Abstract
Each year more than 400 physicians take their lives, likely related to increasing depression and burnout. Burnout—a psychological syndrome featuring emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment—is a disturbingly and increasingly prevalent phenomenon in healthcare, and emergency medicine (EM) in particular. As self-care based solutions have proven unsuccessful, more system-based causes, beyond the control of the individual physicians, have been identified. Such system-based causes include limitations of the electronic health record, long work hours and substantial educational debt, all in a culture of “no mistakes allowed.” Blame and isolation in the face of medical errors and poor outcomes may lead to physician emotional injury, the so-called “second victim” syndrome, which is both a contributor to and consequence of burnout. In addition, emergency physicians (EP) are also particularly affected by the intensity of clinical practice, the higher risk of litigation, and the chronic fatigue of circadian rhythm disruption. Burnout has widespread consequences, including poor quality of care, increased medical errors, patient and provider dissatisfaction, and attrition from medical practice, exacerbating the shortage and maldistribution of EPs. Burned-out physicians are unlikely to seek professional treatment and may attempt to deal with substance abuse, depression and suicidal thoughts alone. This paper reviews the scope of burnout, contributors, and consequences both for medicine in general and for EM in particular.
INTRODUCTION
“Burnout” evokes images of harried, sleep-deprived, hungry physicians, overwhelmed with “paperwork,” administrative complaints of missed metrics, and pending tasks for family and patients. For the physician suffering from burnout, recovery can seem daunting or even impossible. For healthcare, burnout has been branded an epidemic, with societal and human economic and personal costs.1 This article, the first of two parts, synthesizes information on burnout—the scope of the problem, its causes and consequences—from the perspective of the emergency physician (EP). Part II will focus on wellness and seek to make recovery less daunting.
Burnout: Definition and Measurement
Burnout is a complex condition with a history in many disciplines. Based on his research, Freudenberger used “burnout” as shorthand for a psychological syndrome with three dimensions: emotional exhaustion, depersonalization, and reduced personal accomplishment.2 Maslach subsequently summarized the dimensions of burnout as “exhaustion,” “cynicism,” and “inefficacy,” providing more identifiable definitions of each dimension that align well with her measurement tool.3 Those who score high in “exhaustion” feel over-extended, their emotional and physical resources depleted.3 High scorers in “cynicism” (depersonalization) appear more callous or detached than would be expected for normal “coping.”3 Those lacking confidence or feeling they have achieved little work success score high in the “inefficacy” (reduced personal accomplishment) dimension.3 Overall, sufferers from burnout are frequently exhausted, diminished in their ability to care, and feel as though their work makes little difference.
Maslach used these definitions to create the most frequently used assessment tool for identifying burnout, the Maslach Burnout Inventory (MBI). This tool contains 22 questions addressing the three dimensions and provides scores in each. The higher the score, the higher the burnout in that dimension.4 Rather than a dichotomous cutoff score of burnout as a diagnosis, the MBI describes a spectrum with higher scores equating to more severe symptoms and consequences.5 While the MBI has been modified and abbreviated for specific populations and ease of use, it remains proprietary. The next most common tool used in healthcare burnout research, the Oldenburg Burnout Inventory, focuses on emotional exhaustion and depersonalization/disengagement, while leaving out personal accomplishment.6 A list of burnout assessment tools appears in Appendix 1; however, readers may consider simply asking physicians if they are burned out: In one study, self-reported burnout accurately predicted meeting MBI burnout criteria 72% of the time.7
METHODS
Keywords
We chose “burnout” and its main components (“emotional exhaustion,” “depersonalization,” “cynicism,” “job dissatisfaction”) as the endpoint keywords. Because healthcare burnout researchers leave out the “lack of personal accomplishment” dimension, we did the same here.8 “Depression” and “suicide,” the ultimate consequences of burnout, were also included as endpoints. These keywords were paired with population keywords: “physicians,” “residents,” “medical students,” and “emergency medicine” (EM) to find relevant articles in the medical literature.
Search
We searched all combinations of pairings of each “endpoint” keyword with a “population” keyword from 1974 to the present in both Ovid Medline and PubMed. To ensure more esoteric sources were included we conducted searches for “endpoint” keywords on various EM/critical care blogs and lay press Web sites.9
Article Inclusion Criteria
We categorized all search results into primary research studies, commentary/opinion pieces, and review articles. Primary research studies, inclusive of their relevant references, provided the database of supporting information for the composition of the review. Additionally, we attempted to identify the primary literature for all Internet-based resources.
RESULTS
Scope of Burnout in Physicians
Freudenberger and Maslach initially identified and studied burnout in non-medical fields; however, as early as 1981, research began to focus on burnout in physicians and medicine.10 In 2012 a landmark study identifying burnout as high scores in either the MBI’s depersonalization or emotional exhaustion dimension found that 37.9% of physicians met criteria for burnout compared to 27.8% of the general United States (U.S.) workforce.8 Since 2013, Medscape has published the results of an annual survey of physicians. Per this report, the percentage of physicians experiencing burnout has steadily risen.11 Most recently, 44% of respondent physicians indicated feeling burned out, a percentage that correlates with the most recent survey by Shanafelt et al. (43.9% respondents had at least one symptom of burnout).11,12
Burnout has been studied at all levels of medical training and starts early: one study identified 52.8% of students (an equal mix of all four years) from seven medical schools meeting criteria.13 Burnout continues during residency, though it has been less frequently explored. In 2002 Shanafelt et al. found that 76% (n = 87/115) of one internal medicine program’s residents met criteria for burnout.14 In a 2018 study, researchers surveying 3588 second-year resident physicians across multiple specialties found that 45.2% experienced at least one symptom of burnout at least weekly.15 A recent systematic review and meta-analysis aggregated 26 studies including 4664 residents of multiple specialties and found a burnout prevalence of 35.7%, consistent with previous work.16 This early-career burnout seems to predict later-career burnout, as suggested by a small study of internal medicine residents (N = 81) over 10 years.17 They found high univariate correlations between emotional distress in residency and later emotional exhaustion (correlation coefficient=0.30, P = 0.007) and depersonalization (correlation coefficient=0.25, P = 0.029).17 For an expanded list of different burnout and wellness surveys and scales, please see Table 1 in the Appendix.
Causes of Burnout
Historically, medicine saw burnout as a sign of personal weakness or of being ill-suited to the profession.18 Without consideration of organizational and societal influences on burnout development, authors suggested that “self-rescue” would occur if one simply recognized his or her condition and engaged in improved communication and management-skills training or routine exercise.19–21 Even leading researchers espoused these beliefs: Shanafelt et al. stated that physician burnout was related to stressful work, doing too much and putting others’ needs before their own.22 However, the results of Shanafelt’s landmark 2012 study on the prevalence of burnout appeared to have changed his views, and he called on others to take a different perspective:
“The fact that almost 1 in 2 U.S. Physicians has symptoms of burnout implies that the origins of this problem are rooted in the environment and care delivery system rather than in the personal characteristics of a few susceptible individuals.”8
Although individual characteristics do contribute to burnout susceptibility, and physicians cope with burnout using exercise and meditation, the problem has not improved.11,23 Individual physicians seem to recognize the importance of outside forces on their experience of burnout, even if society and organizations have not fully embraced this. The responses to the yearly Medscape survey now lists only organizational and environmental causes for burnout, such as bureaucratic tasks, long work hours, electronic health records (EHR), lack of respect, lack of control/autonomy, and profits over patients.11 The following discussion will focus on three contributing factors: EHRs, financial concerns, and the “second victim” syndrome (SVS).
Electronic Health Records
While charting was once used to communicate relevant clinical information between members of the healthcare team, the EHR has shifted medicine’s focus to billing, coding, and protection from litigation. EHRs are independently associated with higher rates of burnout among users.24 Clinical time spent more on the computer than with patients impairs patient contact (ie, “the best part of being a doctor”). Less one-on-one time with patients leads to a decrease in humanism and conflicts with physicians’ inherent altruism. This in turn increases the risk of burnout and substantiates the views of the Medscape respondents: profits over patients.25, 26
EHRs impact physician workflow as time-consuming distractions that create new problems, such as downtimes and electronic-prescription system failures. Downtimes are typically scheduled at “slow times” for the hospital in the middle of the night, when EPs and emergency departments (ED) are often busiest and staffing scarce. The EHR’s billing-centric design slows chart-completion, and online availability can lead to uncompensated charting at home.26,27 While physicians generally agree that EHRs have improved access to medical records and provide some benefits, they decrease patient interaction, worsen work-life balance, and decrease job satisfaction, resulting in overall net harm to physicians.27
Financial Concerns
While Medscape respondents mention “lack of compensation/reimbursement,” their concerns may be tied to medical school debt.11 The cost of medical education continues to rise; physicians who graduated in 2016 carry an average debt over $190,000, which correlates with burnout.28,29 Additionally, physicians feel under-prepared to navigate their finances while transitioning to attending-level income.30 This lack of preparation may lead to living above their means, worsening their debt despite high income, resulting in increased stress and burnout.31
Second Victim Syndrome
Another likely contributor to and consequence of burnout is the SVS phenomenon.34–36 SVS embodies the psychological trauma healthcare workers suffer from involvement in an “adverse event.” Typically related to committing a medical error resulting in a poor patient outcome, SVS may also involve any adverse patient outcome, expected or unexpected, with the physician becoming the “second victim.”37 One study found that 30% of physicians (all specialties) experienced emotional issues related to a “bad outcome,” while another found up to 60% of surgical residents experienced SVS.38, 39
Society sets a zero-mistake standard for physicians.32 This high standard may isolate those who make mistakes leaving them without healthy ways to cope, resulting in dysfunctional approaches to recovery.32,35,36 Poor responses (isolation, anger, sadness, substance abuse, and callousness toward patients and colleagues) place the physician more at risk for burnout.35,36 When suffering from SVS, the perception of not being supported or even of being victimized by one’s own hospital or organization can exacerbate the syndrome.32,40 This sense of victimization comes despite research suggesting that medical errors leading to poor patient outcomes stem from system failures and not just the individual who committed the error.41,42 This is a continuous chain of events; if a physician is burned out, he or she is more likely to commit an error during patient care, which puts them at risk for SVS and litigation stress and likely exacerbates their burnout.32,36,43–45 This cycle and its associated emotional toll lead to negative consequences, which may include depression and departing medicine by either attrition or suicide.35
Consequences of Burnout
Additional consequences of burnout include poor clinical care, increased mistakes, patient dissatisfaction, dysfunctional interactions between colleagues, the contagion of burnout, substance abuse/self-medication, depression, and suicide.
Clinical Care
Health systems now recognize the negative impact of burnout on healthcare quality, patient safety, and financial performance.46 A study of U.S. surgeons found both an increased rate of medical errors and greater medicolegal risk for physicians experiencing burnout.47 A recent meta-analysis found a statistically significant negative relationship between physician burnout and patient safety (r = −0.23), as well as burnout and quality of care (r = −0.26).48 As clinical care suffers, so does patient satisfaction, which in turn may further decrease health outcomes.49,50 Burnout may also affect a physician’s colleagues by being contagious: burned-out physicians negatively interact with co-workers and perform more poorly at their jobs, creating a negative work environment and putting others at risk for burnout.3,51,52
Leaving Jobs/Medicine
Physicians suffering burnout are significantly more likely to leave healthcare.53,54 Physicians first reduce work hours or change jobs or specialties, negatively affecting the health system. The estimated cost to replace a physician is $160,000–$1,000,000, depending on specialty and experience. This estimate does not include intangibles such as team disruption.11,46,55–57 If this job change does not help, physicians may seek administrative positions or leave medicine entirely.58
Depression and Self-medication
Burnout occurs on a continuum with depression. The 2012 study by Shanafelt et al. found that 37.8% of respondents screened positive for depression on a standardized and validated two-question screening tool.8 The most recent Medscape survey indicated that 15% are not only burned out, but also are either “colloquially” or clinically depressed.11 Multiple barriers separate physicians from depression assistance. Such barriers include feeling that they do not require professional intervention and, perhaps more importantly, fearing the loss of medical licensure and hospital credentialing.11,59 A 2014 survey found that nearly 40% of physicians would be reluctant to seek care for mental health due to licensure concerns.60
While many physicians deal with burnout and depression in isolation, some have developed harmful coping strategies such as alcohol and drug use.11 In general, older research suggests that approximately 10–12% of physicians will develop at least one substance abuse disorder, similar to the general population rate.61 More recent data suggest physicians primarily abuse alcohol, with 12.9% of male physicians and 21.9% of female physicians affected, numbers higher than the general population. (Overall 6.2% of the U.S. population 18 years or older has an alcohol use disorder, 8.4% of men and 4.2% of women.)62,63
Suicide
Society is shocked when a physician commits suicide. It is estimated that 400 physicians in the U.S. die by suicide each year.64 Compared to the general population, male and female physicians are at greater relative risk (RR) of suicide (RR = 3.4 and RR = 5.7, respectively).65,66 Shanafelt, et al. reported that 6.4% of respondents had considered suicide in the previous year.8 In the most recent Medscape report, 14% of respondents had considered suicide and 1% of respondents had attempted suicide, results similar to a study of female physicians (1.5% attempted suicide).11, 67 Physicians in training are not immune to these risks. Approximately 10% of medical students report suicidal ideation, and suicide is the second leading cause of death among resident trainees in the U.S. (4.1 per 100,000, or approximately five residents per year).68–70
While these rates of physician depression and suicidal ideation do not significantly differ from those of the general working population (37.8% and 6.4%, respectively), there are reasons to believe that physician depression is both under-reported and under-treated.8 Physicians are less likely to seek treatment since depression remains stigmatized in medical culture.41,71 Depressed physicians may feel like failures, isolated and cut off from their colleagues whom they believe are coping better. Feelings of isolation, loss of belonging, and failure, combined with the perception of being a burden on partners, family, friends and society, drive some to see suicide as an answer.72
Given that physicians do not seek help and approximately one in seven has considered suicide, someone reading this may be suffering from depression and contemplating suicide. If that is you, please reach out to a friend, a helpline (call 1-800-273-8255 or text HOME to 741741), a therapist, or to an employee assistance program. Anyone with concerns that a colleague is suffering should reach out, ask, listen, and assist him or her in finding help. For a comprehensive list of suicide prevention and self help resources, please see Table 2 in the Appendix.
DISCUSSION
In medicine, EM is unique in its hours, patient population and stressors. This uniqueness translates into more EP burnout. A four-year survey published in 1996 found that 60% of EP respondents “registered in the moderate to high burnout ranges” on the MBI.7 In the 2012 landmark burnout study, EM was the most burned-out specialty (~65%), over 10% more “burned out” than the next closest specialty (general internal medicine), and close to 20% more than the mean rate for all physicians responding.8 While burnout in EM has continued, the most recent Medscape report indicates that EM is the fifth most burned-out specialty behind urology, neurology, physical medicine and rehabilitation, and internal medicine.11 Like other specialties, burnout in EM starts early, with studies showing between 65–74% of residents (all levels) meet criteria for burnout.73,74
Causes of Burnout in Emergency Medicine
The unique stressors in EM may easily lead EP burnout to be attributed to personal characteristics such as poor coping skills or lack of exercise, rest, and hobbies, a view that continues to this day. However, organizational and environmental causes of burnout certainly apply to EPs. One notable exception is the usual connection between burnout and increased work hours. For non-EPs, burnout appears to directly correlate with increasing work hours.11 On the contrary, while EPs are the least likely specialists to work excessive hours (>40 hours/week), the necessity of working nights and on weekends and holidays may contribute to burnout.11 Furthermore, the lack of support staff and medical infrastructure during these “off” hours, coupled with high intensity work (heavy workload, multiple sick patients, frequent task-switching, patient and colleague rudeness, and constant uncertainty) may have a similar effect on EP emotional health as the longer hours of other specialists.75–79
With fewer weekly hours than other specialties, EPs have the ability to “pick up” extra shifts, increasing their work hours and the associated stress. Many EPs work extra shifts to pay off debt, another stressor and contributor to burnout.80 In 2016 the median debt of EM residents in one study was $212,000.81 This debt caused stress and changed plans: getting out of debt reportedly took priority over pursuing further educational opportunities, vacations, and spending time with family, all things that might counter burnout.80,81 The ability to “pick up” extra shifts to pay down debt and the perception that they are working less than other physicians are examples of particular attributes of EM that increase susceptibility to burnout.82 Three other causes of burnout in EM deserve mention: clinical pressures/expectations, litigation stress, and fatigue/sleep loss.
Clinical Pressures and Expectations
Society perceives EM as a world of excitement, drama, and miraculous saves.83 While not wholly inaccurate, television dramas do not show the persistent demand for immediate and error-free care despite limited resources.84 This mismatch between demands and resources, coupled with constant diagnostic uncertainty, significantly stresses EPs and promotes burnout and emotional exhaustion.79,84–86
Both EDs and EPs are limited resources: EDs are closing while visits are increasing, and there is a national shortage of EPs, particularly in less geographically desirable areas.87,88 Despite a consistent increase in EM first-year residency training positions (1786 in 2014 to 2278 in 2018, 27.5% increase), only 61% of U.S. emergency care providers are EPs, with the rest a combination of advanced practice providers (APPs) (24.5%) and non-EPs (14.3%).89, 90 This shortfall particularly affects rural areas where only 44.8% of rural emergency care providers are EPs.90 Despite this shortfall, EPs provide care for 85.3% of ED patients, meaning they are working more clinical hours while being responsible for care being provided by APPs.88, 91
Compensation is often based on productivity, patient satisfaction, and “quality” measures.92 With more patients and less time to see them, EPs who are judged on patient satisfaction may choose to acquiesce to requested, but not medically indicated, care. This occurs despite patient satisfaction correlating poorly with quality of care.93–97 Similarly, the guidelines and care metrics nominally designed to improve patient care (eg, door-to-doc/needle/antibiotics time) are rigorously enforced despite lack of evidence of patient benefit.98–99 Such metrics and guidelines, particularly prominent in EM as the initial provider of care, deprive physicians of autonomy and the ability to practice the art of medicine, leading to job dissatisfaction and burnout.82, 100
Litigation Stress
Being the first care provider for so many sick patients means inevitably dealing with a malpractice claim, another cause of burnout.101 Annually, EPs face malpractice claims at a slightly higher rate than the average physician (8.7% vs 7.2%).102 Each litigation episode can last years, and physicians are counseled not to discuss such cases with anyone, adding to the isolation and lack of peer support.103,104 Annually, up to 73% of EPs admit to practicing “defensive medicine,” ordering extra tests to avoid missing anything, and cite fear of litigation as the reason.105 This practice leads to physician cynicism and disengagement (precursors to burnout), and increases healthcare spending (by an estimated $750 billion in 2010).106
Sleep loss and fatigue
One reason EPs likely face higher litigation rates is that they simply encounter more sick patients than other physicians, as their work environment is available at all times. To fulfill the 24-hour need for high quality emergency care, EM is built around shift work. The resulting disruption of circadian rhythms leads to sleep loss and its associated detrimental effects on health: increased cardiovascular disease, metabolic syndrome, sleep disorders, and possibly even increased mortality.107,108 The effects of shift work are felt early (84% of five cohorts of EM residents felt a need for intervention for their sleep deprivation and self-perceived exhaustion) and become more pronounced with age.109,110 Sleep deprivation is associated with worse patient care, decreased job satisfaction, and less personal well-being, all of which contribute to burnout.111
Consequences of Burnout in Emergency Medicine
While the consequences of burnout for EPs are similar to those for physicians in general, certain areas deserve specific mention: clinical care, depression, substance abuse, SVS, and suicide.
Clinical Care
Like other physicians, burned-out EPs self-report delivering suboptimal clinical care and more often perceive they have erred medically.73 Such EPs also have lower patient satisfaction scores and perform worse during high-fidelity simulations compared with their peers who are not burned out.111, 112
Physician Drop Out
Although attrition from EM has historically been low (1.7% per year, in a 2010 study), attrition rates do not account for those feeling “trapped” in their current jobs due to debt.81,113 This may be one reasons why EPs are the second least happy at work behind physical medicine and rehabilitation.11 EPs may forego further training or changing jobs due to debt, creating a feeling of hopelessness that further contributes to stress and burnout.81 Ironically, further training in a subspecialty of EM could serve to reduce burnout by adding variation to an EP’s work schedule and duty.114
Depression
Researchers have found rates of depression in EPs (12.1% – 19.3%) consistent with the Medscape survey of depression rates in all respondents (11–15%). 11,115–116
Self-medication
Both EPs and EM residents experience higher rates of substance abuse than other specialties, with studies estimating that 4.9–12.5% of EM residents drink daily.116,117 Other research suggests that 7–18% of the physicians treated for substance abuse are EPs, despite only 4.7% of all physicians being EPs.118–120
Second Victim Syndrome
While no specialty-specific numbers exist, EPs seem especially susceptible to SVS. EPs rarely have time to debrief or grieve after an adverse patient outcome, because there is always the next patient.37 Most EPs have a story about a patient dying despite their best efforts and then having to see a lower acuity patient unhappy because of an extended wait. This lack of processing time for patient deaths or medical errors may make EPs more susceptible to SVS and, by extension, burnout. Conversely, burned-out physicians are more likely to commit a medical error and have poorer job-coping skills. SVS is complex and intimately tied to depression and burnout, with all three contributing to and resulting from the others.37 However, they are related: SVS, burnout, and depression may all result in an EP leaving the specialty in the most final way – suicide.
Suicide
While no specialty-specific data exists and the Medscape data may contain biased responses, extrapolation from that data suggests that, in the last year, as many as 6,000 EPs have contemplated and up to 400 have attempted suicide.11,121 The following factors may explain why these numbers are so high: (a) EM seems to have a higher rate of gender-based harassment of women (45.3% vs 20.3%) than the medicine average;122 (b) female physicians have a much higher rate of suicide than their general population counterparts (130% higher);123 (c) there is an association between workplace harassment, depression and suicide;122 and (d) physicians tend to “succeed” in their suicide attempts more often than the general population.72
CONCLUSION
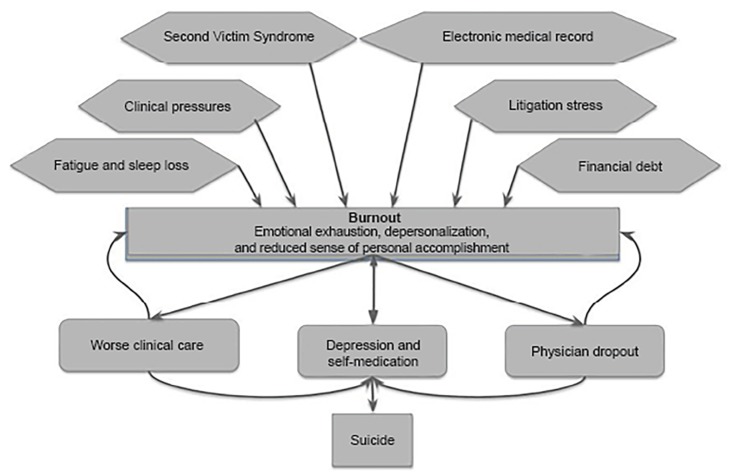
While suicide is its ultimate tragic outcome, burnout is a complex condition resulting in many consequences. Since EPs are particularly vulnerable to burnout due to the system, culture and society in which they practice, we need to understand the complicated interaction between the signs, symptoms, causes, and consequences of burnout (Figure 1). This understanding can help create a path to recovery, both individually and as a specialty. As practitioners of a specialty who experience burnout at such high levels, EPs should take the lead in this recovery. Resources to aid in recovery will be found in Part II of this series, which discusses mitigating burnout and its consequences through wellness, “the anti-burnout.”
Figure 1.
The causes and consequences of physician burnout.
Supplementary Information
Footnotes
Section Editor: John Burkhardt, MD, MA
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
REFERENCES
- 1.West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–81. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 2.Freudenberger HJ. Staff burn-out. J Soc Issues. 1974;30(1):159–65. [Google Scholar]
- 3.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 4.Maslach C, Jackson S, Leiter M. The Maslach Burnout Inventory Manual. In: Zalaquett CP, Wood RJ, editors. Evaluating Stress: A Book of Resources. Lanham, MD: The Scarecrow Press; 1997. pp. 191–218. [Google Scholar]
- 5.Palamara K, Linzer M, Shanafelt TD. Addressing uncertainty in burnout assessment. Acad Med. 2018;93(4):518. doi: 10.1097/ACM.0000000000002116. [DOI] [PubMed] [Google Scholar]
- 6.Halbesleben JR, Demerouti E. The construct validity of an alternative measure of burnout: investigating the English translation of the Oldenburg Burnout Inventory. Work & Stress. 2005;19(3):208–20. [Google Scholar]
- 7.Goldberg R, Boss RW, Chan L, et al. Burnout and its correlates in emergency physicians: four years’ experience with a wellness booth. Acad Emerg Med. 1996;3(12):1156–64. doi: 10.1111/j.1553-2712.1996.tb03379.x. [DOI] [PubMed] [Google Scholar]
- 8.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–85. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 9.Emergency Medicine and Critical Care. Life in the Fast Lane Web site. [Accessed February 23, 2019]. Available at: https://litfl.com/emcc/
- 10.Battle CU. The iatrogenic disease called burnout. JAMWA (1972) 1981;36(12):357. [PubMed] [Google Scholar]
- 11.Peckham C. Medscape National Physician Burnout & Depression Report 2019. Medscape. 2019. [Accessed February 23, 2019]. Available at: https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056#2.
- 12.Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019 doi: 10.1016/j.mayocp.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 13.Dyrbye LN, Massie FS, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304(11):1173–80. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 14.Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–67. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 15.Dyrbye LN, Burke SE, Hardeman RR, et al. Association of clinical specialty with symptoms of burnout and career choice regret among US resident physicians. JAMA. 2018;320(11):1114–30. doi: 10.1001/jama.2018.12615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodrigues H, Cobucci R, Oliveira A, et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PloS One. 2018;13(11):e0206840. doi: 10.1371/journal.pone.0206840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raimo J, LaVine S, Spielmann K, et al. The correlation of stress in residency with future stress and burnout: a 10-year prospective cohort study. J Grad Med Educ. 2018;10(5):524–31. doi: 10.4300/JGME-D-18-00273.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suran BG, Sheridan EP. Management of burnout: training psychologists in Professional Life Span Perspectives. Prof Psychol Res Pr. 1985;16(6):741–52. [Google Scholar]
- 19.Orlowski JP, Gulledge AD. Critical Care Stress and Burnout. Crit Care Clin. 1986;2(1):173–81. [PubMed] [Google Scholar]
- 20.Graham J, Ramirez AJ, Cull A, et al. Job stress and satisfaction among palliative physicians. Palliat Med. 1996;10(3):185–94. doi: 10.1177/026921639601000302. [DOI] [PubMed] [Google Scholar]
- 21.Fields AI, Cuerdon TT, Brasseux CO, et al. Physician burnout in pediatric critical care medicine. Crit Care Med. 1995;23(8):1425–9. doi: 10.1097/00003246-199508000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–67. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 23.Deary IJ, Blenkin H, Agius RM, et al. Models of job-related stress and personal achievement among consultant doctors. Br J Psychol. 1996;87(1):3–29. doi: 10.1111/j.2044-8295.1996.tb02574.x. [DOI] [PubMed] [Google Scholar]
- 24.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(7):836–48. doi: 10.1016/j.mayocp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 25.Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419–26. doi: 10.1370/afm.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alexander AG, Ballou KA. Work-life balance, burnout, and the electronic health record. Am J Med. 2018;131(8):857–8. doi: 10.1016/j.amjmed.2018.02.033. [DOI] [PubMed] [Google Scholar]
- 27.Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Rand Health Q. 2014;3(4):1. [PMC free article] [PubMed] [Google Scholar]
- 28.Wisenberg Brin D. Taking the sting out of medical school debt. Association of American Medical Colleges Web site. 2017. [Accessed March 9, 2019]. Available at: https://news.aamc.org/medical-education/article/taking-sting-out-medical-school-debt/
- 29.West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952–60. doi: 10.1001/jama.2011.1247. [DOI] [PubMed] [Google Scholar]
- 30.Ahmad FA, White AJ, Hiller KM, et al. An assessment of residents’ and fellows’ personal finance literacy: an unmet medical education need. Int J Med Educ. 2017;8:192–204. doi: 10.5116/ijme.5918.ad11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Butcher L. A real education for future doctors: dealing with debt. American Association for Physician Leadership; 2018. [Accessed March 9, 2019]. Available at: https://www.physicianleaders.org/news/a-real-education-dealing-with-debt. [Google Scholar]
- 32.Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ. 2000;320(7237):726–7. doi: 10.1136/bmj.320.7237.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grissinger M. Too many abandon the “second victims” of medical errors. Pharm Ther. 2014;39(9):591–2. [PMC free article] [PubMed] [Google Scholar]
- 34.Coughlan B, Powell D, Higgins MF. The second victim: a review. Eur J Obstet Gynecol Reprod Biol. 2017;213:11–16. doi: 10.1016/j.ejogrb.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 35.Tamburri LM. Creating healthy work environments for second victims of adverse events. AACN Adv Crit Care. 2017;28(4):366–74. doi: 10.4037/aacnacc2017996. [DOI] [PubMed] [Google Scholar]
- 36.Gispen F, Wu AW. Psychological first aid: CPR for mental health crises in healthcare. JPSRM. 2018;23(2):51–3. [Google Scholar]
- 37.Lam R. Bouncing Back: The struggle of second victim syndrome. Emergency Medicine News. 2018;40(1):16. [Google Scholar]
- 38.Scott SD, Hirschinger LE, Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010;36(5):233–40. doi: 10.1016/s1553-7250(10)36038-7. [DOI] [PubMed] [Google Scholar]
- 39.Marmon LM, Heiss K. Improving surgeon wellness: the second victim syndrome and quality of care. Semin Pediatr Surg. 2015;24(6):315–8. doi: 10.1053/j.sempedsurg.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 40.Denham CR. TRUST: the 5 rights of the second victim. J Patient Saf. 2007;3(2):107–19. [Google Scholar]
- 41.Wallace JE. Mental health and stigma in the medical profession. Health (London) 2012;16(1):3–18. doi: 10.1177/1363459310371080. [DOI] [PubMed] [Google Scholar]
- 42.Pham JC, Story JL, Hicks RW, et al. National study on the frequency, types, causes, and consequences of voluntarily reported emergency department medication errors. J Emerg Med. 2011;40(5):485–92. doi: 10.1016/j.jemermed.2008.02.059. [DOI] [PubMed] [Google Scholar]
- 43.Burlison JD, Scott SD, Browne EK, et al. The second victim experience and support tool: validation of an organizational resource for assessing second victim effects and the quality of support resources. J Patient Saf. 2017;13(2):93–102. doi: 10.1097/PTS.0000000000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Quillivan RR, Burlison JD, Browne EK, et al. Patient safety culture and the second victim phenomenon: connecting culture to staff distress in nurses. Jt Comm J Qual Patient Saf. 2016;42(8):377-AP2. doi: 10.1016/s1553-7250(16)42053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Seys D, Scott S, Wu A, et al. Supporting involved health care professionals (second victims) following an adverse health event: a literature review. Int J Nurs Stud. 2013;50(5):678–87. doi: 10.1016/j.ijnurstu.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 46.Dyrbye LN, Shanafelt TD, Sinsky CA, et al. Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care. National Academy of Medicine; 2017. [Accessed March 16, 2019]. Available at: https://nam.edu/burnout-among-health-care-professionals-a-call-to-explore-and-address-this-underrecognized-threat-to-safe-high-quality-care/ [Google Scholar]
- 47.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 48.Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. J Gen Intern Med. 2017;32(4):475–82. doi: 10.1007/s11606-016-3886-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Halbesleben JR, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev. 2008;33(1):29–39. doi: 10.1097/01.HMR.0000304493.87898.72. [DOI] [PubMed] [Google Scholar]
- 50.Haas JS, Cook EF, Puopolo AL, et al. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15(2):122–8. doi: 10.1046/j.1525-1497.2000.02219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Smith KP, Christakis NA. Social networks and health. Annu Rev Sociol. 2008;34:405–29. [Google Scholar]
- 52.Christakis NA, Fowler JH. Social contagion theory: examining dynamic social networks and human behavior. Stat Med. 2013;32(4):556–77. doi: 10.1002/sim.5408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Landon BE, Reschovsky JD, Pham HH, et al. Leaving medicine: the consequences of physician dissatisfaction. Med Care. 2006;44(3):234–42. doi: 10.1097/01.mlr.0000199848.17133.9b. [DOI] [PubMed] [Google Scholar]
- 54.Sinsky CA, Dyrbye LN, West CP, et al. Professional satisfaction and the career plans of US physicians. Mayo Clin Proc. 2017;92(11):1625–35. doi: 10.1016/j.mayocp.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 55.Dewa CS, Loong D, Bonato S, et al. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14:325. doi: 10.1186/1472-6963-14-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shah S. The real cost of emergency department physician turnover. The Studor Group; 2016. [Accessed March 10, 2019]. Available at: https://www.studergroup.com/resources/articles-and-industry-updates/insights/january-2016/the-real-cost-of-emergency-department-physician-tu. [Google Scholar]
- 57.Berg S. At Stanford, physician burnout costs at least $775 million a year. The American Medical Association; 2017. [Accessed March 16, 2019]. Available at: https://www.ama-assn.org/practice-management/physician-health/stanford-physician-burnout-costs-least-775-million-year. [Google Scholar]
- 58.Page L. Tired of Medicine? 20 Nonclinical Career Options. Medscape. 2018. [Accessed December 3, 2018]. Available at: https://www.medscape.com/viewarticle/893481_11.
- 59.Hengerer A, Kishore S. Breaking a culture of silence: The role of state medical boards. National Academy of Medicine; 2017. [Accessed March 9, 2019]. Available at: https://nam.edu/breaking-a-culture-of-silence-the-role-of-state-medical-boards/ [Google Scholar]
- 60.Dyrbye LN, West CP, Sinsky CA, et al. Medical licensure questions and physician reluctance to seek care for mental health conditions. Mayo Clin Proc. 2017;92(10):1486–93. doi: 10.1016/j.mayocp.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 61.Hughes PH, Brandenburg N, Baldwin DC, et al. Prevalence of substance use among US physicians. JAMA. 1992;267(17):2333–9. [PubMed] [Google Scholar]
- 62.Oreskovich MR, Shanafelt T, Dyrbye LN, et al. The prevalence of substance use disorders in American physicians. Am J Addict. 2015;24(1):30–8. doi: 10.1111/ajad.12173. [DOI] [PubMed] [Google Scholar]
- 63.Alcohol Facts and Statistics. National Institute on Alcohol Abuse and Alcoholism; 2019. [Accessed March 14, 2019]. Available at: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-facts-and-statistics. [Google Scholar]
- 64.Kishore S, Dandurand DE, Mathew A, et al. Breaking the culture of silence on physician suicide. National Academy of Medicine; 2016. [Accessed March 15, 2019]. Available at: https://nam.edu/breaking-the-culture-of-silence-on-physician-suicide/ [Google Scholar]
- 65.Lindeman S, Laara E, Hakko H, et al. A systematic review on gender-specific suicide mortality in medical doctors. Br J Psychiatry. 1996;168(3):274–9. doi: 10.1192/bjp.168.3.274. [DOI] [PubMed] [Google Scholar]
- 66.Schernhammer ES, Colditz GA. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis) Am J Psychiatry. 2004;161(12):2295–302. doi: 10.1176/appi.ajp.161.12.2295. [DOI] [PubMed] [Google Scholar]
- 67.Frank D, Dingle AD. Self-reported depression and suicide attempts among U.S. women physicians. Am J Psychiatry. 1999;156(12):1887–94. doi: 10.1176/ajp.156.12.1887. [DOI] [PubMed] [Google Scholar]
- 68.Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334–41. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 69.Yaghmour NA, Brigham TP, Richter T, et al. Causes of death of residents in ACGME-accredited programs 2000 through 2014: implications for the learning environment. Acad Med. 2017;92(7):976–983. doi: 10.1097/ACM.0000000000001736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Association of American Medical Colleges. 2017 State Physician Workforce Data Report. [Accessed March 16, 2019]. Available at: https://members.aamc.org/eweb/upload/2017%20State%20Physician%20Workforce%20Data%20Report.pdf.
- 71.Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289(23):3161–6. doi: 10.1001/jama.289.23.3161. [DOI] [PubMed] [Google Scholar]
- 72.Joiner T. The interpersonal-psychological theory of suicidal behavior: current empirical status. American Psychological Association; 2009. [Accessed March 13, 2019]. Available at: http://www.apa.org/science/about/psa/2009/06/sci-brief.aspx. [Google Scholar]
- 73.Lu DW, Dresden S, McCloskey C, et al. Impact of burnout on self-reported patient care among emergency physicians. West J Emerg Med. 2015;16(7):996–1001. doi: 10.5811/westjem.2015.9.27945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kimo Takayesu J, Ramoska EA, Clark TR, et al. Factors associated with burnout during emergency medicine residency. Acad Emerg Med. 2014;21(9):1031–5. doi: 10.1111/acem.12464. [DOI] [PubMed] [Google Scholar]
- 75.Muller IR, Eldakar-Hein ST, Ames SE, et al. Potential association between physician burnout rates and operating margins: specialty-specific analysis. J Med Pract Manage. 2017;32(4):233. [PubMed] [Google Scholar]
- 76.Westbrook JI, Raban MZ, Walter SR, et al. Task errors by emergency physicians are associated with interruptions, multitasking, fatigue and working memory capacity: a prospective, direct observation study. BMJ Qual Saf. 2018;27(8):655–63. doi: 10.1136/bmjqs-2017-007333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chang BP, Carter E, Ng N, et al. Association of clinician burnout and perceived clinician-patient communication. Am J Emerg Med. 2018;36(1):156–8. doi: 10.1016/j.ajem.2017.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mareiniss DP. Emergency medicine burnout and abuse—one doctor’s perspective. Am J Emerg Med. 2018;36(4):720–1. doi: 10.1016/j.ajem.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 79.Moukarzel A, Michelet P, Durand AC, et al. Burnout syndrome among emergency department staff: prevalence and associated factors. BioMed Res Int. 2019;4:1–10. doi: 10.1155/2019/6462472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Glaspy JN, Ma OJ, Steele MT, et al. Survey of emergency medicine resident debt status and financial planning preparedness. Acad Emerg Med. 2005;12(1):52–6. doi: 10.1197/j.aem.2004.02.532. [DOI] [PubMed] [Google Scholar]
- 81.Young TP, Brown MM, Reibling ET, et al. Effect of educational debt on emergency medicine residents: a qualitative study using individual interviews. Ann Emerg Med. 2016;68(4):409–18. doi: 10.1016/j.annemergmed.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 82.Silverman M. Beating the burnout blues. Emergency Physicians Monthly. 2015. [Accessed March 16, 2019]. Available at: http://epmonthly.com/article/beating-the-burnout-blues/
- 83.Harris D, Willoughby H. Resuscitation on television: Realistic or ridiculous? A quantitative observational analysis of the portrayal of cardiopulmonary resuscitation in television medical drama. Resuscitation. 2009;80(11):1275–9. doi: 10.1016/j.resuscitation.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 84.Kuhn G, Goldberg R, Compton S. Tolerance for uncertainty, burnout, and satisfaction with the career of emergency medicine. Ann Emerg Med. 2009;54(1):106–13. doi: 10.1016/j.annemergmed.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 85.Schaufeli WB, Leiter MP, Maslach C. Burnout: 35 years of research and practice. Career Dev Int. 2009;14(3):204–20. [Google Scholar]
- 86.Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Report. 2010;26:1–31. [PubMed] [Google Scholar]
- 87.Committee on the Future of Emergency Care in the United States Health System. Hospital-based emergency care: at the breaking point. National Academies Press; 2007. pp. 17–27. [Google Scholar]
- 88.Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2015 Emergency Department Summary Tables. Centers for Disease Control; [Accessed March 15, 2019]. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2015_ed_web_tables.pdf. [Google Scholar]
- 89.National Resident Matching Program, Results and Data: 2018 Main Residency Match®. National Resident Matching Program; Washington, DC: 2018. [Google Scholar]
- 90.Hall MK, Burns K, Carius M, et al. State of the national emergency department workforce: who provides care where? Ann Emerg Med. 2018;72(3):302–7. doi: 10.1016/j.annemergmed.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 91.Hooker RS, Klocko DJ, Luke Larkin G. Physician assistants in emergency medicine: the impact of their role. Acad Emerg Med. 2011;18(1):72–7. doi: 10.1111/j.1553-2712.2010.00953.x. [DOI] [PubMed] [Google Scholar]
- 92.Fenton JJ, Jerant AF, Bertakis KD, et al. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172(5):405–11. doi: 10.1001/archinternmed.2011.1662. [DOI] [PubMed] [Google Scholar]
- 93.Kravitz RL, Epstein RM, Feldman MD, et al. Influence of patients’ requests for direct-to-consumer advertised antidepressants: a randomized controlled trial. JAMA. 2005;293(16):1995–2002. doi: 10.1001/jama.293.16.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Macfarlane J, Holmes W, Macfarlane R, et al. Influence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: questionnaire study. BMJ. 1997;315(7117):1211–4. doi: 10.1136/bmj.315.7117.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pham HH, Landon BE, Reschovsky JD, et al. Rapidity and modality of imaging for acute low back pain in elderly patients. Arch Intern Med. 2009;169(10):972–81. doi: 10.1001/archinternmed.2009.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kennedy GD, Tevis SE, Kent KC. Is there a relationship between patient satisfaction and favorable outcomes? Ann Surg. 2014;260(4):592–8. doi: 10.1097/SLA.0000000000000932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Farley H, Enguidanos ER, Coletti CM, et al. Patient satisfaction surveys and quality of care: an information paper. Ann Emerg Med. 2014;64(4):351–7. doi: 10.1016/j.annemergmed.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 98.Kalantari A, Rezaie S. Challenging the one-hour sepsis bundle. West J Emerg Med. 2019;20(2):185–90. doi: 10.5811/westjem.2018.11.39290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Spiegel R, Farkas JD, Rola P, et al. The 2018 surviving sepsis campaign’s treatment bundle: when guidelines outpace the evidence supporting their use. Ann Emerg Med. 2019 doi: 10.1016/j.annemergmed.2018.06.046. [DOI] [PubMed] [Google Scholar]
- 100.Lathrop D. Disenfranchised grief and physician burnout. Ann Fam Med. 2017;15(4):375–78. doi: 10.1370/afm.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chen KY, Yang CM, Lien CH, et al. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci. 2013;10(11):1471. doi: 10.7150/ijms.6743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jena AB, Seabury S, Lakdawalla D, et al. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629–36. doi: 10.1056/NEJMsa1012370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Charles SC. Coping with a medical malpractice suit. West J Med. 2001;174(1):55. doi: 10.1136/ewjm.174.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Andrew LB. Litigation Stress. MD Mentor; [Accessed March 16, 2019]. Available at: http://mdmentor.com/resources/eMedicine+Litigation+Stress.pdf. [Google Scholar]
- 105.Kanzaria HK, Hoffman JR, Probst MA, et al. Emergency physician perceptions of medically unnecessary advanced diagnostic imaging. Acad Emerg Med. 2015;22(4):390–8. doi: 10.1111/acem.12625. [DOI] [PubMed] [Google Scholar]
- 106.Jackson Healthcare. Physician study: quantifying the cost of defensive medicine. [Accessed March 16, 2019]. Available at: https://jacksonhealthcare.com/media-room/surveys/defensive-medicine-study-2010/
- 107.Hartenbaum NP, Zee PC. Shift work and sleep optimizing health, safety, and performance. J Occup Environ Med. 2011;53(5):S1–10. doi: 10.1097/JOM.0b013e31821aec20. [DOI] [PubMed] [Google Scholar]
- 108.Violanti JM, Hartley TA, Gu JK, et al. Life expectancy in police officers: a comparison with the US general population. Int J Emerg Ment Health. 2013;15(4):217. [PMC free article] [PubMed] [Google Scholar]
- 109.Papp KK, Stoller EP, Sage P, et al. The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad Med. 2004;79(5):394–406. doi: 10.1097/00001888-200405000-00007. [DOI] [PubMed] [Google Scholar]
- 110.Nelson D. Prevention and treatment of sleep deprivation among emergency physicians. Pediatr Emerg Care. 2007;23(7):498–503. doi: 10.1097/01.pec.0000280519.30570.fa. [DOI] [PubMed] [Google Scholar]
- 111.Machi MS, Staum M, Callaway CW, et al. The relationship between shift work, sleep, and cognition in career emergency physicians. Acad Emerg Med. 2012;19(1):85–91. doi: 10.1111/j.1553-2712.2011.01254.x. [DOI] [PubMed] [Google Scholar]
- 112.Lu DW, Weygandt PL, Pinchbeck C, et al. Emergency medicine trainee burnout is associated with lower patients’ satisfaction with their emergency department care. AEM E&T. 2018;2(2):86–90. doi: 10.1002/aet2.10094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ginde AA, Sullivan AF, Camargo CA. Attrition from emergency medicine clinical practice in the United States. Ann Emerg Med. 2010;56(2):166–71. doi: 10.1016/j.annemergmed.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 114.Cameron PA. Will Subspecialization benefit the practice of Australasian emergency medicine? Yes. Emerg Med Australas. 2016;28(4):471–2. doi: 10.1111/1742-6723.12632. [DOI] [PubMed] [Google Scholar]
- 115.Katz ED, Sharp L, Ferguson E. Depression among emergency medicine residents over an academic year. Acad Emerg Med. 2006;13(3):284–7. doi: 10.1197/j.aem.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 116.McBeth BD, Ankel FK, Ling LJ, et al. Substance use in emergency medicine training programs. Acad Emerg Med. 2008;15(1):45–53. doi: 10.1111/j.1553-2712.2007.00008.x. [DOI] [PubMed] [Google Scholar]
- 117.Hughes PH, Conard SE, Baldwin DC, et al. Resident physician substance use in the United States. JAMA. 1991;265(16):2069–73. [PubMed] [Google Scholar]
- 118.Hughes PH, Storr CL, Brandenburg NA, et al. Physician substance use by medical specialty. J Addict Dis. 1999;18(2):23–37. doi: 10.1300/J069v18n02_03. [DOI] [PubMed] [Google Scholar]
- 119.Cottler LB, Ajinkya S, Merlo LJ, et al. Lifetime psychiatric and substance use disorders among impaired physicians in a physicians health program: comparison to a general treatment population. J Addict Med. 2013;7(2):108. doi: 10.1097/ADM.0b013e31827fadc9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.McLellan AT, Skipper GS, Campbell M, et al. Five year outcomes in a cohort study of physicians treated for substance use disorders in the United States. BMJ. 2008;337:a2038. doi: 10.1136/bmj.a2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Active Physicians in the Largest Specialties. American Association of Medical Colleges; 2017. [Accessed March 14, 2019]. Available at: https://www.aamc.org/data/workforce/reports/492556/1-1-chart.html. [Google Scholar]
- 122.Frank E, Brogan D, Schiffman M. Prevalence and correlates of harassment among US women physicians. Arch Intern Med. 1998;158(4):352–8. doi: 10.1001/archinte.158.4.352. [DOI] [PubMed] [Google Scholar]
- 123.Schernhammer E. Taking their own lives -- the high rate of physician suicide. N Engl J Med. 2005;352(24):2473–6. doi: 10.1056/NEJMp058014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.