Abstract
Objective:
The current review provides an evidence base update of psychosocial treatments for self-injurious thoughts and behaviors (SITBs) in youth.
Method:
A systematic search was conducted of two major scientific databases (PsycInfo and PubMed) and ClinicalTrials.gov for relevant randomized controlled trials (RCTs) published prior to June 2018.
Results:
The search identified 26 RCTs examining interventions for SITBs in youth: 17 were included in the 2015 review and 9 trials were new to this update. The biggest change since the prior review was the evaluation of Dialectical Behavior Therapy for Adolescents (DBT-A) as the first Level 1: Well-established intervention for reducing deliberate self-harm (composite of nonsuicidal and suicidal self-injury) and suicide ideation in youth and Level 2: Probably efficacious for reducing nonsuicidal self-injury and suicide attempts. Five other interventions were rated as Level 2: Probably efficacious for reducing SITBs in youth, with the new addition of Integrated Family Therapy.
Conclusions:
This evidence base update indicates that there are a few promising treatments for reducing SITBs in youth. Efficacious interventions typically include a significant family or parent training component as well as skills training (e.g., emotion regulation skills). Aside from DBT-A, few treatments have been examined in more than one RCT. Given that replication by independent research groups is needed to evaluate an intervention as Well-established, future research should focus on replicating the five promising interventions currently evaluated as Probably efficacious. In addition, an important future direction is to develop brief efficacious interventions that may be scalable to reach large numbers of youth.
Keywords: nonsuicidal self-injury, randomized controlled trial, suicide, treatment, treatment effectiveness
Self-injurious thoughts and behaviors (SITBs) refers to a range of thoughts and actions related to deliberate, self-directed, and non-fatal harm (Nock, 2010). This broad class can be divided into two subcategories—nonsuicidal self-injury and suicidal self-injury—both of which are highly prevalent and impairing among youth. Nonsuicidal self-injury (NSSI) refers to cognitions and behaviors related to self-inflicted harm without any intent to die, such as nonsuicidal cutting, burning, and scratching (Nock, 2010; Silverman, Berman, Sanddal, O’Carroll, & Joiner, 2007). Cross-national estimates indicate that approximately 17–18% of youth will engage in NSSI in their lifetime (Muehlenkamp, Claes, Havertape, & Plener, 2012; Swannell, Martin, Page, Hasking, & St John, 2014). Suicidal self-injury refers to cognitions (suicide ideation) and behaviors (suicide attempts) related to self-inflicted harm with at least some intent to die (Nock, 2010; Silverman et al., 2007). In 2017 in the U.S., approximately 17.2% of youth seriously considered suicide and 7.4% made at least one suicide attempt (CDC, 2017b).
SITBs are relatively rare in childhood but increase significantly during the transition to and throughout adolescence (Glenn et al., 2017; Nock et al., 2008; Nock et al., 2013). Among youth 10–19 years old, SITBs are associated with significant academic and social impairment (Copeland, Goldston, & Costello, 2017; Foley, Goldston, Costello, & Angold, 2006), substantial burden to the healthcare system (CDC, 2017a), and significantly increased risk for suicide death—the 2nd leading cause of death among this age group (CDC, 2017a). Taken together, adolescence is a developmental period where SITBs typically begin, increase in prevalence, and significantly impair functioning. As such, this period represents a critical opportunity for effective intervention and prevention of SITBs (National Action Alliance for Suicide Prevention (NAASP): Research Prioritization Task Force, 2014; Wyman, 2014).
Interventions specifically designed for reducing SITBs in children and adolescents have increased significantly over the past 15 years. The 2015 review on this topic (Glenn, Franklin, & Nock, 2015) was the first JCCAP Evidence-Base Update of psychosocial treatments for SITBs in youth. This prior review included 18 randomized controlled trials (RCTs), five non-randomized controlled trials, and six pilot studies of various psychological interventions for reducing SITBs in youth. No treatments were identified as Well-established, or leading, interventions for SITBs in children and adolescents. However, a number of interventions were identified as Probably efficacious, but most had only been tested in one RCT.
The purpose of the current Evidence Base Update is to provide an updated review of psychosocial treatments for SITBs in youth (i.e., covering the past five years since the prior review ended in September 2013). Given the increasing number of RCTs, and because such research designs provide the best test of treatment efficacy, we chose to focus this review exclusively on RCTs. When evaluating the overall research literature, we briefly review the RCTs that were included in the 2015 review (and refer the reader to that review for additional details). The focus of this review is on the new trials identified since the prior review and changes in treatment efficacy based on this new research.
Update Review Parameters
To identify all relevant trials that examined a psychosocial intervention aimed at reducing SITBs in children or adolescents, we performed a comprehensive search of two major scientific databases (PsycInfo and PubMed) for journal articles in English published or in press prior to June 1, 2018. Searches included combinations of terms for SITBs (NSSI, nonsuicidal self-injury, cutting, parasuicide, self-harm, self-injury, self-injurious, self-mutilation, self-poisoning, suicide, suicide ideation, suicidal thoughts, suicide gesture, suicide attempt, suicidal behavior, suicide event, suicide plan, suicidality), interventions (clinical trial, counseling, counselling, intervention, program, randomized, psychotherapy, therapy, therapeutic, treatment), and children and adolescents (adolescence, adolescent, child, childhood, children, teen, teenagers, student, young people, youth). In addition to these online databases, we also searched ClinicalTrials.gov for any relevant ongoing or recently completed clinical trials that may be relevant to this review.
Inclusion and exclusion criteria
Studies were included if they: (1) targeted children and/or adolescents under the age of 19, (2) examined a psychosocial intervention (i.e., medication trials were excluded) specifically designed to treat SITBs, (3) measured a specific SITB outcome, (4) included a control or comparison group to the experimental intervention, (5) randomly assigned participants to treatment groups, and (6) included sample sizes larger than or equal to 20 subjects per group at the point of randomization (Hsu, 2016). First, we restricted our review to interventions that explicitly targeted children and adolescents. Given that SITBs are relatively rare in childhood, most studies focused on treating SITBs in adolescents. A few studies included children as young as age 10 (Asarnow et al., 2011; Harrington et al., 1998; Huey et al., 2004). Some of the reviewed studies included participants who were older than 19 years of age (Morthorst, Krogh, Erlangsen, Alberdi, & Nordentoft, 2012; Robinson et al., 2012; Rudd et al., 1996). However, these studies were only included if they assessed a SITB outcome in a subset of participants who were younger than 19.
Second, and consistent with the 2015 review (Glenn et al., 2015), we elected to only include interventions specifically designed to treat SITBs in at-risk youth. Thus, we excluded treatments that were designed to treat specific psychiatric disorders (e.g., borderline personality disorder, major depressive disorder) and school-based prevention programs. The rationale for this decision was twofold. First, SITBs are transdiagnostic, and as such, we did not want to include studies in which participants were recruited based on a particular diagnostic status. Doing so would give preferential attention to treatments for some disorders over others, which would potentially bias our review of existing evidence. Second, we excluded school-based prevention programs, as such programs are generally aimed to prevent incidents or reduce overall rates of SITBs in a group that includes both at-risk and healthy youth, rather than to intervene among youth who were already determined to be at high-risk (for reviews of prevention programs: see Katz et al., 2013; Robinson et al., 2013; Singer, Erbacher, & Rosen, 2018).
Third, we included studies that reported at least one of the following specific SITB outcomes: (a) suicide ideation (SI: active thoughts of ending one’s life), (b) suicide attempts (SAs: self-injurious behavior engaged in with some intent to die), (c) suicide-related behavior (SRB: refers collectively to suicide ideation, plans/preparations, and attempts), (d) nonsuicidal self-injury (NSSI: self-injurious behavior engaged in without intent to die), or (e) deliberate self-harm (DSH: refers collectively to self-injurious behaviors performed with OR without intent to die). Our search also included studies that examined suicide planning and suicide gestures, but no such studies met the other inclusion criteria for the current review. It is important to note that most studies in this review recruited youth based on prior history of SITBs. Thus, treatment efficacy for most studies was evaluated by examining between-group differences in the recurrence of SITBs over the treatment period (e.g., repetition of DSH, suicide reattempts). Moreover, because our review was focused on treatments for SITBs, we report changes in SITB outcomes specifically, and not changes in all potentially relevant clinical symptoms or indices of functioning/impairment.
Finally, the current review focused on RCTs with sample sizes of at least 20 subjects per group (at randomization). We chose to exclude studies with smaller sample sizes due to problems of group nonequivalence that often arise in such cases (Hsu, 2016). That is, when groups have small sample sizes, random assignment often fails to account for all possible nuisance variables. Thus, any differences that are detected between groups may be due to factors other than the effects of the treatment under investigation. We do note, however, promising randomized trials that included smaller sample sizes where relevant.
Evaluation criteria
Psychosocial interventions were evaluated using the JCCAP Evidence Base Update EBT evaluation criteria (see Table 1). JCCAP uses a 5-level ranking system (Southam-Gerow & Prinstein, 2014), adapted from the APA Division 12 Task Force on the Promotion and Dissemination of Psychological Procedures to determine intervention potency (Chambless et al., 1998; Chambless & Hollon, 1998; Silverman & Hinshaw, 2008). Using these criteria, intervention efficacy is evaluated by the number and quality of studies. RCTs are the highest-quality studies comparing the experimental treatment to another active treatment/psychological placebo or to a wait list/no treatment control. Table 1 displays the criteria for the five levels of treatment efficacy—Level 1: Well-established, Level 2: Probably efficacious, Level 3: Possibly efficacious, Level 4: Experimental, and Level 5: Questionable efficacy.
Table 1.
JCCAP Evidence Base Updates EBT Evaluation Criteria.
| Methods criteria |
| M.1. Group design: Study involved a randomized controlled design |
| M.2. Independent variable defined: Treatment manuals or logical equivalent were used for the treatment |
| M.3. Population clarified: Conducted with a population, treated for specified problems, for whom inclusion criteria have been clearly delineated |
| M.4. Outcomes assessed: Reliable and valid outcome assessment measures gauging the problems targeted (at a minimum) were used |
| M.5. Analysis adequacy: Appropriate data analyses were used and sample size was sufficient to detect expected effects |
| Level 1: Well-Established Treatments |
| Evidence criteria |
| 1.1 Efficacy demonstrated for the treatment by showing the treatment to be either: |
| 1.1.a. Statistically significantly superior to pill or psychological placebo or to another active treatment |
| OR |
| 1.1.b. Equivalent (or not significantly different) to an already well-established treatment in experiments |
| AND |
| 1.1c In at least two (2) independent research settings and by two (2) independent investigatory teams demonstrating efficacy |
| AND |
| 1.2 All five (5) of the Methods Criteria |
| Level 2: Probably Efficacious Treatments |
| Evidence criteria |
| 2.1 There must be at least two good experiments showing the treatment is superior (statistically significantly so) to a wait-list control group |
| OR |
| 2.2 One (or more) good experiments meeting the Well-Established Treatment level except for criterion 1.1c (i.e., Level 2 treatments will not involve independent investigatory teams) |
| AND |
| 2.3 All five (5) of the Methods Criteria |
| Level 3: Possibly Efficacious Treatments |
| Evidence criterion |
| 3.1 At least one good randomized controlled trial showing the treatment to be superior to a wait list or no-treatment control group |
| AND |
| 3.2 All five (5) of the Methods Criteria |
| OR |
| 3.3 Two or more clinical studies showing the treatment to be efficacious, with two or more meeting the last four (of five) Methods Criteria, but none being randomized controlled trials |
| Level 4: Experimental Treatments |
| Evidence criteria |
| 4.1. Not yet tested in a randomized controlled trial |
| OR |
| 4.2. Tested in 1 or more clinical studies but not sufficient to meet level 3 criteria. |
| Level 5: Treatments of Questionable Efficacy |
| 5.1. Tested in good group-design experiments and found to be inferior to other treatment group and/or wait-list control group; i.e., only evidence available from experimental studies suggests the treatment produces no beneficial effect. |
Adapted from Silverman and Hinshaw (2008) and Division 12 Task Force on Psychological Interventions’ reports (Chambless et al., 1996, 1998), from Chambless and Hollon (1998), and from Chambless and Ollendick (2001). Chambless and Hollon (1998) described criteria for methodology.
For JCCAP Evidence Base Updates, interventions are classified into broad families of treatments based on the type and mode of treatment (e.g., Cognitive behavioral therapy—Individual) rather than by treatment “brand names” (e.g., Reframe-IT; Hetrick et al., 2017). The rationale for this classification is provided in Southam-Gerow and Prinstein (2014). It is important to note that some of the treatment family names have changed since the 2015 review to best reflect the RCTs included in this updated review. When applicable, we note both the old and new treatment family names.
Evaluations of treatment families were made by two authors (CG, EE, DP) independently with discrepancies resolved in consensus coding meetings with all three authors. For treatment families with mixed results, we evaluated whether the majority of evidence suggests an intervention is efficacious (Chambless & Hollon, 1998). If comparable designs yielded conflicting findings, we evaluated interventions conservatively and did not classify them as Level 1: Well-established or Level 2: Probably efficacious. We were also conservative when classifying interventions as Level 5: Questionable efficacy and only did so when there were at least two trials indicating that the experimental intervention was not beneficial as compared to the control/comparison treatment group.
In the sections that follow, we review the existing RCTs testing treatments for SITBs in youth in two ways. Consistent with the guidelines for JCCAP Evidence Base Updates, we review and evaluate the broad treatment families (type and mode) using the JCCAP criteria in Table 1. However, we recognize that this classification method requires collapsing across different types of interventions, thereby minimizing differences across treatment programs that may be important. Therefore, we also discuss each individual trial using its “brand name” and specific aspects of the treatment package and trial that may be important for evaluating its efficacy.
Review of Interventions for Self-Injurious Thoughts and Behaviors
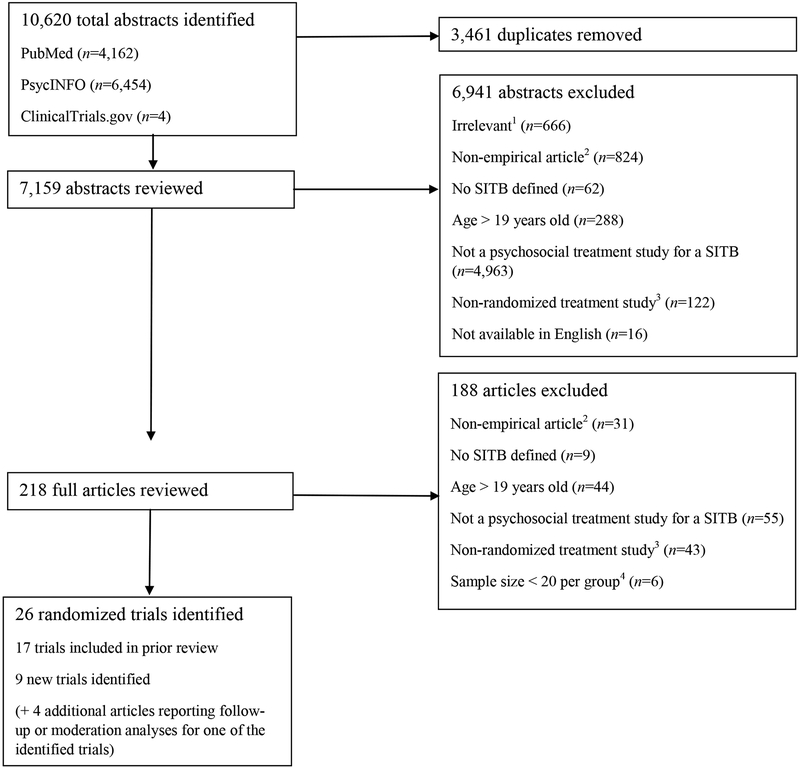
Based on the review parameters described above, our comprehensive search yielded 26 RCTs of psychosocial interventions for youth SITBs: 17 RCTs were included in the 2015 review and 9 RCTs are new to this review (see Figure 1 PRISMA diagram). Table 2 provides the following detailed information for each trial: sample size, sample demographic characteristics, recruitment setting, sample inclusion and exclusion criteria, major diagnoses of the sample, SITB outcomes assessed and how they were measured, treatment type, treatment dose, number of assessments in the trial, treatment completion and study attrition (when available), and main trial results. Table 3 displays the treatment efficacy ratings for the broad treatment families and references for the trials that were evaluated when making these ratings.
Figure 1.
PRISMA diagram for systematic literature review.
SITB=self-injurious thought and behavior
1 Irrelevant refers to abstracts that resulted from the search terms but were not relevant for our review (e.g., cell death, suicide gene, general mortality data, medical procedures referred to as “cutting-edge”).
2 Non-empirical refers to review papers, opinion pieces, commentaries, and procedure descriptions.
3 Non-randomized treatment study refers to case studies, pilot studies, or non-randomized control studies.
4 Studies with less than 20 subjects per group were removed due to the increased likelihood of nonequivalence between groups (Hsu, 2016).
Table 2.
Randomized Trials of Psychosocial Interventions for Self-injurious Thoughts and Behaviors in Youth.
| Treatment Family | Citation | Sample Size (at randomization) | Sample Characteristics | Recruitment Setting | Inclusion (In) and Exclusion (Ex) Criteria | Major Diagnoses | SITB Outcomes (Measures) |
Treatment Conditions, Dose, and Assessments | Treatment Attrition and Completion (if available) | Main Results |
|---|---|---|---|---|---|---|---|---|---|---|
| DBT-A | McCauley et al. (2018) | 173; T=86, C=87 |
12–18 years old; 95% female; 56% Caucasian, 27% Hispanic, 7% African American, 6% Asian American, <1% Native American, 2% other | ED, inpatient, outpatient, community | In: Lifetime SA≥1; elevated past-month SI (SIQ-Jr≥24); DSH lifetime≥3 episodes + at least 1 DSH episode in past 12 weeks; meet at least 3 BPD criteria Ex: IQ<70; psychosis; mania; AN; life-threatening condition; youth not fluent in English; parent not fluent in English or Spanish |
MDD (84%); ANX (54%); BPD (53%); ED (<1%) |
SI (SIQ-Jr); SA (SASII); NSSI (SASII); DSH (SASII) |
T: DBT-A (individual sessions, multifamily group skills training, youth and parent telephone coaching, individual parent session, family sessions [as needed]); Dose: 6 months of weekly individual and group sessions, weekly therapist team consultation C: Individual and Group Supportive Therapy (IGST; individual and group sessions, parent sessions [as needed]); Dose: 6 months of weekly individual and group sessions, weekly therapist team consultation Assessments: Pre-treatment (BL), mid-treatment (3 months), post-treatment (6 months), F/U at 9 and 12 months |
Treatment completion (≥24 adolescent sessions): T: 45.4% C: 16.1% Attrition: Post-treatment: T: 10.5% C: 24.1% 12-month F/U: T: 19.8% C: 26.4% |
Significantly greater decrease in SI and SA, NSSI, and DSH frequency for T as compared to C at post-treatment. NS between group differences in SI, SA, NSSI, or DSH from post-treatment to 12-month F/U. |
| DBT-A | Mehlum et al. (2014; 2016) | 77; T=39, C=38 |
12–18 years old; 88% female; 85% Norwegian | Outpatient | In: Lifetime DSH≥2 episodes + at least 1 DSH episode in past 16 weeks; at least 2 DSM-IV BPD criteria or 1 BPD criterion + 2 sub-threshold-level criteria; fluent in Norwegian Ex: BP; SZ; SCAD; psychotic disorder not otherwise specified; intellectual disability; Asperger syndrome |
ANX (43%); Other depressive disorder (38%); MDD (22%); BPD (21%); PTSD (17%); PD (9%); ED (8%); SUD (3%) |
DSH (LPC); SI (SIQ-Jr) |
T: DBT-A (individual sessions, multifamily skills training, family therapy or telephone coaching [as needed]); Dose: 19 weeks of weekly individual sessions (1 hour), weekly multi-family skills training (1.5 hours) C: EUC (TAU + therapists agreed to minimum dose); Dose: 19 weeks (minimum) of weekly individual sessions Assessments: Pre-treatment (BL), F/U at 9 and 15 weeks (during treatment), post-treatment (19 weeks), F/U at 71 weeks (1-year post-treatment) |
Treatment completion (≥ 50% of sessions): T: 74.4% C: 71% Attrition: Post-treatment: T: 0% C: 0% 71-week F/U: T: 2.6% C: 2.6% |
Significantly fewer DSH episodes and significantly greater decrease in SI for T as compared to C at post-treatment. Significantly fewer DSH episodes in T as compared to C from post-treatment to 71-week F/U. NS between group differences in SI at 71-week F/U. |
| CBT—Individual | Hetrick et al. (2017) | 50; T=26, C=24 |
13–19 years old; high school students; 82% female; race/ethnicity NR | High school | In: High school student; engaged with a well-being staff member (i.e., school counselor); experienced any level of SI in past 4-week period Ex: Intellectual disability; psychotic symptoms; youth not fluent in English |
NR | SI (SIQ); SA (2-item questionnaire) |
T: Reframe-IT (online CBT modules), TAU; Dose: 8 modules of CBT delivered over 10 weeks C: TAU (contact with school well-being staff, outpatient mental health counseling and medication management); Dose: Varied Assessments: Pre-treatment (BL), post-treatment (10 weeks), F/U at 22 weeks |
Attrition: Post-treatment: T: 30.8% C: 12.5% 22-week F/U: T: 50% C: 29.2% |
NS between group differences in SI or SA from BL to post-treatment or BL to 22-week F/U. |
| CBT— Individual + Family | Esposito-Smythers, Spirito, Kahler, Hunt, & Monti (2011)1 | 40; T=20, C=20 |
13–17 years old; 67% female; 89% Caucasian, 14% Hispanic | Inpatient | In: SA in past 3 months or significant SI (SIQ-Sn≥41); AUD or CUD; lived in the home with a parent/guardian willing to participate Ex: Verbal IQ<70; active psychosis; current homicidal ideation; BP; SUD other than AUD or CUD |
UMD (94%); CUD (83%); AUD (64%); ANX (56%); DBD (50%) |
SA (K-SADS-PL; depression module suicide items); SI (SIQ-Sn) |
T: Integrated CBT for AUD/SUD and suicide (CBT skills, family and parent training, [1] MI session), 18 months of free medication management; Dose: 6 months of weekly individual and weekly-biweekly parent sessions, 3 months of biweekly individual and biweekly-monthly parent sessions, 3 months of monthly individual sessions (monthly parent sessions as needed), conjoint family sessions as needed C: Enhanced TAU – diagnostic evaluation, offer for 18 months of free medication management, community-based TAU; Dose: Varied over 12 months Assessments: Pre-treatment (BL), F/U at 3, 6, 12, and 18 months post-enrollment |
Treatment completion (≥24 adolescent sessions, ≥12 parent sessions): T: 74% adolescents + 90% parents C: 44% adolescents + 25% parents Attrition: 18-month F/U: T: 25% C: 15% |
Significantly fewer T participants made a SA as compared to C over 18-month F/U. NS between group difference in SI over 18-month F/U. |
| IPT-A—Individual | Tang, Jou, Ko, Huang, & Yen (2009)1 | 73; T=35, C=38 |
12–18 years old; high school students; 66% female; race/ethnicity NR (study conducted in Taiwan) | High school | In: Moderate to severe MDD (BDI>19); SI or lifetime history of SA (BSS>0); moderate to severe ANX (BAI>16); significant hopelessness (BHS>8) in past 2 weeks Ex: Acute psychosis; drug abuse; PD; serious medical condition; severe (e.g., high-lethality) suicidal behaviors; lack of proper care for suicidal risk by family |
MDD (100%) | SI (BSS) |
T: Intensive Interpersonal Psychotherapy for depressed adolescents with suicide risk (IPT-A-IN; school-based intervention); Dose: 2 sessions weekly, 30-minute phone F/U for 6 weeks C: TAU in schools (psychoeducation, irregular supportive counseling [parent included as needed]); Dose: 30- to 60-minute sessions once or twice weekly for 6 weeks Assessments: Pre-treatment (BL), post-treatment (6 weeks) |
Treatment completion: T: 100% C: 92.1% Attrition: Post-treatment: T: 0% C: 7.9% |
Significantly greater decrease in SI for T as compared to C at post-treatment. |
| Psychodynamic Therapy —Individual + Family | Rossouw & Fonagy (2012)1 | 80; T=40, C=40 |
12–17 years old; 85% female; 75% Caucasian, 10% Asian, 5% African American, 8% mixed race, 3% other | ED, community mental health | In: ≥1 DSH episode in past month Ex: Required inpatient care; ED (in the absence of self-harm); PDD; psychosis; severe learning disability (IQ<65); chemical dependence |
MDD (96%); BPD (73%); Alcohol problems (44%); Substance misuse (28%) |
DSH (RTSHI) |
T: Mentalization-Based Treatment (MBT-A; individual + family therapy) for self-harm; Dose: Weekly individual + monthly family therapy for 12 months C: Community-based TAU (varied, [e.g., individual counseling, family therapy]); Dose: 12 months, varied Assessments: Pre-treatment (BL), 3, 6, and 9 months after randomization, post-treatment (12 months) |
Treatment completion: T: 50% C: 42.5% Attrition: 3-month F/U: T: 13% C: 8% 6-month F/U: T: 3% C: 10% 9-month F/U: T: 13% C: 15% 12-month F/U: T: 10% C: 13% |
Significantly greater decrease in DSH (RTSHI scores) for T as compared to C at post-treatment. Significantly lower odds of reporting ≥ 1 DSH episode in past 3 months for T as compared to C at post-treatment. Significantly greater rate of decline in DSH (RTSHI scores) for T as compared to C over treatment period. |
| Psychodynamic Therapy—Family-Based | Diamond et al. (2010)1 | 66; T=35, C=31 |
12–17 years old; 83% female; 74% African American | ED, primary care | In: SI (SIQ-Jr>31) and moderate depression (BDI-II >20) at 2 pre-BL screenings Ex: Needed psychiatric hospitalization; recent discharge from psychiatric hospital; psychosis; mental retardation or borderline intellectual functioning |
ANX (67%); ADHD or DBD (58%); MDD (39%) |
SI (SIQ-Jr, self-report; SSI, clinician-report) | T: Attachment-Based Family Therapy (ABFT; individual youth and parent sessions, joint parent-youth sessions); Dose: Weekly sessions for 3 months C: Enhanced TAU (E-TAU; referral to care, clinical monitoring); Dose: Varied Assessments: Pre-treatment (BL), mid-treatment (6 weeks), post-treatment (12 weeks), F/U at 24 weeks |
Treatment completion: ≥ 1 session: T: 91.4% C: 67.7% ≥ 6 sessions: T: 68.6% C: 19.4% ≥ 10 sessions: T: 62.9% C: 6.5% Attrition: Mid-treatment: T: 5.7% C: 12.9% Post-treatment: T: 11.4% C: 6.5% 24-week F/U: T: 11.4% C: 16.1% |
Significant decrease in SI (self- and clinician-reported) for T as compared to C at post-treatment and 24-week F/U. Significantly greater rate of change in SI over treatment period for T as compared to C. Significantly greater proportion of T reported no past-week SI as compared to C at post-treatment and 24-week F/U (self- and clinician-reported). |
| Psychodynamic Therapy — Family-Based | Diamond et al. (2018) | 129; T=66, C=63 |
12–18 years old; 82% female; 50% African American, 29% Caucasian, 2% Asian, 2% American Indian or Alaskan Native, <1% Native Hawaiian/Pacific Islander, 8% mixed race, 9% other; 31% identified as lesbian, gay, or bisexual | ED, inpatient, mental health agencies, primary care, schools, community | In: SI (SIQ-Jr≥31) and moderate depressive symptoms (BDI-II >20) at 2 pre-BL screenings Ex: Imminent risk of harm to self or others; psychosis; severe cognitive impairment; start psychiatric medication within 3-weeks of BL; parent not fluent in English |
ANX (47%); MDD (41%) |
SI (SIQ-Jr); SA (C-SSRS); NSSI (C-SSRS) |
T: Attachment-Based Family Therapy (ABFT; individual youth and parent sessions, joint parent-youth sessions); Dose: 16 weeks C: Family-enhanced nondirective supportive therapy (FE-NST; individual youth and parent sessions, joint parent-youth sessions); Dose: 16 weekly individual sessions, 1 joint youth-parent session, 4 parent education sessions Assessments: Pre-treatment (BL), post-treatment (4, 8, 12, and 16 weeks), (F/U data collected at 24, 32, 40, and 52 weeks not reported here) |
Treatment completion: T: 81.8% C: 82.5% Attrition: T: 18.2% C: 17.5% |
NS between group differences in rate of change of SI, SI remission rate (SIQ-Jr <12), and SI response rate (≥50% decrease from BL SIQ-Jr) over treatment period. NS between group difference in SA over treatment period. |
| Family Therapy | Cottrell et al. (2018) | 832; T=415, C=417 |
11–17 years old; 89% female; race/ethnicity NR | Mental health services | In: ≥2 DSH episodes prior to referral to Child and Adolescent Mental Health Services (CAMHS); living with primary caregiver willing to participate Ex: Severe suicide risk; ongoing child protection investigation; pregnancy; treatment by CAMHS specialist; residence in short-term foster care; learning disabilities; involvement in another study in past 6 months; sibling participation in other CAMHS family therapy trial; youth not proficient in English |
NR | SI (BSS); DSH (SASII) |
T: Self-Harm Intervention Family Therapy (SHIFT); Dose: 6–8, 1.25-hour sessions over 6 months C: TAU; Dose: Varied Assessments: Pre-treatment (BL), F/U at 3, 6, 12, and 18 months |
Treatment completion (≥ 1 session): T: 94.9% C: 81.3% Attrition: 3-month F/U: T: 45.1% C: 52.5% 6-month F/U: T: 50.8% C: 64.3% 12-month F/U: T: 40.2% C: 54.7% 18-month F/U: T: 50.8% C: 60.4% Withdrew over F/U: T: 26% C: 46.5% |
Significantly greater decrease in SI for T as compared to C at 12-month F/U. NS between group differences in SI at 18-month F/U. NS between group differences in hospitalizations for DSH at 12- or 18-month F/U. |
| Family Therapy | Harrington et al. (1998)1 | 162; T=85, C=77 |
10–16 years old; 90% female; race/ethnicity NR | Inpatient | In: DSP Ex: DSH (other than DSP); inability to engage in family intervention; psychiatrist decided participation was contraindicated (e.g., psychosis); cases where unclear if overdose was deliberate |
MDD (67%); CD (10%) |
SI (SIQ) |
T: Family-based problem solving (youth and at least 1 parent present at all sessions), TAU; Dose: 5 home sessions C: TAU; Dose: Varied Assessments: Pre-treatment (BL), F/U at 2 and 6 months |
Treatment completion (≥ 1 session): T: 74% C: NR Attrition (Total sample): 2-month F/U: 4% 6-month F/U: 8% |
NS between group difference in SI at 2- and 6-month F/U. Significantly greater decrease in SI for T as compared to C at 2- and 6-month F/U in a subsample of non-depressed adolescents. |
| Multiple Systems Therapy | Huey et al. (2004)1 | T and C sample size NR | 10–17 years old; 35% female; 65% African American, 33% Caucasian |
ED, inpatient | In: Hospitalization for SA, SI, or SP; homicidal ideation or behavior; psychosis; threat to harm self or others; Medicaid-funded or w/out health insurance; residing in non-institutional environment Ex: ASD |
NR | DSH or SA (CBCL – caregiver-reported); SA (YRBS – self-reported); SI (BSI and YRBS) |
T: Multisystemic Therapy; Dose: Daily contact if needed for 3–6 months C: Inpatient hospitalization; Dose: Daily behaviorally-based milieu program Assessments: Pre-treatment, 4 months post-recruitment, F/U at 1 year post-treatment |
NR | Reduced SAs from pre- to post-treatment in T as compared to C (YRBS only); NS for SI. |
| Integrated Family Therapy | Asarnow, Hughes, Babeva, & Sugar (2017) | 42; T=20, C=22 |
11–18 years old; 88% female; 83% Caucasian, 21% Hispanic, 12% Asian, 5% African American, 7% other; 22% identified as lesbian, gay, or bisexual | ED, inpatient, partial hospitalization, outpatient | In: NSSI as primary problem (with ≥3 lifetime DSH episodes) or SA in past 3 months; stable family situation; parent willing to participate in treatment Ex: Psychosis; substance dependence; youth not fluent in English |
MDD (55%); Problematic substance use (48%) |
SA (C-SSRS); DSH (C-SSRS) |
T: Safe Alternatives for Teens and Youths (SAFETY; youth and parent individual sessions + joint parent-youth sessions; CBT + DBT skills + homework); Dose: 12 weeks C: Enhanced TAU (E-TAU; in-clinic parent session, phone calls ensuring treatment adherence); Dose: In-clinic parent session and >3 telephone calls Assessments: Pre-treatment (BL), F/U at 3 months and between 6 and 12 months |
Treatment completion: T (9–12 sessions): 70% C: 95.5% received in-clinic parent session (M=1.56 F/U calls) Attrition (Youth report): T: 0% C: 45% |
Significantly longer time to first SA for T as compared to C over 3-month F/U. NS between group differences in NSSI or in time to first NSSI event at any F/U time point. |
| Brief Family-Based Therapy | Asarnow et al. (2011)1 | 181; T=89, C=92 |
10–18 years old; 69% female; 45% Hispanic, 33% Caucasian, 13% African American, 9% other |
ED | In: Presented to ED with SA and/or SI Ex: Acute Psychosis; symptoms or other factors that interfered with ability to provide consent; no parent/guardian to provide consent; youth not fluent in English |
UMD (40%) | SA (DISC-IV and HASS); SI (HASS) |
T: Family Intervention for Suicide Prevention; Dose: One family-based CBT session in ED, phone contact 48 hours post-discharge and several other times over 1 month C: Enhanced ED TAU; Dose: ED usual care, specialized staff training Assessments: Pre-treatment, F/U at 2 months |
Treatment completion: 100% Attrition: 2-month F/U: T: 15% C: 9% |
NS differences between groups for all SITB outcomes. |
| Brief Family-Based Therapy | Ougrin et al. (2011; 2013)1 | 69; T=35, C=34 Originally randomized 70 (35 in each group) but analysis done with 69 |
12–18 years old; 80% female; 53% Caucasian, 20% African American, 11% Asian | Mental health services | In: Recent DSH or DSP but not currently receiving psychiatric services Ex: Gross reality distortion; history of at least moderately severe intellectual disability; imminent violence or suicide risk; need for inpatient psychiatric admission; youth not fluent in English |
EMD (60%); DBD (13%) |
DSH (accident and ED reports and patient health records) | T: Therapeutic Assessment; Dose: 1-hour Psychosocial history and risk assessment (“Assessment as Usual” per NICE guidelines), 30-minute session using cognitive analytic therapy paradigm with family C: Assessment as Usual; Dose: 1-hour Psychosocial history and risk assessment Assessments: Data on SITB outcomes were collected 2 years post-intervention via electronic hospital, primary care, and patient health records |
Treatment completion: 100% Attrition: F/U: T: 6% C: 9% |
NS between groups for all DSH outcomes. |
| Parent Training | Pineda & Dadds (2013)1 | 48; T=24, C=24 |
12–17 years old; T: 73% female; C: 78% female; T: 64% Caucasian, 27% mixed race; C: 50% Caucasian, 44% mixed race | ED | In: Residing with at least one parent; ≥1 SITBs in past two months; primary diagnosis of MDD, PTSD, or ANX Ex: PDD; psychosis; poisoning from recreational drugs |
MDD (100%); At least 2 psychiatric diagnoses (38%) |
SITB (ASQ-R) | T: Resourceful Adolescent Parent Program (RAP-P); Dose: Four 2-hour sessions weekly or biweekly, crisis management and safety planning, parents invited to all programs C: TAU; Dose: Varied outpatient treatment, family intervention limited to crisis management and safety planning only Assessments: Pre- and post-treatment, F/U at 6 months |
Treatment completion (all four sessions): 100% Attrition: 6-month F/U: T: 8.3% C: 25% |
Reduced SITBs in T as compared to C from pre- to post-treatment; reductions maintained at 6-month F/U. |
| Support-Based Therapy | King et al. (2006)1 | 289; T=151, C=138 |
12–17 years old; 68% female; 82% Caucasian, 10% African American, 7% other | Inpatient | In: Recent psychiatric hospitalization; past month SA or SI; CAFAS self-harm subscale = 20 or 30 Ex: Psychosis; severe mental disability |
NR | SI (SIQ-Jr, SSBS); SA (SSBS) |
T: Youth-nominated Support Team-I + TAU (varied); Dose: Psychoeducation for supports, weekly contact between supports and adolescents, supports contacted by intervention specialists over 6 months C: TAU (varied); Dose: 6 months Assessments: Pre-treatment (BL), post-treatment (6 months) |
Treatment completion: T: 76% C: 87% Attrition: T: 25.1% C: 10.9% |
NS between group differences in SI and the proportion of participants reporting ≥ 1 SA at post-treatment. Significantly greater decrease in SI for T as compared to C at post-treatment in a subsample of female adolescents. |
| Support-Based Therapy | King et al. (2009)1 | 448; T=223, C=225 |
13–17 years old; 71% female; 84% Caucasian, 6% African American, 2% Hispanic, 8% other | Inpatient | In: Recent psychiatric hospitalization; past month SA or frequent (“many times”) SI Ex: Severe cognitive impairment; psychosis; medical instability; residential placement; no legal guardian available |
UMD (88%); DBD (42%); ANX (29%); PTSD or acute stress disorder (25%); AUD or SUD (21%) |
SI (SIQ-Jr); SA (DISC-IV) |
T: Youth-nominated Support Team-II, TAU (varied); Dose: Psychoeducation for supports, weekly contact between supports and adolescents for 3 months C: TAU (varied); Dose: 3 months Assessments: Pre-treatment (BL), mid-treatment (6 weeks), post-treatment (3 months), F/U at 6 and 12 months |
Treatment completion (≥ 2 support people for 12 weeks): T: 74% Attrition: Post-treatment: T: 23.7% C: 21.8% 12-month F/U: T: 19.3% C: 21.8% |
Significantly greater decrease in SI for T as compared to C at mid-treatment. NS between group differences in SI at post-treatment and over 12-month F/U. NS between group differences in frequency of SA or SA rate over 12-month F/U. |
| Eclectic Group Therapy | Green et al. (2011)1 | 366; T=183, C=183 |
12–17 years old; 89% female; 94% Caucasian | Mental health service | In: ≥2 DSH episodes in past year Ex: Severe AN; active psychosis; current confinement in secure care; attendance at special learning disability school; youth not fluent in English |
UMD (62%); DBD (33%) |
DSH (interview validated in Harrington et al., 1998); SI (SIQ) |
T: DGT (see Wood et al., 2001), TAU; Dose: (see Wood et al.) C: TAU, no group therapy permitted during trial; Dose: Varied Assessments: Pre-treatment (BL), F/U at 6 and 12 months |
Treatment completion (≥ 5 sessions): T: 79% C: 63% Attrition: T: 1.6% C: 2.3% |
NS between group differences in frequency of DSH, severity of DSH, or SI at 6- and 12-month F/U. |
| Eclectic Group Therapy | Hazell et al. (2009)1 | 72; T=35, C=37 |
12–16 years old; 90% female; race/ethnicity NR | Mental health service | In: ≥2 DSH episodes in past year + at least 1 DSH episode in past 3 months Ex: More intensive treatment required; active psychosis; inability to attend groups; intellectual disability |
MDD (57%); DBD (7%); Alcohol problems (4%) |
DSH (PHI); SI (SIQ) |
T: DGT (see Wood et al.) + TAU; Dose: 1 hour/week for 6 sessions for up to 1 year (see Wood et al.) C: TAU (individual or family sessions); Dose: Varied Assessments: Pre-treatment (BL), F/U at 2, 6, and 12 months |
Treatment completion (≥ 4 sessions): T: 71.4% C: 62.2% Attrition: T: 2.8% C: 8.1% |
Significantly more participants in T reported DSH behavior as compared to C at 6-month F/U. NS between group difference in the proportion of participants reporting DSH behavior between 6- and 12-month F/U. NS between group differences in the proportion of participants engaging in >1 DSH episode between BL and 6-month F/U or between 6- and 12-month F/U. NS between group difference in SI over 12-month F/U. |
| Eclectic Group Therapy | Rudd et al. (1996)1 | 264; T=143, C=121 |
15–24 years old; 18% female; 61% Caucasian, 26% African American, 11% Hispanic | Mental health service | In: Previous SA; UMD + SI; AUD + SI Ex: SUD or chronic abuse; psychosis or thought disorder; severe PD |
MD (72%); AUD (44%); ANX (37%) |
SI (MSSI) | T: Time-limited CBT group therapy (psychoeducation classes, problem-solving group, experiential-affective group, homework), TAU; Dose: 9 hours daily for 2 weeks C: TAU (inpatient, outpatient); Dose: Varied combination of individual and group therapy Assessments: Pre-treatment (BL), post-treatment (1 month), F/U at 6 and 12 months (18- and 24-month F/U data not reported here) |
Treatment completion: T: 79% C: NR Attrition: Post-treatment: T: 16.1% C: 24.8% 6-month F/U: T: 47.6% C: 54.5% 12-month F/U: T: 67.8% C: 79.3% |
NS between group differences in SI at post-treatment and at 6- and 12-month F/U. |
| Eclectic Group Therapy | Wood, Trainor, Rothwell, Moore, & Harrington (2001)1 | 63; T=32, C=31 |
12–16 years old; 78% female; race/ethnicity NR | Mental health service | In: ≥1 DSH episode in past year; referred to mental health services following DSH incident Ex: Severe suicide risk; inability to attend groups; psychosis; significant learning problems |
MDD (83%); DBD (67%) |
DSH (interview-see Kerfoot, 1984); SI (SIQ) |
T: Developmental group psychotherapy (DGT; acute and long-term groups, individual sessions [as needed]), TAU; Dose: 6 acute sessions, weekly long-term group as needed for 6 months C: TAU; Dose: Varied Assessments: Pre-treatment (BL), F/U at 6 weeks and 7 months |
Treatment completion (≥ 4 sessions): T: 71.9% C: 61.3% Attrition: 7-month F/U: T: 3.1% C: 0% |
Significantly greater decrease in DSH episodes for T as compared to C. Significantly longer time to first DSH episode for T as compared to C over 7-month F/U. NS between group differences in SI at post-treatment and at 7-month F/U. |
| Resource Intervention | Cotgrove, Zirinsky, Black, & Weston (1995)1 | 105; T=47, C=58 |
12–16 years old; 85% female; race/ethnicity NR | Inpatient | In: Admitted for DSH, DSP, or SA Ex: NR |
NR | SA (unspecified psychiatrist questionnaire) | T: Green card for re-admission to the hospital C: Clinic or child psychiatry department TAU Assessments: Pre-treatment and F/U at 1 year |
Treatment completion: T: 11% used green card Attrition: Total sample: 0% |
NS between group differences in SA (statistically), but some lower rates of SA in treatment group. |
| Resource Intervention | Morthorst, Krogh, Erlangsen, Alberdi, & Nordentoft (2012) | 243; T=123, C=120 |
≥ 12 years old; 76% female; 68% Danish, 14% Middle Eastern, 8% European and American, 10% other | ED, intensive care, pediatric units | In: Admitted to hospital after SA (within past 14 days); self-injuries included if they met WHO definition of SA Ex: Admitted to psychiatric ward for more than 14 days after attempt; SZ spectrum disorders; severe MDD; severe BP; severe dementia; needed inpatient care; receiving outreach services from social services; living in institutions |
NR | SA (unspecified self-report) | T: Assertive Intervention for Deliberate Self-harm (AID), TAU; Dose: 8–20 outreach consultations over 6 months C: TAU; Dose: Optional 6–8 sessions for those not receiving other care Assessment: Pre-treatment, F/U at 1 year |
Treatment completion: T: 96% C: 100% Attrition: F/U: T: 22.8% C: 38.3% |
NS between rates of subsequent suicide attempts in treatment and control groups. |
| Resource Intervention | Robinson et al. (2012)1 | 164; T=81, C=83 |
15–24 years old; 65% female; race/ethnicity NR | Community | In: Living inside target area; did not meet entry criteria for mental health service; history of DSH or SRB Ex: Known organic cause for DSH/SRB; intellectual disability; youth not fluent in English |
MD (67%); ANX (63%); SUD (25%) |
DSH (SBQ-14, BRFL-Adolescent); SA (SBQ-14, BRFL-Adolescent); SI (BSS) |
T: Post cards promoting well-being and evidence-based skills use, community-based TAU; Dose: Monthly for 12 months C: Community-based TAU; Dose: 12 months Assessments: Pre-treatment, F/U at 12 and 18 months |
Attrition: 12-month F/U: T: 25.9% C: 37.4% 18-month F/U: T: 38.3% C: 55.4% |
Reduced DSH and SI in both groups, but NS between groups. |
| Motivational Interviewing | King et al. (2015) | 49; T=27, C=22 |
14–19 years old; 80% female; 57% African American, 39% Caucasian, 4% American Indian or Alaskan Native, 2% Hispanic, 2% Native Hawaiian/Pacific Islander, 2% other | ED | In: Positive suicide risk screen (SI, recent SA, or depression and substance abuse); presented with non-psychiatric complaint Ex: Level 1 trauma; significant cognitive impairment; psychiatric hospitalization |
NR | SI (SIQ-Jr) | T: Teen Options for Change (TOC); Dose: Crisis card + resources, feedback on screenings, 35–45 minute adapted motivational interview C: Enhanced TAU (crisis card for suicidal emergency support) Assessments: Pre-treatment (BL), F/U at 2 months |
Treatment completion: Total: 85% Attrition: Total: 6% |
NS between-group differences in SI. |
| Brief Skills Training | Kennard et al. (2018) | 66; T=34, C=32 |
12–18 years old; 89% female; 77% Caucasian | Inpatient | In: Presented to psychiatric inpatient unit with recent SP or recent SA Ex: Needed residential treatment; active involvement in child protective services; mania; psychosis; autism; intellectual disability |
MDD (86%); Of those with MDD, 58% had a comorbid ANX |
SI (SIQ-Jr); SA (C-SSRS); NSSI (C-SSRS) |
T: As Safe as Possible (ASAP), TAU; Dose: 3-hour ASAP intervention, BRITE app use C: TAU; Dose: Varied Assessments: Pre-treatment, F/U at 4, 12, and 24 weeks post-discharge |
Treatment completion: Varies based on treatment component Attrition: 4-week F/U: T: 8.8% C: 21.9% 12-week F/U: T: 20.6% C: 28.1% 24-week F/U: T: 17.6% C: 18.8% |
NS for all SITB outcomes. |
BL=baseline assessment; ED=emergency department; F/U=follow-up; NR=not reported; NS=non-significant
Major Diagnoses: ADHD=attention-deficit/hyperactivity disorder; AN=anorexia nervosa; ANX=anxiety disorder–type not specified; ASD=autism spectrum disorder; AUD=alcohol use disorder; BP=bipolar disorder; BPD=borderline personality disorder; CD=conduct disorder; CUD=cannabis use disorder; DBD=disruptive behavior disorder; ED=eating disorder; EMD=emotional disorder; MD=mood disorder (bipolar or unipolar); MDD=major depressive disorder; PD=personality disorder; PDD=pervasive developmental disorder; PTSD=post-traumatic stress disorder; SCAD=schizoaffective disorder; SUD=substance use disorder; SZ=schizophrenia; UMD=unipolar mood disorder
Measures: ASQ-R=Adolescent Suicide Questionnaire Revised; BAI=Beck Anxiety Inventory; BDI=Beck Depression Inventory; BHS=Beck Hopelessness Scale; BRFL=Brief Reasons for Living Inventory; BSI=Brief Symptom Inventory; BSS=Beck Scale for Suicide Ideation; CAFAS=Child and Adolescent Functional Assessment Scale; CBCL=Children Behavior Checklist; C-SSRS=Columbia Suicide Severity Rating Scale; DISC-IV=Diagnostic Interview Schedule for Children Version IV; HASS=Harkavy-Asnis Suicide Scale; K-SADS-PL=Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime Version; LPC=Lifetime Parasuicide Count; MSSI=Modified Scale for Suicide Ideation; PHI=Parasuicide History Interview; RTSHI=Risk Taking and Self Harm Inventory; SASII=Suicide Attempt Self-Injury Interview; SBQ-14=Suicide Behavior Questionnaire; SIQ (Jr or Sn)=Suicide Ideation Questionnaire; SSBS=Spectrum of Suicide Behavior Scale; SSI=Scale for Suicidal Ideation; YRBS=Youth Risk Behavior Survey
Self-Injurious Outcomes: DSH=deliberate self-harm; DSP=deliberate self-poisoning; NSSI=nonsuicidal self-injury; SA=suicide attempt; SI=suicide ideation; SITB=self-injurious thought or behavior (suicidal and nonsuicidal); SP=suicide planning or preparation; SRB=suicide-related behavior (suicide thoughts, plans, attempts)
Treatments and Conditions: C=control or comparison group; CBT=Cognitive-Behavioral Therapy; DBT-A=Dialectical Behavior Therapy for adolescents; EUC=Enhanced Usual Care; IPT-A=interpersonal psychotherapy for adolescents; MI=Motivational Interviewing; T=experimental treatment group; TAU=treatment as usual
Trial was included in the prior JCCAP Evidence Base Update (Glenn et al., 2015).
Table 3.
Efficacy of Psychosocial Treatments for Self-Injurious Thoughts and Behaviors in Youth: Summary1
| Level 1: Well-Established |
Level 2: Probably Efficacious |
Level 3: Possibly Efficacious |
Level 4: Experimental |
Level 5: Questionable Efficacy |
|---|---|---|---|---|
|
DBT-A (DSH, SI) McCauley et al. (2018) Mehlum et al. (2014) |
DBT-A (NSSI, SA) McCauley et al. (2018) CBT–Individual + Family (SA) Esposito-Smythers et al. (2011) Integrated Family Therapy (SA) Asarnow et al. (2017) IPT-A–Individual (SI) Tang et al. (2009) Psychodynamic Therapy–Individual + Family (DSH) Rossouw & Fonagy (2012) Parent Training (SITB) Pineda & Dadds (2013) |
Multiple Systems Therapy (SA) Huey et al. (2004) |
CBT–Individual (SA, SI) Hetrick et al. (2017) CBT–Individual + Family (SI) Esposito-Smythers et al. (2011) Psychodynamic Therapy–Family-Based Diamond et al. (2010) (SI) Diamond et al. (2018) (SA, SI) Integrated Family Therapy (NSSI) Asarnow et al. (2017) Family Therapy Harrington et al. (1998) (SI) Cottrell et al. (2018) (DSH, SI) Multiple Systems Therapy (SI) Huey et al. (2004) Brief Family-Based therapy Asarnow et al. (2011) (SA, SI) Ougrin et al. (2013) (DSH) Support-Based Therapy (SI) King et al. (2006) King et al. (2009) Brief Skills Training (NSSI, SA, SI) Kennard et al. (2018) Motivational Interviewing (SI) King et al. (2015) Resource Interventions (DSH, SI) Robinson et al. (2012) |
Eclectic Group Therapy Green et al. (2011) (DSH, SI) Hazell et al. (2009) (DSH, SI) Rudd et al. (1996) (SI) Wood et al. (2001) (DSH, SI) Support-Based therapy (SA) King et al. (2006) King et al. (2009) Resource Intervention (SA) Cotgrove et al. (1995) Morthorst et al. (2012) Robinson et al. (2012) |
Treatments: CBT=Cognitive-Behavioral Therapy; DBT-A=Dialectical Behavior Therapy for adolescents; IPT-A=interpersonal psychotherapy for adolescents
Self-Injurious Outcomes: DSH=deliberate self-harm; NSSI=nonsuicidal self-injury; SA=suicide attempt; SI=suicide ideation; SITB=self-injurious thought or behavior (suicidal and nonsuicidal)
For each treatment family, the SITB outcomes examined in the relevant trials are listed in parentheses. In cases where efficacy ratings for a specific SITB outcome were based on a subset of articles in a broader treatment family, the SITB outcomes are listed separately for each contributing trial. For some treatments, there are different efficacy ratings based on the SITB outcome. In these cases, a treatment family may appear twice in the summary table illustrating a different level of evidence for a specific SITB outcome (e.g., DBT-A Level 1 for DSH and SI; Level 2 for NSSI and SA).
Five considerations should be kept in mind when evaluating the treatment literature. First, broad classification of interventions based on treatment type and mode were complicated in a number of ways. Most notably, categorization based on the role of the adolescent’s family was challenging as most interventions designed for youth include at least a small family component, even if primarily designed as an individual treatment package. Consistent with decisions made in the prior review (Glenn et al., 2015) and other Evidence Base Updates (e.g., Freeman et al., 2014), we classified interventions in the following ways: (1) interventions in which the adolescent was the main target of treatment, and family sessions were optional or included as needed, were classified as individual interventions (e.g., Cognitive-behavioral therapy—Individual; Hetrick et al., 2017), (2) interventions in which individual therapy was augmented with a family component were classified as individual + family treatments (e.g., Cognitive-behavioral therapy—Individual + Family; Esposito-Smythers, Spirito, Kahler, Hunt, & Monti, 2011), and (3) interventions in which the family was the primary focus of the intervention were classified as family-based therapy (e.g., Psychodynamic therapy—Family-based; Diamond et al., 2010; 2018).
Second, although every effort was made to combine similar interventions when possible, few RCTs have examined the same intervention for SITBs in youth. Therefore, many broad treatment categories only contain a single trial.
Third, interventions included in this review targeted a range of SITBs from nonsuicidal (NSSI) to suicidal outcomes (SI, SA). The specific SITB outcomes are specified for each trial in Table 2 and treatment efficacy is evaluated with respect to each of these outcomes. This means that in some cases an intervention may have greater efficacy for reducing one SITB outcome but not a separate SITB outcome (e.g., significant reduction in SI but no significant reduction in SA).
Fourth, it is not uncommon in intervention research for both treatment groups (experimental and control/comparison groups) to exhibit a reduction in symptoms over time (e.g., regression to the mean; Morton & Torgerson, 2005). Given that our review included only RCTs, we were able to focus our evaluation on between-group differences and specifically whether the experimental treatment led to significant reductions in SITBs compared to the control/comparison treatment.
Fifth, and finally, treatment attrition is a significant concern in intervention research with youth (Kazdin, 1996), and becomes even more problematic when dropout rates differ between experimental and control groups (Chambless & Hollon, 1998). In Table 2, we provide details regarding treatment completion and study attrition when reported. Moreover, in our discussion of each trial, we examine the dropout rates for each intervention and report intention-to-treat (ITT) analyses when available. ITT analyses evaluate treatment outcomes for all youth randomized to a specific intervention group, which provides a more conservative test of a treatment’s efficacy (Chambless & Hollon, 1998).
Dialectical behavior therapy for adolescents (DBT-A)
DBT was one of the first treatments designed specifically to target SITBs (Linehan, 1993). This intervention was originally developed to treat adults with borderline personality disorder (BPD), but has since been adapted for other demographic and diagnostic groups including suicidal adolescents (DBT-A) with or without BPD (Miller, Rathus, Linehan, Wetzler, & Leigh, 1997; Rathus & Miller, 2014). The full DBT-A treatment package includes weekly individual therapy, weekly multifamily group skills training (i.e., mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness skills), telephone coaching with the therapist when needed, and weekly consultation among the treatment team. DBT aims to reduce the emotional, interpersonal, and behavioral dysregulation that leads to maladaptive behaviors, such as SITBs, and has demonstrated good efficacy in adults for reducing these outcomes (Kliem, Kröger, & Kosfelder, 2010; Linehan et al., 2006; Linehan, Heard, & Armstrong, 1993).
There have been significant changes in the evaluation of this intervention for youth since the prior review. At the time of the 2015 review, no RCTs had tested the efficacy of DBT-A in youth. Therefore, the prior review evaluated DBT-A based on four pilot studies (one was a DBT skills only group) and two non-randomized trials. Based on the evidence at that time, DBT-A was evaluated as Level 4: Experimental for reducing DSH, NSSI, and SI in youth. Since the prior review, two RCTs, conducted by two independent research groups have examined a form of DBT-A for reducing SITBs in youth. Details of these trials are provided below.
In the first RCT (Mehlum et al., 2014), a shortened form of DBT-A (19 weeks vs. typical six-month package) was compared to enhanced usual care (EUC; weekly therapy ranging from psychodynamic to cognitive-behavioral therapy, plus medication as needed) among 77 adolescents with a history of repetitive DSH and BPD features who were receiving outpatient care. Over the course of treatment, the DBT-A group reported reductions in DSH that were significantly greater than those observed in the EUC group (ITT analyses). In addition, the DBT-A group also had significantly greater reduction in SI over the course of treatment, most notably at the end of the treatment period (19 weeks). Importantly, treatment effects for DSH held over a 52-week follow-up; the DBT-A group reported a significantly lower frequency of DSH over follow-up compared to the EUC group (Mehlum et al., 2016). However, between-groups differences in SI were not maintained over this follow-up period; DBT-A maintained reductions in SI but EUC also led to significantly reduced SI over the 52-week follow-up (Mehlum et al., 2016).
It is important to note a few limitations of the comparison treatment for this study. EUC required weekly individual treatment but not a group skills component, unlike the DBT-A group. Therefore, the DBT-A received a higher dose of treatment than the control group given the inclusion of a multifamily group skills component in the treatment package. In addition, EUC was not a manualized treatment nor was it monitored for fidelity, which means that control participants likely did not receive the same type or dose of treatment. Some of these limitations were addressed in a recent and independent DBT-A trial.
A second RCT compared DBT-A (six-month package) to individual and group supportive therapy (IGST, also six months) in a large (N=173) sample of adolescents with a history of suicide attempts recruited across four medical centers (McCauley et al., 2018). IGST is a manualized intervention that aims to match the dose of treatment provided in DBT-A, addressing the limitations of the control intervention used in the Mehlum et al. (2014) trial. Specifically, IGST provides individual supportive therapy (focused on validation, acceptance, and connectedness), supportive group therapy, parent sessions as needed, and therapist team consultation. Gains for DBT-A were observed across all SITB outcomes compared to the control condition from pre- to post-treatment (ITT analyses): the DBT-A group reported significantly fewer instances of DSH, NSSI, and SA and significantly greater reductions in SI from baseline to 6 months compared to the IGST group—all effects were small to moderate in size. However, these between-groups differences were not significant at the final 12-month follow-up because adolescents in both treatment conditions improved over time. Although IGST was a conservative control for DBT-A (i.e., manualized and matched in treatment length and modality), youth receiving DBT-A were more likely to participate in treatment and remained in treatment longer than in IGST. Differences in treatment engagement and retention are important to consider when evaluating intervention effects. For instance, greater treatment engagement may suggest that an intervention has more promise for being “scaled up” or easily disseminated outside of an RCT (Becker, Boustani, Gellatly, & Chorpita, 2018). Notably, a recent pilot study found initial evidence for the effectiveness of DBT-A for reducing SITBs among youth in a community clinic (Berk, Starace, Black, & Avina, 2018).
Based on these two high-quality RCTs conducted by two independent research groups, DBT is evaluated as a Level 1: Well-established intervention for reducing DSH and SI in youth (the two SITBs that were examined across both trials). NSSI and SA were examined separately in the second RCT only and therefore DBT is evaluated as a Level 2: Probably efficacious intervention for reducing NSSI and SA in youth.
Cognitive-behavioral therapy (CBT)
CBT is a short-term, problem-oriented treatment approach that aims to modify distorted cognitions and maladaptive behaviors to improve aversive emotional states. To reduce SITBs, CBT approaches focus on restructuring maladaptive thinking patterns and enhancing emotion regulation, problem-solving, and communication skills to increase adaptive coping. Some trials included in the CBT section have changed since the prior review. Given our emphasis on RCTs, we have removed discussion of the pilots and non-randomized trials from the prior review. In addition, we excluded trials with small sample sizes (< 20 adolescents per group; Hsu, 2016), which removed a number of smaller CBT trials (Alavi, Sharifi, Ghanizadeh, & Dehbozorgi, 2013; Donaldson, Spirito, & Esposito-Smythers, 2005; Högberg & Hällström, 2018; Spirito et al., 2015) from the current review. However, we discuss these trials briefly when applicable as potentially promising interventions to be explored in future research.
Based on the more stringent inclusion criteria for this review, two RCTs examining a form of CBT for reducing SITBs in youth met inclusion criteria. One trial examining CBT—Individual is new to this review and the second trial examining CBT—Individual + Family was included in the prior review.
CBT—Individual.
Since the prior review, a new RCT (Hetrick et al., 2017) has examined an internet-based CBT package for suicidal youth called Reframe-IT. Reframe-IT is a 10-week CBT package with a specific focus on SITBs. Modules delivered over the internet include behavioral activation, cognitive restructuring, distress tolerance, and problem-solving skills (Robinson et al., 2014). Students with SI were recruited from schools in Melbourne, Australia and were randomly assigned to either Reframe-IT plus treatment-as-usual (TAU) or TAU only (i.e., school staff support, additional mental health support, and medication if needed). In pilot trials, Reframe-IT was determined to be safe and acceptable (Robinson et al., 2015) and significantly reduced SI in youth (Robinson et al., 2016). Although the Reframe-IT group reported larger reductions in SI over the course of treatment, the differences between treatment groups were not statistically significant post-treatment or at 22-week follow-up (ITT analyses). In addition, although fewer adolescents in the experimental treatment group attempted suicide compared to the control group, differences were not statistically significant post-treatment or at 22-week follow-up.
A few limitations of this trial are important to note when interpreting the findings. First, the trial was underpowered. The targeted sample size was 169 adolescents, but only 50 were randomized with 30 completing the 22-week follow-up, which significantly reduced power to detect effects. This is important to note given that all findings were in the expected direction. Second, TAU, received by both treatment groups, could have included a range of psychotherapies and/or medication. Unrestricted TAU may have made it difficult to detect meaningful effects of the new intervention. Moreover, given the small sample size, differences in TAU across groups could not be controlled.
Although different trials were used to evaluate the efficacy of this intervention type between the 2015 review and current review, CBT—Individual remains classified as Level 4: Experimental for reducing SA and SI in youth.
One additional trial did not meet inclusion criteria for our review based on the small sample size, but is worth mentioning given that it also examined a CBT—Individual treatment. In a small (N=32; 12–15 per group) RCT with depressed youth in outpatient care, mood regulation focused CBT (MR-CBT) was compared to TAU (standard practice in psychiatry; Högberg, &Hällström, 2018). MR-CBT is a treatment based on memory reconsolidation that aims to increase positive and decrease negative emotions related to autobiographical memories. The MR-CBT group reported significantly fewer suicide events (active suicide ideation with any method and/or suicide attempts) over the course of treatment but this change was not significantly different than the TAU group. This trial was underpowered and therefore further testing of this intervention is needed before rating its efficacy.
CBT—Individual + Family.
The evaluation of this intervention type and mode has not changed since the prior review (of note, it was previously labeled “CBT-Individual + CBT-Family + Parent Training” due to the addition of parent training compared to earlier iterations of the treatment package; Donaldson, Spirito, & Esposito-Smythers, 2005; Esposito-Smythers, Spirito, Uth, & LaChance, 2006). In a small (N=40) RCT, Esposito-Smythers et al. (2011) compared integrated CBT (I-CBT), combining individual CBT (e.g., refusal skills), family CBT (e.g., communication), and parent training (e.g., emotion regulation), to enhanced TAU (E-TAU; community TAU enhanced with a diagnostic report shared with the TAU provider, medication management, and additional clinical referrals as needed). Compared to E-TAU, significantly fewer youth receiving I-CBT reported SAs over the 18-month follow-up period (ITT analyses). Both treatment groups reported decreased SI over the course of treatment, but reductions were not significantly greater in the I-CBT group. Therefore, CBT–Individual + Family remains classified as Level 2: Probably efficacious for reducing SAs in youth and Level 4: Experimental for reducing SI in youth.
Two other trials did not meet inclusion criteria for our review due to sample sizes, but are worth discussing as potentially promising CBT interventions for adolescents and families. The first trial tested Parent-Adolescent CBT (PA-CBT), which provides concurrent CBT for depressed adolescents and their parents (Spirito et al., 2015). In a small trial (N=24 adolescent-parent dyads), PA-CBT was compared to adolescent only CBT. PA-CBT was feasible and acceptable for most families with the largest treatment effect on parents’ depression. Adolescents in both groups exhibited significant reductions in SI over the course of treatment, but effects were not significantly greater for the PA-CBT group. Replication in a larger trial is needed to test the efficacy of this new intervention for suicidal youth and families.
A second, small (N=30, 15 per group) clinical trial compared CBT for suicide prevention (CBT-SP; Stanley et al., 2009) to a waitlist control among adolescents who had attempted suicide in the past three months (Alavi et al., 2013). CBT-SP is a 12-session treatment package delivered in three phases: (1) psychoeducation, chain analysis, safety planning, reasons for living, and case conceptualization, (2) a menu of optional CBT modules to enhance individual skills training (e.g., behavioral activation, emotion regulation, distress tolerance, cognitive restructuring, and problem-solving) and family skills (e.g., family communication, family emotion regulation, and family problem solving), and (3) relapse prevention. From pre- to post-treatment, youth receiving CBT-SP reported significant reductions in SI compared to the waitlist control group. Although promising, replication of this intervention in a larger trial with an active control group is needed.
Interpersonal psychotherapy for adolescents (IPT-A)
IPT-A—Individual.
There have been no changes in the status of IPT-A since the prior review. Only one trial has examined individual IPT-A for adolescents (IPT-A) at risk for SITBs (Tang, Jou, Ko, Huang, & Yen, 2009). IPT-A focuses on enhancing interpersonal functioning and resolving interpersonal problems with an emphasis on youth-specific difficulties (e.g., peer pressure; Mufson, Moreau, Weissman, & Klerman, 1993). Tang et al. (2009) found that school-based IPT-A significantly reduced SI over the course of treatment compared to TAU (i.e., psychoeducation and supportive counseling). Based on this trial, IPT-A remains classified as Level 2: Probably efficacious for reducing SI in youth.
Psychodynamic therapy
Psychodynamic therapy—Individual + Family.
The efficacy rating of this mode of psychodynamic therapy has not changed since the prior review. Only one trial has examined a psychodynamic intervention including individual and family components for reducing DSH in adolescents – Mentalization-Based Treatment for Adolescents (MBT-A: Rossouw & Fonagy, 2012). MBT-A aims to reduce DSH by improving mentalization, or the ability to understand the connection between behaviors, thoughts, and feeling among themselves and others. Compared to community-based TAU, MBT-A significantly reduced DSH in adolescents and did so at a significantly faster rate during treatment (ITT analyses). Given that Psychodynamic therapy—Individual + Family was tested in an RCT and found to be superior to an active treatment control, it remains classified as Level 2: Probably efficacious for reducing DSH in youth.
Psychodynamic therapy—Family-based.
Two RCTs conducted by the same research group have examined the same Family-based psychodynamic therapy (previously called “FBT-Attachment”), “brand name” Attachment-Based Family Therapy (ABFT: Diamond, Reis, Diamond, Siqueland, & Isaacs, 2002). ABFT aims to reduce SITBs by enhancing parent-adolescent relationships through process-oriented, cognitive-behavioral, and emotion-focused techniques. One RCT (Diamond et al., 2010) was included in the prior review and the second RCT is new to this review (Diamond et al., 2018). In the first RCT, Diamond et al. (2010) found that youth receiving ABFT reported significantly greater reductions in SI compared to enhanced TAU (referrals and clinical monitoring) over the course of treatment and effects were maintained 12 weeks post-treatment (ITT analyses). SA rates were too small to examine between treatment groups.
However, findings from a second, larger RCT compared ABFT to a more active comparison treatment were not as promising. In this second RCT, Diamond et al. (2018) compared ABFT to family-enhanced nondirective supportive therapy (FE-NST). FE-NST focuses on developing a supportive adolescent-therapist relationship and parent education. The intervention includes individual sessions with the adolescent, individual sessions with the parent, and one joint parent-youth session. Compared to the enhanced TAU control included in the initial trial (Diamond et al., 2010), FE-NST was a more conservative comparison intervention because it is manualized and matches ABFT in treatment dose while targeting different content. Over the course of treatment, both groups reported significant reductions in SI, but this decrease was not significantly greater in the ABFT group (ITT analyses). There were no significant differences between groups in SA rates.
This intervention was previously evaluated as Level 2: Probably efficacious for SI in youth based on the first RCT (Diamond et al., 2010). However, taken together with the null findings from the second RCT (Diamond et al., 2018), Psychodynamic therapy—Family-based is now evaluated as Level 4: Experimental for reducing SA and SI in youth.
Family therapy
Two trials, one reviewed previously (Harrington et al., 1998) and one new to this review (Cottrell et al., 2018), tested a family-focused treatment program that targeted family functioning as a means to decrease SITBs. Therefore, we combined these two trials into one treatment family—Family Therapy. However, specific differences between the intervention packages are also described.
Harrington et al. (1998), reviewed previously, compared a brief (5-session), home-based family intervention (Kerfoot, Harrington, & Dyer, 1995) plus usual outpatient care to outpatient care alone in a large (N=162) RCT with adolescents who recently engaged in deliberate self-poisoning. The intervention focused on family problem-solving, family communication, and addressing family problems that contributed to adolescents’ DSH. The experimental intervention was not superior to TAU for reducing SI (ITT analyses).
The second RCT is new to this review. Among adolescents referred to mental health services for repetitive self-harm, Cottrell et al. (2018) compared Family Therapy (FT) for self-harm to community TAU in the largest (N=832) multi-site RCT included in this review (Self-Harm Intervention: Family Therapy: SHIFT; Wright-Hughes et al., 2015). To reduce adolescents’ DSH, FT included approximately eight 75-minute sessions over six months to enhance family strengths and resources (Wright-Hughes et al., 2015). FT was not significantly more effective than TAU for reducing DSH in youth during treatment or over the 18-month follow-up (ITT analyses). However, FT did reduce SI significantly more than TAU at the 12-month follow-up, but treatment effects did not hold at the 18-month follow-up. Limitations of this trial that may have contributed to the null findings include the relatively low dose of treatment (on average, treatment was monthly for six months), unrestricted TAU that could have included CBT or general (non-manualized) family therapy, and substantial attrition (50–60%) over the long (18-month) follow-up.
Taken together, the efficacy of Family Therapy for reducing SI is mixed across two studies and nonsignificant for DSH in one study (Cottrell et al., 2018). Therefore, the evaluation of Family Therapy is Level 4: Experimental for reducing DSH and SI in youth.
Multiple systems therapy
There have been no changes in the efficacy of Multiple Systems Therapy since the prior review (referred in the prior review as Family-based therapy—Ecological). Only one trial has examined multisystemic therapy (MST) for reducing SAs in youth (Huey et al., 2004). MST is an intensive home-based intervention to reduce problem behaviors among youth by targeting the multiple systems (e.g., peers, family, school, community) that contribute to these behaviors (Henggeler, Schoenwald, Borduin, Rowland, & Cunningham, 2009). Huey et al. (2004) found that adolescents receiving MST reported fewer SAs over the course of treatment compared to a hospitalization control. A range of limitations were noted in the 2015 review (e.g., inclusion criteria based on self- or other-directed violence risk, a significant portion of MST group was also hospitalized) that led to Multiple Systems Therapy remaining classified as Level 3: Possibly efficacious for reducing SAs in youth and Level 4: Experimental for reducing SI in youth.
Integrated family therapy
New to this review, Asarnow et al. (2017) tested a novel family-centered treatment informed by CBT, DBT, and family therapy approaches, as well as social-ecological theory (Asarnow, Berk, Hughes, & Anderson, 2015). Given that this treatment package integrated multiple approaches into a family-based intervention, it did not seem appropriate to combine it with DBT, CBT, or family therapy. Therefore, a new category was created for this intervention: Integrated Family Therapy.
In a small RCT (N=42), Asarnow et al. (2017) compared their novel treatment program, Safe Alternatives for Teens and Youth (SAFETY; Asarnow, Berk, Hughes, & Anderson, 2015), to TAU enhanced with parent psychoeducation and telephone calls to increase motivation for follow-up care (E-TAU). Adolescents were recruited from mental health services across the continuum of care (emergency department, inpatient, partial hospitalization, or outpatient services) if they had attempted suicide in the past three months, or NSSI was identified as a primary problem, and they had engaged in repetitive DSH (3+ lifetime episodes). The SAFETY treatment program is a 12-week, family-centered intervention administered by two therapists—one for the adolescent and one for the parent/guardian. A variety of techniques are used to tailor the intervention for each family including a functional, or chain, analysis to identify antecedents or triggers of the index SA or DSH. In addition, a strong emphasis is placed on addressing practical barriers to care. The first session is conducted in the home and treatment for the family includes motivational enhancement and reducing barriers to care. The treatment program includes a range of skills and techniques to foster SAFE: (1) settings (e.g., means restriction), (2) people (e.g., enhancing social support), (3) activities (e.g., behavioral activation), (4) thoughts (e.g., cognitive restructuring), and (5) stress reactions (e.g., distress tolerance; Asarnow et al., 2015).
Results indicated that the SAFETY treatment program significantly reduced risk for SA compared to E-TAU (ITT analyses). Specifically, there was significantly longer time to SA for adolescents in the SAFETY group as compared to E-TAU over the 3-month follow-up period. Moreover, there were no SAs among adolescents in the SAFETY group over the 3-month intervention period. However, the intervention effect (i.e., between-group difference) weakened after the treatment ended. In addition, the SAFETY intervention did not have a significant effect on NSSI, which was frequent across both treatment groups.
Although promising, some limitations of this first RCT testing SAFETY are worth noting. First, the sample size was small (ns=20–22 per group), and just met the cutoff for inclusion in this review. Further replication in larger trials is needed. In addition, replication by an independent research group is needed to evaluate the intervention as Level 1: Well-established for reducing SA in youth. Second, like many trials in this review, the E-TAU control was not an ideal comparison intervention due to high attrition (45% of youth post-treatment assessments were unavailable). Although this tempers conclusions about the superiority of SAFETY to active intervention, the main analyses did take censoring into account and were significant even with the most conservative assumption about adolescents with unavailable data.
Based on the promising findings from this single RCT, Integrated Family Therapy is evaluated as Level 2: Probably efficacious for reducing SA in youth and Level 4: Experimental for reducing NSSI in youth.
Brief family-based therapy
There has been no change in the efficacy of Brief Family-Based Therapy (previously referred to as “FBT-Emergency interventions” to highlight the family focus and acute administration in the emergency department [ED]). Two trials, reviewed previously, have examined brief family-based interventions in the ED (Asarnow et al., 2011; Ougrin et al., 2011).
In a large RCT (N=181) among youth presenting to the ED with SA or SI, Asarnow et al. (2011) compared ED TAU to a Family Intervention for Suicide Prevention (FISP), which included a family-based CBT session (psychoeducation, enhancing family support, safety planning) and telephone contact over the next month to increase follow-up with treatment. The intervention increased compliance with treatment but did not significantly reduce SA or SI compared to TAU in the ED (ITT analyses).
A separate RCT in adolescents with recent DSH (N=70) compared a family-based intervention in the ED (including motivational enhancement and cognitive analytic therapy assessment of youth’s DSH) to assessment as usual (Ougrin, Boege, Stahl, Banarsee, & Taylor, 2013; Ougrin et al., 2011). Although the brief ED intervention increased treatment compliance, it did not significantly reduce DSH over the two-year follow-up (ITT analyses).
Brief family-based therapies remain classified as Level 4: Experimental for reducing DSH, SA, and SI in youth.
Parent training
There have been no changes to the evaluation of Parent Training only interventions since the prior review. Only one RCT (Pineda & Dadds, 2013) has examined a family intervention that focuses specifically on parent training with little adolescent involvement in the intervention. Resourceful Adolescent Parent Program (RAP-P) is a brief (4-session) treatment package including family psychoeducation about SITBs, parent training, and strategies for addressing family conflict. The group receiving RAP-P plus routine care (crisis management and safety planning) had adolescents who reported fewer SITBs (i.e., combined nonsuicidal and suicidal self-injurious thoughts and behaviors) over the course of treatment and over the 6-month follow-up compared to adolescents whose parents received routine care only (which ranged from crisis management and safety planning to CBT and supportive therapy; ITT analyses). Notably, improved family functioning fully mediated the significant intervention effects (Pineda & Dadds, 2013). Based on the positive results from this RCT, Parent Training remains classified as Level 2: Probably efficacious for reducing SITBs in youth.
Support-based therapy
There have been no changes in the efficacy rating of Support-Based Therapy since the prior review. Two trials, reviewed previously, have examined a Youth-Nominated Support Team (YST) intervention for suicidal adolescents (King et al., 2009; King et al., 2006). In YST, adolescents nominate caring others (family, school, community) to participate in this supportive treatment. Neither trial found that YST reduced rates of SA in youth. Although there was not a main effect of treatment, the first trial found that, among those actually treated, YST reduced SI in girls but not boys (King et al., 2006). The second trial, which restricted nominations to adults only (not peers), found that YST reduced SI from baseline to six weeks, but effects were not maintained over the 3–12-month follow-ups (King et al., 2009). Moreover, effects of YST for reducing SI were stronger among adolescents with a history of multiple SAs. Taken together, Support-Based Therapy was classified as Level 4: Experimental for reducing SI and Level 5: Questionable efficacy for reducing SA in youth.
Eclectic group therapy
In this review, we combined categories previously titled “CBT skills + DBT skills + Psychodynamic therapy skills-Group” and “CBT skills-Group” into one treatment family called “Eclectic group therapy” since all trials examined a group intervention that combined skills across theoretical orientations. The status of eclectic group therapy has not changed since the prior review. Three studies have examined Developmental Group Therapy (DGT; Wood, Trainor, Rothwell, Moore, & Harrington, 2001)—a group intervention that combines skills from CBT, DBT, and psychodynamic group therapy. Although the initial RCT produced promising results for reducing DSH for youth receiving DGT compared to routine care (ITT analyses; Wood et al., 2001), findings failed to replicate in two subsequent trials. One trial (Assessment of Treatment in Suicidal Teenagers; ASSIST trial) reported nonsignificant findings for DSH in DGT compared to routine care (ITT analyses; Green et al., 2011). A second trial indicated that the experimental intervention may actually be iatrogenic with the DGT group reporting more DSH than those receiving routine care (ITT analyses; Hazell et al., 2009). Findings for SI were nonsignificant for all three trials.
Rudd and colleagues (1996) examined a separate eclectic skills group including psychoeducation, problem-solving, social competence skills, and experiential-affective groups. (Of note, this group intervention was previously categorized separately from the three trials above, but was combined in this review given the relative similarities between the treatment packages.) Both the experimental and TAU (included both inpatient and outpatient treatment) groups led to significant reductions in SI over the treatment period, but the group intervention did not lead to significantly greater reductions in SI.
Taken together, Eclectic Group Therapy remains evaluated as Level 5: Questionable efficacy for reducing DSH and SI in youth.
Resource interventions
This category includes a range of interventions focused on increasing youth’s access to mental health resources and care (previously called “Resource interventions—Individual”). Two trials were included in the prior review (Cotgrove, Zirinsky, Black, & Weston, 1995; Robinson et al., 2012) and one trial new to this review (Morthorst et al., 2012).
In the earliest trial to examine a resource intervention, Cotgrove et al. (1995) compared standard care plus a token to access the hospital on demand vs. standard care in an RCT with 105 adolescents with a history of DSH or SA. Youth in the experimental treatment reported fewer SA compared to the control treatment, but between-group differences were not significant.
Using a different approach, Robinson and colleagues (2012) tested whether a modified postcard intervention (Motto, 1976) would increase connection to care among young people. In an RCT, 164 adolescents and young adults at high-risk for suicide were assigned to receive monthly postcards for one year (that promoted use of coping skills and well-being) plus TAU in the community, or TAU alone. Over an 18-month follow-up, there were no significant between-group differences in DSH, SA, or SI.
In a trial not included in the prior review, Morthorst et al. (2012) compared an assertive intervention for deliberate self-harm (AID) to standard care (i.e., referral to a range of treatment modalities). AID included 8–20 sessions over six months focusing on case management, crisis intervention, and outreach to improve compliance with follow-up psychiatric care. The overall RCT included 243 individuals admitted to the hospital for a suicide attempt, with 56 adolescents between the ages of 11 and 19. At one-year follow-up, there were no differences in SA between the AID and standard care groups (ITT analyses).
Resource interventions were previously evaluated as Level 4: Experimental. We have maintained this rating for Resource interventions’ efficacy for reducing DSH and SI since these outcomes have only been examined in one trial. However, given the addition of Morthorst et al. (2012) and the nonsignificant findings for SA across these trials, we have downgraded the efficacy of these treatment packages to Level 5: Questionable efficacy for reducing SA in youth.
Other interventions
Two trials that met inclusion criteria for our review tested other, novel interventions that did not fit into any of the other treatment categories. Therefore, these trials are reviewed separately below.
Motivational interviewing (MI).
This intervention was categorized on its own because, although MI has been included in other treatment packages in this review (Esposito-Smythers et al., 2011; Ougrin et al., 2011), this is the first MI-focused intervention. In addition, even though this was an initial trial, it was large enough (ns ≥ 20 adolescents per group) and included randomization, thereby meeting the inclusion criteria for our review.
King et al. (2015) tested a novel motivational intervention called Teen Options for Change (TOC) plus enhanced TAU vs. enhanced TAU alone (emergency referrals and resources, as well as informational resources about depression, suicide risk, and means restriction). Interventions were compared in a pilot RCT among 49 youth who presented for nonpsychiatric reasons but screened positive for suicide risk (i.e., recent SI, SA, depression and substance abuse) in the ED. In light of research indicating that many individuals visit a treatment provider in the year before suicide death (Ahmedani et al., 2014; O’Connor, Gaynes, Burda, Soh, & Whitlock, 2013), it is particularly important to consider ways to effectively identify youth who may be at high risk for suicide but may not be presenting for psychiatric reasons. In TOC, adolescents receive feedback about their screening responses and a 35–45 minute MI session. From baseline to 2-month follow-up, SI decreased for all adolescents, but there was no significant effect of the intervention. However, the small effect size for TOC was in the expected direction. Given that half the sample (53%) met inclusion criteria for the trial based on depression and substance use instead of SITBs, this trial may have underestimated treatment effects for suicidal youth specifically. Based on this initial RCT, Motivational Interviewing is evaluated as Level 4: Experimental for reducing SI in youth.
A second, recent trial did not meet inclusion criteria for our review due to sample size, but is relevant to this treatment family and therefore reviewed briefly here. In a pilot RCT with 36 adolescents hospitalized for suicide risk, Czyz, King, and Biermann (2018) compared a motivational interview-enhanced safety planning intervention (MI-SafeCope) to hospital TAU plus the Recovery Action Plan (crisis management strategies and safety planning). The MI-SafeCope intervention includes three components: (1) individual session: development of personalized safety plan, MI techniques used to increase motivation to change; (2) family session: review safety plan with family and increase parents’ motivation and commitment to the plan; and (3) post-discharge calls with adolescent and parent separately: to adjust safety plan and enhance motivation as needed (Czyz, King, & Biermann, 2018). For the experimental intervention, completion rates and satisfaction ratings were high suggesting that the intervention was both feasible to administer to hospitalized youth and families as well as acceptable to this population. Although adolescents in the MI-SafeCope group reported greater self-efficacy to refrain from engagement in SITBs (the targeted mechanism of change), there were no differences between groups in SA or SI over the study period. However, as this pilot trial was not intended, nor powered, to examine treatment efficacy, further replication in a large-scale RCT is needed.
Brief skills training.
This intervention also met inclusion criteria for our review but is categorized on its own because it did not fit into a larger treatment family.
As Safe as Possible (ASAP) is a brief (3-hour) skills training intervention and app-supported follow-up for hospitalized youth aimed at reducing suicidal behavior post-discharge (Kennard et al., 2015). Focusing on the post-discharge period is critical given its identification as one of the highest risk periods for suicide attempts and deaths in youth (Chung et al., 2017; Goldston et al., 1999). The ASAP intervention is first administered on the inpatient unit and includes motivational interviewing, psychoeducation, safety planning, behavioral activation, mood monitoring, reasons for living, and emotion regulation and distress tolerance skills training. Next, families are contacted by phone 1–2 weeks post-discharge to encourage follow-up care. Finally, following hospital discharge, a smartphone app provides access to distress tolerance and emotion regulation skills as well as a personalized safety plan. In addition, adolescents rate in daily text messages, via smartphone, their current emotional distress and are offered strategies for coping based on their distress level (e.g., skills at lower distress levels and safety plan at higher distress levels).
In a recent RCT (Kennard et al., 2018), 66 adolescents hospitalized for SA or SI were randomly assigned to ASAP plus TAU or TAU only. Findings indicate that the ASAP intervention group reported fewer SAs over the 24-week follow-up than the TAU group, but this difference was not statistically significant (ITT analyses). In addition, SI decreased in both treatment groups, but between-group differences were not significant. Finally, there was not a significant treatment effect on NSSI.
Although preliminary and without significant effects on SA or SI, this initial RCT suggests that the ASAP intervention is both acceptable and feasible to administer among a high-risk population during a critical and high-risk time period (post-discharge). Further replication is needed in a large-scale RCT to test the efficacy of this treatment package. Based on this initial study, this intervention is rated as Level 4: Experimental for reducing NSSI, SA, and SI in youth.
Clinical trials in progress
Our search of ClinicalTrials.gov resulted in nine clinical trials currently in progress or recently completed that are testing a range of psychosocial interventions for reducing SITBs in youth. These trials are described briefly next.
Three trials include interventions with a strong MI and/or family focus. One RCT will examine a novel intervention for adolescent inpatients with comorbid alcohol use and SITBs. This intervention uses MI with both the adolescent and family as well as an mHealth booster after discharge to enhance commitment to change and support from the family (“Brief Alcohol Intervention and mHealth Booster for Suicidal Adolescents”; NCT03607318: PI: O’Brien). A second, recently completed trial examined an adjunct intervention for adolescents hospitalized for suicide risk. The intervention includes 2–3 individual sessions on the unit using MI acceptance-based strategies, one family session, and phone follow-ups for six months post-discharge (“Coping Long Term with Attempted Suicide – Adolescents [CLASP-A]”; NCT01748760; PI: Yen). Finally, an RCT in progress will examine a 6-week individual and family-centered outpatient intervention for youth presenting to the ED for suicide risk. Individual sessions will focus on strategies to help adolescents manage suicidal thoughts and impulses and family sessions target family conflict and improving communication (“Focused Suicide Prevention Strategy for Youth [FSPS]”; NCT03488602; PI: Korczak).
Two trials will examine different intervention strategies within the healthcare system. One RCT will compare different follow-up services post-hospitalization (e.g., intensive individualized care management with multiple systems in the adolescent’s life) aimed at decreasing risk for subsequent suicidal behavior and rehospitalization (“Promote Access to Stop Suicide [PASS]: comparison of F/U services for Youth at Risk for Suicide”; NCT03016572; PI: Falcone). Another RCT will compare zero suicide best practices (ZSQI) to ZSQI plus a stepped care model for suicide prevention. This stepped care model will use risk assessments for triage, in-person and internet-delivered CBT and DBT treatment components and coaching support, as well as regular monitoring of adolescents’ outcomes to inform treatment planning (Randomized Trial of Stepped Care for Suicide Prevention in Teens and Young Adults [Step2Health]; NCT03092271; PI: Asarnow).
Four trials are focused on specific high-risk populations of youth: one among youth in the juvenile justice system, one in Latinx immigrant youth, and two in American Indian youth. One upcoming RCT will compare a safety planning intervention to TAU among youth in the juvenile justice system (“Screening and Brief Intervention for Suicidality and Nonsuicidal Self-Injury Among Youth in the Juvenile Justice System”; NCT03655470; PI: Spirito). Another upcoming RCT will compare a family-based intervention to enhanced TAU (with safety planning) in Latinx immigrant adolescents and their parents (“Early intervention for Suicide Risk Among Immigrant Youth”; NCT03221530; PI: Alvarez). Finally, two related trials are specifically focused on American Indian (AI) youth, a population with one of the highest suicide death rates in the U.S. (Leavitt et al., 2018). These trials will test and compare the efficacy of two novel interventions for AI youth: (1) the New Hope curriculum, which includes psychoeducation, coping skills, and connection to trusted adults; and (2) the Elders Resiliency curriculum, which is taught by community elders and focuses on values and connectedness (“Southwest Hub for American Indian Youth Suicide Prevention Research”; NCT03543865; PIs: Cwik & O’Keefe; “Brief Interventions for the Prevention of Suicide and the Promotion of Resilience in Suicidal American Indian Youth”; NCT03132766; PIs: Barlow & Cwik).
Summary of Evidence Base Update
Significant changes since the prior 2015 review
With the addition of nine RCTs in this review, there were a number of significant changes to the evidence base since the prior review. The most notable change was the evaluation of DBT-A as the first Level 1: Well-established treatment for reducing DSH and SI among youth (McCauley et al., 2018; Mehlum et al., 2014). This evaluation is consistent with the adult treatment literature in which DBT has demonstrated efficacy in a number of RCTs for reducing suicidal thoughts and behaviors with moderate effect sizes (Kliem et al., 2010). Promising findings were also found for reductions in NSSI and SA in one DBT-A trial (McCauley et al., 2018), but replication is needed across two independent RCTs to reach Level 1 status for these specific SITB outcomes.
RCT replication was less helpful for the status of Psychodynamic Therapy—Family-Based, “brand name” Attachment-Based Family Therapy (Diamond et al., 2018; Diamond et al., 2010), which is now rated as Level 4: Experimental for reducing SI and SA in youth. Although the first RCT was promising for reducing SI (Diamond et al., 2010), the recent replication found that ABFT did not significantly reduce SA or SI in youth compared to a manualized comparison intervention that controlled for experimental treatment dose (Diamond et al., 2018). This failure to replicate an earlier promising intervention highlights the need for additional trials testing the same intervention (an issue we will return to in the Future Research Directions section).
A second major change since the prior review is the evaluation of Integrated Family Therapy, “brand name” Safe Alternatives for Teens and Youth (SAFETY; Asarnow et al., 2017), as Level 2: Probably efficacious for reducing SA in youth. Notably, this is another promising intervention for reducing suicidal behavior in adolescents, which is the most important, yet challenging, target in SITB treatment research.
Third, since the prior review, a few novel and brief interventions have been tested in pilot RCTs (Kennard et al., 2015; King et al., 2015). These treatments may be promising in larger trials but are currently evaluated as Level 4: Experimental for reducing SITBs in youth.
Finally, it is also important to note the lack of change since the prior review. New trials testing CBT—Individual (Hetrick et al., 2017) and Family Therapy (Cottrell et al., 2018) have been added but did not improve the efficacy rating of these interventions. In addition, as highlighted in our review, many treatment families have not changed significantly since the prior review. For a number of promising Level 2 treatments, there remains only one RCT to base evaluations (Esposito-Smythers et al., 2011; Pineda & Dadds, 2013; Rossouw & Fonagy, 2012; Tang et al., 2009), with no replications since the prior review.
Efficacious treatment components across interventions
Although few interventions examined the same treatment package, there are shared components of efficacious interventions that are worth highlighting.
Family-centered.
Five of the six interventions identified as either Level 1: Well-established or Level 2: Probably efficacious for reducing SITBs in youth had an active family therapy or parent training component. Shared features of these interventions include parent/family psychoeducation (Asarnow et al., 2017; Esposito-Smythers et al., 2011; McCauley et al., 2018; Mehlum et al., 2014; Pineda & Dadds, 2013), emotion regulation skills (Asarnow et al., 2017; Esposito-Smythers et al., 2011; McCauley et al., 2018; Mehlum et al., 2014; Rossouw & Fonagy, 2012), communication skills (Asarnow et al., 2017; Esposito-Smythers et al., 2011; Pineda & Dadds, 2013), and problem-solving skills training (Asarnow et al., 2017; Esposito-Smythers et al., 2011; Pineda & Dadds, 2013). IPT-A was the only intervention that did not involve the family; this intervention was delivered to students in schools. Given that IPT-A focuses on ameliorating current interpersonal difficulties (some of which may occur with family members), this intervention may indirectly target family functioning.
However, it is important to note that not all family therapy interventions were efficacious. The two interventions classified as “Family therapy” produced null findings (Cottrell et al., 2018; Harrington et al., 1998) as did “Brief family-based therapy” in the ED (Asarnow et al., 2011; Ougrin et al., 2013). Why were some family interventions efficacious and others not? Comparing multicomponent family-centered interventions to one-session ED interventions is challenging as there are many differences between these treatment packages including, most notably, treatment length. Instead, it may be more appropriate to compare Family therapy and the Level 2 efficacious family-centered interventions. A notable difference between these treatment families is the dose of the intervention, which was substantially less in the Family therapies (five sessions within two months, Harrington et al., 1998; 6–8 sessions over six months; Cottrell et al., 2018) compared to the Level 2 efficacious interventions including a family component, such as DBT-A (weekly individual therapy, weekly multifamily group therapy, and phone skills coaching as needed for 4–6 months; McCauley et al., 2018; Mehlum et al. 2014) and Integrated Family Therapy (average 10 sessions over three months; Asarnow et al., 2017). In one of the few studies to examine treatment mechanisms of a family intervention, Harrington et al. (1998) found that home-based family therapy did not improve family functioning, suggesting that this intervention may not provide a sufficient dose of family treatment. The field would benefit from additional research identifying the optimal amount of family therapy needed to improve family functioning among suicidal youth. Additional dismantling studies may help to clarify the essential components of family therapy that make this intervention efficacious.
Skills training.
Another notable component of efficacious interventions was the delivery of individual skills training for the adolescent. Shared skills training across treatments included emotion regulation skills (Asarnow et al., 2017; Esposito-Smythers et al., 2011; McCauley et al., 2018; Mehlum et al., 2014; Rossouw & Fonagy, 2012)—which were the most common, followed by distress tolerance (Asarnow et al., 2017; McCauley et al., 2018; Mehlum et al., 2014), mindfulness (Asarnow et al., 2017; McCauley et al., 2018; Mehlum et al., 2014), interpersonal effectiveness (McCauley et al., 2018; Mehlum et al., 2014; Tang et al., 2009), and problem-solving skills (Asarnow et al., 2017; Esposito-Smythers et al., 2011). Future research on treatment mechanisms is needed to identify the core skills that make these interventions efficacious.
Treatment dose.
It is unclear what amount of treatment is needed to meaningfully impact SITBs in youth. However, this review does highlight that very brief, or low dose, interventions, whether family-based (Asarnow et al., 2011; Ougrin et al., 2013) or resource/outreach focused (Cotgrove et al., 1995; Morthorst et al., 2012; Robinson et al., 2012), do not appear to be substantial enough for reducing SITBs in youth. The briefest interventions that demonstrated some efficacy were IPT-A, which was delivered twice a week for six weeks (Tang et al., 2009), and parent training, which included four weekly or biweekly sessions (Pineda & Dadds, 2013). However, it is important to note these interventions reduced SI (Tang et al., 2009) or scores on a composite SITB scale (Pineda & Dadds, 2013), rather than the more challenging outcome to impact—suicide attempts. Efficacious interventions for reducing suicide attempts specifically were intensive for 3–12 months (Asarnow et al., 2017; Esposito-Smythers et al., 2011; McCauley et al., 2018; Mehlum et al., 2014)—an issue we return to later when we discuss scalability of these interventions.
Important considerations for treatment evaluation
There were a number of challenges when evaluating interventions for SITBs in youth that warrant discussion. First, it was challenging to classify interventions into broader treatment families as most were multicomponent treatment packages that spanned treatment type (e.g., CBT and DBT), modality (e.g., individual and family components), and ranged in treatment length (from one session to one year). As a result, many “treatment families” contain a single intervention type and trial. We recognize that some of these classifications may change as additional RCTs are added to the evidence base. For now, in the Efficacious treatment components across interventions section, we aimed to summarize the shared components across the Level 1 and 2 efficacious trials (also see Brent et al., 2013 review).
Second, control/comparison treatments varied widely across RCTs. Most trials (92%) included a form of treatment-as-usual (TAU), either on its own (e.g., typical standard of care in that setting) or enhanced with additional components to match the experimental intervention, such as clinical monitoring, phone calls to increase treatment adherence, or medication management. TAU varied as a function of theoretical orientation, number of treatment sessions delivered and attended, as well as the role of the family in treatment. As noted by Spirito et al. (2002), variability of TAU makes interpretation of RCT findings challenging.
Only two trials in this review compared a SITB intervention to a manualized psychological comparison treatment that controlled for the dose of the experimental intervention. Notably, both trials (Diamond et al., 2018; McCauley et al., 2018) were replications of interventions that had demonstrated positive findings in an initial RCT. DBT-A had first demonstrated efficacy for reducing DSH and SI compared to enhanced usual outpatient care (Mehlum et al., 2014). In a second RCT, DBT-A demonstrated efficacy for reducing these SITBs compared to individual and group supportive therapy (IGST), which is a manualized treatment that matches the dose of treatment provided in DBT-A (McCauley et al., 2018). However, the outcome for the second treatment family replication was not as promising. Psychodynamic therapy—Family-based (“brand name” Attachment-Based Family Therapy) had proven efficacious compared to enhanced usual care (i.e., referral + clinical monitoring) in an initial RCT (Diamond et al., 2010). However, in a second RCT, this intervention was not more efficacious than family-enhanced nondirective support therapy (NE-NST), a manualized intervention that aimed to match the dose of ABFT (Diamond et al., 2018). RCTs including a manualized, active psychological comparison treatment increase confidence that the experimental intervention is responsible for the observed treatment effects (see Future Directions).
A third consideration is that efficacious treatments also varied in the clinical severity of the adolescents targeted. Samples were recruited from emergency departments (Pineda & Dadds, 2013), inpatient units (Esposito-Smythers et al., 2011), outpatient treatment clinics (Mehlum et al., 2014), high schools (Tang et al., 2009), or a mixture of these recruitment settings (Asarnow et al., 2017; McCauley et al., 2018; Rossouw & Fonagy, 2012). Further research is needed to determine whether certain interventions may work better for more vs. less clinically severe youth.
Fourth, evaluation of treatment efficacy was also complicated by inconsistent information reported about intervention completion and attrition across trials. Some studies reported detailed information about treatment completion across all groups and follow-up assessments, whereas others did not. In order to accurately evaluate experimental treatment efficacy, it is essential to know how well adolescents and families engaged with both the experimental and the control/comparison interventions (Becker et al., 2018).
Finally, the SITB outcomes targeted in treatment varied across studies: some distinguished nonsuicidal (e.g., nonsuicidal self-injury) and suicidal outcomes (e.g., suicide ideation, suicide attempts), whereas others did not distinguish behaviors based on suicide intent (e.g., deliberate self-harm, which is a composite of suicidal and nonsuicidal self-injury) or combined suicidal thoughts and behaviors into one continuous outcome. Although nonsuicidal and suicidal self-injury are strongly linked, they have clinically relevant differences (Grandclerc, De Labrouhe, Spodenkiewicz, Lachal, & Moro, 2016) that suggest the importance of developing treatments targeting each outcome specifically. It is also important to distinguish between suicidal thoughts and behaviors. Although SI is impairing for youth (Copeland et al., 2017; Foley et al., 2006), only a third of adolescents who think about suicide will engage in suicidal behavior (Glenn et al., 2017; Nock et al., 2013). Moreover, a history of suicide attempts is the most robust predictor of suicide deaths (Ribeiro et al., 2016). Thus, treatments that target SI may not have implications for reductions in suicidal behavior. Moreover, in studies that examine deliberate self-harm as an outcome, it is unclear whether the intervention is efficacious for reducing nonsuicidal self-injury, suicide self-injury, or both. Future research would benefit from distinguishing between suicidal and nonsuicidal outcomes, as well as between thoughts and behaviors.
Future Research Directions
RCT replication
Consistent with the recommendations from the prior review, there is a great need for replication of promising interventions by independent research groups. As already noted, important replications have occurred in the past five years to establish DBT-A as a Level 1: Well-established treatment for youth DSH and SI and to downgrade Psychodynamic Therapy—Family-based to a Level 4: Experimental intervention for reducing SA and SI in youth. There are five other promising Level 2: Probably efficacious interventions that warrant replication by independent research groups. In particular, the field would benefit from replications of the two family-centered interventions that have demonstrated initial promise for reducing suicide attempts in youth (CBT—Individual + Family; Esposito-Smythers et al., 2011; Integrated Family Therapy; Asarnow et al., 2017). Moreover, as already discussed, it will be important for replications to include manualized, active psychological comparison treatments.
Treatment mediators and moderators
Replication in larger trials is also important to examine potential mechanisms of change (mediators) among efficacious interventions as well as clarification of which interventions work best for which youth (moderators).
A few of the Level 2: Probably efficacious trials have identified potential mediators of treatment efficacy supporting the mechanisms of change proposed in these trials. In the parent training trial (“brand name” Resourceful Adolescent Parent Program; RAP-P), improved family functioning mediated (full mediation via parent report, partial mediation via adolescent report) the intervention effect on adolescents’ SITBs (Pineda & Dadds, 2013). In addition, in Psychodynamic therapy—Individual + Family (“brand name” Mentalization-Based Treatment for Adolescents; MBT-A), enhancements in attachment and mentalization mediated the treatment effect on adolescents’ DSH. Moreover, new to this review, one of the DBT-A trials found that the total number of treatment contacts partially mediated the effect of DBT on adolescents’ DSH and SI (Mehlum et al., 2014). Identifying mechanisms of change in efficacious interventions is essential for understanding how these treatments work and for developing brief versions of these treatments (see Future Directions).
It is also important to identify which interventions may work for which youth as a one-size-fits-all approach will likely not be sufficient (Kraemer, Wilson, Fairburn, & Agras, 2002). A few of the Level 4: Experimental trials identified potential treatment moderators. For instance, although Harrington et al. (1998) did not find a main effect of their home-based family intervention in the full sample, they did find significantly greater decreases in SI among non-depressed adolescents who received the experimental intervention. In addition, although the main findings of Support-Based Therapy (“brand name” Youth-Nominated Support Team) were mixed, treatment effects on SI reductions were stronger among girls (King et al., 2006) and among youth with a history of multiple suicide attempts (King et al., 2009). However, none of the interventions evaluated at Level 1 or Level 2 examined potential treatment moderators. Small sample sizes in some of these trials (20–40 adolescents per group) may have limited the statistical power to examine treatment effects based on major sociodemographic variables or severity of prior SITBs, which will be important in future trials.
Scalable and adaptive treatments
An important direction for future SITB treatment research is to consider methods for scaling efficacious interventions to reach large numbers of youth. Sadly, most youth with mental health difficulties do not receive adequate mental health treatment (Jensen et al., 2011; Kataoka, Zhang, & Wells, 2002). Accessibility concerns (e.g., cost, long waitlists, travel length, access to qualified providers), stigma (related to psychiatric disorders and treatment), and perception of treatment efficacy are among the top barriers to treatment among youth (Gulliver, Griffiths, & Christensen, 2010; Owens et al., 2002; Smith, Linnemeyer, Scalise, & Hamilton, 2013). These treatment barriers could be targeted in three, non-mutually exclusive, ways.
First, the development of briefer interventions would increase accessibility for youth across a range of treatment settings. Most efficacious interventions, especially those that reduce suicide attempts in youth, are relatively long and intensive. The interventions found to be efficacious for reducing self-injurious behavior (i.e., DSH or SA) in youth range from three months to one year: the new Integrated Family Therapy trial (“brand name” SAFETY; Asarnow et al., 2017) is the shortest at three months, the DBT-A treatment packages are 4–6 months long (McCauley et al., 2018; Mehlum et al., 2014), and finally CBT—Individual + Family (“brand name” I-CBT; Esposito-Smythers et al., 2011) and Psychodynamic Therapy—Individual + Family (“brand name” Mentalization-Based Treatment for Adolescents (MBT-A: Rossouw & Fonagy, 2012) are both year-long interventions. Most of these interventions are also intensive. For instance, DBT-A includes individual therapy, multifamily group skill training, and phone skills coaching with the therapist as needed (McCauley et al., 2018; Mehlum et al., 2014). Integrated Family Therapy requires two therapists (one for the adolescent and one for the parent) and treatment may occur in the home as needed (Asarnow et al., 2017). Thus, these efficacious psychotherapies may not be feasible for youth receiving treatment in many health care settings, particularly those from disadvantaged backgrounds (Kataoka et al., 2002). As already noted, research is needed to clarify the core treatment components and sufficient dose to develop briefer versions of these efficacious interventions.
A second way to enhance scalability of evidence-based treatments is to consider digital, or internet-based, versions rather than those using in-person delivery. Growing research indicates that digital interventions are feasible and acceptable for youth (Friedberg et al., 2014; Richardson, Stallard, & Velleman, 2010) and may be just as efficacious as in-person delivery (Werner-Seidler, Johnston, & Christensen, 2018; Zachariae, Lyby, Ritterband, & O’Toole, 2016). Moreover, young people are likely to choose electronic versions of interventions when available (de Bruin, Bogels, Oort, & Meijer, 2015). Taken together, digital interventions may be a promising way to close gaps in treatment and scale efficacious interventions to reach large numbers of suicidal youth who are in great need of treatment. It is important to note that the main digital intervention included in this review, internet-based CBT—Individual (Hetrick et al., 2017), was not significantly efficacious for reducing SITBs in youth. Perhaps this is not surprising given that in-person CBT—Individual did not demonstrate efficacy for reducing SITBs in youth in the prior review (Glenn et al., 2015). Future studies should consider adapting efficacious in-person interventions into digital, or internet-based, forms.
Finally, it is important to consider other novel approaches for delivering efficacious intervention components. One promising future direction is the development of just-in-time adaptive interventions (JITAIs). JITAIs aim to apply interventions at the right time (i.e., when the intervention is needed and not when it is not needed) and in an adaptive manner (i.e., varying the timing, type, and amount of intervention as needed; see review; Nahum-Shani et al., 2017). One example of an early stage adaptive intervention for reducing SITBs in youth is the ASAP treatment for recently hospitalized youth, which provides differential feedback to youth based on their self-reported level of distress (Kennard et al., 2018). Notably, the treatment strategies included in this intervention package (e.g., coping skills, safety plan) are not novel to this intervention, but are being applied in a novel way—at the time they may be most needed and in a way that is tailored, or adapted, to the adolescent’s current needs. The efficacy of JITAIs hinges on being able to identify dynamic changes that increase vulnerability—specifically when these changes are likely to occur and at which point they are clinically meaningful (Nahum-Shani et al., 2017). Ecological momentary assessment (EMA) research with suicidal populations (Kleiman et al., 2017; Nock, Prinstein, & Sterba, 2009) will be crucial to identify dynamic, within-person fluctuations in risk factors that may be targeted in future JITAIs.
Concluding Comments
Over the past five years (since the search ended for the prior Evidence Base Update; Glenn et al., 2015), there has been a significant increase in RCTs testing psychosocial interventions for reducing SITBs among youth. This review identified nine additional RCTs since the prior review—many of which were previously in the clinical trials phase. The most significant change since the prior review is that DBT-A has been evaluated as the first Level 1: Well-established intervention for reducing DSH and SI in youth. Five other promising interventions were identified that include significant family therapy and skills training components. Future research should focus on replicating promising interventions currently evaluated as Level 2: Probably efficacious as well as developing brief interventions that may be scalable to treat large numbers of youth.
Acknowledgments
The authors would like to thank Anne Boatman, Elizabeth Finer, John Kellerman, and Da Min Paik for their assistance reviewing the relevant literature for this manuscript.
References
(*Denotes RCTs included in this review.)
- Ahmedani BK, Simon GE, Stewart C, Beck A, Waitzfelder BE, Rossom R, … Operskalski BH (2014). Health care contacts in the year before suicide death. Journal of General Internal Medicine, 29(6), 870–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alavi A, Sharifi B, Ghanizadeh A, & Dehbozorgi G (2013). Effectiveness of cognitive-behavioral therapy in decreasing suicidal ideation and hopelessness of the adolescents with previous suicidal attempts. Iranian Journal of Pediatrics, 23(4), 467–472. [PMC free article] [PubMed] [Google Scholar]
- *.Asarnow JR, Baraff LJ, Berk M, Grob CS, Devich-Navarro M, Suddath R, … Tang L (2011). An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatric Services, 62(11), 1303–1309. doi: 10.1176/ps.62.11.pss6211_1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Berk M, Hughes JL, & Anderson NL (2015). The SAFETY Program: A treatment-development trial of a cognitive-behavioral family treatment for adolescent suicide attempters. Journal of Clinical Child & Adolescent Psychology, 44(1), 194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Asarnow JR, Hughes JL, Babeva KN, & Sugar CA (2017). Cognitive-behavioral family treatment for suicide attempt prevention: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 56(6), 506–514. doi: 10.1016/j.jaac.2017.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker KD, Boustani M, Gellatly R, & Chorpita BF (2018). Forty years of engagement research in children’s mental health services: Multidimensional measurement and practice elements. Journal of Clinical Child & Adolescent Psychology, 47(1), 1–23. [DOI] [PubMed] [Google Scholar]
- Berk MS, Starace NK, Black VP, & Avina C (2018). Implementation of dialectical behavior therapy with suicidal and self-harming adolescents in a community clinic. Archives of Suicide Research. [DOI] [PubMed] [Google Scholar]
- Brent DA, McMakin DL, Kennard BD, Goldstein TR, Mayes TL, & Douaihy AB (2013). Protecting adolescents from self-harm: a critical review of intervention studies. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1260–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Web-based Injury Statistics Query and Reporting System (WISQARS). (2017a). National Center for Injury Prevention and Control, Center for Disease Control and Prevention. Available from www.cdc.gov/injury/wisqars/index.html
- Centers for Disease Control and Prevention [CDC]. (2017b). Youth Risk Behavior Survey Questionnaire. Retrieved September 5, 2018 Available at: www.cdc.gov/yrbs
- Chambless DL, Baker MJ, Baucom DH, Beutler LE, Calhoun KS, Crits-Christoph P, … Woody SR (1998). Update on empirically validated therapies, II. Clinical Psychologist, 51(1), 3–16. [Google Scholar]
- Chambless DL, & Hollon SD (1998). Defining empirically supported therapies. Journal of Consulting and Clinical Psychology, 66, 7–18. [DOI] [PubMed] [Google Scholar]
- Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, & Large MM (2017). Suicide rates after discharge from psychiatric facilities: a systematic review and meta-analysis. JAMA Psychiatry, 74(7), 694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Goldston DB, & Costello EJ (2017). Adult associations of childhood suicidal thoughts and behaviors: a prospective, longitudinal analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 56(11), 958–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Cotgrove A, Zirinsky L, Black D, & Weston D (1995). Secondary prevention of attempted suicide in adolescence. Journal of Adolescence, 18, 569–577. doi: 10.1006/jado.1995.1039 [DOI] [Google Scholar]
- *.Cottrell DJ, Wright-Hughes A, Collinson M, Boston P, Eisler I, Fortune S, … Farrin AJ (2018). Effectivenenss of systemic family therapy versus treatment as usual for young people after self-harm: a pragmatic, phase 3, multicentre, randomized controlled trial. Lancet Psychiatry, 5, 203–216. doi: 10.1016/S2215-0366(18)30058-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czyz EK, King CA, & Biermann BJ (2018). Motivational interviewing-enhanced safety planning for adolescents at high suicide risk: A pilot randomized controlled trial. Journal of Clinical Child and Adolescent Psychology, 1–13. doi: 10.1080/15374416.2018.1496442 [DOI] [PubMed] [Google Scholar]
- de Bruin E, Bogels S, Oort F, & Meijer AM (2015). Efficacy of cognitive behavioral therapy for insomnia in adolescents: a randomized controlled trial with internet therapy, group therapy and a waiting list condition. Sleep, 38(12), 1913–1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Diamond GS, Kobak RR, Ewing ESK, Levy SA, Herres JL, Russon JM, & Gallop RJ (2018). A randomized-controlled trial: Attachment-based family and nondirective supportive treatments for suicidal youth. Journal of the American Academy of Child & Adolescent Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond GS, Reis BF, Diamond GM, Siqueland L, & Isaacs L (2002). Attachment-based family therapy for depressed adolescents: A treatment development study. Journal of the American Academy of Child & Adolescent Psychiatry, 41(10), 1190–1196. [DOI] [PubMed] [Google Scholar]
- *.Diamond GS, Wintersteen MB, Brown GK, Diamond GM, Gallop R, Shelef K, & Levy S (2010). Attachment-based family therapy for adolescents with suicidal ideation: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 49(2), 122–131. doi: 10.1016/j.jaac.2009.11.002 [DOI] [PubMed] [Google Scholar]
- Donaldson D, Spirito A, & Esposito-Smythers C (2005). Treatment for adolescents following a suicide attempt: Results of a pilot trial. Journal of the American Academy of Child Adolescent Psychiatry, 44(2), 113–120. doi: 10.1097/00004583-200502000-00003 [DOI] [PubMed] [Google Scholar]
- *.Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, & Monti P (2011). Treatment of co-occurring substance abuse and suicidality among adolescents: A randomized trial. Journal of Consulting and Clinical Psychology, 79(6), 728–739. doi: 10.1037/a0026074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito-Smythers C, Spirito A, Uth R, & LaChance H (2006). Cognitive behavioral treatment for suicidal alcohol abusing adolescents: Development and pilot testing. American Journal of Addiction, 15, 126–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foley DL, Goldston DB, Costello EJ, & Angold A (2006). Proximal psychiatric risk factors for suicidality in youth: The Great Smoky Mountains Study. Archives of General Psychiatry, 63(9), 1017–1024. [DOI] [PubMed] [Google Scholar]
- Freeman J, Garcia A, Frank H, Benito K, Conelea C, Walther M, & Edmunds J (2014). Evidence base update for psychosocial treatments for pediatric obsessive-compulsive disorder. Journal of Clinical Child and Adolescent Psychology, 43(1), 7–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedberg RD, Hoyman LC, Behar S, Tabbarah S, Pacholec NM, Keller M, & Thordarson MA (2014). We’ve come a long way, baby!: Evolution and revolution in CBT with youth. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 32(1), 4–14. [Google Scholar]
- Glenn CR, Franklin JC, & Nock MK (2015). Evidence-based psychosocial treatments for self-injurious thoughts and behaviors in youth. Journal of Clinical Child & Adolescent Psychology, 44(1), 1–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Lanzillo EC, Esposito E, Santee AC, Nock MK, & Auerbach RP (2017). Examining the course of suicidal and nonsuicidal self-injurious thoughts and behaviors in outpatient and inpatient adolescents. Journal of Abnormal Child Psychology, 45(5), 971–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Reboussin DM, Reboussin BA, Frazier PH, & Kelley AE (1999). Suicide attempts among formerly hospitalized adolescents: A prospective naturalistic study of risk during the first 5 years after discharge. Journal of the American Academy of Child & Adolescent Psychiatry, 38(6), 660–671. [DOI] [PubMed] [Google Scholar]
- Grandclerc S, De Labrouhe D, Spodenkiewicz M, Lachal J, & Moro MR (2016). Relations between nonsuicidal self-injury and suicidal behavior in adolescence: A systematic review. PLoS One, 11(4), e0153760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Green JM, Wood AJ, Kerfoot MJ, Trainor G, Roberts C, Rothwell J, … Harrington R (2011). Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ, 342, d682. doi: 10.1136/bmj.d682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, & Christensen H (2010). Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry, 10(1), 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Harrington R, Kerfoot M, Dyer E, McNiven F, Gill J, Harrington V, … Byford S (1998). Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves. Journal of the American Academy of Child & Adolescent Psychiatry, 37(5), 512–518. doi: 10.1016/s0890-8567(14)60001-0 [DOI] [PubMed] [Google Scholar]
- *.Hazell PL, Martin G, McGill K, Kay T, Wood A, Trainor G, & Harrington R (2009). Group therapy for repeated deliberate self-harm in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 48(6), 662–670. doi: 10.1097/CHI.0b013e3181a0acec [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Schoenwald SK, Borduin CM, Rowland MD, & Cunningham PB (2009). Multisystemic therapy for antisocial behavior in children and adolescents (2nd edition). New York, NY: Guilford. [Google Scholar]
- *.Hetrick SE, Yuen HP, Bailey E, Cox GR, Templer K, Rice SM, … Robinson J (2017). Internet-based cognitive behavioural therapy for young people with suicide-related behaviour (Reframe-IT): a randomised controlled trial. Evid Based Mental Health, 20(3), 76–82. doi: 10.1136/eb-2017-102719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Högberg G, & Hällström T (2018). Mood regulation focused CBT based on memory reconsolidation, reduced suicidal ideation and depression in youth in a randomised controlled study. Int J Environ Res Public Health, 15(5), 1–10. doi: 10.3390/ijerph15050921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu LM (2016). Random sampling, randomization, and equivalence of contrasted groups in psychotherapy outcome research In Kazdin AE (Ed.), Methodological Issues and Strategies in Clinical Research (4th ed.) (pp. 143–152). Washington, DC: American Psychological Association. [DOI] [PubMed] [Google Scholar]
- *.Huey SJ, Henggeler SW, Rowland MD, Halliday-Boykins CA, Cunningham PB, Pickrel SG, & Edwards J (2004). Multisystemic therapy effects on attempted suicide by youths presenting psychiatric emergencies. Journal of the American Academy of Child and Adolescent Psychiatry, 43(2), 183–190. doi: 10.1097/01.chi.0000101700.15837.f3 [DOI] [PubMed] [Google Scholar]
- Jensen PS, Goldman E, Offord D, Costello EJ, Friedman R, Huff B, … Conger R (2011). Overlooked and underserved:”action signs” for identifying children with unmet mental health needs. Pediatrics, 128(5), 970–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kataoka SH, Zhang L, & Wells KB (2002). Unmet need for mental health care among US children: Variation by ethnicity and insurance status. American Journal of Psychiatry, 159(9), 1548–1555. [DOI] [PubMed] [Google Scholar]
- Katz C, Bolton S-L, Katz LY, Isaak C, Tilston-Jones T, Sareen J, & Team SCSP (2013). A systematic review of school-based suicide prevention programs. Depression and Anxiety. [DOI] [PubMed] [Google Scholar]
- Kazdin AE (1996). Dropping out of child psychotherapy: Issues for research and implications for practice. Clinical Child Psychology and Psychiatry, 1(1), 133–156. [Google Scholar]
- Kennard BD, Biernesser C, Wolfe KL, Foxwell AA, Craddock Lee SJ, Rial KV, … Blastos B (2015). Developing a brief suicide prevention intervention and mobile phone application: A qualitative report. Journal of Technology in Human Services, 33(4), 345–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kennard BD, Goldstein T, Foxwell AA, McMakin DL, Wolfe K, Biernesser C, … Brent D (2018). As Safe as Possible (ASAP): A brief app-supported inpatient intervention to prevent postdischarge suicidal behavior in hospitalized, suicidal adolescents. American Journal of Psychiatry, 175(9), 864–872. doi: 10.1176/appi.ajp.2018.17101151) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerfoot M, Harrington R, & Dyer E (1995). Brief home-based intervention with young suicide attempters and their families. Journal of Adolescence, 18(5), 557–568. [Google Scholar]
- *.King CA, Gipson PY, Horwitz AG, & Opperman KJ (2015). Teen Options for Change: An intervention for young emergency patients who screen positive for suicide risk. Psychiatric Services, 66(1), 97–100. doi: 10.1176/appi.ps.201300347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.King CA, Klaus N, Kramer A, Venkataraman S, Quinlan P, & Gillespie B (2009). The Youth-Nominated Support Team-Version II for suicidal adolescents: A randomized controlled intervention trial. Journal of Consulting and Clinical Psychology, 77(5), 880–893. doi: 10.1037/a0016552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.King CA, Kramer A, Preuss L, Kerr DC, Weisse L, & Venkataraman S (2006). Youth-Nominated Support Team for Suicidal Adolescents (Version 1): A randomized controlled trial. Journal of Consulting and Clinical Psychology, 74(1), 199–206. doi: 10.1037/0022-006X.74.1.199 [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, & Nock MK (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726–738. [DOI] [PubMed] [Google Scholar]
- Kliem S, Kröger C, & Kosfelder J (2010). Dialectical behavior therapy for borderline personality disorder: A meta-analysis using mixed-effects modeling. Journal of Consulting and Clinical Psychology, 78(6), 936–951. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, & Agras WS (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59(10), 877–883. [DOI] [PubMed] [Google Scholar]
- Leavitt RA, Ertl A, Sheats K, Petrosky E, Ivey-Stephenson A, & Fowler KA (2018). Suicides among American Indian/Alaska Natives—National Violent Death Reporting System, 18 States, 2003–2014. Morbidity and Mortality Weekly Report, 67(8), 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan M (1993). Cognitive behavioral treatment of borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, … Lindenboim N (2006). Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry, 63(7), 757. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Heard HL, & Armstrong HE (1993). Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Archives of General Psychiatry, 50(12), 971. [DOI] [PubMed] [Google Scholar]
- *.McCauley E, Berk MS, Asarnow JR, Adrian M, Cohen J, Korslund K, … Linehan MM (2018). Efficacy of dialectical behavior therapy for adolescents at high risk for suicide: A randomized clinical trial. JAMA Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Mehlum L, Ramberg M, Tormoen AJ, Haga E, Diep LM, S. L, … Groholt B (2014). Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: A randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry, 53(10), 1082–1091. doi: 10.1016/j.jaac.2014.07.003 [DOI] [PubMed] [Google Scholar]
- Mehlum L, Ramberg M, Tormoen AJ, Haga E, Diep LM, Stanley BH, … Groholt B (2016). Dialectical behavior therapy compared with enhanced usual care for adolescents with repeated suicidal and self-harming behavior: Outcomes over a one-year follow-up. Journal of the American Academy of Child and Adolescent Psychiatry, 55(4), 295–300. doi: 10.1016/j.jaac.2016.01.005 [DOI] [PubMed] [Google Scholar]
- Miller AL, Rathus JH, Linehan MM, Wetzler S, & Leigh E (1997). Dialectical behavior therapy adapted for suicidal adolescents. Journal of Psychiatric Practice, 3(2), 78. [Google Scholar]
- *.Morthorst B, Krogh J, Erlangsen A, Alberdi F, & Nordentoft M (2012). Effect of assertive outreach after suicide attempt in the AID (assertive intervention for deliberate self harm) trial: randomised controlled trial. BMJ, 345, e4972. doi: 10.1136/bmj.e4972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton V, & Torgerson DJ (2005). Regression to the mean: treatment effect without the intervention. Journal of Evaluation in Clinical Practice, 11(1), 59–65. [DOI] [PubMed] [Google Scholar]
- Motto JA (1976). Suicide prevention for high‐risk persons who refuse treatment. Suicide and Life-Threatening Behavior, 6, 223–230. [PubMed] [Google Scholar]
- Muehlenkamp JJ, Claes L, Havertape L, & Plener PL (2012). International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child and Adolescent Psychiatry and Mental Health, 6(1), 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mufson L, Moreau D, Weissman MM, & Klerman G (1993). Interpersonal psychotherapy for depressed adolescents. New York, NY: Guilford Press. [Google Scholar]
- Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, & Murphy SA (2017). Just-in-time adaptive interventions (JITAIs) in mobile health: Key components and design principles for ongoing health behavior support. Annals of Behavioral Medicine, 52(6), 446–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Action Alliance for Suicide Prevention (NAASP): Research Prioritization Task Force. (2014). A prioritized research agenda for suicide prevention: An action plan to save lives National Institute of Mental Health and the Research Prioritization Task Force. Rockville, MD. [Google Scholar]
- Nock MK (2010). Self-Injury. Annual Review of Clinical Psychology, 6, 339–363. doi: 10.1146/annurev.clinpsy.121208.131258 [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, & Lee S (2008). Suicide and suicidal behavior. Epidemiologic Reviews, 30(1), 133–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, & Kessler RC (2013). Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry, 70(3), 300–310. doi: 10.1001/2013.jamapsychiatry.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ, & Sterba S (2009). Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology, 118(4), 816–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor E, Gaynes BN, Burda BU, Soh C, & Whitlock EP (2013). Screening for and treatment of suicide risk relevant to primary care: a systematic review for the US Preventive Services Task Force. Annals of Internal Medicine, 158(10), 741–754. [DOI] [PubMed] [Google Scholar]
- Ougrin D, Boege I, Stahl D, Banarsee R, & Taylor E (2013). Randomised controlled trial of therapeutic assessment versus usual assessment in adolescents with self-harm: 2-year follow-up. Archives of Disease in Childhood, 98(10), 772–776. doi: 10.1136/archdischild-2012-303200 [DOI] [PubMed] [Google Scholar]
- *.Ougrin D, Zundel T, Ng A, Banarsee R, Bottle A, & Taylor E (2011). Trial of therapeutic assessment in London: Randomised controlled trial of therapeutic assessment versus standard psychosocial assessment in adolescents presenting with self-harm. Archives of Disease in Childhood, 96(2), 148–153. [DOI] [PubMed] [Google Scholar]
- Owens PL, Hoagwood K, Horwitz SM, Leaf PJ, Poduska JM, Kellam SG, & Ialongo NS (2002). Barriers to children’s mental health services. Journal of the American Academy of Child & Adolescent Psychiatry, 41(6), 731–738. [DOI] [PubMed] [Google Scholar]
- *.Pineda J, & Dadds MR (2013). Family intervention for adolescents with suicidal behavior: A randomized controlled trial and mediation analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 52(8), 851–862. doi: 10.1016/j.jaac.2013.05.015 [DOI] [PubMed] [Google Scholar]
- Rathus JH, & Miller AL (2014). Dialectical behavior therapy skills manual for adolescents. New York, NY: The Guilford Press. [Google Scholar]
- Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, & Nock MK (2016). Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: A meta-analysis of longitudinal studies. Psychological Medicine, 46(2), 225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson T, Stallard P, & Velleman S (2010). Computerized cognitive behavioural therapy for the prevention and treatment of depression and anxiety in children and adolescents: A systematic review. Clinical Child and Family Review, 13, 275–290. [DOI] [PubMed] [Google Scholar]
- Robinson J, Cox G, Malone A, Williamson M, Baldwin G, Fletcher K, & O’Brien M (2013). A systematic review of school-based interventions aimed at preventing, treating, and responding to suicide-related behavior in young people. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 34(3), 164. [DOI] [PubMed] [Google Scholar]
- Robinson J, Hetrick S, Cox G, Bendall S, Yuen HP, Yung A, & Pirkis J (2016). Can an internet‐based intervention reduce suicidal ideation, depression and hopelessness among secondary school students: Results from a pilot study. Early Intervention in Psychiatry, 10(1), 28–35. [DOI] [PubMed] [Google Scholar]
- Robinson J, Hetrick S, Cox G, Bendall S, Yung A, & Pirkis J (2015). The safety and acceptability of delivering an online intervention to secondary students at risk of suicide: Findings from a pilot study. Early Intervention in Psychiatry, 9(6), 498–506. [DOI] [PubMed] [Google Scholar]
- Robinson J, Hetrick S, Cox G, Bendall S, Yung A, Yuen HP, … Pirkis J (2014). The development of a randomised controlled trial testing the effects of an online intervention among school students at risk of suicide. BMC Psychiatry, 14(1), 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Robinson J, Yuen HP, Gook S, Hughes A, Cosgrave E, Killackey E, … Yung A (2012). Can receipt of a regular postcard reduce suicide-related behaviour in young help seekers? A randomized controlled trial. Early Intervention in Psychiatry, 6(2), 145–152. doi: 10.1111/j.1751-7893.2011.00334.x [DOI] [PubMed] [Google Scholar]
- *.Rossouw TI, & Fonagy P (2012). Mentalization-based treatment for self-harm in adolescents: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 51(12), 1304–1313. doi: 10.1016/j.jaac.2012.09.018 [DOI] [PubMed] [Google Scholar]
- *.Rudd D, Rajab H, Orman DT, Stulman DA, Joiner T, & Dixon W (1996). Effectiveness of an outpatient intervention targeting suicidal young adults: Preliminary results. Journal of Consulting and Clinical Psychology, 64(1), 179–790. [DOI] [PubMed] [Google Scholar]
- Silverman MM, Berman AL, Sanddal ND, O’Carroll PW, & Joiner TE (2007). Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide and Life-Threatening Behavior, 37(3), 248–263. [DOI] [PubMed] [Google Scholar]
- Silverman WK, & Hinshaw SP (2008). The second special issue on evidence-based psychosocial treatments for children and adolescents: A 10-year update. Journal of Clinical Child and Adolescent Psychology, 37(1), 1–7. [DOI] [PubMed] [Google Scholar]
- Singer JB, Erbacher TA, & Rosen P (2018). School-based suicide prevention: A framework for evidence-based practice. School Mental Health: A Multidisciplinary Research and Practice Journal, 1–18. [Google Scholar]
- Smith T, Linnemeyer R, Scalise D, & Hamilton J (2013). Barriers to outpatient mental health treatment for children and adolescents: Parental perspectives. Journal of Family Psychotherapy, 24(2), 73–92. [Google Scholar]
- Southam-Gerow MA, & Prinstein MJ (2014). Evidence base updates: The evolution of the evaluation of psychological treatments for children and adolescents. Journal of Clinical Child and Adolescent Psychology, 43(1), 1–6. [DOI] [PubMed] [Google Scholar]
- Spirito A, Stanton C, Donaldson D, & Boergers J (2002). Treatment-as-usual for adolescent suicide attempters: Implications for the choice of comparison groups in psychotherapy research. Journal of Clinical Child and Adolescent Psychology, 31(1), 41–47. [DOI] [PubMed] [Google Scholar]
- Spirito A, Wolff JC, Seaboyer LM, Hunt J, Esposito-Smythers C, Nugent N, … Miller I (2015). Concurrent treatment for adolescent and parent depressed mood and suicidality: feasibility, acceptability, and preliminary findings. Journal of Child and Adolescent Psychopharmacology, 25(2), 131–139. doi: 10.1089/cap.2013.0130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley B, Brown G, Brent DA, Wells K, Poling K, Curry J, … Goldstein T (2009). Cognitive-behavioral therapy for suicide prevention (CBT-SP): Treatment model, feasibility, and acceptability. Journal of the American Academy of Child & Adolescent Psychiatry, 48(10), 1005–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swannell SV, Martin GE, Page A, Hasking P, & St John NJ (2014). Prevalence of nonsuicidal self-injury in nonclinical samples: Systematic review, meta-analysis and meta-regression. Suicide and Life-Threatening Behavior, 44(3), 273–303. [DOI] [PubMed] [Google Scholar]
- *.Tang TC, Jou SH, Ko CH, Huang SY, & Yen CF (2009). Randomized study of school-based intensive interpersonal psychotherapy for depressed adolescents with suicidal risk and parasuicide behaviors. Psychiatry and Clinical Neurosciences, 63(4), 463–470. doi: 10.1111/j.1440-1819.2009.01991.x [DOI] [PubMed] [Google Scholar]
- Werner-Seidler A, Johnston L, & Christensen H (2018). Digitally-delivered cognitive-behavioural therapy for youth insomnia: A systematic review. Internet Interventions, 11, 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Wood A, Trainor G, Rothwell J, Moore A, & Harrington R (2001). Randomized trial of group therapy for repeated deliberate self-harm in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 40(11), 1246–1253. doi: 10.1097/00004583-200111000-00003 [DOI] [PubMed] [Google Scholar]
- Wright-Hughes A, Graham E, Farrin A, Collinson M, Boston P, Eisler I, … Simic M (2015). Self-Harm Intervention: Family Therapy (SHIFT), a study protocol for a randomised controlled trial of family therapy versus treatment as usual for young people seen after a second or subsequent episode of self-harm. Trials, 16(1), 501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyman PA (2014). Developmental approach to prevent adolescent suicides: Research pathways to effective upstream preventive interventions. American Journal of Preventive Medicine, 47(3), S251–S256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachariae R, Lyby MS, Ritterband LM, & O’Toole MS (2016). Efficacy of internet-delivered cognitive-behavioral therapy for insomnia–a systematic review and meta-analysis of randomized controlled trials. Sleep Medicine Reviews, 30, 1–10. [DOI] [PubMed] [Google Scholar]