Abstract
The antispasmodic effect of drugs is used for the symptomatic treatment of cramping and discomfort affecting smooth muscles from the gastrointestinal, billiary or genitourinary tract in a variety of clinical situations.The existing synthetic antispasmodic drugs may cause a series of unpleasant side effects, and therefore the discovery of new molecules of natural origin is an important goal for the pharmaceutical industry. This review describes a series of recent studies investigating the antispasmodic effect of essential oils from 39 plant species belonging to 12 families. The pharmacological models used in the studies together with the mechanistic discussions and the chemical composition of the essential oils are also detailed. The data clearly demonstrate the antispasmodic effect of the essential oils from the aromatic plant species studied. Further research is needed in order to ascertain the therapeutic importance of these findings.
Keywords: essential oils, aromatic plants, antispasmodic effect, isolated ileum, monoterpenes
1. Introduction
The antispasmodic (spasmolytic) effect of drugs is commonly used for the reduction of excessive smooth muscle contractility, responsible for cramping and discomfort in the abdominal area, caused by multiple conditions affecting the gastrointestinal, biliary or genitourinary tract [1]. Irritable bowel syndrome (IBS), biliary colic caused by gallstones, gastritis, colitis and pancreatitis or dysmenorrhea may affect large numbers of patients and usually require antispasmodic treatment for the relief of symptoms [1,2,3]. Additionally, antispasmodic compounds are also used for the reduction of discomfort caused by medical procedures like colonoscopy [4]. A variety of synthetic antispasmodic drugs have been authorized worldwide by the regulatory agencies, the most important being anticholinergic agents (butylscopolamine), direct smooth muscle relaxants (papaverine), calcium antagonists (pinaverium) or opioid receptor modulators (trimebutine) [1,2]. Despite their clinical efficacy, the use of these molecules is often limited by the development of unpleasant and sometimes severe side effects which may reduce patient compliance and impair treatment efficiency [1,4]. Historically, a long time before the golden age of medicinal chemistry, several aromatic plants were used in traditional medicine for the treatment of different ailments in some parts of the world. In Europe, aromatic plants like peppermint or thyme have been used for medical purposes since antiquity while in Chinese or Indian traditional medicine other aromatic species like cinnamon or sandalwood were known for centuries [5]. Nowadays, antispasmodic botanical remedies are used by a constantly increasing number of patients for symptomatic treatment of functional dyspepsia, intestinal, colonic or ureteral spasms, gallbladder hyperactivity and uterine cramps [6]. In the large category of medicinal plants, aromatic plants rich in essential oils are considered a valuable and easily accessible natural resource for the development of new molecules capable of becoming drug candidates. Essential oils are complex mixtures containing mainly aromatic terpenes classified in monoterpenes and sesquiterpenes according to the number of isoprene units but also phenylpropanoid compounds. These compounds are secondary metabolites formed by isoprenoid pathways in specialized secretory tissues of aromatic plants and diffused at the surface of their flowers or leaves [7]. The biological effects of essential oils have been extensively researched, as they can easily pass through cellular membranes and influence a variety of molecular targets from ion channels to intracellular enzymes [8]. Multiple in vitro and in vivo studies have confirmed the anti-oxidant, antimicrobial, antifungal, antiparasitary, anti-inflammatory, antinociceptive or antitumoral effects of essential oils [7], but the antispasmodic effect has been less studied experimentally, despite being mentioned in traditional medicine sources. Hence, this review was aimed at the investigation of the antispasmodic effect of essential oils, presenting the experimental models used for pharmacological testing with the subsequent mechanistic explanations, but also the chemical composition of the studied essential oils.
2. Methodology
A search was performed in Web of Science, PubMed and Scopus scientific databases, including the last 20 years (1998–2018). The search terms “essential oils” and “antispasmodic” (“spasmolytic”) were used for data selection. Only articles in English were included in this work. Our study investigated the antispasmodic effect of the essential oils and was not focused on the bronchodilator and vasodilator effects, presented by other reviews.
3. Results and Discussion
3.1. Preclinical Studies Investigating Antispasmodic Effect of Essential Oils
This review showed that essential oils from thirty-nine plant species belonging to twelve families presented antispasmodic properties demonstrated by specific animal models. The plants were organized alphabetically by family and botanical name, the proposed antispasmodic mechanism being also presented, where available. The families with the highest proportion of plant species showing antispasmodic effects due to essential oils (EO) were Lamiaceae (13 species), Apiaceae (6 species), and Asteraceae (5 species). Other identified families were Annonaceae and Poaceae (3 species), Rutaceae and Verbenaceae (2 species) while Anacardiaceae, Araceae, Geraniaceae, Rosaceae and Zingiberaceae families each presented only one plant species with antispasmodic essential oil (Table 1).
Table 1.
Plant species containing essential oils with antispasmodic activity demonstrated in preclinical studies.
| No. | Plant Species with Essential Oils | Experimental Model/Concentration of EO in Organ Bath | Mechanism of Antispasmodic Effect | Reference |
|---|---|---|---|---|
| Anacardiaceae | ||||
| 1. | Pistacia integerrima—zebrawood | Isolated guinea pig ileum/50 μg/mL | Inhibition of Ca2+ channels | Shirole et al., 2015 [9] |
| Annonaceae | ||||
| 2. | Cananga odorata var. genuina—ylang ylang | Isolated rat bladder/0.05 mL/20 mL; white rabbit bladder in vivo/0.01–0.05 mL/rabbit ∗ | Increase of cAMP | Kim et al., 2003 [10] |
| 3. | Xylopia frutescens | Isolated guinea pig ileum/3–729 μg/mL | Inhibition of Ca2+channels; antagonism of histaminergic receptors | Souza et al., 2015 [11] |
| 4. | Xylopia langsdorffiana | Isolated guinea pig ileum; isolated rat uterus/243–729 μg/mL | Decrease in cytosolic calcium concentration | Correia et al., 2015 [12] |
| Apiaceae | ||||
| 5. | Anethum graveolens—dill | Isolated rat ileum/0.5–2 mg/mL | Inhibition of Ca2+ channels | Gharib Naseri et al., 2007 [13] |
| 6. | Carum carvi—caraway | Isolated guinea pig ileum/2.20–6.63 mg/mL; Dispersed smooth muscle cells of guinea pigs/2.5 mg/mL |
Not available | Heinle et al., 2006 [14]; Al-Essa et al., 2010 [15] |
| 7. | Coriandrum sativum—coriander | Isolated rabbit jejunum/ 1–30 mg/mL |
Inhibition of Ca2+ channels | Jabeen at al., 2009 [16] |
| 8. | Ferula heuffelii Griseb. | Isolated rat ileum/ 75–250 μg/mL |
Not available | Pavlovic et al., 2012 [17] |
| 9. | Foeniculum vulgare—fennel | Isolated rat uterus/10–40 mg/mL | Not available | Ostad et al., 2001 [18] |
| 10. | Pimpinella anisum—aniseed | Isolated rat anococcygeus muscle/5–50 μg/mL | Activation of NO-cGMP pathway | Tirapelli et al., 2007 [19] |
| Araceae | ||||
| 11. | Acorus calamus—sweet flag, calamus | Isolated rabbit jejunum/ 0.3–1 mg/mL |
Inhibition of Ca2+ channels | Gilani et al., 2006 [20] |
| Asteraceae | ||||
| 12. | Artemisia dracunculus—tarragon | Isolated sheep ruminal and abomasal smooth muscles/0.1–100 μg/mL | Not available | Jalilzadeh-Amin et al., 2012 [21] |
| 13. | Chamaemelum nobile—roman chamomile | Isolated guinea pig ileum/60 μg/mL | Direct smooth muscle relaxation | Sandor et al., 2018 [22] |
| 14. | Chrysactinia mexicana—damianita daisy | Isolated rabbit ileum/30 μg/mL | Inhibition of Ca2+ channels; increase of cAMP | Zavala-Mendoza et al., 2016 [23] |
| 15. | Hofmeisteria schaffneri | Gastrointestinal transit test in mouse (in vivo)/316 mg/kg ∗ | Not available | Perez-Vasquez et al., 2017 [24] |
| 16. | Matricaria recutita (chamomila)—German chamomile | Isolated rabbit jejunum/0.3–3 mg/mL | K+ channels activation | Mehmood et al., 2015 [25] |
| Geraniaceae | ||||
| 17. | Pelargonium graveolens—geranium | Isolated guinea pig ileum/ 4.8–6 μg/mL | Reduction of calcium flux into the intestinal smooth muscles | Lis-Balchin et al., 1997 [26] |
| Lamiaceae | ||||
| 18. | Lavandula angustifolia—true lavender | Isolated guinea pig ileum, isolated rat uterus/6 μg/mL | Increase of cAMP | Lis-Balchin and Hart, 1999 [27] |
| 19. | Melissa officinalis—melissa | Isolated rat ileum/20 μg/mL; isolated mouse jejunum/1–50 mg/mL | Inhibition of Ca2+ channels; Not available | Sadraei et al., 2003 [28]; Aubert et al., 2016 [29] |
| 20. | Mentha x piperita—peppermint | Isolated guinea pig ileum; isolated rat ileum/10–320 μL/mL | Inhibition of Ca2+ channels; Inhibition of 5HT3 receptor channels | Grigoleit et al., 2005 [30]; Heimes et al., 2011 [31] |
| 21. | Mentha spicata—spearmint | Isolated guinea pig ileum/0.1 nM–10 μM | Inhibition of Ca2+channels | Souza et al., 2013 [32] |
| 22. | Mentha x villosa—mojito mint | Isolated guinea pig ileum/0.9 μM–2.5 μM | Not available | De Sousa et al., 2008 [33] |
| 23. | Ocimum basilicum—basil | Isolated guinea pig ileum/3–10 mg/mL | Inhibition of Ca2+ channels | Janbaz et al., 2014 [34] |
| 24. | Ocimum selloi—green pepperbasil | Isolated guinea pig ileum/250 μg/mL–1 mg/mL | Inhibition of Ca2+ channels | Souza et al., 2015 [35] |
| 25. | Ocimum gratissimum—African basil | Isolated guinea pig ileum/0.1–1000 μg/mL | Not available | Madeira et al., 2002 [36] |
| 26. | Origanum majorana—sweet marjoram | Isolated rabbit jejunum, isolated rat jejunum/0.01–0.3 mg/mL | Inhibition of Ca2+ channels | Makrane et al., 2018 [37] |
| 27. | Plectranthus barbatus synonym Coleus forskohlii—Indian coleus | Isolated guinea pig ileum/1–300 μg/mL | Direct smooth muscle relaxation | Camara et al., 2003 [38] |
| 28. | Rosmarinus officinalis —rosemary | Isolated guinea pig ileum/150–1200 μg/mL | Inhibition of Ca2+ channels | Ventura-Martinez et al., 2011 [39] |
| 29. | Salvia officinalis—sage | Isolated rabbit jejunum/0.1–3 mg/mL | K+ channels activation | Khan et al., 2011 [40] |
| 30. | Satureja hortensis—summer savory | Isolated rat ileum/1.55 μg/mL | Not available | Hajhashemi et al., 2000 [41] |
| Poaceae | ||||
| 31. | Cymbopogon citratus—lemongrass | Isolated rabbit ileum/0.001–1 mg/mL | Inhibition of Ca2+ channels | Devi et al., 2011 [42] |
| 32. | Cymbopogon schoenantus (L.) Spreng.—camelgrass | Isolated rat ileum/30–120 μg/mL | Not available | Pavlovic et al., 2017 [43] |
| 33. | Cymbopogon martinii —palmarosa | Isolated rabbit jejunum/0.01–3 mg/mL | Inhibition of Ca2+ channels | Janbaz et al., 2014 [44] |
| Rosaceae | ||||
| 34. | Rosa indica (L.) | Isolated rabbit jejunum/0.01–1 mg/mL | Inhibition of Ca2+ channels | Rasheed et al., 2015 [45] |
| Rutaceae | ||||
| 35. | Citrus aurantifolia var. acida—lime | Isolated rabbit jejunum/Not available | Not available | Spadaro et al., 2012 [46] |
| 36. | Citrus aurantium var. sinensis—sweet orange | Isolated rat ileum/9.7–1000 μg/mL | Not available | Sanchez-Recillas et al., 2017 [47] |
| Verbenaceae | ||||
| 37. | Lippia alba | Isolated rat ileum/7–37 mg/mL | Reduction of calcium influx, stimulation of NO production | Blanco et al., 2013 [48] |
| 38. | Lippia thymoides | Isolated guinea pig ileum/11.56–48.83 μg/mL | Not available | Menezes et al., 2018 [49] |
| Zingiberaceae | ||||
| 39. | Elettaria cardamomum—cardamom | Isolated rabbit jejunum/3–10 mg/mL | Inhibition of Ca2+ channels | Gilani et al., 2008 [50] |
∗ For the in vivo experimental models dose of essentials oils (EO) was expressed in mL/animal or mg/kg.
The majority of the presented preclinical studies used whole essential oils, the antispasmodic effect of individual chemical constituents of essential oils being rarely investigated. Sadraei et al. [28] demonstrated antispasmodic effects not only for the essential oil from Melissa officinalis but also for citral, one of its main components. Heimes et al. [31] investigated the spasmolytic effects of menthol, a major constituent in the essential oil from Mentha x piperita. De Souza et al. [33] tested the antispasmodic effect of several monoterpenes from Mentha x villosa essential oil, carvone and rotundifolone being the most active compounds.
While several studies confirmed the antispasmodic effect of essential oils extracted from common vegetal species extensively used in Asia or Europe like Cananga odorata [10], Foeniculum vulgare [18] or Artemisia dracunculus [21], other studies showed significant spasmolytic effects of essential oils from less-known plant species like Xylopia langsdorffiana [12], Ferula heuffelii [17] or Hofmeisteria schaffneri [24], proving that new natural sources of bioactive molecules are constantly being discovered.
The collected data from this review confirmed other studies investigating biological effects of essential oils. Martinez-Perez et al. [51] showed that monoterpenes frequently found in essential oils are the leading class of natural molecules responsible for the antispasmodic effect, followed by flavonoids and alkaloids. De Almeida et al. [52] and Sarmento-Neto et al. [53] also showed in their studies that aromatic plants from the Lamiaceae, Apiaceae and Asteraceae families are a rich source of essential oils, highly valuable for medicinal or industrial purposes.
Also, analysis of the included studies showed that, generally, the experimental models used for the assesement of essential oil antispasmodic activity were represented by ex vivo techniques. Among these, the isolated guinea pig ileum method was preferred, being considered a precise pharmacological tool capable of investigating the antispasmodic effect of natural or synthetic compounds [54]. Other isolated organs used for the evaluation of antispasmodic effect were rabbit jejunum, rat ileum, bladder or uterus and sheep ruminal and abomasal muscles. An experimental model used in vitro cell cultures [15] and only two experiments used in vivo techniques: rabbit bladder in vivo and gastrointestinal transit test in mouse [10,24]. The ex vivo techniques are predominant due to their use without the limitations of drug bioavailability which may be a problematic issue for the in vivo models. Ex vivo methods are also well suited for mechanistic studies due to the diversity of contractile agents which could be used experimentally [55].
3.2. Clinical Studies Evaluating Antispasmodic Potential of Essential Oils
Antispasmodic effect of essential oils was investigated in several clinical studies for different situations: functional dyspepsia, irritable bowel syndrome, discomfort produced by endoscopic procedures, infantile colic or dysmenorrhea (Table 2).
Table 2.
Clinical studies evaluating antispasmodic potential of essential oils.
| Area of Interest | Authors | Type of Clinical Study | Number of Patients | Treatment | Results |
|---|---|---|---|---|---|
| Functional dyspepsia | Papathanasopoulos et al., 2013 [56] | Randomized, crossover study | 13 healthy volunteers | Peppermint oil 182 mg p.o., single dose | Decreased intragastric pressure and gastric motility |
| Functional dyspepsia | Inamori et al., 2007 [57] | Randomized control study | 10 healthy volunteers | Peppermint oil 0.64 mL p.o., single dose | Enhancement of gastric emptying without altering gastric emptying coefficient |
| Functional dyspepsia | May et al., 2000 [58] | Randomized control study | 96 patients with functional dyspepsia | Peppermint oil and caraway oil combination 90 mg + 50 mg p.o., 4 weeks | Reduction of symptoms (pain, fulness, heaviness) |
| Functional dyspepsia | Madisch et al., 1999 [59] | Randomized control study | 118 patients with functional dyspepsia | Peppermint oil and caraway oil combination 90 mg + 50 mg p.o., 4 weeks | Reduction of dyspeptic symptoms |
| Irritable bowel syndrome (IBS) | Cash et al., 2016 [60] | Randomized control study | 72 patients with IBS | Peppermint oil 180 mg p.o., 4 weeks | Reduction of symptoms |
| IBS | Khanna et al., 2014 [61] | Meta-analysis | 9 studies with 726 patients with IBS | Peppermint oil 200 mg | Global improvement of IBS symptoms (RR 2.23, 95% CI 1.78–2.81) |
| IBS | Merat et al., 2010 [62] | Randomized control study | 90 patients with IBS | Peppermint oil 187 mg p.o., 8 weeks | Reduction of abdominal pain and discomfort |
| IBS | Cappello et al., 2007 [63] | Randomized control study | 57 patients with IBS | Peppermint oil 225 mg p.o., 4 weeks |
Reduction of total IBS symptoms |
| IBS | Pittler and Ernst 1998 [64] | Meta-analysis | 8 randomized control studies | Peppermint oil | Reduction of IBS symptoms not established beyond reasonable doubt |
| IBS | Liu et al., 1997 [65] | Randomized control study | 110 patients with IBS | Peppermint oil 187 mg p.o., 4 weeks | Improvement of pain and other IBS symptoms |
| Endoscopic procedures | Inoue et al., 2014 [66] | Randomized control study | 226 patients with colonoscopy | L-menthol applied on the mucosa | Reduction of discomfort |
| Endoscopic procedures | Hiki et al., 2012 [67] | Randomized control study | 131 patients with gastric endoscopy | L-menthol applied on the mucosa | Reduction of peristalsis |
| Endoscopic procedures | Yamamoto et al., 2006 [68] | Randomized, control study | 40 patients with endoscopic cholangiopancreatography | Peppermint oil applied to papilla | Non-significant reduction of duodenal contractions |
| Infantile colic | Bezerra Alves et al., 2012 [69] | Randomized crossover study | 30 infants | Mentha piperita liquid drops, 1 drop/kg | Decreased frequency and duration of infantile colic |
| Primary dysmenorrhea | Ghodsi and Asltoghiri, 2014 [70] | Randomized control study | 80 female students | Fennel capsules 180 mg/day, 3 months | Reduction of dysmenorrhea symptoms |
The analysis of data resulted from the presented clinical studies show that peppermint oil was the predominant essential oil used for symptomatic treatment of various conditions, the strongest evidence being available for irritable bowel syndrome (IBS). The randomized controlled studies of Cash et al. [60], Merat et al. [62] and Capello et al. [63] enrolled patients with IBS diagnosed according to Rome II or III criteria, showing that peppermint oil was superior to placebo in reducing the symptom score of irritable bowel syndrome (IBS) after oral administration for one or two months. According to other studies [58,59], peppermint and caraway essential oils are a possible treatment option for patients with functional dyspepsia, reducing epigastric discomfort and abdominal bloating over four weeks of treatment. Also, L-menthol and peppermint oil were tested for the reduction of discomfort caused by endoscopic procedures being used with good results in upper GI endoscopies, colonoscopies [66,67] but also in cholangiopancreatographies [68]. The study of Bezerra Alves et al. [69] found that Mentha piperita essential oil reduced the frequency of infantile colic. In addition, Ghodsi and Asltoghiri [70] found that fennel essential oil reduced primary dysmenorrhea symptoms after a prolonged oral administration [70].
The systematic reviews of Chumpitazi et al. [71] and Shams et al. [72] pointed out that peppermint oil was safe and well-tolerated by the patients, with a minimal side effect profile. Nevertheless, clinical studies evaluating the antispasmodic potential of essential oils have some limitations. They were represented mainly by randomized crossover or control studies using small numbers of patients with an insufficient statistical significance. Only the studies of Khanna et al. [61] and Pittler and Ernst [64] were metaanalysis with superior statistical power. Therefore, additional clinical studies are necessary to ascertain the therapeutic value of antispasmodic essential oils.
3.3. Mechanisms of Antispasmodic Effect of Essential Oils and Their Constituents
Smooth muscles are a key element present in the internal structure of multiple abdominal organs including stomach, intestine, bladder or uterus, receiving innervation from the autonomic nervous system but also autocrine or paracrine stimuli [73]. Recently, considerable progress was made to understand in great molecular detail the complex physiology of smooth muscle contraction. Excitation-contraction coupling occurs when Ca2+ ions enter from the extracellular side into the smooth muscle cells through sarcolemma voltage-dependent calcium channels, being also released from intracellular stores via inositol 1,4,5-triphosphate receptor (IP3R) situated on endoplasmic reticulum (ER) [74]. The calcium release from ER is triggered by the binding of agonists like acetylcholine or histamine on specific G-protein coupled receptors (GPCRs) from the membrane of smooth muscle cells, which activate phospholipase-C (PLC) to generate IP3. After the intracellular concentration of calcium has increased, Ca2+ ions bind to calmodulin (CaM) and phosphorylate the myosin light-chain kinase (MLCK) with the subsequent activation of the contractile apparatus [75].
Thus, the identification and characterization of multiple molecular targets involved in smooth muscle contraction has led to the development of a variety of drugs able to reduce excessive contractility responsible for cramps and colics of the abdominal organs. Among potential new drug candidates, essential oils have become increasingly attractive due to their complex chemical composition and multiple pharmacological mechanisms: inhibition of voltage-dependent calcium channels, modulation of potassium channels, antagonism of cholinergic receptors, and modulation of intracellular cyclic adenosine monophosphate (cAMP) (Figure 1). Although some details of the antispasmodic effect of essential oils and their constituents have been explained, further research is needed to better understand their mechanism of action at cellular and molecular levels.
Figure 1.
Main mechanisms of antispasmodic effect of essential oils: a. inhibition of voltage-dependent calcium channels; b. modulation of potassium channels; c. modulation of intracellular cAMP (EO—essential oil, VDCC—voltage-dependent calcium channel; KC—potasium channel, GPCR—G-protein coupled receptors, CaM—calmoduline, PLC—phospholipase C, AC—adenylyl cyclase, MLCK—myosin-light chain kinase, MLCP—myosin-light chain phosphatase, ER—endoplasmic reticulum, cGMP—cyclic guanosine monophosphate, cAMP—cyclic adenosine monophosphate, NO—nitric oxide).
3.3.1. Inhibition of Voltage-Dependent Calcium Channels
The opening of voltage-dependent calcium channels (VDCCs) is directly responsible for Ca2+ influx into the smooth muscle cells, partially triggering the contractile mechanism. Thus, inhibition of VDCCs has a good potential of relaxing smooth muscles, already used by several antispasmodic drugs like pinaverium [76]. Essential oils have been studied for their antispasmodic effect, the inhibitory effect on voltage-dependent calcium channels being the most commonly reported mechanism of action in the studies mentioned in our review (19 studies from 39). Some of these studies presented detailed mechanistic explanations of the antispasmodic effect for the non-fractioned essential oils. Makrane et al. [37] showed that organic fractions rich in essential oils from Origanum majorana showed a consistent spasmolytic effect on isolated rat and rabbit ileum not altered by atropine, L-NAME or methylene blue, and shifted to the right the concentrations-response curves for CaCl2, suggesting a calcium channel blocking effect. Rasheed et al. [45] showed in an experiment on isolated rabbit jejunum that essential oil from Rosa indica relaxed the organ, shifting the calcium curves to the right, showing a similar effect to verapamil, a phenylalkylamine derivative from the calcium channel blocker class. The study of Souza et al. [35] identified the same mechanism for the essential oil from Ocimum selloi which reduced the contraction of isolated guinea pig ileum induced by carbachol, BaCl2 and K+ and shifted calcium concentration-response curves to the right.
Other studies were focused on the individual components of the essential oils. Amato et al. showed that menthol (0.1 mM–30 mM) reduced in a concentration-dependent manner the contractility of human colon circular muscle, acting by an antagonistic effect on L-type Ca2+ channels [77]. The study of Ramos-Filho et al. [78] showed that menthol markedly inhibited contractions of wild and TRPM8 knockout mice bladder strips evoked by carbachol, CaCl2 or electric field stimulation. The effects of menthol were not influenced by previous incubation with sodium or potassium channel inhibitors or by the removal of urothelium, suggesting a blockade of calcium channels. Electrophysiological studies have shown that menthol was able to inhibit the calcium influx through the low-voltage activated Ca2+ channels but also to enhance the inactivation of high-voltage activated Ca2+ channels [79]. Another monoterpene, (-)-carvone was tested by Souza et al. [32] on guinea pig ileum in order to ascertain the mechanism of its spasmolytic effect, proving to be almost 100 times more potent than verapamil, a well-known calcium channel blocker (CCB) with a similar mode of action.Devi et al. [42] studied the antispasmodic effect of another terpene, citral, the major component of Cymbopogon citratus essential oil on rabbit ileum, the results showing a marked reduction of contractions evoked by CaCl2, similarly to verapamil.
3.3.2. Modulation of Potassium Channels
Potassium channels are largely distributed in human and animal tissues, having important physiological roles such as the regulation of smooth muscle tone [80]. Generally, the activation of voltage-gated potassium channels induces a hyperpolarisation of cell membrane with a subsequent de-activation of calcium channels leading to smooth muscle relaxation. Only a few studies investigated the effect of essential oils on potassium channels situated on smooth muscles of internal organs. Mehmood et al. [25] showed that a crude extract from Matricaria chamomilla L. containing sesquiterpenes (bisabolol) and flavonoids produced a significant antispasmodic effect on isolated rabbit jejunum. The effect on low K+ induced contractions was completely blocked by 4-aminopyridine, suggesting that the activation of potassium channels was responsible for smooth muscle relaxation. Khan et al. [40] showed that a crude extract from Salvia officinalis rich in essential oils (thujone, 1,8-cineole, camphor, linalool) caused a dose-dependent relaxation of isolated rabbit jejunum by an activation of K+ channels.
Silva et al. [81] investigated the mechanism of smooth muscle relaxation of rotundifolone, the major constituent of Mentha x villosa essential oil. Patch-clamp recordings made in mesenteric smooth muscle cells showed that rotundifolone significantly increased K+ currents, effect blocked by charybdotoxin which suggested the participation of big potassium (BK) channels.
3.3.3. Antagonism of Cholinergic Receptors
The parasympathetic nervous system has an important role in the regulation of gastrointestinal motility. Muscarinic receptors located directly on smooth muscle cells can trigger their contraction in response to acetylcholine, but nicotinic receptors have also been identified on the nerve cells from the enteric nervous system. Research on the effect of essential oils on cholinergic receptors from smooth muscles is extremely rare, only a few studies being published to date. Amato et al. [82] found that menthol induced relaxation of isolated mouse stomach by inhibiting nicotinic receptors from the enteric nervous system, reducing the release of acetylcholine from enteric nerves. The study of Lozon et al. [83] investigated the effects of vanilin, pulegone, eugenole, carvone, carvacrol, carveol, thymol, thymoquinone, menthone, and limonene on human nicotinic cholinergic receptors expressed in Xenopus oocytes. Carveol showed the most potent inhibition at the α 7 subunit of the nicotinic receptor. The molecular interactions between terpenic compounds from essential oils and nicotinic cholinergic receptors were investigated by electrophysiological studies which showed that menthol caused a shortening of channel open time and a prolongation of channel closed time of human α4β2 nicotinic receptors [83].
3.3.4. Modulation of Intracellular Cyclic Adenosine Monophosphate (cAMP)
The main intracellular second messengers cAMP and cGMP are directly involved in smooth muscle relaxation. cAMP is generated by adenylyl cyclase mainly as a result of beta-adrenergic receptor activation. cGMP is produced by soluble guanylyl cyclase activated by nitric oxide or other mediators. Both cAMP and cGMP activate protein kinases PKA and PKG which may relax smooth muscles either by increasing the expulsion of calcium from the cell or by activation of MLC phosphatase which inhibits MLCK. The levels of cAMP and cGMP are severely reduced by the intervention of phosphodiesterases (PDE) involved in their degradation to inactive metabolites [73]. Multiple studies have investigated the effects of essential oils on the intracellular mechanisms of smooth muscle relaxation. In a study from 2018, Sandor et al. [22] studied the effects of the essential oil and extract from Chamaemelum nobile L. (roman chamomile) on isolated guinea pig ileum and rat gastrointestinal preparations. The essential oil significantly relaxed the isolated organs contracted with histamine, without any influence of a pretreatment with atropine, tetrodotoxin, propranolol or NG–nitro-L-arginine, thus suggesting an intracellular mechanism of the antispasmodic effect. Zavala-Mendoza et al. [23] investigated the antispasmodic mechanism of the essential oil from Chrysactinia mexicana on isolated rabbit ileum. The effect was reduced by the preincubation with dibutyryl-cAMP but increased by forskolin, whereas chelerytrine or L-NNA did not modify the response, suggesting an involvement of cAMP in the antispasmodic mechanism of the essential oil. The study of Kim et al. [10] showed that essential oil from Cananga odorata (ylang-ylang) relaxed the isolated rat bladder muscle, the effect being reduced by N-ethylmaleimide but not by inhibitors of NO pathway, demonstrating the involvement of cAMP. Also, Lis-Balchin and Hart [27] found that essential oil from Lavandula angustifolia induced relaxation of isolated guinea-pig ileum through a rise in intracellular level of cAMP The effects of individual components from essential oils on intracelullar mechanism of antispasmodic effect were less studied. Leal-Cardoso et al. [84] found that eugenol (1–2000 microM) relaxed the isolated rat ileum precontracted with KCl, without any influence from tetrodotoxin, L-NAME, hexamethonium or indomethacin, thus suggesting an intracellular mechanism.
3.4. Chemical Composition of the Essential Oils with Antispasmodic Activity
Essential oils are complex mixtures of volatile compounds with terpenoid or non-terpenoid structure that can be extracted from different parts of plants (flower, buds, seed, leaves, and fruits). Many of those compounds have been identified in essential oils and clasiffied as functionalized derivatives of alcohols, ketones or aldehydes, esters, ethers, oxydes and phenols [85,86]. The composition of an essential oil may vary according to the plant’s environment and growing conditions, stage of development, methods of harvesting, extraction, and storage. The major constituents of an essential oil can also vary according to different chemotypes of the same plant species [85]. Although there is a tendency to correlate pharmacological properties with the presence of certain functional groups, this concept cannot be generalized. Thus, neurotoxicity cannot be reported for all ketones, even if it was reported in the case of thujone [86,87], as not all the alcohols have a sedative action, even if it was described for l-linalool [86,88,89].
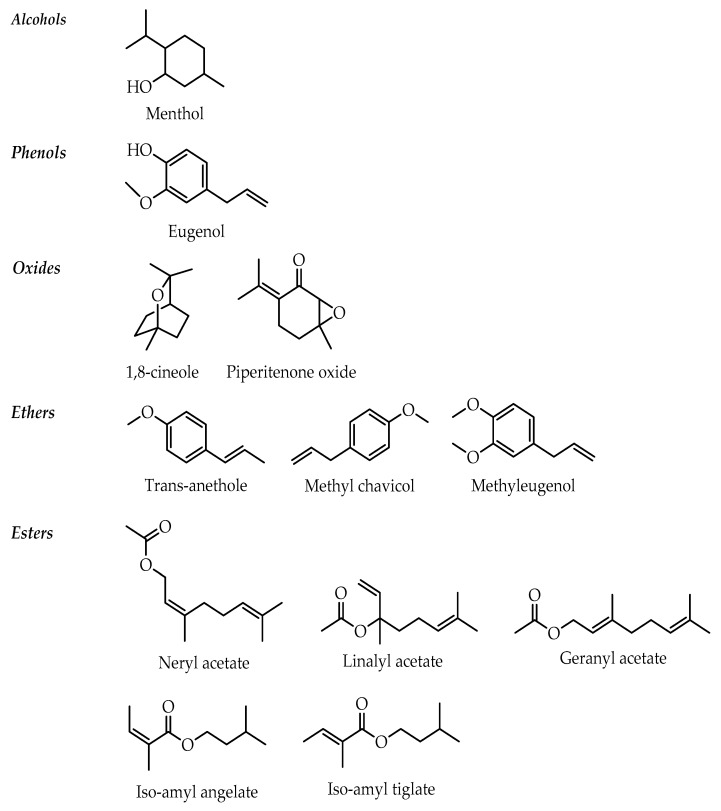
Several molecules with a structure clearly linked to the antispasmodic effect have been identified by our review. According to the surveyed literature, they are classified as alcohols (menthol), phenols (eugenol) [84], esters (linalyl acetate, neryl acetate, geranyl acetate, iso-amyl angelate and tiglate), ethers (trans-anethole, methyl chavicol or estragole, methyleugenol) [90], oxides (1,8-cineole, piperitenone oxide) [86,91,92] (Figure 2). However, other constituents present in low concentrations could be important for the pharmacological activity.
Figure 2.
Chemical structures of main constituents from antispasmodic essential oils.
Chemical composition of the antispasmodic essential oils included in our study is presented in Table 3.
Table 3.
Chemical composition of the studied antispasmodic essential oils.
| Plant Species | Part Use | Representative Compounds | Reference |
|---|---|---|---|
| Pistacia integerrima, (Anacardiaceae)-zebrawood | Galls | Hydrocarbons: monoterpenes: α-pinene 21.81%, β-pinene 16.18, α-terpinene 1.37%, carene 11.09%, limonene 6.35%, α-phellandrene 15.48%, β-phellandrene 5.72%, cis-ß-ocimene 4.13%, trans-ß-ocimene 4.25%; sesquiterpenes: β-caryophyllene 3.88–5.33%, β-farnesene 7.88%; aromatic: p-cymene 11.54% Alcohols: terpinen-4-ol 11.93–28.82%, 4-carvomenthenol 17.06%, p-meth-1-en-8-ol 43.38%, borneol 8.90%, spathulenol 6.35% Ketones: tetrahydrocarvone 10.27% Esters: bornyl acetate 13.99% |
[93,94,95] |
| Cananga odorata var. genuina, (Annonaceae)—ylang ylang | Flowers | Major components differ significantly depending on the fraction of essential oil, origin of the plant material and harvesting time Hydrocarbons: sesquiterpenes: ß-caryophyllene 15–26.8%, germacrene D 8.1–25.13%, δ-cadinene 2–4.7%, α-humulene 0.9–7.1%, α-farnesene 0.3–23.75% Alcohols: linalool 8.7–30%, farnesol 5.6% Ethers: p-methyl anisole 0.39–16.5% Esters: geranyl acetate 5–10%, farnesyl acetate 1–7%, methyl salicylate 1–10%, benzyl benzoate 3.8–27.48%, benzyl acetate 3–8%, methyl benzoate 1–6.05% |
[86,96,97,98,99] |
| Xylopia frutescens, (Annonaceae) | Leaves | Hydrocarbons:monoterpenes: α-pinene 2.30%,β-ocimene 8.19%; sesquiterpenes: caryophyllene 23.91%, γ-cadinene 12.48%, γ-elemene 4.55%, β-elemene 4.31%, α-selinene 4.29%, δ-cadinene 3.02%, α-humulene 2.48%, γ-muurolene 2.23%, β-selinene 2.11% Alcohols: cadin-4-en-10-ol 5.78%, viridiflorol 4.83%, sphatulenol 3.97% |
[11] |
| Xylopia langsdorfiana, (Annonaceae) | Fruits | Hydrocarbons:monoterpenes: α-pinene 37.73%, camphene 11.50%, β-pinene 4.04%, limonene 31.75%; sesquiterpenes: sclarene 10.38% Alcohols: α-terpineol 1.08%, spathulenol 1.74% Oxides: 1,8-cineol 1.15%, caryophyllene oxide 3.79% |
[100] |
| Anethum graveolens, (Apiaceae)—dill | Seeds | Hydrocarbons: monoterpenes: limonene 1.11–83%, α-phellandrene trace–25%, β-phellandrene 0–3.38% Phenols: carveol 2%, eugenol Ketones: carvone (28–62.48%), cis-dihydrocarvone 0–5.87%, trans-dihydrocarvone 0–11.7%, piperitone 0–8.2% Ethers: apiole 0–16.79%, dillapiole 0–26.8 |
[86,101,102,103,104,105,106,107,108] |
| Carum carvi, (Apiaceae)—caraway | Fruits | Hydrocarbons: monoterpenes: limonene 1.5–51.3%, carvene 30% Alcohols: cis-carveol 5.5% Ketones: carvone 44.5–95.9% Ethers: trans-anethole 0–2.2%, apiole 12.3% |
[86,109,110,111] |
| Coriandrum sativum, (Apiaceae)—coriander | Fruits | Hydrocarbons: monoterpenes: γ-terpinene 1–8%, limonene 0.1–4%, α-pinene 0–10.9%, ß-myrcene 0.2–2%; aromatic p-cymene trace–8.1% Alcohols: linalool 60–87%, geraniol 1.2–3.6%, terpinen-4-ol trace–3% Ketones: camphor 0.9–5.3% Esters: geranyl acetate 0.1–5.4%,linalyl acetate 0–2.7% |
[86,89,112,113] |
| Ferula heuffelii Griseb., (Apiaceae) | Hydrocarbons: monoterpenes: α-pinene 4%, γ-terpinene 1.2%; sesquiterpenes: α-cadinene 3.4%, aromadendrene 1.8%, viridiflorene 2.1%, α-muurolene 1.7% Alcohols: viridoflorol 1.0%, cedrol 5.1% Ethers: myristicin 20.6%, elemicin 35.4% Esters: bornyl acetate 1.9% |
[17] | |
| Foeniculum vulgare var. dulce, (Apiaceae)—sweet fennel | Fruits | Hydrocarbons: monoterpenes α-pinene 0.4–10%, limonene 1.4–26.44%, α-phellandrene 0.2–9.26%, ß-myrcene 0.5–3%, ß-phellandrene 0.4–2.6%, γ-terpinene 10.5%, cis-ß ocimene 1.6–12%, α-terpinolene trace–3.3%; aromatic: p-cymene 0.1–4.7% Alcohols: fenchol trace–4% Ketones: fenchone trace–22% Ethers: methyl chavicol trace–17%, cis-anethole trace–1.7%, trans-anethole 50–90% Oxides: 1,8-cineole 1–6% |
[86,114,115,116,117,118] |
| Pimpinella anisum, (Apiaceae) - aniseed | Fruits | Hydrocarbons: sesquiterpenes: γ-himachalene 0.4–8.2% Alcohols: anisol 0.5–4% Ethers: cis-anethole 0–1%, trans-anethole 90–93.7%, methyl chavicol 0–2.3% Aldehydes: anisaldehyde 0–5.4% |
[86,119,120,121] |
| Acorus calamus, (Araceae)—sweet flag, calamus | Rhizomes | Hydrocarbons: monoterpenes: α-pinene 2.96%, limonene 0.1–2.8%; sesquiterpenes: ß-gurjunene 0.2–28.0%, calamenene 0.1–9.75%, δ-cadinene 0.5–2.1%, α-cedrene 3.09% Alcohols: linalool 0.3–12% Phenols: cis-isoeugenol 2.5–25%, trans-isoeugenol 0.5–2% Aldehydes: asaronal 0.2–6%, citronellal 2.82%, neral 2.57% Ketones: shyobunone trace–13.3%, epishyobunone 0.1–4.8%, isoshyobunone 0.6–13.0%, camphor 2.42% Ethers: methyl eugenol trace–8.59%, cis-methyl isoeugenol 2.4–49%, trans-methyl isoeugenol 1.1–7.9%, α-asarone 1–50.09%, ß-asarone 2.22–83.2% |
[86,122,123,124,125,126] |
| Artemisia dracunculus, (Asteraceae)—tarragon | Flowering tops and leaves | Major components differ significantly depending on the origin of the plant material and harvesting time Hydrocarbons: monoterpenes: α-pinene 5.1%, limonene 2.40–12.4%, trans-ocimene 2.99–20.6%, α-terpinolene 0.5–25.4%, cis-ocimene 2.65 –22.2% sabinene 14.28–39.44% Ethers: trans-anethole 10–21.2%, cis-anethole 53.37–81.0%, methyl eugenol 2.2–39.35%, methyl isoeugenol 1.8–35.8%, methyl chavicol 1.09–74.46% Others: asarone 21.69–40.36 |
[127,128,129,130,131,132] |
| Chamaemelum nobile (Asteraceae)—roman chamomile | Flowers | Hydrocarbons: monoterpenes: α-terpinene 0–10%, α-pinene 0–10%, ß-pinene 0–10%, sabinene 0–10%; sesquiterpenes: caryophyllene 0–10% Alcohols: trans-pinocarveol 5% Aldehydes: myrtenal 0–10% Ketones: pinocarvone 13% Oxides: 1,8-cineole 0–25% Ethers: methyl chavicol 5% Esters: 2-methylbutyl 2-methyl propionate 0.5–25%, 2-methylpropyl butanoate 0.5–10%, 2-methylbutyl, 2-methylbutanoate 0.5–25%, 2-methylpropyl 3-methylbutanoate 0–10%, propyl angelate 0.5–10%, 2-methylpropyl angelate 0.5–25%, butyl angelate 0.5–10%, 3-methylpentyl angelate 0–10%, isobutyl angelate 36–40%, isobutyl isobutanoate 4%, 2-methylbutyl methyl-2-butanoate 3%, isoamyl methyl-2 butanoate 3%, hexyl acetate 0.5–10% |
[86,133,134,135,136,137,138] |
| Chrysactinia mexicana, (Asteraceae)—damianita daisy | Leaves | Hydrocarbons: monoterpenes: α-myrcene 1.20% Alcohols: linalool 1.39% Ketones: α-thujone 1.17%, piperitone 37.74% Oxides: 1,8-cineole 41.3% Esters: linalyl acetate 9.08% |
[139] |
| Hofmeisteria schaffneri (Asteraceae) | Aerial parts | Major components differ depending on the harvesting time Alcohols: linalool 0.25–1.38% Esters: thymyl isobutyrate 1.54–3-41%, thymyl isovalerate 14.12–30.97%, 9-acetoxy-8,9-dehydrothymyl angelate 2.36–5.23%, 8,9-epoxy-10-acetoxythymyl angelate 0.41–15% Others: hofmeisterin III 24.12–34.85% |
[140] |
| Matricaria recutita (Asteraceae)—german chamomile | Flowers | Hydrocarbons: sesquiterpenes chamazulene 1–35%, trans-ß-farnesene 2–13%, trans-α-farnesene 27%, δ-cadinene 5.2%, γ-muurolene 1.3%, α-muurolene 3.4% Alcohols: sesquiterpenols: α-bisabolol 2–67% Oxides:α-bisabol oxide A 0–55%, α-bisabolol oxide B 4.3–19%, bisabolone oxide A 0–64% |
[127,133,134,135] |
| Pelargonium graveolens, (Geraniaceae)—geranium | Aerial parts | Hydrocarbons: monoterpenes:α-pinene 22.47%; sesquiterpenes: guai-6,9-diene 3.9–5.3%, β-bourbonene 2.7–3.14%, germacrene D 2.92–4.33%, γ-cadinene 2.38% Alcohols: citronellol 15.2–48.44%, geraniol 6–25%, linalool 1–13.79%, octen-1-ol 18.61% Aldehydes:geranial 0–9% Ketones: menthone 0.6–6.96%, isomenthone 4–8.4% Oxides: cis-rose oxide 0.69–25%, trans-rose oxide 0.31–2.01%, cariopyllene oxide 2.52–3.7% Esters: citronellyl formate 8–24.4%, geranyl formate 1–6.22%, citronellyl propionate 1–3%, geranyl angelate 1–2%, citronellyl butanoate 1.3%, geranyl butanoate 1.3% |
[86,99,141,142,143,144] |
| Lavandula angustifolia (Lamiaceae)—true lavender | Flowers | Hydrocarbons: monoterpenes:cis-ß-ocimene 1.3–10.9%, trans-ß-ocimene 0.8–5.8%, limonene 0.2–7%; sesquiterpenes: ß-caryophyllene 2.6–7.6% Alcohols: linalool 26–49%, terpinen-4-ol 0.03–6.4%, α-terpineol 0.1–1.4%, borneol 0.8–1.4%, lavandulol 0.5–1.5% Oxides: 1,8-cineole 0.5–2.5% Esters: linalyl acetate 35–55%, lavandulyl acetate 0.2–5.9% |
[33,89,99,137,145,146,147,148] |
| Melissa officinalis (Lamiaceae)—melissa | Aerial parts | Major components differ significantly depending on the origin of the plant material Hydrocarbons: sesquiterpenes: ß-caryophyllene 8–10%, α-copaene 4–5% Alcohols: linalool 0.4–2.74%, nerol 1.4%, geraniol 0.20-27.22%, citronelol 0-36.71% Aldehydes: neral 3.28–31.5%, geranial 0-38.13%, citronellal 1.48–39.6% Oxides: caryophyllene oxide 0.2–10.26% |
[149,150,151,152] |
| Mentha × piperita (Lamiaceae)—peppermint | Aerial parts | Hydrocarbons: monoterpenes: α-pinene 0.2–2%, ß-pinene 0.3–4%, limonene 0.6–6%; sesquiterpenes: germacrene D 1.75–4.3% Alcohols: menthol 25.16–48%, neomenthol 2–7.7%, α-terpineol 0.1–1.9%, cis-carveol 3.35%, terpinen-4-ol 0–2.4%, cis-thujan-4-ol 0.2–1.4%, viridiflorol 0.5–1.3%, Ketones: menthone 16–42.97%, isomenthone 4–10.4%, neomenthone 2–3%, piperitone 0.5–1.2%, pulegone 4.39% Oxides: 1,8-cineole 2.15–7.4%, transpiperitonoxide 0.5–3.1% Esters: menthyl acetate 1.6–10% Benzofurans: menthofuran 0.1–5.7% |
[153,154,155,156] |
| Mentha spicata (Lamiaceae)—spearmint | Aerial parts | Hydrocarbons: monoterpenes: ß-pinene 0.3–2.3%, ß-myrcene 1.2–5.5, limonene 2–25%; sesquiterpenes: ß-caryophyllene 0.3–4.41%, β –farnesene 1.71%, ß-bourbonene trace–2.14%, germacrene D 0–3.14% Alcohols: cis-carveol 5.30%, menthol 0.5–2%, terpinen-4-ol trace–6.1%, α-terpineol 0–2.7% Ketones: carvone 39–70%, menthone trace–5.2%, cis-dihydrocarvone 3.1–21.6%, trans-dihydrocarvone 0–21%, isomenthone 3.33% Oxides: 1,8-cineole 0.5–17.0%, piperetenone oxide trace—79.2% Esters: dihydrocarvyl acetate 1.2–24.8%, cis-carvyl acetate 0.2–5.5%, trans-carvyl acetate 0.7–5.9%, neoisodihydrocarveol acetate 0–21%, menthyl acetate 2% Benzofurans: menthofuran 2% |
[86,99,156,157,158] |
| Mentha x vilosa Huds.(Lamiaceae)—mojito mint | Aerial parts | Hydrocarbons: monoterpenes:ß-pinene 1.42–4.04%, myrcene 3.10–3.66%, limonene 2.38–8.75%; sesquiterpenes: ß-caryophyllene 2.82–5.16%,δ-cardinene 9.69%, γ-muurolene 2.18–16.02%, germacrene-D 3.81% Oxides: 1,8-cineole 1.58–3.93%, piperitenone oxide 58.74–79.03%, cariophyllene oxide 2.82% |
[33,91,159,160,161] |
| Ocimum basilicum (Lamiaceae)—basil | Aerial parts | Hydrocarbons: sesquiterpenes:ß-caryophyllene 2–3% Alcohols: linalool 40–55%, α-fenchyl alcohol 3–12%, terpinen-4-ol 1.6%, α-terpineol 2% Phenols: eugenol 1–19%, iso-eugenol 2% Oxides: 1,8-cineole 2–8% Ethers: methyl chavicol 3–31%, methyl eugenol 1–9% Esters: methyl cinnamate 0.1–7% |
[86,162] |
| Ocimum selloi (Lamiaceae) —green pepper basil | Aerial parts | Hydrocarbons: sesquiterpenes:ß-caryophyllene 2.2–3%, germacrene D 0–3.14% Alcohols: linalool 20.6%, spathulenol 1.3% Ethers: trans-anethole 45.42%, cis-anethole 3.95%, methyl chavicol 24.14–93.2%, methyl eugenol 2.2-39.35% |
[35,162,163,164] |
| Ocimum gratissimum (Lamiaceae)—african basil | Aerial parts | Hydrocarbons: monoterpenes:β-pinene 6.2%, cis-ocimene 13.9–23.97%, trans-ocimene 19.60–48.28%, γ-terpinene 0.20–28.10%, limonene 11.40%; sesquiterpenes: ß-caryophyllene 2.7–3.06%, β-phellandrene (21.10), germacrene D 7.30-10.36%, α-trans-bergamotene 4.1%, γ- muurolene 9.32–11.6%; aromatic: p-cymene 4.40–19.90% Phenols: eugenol 10.70–74.80%, thymol 13.10–46.60% Oxides: 1,8-cineole 0–54.94% |
[36,162,165,166] |
| Origanum majorana, (Lamiaceae)—sweet marjoram | Aerial parts | Major components differ significantly depending on chemotype and the origin of the plant material Hydrocarbons: monoterpenes: sabinene 1.45–10%, ß-myrcene 1–9%, α-terpinolene 1–7%, α-pinene 1–5%, cis-/trans-ß-ocimenes 6.4%, 3-carene 6.2%, myrcene 1.12-4.7%, α-terpinene 3.9–8%, γ-terpinene 11.16–20%; sesquiterpenes: ß-caryophyllene 2–7.44%, δ-cadinene 4.2%, α-farnesene 4.58%, germacrene D 9.2%; aromatic: benzene 13.34%, p-cymene 7.0–12.05% Alcohols: terpinen-4-ol 14–38.4%, cis-thujan-4-ol 0.11–44%, trans-thujan-4-ol 1–5%, linalool 2–31.68%, α-terpineol 7–27% Phenols: carvacrol 0–83.47% Esters: terpenyl acetate 0–3%, geranyl acetate 1–7.8%, linalyl acetate 2.41–17.4% |
[86,167,168,169,170,171] |
| Plectranthus barbatus synonym Coleus forskohlii, (Lamiaceae)—Iindian coleus | Aerial parts | Hydrocarbons: monoterpenes: α-pinene 12–67%,β-pinene 0.1-22%, β-myrcene 1.8%, cis-β-ocimene 1.9%, trans-β-ocimene 1.2%; sesquiterpenes: β-caryophyllene 7-12%, α-copaene 8.9%, β-cubebene 3.7% Alcohols: oct-1-en-3-ol traces–28% Phenols: thymol 15.3%, carvacrol 12.1%, eugenol 25.1% |
[38,172,173,174] |
| Rosmarinus officinalis ct. verbenone, (Lamiaceae)—rosemary | Aerial parts | Hydrocarbons: monoterpenes: α-pinene 15–34% Alcohols: borneol trace–16.63% Ketones: verbenone 15–37%, camphor 1–22.35% Oxides: 1,8-cineole trace–20% Esters: bornyl acetate 12% |
[86,175,176,177] |
| Salvia officinalis (Lamiaceae)—sage | Aerial parts | Hydrocarbons: monoterpenes: α-pinene 2.02–6.4%, ß-pinene 1.9–8.20%, camphene 1–8.49%, ß-myrcene 0.4–5.66%, limonene 0.9–4%; sesquiterpenes: ß-caryophyllene 1–7%, α-humulene 1.6–5% Alcohols: linalool 0.4–12%, terpinen-4-ol 0.2–4%, α-terpineol trace–9%, borneol 1.5–14%, viridiflorol 0–10% Ketones:α-thujone1.1–35.7%,ß-thujone 1.71–33%, camphor 4.1–43.83% Oxides: 1,8-cineole 5–57.18%, caryophyllene oxide 0.4–2.1% Esters: bornyl acetate 0.1–5.59%, linalyl acetate 1–2% |
[40,86,178,179] |
| Satureja hortensis (Lamiaceae)—summer savory | Aerial parts | Hydrocarbons: monoterpenes: α-terpinene 1.29-3.1%, γ-terpinene 12.8-24%, β-myrcene 1–2.8%; sesquiterpenes: ß-caryophyllene 1.2–4%, δ-cadinene 3%; aromatic: p-cymene 3.7–20% Alcohols: linalool 9–54%, terpinen-4-ol trace–7%, α-terpineol 6–9% Phenols: carvacrol 59.70–67.00%, eugenol 1–1.7%, thymol 0-29.0% Oxides: 1,8-cineole 0-37.82% |
[86,99,180,181] |
| Cymbopogon citratusStapf(Poaceae)—West Indian lemongrass | Aerial parts | Hydrocarbons: monoterpenes: limonene 2.4–2.6%, β-myrcene 2.34–21% Alcohols: α-terpineol 0.2–2.3%, linalool 1.2–3.4%, geraniol 2.6–40%, nerol 0.8–4.5%, citronellol 0.1–8%, farnesol 12.8% Aldehydes: neral 3–43%, geranial 4.5–58%, citronellal 0.1–9% Esters: geranyl acetate 0.1–3.0% |
[42,86,182,183,184,185] |
| Cymbopogon schoenantus (L.) Spreng (Poaceae)—camelgrass | Aerial parts | Hydrocarbons: monoterpenes: limonene 1.5–3.12%; sesquiterpenes: β-elemene 11.6%, δ-2-carene 10% Alcohols: α-eudesmol 11.5%, elemol 10.8%, β-eudesmol 8.5%, γ- eudesmol 4.2%, intermedeol 6.1–17.3%, linalool 21.6% Aldehydes: neral 3.3%, geranial 2.4% Ketones: piperitone 47.7–71.5% |
[43,185] |
| Cymbopogon martini (Poaceae)—palmarosa | Aerial parts | Alcohols: linalool 1.6–3.4%, geraniol 67.6–83.6%, citronellol 1.6–2.1% Aldehydes: geranial 1–8.8% Esters: geranyl acetate 2.2–24.6% |
[185,186] |
| Rosa indica L, (Rosaceae) |
Hydrocarbons: nonadecane 3.4%, (Z)-9-nonadecene 3.3%, heneicosane 6.7%, tricosane 5.6%, pentacosane 4.9% Alcohols: citronellol 11.7%, nerol 8.0%, geraniol 24.8%, farnesol 2.0% |
[45,187] | |
| Citrus aurantifolia/Citrus medica var. acida (Rutaceae)—lime | Pericarps | Hydrocarbons: monoterpenes: limonene 36–60%, γ-terpinene 6–17.6%, α-pinene 0.2–5.03%, ß-pinene 4.9–19.5%, ß-myrcene 1–2.6%; sesquiterpenes: ß-caryophyllene 1.3–3.4%, α-bisabolene 2.3%; aromatic p-cymene 0.1–6.8% Alcohols: linalool 1.4–16.9%, α-terpineol 13–23% Aldehydes: citronellal 0–5.3%, neral 0.7–4.7%, geranial 1.81–6.4% Esters: linalyl acetate 26–27% |
[46,86,99,188,189] |
| Citrus aurantium var. sinensis (Rutaceae)—sweet orange | Pericarps | Hydrocarbons: limonene 87.9–96.8%, ß-myrcene 1.37–2.5%, ß-phellandrene 0–1.5% Alcohols: linalool 0.5–2.4% Ketones: carvone 1.8% |
[86,99,190,191] |
| Lippia alba, (Verbenaceae) | Leaves | The plant presents a great morphological and chemical variability with a predominance of monoterpene type compounds such as citral, β-myrcene, limonene and carvone, based on which several chemotyps have been described. Hydrocarbons: monoterpenes: limonene 8.2–15.7%, γ-terpinene 4.09%, myrcene 6.6–8.3%; sesquiterpenes: β-caryophyllene 2.7–3.07%, germacrene D 3.0–5.47% Alcohols: β-elemol 5.37%, nerol 2.2%, geraniol 2.9%, linalool 0.8–64.2% Aldehydes: geranial 6.5–50.94%, neral 11.5–33.32% Ketones: carvone 16.7–33.7% Oxides: cariopyllene oxide 0–2.64% |
[48,192,193,194,195] |
| Lippia thymoides, (Verbenaceae) | Leaves | Hydrocarbons: monoterpenes: α-pinene 0.94–2.38%, camphene 2.64–5.66%, limonene 1.67–3.75%,; sesquiterpenes: copaene 2.42–3.38%, β-caryophyllene 5.32–26.27%, α-caryophyllene 3.06-5.48%, germacrene D 4.72–6.18% Alcohols: borneol 4.45–7.36% Phenols: thymol trace–66.33% Ketones: camphor 3.22–8.61% Oxides: cariopyllene oxide 0.9–2.7% Ethers: 1,8-cineole 1.86–4.5% Esters: thymol acetate 0-7.49% |
[49,196,197] |
| Elettaria cardamomum, (Zingiberaceae)—cardomom | Fruits | Hydrocarbons: monoterpenes: limonene 1.7–14%, sabinene 1.3–5%, ß-myrcene 0.2–2.2% Alcohols: linalool 0.4–6.9%, terpinen-4-ol 0.1–3.2%, α-terpineol 0.8–5.25%, geraniol 0.2–1.6%, trans-nerolidol 0.1–2.7%, cis-nerolidol 0.2–1.6% Oxides: 1,8-cineole 15.13–50% Esters: α-terpinyl acetate 29–56.87%, linalyl acetate 0.2–7.7% |
[86,198,199,200,201,202] |
4. Conclusions
This review identified 39 plant species bearing essential oils with antispasmodic effect demonstrated in preclinical studies. The main mechanisms of the antispasmodic effect were represented by inhibition of voltage-dependent calcium channels, modulation of potassium channels and modulation of intracellular cAMP. Certain individual components identified in the chemical composition of the essential oils studied could become promising new drug candidates but future clinical studies are needed in order to ascertain their therapeutical value.
Author Contributions
Conceptualization, S.C.H. and O.V.; Methodology, O.V.; Software, L.R.; Validation, S.C.H., O.V. and C.M.; Formal Analysis, L.R.; Investigation, S.C.H. and O.V.; Resources, S.C.H. and O.V.; Data Curation, L.R. and C.A.I.; Writing—Original Draft Preparation, S.C.H. and O.V.; Writing—Review andEditing, S.C.H., L.R. and O.V.; Visualization, L.F.; Supervision, C.M., C.A.I. and L.F.; Project Administration, L.F.; Funding Acquisition, L.F.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Hicks G.A. Irritable Bowel Syndrome. In: Taylor J.B., Triggle D.J., editors. Comprehensive Medicinal Chemistry. Elsevier Science; London, UK: 2007. pp. 643–670. [Google Scholar]
- 2.Annaházi A., Róka R., Rosztóczy A., Wittmann T. Role of antispasmodics in the treatment of irritable bowel syndrome. World J. Gastroenterol. 2014;20:6031–6043. doi: 10.3748/wjg.v20.i20.6031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baiu I., Hawn M.T. Gallstones and Biliary Colic. JAMA. 2018;320:1612. doi: 10.1001/jama.2018.11868. [DOI] [PubMed] [Google Scholar]
- 4.Sanagapalli S., Agnihotri K., Leong R., Corte C.J. Antispasmodic drugs in colonoscopy: A review of their pharmacology, safety and efficacy in improving polyp detection and related outcomes. Therap. Adv. Gastroenterol. 2017;10:101–113. doi: 10.1177/1756283X16670076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Can Baser H.K., Buchbauer G. Handbook of Essential Oils: Science, Technology and Applications. CRC Press; Boca Raton, FL, USA: 2010. pp. 3–39. [Google Scholar]
- 6.Yarnell E., Abascal K. Spasmolytic botanicals. Altern. Complement. Ther. 2011;17:169–172. doi: 10.1089/act.2011.17305. [DOI] [Google Scholar]
- 7.Sharifi-Rad J., Sureda A., Tenore G.C., Daglia M., Sharifi-Rad M., Valussi M., Tundis R., Sharifi-Rad M., Loizzo M.R., Oluwaseun Ademiluyi A., et al. Biological activities of essential oils: From plant chemoecology to traditional healing systems. Molecules. 2017;22:70. doi: 10.3390/molecules22010070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Araújo D.A.M., Freitas C., Cruz J.S. Essential oils components as a new path to understand ion channel molecular pharmacology. Life Sci. 2011;89:540–544. doi: 10.1016/j.lfs.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 9.Shirole R.L., Shirole N.L., Saraf M.N. In vitro relaxant and spasmolytic effects of essential oil of Pistacia integerrima Stewart ex Brandis Galls. J. Ethnopharmacol. 2015;168:61–65. doi: 10.1016/j.jep.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Kim H.J., Yang H.M., Kim D.H., Kim H.G., Jang W.C., Lee Y. Effects of ylang-ylang essential oil on the relaxation of rat bladder muscle in vitro and white rabbit bladder in vivo. J. Korean Med. Sci. 2003;18:409–414. doi: 10.3346/jkms.2003.18.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Souza I.L.L., de Carvalho Correia A.C., da Cunha Araujo L.C., Vasconcelos L.H.C., Silva M.D.C.C., de Oliveira Costa V.C., Tavares J.F., Paredes-Gamero E.J., de Andrade Cavalcante F., da Silva B.A. Essential oil from Xylopia frutescens Aubl. reduces cytosolic calcium levels on guinea pig ileum: Mechanism underlying its spasmolytic potential. BMC Complement. Altern. Med. 2015;15:327. doi: 10.1186/s12906-015-0849-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de C. Correia A.C., Ferreira T.F., Martins I.R.R., Macêdo C.L., de S. Monteiro F., Costa V.C.O., Tavares J.F., Silva M.S., Paredes-Gamero E.J., Buri M.V., et al. Essential oil from the leaves of Xylopia langsdorffiana (Annonaceae) as a possible spasmolytic agent. Nat. Prod. Res. 2015;29:980–984. doi: 10.1080/14786419.2014.964706. [DOI] [PubMed] [Google Scholar]
- 13.Gharib Naseri M.K., Heidari A. Antispasmodic effect of Anethum graveolens fruit extract on rat ileum. Int. J. Pharmacol. 2007;3:260–264. doi: 10.3923/ijp.2007.260.264. [DOI] [Google Scholar]
- 14.Heinle H., Hagelauer D., Pascht U., Kelber O., Weiser D. Intestinal spasmolytic effects of STW 5 (Iberogast®) and its components. Phytomedicine. 2006;13:75–79. doi: 10.1016/j.phymed.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Al-Essa M.K., Shafagoj Y.A., Mohammed F.I., Afifi F.U. Relaxant effect of ethanol extract of Carum carvi on dispersed intestinal smooth muscle cells of the guinea pig. Pharm. Biol. 2010;48:76–80. doi: 10.3109/13880200903046161. [DOI] [PubMed] [Google Scholar]
- 16.Jabeen Q., Bashir S., Lyoussi B., Gilani A.H. Coriander fruit exhibits gut modulatory, blood pressure lowering and diuretic activities. J. Ethnopharmacol. 2009;122:123–130. doi: 10.1016/j.jep.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 17.Pavlović I., Petrović S., Radenković M., Milenković M., Couladis M., Branković S., Drobac M.P., Niketić M. Composition, antimicrobial, antiradical and spasmolytic activity of Ferula heuffelii Griseb. ex Heuffel (Apiaceae) essential oil. Food Chem. 2012;130:310–315. doi: 10.1016/j.foodchem.2011.07.043. [DOI] [Google Scholar]
- 18.Ostad S.N., Soodi M., Shariffzadeh M., Khorshidi N., Marzban H. The effect of fennel essential oil on uterine contraction as a model for dysmenorrhea, pharmacology and toxicology study. J. Ethnopharmacol. 2001;76:299–304. doi: 10.1016/S0378-8741(01)00249-5. [DOI] [PubMed] [Google Scholar]
- 19.Tirapelli C.R., de Andrade C.R., Cassano A.O., De Souza F.A., Ambrosio S.R., da Costa F.B., de Oliveira A.M. Antispasmodic and relaxant effects of the hidroalcoholic extract of Pimpinella anisum (Apiaceae) on rat anococcygeus smooth muscle. J. Ethnopharmacol. 2007;110:23–29. doi: 10.1016/j.jep.2006.08.031. [DOI] [PubMed] [Google Scholar]
- 20.Gilani A.U., Shah A.J., Ahmad M., Shaheen F. Antispasmodic effect of Acorus calamus Linn. is mediated through calcium channel blockade. Phytother. Res. 2006;20:1080–1084. doi: 10.1002/ptr.2000. [DOI] [PubMed] [Google Scholar]
- 21.Jalilzadeh-Amin G., Maham M., Dalir-Naghadeh B., Kheiri F. In vitro effects of Artemisia dracunculus essential oil on ruminal and abomasal smooth muscle in sheep. Comp. Clin. Path. 2012;21:673–680. doi: 10.1007/s00580-010-1155-6. [DOI] [Google Scholar]
- 22.Sándor Z., Mottaghipisheh J., Veres K., Hohmann J., Bencsik T., Horváth A., Kelemen D., Papp R., Barthó L., Csupor D. Evidence supports tradition: The in vitro effects of Roman Chamomile on smooth muscles. Front. Pharmacol. 2018;9:1–11. doi: 10.3389/fphar.2018.00323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zavala-Mendoza D., Grasa L., Zavala-Sánchez M.Á., Pérez-Gutiérrez S., Murillo M.D. Antispasmodic effects and action mechanism of essential oil of Chrysactinia mexicana A. Gray on rabbit ileum. Molecules. 2016;21:783. doi: 10.3390/molecules21060783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perez-Vasquez A., Angeles-Lopez G., Rivero-Cruz I., Flores-Bocanegra L., Linares E., Bye R., Mata R. Spasmolytic action of preparations and compounds from Hofmeisteria schaffneri. Nat. Prod. Commun. 2017;12:475–476. doi: 10.1177/1934578X1701200401. [DOI] [PubMed] [Google Scholar]
- 25.Mehmood M.H., Munir S., Khalid U.A., Asrar M., Gilani A.H. Antidiarrhoeal, antisecretory and antispasmodic activities of Matricaria chamomilla are mediated predominantly through K+-channels activation. BMC Complement. Altern. Med. 2015;15:75. doi: 10.1186/s12906-015-0595-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lis-Balchin M., Hart S., Roth G. The spasmolytic activity of the essential oils of scented Pelargoniums (Geraniaceae) Phytother. Res. 1997;11:583–584. doi: 10.1002/(SICI)1099-1573(199712)11:8<583::AID-PTR148>3.0.CO;2-6. [DOI] [Google Scholar]
- 27.Lis-Balchin M., Hart S. Studies on the mode of action of the essential oil of Lavender (Lavandula angustifolia P. Miller) Phytother. Res. 1999;13:540–542. doi: 10.1002/(SICI)1099-1573(199909)13:6<540::AID-PTR523>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 28.Sadraei H., Ghannadi A., Malekshahi K. Relaxant effect of essential oil of Melissa officinalis and citral on rat ileum contractions. Fitoterapia. 2003;74:445–452. doi: 10.1016/S0367-326X(03)00109-6. [DOI] [PubMed] [Google Scholar]
- 29.Aubert P., Guinobert I., Guilbot A., Dubourdeaux M., Neunlist M. Antispasmodic and spamolytic activity of Melissa officinalis EPS upon mice gastrointestinal tract: An ex vivo pilot study. Planta Med. 2016;82:S1–S381. [Google Scholar]
- 30.Grigoleit H.G., Grigoleit P. Pharmacology and preclinical pharmacokinetics of peppermint oil. Phytomedicine. 2005;12:612–616. doi: 10.1016/j.phymed.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Heimes K., Hauk F., Verspohl E.J. Mode of action of peppermint oil and (-)-menthol with respect to 5-HT 3 receptor subtypes: Binding studies, cation uptake by receptor channels and contraction of isolated rat ileum. Phytother. Res. 2011;25:702–708. doi: 10.1002/ptr.3316. [DOI] [PubMed] [Google Scholar]
- 32.Souza F.V.M., Da Rocha M.B., De Souza D.P., Marçal R.M. Carvone: Antispasmodic effect and mode of action. Fitoterapia. 2013;85:20–24. doi: 10.1016/j.fitote.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 33.De Sousa D.P., Júnior G.A.S., Andrade L.N., Calasans F.R., Nunes X.P., Barbosa-Filho J.M., Batista J.S. Structure and Spasmolytic Activity Relationships of Monoterpene Analogues Found in Many Aromatic Plants. Z. Naturforsch. C. 2008;63:808–812. doi: 10.1515/znc-2008-11-1205. [DOI] [PubMed] [Google Scholar]
- 34.Janbaz K.H., Hamid I., Gilani A.-H., Qadir M.I. Spasmolytic, Bronchodilator and Vasodilator Activities of Aqueous-methanolic Extract of Ocimum basilicum. Int. J. Agric. Biol. 2014;16:321–327. [Google Scholar]
- 35.Souza S.D.F., Franca C.S.L., Niculau E.S., Costa L.C.B., Pinto J.E.B., Alves P.B., Marçal R.M. Antispasmodic effect of Ocimum selloi essential oil on the guinea-pig ileum. Nat. Prod. Res. 2015;29:2125–2128. doi: 10.1080/14786419.2014.989392. [DOI] [PubMed] [Google Scholar]
- 36.Madeira S.V.F., Matos F.J.A., Leal-Cardoso J.H., Criddle D.N. Relaxant effects of the essential oil of Ocimum gratissimum on isolated ileum of the guinea pig. J. Ethnopharmacol. 2002;81:1–4. doi: 10.1016/S0378-8741(02)00049-1. [DOI] [PubMed] [Google Scholar]
- 37.Makrane H., Aziz M., Mekhfi H., Ziyyat A., Bnouham M., Abdelkhaleq L., Gressier B., Eto B. Antispasmodic and Myorelaxant Activity of Organic Fractions from Origanum majorana L. on Intestinal Smooth Muscle of Rodents. European J. Med. Plants. 2018;23:1–11. doi: 10.9734/EJMP/2018/41075. [DOI] [Google Scholar]
- 38.Câmara C.C., Nascimento N.R.F., Macêdo-Filho C.L., Almeida F.B.S., Fonteles M.C. Antispasmodic Effect of the Essential Oil of Plectranthus barbatus and some Major Constituents on the Guinea-Pig Ileum. Planta Med. 2003;69:1080–1085. doi: 10.1055/s-2003-45186. [DOI] [PubMed] [Google Scholar]
- 39.Ventura-Martínez R., Rivero-Osorno O., Gómez C., González-Trujano M.E. Spasmolytic activity of Rosmarinus officinalis L. involves calcium channels in the guinea pig ileum. J. Ethnopharmacol. 2011;137:1528–1532. doi: 10.1016/j.jep.2011.08.047. [DOI] [PubMed] [Google Scholar]
- 40.Khan A., Najeeb-ur-Rehman, Alkharfy K.M., Gilani A.H. Antidiarrheal and antispasmodic activities of Salvia officinalis are mediated through activation of K + channels. Bangladesh J. Pharmacol. 2011;6:111–116. doi: 10.3329/bjp.v6i2.9156. [DOI] [Google Scholar]
- 41.Hajhashemi V., Sadraei H., Ghannadi A.R., Mohseni M. Antispasmodic and anti-diarrhoeal effect of Satureja hortensis L. essential oil. J. Ethnopharmacol. 2000;71:187–192. doi: 10.1016/S0378-8741(99)00209-3. [DOI] [PubMed] [Google Scholar]
- 42.Devi R.C., Sim S.M., Ismail R. Spasmolytic effect of citral and extracts of Cymbopogon citratus on isolated rabbit ileum. J. Smooth Muscle Res. 2011;47:143–156. doi: 10.1540/jsmr.47.143. [DOI] [PubMed] [Google Scholar]
- 43.Pavlovic I., Omar E., Drobac M., Radenkovic M., Brankovic S., Kovacevic N. Chemical composition and spasmolytic activity of Cymbopogon schoenanthus (L.) Spreng. (Poaceae) essential oil from Sudan. Arch. Biol. Sci. 2017;69:409–415. doi: 10.2298/ABS160506113P. [DOI] [Google Scholar]
- 44.Janbaz K.H., Qayyum A., Saqib F., Imran I., Zia-Ul-Haq M., De Feo V. Bronchodilator, vasodilator and spasmolytic activities of Cymbopogon martinii. J. Physiol. Pharmacol. 2014;65:859–866. [PubMed] [Google Scholar]
- 45.Rasheed H.M., Khan T., Wahid F., Khan R., Shah A.J. Chemical Composition and Vasorelaxant and Antispasmodic Effects of Essential Oil from Rosa indica L. Petals. Evid. Based Complement. Alternat. Med. 2015;2015:279247. doi: 10.1155/2015/279247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Spadaro F., Costa R., Circosta C., Occhiuto F. Volatile composition and biological activity of key lime Citrus aurantifolia essential oil. Nat. Prod. Commun. 2012;7:1523–1526. doi: 10.1177/1934578X1200701128. [DOI] [PubMed] [Google Scholar]
- 47.Sánchez-Recillas A., Arroyo-Herrera A.L., Araujo-León J.A., Hernández Núñez E., Ortiz Andrade R. Spasmolytic and Antibacterial Activity of Two Citrus sinensis Osbeck Varieties Cultivated in Mexico. Evid. Based Complement. Alternat. Med. 2017;2017:3960837. doi: 10.1155/2017/3960837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Blanco M.A., Colareda G.A., Van Baren C., Bandoni A.L., Ringuelet J., Consolini A.E. Antispasmodic effects and composition of the essential oils from two South American chemotypes of Lippia alba. J. Ethnopharmacol. 2013;149:803–809. doi: 10.1016/j.jep.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 49.Menezes P.M.N., de Oliveira H.R., Brito M.C., de Paiva G.O., Ribeiro L.A.D.A., Lucchese A.M., Silva F.S. Spasmolytic and antidiarrheal activities of Lippia thymoides (Verbenaceae) essential oil. Nat. Prod. Res. 2018:1–3. doi: 10.1080/14786419.2018.1457665. [DOI] [PubMed] [Google Scholar]
- 50.Gilani A.H., Jabeen Q., Khan A.U., Shah A.J. Gut modulatory, blood pressure lowering, diuretic and sedative activities of cardamom. J. Ethnopharmacol. 2008;115:463–472. doi: 10.1016/j.jep.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 51.Martínez-Pérez E.F., Juárez Z.N., Hernández L.R., Bach H. Natural Antispasmodics: Source, Stereochemical Configuration, and Biological Activity. Biomed Res. Int. 2018;3819714:1–32. doi: 10.1155/2018/3819714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.de Almeida N.R., de Fátima Agra M., Negromonte Souto Maior F., De Sousa D.P. Essential Oils and Their Constituents: Anticonvulsant Activity. Molecules. 2011;16:2726–2742. doi: 10.3390/molecules16032726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sarmento-Neto J.F., Do Nascimento L.G., Felipe C.F.B., De Sousa D.P. Analgesic potential of essential oils. Molecules. 2016;21:20. doi: 10.3390/molecules21010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ielciu I., Voştinaru O., Oniga S., Mogoşan C., Vlase L., Parnau A., Araniciu C., Palage M. Synthesis and effects of some new 2-aryl-thiazole ammonium salts on isolated ileum motility. Dig. J. Nanomater. Bios. 2013;8:1089–1099. [Google Scholar]
- 55.Mukai T., Yamaguchi E., Goto J., Takagi K. Smooth muscle relaxing drugs and guinea pig ileum. Jpn. J. Pharmacol. 1981;31:147–157. doi: 10.1254/jjp.31.147. [DOI] [PubMed] [Google Scholar]
- 56.Papathanasopoulos A., Rotondo A., Janssen P., Boesmans W., Farré R., Vanden Berghe P., Tack J. Effect of acute peppermint oil administration on gastric sensorimotor function and nutrient tolerance in health. Neurogastroenterol. Motil. 2013;25:e263–e271. doi: 10.1111/nmo.12102. [DOI] [PubMed] [Google Scholar]
- 57.Inamori M., Akiyama T., Akimoto K., Fujita K., Takahashi H., Yoneda M., Abe Y., Kubota K., Saito S., Ueno N., et al. Early effects of peppermint oil on gastric emptying: A crossover study using a continuous real-time 13C breath test (BreathID system) J. Gastroenterol. 2007;42:539–542. doi: 10.1007/s00535-007-2067-3. [DOI] [PubMed] [Google Scholar]
- 58.May B., Köhler S., Schneider B. Efficacy and tolerability of a fixed combination of peppermint oil and caraway oil in patients suffering from functional dyspepsia. Aliment. Pharmacol. Ther. 2000;14:1671–1677. doi: 10.1046/j.1365-2036.2000.00873.x. [DOI] [PubMed] [Google Scholar]
- 59.Madisch A., Heydenreich C.-J., Wieland V., Hufnagel R., Hotz J. Treatment of Functional Dyspepsia with a Fixed Peppermint Oil and Caraway Oil Combination Preparation as Compared to Cisapride. Arzneimittelforschung. 1999;49:925–932. doi: 10.1055/s-0031-1300528. [DOI] [PubMed] [Google Scholar]
- 60.Cash B.D., Epstein M.S., Shah S.M. A Novel Delivery System of Peppermint Oil Is an Effective Therapy for Irritable Bowel Syndrome Symptoms. Dig. Dis. Sci. 2016;61:560–571. doi: 10.1007/s10620-015-3858-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Khanna R., MacDonald J.K., Levesque B.G. Peppermint Oil for the Treatment of Irritable Bowel Syndrome. J. Clin. Gastroenterol. 2013;48:505–512. doi: 10.1097/MCG.0b013e3182a88357. [DOI] [PubMed] [Google Scholar]
- 62.Merat S., Khalili S., Mostajabi P., Ghorbani A., Ansari R., Malekzadeh R. The Effect of Enteric-Coated, Delayed-Release Peppermint Oil on Irritable Bowel Syndrome. Dig. Dis. Sci. 2010;55:1385–1390. doi: 10.1007/s10620-009-0854-9. [DOI] [PubMed] [Google Scholar]
- 63.Cappello G., Spezzaferro M., Grossi L., Manzoli L., Marzio L. Peppermint oil (Mintoil®) in the treatment of irritable bowel syndrome: A prospective double blind placebo-controlled randomized trial. Dig. Liver Dis. 2007;39:530–536. doi: 10.1016/j.dld.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 64.Pittler M.H., Ernst E. Peppermint oil for irritable bowel syndrome: A critical review and metaanalysis. Am. J. Gastroenterol. 1998;93:1131–1135. doi: 10.1111/j.1572-0241.1998.00343.x. [DOI] [PubMed] [Google Scholar]
- 65.Liu J.H., Chen G.H., Yeh H.Z., Huang C.K., Poon S.K. Enteric-coated peppermint-oil capsules in the treatment of irritable bowel syndrome: A prospective, randomized trial. J. Gastroenterol. 1997;32:765–768. doi: 10.1007/BF02936952. [DOI] [PubMed] [Google Scholar]
- 66.Inoue K., Dohi O., Gen Y., Jo M., Mazaki T., Tokita K., Yoshida N., Okayama T., Kamada K., Katada K., et al. L-menthol improves adenoma detection rate during colonoscopy: A randomized trial. Endoscopy. 2014;46:196–202. doi: 10.1055/s-0034-1365035. [DOI] [PubMed] [Google Scholar]
- 67.Hiki N., Kaminishi M., Yasuda K., Uedo N., Kobari M., Sakai T., Hiratsuka T., Ohno K., Honjo H., Nomura S., et al. Multicenter phase II randomized study evaluating dose-response of antiperistaltic effect of L-menthol sprayed onto the gastric mucosa for upper gastrointestinal endoscopy. Dig. Endosc. 2012;24:79–86. doi: 10.1111/j.1443-1661.2011.01163.x. [DOI] [PubMed] [Google Scholar]
- 68.Yamamoto N., Nakai Y., Sasahira N., Hirano K., Tsujino T., Isayama H., Komatsu Y., Tada M., Yoshida H., Kawabe T., et al. Efficacy of peppermint oil as an antispasmodic during endoscopic retrograde cholangiopancreatography. J. Gastroenterol. Hepatol. 2006;21:1394–1398. doi: 10.1111/j.1440-1746.2006.04307.x. [DOI] [PubMed] [Google Scholar]
- 69.Bezerra Alves J.G., de Cássia Coelho Moraes de Brito R., Cavalcanti T.S. Effectiveness of Mentha piperita in the Treatment of Infantile Colic: A Crossover Study. Evid. Based Complement. Alternat. Med. 2012;2012:981352. doi: 10.1155/2012/981352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ghodsi Z., Asltoghiri M. The Effect of Fennel on Pain Quality, Symptoms, and Menstrual Duration in Primary Dysmenorrhea. J. Pediatr. Adolesc. Gynecol. 2014;27:283–286. doi: 10.1016/j.jpag.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 71.Chumpitazi B.P., Kearns G.L., Shulman R.J. Review article: The physiological effects and safety of peppermint oil and its efficacy in irritable bowel syndrome and other functional disorders. Aliment. Pharmacol. Ther. 2018;47:738–752. doi: 10.1111/apt.14519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Shams R., Copare J.L., Johnson D.A. Peppermint oil: Clinical uses in the treatment of gastrointestinal diseases. JSM Gastroenterol. Hepatol. 2015;3:1036. [Google Scholar]
- 73.Kuo I.Y., Ehrlich B.E. Signaling in Muscle Contraction. Cold Spring Harb. Perspect. Biol. 2015;7:a006023. doi: 10.1101/cshperspect.a006023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sanders K.M. Regulation of smooth muscle excitation and contraction. Neurogastroenterol. Motil. 2008;20:39–53. doi: 10.1111/j.1365-2982.2008.01108.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sanders K.M., Koh S.D., Ro S., Ward S.M. Regulation of gastrointestinal motility—insights from smooth muscle biology. Nat. Rev. Gastroenterol. Hepatol. 2012;9:633–645. doi: 10.1038/nrgastro.2012.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Evangelista S. Quaternary ammonium derivatives as spasmolytics for irritable bowel syndrome. Curr. Pharm. Des. 2004;10:3561–3568. doi: 10.2174/1381612043382972. [DOI] [PubMed] [Google Scholar]
- 77.Amato A., Liotta R., Mulè F. Effects of menthol on circular smooth muscle of human colon: Analysis of the mechanism of action. Eur. J. Pharmacol. 2014;740:295–301. doi: 10.1016/j.ejphar.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 78.Ramos-Filho A.C.S., Shah A., Augusto T.M., Barbosa G.O., Leiria L.O., de Carvalho H.F., Antunes E., Grant A.D. Menthol Inhibits Detrusor Contractility Independently of TRPM8 Activation. PLoS ONE. 2014;9:e111616. doi: 10.1371/journal.pone.0111616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Oz M., El Nebrisi E.G., Yang K.-H.S., Howarth F.C., Al Kury L.T. Cellular and Molecular Targets of Menthol Actions. Front. Pharmacol. 2017;8:472. doi: 10.3389/fphar.2017.00472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tian C., Zhu R., Zhu L., Qiu T., Cao Z., Kang T. Potassium Channels: Structures, Diseases, and Modulators. Chem. Biol. Drug Des. 2014;83:1–26. doi: 10.1111/cbdd.12237. [DOI] [PubMed] [Google Scholar]
- 81.Silva D.F., Araújo I.G.A., Albuquerque J.G.F., Porto D.L., Dias K.L.G., Cavalcante K.V.M., Veras R.C., Nunes X.P., Barbosa-Filho J.M., Araújo D.A.M., et al. Rotundifolone-Induced Relaxation is Mediated by BKCa Channel Activation and Cav Channel Inactivation. Basic Clin. Pharmacol. Toxicol. 2011;109:465–475. doi: 10.1111/j.1742-7843.2011.00749.x. [DOI] [PubMed] [Google Scholar]
- 82.Amato A., Serio R., Mulè F. Involvement of cholinergic nicotinic receptors in the menthol-induced gastric relaxation. Eur. J. Pharmacol. 2014;745:129–134. doi: 10.1016/j.ejphar.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 83.Lozon Y., Sultan A., Lansdell S.J., Prytkova T., Sadek B., Yang K.-H.S., Howarth F.C., Millar N.S., Oz M. Inhibition of human α7 nicotinic acetylcholine receptors by cyclic monoterpene carveol. Eur. J. Pharmacol. 2016;776:44–51. doi: 10.1016/j.ejphar.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 84.Leal-Cardoso J.H., Lahlou S., Coelho-de-Souza A.N., Criddle D.N., Pinto Duarte G.I.B., Santos M.A.V., Magalhães P.J.C. Inhibitory actions of eugenol on rat isolated ileum. Can. J. Physiol. Pharmacol. 2002;80:901–906. doi: 10.1139/y02-117. [DOI] [PubMed] [Google Scholar]
- 85.Dhifi W., Bellili S., Jazi S., Bahloul N., Mnif W., Dhifi W., Bellili S., Jazi S., Bahloul N., Mnif W. Essential Oils’ Chemical Characterization and Investigation of Some Biological Activities: A Critical Review. Medicines. 2016;3:25. doi: 10.3390/medicines3040025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Price S., Price L. Aromatherapy for Health Professionals. 3rd ed. Churchill Livingstone; London, UK: 2007. pp. 385–478. [Google Scholar]
- 87.Pelkonen O., Abass K., Wiesner J. Thujone and thujone-containing herbal medicinal and botanical products: Toxicological assessment. Regul. Toxicol. Pharmacol. 2013;65:100–107. doi: 10.1016/j.yrtph.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 88.Aprotosoaie A.C., Hăncianu M., Costache I.-I., Miron A. Linalool: A review on a key odorant molecule with valuable biological properties. Flavour Fragr. J. 2014;29:193–219. doi: 10.1002/ffj.3197. [DOI] [Google Scholar]
- 89.Caputo L., Souza L.F., Alloisio S., Cornara L., De Feo V. Coriandrum sativum and Lavandula angustifolia essential oils: Chemical composition and activity on central nervous system. Int. J. Mol. Sci. 2016;17:1999. doi: 10.3390/ijms17121999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lima C.C., Criddle D.N., Coelho-de-Souza A.N., Monte F.J.Q., Jaffar M., Leal-Cardoso J.H. Relaxant and Antispasmodic Actions of Methyleugenol on Guinea-Pig Isolated Ileum. Planta Med. 2000;66:408–411. doi: 10.1055/s-2000-8594. [DOI] [PubMed] [Google Scholar]
- 91.Sousa P.J.C., Linard C.F.B.M., Azevedo-Batista D., Oliveira A.C., Coelho-de-Souza A.N., Leal-Cardoso J.H. Antinociceptive effects of the essential oil of Mentha x villosa leaf and its major constituent piperitenone oxide in mice. Brazilian J. Med. Biol. Res. 2009;42:655–659. doi: 10.1590/S0100-879X2009000700010. [DOI] [PubMed] [Google Scholar]
- 92.Bowles E.J. The Chemistry of Aromatherapeutic Oils. 3rd ed. Allen & Unwin; Crows Nest, Australia: 2003. pp. 1–256. [Google Scholar]
- 93.Ansari S.H., Ali M., Qadry J.S. Essential oils of Pistacia integerrima galls and their effect on the central nervous system. Pharm. Biol. 1993;31:89–95. doi: 10.3109/13880209309082924. [DOI] [Google Scholar]
- 94.Shirole R.L., Shirole N.L., Kshatriya A.A., Kulkarni R., Saraf M.N. Investigation into the mechanism of action of essential oil of Pistacia integerrima for its antiasthmatic activity. J. Ethnopharmacol. 2014;153:541–551. doi: 10.1016/j.jep.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 95.Rauf A. Chemical composition and biological screening of essential oils from Pistacia integerrima. African J. Pharm. Pharmacol. 2014;7:1220–1224. doi: 10.5897/AJPP2013.3467. [DOI] [Google Scholar]
- 96.Benini C., Mahy G., Bizoux J.-P., Wathelet J.-P., du Jardin P., Brostaux Y., Fauconnier M.-L. Comparative Chemical and Molecular Variability of Cananga odorata (Lam.) Hook.f. & Thomson forma genuina (Ylang-Ylang) in the Western Indian Ocean Islands: Implication for Valorization. Chem. Biodivers. 2012;9:1389–1402. doi: 10.1002/cbdv.201100306. [DOI] [PubMed] [Google Scholar]
- 97.Brokl M., Fauconnier M.-L., Benini C., Lognay G., Jardin P., Focant J.-F. Improvement of Ylang-Ylang Essential Oil Characterization by GC×GC-TOFMS. Molecules. 2013;18:1783–1797. doi: 10.3390/molecules18021783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tan L.T.H., Lee L.H., Yin W.F., Chan C.K., Abdul Kadir H., Chan K.G., Goh B.H. Traditional Uses, Phytochemistry, and Bioactivities of Cananga odorata (Ylang-Ylang) Evid. Based Complement. Alternat. Med. 2015;896314:1–30. doi: 10.1155/2015/896314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Preedy V.R. Essential oils in food preservation, flavor and safety. Elsevier; New York, USA: 2016. p. 895. [Google Scholar]
- 100.Moura A.P.G., Beltrão D.M., Pita J.C.L.R., Xavier A.L., Brito M.T., de Sousa T.K.G., Batista L.M., de Carvalho J.E., Ruiz A.L.T.G., Della Torre A., et al. Essential oil from fruit of Xylopia langsdorffiana: Antitumour activity and toxicity. Pharm. Biol. 2016;54:3093–3102. doi: 10.1080/13880209.2016.1211154. [DOI] [PubMed] [Google Scholar]
- 101.Rana V.S., Blazquez M.A. Chemical Composition of the Essential Oil of Anethum graveolens Aerial Parts. J. Essent. Oil Bear. Plants. 2014;17:1219–1223. doi: 10.1080/0972060X.2014.894894. [DOI] [Google Scholar]
- 102.Kazemi M., Abdossi V. Chemical composition of the essential oils of Anethum graveolens L. Bangladesh J. Bot. 2015;44:159–161. doi: 10.3329/bjb.v44i1.22742. [DOI] [Google Scholar]
- 103.Stanojević L.P., Stanković M.Z., Cvetković D.J., Danilović B.R., Stanojević J.S. Dill (Anethum graveolens L) seeds essential oil as a potential natural antioxidant and antimicrobial agent. Biol. Nyssana. 2016;7:31–39. doi: 10.5281/zenodo.159101. [DOI] [Google Scholar]
- 104.Rãdulescu V., Popescu M.L., Ilieş D.C. Chemical composition of the volatile oil from different plant parts of Anethum graveolens L. (Umbelliferae) cultivated in Romania. Farmacia. 2010;58:594–600. [Google Scholar]
- 105.Mahran G.H., Kadry H.A., Thabet C.K., El-Olemy M.M., Al-Azizi M.M., Schiff P.L., Wong L.K., Liv N. GC/MS Analysis of Volatile Oil of Fruits of Anethum graveolens. Int. J. Pharmacogn. 1992;30:139–144. doi: 10.3109/13880209209053978. [DOI] [Google Scholar]
- 106.Charles D.J., Simon J.E., Widrlechner M.P. Characterization of Essential Oil of Dill (Anethum graveolens L.) J. Essent. Oil Res. 1995;7:11–20. doi: 10.1080/10412905.1995.9698456. [DOI] [Google Scholar]
- 107.Chahal K.K., Kumar A., Bhardwaj U., Kaur R. Chemistry and biological activities of Anethum graveolens L. ( dill ) essential oil: A review. J. Pharmacogn. Phytochem. 2017;6:295–306. [Google Scholar]
- 108.Ahl H.A.H.S., Sarhan A.M., Dahab A., Dahab M.A. Essential Oils of Anethum graveolens L.: Chemical Composition and Their Antimicrobial Activities at Vegetative, Flowering and Fruiting Stages of Essential Oils of Anethum graveolens L.: Chemical Composition and Their Antimicrobial Activities at Vegetat. Int. J. Plant Res. 2015;1:98–102. [Google Scholar]
- 109.Meshkatalsadat M.H., Salahvarzi S., Aminiradpoor R., Abdollahi A. Identification of essential oil constituents of caraway (Carum carvi) using ultrasonic assist with headspace solid phase microextraction (UA-HS-SPME) Dig. J. Nanomater. Bios. 2012;7:637–640. [Google Scholar]
- 110.Raal A., Arak E., Orav A. The content and composition of the essential oil found in Carum carvi L. commercial fruits obtained from different countries. J. Essent. Oil Res. 2012;24:53–59. doi: 10.1080/10412905.2012.646016. [DOI] [Google Scholar]
- 111.Sedláková J., Kocourková B., Lojková L., Kubáň V. The essential oil content in caraway species (Carum carvi L.) Hortic. Sci. 2018;30:73–79. doi: 10.17221/3818-HORTSCI. [DOI] [Google Scholar]
- 112.Orav A., Arak E., Raal A. Essential Oil Composition of Coriandrum sativum L. Fruits from Different Countries. J. Essent. Oil-Bear. Plants. 2011;14:118–123. doi: 10.1080/0972060X.2011.10643910. [DOI] [Google Scholar]
- 113.Mandal S., Mandal M. Coriander (Coriandrum sativum L.) essential oil: Chemistry and biological activity. Asian Pac. J. Trop. Biomed. 2015;5:421–428. doi: 10.1016/j.apjtb.2015.04.001. [DOI] [Google Scholar]
- 114.Stefanini, Ming L.C., Marques M., Meireles M.A.A., Moura L.S. Marchese Seed productivity, yield and composition of the essential oil of fennel Foeniculum vulgare var. dulcis in the season of the year. A Rev. Bras. Plantas Med. 2006;8:86–90. [Google Scholar]
- 115.Hammouda F., Saleh M., Abdel-Azim N., Shams K., Ismail S., Shahat A., Saleh I. Evaluation Of The Essential Oil Of Foeniculum Vulgare Mill (Fennel) Fruits Extracted By Three Different Extraction Methods By GC/MS. African J. Tradit. Complement. Altern. Med. 2014;11:277–279. doi: 10.4314/ajtcam.v11i2.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Miguel M.G., Cruz C., Faleiro L., Simões M.T.F., Figueiredo A.C., Barroso J.G., Pedro L.G. Foeniculum vulgare essential oils: Chemical composition, antioxidant and antimicrobial activities. Nat. Prod. Commun. 2010;5:319–328. doi: 10.1177/1934578X1000500231. [DOI] [PubMed] [Google Scholar]
- 117.Marín I., Sayas-Barberá E., Viuda-Martos M., Navarro C., Sendra E. Chemical Composition, Antioxidant and Antimicrobial Activity of Essential Oils from Organic Fennel, Parsley, and Lavender from Spain. Foods. 2016;5:18. doi: 10.3390/foods5010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Aprotosoaie A.C., Spac A., Hancianu M., Miron A., Tanasescu V.F., Dorneanu V., Stanescu U. The chemical profile of essential oils obtained from fennel fruits (Foeniculum vulgare Mill.) Farmacia. 2010;58:46–53. [Google Scholar]
- 119.Orav A., Raal A., Arak E. Essential oil composition of Pimpinella anisum L. fruits from various European countries. Nat. Prod. Res. 2008;22:227–232. doi: 10.1080/14786410701424667. [DOI] [PubMed] [Google Scholar]
- 120.Özcan M.M., Chalchat J.C. Chemical composition and antifungal effect of anise (Pimpinella anisum L.) fruit oil at ripening stage. Ann. Microbiol. 2006;56:353–358. doi: 10.1007/BF03175031. [DOI] [Google Scholar]
- 121.Saibi S., Belhadj M., Benyoussef E.-H. Essential Oil Composition of Pimpinella anisum from Algeria. Anal. Chem. Lett. 2012;2:401–404. doi: 10.1080/22297928.2012.10662624. [DOI] [Google Scholar]
- 122.Punetha V.D. Essential oil composition of Acorus calamus from district - Pithoragarh, Uttarakhad, India. World J. Pharm. Res. 2015;4:1158–1166. [Google Scholar]
- 123.Raina V.K., Srivastava S.K., Syamasunder K.V. Essential oil composition of Acorus calamus L. from the lower region of the Himalayas. Flavour Fragr. J. 2003;18:18–20. doi: 10.1002/ffj.1136. [DOI] [Google Scholar]
- 124.Liu X.C., Zhou L.G., Liu Z.L., Du S.S. Identification of insecticidal constituents of the essential oil of Acorus calamus rhizomes against Liposcelis bostrychophila badonnel. Molecules. 2013;18:5684–5696. doi: 10.3390/molecules18055684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Verma R.S., Padalia R.C., Chauhan A. Chemical Composition of Root Essential Oil of Acorus calamus L. Natl. Acad. Sci. Lett. 2015;38:121–125. doi: 10.1007/s40009-014-0304-x. [DOI] [Google Scholar]
- 126.Lohani H., Andola H.C., Chauhan N., Bhandari U. Variations of Essential oil composition of Acorus calamus from Uttarakhand Himalaya. J. Pharm. Res. 2012;5:1246–1247. [Google Scholar]
- 127.Ayoughi F., Barzegar M., Sahari M.A., Naghdibadi H. Chemical compositions of essential oils of Artemisia dracunculus L. and endemic Matricaria chamomilla L. and an evaluation of their antioxidative effects. J. Agric. Sci. Technol. 2011;13:79–88. [Google Scholar]
- 128.Verma M.K., Anand R., Chisti A.M., Kitchlu S., Chandra S., Shawl A.S., Khajuria R.K. Essential oil composition of Artemisia dracunculus L. (tarragon) growing in Kashmir -India. J. Essent. Oil-Bear. Plants. 2010;13:331–335. doi: 10.1080/0972060X.2010.10643830. [DOI] [Google Scholar]
- 129.Asili J., Rajabian A., Tayarani-Najaran Z., Rahimzadeh Oskooie R., Emami S.A., Hassanzadeh Khayyat M. Phytochemical Evaluation and Antioxidant Activity of Essential Oil, and Aqueous and Organic Extracts of Artemisia dracunculus. Jundishapur J. Nat. Pharm. Prod. 2017;12:e32325. doi: 10.5812/jjnpp.32325. [DOI] [Google Scholar]
- 130.Sayyah M., Nadjafnia L., Kamalinejad M. Anticonvulsant activity and chemical composition of Artemisia dracunculus L. essential oil. J. Ethnopharmacol. 2004;94:283–287. doi: 10.1016/j.jep.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 131.Obolskiy D., Pischel I., Feistel B., Glotov N., Heinrich M. Artemisia dracunculus L. (Tarragon): A Critical Review of Its Traditional Use, Chemical Composition, Pharmacology, and Safety. J Agric Food Chem. 2011;59:11367–11384. doi: 10.1021/jf202277w. [DOI] [PubMed] [Google Scholar]
- 132.Irfan-ur-Rauf T., Dawood M., Ganai B.A., Chishti M.Z., Fayaz A., Jehangir S.D. Phytochemical studies on the extract and essential oils of Artemisia dracunculus L. (Tarragon) African J. Plant Sci. 2014;8:72–75. doi: 10.5897/AJPS2013.1145. [DOI] [Google Scholar]
- 133.Srivastava J.K., Shankar E., Gupta S. Chamomile: A herbal medicine of the past with bright future. Mol. Med. Rep. 2010;3:895–901. doi: 10.3892/mmr.2010.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Gardiner P. Complementary, holistic, and integrative medicine: Chamomile. Pediatr. Rev. 2007;28:e16-8. doi: 10.1542/pir.28-4-e16. [DOI] [PubMed] [Google Scholar]
- 135.Sharafzadeh S., Alizadeh O. German and roman chamomile. J. Appl. Pharm. Sci. 2011;1:1–5. [Google Scholar]
- 136.Aremu O.O., Tata C.M., Sewani-rusike C.R. Phytochemical composition, and analgesic and anti- inflammatory properties of essential oil of Chamaemelum nobile (Asteraceae L All) in rodents. Trop. J. Pharm. Res. 2018;17:1939–1945. doi: 10.4314/tjpr.v17i10.7. [DOI] [Google Scholar]
- 137.De Groot A.C., Schmidt E. Essential Oils, Part III: Chemical Composition. Dermatitis. 2016;27:161–169. doi: 10.1097/DER.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 138.Al-snafi A.E. Medical importance of Anthemis nobilis (Chamaemelum nobile)—A review. Asian J. Pharm. Sci. Technol. 2016;6:89–95. [Google Scholar]
- 139.Cárdenas-Ortega N.C., Zavala-Sánchez M.A., Aguirre-Rivera J.R., Pérez-González C., Pérez-Gutiérrez S. Chemical Composition and Antifungal Activity of Essential Oil of Chrysactinia mexicana Gray. J. Agric. Food Chem. 2005;53:4347–4349. doi: 10.1021/jf040372h. [DOI] [PubMed] [Google Scholar]
- 140.Pérez-Vásquez A., Capella S., Linares E., Bye R., Angeles-López G., Mata R. Antimicrobial activity and chemical composition of the essential oil of Hofmeisteria schaffneri. J. Pharm. Pharmacol. 2011;63:579–586. doi: 10.1111/j.2042-7158.2010.01243.x. [DOI] [PubMed] [Google Scholar]
- 141.Mousavi E.S., Dehghanzadeh H., Abdali A. Chemical Composition and Essential Oils of Pelargonium graveolens (Geraniaceae) By Gas Chromatography—Mass Spectrometry (GC/MS) Bull. Env. Pharmacol. Life Sci. 2014;3:182–184. [Google Scholar]
- 142.Boukhris M., Simmonds M.S.J., Sayadi S., Bouaziz M. Chemical Composition and Biological Activities of Polar Extracts and Essential Oil of Rose-scented Geranium, Pelargonium graveolens. Phytother. Res. 2013;27:1206–1213. doi: 10.1002/ptr.4853. [DOI] [PubMed] [Google Scholar]
- 143.Rana V.S., Juyal J.P., Amparo Blazquez M. Chemical constituents of essential oil of Pelargonium graveolens leaves. Int. J. Aromather. 2002;12:216–218. doi: 10.1016/S0962-4562(03)00003-1. [DOI] [Google Scholar]
- 144.Sharopov F.S., Zhang H., Setzer W.N. Composition of geranium (Pelargonium graveolens) essential oil from Tajikistan. Am. J. Essent. Oils Nat. Prod. 2014;2:13–16. [Google Scholar]
- 145.Tarakemeh A., Rowshan V., Najafian S. Essential Oil Content and Composition of Lavandula Angustifolia Mill. as Affected by Drying Method and Extraction Time. Anal. Chem. Lett. 2013;2:244–249. doi: 10.1080/22297928.2012.10648276. [DOI] [Google Scholar]
- 146.Mirensha, Wang X., Zhi L., Cong Y., Abulizi P. Chemical composition of the essential oil of Lavandula angustifolia from Xinjiang, China. Chem. Nat. Compd. 2009;44:810. doi: 10.1007/s10600-009-9210-8. [DOI] [Google Scholar]
- 147.Smigielski K., Prusinowska R., Stobiecka A., Kunicka-Styczyñska A., Gruska R. Biological Properties and Chemical Composition of Essential Oils from Flowers and Aerial Parts of Lavender (Lavandula angustifolia) J. Essent. Oil-Bear. Plants. 2018;21:1303–1314. doi: 10.1080/0972060X.2018.1503068. [DOI] [Google Scholar]
- 148.Şerban E.S., Socaci S.A., Tofană M., Maier S.C., Bojiţă M.T. Chemical composition of some essential oils of Lamiaceae family. Clujul Med. 2010;LXXXIII:286–289. [Google Scholar]
- 149.Abdellatif F., Hassani A. Chemical composition of the essential oils from leaves of Melissa officinalis extracted by hydrodistillation, steam distillation, organic solvent and microwave hydrodistillation. J. Mater. Environ. Sci. 2015;6:207–213. [Google Scholar]
- 150.Verma R.S., Padalia R.C., Chauhan A. Evaluation of essential oil quality of lemon balm ( Melissa officinalis L.) grown in two locations of northern India. J. Essent. Oil Res. 2015;27:412–416. doi: 10.1080/10412905.2015.1015692. [DOI] [Google Scholar]
- 151.Chizzola R., Lohwasser U., Franz C. Biodiversity within Melissa officinalis: Variability of Bioactive Compounds in a Cultivated Collection. Molecules. 2018;23:294. doi: 10.3390/molecules23020294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Efremov A.A., Zykova I.D., Gorbachev A.E. Composition of the essential oil from the lemon balm growing in the neighborhood of Krasnoyarsk as indicated by gas chromatography–mass spectrometry data. Russ. J. Bioorganic Chem. 2017;42:726–729. doi: 10.1134/S1068162016070049. [DOI] [Google Scholar]
- 153.Taherpour A.A., Khaef S., Yari A., Nikeafshar S., Fathi M., Ghambari S. Chemical composition analysis of the essential oil of Mentha piperita L. from Kermanshah, Iran by hydrodistillation and HS/SPME methods. J. Anal. Sci. Technol. 2017;8:11. doi: 10.1186/s40543-017-0122-0. [DOI] [Google Scholar]
- 154.Moghaddam M., Pourbaige M., Tabar H.K., Farhadi N., Hosseini S.M.A. Composition and Antifungal Activity of Peppermint (Mentha piperita) Essential Oil from Iran. J. Essent. Oil-Bear. Plants. 2013;16:506–512. doi: 10.1080/0972060X.2013.813265. [DOI] [Google Scholar]
- 155.Shahi A.K., Chandra S., Dutt P., Kaul B.L., Tava A., Avato P. Essential oil composition of Mentha x piperita L. from different environments of north India. Flavour Fragr. J. 1999;14:5–8. doi: 10.1002/(SICI)1099-1026(199901/02)14:1<5::AID-FFJ768>3.0.CO;2-3. [DOI] [Google Scholar]
- 156.Ainane A. Chemical Study by GC-MS of the Essential Oils of Certain Mints Grown In the Region of Settat (Morocco): Mentha Piperita, Mentha Pulegium and Mentha Spicata. Drug Des. Intellect. Prop. Int. J. 2018;1:124–127. doi: 10.32474/DDIPIJ.2018.01.000120. [DOI] [Google Scholar]
- 157.Hussain A.I., Anwar F., Shahid M., Ashraf M., Przybylski R. Chemical Composition, and Antioxidant and Antimicrobial Activities of Essential Oil of Spearmint ( Mentha spicata L.) From Pakistan. J. Essent. Oil Res. 2010;22:78–84. doi: 10.1080/10412905.2010.9700269. [DOI] [Google Scholar]
- 158.Snoussi M., Noumi E., Trabelsi N., Flamini G., Papetti A., De Feo V. Mentha spicata essential oil: Chemical composition, antioxidant and antibacterial activities against planktonic and biofilm cultures of vibrio spp. strains. Molecules. 2015;20:14402–14424. doi: 10.3390/molecules200814402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Lahlou S., Carneiro-Leão R.F.L., Leal-Cardoso J.H., Toscano C.F. Cardiovascular Effects of the Essential Oil of Mentha x villosa and its Main Constituent, Piperitenone Oxide, in Normotensive Anaesthetised Rats: Role of the Autonomic Nervous System. Planta Med. 2001;67:638–643. doi: 10.1055/s-2001-17352. [DOI] [PubMed] [Google Scholar]
- 160.Lima T.C., da Silva T.K.M., Silva F.L., Barbosa-Filho J.M., Marques M.O.M., Santos R.L.C., de Holanda Cavalcanti S.C., de Sousa D.P. Larvicidal activity of Mentha x villosa Hudson essential oil, rotundifolone and derivatives. Chemosphere. 2014;104:37–43. doi: 10.1016/j.chemosphere.2013.10.035. [DOI] [PubMed] [Google Scholar]
- 161.Fogaca R.T.H., Cavalcante A.D.A., Serpa A.K.L., Sousa P.J.C., Coelho-de-Souza A.N., Leal-Cardoso J.H. The effects of essential oil of Mentha x villosa on skeletal muscle of the toad. Phytother. Res. 1997;11:552–557. doi: 10.1002/(SICI)1099-1573(199712)11:8<552::AID-PTR154>3.0.CO;2-N. [DOI] [Google Scholar]
- 162.Pandey A.K., Singh P., Tripathi N.N. Chemistry and bioactivities of essential oils of some Ocimum species: An overview. Asian Pac. J. Trop. Biomed. 2014;4:682–694. doi: 10.12980/APJTB.4.2014C77. [DOI] [Google Scholar]
- 163.Costa L.C.B., Pinto J.E.B.P., Castro E.M., Alves E., Rosal L.F., Bertolucci S.K.V., Alves P.B., Evangelino T.S. Yield and Composition of the Essential Oil of Ocimum selloi Benth. Cultivated Under Colored Netting. J. Essent. Oil Res. 2010;22:34–39. doi: 10.1080/10412905.2010.9700260. [DOI] [Google Scholar]
- 164.Moraes L.A.S., Facanali R., Marques M.O.M., Lin C.M., Meireles M.A.A. Phytochemical characterization of essential oil from Ocimum selloi. An. Acad. Bras. Cienc. 2002;74:183–186. doi: 10.1590/S0001-37652002000100014. [DOI] [PubMed] [Google Scholar]
- 165.Chimnoi N., Reuk-ngam N., Chuysinuan P., Khlaychan P., Khunnawutmanotham N., Chokchaichamnankit D., Thamniyom W., Klayraung S., Mahidol C., Techasakul S. Characterization of essential oil from Ocimum gratissimum leaves: Antibacterial and mode of action against selected gastroenteritis pathogens. Microb. Pathog. 2018;118:290–300. doi: 10.1016/j.micpath.2018.03.041. [DOI] [PubMed] [Google Scholar]
- 166.Madeira S.V.F., Rabelo M., Soares P.M.G., Souza E.P., Meireles A.V.P., Montenegro C., Lima R.F., Assreuy A.M.S., Criddle D.N. Temporal variation of chemical composition and relaxant action of the essential oil of Ocimum gratissimum L. (Labiatae) on guinea-pig ileum. Phytomedicine. 2005;12:506–509. doi: 10.1016/j.phymed.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 167.Rus C., POP G., Alexa E., Renata M.S., Dana M.C. Antifungal activity and chemical composition of Origanum majorana L. essential oil. Res. J. Agric. Sci. 2015;47:179–185. [Google Scholar]
- 168.Komaitis M.E., Ifanti-Papatragianni N., Melissari-Panagiotou E. Composition of the essential oil of marjoram (Origanum majorana L.) Food Chem. 1992;45:117–118. doi: 10.1016/0308-8146(92)90020-3. [DOI] [Google Scholar]
- 169.Brada M., Saadi A., Wathelet J.P., Lognay G. The essential oils of Origanum majorana l. and Origanum floribundum munby in Algeria. J. Essent. Oil-Bear. Plants. 2012;15:497–502. doi: 10.1080/0972060X.2012.10644078. [DOI] [Google Scholar]
- 170.Raina A.P., Negi K.S. Essential oil composition of Origanum majorana and Origanum vulgare ssp. hirtum growing in India. Chem. Nat. Compd. 2012;47:1015–1017. doi: 10.1007/s10600-012-0133-4. [DOI] [Google Scholar]
- 171.Bağci Y., Kan Y., Doğu S., Çelik S.A. The essential oil compositions of Origanum majorana L. cultivated in Konya and collected from Mersin-Turkey. Indian J. Pharm. Educ. Res. 2017;51:S463–S469. doi: 10.5530/ijper.51.3s.68. [DOI] [Google Scholar]
- 172.Alasbahi R., Melzig M. Plectranthus barbatus: A Review of Phytochemistry, Ethnobotanical Uses and Pharmacology – Part 1. Planta Med. 2010;76:653–661. doi: 10.1055/s-0029-1240898. [DOI] [PubMed] [Google Scholar]
- 173.Kerntopf M.R., de Albuquerque R.L., Machado M.I.L., Matos F.J.A., Craveiro A.A. Essential Oils from Leaves, Stems and Roots of Plectranthus barbatus Andr. (Labiatae) Grown in Brazil. J. Essent. Oil Res. 2002;14:101–102. doi: 10.1080/10412905.2002.9699783. [DOI] [Google Scholar]
- 174.Galvão Rodrigues F.F., Costa J.G.M., Rodrigues F.F.G., Campos A.R. Study of the Interference between Plectranthus Species Essential Oils from Brazil and Aminoglycosides. Evid. Based. Complement. Alternat. Med. 2013;724161:1–7. doi: 10.1155/2013/724161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Adel K., Zied Z., Ben Choba I., Bekir A., Gharsallah N., Damak M., Gdoura R. Chemical constituents and antioxidant properties of Rosmarinus officinalis L. essential oil cultivated from the South-Western of Tunisia. J. Med. Plants Res. 2011;5:5999–6004. doi: 10.5897/jmpr11.423. [DOI] [Google Scholar]
- 176.Belkhodja H., Meddah B., Touil A.T., Şekeroğlu N., Sonnet P. Chemical Composition and Properties of Essential Oil of Rosmarinus Officinalis and Populus Alba. World J. Pharm. Pharm. Sci. 2016;5041:108–119. doi: 10.20959/wjpps20169-7558. [DOI] [Google Scholar]
- 177.Satyal P., Jones T.H., Lopez E.M., McFeeters R.L., Ali N.A.A., Mansi I., Al-Kaf A.G., Setzer W.N. Chemotypic Characterization and Biological Activity of Rosmarinus officinalis. Foods. 2017;6:20. doi: 10.3390/foods6030020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Gezici S., Karik U., Sekeroglu N., Tuncturk M., Cinar O. Essential Oil Composition of Some Sage (Salvia spp.) Species Cultivated in İzmir (Turkey) Ecological Conditions. Indian J. Pharm. Educ. Res. 2018;52:s102–s107. doi: 10.5530/ijper.52.4s.83. [DOI] [Google Scholar]
- 179.Khedher M.R.B., Khedher S.B., Chaieb I., Tounsi S., Hammami M. Chemical composition and biological activities of Salvia officinalis essential oil from Tunisia. EXCLI J. 2017;16:160–173. doi: 10.17179/excli2016-832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Mohammadhosseini M., Beiranvand M. Chemical Composition of the Essential Oil from the Aerial Parts of Satureja hortensis As a Potent Medical Plant Using Traditional Hydrodistillation. J. Chem. Health Risks. 2013;3:49–60. [Google Scholar]
- 181.Mihajilov-Krstev T., Radnović D., Kitić D., Zlatković B., Ristić M., Branković S. Chemical composition and antimicrobial activity of Satureja hortensis L. essential oil. Open Life Sci. 2009;4:411–416. doi: 10.2478/s11535-009-0027-z. [DOI] [Google Scholar]
- 182.Matasyoh J., Wagara I., Nakavuma J., Kiburai A. Chemical composition of Cymbopogon citratus essential oil and its effect on mycotoxigenic Aspergillus species. African J. Food Sci. 2011;5:138–142. [Google Scholar]
- 183.Mohamed Hanaa A.R., Sallam Y.I., El-Leithy A.S., Aly S.E. Lemongrass (Cymbopogon citratus) essential oil as affected by drying methods. Ann. Agric. Sci. 2012;57:113–116. doi: 10.1016/j.aoas.2012.08.004. [DOI] [Google Scholar]
- 184.Machraoui M., Kthiri Z., Ben Jabeur M., Hamada W. Ethnobotanical and phytopharmacological notes on Cymbopogon citratus ( DC.) Stapf. J. New Sci. Agric. Biotechnol. 2018;55:3642–3652. [Google Scholar]
- 185.Akhila A. Essential Oil-Bearing Grasses: The genus Cymbopogon. CRC Press; Boca Raton, FL, USA: 2010. p. 284. [Google Scholar]
- 186.Raina V.K., Srivastava S.K., Aggarwal K.K., Syamasundar K.V., Khanuja S.P.S. Essential oil composition of Cymbopogon martinii from different places in India. Flavour Fragr. J. 2003;18:312–315. doi: 10.1002/ffj.1222. [DOI] [Google Scholar]
- 187.Gupta R., Mallavarapu G.R., Ramesh S., Kumar S. Composition of flower essential oils of Rosa damascena and Rosa indica grown in Lucknow. J. Med. Aromat. Plant Sci. 2000;22:9–12. [Google Scholar]
- 188.Dugo G., Mondello L. Citrus oils: Composition, advanced analytical techniques, contaminants, and biological activity. CRC Press; Boca Raton, FL, USA: 2011. p. 642. [Google Scholar]
- 189.Garza-González E., Alvarez L., Sandoval-Montemayor N.E., del Rayo Camacho-Corona M., García A., Elizondo-Treviño E. Chemical Composition of Hexane Extract of Citrus aurantifolia and Anti-Mycobacterium tuberculosis Activity of Some of Its Constituents. Molecules. 2012;17:11173–11184. doi: 10.3390/molecules170911173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Azar P.A., Nekoei M., Larijani K., Bahraminasab S. Chemical composition of the essential oils of Citrus sinensis cv. Valencia and a quantitative structure-retention relationship study for the prediction of retention indices by multiple linear regression. J. Serbian Chem. Soc. 2011;76:1627–1637. doi: 10.2298/JSC101218141A. [DOI] [Google Scholar]
- 191.Njoroge S.M., Phi N.T.L., Sawamura M. Chemical Composition of Peel Essential Oils of Sweet Oranges (Citrus sinensis) from Uganda and Rwanda. J. Essent. Oil-Bear. Plants. 2009;12:26–33. doi: 10.1080/0972060X.2009.10643687. [DOI] [Google Scholar]
- 192.Mamun-Or-Rashid A.N.M., Sen M.K., Jamal M.A.H.M., Nasrin S. A Comprehensive Ethnopharmacological Review on Lippia Alba M. Int. J. Biomed. Mater. Res. 2014;1:14–20. doi: 10.11648/j.ijbmr.20130101.13. [DOI] [Google Scholar]
- 193.Juiz P.J.L., Lucchese A.M., Gambari R., Piva R., Penolazzi L., Di Ciano M., Uetanabaro A.P.T., Silva F., Avila-Campos M.J. Essential oils and isolated compounds from Lippia alba leaves and flowers: Antimicrobial activity and osteoclast apoptosis. Int. J. Mol. Med. 2015;35:211–217. doi: 10.3892/ijmm.2014.1995. [DOI] [PubMed] [Google Scholar]
- 194.Machado T.F., Nogueira N.A.P., de Cássia Alves Pereira R., de Sousa C.T., Batista V.C.V. The antimicrobial efficacy of Lippia alba essential oil and its interaction with food ingredients. Braz. J. Microbiol. 2014;45:699–705. doi: 10.1590/S1517-83822014000200045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Glamočlija J., Soković M., Tešević V., Linde G.A., Colauto N.B. Chemical characterization of Lippia alba essential oil: An alternative to control green molds. Braz. J. Microbiol. 2011;42:1537–1546. doi: 10.1590/S1517-83822011000400041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Silva S.G., da Costa R.A., de Oliveira M.S., da Cruz J.N., Figueiredo P.L.B., Brasil D.D.S.B., Nascimento L.D., Chaves Neto A.M.D.J., de Carvalho Junior R.N., Andrade E.H.D.A. Chemical profile of Lippia thymoides, evaluation of the acetylcholinesterase inhibitory activity of its essential oil, and molecular docking and molecular dynamics simulations. PLoS ONE. 2019;14:e0213393. doi: 10.1371/journal.pone.0213393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Silva F.S., Menezes P.M.N., de Sá P.G.S., Oliveira A.L.D.S., Souza E.A.A., Almeida J.R.G.D.S., de Lima J.T., Uetanabaro A.P.T., Silva T.R.D.S., Peralta E.D., et al. Chemical composition and pharmacological properties of the essential oils obtained seasonally from Lippia thymoides. Pharm. Biol. 2016;54:25–34. doi: 10.3109/13880209.2015.1005751. [DOI] [PubMed] [Google Scholar]
- 198.Mahmud S. Composition of essential oil of Elettaria cardamomum Maton leaves. Pak. J. Sci. 2008;60:111–114. [Google Scholar]
- 199.Leela N.K., Prasath D., Venugopal M.N. Essential oil composition of selected cardamom genotypes at different maturity levels. Indian J. Hortic. 2008;65:366–369. [Google Scholar]
- 200.Masoumi-Ardakani Y., Mandegary A., Esmaeilpour K., Najafipour H., Sharififar F., Pakravanan M., Ghazvini H. Chemical Composition, Anticonvulsant Activity, and Toxicity of Essential Oil and Methanolic Extract of Elettaria cardamomum. Planta Med. 2016;82:1482–1486. doi: 10.1055/s-0042-106971. [DOI] [PubMed] [Google Scholar]
- 201.Noumi E., Snoussi M., Alreshidi M.M., Rekha P.-D., Saptami K., Caputo L., De Martino L., Souza L.F., Msaada K., Mancini E., et al. Chemical and Biological Evaluation of Essential Oils from Cardamom Species. Molecules. 2018;23:2818. doi: 10.3390/molecules23112818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Kumar A., Tandon S., Ahmad J., Yadav A., Kahol A.P. Essential Oil Composition of Seed and Fruit Coat of Elettaria cardamomum from South India. J. Essent. Oil-Bear. Plants. 2005;8:204–207. doi: 10.1080/0972060X.2005.10643446. [DOI] [Google Scholar]