Abstract
Background
Elevated blood pressure (hypertension) affects about one billion people worldwide. It is important as it is a major risk factor for stroke and myocardial infarction. However, it remains a challenge for the medical profession as many people with hypertension have blood pressure (BP) that is not well controlled. According to Traditional Chinese Medicine theory, acupuncture has the potential to lower BP.
Objectives
To assess the effectiveness and safety of acupuncture for lowering blood pressure in adults with primary hypertension.
Search methods
We searched the Hypertension Group Specialised Register (February 2017); the Cochrane Central Register of Controlled Trials (CENTRAL) 2017, Issue 2; MEDLINE (February 2017); Embase (February 2017), China National Knowledge Infrastructure (CNKI) (January 2015), VIP Database (January 2015), the World Health Organisation Clinical Trials Registry Platform (February 2017) and ClinicalTrials.gov (February 2017). There were no language restrictions.
Selection criteria
We included all randomized controlled trials (RCTs) that compared the clinical effects of an acupuncture intervention (acupuncture used alone or add‐on) with no treatment, a sham acupuncture or an antihypertensive drug in adults with primary hypertension.
Data collection and analysis
Two review authors independently selected studies according to inclusion and exclusion criteria. They extracted data and assessed the risk of bias of each trial, and telephoned or emailed the authors of the studies to ask for missing information. A third review author resolved disagreements. Outcomes included change in systolic blood pressure (SBP), change in diastolic blood pressure (DBP), withdrawal due to adverse effects, and any adverse events. We calculated pooled mean differences (MD) with 95% confidence intervals (CI) for continuous outcomes using a fixed‐effect or random‐effects model where appropriate.
Main results
Twenty‐two RCTs (1744 people) met our inclusion criteria. The RCTs were of variable methodological quality (most at high risk of bias because of lack of blinding). There was no evidence for a sustained BP lowering effect of acupuncture; only one trial investigated a sustained effect and found no BP lowering effect at three and six months after acupuncture. Four sham acupuncture controlled trials provided very low quality evidence that acupuncture had a short‐term (one to 24 hours) effect on SBP (change) ‐3.4 mmHg (‐6.0 to ‐0.9) and DBP ‐1.9 mmHg (95% CI ‐3.6 to ‐0.3). Pooled analysis of eight trials comparing acupuncture with angiotensin‐converting enzyme inhibitors and seven trials comparing acupuncture to calcium antagonists suggested that acupuncture lowered short‐term BP better than the antihypertensive drugs. However, because of the very high risk of bias in these trials, we think that this is most likely a reflection of bias and not a true effect. As a result, we did not report these results in the 'Summary of findings' table. Safety of acupuncture could not be assessed as only eight trials reported adverse events.
Authors' conclusions
At present, there is no evidence for the sustained BP lowering effect of acupuncture that is required for the management of chronically elevated BP. The short‐term effects of acupuncture are uncertain due to the very low quality of evidence. The larger effect shown in non‐sham acupuncture controlled trials most likely reflects bias and is not a true effect. Future RCTs must use sham acupuncture controls and assess whether there is a BP lowering effect of acupuncture that lasts at least seven days.
Plain language summary
Acupuncture for primary hypertension in adults
Background
Hypertension (high blood pressure) affects about one billion people worldwide. Moreover, hypertension increases the risk of stroke and heart attack. Acupuncture is an important part of Traditional Chinese Medicine, in which thin needles are inserted into the skin at defined points. Acupuncture has been used to lower blood pressure and relieve symptoms of hypertension.
Study characteristics
We performed a systematic review of medical databases to find clinical trials that compared the effects of acupuncture to controls (sham (pretend) acupuncture, no treatment, or medicines) on blood pressure and safety in adults with hypertension. The results are current to February 2017.
Key results and certainty of the evidence
We found 22 trials including 1744 people. The trials did not look at death and general health. Four trials compared acupuncture with sham acupuncture and suggested a small short‐lasting (one to 24 hours) reduction in blood pressure. The other trials were of very poor quality. There was no evidence for a long‐lasting lowering of blood pressure by acupuncture that would be useful in the treatment of hypertension. We could not assess the safety of acupuncture as few trials reported this. At present, there is no evidence that acupuncture is useful in the management of long‐lasting hypertension. Future trials must be designed to measure a sustained blood pressure lowering effect of acupuncture.
Summary of findings
Background
Description of the condition
Elevated blood pressure (hypertension) is an important public‐health problem (Kearney 2005), affecting an estimated 640 million people worldwide (Mensah 2002). People with resting sustained elevated blood pressure are at higher risk of myocardial infarction, stroke (cerebral infarction and hemorrhage), congestive heart failure, and renal failure (Chobanian 2003; Howell 2004). Lifestyle changes, such as reducing salt intake, weight loss, and exercise, may lower blood pressure, but it is difficult to achieve and even more difficult to maintain. Several classes of antihypertensive medication are commonly prescribed, but they can be unaffordable and cause unacceptable adverse effects leading to lack of patient adherence (Chobanian 2003). Numerous studies have suggested that blood pressure is not adequately controlled in a significant number of people with hypertension (Wolf‐Maier 2004), and have emphasized that many people with elevated blood pressure resort to individualized therapy (Spence 2006). Since elevated blood pressure is a chronic condition, any treatment would need to have a sustained blood pressure lowering effect to be effective.
Description of the intervention
Acupuncture is an important part of Traditional Chinese Medicine (TCM) and it has been used to treat people with elevated blood pressure (BP) in China for centuries (Kaptchuk 2000). Presently, acupuncture is mainly used on people with elevated BP who want to avoid drug therapy or regard it as an alternative therapeutic option to reduce dosages of antihypertensive drugs (Napadow 2004; Turnbull 2007; Wan 2009). In the context of this review, acupuncture was defined as the needling of specific points of the body. Acupuncture is generally administered in a therapist's office.
How the intervention might work
The mechanism whereby acupuncture can lower BP is unclear. Acupuncture use is based on the TCM concept that diseases are due to disharmony in the body and there are channels (or 'meridians') of energy flow (called 'qi') within the body that can regulate the disharmony (Kalish 2004). When selected places (also called acupoints) on the meridians or collaterals are stimulated, diseases caused by dysregulation can be treated (Kaptchuk 2002). Mechanistic studies have demonstrated that acupuncture can normalize decreased parasympathetic nerve activity (Huang 2005), which is thought to result in increased excretion of sodium; reduced plasma renin, aldosterone, and angiotensin II activity; and changes in plasma norepinephrine, serotonin, and endorphin levels (Kalish 2004). For the management of chronic conditions, acupuncture can be practically administered monthly or at most weekly. Therefore, for it to be effective, it would need to reverse the elevated BP permanently or have a sustained effect for one week or more. A short‐term effect on BP for hours or even one to three days would not be sufficient to make it a practical therapy.
Why it is important to do this review
Several clinical trials have investigated the efficacy of acupuncture in lowering BP, but there is still debate as to whether acupuncture is a practical approach for this (Kaplan 2006; Moffet 2006). Previous systematic reviews have not used up‐to‐date Cochrane methodology to assess risk of bias and interpret the evidence in view of the biases, and have not addressed the important issue of duration of any BP lowering effect of the acupuncture (Dong 2012; Kim 2010; Kim 2012; Lee 2009). Consequently, we decided to conduct a systematic review based on the best currently available evidence and methodology to evaluate whether acupuncture lowers BP and whether the duration of the BP lowering effect is sufficiently long for the long‐term management of elevated BP.
Objectives
To assess the effectiveness and safety of acupuncture for lowering blood pressure in adults with primary hypertension.
Methods
Criteria for considering studies for this review
Types of studies
We included parallel randomized controlled trials (RCTs), and excluded cross‐over trials and trials that used a clearly inappropriate method of randomization (e.g. open alternation).
Types of participants
The review included men and non‐pregnant women over 18 years old who had been diagnosed with primary hypertension, with a systolic blood pressure (SBP) of 140 mmHg or greater or a diastolic blood pressure (DBP) of 90 mmHg or greater, or both or used antihypertensive drugs. We excluded participants with secondary hypertension, such as renal hypertension or hyperthyroidism; diabetes mellitus; atrial fibrillation; at least moderate valvular heart disease; and history of cerebrovascular events, endocrine disorders, and renal insufficiency.
Types of interventions
The interventions considered had to involve needle insertion at acupuncture points, pain points, or trigger points, and had to be described as acupuncture. We excluded other methods of stimulating acupuncture points without needle insertion (such as laser stimulation or transcutaneous electrical stimulation). Acupuncture could be used alone or as an add‐on to anti‐hypertensive drugs.
Control interventions accepted were:
no treatment;
sham acupuncture or minimal acupuncture (interventions mimicking 'true' acupuncture/true treatment, but deviating in at least one aspect considered important by acupuncture theory, such as skin penetration or non‐acupoint location);
antihypertensive drugs.
We excluded studies that only compared different forms or methods of acupuncture (e.g. transcutaneous electrical nerve stimulation) and compared acupuncture with any complementary and alternative therapies for which the efficacy is not yet established (e.g. Chinese herbs).
Types of outcome measures
We included studies that reported at least one clinical outcome related to hypertension, change in SBP or change in DBP. We documented the time after acupuncture that the BP measurement was taken if possible. We excluded studies reporting only physiological or laboratory parameters.
Primary outcomes
Change in SBP from baseline.
Change in DBP from baseline.
Secondary outcomes
Withdrawal due to adverse effects.
Adverse effect.
Search methods for identification of studies
Electronic searches
The Cochrane Hypertension Information Specialist searched the following databases without language, publication year or publication status restrictions:
the Cochrane Hypertension Specialised Register via the Cochrane Register of Studies (CRS‐Web) (searched 9 February 2017);
the Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Register of Studies (CRS‐Web) (searched 9 February 2017);
MEDLINE Ovid (from 1946 onwards), MEDLINE Ovid Epub Ahead of Print, and MEDLINE Ovid In‐Process & Other Non‐Indexed Citations (searched9 February 2017);
Embase Ovid (from 1974 onwards) (searched 9 February 2017);
ClinicalTrials.gov (www.clinicaltrials.gov) (9 February 2017);
World Health Organization International Clinical Trials Registry Platform (www.who.it.trialsearch) (searched 9 February 2017).
We also searched the China National Knowledge Infrastructure (CNKI) (1917 to January 2015), and the VIP Database (1989 to January 2015).
We searched the Database of Abstracts of Reviews of Effectiveness (DARE) and the Cochrane Database of Systematic Reviews (CDSR) for related reviews.
The MEDLINE Ovid search strategy (Appendix 2) was translated into the Cochrane Hypertension Specialised Register (Appendix 3), CENTRAL (Appendix 4), Embase (Appendix 5), AMED (Appendix 6), CNKI (Appendix 7), and VIP (Appendix 8) using appropriate controlled vocabulary. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled (as described in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, Box 6.4.c. (Handbook 2011)).
Searching other resources
The Cochrane Hypertension Information Specialist searched the Hypertension Specialised Register segment (which includes searches of MEDLINE, Embase, and Epistemonikos for systematic reviews) to retrieve existing reviews relevant to this systematic review, so that we could scan their reference lists for additional trials. The Specialised Register also includes searches for controlled trials in the Allied and Complementary Medicine Database (AMED), CAB Abstracts & Global Health, CINAHL, ProQuest Dissertations & Theses and Web of Science.
We checked the bibliographies of included studies and any relevant systematic reviews identified for further references to relevant trials.
Where necessary, we contacted authors of key papers and abstracts to request additional information about their trials.
We also searched Current Controlled Trials (www.controlled‐trials.com) and the Chinese Clinical Trial Register (www.chictr.org.cn).
Data collection and analysis
Selection of studies
Two review authors (JC, YR) independently screened all abstracts identified from the literature search, they excluded those that were clearly irrelevant (e.g. studies focusing on other conditions, reviews, etc.). We obtained full texts of all remaining references and the same two review authors screened and excluded clearly irrelevant papers according to the selection criteria. We resolved disagreements by discussion or with a third review author.
Data extraction and management
Two review authors (JC, YR) independently used a specially designed form to extract information on participants, methods, interventions, outcomes, and results. In particular, we extracted first author's name, year of publication; age; sex; duration of disease; sample size; number and type of centers, treated and analyzed; number of reasons for dropouts; duration of baseline, treatment, and follow‐up; details of acupuncture treatments (such as selection of points; number, frequency, and duration of sessions); achievement of De‐Qi (an irradiating feeling considered to indicate effective needling); number, training, and experience of acupuncturists; and details of control interventions (sham technique, type, and dosage of drugs). We extracted the net changes in SBP and DBP before and after acupuncture treatment as main outcome measures. We contacted the first or corresponding authors via email and asked them to provide additional information if necessary.
Assessment of risk of bias in included studies
At least two review authors (JY, JC, and MY) independently assessed risk of bias for each study as low, high, or unclear, using the 'Risk of bias' tool for Cochrane Reviews (Higgins 2011). We resolved disagreements by discussion or with a third review author. We used the following six criteria:
adequate sequence generation;
allocation concealment;
blinding (performance bias and detection bias);
incomplete outcome data;
selective reporting;
other bias.
We assessed risk of bias using the following recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
1. Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk (any truly random process, e.g. random number table, computer random number generator);
high risk (judged unlikely to be randomized);
unclear risk (method not reported).
2. Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal the allocation sequence in sufficient detail and determine whether intervention allocation could have been foreseen in advance of, or during, recruitment, or changed after assignment.
We assessed the methods as:
low risk (e.g. telephone or central randomization, consecutively numbered sealed opaque envelopes);
high risk (unsealed or non‐opaque envelopes);
unclear risk.
3. Blinding (checking for possible performance bias and detection bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We judged studies at low risk of bias if they were blinded, or if we judged that the lack of blinding could not have affected the results. We assessed blinding separately for different outcomes or classes of outcomes. A problem specific to acupuncture trials is that it is difficult to achieve blinding.
We assessed the methods as:
low risk, high risk, or unclear risk for participants;
low risk, high risk, or unclear risk for personnel;
low risk, high risk, or unclear risk for outcome assessors.
4. Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported; the numbers included in the analysis at each stage (compared with the total randomized participants); reasons for attrition or exclusion where reported; and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or was supplied by the trial authors, we reincluded missing data in the analyses that we undertook. We assessed the methods as:
low risk: trials where few dropout/losses to follow‐up were noted and an intention‐to‐treat (ITT) analysis was possible;
high risk: rate of exclusion was at least 20%, or wide differences in exclusions between groups whatever the ITT was used;
unclear risk.
5. Selective reporting bias (checking for possible reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk (where it was clear that all the study's prespecified outcomes and all expected outcomes of interest to the review were reported);
high risk (where not all the study's prespecified outcomes were reported; one or more reported primary outcomes were not prespecified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
unclear risk.
6. Other bias
We described for each included study any important concerns we had about other possible sources of bias.
We assessed whether each study was free of other problems that could put it at risk of bias as:
low risk;
high risk;
unclear risk.
Quality of the evidence
We used the GRADE system for grading the overall quality of the evidence (Atkins 2004). In GRADE, RCTs without important limitations and some observational studies are considered as high‐quality evidence. Five limitations can downgrade the quality of the evidence (Gordon 2008):
study limitations;
inconsistent results;
indirectness of evidence;
imprecision;
publication bias.
Three factors can upgrade the quality of evidence:
large magnitude of effect;
plausible confounding, which would reduce a demonstrated effect;
dose‐response gradient.
The quality of evidence and definitions were (Gordon 2008a):
high quality: further research is very unlikely to change our confidence in the estimate of effect;
moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate;
low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate;
very low quality: any estimate of effect is very uncertain.
Measures of treatment effect
Dichotomous data
For dichotomous data, we recorded the number of participants and incidence of events in each group; we expressed results as summary risk ratio (RR) with 95% confidence intervals (CI).
Continuous data
For continuous data, we used the mean difference (MD) if outcomes were measured in the same way between studies, and the standardized mean difference (SMD) to combine studies that measured the same outcome, but used different methods.
For the purposes of summarizing results, we categorized the included trials according to control groups: comparisons with sham acupuncture; comparisons with angiotensin‐converting enzyme inhibitor (ACEI); comparisons with calcium antagonists; comparisons with beta‐blockers; acupuncture plus ACEI compared with ACEI alone; acupuncture plus calcium antagonists compared with calcium antagonists alone.
Unit of analysis issues
Different units of analysis were planned to be subjected to a sensitivity analysis.
Dealing with missing data
We contacted the authors in China via telephone, and authors from elsewhere via email to obtain missing data, if necessary. For all outcomes, we carried out analyses, both per‐protocol (PP) analysis and ITT analysis would be accepted. Attrition rates, for example dropouts, losses to follow‐up, and withdrawals, were investigated.
Dealing with duplicate publications
In the case of duplicate publications and companion papers of a primary study, we tried to maximize yield of information by simultaneous evaluation of all available data. In cases of doubt, the original publication (usually the oldest version) was given priority.
Assessment of heterogeneity
We used the Chi2 and I2 test were used to assess for heterogeneity among the studies. I2 values were used to assess the degree of statistical heterogeneity. Less than 50% heterogeneity was accepted as homogeneous. When significant heterogeneity was present, we attempted to explain it by subgroup analyses.
Assessment of reporting biases
We did not perform funnel plots to assess the reporting bias due to the lack of sufficient studies (fewer than 10).
Data synthesis
We used Review Manager 5 software to carry out statistical analysis (RevMan 2014). We used MD for continuous data. There were no dichotomous data in this review (Higgins 2011). In the case of homogeneous data, we used the fixed‐effect model. In case of heterogeneity, we also used the random‐effects model. In this study, we identified five studies that included three arms (Li 2012a; Macklin 2006; Wang 2012a; Xie 2004; Zhang 2012a). Li 2012a compared warm acupuncture versus standard acupuncture versus captopril; Macklin 2006 compared traditional acupuncture versus standardized acupuncture versus sham acupuncture; Xie 2004 compared chronological acupuncture versus traditional acupuncture versus nitrendipine; Zhang 2012a compared acupuncture plus psychological counselling versus acupuncture versus captopril. In these four studies, the effect of groups that conveyed acupuncture treatment were combined to form a new group, because they compared different acupuncture methods and thus could be combined. Wang 2012a compared acupuncture versus nicardipine versus acupuncture plus nicardipine. In this case, we only extracted the data of acupuncture group and nicardipine group for analysis.
Subgroup analysis and investigation of heterogeneity
If one of the primary outcome parameters demonstrated statistically significant differences between intervention groups, we planned to use subgroup analyses. Planned subgroup analyses were:
different levels of hypertension;
different interventions;
sex.
Sensitivity analysis
We planned to test the robustness of the studies by contrasting the results of different measures, such as fixed‐effect model to random‐effects model, the robustness of the studies should not be reversed by changing of the models.
However, we did not perform sensitivity analyses due to an insufficient number trials.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; and Characteristics of ongoing studies tables.
Results of the search
We retrieved the following: 173 records from the Cochrane Hypertension Specialised Register, 460 from Cochrane Central Register of Controlled Trials, 270 from Ovid MEDLINE, 405 from Embase, 40 from AMED, 7 from ClinicalTrials.gov, 307 from CNKI, 518 from WangFang database, and 198 from VIP, 5 from Chinese Clinical Trial Register, giving a total of 1479 records after removal of duplicates.
We selected records that related to our question by scanning the title and reading the abstract of trials. The most frequent reasons for exclusion at this level were: studies were reviews or commentaries, studies of non‐primary hypertension, clearly non‐randomized design, and investigation of an intervention that was not true acupuncture involving skin penetration.
Two review authors assessed 107 full‐text papers for eligibility; 85 reports (including duplicates) did not meet the selection criteria. Common reasons for exclusion included: trial had mixed hypertension participants or not primary hypertension (21 trials); interventions did not meet our definition of acupuncture (eight trials); different forms or methods of acupuncture and compared acupuncture with any complementary and alternative therapies (25 trials); and incorrect randomization method (nine trials); design of trial was cross‐over (three trials); study with irrelevant outcome, such as only physiological or laboratory parameters (14 trials); trial with duplicate publications (five trials). Finally, we included 27 citations to 22 trials, 23 were published in journals (including published protocols), and four were published as part of Master's theses (Figure 1).
1.
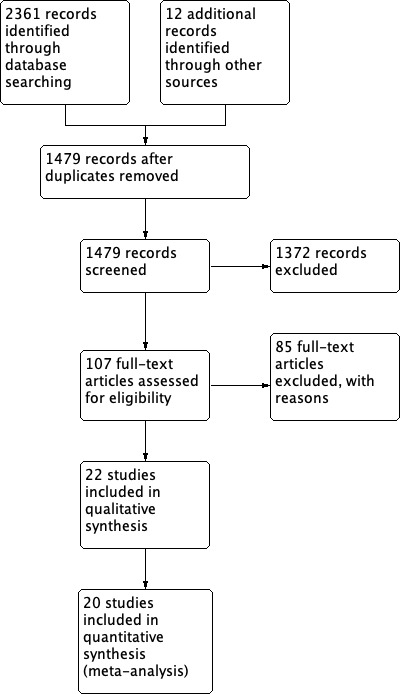
Study flow diagram.
Searches in the clinical trial registers identify one ongoing trial (Liang; see Characteristics of ongoing studies table).
Included studies
Participants
In total, 1744 people (972 in the acupuncture group, 772 in the control group) participated in the included studies, and the mean number of participants in each trial was 79 (ranging from 28 to 188 participants per trial). The participants were men and non‐pregnant women over 18 years old, with primary hypertension documented by at least three resting BP readings above (SBP/DBP) 140/90 mmHg or a history of hypertension with current use of antihypertensive medication. All the participants had primary hypertension. The number of participants ranged from 14 to 124 in the acupuncture groups and 14 to 68 in the controlled groups. Age ranged from 28 to 71 years. The participants receiving antihypertensive medicine accounted for 19.34% in the acupuncture group and 75.00% in the control group (drug control and sham acupuncture control), separately. All studies included both men and women. All studies were performed in a single center. Eighteen RCTs (1358 participants) originated in China, one (188 participants) came from the US (Macklin 2006), one (140 participants) came from Germany (Flachskampf 2007), and two (58 participants) came from Korea (Kim 2012; Yin 2007).
Interventions
All trials used a parallel group design, 17 trials had two arms (one acupuncture group and one control group) and five trials had three arms (Li 2012a; Macklin 2006; Wang 2012a; Xie 2004; Zhang 2012a).
The acupuncture interventions tested in the included trials varied. In 15 trials, acupuncture treatments were standardized (all participants were treated at the same points); in three trials, treatments were semi‐standardized (either all participants were treated with some basic points and additional individualized points depending on symptom patterns) (Chen 2010a; Dan 1998; Liu 2011); in two trials, the selection of acupuncture points was individualized (all participants were treated at individualized points depending on symptom patterns) (Flachskampf 2007; Yin 2007); and in two trials participants were randomized to two acupuncture groups: in one group the needles were placed at correct, individualized points after the full process of Chinese diagnosis, in the other group needles were placed at standardized points without the 'Chinese ritual' (to investigate whether the different interaction and process affected outcomes) (Macklin 2006;Xie 2004).
Four trials compared acupuncture with sham acupuncture interventions and 18 trials compared acupuncture and antihypertensive medicine treatment. The sham techniques varied considerably in the four sham controlled trials (Flachskampf 2007; Kim 2012; Macklin 2006; Yin 2007). Yin 2007 used the Park's sham needle device, in which the needles did not penetrate the skin, and the points were placed at the same predefined points as in the true treatment group. The other three sham controlled trials used non‐acupuncture points considered at variable distance from true points. Kim 2012 used needles superficially; Macklin 2006 inserted needles perpendicular to the skin without stimulation; and Flachskampf 2007 used acupuncture with the same technique as for active treatment, but used needling points without relevance for BP lowering according to TCM concepts.
In total, 18 trials compared acupuncture to antihypertensive medicine treatment using: nifedipine (Chen 2000; Dan 1998; Shen 2010a), nicardipine (Ma 2011; Wang 2012a), nitrendipine (Xie 2004), metoprolol (Chen 2006a), valsartan (Chen 2010a), metoprolol tartrate (Wu 2011), captopril (Hao 2006; Li 2012a; Liu 2011; Wu 2003; Yang 2010a; Zhang 2012a), enalapril maleate capsules (Guo 2009), levamlodipine besylate tablets/levamlodipine besylate tablets (Tian 2007), or captopril plus aspirin (Liao 2006).
Few trials provided detailed information about the acupuncturists' experience or expertise, treatment rationale, and reproducible description of the intervention.
Outcomes
The main outcome reported was change in BP and most trials (13) measured BP within minutes of an acupuncture session. Exceptions to that included six trials that measured BP by 24‐hour monitoring (Chen 2010a; Dan 1998; Flachskampf 2007; Hao 2006; Kim 2012; Yang 2010a). In those trials, the effect reflected the mean effect over the 24 hours after the session. Three trials measured BP one day (Wang 2012a), three days (Chen 2000), or within five days (Wu 2003) after the last acupuncture session. Thus, none of the RCTs assessed whether there was a sustained effect of acupuncture on BP. Further considerations of the impact of time of measurement are addressed in the Discussion. For the safety of acupuncture for hypertension, only eight trials recorded any adverse events.
Excluded studies
Eighty‐five studies did not meet the selection criteria (see Characteristics of excluded studies table). Common reasons for exclusion included: mixed hypertension participants or not primary hypertension (21 trials); interventions did not meet our definition of acupuncture (eight trials); different forms or methods of acupuncture and compared acupuncture with any complementary and alternative therapies (25 trials); and incorrect randomization method (nine trials); design of trial was cross‐over (three trials); no relevant outcomes reported, such as only physiological or laboratory parameters (14 trials); and trial with duplicate publications (five trials). We telephoned or emailed the original authors for detail of the studies, if necessary.
Risk of bias in included studies
We used the Cochrane 'Risk of bias' tool to assess the methodological quality of the trials (Figure 2; Figure 3).
2.
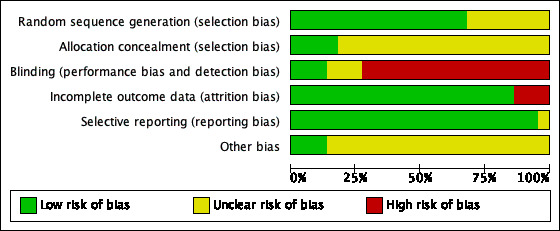
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
3.
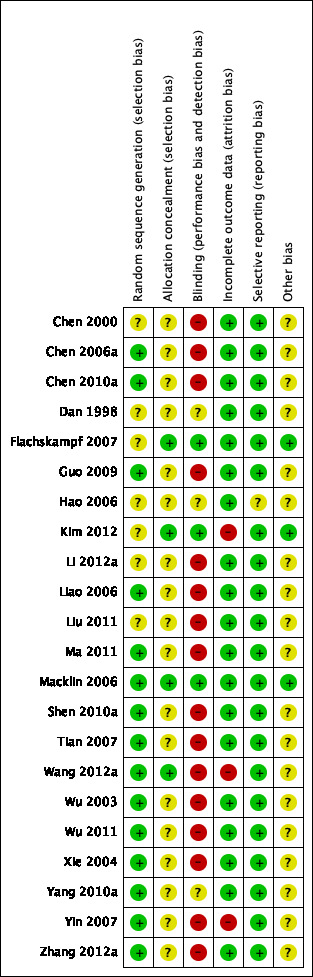
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Allocation
Eight studies described the method of generation of allocation sequence, which was by 'random number table' (Chen 2006a; Chen 2010a; Guo 2009; Ma 2011; Shen 2010a; Wu 2011; Xie 2004; Zhang 2012a); one study allocated the participants by 'random digits' (Wu 2003); one study reported the generation of randomization sequence by 'draw lots random' (Liao 2006); five studies allocated the participants by 'randomization software' used, such as NERI's software, SAS software, and excel software (Macklin 2006; Tian 2007; Wang 2012a; Yang 2010a; Yin 2007). However, seven studies mentioned randomly allocate participants, but gave no description of the randomization method in detail (Chen 2000; Dan 1998; Flachskampf 2007; Hao 2006; Kim 2012; Li 2012a; Liu 2011).
Four studies had low risk of allocation concealment, these guided a critical and feasible concealment for allocation of participants, such as opaque, sealed envelopes (Flachskampf 2007; Kim 2012; Macklin 2006; Wang 2012a), and one study had opened the envelopes after the participants had been included in the study, but the physician was not involved further (Kim 2012).
Blinding
Only five trials mentioned blinding, two of them had low risk of bias: Macklin 2006 masked the acupuncturist to random assignments, and did not inform participants that the control points were not traditional acupuncture points; in Yin 2007, the double‐blinding was likely successful as no‐one dropped out due to finding out the sham nature of their acupuncture sessions; the other three had unclear risk: Flachskampf 2007 described the test as single blinded, the Chinese physician who included participants was blinded, but with very short description only, unclear how participants were informed about the sham acupuncture; Kim 2012 described the test as double‐blinded, with very short description about participants and observers, and no information about how participants were informed about the sham acupuncture; Wang 2012a masked surveyor and statistics to random assignments, but did not mention whether acupuncturists and participants were blinded. The other trials did not mention blinding, and were at high risk of performance bias and detection bias.
Incomplete outcome data
Seventeen trials were at low risk of attrition bias, which reported no participants dropped out or were excluded from the primary analysis, and two trials had low risk for reporting the number of dropouts and related reasons, and using ITT analyses (Flachskampf 2007; Macklin 2006). Three trials were at high risk, two had participants who dropped out early or could not be analyzed, but there were no reasons given and no ITT analysis (Kim 2012; Wang 2012a). One trial had participants who dropped out, but they only used a PP analysis, and related reasons were explained (Yin 2007).
Selective reporting
Twenty‐one studies reported relevant outcomes in detail, which had low risk of reporting bias. Only one trial had unclear risk as they reported relevant outcomes during the treatment period, but no outcome reported in follow‐up (Hao 2006).
Other potential sources of bias
Similarity of comparison groups at baseline
Age, gender, race, clinical characteristics, and history were regarded as significant elements, which possibly affect the outcome measurements. All studies reported that the demographic, clinical status, and history of the two groups did not differ significantly, except the racial profile of one study that had more minority group participants in the control group by chance (Macklin 2006).
Conflicts of interest
Nine studies reported the source of financial support and declared no competing financial interests. The others neither stated the funding source nor mentioned whether the research was approved by an ethics committee.
Effects of interventions
Summary of findings for the main comparison. Acupuncture compared to sham acupuncture for hypertension.
| Acupuncture compared to sham acupuncture | |||
|
Patient or population: people with primary hypertension Settings: outpatient Intervention: acupuncture for 6‐10 weeks Comparison: sham acupuncture for 6‐10 weeks | |||
| Outcomes |
Mean difference (95% CI) mmHg |
No of participants (studies) | Certainty of the evidence (GRADE) |
| Change in SBP shortly after last session | ‐3.4 (‐6.0 to ‐0.9) | 386 (4 studies) | ⊕⊝⊝⊝ Very low1,2,3 |
| Change in DBP shortly after last session | ‐2.0 (‐3.6 to ‐0.3) | 386 (4 studies) | ⊕⊝⊝⊝ Very low3,4 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DBP: diastolic blood pressure; SBP: systolic blood pressure. | |||
| GRADE Working Group grades of evidence High certainty: Further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: We are very uncertain about the estimate. | |||
1Downgraded due to high risk of bias.
2Downgraded due to unexplained large heterogeneity (I2 = 76%).
3Downgraded due to small population and wide confidence intervals.
4Downgraded 2 levels due to high risk of bias.
Summary of findings 2. Safety of acupuncture for primary hypertension.
| Safety of acupuncture for primary hypertension | |||
|
Patient or population: people with primary hypertension Settings: primary care and community settings Intervention: acupuncture for 6‐10 weeks Comparison: sham acupuncture and antihypertensive drugs | |||
| Outcomes | Impacts | No of participants (studies) | Certainty of the evidence (GRADE) |
| Adverse events | There were adverse events associated with acupuncture in treating hypertension. Most events were trivial, including pain sensation during needle insertion and small spot‐bleeding (Kim 2012; Macklin 2006; Yin 2007). One study reported a serious adverse event, hypertensive emergency, in the acupuncture group (Flachskampf 2007). No deaths were reported from these trials. | 426 (4 studies) |
⊕⊕⊝⊝1 Low |
| GRADE Working Group grades of evidence High certainty: Further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: We are very uncertain about the estimate. | |||
1Downgraded 2 levels due to limited available data for judgment and lack of consistency of reports across studies.
Primary outcomes
Change in blood pressure
Sustained blood pressure lowering effect (greater than seven days)
Only one RCT investigated whether acupuncture had a sustained effect on BP (Flachskampf 2007). There was no BP lowering effect at three and six months after the last acupuncture session.
Short‐term blood pressure lowering effect (less than seven days, mostly within one to 24 hours)
Acupuncture versus sham acupuncture
This was the most important comparison in this review as it represented the best attempt to assess the short‐term BP lowering effect of acupuncture and reduce bias due to loss of blinding. Four trials compared acupuncture with sham acupuncture (Flachskampf 2007; Kim 2012; Macklin 2006; Yin 2007). Acupuncture reduced SBP compared to sham acupuncture (MD ‐3.43, 95% CI ‐5.92 to ‐0.85; Analysis 1.1), and reduced DBP (MD ‐1.95, 95% CI ‐3.95 to ‐0.32; Analysis 1.2). However, heterogeneity was high for SBP (I2 = 76%).
1.1. Analysis.
Comparison 1 Acupuncture versus sham acupuncture, Outcome 1 Change in systolic blood pressure.
1.2. Analysis.
Comparison 1 Acupuncture versus sham acupuncture, Outcome 2 Change in diastolic blood pressure.
Acupuncture versus renin‐angiotensin system (RAS) inhibitors
Eight trials compared acupuncture with RAS inhibitors (Chen 2010a; Guo 2009; Hao 2006; Li 2012a; Liao 2006; Wu 2003; Yang 2010a; Zhang 2012a). One of the trials was a three‐arm trial comparing acupuncture, warm needling, and ACEI (Li 2012a). The pooled result suggested that acupuncture reduced BP more than RAS inhibitors (SBP: MD ‐3.48, 95% CI ‐5.22 to ‐1.74; Analysis 2.1; DBP: MD ‐1.64, 95% CI ‐2.81 to ‐0.48; Analysis 2.2). However, these trials were not blinded and there was significant heterogeneity for SBP (I2 = 66%).
2.1. Analysis.
Comparison 2 Acupuncture versus RAS inhibitors, Outcome 1 Change in systolic blood pressure.
2.2. Analysis.
Comparison 2 Acupuncture versus RAS inhibitors, Outcome 2 Change in diastolic blood pressure.
Acupuncture versus calcium antagonists
Seven trials compared acupuncture with calcium antagonists (Chen 2000; Dan 1998; Ma 2011; Shen 2010a; Tian 2007; Wang 2012a; Xie 2004). One was a three‐arm trial comparing standard acupuncture, midnight‐noon ebb‐flow acupuncture, and calcium antagonists (Xie 2004). Another was a three‐arm trial comparing acupuncture, acupuncture plus calcium, and calcium antagonists (Wang 2012a). The pooled results suggested that acupuncture lowered BP more than calcium antagonists (SBP: MD ‐2.98, 95% CI ‐5.03 to ‐0.92; Analysis 3.1; DBP: MD ‐1.41, 95% CI ‐2.73 to ‐0.09; Analysis 3.2). However, these trials were not blinded and there was significant heterogeneity for both SBP (I2 = 92%) and DBP (I2 = 97%).
3.1. Analysis.
Comparison 3 Acupuncture versus calcium antagonists, Outcome 1 Change in systolic blood pressure.
3.2. Analysis.
Comparison 3 Acupuncture versus calcium antagonists, Outcome 2 Change in diastolic blood pressure.
Acupuncture versus beta‐blocker
Two trials compared acupuncture with beta‐blocker (Chen 2006a; Wu 2011). The pooled results showed no difference between treatments (SBP: MD 0.41, 95% CI ‐1.72 to 2.55; Analysis 4.1; DBP: MD ‐0.62, 95% CI ‐2.88 to 1.64; Analysis 4.2). However, these trials were not blinded and they showed significant heterogeneity for SBP (I2 = 82%).
4.1. Analysis.
Comparison 4 Acupuncture versus beta‐blocker, Outcome 1 Change in systolic blood pressure.
4.2. Analysis.
Comparison 4 Acupuncture versus beta‐blocker, Outcome 2 Change in diastolic blood pressure.
Acupuncture plus angiotensin‐converting enzyme inhibitor versus angiotensin‐converting enzyme inhibitor alone
One trial compared acupuncture plus ACEI with ACEI alone (Liu 2011). Acupuncture plus ACEI reduced SBP more than ACEI alone (MD ‐10.79, 95% CI ‐16.80 to ‐4.78), but not DBP (MD ‐0.24, 95% CI ‐3.94 to 3.46).
Acupuncture plus calcium antagonists versus calcium antagonists alone
One trial compared acupuncture plus calcium antagonists with calcium antagonists alone (Wang 2012a). Acupuncture plus calcium antagonists lowered SBP more than calcium antagonists alone (MD ‐6.25, 95% CI ‐11.65 to ‐0.85) but not DBP (MD ‐1.42, 95% CI ‐4.66 to 1.82)
Secondary outcomes
Adverse events
Eight trials recorded adverse events. Major adverse events occurring in the acupuncture group were headache (one participant in Chen 2010a), pain (two participants in Flachskampf 2007; Kim 2012), spot‐bleeding (eight participants in Yin 2007; Kim 2012), time‐related reason (Flachskampf 2007). Serious adverse events were reported in Macklin 2006: hypertensive urgencies (two participants) and congestive heart failure (one participant). Adverse events in the control group were headache (six participants in Chen 2010a (Drug: Diovan); two participants in Tian 2007 (Drug: levamlodipine maleate tablets)), dizziness (seven participants in Chen 2010a (Drug: Diovan)), cough (one participant in Chen 2010a (Drug: Diovan)), nausea and heart palpitations (two participants in Tian 2007 (Drug: levamlodipine maleate tablets)), foot edema/flush/rash/flustered (six participants in Wang 2012a (Drug: Nicardipine)). Two trials reported no serious adverse events (Hao 2006; Kim 2012).
Subgroup analyses
We performed no subgroup analyses due to an insufficient number of trials.
Discussion
Summary of main results
In recent years, there have been many publications and studies on the BP lowering effect of acupuncture. However, interpretation of this evidence from these studies is difficult. Thus, at present, it is not known whether acupuncture is an effective therapy for chronic hypertension. In this review, we attempted to clarify this by identifying what type of evidence is required for acupuncture to be a useful therapy in the community. Since elevated blood pressure is a chronic condition, in order to be effective any treatment would need to have a blood pressure lowering effect sustained for at least seven days and preferably for one month. We found only one trial that tested whether there was a sustained BP lowering effect of acupuncture compared to sham acupuncture after a six‐week course of active acupuncture (Flachskampf 2007). In that trial, there was no change in BP at three and six months after the last acupuncture treatment. None of the other trials reported the effect on BP more than five days after the last session. Therefore, we can report that, at present, there is no evidence for the use of acupuncture to treat chronic hypertension in the community.
The results of this review only relate to the short‐term effects of acupuncture, in most cases within one hour or one day of the last acupuncture session. There are only four RCTs with a rigorous design in which acupuncture was compared to a form of sham acupuncture (Flachskampf 2007; Kim 2012; Macklin 2006; Yin 2007). The pooled effect of these trials suggested that acupuncture causes a short‐term non‐clinically significant reduction of BP by 3/2 mmHg when compared with sham acupuncture; however, this was very low quality evidence (see Table 1).
In the other trials, the participants were not blinded to the acupuncture intervention and BP was measured within hours to one day after the last acupuncture session. Eight trials compared acupuncture with RAS inhibitors administered daily and suggested that acupuncture lowered BP by 3/2 mmHg more than RAS inhibitors (Chen 2010a; Guo 2009; Hao 2006; Li 2012a; Liao 2006; Wu 2003; Yang 2010a; Zhang 2012a). If this were true and it was sustained, it would be clinically important as ACEI have been shown in one Cochrane Review to lower BP by 8/5 mmHg (Heran 2008). However, this suggests a BP lowering effect of 11/7 mmHg, which is not consistent with the findings compared to sham acupuncture. Because of this, and the high risk of loss of blinding bias and publication bias, we have not reported these data in a 'Summary of findings' table.
Nine trials suggested that acupuncture reduced BP by 3/1 mmHg more than daily calcium antagonists (Chen 2000; Chen 2006a; Dan 1998; Ma 2011; Shen 2010a; Tian 2007; Wang 2012a; Wu 2011; Xie 2004). If this were sustained and true it would be clinically important as calcium antagonists lower BP by about 10/6 mmHg on average based on one Cochrane Review in preparation (Wong 2002). This suggests a large effect of 13/7 mmHg, which is not consistent with the sham blinded trials. In the forest plot, the obvious outlier, Shen 2010a, contributed to the high heterogeneity. The large BP lowering effect of acupuncture in this trial could be explained by the mean baseline BP being over 200/120 mmHg, which is much higher than the other included studies. This may result in overestimation of acupuncture effect and underestimation of drug effect. Therefore, this finding has inconsistency problems and the same risk of bias as with the ACEIs; for this reason, we have not reported these data in a 'Summary of findings' table.
Two trials suggested that acupuncture lowered BP the same as daily metoprolol beta‐blocker therapy (Chen 2006a; Wu 2011). One Cochrane Review showed that metoprolol lowered BP by 6/5 mmHg (Wong 2016). One trial (Liu 2011) investigated the addition of acupuncture to ACEI and did not add any additional evidence. If future trials of acupuncture are conducted, they need to be designed to measure a sustained BP lowering effect at least seven days and preferably one month after the acupuncture.
This review provided very little information as to the safety of acupuncture.
Overall completeness and applicability of evidence
Acupuncture treatment approaches vary in different countries and settings. The trials included in our review came from a variety of countries. In the German trial, acupuncture was mainly provided by Chinese physicians, who were professionally trained in China for acupuncture (Flachskampf 2007). All Chinese physicians had at least five years of training in TCM, combined with five years of training in Western medicine, with additional practice of acupuncture of several years. In the US trial, TCM diagnosing and acupuncture treatment were performed independently by diagnosing acupuncturist with a minimum three years' postgraduate experience and treating acupuncturist with a minimum 1 year' postgraduate experience. In practice, the participating diagnosing acupuncturists had 13 to 22 years' experience, and all had received acupuncture training in colleges in China. All participating acupuncturists delivering acupuncture treatment had two to eight years' experience, and were licensed to practice in Massachusetts. (Training and certification for acupuncturists consisted of studying detailed training manuals and videotapes and attending an eight‐hour practical training session with a competency/certification exam (Macklin 2006). In atrial from Korea, physicians were trained in the context of traditional Korean medicine (Kim 2012). The acupuncture treatment forms differed due to practitioners with different qualifications in different countries may confound the results. Sessions of acupuncture treatment may vary in different countries, which may lead to differences. For instance, in most trials from China, acupuncture was performed once a day for a consecutive course, while in the US or Germany, acupuncture was mostly conducted two or three times a week. None of the trials reflected a course of treatment that would be practical in real practice. Moreover, most clinical trials were performed in a restricted experimental condition, by which the inclusion of the participants was highly selective. This is likely quite different from real‐world conditions where hypertension is commonly accompanied with other conditions. As explained, the results only relate to a short‐term effect of acupuncture, which does not answer whether it would be effective in managing chronic hypertension.
Quality of the evidence
The methodological quality of included trials was variable. Even in the sham controlled trials, we downgraded the evidence to very low using GRADEPro (https://gradepro.org/). We appreciate that designing and performing clinical trials of acupuncture is a challenge, particularly with respect to blinding and selection of control interventions. Many old and small trials from China decrease the validity of the results. Since journals are more likely to report positive results, there is a high risk of publication bias. The wide clinical heterogeneity of included trials was also a limitation. Differences in controls, duration of treatment, frequency of sessions, the selected acupoints used, the number of acupoints, and the use of different antihypertensive medicines all added to the heterogeneity.
Potential biases in the review process
First, bias could be generated by the omission of completed studies. Although we conducted extensive searches to identify relevant trials, we cannot rule out the possibility that there are additional trials that are unpublished or published in sources inaccessible to our search. Second, we could not include the data from ongoing clinical trials. Though we approached the responsible investigators, we were not provided with the data.
Agreements and disagreements with other studies or reviews
Our review agrees with other studies in the aspect that acupuncture as a complement to conventional drugs reduces BP, though with uncertainty. One systematic review reported that acupuncture significantly improved both SBP and DBP in people receiving antihypertensive medication (Li 2014). They did not address the issue of duration of effect. It was similar to our findings with non‐sham acupuncture controlled trials, but we disregarded the findings from those trials due to the high risk of bias. In their review, only minor adverse events were identified and this agrees with our results. One review assessed acupuncture either as an adjunct or an alternative in lowering BP, and reported that it was inconclusive whether acupuncture lowers high BP (Lee 2009). The difference with our review was that it used a slightly wider inclusion criterion on mild arterial hypertension, mild or moderate arterial hypertension, or BP within or higher than the prehypertension category, without predescribing a limit to primary hypertension. Another review assessed the efficacy of acupuncture for essential hypertension, particularly that of individualized acupuncture treatment based on TCM diagnosis (Kim 2010). They showed reduction in BP between acupuncture and control, but did not include trials published after 2008. More well designed, rigorous, and large trials in the field are needed. Moreover, our conclusions on the certainty of evidence agrees with a study published in 2013, which emphasized that the methodological quality of the included trials was evaluated as generally low (Wang 2013).
Authors' conclusions
Implications for practice.
At present, there is no evidence for the sustained blood pressure lowering effect of acupuncture that is required for the management of hypertension. Acupuncture may be associated with a short‐term (one to 24 hour) reduction in blood pressure; however, in sham acupuncture trials, the effect at best is small (reduction in systolic/diastolic blood pressure of 3/2 mmHg) and likely clinically irrelevant. The larger effect shown in non‐sham acupuncture controlled trials most likely reflects bias and not a true effect.
Implications for research.
As hypertension is a chronic condition, it is essential that for acupuncture to be useful it must cause a sustained blood pressure lowering effect. Future randomized controlled trials (RCTs) are needed to determine whether acupuncture lowers blood pressure for at least seven days and preferably longer. The control group in these RCTs must be sham acupuncture. RCTs with improper controls and measuring short term effects on blood pressure are not needed.
Acknowledgements
We thank Ciprian Jauca, Managing Editor of Cochrane Hypertension Review Group, for suggesting improvements to the protocol and co‐ordinating the entire process of our review, Douglas Salzwedel, Cochrane Information Specialist of Cochrane Hypertension Review Group, for literature retrieving, and the editorial board members of Cochrane Hypertension Review Group for suggestions and comments to our review.
Appendices
Appendix 1. Data extraction forms
|
General information |
Notes | |
| Title | ||
| First author | |
|
| Author affiliation | ||
| Author degree | ||
| Institution | ||
| Source of this article | ||
| Verification of study eligibility | Correct population? Correct intervention? Correct outcome? Correct study design? |
|
|
Methods |
||
| Posture of measuring blood pressure | Standing, sitting, supine, other | |
| Blood pressure measurements | Hand movement, electronic, 24‐hour ambulatory blood pressure monitoring, other | |
| Study design | RCT, other | |
| Unit of allocation | Patient, hospital, school | |
| Unit of analysis | ||
| Power calculation | ||
| Method of randomisation | ||
| Allocation concealment | ||
| Blindedness | ||
|
Population |
||
| Recruitment of patients | ||
| Place | Hospital / City / Country | |
| Enrollment dates | ||
| Inclusion criteria | ||
| Exclusion criteria | ||
| Age | ||
| Sex | ||
| Ethnicity | ||
| Work status | ||
| Diagnosis of disease |
How did the authors define the disease? | |
| Outcome measures |
For example, duration of illness, severity of symptoms, etc. | |
| Total number of patients recruited | ||
| Number of patients who met inclusion criteria | ||
| Total number of patients randomised | ||
| Total number of patients followed up | ||
|
Interventions: |
||
| Intervention | ||
| Control group(s) | ||
|
Outcomes |
||
| Who carried out the measurement? | ||
| What was measured at baseline? How was it measured? Is the tool validated (as stated in the article)? | ||
| What was measured immediately after the intervention? How was it measured? Is the tool validated (as stated in the article)? | ||
| When was the first follow‐up? What was measured at the first follow‐up? How was it measured? Is the tool validated (as stated in the article)? |
||
|
Analysis: |
||
| Statistical technique used: |
Which tests? Alpha? Power? Sample size calculation? Software used. | |
| Intention‐to‐treat analysis? |
Patients were analysed according to the group they were randomised. | |
| Does the technique adjust for confounding? | ||
| Number (or %) of followed up from each group | ||
|
Results: |
|
|
| Quantitative results (e.g. estimates of effect size, between group P values) |
If between‐group comparisons are given, please use the next page. If no between‐group comparisons are given, then report here the general results. |
|
| Qualitative results | ||
| Cost of intervention | ||
| Cost‐effectiveness | ||
| Adverse effects or complications |
Appendix 2. MEDLINE search strategy
Database: Ovid MEDLINE(R) 1946 to Present with Daily Update
Search Date: 9 February 2017
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 exp acupuncture therapy/ 2 (acupunctur$ or electroacupunctur$ or electro‐acupunctur$ or acupoint$ or acu‐point$ or acupress$).mp. 3 ((meridian$ or non‐meridian or trigger) adj10 point$).tw. 4 (zhenjiu or zhen jiu or zhenci or zhen ci or cizhen or dianzhen or dian zhen or zhen ya or er zhen or ti zhen or she zhen or tou pi zhen or zue wei).tw. 5 ((ching adj2 lo) or (jing adj2 luo) or jinglo).tw. 6 or/1‐5 7 hypertension/ 8 hypertens$.tw. 90 exp blood pressure/ 10 (blood pressure or bloodpressure).tw. 11 or/7‐10 12 randomized controlled trial.pt. 13 controlled clinical trial.pt. 14 randomized.ab. 15 placebo.ab. 16 drug therapy.fs. 17 randomly.ab. 18 trial.ab. 19 groups.ab. 20 or/12‐19 21 animals/ not (humans/ and animals/) 22 20 not 21 23 6 and 11 and 22 24 remove duplicates from 23
Appendix 3. Cochrane Hypertension Specialised Register search strategy
Database: Cochrane Hypertension Specialised Register
Search Date: 9 February 2017
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
#1 ((acupunctur* or electroacupunctur* or electro‐acupunctur* or acupoint* or acu‐point* or acupress* or meridian* or non‐meridian* or trigger point*)) AND INSEGMENT #2 (meridian* or non‐meridian or trigger) AND INSEGMENT #3 (zhenjiu or zhen jiu or zhenci or zhen ci or cizhen or dianzhen or dian zhen or zhen ya or er zhen or ti zhen or she zhen or tou pi zhen or zue wei) AND INSEGMENT #4 (ching lo or jing luo or jinglo) AND INSEGMENT #5 #1 OR #2 OR #3 OR #4 AND INSEGMENT #6 (antihypertens* OR hypertens*) AND INSEGMENT #7 (blood pressure OR bloodpressure) AND INSEGMENT #8 #6 OR #7 AND INSEGMENT #9 #5 AND #8 AND INSEGMENT #10 RCT:DE AND INSEGMENT #11 (Review OR Meta‐Analysis):MISC2 AND INSEGMENT #12 #9 AND (#10 OR #11)
Appendix 4. CENTRAL search strategy
Database: Cochrane Central Register of Controlled Trials (2017 Issue 2) via Cochrane Register of Studies Online
Search Date: 9 February 2017
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
#1 (acupunctur* or electroacupunctur* or electro‐acupunctur* or acupoint* or acu‐point* or acupress*) #2 (meridian* or non‐meridian or trigger) #3 (zhenjiu or zhen jiu or zhenci or zhen ci or cizhen or dianzhen or dian zhen or zhen ya or er zhen or ti zhen or she zhen or tou pi zhen or zue wei) #4 (ching lo or jing luo or jinglo) #5 #1 or #2 or #3 or #4 or #6 antihypertens* or hypertens* #7 (blood pressure or bloodpressure) #8 #6 OR #7 #9 #5 AND #8
Appendix 5. EMBASE search strategy
Database: Embase <1974 to 9 February 2017>
Search Date: 9 February 2017
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 exp acupuncture/ 2 (acupunctur$ or electroacupunctur$ or electro‐acupunctur$ or acupoint$ or acu‐point$ or acupress$).mp. 3 ((meridian$ or non‐meridian or trigger) adj10 point$).tw. 4 (zhenjiu or zhen jiu or zhenci or zhen ci or cizhen or dianzhen or dian zhen or zhen ya or er zhen or ti zhen or she zhen or tou pi zhen or zue wei).tw. 5 ((ching adj2 lo) or (jing adj2 luo) or jinglo).tw. 6 or/1‐5 7 exp hypertension/ 8 hypertens$.tw. 9 (blood pressure or bloodpressure).mp. 10 or/7‐9 11 randomized controlled trial/ 12 crossover procedure/ 13 double‐blind procedure/ 14 (randomi?ed or randomly).tw. 15 (crossover$ or cross‐over$).tw. 16 placebo.ab. 17 (doubl$ adj blind$).tw. 18 assign$.ab. 19 allocat$.ab. 20 or/11‐19 21 10 and 20 22 (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 23 21 not 22 24 6 and 10 and 23 25 remove duplicates from 24
Appendix 6. AMED search strategy
Database: AMED (Allied and Complementary Medicine) <1985 to January 2014>
Search Date: 9 February 2017
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 exp acupuncture therapy/ 2 (acupuncture$ or electroacupuncture$ or electro‐acupuncture$ or acupoint$ or acupoint$ or acupress$).mp. 3 ((meridian$ or non‐meridian or trigger) adj10 point$).tw. 4 (zhenjiu or zhen jiu or zhenci or zhen ci or cizhen or dianzhen or dian zhen or zhen ya or er zhen or ti zhen or she zhen or tou pi zhen or zue wei).tw. 5 ((ching adj2 lo) or (jing adj2 luo) or jinglo).tw. 6 or/1‐5 7 hypertension/ 8 antihypertensive agents/ 9 hypertens$.tw. 10 blood pressure/ 11 ((blood or arterial or diastolic or systolic) adj2 pressure).tw. 12 bloodpressure.tw. 13 or/7‐12 14 randomised controlled trials/ 15 randomised controlled trial.pt. 16 double blind method/ 17 random allocation/ 18 (randomised or randomised).tw. 19 (crossover or cross‐over).tw. 20 placebo$.tw. 21 (single$ blind$ or double$ blind$).tw. 22 assign$.ab. 23 allocate$.ab. 24 group$.ab. 25 trial.tw. 26 or/14‐25 27 76 and 13 and 26
Appendix 7. CKNI search strategy
Database: China National Knowledge Infrastructure
Search Date: 9 February 2017
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
((( (全文=中英文扩展(针刺) 并且 全文=中英文扩展(高血压))) 或者 (题名=中英文扩展(针刺) 并且 题名=中英文扩展(高血压))) 或者 (主题=中英文扩展(针刺) 并且 主题=中英文扩展(高血压))) 或者 (关键词=中英文扩展(针刺) 并且 关键词=中英文扩展(高血压)))
Appendix 8. VIP search strategy
Database: Chongqing VIP
Search Date: 9 February 2017
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
(((((文摘=针刺)*1989‐2013)*(文摘=高血压) + ((题名=针刺) * 1989‐2013) * (题名=高血压)) + ((关键词=针刺) * 1989‐2013) * (关键词=高血压)) + (题名或关键词=针刺*年=1989‐2013) * (题名或关键词=高血压))
Data and analyses
Comparison 1. Acupuncture versus sham acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in systolic blood pressure | 4 | 386 | Mean Difference (IV, Fixed, 95% CI) | ‐3.38 [‐5.92, ‐0.85] |
| 2 Change in diastolic blood pressure | 4 | 386 | Mean Difference (IV, Fixed, 95% CI) | ‐1.95 [‐3.59, ‐0.32] |
Comparison 2. Acupuncture versus RAS inhibitors.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in systolic blood pressure | 8 | 532 | Mean Difference (IV, Fixed, 95% CI) | ‐3.48 [‐5.22, ‐1.74] |
| 2 Change in diastolic blood pressure | 8 | 532 | Mean Difference (IV, Fixed, 95% CI) | ‐1.64 [‐2.81, ‐0.48] |
Comparison 3. Acupuncture versus calcium antagonists.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in systolic blood pressure | 7 | 472 | Mean Difference (IV, Fixed, 95% CI) | ‐2.98 [‐5.03, ‐0.92] |
| 2 Change in diastolic blood pressure | 7 | 472 | Mean Difference (IV, Fixed, 95% CI) | ‐1.41 [‐2.73, ‐0.09] |
Comparison 4. Acupuncture versus beta‐blocker.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in systolic blood pressure | 2 | 180 | Mean Difference (IV, Fixed, 95% CI) | 0.41 [‐1.72, 2.55] |
| 2 Change in diastolic blood pressure | 2 | 180 | Mean Difference (IV, Fixed, 95% CI) | ‐0.62 [‐2.88, 1.64] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chen 2000.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 2 weeks' treatment; no follow‐up. |
|
| Participants |
Number of participants screened/included/analyzed: not reported/70/70. Number of participants in each group: 35:35. Demographics: mean age 63.57 years in A, mean age 65.20 years in B; number of women 16:16. Number of participants who used antihypertensive: no information. Course of disease: no information. Setting: inpatients and outpatients from The First People's Hospital of Chengdu. |
|
| Interventions |
Acupuncture points: Quchi, Fenglong. Information on acupuncturists: none. Deqi achieved?: yes. Frequency and duration of treatments: BP measured every 4 hours, when BP at stable normal level, BP measured every morning and before retiring. Control group intervention: nifedipine (Chengdu Pharmaceutical factory), 10‐20 mg, TID, at 8 a.m., for 2 weeks. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
|
|
| Study detail |
Position for measuring BP: decubitus position. BP measurements: no information. Time of each session: needles retained for 15‐30 min, stimulated every 5 min. Number of treatment sessions: 14 (continuously for 14 days). Frequency of treatment sessions: no information, 2 weeks was a course. Time of recruiting: 1997‐1999. Adverse events: no information. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: peer review journal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly allocate participants" mentioned, but no detailed description of the randomization method. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "70 participants included" mentioned in results, numbers of participants were matched with information. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Unclear risk | No description. |
Chen 2006a.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 4 weeks' treatment; no follow‐up. |
|
| Participants |
Number of participants screenings/included/analyzed: not reported/60/60. Number of participants in each group: 30:30 Demographics: aged 36‐65 years, mean age 54.75 years in A, aged 33‐61 years, mean age 51.72 years in B; number of women 10:9. Number of participants who used antihypertensive: no information. Course of disease: from 1 month to 10 years, mean 5.65 years in A; from 6.5 months to 10.42 years, mean 5.39 years in B Setting: inpatients from Department of Acupuncture and Moxibustion in the first hospital in Wuhan. |
|
| Interventions |
Acupuncture points: Fengchi (bilateral). Information on acupuncturists: none. Deqi achieved?: yes. Control group intervention: metoprolol (25 mg pills, Batch number Su Wei medicine approved by 1985, 326201), 100 mg, once daily, at 8 a.m., for 4 weeks. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: no information. Time of each session: needles retained for 30 min, stimulated every 10 min. Number of treatment sessions: 28 (continuously for 4 weeks). Frequency of treatment sessions: no information, 2 weeks was a course. Time of recruiting: March 2004 to December 2004. Adverse events: no information. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. Non‐commercial funding: yes (State administration of TCM). Publication status: peer review journal. |
|
| Notes | Baseline BP: mean BP on 3 different days before treatment. Last BP: mean BP in last 3 days before ceasing treatment. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or exclusions from analysis. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Unclear risk | No description. |
Chen 2010a.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 34 days' treatment; no follow‐up. |
|
| Participants |
Number of participants screened/included/analyzed: not reported/80/80. Number of participants in each group: 40:40. Demographics: mean age 61.3 years in A, mean age 62 years in B; number of women 19:20. Number of participants who used antihypertensives: no information. Course of disease: mean 16 years in A; mean 17.3 years in B. Setting: outpatients and inpatients from German Otto Boylen Hospital. |
|
| Interventions |
Acupuncture points: main points: Fengchi (GB20), Quchi (LI11), Taichong (LR3), Sanyinjiao; assistant points: Xingjian (LR2), Xiaxi (GB43); Yin deficiency and yang excess: Ganshu (BL18) and Fuliu (KI7); Phlegm wet indicates sheng: Fenglong and Yinlingquan; Yin‐yang deficiency: Guanyuan (CV4) and Shenshu (BL23). Information on acupuncturists: none. Deqi achieved?: yes. Control group intervention: valsartan (Novartis), 80 mg, once daily for 30 days. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
|
|
| Study detail |
Position for measuring BP: sitting position and ambulatory BP monitoring. BP measurements: ambulatory BP monitoring by MOBIL‐O‐GRAPHÓ, made in Germany. Time of each session: needles retained for 30 min, stimulated every 10 min. Number of treatment sessions: 28 (continuously for 4 courses). Frequency of treatment sessions: once daily, 7 days was a course, 2‐day interval between 2 courses. Time of recruiting: December 2004 to December 2008. Adverse events: 1/40 had headache in A; 6/40 had headache, 7/40 had dizziness, 1/40 had cough in B. |
|
| Publication detail |
Language of publication: Chinese Commercial funding: no Non‐commercial funding: no Publication status: peer review journal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or exclusions from analysis. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Unclear risk | No description. |
Dan 1998.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 3 weeks' treatment; no follow‐up. |
|
| Participants |
Number of participants screenings/included/analyzed: not reported/52/52. Number of participants in each group: 26:26. Demographics: mean age 57.8 years in A, 48.35 years in B; number of women 7:8. Number of participants who used antihypertensives: no information. Course of disease: 5‐25 years, mean 9.4 years in A; 4‐26 years, mean 8.8 years in B. Setting: inpatients from Beijing Chaoyang Second Hospital. |
|
| Interventions |
Acupuncture points: main points: Quchi, Hegu, Taichong, Fengchi, Geshu; assistant points: Yin deficiency and yang excess: Fuliu, Neiguan; The phlegm wet resistance: Fenglong, Gongsun; Yin‐yang deficiency: Zusanli, Sanyinjiao. Information on acupuncturists: none. Deqi achieved?: yes. Control group intervention: nifedipine, 10 mg, TID, for 3 weeks. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
|
|
| Study detail |
Position for measuring BP: activity not restricted for ambulatory BP monitoring. BP measurements: Accutracker Ⅱ (Suntech MedicalIns, Raleigh, NC USA), non‐invasive portable ambulatory BP monitoring. Time of each session: needles retained for 20‐30 min, stimulated after 10 min of inserting needle. Number of treatment sessions: 15 (lasting 3 weeks). Frequency of treatment sessions: once daily, 5 times a week. Time of recruiting: no information. Adverse events: no information. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: peer review journal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only described randomization used, but no description of the method and detail of randomization. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants and investigators not blinded to acupuncture or pills. Detection bias reduced as BP was measured with automatic 24‐hour monitor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or exclusions from analysis. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Unclear risk | No description. |
Flachskampf 2007.
| Methods |
Groups: A: active acupuncture, B: sham acupuncture (80% of participants with antihypertensive). Blinding: participants, Chinese physician who included participants. Dropouts/withdrawals: in 2 weeks between randomization and initiation of treatment: 7/83 in A, 4/77 in B; during the treatment course: 4/76 in A, 5/73 in B; first follow‐up visit: 0/72 in A, 0/68 in B; second follow‐up visit: 4/72 in A, 1/68 in B; third visit: 1/68 in A, 1/67 in B. Duration of intervention: no information of baseline; 6 weeks' treatment; 3 follow‐up visits: first (immediate) post‐treatment follow‐up visit within 3 working days after finishing treatment; second 3 months after finishing treatment; third 6 months after finishing treatment. |
|
| Participants |
Number of participants screenings/included/analyzed: 342/160/140. Number of participants in each group: 72:68. Demographics: mean age 58.8 years in A, 58.0 years in B; number of women 46:60. Number of participants who used antihypertensives: 53:52. Course of disease: no information. Setting: outpatients at Med Klinik, Klinikum Ottobeuren. |
|
| Interventions |
Acupuncture points: needling points chosen according to Chinese type of hypertension, and angle, depth, and type of manipulation of needling conformed to typical prescriptions (3 acupuncture points were needled bilaterally except single points such as Taiyang): Taiyang, KG12, KG6, KG4, Di11, Di4, Ks6, Ma36, Ma40, Mp9, Mp6, Ni3, Le3, Le2, LG20, Gb20, BI18, BI23. Information on acupuncturists: 7; Chinese physicians included participants, Chinese physicians trained and accredited at the Nanjing School of Traditional Chinese Medicine (Nanjing, People's Republic of China) administered acupuncture. All Chinese physicians had ≥ 5 years of training in Traditional Chinese Medicine, combined with 5 years of training in Western medicine, with additional practice of acupuncture of several years. Deqi achieved?: yes. Control group intervention: needling performed with same technique as for active treatment, but needling points were without relevance for BP lowering according to Traditional Chinese Medicine concepts. Pl1, dorsolateral forearm between traditional acupuncture points SI 7 and 8 on the small intestine meridian; Pl2, lateral thigh between acupuncture points Gb32 and Gb31 on the gall bladder meridian; and Pl3, lateral lower limb between acupuncture points Gb 34 and Gb35 on the gall bladder meridian. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: sitting position for auscultatory cuff BP measurements. BP measurements: ambulatory BP measurements were performed with an oscillometric device (Tracker NIBP, Reynolds Medical, Feucht, Germany); auscultatory cuff BP measurements with calibrated instruments. Time of each session: needles retained for 30 min. Number of treatment sessions: 22. Frequency of treatment sessions: during first 2 weeks: 5 sessions once a week, and in the following 4 weeks: 3 sessions weekly. Time of recruiting: January 2001 to May 2004. Adverse events: no local complications noted. Most frequent complaint about acupuncture therapy concerned the time demand for the treatment sessions. 2 participants terminated study early, complaining that acupuncture was too painful to continue. |
|
| Publication detail |
Language of publication: English. Commercial funding: no. Non‐commercial funding: yes (the Schöller‐Stiftung, Nürnberg, Germany). Publication status: peer review journal. |
|
| Notes | None of the physicians spoke German. 1 participant developed atrial fibrillation during treatment and was excluded because of necessity of anticoagulation. Other participants discontinuing study stated difficulty in keeping to time schedule, advised by family practitioner, or no reason for discontinuation. Participants taking antihypertensives continued their treatment without change in dosage or type of medication. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only described the block randomization used, but no description of method and detail of randomization. |
| Allocation concealment (selection bias) | Low risk | Closed envelope, without indicating assignment to participants. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Study described as single blind, Chinese physicians who included participants blinded. Very short description only, unclear how participants were informed about sham acupuncture. Low risk of detection bias as BP was by automatic 24‐hour monitoring. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Mentioned intention‐to‐treat analyses and reported number of dropouts and related reasons. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Low risk | There is no conflict of interest. |
Guo 2009.
| Methods |
Groups: A: acupuncture (electroacupuncture), B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: 3 weeks of baseline; 4 weeks' treatment; no follow‐up visit. |
|
| Participants |
Number of participants screenings/included/analyzed: not reported/60/60. Number of participants in each group: 30:30. Demographics: aged 32‐64 years in A; aged 29‐65 years in B; number of women 14:13. Number of participants who used antihypertensives: no detailed information. Course of disease: 0.5‐10 years in A; 1‐9 years in B. Setting: no information. |
|
| Interventions |
Acupuncture points: Baihui, Fengchi, Fenglong, Taichong, Taixi, Zusanli, Sanyinjiao. Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: enalapril maleate capsules (Yangzijiang Pharmaceutical Group, Jiangsu), 10 mg once daily, for 4 weeks. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: supine. BP measurements: no information. Time of each session: needles retained for 30 min, stimulating every 10 min. Number of treatment sessions: 28. Frequency of treatment sessions: once daily (for 4 weeks). Time of recruiting: June 2008 to June 2010. Adverse events: no information. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: peer review journal. |
|
| Notes | Antihypertensive withdrawal 2 weeks before treatment, BP in 3 different days as baseline BP in the third week before treatment, BP at 3 different days before ceasing treatment as last BP. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No mention of dropout and withdrawals. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Unclear risk | No description. |
Hao 2006.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 7 days' treatment; follow‐up visits: at 1 month after ceasing treatment. |
|
| Participants |
Number of participants screenings/included/analyzed: not reported/60/60. Number of participants in each group: 30:30. Demographics: mean age 64.57 years in A, mean age 64.77 years in B; number of women 15:15. Number of participants who used antihypertensives: no information. Course of disease: no information. Setting: inpatients and outpatients from Affiliated hospital of Guangzhou University of TCM. |
|
| Interventions |
Acupuncture points: Taichong (bilateral). Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: captopril, 12.5 mg, BID, for 7 days. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: no information. Time of each session: needles retained for 20 min, stimulated every 5‐10 min. Number of treatment sessions: 7. Frequency of treatment sessions: once daily, 7 days was a course. Time of recruiting: 2004 to December 2005. Adverse events: no reported liver and kidney function damage, pulmonary infection, or arrhythmia by acupuncture. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. NON‐Commercial funding: no. Publication status: Masters thesis. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only described simple randomization used, but no description of the method and detail of randomization. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants and investigators not blinded to acupuncture or pills. Detection bias reduced as BP was measured with automatic 24‐hour monitor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts and withdrawals mentioned. |
| Selective reporting (reporting bias) | Unclear risk | Relevant outcomes reported, but no outcome reported in follow‐up period. |
| Other bias | Unclear risk | No description. |
Kim 2012.
| Methods |
Groups: A: active acupuncture, B: sham acupuncture. Blinding: participants and observers. Dropouts/withdrawals: in the 2 weeks between randomization and initiation of treatment: 7/83 in A, 4/77 in B; during treatment course: 4/76 in A, 5/73 in B; first post‐treatment follow‐up visit: 0/72 in A, 0/68 in B; second follow‐up visit: 4/72 in A, 1/68 in B; third visit: 1/68 in A, 1/67 in B. Duration of intervention: no information of baseline; 8 weeks' treatment; 8 weeks' follow‐up visits: 1 participant was eliminated (drank alcohol several hours before follow‐up 24‐hour ambulatory BP measurement); 4 participants dropped out for personal reasons (distance, personal work, etc.). |
|
| Participants |
Number of participants screening/included/analyzed: 72/33/28. Number of participants in each group: 17:16. Demographics: mean age 52.08 years in A, 52.38 years in B; number of women 4:8. Number of participants who used antihypertensives: no previous use of antihypertensive medication. Course of disease: no information. Setting: outpatients at the Kyung Hee University Hospital at Gangdong, Korea. |
|
| Interventions |
Acupuncture points: ST36, PC6 (bilateral). Information on acupuncturists: 1 physician trained in traditional Korean medicine. Deqi achieved?: yes. Control group intervention: non‐acupuncture points (which were 1 cm lateral from ST36 and PC6) were needled superficially and bilaterally; Deqi was avoided. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: oscillometric device (Tonoport V, GE Medical System Information, Germany). Time of each session: needles retained for 20 min. Number of treatment sessions: 16 (for 8 weeks). Frequency of treatment sessions: twice a week. Time of recruiting: July 2009 to June 2010. Adverse events: no serious adverse events reported. Observed adverse effects were related to insertion of needles, such as: transient slight injection‐site pain and small bleeding. |
|
| Publication detail |
Language of publication: English. Commercial funding: no. Non‐commercial funding: yes (Korea Research Foundation Grant funded by the Korean Government (MOEHRD, Basic Research Promotion Fund)). Publication status: peer review journal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only described block randomization used (block size 4), but no description of method and detail of randomization. |
| Allocation concealment (selection bias) | Low risk | Inadequate method, although used consecutively numbered, opaque envelopes, but were opened to physician after participants were included in study; however, physician was not involved further. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Study described as double blind, participants and observers, but very short description, unclear how participants were informed about sham acupuncture. No detection bias as BP was by automatic 24‐hour monitoring. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 28/33 participants (5 in A, 0 in B) dropped out early or could not be analyzed. Detailed description, no intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Low risk | Thers is no conflict of interest. |
Li 2012a.
| Methods |
Groups: A: warm needling, B: acupuncture, C: medicine. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 2 weeks' treatment (total 14 treatments, with no elapsed days between consecutive treatment sessions), no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/60/60. Number of participants in each group: 20:20:20. Demographics: mean age 63.1 years in A, 61.7 years in B, 62.0 years in C; number of women 7:6:7. Number of participants who used antihypertensives: 3:5:4. Course of disease: 2.08‐8.33 years, mean 5.11 years in A; 1.67‐7.75 years, mean 4.35 years in B; 1.33‐8.67 years, mean 4.89 years in C. Setting: outpatients from Community Health Station, Beipei, Chongqin and the First Affiliated Hospital to TCM of Guangzhou. |
|
| Interventions |
Acupuncture points: in A: Siguan points (Hegu LI4 and Taichong LR3); in B: Siguan points (Hegu LI4 and Taichong LR3). Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: captopril 12.5 mg, BID, 14 days. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
|
|
| Study detail |
Position for measuring BP: sitting or decubitus. BP measurements: mercurial sphygmomanometer. Time of each session: A: until moxa stick moxibustion (length 2 cm) burning out; B: needles retained for 30 min and stimulated every 10 min. Number of treatment sessions: 14 (for 2 courses). Frequency of treatment sessions: every day, 7 days was a course. Time of recruiting: May 2011 and January 2012. Adverse events: no information. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: Masters thesis. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition. |
| Selective reporting (reporting bias) | Low risk | Relevant outcome reported. |
| Other bias | Unclear risk | No description. |
Liao 2006.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 14 days' treatment; no follow‐up visits. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/90/90. Number of participants in each group: 59:31. Demographics: mean age 56.5 years in A, mean age 55.6 years in B; number of women 28:14. Number of participants who used antihypertensives: no information. Course of disease: mean 9.20 years in A; mean 8.56 years in B. Setting: inpatients in integrative traditional Chinese and western medicine in the Fourth Central Hospital of Tianjin. |
|
| Interventions |
Acupuncture points: use "reducing south and reinforcing north" needling method, the points of "reducing south" were Taichong and Xingjian, Daling and Neiguan; the points of "reinforcing north" were Ququan, Taixi, Kunlun and Fuliu; assistant points were: Quchi, Fenglong. Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: captopril 12.5 mg TID + aspirin 75 mg once daily for 14 days. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: decubitus. BP measurements: no information. Time of each session: needles retained for 30 min, stimulated 3 times (immediately after inserting needle, middle of treatment, before withdrawing the needle), lasting 5 min every time. Number of treatment sessions: 28 (continuously for 2 weeks). Frequency of treatment sessions: twice a day, 7 days was a course. Time of recruiting: 2003‐2004. Adverse events: no information. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: peer review journal. |
|
| Notes | Average BP during 3 days before treatment and during 3 days after treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly drawn lots. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or exclusions from analysis. |
| Selective reporting (reporting bias) | Low risk | Relevant outcome reported. |
| Other bias | Unclear risk | No description. |
Liu 2011.
| Methods |
Groups: A: acupuncture + medicine, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 30 days' treatment; no follow‐up visits. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/106/106. Number of participants in each group: 53:53. Demographics: mean age 46.5 years in A, mean age 45.2 years in B; number of women 23:25. Number of participants who used antihypertensives: no information. Course of disease: mean 10.68 years in A; mean 11.16 years in B. Setting: People's Hospital in Tianzhu. |
|
| Interventions |
Acupuncture points: main points: Fengchi, Quchi, Zusanli, Sanyinjiao; supplementary points: deficiency of liver‐yin and kidney‐yin: Taixi, Taichong; the phlegm wet resistance: Fenglong. Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: captopril, 12.5 mg TID for 30 days. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: no information. Time of each session: needles retained for 20 min. Number of treatment sessions: 30 (lasting 2 courses). Frequency of treatment sessions: once daily, 15 days was a course. Time of recruiting: January 2002 to December 2009. Adverse events: no information. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: peer review journal: yes. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only described the randomization used, but no description of the method and detail of randomization. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators were not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition. |
| Selective reporting (reporting bias) | Low risk | Relevant outcome reported. |
| Other bias | Unclear risk | No description. |
Ma 2011.
| Methods |
Groups: A: acupuncture (electroacupuncture), B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 15‐day treatment; no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/80/80. Number of participants in each group: 40:40. Demographics: mean age 66.39 years in A, mean age 64.58 years in B; number of women 15:18. Number of participants who used antihypertensives: no information. Course of disease: mean 14.94 years in A; mean 15.4 years in B. Setting: outpatients and inpatients from rehabilitation department in Central hospital in Wuhan. |
|
| Interventions |
Acupuncture points: Quchi (LI11) bilateral (f:20 Hz, stimulation intensity:10‐20 mA). Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: nicardipine (Beijing Double‐crane Pharmaceutical), 20mg, TID, for 15 days. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: no information. Time of each session: needles retained for 10 min. Number of treatment sessions: 15. Frequency of treatment sessions: once a day (for 15 days). Time of recruiting: June 2008 to June 2010. Adverse events: no information. |
|
| Publication detail |
LANGUAGE OF PUBLICATION: Chinese. Commercial funding: no. Non‐commercial funding: yes (Health Bureau, in Wuhan). Publication status: peer review journal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition. |
| Selective reporting (reporting bias) | Low risk | Relevant outcome reported. |
| Other bias | Unclear risk | No description. |
Macklin 2006.
| Methods |
Groups: A: individualized acupuncture, B: standardized acupuncture , C: sham/control acupuncture . Blinding: participant (participants not informed that the control points were not traditional acupuncture points used to treat hypertension), a diagnosing acupuncturist masked to random assignments, treating acupuncturists masked to diagnosing. Dropouts/withdrawals: in treatment period (the first 6 weeks): 5/64 in A, 2/64 in B, 4/64 in C; in the follow‐up period, 1. with no follow‐up: 4/64 in A, 0/64 in B, 0/64 in C; 2. weeks 2‐10: 1/64 in A, 2/64 in B, 6/64 in C; 3. at week 10: 5/64 in A, 5/64 in B, 7/64 in C. Duration of intervention: 6 months' baseline; 6 weeks' treatment (total 12 treatments, with 3 or 4 elapsed days between consecutive treatment sessions, treatment period could extend to 8 weeks to complete), follow‐up every 2 weeks to week 10, then at months 4, 6, 9, and 12. |
|
| Participants |
Number of participants screening/included/analyzed: 424/192/188. Number of participants in each group: 64:64:64. Demographics: mean age 56.8 years in A, 55.9 years in B, 53.2 years C; 46% women; more minority ethnic participants in C by chance. Number of participants who used antihypertensives: 44:44:47. Course of disease: no information. Setting: outpatient clinics, at Massachusetts General Hospital in Boston, US. |
|
| Interventions |
Acupuncture points: in A: if flare‐up of liver fire: GB20, GB21, GB34, GB43, GV20, LI04, LI1, LR02, LR03, ST36, ST44, Tai Yang; liver yang rising with kidney yin deficiency: BL18, BL 23, GB20, GV20, HT07, KI03, LI04, LI11, LR03, SP06, Yin Tang; obstruction of phlegm and dampness: BL20, BL64, CV12, GB20, GV20, LI04, LI11, LR03a, PC06, SP06, ST08, ST 36, ST 40; Yin and yang deficiency: BL23, CV04, CV06, GB20, GV04, GV20, KI03, LI04, LI11, LR03, SP06, ST36; Qi and blood deficiency leading to liver yang rising: BL18, BL20, BL23, CV04, CV06, GB20, GV20, HT 07, KI03, LI04, LI11, LR03, SP06, ST36. the total number of a prescription points could not exceed 12, which might have consisted of 5 bilateral points and 1 point on the midline. Auricular points: liver, heart, Shen Men, Jiang Ya Gou, autonomic/sympathetic (at each treatment session). Corporeal acupuncture at 10‐12 points (median: 12, counting bilateral points twice) selected and stimulated as individually prescribed. Auricular acupuncture at the 2 most active points identified with a point detector at the start of each treatment session. In B: standardized acupuncture, corporeal acupuncture at 5 bilateral points with neutral stimulation: GB20, LI11, LR03, SP06, and ST36. Auricular acupuncture at Heart and Jiang Ya Gou. Points selected a priori by an expert panel. In C: sham/control acupuncture, corporeal acupuncture at 5 bilateral points that did not fall along any TCM meridian with no stimulation. Auricular acupuncture in Darwin's tubercle and the posterior ear lobe. All corporal and auricular acupuncture points in areas considered inactive according to TCM. Information on acupuncturists: number not reported; diagnosing acupuncturist had minimum 3 years' postgraduate experience and treating acupuncturist had minimum 1 year' postgraduate experience. In practice, participating diagnosing acupuncturists had 13‐22 years' experience, and all had received acupuncture training at colleges in the Peoples' Republic of China. Participating treating acupuncturists had 2‐8 years' experience. All study acupuncturists were licensed to practice in Massachusetts. (Training and certification for acupuncturists consisted of studying detailed training manuals and videotapes and attending an 8‐hour practical training session with a competency/certification exam.) Deqi achieved?: in B: used a neutral method of stimulation (obtaining 'De Qi' without any further stimulation). At 10, 20, and 30 min, acupuncturist touched each corporeal needle but did not stimulate the needles. Control group intervention: 5 control corporeal locations needled bilaterally (total of 10 points), in all corporeal locations, needles were inserted perpendicular to the skin without stimulation, and 2 auricular locations needled unilaterally at each visit, inserted perpendicular to the skin without stimulation. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: manual mercury sphygmomanometers by trained staff. Time of each session: in A: if prescription included only anterior corporeal points, participant was needled in supine position. Needles were retained for 30 min and stimulated according to the prescription at the time of initial insertion, and again at 10 and 20 min. If both anterior and posterior points were prescribed, anterior points were needled first (supine position) and retained for 20 min with the prescribed needle stimulation at the time of initial insertion and at 10 min. Needles were then removed and participant placed in prone position. Posterior points were then needled and retained for 10 min, with the prescribed needle stimulation at the time of insertion. In B: needled in the supine position. In C: supine corporeal points were touched by the acupuncturist at 10 min and withdrawn at 20 min, then turned over to lie prone and the remainder of the corporeal needles inserted. After an additional 10 min (30 min total time), the needles were touched and removed without stimulation. Auricular acupuncture needles were inserted prior to corporeal needling, without stimulation and were retained without stimulation during the 30‐min treatment period. Number of treatment sessions: 12. Frequency of treatment sessions: twice a week. Time of recruiting: March 2001 and July 2002. Adverse events: 3 study related serious adverse events occurred over 165 participant‐years of follow‐up: 2 participants experienced hypertensive urgencies, in B and 1 participant experienced congestive heart failure in C. No deaths occurred. |
|
| Publication detail |
Language of publication: English. Commercial funding: no. Non‐commercial funding: yes. Publication status: peer review journal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use the NERI's randomization software (used centralized computer). |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes, inclusion, diagnosing, and treating by different acupuncturist. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Acupuncturist masked to random assignments; participants not informed that the control points were not traditional acupuncture points. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Mentioned intention‐to‐treat analyses and reported the number of dropouts and related reasons. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes described in publication and additional data provided on request. |
| Other bias | Low risk | There is no conflict of interest. |
Shen 2010a.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 1 day' treatment; no follow‐up visits. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/60/60. Number of participants in each group: 30:30. Demographics: mean age 50.6 years in A, mean age 51.13 years in B; number of women 13:14. Number of participants who used antihypertensives: no information. Course of disease: mean 4.73 years in A; mean 4.67 years in B. Setting: inpatients from Department of Acupuncture and Moxibustion and emergency department in The First Affiliated Hospital of Tianjin Medical University. |
|
| Interventions |
Acupuncture points: Renyin, Hegu, Taichong, Quchi, Zusanli. Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: nifedipine, 10 mg daily, immediately after patient hospitalization. |
|
| Outcomes |
Primary outcome:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: no information. Time of each session: needles retained for 30 min. Number of treatment sessions: 1 (once). Frequency of treatment sessions: once a day. Time of recruiting: April to June 2009. Adverse events: no information. |
|
| Publication detail |
LANGUAGE OF PUBLICATION: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: peer review journal.. |
|
| Notes | Only 1 treatment. BP measured at 3, 15, 30, 60 min, and 2, 4, and 6 hours. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant dropout and withdraw. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes presented. |
| Other bias | Unclear risk | No description. |
Tian 2007.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 30 days' treatment; no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/60/60. Number of participants in each group: 30:30. Demographics: mean age 59.17 years in A, mean age 59 years in B; number of women 13:14. Number of participants who used antihypertensives: no information. Course of disease: mean 7.67 years in A; mean 8.03 years in B. Setting: inpatients from internal medicine in the People's Hospital Zhuzhou. |
|
| Interventions |
Acupuncture points: Quchi, Taichong, Fengchi (bilateral). Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: levamlodipine besylate pills, 2.5 mg, once daily, at 7 a.m. for 30 days. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: no information. Time of each session: needles retained for 30 min, stimulated every 10 min. Number of treatment sessions: 30. Frequency of treatment sessions: once daily, 30 days was a course (at 9 a.m.). Time of recruiting: January 2006 to January 2007. Adverse events: 2/30 headache, nausea and 2/30 heart palpitations in B. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: Masters thesis. |
|
| Notes | BP measured at 7 a.m. and 5 p.m. by nurse. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer program (DPS8.01 Chinese Statistical software). |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant dropout and withdraw. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes presented. |
| Other bias | Unclear risk | No description. |
Wang 2012a.
| Methods |
Groups: A: acupuncture (electroacupuncture), B: medicine control, C: acupuncture + medicine control. Blinding: assessor and statistician. Dropouts/withdrawals: in treatment: 2/47 unfinished treatment, 3/45 incomplete data, 2/42 non‐compliant participants; B: 4/45 adverse drug reaction, 1/41 non‐compliant participant; C: 2/50 adverse drug reaction. Duration of intervention: no information of baseline; 28 days' treatment: A: 2/47 unfinished treatment, 3/45 incomplete data, 2/42 non‐compliant participants; B: 4/45 adverse drug reaction, 1/41 non‐compliant participant; C: 2/50 adverse drug reaction; no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: 142/128/128. Number of participants in each group: 47:45:50 (at end of treatment: 40:40:48). Demographics: mean age 66.39 years in A, mean age 64.58 years in B, mean age 64.29 years in C; number of women 15:18:20. Number of participants who used antihypertensives: no information. Course of disease: mean 14.94 years in A; mean 15.39 years in B; mean 15.03 years. Setting: outpatients and inpatients from rehabilitation department in Hubei University of Chinese Medicine. |
|
| Interventions |
Acupuncture points: Quchi (bilateral); and non‐acupoint: ligature between Quchi and Yangxi, 5 Cun below Quchi (f:20 Hz). Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: B and C: nicardipine (Beijing ShuangHe Pharmaceutical Co. Ltd.), 20 mg, TID, for 28 days. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: supine. BP measurements: mercurial sphygmomanometer (XJ11D). Time of each session: needles retained for 10 min. Number of treatment sessions: 28 (continuously for 4 courses). Frequency of treatment sessions: once daily, 7 days was a course. Time of recruiting: March 2010 to February 2012. Adverse events: B: 4/40: foot edema, flush, rash, flustered, headache; C: 2/40: foot edema, flush, rash. |
|
| Publication detail |
Language of publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: Masters thesis. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization by Excel software. |
| Allocation concealment (selection bias) | Low risk | Opaque envelop. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Assessor and statistician masked to random assignments, but acupuncturists and participants were not masked. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 14/142 participants dropped out early or could not be analyzed during treatment. No related reason description, no intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes presented. |
| Other bias | Unclear risk | No description. |
Wu 2003.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 30 days' treatment; no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/80/80. Number of participants in each group: 40:40. Demographics: mean age 48.55 years in A, 47.85 years in B; number of women 17:19. Number of participants who used antihypertensives: no information. Course of disease: 6 months to 10 years, mean 5.15 years in A; 6 months to 10 years; mean 4.95 years in C. Setting: no information. |
|
| Interventions |
Acupuncture points: acupuncture at Hegu (LI4), Taichong (LR3) and warming acupuncture‐moxibustion at Baihui (GV20). Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: captopril (Bristol‐Myers Squibb, Shanghai), 25 mg TID, for 30 days. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: no information. Time of each session: needles retained for 20 min, stimulated every 5 min and lasting 30 seconds. Number of treatment sessions: 30 (for 30 days). Frequency of treatment sessions: once daily. Time of recruiting: January 2000 to December 2002. Adverse events: no information. |
|
| Publication detail | Language or publication: Chinese. Commercial funding: no Non‐commercial funding: yes (Hunan Technology Gallery). Publication status: peer review journal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of random digits. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or withdrawals from analysis. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes presented. |
| Other bias | Unclear risk | No description. |
Wu 2011.
| Methods |
Groups: A: acupuncture, B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 22 days' treatment; no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/120/120. Number of participants in each group: 60:60. Demographics: mean age 54.75 years in A, mean age 51.72 years in B; number of women 26:24. Number of participants who used antihypertensives: no information. Course of disease: mean 6.78 years in A; mean 7.01 years in B. Setting: outpatients from The Second Affiliated Hospital of Zhengzhou University. |
|
| Interventions |
Acupuncture points: Zhigou, Yanglingquan, Taiyang, Taichong (bilateral). Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: metoprolol, 100 mg, QD, for 20 days. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
|
|
| Study detail |
Position for measuring BP: sitting position and ambulatory BP monitoring. BP measurements: mercury column sphygmomanometer sleeve belt. Time of each session: needles retained for 30 min, stimulated every 10 min, lasting 1 min. Number of treatment sessions: 20 (continuously for 2 courses). Frequency of treatment sessions: once daily, 10 days was a course, 2‐day interval between 2 courses. Time of recruiting: no information. Adverse events: no information. |
|
| Publication detail |
Language or publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: peer review journal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or withdrawals from analysis. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes presented. |
| Other bias | Unclear risk | No description. |
Xie 2004.
| Methods |
Groups: A: Lingguibafa acupuncture, B: point selection by pattern identification, C: medicine. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 3 months' treatment; no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/90/90. Number of participants in each group: 30:30:30. Demographics: aged 38‐71 years, mean age 56.77 years; number of women 47/90. Number of participants who used antihypertensives: no information. Course of disease: no information. Setting: inpatients from First Affiliated Hospital to Guangxi University of TCM. |
|
| Interventions |
Acupuncture points: Quchi, Zusanli; Fengchi, Taichong; headache: Yintang, Taiyang; insomnia: Anmian, Shenmen; palpitation: Ximen, Neiguan (bilateral). Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: nitrendipine, 10 mg, BID. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: no information. BP measurements: desktop water silver column sphygmomanometer. Time of each session: needles retained for 30 min, with needle manipulation once during treatment. Number of treatment sessions: 1. Frequency of treatment sessions: no information. Time of recruiting: no information. Adverse events: no information. |
|
| Publication detail |
Language or publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: peer review journal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or withdrawals. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes presented. |
| Other bias | Unclear risk | No description. |
Yang 2010a.
| Methods |
Groups: A: acupuncture (electroacupuncture), B: medicine control. Blinding: no information. Dropouts/withdrawals: 0. Duration of intervention: no information of baseline; 14 days' treatment; no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/60/60. Number of participants in each group: 30:30. Demographics: aged 28‐44 years, mean age 40.4 years in A: 30‐45 years, mean age 41.7 years in B; number of women 13:10. Number of participants who used antihypertensives: no information. Course of disease: 0.6‐9.3 years, mean 5.2 years in A; 0.5‐8.6, mean 4.2 years in B. Setting: outpatients from affiliated hospital of Shandong University of TCM. |
|
| Interventions |
Acupuncture points: Quchi (LI11) and Taichong (LR3) (f:2 Hz/100 Hz, stimulation intensity: 10‐20 mA). Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: captopril (Bristol‐Myers Squibb, Shanghai),12.5 mg/day, TID, for 14 days. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: no information (dynamic monitoring BP). BP measurements: non‐invasive diagnosis of portable dynamic monitoring BP (type of ambulatory BP monitoring, US). Time of each session: needles retained for 30 min. Number of treatment sessions: 14. Frequency of treatment sessions: once daily (for 14 days). Time of recruiting: January 2007 to December 2008. Adverse events: no information. |
|
| Publication detail |
Language or publication: Chinese. Commercial funding: no. Non‐commercial funding: yes (Development of Science and Technology Plan project of TCM 20052006, in Shandong province). Publication status: peer review journal. |
|
| Notes | BP also measured once before 3 days' and after 3 days' acupuncture treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | SAS software Proc plan to randomization. |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants and investigators not blinded to acupuncture or pills. Detection bias was reduced as BP was measured with automatic 24‐hour monitor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or exclusions from analysis. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes presented. |
| Other bias | Unclear risk | No description. |
Yin 2007.
| Methods |
Groups: A: active acupuncture, B: sham acupuncture (all participants were antihypertensive). Blinding: assessor and participants (a single assessor made the measurements including BP, psychologic factors, and lifestyle). Dropouts/withdrawals: in treatment: after 4 weeks: 3/21 in A, 1/20 in B had dropped for job‐related reasons; 1/19 in A, 1/19 in B for distance to hospital; 0/18 to A, 1/18 to B for severe gonalgia; 1/18 in A, 1/17 in B for uncertainty about effectiveness of treatment; 0/17 in A, 1/16 in B for personal reasons; after 8 weeks: 1/17 in A, 1/15 in B dropped out for job‐related reasons. Duration of intervention: 8 weeks. After 4 weeks: 3/21 in A, 1/20 in B dropped for job‐related reasons; 1/19 in A, 1/19 in B discontinued for far distance to hospital; 0/18 in A, 1/18 in B for severe gonalgia; 1/18 in A, 1/17 in B for uncertainty about effectiveness of treatment, 0/17 in A, 1/16 in B for personal reasons; after 8 weeks: 1/17 in A, 1/15 in B dropped out for job‐related reasons; no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/41/30. Number of participants in each group: 21:20. Demographics: mean age 52 years in A, mean age 54 years in B; number of women 11:10. Number of participants who used antihypertensives: all. Course of disease: 3.4 years in A, 4.2 years in B. Setting: institutional review board at Kyung Hee University Hospital of Oriental Medicine, Seoul, Korea. |
|
| Interventions |
Acupuncture points: acupuncture formula based on and modified from the Saam acupuncture theory of Korean acupuncture. The 4 formulas were: 1. ST36, LI11 and BL25 for toning the large intestine (L1) meridian energy; 2. SP3, LU9, and BL13 for the lung (LU); 3. K17, K12, and CV4 for the kidney (K1); 4. LI1, GV14, and GB20 for the bladder (BL). L1, LU, KI, or BL energy is typically considered deficient when a body is in a state of dampness, dryness, cold or hot, respectively. Optionally, PC6 and HT7 were added when a psychologic factor was considered of importance. Information on acupuncturists: no information. Deqi achieved?: yes. Control group intervention: using Park's sham needle (a new non‐penetrating sham acupuncture device), needle did not penetrate skin, but was twisted slowly to imitate real acupuncture. After the Deqi sensation detected, the needle was withdrawn immediately. All participants were encouraged to follow the instructions for 10 min' deep, slow breathing exercise and to walk for 30 min a day at an easy pace during the 8‐week period. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: supine. BP measurements: automated sphygmomanometer (model T4, Omron, Japan). Time of each session: needles retained for 30 min, stimulated every 5 min. Number of treatment sessions: 17. Frequency of treatment sessions: once daily, 3‐ to 4‐day interval between sessions for 8 weeks. Time of recruiting: 1 January to 31 May 2004. Adverse events: spot‐bleeding (8 in A). |
|
| Publication detail |
Language or publication: English. Commercial funding: no. Non‐commercial funding: yes (supported by the SRC program of KOSEF, Korea). Publication status: peer review journal. |
|
| Notes | BP measured on right upper arm, mean of 3 readings with a 5‐min interval. BP was taken 6 times for the baseline measurement and 3 times for the outcome measurement. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerized random allocation. |
| Allocation concealment (selection bias) | Unclear risk | No detail mentioned. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding unlikely to have been achieved as sham procedure did not involve needle penetration. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Reported number of dropouts and related reasons, but no intention‐to‐treat. |
| Selective reporting (reporting bias) | Low risk | Relevant outcome reported. |
| Other bias | Unclear risk | No description. |
Zhang 2012a.
| Methods |
Groups: A: acupuncture + psychotherapy, B: acupuncture, C: medicine. Blinding: participants, Chinese physician who included participants. Dropouts/withdrawals: not reported. Duration of intervention: no information of baseline; 8 weeks' treatment; no follow‐up. |
|
| Participants |
Number of participants screening/included/analyzed: not reported/42/42. Number of participants in each group: 14:14:14. Demographics: aged 42‐60 years for all participants; number of women 19. Number of participants who used antihypertensives: no information. Course of disease: no information. Setting: no information. |
|
| Interventions |
Acupuncture points: B: Quchi, Taichong, Zusanli, Sanyinjiao. Information on acupuncturists: no information. Deqi achieved?: no information. Control group intervention: A: acupuncture + psychotherapy: 1. supportive psychotherapy, 30‐min sessions, twice a week, 8 weeks was a course; 2. cognitive therapy, 30‐min sessions, twice a week, 8 weeks was a course; 3. relaxation therapy, 30 min sessions, twice or three times a week, 8 weeks was a course; C: captopril (Bristol‐Myers Squibb, Shanghai), 25 mg, TID. |
|
| Outcomes |
Primary outcome:
Secondary outcome:
|
|
| Study detail |
Position for measuring BP: sitting. BP measurements: auscultatory cuff BP measurements. Time of each session: needles retained for 30 min, stimulated every 15 min. Number of treatment sessions: 24 (for 8 weeks). Frequency of treatment sessions: 3 times a week. Time of recruiting: no information. Adverse events: no information. |
|
| Publication detail |
Language or publication: Chinese. Commercial funding: no. Non‐commercial funding: no. Publication status: peer review journal. |
|
| Notes | No detailed information of demographics. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Unclear risk | No description. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and investigators not blinded to acupuncture or pills. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or withdrawals. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Other bias | Unclear risk | No description. |
BID: twice a day; BP: blood pressure; DBP: diastolic blood pressure; min: minute; NPY: neuropeptide Y; NT: neurotensin; QD: once a day; SAS: Zung self‐rating anxiety scale; SBP: systolic blood pressure; SDS: Zung self‐rating depression scale; TCM: Traditional Chinese Medicine; TID: three times a day.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| An 2001 | Methods: incorrect randomization method. |
| Cao 2007 | Participants: only included cervical hypertension, but no description of primary hypertension. |
| Chen 1990 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Chen 1995 | Method: not randomized. |
| Chen 2006b | Intervention: abdominal acupuncture therapy. |
| Chen 2009 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Chen 2010b | Outcome with no indication of blood pressure change. |
| Chen 2011 | Outcome with no indication of blood pressure change. |
| Dong 2012 | Outcomes: no relevant outcomes reported. |
| Fang 1998 | Case observation. |
| Fang 2012 | Intervention: acupuncture vs acupuncture. |
| Feng 2003 | Outcome with no indication of blood pressure change. |
| Gao 2009 | Included the comparison of a complementary and alternative intervention, which is lifestyle training. Thus, study was excluded. |
| Hao 2009 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| He 2002 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| He 2012 | Participants: included elderly participants with systolic hypertension. |
| Hong 2009 | Cross‐over trial. |
| Hu 2010 | Outcome with no indication of blood pressure change. |
| Huang 1991 | Intervention: auricular acupuncture at Erxin. |
| Huang 2007a | Outcome with no indication of blood pressure change. |
| Huang 2007b | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Jiang 2003 | Intervention: magnetic needle acupuncture + captopril. |
| Jin 2010 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Jung 2010 | Cross‐over study. |
| Li 2008a | Outcome with no indication of blood pressure change. |
| Li 2008b | Participants: only included cervical hypertension, but no description of primary hypertension. |
| Li 2012b | Outcome with no indication of blood pressure change. |
| Liu 2012 | Intervention: acupuncture vs acupuncture. |
| Luo 2011 | Intervention: acupuncture + bloodletting on ear‐tip. |
| Mou 1991 | Intervention: acupuncture vs acupuncture. |
| Mu 2009 | Method: not randomized |
| Ning 2012 | Participants: only included cervical hypertension, but no description of primary hypertension. |
| Qian 1996 | Participants: only included cervical hypertension, but no description of primary hypertension. |
| Qu 2009 | Intervention: auricular acupuncture and wrist‐ankle acupuncture analgesia. |
| Shen 2010b | Intervention: acupuncture vs acupuncture. |
| Song 2003 | Intervention: acupuncture + Chinese herb + western medicine vs Chinese herb. |
| Song 2006 | Intervention: acupuncture vs acupuncture. |
| Sui 2012 | Intervention: acupuncture vs acupuncture. |
| Sun 2009 | Participants: only included cervical hypertension, but no description of primary hypertension. |
| Tang 2003 | Method: incorrect randomization method. |
| Tian 2012 | Cross‐over trial. |
| Wang 1994 | Intervention: acupuncture vs acupuncture. |
| Wang 2003 | Outcome with no indication of blood pressure change. |
| Wang 2006 | Intervention: acupuncture + Chinese herb vs western medicine. |
| Wang 2012b | Intervention: acupuncture + Chinese herb vs western medicine. |
| Wei 2010 | Outcome with no indication of blood pressure change. |
| Wei 2012 | Intervention: acupuncture vs acupuncture. |
| Wu 2004a | Outcomes: only laboratory parameters. |
| Wu 2004b | Wrong randomization method. |
| Wu 2005 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Xia 2006 | Change in diastolic blood pressure. |
| Xia 2012 | Intervention: acupuncture vs acupuncture. |
| Xie 2000 | Methods: not a randomized trial. |
| Xie 2014 | Included the comparison of a complementary and alternative intervention, which is lifestyle training. Thus, this study was excluded. |
| Xing 2005 | Intervention: acupuncture vs acupuncture. |
| Xing 2011 | Intervention: acupuncture vs acupuncture. |
| Yang 2002a | Methods: not randomized trial. |
| Yang 2002b | Methods: not randomized trial. |
| Yang 2010b | Intervention: bloodletting at the Erjian‐point. |
| Yao 1994 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Yi 1988 | Methods: not randomized trial. |
| Yin 1994 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Yin 2002 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Yu 2007 | Outcome with no indication of blood pressure change. |
| Zhang 1999 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Zhang 2001 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Zhang 2002 | inappropriate control design (compound medicine made of ≥ 2 ingredients). |
| Zhang 2004 | inappropriate control design (compound medicine made of ≥ 2 ingredients). |
| Zhang 2005 | Methods: incorrect randomization method. |
| Zhang 2008 | Intervention: laser acupoint treatment. |
| Zhang 2009 | Intervention: acupuncture vs acupuncture. |
| Zhang 2011 | Intervention: catgut embedding in acupoint. |
| Zhang 2012b | Intervention: acupuncture + Chinese herb vs western medicine. |
| Zhao 2003 | Included the comparison of a complementary and alternative intervention, which is lifestyle training. Thus, this study was excluded. |
| Zhao 2011 | Case observation. |
| Zhao 2012 | Intervention: acupuncture vs acupuncture. |
| Zheng 2012 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Zhou 1997 | Intervention: acupuncture vs acupuncture. |
| Zhou 2012 | Participants: no detail description of participant criteria, not only included primary hypertension. |
| Zhu 2006 | Participants: no detail description of participant criteria, not only included primary hypertension. |
Characteristics of ongoing studies [ordered by study ID]
Liang.
| Trial name or title | Effect of Acupuncture on Patients with Mild Hypertension (EAPMH). |
| Methods | Large scale, open label, multicenter, randomized controlled clinical trial. |
| Participants | Adults with mild essential hypertension; estimated enrolment: 428. |
| Interventions | 2 acupuncture arms, 1 sham acupuncture arm, and 1 waiting list arm. |
| Outcomes | Primary outcome: mean systolic and average diastolic blood pressure by 24‐hour ambulatory blood pressure monitoring. Secondary outcomes: mean systolic and diastolic blood pressure during the daytime and night‐time; changes in health‐related quality of life; expectation of treatment; adverse events. |
| Starting date | July 2012. |
| Contact information | Liang FR, Chengdu University of Traditional Chinese Medicine. |
| Notes |
Differences between protocol and review
We made the following changes from the protocol.
Used GRADEPro in the 'Summary the findings' tables to grade the quality of evidence.
Removed the item 'change in heart rate,' from the primary outcomes of the protocol due to its lack of clinical significance.
Discarded a secondary outcome, 'relative risk of number of patients withdrawn due to adverse events' from the protocol as most trials did not report this parameter.
Removed one item 'the control group (lifestyle change, relaxation, etc.)' from the inclusion criteria as the effect of these interventions on blood pressure is not well established.
Excluded studies that only compared different forms or methods of acupuncture (e.g. transcutaneous electrical nerve stimulation) or compared acupuncture with any complementary and alternative therapies for which the efficacy is not yet established (e.g. Chinese herbs).
Contributions of authors
JY, JC and MY: contributed equally to this review.
FL and JY: conceived the review.
FL, JY, JC and MY: drafted the review.
FL, JY, JC, MY and JW: contributed to the interpretation of the data in the review.
MY and JW: revised the manuscript.
YR, SY and JC: searched the references and helped assess eligibility.
GJL and LY: analyzed the data.
JY and FL are responsible for updating the systematic review.
Sources of support
Internal sources
-
Chengdu University of Traditional Chinese Medicine, China.
infrastructure support
External sources
-
National Basic Research Program, China.
973 program, No. 2012CB518501
-
National Natural Science Foundation of China, China.
No.81303060, 81273854
Declarations of interest
JY: nothing to declare.
JC: nothing to declare.
MY: nothing to declare.
SY: nothing to declare.
LY: nothing to declare.
GJL: nothing to declare.
YR: nothing to declare.
JW: nothing to declare.
FL: nothing to declare.
New
References
References to studies included in this review
Chen 2000 {published data only}
- Chen YF, Qian H, Li L, Mao M, Qian WH, He XQ, et al. The study about impact of acupuncture to hypertension patients plasma endothelin angiotensin Ⅱ. Chinese Acupuncture and Moxibustion 2000;20(11):691‐3. [Google Scholar]
Chen 2006a {published data only}
- Chen BG, Qian CY, Zhang JN, Miao HR. Clinical observations on the hypotensive effect of point Fengchi acupuncture on hypertension. Shanghai Journal of Acupuncture and Moxibustion 2006;25(3):15‐6. [Google Scholar]
- Wang LY, Chen BG. Clinical study on therapeutic effect and adjustment to plasma ET and serum TNF‐α in the patient of essential hypertension with acupuncture at Fengchi point. Journal of Hubei College of TCM 2006;8(1):8‐10. [Google Scholar]
Chen 2010a {published data only}
- Chen NY, Zhou Y, Dong Q, Zhou CX. Observation on Therapeutic Effect of Acupuncture in the Treatment of German Hypertension Patients. Acupuncture Research 2010;35(6):462‐6. [PubMed] [Google Scholar]
Dan 1998 {published data only}
- Dan Y. The clinical observation of dynamic blood pressure monitoring and evaluation of the acupuncture treatment of hypertension. Chinese Journal of Integrated Traditional and Western Medicine 1998;18(1):26‐7. [PubMed] [Google Scholar]
Flachskampf 2007 {published data only}
- Flachskampf FA, Gallasch J, Gefeller O, Gan J, Mao J, Pfahlberg AB, et. Randomized trial of acupuncture to lower blood pressure. Circulation 2007;115:3121‐9. [DOI] [PubMed] [Google Scholar]
Guo 2009 {published data only}
- Guo YH, Teng XY, Zhang CF, Dai XH, Li D, Wang YX. The influence the level of insulin resistance and TNF‐α in acupuncture for primary hypertension. Acta Chinese Medicine and Pharmacology 2009;37(5):76‐8. [Google Scholar]
Hao 2006 {published data only}
- Hao PY, Wen WX. Acupuncturing Taichong to Treat Hypertension Patients with Syndrome of Hyperactivity of Liver Fire [Masters thesis]. Guangzhou (China): Guangzhou University of Traditional Chinese Medicine, 2006. [Google Scholar]
Kim 2012 {published data only}
- Kim HM, Cho SY, Park SU, Sohn IS, Jung WS, Moon SK, et al. Can acupuncture affect the circadian rhythm of blood pressure? A randomized, double‐blind, controlled trial. Journal of Alternative and Complementary Medicine 2012;18(10):918‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2012a {published data only}
- Li LC, Chai TQ. Clinical Study on Hypertension of Hyperactivity of Yang due to Yin Deficiency Pattern Treated with Warm Needling Siguan Points [Masters thesis]. Guangzhou, China: Guangzhou University of Chinese Medicine, 2012. [Google Scholar]
Liao 2006 {published data only}
- Liao H, Li DP, Chen Q, Yi L. Observation on therapeutic effect of "reducing south and reinforcing north" needling method on hypertension of type of yang‐hyperactivity due to yin‐deficiency. Chinese Acupuncture and Moxibustion 2006;26(2):91‐3. [PubMed] [Google Scholar]
Liu 2011 {published data only}
- Liu CJ, He XF, Yuan LX. Acupuncture combined with medicine for 106 cases hypertension. Chinese and Foreign Medical Research 2011;9(14):137‐8. [Google Scholar]
Ma 2011 {published data only}
- Ma CY, Wang YF, Wan WJ, Xiong XA, Wang Y, Wang L, et al. The influence of density plasma NPY and NT acupuncture Quchi for primary hypertension. Journal of New Chinese Medicine 2011;43(4):89‐91. [Google Scholar]
Macklin 2006 {published data only}
- Macklin EA, Wayne PM, Kalish LA, Valaskatgis P, Thompson J, Pian‐Smith MCM, et al. Stop hypertension with the Acupuncture Research Program (SHARP): results of a randomized, controlled clinical trial. Hypertension 2006;48:838‐45. [DOI] [PubMed] [Google Scholar]
Shen 2010a {published data only}
- Shen PF, Shi XM. Acupuncture for subacute essential hypertension in 30 cases. Journal of Traditional Chinese Medicine 2010;51(1):57‐8. [Google Scholar]
Tian 2007 {published data only}
- Tian L, Chen JJ. Clinical Observe on Acupuncture in Treating Hypertension of Liver‐YANG with Intention [Masters thesis]. Changsha (China): Hunan University of Traditional Chinese Medicine, 2007. [Google Scholar]
Wang 2012a {published data only}
- Wang YF, Ma CY. Clinical Research on the Therapeutic Effect of Electroacupuncture at Quchi(LIll) on Blood Plasma NPY and NT of Essential Hypertension Patients [Masters thesis]. Wuhan City (China): Hubei University of Chinese Medicine, 2012. [Google Scholar]
Wu 2003 {published data only}
- Wu QM, Feng GX. The correlation between hypotensive effect and plasma Ang II after warm Acu‐Moxi on Kaisiguan and Baihui points. Journal of New Chinese Medicine 2003;35(12):45‐8. [Google Scholar]
Wu 2011 {published data only}
- Wu YR, LI HX. The clinical observation of acupuncture for hypertension. China Medical Herald 2011;8(19):102‐3. [Google Scholar]
Xie 2004 {published data only}
- Xie GG, Zheng Z, Lu XQ, Zhao CJ. Immediate effect observation of Ninguibafa for essential hypertension. Journal of Clinical Acupuncture Medicine 2004;20(7):36‐40. [Google Scholar]
Yang 2010a {published data only}
- Liu JY, Yang DH. The Intervention Study of Electro‐acupuncture in Quchi, Taichongon Blood Pressure Variability of Patients with Essential Hypertension [Masters thesis]. Jinan City (China): Shandong University of Traditional Chinese Medicine, 2009. [Google Scholar]
- Yang DH. Effect of electroacupuncture at Qūchí (LI 11) andTàichōng (LR 3) on blood pressure variability in young patients with hypertension. World Journal of Acupuncture‐Moxibustion 2011;21(1):8‐12. [PubMed] [Google Scholar]
- Yang DH. Effect of electroacupuncture on Quchi (LI 11) and Taichong (LR 3) on blood pressure variability in young patients with hypertension. Chinese Acupuncture and Moxibustion 2010;30(7):547‐50. [PubMed] [Google Scholar]
Yin 2007 {published data only}
- Yin CS, Seo BK, Park HJ, Cho M, Jung WS, Choue R, et al. Acupuncture, a promising adjunctive therapy for essential hypertension: a double‐blind, randomised, controlled trial. Neurological Research 2007;29:S98‐103. [DOI] [PubMed] [Google Scholar]
Zhang 2012a {published data only}
- Zhang Y, Liu XG, Dong XY, Liu Y, Xu JY. Clinical research of acupuncture adding psychotherapy in treating essential hypertension. Journal of Chengdu University of Traditional Chinese Medicine 2012;35(4):16‐8. [Google Scholar]
References to studies excluded from this review
An 2001 {published data only}
- An CF, Yu CJ. Effect of acupuncture plus exercise therapy for hypertension. Modern Rehabilitation 2001;5(5):135. [Google Scholar]
Cao 2007 {published data only}
- Cao L, Hou GY, Fan WS. Analysis on the therapeutic effect of acupuncture of Jiaji (EX‐B 2) for treatment of cervical hypertension. Acupuncture Research 2007;32(3):195‐8. [PubMed] [Google Scholar]
Chen 1990 {published data only}
- Chen J, Zhou YP. Influence of nail fold microcirculation in acupuncture for hypertension. Journal of Anhui TCM College 1990;9(3):49‐51. [Google Scholar]
Chen 1995 {published data only}
- Chen J, Zhou YP. Influence hemorheology of acupuncture for hypertension. Journal of Clinical Acupuncture and Moxibustion 1995;11(8):28. [Google Scholar]
Chen 2006b {published data only}
- Chen J, Zou X. Clinical Observation of Abdominal Acupuncture Therapy for Hypertension [Masters thesis]. Guangzhou (China): Guangzhou University of TCM, 2006. [Google Scholar]
Chen 2009 {published data only}
- Chen ZB, Xu NG. Research of the Effect of Acupuncture 'SiGuan points' for the Earlier Period Hypertension Patients with the Hyperactivity of Liver‐yang Syndrome [Masters thesis]. Guangzhou (China): Guangzhou University of TCM, 2009. [Google Scholar]
Chen 2010b {published data only}
- Chen J, Li J, Wang ZR. Clinical study on therapeutic effect of acupuncture and its adjustment for E‐selectin, iNOS and eNOS in patients of essential hypertension. World Science and Technology/Modernization of Traditional Chinese Medicine and Materia Medica 2010;12(3):352‐4. [Google Scholar]
- Chen J, Li J, Wang ZR. Therapeutic effect on essential hypertension treated with combined therapy of acupuncture and medication. Chinese Acupuncture and Moxibustion 2010;30(11):896‐8. [PubMed] [Google Scholar]
Chen 2011 {published data only}
- Chen Q, Chen BG. Clinical observation on acupuncture at Quchi (LI 11) and Fengchi (GB 20) for hypertension. Shanghai Journal of Acu‐mox 2011;30(10):659‐60. [Google Scholar]
Dong 2012 {published data only}
- Dong YS, Xing SL. Effect of acupuncture needle‐retention duration at Baihui (GV 20) and Sishencong (EX‐HN 1) on blood pressure in hypertension patients. Acupuncture Research 2012;37(3):233‐6. [PubMed] [Google Scholar]
Fang 1998 {published data only}
- Fang CL. Acupuncture treatment of 21 cases of hypertension. Acupuncture Research 1998;23(3):202. [Google Scholar]
Fang 2012 {published data only}
- Fang LJ, Wang R. The Effects of Acupuncture Lingtai and Shendao Points on Heart Rate Variability in Patients with Essential Hypertension [Masters thesis]. Jinan City (China): Shandong University of TCM, 2012. [Google Scholar]
Feng 2003 {published data only}
- Feng GX, Wu QM. Clinical study on treatment of essential hypertension with acupuncture at "Siguan" points plus warming acupuncture‐moxibustion at Baihui (GV20) point. Chinese Acupuncture and Moxibustion 2003;23(4):193‐5. [Google Scholar]
Gao 2009 {published data only}
- Gao XA, Jin CN, Zhang TS, An YL. Clinic observation on essential hypertension by acupuncture combined with behavior training. Chinese Archives of Traditional Chinese Medicine 2009;27(2):325‐6. [Google Scholar]
Hao 2009 {published data only}
- Hao DF, Wang ZH. Comparison Trial Massage and Acupuncture for Liver Yang Syndrome Type Hypertension [Masters thesis]. Changchun (China): Changchun University of TCM, 2009. [Google Scholar]
He 2002 {published data only}
- He NMZ. Effect of acupuncture Zusanli for hypertension. International Journal of Traditional Chinese Medicine 2002;24(1):51‐2. [Google Scholar]
He 2012 {published data only}
- He JW, Du LP, Gu H, Zhang WH, Xia F, Xu Z, et al. Comparative analysis of acupuncture combined with acupoint application and Nitrendipine therapy in the treatment of elderly patients with systolic hypertension. China Medial Herald 2012;9(20):151‐2. [Google Scholar]
Hong 2009 {published data only}
- Hong ZP, Xu NG. The Influence of Acupuncture and Electro‐acupuncture in Blood Pressure and Hemodynamic Control of Hypertensive Patients [Masters thesis]. Guangdong Sheng (China): Guangzhou University of TCM, 2009. [Google Scholar]
Hu 2010 {published data only}
- Hu SK. Acupuncture for hypertension in 48 cases. Journal of Clinical Acupuncture and Moxibustion 2010;26(11):19‐20. [Google Scholar]
Huang 1991 {published data only}
- Huang HQ, Liang SZ. Clinical observation of auricular at Erxin for hypertension. Hubei Journal of Traditional Chinese Medicine 1991;13(85):34‐5. [Google Scholar]
Huang 2007a {published data only}
- Huang JF, Wei CE, He JP, Feng JJ. The clinical observation of acupuncture Fengchi for essential hypertension. Chinese Journal of Integrative Medicine on Cardio‐/Cerebrovascular Disease 2007;5(11):1130‐1. [Google Scholar]
Huang 2007b {published data only}
- Huang F, Yao GX, Huang XL, Liu YN. Clinical observation on acupuncture for treatment of hypertension of phlegm stasis blocking collateral type. Chinese Acupuncture and Moxibustion 2007;27(6):403‐6. [PubMed] [Google Scholar]
Jiang 2003 {published data only}
- Jiang Xiaolin. Effects of magnetic needle acupuncture on blood pressure and plasma ET‐1 level in the patient of hypertension. Journal of Traditional Chinese Medicine 2003;23(4):290‐1. [PubMed] [Google Scholar]
Jin 2010 {published data only}
- Jin CN, An YL, Zhang TS, Gao XA, Tian YF, Ji LX. Clinical effective observation on hypertension in early and middle periods by puncture acupoints group for hypertension. Chinese Archives of TCM 2010;28(8):1651‐3. [Google Scholar]
Jung 2010 {published data only}
- Park JM, Shin AS, Park SU, Sohn IlS, Jung WS, Moon SK. The acute effect of acupuncture on endothelial dysfunction in patients with hypertension: a pilot, randomized, double‐blind, placebo‐controlled crossover trial. Journal of Alternative and Complementary Medicine 2010;16(8):883‐8. [DOI] [PubMed] [Google Scholar]
Li 2008a {published data only}
- Li DZ, Niu CF. The effect of acupuncture for primary hypertension. Chinese Journal of Gerontology 2008;28:1963‐4. [Google Scholar]
Li 2008b {published data only}
- Li XQ, Wang X, Wu HL. Clinical randomised controlled trial of acupuncture Taichong for hypertension. Liaoning Journal of Traditional Chinese Medicine 2008;35(6):919‐20. [Google Scholar]
Li 2012b {published data only}
- Li HB, Chen CH. Acupuncture Taichong (LR 3) combined with amlodipine for 30 cases essential hypertension. Shaanxi Journal of Traditional Chinese 2012;33(8):1065‐6. [Google Scholar]
Liu 2012 {published data only}
- Liu SH, Wang JM. Clinical research of Neck acupuncture treatment combined with syndrome differentiation acupuncture to primary hypertension. Clinical Research of Neck Acupuncture Treatment Combined with Syndrome Differentiation Acupuncture to Primary Hypertension [Masters thesis]. Kunming (China): Yunnan Institute of Traditional Chinese Medicine, 2012. [Google Scholar]
Luo 2011 {published data only}
- Luo JC, Liang BX. Observation on the real‐time effect of acupuncture plus bloodletting on ear‐tip in reducing high blood pressure. Shanghai Journal of Acu‐mox 2011;30(12):838‐40. [Google Scholar]
Mou 1991 {published data only}
- Mou SL, Ma RL. Effect for nail fold microcirculation of acupuncture for hypertension. Journal of Clinical Acupuncture and Moxibustion 1991;10(4):10‐2. [Google Scholar]
Mu 2009 {published data only}
- Mu XH, Li QX. Clinical observations on acupuncture at Taichong and Zusanli for treating hypertension. Shanghai Journal of Acu‐mox 2009;28(6):328‐9. [Google Scholar]
Ning 2012 {published data only}
- Ning GL, Ma L, Dai GQ, Liu XL. Acupuncture Quchi and Fengchi plus message for cervical hypertension in 99 cases. TCM Research 2012;25(9):50‐2. [Google Scholar]
Qian 1996 {published data only}
- Qian J, Cheng XL, Liu HX. The immediately effect of acupuncture Yinxi for hypertension. Journal of Chinese Medicine 1996;11(6):27‐9. [Google Scholar]
Qu 2009 {published data only}
- Qu F, Hou SW. Comparative Observation About the Immediate Effect of Essential Hypertension Patients with Auricular Acupuncture and Wrist‐ankle Acupuncture Analgesia[Masters thesis]. Jinan City (China): Shandong University of TCM, 2009. [Google Scholar]
Shen 2010b {published data only}
- Shen PF, Bian JL, Meng ZH, Shi XM. Observations on the efficacy of acupuncture at point Renying (ST 9) by a twirling reinforcement method in treating hypertensive urgencies in primary hypertension patients. Shaihai Journal of Acu‐mox 2010;29(2):71‐3. [Google Scholar]
Song 2003 {published data only}
- Song YM, Zhu L, Du LL. Acupuncture combined with medicine for 64 cases primary hypertension. Shaanxi Journal of Traditional Chinese 2003;24(11):1005‐6. [Google Scholar]
Song 2006 {published data only}
- Song HQ, Liu GZ. Clinical Observation the Curative Effect on Acupuncture Quchi point vs Acupuncture both Quchi Point and Taichong Point Treating Essential Hypertension[Masters thesis]. Jinan City (China): Shandong University of TCM, 2006. [Google Scholar]
Sui 2012 {published data only}
- Sui MH, Wang CY, Ma WZ. Effect of arrival of qi and the method of reinforcing ‐ reducing by twirling and rotating the needle by acupuncture Quchi (LI 11) on the blood pressure of essential hypertension patients. Information on Traditional Chinese Medicine 2012;29(3):87‐90. [Google Scholar]
Sun 2009 {published data only}
- Sun J, Duan Q, Wang Q, Zhu XP, Fu WB. Clinical research for acupuncture for mild hypertension. Journal of New Chinese Medicine 2009;41(8):94‐5. [Google Scholar]
Tang 2003 {published data only}
- Tang SX, Xu ZH, Tang P. Flying needle method plus Morita therapy for hypertension. Chinese Journal of Clinical Rehabilitation 2003;7(21):2974. [Google Scholar]
Tian 2012 {published data only}
- Tian NJ, Tan QW. The Instant Effect of Needling Acupoint Quchi and Taichong in Lowering Blood Pressure of Primary Hypertension [Masters thesis]. Jinan City (China): Shandong University of TCM, 2012. [Google Scholar]
Wang 1994 {published data only}
- Wang SP, Hou M. Clinical observation of Aqunzhen therapy for 78 cases hypertension. Journal of Changchun College of Traditional Chinese Medicine 1994;10(40):41. [Google Scholar]
Wang 2003 {published data only}
- Wang X, Zou X, Li Q, Li S. Clinical study of acupuncture Taichong (LR 3) for hypertension. Journal of Practical Medicine 2003;19(5):565‐6. [Google Scholar]
Wang 2006 {published data only}
- Wang ZG, Chen YG. Clinical observation of acupuncture combined with medicine for hypertension. Liaoning Journal of Traditional Chinese Medicine 2006;33(4):430‐1. [Google Scholar]
Wang 2012b {published data only}
- Wang W, Wang ZG. Clinical observation for acupuncture combined with medicine of 80 cases primary hypertension. Chinese Community Doctor 2012;14(8):220‐1. [Google Scholar]
Wei 2010 {published data only}
- Wei Y, Kou JY, Chen J. Study on vaso‐active substance in serum of essential hypotensively the treatment of acupuncturing Renying point. Journal of Clinical Acupuncture Medicine 2010;26(2):12‐4. [Google Scholar]
- Wei Y, Sun ZR, Kou JY, Guo Y. clinical observation of acupuncture Renyin for hypertension. Journal of Clinical Acu‐Mox 2006;22(2):4‐5. [Google Scholar]
Wei 2012 {published data only}
- Wei N, Hou SW. The Observation of Immediate Antihypertensive Effects Using Xingjian and Taixi in Treating Hypertension [Masters thesis]. Jinan City (China): Shandong University of TCM, 2012. [Google Scholar]
Wu 2004a {published data only}
- Wu QM, Feng GX, Tang XF. Effects of acupuncture at Siguan points plus warming acupuncture‐moxibustion at Baihui (GV 20) on contents of plasma ET and NO in the patient of essential hypertension. Chinese Acupuncture and Moxibustion 2004;24(1):53‐5. [Google Scholar]
Wu 2004b {published data only}
- Wu YH, Zhu GQ, Lin XY, Ou YLX, Su HM, Wu BQ. Effect of needling Quchi and Taichong points on blood levels of endothelin and angiotension converting enzyme in patients with hypertension. Chinese Journal of Integrated Traditional and Western Medicine 2004;24(12):1080‐4. [PubMed] [Google Scholar]
Wu 2005 {published data only}
- Wu YH, Zhu GQ, Wen J, Ouyang LX, Wu BQ, Su HM, et al. Influence for ACE and ET in blood acupuncture for hypertension. TCM Research 2005;18(9):25‐7. [Google Scholar]
Xia 2006 {published data only}
- Xia YJ. Observation the effectiveness of acupuncture for essential hypertension. Journal of Practical Traditional Chinese Medicine 2006;22(9):568‐9. [Google Scholar]
Xia 2012 {published data only}
- Xia LJ. Clinical observation of 'Tsing lung put tail, white tiger shook his head' acupuncture for hypertension in Europe. Journal of Changchun University of Traditional Chinese Medicine 2012;28(4):659‐61. [Google Scholar]
Xie 2000 {published data only}
- Xie Y. Clinical observation of acupuncture and auricular point press for essential hypertension. Chinese Acupuncture and Moxibustion 2000;20(6):335‐6. [Google Scholar]
Xie 2014 {published data only}
- Xie B, Lin Y. Efficacy observation on acupuncture for essential hypertension of yin deficiency due to yang hyperactivity pattern. Chinese Acupuncture and Moxibustion 2014;34(6):547‐50. [PubMed] [Google Scholar]
Xing 2005 {published data only}
- Xing XM, Huang ZH, Fang YZ. Influence of nail fold microcirculation in acupuncture for primary hypertension. Journal of Chinese Clinical Rehabilitation 2005;9(7):106‐7. [Google Scholar]
Xing 2011 {published data only}
- Xing XM, Wang RC, Sun QW, Li H. Effect on blood pressure and microcirculation of nail fold in primary hypertension patients treated with acupuncture according to syndrome differentiation. Chinese Acupuncture & Moxibustion 2011;31(4):301‐4. [PubMed] [Google Scholar]
Yang 2002a {published data only}
- Yang F, Xu GL, Gao PY. Influence of immediate effect in BP and nail fold microcirculation in acupuncture for hypertension. Chinese Journal of Information on Traditional Chinese Medicine 2002;9(9):18‐9. [Google Scholar]
Yang 2002b {published data only}
- Yang F, Wang P, Ang WP, Ji QS. The immediate effect of time acupuncture on blood pressure and hemodynamics in essential hypertension patients. Shanghai Journal of Acu‐mox 2002;21(2):8‐9. [Google Scholar]
Yang 2010b {published data only}
- Yang F, Tan QW. Clinical Curative Comparison Between Bloodletting at the Erjian‐point and Acupuncture Quchi Plus Taichong Points in the Treatment of Essential Youth Hypertension [Masters thesis]. Jinan City (China): Shandong University of TCM, 2010. [Google Scholar]
Yao 1994 {published data only}
- Yao WH, Liu HX. Clinical effect of acupuncture Canzhu for hypertension. Journal of Traditional Chinese Medicine 1994;35(6):340. [Google Scholar]
Yi 1988 {published data only}
- Yi SX, Wang LH, Yan J, Li WL, Wang JJ, Yao XY. Effect of acupuncture for hypertension and relationship of cardiovascular function. Journal of Hunan College of TCM 1988;8(4):43‐4. [Google Scholar]
Yin 1994 {published data only}
- Yin ZF. Clinical observation of acupuncture for hypertension. Journal of Sichuan of TCM 1994;9(9):52‐3. [Google Scholar]
Yin 2002 {published data only}
- Yin ZF, Wang SY, Xiao D. Clinical observations on the treatment of hypertension with nape acupuncture. Shanghai Journal Acu‐mox 2002;21(5):10‐1. [Google Scholar]
Yu 2007 {published data only}
- Yu ZY, Lin B, Chen LR. Acupuncture combine with exercise therapy for 30 cases essential hypertension. Fujian Journal of Traditional Chinese Medicine 2007;38(1):22‐3. [Google Scholar]
Zhang 1999 {published data only}
- Zhang TF, Zhang HX, Liu YP. Observation of single point for hypertension. Hubei Journal of TCM 1999;21(5):235. [Google Scholar]
Zhang 2001 {published data only}
- Zhang HX, Zhang TF, Liu YP. Control observation on acupuncture of Quchi (LI 11) and medication in transient action of decreasing blood pressure. Chinese Acupuncture and Moxibustion 2001;21(11):645‐6. [Google Scholar]
Zhang 2002 {published data only}
- Zhang ZH, Wang Q. Effects of acupuncture on plasma endothelin content in the patient of primary hypertension. Chinese Acupuncture and Moxibustion 2002;22(3):147‐8. [Google Scholar]
Zhang 2004 {published data only}
- Zhang ZH, Zhou J, Wang Q, Ma X. Acupuncture for treatment of primary hypertension and effect on functions of vascular endothelium. Chinese Acupuncture and Moxibustion 2004;24(8):539‐40. [Google Scholar]
Zhang 2005 {published data only}
- Zhang YL, Li CP, Peng M, Yang HS. Effect of acupuncture combined with medicine on neuropeptide Y in the patient of hypertension. Chinese Acupuncture and Moxibustion 2005;25(3):155‐7. [PubMed] [Google Scholar]
Zhang 2008 {published data only}
- Zhang J, Marquina N, Oxinos G, Sau A, Ng D. Effect of laser acupoint treatment on blood pressure and body weight ‐ a pilot study. Journal of Chiropractic Medicine 2008;7:134‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2009 {published data only}
- Zhang J, Ng D, Sau A. Effects of electrical stimulation of acupuncture points on blood pressure. Journal of Chiropractic Medicine 2009;8:9‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2011 {published data only}
- Zhang P, Zhang T. The Influence of Catgut Embedding in Acupoint to ET and NO Level of Essential Hypertension (EH) Patients with Phlegm Dampness[Masters thesis]. Jinan City (China): Shandong University of TCM, 2011. [Google Scholar]
Zhang 2012b {published data only}
- Zhang XQ. Clinical observation for acu‐mox combined with medicine for moderate hypertension. Qinhai Medical Journal 2012;42(9):65‐6. [Google Scholar]
Zhao 2003 {published data only}
- Zhao DJ, Fan QL. Effect of acupuncture on insulin resistance in the patient of hypertension. Chinese Acupuncture and Moxibustion 2003;23(3):165‐7. [Google Scholar]
Zhao 2011 {published data only}
- Zhao R, Fu LX. Immediate effect on blood pressure of acupuncture at Renying (ST 9) in 53 cases of hypertension patient. Chinese Acupuncture and Moxibustion 2011;31(5):466. [PubMed] [Google Scholar]
Zhao 2012 {published data only}
- Zhao QY, Fu WB. Clinical Observations on Acupuncture Treating Anxiety State of Essential Hypertension Patients[Masters thesis]. Guangzhou (China): Guangzhou University of TCM, 2012. [Google Scholar]
Zheng 2012 {published data only}
- Zheng ZY, Lv XP, Xu R, Dong LX. Clinical observation of acupuncture for hypertension. Chinese and Foreign Medical Research 2012;10(3):77‐8. [Google Scholar]
Zhou 1997 {published data only}
- Zhou H. Clinical observation of acupuncture Neiguan and Taichong for primary hypertension. Shanghai Journal of TCM 1997;16(4):10. [Google Scholar]
Zhou 2012 {published data only}
- Zhou YL. Clinical observation of acupuncture Zhigou, Yanglinquan, Taiyang, Taichong for hypertension. Journal of Changchun University of Traditional Chinese Medicine 2012;28(8):744. [Google Scholar]
Zhu 2006 {published data only}
- Zhu GQ, Wu YH, Wu BQ, Su HM, Ouyang LX, Su ZH, et al. Research of needling Quchi and Taichong points on treating hypertension patients with different syndrome. Zhejiang Journal of of Integrated Traditional Chinese and Western Medicine 2006;16(1):4‐6. [Google Scholar]
References to ongoing studies
Liang {unpublished data only}
- Effect of Acupuncture on Patients with Mild Hypertension (EAPMH).. Ongoing study July 2012..
Additional references
Atkins 2004
- Atkins D, Best D, Briss PA, Eccles M, Falck‐Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chobanian 2003
- Aram V, Chobanian GL, Bakris HR, Black WC, Cushman LA, Green JL, et al. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003;42:1206‐52. [DOI] [PubMed] [Google Scholar]
Gordon 2008
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schünemann HJ, GRADE Working Group. GRADE: what is "quality of evidence" and why is it important to clinicians?. BMJ 2008;336:995‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gordon 2008a
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heran 2008
- Heran BS, Wong MMY, Heran IK, Wright JM. Blood pressure lowering efficacy of angiotensin converting enzyme (ACE) inhibitors for primary hypertension. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD003823.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
Howell 2004
- Howell SJ, Sear JW, Foex P. Hypertension, hypertensive heart disease and perioperative cardiac risk. British Journal of Anaesthesia 2004;92(4):570‐83. [DOI] [PubMed] [Google Scholar]
Huang 2005
- Huang ST, Chen GY, Lo HM, Lin JG, Lee YS, Kuo CD. Increase in the vagal modulation by acupuncture at Neiguan point in the health subjects. American Journal of Chinese Medicine 2005;33(1):157‐64. [DOI] [PubMed] [Google Scholar]
Kalish 2004
- Kalisha LA, Buczynskib B, Connella P, Gemmela A, Goertzc C, Macklin EA, et al. Stop Hypertension with the Acupuncture Research Program (SHARP): clinical trial design and screening results. Controlled Clinical Trials 2004;25:76‐103. [DOI] [PubMed] [Google Scholar]
Kaplan 2006
- Kaplan NM. Acupuncture for hypertension: can 2500 years come to an end?. Hypertension 2006;48:815. [DOI] [PubMed] [Google Scholar]
Kaptchuk 2000
- Kaptchuk TJ. The Web That Has No Weaver: Understanding Chinese Medicine. The Web That Has No Weaver: Understanding Chinese Medicine. Revised. Chicago (IL): McGraw‐Hill, 2000. [Google Scholar]
Kaptchuk 2002
- Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Annals of Internal Medicine 2005;136(5):374‐83. [DOI] [PubMed] [Google Scholar]
Kearney 2005
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet 2005;365:217‐23. [DOI] [PubMed] [Google Scholar]
Kim 2010
- Kim LW, Zhu J. Acupuncture for essential hypertension. Alternative Therapies in Health and Medicine 2010 ;16(2):18‐29. [PubMed] [Google Scholar]
Lee 2009
- Lee H, Kim SY. Acupuncture for lowering blood pressure: systematic review and meta‐analysis. American Journal of Hypertension 2009;22(1):122‐8. [DOI] [PubMed] [Google Scholar]
Li 2014
- Li DZ, Zhou Y, Yang YN, Ma YT, Li XM, Yu J, et. Acupuncture for essential hypertension: a meta‐analysis of randomized sham‐controlled clinical trials. Evidence‐Based Complementary and Alternative Medicine 2014;2014:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mensah 2002
- Mensah GA. The global burden of hypertension: good news and bad news. Cardiology Clinics 2002;20:181‐5. [DOI] [PubMed] [Google Scholar]
Moffet 2006
- Moffet HH. Hasty conclusion about acupuncture for hypertension?. Hypertension 2007;49:e5. [DOI] [PubMed] [Google Scholar]
Napadow 2004
- Napadow V, Kaptchuk TJ. Patient characteristics for outpatient acupuncture in Beijing, China. Journal of Alternative and Complement Medicine 2004;10:565‐72. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Spence 2006
- Spence JD. Individualized therapy for hypertension. Hypertension 2006;47(3):e11. [DOI] [PubMed] [Google Scholar]
Turnbull 2007
- Turnbull F, Patel A. Acupuncture for blood pressure lowering: needling the truth. Circulation 2007;115(4):3048‐9. [DOI] [PubMed] [Google Scholar]
Wan 2009
- Wan WJ, Ma CY, Xiong XA, Wang L, Ding L, Zhang YX, et al. Clinical observation on therapeutic effect of electroacupuncture at Quchi (LI 11) for treatment of essential hypertension. Zhongguo Zhen Jiu 2009;29(5):349‐52. [PubMed] [Google Scholar]
Wang 2013
- Wang J, Xiong X, Liu W. Acupuncture for essential hypertension. International Journal of Cardiology 2013;169(5):317‐26. [DOI] [PubMed] [Google Scholar]
Wolf‐Maier 2004
- Wolf‐Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension 2004;43(1):10‐7. [DOI] [PubMed] [Google Scholar]
Wong 2002
- Wong MMY, Heran BS, Wright JM. Blood pressure lowering efficacy of calcium channel blockers for primary hypertension. Cochrane Database of Systematic Reviews 2002, Issue 2. [DOI: 10.1002/14651858.CD003657] [DOI] [Google Scholar]
Wong 2016
- Wong GWK, Boyda HN, Wright JM. Blood pressure lowering efficacy of beta‐1 selective beta blockers for primary hypertension. Cochrane Database of Systematic Reviews 2016, Issue 3. [DOI: 10.1002/14651858.CD007451.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


