti I. IgG anti-IgE from atopic dermatitis induces mediator release from basophils and mast cells. J. Investig. Dermatol. 1989;93:246–252. doi: 10.1111/1523-1747.ep12277582. [DOI] [PubMed] [Google Scholar]
- 87.Taimeh Z., Loughran J., Birks E.J., Bolli R. Vascular endothelial growth factor in heart failure. Nat. Rev. Cardiol. 2013;10:519–530. doi: 10.1038/nrcardio.2013.94. [DOI] [PubMed] [Google Scholar]
- 88.Varricchi G., Harker J., Borriello F., Marone G., Durham S.R., Shamji M.H. T follicular helper (Tfh) cells in normal immune responses and in allergic disorders. Allergy. 2016;71:1086–1094. doi: 10.1111/all.12878. [DOI] [PubMed] [Google Scholar]
- 89.Wang J., Cheng X., Xiang M.X., Alanne-Kinnunen M., Wang J.A., Chen H., He A., Sun X., Lin Y., Tang T.T., et al. IgE stimulates human and mouse arterial cell apoptosis and cytokine expression and promotes atherogenesis in Apoe-/-mice. J. Clin. Investig. 2011;121:3564–3577. doi: 10.1172/JCI46028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Szczeklik A., Sladek K., Szczerba A., Dropinski J. Serum immunoglobulin E response to myocardial infarction. Circulation. 1988;77:1245–1249. doi: 10.1161/01.CIR.77.6.1245. [DOI] [PubMed] [Google Scholar]
- 91.Kovanen P.T., Manttari M., Palosuo T., Manninen V., Aho K. Prediction of myocardial infarction in dyslipidemic men by elevated levels of immunoglobulin classes A, E, and G, but not M. Arch. Intern. Med. 1998;158:1434–1439. doi: 10.1001/archinte.158.13.1434. [DOI] [PubMed] [Google Scholar]
- 92.Kareinen I., Baumann M., Nguyen S.D., Maaninka K., Anisimov A., Tozuka M., Jauhiainen M., Lee-Rueckert M., Kovanen P.T. Chymase released from hypoxia-activated cardiac mast cells cleaves human apoA-I at Tyr(192) and compromises its cardioprotective activity. J. Lipid Res. 2018;59:945–957. doi: 10.1194/jlr.M077503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Theoharides T.C., Sismanopoulos N., Delivanis D.A., Zhang B., Hatziagelaki E.E., Kalogeromitros D. Mast cells squeeze the heart and stretch the gird: their role in atherosclerosis and obesity. Trends Pharmacol. Sci. 2011;32:534–542. doi: 10.1016/j.tips.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 94.Dell’Italia L.J., Collawn J.F., Ferrario C.M. Multifunctional role of chymase in acute and chronic tissue injury and remodeling. Circ. Res. 2018;122:319–336. doi: 10.1161/CIRCRESAHA.117.310978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Uemura K., Kondo H., Ishii Y., Kobukata M., Haraguchi M., Imamura T., Otsubo T., Ikebe-Ebata Y., Abe I., Ayabe R., et al. Mast cells play an important role in the pathogenesis of hyperglycemia-induced atrial fibrillation. J Cardiovasc. Electrophysiol. 2016;27:981–989. doi: 10.1111/jce.12995. [DOI] [PubMed] [Google Scholar]
- 96.Shubin N.J., Glukhova V.A., Clauson M., Truong P., Abrink M., Pejler G., White N.J., Deutsch G.H., Reeves S.R., Vaisar T., et al. Proteome analysis of mast cell releasates reveals a role for chymase in the regulation of coagulation factor XIIIA levels via proteolytic degradation. J. Allergy Clin. Immunol. 2017;139:323–334. doi: 10.1016/j.jaci.2016.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wroblewski M., Bauer R., Cubas Cordova M., Udonta F., Ben-Batalla I., Legler K., Hauser C., Egberts J., Janning M., Velthaus J., et al. Mast cells decrease efficacy of anti-angiogenic therapy by secreting matrix-degrading granzyme B. Nat. Commun. 2017;8:269. doi: 10.1038/s41467-017-00327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nascimento C.R., Andrade D., Carvalho-Pinto C.E., Serra R.R., Vellasco L., Brasil G., Ramos-Junior E.S., da Mota J.B., Almeida L.N., Andrade M.V., et al. Mast cell coupling to the kallikrein-kinin system fuels intracardiac parasitism and worsens heart pathology in experimental chagas disease. Front. Immunol. 2017;8:840. doi: 10.3389/fimmu.2017.00840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Marone G., Borriello F., Varricchi G., Genovese A., Granata F. Basophils: Historical reflections and perspectives. Chem. Immunol. Allergy. 2014;100:172–192. doi: 10.1159/000358734. [DOI] [PubMed] [Google Scholar]
- 100.Sun Y., Vandenbriele C., Kauskot A., Verhamme P., Hoylaerts M.F., Wright G.J. A human platelet receptor protein microarray identifies the high affinity immunoglobulin E receptor subunit alpha (FcepsilonR1alpha) as an activating platelet endothelium aggregation receptor 1 (PEAR1) ligand. Mol. Cell Proteom. 2015;14:1265–1274. doi: 10.1074/mcp.M114.046946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nawata Y., Koike T., Hosokawa H., Tomioka H., Yoshida S. Anti-IgE autoantibody in patients with atopic dermatitis. J. Immunol. 1985;135:478–482. [PubMed] [Google Scholar]
- 102.Sabroe R.A., Seed P.T., Francis D.M., Barr R.M., Black A.K., Greaves M.W. Chronic idiopathic urticaria: comparison of the clinical features of patients with and without anti-FcepsilonRI or anti-IgE autoantibodies. J. Am. Acad. Dermatol. 1999;40:443–450. doi: 10.1016/S0190-9622(99)70495-0. [DOI] [PubMed] [Google Scholar]
- 103.Gruber B.L., Baeza M.L., Marchese M.J., Agnello V., Kaplan A.P. Prevalence and functional role of anti-IgE autoantibodies in urticarial syndromes. J. Investig. Dermatol. 1988;90:213–217. doi: 10.1111/1523-1747.ep12462239. [DOI] [PubMed] [Google Scholar]
- 104.Sanjuan M.A., Sagar D., Kolbeck R. Role of IgE in autoimmunity. J. Allergy Clin. Immunol. 2016;137:1651–1661. doi: 10.1016/j.jaci.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 105.Marone G., Granata F. Angiogenesis, lymphangiogenesis and clinical implications. Preface. Chem. Immunol. Allergy. 2014;99:11–12. doi: 10.1159/000352074. [DOI] [PubMed] [Google Scholar]
- 106.Bry M., Kivela R., Holopainen T., Anisimov A., Tammela T., Soronen J., Silvola J., Saraste A., Jeltsch M., Korpisalo P., et al. Vascular endothelial growth factor-B acts as a coronary growth factor in transgenic rats without inducing angiogenesis, vascular leak, or inflammation. Circulation. 2010;122:1725–1733. doi: 10.1161/CIRCULATIONAHA.110.957332. [DOI] [PubMed] [Google Scholar]
- 107.Bosisio D., Ronca R., Salvi V., Presta M., Sozzani S. Dendritic cells in inflammatory angiogenesis and lymphangiogenesis. Curr. Opin. Immunol. 2018;53:180–186. doi: 10.1016/j.coi.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 108.Longo V., Tamma R., Brunetti O., Pisconti S., Argentiero A., Silvestris N., Ribatti D. Mast cells and angiogenesis in pancreatic ductal adenocarcinoma. Clin. Exp. Med. 2018;18:319–323. doi: 10.1007/s10238-018-0493-6. [DOI] [PubMed] [Google Scholar]
- 109.Albini A., Bruno A., Noonan D.M., Mortara L. Contribution to tumor angiogenesis from innate immune cells within the tumor microenvironment: Implications for immunotherapy. Front. Immunol. 2018;9:527. doi: 10.3389/fimmu.2018.00527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wilson A.M., Shao Z., Grenier V., Mawambo G., Daudelin J.F., Dejda A., Pilon F., Popovic N., Boulet S., Parinot C., et al. Neuropilin-1 expression in adipose tissue macrophages protects against obesity and metabolic syndrome. Sci. Immunol. 2018;3:eaan4626. doi: 10.1126/sciimmunol.aan4626. [DOI] [PubMed] [Google Scholar]
- 111.Miller A.J. The grossly invisible and generally ignored lymphatics of the mammalian heart. Med. Hypotheses. 2011;76:604–606. doi: 10.1016/j.mehy.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 112.Aspelund A., Robciuc M.R., Karaman S., Makinen T., Alitalo K. Lymphatic system in cardiovascular medicine. Circ. Res. 2016;118:515–530. doi: 10.1161/CIRCRESAHA.115.306544. [DOI] [PubMed] [Google Scholar]
- 113.Kholova I., Dragneva G., Cermakova P., Laidinen S., Kaskenpaa N., Hazes T., Cermakova E., Steiner I., Yla-Herttuala S. Lymphatic vasculature is increased in heart valves, ischaemic and inflamed hearts and in cholesterol-rich and calcified atherosclerotic lesions. Eur. J. Clin. Investig. 2011;41:487–497. doi: 10.1111/j.1365-2362.2010.02431.x. [DOI] [PubMed] [Google Scholar]
- 114.Norman S., Riley P.R. Anatomy and development of the cardiac lymphatic vasculature: Its role in injury and disease. Clin. Anat. 2016;29:305–315. doi: 10.1002/ca.22638. [DOI] [PubMed] [Google Scholar]
- 115.Machnik A., Neuhofer W., Jantsch J., Dahlmann A., Tammela T., Machura K., Park J.K., Beck F.X., Muller D.N., Derer W., et al. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C-dependent buffering mechanism. Nat. Med. 2009;15:545–552. doi: 10.1038/nm.1960. [DOI] [PubMed] [Google Scholar]
- 116.Wiig H., Schroder A., Neuhofer W., Jantsch J., Kopp C., Karlsen T.V., Boschmann M., Goss J., Bry M., Rakova N., et al. Immune cells control skin lymphatic electrolyte homeostasis and blood pressure. J. Clin. Investig. 2013;123:2803–2815. doi: 10.1172/JCI60113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chen H.I., Poduri A., Numi H., Kivela R., Saharinen P., McKay A.S., Raftrey B., Churko J., Tian X., Zhou B., et al. VEGF-C and aortic cardiomyocytes guide coronary artery stem development. J. Clin. Investig. 2014;124:4899–4914. doi: 10.1172/JCI77483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mylonakis E., Calderwood S.B. Infective endocarditis in adults. N. Engl. J. Med. 2001;345:1318–1330. doi: 10.1056/NEJMra010082. [DOI] [PubMed] [Google Scholar]
- 119.Shahreyar M., Fahhoum R., Akinseye O., Bhandari S., Dang G., Khouzam R.N. Severe sepsis and cardiac arrhythmias. Ann. Transl. Med. 2018;6:6. doi: 10.21037/atm.2017.12.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ulloa-Morales A.J., Goodyear C.S., Silverman G.J. Essential domain-dependent roles within soluble IgG for in vivo superantigen properties of staphylococcal Protein A: Resolving the B-Cell Superantigen paradox. Front. Immunol. 2018;9:2011. doi: 10.3389/fimmu.2018.02011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Vigorito C., Giordano A., Cirillo R., Genovese A., Rengo F., Marone G. Metabolic and hemodynamic effects of peptide leukotriene C4 and D4 in man. Int. J. Clin. Lab. Res. 1997;27:178–184. doi: 10.1007/BF02912454. [DOI] [PubMed] [Google Scholar]
- 122.Levi R., Malm J.R., Bowman F.O., Rosen M.R. The arrhythmogenic actions of histamine on human atrial fibers. Circ. Res. 1981;49:545–550. doi: 10.1161/01.RES.49.2.545. [DOI] [PubMed] [Google Scholar]
- 123.Vigorito C., Poto S., Picotti G.B., Triggiani M., Marone G. Effect of activation of the H1 receptor on coronary hemodynamics in man. Circulation. 1986;73:1175–1182. doi: 10.1161/01.CIR.73.6.1175. [DOI] [PubMed] [Google Scholar]
- 124.Hattori Y., Levi R. Effect of PGD2 on cardiac contractility: A negative inotropism secondary to coronary vasoconstriction conceals a primary positive inotropic action. J. Pharmacol. Exp. Ther. 1986;237:719–724. [PubMed] [Google Scholar]
- 125.Gelderblom H.R., Hausmann E.H., Ozel M., Pauli G., Koch M.A. Fine structure of human immunodeficiency virus (HIV) and immunolocalization of structural proteins. Virology. 1987;156:171–176. doi: 10.1016/0042-6822(87)90449-1. [DOI] [PubMed] [Google Scholar]
- 126.Tseng Z.H., Secemsky E.A., Dowdy D., Vittinghoff E., Moyers B., Wong J.K., Havlir D.V., Hsue P.Y. Sudden cardiac death in patients with human immunodeficiency virus infection. J. Am. Coll. Cardiol. 2012;59:1891–1896. doi: 10.1016/j.jacc.2012.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zaaqoq A.M., Khasawneh F.A., Smalligan R.D. Cardiovascular complications of HIV-associated immune dysfunction. Cardiol. Res. Pract. 2015;2015:302638. doi: 10.1155/2015/302638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Theoharides T.C., Kavalioti M. Stress, inflammation and natural treatments. J. Biol. Regul. Homeost Agents. 2018;32:1345–1347. [PubMed] [Google Scholar]
- 129.Kritas S.K., Gallenga C.E., Ronconi G., Caraffa A., Toniato E., Lauritano D., Conti P. Impact of mold on mast cell-cytokine immune response. J. Biol. Regul. Homeost. Agents. 2018;32:763–768. [PubMed] [Google Scholar]
- 130.Gupta K., Idahosa C., Roy S., Lee D., Subramanian H., Dhingra A., Boesze-Battaglia K., Korostoff J., Ali H. Differential regulation of mas-related G Protein-coupled receptor X2-mediated mast cell degranulation by antimicrobial host defense peptides and porphyromonas gingivalis Lipopolysaccharide. Infect. Immun. 2017;85:e00246-17. doi: 10.1128/IAI.00246-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sala P., Tonutti E., Ruscio M., Colle R., Antonutto G., Falconieri G. IgE myeloma. Report of a new case and review of the literature. Haematologica. 1981;66:787–795. [PubMed] [Google Scholar]
- 132.Marone G., Tamburini M., Giudizi M.G., Biagiotti R., Almerigogna F., Romagnani S. Mechanism of activation of human basophils by Staphylococcus aureus Cowan 1. Infect. Immun. 1987;55:803–809. doi: 10.1128/iai.55.3.803-809.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Patella V., Giuliano A., Bouvet J.P., Marone G. Endogenous superallergen protein Fv induces IL-4 secretion from human Fc epsilon RI+ cells through interaction with the VH3 region of IgE. J. Immunol. 1998;161:5647–5655. [PubMed] [Google Scholar]
- 134.Siraganian R.P. An automated continuous-flow system for the extraction and fluorometric analysis of histamine. Anal. Biochem. 1974;57:383–394. doi: 10.1016/0003-2697(74)90093-1. [DOI] [PubMed] [Google Scholar]
- 135.De Paulis A., Cirillo R., Ciccarelli A., de Crescenzo G., Oriente A., Marone G. Characterization of the anti-inflammatory effect of FK-506 on human mast cells. J. Immunol. 1991;147:4278–4285. [PubMed] [Google Scholar]
- 136.Loffredo S., Ferrara A.L., Bova M., Borriello F., Suffritti C., Veszeli N., Petraroli A., Galdiero M.R., Varricchi G., Granata F., et al. Secreted phospholipases A2 in hereditary angioedema with C1-inhibitor deficiency. Front. Immunol. 2018;9:1721. doi: 10.3389/fimmu.2018.01721. [DOI] [PMC free article] [PubMed] [Google Scholar]