Abstract
Objective
The aim of this review was to identify, appraise and synthesise studies that reported on the contribution of women’s development army (WDA) to maternal and child health development.
Setting
Studies conducted in Ethiopia 2010 onwards and published in English were considered.
Data sources
Evidence were searched in MEDLINE, CINAHL and EBSCOhost from 25 March to 10 April 2018.
Eligibility criteria
Both quantitative and qualitative studies assessing the contribution of WDA to maternal and child health were considered.
Data extraction and synthesis
Two independent reviewers have extracted data using pre-planned data extraction tool separately for each study design. Findings were synthesised using tables and narrative summary.
Outcome
Maternal and child health services; maternal and child mortality.
Results
Nine studies met the inclusion criteria and were used for synthesis. The results revealed that participation and membership in women’s development teams (WDTs) have a positive effect on minimising maternal death and improving child immunisation service use. Skilled delivery and antenatal care service use were higher in WDTs located within a radius of 2 km from health facilities. Women’s development teams were also the main sources of information for mothers to prepare themselves for birth and related complications. Moreover, well-established groups have strengthened the linkage of the health facility to the community so that delays in maternal health service use were minimised; health extension workers could effectively refer women to a health facility for birth and utilisation of skilled birth service was improved.
Conclusion
Voluntary health service intervention in Ethiopia has improved maternal and child health services’ outcome. A decrease in maternal deaths, increase in antenatal and delivery service use and improved child immunisation service uptake are attributable to this intervention. The linkage between community members and the primary healthcare system served as an effective and efficient mechanism to share information.
Keywords: women’s development army, maternal and child health, Ethiopia
Strengths and limitations of this study.
The review has used two independent reviewers who rigorously searched and reviewed the published materials. Furthermore, a third reviewer participated when disagreements arose between the two reviewers.
The review has used structured procedure during literature search, appraisal, data collection and synthesis
Despite the strengths described above, we have not conducted meta-analysis due to the heterogeneous nature of the study design and population included in this review.
We have included only full-text articles found free online.
Introduction
Evidence from various countries in the world disclosed that community volunteers’ health service intervention has shown significant health impact.1 2 They accomplish various functions related to health service delivery. In fact, usually, they do not have formal professional or paraprofessional education and can be involved in voluntary care. They intervene in healthcare after attending job-related pieces training. These community health volunteers have different names in different settings, for example, lay health workers, community health workers and unpaid community volunteers.3 4
Community health volunteers have great importance, especially in less developed countries, so as to overcome the increasing demand for healthcare services and the shortage of formal healthcare providers.5 After the Alma Ata declaration of Primary Healthcare (PHC) in 1978, community involvement in the healthcare was given due attention in order to improve the wide access and acceptance of the services by service users and the community at large. It is believed that problems cannot be solved from only the side of service providers and programmers. Moreover, it is a good strategy to mobilise resources relevant to health services.6–8
Health service interventions using community volunteers have a sort of structure in some countries and are unstructured in others.1 5 Some nations linked the service under their PHC structure. Ethiopia is a good example of well-structured community health interventions. The primary healthcare unit (PHCU) is in the front line to PHC in the country. This system encompasses five satellite health posts (the lowest being the village-level health service facility) and a referral health centre (HC). In the country’s healthcare system, PHC is administered and the services facilitated in this point.9 In order to address the deficit in human resources in healthcare, Ethiopia launched the community health extension programme (HEP) in 2004. It was implemented by establishing a health post in every kebele (the smallest administrative division in Ethiopia) and positioning two female health extension workers (HEWs). The HEP was launched to improve access to preventive, essential health services and to create a healthy environment. This programme works to increase and sustain preventive health actions and health awareness. HEP has 16 packages divided into four major categories.9–11
Six years after its introduction, in 2010, a new innovative approach, women’s development army (WDA) was linked with HEP. The WDA is a structural arrangement that involves women’s development teams (WDTs) and one-to-five connections. One-to-five connections involve six households within the same neighbourhood. A women who knows 16 packages of HEP and practises them all is chosen as the leader to serve five households. A household that implemented the 16 packages of HEP is recognised as a model family. Five to six one-to-five connections together formulate a WDT, which means that 30–36 households in the same neighbourhood constitute a WDT. A similar procedure followed to select the leader of WDTs in addition to says of members. They serve as volunteers.12 This structure has various development roles, of which health is the major one.9 At the community level, members of the community are linked with the PHC system through this strategy.13 It was adopted based on the experience that using a network of the community health volunteers increased the efficiency of HEWs in reaching households with actionable health messages.10 14 15
The WDT’s developmental works are monitored in a meeting every 2 weeks by a command post formulated at the kebele level, which is led by the kebele leader. The development team leaders undertake similar follow-up of the one-to-five networks.9 WDTs and the leaders of the one-to-five networks are selected with full participation of the members. Their trustworthiness to the team members and being a model family are considered as criteria for selection.16
HEWs in collaboration with kebele administration and personnel from other developmental sectors (agriculture and education) facilitate the formation of the WDTs and one-to-five networks. These unpaid health volunteers, WDT leaders, undertake various preventive and promotive health services in collaboration with HEWs. They carry out a number of tasks, including support during health information delivery programmes, keeping track of pregnancies and illnesses, helping during immunisation campaigns and transmitting messages between households and HEWs.9 10
The WDA’s contribution can be related to maternal and child health indicators as consecutive Ethiopian demographic and health surveys indicated. For instance, maternal death was 673 in 2005 and 676 in 2011 per 100 000 live births. However, it became 412 in 2016; note that WDA structure was introduced in Ethiopia in 2010. Under five mortality also decreased from 88 in 2011 to 67 in 2016. Maternal health services have shown a massive increase during these points as compared with prior years. Antenatal care (ANC) increased from 28% in 2005 to 34% in 2011 and 62% in 2016. Institutional delivery increased from 5% in 2005 to 10% in 2011 and 26% in 2016. Postnatal care also increased from 5% in 2005 to 8% in 2011 and 17% in 2016.17–20 These figures indicated that there is an impressive improvement in maternal and child health and service use after the introduction of WDA in the country.
The Ethiopian unpaid community health intervention has a unique structural arrangement. It has included the strategic plans of various development sectors.14 Some evidence claim that the programme has variations in aims, goals and experiences among various players included and suggests further researchers.21 This review aimed to assess the contribution of this structured community involvement in maternal and child health and service use.
Methods
Search strategy
The search strategy targeted to find both published and unpublished studies. A step-by-step search strategy was utilised in this review. Primarily, major databases that comprise health system research including MEDLINE, CINAHL, and EBSCOhost were utilised. Unpublished works were also searched from ProQuest Dissertations and Theses and Google Scholar. Afterward, the reference list of all identified reports and articles were searched for additional studies. Keywords initially used were: community health workers, community volunteer, WDA, women’s development group (WDG), WDT, health development team, lay health workers, health development army, Ethiopia, maternal health, child health and maternal health services. Extracted references were downloaded and stored into Mendeley reference manager file. MEDLINE (on PubMed platform) search strategy is included in online supplementary file I.
bmjopen-2018-025937supp001.pdf (181.9KB, pdf)
To guide the overall review, the PRISMA flow diagram was used (figure 1).22 Starting from the identification of records up to the inclusion of relevant literature for the review question were documented to comprehensive and accurate reporting.
Figure 1.
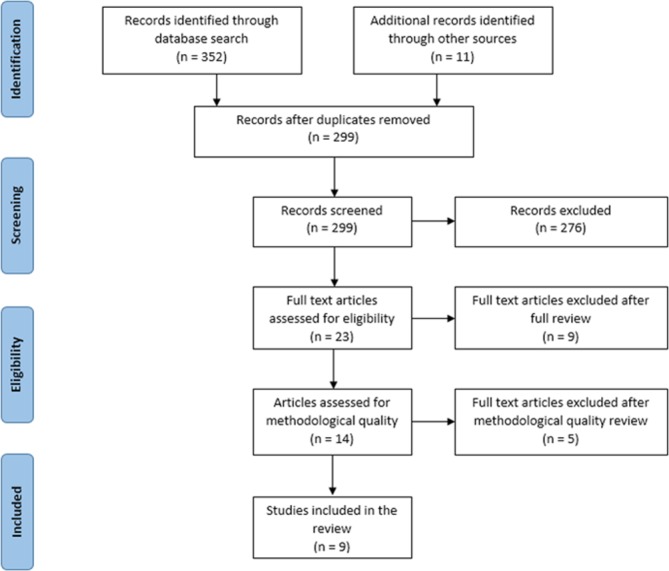
Literature search and screening.
Inclusion and exclusion criteria
Both quantitative and qualitative studies were included in this review regardless of their study design, given that they included women in the reproductive age group (14–49 years) and children less than 5 years of age for both sexes. To be considered, the studies should have evaluated the effect of WDA, and participation in the WDT on maternal mortality, maternal and child health service use. These are major intervention areas of WDAs regarding maternal and child health. Moreover, studies conducted in Ethiopia, 2010 (a year when WDA was introduced in Ethiopia) onward and published in English language were considered for inclusion in this review. We have excluded narrative summaries, case reports and technical reports.
Description of studies
Eleven potentially relevant studies were found with a free search in Google Scholar and Google Search bars in addition to the three hundred fifty-two studies identified in database searches. A total of 299 articles were eligible for primary examination after duplications were removed. On reviewing titles and abstracts against the review objectives and inclusion criteria, 276 studies were excluded. The full text of the remaining 23 studies was then retrieved for detailed examination and 9 were excluded. Later, 14 studies were assessed for methodological quality. The quality assessment was done by two independent reviewers for methodological validity prior to inclusion in the review using standardised critical appraisal instruments from the Joanna Briggs Institute.23–25 Disagreements that arise between the reviewers were resolved through discussion, and with the participation of a third reviewer. After the appraisal, five studies that did not meet the minimum requirements of methodological appraisal tools were excluded and nine were finally reviewed.
Patient and public involvement
Patients and/or public were not involved in this review.
Data collection
Before data collection, all titles and abstracts of the searched pieces of literature were assessed for potential relevance, and those records deemed not relevant were verified. Later on, full-text reports were assessed for eligibility. In the cases we fail to get articles free online, we tried to obtain full texts from research-gate26 authors’ pages and we obtained three. Reports that are co-publications or multiple reports of the same study were identified. The eligibility criteria were applied to all reports. Only evidence thoughtful of the review’s eligibility criteria were included. Studies that fulfilled more than 70% of the critical appraisal checklists’ requirements were selected to be included in the review (online supplementary file II).
bmjopen-2018-025937supp002.pdf (92.7KB, pdf)
Two independent reviewers collected information relevant for the review. Data extraction for quantitative and qualitative studies was done separately using pre-designed checklists (online supplementary file III). The extracted data have included specific details about the interventions, populations, study methods and outcomes of significance to the review question and objectives (online supplementary file IV).
bmjopen-2018-025937supp003.pdf (85KB, pdf)
bmjopen-2018-025937supp004.pdf (206.8KB, pdf)
Data synthesis and analysis
Findings from the included studies were synthesised using tables and a narrative summary. Meta-analysis was not possible since the included studies were heterogeneous in terms of the populations, methods and outcomes. We have categorised the results into participation in WDTs, distance of WDTs from health facility and effective functioning of WDTs. When we categorise the synthesis into these three parts, we put a base on some major principles of PHC and their effectiveness. Access to basic preventive and promotive healthcare, active participation of the community in their health issues and effectiveness of the system.27
Results: findings of the review
We have included a total of nine studies that met the requirements of critical appraisal checklists, regardless of their study design. These studies met the critical appraisal requirements by more than 70% (online supplementary file II). The review comprised both observational and qualitative studies. The studies were conducted on various maternal and child health issues including child immunisation, maternal mortality, birth preparedness and complication readiness (BPCR), skilled delivery, ANC, linking pregnant women with health facilities for delivery, delays in maternal health services and community relationships with HEWs and the healthcare sector (table 1).
Table 1.
Characteristics of the studies included for review
| Category | Sub-category | Frequency | % |
| Study design | Cross-sectional | 3 | 33.33 |
| Case–control | 2 | 22.22 | |
| Qualitative | 4 | 44.44 | |
| Year of publication | 2015 | 2 | 22.22 |
| 2016 | 3 | 33.33 | |
| 2017 | 3 | 33.33 | |
| 2018 | 1 | 11.11 | |
| Addressed maternal and child health issue | Skilled maternal health service use | 3 | 33.33 |
| Relationship of community with healthcare sector | 3 | 33.33 | |
| Child immunisation | 1 | 11.11 | |
| Maternal mortality | 1 | 11.11 | |
| Birth preparedness and complication readiness | 1 | 11.11 |
Narrative synthesis
Participation in WDTs
We found two studies that focused on participation in WDTs. Aregawi et al 28 studied 270 children aged between 9 and 23 months for immunisation status using the case–control method. Out of the total 270 children, 90 were from the case group (children who default from immunisation programme) and 180 were from the control group (children who have taken all recommended vaccines). Only 14 (15.6%) children from the case group were from mothers who have good participation in WDT and 76 (84.4%) were from poor participant mothers. On the other hand, Godefay et al’s29 study focused on maternal mortality. Out of 310 mothers, 62 died and 248 were alive. Out of the 62 dead mothers, 40 (64.5%) were members of WDTs and out of the 248 alive mothers, 197 (79.4%) were members of WDTs. This shows that more women (30.7%) who died and less women (22.6%) who were alive were not members of WDTs. In both categories, the majority of the mothers were members of WDTs. However, the proportion of alive mothers outweigh the dead ones.
Results from statistical analysis revealed that participation in WDTs has a positive effect on both child immunisation and maternal survival. Poor participation in WDTs (Adjusted Odds Ratio (AOR)=3.3, 95% CI 1.54±7.08) is a determinant of defaulting immunisation among children aged between 9 and 23 months. Similarly, women who were not members of the voluntary WDT were more likely to experience maternal death (OR 2.07, 95% CI 1.04 to 4.11) (table 2).
Table 2.
Evidence summary of the effect of participation in a WDT on maternal and child health service
| Author, year | Target population | Study design | Outcome | Result |
| Aregawi et al,28 2017 |
Children aged between 9 and 23 months | Case–control | Default from immunisation among children aged between 9 and 23 months | Poor participation in WDTs (AOR=3.3,95% CI 1.54±7.08) is a determinant of defaulting |
| Godefay et al,29 2015 |
Mothers in the reproductive age group | Case–control | Maternal mortality | Women who were not members of a WDT were more likely to experience maternal death (OR 2.07, 95% CI 1.04 to 4.11) |
AOR, adjusted odds ratio; WDT, women’s development team.
Distance of WDTs from health facility
In relation to the distance of WDTs from the health facility, we have found two studies by Negero et al 30 and Girmaye and Berhan 31 The first study has evaluated skilled delivery attendance and the second one ANC service use. Both studies totally assessed 748 reproductive-age women who gave birth in 1 year preceding the study in 380 clusters of WDT. In the study by Negero et al,30 336 (45%) of women have received skilled delivery care. While 531 (71%) of the participants received skilled ANC service at least once, as indicated in the other study.31 In both studies, a significant heterogeneity was observed between WDT (clusters) for skilled delivery care service utilisation, which explains about 62% of the total variation. Even if the distance of WDTs within 2 km radius from the nearest health facility was significant predictor in both studies, the adjusted OR result has shown a strong association with ANC service utilisation (AOR=8.28; 95% CI 1.08 to 62.20) as compared with skilled delivery care (AOR (95% CI) 6.03 (1.92, 18.93)) (table 3).
Table 3.
Evidence summary of the effect of WDT distance from health facility on maternal health service
| Author, year | Target population | Study design | Outcome | Result |
| Negero et al,30 2018 | Reproductive-age women who gave birth in 1 year preceding the study | Cross-sectional | Skilled delivery service utilisation | The distance of WDTs within 2 km radius from the nearest health facility was significantly associated with skilled delivery service use (AOR (95% CI) 6.03 (1.92, 18.93)) |
| Girmaye and Berhan, 31 2016 | Reproductive-age women who gave birth in 1 year preceding the study | Cross-sectional | Skilled ANC utilisation | Distance of WDT within 2 km radius from the nearest health facility was significant predictor of skilled ANC service utilisation (AOR=8.28; 95% CI 1.08 to 62.20) |
ANC, antenatal care; AOR, adjusted odds ratio; WDT, women’s development team.
Effective functioning of WDTs
When WDTs and one-to-five connections perform what they are intended to do effectively, good improvements on maternal health services use were seen. In a study by Zepre and Kaba,32 the BPCR of pregnant women was assessed. From 454 pregnant women, 44 were members of one-to-five connections. Sixty eight per cent got information from their network and prepared for birth and its complications as compared with 34% among non-members. There was also a statistically significant association between effective information delivery in one-to-five connection and BPCR (OR 2.52, 95% CI 1.17, 5.39). Whereas performance of WDTs has no significant effect on skilled delivery service and ANC service utilisation in the two studies by Negero et al 30 and Girmaye and Berhan.31
A strong and functional relationship between WDTs and HEWs is one aspect of good functioning WDT. Regarding this we have reviewed four studies. A study by Jackson and Hailemariam33 has assessed the role of HEWs in linking pregnant women with health facilities for delivery. Two studies by Jackson et al 34 35 aimed to document the factors that hinder or enable strategies to reduce the first and second delays of the three delays in rural and pastoralist areas in Ethiopia; and exploring HEWs' and mothers' attitudes to maternal health service utilisation and acceptance. Another study by Kok et al 36 has addressed HEWs’ relationships with the community and the healthcare sector in Ethiopia: opportunities for enhancing maternal health performance.
A well-established WDA structure has facilitated the linkage and relationship between the health system and mothers.33–36 Support from well-established WDTs has enabled HEWs to effectively refer more women to give birth in health facilities. Moreover, initiatives to reduce delays in maternal health service use were effective with the support of WDTs. HEWs easily get information about the date of delivery of each member of women in the community through HDTs so that they facilitate transportation to a health facility and additional services.34 35 These relationships have increased skilled birth attendance in many parts of the country. In general, WDTs are serving as liaising agents in the community to link the health system with mothers and children in the community.35 36 (table 4).
Table 4.
Summary of evidence on WDA’s effective functioning on maternal health services
| Author, year | Target population | Study design | Outcome | Result |
| Zepre and Kaba,32 2017 |
Pregnant women | Cross-sectional | Birth preparedness and complication readiness | Those who got information from their one-to-five connections are more likely to prepare for birth and its complications (OR 2.52, 95% CI 1.17 to 5.39) |
| Jackson and Hailemariam,33 2016 | Pregnant women | Qualitative | Linking pregnant women with health facilities for delivery | HEWs can effectively refer more women to give birth in health facilities when the WDA is well functioning |
| Jackson et al,34 2017 | Pregnant women | Qualitative | Delays in maternal health service use | Initiatives to reduce delays can improve access to maternal health services, especially when HEWs are supported by WDTs |
| Jackson R et al,35 2016 | Mothers and HEWs | Qualitative | Maternal health service utilisation and acceptance | With the support of WDTs, HEWs have increased the rate of skilled birth attendance |
| Kok et al,36 2015 | Mothers and HEWs | Qualitative | Relationship of community with HEWs and the healthcare sector | WDTs supported HEWs in liaising with community members |
HEW, health extension worker; WDA, women’s development army; WDT, women’s development team.
Discussion
The main objective of this systematic review was to identify, appraise and synthesise studies that reported on the contribution of Ethiopian women’s innovative voluntary health intervention’s (WDA’s) contribution to maternal and child health development. The major activity of this structure is supporting the primary healthcare intervention under the HEP.37 38 Most probably, this is the first systematic review that synthesised information on WDA and its contribution. Nine studies were assessed and all of them revealed that WDA has contributed towards the improved maternal and child health, and health service use. The evidence has shown that the benefit of WDA was obtained through participation in the group,28 29 closeness of the groups to health facilities30 31 and their effective functioning.32–36
Despite the fact that the Ethiopian female community health intervention has special features, unpaid community health intervention has been used in various countries to improve population’s health.15 As various findings indicated, it is a cost-effective measure, especially in low-income countries with low access to health services. They applied this strategy to curve the disastrous shortfalls in the health workforce and to improve community ownership.39–42
Women at the village level are expected to be a part of and actively participate in the one-to-five connections under the WDTs. By doing so, they can easily obtain information, care and support from the primary healthcare structure.16 21 Involving community members in health services brings about an improvement in health service use and the health status of the community.10 43 44 A low level of default from immunisation was found among children whose mothers have a good experience of participating in WDTs. Those who were not members of WDTs are more than three times more likely to default from the service as compared with those included.28 Community involvement in vaccination programmes for children was found to be effective in many low-income and middle-income countries.45 46 For example, two systematic reviews focused on low-income population revealed that participation of community health workers has improved child immunisation.47 48 Their involvement lets the community participate in decision making and improves their knowledge, so that ownership improved.49
Participation in WDTs in Ethiopia minimised maternal deaths. Women who are not members of WDTs are two times more at risk of experiencing maternal death in the study area.29 The participation of community members had a positive effect on maternal survival.50 Moreover, the Ethiopian WDT involvement resulted in improved BPCR.32 Community health participation in India has also significantly minimised maternal death.51 This implied that those who took part in promoting health with WDTs could improve their health literacy and develop a good attitude towards the use of maternal health services.
The other major issues regarding WDA’s contribution to maternal health and health service use is the distance from health facilities in reference to their meeting area. When the distance became beyond 2 km from the nearest health centre or hospital, members were less likely to use ANC and delivery service as compared with their counterparts.30 31 As the meeting area of WDTs became nearer to health facilities, HEWs and health professionals from the health facilities could easily supervise and support the members during their meeting. Even if many national and international policy documents have given due concern for physical access to improve maternal health service use,14 52 53 the problem prevails in many low-income and middle-income countries.54–57 This concern is also experienced by WDTs in Ethiopia.
Although there is some information that revealed that the performance of WDTs does not have anything in improving maternal health service use,30 31 there is ample of evidence that shows effective functioning and good performance of these groups would result in improved maternal health and health service use.32–36 In the previous studies, performance of the groups was measured by traditional ways of performance measurement at the village level. The performance measurement ways, measurement indicators and evaluators may not be effective in measuring the actual performance of the groups. Other evidence revealed that well-performing WDTs facilitated the linkage between mothers and the primary healthcare system. As a result, service utilisation and acceptance were improved.33–35 Although the performance measurement ways differ in diverse settings, good performing community health interventions succeeded in improving maternal and child health development in low-income countries.58–60 As a result, countries tend to improve the performance of their community health practitioners.61 62 These findings add to the growing body of evidence that, health workers at the community level can work with women’s groups to improve maternal health, thus reducing the need for emergency obstetric care in low-income countries.
On top of this, strongly operating WDTs and their linkage with the primary healthcare system ease the health service practitioners, especially HEWs' effort to refer significant amount of women to give birth in health facilities.33 HEWs are required to deliver health information and other health service packages to the community.63 64 These health workers are using the WDA structure as a perfect strategy to share information and create linkage with the community members at the household and individual level.36 By doing so, they could deliver the services effectively. Moreover, this voluntary system is serving as an initiative to reduce delays in maternal health services use.34
Several improvements were seen in the maternal and child health indicators in Ethiopia in the past decade. Even though we cannot hide the contribution of other interventions for the achievements, WDA’s contribution has accelerated the improvements.
Limitations of the review
A potential limitation of the present review might be that a meta-analysis has not been conducted due to the heterogeneous nature of study designs and the population included. Furthermore, we have included only full-text articles found free online.
Conclusions
The results from the review have indicated that the WDA structure has contributed to the improvement of maternal and child health and service use in many ways. Being a member of a WDT and a one-to-five connection under the team has a positive effect on child immunisation service use, minimises maternal mortality, improves BPCR, skilled delivery and skilled ANC, and minimises delays in using maternal health services. Moreover, it was found to be an effective and efficient mechanism to share information to the community as well as to create links between the communities and the primary healthcare system.
Implication for practice
The government is required to continue the existing achievements regarding WDA’s contribution for maternal and child health services utilisation. Again, responsible bodies at each level in the structure of Ethiopian healthcare system have to extend the benefits from WDA to other health issues in addition to maternal and child health.
Periodic measurement and improvement of performance advances the benefit of WDTs to maternal and child health and service use.
Since the distance of the existing WDTs from health facilities is an important determinant of maternal health service utilisation, the government is supposed to establish new health facilities as close as possible to the population and organise the communities living near the health facilities into WDTs. The government should also improve other infrastructure like all weather roads and transportation. Moreover, HEWs and health professionals from health facilities are expected to support and supervise WDTs far away from health facilities.
Implications for research
Although there are some studies regarding WDA, still there is a paucity of literature. Therefore, researchers are responsible to conduct various inquiries on the issue.
Moreover, researchers are supposed to examine the WDA’s contribution to other health issues in addition to maternal and child health service use.
Supplementary Material
Acknowledgments
We would like to thank the Ethiopian Federal Ministry of Health for raising this research question.
Footnotes
Contributors: KY and SM conceived the paper and wrote the protocol for a systematic review. KY and GA conducted the literature search, extracted data, analysed the data, drafted the first version of this paper and finalized the final version. KY, GA and SM have written and revised the manuscript.
Funding: This work was supported by the Alliance for Health Policy and Systems Research/WHO Geneva (Grant Number SRC – Ethiopia 2016/659070-0).
Competing interests: The authors declared that they have no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All relevant data are provided in the paper and supplementary files. Additional details can be provided by the contact author on request.
Patient consent for publication: Not required.
References
- 1. Glenton C, Scheel IB, Pradhan S, et al. . The female community health volunteer programme in Nepal: decision makers' perceptions of volunteerism, payment and other incentives. Soc Sci Med 2010;70:1920–7. 10.1016/j.socscimed.2010.02.034 [DOI] [PubMed] [Google Scholar]
- 2. Hadi A. Management of acute respiratory infections by community health volunteers: experience of Bangladesh Rural Advancement Committee (BRAC). Bull World Health Organ 2003;81:183–9. [PMC free article] [PubMed] [Google Scholar]
- 3. Lewin S, Munabi-Babigumira S, Glenton C, et al. . Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev 2010;3:CD004015 10.1002/14651858.CD004015.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lewin S, Dick J, Pond P, et al. . Lay health workers in primary and community health care. Cochrane Database Syst Rev 2005:004015 10.1002/14651858 [DOI] [PubMed] [Google Scholar]
- 5. Chung MH, Hazmi H, Cheah WL. Role Performance of Community Health Volunteers and Its Associated Factors in Kuching District, Sarawak. J Environ Public Health 2017;2017:1–9. 10.1155/2017/9610928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cueto M. The origins of primary health care and selective primary health care. Am J Public Health 2004;94:1864–74. 10.2105/AJPH.94.11.1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kuule Y, Dobson AE, Woldeyohannes D, et al. . Community Health Volunteers in Primary Healthcare in Rural Uganda: Factors Influencing Performance. Front Public Health 2017;5:1–8. 10.3389/fpubh.2017.00062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Weidert K, Gessessew A, Bell S, et al. . Community Health Workers as Social Marketers of Injectable Contraceptives: A Case Study from Ethiopia. Glob Health Sci Pract 2017;5:44–56. 10.9745/GHSP-D-16-00344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sudhakar M, Woldie M, Yitbarek K, et al. . Primary Care Systems Profiles and Performance (PRIMASYS): Ethiopian Case study. Alliance Heal Policy Syst Res 2017. [Google Scholar]
- 10. Banteyerga H. Ethiopia’s health extension program: improving health through community involvement. MEDICC Rev 2011;13:46–9. 10.1590/S1555-79602011000300011 [DOI] [PubMed] [Google Scholar]
- 11. Wang H, Tesfaye R, Ramana GN V, et al. . Ethiopia Health Extension Program: Publishing and Knowledge Division, The World Bank, 2016. [Google Scholar]
- 12. Betemariam W, Zigene ZD, Fesseha N, et al. . Correlates of the Women’ s Development Army strategy implementation strength with household reproductive, maternal, newborn and child healthcare practices : a cross-sectional study in four regions of Ethiopia. BMC Pregnancy Childbirth 2017;18(373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Selamu M, Asher L, Hanlon C, et al. . Beyond the biomedical: community resources for mental health care in rural Ethiopia. PLoS One 2015;10:e0126666–14. 10.1371/journal.pone.0126666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ethiopian Federal Minstry of Health. Health Sector Transformation Plan (2015/16 - 2019/20). Addis Ababa, Ethiopia, 2015. https://searchworks.stanford.edu/view/11700944. [Google Scholar]
- 15. Betemariam W, Damtew Z, Tesfaye C, et al. . Effect of Ethiopia’s Health Development Army on maternal and newborn health care practices: A multi-level cross-sectional analysis. Ann Glob Health 2017;83:24 10.1016/j.aogh.2017.03.051 [DOI] [Google Scholar]
- 16. Maes K, Closser S, Vorel E, et al. . Using community health workers: Discipline and hierarchy in Ethiopia’s women’s development army Ethiopia’s women’s development army. Ann Anthropol Pract 2015;39:42–57. [Google Scholar]
- 17. Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey, 2016. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf.
- 18. Central Statistical Authority [Ethiopia], ORC Macro. Ethiopia Demogeraphic and Health Survey 2011. 2011. [Google Scholar]
- 19. Central Statistical Authority [Ethiopia], ORC Macro. Ethiopia Demographic and Health Survey 2000, 2000. [Google Scholar]
- 20. Central Statistical Authority [Ethiopia], ORC Macro. Ethiopia Demographic and Health Survey 2005, 2006. [Google Scholar]
- 21. Maes K, Closser S, Vorel E, et al. . A women’s development army: Narratives of community health worker investment and empowerment in rural ethiopia. Stud Comp Int Dev 2015;50:455–78. 10.1007/s12116-015-9197-z [DOI] [Google Scholar]
- 22. George AS, Mehra V, Scott K, et al. . Community participation in health systems research: a systematic review assessing the state of research, the nature of interventions involved and the features of engagement with communities. PLoS One 2015;10:e0141091–25. 10.1371/journal.pone.0141091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. The Joanna Briggs Institute. Checklist for Analytical Cross Sectional Studies, 2017. [Google Scholar]
- 24. The Joanna Briggs Institute. Checklist for Case Control Studies, 2017. [Google Scholar]
- 25. The Joanna Briggs Institute. Checklist for Qualitative Research, 2017. [Google Scholar]
- 26. Madisch I, Hofmayer S, Fickenscher H. Research-Gate authors page. [Google Scholar]
- 27. VON Programs and Services. Principles of Primary Health Care. http://www.von.ca/en/principles-primary-health-care (Accessed 20 Feb 2010).
- 28. Aregawi HG, Gebrehiwot TG, Abebe YG, et al. . Determinants of defaulting from completion of child immunization in Laelay Adiabo District, Tigray Region, Northern Ethiopia: A case-control study. PLoS One 2017;12:e0185533–13. 10.1371/journal.pone.0185533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Godefay H, Byass P, Graham WJ, et al. . Risk Factors for Maternal Mortality in Rural Tigray, Northern Ethiopia: A Case-Control Study. PLoS One 2015;10:e0144975–12. 10.1371/journal.pone.0144975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Negero MG, Mitike YB, Worku AG, et al. . Skilled delivery service utilization and its association with the establishment of Women’s Health Development Army in Yeky district, South West Ethiopia: a multilevel analysis. BMC Res Notes 2018;11:83 10.1186/s13104-018-3140-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Girmaye M, Berhan Y. Skilled antenatal care service utilization and its association with the characteristics of women’s health development team in yeky district, south-west ethiopia: A multilevel analysis. Ethiop J Health Sci 2016;26:369–80. 10.4314/ejhs.v26i4.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Zepre K, Kaba M. Birth preparedness and complication readiness among rural women of reproductive age in Abeshige district, Guraghe zone, SNNPR, Ethiopia. Int J Womens Health 2017;9:11–21. 10.2147/IJWH.S111769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jackson R, Hailemariam A. The role of health extension workers in linking pregnant women with health facilities for delivery in rural and pastoralist areas of ethiopia. Ethiop J Health Sci 2016;26:471 10.4314/ejhs.v26i5.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jackson R, Tesfay FH, Gebrehiwot TG, et al. . Factors that hinder or enable maternal health strategies to reduce delays in rural and pastoralist areas in Ethiopia. Trop Med Int Health 2017;22:148–60. 10.1111/tmi.12818 [DOI] [PubMed] [Google Scholar]
- 35. Jackson R, Tesfay FH, Godefay H, et al. . Health Extension Workers' and Mothers' Attitudes to Maternal Health Service Utilization and Acceptance in Adwa Woreda, Tigray Region, Ethiopia. PLoS One 2016;11:e0150747–15. 10.1371/journal.pone.0150747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kok MC, Kea AZ, Datiko DG, et al. . A qualitative assessment of health extension workers’ relationships with the community and health sector in Ethiopia: opportunities for enhancing maternal health performance. Hum Resour Health 2015;13:1–12. 10.1186/s12960-015-0077-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Federal Democratic Republic of Ethiopia Ministry of Health. Health Sector Development Program III (2005/6-2009/10) . Addis Ababa, Ethiopia 2005. [Google Scholar]
- 38. Federal Democratic Republic of Ethiopia Ministry of Health. Health Sector Development Program IV October 2010 Contents. Addis Ababa, Ethiopia, 2010. [Google Scholar]
- 39. Gopalan SS, Mohanty S, Das A. Assessing community health workers’ performance motivation: a mixed-methods approach on India’s Accredited Social Health Activists (ASHA) programme. BMJ Open 2012;2:e001557–10. 10.1136/bmjopen-2012-001557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Singh D, Negin J, Orach CG, et al. . Supportive supervision for volunteers to deliver reproductive health education: a cluster randomized trial. Reprod Health 2016;13:1–10. 10.1186/s12978-016-0244-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Glenton C, Colvin CJ, Carlsen B, et al. . Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev 2013;2013:326–8. 10.1002/14651858.CD010414.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Panday S, Bissell P, van Teijlingen E, et al. . The contribution of female community health volunteers (FCHVs) to maternity care in Nepal: a qualitative study. BMC Health Serv Res 2017;17:1–11. 10.1186/s12913-017-2567-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. World Health Organization. Community involvement in health development: challenging health services, report of a WHO study group [meeting in Geneva from 11 to 18 December 1989: WHO Tech Rep Ser, 1991:56. [PubMed] [Google Scholar]
- 44. Hitchcock JM. Providing health care: community agency involvement. Bull Am Coll Nurse Midwives 1971;16:12–18. 10.1111/j.1542-2011.1971.tb00056.x [DOI] [PubMed] [Google Scholar]
- 45. Suryadevara M, Bonville CA, Ferraioli F, et al. . Community-centered education improves vaccination rates in children from low-income households. Pediatrics 2013;132:319–25. 10.1542/peds.2012-3927 [DOI] [PubMed] [Google Scholar]
- 46. Kawakatsu Y, Tanaka J, Ogawa K, et al. . Effects of three interventions and determinants of full vaccination among children aged 12-59 months in Nyanza province, Kenya. Public Health 2015;129:1530–8. 10.1016/j.puhe.2015.07.008 [DOI] [PubMed] [Google Scholar]
- 47. Lewin S, Munabi-Babigumira S, Glenton C, et al. . Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev 2010:CD004015 10.1002/14651858.CD004015.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Glenton C, Scheel IB, Lewin S, et al. . Can lay health workers increase the uptake of childhood immunisation? Systematic review and typology. Trop Med Int Health 2011;16:1044–53. 10.1111/j.1365-3156.2011.02813.x [DOI] [PubMed] [Google Scholar]
- 49. Saeterdal I, Lewin S, Austvoll-Dahlgren A, et al. . Interventions aimed at communities to inform and/or educate about early childhood vaccination. Cochrane Database Syst Rev 2014;9 Suppl 1 10.1002/14651858.CD010232.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rai SK, Anand K, Misra P, Upadhyay R, et al. . Public health approach to address maternal mortality. Indian J Public Health 2012;56:196 10.4103/0019-557X.104231 [DOI] [PubMed] [Google Scholar]
- 51. Charanthimath U, Vidler M, Katageri G, et al. . The feasibility of task-sharing the identification, emergency treatment, and referral for women with pre-eclampsia by community health workers in India. Reprod Health 2018;15:77–86. 10.1186/s12978-018-0532-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. World Health Organization/United Nations Childrens Fund. WHO/UNICEF Joint statement: Home visits for the newborn child: a strategy to improve survival: WHO Libr, 2009:1–8. [PubMed] [Google Scholar]
- 53. World Health Organization. WHO Recommendations on Interventions to Improve Preterm Birth Outcomes, 2015. [PubMed] [Google Scholar]
- 54. Keya KT, Rob U, Rahman M, et al. . Distance, transportation cost, and mode of transport in the utilization of facility-based maternity services: evidence from rural Bangladesh. Int Q Community Health Educ 2014;35:37–51. 10.2190/IQ.35.1.d [DOI] [PubMed] [Google Scholar]
- 55. Gage AJ, Guirlène Calixte M. Effects of the physical accessibility of maternal health services on their use in rural Haiti. Popul Stud 2006;60:271–88. 10.1080/00324720600895934 [DOI] [PubMed] [Google Scholar]
- 56. Ebu NI, Gross J. Factors influencing access to antenatal services and delivery care in sub-Saharan Africa. Afr J Midwifery Womens Health 2015;9:58–65. 10.12968/ajmw.2015.9.2.58 [DOI] [Google Scholar]
- 57. Keya KT, Rahman MM, Rob U, et al. . Distance travelled and cost of transport for use of facility-based maternity services in rural Bangladesh: a cross-sectional survey. The Lancet 2013;382:17 10.1016/S0140-6736(13)62178-9 [DOI] [Google Scholar]
- 58. Kawakatsu Y, Sugishita T, Oruenjo K, et al. . Determinants of health facility utilization for childbirth in rural western Kenya: cross-sectional study. BMC Pregnancy Childbirth 2014;14:265 10.1186/1471-2393-14-265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Saprii L, Richards E, Kokho P, et al. . Community health workers in rural India: analysing the opportunities and challenges Accredited Social Health Activists (ASHAs) face in realising their multiple roles. Hum Resour Health 2015;13:1–13. 10.1186/s12960-015-0094-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wilford A, Phakathi S, Haskins L, et al. . Exploring the care provided to mothers and children by community health workers in South Africa: missed opportunities to provide comprehensive care. BMC Public Health 2018;18:1–10. 10.1186/s12889-018-5056-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. O’Donovan J, O’Donovan C, Kuhn I, et al. . Ongoing training of community health workers in low-income andmiddle-income countries: a systematic scoping review of the literature. BMJ Open 2018;8:e021467 10.1136/bmjopen-2017-021467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ballard M, Montgomery P. Systematic review of interventions for improving the performance of community health workers in low-income and middle-income countries. BMJ Open 2017;7:e014216 10.1136/bmjopen-2016-014216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wakabi W. Extension workers drive Ethiopia’s primary health care. Lancet 2008;372:880 10.1016/S0140-6736(08)61381-1 [DOI] [PubMed] [Google Scholar]
- 64. World Health Organization. Global Health Workforce Alliance. Country Case Study: Ethiopia’s human resources for health program. Heal (San Fr) 2008:1–7. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-025937supp001.pdf (181.9KB, pdf)
bmjopen-2018-025937supp002.pdf (92.7KB, pdf)
bmjopen-2018-025937supp003.pdf (85KB, pdf)
bmjopen-2018-025937supp004.pdf (206.8KB, pdf)


