Abstract
Introduction:
In order to address health disparities, it is important to understand how vulnerable individuals seek information. This study used an adapted version of the Health Information National Trends Survey (HINTS) administered in English, Spanish, and Chinese to describe the behaviors and preferences of a diverse group of vulnerable urban residents.
Methods:
We administered a modified HINTS survey in English, Spanish, and Chinese and used purposive sampling to ensure 50% were non-English speakers evenly divided between Spanish and Chinese speakers and 50% of English-speakers identified as Black. We use multivariable logistic regression to determine characteristics associated with sources used for health information and preferences for delivery of health information.
Results:
Of 1027 survey respondents (514 English, 256 Spanish, 260 Chinese), 55% had adequate health literacy, and 50% reported household income <$20,000, but 77% reported owning a smartphone. A plurality sought health information on the Internet (39%) or from a healthcare provider (36%). In multivariable analyses, smartphone ownership predicted higher odds of seeking health information on the Internet (odds ratio [OR] 2.98; 95% confidence interval [CI] 1.81, 4.91). Participants most preferred email (41%) and brochures (40%) for delivery of health information, but non-English-survey respondents were less likely to prefer email: Spanish (OR 0.30; 95% CI 0.11, 0.83); Chinese (OR 0.25; 95% CI 0.09, 0.71). Smartphone ownership predicted an email preference (OR 2.19; 95% CI 1.43, 3.36).
Conclusion:
Among vulnerable populations, smartphone ownership and language preferences impact preferences for seeking and receiving health information. These preferences need to be considered in designing health messages.
Keywords: Vulnerable Populations, Digital Divide, Information Seeking Behavior, Limited English Proficiency
INTRODUCTION
The Internet and social media have revolutionized communication, impacting healthcare and public health. Nearly 90% of Americans currently have internet access,1 and this growth has coincided with an increase in the use of the Internet to seek health information. Although both individuals and providers have concerns about the quality of online health information,2,3 a 2013 study estimated that one in three Americans has used the Internet to self-diagnose a medical condition.4 A more recent study found that nearly half of Americans first consulted the Internet for information about health or medical topics.5
Despite this overall increasing access, older, lower income, and less educated US adults have lower rates of access to the internet.1 Furthermore, non-White and lower income Americans are more likely to access the Internet solely through their mobile devices.1 As a result of these internet access disparities, vulnerable populations (e.g., non-White, lower-income, older, less-educated and limited English proficient individuals) less frequently seek health information online or communicate with providers using platforms such as patient portals.6–9
Low-income, limited English proficient (LEP), non-White populations also have well-documented disparities in healthcare outcomes.10 In an effort to provide patient-centered care, healthcare providers are increasingly using technology to communicate health information to patients.11 However, if these populations consult the Internet less frequently for health information, without careful attention, reliance on technology to disseminate health information may further exacerbate inequities.12
Since 2003, individual health information seeking behaviors have been surveyed by the Health Information National Trends Survey (HINTS).13 Organizations have used findings from this survey to determine how to disseminate health information to their members and patients. However, this survey is available only in English and Spanish, therefore limiting its utility for populations with large non-English/Spanish-speaking populations, such as San Francisco, where the most common non-English language is Chinese.14 Furthermore, HINTS does not include an assessment of health literacy, which may affect the impact of language on health information seeking behaviors and preferences. Moreover, limited research has been conducted on how low-income, LEP, non-White individuals who own smartphones (and likely more frequently use the Internet, email, or text message) may differ from non-smartphone owning vulnerable individuals in their behaviors for seeking and preferences for receiving health information.
Given these gaps in knowledge, as part of a larger effort to address local San Francisco disparities in cancer prevention and control, we were awarded funding by the National Cancer Institute to create and administer a modified HINTS to better understand the health information seeking behaviors and preferences of vulnerable San Francisco residents. Specifically, part of this survey assessed what sources participants currently use when seeking health information (i.e., health information seeking behaviors) and how they preferred that providers delivered health information (i.e., health information preferences). As a racially and linguistically diverse population near technology-rich Silicon Valley, surveying this population provides new insights into the health information seeking behaviors and preferences in Chinese and Spanish-speaking populations as well as the impact of English proficiency, health literacy, and smartphone ownership on health information seeking behaviors in vulnerable populations. Through these insights, this report aims to provide guidance on considerations when disseminating health information to diverse, vulnerable populations.
METHODS
Research Setting
The City and County of San Francisco is a highly diverse community where Whites are less than half of the population. Asians comprise 34%, Latinos 15%, and African Americans 5% of the population. Approximately 40% of the population speak languages other than English, with Chinese as the most common non-English language and spoken by 17% of San Francisco residents.14
Survey Development
We used a pool of HINTS survey questions13 in English and Spanish and included validated additional questions about healthcare access15 and health literacy16 to create our local survey (SF HINTS). (Development of the full survey is described in greater detail in a forthcoming paper; English survey is available as Supplemental Digital Content 1 with relevant questions in sections A-D, G and H.) To create the Chinese survey, we used a standard dual-reviewer process:18 a staff member directly translated questions from the English SF HINTS and a second individual back-translated it into English to verify accuracy. The same process was used for the Spanish survey for questions that did not already exist in Spanish. All three surveys (English, Spanish, Chinese) were pilot-tested with community advisors and selected participants to ensure cultural appropriateness and translation accuracy prior to full implementation.
Sampling Procedure
We conducted community-based snowball sampling with pre-specified targets for language and race/ethnicity to optimize response rates in our target populations. We aimed for 50% of surveys to be completed in English, of which half the participants would be African-American, and for the non-English surveys to be equally divided between Spanish and Chinese surveys.
Recruitment and Survey Administration
We worked with community partners to spread awareness of and support for the survey by engaging in monthly community advisory meetings. From May to September 2017, our bilingual and bicultural research staff administered the survey in-person on tablet devices at popular community establishments (e.g., restaurants, churches, salons, and community centers), community events (e.g., health and wellness fairs, street fairs, and support groups), and small-businesses and street locations in specific neighborhoods to target populations of interest. Trained bilingual staff explained the purpose of the survey using approved verbal consent language and administered the survey in the participants’ preferred language. A small token of $25 was provided to participants. The University of California, San Francisco Institutional Review Board approved this study.
Variables
We collected sociodemographic characteristics of participants based on self-report: age, sex, race/ethnicity, US-born (or nativity), preferred language, English proficiency, highest education attained, health literacy, and household income. We also collected self-reported health status, access to at least one usual source of care, and ownership of a smartphone (such as an iPhone, Android, Blackberry, or Windows phone). English proficiency and health literacy were dichotomized into adequate or not. (English proficiency was adequate if participants spoke English “well” or “very well”; health literacy was adequate if participants reported feeling “quite a bit” or “extremely comfortable” completing medical forms independently.) For analyses, age was grouped into four categories (18–35, 36–49, 50–64, 65+), as was education (less than high school; high school or equivalent; some college / vocational training; at least college graduate). Household income data were also aggregated into five categories (<$10,000; $10000 to <$20000; $20000 to <$35000; $35000 to <$50000; $50000+).
Outcomes of Interest
We report participants’ health information seeking behaviors and preferences. We report if participants sought health information (question A1 in Supplemental Digital Content 1, or SDC 1) as a binary variable (yes versus no / don’t know / refused) and what sources (e.g., books, brochures, Internet) participants used for health information (question A2 in SDC 1). Although question A2 intends to identify one source for each participant, survey administration and coding resulted in participants being asked about their use of every source. Therefore, each source is reported as its own binary outcome variable (yes versus no); we report only sources that were used by at least 10% of survey participants. We also combined family and friend/coworker, as these are similar concepts for social support; this combined variable is also reported as binary variable (yes for either family or friend/coworker versus no for either).
In addition, we report participants’ preferences for how providers deliver health information (question A3 in SDC 1). Each information source was its own binary outcome variable (yes versus no), and we again only report sources preferred by at least 10% of survey participants.
Statistical Analyses
We used descriptive statistics to report the sociodemographic characteristics and health information seeking behaviors and preferences of survey participants. We used chi-squared analyses with a significance level of p < 0.05 to assess baseline differences by preferred language in sociodemographic characteristics, smartphone ownership, health status, and usual source of care; for differences between specific language groups, we used a Bonferroni correction (significance at p < 0.0167).
We also conduct multivariable logistic regression analyses to determine traits associated with the sources used for health information and preferences for how providers deliver health information. Seven variables that have been previously established in literature to impact health information seeking behaviors were included in every multivariable model: age, sex, race/ethnicity, preferred language, English proficiency, education, and income. Five variables (US-born/nativity, health literacy, self-reported health status, at least one usual source of care, and smartphone ownership) and two-way interactions between five variables (preferred language, English-proficiency, US-born/nativity, education, and race/ethnicity) were included in multivariable models only if found to be significant at p < 0.10 in a bivariable analysis with the outcome of interest. Prior to model creation, we used a multiple imputation by chained equations (MICE) procedure to address missing values for income range, assuming data were missing at random. Imputation was done using SAS 9.4 (Cary, North Carolina, US). We determined that there was no statistically significant collinearity (tolerance > 0.10) between predictor variables and used Stata 15.1 (College Station, Texas, US) to conduct the logistic regression analyses.
RESULTS
Participant Characteristics
The study team administered a total of 1027 surveys; approximately half were in English (514), one-quarter in Spanish (256) and one-quarter in Chinese (257). (Table 1) Chinese survey respondents were older than English survey respondents (mean age: 52.8 vs 44.8, p < 0.001). The English survey included many participants that identified as Hispanic (22%) and Asian (11%). A large portion of both the Spanish-survey respondents (43%) and Chinese-survey respondents (34%) reported adequate English proficiency despite preferring a non-English language, although both groups reported lower proficiency than English-survey respondents (95%, p < 0.0167). Lower rates of higher educational attainment were reported for both Spanish and Chinese-survey respondents compared to English-survey respondents (p < 0.0167). However, Chinese-survey respondents reported more vulnerabilities -- lower health literacy, worse health, and lack of usual source of care -- compared to both English-survey and Spanish-survey respondents with no significant differences between English-survey and Spanish-survey respondents (p < 0.0167). Smartphone ownership (overall: 77%) was significantly lower among Chinese-survey respondents compared to Spanish-survey respondents (71% vs 82% respectively, p = 0.002) but not English-survey respondents (77%).
Table 1.
Demographic Characteristics of Participants by Preferred Language
| Characteristic Trait | All (n = 1027) | English (n = 514) | Spanish (n = 256) | Chinese (n = 257) |
|---|---|---|---|---|
| Age (mean, SD) † ˆ | 47.4 (16.7) | 44.8 (15.6) | 47.0 (15.3) | 52.8 (18.9) |
| Female (n, %) | 536 (52.2%) | 286 (55.6%) | 122 (47.7%) | 128 (49.8%) |
| Race / Ethnicity (n, %) ‡ | ||||
| Non-Hispanic White | 44 (4.3%) | 43 (8.4%) | 1 (0.4%) | 0 (0.0%) |
| Non-Hispanic Black | 243 (23.7%) | 242 (47.1%) | 1 (0.4%) | 0 (0.0%) |
| Hispanic / Latinx | 365 (35.5%) | 115 (22.4%) | 250 (97.7%) | 0 (0.0%) |
| Non-Hispanic Asian / Pacific-Islander | 317 (30.9%) | 58 (11.3%) | 2 (0.8%) | 257 (100.0%) |
| Other | 58 (5.7%) | 56 (10.9%) | 2 (0.8%) | 0 (0.0%) |
| Born in the US (n, %) ‡ § † | 482 (46.9%) | 424 (82.5%) | 33 (12.9%) | 25 (9.7%) |
| Adequate English Proficiency (n, %) ‡ § † | 683 (66.5%) | 487 (94.8%) | 109 (42.6%) | 87 (33.9%) |
| Highest Education Attained (n, %) ‡ § † | ||||
| Less than high school | 236 (23.0%) | 61 (11.9%) | 88 (34.4%) | 87 (33.9%) |
| High school or equivalent | 305 (29.7%) | 160 (31.5%) | 75 (29.3%) | 70 (27.2%) |
| Some college / vocational training | 284 (27.7%) | 167 (32.9%) | 59 (23.1%) | 58 (27.6%) |
| At least college graduate | 186 (18.1%) | 115 (22.4%) | 31 (12.1%) | 40 (15.6%) |
| Adequate Health Literacy (n, %) ‡ † ˆ | 565 (55.0%) | 322 (62.6%) | 148 (57.8%) | 95 (37.0%) |
| Household Income ‡ † | ||||
| < $10,000 | 237 (23.1%) | 129 (25.1%) | 58 (22.7%) | 50 (19.5%) |
| $10,000 to < $20,000 | 274 (26.7%) | 117 (22.8%) | 62 (24.2%) | 95 (37.0%) |
| $20,000 to < $35,000 | 111 (10.8%) | 50 (9.7%) | 33 (12.9%) | 28 (10.9%) |
| $35,000 to < $50,000 | 110 (10.7%) | 58 (11.3%) | 28 (10.9%) | 24 (9.3%) |
| $50,000 and above | 158 (15.4%) | 94 (18.3%) | 30 (11.7%) | 34 (13.2%) |
| Smartphone ownership (n, %) ‡ ˆ | 791 (77.0%) | 398 (77.4%) | 211 (82.4%) | 182 (70.8%) |
| At least good health status ‡ † ˆ | 681 (66.3%) | 375 (73.0%) | 167 (65.2%) | 139 (54.1%) |
| At least one usual source of care ‡ † ˆ | 848 (82.7%) | 431 (84.2%) | 222 (86.7%) | 195 (75.9%) |
significant differences among all groups (p < 0.05)
significant differences between English and Spanish survey respondents (p < 0.0167)
significant differences between English and Chinese survey respondents (p < 0.0167)
significant differences between Spanish and Chinese survey respondents (p < 0.0167)
Note: Data was missing for < 10 participants for gender, education, presence of usual source of care; 17 participants for their country of birth; 22 participants for education; and 107 participants for household income
Health Information Seeking Behaviors
A majority of participants frequently sought health information (overall: 801 participants, or 78%) with no significant differences by preferred language (80% English-survey; 77% Spanish-survey; 75% Chinese-survey; p > 0.05). In a multivariable analysis, older age, higher education, smartphone ownership, and access to a usual source of care were associated with increased odds of searching for health information (p < 0.05; see Supplemental Digital Content 2).
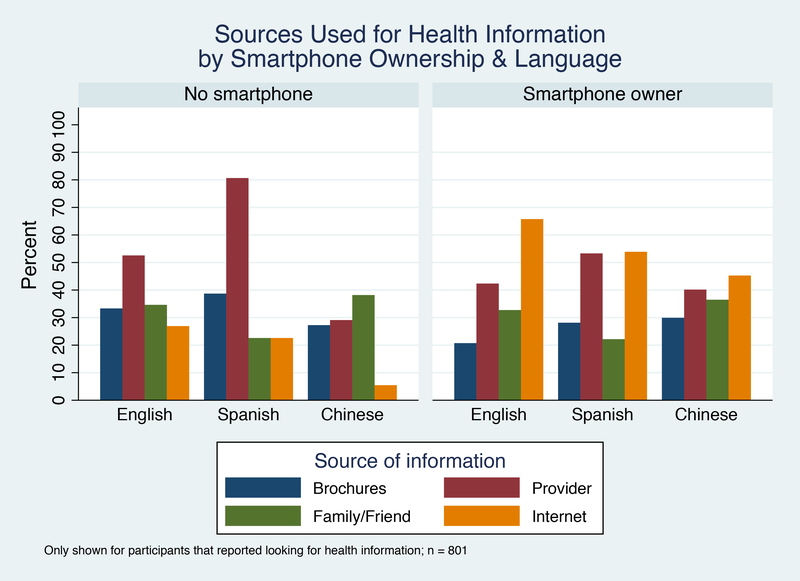
Only four sources (brochures, family or friends, provider, and Internet) were used by at least 15% of the survey respondents with healthcare provider (36%) and Internet (39%) as the most frequently used sources of information. The populations that used each source were different; smartphone users most frequently used the Internet as a source of health information while non-smartphone owners most frequently consulted their providers. These differences are shown by preferred language and smartphone ownership status in Figure 1. (Supplemental Digital Content 3 reports differences in sources used by language).
Figure 1 –
Sources Used for Health Information by Smartphone Ownership and Language
Multivariable models show traits associated with use of brochures, family/friends, providers, or Internet as a source of health information. (Table 2 shows results of the multivariable analyses; bivariable analyses results are presented in Supplemental Digital Content 4). Only education and smartphone ownership were significant factors in more than one multivariable model. Higher educational status was found to be significantly associated with more frequent use of family/friends or Internet but less frequent use of healthcare providers (p < 0.05). Smartphone ownership was both associated with increased odds of using the Internet (odds ratio [OR] 2.98; 95% confidence interval [CI] 1.81, 4.91) and decreased odds of using brochures for health information (OR 0.64; 95% CI 0.41, 0.99). Older and Black survey participants were less likely to use the Internet (p < 0.05). Spanish-survey respondents were less likely to use their family/friends for health information (OR 0.21; 95% CI 0.06, 0.69) but this relationship was reversed among English proficient Spanish-survey respondents (OR 3.96; 95% CI 1.13, 13.94). Participants with a usual source of care had higher odds of using their provider as a source of health information (OR 2.27; 95% CI 1.41, 3.63). Income and gender were not found to be significant predictors for use of any particular source of information.
Table 2.
Multivariable logistic regression models for odds of reporting use of each source for health information (n = 801)
| Predictor | Brochures (n = 799) | Family/ Friends (n = 799) | Provider (n = 794) | Internet (n = 789) |
|---|---|---|---|---|
| OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| Age § | ||||
| 18–35 years | 1.15 [0.63, 2.11] | 1.64 [0.95, 2.86] | 0.93 [0.55, 1.56] | 3.65 [1.98, 6.73] ‡ |
| 36–49 years | 1.40 [0.80, 2.47] | 0.95 [0.55, 1.66] | 0.94 [0.57, 1.54] | 3.08 [1.73, 5.49] ‡ |
| 50–64 years | 1.43 [0.85, 2.42] | 0.73 [0.43, 1.23] | 1.10 [0.69, 1.75] | 1.23 [0.71, 2.14] |
| Female | 1.25 [0.89, 1.76] | 0.77 [0.56, 1.07] | 0.99 [0.73, 1.34] | 1.10 [0.78, 1.55] |
| Race/ethnicity § | ||||
| Black | 0.94 [0.41, 2.18] | 1.50 [0.66, 3.40] | 0.62 [0.30, 1.29] | 0.42 [0.18, 0.99] ‡ |
| Hispanic | 0.70 [0.29, 1.70] | 1.40 [0.59, 3.29] | 0.76 [0.35, 1.64] | 1.22 [0.49, 3.06] |
| Asian | 1.15 [0.41, 3.21] | 2.04 [0.77, 5.38] | 0.53 [0.20, 1.37] | 0.72 [0.24, 2.18] |
| Other | 0.88 [0.31, 2.47] | 1.68 [0.64, 4.45] | 1.37 [0.55, 3.38] | 0.69 [0.25, 1.94] |
| Language § | ||||
| Spanish | 1.35 [0.67, 2.70] | 0.21 [0.06, 0.69] ‡ | 1.25 [0.68, 2.29] | 0.93 [0.26, 3.32] |
| Chinese | 0.82 [0.39, 1.73] | 0.50 [0.17, 1.50] | 0.80 [0.39,1.66] | 0.92 [0.27, 3.10] |
| English proficient | 0.99 [0.60, 1.65] | 0.59 [0.16, 2.16] | 1.17 [0.71, 1.92] | 2.29 [0.72, 7.24] |
| Education § | ||||
| High school graduate / equivalent | 1.16 [0.72, 1.86] | 0.97 [0.50, 1.90] | 0.81 [0.52, 1.25] | 1.55 [0.93, 2.57] |
| Some college / vocational training | 1.13 [0.66, 1.92] | 2.36 [1.01, 5.53] ‡ | 0.91 [0.57, 1.46] | 2.05 [1.20, 3.51] ‡ |
| College grad | 1.60 [0.88, 2.89] | 0.48 [0.14, 1.68] | 0.57 [0.33, 0.98] ‡ | 2.07 [1.12, 3.83] |
| Household Income § | ||||
| 10 to <20K | 0.80 [0.52, 1.24] | 0.85 [0.55, 1.30] | 0.96 [0.65, 1.43] | 1.18 [0.75, 1.86] |
| 20 to <35K | 1.04 [0.59, 1.81] | 0.94 [0.55, 1.62] | 0.80 [0.48, 1.33] | 1.92 [1.09, 3.36] |
| 35 to <50K | 0.86 [0.49, 1.53] | 1.04 [0.60, 1.78] | 0.67 [0.40, 1.13] | 1.49 [0.85, 2.61] |
| 50K | 0.71 [0.40, 1.27] | 0.60 [0.34, 1.04] | 0.76 [0.46, 1.26] | 2.27 [1.27, 4.03] |
| US-born | 0.58 [0.33, 1.02] | -- | 2.42 [0.53, 11.12] | 1.15 [0.65, 2.01] |
| Health literate | -- | -- | -- | 1.08 [0.75, 1.54] |
| Smartphone owner | 0.64 [0.41, 0.99] ‡ | -- | -- | 2.98 [1.81, 4.91] ‡ |
| At least good health status | -- | -- | -- | 0.81 [0.55, 1.18] |
| At least one usual source of care | -- | -- | 2.27 [1.41, 3.63] ‡ | -- |
| English proficient * US-born † | -- | -- | 0.28 [0.06, 1.33] | -- |
| English proficient * Spanish † | -- | 3.96 [1.13, 13.94] ‡ | -- | 0.43 [0.12, 1.56] |
| English proficient * Chinese † | -- | 1.33 [0.39, 4.49] | -- | 0.45 [0.12, 1.72] |
| English proficient * HS grad † | -- | 0.93 [0.36, 2.42] | -- | -- |
| English proficient * Some college † | -- | 0.38 [0.13, 1.13] | -- | -- |
| English proficient * College grad † | -- | 1.61 [0.38, 6.86] | -- | -- |
p < 0.05
The reference group for each variable is: age (65+ years); race/ethnicity (non-Hispanic White); language (English); education (less than high school graduate); and household income (<$10000)
An interaction term
Notes: Odds ratios (OR) and confidence intervals (CI) are only reported for variables included in each model.
Health Information Seeking Preferences
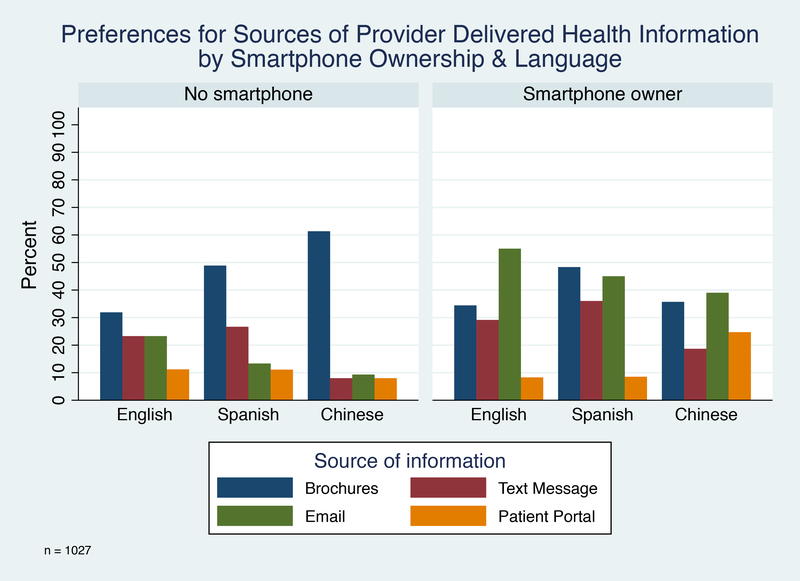
Preferences for delivery of health information are shown by preferred language and smartphone ownership in figure 2. (Supplemental Digital Content 3 presents this data by language only.) Of the options on the survey, participants most frequently preferred email (overall: 425 participants, 41%) and brochures (overall: 409 participants, 40%) over text message (overall: 26%) or patient portal (overall: 12%).
Figure 2 –
Preferences for Sources of Provider Delivered Health Information by Smartphone Ownership and Language
Age was an important predictor of preferences for all four types of information with increasing age predicting high preference for brochures but lower preference for text message, email, and patient portal (p < 0.05). (Table 3 shows results of the multivariable analyses; results of bivariable analyses are presented in Supplemental Digital Content 5.) In multivariable analyses, a non-English language preference was associated with lower odds of preferring email (Spanish-survey: OR 0.30, 95% CI 0.11, 0.83; Chinese-survey: OR 0.25, 95% CI 0.09, 0.71) but higher odds of preferring patient portals for Chinese-survey respondents (OR 6.08; 95% CI 1.76, 20.99). Smartphone-owning participants were more likely to prefer both text message and email (p < 0.05). Blacks and Asians were less likely to prefer patient portals (p < 0.05) while higher educated, higher income participants preferred email (p < 0.05). Women were more likely to prefer brochures (OR 1.47; 95% CI 1.11, 1.94) while US-born / native respondents were less likely to prefer brochures (OR 0.62; 95% CI 0.38, 0.99).
Table 3.
Multivariable logistic regression models for odds of preferring each type of media for provider delivery of health information (n = 1027)
| Predictor | Brochures (n = 1016) | Text Message (n =1024) | Email (n = 1002) | Patient Portal (n = 1024) |
|---|---|---|---|---|
| OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| Age § | ||||
| 18–35 years | 0.36 [0.22, 0.60] ‡ | 2.53 [1.39, 4.62] ‡ | 3.42 [1.96, 5.95] ‡ | 2.25 [1.06, 4.81] ‡ |
| 36–49 years | 0.50 [0.32, 0.79] ‡ | 3.15 [1.76, 5.63] ‡ | 2.11 [1.23, 3.62] ‡ | 1.65 [0.77, 3.50] |
| 50–64 years | 0.64 [0.42, 0.97] ‡ | 2.46 [1.40, 4.32] ‡ | 1.20 [0.71, 2.03] | 1.92 [0.96, 3.85] |
| Female | 1.47 [1.11, 1.94] ‡ | 0.97 [0.72, 1.31] | 0.86 [0.64, 1.16] | 0.91 [0.60, 1.38] |
| Race/ethnicity § | ||||
| Black | 1.16 [0.55, 2.44] | 1.21 [0.55, 2.64] | 1.63 [0.77, 3.40] | 0.34 [0.13, 0.88] ‡ |
| Hispanic | 1.42 [0.65, 3.12] | 1.23 [0.52, 2.81] | 1.16 [0.54, 2.53] | 0.63 [0.24, 1.62] |
| Asian | 1.55 [0.62, 3.85] | 0.86 [0.32, 2.28] | 1.06 [0.42, 2.63] | 0.22 [0.05, 0.89] ‡ |
| Other | 1.17[0.48, 2.86] | 0.89 [0.34, 2.30] | 1.47 [0.61, 3.54] | 0.44 [0.13, 1.47] |
| Language § | ||||
| Spanish | 0.89 [0.51, 1.56] | 1.21 [0.72, 2.05] | 0.30 [0.11, 0.83] ‡ | 0.77 [0.37, 1.63] |
| Chinese | 0.56 [0.29, 1.08] | 0.81 [0.38, 1.74] | 0.25 [0.09, 0.71] ‡ | 6.08 [1.76, 20.99] ‡ |
| English proficient | 0.71 [0.46, 1.08] | 1.15 [0.74, 1.80] | 0.51 [0.20, 1.26] | 0.88 [0.48, 1.60] |
| Education § | ||||
| High school graduate / equivalent | 0.69 [0.47, 1.01] | 1.17 [0.77, 1.78] | 1.45 [0.92, 2.29] | 1.08 [0.58, 2.00] |
| Some college / vocational training | 0.88 [0.57, 1.35] | 0.77 [0.48, 1.22] | 1.90 [1.17, 3.07] ‡ | 1.42 [0.73, 2.74] |
| College grad | 0.76 [0.46, 1.25] | 0.65 [0.37, 1.14] | 2.57 [1.48, 4.44] ‡ | 1.39 [0.67, 2.91] |
| Household Income § | ||||
| 10 to <20K | 0.96 [0.67, 1.36] | 1.02 [0.69, 1.49] | 1.22 [0.82, 1.83] | 0.80 [0.46, 1.40] |
| 20 to <35K | 1.45 [0.91, 2.31] | 1.09 [0.67, 1.77] | 1.54 [0.94, 2.50] | 1.17 [0.60, 2.28] |
| 35 to <50K | 1.57 [0.98, 2.52] | 0.74 [0.44, 1.23] | 1.67 [1.02, 2.73] ‡ | 1.15 [0.59, 2.26] |
| 50K | 1.15 [0.72, 1.86] | 0.75 [0.45, 1.24] | 2.00 [1.22, 3.28] ‡ | 1.02 [0.52, 1.99] |
| US-born | 0.62 [0.38, 0.99] ‡ | -- | 0.84 [0.53, 1.33] | -- |
| Health literate | -- | -- | 0.91 [0.67, 1.24] | -- |
| Smartphone owner | 1.01 [0.70, 1.44] | 1.55 [1.03, 2.33] ‡ | 2.19 [1.43, 3.36] ‡ | -- |
| At least good health status | -- | -- | 1.12 [0.81, 1.56] | -- |
| At least one usual source of care | 1.20 [0.82, 1.75] | -- | -- | -- |
| English proficient * Spanish | -- | -- | 4.69 [1.62, 13.59] | -- |
| English proficient * Chinese | -- | -- | 3.61 [1.20, 10.83] | -- |
p < 0.05
The reference group for each variable is: age (65+ years); race/ethnicity (non-Hispanic White); language (English); education (less than high school graduate); and household income (<$10000)
An interaction term
Notes: Odds ratios (OR) and confidence intervals (CI) are only reported for variables used in each model.
DISCUSSION
In this study of health information seeking behaviors and preferences of a multi-lingual vulnerable cohort, we found that both language preference and smartphone ownership were significant predictors after accounting for known predictors of health information seeking behaviors and preferences, namely age, race/ethnicity, education and income. 5–9 Language preference was an important predictor among Chinese-speakers, a population not assessed by the parent national HINTS. Language was also important after accounting for English proficiency and health literacy, which is not currently assessed on HINTS. We also found rates of smartphone ownership (77%) in this vulnerable population consistent with that of the US population (78.2%) and higher than the most recent HINTS survey in 2017 (72.6%: HINTS 5, cycle 1).13 This study also oversampled from vulnerable populations that are less represented in the national HINTS survey (2017 national HINTS sample vs SF HINTS sample: 42% household income < $50,000 vs 85%; 2% LEP vs 33%; 13% Non-Hispanic Black vs 24%; 84% native-born vs 47%).13
We found that language preference (even after considering English proficiency, nativity, and health literacy) impacted how frequently participants consulted friends/family for health information as well as their preference for email or patient portals to receive health information. Language was a more important (significant) predictor than English proficiency, which was not significantly associated with any health information seeking behaviors or preferences. This is inconsistent with literature that found English proficiency to predict online health-information seeking behaviors. 8 However, often English proficiency is asked without also assessing participants’ preferred language; these findings support prior studies that advocate assessing both English proficiency and language preference. 19
Nativity was also found to be significantly associated with preferring brochures as a source of information. This is consistent with prior literature that shows nativity predicts health-information seeking behaviors even after adjusting for language preference and English proficiency.9 It is unclear what drives these differences, but it may suggest impact of acculturation that should be further explored.
Patient portals have been widely promoted as patient-centered, but overall few participants in our survey expressed this preference (overall 12%) in receiving health-related information from providers. This does not reflect aversion to mobile technology since participants preferred email (41%) and text message (26%) more frequently. Instead, it likely reflects that patient portal usability is often low and not optimized for mobile use. 20,21 Despite their overall lower use by patients, patient portals show promise in reaching Chinese-speaking population, as Chinese-speakers had higher odds of using them in comparison to other study groups.
The rate of smartphone ownership in this vulnerable population (77%) is consistent with national averages, suggesting the gap in smartphone ownership is starting to close in vulnerable urban populations.22 Our data is consistent with a study in East Harlem that also found high rates of smartphone ownership (82%).23 We also found that even in this vulnerable population, after considering other factors, smartphone ownership predicted use of the Internet or avoidance of brochures for health information as well as preference for email or text messaging for health information delivery. Given the importance of smartphone ownership in vulnerable populations, it is important that efforts to disseminate information to these groups are optimized for mobile viewing. Many health system websites and resources are not mobile friendly,24 potentially worsening information access disparities, since vulnerable groups disproportionately rely on mobile devices to access the Internet. 1
This study is limited by its sample from a single city, but this was done by design to help determine communication efforts for the San Francisco Cancer Initiative (SF CAN), an on-going cancer prevention and early detection dissemination project in San Francisco.25 Despite being a single city, we surveyed over 1000 residents and oversampled from groups that are underrepresented in HINTS.13 Nearly all respondents were members of racial/ethnic minority groups (only 4% were White), and approximately half had household income < $20,000 and limited health literacy. In addition, one-third were limited English proficient. We are unable to report a response rate since survey administrators did not record when approached individuals declined the survey, but in general, reviews of face-to-face surveys show higher survey response rates than other survey methods.26 As a cross-sectional study, we are limited in the conclusions we can draw regarding causation.
Implications
Despite these limitations, this study has implications for members at various levels of the healthcare system. Stakeholders at all levels of the healthcare system need to acknowledge patient differences in health information seeking behaviors and preferences. Effective patient communication cannot occur with a one-size-fits-all approach; to ensure equal information access, health information needs to be tailored to be delivered in a culturally appropriate format.
For public health system leaders, clinicians, and direct healthcare providers in urban safety net settings, there are takeaways for how to deliver information. Although healthcare providers have been incentivized to use patient portals, vulnerable urban patients are less likely to prefer portals, which is consistent with previous literature.27 Instead, text messaging and email are preferred by patients, and is consistent with how patients currently use technology to communicate with their providers.28–30 In particular, providers and population health leaders should consider both language preference and smartphone ownership in considering how to disseminate information to reach all populations since both these factors were important predictors of how participants sought health information.
Health researchers need to concurrently measure language preference, English proficiency, and nativity among study participants to improve understanding about how these factors interact to impact disparities. Moreover, as the prevalence and importance of smartphone ownership in this study shows, greater representation of vulnerable populations in studies allows verification that findings in the general population also apply to vulnerable groups. Specific directions for future research include exploring: if and why patient portals are preferred by Chinese-speakers; the impact of language-concordant Internet or paper materials on preferences; and if provision of smartphone ownership modifies health information seeking behaviors / preferences.
Both developers of health information technology and health policy makers should acknowledge the patient preference for email and text message over current patient-facing health-specific communication tools (e.g., patient portals). Patient portal developers should improve portal usability to better meet the needs of vulnerable populations by learning from mobile health applications. 31 Concurrently, policy makers should consider regulation and encouragement of health information distribution through text message and/or email. In particular, only younger age and smartphone ownership predicted preference for text messaging; otherwise, it was equally preferred among all individuals, suggesting it may have potential to reach many groups.
The findings from this survey describe how a multi-lingual, urban cohort currently seek information and prefer to receive health information. We found language-based differences in where individuals sought information and how they preferred providers to disseminate information. Smartphone ownership was high and significantly impacted participants’ current behaviors for seeking and preferences for receiving health information. To prevent exacerbation of health disparities, preference variations based on language preference and smartphone ownership need to be considered in designing health communication for diverse communities.
Supplementary Material
Acknowledgements:
We want to acknowledge Cynthia Cheung, Corina Liew, Alejo Perez-Stable, Francisco Quintanilla, Pamela Williams, Ching Wong as well as the San Francisco Cancer Initiative Steering Committee and the San Francisco HINTS steering committee (Anna Napoles, Tung Nguyen, Rena Pasick). We also want to acknowledge community partners including Angela Sun at the Chinese Community Health Resource Center and Monique LaSalle at the Rafiki Health Center.
Funding Information
National Cancer Institute (P30CA082103–18S7)
National Institute for Health’s National Research Service Award (grant number T32HP19025)
Footnotes
Conflicts of Interest:
Our study has multiple authors. None of us have any competing interests.
Contributor Information
Elaine C. Khoong, Division of General Internal Medicine, Dept. of Medicine, University of California San Francisco, San Francisco, CA, USA, elaine.khoong@ucsf.edu.
Gem Le, Division of General Internal Medicine, Dept. of Medicine at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, CA, USA; Center for Vulnerable Populations at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, CA, USA, gem.le@ucsf.edu.
Mekhala Hoskote, Division of General Internal Medicine, Dept. of Medicine at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, CA, USA; Center for Vulnerable Populations at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, CA, USA, mekhala.hoskote@ucsf.edu.
Natalie Rivadeneira, Division of General Internal Medicine, Dept. of Medicine at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, CA, USA; Center for Vulnerable Populations at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, CA, USA, natalie.rivadeneira@ucsf.edu.
Robert A. Hiatt, Dept. of Epidemiology and Biostatistics, University of California San Francisco, San Francisco, CA, USA; UCSF Hellen Diller Family Comprehensive Cancer Center, University of California San Francisco, San Francisco, CA, USA, robert.hiatt@ucsf.edu.
Urmimala Sarkar, Division of General Internal Medicine, Dept.of Medicine at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, CA, USA; Center for Vulnerable Populations at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, CA, USA, urmimala.sarkar@ucsf.edu.
REFERENCES
- 1.Pew Research Center. Demographics of Internet and Home Broadband Usage in the United States [Internet]. [cited 2018 Jul 30]. Available from: http://www.pewinternet.org/fact-sheet/internet-broadband/
- 2.Silver MP. Patient Perspectives on Online Health Information and Communication With Doctors: A Qualitative Study of Patients 50 Years Old and Over. J Med Internet Res. 2015. January 13;17(1):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eysenbach G, Powell J, Kuss O, Sa E-R. Empirical Studies Assessing the Quality of Health Information for Consumers on the World Wide Web. JAMA. 2002. May 22;287(20):2691. [DOI] [PubMed] [Google Scholar]
- 4.Pew Research Center. Health Online [Internet]. 2013. [cited 2018 Feb 1]. p. 1–55. Available from: http://www.pewinternet.org/2013/01/15/health-online-2013/
- 5.Jacobs W, Amuta AO, Jeon KC. Health information seeking in the digital age: An analysis of health information seeking behavior among US adults. Alvares C, editor. Cogent Soc Sci. 2017. March 13;3(1). [Google Scholar]
- 6.Kontos E, Blake KD, Chou W-YS, Prestin A. Predictors of eHealth Usage: Insights on The Digital Divide From the Health Information National Trends Survey 2012. J Med Internet Res. 2014. July 16;16(7):e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gordon NP, Hornbrook MC. Differences in Access to and Preferences for Using Patient Portals and Other eHealth Technologies Based on Race, Ethnicity, and Age: A Database and Survey Study of Seniors in a Large Health Plan. J Med Internet Res. 2016. March 4;18(3):e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen A, Mosadeghi S, Almario CV. Persistent digital divide in access to and use of the Internet as a resource for health information: Results from a California population-based study. Int J Med Inform. 2017. July 1;103:49–54. [DOI] [PubMed] [Google Scholar]
- 9.Massey PM, Langellier BA, Sentell T, Manganello J. Nativity and language preference as drivers of health information seeking: examining differences and trends from a U.S. population-based survey. Ethn Health. 2017. November 2;22(6):596–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality. 2016 National Health Quality and Disparities Report. 2017;AHRQ Pub; No. 17–0001. [Google Scholar]
- 11.Crotty BH, Tamrat Y, Mostaghimi A, Safran C, Landon BE. Patient-To-Physician Messaging: Volume Nearly Tripled As More Patients Joined System, But Per Capita Rate Plateaued. Health Aff. 2014. October 1;33(10):1817–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lyles C, Schillinger D, Sarkar U. Connecting the Dots: Health Information Technology Expansion and Health Disparities. PLOS Med. 2015. July 14;12(7):e1001852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Cancer Institute. Health Information National Trends Survey [Internet]. Vol. 2016. 2018. [cited 2018 Sep 23]. Available from: https://hints.cancer.gov/about-hints/learn-more-about-hints.aspx
- 14.San Francisco, CA | Data USA [Internet]. [cited 2018 Feb 1]. Available from: https://datausa.io/profile/geo/san-francisco-ca/
- 15.Centers for Disease Control and Prevention. National Health Interview Survey (NHIS) [Internet]. Vol. 2013. 2013. [cited 2018 Feb 9]. Available from: http://www.cdc.gov/nchs/nhis/about_nhis.htm
- 16.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, et al. Validation of Screening Questions for Limited Health Literacy in a Large VA Outpatient Population. J Gen Intern Med. 2008. May 12;23(5):561–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United States Census Bureau. Language Use [Internet]. 2017. [cited 2018 Sep 23]. Available from: https://www.census.gov/topics/population/language-use/about/faqs.html
- 18.Maneesriwongul W, Dixon JK. Instrument translation process: a methods review. J Adv Nurs. 2004. October;48(2):175–86. [DOI] [PubMed] [Google Scholar]
- 19.Karliner LS, Napoles-Springer AM, Schillinger D, Bibbins-Domingo K, Pérez-Stable EJ. Identification of Limited English Proficient Patients in Clinical Care. J Gen Intern Med. 2008. October 10;23(10):1555–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tieu L, Schillinger D, Sarkar U, Hoskote M, Hahn KJ, Ratanawongsa N, et al. Online patient websites for electronic health record access among vulnerable populations: portals to nowhere? J Am Med Informatics Assoc. 2016. July 8;24(e1):ocw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Irizarry T, DeVito Dabbs A, Curran CR. Patient Portals and Patient Engagement: A State of the Science Review. J Med Internet Res. 2015. June 23;17(6):e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pew Research Center. Demographics of Mobile Device Ownership and Adoption in the United States [Internet]. 2018. [cited 2018 Jul 30]. Available from: http://www.pewinternet.org/fact-sheet/mobile/
- 23.Vangeepuram N, Mayer V, Fei K, Hanlen-Rosado E, Andrade C, Wright S, et al. Smartphone ownership and perspectives on health apps among a vulnerable population in East Harlem, New York. mHealth. 2018. August;4:31–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheng C, Dunn M. How well are health information websites displayed on mobile phones? Implications for the readability of health information. Heal Promot J Aust. 2017. April;28(1):15–20. [DOI] [PubMed] [Google Scholar]
- 25.Hiatt RA, Sibley A, Fejerman L, Glantz S, Nguyen T, Pasick R, et al. The San Francisco Cancer Initiative: A Community Effort To Reduce The Population Burden Of Cancer. Health Aff. 2018. January;37(1):54–61. [DOI] [PubMed] [Google Scholar]
- 26.Sitzia J, Wood N. Response rate in patient satisfaction research: an analysis of 210 published studies. Int J Qual Heal care J Int Soc Qual Heal Care. 1998. August;10(4):311–7. [DOI] [PubMed] [Google Scholar]
- 27.Haun JN, Patel NR, Lind JD, Antinori N. Large-Scale Survey Findings Inform Patients’ Experiences in Using Secure Messaging to Engage in Patient-Provider Communication and Self-Care Management: A Quantitative Assessment. J Med Internet Res. 2015. December 21;17(12):e282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mirsky JB, Tieu L, Lyles C, Sarkar U. A Mixed-Methods Study of Patient–Provider E-Mail Content in a Safety-Net Setting. J Health Commun. 2016. January 2;21(1):85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schickedanz A, Huang D, Lopez A, Cheung E, Lyles CR, Bodenheimer T, et al. Access, Interest, and Attitudes Toward Electronic Communication for Health Care Among Patients in the Medical Safety Net. J Gen Intern Med. 2013. July 20;28(7):914–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ye J, Rust G, Fry-Johnson Y, Strothers H. E-mail in patient–provider communication: A systematic review. Patient Educ Couns. 2010. August;80(2):266–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baldwin JL, Singh H, Sittig DF, Giardina TD. Patient portals and health apps: Pitfalls, promises, and what one might learn from the other. Healthc (Amsterdam, Netherlands). 2017. September 1;5(3):81–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.