Abstract
Background and Objectives
Obesity is increasing among people residing in nursing homes, and resident obesity substantially affects services needed, equipment and facilities provided, and morbidity in this setting. The purpose of this article is to describe the scope and depth of evidence regarding the impact of obesity among nursing home residents in the United States.
Research Design and Methods
A systematic literature review was performed in PubMed, EMBASE, CINAHL, and Web of Science databases as well as additional hand-searched documents. Included articles were published from 1997 to March 2017. The characteristics and content of the included articles were systematically reviewed and reported.
Results
Twenty-eight studies met inclusion criteria for review. The median study size was 636 residents (interquartile range 40–11,248); 18 (64%) studies were retrospective and 10 (36%) were prospective in nature. Ten (36%) studies examined medical and functional morbidity, 10 (36%) examined health system effects, and 5 (18%) examined the risk of admission to nursing homes. Most studies found that obesity poses serious issues to resident health and the provision of health care, as well as broad health system and nursing challenges in the provision of high-quality nursing home care and services.
Discussion and Implications
Although obesity affects about one in four nursing home residents in the United States, relatively limited evidence exists on the complex challenges of obesity for their residents and their care. A continued focus on resident quality of life, health system improvement, and nursing best practices for properly caring for individuals with obesity is needed.
Keywords: Access to and utilization of services, Disparities (health, racial), Healthcare policy, Nursing home, Obesity
Background and Objectives
Obesity and its related medical conditions increase the difficulty for formal and informal caregivers in providing medical, nursing, and custodial care. For instance, obesity makes medical exams less informative, and obesity increases the physical demand of assisting a disabled individual with mobility. As the prevalence of obesity increases across the world and people with obesity live into old age, the challenges associated with care for people with obesity and disability will increase globally. Nursing homes, which specialize in care for people with disabilities and serious illness, may well be where the burden of obesity care and the increase in obesity rates will be most apparent in the health care system for seniors. Nursing homes will therefore be a key area of health care to understand the wide-ranging effects of obesity on health and aging. Using a systematic search of the literature on obesity in nursing homes in the United States, the present study identifies, describes, and synthesizes research in this area.
Obesity in adults is generally defined as a body mass index (BMI) of 30 kg/m2 or greater by the World Health Organization (WHO). As people with obesity make up a greater proportion of the elderly and disabled population, they also constitute an increased proportion of the nursing home population. In a sample of U.S. nursing home residents from 2000 to 2008, the rate of obesity increased from 17% to 26% (Cai, Rahman, & Intrator, 2013). Many of these residents have moderate (BMI 35–39.9 kg/m2) to severe (BMI ≥ 40 kg/m2) levels of obesity; rates of moderate to severe obesity increased from 7% to 12% during the same period. This dramatic demographic shift is leading to growing demands for obesity-specific medical, nursing, and custodial services for these residents.
No recent systematic review on this topic has been published and the literature in this area is expanding. The objective of this systematic review is to examine the scope of existing literature on the effect of obesity on nursing home residents, nursing home services provided, and nursing home systems in the United States. The methods and key findings of these studies as well as gaps in the current knowledge are identified and discussed.
Research Design and Methods
A complete search of the literature on obesity in nursing homes and a review of key findings were performed. This was conducted using systematic search principles from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, Guidelines for Meta-Analyses and Systematic Reviews of Observational Studies, and the recommendations for scoping reviews from (Arksey & O’Malley, 2005; Grant & Booth, 2009; Popay et al., 2006).
Study Identification
Studies were identified using controlled vocabulary and keywords in PubMed, Embase, CINAHL (Cumulative Index to Nursing and Allied Health Literature), and Web of Science. The search strategy included vocabulary or keywords like “obesity” and “long-term care” including “nursing home,” “assisted living,” “adult day,” “home health,” and “hospice care” present in the title of the manuscript or abstract. Complete details of the search strategies are noted in the Supplementary Appendix Table 1. We included all prospective or retrospectives studies as well as previous reviews, commentary, and editorials.
PubMed (January 1966 to April 2017), EMBASE (January 1980 to April 2017), CINAHL (September 1981 to April 2017), and Web of Science (January 1900 to April 2017) databases were searched using the preassigned search terms. Additionally, the references of each study were examined (i.e., “snowball search”) and studies that met inclusion criteria were included in the initial set of studies screened for possible for inclusion.
Screening and Data Extraction
All articles and abstracts were examined to see if they met inclusion and exclusion criteria. The inclusion criteria for the first screening were: the study included a population that was in a nursing home in the United States where a measure of obesity or body size was used as a predictor. Then, the full article was reviewed and a second screening was performed to identify additional information and ensure that the study met the inclusion criteria. Information was abstracted from each study including study objective, design, participants, covariates, outcomes, and statistical methods.
Collation, Summarizing, and Synthesis
Tables were created to summarize study characteristics including study design, sample size, outcome type, and obesity classification definitions. Additionally, international and long-term care studies not within nursing homes were summarized and synthesized for presentation in the appendix as related content.
Results
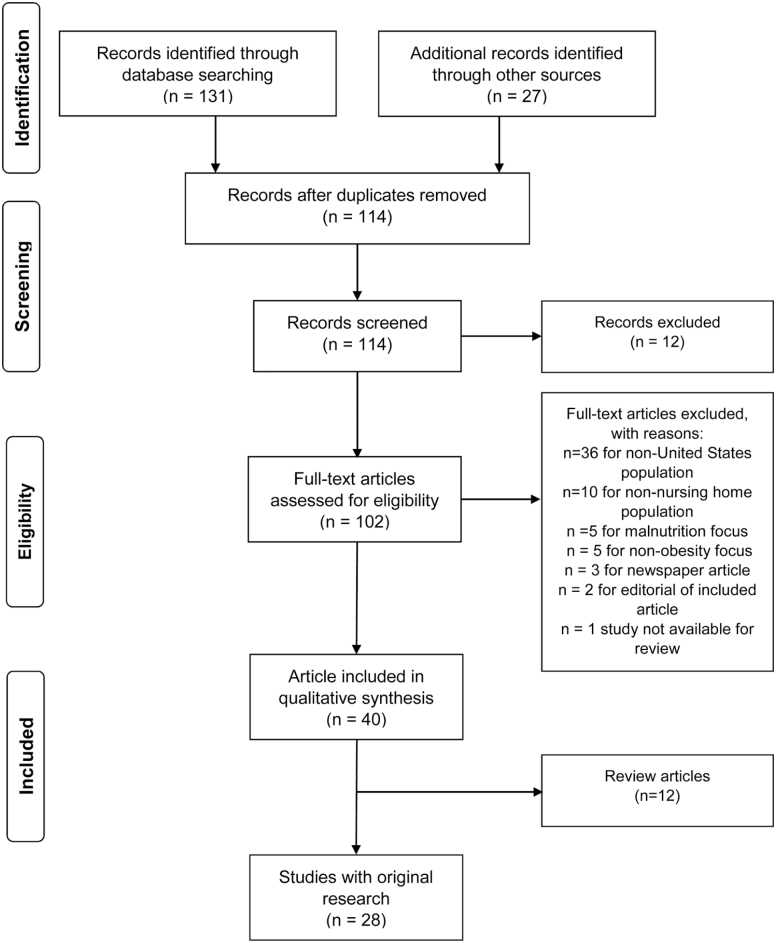
Of 158 manuscripts and abstracts identified in the full search of four databases and reference citation “snowball” searching, 40 articles met the criteria used, and 28 of those articles represented original research (see Figure 1). For the full list of included studies, see Supplementary Appendix Tables 1 and 2.
Figure 1.
PRISMA flow diagram.
Study Design
The most common study design was a cohort study (14/28, 50%), followed by cross-sectional (9/28, 32%), case study (4/28, 14%), and a single (1/28, 4%) simulation study. Most studies used a retrospective study design (64% 18/28) (see Table 1).
Table 1.
Study Long-term Care Population and Number, Type, and Location of Studiesa
| Study design | Number of studies | Types of study outcomes (number of studies) | Prospective, retrospective design (number of studies) |
|---|---|---|---|
| Cohort | 14 | Comorbid medical and functional conditions (7), Costs (1), Health System effects (3), Mortality (1), Risk of admission to long-term care (5) | Prospective (5), Retrospective (9) |
| Cross-sectional | 9 | Comorbid medical and functional conditions (3), Costs (1), Health System effects (4), Nursing Practices (1), | Prospective (4), Retrospective (5) |
| Case study | 4 | Costs (2), Health System effects (1), Nursing Practices (2), | Retrospective (4) |
| Simulation | 1 | Health System effects (1) | Prospective (1) |
Note: aCounts include studies examining multiple outcomes as counted in both groups.
Study Sizes
The size of studies varied from 2,295,647 residents with data from the U.S. Minimum Data Set to 1 resident in a case report. The median study size was 636 residents (interquartile range 40–11,248).
Outcomes Types
Studies examining obesity in nursing homes were broadly classified into those examining the effect of obesity on health systems (10/28, 36%), comorbid medical conditions (10/28, 36%), risk of admission to nursing homes (5/28, 18%), costs (4/28, 14%), nursing practices (3/28, 11%), and mortality (1/28, 3%) (see Table 2).
Table 2.
Study Outcome Types and Outcome Measuresa
| Type of study outcome (number of studies) | Specific outcome measures |
|---|---|
| Comorbid medical and functional conditions (10) | ADL impairments, allergies, anemia, arthritis, asthma, bladder incontinence, cancer, cardiovascular disease, cognitive impairment, chronic obstructive pulmonary disease, congestive heart failure, dementia, depression, diabetes, falls, fecal incontinence, fractures, hypertension, pressure ulcers, stroke |
| Costs (4) | Medicaid long-term care costs, costs related to increased nursing care, nursing home administrators’ perception of patient finances as a barrier to admission |
| Health System effects (10) | Prevalence of obesity in nursing homes, staffing in nursing homes, nursing home deficiency citations, hospital admissions, barriers to placement in long-term care from acute care, nurse administrator perceptions of adequate staffing and equipment |
| Mortality (1) | Odds ratio of death |
| Nursing Practices (3) | Qualitative themes from nurses and nurse aids, Minutes for nurse to perform caretaking task |
| Risk of admission to long- term care (5) | Age-adjusted rates of nursing home admission, hazard ratio of admission |
Note: ADL = Activities of daily living.
aCounts include studies examine multiple outcome types as counted in both groups.
A wide range of related outcomes were examined within each of these groups of studies. The primary outcomes of studies on comorbid medical conditions for residents with obesity in nursing homes included diabetes, hypertension, congestive heart failure, chronic obstructive pulmonary disease, depression, cognitive impairment, urinary incontinence, sarcopenia, and functional status.
The primary outcomes of studies of costs were extra costs associated with nursing care or equipment (Felix et al., 2010) or the cost of additional long-term care home days (Yang & Zhang, 2014). The primary outcomes of studies of health system effects included additional long-term care days (Yang & Zhang, 2014), the increasing prevalence of obesity in nursing homes (Felix, Bradway, Chisholm, Pradhan, & Weech-Maldonado, 2015; Lapane & Resnik, 2005), nursing home characteristics associated with increased prevalence of obesity (Zhang, Li, & Temkin-Greener, 2013), and utilization of long-term care days (Yang & Zhang, 2014).
The primary outcomes for the study of mortality were the odds ratio of death over the study period (Grabowski, Campbell, & Ellis, 2005). The primary outcomes for studies of nursing and custodial issues included feelings and beliefs of nurses and nurse aids about providing care for obese residents (Bradway, Miller, Heivly, & Fleshner, 2010; Gallagher, 1998), and opinions provided by nursing home administrators (Felix, Bradway, Ali, & Li, 2016; Miles et al., 2012).
The primary outcome of studies examining the effect of obesity on future utilization of nursing home care was the odds of nursing home admission among a cohort of community-dwelling individuals (Buys et al., 2014; Elkins et al., 2006; Zizza et al., 2003; Zizza, Herring, Stevens, & Popkin, 2002). A summary of findings from each study by outcome group is presented in Tables 3–5.
Table 3.
Studies on Health System Impact of Long-term Care for People With Obesity
| Author (year) | Sample size | Summary findings (statistically significant unless noted) |
|---|---|---|
| Bradway et al. (2009) | 1 (case report) | Nursing home system tried to improve care for morbidly obese through injury reduction program, competency-based education/training, proper equipment, redesign of physical environment, appropriate staffing, an interdisciplinary care model. |
| Bradway et al. (2017) | 97 discharge planners | Respondents perceiving nursing homes to have equipment concerns were 7 times more likely to report resident size as a barrier to admission. |
| Cai et al. (2013) | 22,17,961 residents | The odds of pressure ulcers were 18.9% higher for residents with moderate or severe obesity when nursing assistant staffing was in bottom quartile compared to 12.8% higher for residents when nursing assistant staffing was top quartile |
| Felix et al. (2015) | 10,538 nursing homes | Prevalence of moderate to severe obesity in U.S. nursing homes has increased from 14.7% to 23.9% from 2000 to 2010. |
| Felix et al. (2016) | 360 Nursing home administrators | 66% of respondents reported the size of morbidly obese residents was a barrier to admission to nursing home. |
| Lapane & Resnik (2005) | 22,95,647 residents | Prevalence of obesity among nursing home residents in five U.S. states increased from 15% to 25% from 1992 to 2002. |
| Miles et al. (2012) | 183 home health and nursing home administrators | 81% of nursing home and 34% and home health administrators reported special equipment as being a barrier to transitioning from acute care for morbidly obese residents. |
| Yang & Zhang (2014) | Not applicable (simulation) | Obesity and related diseases will lead to estimated 1.3 billion long-term care resident days for baby boomer generation. |
| Zhang et al. (2016) | 636 nursing homes | Residents with morbid obesity were admitted to nursing homes with four times the number deficiencies. |
| Zhang et al. (2013) | 636 nursing homes | For each 0.1 increase in staffing ratio, average obesity prevalence in nursing homes increased 4%. Presence of severe deficiencies was associated with an increase in average obesity prevalence in nursing homes of 8%. |
Table 5.
Studies on Mortality and Morbidity of Long-term Care for People With Obesity
| Author (year) | Sample size | Summary findings (statistically significant unless noted) |
|---|---|---|
| Mortality | ||
| Grabowski et al. (2005) | 5,899 | BMI > 28 was had an odds ratio of death of 0.75 compared to normal weight individuals. |
| Morbidity | ||
| Battisti et al. (2014) | Unknown | In first year of residence in a nursing home, the mean body weight increased 8.4 lbs. |
| Cai et al. (2013) | 22,17,961 | Individuals with BMI ≥ 30 had odds ratio of having a pressure ulcer of 1.16 compared to BMI 18.5–29.9. |
| Felix (2008) | 47,932 | Individuals with BMI ≥ 30 had odds ratio of having needing extensive assistance of 1.18 to 1.70 compared to BMI < 30. |
| Felix et al. (2013) | 3,879 | Individuals with BMI ≥ 35 did not have an increased risk for indwelling urinary catheter use compared to individuals with a normal weight. |
| Grabowski et al. (2005) | 5,899 | Individuals with BMI > 28 were less likely to have ADL impairments (4.1 vs 4.5) and more likely to have diabetes (26% vs 18%) compared to individuals with a normal weight. |
| Johnson, Hasse, & Shumaker (1997) | Unknown | Residents with obesity had higher prevalence of congestive heart failure, depression, and COPD. |
| Johnson et al. (1997) | 58 | 22% of obese residents lose ≥10% of admission weight in 1st year of NH stay, 44% lose ≥10% of admission weight by 4th year of NH stay. |
| Millson et al. (2010) | 21 | Diabetic residents were more likely to have a high BMI than non-diabetic residents. |
| Ventura Marra et al. (2016) | 247 | Increasing BMI was associated with increased serum osmolality and great fluid intake deficit. |
| Zarowitz et al. (2014) | 229283 | 41% of nursing home residents with diabetes are obese. |
Note: ADL = Activities of daily living; BMI = Body mass index; COPD = Chronic obstructive pulmonary disease.
Table 4.
Studies on Future Risk of Admission, Costs, and Nursing Care for Long-term Care for People With Obesity
| Author (year) | Sample size | Summary findings (statistically significant unless noted) |
|---|---|---|
| Future risk of admission | ||
| Buys et al. (2014) | 978 respondents | Obesity in elderly was not associated with increased risk of future nursing home admission. |
| Elkins et al. (2006) | 8,804 respondents | Obesity in midlife was is associated with hazard ratio of 1.3 of future nursing home admission. |
| Valiyeva et al. (2006) | 3,526 respondents | Obesity with concurrent hypertension in elderly is associated with hazard ratio of 1.68 of future nursing home admission. |
| Zizza et al. (2002) | 5,960 respondents | Obesity in midlife was associated with hazard ratio of 1.31 of future nursing home admission. |
| Zizza et al. (2003) | 3,742 respondents | Large average annual weight gain over time in people who had BMI ≥ 25 kg/m2 was associated with hazard ratio of 2.13 of future nursing home admission. |
| Costs | ||
| Felix et al (2016) | 360 residents | 30% of nursing home administrators reported the resident’s finances always or often act as an admission barrier for morbidly obese residents. |
| Felix et al. (2010) | 1 (case report) | Average U.S. nursing home total nursing home labor costs for bathing obese residents were $40 thousand U.S. dollars more than if residents were normal weight. |
| Powell et al. (2010) | 1 (case report) | Bathing costs alone for morbidly obese nursing home residents increase the total costs of care 3%. |
| Yang & Zhang (2014) | Not applicable (simulation) | Obesity and related diseases will lead to estimated $68 billion U.S. dollars in Medicaid long-term care costs for baby boomer generation. |
| Nursing Care | ||
| Bradway et al. (2010) | 5 residents, 8 nursing staff | Morbid obesity and incontinence makes it hard to provide good care because inadequate physical space to provider nursing care and strenuous nature of nursing tasks. |
| Felix et al. (2010) | 1 (case report) | Bathing of one morbidly obese resident took a total of 105 minutes of staff time for 2 nurse assistants. |
| Rotkoff (1999) | 1 (case report) | Limitations of providing standard care due to staffing, equipment and nursing home constraints. |
Obesity Classifications
Among the included studies, obesity was most frequently measured by BMI, using NIH criteria, which was most often defined as underweight (BMI < 18.5 kg/m2), healthy weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), obese (BMI ≥ 30 kg/m2) or defined by WHO cutoff points as underweight (BMI < 18.5 mg/m2), healthy weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), obesity Class I (BMI 30–34.9), obesity Class II (BMI 35–39.9 kg/m2), obesity Class III (BMI ≥ 40 kg/m2) (see Table 6) (NHLBI Obesity Education Initiative Expert Panel on the Identification Evaluation and Treatment of Obesity in Adults, 1998; WHO Expert Committee, 1995).
Table 6.
Study Definition of Underweight, Normal Weight, and Obesity
| Definitions for underweight (number of studies) | Definitions for normal weight (number of studies) | Definitions for obesity (number of studies) |
|---|---|---|
| <18.5 kg/m2 | 18.5–24.9 kg/m2 | ≥25 kg/m2 |
| <19 kg/m2 | 19–28 kg/m2 | >28 kg/m2 |
| ≥30 kg/m2 | ||
| 30–34.9, 35–39.9, ≥40 kg/m2 | ||
| 30–39.9, ≥40 kg/m2 | ||
| >120% master’s weight standard | ||
| ≥35 kg/m2 | ||
| ≥40 kg/m2 | ||
| >300 lbs | ||
| >325 lbs | ||
| >400 lbs |
Some studies examining the effect of obesity on nursing care used weight-based cutoffs (>300 lbs, >325 lbs, >400 lbs), based on expert opinion as well as a qualitative study that identifies 300 lbs as a cutoff where obesity becomes a serious problem in nursing care (Drake, Dutton, Engelke, McAuliffe, & Rose, 2005).
Studies Outside of U.S. Nursing Homes
While not included as the main subject of this review, we did find 36 studies of non-U.S. nursing home populations in 17 different countries (Germany and Italy were most frequent with six studies each) (see Supplementary Appendix Table 3). A large proportion of these studies were mortality studies, many of which were the subject of a separate meta-analysis (Veronese et al., 2015). There were also nine studies that included long-term care populations that were not nursing homes: home health (4/9) and hospice (3/9) were the most common settings (see Supplementary Appendix Table 4). Twelve review studies, two of which included systematic searches, have examined obesity in nursing home settings (see Supplementary Appendix Table 5). The most recent systematic review of obesity in nursing home settings was in 2008 (Bradway, DiResta, Fleshner, & Polomano, 2008).
Discussion and Implications
This systematic research and review identified 28 articles in the U.S. nursing home literature examining obesity. We focus on the scope of included research content by examining three main areas of research: how obesity affects the individual nursing home resident, nursing home care and experience, and the nursing home system. In this discussion, we synthesize the findings from the systematic review and discuss areas for further examination.
Obesity and the Nursing Home Resident: Nursing Home Admission
Multiple studies found that the presence of obesity earlier in life is a risk factor for needing nursing home care later in life. This is not surprising as obesity has been associated with increased odds of developing functional disabilities as people age. It is reasonable to hypothesize that this disability will lead to use of long-term care services, including nursing home care, to assist with these daily needs. In the studies examined, obesity is associated with increased risk of nursing home admission. Given obesity levels in the general population, obesity rates are likely to increase in nursing homes. However, this relationship is complex, moderated through age, race, gender, and the severity of obesity earlier in life.
In the U.S. National Health and Nutrition Examination Survey Epidemiological Follow-up Survey (NHEFS) as well as the Kaiser Permanente Medical Care Plan, obesity and White race were associated with greater rates of admission to nursing homes, but this relationship was not present among participants of Black race (Elkins et al., 2006; Zizza et al., 2002). Using the NHEFS, age was also found to moderate this association; adults with obesity between the ages of 65 and 74 had greater odds of nursing home admission, while younger people with obesity did not (Valiyeva, Russell, Miller, & Safford, 2006). Using the Medicare Current Beneficiary Survey (MCBS), women with obesity were more likely to be admitted to nursing homes. However, among men, only those with moderate to severe obesity were more likely to being admitted to nursing homes compared to those of normal weight (Yang & Zhang, 2014). There was no association between obesity and nursing home admission in the University of Alabama at Birmingham Study of Aging cohort (Buys et al., 2014). After adjusting for basic demographic factors, social support, and isolation metrics, they did not find any differences in the risk of admission in the future for obese versus nonobese individuals.
Beyond age, race, and gender, the relationship between obesity in mid and late life and future nursing home admission likely also depends on the severity of obesity, the severity of obesity-related disease and functional impairment, social supports, and financial resources. Additionally, these studies on likelihood of future nursing home admission do not account for length of nursing home stays; the distribution of residents with obesity among nursing homes may depend on short-term stays and long-term stays. The risk factors as well as protective factors that mediate the relationship between obesity and nursing home admissions deserve further attention so that policymakers can understand the effect of policies on obesity care and long-term care in the future.
If obesity is associated with an accumulation of disability but the relationship between obesity and nursing home use is mixed, it may mean that obese, disabled individuals may not be receiving nursing home services that normal or underweight individuals are receiving, leading to higher rates of unmet caregiving needs (Ankuda et al., 2017). Additionally, there is evidence of racial disparities in nursing home admissions rates for obese individuals, which may lead to minorities with obesity being less likely to receive assistance for disabilities. We propose that further research examine racial disparities in admission to nursing homes, which may be caused by variation in available services due to differences in local access, social support, cost, and preference.
Obesity and the Nursing Home Resident: Resident Needs and Morbidity
Once in nursing homes, residents with obesity have different medical and functional profiles than normal or underweight residents. Associations between obesity and other diseases, including diabetes and cardiovascular disease, are well-known and these relationships are also generally present among individuals with obesity in nursing homes (Cai et al., 2013; Felix, 2008). Obesity has been associated with increased diagnoses of diabetes, hypertension, arthritis, pressure ulcers, renal failure, indwelling catheter use, and wound infections (Felix, 2008; Felix, Thostenson, Bursac, & Bradway, 2013; Millson, Peters, & Anderson, 2010). Obesity is also associated with lower levels of cancer, pneumonia, hip fracture, cognitive impairment, and incontinence compared to normal or underweight individuals. In some of these case, obesity is likely to be directly causative of the outcome (pressure ulcers or incontinence), but in other cases, obesity is a marker of the absence of underlying chronic disease which lead to cachexia (a general state of ill health involving significant weight loss and muscle loss).
Obesity and the Nursing Home Resident: Mortality
In U.S. nursing home research, there was a single study identified that examined mortality. When examining resident BMI at time of admission, the authors noted obesity (which was defined at BMI > 28 kg/m2) was associated with a lower odds ratio of death compared to underweight residents, and there was no significant difference between the obese and normal weight groups (Grabowski et al., 2005). Severity of obesity did moderate this relationship; individuals with a BMI ≥ 40 kg/m2 had greater mortality compared to normal-weight individuals.
While this appears to suggest a protective effect of obesity, these findings must be set in context. First, increased mortality rates for obese individuals in the community-dwelling population have been described many times (Flegal, Kit, Orpana, & Graubard, 2013; Fontaine, Redden, Wang, Westfall, & Allison, 2003). Second, the relationship between BMI and mortality in the community-dwelling population is not linear and is generally reported as a U- or J- shaped relationship with increased mortality for both underweight and obese individuals (Allison, Faith, Heo, & Kotler, 1997; Flegal, Kit, & Graubard, 2014; Wong et al., 2011). In comparison, this relationship is reversed in nursing homes, with increasing BMI associated with decreased mortality.
The association with increasing BMI and decreasing mortality in nursing homes does not mean that obese individuals in nursing homes are living longer lives. They are admitted to nursing homes younger in life, and though they live in nursing homes longer, when they die they are still younger than normal or underweight peers (Fontaine et al., 2003). Among U.S. nursing home residents from 2000 to 2008, the average age of nonobese, mild obesity, and moderate to severe obesity residents was 80.0, 76.1, and 70.3 years old, respectively (Cai et al., 2013).
Obesity and the Nursing Home Care and Experience
The clinical picture of obese nursing home residents is one of individuals with many chronic medical conditions like diabetes or hypertension compared to normal or underweight residents, however, these obese residents may have higher functional status and less cognitive impairment. We still need to understand how obesity and related medical conditions affect the receipt and quality of care for residents of nursing homes. Researchers have examined how daily nursing and custodial care differs for residents with obesity and how residents’ experiences differ because of their size and weight.
Interview and survey research identified in this systematic review show a theme of inherent nursing challenges of providing care for people with obesity in nursing homes. This research has identified several areas of care that are more complex for people with obesity than for normal or underweight individuals. A study of nursing care for obese nursing home residents with urinary or fecal incontinence identified three themes including (a) the synergistic effect of obesity and incontinence leading to isolation and shame, (b) inadequate physical space in the nursing home to provide toileting and bathing care due to existing small room size, and (c) the demanding but rewarding task of providing dignity to individuals by providing challenging nursing and custodial care (Bradway et al., 2010).
While outside the scope of this systematic review, these issues closely correlate to similar issues concerning increased nursing effort, a more challenging therapeutic relationship, and an absence of necessary equipment and facilities raised in literature about obesity in the acute care setting in the United States and long-term care settings outside the United States (Apelt, Ellert, Kuhlmey, & Garms-Homolová, 2012; Apelt, Fabich, Laurisch, Paul, & Garms-Homolová, 2012; Cienki, 2016; Drake et al., 2005; Rose et al., 2007).
A few studies have attempted to quantitatively measure the increased effort and time needed to provide care for residents with obesity in nursing homes. A case study examining bathing a morbidly obese nursing home resident noted a 105-min time to complete the task versus a historical average of 45 min in a hospital setting (Felix et al., 2010). A case study described the nursing plan for obese residents within a nursing home which includes increased staffing for all morbidly obese residents (Bradway et al., 2009). A survey of nursing home administrators reported inadequate staffing for the care of morbidly obese residents in 31% of nursing homes and reported concerns about having the necessary specialized equipment in 68% of nursing homes (Felix et al., 2016). The staffing implications of longer time needed for care or the need for multiple care providers rather than one highlights the stress to the system caused by increased prevalence of obesity in nursing homes. We need to examine how providers decide to deploy resources to care for obesity residents. For example, how many staff or what equipment, for which residents, leads to the best outcomes for each resident and nursing home.
Obesity causes challenges in providing the equipment, staffing, and social support necessary to provide appropriate and safe nursing and custodial care. Many of these studies touch upon the challenging and difficult experience of nursing providers caring for these residents. Especially in settings where the prevalence of obesity is particularly high, little is known about how obese affects the ability to hire and retain staff to provide care that may be more difficult than in the past. Little is known about how obesity affects satisfaction with care in nursing homes. The nursing challenges described above may well lead to lower resident satisfaction.
While various studies have started to examine these issues from the perspective of nurse aids and nursing home administrators, the voice and experience from the resident perspective is missing. Residents with obesity are perceived to have a lack of motivation and social support, while also having more dependence, depression, anxiety, and shame related to the disease and its effects (Phelan et al., 2015; Puhl & Brownell, 2001; Puhl & Heuer, 2010). No U.S. studies have examined the relationship between obesity and quality of life metrics, including social engagement and satisfaction, in nursing homes.
Obesity and the Nursing Home System: Prevalence and Temporal Trends
Specialized medical, nursing, and custodial care for residents with obesity is needed for hundreds of thousands of nursing home residents each year. At the beginning of this decade, almost a quarter (23.9%) of residents in U.S. nursing homes had moderate to severe obesity, an increase from 14.7% in 2000 (Felix et al., 2015).
The rate of obesity in nursing homes in the United States varies by region (highest in the Midwest and lowest in the West census regions) (Felix et al., 2015). The rate of obesity also varies widely between nursing homes with a range of 0% to 75% of residents in different nursing homes (Felix et al., 2015). In New York State, the mean prevalence of morbid obesity was 5%, but the range among all nursing homes was 0% to 44% (Zhang et al., 2013). In the same study, nursing homes with a higher prevalence of obesity were in more rural areas of the state. The burden of obesity in terms of proportion of nursing home residents is large and is continuing to grow. Furthermore, a wide variation in obesity rates between nursing homes suggests that some nursing homes have a much greater exposure to this population than other nursing homes.
Obesity and the Nursing Home System: Admission Barriers
A growing area of study is to understand the characteristics of nursing homes that have low or high rates of obese residents and to understand what factors lead to high or low quality of care. In the common scenario where an individual receiving acute care is being transferred to a nursing home, there is evidence that this transition may be more difficult for obese individuals (Felix et al., 2016; Miles et al., 2012).
In a survey of nursing home administrators in two states, 66% of respondents said that morbid obesity acts as an admission barrier (Felix et al., 2016). Specifically, the respondents identified the prospective resident’s degree of independence as being a barrier to admission 48% of the time, prospective resident’s finances as always or often being a barrier to admission 30% of the time, and prospective resident’s personal care requirements as being a barrier to admission 18% of the time. A similar incidence of barriers in the transition from acute care to nursing homes was noted in survey of hospital case managers, nursing home directors, and home care administrators (Miles et al., 2012). For a morbidly obese resident in this study, 81% of nursing homes reported lack of necessary equipment as being a barrier to admitting a new resident. The presence of “equipment concerns” at a nursing home was independently associated (p < .01) with reporting morbid obesity as a barrier to admission to a nursing home from a hospital (Bradway, Felix, Whitfield, & Li, 2017).
Due to the perceived challenges of providing appropriate care, these challenges often act as barriers to individuals with obesity entering nursing homes. Little is known about the characteristics of nursing homes that find this care to be especially difficult or what nursing home characteristics make this care efficient and high quality. For example, equipment that may be needed includes larger rooms and bathrooms, bariatric beds, larger therapy tables, and wider walkers and wheelchairs.
Obesity and the Nursing Home System: Quality of Care
The characteristics and outcomes of nursing homes that accept a disproportionate proportion of obese residents may be different from nursing homes that accept smaller proportions of obese residents. In a study of New York State nursing homes, there were significant differences in affiliation (hospital-based or chain-affiliated), occupancy rates, profit status, and staffing levels in nursing homes with obesity rates greater than the median value than for all nursing homes (Zhang et al., 2013). This may be due to need for special equipment, but it may also be due to perceived profit margin related to equipment or staffing necessary for caring for these residents.
Additionally, in the same analysis, obese residents were more likely to be admitted to lower-quality nursing homes, in terms of total and health care-related nursing home deficiencies (Zhang et al., 2016). Staffing rates were independently associated with resident outcomes in a study examining the association of obesity with pressure ulcers; the odds of pressure ulcers were 18.9% higher for residents with moderate or severe obesity than nonobese residents within nursing homes with nurse assistant staffing in the bottom quartile (Cai et al., 2013).
Little is known about the various strategies utilized by different nursing homes to provide care for obese residents. It is unclear how much staffing, what type of staffing, and what organization of staffing may be most helpful to provide high quality care for these obese residents. Additionally, little is known about how many specialized lifts, beds, treatment tables, or wheelchairs are necessary and what benefit they offer.
Finally, the built environment of nursing homes is frequently inadequate to provide the space for residents, staff, and equipment to work together to provide appropriate and sensitive care. The utility of larger resident rooms, treatment areas, and doorways is not well understood. By looking at how the staffing, the built environment, and policies affect resident outcomes such as hospital readmissions, return to community, quality of life, and medical complications, best practice recommendations may be defined and implemented.
Obesity and the Nursing Home System: Cost of Care
Increased equipment and staffing lead to great costs that are passed along to nursing homes and agencies and ultimately to payers including residents and families as well as private and governmental long-term insurance providers. The costs of nursing care, for staffing related to bathing for a single obese resident in a single year, was estimated to be $1670 in 2010 U.S. dollars (Felix et al., 2010). From the perspective of the U.S. Medicaid payer, a simulation study examined the impact of obesity and related disease on total long-term care days and costs for the U.S. baby boomer generation. In this generational cohort, there were an estimated 1.3 billion long-term care days and $68 billion in Medicaid costs (Yang & Zhang, 2014). The costs of increased staffing and specialized equipment when multiplied by millions of individuals receiving long-term care indeed would be a very large cost for an industry that, in the United States, operates on narrow profit margins. Policy proposals to improve care for the obese in nursing homes may need to include new or alternative payment systems for this population, or improved support for alternatives to nursing home care including intensive home health care.
Conclusion
As people with obesity make up a greater proportion of the elderly and disabled population, they are also making up a great proportion of the nursing home population. In a sample of most U.S. nursing home residents from 2000 to 2008, the rate of obesity increased from 17% to 26% (Cai et al., 2013); if this trend continues unabated, by 2025 46% of U.S. nursing home residents will be obese. Even if the increasing obesity rate stabilizes, it is unclear how this increase in the prevalence of obesity will affect care as well as threaten the sustainability of present nursing home care delivery models.
The impact of obesity on nursing homes is great due to the intersection of multiple dynamics. First, obese adults in need of formal and informal care are a growing demographic in an industry that must avoid excess operational capacity and costs. Next, obese individuals will require different services requiring greater staffing and different equipment than normal or underweight residents. The present funding design for long-term care in the United States, is poorly responsive to the special services necessary for the care of people with obesity. Because this care can be detrimental to the business of nursing home providers, there is evidence that adaptation to this need, such as refusal of services, adversely affects the most vulnerable, who most need the help and support.
Like many important questions, provision of nursing home care for people with obesity is at the crossing of two broad trends: an epidemic of obesity in the elderly and the long-term care system in crisis. To improve the care for people with obesity, disability, and serious illness, both issues must be addressed by researchers, policymakers, and society in general.
Funding
This work was supported by the National Institutes of Health (K12HD063087).
Conflict of Interest
None reported.
Supplementary Material
References
- Allison D. B. Faith M. S. Heo M. & Kotler D. P (1997). Hypothesis concerning the U-shaped relation between body mass index and mortality. American Journal of Epidemiology, 146, 339–349. doi:10.1093/oxfordjournals.aje.a009275 [DOI] [PubMed] [Google Scholar]
- Ankuda C. K., Harris J., Ornstein K., Levine D. A., Langa K. M., & Kelley A. S (2017). Caregiving for older adults with obesity in the United States. Journal of the American Geriatrics Society. [Epub ahead of print]. doi:10.1111/jgs.14918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apelt G. Ellert S. Kuhlmey A. & Garms-Homolová V (2012). [Temporal and structural differences in the care of obese and non-obese people in nursing homes]. Pflege, 25, 271–283. doi:10.1024/1012-5302/a000215 [DOI] [PubMed] [Google Scholar]
- Apelt G., Fabich A., Laurisch E., Paul M., & Garms-Homolová V (2012). [A qualitative study on Nurses’ attitudes towards obese clients in long-term care.]. Pflegewissenschaft, 14, 324–333. doi:10.1111/j.1365-2648.2006.03718.x [Google Scholar]
- Arksey H., & O’Malley L (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8, 19–32. doi:10.1080/1364557032000119616 [Google Scholar]
- Battisti H. E., Harrison L., Levine A., Dawson G (2014). Health care policies in long-term care facilities may be contributing to overweight and obesity in the resident. Journal of the Academy of Nutrition and Dietetics, 114(9), A38. [Google Scholar]
- Bradway C. DiResta J. Fleshner I. & Polomano R. C (2008). Obesity in nursing homes: A critical review. Journal of the American Geriatrics Society, 56, 1528–1535. doi:10.1111/j.1532-5415.2008.01821.x [DOI] [PubMed] [Google Scholar]
- Bradway C., DiResta J., Miller E., Edmiston M., Fleshner I., & Polomano R. C (2009). Caring for obese individuals in the long-term care setting. Annals of Long- Term Care: Clinical Care and Aging, 17, 17–21. [Google Scholar]
- Bradway C. Felix H. C. Whitfield T. & Li X (2017). Barriers in transitioning patients with severe obesity from hospitals to nursing homes. Western Journal of Nursing Research, 39, 1151–1168. doi:10.1177/0193945916683682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradway C. Miller E. Heivly A. & Fleshner I (2010). Continence care for obese nursing home residents. Urologic Nursing, 30, 121–129. [PubMed] [Google Scholar]
- Buys D. R., Roth D. L., Ritchie C. S., Sawyer P., Allman R. M., Funkhouser E. M.,…, Locher J. L. (2014). Nutritional risk and body mass index predict hospitalization, nursing home admissions, and mortality in community-dwelling older adults: Results from the UAB Study of Aging with 8.5 years of follow-up. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 69, 1146–1153. doi:10.1093/gerona/glu024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai S. Rahman M. & Intrator O (2013). Obesity and pressure ulcers among nursing home residents. Medical Care, 51, 478–486. doi:10.1097/MLR.0b013e3182881cb0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cienki J. J. (2016). Emergency medical service providers’ perspectives towards management of the morbidly obese. Prehospital and Disaster Medicine, 31, 471–474. doi:10.1017/S1049023X16000595 [DOI] [PubMed] [Google Scholar]
- Drake D. Dutton K. Engelke M. McAuliffe M. & Rose M. A (2005). Challenges that nurses face in caring for morbidly obese patients in the acute care setting. Surgery for Obesity and Related Diseases: Official Journal of the American Society for Bariatric Surgery, 1, 462–466. doi:10.1016/j.soard.2005.06.003 [DOI] [PubMed] [Google Scholar]
- Elkins J. S. Whitmer R. A. Sidney S. Sorel M. Yaffe K. & Johnston S. C (2006). Midlife obesity and long-term risk of nursing home admission. Obesity (Silver Spring, Md.), 14, 1472–1478. doi:10.1038/oby.2006.167 [DOI] [PubMed] [Google Scholar]
- Felix H. C. (2008). Personal care assistance needs of obese elders entering nursing homes. Journal of the American Medical Directors Association, 9, 319–326. doi:10.1016/j.jamda.2008.01.011 [DOI] [PubMed] [Google Scholar]
- Felix H. C. Bradway C. Ali M. M. & Li X (2016). Nursing home perspectives on the admission of morbidly obese patients from hospitals to nursing homes. Journal of Applied Gerontology: The Official Journal of the Southern Gerontological Society, 35, 286–302. doi:10.1177/0733464814563606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felix H. C. Bradway C. Chisholm L. Pradhan R. & Weech-Maldonado R (2015). Prevalence of moderate to severe obesity among U.S. nursing home residents, 2000-2010. Research in Gerontological Nursing, 8, 173–178. doi:10.3928/19404921-20150223-01 [DOI] [PubMed] [Google Scholar]
- Felix H. C. Bradway C. Miller E. Heivly A. Fleshner I. & Powell L. S (2010). Obese nursing home residents: A call to research action. Journal of the American Geriatrics Society, 58, 1196–1197. doi:10.1111/j.1532-5415.2010.02879.x [DOI] [PubMed] [Google Scholar]
- Felix H. C. Thostenson J. D. Bursac Z. & Bradway C (2013). Effect of weight on indwelling catheter use among long-term care facility residents. Urologic Nursing, 33, 194–200. [PMC free article] [PubMed] [Google Scholar]
- Flegal K. M., Kit B. K., & Graubard B. I (2014). Body mass index categories in observational studies of weight and risk of death. American Journal of Epidemiology, 180, 288–296. doi:10.1093/aje/kwu111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal K. M., Kit B. K., Orpana H., & Graubard B. I (2013). Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA, 309, 71–82. doi:10.1001/jama.2012.113905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontaine K. R. Redden D. T. Wang C. Westfall A. O. & Allison D. B (2003). Years of life lost due to obesity. JAMA, 289, 187–193. doi:10.1001/jama.289.2.187 [DOI] [PubMed] [Google Scholar]
- Gallagher S. M. (1998). Needs of the homebound morbidly obese patient: A descriptive survey of home health nurses. Ostomy/Wound Management, 44, 32–4, 36, 38 passim. [PubMed] [Google Scholar]
- Grabowski D. C. Campbell C. M. & Ellis J. E (2005). Obesity and mortality in elderly nursing home residents. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 60, 1184–1189. doi:10.1093/gerona/60.9.1184 [DOI] [PubMed] [Google Scholar]
- Grant M. J. & Booth A (2009). A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information and Libraries Journal, 26, 91–108. doi:10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- Johnson L. E., Hasse L. A., Shumaker H (1997). A comparison of health status in obese and average weight elderly nursing home residents. Am J Clin Nutr, 66(1), 209. [Google Scholar]
- Lapane K. L. & Resnik L (2005). Obesity in nursing homes: An escalating problem. Journal of the American Geriatrics Society, 53, 1386–1391. doi:10.1111/j.1532-5415.2005.53420.x [DOI] [PubMed] [Google Scholar]
- Miles J., Anderson D. P., Engelke M., Kirkpatrick M. K., Pories M. L., Waters W. G.,…, Rose M. A. (2012). Barriers to transition of obese patients from hospital to community. The American Journal of Managed Care, 18, e234–e237. [PubMed] [Google Scholar]
- Millson J., Peters N., & Anderson G. H (2010). Obesity and diabetes in a nursing home. Paper presented at the Diabetes Orlando, FL: American Diabetes Association. [Google Scholar]
- NHLBI Obesity Education Initiative Expert Panel on the Identification Evaluation and Treatment of Obesity in Adults (1998). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults--The evidence report. National Institutes of Health. Obesity Research, 6(Suppl. 2), 51s–209s. [PubMed] [Google Scholar]
- Phelan S. M. Burgess D. J. Yeazel M. W. Hellerstedt W. L. Griffin J. M. & van Ryn M (2015). Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obesity Reviews: An Official Journal of the International Association for the Study of Obesity, 16, 319–326. doi:10.1111/obr.12266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popay J., Roberts H., Sowden A., Petticrew M., Arai L., Rodgers M., … Duffy S (2006). Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version, 1, b92.Lancaster: Institute of Health Research. [Google Scholar]
- Powell L. S., Felix H. C., Bradway C., Miller E., Heivly A., Fleshner I (2010). Additional research on the cost of caring for obese nursing home residents is critical to maintaining adequate resources in the long-term care industry. Journal of the American Medical Directors Association, 11(3), 222. [DOI] [PubMed] [Google Scholar]
- Puhl R. & Brownell K. D (2001). Bias, discrimination, and obesity. Obesity Research, 9, 788–805. doi:10.1038/oby.2001.108 [DOI] [PubMed] [Google Scholar]
- Puhl R. M. & Heuer C. A (2010). Obesity stigma: Important considerations for public health. American Journal of Public Health, 100, 1019–1028. doi:10.2105/AJPH.2009.159491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose M. A., Baker G., Drake D. J., Engelke M., McAuliffe M., Pokorny M., … Watkins F (2007). A comparison of nurse staffing requirements for the care of morbidly obese and non-obese patients in the acute care setting. Bariatric Nursing and Surgical Patient Care, 2, 53–56. [Google Scholar]
- Rotkoff N. (1999). Care of the morbidly obese patient in a long-term care facility. Geriatric Nursing (New York, NY), 20(6), 309–313. [DOI] [PubMed] [Google Scholar]
- Valiyeva E. Russell L. B. Miller J. E. & Safford M. M (2006). Lifestyle-related risk factors and risk of future nursing home admission. Archives of Internal Medicine, 166, 985–990. doi:10.1001/archinte.166.9.985 [DOI] [PubMed] [Google Scholar]
- Ventura M. M., Simmons S. F., Shotwell M. S., Hudson A., Hollingsworth E. K., Long E., … Silver H. J (2016). Elevated serum osmolality and total water deficit indicate impaired hydration status in residents of long-term care facilities regardless of low or high body mass index. Journal of the Academy of Nutrition and Dietetics, 116(5), 828–836. e822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N., Cereda E., Solmi M., Fowler S. A., Manzato E., Maggi S.,…, Correll C. U. (2015). Inverse relationship between body mass index and mortality in older nursing home residents: A meta-analysis of 19,538 elderly subjects. Obesity Reviews: An Official Journal of the International Association for the Study of Obesity, 16, 1001–1015. doi:10.1111/obr.12309 [DOI] [PubMed] [Google Scholar]
- WHO Expert Committee.(1995). Physical status: The use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organization Technical Report Series, 854, 1–452. [PubMed] [Google Scholar]
- Wong E. S. Wang B. C. Garrison L. P. Alfonso-Cristancho R. Flum D. R. Arterburn D. E. & Sullivan S. D (2011). Examining the BMI-mortality relationship using fractional polynomials. BMC Medical Research Methodology, 11, 175. doi:10.1186/ 1471-2288-11-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z. & Zhang N (2014). The burden of overweight and obesity on long-term care and Medicaid financing. Medical Care, 52, 658–663. doi:10.1097/MLR.0000000000000154 [DOI] [PubMed] [Google Scholar]
- Zarowitz B. J., Allen C., O’Shea T., Dalal M., Haumschild M. J., Digenio A (2014). Prevalence of obesity among U.S. nursing home residents (NHR) with T2DM. Diabetes, 63(1), A660. [Google Scholar]
- Zhang N., Li Y., Rodriguez-Monguio R., Barenberg A., Temkin-Greener H., & Gurwitz J (2016). Are obese residents more likely to be admitted to nursing homes that have more deficiencies in care?Journal of the American Geriatrics Society, 64, 1085–1090. doi:10.1111/jgs.14105 [DOI] [PubMed] [Google Scholar]
- Zhang N. Li Y. & Temkin-Greener H (2013). Prevalence of obesity in new york nursing homes: Associations with facility characteristics. The Gerontologist, 53, 567–581. doi:10.1093/geront/gnt011 [DOI] [PubMed] [Google Scholar]
- Zizza C. Herring A. Domino M. Haines P. Stevens J. & Popkin B. M (2003). The effect of weight change on nursing care facility admission in the NHANES I Epidemiologic Followup Survey. Journal of Clinical Epidemiology, 56, 906–913. doi:10.1016/S0895-4356(03)00142-2 [DOI] [PubMed] [Google Scholar]
- Zizza C. A. Herring A. Stevens J. & Popkin B. M (2002). Obesity affects nursing-care facility admission among whites but not blacks. Obesity Research, 10, 816–823. doi:10.1038/oby.2002.110 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.