Abstract
Purpose:
Rural residents may have lower access to and use of certain health information sources relative to urban residents. We investigated differences in information source access and use between rural and urban US adults and whether having low health literacy might exacerbate rural disparities in access to and use of health information.
Methods:
Six hundred participants (50% rural) completed an online survey about access and use of 25 health information sources. We used logistic regression models to test associations between rurality and access to and use of health information sources and whether rurality interacted with health literacy to predict the access and use.
Findings:
Compared to urban residents, rural residents had lower access to health information from sources including primary care providers, specialist doctors, blogs, and magazines, and less use of search engines. After accounting for sociodemographics, rural residents only had lower access to specialist doctors than urban residents. Rural residents with limited health literacy had lower access to mass media and scientific literature but higher use of corporations/companies than rural residents with adequate health literacy and urban residents regardless of health literacy level.
Conclusions:
Some differences in access and use of health information sources may be accounted for by sociodemographic differences between rural and urban populations. There may be structural barriers such as shortage of specialist doctors and limited media exposure that make it harder for rural residents to access health information, especially those with limited health literacy.
Keywords: health information access, health information use, health literacy, rural-urban health disparities
Access to and use of health information are critical to personal and public health outcomes. Better health information access and use help individuals improve knowledge, increase use of health services, reduce health care costs, adopt healthier behavioral patterns, and therefore promote health.1,2 Access refers to people’s ability to seek, find, and obtain health-related information.1 Use refers to people’s ability to make decisions that maintain and/or improve their health based on the health information they receive.1 Whether an individual has health information access and how the individual uses such information can influence that person’s health behavior, health care utility, health outcomes, and quality of life.1 For example, higher levels of health information access and use are associated with lower levels of smoking and alcohol consumption, higher levels of exercise and health checkups, and better self-rated health status.3
Multiple barriers create challenges for rural residents to access and use reliable health information, including barriers such as geography, distance, inclement weather, and lack of financial resources and specialty health care services.4 Furthermore, there are rural-urban health disparities that disadvantage the 20% of the US population who live in rural areas.5 Compared to urban residents, rural residents have higher all-cause mortality rates,6 higher rates of premature morbidity and mortality from diseases such as cancer, heart disease, and childhood obesity,7–10 lower access and use of preventive health care services,11,12 and they are more likely to engage in unhealthy behaviors.13,14 Due to the connection between health information access/use and health outcomes, examining the rural-urban health information access/use differences may help reduce rural-urban health disparities.
The knowledge gap hypothesis15 may also be helpful for understanding the role of information access and use in the development of rural-urban health disparities. In its original formulation, the hypothesis posits that, compared to those with lower socioeconomic status (SES), individuals with higher SES should have more access to and use of health information and thus will be more likely to benefit from new health information.15 Over time this creates a gap in health knowledge between those with higher and lower SES15,16 that contributes to health disparities.17 Research has shown that rural residents have lower SES than urban residents,7 and thus they may have limited access to and use of health information due to the differential access posited by the knowledge gap hypothesis.
Finally, research has shown that rural residents have limited access to and use of online health information compared to urban residents,18 particularly online access involving high speed Internet.19 They also have lower access to health care providers.20 Given that people identify health care professionals and Internet as their primary sources of health information,1,21,22 these infrastructure limitations may be significant obstacles to health information access and use in rural areas. However, less is known about the differences in health information source access and use between rural and urban residents.
This study contributes to the literature by investigating the access/use patterns among 25 health information sources including health professionals, lay individuals, mass media, and different types of online sources (eg, social media, medical websites, and blogs or celebrity webpages). We explored a wide range of health information sources because consumers report consulting multiple kinds of sources for information when making health decisions.23 For example, individuals tend to use health professionals for information related to diagnosis or standard treatment, but they use friends for information related to coping strategies.23 Also, many previous studies categorized online health information sources as a single source, rather than differentiating between types of online sources; however, the use patterns vary among medical websites, social media, and celebrity webpages.24 Thus, it is important to differentiate among the wide variety of online health information sources to investigate people’s health information access/use patterns in greater detail.
In addition to examining overall differences in access and use, we also explored the role of health literacy in these differences. Health literacy has profound effects on people’s ability to understand and use health information25,26 and therefore is an essential factor to consider as a possible determinant of information access and use. For example, compared to patients with adequate health literacy, those with limited health literacy learned significantly less from health education information.27 Studies have shown that rural residents have lower health literacy than urban residents; however, this may due to differences in age, gender, race/ethnicity, education, and income.28 Nevertheless, it is possible that people with limited health literacy who live in rural areas face qualitatively different challenges of accessing and using health information than people with limited health literacy living in urban environments. There may be more health information sources in urban than rural environments that are accessible and understandable among people with low health literacy (eg, billboards, transportation signage, greater density of health clinics). Consequently, limited health literacy may be less of a barrier to access to and use of health information among people living in urban environments than rural areas.
The purpose of this study was to examine differences in health information access and use between rural and urban adults in the US. We conducted a nationally representative survey in which participants reported their access to and use of 25 health information sources. We hypothesized that rural residents would have lower access to and use of some sources compared to urban residents and that rural-urban disparities in health information access and use would be greater among people with limited health literacy.
Methods
Procedure and Participants
The Institutional Review Board at University at Buffalo approved the data collection protocol. Participant recruitment and data collection were conducted by GfK Group (Nuremberg, Germany), a market research firm with an academic research arm. Participants were members of the GfK KnowledgePanel®. The KnowledgePanel includes 55,000 people selected by GfK using probability-based sampling methodology based on the most recent Delivery Sequence File of the United States Postal Service that provides an effective sampling infrastructure for recruitment of hard-to-reach individuals, such as young adults and those from racial minority groups. These members were invited to join KnowledgePanel through a series of mailings. GfK provides Internet-enabled devices for those who would like to join the panel but have no Internet connection, which helps in reducing selection bias among individuals who lack Internet access. When analyzed with proper analytic procedures that account for weighting (see Data Analysis section below),29 data from GfK samples can be considered representative of the non-institutionalized US population. For this study, GfK used its internal records about the panel to identify panelists who were eligible for this study. GfK then sent email invitations to a randomly selected subset of 1,066 members of the panel. Eligibility criteria were: 18 years or older, residing in metropolitan or nonmetropolitan areas in the US, and ability to communicate in English. There were 618 people (58% of invited respondents) who completed the survey between February and April 2017.
Responses for 18 participants were dropped because they met 2 or more of the following 4 a priori criteria indicating a lack of attention to survey completion: (1) completed the survey in less than 8 minutes (ie, one-quarter of the median time of 32 minutes), (2) straight-lined or marked identical responses on more than 4 grids that contained one or more items that were worded in the direction opposite to the others (suggesting lack of attention to individual questions), (3) failed both of the survey validation items (asking participants to select “somewhat agree” for one item and “somewhat disagree” for the other item), and (4) gave different answers to a repeated factual question about their health insurance types. Given these exclusions, the final analysis sample included 600 participants with 302 rural and 298 urban residents.
Measures
Rural-Urban Residence
Rural-urban residence was defined based on participants’ location of primary residence (identified by GfK from the participant’s IP address) as identified by the Office of Management and Budget (OMB).30 Specifically, urban residence refers to urbanized areas with a population of at least 50,000, which are classified as “Core Based Statistical Areas” (CBSAs); rural residence refers to areas that are not included in CBSAs.
Access to and Use of Health Information Sources
We assessed access to information source with the question, “Can you easily and affordably get health information from the following sources? [Yes/No].” We assessed use of sources with the question, “Do you get health information from the following sources? [Yes/No].” We asked these 2 questions for each of 25 health information sources that were adapted from the Health Information National Trends Survey31 and the Pew Research Center.32,33 Then, we grouped the 25 sources into 6 categories: (1) health professionals: primary care providers, nurses, specialist doctors, pharmacists, veterinarians, and dentists; (2) lay individuals: friends, family, religious organizations and leaders; (3) health authorities: health fairs, local health department, federal government organizations, scientists, and scientific literature; (4) online sources: search engines, social media, medical websites, and blogs or celebrity webpages; (5) mass media: newspapers, magazines, books, television, and radio; (6) companies: pharmaceutical companies, and other companies or corporations (eg, the retailer GNC (GNC Holdings Inc., Pittsburgh, PA)).
Health Literacy
We assessed health literacy using the Newest Vital Sign (NVS).34 The NVS asks 6 open-ended questions based on the information on a mock ice cream nutrition label. Participants receive 1 point for each correct answer. They receive 0 points on incorrect or missing items. The NVS total score ranges from 0 to 6. A score < 4 indicates the possibility of limited health literacy and a score ≥ 4 indicates adequate health literacy.34 This cut-off score has high sensitivity for detecting individuals with limited health literacy.34 Therefore, we dichotomized health literacy as limited (NVS score < 4) or adequate (NVS score ≥ 4).34–38
Sociodemographics
Sociodemographic variables included age, sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic other), household annual income (<$25k, $25k to <$50k, $50k to <$75k, $75k to <$100k, $100k to <$125k, $125k and up), and education (less than high school, high school graduate, some college, and Bachelor’s degree and above).
Data Analysis
We performed Chi-square and t-tests using unweighted data to compare sociodemographics and health literacy between rural and urban participants. The rural and urban subsamples were weighted using the geodemographic benchmarks from the Current Population Survey (CPS)39 information released in March 2017. Analyses applying survey weights reduce the likelihood of Type I errors by accounting for the survey’s complex design and sampling scheme.29 This weighting approach yields estimates that are representative of the US rural and urban populations. We used unadjusted and adjusted logistic regression models with weighted data to test associations between rurality and access to and use of each of the 25 health information sources separately. Outcomes were each source, each category of sources, and all sources aggregated together. Covariates were race/ethnicity, income, and education because, as expected based on prior research7 and our descriptive results, rural and urban residents significantly differed on these 3 demographic variables. Where source use was the outcome, we added access to the models because use of information is contingent upon access to such information. Unadjusted models provide valuable information about the aggregate experiences of actual people living in rural and urban areas; in contrast, adjusted estimates tell us more about people’s hypothetical behavior if they had similar racial/ethnic and SES characteristics.40 To better understand the source access and use patterns, we performed Hierarchical Linear Modeling (HLM) because HLM provides more accurate estimates compared to linear regression models when analyzing nested data.41 We classified the 25 sources into 6 categories; therefore, sources were nested within each category. Finally, we used logistic regressions to test whether or not rurality interacted with health literacy to predict access to and use of the individual health information sources. We also performed the relative excess risk due to interaction (RERI) to test the departure from additivity of effects.42–44 We conducted regression analyses using Stata (StataCorp LLC, College Station, TX) and HLM using SAS (SAS Institute Inc., Cary, NC). We set the significance level at α=0.05.
Results
Sociodemographics and Health Literacy Differences between Rural and Urban Residents
Differences in sociodemographics and health literacy between the unweighted rural and urban samples are shown in Table 1. Rural participants were less racially and ethnically diverse than urban participants (P < .001). Compared to urban participants, more rural participants self-identified as non-Hispanic white, and fewer were non-Hispanic black, Hispanic, or non-Hispanic other. Rural participants had lower income (P < .001) and education (P < .001) than urban participants. We found no differences in health literacy (P = .538) or age (P = .725) between rural and urban participants. About 83.7% of the rural participants and 81.8% of the urban participants had adequate health literacy (NVS score ≥4).
Table 1.
Demographics and Health Literacy among Rural and Urban Participants (N = 600)
| Demographic | Rural (n = 302) | Urban (n = 298) | χ2 | P | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Race / Ethnicity | ||||||
| Non-Hispanic white | 262 | 86.3 | 216 | 72.5 | 20.92 | < .001 |
| Non-Hispanic black | 16 | 5.3 | 25 | 8.4 | ||
| Hispanic | 12 | 4.0 | 36 | 12.1 | ||
| Non-Hispanic Other | 12 | 4.0 | 21 | 7.0 | ||
| Household Annual Income | ||||||
| <$25k | 67 | 22.0 | 34 | 11.4 | 28.80 | < .001 |
| $25k to <$50k | 70 | 23.2 | 63 | 21.1 | ||
| $50k to <$75k | 61 | 20.2 | 46 | 15.4 | ||
| $75k to <$100k | 44 | 14.6 | 49 | 16.4 | ||
| $100k to <$125k | 27 | 8.9 | 31 | 10.4 | ||
| $125k and up | 33 | 10.9 | 75 | 25.2 | ||
| Education | ||||||
| Less than high school | 27 | 8.9 | 21 | 7.0 | 23.75 | < .001 |
| High school graduate | 115 | 38.1 | 86 | 28.9 | ||
| Some college | 92 | 30.5 | 69 | 23.2 | ||
| Bachelor and above | 68 | 22.5 | 122 | 40.9 | ||
| Health Literacy | ||||||
| Limited | 49 | 16.3 | 54 | 18.2 | 0.38 | .538 |
| Adequate | 251 | 83.7 | 242 | 81.8 | ||
| Age | M = 51.70, SD = 17.61 | M = 52.18, SD = 15.52 | t = 0.35 | .725 | ||
Note. Results were unweighted; Health literacy scale: NVS ranges from 0 to 6, scores ≤3 indicate limited health literacy, scores ≥4 indicate adequate health literacy.
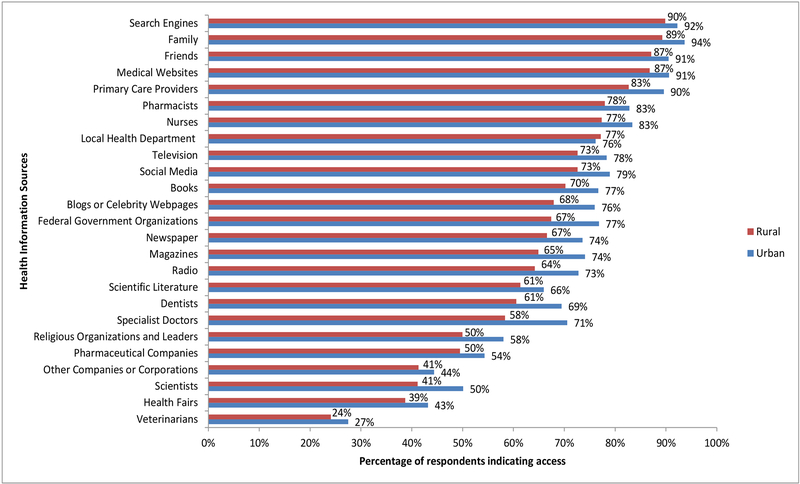
Access to Health Information Sources
Apart from descriptive statistics and comparisons in Table 1 reported above, all other analyses were conducted with weighted data. Among rural residents, the 3 most accessible health information sources were search engines (90%), family (89%), and friends (87%); the 3 least accessible sources were veterinarians (24%), health fairs (39%), and scientists (41%). Among urban residents, the 3 most accessible sources were family (94%), search engines (92%), and medical websites (91%); the 3 least accessible sources were veterinarians (27%), health fairs (43%), and companies or corporations other than pharmaceutical companies (44%). Figure 1 contains weighted frequency of access to each source of health information among rural and urban residents.
Figure 1.
Access to Health Information Sources
In Table 2, we present the unadjusted and adjusted HLM findings of 6 categories (capitalized), as well as the logistic regression findings of each individual health information source. In the unadjusted HLM models, compared to urban residents, rural residents had significantly lower access to health information from the following source categories: health professionals (OR=0.70, 95% CI: 0.55–0.88, P = .003), online sources (OR=0.67, 95% CI: 0.45–1.00, P = .047), and mass media (OR=0.63, 95% CI: 0.41–0.97, P = .034). In the adjusted model, there were no statistical rural-urban differences among any of the source categories.
Table 2.
Comparing Access to and Use of Health Information Sources between Rural and Urban Residents
| ACCESS | USE | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | ||||||||||||
| Sources | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |||
| ALL SOURCES | 0.68 | 0.53, 0.87 | .002** | 0.85 | 0.66, 1.10 | .208 | 1.01 | 0.86, 1.19 | .882 | 1.07 | 0.91, 1.27 | .410 | |||
| HEALTH PROFESSIONALS | 0.70 | 0.55, 0.88 | .003** | 0.82 | 0.65, 1.05 | .115 | 1.00 | 0.83, 1.20 | .970 | 1.05 | 0.86, 1.28 | .628 | |||
| Primary care providers | 0.56 | 0.34, 0.90 | .016* | 0.65 | 0.39, 1.08 | .094 | 0.88 | 0.48, 1.62 | .690 | 1.00 | 0.53, 1.89 | .997 | |||
| Nurses | 0.68 | 0.45, 1.03 | .069 | 0.96 | 0.61, 1.49 | .841 | 1.44 | 0.94, 2.21 | .094 | 1.68 | 1.06, 2.64 | .026* | |||
| Specialist doctors | 0.58 | 0.41, 0.82 | .002** | 0.62 | 0.43, 0.90 | .011* | 0.78 | 0.52, 1.17 | .229 | 0.78 | 0.50, 1.21 | .266 | |||
| Pharmacists | 0.73 | 0.49, 1.11 | .144 | 0.87 | 0.56, 1.36 | .549 | 1.34 | 0.92, 1.94 | .126 | 1.37 | 0.93, 2.04 | .114 | |||
| Veterinarians | 0.84 | 0.57, 1.23 | .359 | 0.86 | 0.57, 1.29 | .461 | 1.53 | 0.66, 3.56 | .325 | 2.22 | 0.85, 5.83 | .106 | |||
| Dentists | 0.68 | 0.48, 0.95 | .026* | 0.89 | 0.61, 1.29 | .528 | 0.80 | 0.53, 1.21 | .297 | 0.83 | 0.53, 1.30 | .425 | |||
| LAY INDIVIDUALS | 0.75 | 0.56, 1.01 | .056 | 0.84 | 0.62, 1.14 | .260 | 1.24 | 0.90, 1.71 | .199 | 1.32 | 0.94, 1.85 | .105 | |||
| Friends | 0.71 | 0.42, 1.18 | .188 | 0.77 | 0.44, 1.33 | .343 | 1.06 | 0.73, 1.54 | .741 | 1.16 | 0.78, 1.72 | .471 | |||
| Family | 0.56 | 0.31, 1.02 | .059 | 0.68 | 0.36, 1.27 | .221 | 1.21 | 0.79, 1.86 | .382 | 1.31 | 0.83, 2.06 | .249 | |||
| Religious organizations and leaders | 0.72 | 0.52, 1.00 | .049* | 0.79 | 0.56, 1.11 | .172 | 1.66 | 0.96, 2.88 | .070 | 1.83 | 0.97, 3.43 | .061 | |||
| HEALTH AUTHORITIES | 0.83 | 0.63, 1.09 | .171 | 1.00 | 0.75, 1.34 | .983 | 1.05 | 0.65, 1.69 | .850 | 1.32 | 0.80, 2.20 | .279 | |||
| Health fairs | 0.83 | 0.59, 1.17 | .283 | 0.98 | 0.68, 1.40 | .892 | 1.70 | 0.98, 2.95 | .060 | 1.91 | 1.03, 3.53 | .039* | |||
| Local health department | 1.06 | 0.72, 1.55 | .767 | 1.05 | 0.70, 1.57 | .813 | 1.42 | 0.97, 2.09 | .073 | 1.38 | 0.91, 2.10 | .129 | |||
| Federal government organizations | 0.63 | 0.44, 0.90 | .011* | 0.72 | 0.49, 1.07 | .101 | 0.85 | 0.58, 1.24 | .396 | 0.91 | 0.60, 1.37 | .649 | |||
| Scientists | 0.70 | 0.50, 0.96 | .028* | 0.75 | 0.53, 1.06 | .103 | 0.72 | 0.47, 1.10 | .121 | 0.86 | 0.54, 1.35 | .506 | |||
| Scientific literature | 0.82 | 0.59, 1.15 | .245 | 1.03 | 0.71, 1.48 | .879 | 0.90 | 0.62, 1.32 | .595 | 1.06 | 0.70, 1.60 | .796 | |||
| ONLINE SOURCES | 0.67 | 0.45, 1.00 | .047* | 0.87 | 0.57, 1.32 | .506 | 0.89 | 0.71, 1.11 | .302 | 0.95 | 0.75, 1.20 | .660 | |||
| Search engines | 0.74 | 0.42, 1.31 | .302 | 0.90 | 0.49, 1.65 | .731 | 0.66 | 0.45, 0.97 | .036* | 0.74 | 0.49, 1.11 | .144 | |||
| Social media | 0.71 | 0.48, 1.03 | .074 | 0.86 | 0.57, 1.29 | .456 | 0.67 | 0.44, 1.01 | .055 | 0.70 | 0.45, 1.09 | .111 | |||
| Medical websites | 0.68 | 0.41, 1.14 | .142 | 0.83 | 0.47, 1.44 | .502 | 0.86 | 0.57, 1.31 | .489 | 0.94 | 0.61, 1.46 | .792 | |||
| Blogs or celebrity webpages | 0.67 | 0.47, 0.96 | .030* | 0.81 | 0.55, 1.20 | .303 | 0.96 | 0.54, 1.69 | .875 | 1.19 | 0.64, 2.22 | .585 | |||
| MASS MEDIA | 0.63 | 0.41, 0.97 | .034* | 0.87 | 0.55, 1.37 | .542 | 1.05 | 0.69, 1.60 | .813 | 1.20 | 0.78, 1.86 | .413 | |||
| Newspapers | 0.72 | 0.50, 1.02 | .064 | 0.85 | 0.58, 1.24 | .391 | 0.85 | 0.56, 1.27 | .422 | 0.90 | 0.58, 1.40 | .637 | |||
| Magazines | 0.65 | 0.45, 0.92 | .016* | 0.77 | 0.53, 1.13 | .185 | 1.01 | 0.70, 1.47 | .951 | 1.14 | 0.77, 1.71 | .513 | |||
| Books | 0.72 | 0.50, 1.03 | .075 | 0.88 | 0.59, 1.31 | .529 | 1.52 | 1.05, 2.18 | .025* | 1.66 | 1.13, 2.45 | .011* | |||
| Television | 0.73 | 0.50, 1.07 | .107 | 0.84 | 0.56, 1.25 | .381 | 1.03 | 0.72, 1.47 | .866 | 1.21 | 0.83, 1.79 | .324 | |||
| Radio | 0.67 | 0.47, 0.95 | .025* | 0.81 | 0.27, 1.18 | .273 | 0.84 | 0.53, 1.34 | .466 | 1.01 | 0.61, 1.67 | .960 | |||
| COMPANIES | 0.79 | 0.54, 1.17 | .243 | 0.90 | 0.59, 1.36 | .613 | 1.58 | 0.71, 3.51 | .265 | 1.72 | 0.76, 3.90 | .196 | |||
| Pharmaceutical companies | 0.82 | 0.60, 1.14 | .241 | 0.90 | 0.64, 1.27 | .536 | 1.13 | 0.75, 1.71 | .564 | 1.19 | 0.77, 1.86 | .431 | |||
| Other companies or corporations | 0.88 | 0.64, 1.22 | .452 | 0.92 | 0.65, 1.31 | .652 | 1.90 | 1.04, 3.48 | .038* | 1.82 | 0.95, 3.48 | .070 | |||
Note. Results were weighted using the rural-urban specific weight; OR = odds ratio; SE = standard error; CI = confidence interval;
indicates P < .05;
indicates P < .01.
For Access, unadjusted models contained the single predictor (rural versus urban); adjusted models included race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic other), income (continuous), and education (continuous) as covariates; For Use, unadjusted models contained Access as a covariate; adjusted models included Access, race/ethnicity, income, and education as covariates.
In the unadjusted models for each individual source, compared to urban residents, rural residents had significantly lower access to health information from primary care providers (OR=0.56, 95% CI: 0.34–0.90, P = .016), specialist doctors (OR=0.58, 95% CI: 0.41–0.82, P = .002), dentists (OR=0.68, 95% CI: 0.48–0.95, P = .026), religious organizations and leaders (OR=0.72, 95% CI: 0.52–1.00, P = .049), federal government organizations (OR=0.63, 95% CI: 0.44–0.90, P = .011), scientists (OR=0.70, 95% CI: 0.50–0.96, P = .028), blogs or celebrity webpages (OR=0.67, 95% CI: 0.47–0.96, P = .030), magazines (OR=0.65, 95% CI: 0.45–0.92, P = .016), and radio (OR=0.67, 95% CI: 0.47–0.95, P = .025). In the adjusted models, only the difference in access to health information from specialist doctors remained significant (AOR=0.62, 95% CI: 0.43–0.90, P = .011).
Demographic Predictors for Health Information Access
In the adjusted models in which each category of source was regressed on rural-urban residence, higher income was associated with more access to all the categories but education was not associated with access to any category. Race/ethnicity was associated with access to the online sources category. Compared to whites, Hispanics and blacks had higher odds but non-Hispanic others had lower odds of having access to these sources.
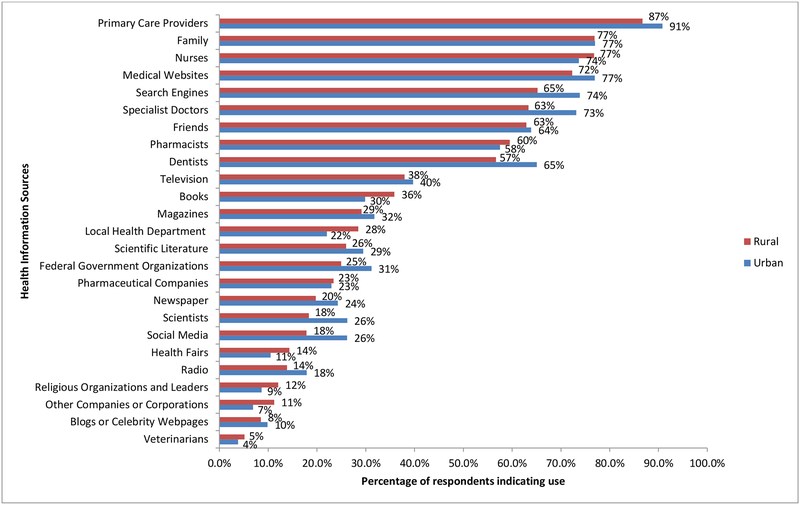
Use of Health Information Sources
As seen in Figure 2, the weighted analyses show that among rural residents, the 3 most used sources were primary care providers (87%), family (77%), and nurses (77%); the 3 least used sources were veterinarians (5%), blogs or celebrity webpages (8%), and companies or corporations other than pharmaceutical companies (11%). Among urban residents, the 3 most used sources were primary care providers (91%), family (77%), and medical websites (77%); the 3 least used sources were veterinarians (4%), companies or corporations other than pharmaceutical companies (7%), and religious organizations and leaders (9%).
Figure 2.
Use of Health Information Sources
As shown in Table 2, the unadjusted and adjusted HLM models indicated no rural-urban differences in using these 6 source categories. In the unadjusted models for each individual source, compared to urban residents, rural residents had significantly lower use of health information from search engines (OR=0.66, 95% CI: 0.45–0.97, P = .036), books (OR=1.52, 95% CI: 1.05–2.18, P = .025), and other companies or corporations (OR=1.90, 95% CI: 1.04–3.48, P = .038). In the adjusted models, compared to urban residents, rural residents had higher use of nurses (AOR=1.68, 95% CI: 1.06–2.64, P = .026), health fairs (AOR=1.91, 95% CI: 1.03–3.53, P = .039), and books (AOR=1.66, 95% CI: 1.13–2.45, P = .011).
Demographic Predictors for Health Information Use
In the adjusted models in which each category of source was regressed on rural-urban residence, higher income was associated with more use of the health authorities category, and higher education was associated with more use of health professionals, mass media, and health authorities categories. Race/ethnicity was associated with use of the following categories: online sources, mass media, lay individuals, and health authorities. For the use of online sources, mass media, and lay individuals, non-Hispanics others, blacks, and Hispanics had higher rates than whites. For the use of health authorities, compared to whites, Hispanics and non-Hispanic others had higher rates but blacks had a lower rate of using these sources.
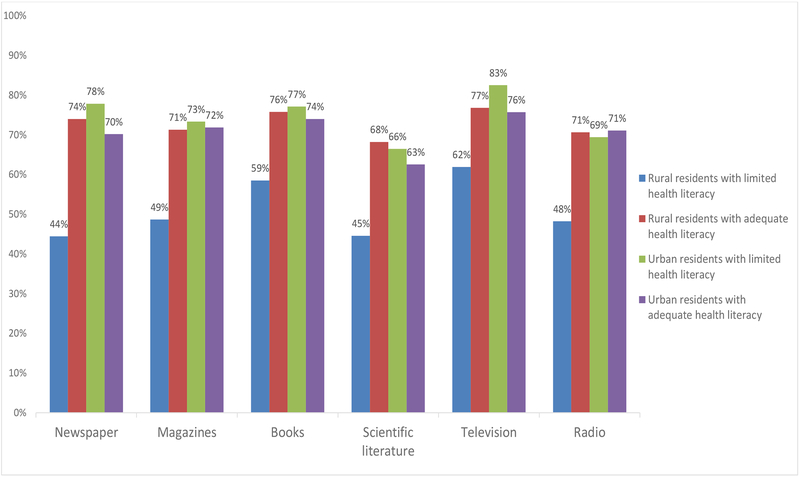
Interaction Effects of Health Literacy and Rural-Urban on Source Access and Use
We tested whether rural-urban residence interacted with health literacy to predict access to and use of health information sources. We found interaction effects between rural-urban residence and health literacy on access to newspapers (interaction P < .001), magazines (interaction P = .008), books (interaction P = .014), scientific literature (interaction P = .003), television (interaction P = .011), and radio (interaction P = .021). Among rural residents, having limited health literacy was associated with lower odds of access to health information from newspapers (OR=0.20, P < .001), magazines (OR=0.25, P < .001), books (OR=0.29, P < .001), scientific literature (OR=0.24, P < .001), television (OR=0.41, P = .004), and radio (OR=0.32, P < .001). Among urban residents, health literacy was not associated with access to health information from newspapers (OR=1.21, P = .566), magazines (OR=0.81, P = .511), books (OR=0.87, P = .674), scientific literature (OR=0.87, P = .643), television (OR=1.39, P = .368), or radio (OR=0.89, P = .701). As shown in Figure 3, fewer than half of the rural residents with limited health literacy had access to health information from newspapers, magazines, the scientific literature, and radio. Many (between 68% and 78%) rural residents with adequate health literacy and urban residents (regardless of their health literacy level) had access to health information from these mass media sources. We observed the same patterns and significant results when adjusting for race/ethnicity, income, and education. Results from the relative excess risk due to interaction (RERI) indicated that there were significant multiplicative interactions but no significant additive interactions.
Figure 3.
Access to Newspapers, Magazines, Books, and Scientific Literature among Rural-Urban Residents with Adequate/Limited Health Literacy
We also found an interaction between health literacy and rural-urban residence for use of “other companies or corporations” (companies or corporations other than pharmaceutical companies) for health information (interaction P = .010). Among rural residents, having limited health literacy was associated with higher odds of using health information from “other companies or corporations” (OR=8.22, P < .001). Among urban residents, health literacy was not associated with using this source for health information (OR=0.73, P = .686). Nearly one-third of rural residents with limited health literacy used companies or corporations other than pharmaceutical companies for health information; however, only a small portion (6% to 8%) of rural residents with adequate health literacy and urban residents used this source. Again, we observed the same pattern and significant results when adding race/ethnicity, income, and education as covariates. Results from RERI also indicated that there was significant multiplicative interaction but no significant additive interaction.
Discussion
This study examined the differences between US rural and urban residents’ access to and use of health information from 25 sources and the degree to which health literacy exacerbated these differences. Our study contributes to the current literature by investigating the rural-urban differences in health information access and use across a wide range of sources, including from specific types of online health information sources (eg, medical websites and social media) and more traditional sources (eg, physicians, health fairs). We found that compared to urban residents, rural residents had lower access to several health information sources: primary care providers, specialist doctors, dentists, religious organizations and leaders, federal government organizations, scientists, blogs or celebrity webpages, magazines, and radio. They also had lower use of search engines for health information compared to urban residents.
After adjusting for race/ethnicity, income, and education, rural residents still had lower access to health information from specialist doctors than urban residents. Such a difference may stem from the shortages in specialist health care providers in rural areas in the US.20 Access to specialists may also be constrained by lower health care coverage and lack of access to transportation among rural residents compared to urban residents.20,45 Patients in rural areas travel 2 to 3 times farther to visit specialists than those living in urban areas.46 Thus, rural residents may have reduced opportunities to ask for or be provided with health information from specialists. Holding race/ethnicity, income, and education constant rendered the differences in access non-significant except for specialist doctors. Our results indicate that race/ethnicity, income, and education are likely explanations for why rural-urban differences are observed. Individuals with lower incomes, those with less education, and those of minority race/ethnicity have less access to health information from a variety of sources.47,48 These socioeconomic factors characterize many rural areas.49 Thus, rural residents experience disparities in health information access that may ultimately be contributing to health disparities.
We found that rural residents with limited health literacy had lower access to mass media and scientific literature compared to rural residents with adequate health literacy, but there was no such relationship for urban residents. Compared to urban areas, rural areas have lower levels of media coverage of health information because mass media in rural areas may not have as many resources as urban areas have to conduct in-depth health reporting or purchase wire stories.49,50 Such shortages of health information coverage in rural areas might cause extra challenges for rural residents who have limited health literacy to seek easy-to-understand health information.
We also found that rural residents with limited health literacy had a higher likelihood of using companies or corporations other than pharmaceutical companies for health information, but there was no such relationship for urban residents. Studies show that some health information from for-profit corporations/companies can be misleading because the messages were created for advertising purposes.51,52 Urban residents historically have a negative impression of health information from corporations such as tobacco and fast food markets because these corporations have been criticized for creating misleading health information to encourage unhealthy behaviors to maximize profitability.53 In addition, people with limited health literacy can have relatively more difficulty evaluating and differentiating accurate health information sources from inaccurate ones.54 Thus, negative impressions and difficulty evaluating information should be explored in future research as possible explanations for higher rates of using companies or corporations as a source for health information among rural residents with limited health literacy.
Implications
We found no rural-urban differences in using primary care providers and family for health information. The majority (more than three-quarters) of our sample used these 2 sources for health information regardless of their rurality status. Also, rural residents were slightly more likely to turn to nurses and local health departments for information compared to urban residents. Previous studies also reported that compared to urban residents, people in rural areas were more likely to rely on nurse practitioners as a usual source of care.55 Therefore, nurses, primary care providers, family members, and local health departments are effective health information sources to disseminate health education and campaign messages targeting rural populations. The Federal Office of Rural Health Policy encourages collaborations among rural health care providers and organizations to establish rural health networks and promote health care access in rural areas.56
Rural residents nevertheless have lower access to and use of several common sources including primary care providers and specialist doctors. Telemedicine, which uses interactive audio-visual tools so the usual face-to-face communication between physician and patient is not required,57 could be used to improve access to and use of health information from health professionals in rural areas.58,59 Health professionals could develop interventions that target rural residents with limited health literacy to enhance their ability to evaluate the quality of health information, especially information from for-profit companies.24 In newspapers and magazines, rural residents would also benefit from tailored health news, eliminating medical terms, and adding figures and pictures to help them understand the health information.60,61 In addition, a lack of statistical significance does not necessarily mean a lack of clinical or practical significance.62 The odds ratios exhibited clear trends that rural residents had lower access and use of various credible health information sources (eg, health professionals) compared to urban residents. Health professionals and policy makers should recognize this issue.
Limitations
The cross-sectional design of our study hinders the ability to infer causal relationships. Our classification of information health sources into categories was exploratory. These groups might not be mutually exclusive. For example, mass media sources such as newspapers and magazines have both printed and digital versions. We did, however, try to capture the most commonly used online sources. We assessed participants’ perceived access instead of objective access barriers. It could be possible that the sources were available, but the participants were not aware of or did not know how to access those sources. In this exploratory study focusing on the patterns of which information sources did versus which did not show rural-urban differences, we did not apply multiple comparisons corrections; there are persuasive arguments that such corrections are less appropriate when conducting exploratory rather than confirmatory analyses.63–66 In addition, although CBSAs are commonly used to classify rural and urban status, other classification methods were available to us such as Rural-Urban Continuum Codes (RUCCs), Urban Influence Codes (UICs), and ZIP Code Tabulation Areas (ZCTAs).67 Different rural-urban classifications could produce different results. We adapted the NVS to measure health literacy because it is an objective assessment that yields reliable and valid scores among global populations across different age and race/ethnicity groups and with various health conditions.34,68 However, health literacy is a multidimensional construct and different measures could produce different results because different measures might assess different health literacy skills.69
Conclusion
This study makes an important contribution to our understanding of the prevalence and patterns in health information access and use among US rural and urban populations. Compared to urban residents, rural residents have lower access to several common sources (eg, primary care providers and specialist doctors) and less use of search engines for health information. Some differences in access and use of health information sources were accounted for by sociodemographic differences between rural and urban populations. There may be structural barriers (eg, shortage of specialist doctors and limited media exposure) that make it harder for rural residents to access health information, especially those with limited health literacy.
Acknowledgments
Funding: Funding for the project leading to this manuscript was made possible by R01CA197351 from the National Cancer Institute.
For further information, contact: Xuewei Chen, Department of Community Health and Health Behavior, University at Buffalo, 3435 Main St., Buffalo, NY 14214; xueweich@buffalo.edu
Footnotes
Disclosures: The authors report no conflicts of interest.
References
- 1.Kelley MS, Su D, Britigan DH. Disparities in Health Information Access: Results of a County-Wide Survey and Implications for Health Communication. Health Commun. 2016;31(5):575–582. [DOI] [PubMed] [Google Scholar]
- 2.Eng TR, Maxfield A, Patrick K, Deering MJ, Ratzan SC, Gustafson DH. Access to health information and support: a public highway or a private road? JAMA. 1998;280(15):1371–1375. [DOI] [PubMed] [Google Scholar]
- 3.Suka M, Odajima T, Okamoto M, et al. Relationship between health literacy, health information access, health behavior, and health status in Japanese people. Patient education and counseling. 2015;98(5):660–668. [DOI] [PubMed] [Google Scholar]
- 4.McIlhenny C, Guzic B, Knee D, Demuth B, Roberts J. Using technology to deliver healthcare education to rural patients. Rural & Remote Health. 2011;11(4). www.rrh.org.au/journal/article/1798. Accessed October 24, 2018. [PubMed] [Google Scholar]
- 5.Census Bureau US. New census data show differences between urban and rural populations.Washington, DC: U.S. Census Bureau; 2016. https://www.census.gov/newsroom/press-releases/2016/cb16-210.html. Accessed April 20, 2018. [Google Scholar]
- 6.Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. J Urban Health. 2014;91(2):272–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meit M, Knudson A, Gilbert T, et al. The 2014 update of the rural-urban chartbook. Bethesda, MD: Rural Health Reform Policy Research Center; 2014. [Google Scholar]
- 8.Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the Case for Investment in Rural Cancer Control: An Analysis of Rural Cancer Incidence, Mortality, and Funding Trends. Cancer Epidemiology Biomarkers & Prevention. 2017;26(7):992–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh GK, Daus GP, Allender M, et al. Social Determinants of Health in the United States: Addressing Major Health Inequality Trends for the Nation, 1935–2016. Int J MCH AIDS. 2017;6(2):139–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zahnd WE, James AS, Jenkins WD, et al. Rural-Urban Differences in Cancer Incidence and Trends in the United States. Cancer Epidemiol Biomarkers Prev. 2017. July 27. doi: 10.1158/1055-9965.EPI-17-0430. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doescher MP, Jackson JE. Trends in Cervical and Breast Cancer Screening Practices Among Women in Rural and Urban Areas of the United States. Journal of Public Health Management and Practice. 2009;15(3):200–209. [DOI] [PubMed] [Google Scholar]
- 12.Cole AM, Jackson JE, Doescher M. Urban-rural disparities in colorectal cancer screening: cross-sectional analysis of 1998–2005 data from the Centers for Disease Control’s Behavioral Risk Factor Surveillance Study. Cancer Med. 2012;1(3):350–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen X, Cisse-Egbuonye N, Spears EC, Mkuu R, McKyer ELJ. Children’s healthy eating habits and parents’ socio-demographic characteristics in rural Texas, USA. Health Education Journal. 2018:0017896917752014. [Google Scholar]
- 14.Wilcox S, Castro C, King AC, Housemann R, Brownson RC. Determinants of leisure time physical activity in rural compared with urban older and ethnically diverse women in the United States. Journal of Epidemiology and Community Health. 2000;54(9):667–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tichenor PJ, Donohue GA, Olien CN. Mass media flow and differential growth in knowledge. Public opinion quarterly. 1970;34(2):159–170. [Google Scholar]
- 16.Viswanath K, Finnegan JR Jr. The knowledge gap hypothesis: Twenty-five years later. Annals of the International Communication Association. 1996;19(1):187–228. [Google Scholar]
- 17.Kiviniemi MT, Orom H, Waters EA, McKillip M, Hay JL. Education-based disparities in knowledge of novel health risks: The case of knowledge gaps in HIV risk perceptions. British journal of health psychology. 2018;23(2):420–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lustria ML, Smith SA, Hinnant CC. Exploring digital divides: an examination of eHealth technology use in health information seeking, communication and personal health information management in the USA. Health Informatics J. 2011;17(3):224–243. [DOI] [PubMed] [Google Scholar]
- 19.Greenberg AJ, Haney D, Blake KD, Moser RP, Hesse BW. Differences in access to and use of electronic personal health information between rural and urban residents in the United States. J Rural Health. 2018;34(S1):s30–s38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–620. [DOI] [PubMed] [Google Scholar]
- 21.Learmonth YC, Adamson BC, Balto JM, et al. Multiple sclerosis patients need and want information on exercise promotion from healthcare providers: a qualitative study. Health Expect. 2017;20(4):574–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jacobs W, Amuta AO, Jeon KC. Health information seeking in the digital age: An analysis of health information seeking behavior among US adults. Cogent Social Sciences. 2017;3(1):1302785. [Google Scholar]
- 23.Xie B, Su Z, Liu Y, Wang M, Zhang M. Health information sources for different types of information used by Chinese patients with cancer and their family caregivers. Health Expectations. 2017;20(4):665–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen X, Hay JL, Waters EA, et al. Health Literacy and Use and Trust in Health Information. Journal of Health Communication. 2018:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. [DOI] [PubMed] [Google Scholar]
- 26.Neter E, Brainin E. eHealth literacy: extending the digital divide to the realm of health information. J Med Internet Res. 2012;14(1):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kandula NR, Nsiah-Kumi PA, Makoul G, et al. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient education and counseling. 2009;75(3):321–327. [DOI] [PubMed] [Google Scholar]
- 28.Zahnd WE, Scaife SL, Francis ML. Health Literacy Skills in Rural and Urban Populations. American Journal of Health Behavior. 2009;33(5):550–557. [DOI] [PubMed] [Google Scholar]
- 29.Korn EL, Graubard BI. Analysis of Health Surveys. Hoboken, NJ: John Wiley & Sons Inc.; 2011. [Google Scholar]
- 30.U.S. Census Bureau. Metropolitan and Micropolitan 2010. Washington, DC: U.S. Census Bureau; https://www.census.gov/programs-surveys/metro-micro/about.html. Accessed April 20, 2018. [Google Scholar]
- 31.National Cancer Institute. Health Information National Trends Survey (HINTS). Bethesda, MD: NCI; 2017. https://hints.cancer.gov/data/survey-instruments.aspx. Accessed April 20, 2018. [Google Scholar]
- 32.Livingston G, Minushkin S, Cohn D. Sources of information on health and health care In: Hispanics and Health Care in the United States: Access, Information and Knowledge, Chapter IV. Washington, DC: Pew Research Center; 2008. http://www.pewhispanic.org/2008/08/13/iv-sources-of-information-on-health-and-health-care/. Accessed April 20, 2018. [Google Scholar]
- 33.Fox S, Duggan M. Part two: Sources of health information In: The Diagnoses Difference. Washington, DC: Pew Research Center; 2013. http://www.pewinternet.org/2013/11/26/part-two-sources-of-health-information/. Accessed April 20, 2018. [Google Scholar]
- 34.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: The newest vital sign. Annals of Family Medicine. 2005;3(6):514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Protheroe J, Whittle R, Bartlam B, Estacio EV, Clark L, Kurth J. Health literacy, associated lifestyle and demographic factors in adult population of an English city: a cross-sectional survey. Health Expect. 2017;20(1):112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Griffey RT, Melson AT, Lin MJ, Carpenter CR, Goodman MS, Kaphingst KA. Does numeracy correlate with measures of health literacy in the emergency department? Academic Emergency Medicine. 2014;21(2):147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hudon C, Fortin M, Poitras M-E, Almirall J. The relationship between literacy and multimorbidity in a primary care setting. BMC family practice. 2012;13(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ghaddar SF, Valerio MA, Garcia CM, Hansen L. Adolescent health literacy: the importance of credible sources for online health information. J Sch Health. 2012;82(1):28–36. [DOI] [PubMed] [Google Scholar]
- 39.U.S. Census Bureau. Current Population Survey (CPS). Washington, DC: U.S. Census Bureau; 2017. https://www.census.gov/programs-surveys/cps.html. Accessed April 20, 2018. [Google Scholar]
- 40.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8(6):621–628. [PubMed] [Google Scholar]
- 41.Osborne JW. The advantages of hierarchical linear modeling ERIC/AE Digest. College Park, MD: ERIC Clearinghouse on Assessment and Evaluation; 2000. [Google Scholar]
- 42.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology, 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 43.Hosmer DW, Lemeshow S. Confidence interval estimation of interaction. Epidemiology. 1992;3(5):452–456. [DOI] [PubMed] [Google Scholar]
- 44.Andersson T, Alfredsson L, Kallberg H, Zdravkovic S, Ahlbom A. Calculating measures of biological interaction. Eur J Epidemiol. 2005;20(7):575–579. [DOI] [PubMed] [Google Scholar]
- 45.Anderson TJ, Saman DM, Lipsky MS, Lutfiyya MN. A cross-sectional study on health differences between rural and non-rural US counties using the County Health Rankings. Bmc Health Services Research. 2015;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chan L, Hart LG, Goodman DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health. 2006;22(2):140–146. [DOI] [PubMed] [Google Scholar]
- 47.Manierre M Examining the relationship between flexible resources and health information channel selection. Health communication. 2016;31(1):22–34. [DOI] [PubMed] [Google Scholar]
- 48.Viswanath K, Ackerson LK. Race, ethnicity, language, social class, and health communication inequalities: a nationally-representative cross-sectional study. PLoS One. 2011;6(1):e14550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ramirez AS, Estrada E, Ruiz A. Mapping the Health Information Landscape in a Rural, Culturally Diverse Region: Implications for Interventions to Reduce Information Inequality. J Prim Prev. 2017;38(4):345–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Krieger JL, Katz ML, Eisenberg D, Heaner S, Sarge M, Jain P. Media coverage of cervical cancer and the HPV vaccine: implications for geographic health inequities. Health Expect. 2013;16(3):e1–e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Strasser AA, Tang KZ, Tuller MD, Cappella JN. PREP advertisement features affect smokers’ beliefs regarding potential harm. Tobacco control. 2008;17(Suppl 1):i32–i38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Niemiec E, Borry P, Pinxten W, Howard HC. Content Analysis of Informed Consent for Whole Genome Sequencing Offered by Direct-to-Consumer Genetic Testing Companies. Hum Mutat. 2016;37(12):1248–1256. [DOI] [PubMed] [Google Scholar]
- 53.Freudenberg N, Galea S. Cities of consumption: the impact of corporate practices on the health of urban populations. J Urban Health. 2008;85(4):462–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Diviani N, van den Putte B, Giani S, van Weert JC. Low health literacy and evaluation of online health information: a systematic review of the literature. J Med Internet Res. 2015;17(5):e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Everett CM, Schumacher JR, Wright A, Smith MA. Physician assistants and nurse practitioners as a usual source of care. J Rural Health. 2009;25(4):407–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Manning L Rural health networks: adapting to a changing health care environment. J Rural Health. 2014;30(3):333–334. [DOI] [PubMed] [Google Scholar]
- 57.Sood S, Mbarika V, Jugoo S, et al. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemedicine and e-Health. 2007;13(5):573–590. [DOI] [PubMed] [Google Scholar]
- 58.Heath B, Salerno R, Hopkins A, Hertzig J, Caputo M. Pediatric critical care telemedicine in rural underserved emergency departments. Pediatr Crit Care Med. 2009;10(5):588–591. [DOI] [PubMed] [Google Scholar]
- 59.Raza T, Joshi M, Schapira RM, Agha Z. Pulmonary telemedicine--a model to access the subspecialist services in underserved rural areas. Int J Med Inform. 2009;78(1):53–59. [DOI] [PubMed] [Google Scholar]
- 60.Young R, Willis E, Stemmle J, Rodgers S. Localized Health News Releases and Community Newspapers: A Method for Rural Health Promotion. Health Promotion Practice. 2015;16(4):492–500. [DOI] [PubMed] [Google Scholar]
- 61.Len-Ríos ME, Hinnant A. Health literacy and numeracy: A comparison of magazine health messages. Howard Journal of Communications. 2014;25(3):235–256. [Google Scholar]
- 62.Page P Beyond statistical significance: clinical interpretation of rehabilitation research literature. Int J Sports Phys Ther. 2014;9(5):726–736. [PMC free article] [PubMed] [Google Scholar]
- 63.Vasilopoulos T, Morey TE, Dhatariya K, Rice MJ. Limitations of significance testing in clinical research: a review of multiple comparison corrections and effect size calculations with correlated measures. Anesthesia & Analgesia. 2016;122(3):825–830. [DOI] [PubMed] [Google Scholar]
- 64.Bender R, Lange S. Adjusting for multiple testing—when and how? Journal of clinical epidemiology. 2001;54(4):343–349. [DOI] [PubMed] [Google Scholar]
- 65.Feise RJ. Do multiple outcome measures require p-value adjustment? BMC medical research methodology. 2002;2(1):8 10.1186/1471-2288-2-8. Accessed October 24, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Perneger TV. What’s wrong with Bonferroni adjustments. BMJ. 1998;316(7139):1236–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. J Urban Health. 2006;83(2):162–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shealy KM, Threatt TB. Utilization of the Newest Vital Sign (NVS) in Practice in the United States. Health Commun. 2016;31(6):679–687. [DOI] [PubMed] [Google Scholar]
- 69.Haun JN, Valerio MA, McCormack LA, Sorensen K, Paasche-Orlow MK. Health literacy measurement: an inventory and descriptive summary of 51 instruments. J Health Commun. 2014;19(Suppl 2):302–333. [DOI] [PubMed] [Google Scholar]