Abstract
Background
Chronic obstructive pulmonary disease (COPD; including chronic bronchitis and emphysema) is a chronic respiratory condition characterised by shortness of breath, cough and recurrent exacerbations. Long‐term antibiotic use may reduce both bacterial load and inflammation in the airways. Studies have shown a reduction of exacerbations with antibiotics in comparison to placebo in people with COPD, but there are concerns about antibiotic resistance and safety.
Objectives
To compare the safety and efficacy of different classes of antibiotics (continuous, intermittent or pulsed) for prophylaxis of exacerbations in patients with COPD.
Search methods
We searched the Cochrane Airways Group Trials Register and bibliographies of relevant studies. The latest literature search was conducted on 6 February 2019.
Selection criteria
Randomised controlled trials (RCTs) were selected that compared one prophylactic antibiotic with another in patients with COPD.
Data collection and analysis
We used the standard Cochrane methods. Two independent review authors selected trials for inclusion, extracted data and assessed risk of bias. Discrepancies were resolved by involving a third review author.
Main results
We included two RCTs, both published in 2015 involving a total of 391 participants with treatment duration of 12 to 13 weeks. One RCT compared a quinolone (moxifloxacin pulsed, for 5 days every 4 weeks), with a tetracycline (doxycycline continuous) or a macrolide (azithromycin intermittent).
The second RCT compared a tetracycline (doxycycline continuous) plus a macrolide (roxithromycin continuous), with roxithromycin (continuous) alone.
The trials recruited participants with a mean age of 68 years, with moderate‐severity COPD. Both trials included participants who had between two and five exacerbations in the previous one to two years. In one trial, 17% of patients had previously been using inhaled corticosteroids. In the other study, all patients were positive for Chlamydophila pneumoniae (C pneumoniae).
Overall, we judged the evidence presented to be of very low‐certainty, mainly due to imprecision, but we also had concerns about indirectness and methodological quality of the included studies. The primary outcome measures for this review included exacerbations, quality of life, drug resistance and serious adverse events.
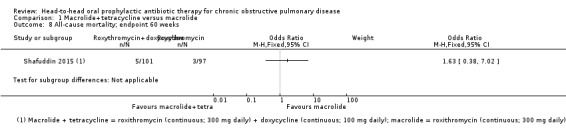
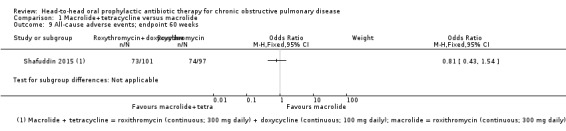
Macrolide + tetracycline versus macrolide
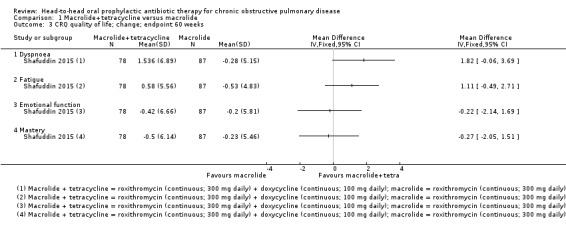
There was no clear difference between treatments in improvement in quality of life as assessed by the Chronic Respiratory Questionnaire (CRQ). The CRQ scale ranges from 0 to 10 and higher scores on the scale indicate better quality of life. CRQ sub‐scales for dyspnoea (mean difference (MD) 0.58, 95% confidence interval (CI) ‐0.84 to 2.00; 187 participants; very low‐certainty evidence), fatigue (MD 0.02, 95% CI ‐1.08 to 1.12; 187 participants; very low‐certainty evidence), emotional function (MD ‐0.37, 95% CI ‐1.74 to 1.00; 187 participants; very low‐certainty evidence), or mastery (MD ‐0.79, 95% CI ‐1.86 to 0.28; 187 participants; very low‐certainty evidence) at 12 weeks. For serious adverse events, it was uncertain if there was a difference between combined roxithromycin and doxycycline versus roxithromycin alone at 48 weeks follow‐up after active treatment of 12 weeks (odds ratio (OR) 1.00, 95% CI 0.52 to 1.93; 198 participants; very low‐certainty evidence). There were five deaths reported in the combined treatment arm, versus three in the single treatment arm at 48 weeks follow‐up after active treatment of 12 weeks (OR 1.63, 95% CI 0.38 to 7.02; 198 participants; very low‐certainty evidence).
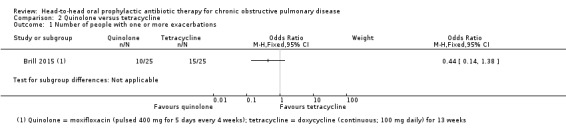
Quinolone versus tetracycline
There was no clear difference between moxifloxacin and doxycycline for the number of participants experiencing one or more exacerbations (OR 0.44, 95% CI 0.14 to 1.38; 50 participants, very low‐certainty evidence) at 13 weeks. There were no serious adverse events or deaths reported in either treatment groups. We did not identify any evidence for our other primary outcomes.
Quinolone versus macrolide
There was no clear difference between moxifloxacin and azithromycin for the number of participants experiencing one or more exacerbations (OR 1.00, 95% CI 0.32 to 3.10; 50 participants; very low‐certainty evidence) at 13 weeks. There were no serious adverse events or deaths reported in either treatment groups. We did not identify any evidence for our other primary outcomes.
Marcolide versus tetracycline
There was no clear difference between azithromycin and doxycycline for the number of participants experiencing one or more exacerbations (OR 0.44, 95% CI 0.14 to 1.38; 50 participants; very low‐certainty evidence) at 13 weeks. There were no serious adverse events or deaths reported in either treatment groups. We did not identify any evidence for our other primary outcomes.
We did not find head‐to‐head evidence for impact of antibiotics on drug resistance.
Authors' conclusions
It is not clear from the evidence included in this review whether there is a difference in efficacy or safety between different classes or regimens of prophylactic antibiotic, given for 12 to 13 weeks to people with COPD. Whilst no head‐to‐head comparisons of antibiotic resistance were identified, concerns about this continue. The sample size in this review is small and both included studies are of short duration. Thus, there is considerable uncertainty in effects observed and the effects of different prophylactic antibiotics requires further research.
Plain language summary
Prophylactic antibiotic therapy for people with chronic obstructive lung disease (COPD)
What is COPD?
COPD is a common condition caused mainly by smoking and can lead to long‐term breathing problems. Symptoms include shortness of breath, and cough with sputum production due to airways and lung damage. Infection can trigger severe symptoms, with breathing becoming worse and increased cough and sputum. This is more commonly known as an exacerbation or 'flare‐up' which can cause further damage to lung function. Frequent exacerbations can lead to hospital admissions, reduced quality of life, and increase the risk of death.
Why did we do this review?
We wanted to know whether one preventative antibiotic was better than another preventative antibiotic in reducing exacerbations, and improving quality of life for people with COPD.
What evidence did we find?
We found two randomised trials, including 391 people with COPD. The participants had an average age of 68 years. The first study included three groups of COPD patients taking either moxifloxacin (daily for 5 days every 4 weeks), doxycycline (daily for 13 weeks) or azithromycin (3 times per week for 13 weeks). The second study investigated the use of doxycycline (daily) in addition to roxithromycin (daily) for 12 weeks in COPD. Our main outcomes were number of exacerbations, quality of life, serious side effects (known as 'adverse events') and antibiotic resistance.
Results and conclusions
Overall, we were unable to determine any difference between one antibiotic compared with each other in improving the main outcomes we measured.
We were unclear whether one antibiotic was better or worse than another in terms of reducing exacerbations or improving quality of life. Neither of the studies reported a comparison between antibiotics for drug resistance.
In one study lasting 13 weeks we found no serious side effects of taking moxifloxacin, azithromycin or doxycycline, and no deaths were reported. In the other study, very similar numbers of people experienced serious side effects in both the combined antibiotic and single antibiotic treatment groups after 12 weeks of treatment and 48 weeks of follow‐up. However, the numbers were small so we are not sure if one treatment option may cause more side effects than the other. In the same study, five people in the combined treatment group died, compared to three people in the single treatment group. Again, these numbers are too small to draw any conclusions.
Certainty of the evidence
We were very uncertain about the results due to finding only two small studies that gave people with COPD antibiotics for only 12 or 13 weeks. The studies only looked at four different antibiotics and did not measure all the things we were interested in.
Summary of findings
Summary of findings for the main comparison. Macrolide+tetracycline versus macrolide.
| Macrolide+tetracycline compared to macrolide for chronic obstructive pulmonary disease | ||||||
| Patient or population: chronic obstructive pulmonary disease Setting: 16 centres across Australia and New Zealand Intervention: roxithromycin (continuous; 300 mg daily) + doxycycline (continuous; 100 mg daily) Comparison: roxithromycin (continuous; 300 mg daily) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with macrolide | Risk with Macrolide+tetracycline | |||||
|
Quality of life, measured by CRQ (dyspnoea, fatigue, emotional function, and mastery subscales) Follow‐up 12 weeks (end of treatment) Scale from 0 to 10. Higher scores on the scale indicates better quality of life |
The mean change in CRQ HRQoL (dyspnoea) was 2.21 |
MD 0.58 higher (0.84 lower to 2.00 higher) | ‐ | 187 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,d | An increase of three points in this domain refers to a clinically significant reduction in dyspnoea (Jaeschke 1989; Jones 2002) |
| The mean change in CRQ HRQoL (fatigue) was 0.68 |
MD 0.02 higher (1.08 lower to 1.12 higher) | ‐ | 187 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,d,e | An increase of four points in this domain refers to a clinically significant reduction in fatigue (Jaeschke 1989; Jones 2002) | |
| The mean change in CRQ HRQoL (emotional function) was 0.45 |
MD 0.37 lower (1.74 lower to 1.00 higher) | ‐ | 187 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,d,f | An increase of two points in this domain refers to a clinically significant improvement in emotional function (Jaeschke 1989; Jones 2002) | |
| The mean change in CRQ HRQoL (mastery) was 0.53 |
MD 0.79 lower (1.86 lower to 0.28 higher) | ‐ | 187 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,d,f | No reported minimally important difference (MID) | |
|
All‐cause serious adverse events 60 weeks (end of study) |
237 per 1000 | 237 per 1000 (139 to 375) | OR 1.00 (0.52 to 1.93) | 198 (1 RCT) | ⊕⊝⊝⊝ Very lowa,d,e,g | |
|
Lung function (trough FEV1) Change from baseline to 12 weeks (end of active treatment) |
The mean change in trough FEV1 was 0.047 L | MD 0.01 L lower (0.09 lower to 0.07 higher) | 182 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,d,f | An improvement of 100 mL (0.1 L) for FEV1 trough is considered clinically significant (Donohue 2005) | |
|
All‐cause mortality 60 weeks (end of study) |
31 per 1000 | 49 per 1000 (12 to 183) | OR 1.63 (0.38 to 7.02) | 198 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,d | |
|
Number of people experiencing one or more exacerbations, Drug resistance/microbial sensitivity (as reported by trialists), including emergence of atypical bacteria, Number of participants colonised with Pseudomonas aeruginosa |
Information for these outcomes was not presented as data for head‐to‐head comparisons were not available | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CRQ: Chronic Respiratory Questionnaire; FEV1: forced expiratory volume in one second; HRQoL: health‐related quality of life; MD: mean difference; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aThe evidence was downgraded by 1 due to attrition bias in the combined treatment arm. bThe evidence was downgraded by 2 due to indirectness of population and intervention. The aim was to assess eradication of C pneumoniae and not antibiotic prophylaxis. The comparison of interventions was not an inclusion criterion of this systematic review. cThe evidence was downgraded by 1 due to imprecision. The confidence interval crossed the line of no effect, and failed to exclude worsening of the outcome. dThe evidence was downgraded by 1 due to imprecision. The sample size was small, however, the confidence intervals fell within the minimally important difference for the outcome. eThe evidence was downgraded by 1 due to imprecision. The confidence intervals failed to exclude an important improvement or worsening of the outcome. fThe evidence was downgraded by 1 due to imprecision. The confidence interval crossed the line of no effect, and failed to exclude an important improvement of the outcome. gThe evidence was downgraded by 1 due to indirectness. The time frame when the outcome was measured (at 48 weeks follow‐up after the 12‐week active treatment period) was not included in the inclusion criteria of this review.
Summary of findings 2. Quinolone versus tetracycline.
| Quinolone compared with tetracycline for chronic obstructive pulmonary disease | ||||||
| Patient or population: chronic obstructive pulmonary disease Setting: hospital outpatients, UK Intervention: moxifloxacin (pulsed; 400 mg per day for 5 days every 4 weeks) Comparison: doxycycline (continuous; 100 mg daily) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of Participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Quinlone | Tetracycline | |||||
|
Number of participants experiencing one or more exacerbations Quinolone versus tetracycline Follow‐up 13 weeks (end of treatment) |
600 per 1000 | 398 per 1000 (174 to 674) | OR 0.44 (0.14 to 1.38) | 50 (1 RCT) | ⊕⊝⊝⊝ Lowa | |
|
All‐cause mortality Follow‐up 13 weeks (end of treatment) |
‐ | ‐ | ‐ | 50 (1 RCT) |
‐ | No deaths reported in either treatment arm |
|
Quality of life Drug resistance/microbial sensitivity Serious adverse events Lung function Hospitalisations Adverse events/side effects Number of participants colonised with P aeruginosa |
Information for these outcomes was not presented as data for head‐to‐head comparisons were not available | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aThe evidence was downgraded by 2 due to imprecision. The sample size was small, and the confidence interval crossed the line of no effect, and failed to exclude important harm.
Summary of findings 3. Quinolone versus macrolide.
| Quinlone compared with macrolide for chronic obstructive pulmonary disease | ||||||
| Patient or population: chronic obstructive pulmonary disease Setting: hospital outpatients, UK Intervention: moxifloxacin (pulsed; 400 mg per day for 5 days every 4 weeks) Comparison: azithromycin (intermittent; 250 mg 3 times per week) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of Participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Quinlone | Macrolide | |||||
|
Number of participants experiencing one or more exacerbations Quinolone versus macrolide Follow‐up 13 weeks (end of treatment) |
400 per 1000 | 400 per 1000 (176 to 674) | OR 1.00 (0.32 to 3.10) | 50 (1 RCT) | ⊕⊝⊝⊝ Lowa | |
|
All‐cause mortality Follow‐up 13 weeks (end of treatment) |
‐ | ‐ | ‐ | 50 (1 RCT) |
‐ | No deaths reported in either treatment arm |
|
Quality of life Drug resistance/microbial sensitivity Serious adverse events Lung function Hospitalisations Adverse events/side effects Number of participants colonised with P aeruginosa |
Information for these outcomes was not presented as data for head‐to‐head comparisons were not available | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aThe evidence was downgraded by 2 due to imprecision. The sample size was small, and the confidence interval failed to exclude an important benefit or harm.
Summary of findings 4. Macrolide versus tetracycline.
| Macrolide compared with tetracycline for chronic obstructive pulmonary disease | ||||||
| Patient or population: chronic obstructive pulmonary disease Setting: hospital outpatients, UK Intervention: azithromycin (intermittent; 250 mg 3 times per week) Comparison: doxycycline (continuous; 100 mg daily) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of Participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Quinlone | Macrolide | |||||
|
Number of participants experiencing one or more exacerbations Macrolide versus tetracycline Follow‐up 13 weeks (end of treatment) |
600 per 1000 | 398 per 1000 (174 to 674) | OR 0.44 (0.14 to 1.38) | 50 (1 RCT) | ⊕⊝⊝⊝ Lowa | |
|
All‐cause mortality Follow‐up 13 weeks (end of treatment) |
‐ | ‐ | ‐ | 50 (1 RCT) |
‐ | No deaths reported in either treatment arm |
|
Quality of life Drug resistance/microbial sensitivity Serious adverse events Lung function Hospitalisations Adverse events/side effects Number of participants colonised with P aeruginosa |
Information for these outcomes was not presented as data for head‐to‐head comparisons were not available | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aThe evidence was downgraded by 2 due to imprecision. The sample size was small, and the confidence interval crossed the line of no effect, and failed to exclude important harm.
Background
Description of the condition
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines chronic obstructive pulmonary disease (COPD) as "a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases" (GOLD 2019). Diagnosis is established by typical symptoms, risk factors and spirometry. Typical symptoms consist of dyspnoea, cough with sputum production and recurrent lower respiratory tract infections. The most prevalent risk factor is tobacco smoke; other environmental risk factors include smoke from home cooking and heating fuels, and occupational dust; host factors include genetic conditions such as alpha₁ antitrypsin deficiency. The spirometric criterion for COPD is a post‐bronchodilator fixed ratio of forced expiratory volume in one second/forced vital capacity (FEV1/FVC) < 0.70 (GOLD 2019).
The impact of COPD on world health is substantial. The number of cases of COPD worldwide has increased from approximately 227.3 million in 1990 to 384 million in 2010, with a global prevalence rising from 10.7% to 11.7% (Adeloye 2015). It is the fourth leading cause of death and is predicted to rise to third place by 2020 (GOLD 2019), or 2030 (WHO 2018). COPD is characterised by frequent exacerbations and lower respiratory tract infections, which further increase the risk of mortality (Schmidt 2014; Threapleton 2018). Exacerbations also impact on exercise tolerance, quality of life and muscle strength; and are associated with a faster decline in lung function (Cote 2007; Donaldson 2008; Kessler 2006; Miravitlles 2004; Niewoehner 2006; Seemungal 1998; Wüst 2007). Exacerbations are associated with systemic, upper and lower airway inflammation (Hurst 2006). It is likely that the aetiology of exacerbations is multifactorial, with inflammation caused by bacteria, viruses and environmental pollutants (Beasley 2012). The aetiology of a particular exacerbation is not always clear. Whilst antibiotics are frequently used to treat COPD exacerbations, and bacterial pathogens are isolated from approximately half of patients with an exacerbation (Kuwal 2018; Llor 2006; Sethi 2004), they are also commonly isolated in patients with stable COPD (Sethi 2008). A network analysis of the lung microbiome of COPD patients demonstrated that a reduction in microbial diversity and the proliferation of a single organism were associated with exacerbation events (Wang 2016). It has been hypothesised that lungs of people with COPD are more susceptible to bacteria, which are not normally present in healthy lungs (Rosell 2005). This chronic bacterial presence contributes to a vicious cycle of inflammation, enhances mucus secretion and worsens ciliary activity, leading to further epithelial damage (Matkovic 2013; Sethi 2008).
Description of the intervention
There are a number of strategies available that are effective at reducing COPD exacerbations, including patient self‐management training (Zwerink 2014); pulmonary rehabilitation (McCarthy 2015; Puhan 2016); influenza vaccination (Kopsaftis 2018); inhaled long‐acting bronchodilators and corticosteroids (Chong 2012; Oba 2018; Yang 2012); and roflumilast, a phosphodiesterase 4 inhibitor (Chong 2013). An additional treatment consideration in an attempt to reduce the frequency of exacerbations of COPD, and reverse this potential 'vicious cycle' of inflammation is the use of long‐term antibiotics as prophylaxis (i.e. for prevention of recurring symptoms (Herath 2018). Prophylatic antibiotics are usually given by mouth, but may also be delivered via other routes, including inhalation. This review will examine the use of head‐to‐head oral antibiotics only. Depending on the type of antibiotic, regimens include continuous (daily), intermittent (i.e. 3 times a week) or pulsed (e.g. 5 days of antibiotics every 8 weeks) administration (BNF).
A Cochrane Review analysed 3170 patients across seven RCTs published between 2001 and 2018 (Herath 2018). The authors investigated the effects of macrolides (azithromycin, erythromycin, clarithromycin) and moxifloxacin (a fourth‐generation synthetic fluoroquinolone) compared with placebo. The use of long‐term prophylactic antibiotics was associated with significantly fewer patients who experienced an exacerbation of COPD (odds ratio (OR) 0.57, 95% confidence interval (CI) 0.42 to 0.78; moderate‐certainty evidence) compared with those receiving placebo. However, patients on prophylactic antibiotics were more likely to experience adverse effects, such as hearing loss with azithromycin and gastrointestinal symptoms with moxifloxacin.
How the intervention might work
The effect of prophylactic antibiotics is not completely understood. Antibiotics may offer both antibacterial and anti‐inflammatory effects (Martinez 2008), and therefore may reduce both bacterial load and inflammation in the airways. Choice of prophylactic antibiotic may be guided by factors including clinician and patient preference and prior experience, previously isolated bacteria and side effect profile. Organisms isolated from exacerbating patients include Haemophilus influenzae (H influenzae) (11% of all patients), Streptococcus pneumoniae (S pneumoniae) (10%), Moraxella catarrhalis (M catarrhalis) (10%), Haemophilus parainfluenzae (H parainfluenzae) (10%), and Pseudonomas aeruginosa (P aeruginosa) (4%) (Sapey 2006).
Prophylactic antibiotics may be of greatest benefit in a subset of patients (Miravittles 2015). A 2011 study by Albert and colleagues suggests that compared to placebo, azithromycin (a macrolide antibiotic) reduces exacerbations most markedly in older patients, non‐smokers and those not using oral or inhaled steroids at baseline, which may reflect sub‐optimal treatment (Albert 2011). We prespecified several subgroup analyses which we conducted to explore this in the context of head‐to‐head antibiotics, if sufficient evidence was available.
Why it is important to do this review
COPD represents a huge burden, to both the patient (Cote 2007; Kessler 2006), and healthcare services (López‐Campos 2016; Mannino 2015; Punekar 2014). Therefore it was important to assess treatments that may reduce the risk of exacerbations and improve quality and longevity of life of patients with COPD.
This review builds upon a recently published Cochrane Review comparing prophylactic antibiotics with placebo (Herath 2018). Results of the published review showed that continuous (daily) and intermittent (at least 3 times a week) may be more effective in reducing exacerbations and improving patient‐reported quality of life (Herath 2018). A network meta‐analysis is under development that will complement the already published review comparing antibiotics with placebo (Herath 2018), and this review (head‐to‐head prophylactic antibiotic comparisons). Whilst there is evidence that antibiotic prophylaxis is efficacious in people with COPD, there remains a large concern over the risk of antibiotic resistance (Miravittles 2017; Thurston 2013). It was therefore imperative to identify which antibiotic provided the best prophylaxis against exacerbations of COPD and least evidence of antibiotic resistance and adverse effects.
Objectives
To compare the safety and efficacy of different classes of antibiotics (continuous, intermittent or pulsed) for prophylaxis of exacerbations in patients with COPD.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs). We planned to include cross‐over trials providing there was an adequate wash out period (at least three months) and cluster‐randomised trials. We included studies reported in full‐text, those published as abstracts only and unpublished data.
Types of participants
We included adults (older than 18 years of age) with a diagnosis of COPD according to established criteria (e.g. European Respiratory Society (ERS), American Thoracic Society (ATS) or Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria). We excluded participants with the following co‐morbidities/characteristics: bronchiectasis; asthma; or genetic diseases, such as cystic fibrosis or primary ciliary dyskinesia. However, we recognised that disease definitions may change over time and if older studies were identified we would consider the directness of the evidence when applying GRADE. As we did not identify trials in which only a subset of the participants had COPD, we did not include any disaggregated data. We included participants irrespective of vaccination status (e.g. pneumococcal vaccination), providing vaccination was not part of the randomised treatment.
Types of interventions
We included studies comparing one prophylactic oral antibiotic with another. We excluded studies where the comparison group received a placebo or usual care not involving a prophylactic antibiotic.
To be eligible, studies must randomise participants to receive the antibiotic for at least 12 weeks, either continuously, intermittently or pulsed*. Intermittent antibiotics must be given at least three times per week, and pulsed antibiotics must be given for a minimum of five consecutive days every eight weeks. We excluded studies which delivered antibiotics via a nebuliser, inhaler, intravenously or intramuscularly.
We included the following co‐interventions provided they were not part of the randomised treatment: short‐ and long‐acting bronchodilators, inhaled corticosteroids, oral corticosteroids, oxygen, pulmonary rehabilitation, smoking cessation interventions or any other standard treatment for COPD.
*We categorised the intervention regimen into continuous, intermittent or pulsed as reported in Herath 2018.
We considered the following comparisons.
Macrolides (e.g. azithromycin) versus other antibiotic classes
Quinolones (e.g. moxifloxacin) versus other antibiotics classes
Quinolones versus macrolides
Macrolides versus penicillins (e.g. amoxicillin)
Macrolides versus tetracyclines (e.g. doxycycline
Types of outcome measures
Primary outcomes
Exacerbations (as defined by trialists and grouped by exacerbation severity where possible, e.g. those requiring hospitalisation versus those requiring ambulatory management only). Depending on the available data, we planned to extract either the number of participants experiencing one or more exacerbations, or the exacerbation rate, or both.
Quality of life (validated scales such as the St George's Respiratory Questionnaire preferred)
Drug resistance/microbial sensitivity (as reported by trialists), including emergence of atypical bacteria
Serious adverse events
Primary outcomes were considered to be the most important to patients, healthcare providers and policy‐makers. Specific adverse events reported by trialists (e.g. episodes of Clostridium difficile (C difficile), tendon rupture, hearing difficulties) were extracted and summarised narratively.
Secondary outcomes
Lung function (FEV1 and FVC)
Mortality (we planned to analyse respiratory and all‐cause mortality separately, where possible)
Hospitalisations
Adverse events/side effects
Number of participants colonised with P aeruginosa
Reporting one or more of the outcomes listed here in the study was not an inclusion criterion for the review.
If outcomes were reported at multiple time points, the latest reported time point/end of treatment data was extracted. We planned to group outcomes reported at three months or more to less than six months; six months to less than 12 months; and 12 months or more. If post‐treatment follow‐up was reported, this was extracted and analysed separately.
Search methods for identification of studies
Electronic searches
We identified studies from the Cochrane Airways Trials Register, which is maintained by the Information Specialist for the Group. The Cochrane Airways Trials Register contained studies identified from several sources, as follows.
Monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), through the Cochrane Register of Studies Online (crso.cochrane.org)
Weekly searches of MEDLINE Ovid
Weekly searches of Embase Ovid SP
Monthly searches of PsycINFO Ovid SP
Monthly searches of CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature)
Monthly searches of AMED EBSCO (Allied and Complementary Medicine)
Handsearches of the proceedings of major respiratory conferences
Studies contained in the Trials Register were identified through search strategies based on the scope of Cochrane Airways. Details of these strategies, as well as a list of handsearched conference proceedings, are in Appendix 1. See Appendix 2 for search terms used to identify studies for this review.
We searched the following trials registries.
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.ClinicalTrials.gov)
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch)
We searched the Cochrane Airways Trials Register and additional sources from inception to 6 February 2019, with no restriction on language of publication.
Searching other resources
We checked the reference lists of all primary studies and review articles for additional references. We searched relevant manufacturers' web sites for study information.
We searched for errata or retractions related to the included studies on PubMed on 21 January 2019.
Data collection and analysis
Selection of studies
Two review authors (CT and RN) screened the titles and abstracts of the search results independently and coded them as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. We retrieved the full‐text study reports of all potentially eligible studies and two review authors (CT and RN) independently screened them for inclusion, recording the reasons for exclusion of ineligible studies. We resolved any disagreement through discussion or, if required, we consulted a third review author (EB). We identified and excluded duplicates, and collated multiple reports of the same study so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram and 'Characteristics of excluded studies' table (Moher 2009).
Data extraction and management
We used a data collection form for study characteristics and outcome data, which had been piloted on at least one study in the review. One review author (CT) extracted the following study characteristics from included studies.
Methods: study design, total duration of study, details of any 'run‐in' period, number of study centres and location, study setting, withdrawals and date of study
Participants: N, mean age, age range, gender, severity of condition, diagnostic criteria, baseline lung function, smoking history, inclusion criteria and exclusion criteria
Interventions: intervention, comparison, concomitant medications and excluded medications
Outcomes: primary and secondary outcomes specified and collected, and time points reported. We sought and recorded definitions used to diagnose an exacerbation.
Notes: funding for studies and notable conflicts of interest of trial authors
Two review authors (RN and SJ) independently extracted outcome data from included studies. We noted in the 'Characteristics of included studies' table if outcome data were not reported in a usable way. We resolved disagreements by consensus. One review author (SJ) transferred data into the Review Manager file (Review Manager 2014). We double‐checked that data were entered correctly by comparing the data presented in the systematic review with the study reports. A second review author (RN) spot‐checked study characteristics for accuracy against the study report.
We produced a table summarising the key characteristics of each study, including region, baseline characteristics of participants, size of study, antibiotic regimens investigated and the reported effect, thus facilitating comparison across studies.
Assessment of risk of bias in included studies
Two review authors (CT and RN) assessed risk of bias independently for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion. We assessed the risk of bias according to the following domains.
Random sequence generation
Allocation concealment
Blinding of participants and personnel
Blinding of outcome assessment
Incomplete outcome data
Selective outcome reporting
Other bias
We judged each potential source of bias as high, low or unclear and provided a quote from the study report together with a justification for our judgement in the 'Characteristics of included studies tables. We summarised the 'Risk of bias' judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes where necessary (e.g. for unblinded outcome assessment, risk of bias for all‐cause mortality could be very different than for a patient‐reported quality of life scale). Where information on risk of bias related to unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' table.
When considering treatment effects, we took into account the risk of bias for the studies that contributed to that outcome.
Assessment of bias in conducting the systematic review
We conducted this review according to the published protocol and justified any deviations from it in the Differences between protocol and review section.
Measures of treatment effect
We analysed dichotomous data as odds ratios (ORs) and continuous data as the mean difference (MD) or standardised mean difference (SMD), had we found data on different scales. If we had combined data from rating scales in a meta‐analysis, we planned to ensure they were entered with a consistent direction of effect (e.g. lower scores always indicating improvement).
We planned to undertake meta‐analyses, however, there were insufficient studies from which to pool data.
We described skewed data narratively where possible (for example, as medians and interquartile ranges for each group).
Where multiple trial arms were reported in a single study, we included only the relevant arms. If we had combined two comparisons (e.g. drug A versus drug B and drug C versus drug B) in the same meta‐analysis, we planned to either combine the 'active' arms or halve the 'control' group to avoid double‐counting.
We planned to identify adjusted analyses (ANOVA or ANCOVA), however, we did not find such analyses in the included studies. If a study reported outcomes at multiple time points, we extracted the latest reported time point.
We used intention‐to‐treat (ITT) or 'full analysis set' analyses where they were reported (i.e. those where data had been imputed for participants who were randomly assigned but did not complete the study) instead of completer or per protocol analyses.
Unit of analysis issues
For dichotomous outcomes, we used participants, rather than events, as the unit of analysis (i.e. number of people admitted to hospital, rather than number of admissions per person). However, if rate ratios were reported in a study (e.g. for exacerbations), we planned to analyse them on this basis. We planned to only meta‐analyse data from cluster‐RCTs if the available data had been adjusted (or could be adjusted), to account for the clustering. We planned to enter data from cross‐over trials using generic inverse variance and with the help of a statistician.
Dealing with missing data
We attempted to contact investigators or study sponsors in order to verify key study characteristics and obtain missing numerical outcome data where possible (e.g. when a study was identified as an abstract only). Where this was not possible, and the missing data were thought to introduce serious bias, we took this into consideration in the GRADE rating for affected outcomes.
Assessment of heterogeneity
We were unable to use the I2 statistic to measure heterogeneity and perform prespecified subgroup analyses as there were insufficient studies to meta‐analyse data. Had we been able to perform meta‐analysis, we would have considered the following I2 ranges to assess heterogeneity (Higgins 2011).
0% to 40%: might not be important
30% to 60%: may represent moderate heterogeneity
50% to 90%: may represent substantial heterogeneity
75% to 100%: considerable heterogeneity
Assessment of reporting biases
If we were able to pool more than 10 studies, we planned to create and examine a funnel plot to explore possible small‐study and publication biases. However, there were insufficient studies to pool data and we were unable to explore these reporting biases using a funnel plot.
Data synthesis
We planned to use a fixed‐effect model and perform a sensitivity analysis with a random‐effects model.
'Summary of findings' tables
We created four 'Summary of findings' tables using the following outcomes: exacerbations of COPD, quality of life, serious adverse events, mortality, lung function (FEV1), hospitalisations and antibiotic resistance. We used the five GRADE considerations (risk of bias; consistency of effect; imprecision; indirectness; and publication bias) to assess the certainty of a body of evidence as it related to the studies that contributed data for the prespecified outcomes. We used the methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), using GRADEpro software (GRADEpro GDT). We justified all decisions to downgrade the certainty of studies using footnotes and we made comments to aid the reader's understanding of the review where necessary.
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following subgroup analyses.
Exacerbation history: trials recruiting participants with a group mean of less than one versus one to two versus more than two exacerbations in the preceding year
COPD severity: participants classed as predominantly GOLD group 1 or 2 versus those predominantly GOLD group 3 or 4
Studies with more than 70% on long‐acting beta‐adrenoceptor agonist/long‐acting muscarinic antagonist/inhaled corticosteroid (LABA/LAMA/ICS) at baseline versus those with less than 70% on LABA/LAMA/ICS at baseline
We used the following outcomes in subgroup analyses.
Participants having one or more exacerbations
Quality of life
Serious adverse events
We used the formal test for subgroup interactions in Review Manager 5 (Review Manager 2014).
Sensitivity analysis
We planned to carry out the following sensitivity analyses, removing the following from the primary outcome analyses.
Studies judged to be at high risk of bias in one or more domains
Cross‐over trials
We planned to compare the results from a fixed‐effect model with the random‐effects model.
Results
Description of studies
Results of the search
The database search identified 1416 records. We screened 1415 records after removing duplicates. We excluded 1367 records on the basis of the titles and abstracts, resulting in 48 full‐text articles to be assessed for eligibility. From the full‐text assessment, we identified two studies that were eligible for inclusion in this systematic review (Figure 1).
1.
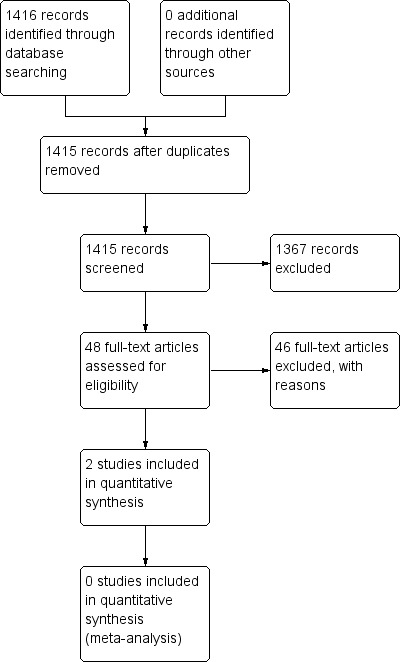
Study flow diagram.
Included studies
We identified two studies that were eligible to include in this systematic review (Brill 2015; Shafuddin 2015).
The first study specifically compared the effect of different antibiotic classes with a placebo group on airway bacteria in people with stable chronic obstructive pulmonary disease (COPD) for 13 weeks (Brill 2015). The second study compared the effect of two antibiotics combined with a single antibiotic treatment and placebo treatment group, which was not a comparison that was originally part of our inclusion criteria. We included the study because regardless of the comparison, the antibiotics included in the study were part of the inclusion criteria for this review. The duration of treatment in the study was 12 weeks in people with moderate to severe COPD (Shafuddin 2015).
One single‐centre, single‐blind, placebo‐controlled study included 99 participants with a mean number of exacerbations per person in the previous year of 2.2 and a mean FEV1% predicted of 50.5% (see Characteristics of included studies for further details). The trial investigated three antibiotics, each from a different antibiotic class. The treatment arms included moxifloxacin, a quinolone (pulsed, 400 mg administered for 5 days every 4 weeks), azithromycin, a macrolide (intermittent, 250 mg administered 3 times per week), and doxycycline, a tetracycline (continuous, 100 mg administered daily) (Brill 2015). For the purpose of this systematic review, we extracted the data for each antibiotic only and not the data for the placebo treatment arm.
One double‐blind, placebo‐controlled study included 292 participants with a mean number of exacerbations per person within two years of 5.11 and a mean FEV1% predicted of 34% (see Characteristics of included studies for further details). The trial investigated roxithromycin, a macrolide (continuous, 300 mg per day), and doxycycline, a tetracycline (100 mg per day), administered together and compared with roxithromycin alone as well as a placebo treatment arm. Originally, the study was designed to investigate the hypothesis that "C pneumoniae was a pathogenic factor in the aetiology of COPD and that eradication of C pneumoniae infection could reduce exacerbation rates". As the participants included in the study were already tested positive for C pneumoniae the aim was to test whether the antibiotic regimens could specifically eradicate C pneumoniae infection. However, the study authors explained in the text of the publication that this hypothesis was "considered unsubstantiated and no longer considered clinically relevant". Instead, they presented the data to investigate the role of prophylactic antibiotics in the reduction of COPD exacerbations (Shafuddin 2015).
Study funding
Brill 2015 was supported by Programme Grants for Applied Research programme and the NIHR Royal Brompton Respiratory Biomedical Research Unit.
Shafuddin 2015 was funded by Sanofi‐Aventis Australia Pty Ltd.
Excluded studies
Excluded studies are listed in the Characteristics of excluded studies table with reasons for exclusions.
Risk of bias in included studies
Judgements for risk of bias and reasons can be found in the Characteristics of included studies table and an overview of judgements for risk of bias can be found in Figure 2.
2.
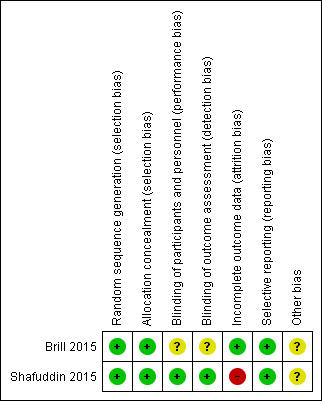
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation and allocation concealment were described in detail by both studies and we judged them to be at low risk of bias in these domains (Brill 2015; Shafuddin 2015).
Blinding
Blinding of participants and personnel was described in detail in Shafuddin 2015 and we judged this domain as low risk of bias. However, Brill 2015 was described as a single‐blind study as participants were blinded but it was unclear if personnel were blinded to treatment allocation. As blinding of outcome assessment (detection bias) was confirmed in detail as a result of contacting corresponding authors for Shafuddin 2015, we judged this domain as low risk of bias. However, there was no description of outcome assessor blinding in the Brill 2015, which resulted in an unclear of bias judgement for this domain.
Incomplete outcome data
Flow of participants throughout both studies were described in detail as they both used a CONSORT diagram to explain attrition (Brill 2015; Shafuddin 2015). Rates of withdrawal in Brill 2015 were low and balanced between groups and were accounted for in the flow diagram. However in Shafuddin 2015, more patients withdrew from the combined antibiotics treatment arm, although trialists reported that this was not related to medication. We judged Brill 2015 to be at low risk and Shafuddin 2015 to be at high risk in this domain.
Selective reporting
Both studies reported all prespecified planned primary and secondary outcomes according to the trial registration (Brill 2015; Shafuddin 2015). It should be noted that some outcomes of both studies were not reported in the format for this systematic review, and after contact with corresponding authors for both trials, we were not able to obtain the data required. To view risk of bias tables see the Characteristics of included studies.
Other potential sources of bias
Although both studies described adequate methods of random sequence generation and allocation concealment, we identified imbalances in baseline characteristics in both studies. Therefore we rated both to be at unclear risk of other bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
An overview of the results together with a summary of our certainty of the evidence per head‐to‐head comparison is presented in Table 1, Table 2, Table 3 and Table 4. Additional information about both trials are presented in Table 5, Table 6, Table 7, Table 8, Table 9 and Table 10.
1. Number of participants experiencing exacerbations.
| Study ID | Antibiotic class | Antibiotic | Antibiotic frequency and amount | Number of participants experiencing exacerbations (N) | Total number of participants (N) | Duration of treatment |
| Brill 2015 | Quinolone | Moxifloxacin | Pulsed (400 mg daily for 5 days every 4 weeks) |
10 | 25 | 13 weeks |
| Brill 2015 | Tetracycline | Doxycycline | Continuous (100 mg daily) | 15 | 25 | 13 weeks |
| Brill 2015 | Macrolide | Azithromycin | Intermittent (250 mg 3 times per week) |
10 | 25 | 13 weeks |
2. Quality of life.
| Study ID | Antibiotic class | Antibiotic | Antibiotic frequency and amount | Quality of life scale | Mean CRQ (SD) |
Total number of participants (N) |
Duration of treatment |
| Shafuddin 2015 | Macrolide+ tetracycline |
Roxithromycin + doxycycline | Continuous (300 mg daily + 100 mg daily) |
CRQ (dyspnoea) |
2.21 (5.35) |
93 | 12 weeks |
| Shafuddin 2015 | Macrolide | Roxithromycin | Continuous (300 mg daily) | CRQ (dyspnoea) |
1.63 (4.53) |
94 | 12 weeks |
| Shafuddin 2015 | Macrolide+ tetracycline |
Roxithromycin + doxycycline | Continuous (300 mg daily + 100 mg daily) |
CRQ (fatigue) |
0.68 (3.79) |
93 | 12 weeks |
| Shafuddin 2015 | Macrolide | Roxithromycin | Continuous (300 mg daily) | CRQ (fatigue) |
0.66 (3.87) |
94 | 12 weeks |
| Shafuddin 2015 | Macrolide+ tetracycline |
Roxithromycin + doxycycline | Continuous (300 mg daily + 100 mg daily) |
CRQ (emotional function) |
0.45 (5.04) |
93 | 12 weeks |
| Shafuddin 2015 | Macrolide | Roxithromycin | Continuous (300 mg daily) | CRQ (emotional function) |
0.82 (4.48) |
94 | 12 weeks |
| Shafuddin 2015 | Macrolide+ tetracycline |
Roxithromycin + doxycycline | Continuous (300 mg daily + 100 mg daily) |
CRQ (mastery) |
0.53 (3.42) |
93 | 12 weeks |
| Shafuddin 2015 | Macrolide | Roxithromycin | Continuous (300 mg daily) | CRQ (mastery) |
1.32 (4) |
94 | 12 weeks |
CRQ: Chronic Respiratory Questionnaire SD: standard deviation
3. Number of participants experiencing serious adverse events (all‐cause).
| Study ID | Antibiotic class | Antibiotic | Antibiotic frequency and amount | Number of participants experiencing SAEs (n) | Total number of participants (N) | Duration of treatment |
| Brill 2015 | Quinolone | Moxifloxacin | Pulsed (400 mg daily for 5 days every 4 weeks) |
0 | 25 | 13 weeks |
| Brill 2015 | Tetracycline | Doxycycline | Continuous (100 mg daily) | 0 | 25 | 13 weeks |
| Brill 2015 | Macrolide | Azithromycin | Intermittent (250 mg 3 times per week) |
0 | 25 | 13 weeks |
| Shafuddin 2015 | Macrolide+ tetracycline |
Roxithromycin+ doxycycline |
Continuous (300 mg + 100 mg daily) |
24 | 101 | 48 weeks follow‐up after 12 weeks active treatment (60 weeks) |
| Shafuddin 2015 | Macrolide | Roxithromycin | Continuous (300 mg daily) | 23 | 97 | 48 weeks follow‐up after 12 weeks active treatment (60 weeks) |
SAE: serious adverse event
4. Lung function (FEV1, FEV1% predicted, and FVC).
| Study ID | Antibiotic class | Antibiotic | Antibiotic frequency and amount |
Mean FEV1 (SD) (trough) |
Mean FEV1 % predicted (SD) (trough) |
Mean FVC (SD) | Total number of participants (N) | Duration of treatment |
| Shafuddin 2015 | Macrolide + tetracycline | Roxithromycin + doxycycline | Continuous (300 mg + 100 mg daily) |
0.047 (026) | 1.7 (9) | 0.06 (0.46) | 88 | 12 weeks |
| Shafuddin 2015 | Macrolide | Roxithromycin | Continuous (300 mg daily) | 0.057 (0.31) | 1.87 (11) | 0.09 (0.55) | 94 | 12 weeks |
FEV1: forced expiratory volume in 1 second FVC: forced vital capacity SD: standard deviation
5. Mortality.
| Study ID | Antibiotic class | Antibiotic | Antibotic frequency and amount | All‐cause mortality (n) | Total number of participants (N) | Duration of treatment |
| Shafuddin 2015 | Macrolide + tetracycline | Roxithromycin + doxycycline | Continuous (300 mg + 100 mg daily) |
5 | 101 | 48 weeks follow‐up after 12 weeks active treatment (60 weeks) |
| Shafuddin 2015 | Macrolide | Roxithromycin | Continuous (100 mg daily) | 3 | 97 | 48 weeks follow‐up after 12 weeks active treatment (60 weeks) |
6. Number of people experiencing adverse events/side effects.
| Study ID | Antibiotic class | Antibiotic | Antibiotic frequency and amount | Adverse event type | Number of participants with adverse events/side effects (n) | Total number of participants (N) | Duration of treatment |
| Shafuddin 2015 | Macrolide + tetracycline | Roxithromycin + doxycycline | Continuous (300 mg + 100 mg daily) |
All‐cause | 73 | 101 | 48 weeks follow‐up after 12 weeks active treatment (60 weeks) |
| Shafuddin 2015 | Macrolide | Roxithromycin | Continuous (100 mg daily) | All‐cause | 74 | 97 | 48 weeks follow‐up after 12 weeks active treatment (60 weeks) |
| Shafuddin 2015 | Macrolide + tetracycline | Roxithromycin + doxycycline | Continuous (300 mg + 100 mg daily) |
Treatment‐ related |
31 | 101 | 48 weeks follow‐up after 12 weeks active treatment (60 weeks) |
| Shafuddin 2015 | Macrolide | Roxithromycin | Continuous (100 mg daily) | Treatment‐ related |
33 | 97 | 48 weeks follow‐up after 12 weeks active treatment (60 weeks) |
We did not identify trials comparing different regimens of the same prophylactic antibiotic (e.g. azithromycin 250 mg daily versus azithromycin 500 mg three times/week). Similarly, we did not identify trials comparing two antibiotics within the same class (e.g. moxifloxacin versus ciprofloxacin, both quinolones).
We identified the following comparisons and outcomes from two studies.
Macrolide plus tetracycline versus macrolide
Primary outcome: number of COPD patients with exacerbations
We did not identify evidence for this outcome.
Primary outcome: time to first moderate or severe exacerbation
Shafuddin 2015 reported the mean time to first moderate or severe exacerbation (days). There was no significant difference between both treatment arms after the active treatment period (mean difference (MD) ‐19.00, 95% confidence interval (CI) ‐52.70 to 14.70; 179 participants; Analysis 1.1).
1.1. Analysis.
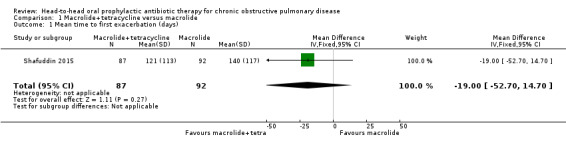
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 1 Mean time to first exacerbation (days).
Primary outcome: quality of life
We analysed data from Shafuddin 2015 as this trial reported each treatment arm separately, which allowed us to compare combined antibiotic treatment (roxithromycin and doxycycline) to single antibiotic treatment (roxithromycin only) (Table 1). The authors did not report a total score for the Chronic Respiratory Questionnaire (CRQ) scale, but reported the mean difference and standard deviations for change in dyspnoea, fatigue, emotional function and mastery sub‐scales from baseline to end of treatment (12 weeks) (Analysis 1.2) or 60 weeks (Analysis 1.3).
1.2. Analysis.
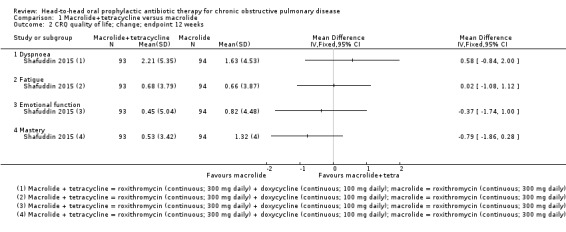
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 2 CRQ quality of life; change; endpoint 12 weeks.
1.3. Analysis.
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 3 CRQ quality of life; change; endpoint 60 weeks.
At the end of the active treatment at 12 weeks, there was no clinical or statistically significant difference in effect between continuous combined treatment compared to continuous single antibiotic treatment on the CRQ sub‐scales for dyspnoea (MD 0.58, 95% CI ‐0.84 to 2.00; 187 participants; very low‐certainty evidence), fatigue (MD 0.02, 95% CI ‐1.08 to 1.12; 187 participants; very low‐certainty evidence), emotional function (MD ‐0.37, 95% CI ‐1.74 to 1.00; 187 participants; very low‐certainty evidence) or mastery (MD ‐0.79, 95% CI ‐1.86 to 0.28; 187 participants; very low‐certainty evidence). These results did not reach published minimally important differences (MID) for the CRQ sub‐scales for dyspnoea (MID = 3 point increase), fatigue (MID = 4 point increase), or emotional function (MID = 2 point increase) (Jaeschke 1989; Jones 2002) (see Table 1).
Primary outcome: drug resistance
We did not identify evidence for this outcome.
Primary outcome: serious adverse events (all‐cause)
Shafuddin 2015 did not report serious adverse events at 12 weeks (end of treatment), but did measure the outcome at the end of the study at 60 weeks. There was no clear difference in serious adverse events between combined continuous or single continuous antibiotic treatment and the confidence intervals around the effect estimate are wide (odds ratio (OR) 1.00, 95% CI 0.52 to 1.93; 198 participants; very low‐certainty evidence; Analysis 1.4; Table 1). Furthermore, there was no clear difference in treatment‐related serious adverse events with combined continuous antibiotics or single continuous antibiotics, and the effect is also very uncertain (OR 0.37, 95% CI 0.07 to 1.96; 198 participants; Analysis 1.5)
1.4. Analysis.
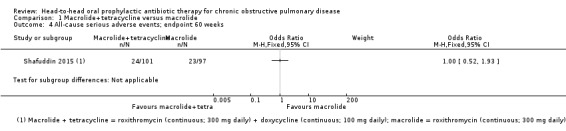
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 4 All‐cause serious adverse events; endpoint 60 weeks.
1.5. Analysis.
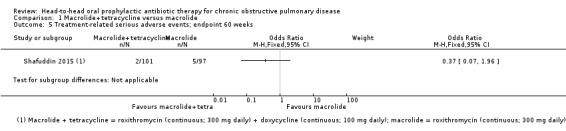
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 5 Treatment‐related serious adverse events; endpoint 60 weeks.
Secondary outcomes: lung function (FEV1 and FVC), mortality (all‐cause), hospitalisations, and adverse events/side effects
Shafuddin 2015 reported data on change in FEV1 (Analysis 1.6) and FVC (Analysis 1.7) at 12 weeks (end of treatment), and mortality (Analysis 1.8); and all‐cause and treatment‐related adverse events at 60 weeks (Analysis 1.9). There were no clinically significant changes in lung function at 12 weeks (very low‐certainty evidence). At 60 weeks, authors found no clear difference in mortality, but the effect estimate is very uncertain (OR 1.63, 95% CI 0.38 to 7.02; 182 participants; very low‐certainty evidence). There was no statistically significant difference in adverse events between combined antibiotic compared with single antibiotics (very low‐certainty evidence). There was one case of an abnormal electrocardiogram (ECG), considered to be related to combined antibiotic treatment (Table 1).
1.6. Analysis.
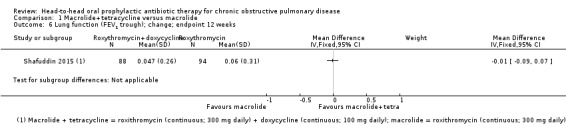
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 6 Lung function (FEV1 trough); change; endpoint 12 weeks.
1.7. Analysis.
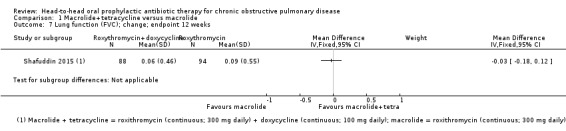
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 7 Lung function (FVC); change; endpoint 12 weeks.
1.8. Analysis.
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 8 All‐cause mortality; endpoint 60 weeks.
1.9. Analysis.
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 9 All‐cause adverse events; endpoint 60 weeks.
We did not identify any evidence for hospitalisations or number of participants colonised with P aeruginosa.
Quinolone versus tetracycline
Although the aim of the study was to compare prophylactic antibiotics with placebo, the data were presented separately per treatment arm, which allowed the analysis between moxifloxacin and doxycycline (Brill 2015). This comparison included 50 participants, 25 in each of the treatment arms of interest.
Primary outcome: number of COPD patients with exacerbations
Brill 2015 reported the number of people with COPD experiencing one or more exacerbations. At 13 weeks of treatment, fewer people with COPD experienced one or more exacerbations with moxifloxacin (pulsed; 400 mg for 5 days every 4 weeks) in comparison to doxycycline (continuous; 100 mg daily). However, this effect was uncertain as the upper confidence interval crossed the line of no effect and failed to exclude important harm (OR 0.44, 95% CI 0.14 to 1.38; 50 participants; low‐certainty evidence; Analysis 2.1; Table 2).
2.1. Analysis.
Comparison 2 Quinolone versus tetracycline, Outcome 1 Number of people with one or more exacerbations.
Primary outcome: quality of life
We did not identify evidence for this outcome.
Primary outcome: drug resistance
We did not identify head‐to‐head evidence for this outcome.
Primary outcome: serious adverse events
Brill 2015 measured the number of people with COPD experiencing serious adverse events. At 13 weeks (end of treatment), there were no reported serious adverse events in either the moxifloxacin (pulsed; 400 mg for 5 days every 4 weeks) or doxycycline (continuous; 100 mg daily) arms.
Secondary outcomes: lung function (FEV1 and FVC), mortality (all‐cause), hospitalisations, adverse events/side effects, and number of participants colonised withP aeruginosa
Brill 2015 did not report any deaths during 13 weeks of treatment, and no participants experienced adverse events when treated with moxifloxacin (pulsed; 400 mg for 5 days every 4 weeks) or doxycycline (100 mg daily) after 13 weeks of treatment.
We did not identify evidence for the following outcomes: lung function, hospitalisations, or number of participants colonised withP aeruginosa.
Quinolone versus macrolide
Although the aim of the study was to compare prophylactic antibiotic with placebo, the data were presented separately per treatment arm, which allowed the analysis between moxifloxacin and azithromycin (Brill 2015). This comparison included 50 participants, 25 in each of the treatment arms of interest.
Primary outcome: number of COPD patients with exacerbations
Brill 2015 reported the number of people with COPD experiencing one or more exacerbations. At 13 weeks of treatment, there was no difference in the number of people with COPD experiencing one or more exacerbations with moxifloxacin (pulsed; 400 mg for 5 days every 4 weeks) or azithromycin (intermittent; 250 mg 3 times per week), but the confidence intervals were wide (OR 1.00, 95% CI 0.32 to 3.10; 50 participants; low‐certainty evidence; Analysis 3.1; Table 3).
3.1. Analysis.
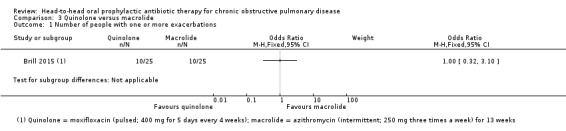
Comparison 3 Quinolone versus macrolide, Outcome 1 Number of people with one or more exacerbations.
Primary outcome: quality of life
We did not identify evidence for this outcome.
Primary outcome: drug resistance
We did not identify any head‐to‐head evidence for this outcome.
Primary outcome: serious adverse events
Brill 2015 measured the number of people with COPD experiencing serious adverse events. At 13 weeks (end of treatment), there were no reported serious adverse events in either the moxifloxacin (pulsed; 400 mg for 5 days every 4 weeks) or azithromycin (intermittent; 250 mg three times per week) arms.
Secondary outcomes: lung function (FEV1 and FVC), mortality (all‐cause), hospitalisations, adverse events/side effects, and number of participants colonised with P aeruginosa
Brill 2015 reported no deaths during the 13‐week treatment period.
We did not identify any evidence for the following outcomes: lung function, hospitalisations, adverse events/side effects, or number of participants colonised with P aeruginosa.
Macrolide versus penicillin
We did not identify evidence for this comparison.
Macrolide versus tetracycline
Although the aim of the study was to compare prophylactic antibiotic with placebo, the data was presented separately per treatment arm, which allowed the analysis between azithromycin and doxycyline (Brill 2015). This comparison included 50 participants, 25 in each of the treatment arms of interest.
Primary outcome: number of COPD patients with exacerbations
Brill 2015 reported the number of people with COPD experiencing one or more exacerbations. At 13 weeks of treatment, fewer people with COPD experienced one or more exacerbations with azithromycin (intermittent; 250 mg three times per week) in comparison to doxycycline (continuous; 100 mg daily). However, this effect was uncertain as the upper confidence interval crossed the line of no effect and failed to exclude important harm (OR 0.44, 95% CI 0.14 to 1.38; 50 participants; low‐certainty evidence; Analysis 4.1; Table 4).
4.1. Analysis.
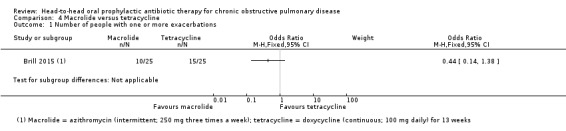
Comparison 4 Macrolide versus tetracycline, Outcome 1 Number of people with one or more exacerbations.
Primary outcome: quality of life
We did not identify evidence for this outcome.
Primary outcome: drug resistance
We did not identify evidence for this outcome.
Primary outcome: serious adverse events
Brill 2015 measured the number of people with COPD experiencing serious adverse events. At 13 weeks (end of treatment), there were no reported serious adverse events in either the azithromycin (intermittent; 250 mg three times per week) or doxycycline (continuous; 100 mg daily) arms.
Secondary outcomes: lung function (FEV1 and FVC), mortality (all‐cause), hospitalisations, adverse events/side effects, and number of participants colonised with P aeruginosa
Brill 2015 reported no deaths during the 13‐week treatment period.
We did not identify evidence for the following outcomes: lung function, hospitalisations, adverse events/side effects or number of participants colonised with P aeruginosa.
Discussion
Summary of main results
Macrolide plus tetracycline versus macrolide
There was no clear benefit or harm of combined continuous roxithromycin plus doxycycline (300 mg plus 100 mg daily) compared to single continuous roxithromycin (300 mg daily) on quality of life as observed on the sub‐scales of the Chronic Respiratory Questionnaire (CRQ) for dyspnoea, fatigue, emotional function, or mastery. Similarly, there was no evidence of benefit or harm on lung function (FEV1 or FVC). No serious adverse events were reported in either treatment group and the effect on mortality was very uncertain (Shafuddin 2015). We were unable to include any evidence on number of people experiencing one or more exacerbations, drug resistance/microbial sensitivity or number of participants colonised with Pseudomonas aeruginosa (P aeruginosa).
Quinolone versus tetracycline
We are uncertain whether moxifloxacin compared to doxycycline has an impact on the number of people experiencing one or more exacerbations at 12 weeks. No serious adverse events or deaths were reported in either treatment group (Brill 2015). We were unable to include any evidence on our other prespecified outcomes.
Quinolone versus macrolide
We are uncertain whether moxifloxacin compared to azithromycin has an impact on the number of people experiencing one or more exacerbations at 12 weeks. No serious adverse events or deaths were reported in either treatment group (Brill 2015). We were unable to include any evidence on our other prespecified outcomes.
Macrolide versus tetracycline
We are uncertain whether azithromycin compared to doxycycline has an impact on the number of people experiencing one or more exacerbations at 12 weeks. No serious adverse events or deaths were reported in either treatment group (Brill 2015). We were unable to include any evidence on our other prespecified outcomes.
Overall completeness and applicability of evidence
We identified two studies, each recruiting a small group of participants. The studies could not be combined due to differences in their aims, the antibiotics investigated and outcomes reported. Therefore, we lack evidence to assess whether one prophylactic antibiotic or regimen is more effective for people with chronic obstructive pulmonary disease (COPD) in terms of exacerbations or quality of life. Importantly, we also lack evidence to comment on which regimens are safer, and whether different regimens are associated with more or less drug resistance. Although one study did report drug resistance to three different antibiotics each compared to placebo, this evidence did not fit the criteria of this review and has been reported in another Cochrane Review (Herath 2018). We do acknowledge, however, that longer and larger studies are needed to determine effects of long‐term antibiotic use. The applicability of the results from these two studies to the general COPD population is uncertain, as the participants either had positive Chlamydophila pneumoniae (C pneumoniae) serology in one study (Shafuddin 2015), or a chronic bronchitis phenotype in the other study (Brill 2015).
It is anticipated that a linked network meta‐analysis (Janjua 2018), will allow comparisons of different prophylactic antibiotics through direct and indirect comparisons and may provide a ranking of prophylactic antibiotics for important outcomes including exacerbations, quality of life and serious adverse events.
Certainty of the evidence
Using the GRADE approach, we assessed the evidence presented in this review as very low‐certainty. Reasons for downgrading included imprecision, indirectness and methodological quality of the included studies.
Brill 2015 was a single‐centre and single‐blinded study as it was not reported that the personnel were blinded to the treatment allocation (Brill 2015). There was also no description of outcome assessor blinding, although blinded participants assessed outcomes such as quality of life. The trial reported outcomes according to their protocol. The aim of the trial was to compare three different prophylactic antibiotics to placebo. This was not a true head‐to‐head study of antibiotics, but we used the data in the trial to compare the three different antibiotics to each other. We were only able to report results for the number of people experiencing one or more exacerbations as the data did not allow us to analyse any other outcomes of interest for this systematic review.
The second study was multi‐centred and double‐blinded. More participants dropped out of the combined antibiotics treatment arm, although the trialists report that reasons were not related to study medication (Shafuddin 2015). The trialists reported all outcomes according to their protocol.
The small sample size of both studies resulted in considerable uncertainty around the true effect and led to downgrading of the all the evidence for imprecision. We also downgraded serious adverse events and mortality by one point for indirectness of the population and intervention. The aim of one of the studies was to assess the eradication of C pneumoniae and not antibiotic prophylaxis. The comparison of interventions was not an inclusion criterion of this systematic review, and both outcomes were measured 48 weeks after the treatment period of 12 weeks. As these were not inclusion criteria prespecified for this systematic review, we downgraded the outcomes further.
Potential biases in the review process
Cochrane methods were adhered to in order to conduct this systematic review and we did not expect there to be any bias in the reviewing process. During the selection of studies, we encountered a study with an unanticipated comparison of interventions. We included this study in this systematic review as it otherwise met our prespecified inclusion criteria. Furthermore, while one of our stated objectives was to assess the comparative safety of prophylactic antibiotic regimens, the limited number of studies meeting our inclusion criteria means that we are unable to comment on this important outcome. We did not search for clinical trial reports or observational data, which may have helped address this objective.
Agreements and disagreements with other studies or reviews
Several systematic reviews have investigated the use of prophylactic antibiotics in COPD compared to placebo or usual care (Donath 2013; Herath 2018; Lee 2013; Ni 2015; Yao 2013). However, we are not aware of any reviews to date that have focused on head‐to‐head comparisons. The majority of evidence for the benefit of antibiotics versus placebo comes from studies of macrolide antibiotics (Herath 2018). This is reflected in current guidelines, which cautiously recommend the use of macrolide antibiotics in selected patients to reduce exacerbations, while acknowledging the lack of evidence for other classes of antibiotic, including quinolones (GOLD 2019; Wedzicha 2017). The planned network meta‐analysis of Janjua 2018 may help resolve the question about the most appropriate choice of antibiotic.
Authors' conclusions
Implications for practice.
It is not clear from the randomised controlled trial (RCT) evidence included in this review whether there is a difference in efficacy or safety between different classes or regimens of prophylactic antibiotic, given for 12 to 13 weeks to people with chronic obstructive pulmonary disease (COPD). The sample size in this review is small and both included studies are of short duration. Whilst no head‐to‐head comparisons of antibiotic resistance were identified, concerns about this continue. Our certainty in our findings is consequently very low and there is insufficient information presented in this review to meaningfully inform practice.
Implications for research.
Given the urgent need for treatment strategies that reduce the burden of exacerbations of COPD and improve quality of life, and the potential benefit of antibiotics demonstrated in placebo‐controlled trials, more research into optimal regimens is needed. Network meta‐analyses, which allow both direct and indirect comparisons of antibiotic treatment options, would be of value. However, the small number of trials and heterogeneity in populations, study design and outcome measures may limit the utility of network meta‐analysis. Therefore, adequately powered studies of sufficient duration to detect differences in important outcomes, such as exacerbations, may still be required. Trialists should seek to characterise carefully the population recruited and report on important patient and healthcare system outcomes, such as exacerbations (using clear diagnostic criteria), hospitalisations, quality of life (using validated scales) and antibiotic resistance. Stratification of outcomes by factors that may influence anti‐inflammatory benefit (e.g. smoking status and inhaled corticosteroid (ICS) use) may help with treatment decisions for certain patient subgroups. To address questions about the comparative safety of different regimens, particularly with regard to rarer adverse events, it may be necessary to assess real‐world observational data sets.
What's new
| Date | Event | Description |
|---|---|---|
| 20 November 2019 | Amended | Funding statement and disclaimer added to acknowledgements. |
Acknowledgements
The Background and Methods sections of this protocol are based on a standard template used by Cochrane Airways.
Ian Yang was the Editor for this review and commented critically on the review.
We would like to acknowledge the valuable contribution of our volunteer translators who helped us determine the eligibility of studies that were not in English. These were: Mia Schmidt‐Hansen, Thomas Aagaard Marina Karanikolos, Stanislav Iakhno, Lena Lantsova, Anja Lieder, Jennifer Brown, Matthias Briel, Angela Lai, Jos Verbeek, Hans van der Wouden, Gianni Virgili and Adolfo Maria Tambella.
The authors and Airways editorial team are grateful to the following peer reviewers for their time and comments: Dr Amir Sharafkhaneh, Baylor College of Medicine and Michael E DeBakey VA Medical Center, Houston; Daniel Tan, Alfred Hospital, Melbourne, Australia; Alexander G Mathioudakis MD, MRCP(UK), Division of Infection, Immunity and Respiratory Medicine, The University of Manchester; and a further peer reviewer who wishes to remain anonymous.
This project was funded by the National Institute for Health Research Systematic Reviews Programme (project number 16/114/21). This project was also supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Cochrane Airways Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Health Research Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendices
Appendix 1. Sources and search methods for the Cochrane Airways Group's Specialised Register (CAGR)
Electronic searches: core databases
| Database | Dates searched | Frequency of search |
| CENTRAL (via the Cochrane Register of Studies (CRS)) | From inception | Monthly |
| MEDLINE (Ovid) | 1946 onwards | Weekly |
| EMBASE (Ovid) | 1974 onwards | Weekly |
| PsycINFO (Ovid) | 1967 onwards | Monthly |
| CINAHL (EBSCO) | 1937 onwards | Monthly |
| AMED (EBSCO) | From inception | Monthly |
Handsearches: core respiratory conference abstracts
| Conference | Years searched |
| American Academy of Allergy, Asthma and Immunology (AAAAI) | 2001 onwards |
| American Thoracic Society (ATS) | 2001 onwards |
| Asia Pacific Society of Respirology (APSR) | 2004 onwards |
| British Thoracic Society Winter Meeting (BTS) | 2000 onwards |
| Chest Meeting | 2003 onwards |
| European Respiratory Society (ERS) | 1992, 1994, 2000 onwards |
| International Primary Care Respiratory Group Congress (IPCRG) | 2002 onwards |
| Thoracic Society of Australia and New Zealand (TSANZ) | 1999 onwards |
MEDLINE search strategy used to identify studies for the Cochrane Airways Trials Register
COPD search
1. Lung Diseases, Obstructive/
2. exp Pulmonary Disease, Chronic Obstructive/
3. emphysema$.mp.
4. (chronic$ adj3 bronchiti$).mp.
5. (obstruct$ adj3 (pulmonary or lung$ or airway$ or airflow$ or bronch$ or respirat$)).mp.
6. COPD.mp.
7. COAD.mp.
8. COBD.mp.
9. AECB.mp.
10. or/1‐9
Filter to identify RCTs
1. exp "clinical trial [publication type]"/
2. (randomised or randomised).ab,ti.
3. placebo.ab,ti.
4. dt.fs.
5. randomly.ab,ti.
6. trial.ab,ti.
7. groups.ab,ti.
8. or/1‐7
9. Animals/
10. Humans/
11. 9 not (9 and 10)
12. 8 not 11
The MEDLINE strategy and RCT filter are adapted to identify studies in other electronic databases.
Appendix 2. Search strategy to identify relevant studies from the Cochrane Airways Trials Register
#1 MeSH DESCRIPTOR Pulmonary Disease, Chronic Obstructive Explode All #2 MeSH DESCRIPTOR Bronchitis, Chronic #3 (obstruct*) near3 (pulmonary or lung* or airway* or airflow* or bronch* or respirat*) #4 COPD:MISC1 #5 (COPD OR COAD OR COBD OR AECOPD):TI,AB,KW #6 #1 OR #2 OR #3 OR #4 OR #5 #7 MESH DESCRIPTOR Anti‐Bacterial Agents EXPLODE ALL #8 antibiotic* NEAR prophyla* #9 continuous NEAR antibiotic* #10 antibiotic* #11 penicillin #12 phenoxymethylpenicillin #13 phenethicillin #14 amoxicillin #15 amoxycillin #16 clavulanic acid #17 tetracycline #18 oxytetracycline #19 doxycycline #20 quinolone #21 ciprofloxacin #22 moxifloxacin #23 macrolide* #24 erythromycin #25 roxithromycin #26 azithromycin #27 sulphonamide #28 co‐trimoxazole #29 sulphaphenazole #30 trimethoprim #31 sigmamycin #32 tetracycline AND oleandomycin #33 sulfamethoxazole #34 sulfaphenazole #35 sulfonamide #36 anti‐bacteri* or antibacteri* #37 ceph* #38 sulpha* #39 {OR #7‐#38} #40 #39 AND #6
Data and analyses
Comparison 1. Macrolide+tetracycline versus macrolide.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean time to first exacerbation (days) | 1 | 179 | Mean Difference (IV, Fixed, 95% CI) | ‐19.0 [‐52.70, 14.70] |
| 2 CRQ quality of life; change; endpoint 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Dyspnoea | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Fatigue | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Emotional function | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Mastery | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 CRQ quality of life; change; endpoint 60 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Dyspnoea | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Fatigue | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Emotional function | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Mastery | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 All‐cause serious adverse events; endpoint 60 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5 Treatment‐related serious adverse events; endpoint 60 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6 Lung function (FEV1 trough); change; endpoint 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7 Lung function (FVC); change; endpoint 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8 All‐cause mortality; endpoint 60 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9 All‐cause adverse events; endpoint 60 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10 Treatment‐related adverse events; endpoint 60 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11 Lung function (FEV1 % predicted); change; endpoint 60 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12 Lung function (FEV1 trough); change; endpoint 60 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 13 Lung function (FEV1 % predicted); change; endpoint 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 14 Lung function (FVC); change; endpoint 60 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
1.10. Analysis.
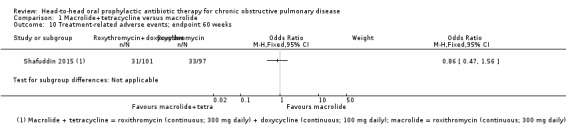
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 10 Treatment‐related adverse events; endpoint 60 weeks.
1.11. Analysis.
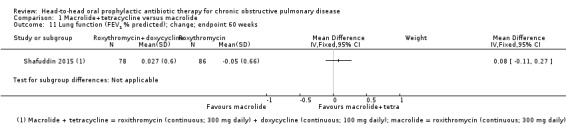
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 11 Lung function (FEV1 % predicted); change; endpoint 60 weeks.
1.12. Analysis.
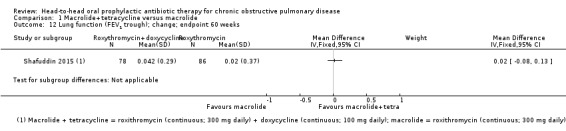
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 12 Lung function (FEV1 trough); change; endpoint 60 weeks.
1.13. Analysis.
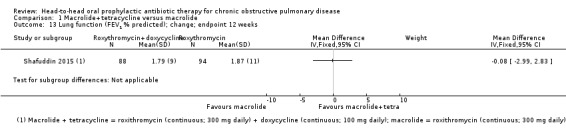
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 13 Lung function (FEV1 % predicted); change; endpoint 12 weeks.
1.14. Analysis.
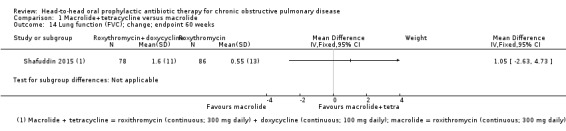
Comparison 1 Macrolide+tetracycline versus macrolide, Outcome 14 Lung function (FVC); change; endpoint 60 weeks.
Comparison 2. Quinolone versus tetracycline.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people with one or more exacerbations | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
Comparison 3. Quinolone versus macrolide.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people with one or more exacerbations | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
Comparison 4. Macrolide versus tetracycline.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people with one or more exacerbations | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Brill 2015.
| Methods |
Design: single‐centre, single‐blind, randomised placebo‐controlled trial in the UK Duration: 13 weeks Setting: hospital outpatients |
|
| Participants |
Population: 99 stable participants recruited from primary (local general practices and pulmonary rehabilitation groups) and secondary care (hospital outpatient clinics and local research cohorts) Baseline characteristics: mean age: 69.4 years, current smokers (n): 41/99, mean pack years: 53, mean number of exacerbations in the previous year (self‐reported): 2.2, mean ICS use (n): 17/99, mean FEV1% predicted: 50.5%, FEV1:FVC ratio: 0.50 Inclusion criteria: age ≥ 45 years at screening, with chronic bronchitis, spirometry confirmed COPD as FEV1 < 80% predicted with FEV1:FVC ratio < 0.7 and history of smoking or other plausible irritant exposure, chronic sputum production (expectoration of sputum on most days), able to give informed consent and able to complete symptom questionnaires and a daily diary card Exclusion criteria: other significant respiratory disease, COPD exacerbation four weeks prior to randomisation, clinically significant hepatic or renal impairment on screening blood tests, evidence of tuberculosis on screening sputum sample at recruitment, uncontrolled hypertension, prolonged QT on electrocardiogram or history of long QT syndrome, already taking long‐term antibiotics for any reason or any other contraindicated medication, hypersensitivity to any trial antibiotics |
|
| Interventions |
|
|
| Outcomes |
We were only able to report the number of participants with one or more exacerbations as other outcome results were reported as change from baseline relative to the placebo group. |
|
| Notes | Funding: National Institute for Health Research (NIHR) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Internet randomisation was performed using a computer‐generated permuted block system of variable sizes (sealed envelope, UK) |
| Allocation concealment (selection bias) | Low risk | Internet randomisation was performed using a computer‐generated permuted block system of variable sizes (sealed envelope, UK) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Patients remained blinded to treatment allocation. It was not clear if study personnel were blinded. The study is described as single‐blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description of outcome assessor blinding, although blinded participants assessed outcomes such as quality of life |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout low and balanced. All participants accounted for in the flow diagram |
| Selective reporting (reporting bias) | Low risk | Planned outcomes according to trial |
| Other bias | Unclear risk | Imbalance in baseline characteristics may affect the study results |
Shafuddin 2015.
| Methods |
Design: double‐blind, randomised, placebo‐controlled multi‐centred study carried out across Australia and New Zealand Duration: 12 weeks active treatment period followed by 48 weeks post‐treatment period Setting: 16 centres (15 hospitals and one research centre) across Australia and New Zealand |
|
| Participants |
Population: 292 adults with symptomatic COPD and positive Chlamydia pneumoniae (C pneumoniae) serology Baseline characteristics: age (mean, SD): 67.3 (8.58), current smoker (n): 71/292, tobacco consumption (pack year, mean, SD): 56.58 (33.3), number of previous exacerbations within two years (mean, SD): 5.11 (2.4), FEV1 (% predicted, mean, SD): 34 (14.8), FVC (L, mean, SD): 2.23 (0.83), FEV1/FVC (mean, SD): 42 (10.2) Inclusion criteria: age 45 years and over, FEV1 ≤ 70% of predicted, FEV1/FVC ≤ 60% and reversibility < 15% and/or 200 mL, smoking history of ≥ 20 pack years, at least three confirmed COPD exacerbations in the last two years, positive serology for C. pneumoniae (IgG antibody titre ≥ 1:64), informed consent to participate in the trial Exclusion criteria: pulmonary disease other than COPD, antibiotic treatment four weeks prior to randomisation, exacerbations four weeks prior to randomisation, pregnancy or breastfeeding, hypersensitivity to trial antibiotics (macrolides, tetracyclines, beta‐lactams or sulphamethoxazole, trimethoprim), clinically significant cardiovascular, hepatic, renal or other systemic disease, known long QT syndrome or QTc > 450 ms, sick sinus syndrome, bradycardia (< 50 bpm), or severe hypokalaemia, epilepsy, treatment with an investigative drug four weeks prior to randomisation, treatment with medicine known to have important interactions with macrolides or tetracyclines, unlikely to comply |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
Funding: Sanofi‐Aventis Australia Pty Ltd (formally Hoechst Marion Roussel Pty Ltd) Aim of study: the original aim of the study was to assess whether treatment with roxithromycin with or without doxycycline can eradicate C pneumoniae infection and subsequently reduce exacerbation rates, but the authors considered this hypothesis unsubstantiated and clinically no longer relevant. The study allowed authors to address the role of prophylactic antibiotics in reducing COPD exacerbations. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Each eligible participant was assigned a sequential subject number followed by randomisation number provided by Hoechst Marion Roussel, Australia. Subjects were supplied with one of the three treatments according to their randomisation number. |
| Allocation concealment (selection bias) | Low risk | Each eligible participant was assigned a sequential subject number followed by randomisation number provided by Hoechst Marion Roussel, Australia. Subjects were supplied with one of the three treatments according to their randomisation number. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study medication was packed by Hoechst Marion Roussel in bottles labelled with the randomisation and batch numbers. The investigators, pharmacists and subjects were blinded to the study medication in these bottles. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Trialists confirm that all participants, personnel and outcome assessors remained blinded until data had been analysed. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More participants dropped out of combined antibiotics treatment arm (21 versus 13 in single antibiotic arm and 10 in placebo arm), although according to trialists reasons were not related to study medication. All patients included in ITT analysis |
| Selective reporting (reporting bias) | Low risk | Planned outcomes according to trial |
| Other bias | Unclear risk | Imbalance in baseline characteristics may affect the study results |
Bpm: beats per minute COPD: chronic obstructive pulmonary disease CRQ: Chronic Respiratory Questionnaire FEV1:FVC: forced expiratory volume in one second/forced vital capacity
FVC: forced vital capacity (Iitres) ICS: inhaled corticosteroids IgA: immunoglobulin A IgG: immunoglobulin G ITT: intention‐to‐treat SGRQ: Saint George's Respiratory Questionnaire
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Astaf'ev 2013 | Treatment duration was only 5 to 10 days |
| Blasi 2006/2010 | Comparison does not meet inclusion criteria: standard care + azithromycin versus standard care |
| Braendli 1982 | Treatment duration was only 10 days; abstract only |
| Cherniak 1959 | Unclear COPD diagnosis |
| Cooper 1975 | Treatment duration was only 7 days |
| Djajadiningrat 1964 | Population not clearly defined as COPD |
| Djajadiningrat 1966 | Unclear COPD diagnosis |
| Douglas 1957 | Treatment duration was 5 to 7 days |
| Edwards 1958 | Comparison does not meet inclusion criteria: oxytetracycline versus blank control |
| Fear 1962 | Population not clearly defined as COPD |
| Ferguson 1974 | Unclear COPD diagnosis |
| Francis 1960 | Unclear COPD diagnosis |
| Gaffuri Riva 1990 | Unclear COPD diagnosis; abstract only |
| Gonschewski 1981 | Treatment duration was only 10 days |
| Goslings 1967 | Unclear COPD diagnosis |
| Knothe 1978 | Treatment duration was only 14 days |
| MacKay 1979 | Treatment duration was only 7 days |
| Maesen 1974 | Population does not meet inclusion criteria (acute exacerbations) |
| Maguire 2010 | Comparison does not meet inclusion criteria: azithromycin versus placebo |
| Marcic 1977 | Treatment duration was only 28 days |
| Molla 1974 | Population does not meet inclusion criteria (acute exacerbations) |
| Murdoch 1959 | Unclear population; two trials, each comparing antibiotic versus placebo |
| NCT03262142 | Treatment duration was only 14 days |
| No author 1969 | Cross‐over study with no indication of duration of washout period |
| No author 1972 | Cross‐over study with no indication of washout period |
| Nonikov 2001 | Mixed population; unclear COPD diagnosis |
| Pines 1967 | Description of 3 separate trials, treatment duration was 14 days |
| Pines 1967a | Description of 3 separate trials, treatment duration was 14 days |
| Pines 1973 | Population was not clearly defined, duration of treatment was 10 weeks |
| Pinto 1958 | Treatment duration was only 5 to 9 days; unclear population |
| Puchelle 1975 | Treatment duration was only 7 days |
| Pugh 1964 | Treatment duration was only 6 weeks |
| Ras 1984 | No report of randomisation of participants |
| Schildwächter 1977 | Treatment duration was only 10 days |
| Seemungal 2007 | Comparison does not meet inclusion criteria: macrolide versus placebo |
| Sokolova 2003 | Treatment duration was only 10 to 14 days |
| Uberti 1969 | Duration of treatment was only 5 days; no clear explanation of treatment, population |
| Verbist 1985 | Treatment duration was only 9 days |
| Waagepetersen 1973 | Treatment duration was only 10 days |
| Watanabe 1995 | Mixed population, results were not presented according to different population subgroups |
| Wegmüller 1979 | Treatment duration was only 10 days |
| Wilkinson 2007 | Comparison does not meet inclusion criteria: erythromycin versus placebo |
| Zervos 2005/2006 | Treatment duration was only 7 days |
COPD: chronic obstructive pulmonary disease
Differences between protocol and review
We prespecified that we would include studies comparing one antibiotic with another from different antibiotic classes, or antibiotics of different dosages within the same class. Upon screening references for this review, however, we identified one study that compared a combination of two antibiotics with one antibiotic (Shafuddin 2015). Although we did not anticipate such comparisons, we included the study in the review because it compared different antibiotic regimens, as prespecified in our protocol, and met the rest of our inclusion criteria. We extracted data for the antibiotic treatment arms only. See Characteristics of included studies for further details.
Pulsed, intermittent, and continuous prophylactic antibiotics definitions were used in this review to describe frequency of antibiotics administered, which are in line with the definitions in another review 'prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD) (Herath 2018).
Contributions of authors
CT: drafting of background and methods of protocol. Sifting and write‐up of full review.
SJ: sifting, data extraction, risk of bias assessment and write‐up of full review.
RF: drafting of background and methods of protocol. Sifting, data extraction, risk of bias assessment and write‐up of full review.
EB: conceptual and clinical advice on protocol. Arbitrating conflicts, analysis and interpretation, approval of final draft of full review.
Contributions of editorial team
Chris Cates (Co‐ordinating Editor): checked the data entry prior to the full write‐up of the review; edited the review; advised on methodology, interpretation and content; approved the final review prior to publication.
Ian Yang (Editor): edited the review; approved the final review prior to publication.
Emma Dennett (Managing Editor): coordinated the editorial process; advised on interpretation and content; edited the review.
Emma Jackson (Assistant Managing Editor): conducted peer review; obtained translations; edited the Plain Language Summary and reference sections of the protocol and the review.
Elizabeth Stovold (Information Specialist): designed the search strategy; ran the searches; edited the search methods section.
Sources of support
Internal sources
-
Christopher Threapleton, UK.
Salaried employee of St George's, University of London (supported by a NIHR programme grant)
-
Rebecca Normansell, UK.
Salaried employee of St George's, University of London (supported by a NIHR programme grant)
-
Emma Baker, UK.
Salaried employee of St George's, University of London
-
Sadia Janjua, UK.
Salaried employee at St George's University of London (supported by a NIHR programme grant)
External sources
-
National Institute for Health Research, UK.
Cochrane Programme Grant 16/114/21: NHS priorities in the management of chronic respiratory disease.
Declarations of interest
CT is employed part‐time by a NIHR Programme Grant to complete work on this review and is a clinical fellow in pharmacology.
SJ is employed full‐time as a systematic reviewer by a NIHR Programme Grant to complete work on this review.
RF is employed part‐time by a NIHR Programme Grant to complete work on this review and is a qualified general practitioner.
EB is a consultant clinical pharmacologist.
Edited (no change to conclusions)
References
References to studies included in this review
Brill 2015 {published data only}
- Brill SE, Law M, Allinson J, El‐Emir E, McHugh T, Donaldson G, et al. Bacterial resistance induction with prophylactic antibiotics in COPD [Abstract]. European Respiratory Journal 2014;44:P4731. [Google Scholar]
- Brill SE, Law M, El‐Emir E, Allinson JP, James P, Maddox V, et al. Effects of different antibiotic classes on airway bacteria in stable COPD using culture and molecular techniques: a randomised controlled trial. Thorax 2015;70(10):930‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brill SE, Law M, El‐Emir E, Allinson JP, Nazareth I, Donaldson GC, et al. Effect of antibiotics on airway bacteria in patients with chronic obstructive pulmonary disease (Abstract). American Journal of Respiratory and Critical Care Medicine 2014;189:A2874. [Google Scholar]
- NCT01398072. Development of an optimal antibiotic regime for long‐term therapy in stable chronic obstructive pulmonary disease (COPD) [A phase III single‐blind, randomised placebo controlled trial of long term therapy in patients with stable COPD using moxifloxacin, azithromycin and doxycycline: a bayesian decision analysis, including other criteria, will be used to distinguish the optimal antibiotic treatment]. clinicaltrials.gov/show/NCT01398072 (first received 20 July 2011).
Shafuddin 2015 {published data only}
- Shafuddin E, Mills GD, Holmes MD, Poole PJ, Mullins PR, Black PN, et al. A double‐blind, randomised, placebo‐controlled study of roxithromycin and doxycycline combination, roxithromycin alone, or matching placebo for 12 weeks in adults with frequent exacerbations of chronic obstructive pulmonary disease. Journal of Negative Results in Biomedicine 2015;14(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Astaf'ev 2013 {published data only}
- Astaf'ev AV, Styrt EA, Sinopal'nikov AL. Infectious exacerbation of chronic obstructive pulmonary disease: prospects for high‐dose levofloxacin therapy. Klinicheskaia Meditsina 2013;91:44‐50. [PubMed] [Google Scholar]
Blasi 2006/2010 {published data only}
- Blasi F, Bonardi D, Guffanti E, Confalonieri M, Tarsia P, Alberti S, et al. Azithromycin prophylaxis in COPD patients with tracheostomy. Proceedings of the American Thoracic Society. 2006:A21.
Braendli 1982 {published data only}
- Braendli O, Keller R, Fruehauf B, Matter JP, Finsinger F. Brodimoprim(Reg.trademark) (RO 10‐5970) versus doxycycline in chronic bronchitis. A randomised controlled clinical trial. Chemioterapia. 1982; Vol. 1:157.
Cherniak 1959 {published data only}
- Cherniack NS, Vosti KL, Dowling HF, Lepper MH, Jackson GC. Long‐term treatment of bronchiectasis and chronic bronchitis; a controlled study of the effects of tetracycline, penicillin, and an oleandomycin penicillin mixture. Archives of Internal Medicine 1959;103:345‐53. [DOI] [PubMed] [Google Scholar]
Cooper 1975 {published data only}
- Cooper J, Inman JS, Currie WJ. Prophylactic treatment of chronic bronchitis comparing co‐trimoxazole and amoxicillin. British Journal of Clinical Practice 1975;29:307‐10. [PubMed] [Google Scholar]
Djajadiningrat 1964 {published data only}
- Djajadiningrat RJ, Hrouda J, Goslings WR. The relationship of results of sputum cultures to clinical effects in a controlled trial of continuous antibiotic treatment of chronic bronchitis with demethylchlortetracycline or penicillin‐v. Acta Medica Scandinavica 1964;175:545‐55. [DOI] [PubMed] [Google Scholar]
Djajadiningrat 1966 {published data only}
- Djajadiningrat RJ, Goslings WR, Bergstein PG. The relationship between bacteriological and clinical results in patients with chronic bronchitis during long‐term therapy with tetracycline and sulfaphenazole. Nederlands Tijdschrift voor Geneeskunde 1966;110:427‐32. [PubMed] [Google Scholar]
Douglas 1957 {published data only}
- Douglas AC, Somner AR, Grant BL, Marks IWB. Effect of antibiotics on purulent sputum in chronic bronchitis and bronchiectasis. Lancet 1957;273:214‐18. [DOI] [PubMed] [Google Scholar]
Edwards 1958 {published data only}
- Edwards G, Fear EC. Adult chronic bronchitis: continuous antibiotic therapy. British Medical Journal 1958;2:1010‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fear 1962 {published data only}
- Fear EC, Edwards G. Antibiotic regimens in chronic bronchitis. British Journal of Diseases of the Chest 1962;56:153‐62. [DOI] [PubMed] [Google Scholar]
Ferguson 1974 {published data only}
- Ferguson GC. A comparison of oxytetracycline with doxycycline in the winter chemoprophylaxis of chronic bronchitis. British Journal of Clinical Practice 1974;28:131‐3. [PubMed] [Google Scholar]
Francis 1960 {published data only}
- Francis RS, Spicer CC. Chemotherapy in chronic bronchitis. Influence of daily penicillin and tetracycline on exacerbations and their cost. British Medical Journal 1960;30:297‐303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gaffuri Riva 1990 {published data only}
- Gaffuri Riva V, Piazza G, Calzavara MP, Crippa F, Montoli C. Comparison between ofloxacin and amoxicillin to prevent infective episodes in COPD. European Respiratory Journal 1990;3:117S. [Google Scholar]
Gonschewski 1981 {published data only}
- Gonschewski HH, Stempel G. Treatment of chronic bronchitis with azidocillin and co‐trimoxazole. Fortschritte der Medizin 1981;99:357‐60. [PubMed] [Google Scholar]
Goslings 1967 {published data only}
- Goslings WR, Djajadiningrat RJ, Bergstein PG, Holle P, Goslings WR, Djajadinigrat RJ, et al. Continuous suppressive antimicrobial treatment in chronic infected bronchitis during the winter months. Diseases of the Chest 1967;52:376‐80. [DOI] [PubMed] [Google Scholar]
Knothe 1978 {published data only}
- Knothe H, Wettengel R, Feldmeier W, Primer G. Treatment of chronic bronchitis with Supristol and a cotrimoxazole preparation. Medizinische Klinik 1978;73:1780‐4. [PubMed] [Google Scholar]
MacKay 1979 {published data only}
- MacKay AD. BTA study of amoxicillin and ampicillin in bronchitis. British Journal of Diseases of the Chest 1979;73:412. [Google Scholar]
Maesen 1974 {published data only}
- Maesen F, Buytendijk HJ, Beeuwkes H. Clinical experience with pivampicillin in chronic bronchitis. A comparative study of ampicillin and pivampicillin. Scandinavian Journal of Respiratory Diseases 1974;55:245‐55. [PubMed] [Google Scholar]
Maguire 2010 {published data only}
- Maguire G, Molanus B, Tchan M, Currie B. One year of weekly azithromycin provides no benefit for indigenous Australians living with COPD in remote Australia [Abstract]. Respirology 2010;15:A22. [Google Scholar]
Marcic 1977 {published data only}
- Marcic I. A comparative study of the therapeutic efficacy of azidocillin and doxycycline in chronic recurrent bronchitis. Praxis und Klinik der Pneumologie 1977;31:224‐8. [PubMed] [Google Scholar]
Molla 1974 {published data only}
- Molla AL. A comparative trial of amoxicillin and oxytetracycline in chronic bronchitis. Practitioner 1974;212:123‐8. [PubMed] [Google Scholar]
Murdoch 1959 {published data only}
- Murdoch HM, Leckie WJ, Downie J, Swain RH, Gould JC. An evaluation of continuous antibiotic therapy in chronic bronchitis. British Medical Journal 1959;2:1277‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT03262142 {published data only}
- NCT03262142. Targeted antibiotics for chronic obstructive pulmonary disease: a randomised multicenter trial investigating if targeted antibiotic therapy can improve the prognosis in COPD patients infected with pseudomonas aeruginosa. clinicaltrials.gov/show/NCT03262142 (first received 25 August 2017).
No author 1969 {published data only}
- Trimethoprim‐sulphamethoxazole in chronic bronchitis. The Practitioner 1969; Vol. 203:817‐89. [PubMed]
No author 1972 {published data only}
- A further comparative trial of co‐trimoxazole in chronic bronchitis. The Practitioner 1972; Vol. 209:838‐40. [PubMed]
Nonikov 2001 {published data only}
- Nonikov VE, Il'kovich MM, Konstantinova TD, Korovina OV, Lenkova NI, Ovcharenko SI, et al. Spiramycin and roxithromycin for the treatment of pneumonia and chronic bronchitis exacerbation. Antibiotics and Chemoterapy 2001;46:26‐8. [PubMed] [Google Scholar]
Pines 1967 {published data only}
- Pines A. Four trials of antibiotics in patients with chronic mucopurulent bronchitis. Postgraduate Medical Journal 1967;Suppl 43:14‐8. [PubMed] [Google Scholar]
Pines 1967a {published data only}
- Pines A, Raafat H. Controlled comparisons of cephaloridine with penicillin and streptomycin in chronic purulent bronchitis. Postgraduate Medical Journal 1967;Suppl 43:61‐3. [PubMed] [Google Scholar]
Pines 1973 {published data only}
- Pines A. Trimethoprim‐sulfamethoxazole in the treatment and prevention of purulent exacerbations of chronic bronchitis. Journal of Infectious Diseases 1973;Suppl 128:S706‐9. [DOI] [PubMed] [Google Scholar]
Pinto 1958 {published data only}
- Pinto ODSS. Novobiocin and tetracycline in chronic bronchitis. Lancet 1958;272(7054):1011‐2. [Google Scholar]
Puchelle 1975 {published data only}
- Puchelle E, Sobradillo V, Aug F, Sadoul P. Amoxicillin and ampicillin in the patient with chronic bronchitis. Comparative study : bacteriological, pharmacological and clinical. La Nouvelle Presse Medicale 1975;4:2449‐52. [PubMed] [Google Scholar]
Pugh 1964 {published data only}
- Pugh DL. Propicillin in the treatment of chronic bronchitis. British Journal of Clinical Practice 1964;18:81‐8. [PubMed] [Google Scholar]
Ras 1984 {published data only}
- Ras GJ, Anderson R, Eftychis HA, Koch U, Theron A, Wyk HA Van, et al. Chemoprophylaxis with erythromycin stearate or amoxicillin in patients with chronic bronchitis ‐ effects on cellular and humoral immune functions. South African Medical Journal 1984;66:955‐8. [PubMed] [Google Scholar]
Schildwächter 1977 {published data only}
- Schildwachter G. Azidocillin in chronic bronchitis. A comparative study with SMZ/TMP. Die Medizinische Welt 1977;28:190‐3. [PubMed] [Google Scholar]
Seemungal 2007 {published data only}
- Seemungal TA, Wilkinson TM, Perera W, Hurst J, Wedzicha JA. Long term macrolide therapy decreases exacerbations in COPD. American Thoracic Society International Conference; 2007 May 18‐23; San Francisco. 2007:[C97].
Sokolova 2003 {published data only}
- Sokolova VI, Shenderovich VA, Orlov VA, Smirnova LB. Clinical efficacy of carbapenems in the treatment of destructive pneumonia and chronic purulent bronchitis. Antibiotics and Chemoterapy 2003;48:21‐4. [PubMed] [Google Scholar]
Uberti 1969 {published data only}
- Uberti L. Prolonged preventive antibiotic therapy of chronic bronchitis. Clinica Terapeutica 1969;49:3‐22. [PubMed] [Google Scholar]
Verbist 1985 {published data only}
- Verbist L. Double‐blind comparison of tolerance of minocycline and doxycycline. Tijdschrift voor Geneeskunde 1985;41:281‐5. [Google Scholar]
Waagepetersen 1973 {published data only}
- Waagepetersen R, Thomsen VF, Thomsen V. Sulfhamethoxazole‐trimethoprim and ampicillin in the treatment of bronchitis. A comparative investigation employing a double‐blind technique. Ugeskrift for Laeger 1973;135:746‐50. [PubMed] [Google Scholar]
Watanabe 1995 {published data only}
- Watanabe A, Oizumi K, Motomiya M, Nukiwa T. Daily single‐dose regimen and alternate‐two‐week triple‐dose/day regimen of oral ofloxacin for the prophylaxis and control of exacerbations of chronic respiratory tract infections. Tohoku Journal of Experimental Medicine 1995;176:25‐33. [DOI] [PubMed] [Google Scholar]
Wegmüller 1979 {published data only}
- Wegmuller E. The treatment of chronic bronchitis with trimethoprim‐sulphamethoxazole (bactrim) a double‐blind trial in comparison with epicillin (spectacillin). Schweizerische Rundschau fur Medizin Praxis 1979;68:944‐9. [PubMed] [Google Scholar]
Wilkinson 2007 {published data only}
- Wilkinson TM, Seemungal TA, Sapsford R, Hurst JR, Perera W, Wedzicha JA. Effect of long‐term erythromycin in COPD trial (ELECT): Exacerbations and inflammation. Thorax 2007;62:A46. [Google Scholar]
Zervos 2005/2006 {published data only}
- Zervos M, Breen JD, Jorgensen DM, Goodrich JM. Azithromycin microspheres (AZ‐M) are as effective as levofloxacin (LEV) in subjects with moderate to very severe COPD. Proceedings of the American Thoracic Society. 2006:A121.
Additional references
Adeloye 2015
- Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, et al. Global and regional estimates of COPD prevalence: Systematic review and meta‐analysis. Journal of Global Health 2015;5(2):1‐17. [DOI: 10.7189/jogh.05-020415] [DOI] [PMC free article] [PubMed] [Google Scholar]
Albert 2011
- Albert RK, Connett J, Bailey WC, Casaburi R, Cooper JA Jr, Criner GJ, et al. Azithromycin for prevention of exacerbations of COPD. New England Journal of Medicine 2011;365(8):689‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beasley 2012
- Beasley V, Joshi PV, Singanayagam A, Molyneaux PL, Johnston SL, Mallia P. Lung microbiology and exacerbations in COPD. International Journal of COPD 2012;7:555‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
BNF
- Joint Formulary Committee. British National Formulary. www.medicinescomplete.com/mc (accessed prior to 16 January 2018). [www‐medicinescomplete‐com]
Chong 2012
- Chong J, Karner C, Poole P. Tiotropium versus long‐acting beta‐agonists for stable chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD009157.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chong 2013
- Chong J, Leung B, Poole P. Phosphodiesterase 4 inhibitors for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2013, Issue 11. [DOI: 10.1002/14651858.CD002309.pub4] [DOI] [PubMed] [Google Scholar]
Cote 2007
- Cote CG, Dordelly LJ, Celli BR. Impact of COPD exacerbations on patient‐centred outcomes. Chest 2007;131(3):696‐704. [DOI: 10.1378/chest.06-1610] [DOI] [PubMed] [Google Scholar]
Donaldson 2008
- Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2008;57(10):847‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Donath 2013
- Donath E, Chaudhry A, Hernandez‐Aya LF, Lit L. A meta‐analysis on the prophylactic use of macrolide antibiotics for the prevention of disease exacerbations in patients with chronic obstructive pulmonary disease. Respiratory medicine 2013;107:1385‐92. [DOI] [PubMed] [Google Scholar]
Donohue 2005
- Donohue JF. Minimally clinically important differences in COPD lung function. COPD 2005;2:111‐24. [DOI] [PubMed] [Google Scholar]
GOLD 2019
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of COPD 2019. goldcopd.org/gold‐reports/ (accessed on 5 February 2019).
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed prior to 16 January 2018. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Herath 2018
- Herath SC, Normansell R, Maisey S, Poole P. Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD). Cochrane Database of Systematic Reviews 2018, Issue 10. [DOI: 10.1002/14651858.CD009764.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hurst 2006
- Hurst JR, Perera WR, Wilkinson TM, Donaldson GC, Wedzicha JA. Systemic and upper and lower airway inflammation at exacerbation of chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine 2006;173(1):71‐8. [DOI] [PubMed] [Google Scholar]
Jaeschke 1989
- Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Controlled Clinical Trials 1989;10:407‐15. [DOI] [PubMed] [Google Scholar]
Janjua 2018
- Janjua S, Dias S, Threapleton CJ, Mathioudakis AG, Normansell R. Prophylactic antibiotics for adults with chronic obstructive pulmonary disease: a network meta‐analysis. Cochrane Database of Systematic Reviews 2018, Issue 11. [DOI: 10.1002/14651858.CD013198] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2002
- Jones PW. Interpreting thresholds for a clinically significant change in health status in asthma and COPD. European Respiratory Journal 2002;19:398‐404. [DOI: 10.1183/09031936.02.00063702] [DOI] [PubMed] [Google Scholar]
Kessler 2006
- Kessler R, Ståhl E, Vogelmeier C, Haughney J, Trudeau E, Löfdahl CG, et al. Patient understanding, detection, and experience of COPD exacerbations: an observational, interview‐based study. Chest 2006;130(1):133‐42. [DOI: 10.1378/chest.130.1.133] [DOI] [PubMed] [Google Scholar]
Kopsaftis 2018
- Kopsaftis Z, Wood‐Baker R, Poole P. Influenza vaccine for chronic obstructive pulmonary disease (COPD). Cochrane Database of Systematic Reviews 2018, Issue 6. [DOI: 10.1002/14651858.CD002733.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuwal 2018
- Kuwal A, Joshi V, Dutt N, Singh S, Agarwal KC, Purohit G. A prospective study of bacteriological etiology in hospitalised acute exacerbation of COPD patients: relationship with lung function and respiratory failure. Turkish Thoracic Journal 2018;19(1):19‐27. [DOI: 10.5152/TurkThoracJ.2017.17035] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2013
- Lee JS, Park D‐A, Hong Y, Jo KW, Lee SW, Huh JW, et al. Systematic review and meta‐analysis of prophylactic antibiotics in COPD and/or chronic bronchitis. The International Journal of Tuberculosis and Lung Disease 2013;17(2):153–62. [DOI] [PubMed] [Google Scholar]
Llor 2006
- Llor C, Cots JM, Herreras A. Bacterial etiology of chronic bronchitis exacerbations treated by primary care physicians [Etiología bacteriana de la agudización de la bronquitis crónica en atención primaria]. Archivos de Bronconeumologia 2006;42(8):388‐93. [PUBMED: 16948991] [DOI] [PubMed] [Google Scholar]
López‐Campos 2016
- López‐Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology 2016;21(1):14‐23. [DOI: 10.1111/resp.12660] [DOI] [PubMed] [Google Scholar]
Mannino 2015
- Mannino DM, Higuchi K, Yu TC, Zhou H, Li Y, Tian H, et al. Economic burden of COPD in the presence of co‐morbidities. Chest 2015;148(1):138‐50. [DOI: 10.1378/chest.14-2434] [DOI] [PMC free article] [PubMed] [Google Scholar]
Martinez 2008
- Martinez FJ, Curtis JL, Albery R. Role of macrolide therapy in chronic obstructive pulmonary disease. International Journal of COPD 2008;3(3):331‐50. [PUBMED: 18990961] [DOI] [PMC free article] [PubMed] [Google Scholar]
Matkovic 2013
- Matkovic Z, Miravitlles M. Chronic bronchial infection in COPD. Is there an infective phenotype?. Respiratory Medicine 2013;107(1):10‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
McCarthy 2015
- McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2015, Issue 2. [DOI: 10.1002/14651858.CD003793.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Miravitlles 2004
- Miravitlles M, Ferrer M, Pont Á, Zalacain R, Alvarez‐Sala JL, Masa F, et al. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax 2004;59(5):387‐95. [DOI: 10.1136/thx.2003.008730] [DOI] [PMC free article] [PubMed] [Google Scholar]
Miravittles 2015
- Miravittles M, Anzueto A. Antibiotic prophylaxis in COPD: why, when, and for whom?. Pulmonary Pharmacology and Therapeutics 2015;32:119‐23. [DOI] [PubMed] [Google Scholar]
Miravittles 2017
- Miravitlles M, Anzueto A. Chronic respiratory infection in patients with chronic obstructive pulmonary disease: what is the role of antibiotics?. International Journal of Molecular Sciences 2017;18(7):1344. [DOI: 10.3390/ijms18071344] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ni 2015
- Ni W, Shao X, Cai X, Wei C, Cui J, Wang R, et al. Prophylactic use of macrolide antibiotics for the prevention of chronic obstructive pulmonary disease exacerbation: a meta‐analysis. PLOS ONE 2015;10(3):e0121257. [DOI] [PMC free article] [PubMed] [Google Scholar]
Niewoehner 2006
- Niewoehner DE. The impact of severe exacerbations on quality of life and the clinical course of chronic obstructive pulmonary disease. American Journal of Medicine 2006;119(10 Suppl 1):S38‐S45. [DOI] [PubMed] [Google Scholar]
Oba 2018
- Oba Y, Keeney E, Ghatehorde N, Dias S. Dual combination therapy versus long‐acting bronchodilators alone for chronic obstructive pulmonary disease (COPD): a systematic review and network meta‐analysis. Cochrane Database of Systematic Reviews 2018, Issue 12. [DOI: 10.1002/14651858.CD012620.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Puhan 2016
- Puhan MA, Gimeno‐Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2016, Issue 12. [DOI: 10.1002/14651858.CD005305.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Punekar 2014
- Punekar YS, Shukla A, Müllerova H. COPD management costs according to the frequency of COPD exacerbations in UK primary care. International Journal of Chronic Obstructive Pulmonary Disease 2014;9:65‐73. [DOI: 10.2147/COPD.S54417] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rosell 2005
- Rosell A, Monsó E, Soler N, Torres F, Angrill J, Riise G, et al. Microbiologic determinants of exacerbation in chronic obstructive pulmonary disease. Archives of Internal Medicine 2005;165(8):891‐7. [DOI] [PubMed] [Google Scholar]
Sapey 2006
- Sapey E, Stockley RA. COPD exacerbations. 2: Aetiology. Thorax 2006;61:250‐8. [DOI: 10.1136/thx.2005.041822] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schmidt 2014
- Schmidt SA, Johansen MB, Olsen M, Xu X, Parker JM, Molfino NA, et al. The impact of exacerbation frequency on mortality following acute exacerbations of COPD: a registry‐based cohort study. BMJ Open 2014;4(12):1‐7. [DOI: 10.1136/bmjopen-2014-006720] [DOI] [PMC free article] [PubMed] [Google Scholar]
Seemungal 1998
- Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine 1998;157(5 Pt 1):1418‐22. [DOI] [PubMed] [Google Scholar]
Sethi 2004
- Sethi 2004. Bacteria in exacerbations of chronic obstructive pulmonary disease: phenomenon or epiphenomenon?. Proceedings of the American Thoracic Society 2004;1(2):109‐14. [DOI: 10.1513/pats.2306029] [DOI] [PubMed] [Google Scholar]
Sethi 2008
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. New England Journal of Medicine 2008;359(22):2355‐65. [DOI] [PubMed] [Google Scholar]
Thurston 2013
- Thurston SJ, Garcha DS, Donaldson GC, McHugh TD, Wedzicha JA. Impact of antibiotic exposure on the development of antibiotic resistance in COPD. American Journal of Respiratory and Critical Care Medicine 2013;187:A2181. [Google Scholar]
Wang 2016
- Wang Z, Bafadhel M, Haldar K, Spivak A, Mayhew D, Miller BE, et al. Lung microbiome dynamics in COPD exacerbations. European Respiratory Journal 2016;47(4):1082‐92. [DOI: 10.1183/13993003.01406-2015] [DOI] [PubMed] [Google Scholar]
Wedzicha 2017
- Wedzicha JA, Calverley PM, Albert RK, Anzueto A, Criner GJ, Hurst JR, et al. Prevention of COPD exacerbations:a European Respiratory Society/American Thoracic Society guideline. European Respiratory Journal 2017;50(3):1602265. [DOI] [PubMed] [Google Scholar]
WHO 2018
- World Health Organization. Chronic respiratory diseases: burden of COPD. www.who.int/respiratory/copd/burden/en/ (accessed 21 March 2018).
Wüst 2007
- Wüst RCI, Degens H. Factors contributing to muscle wasting and dysfunction in COPD patients. International Journal of Chronic Obstructive Pulmonary Disease 2007;2(3):289‐300. [PMC free article] [PubMed] [Google Scholar]
Yang 2012
- Yang IA, Clarke MS, Sim EH, Fong KM. Inhaled corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD002991.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yao 2013
- Yao G‐Y, Ma Y‐L, Zhang M‐O, Gao Z‐C. Macrolide therapy decreases chronic obstructive pulmonary disease exacerbation: a meta‐analysis. Respiration 2013;86:254‐60. [DOI] [PubMed] [Google Scholar]
Zwerink 2014
- Zwerink M, Brusse‐Keizer M, Valk PD, Zielhuis GA, Monninkhof EM, Palen J, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2014, Issue 3. [DOI: 10.1002/14651858.CD002990.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Threapleton 2018
- Threapleton CJD, Normansell R, Baker EH. Head‐to‐head oral prophylactic antibiotics therapy for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2018, Issue 5. [DOI: 10.1002/14651858.CD013024] [DOI] [PMC free article] [PubMed] [Google Scholar]


