Abstract
Introduction
There is growing recognition that health disparities research needs to incorporate social determinants in the local environment into explanatory models. In the transdisciplinary setting of the Mid-South Transdisciplinary Collaborative Center (TCC), the Social Determinants (SDH) Core developed an approach to incorporating SDH across a variety of studies. This placed- of Health based approach, which is geographically based, transdisciplinary, and inherently multilevel, is discussed.
Methods
From 2014 through 2016, the SDH Core consulted on a variety of Mid-South TCC approach used geospatial methods (e.g., geocoding) to link individual data files with measures of the physical and social environment in the SDH Core database. Once linked, the method permitted various types of analysis (e.g., multilevel analysis) to determine if racial disparities could be explained in terms of social determinants in the local environment.
Results
The SDH Core consulted on five Mid-South TCC research projects. In resulting analyses for all the studies, a significant portion of the variance in one or more outcomes was partially explained by a social determinant from the SDH Core database.
Conclusions
The SDH Core approach to addressing health disparities by linking neighborhood social and physical environment measures to an individual-level data file proved to be a successful approach across Mid-South TCC research projects.
INTRODUCTION
Two of the four overarching goals of the Healthy People 2020 initiative point to the role of place in dealing with health disparities.1 There is growing recognition that the rising prevalence of obesity in poor and minority populations is implicated in the persistent disparities of chronic disease among these populations.2,3 Despite growing awareness of the negative health impact of poor diet, physical inactivity, and excess weight, the prevalence of obesity among poor and minority populations has increased dramatically in the U.S.3,4 During the last three decades, according to national surveys (i.e., the National Health and Nutrition Examination Survey), the U.S. obesity rate among blacks has doubled in adults and tripled in children and adolescents.5–7 The consensus among public health experts is that human genomic differences are not responsible for the rapid rise in obesity and the explanation must lie with differences in environmental exposures that are socially determined.8,9 The purpose of the current study is to describe an approach to explaining health disparities in terms of social determinants in the context of a transdisciplinary center grant of the Mid-South Transdisciplinary Collaborative Center (TCC). Specifically, this paper discusses one component of the Social Determinants of Health (SDH) Core of the Mid-South TCC that consulted with new and ongoing center grant projects to assess the potential for incorporating SDH into their ongoing analyses.
The acknowledgement of the role of environmental factors in the obesity epidemic has led to a paradigm shift in thinking and research. The dominant, individually focused models of behavior change are not believed to be sufficient either to explain or address the epidemic.8,9 Instead, ecologic models, which acknowledge the role of neighborhood contexts and also take advantage of improved measurement methods, are advocated.10,11 Consequently, incorporating SDH disparities into ongoing Mid-South TCC studies represents a transdisciplinary approach that could also affect the design and conceptualization of these studies.
Although there is consensus on the general role of the local environment in its contribution to health disparities in general and the obesity epidemic in particular, there is little in the way of consensus on the relative contribution of any one social determinant (e.g., social or economic stress, access to medical care, nutritive stress), let alone the relative contribution of any specific neighborhood or community context (e.g., walkability).12–15 The lack of directly measured data on factors in the local environment that are aggregated at a useful areal unit of analysis is often a limitation in this literature.13 Furthermore, many studies of the role of the local environment in health disparities research have used national surveys that either use self-reports for key outcome variables like physical activity (e.g., the Behavioral Risk Factor Surveillance Survey) or do include direct measures (e.g., the National Health and Nutrition Examination Survey) but are structured to be representative at regional levels of aggregation rather than a local environment (e.g., neighborhood).16 The SDH Core acknowledged these issues in developing an approach that was at the same time transdisciplinary and pragmatic. The development of a database of commonly used measures assessing SDH in the neighborhood environment made possible SDH Core consultations to aid new and ongoing Mid-South TCC projects interested in incorporating these measures into their study designs.
CORE CONCEPTUAL MODEL
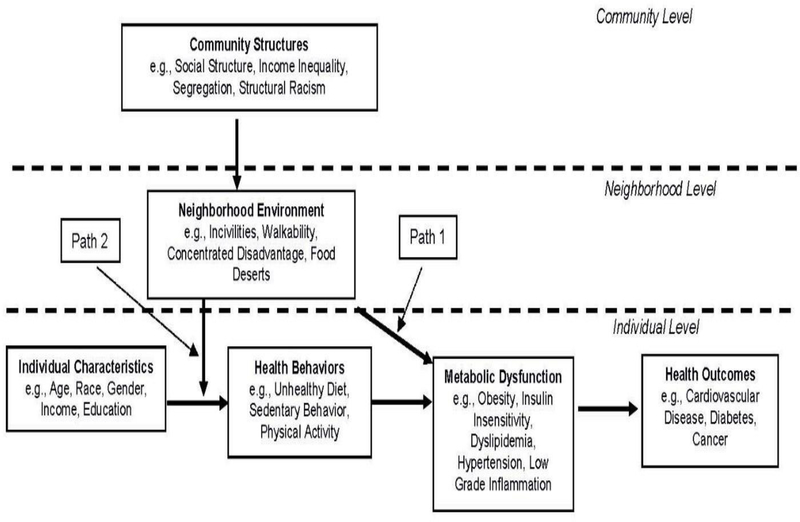
A conceptual model demonstrating multilevel character of the role of the place on health outcomes in the transdisciplinary context of Mid-South TCC research projects is provided in Figure 1. It derives from emerging frameworks that propose a place-based synthesis linking exposures, health behaviors, and genetic susceptibilities.17,18
Figure 1.
Conceptual model demonstrating the SDH Core approach to incorporating social determinants of health into Mid-South TCC research projects.
SDH, social determinants of health; TCC, Transdisciplinary Collaborative Center
It should be noted that, in the model, social determinants at the neighborhood level may affect individual outcomes through both a direct and an indirect path. The direct path operates through chronic exposure to social stressors leading to metabolic disturbances (i.e., elevated blood pressure, dyslipidemia, insulin resistance, and a chronic inflammatory state [Path 1 in Figure 1]).19,20 As the body tries to return a homeostatic balance, many physiologic processes are “reset” in a process known as allostatic load, first described by McEwen.21 The process of allostasis is believed to result in epigenetic changes that alter the expression of genes associated with the functioning of the hypothalamic–pituitary–adrenal axis and the sympathetic–adrenal–medullary axis, leading to metabolic dysfunction and chronic disease.19,22,23
The indirect path operates through the potential constraining effect of the neighborhood environment (e.g., food deserts) on behaviors related to diet and physical (Path 2 in Figure 1).24–26 Here, the effect on metabolic dysfunction is primarily due to chronic exposure to environments that constrain health behaviors associated with diet and physical activity, leading to obesity and metabolic dysfunction.27 This constraining mechanism is proposed by Glass and McAtee28 to explain the effects of SDH. Finally, the conceptual model assumes a multilevel structure of individuals nested within their neighborhood and community environments.
CORE CONSULTING
The process of introducing social determinants in the local environment into new and ongoing Mid-South TCC projects was accomplished through consults with individual researchers. Mid-South TCC researchers were informed about the SDH Core consulting through presentations at annual meetings, monthly conference calls, and the Mid-South TCC website. Only a portion of the consults were conducted with the goal of providing projects the opportunity to incorporate SDH into their research designs. It was a process the SDH Core termed “contextualization” for descriptive value with Mid-South TCC researchers. It should be noted that the term was not meant to suggest social determinant variables were necessarily “contextual” variables. Basically, the method was organized to provide any research project that met basic criteria the opportunity to incorporate social determinants into their ongoing studies. The basic criteria included:
availability of address identifiers for study participants;
a health outcome that demonstrates a disparity by race or ethnicity; and
a willingness to entertain the possibility that social determinants might explain the disparity.
Consults involved several meetings either in person or online. Typically, these meetings involved the exchange of data dictionaries, preliminary results, and research papers on the relevant topics.
Once the criteria were met, a two-step process of geocoding and spatial joining was conducted. Geocoding refers to the process by which a GIS assigns a longitude and latitude to a study participant’s residential address. The assigned longitude and latitude was then linked to the U.S. Census areal units (e.g., block group, Census tract) associated with that longitude and latitude.
Once the U.S. Census areal units were assigned, a spatial join could be conducted using the Federal Information Processing Standard code that identifies each areal unit. At this point, each participant would have a code for their Census tract of residence, for example, included in their data file. The spatial join then used the Federal Information Processing Standard code present in both the participant’s data file and the SDH Core database to merge the two data files. Once merged, the true Census tract was typically removed and a fictitious Census tract identifier added to the file for confidentiality purposes. The fictitious Census tract identifier was included to preserve the multilevel architecture of the data set. It should be noted that Census tract was typically used as the areal unit to approximate a neighborhood exposure. Census tracts are recognized as an effective, area-based measure of social risk.16 In addition, the U.S. Bureau of the Census designs the Census tract to be a “small, relatively permanent statistical subdivision….designed to be relatively homogeneous with respect to population characteristics, economic status, and living conditions.”29
Spatial Issues
Once a research design included participants spatially organized over the study area, a number of spatial issues had to be considered. The primary consideration was the possibility of spatial autocorrelation in the study outcomes. Addressing spatial autocorrelation is important because spatially autocorrelated data violate the assumption of independence assumed in statistical analyses and can lead to either Type I or Type II errors.30,31 In projects involving a relatively small number of participants (e.g., <100) their distribution was rarely into contiguous neighborhoods, making the likelihood of spatial autocorrelation highly unlikely and the assessment of spatial autocorrelation more difficult. In projects involving a much larger number of participants, assessing spatial autocorrelation using a contiguity-based spatial metric for spatial weighting was possible.32 Assessments of spatial autocorrelation were conducted on the mean level of an outcome (e.g., mean BMI) across neighborhoods, when available. Distance and k-nearest neighbor spatial metrics for spatial weighting were not used.
Multilevel Issues
Consultation on multilevel approaches to analysis of data was also provided by the SDH Core. Although including both individual- and Census tract–level measures in a study is conceptually a “multilevel” design, several issues needed to be considered to determine whether a multilevel analysis using random coefficient models could be conducted. The first consideration was grouping of participants across neighborhoods. Though there are no set rules, projects with a large number of groups (e.g., >100) yield more-stable estimates and better model performance.32,33 With regard to group size (e.g., average number of individuals nested in a neighborhood), there are additional considerations. Data sets with large numbers of groups in which there are fewer than five in a group lead to overestimation of the between group variance, leading to Type II errors.33 In fact, only one Mid-South TCC project had a data structure that permitted multilevel analysis using random coefficient models.
Social Determinants of Health Core Database
The SDH Core database was derived from multiple data sources and organized to reflect a variety of constructs theorized to determine health outcomes through neighborhood exposures (Table 1).
Table 1.
Common Measures Available in the SDH Core Database
| Domain | Measures | Source | Time | Scale |
|---|---|---|---|---|
| Food | Fast food availability | Info USA/NCAIS | 2009 | Census tract |
| Environment | Convenience availability | Info USA/NCAIS | 2009 | Census tract |
| Supermarket availability | Info USA/NCAIS | 2009 | Census tract | |
| Healthy/unhealthy food establishments | Info USA/NCAIS | 2009 | Census tract | |
| Physical activity | Physical activity facilities | Info USA/NCAIS | 2009 | Census tract |
| Environment | Street Connectivity | U.S. Census/ACS | 2010 | Census tract |
| Density | U.S. Census/ACS | 2010 | Census tract | |
| Road type | U.S. Census/ACS | 2010 | Census tract | |
| Urban / rural classification | U.S. Census/ACS | 2010 | Census tract | |
| Social and economic environment | Crime | Esri crime data | 2010 | Block group/Census tract |
| Residential segregation | U.S. Census/ACS | 2010 | Census place | |
| Income inequality | U.S. Census/ACS | 2010 | Census tract | |
| Concentrated | 2010 | Census tract | ||
| Disadvantage | U.S. Census/ACS | 2010 | Census tract | |
| Sociodemographics | U.S. Census/ACS | 2010 | Census tract |
SDH, social determinants of health; NCAIS, Industry Classification System; ACS, American Community Survey
The U.S. Census provided data for a number of measures. The U.S. Census’ American Community Survey 5-year estimates provided a variety of social and demographic data to generate measures of social risk. InfoUSA data involving the Industry Classification System and the Standard Industrial Classification (SIC) are used to characterize built environment measures. Data obtained from these sources included business name, geocoded location, and detailed SIC codes for food establishments.
Measures
A variety of measures were available from the U.S. Census to assess the social environment. Neighborhood disadvantage was assessed as an index of neighborhood concentrated disadvantage.34 The Census data items used to generate the concentrated disadvantage measure include:
percentage African American;
percentage Hispanic;
percentage female;
percentage of individuals within standard categorized age groups;
percentage of individuals with less than high school education and the percentage of individuals with a college education or more; and
percentage renting, percentage homeowner, and percentage substandard housing in the neighborhood.
The method for deriving the index is provided in the PhenX tool kit.35
Racial residential segregation is included in the SDH Core database. It was organized for U.S. Census places with populations >50,000 in the five Mid-South TCC states (n=34) consistent with the conceptual model that views the organization of neighborhoods (e.g., Census tracts) within U.S. Census–defined places (e.g., cities, towns, villages) as the relevant unit of analysis for studying structural racism.36 It is calculated based on measures from the 2010 U.S. Census and derived using the dissimilarity index and the isolation index.37 Finally, indices of Uniform Crime Reports was obtained from Esri.38
The SDH Core database defines exposure in a number of ways, including:
as specific food establishment densities (e.g., outlets per capita, outlets per roadway mile); and
as the ratio of unhealthy to healthy food establishments in the neighborhood (continuous scale).
Food establishments were classified using SIC codes from food permit databases obtained from InfoUSA or similar companies. Healthy and unhealthy food establishments include those hypothesized to typically provide healthy and unhealthy food, respectively, based on previous research and evidence.39,40
Specific food establishment availability was broken down into three categories:
fast food availability;
convenience store availability; and
large grocery and supermarket availability.
From the trade addresses provided in the food permit database, a list of all retail outlets selling food, either restaurants or markets, were extracted to calculate specific food establishment measures. A subset of restaurants (i.e., fast food restaurants) are determined using a list of franchise fast food outlets for the state, similarly to previous studies.41
In the SDH Core database, the primary measure used to assess the physical activity environment was street connectivity, a primary construct of the concept of walkability.42,43 As a construct, high street connectivity is believed to make various land uses more proximal and therefore promotes active transportation (i.e., neighborhood street networks that are continuous, integrated, and maximize linkages between starting points and destinations, providing multiple route options).44,45 Indices of street connectivity in the database include:
intersection density, the number of nodes (i.e., intersections) per Census tract;
gamma index, the ratio of observed node linkages to the maximum possible links in the network; and
street density, the number of linear miles of street per square mile of land in the Census tract.
Data were measured using 2010 U.S. Census topologically integrated geographic encoding and referencing files.
In addition to street connectivity, measures assessing exposure to physical activity–related venues in the built environment were also available in the SDH Core database. Commercially available data from InfoUSA were used to characterize the availability of facilities conducive to physical activity using the SIC codes, which correspond to those used by the U.S. Census.46 A list of SIC codes representing physical activity–related facilities was compiled and used to identify and enumerate those facilities, including parks. The number of and availability of such facilities, including their density per capita, were included.
CASE STUDY
A Mid-South TCC pilot project sought consultation with the SDH Core to incorporate SDH as a potential explanatory factor for disparities in glycemic control among pediatric diabetes patients. Glycemic control is an important predictor of later complications from diabetes (e.g., blindness, amputation) and is more common among black diabetic patients.47 The study involved 86 white and black adolescent diabetes patients, which precluded multilevel analysis using random coefficient models. Poor glycemic control, assessed as elevated levels of hemoglobin A1c, was higher in the black diabetes patients. Typically, disparities in glycemic control are attributed to genetic or psychosocial differences between black and white patients.47
With a working hypothesis that greater exposure to disadvantaged environments leads to chronic stress and allostatic changes resulting in metabolic dysfunction including insulin insensitivity, the SDH Core set about contextualizing the patients in the study. The patients’ home addresses were geocoded and each patient was assigned the measure of concentrated disadvantage associated with their Census tract of residence. It should be noted that measures of neighborhood disadvantage have been linked to metabolic dysfunction in prior research.48,49 Stratified analyses found a strong positive association between level of concentrated disadvantage and hemoglobin A1c among the black diabetic patients. It was noted that very few white patients live in high concentrated disadvantage neighborhoods, which could account for the lack of an association observed among this group of patients. In addition, concentrated disadvantage was positively associated with C-reactive protein, a measure of inflammation, in both white and black patients. The study has recently been published.50
CONCLUSIONS
There is growing recognition that in order to address the health disparities that affect poor and minority populations, the research community will have to focus on the characteristics of the local environment to which individuals are exposed.17,51,52 Poor and minority populations in the U.S. are exposed to very different local environments that differentially expose them to social and nutritive stressors associated with chronic disease.12,53 Integrating the relevant social and biological factors to bring health research to bear on this topic therefore requires a multidisciplinary approach. It was an approach that first requires understanding of the biological mechanism and may be affected by environmental stressors. Next, it required a methodology that was geographically based and multilevel in design. The SDH Core of the Mid-South TCC has attempted this integration.
The Mid-South TCC SDH Core approach was fundamentally multidisciplinary, geographically based, and inherently multilevel in design. The SDH Core has provided an opportunity to Mid-South TCC research studies—ranging from studies of the determinants of glycemic control among pediatric diabetes patients to studies of obesity among urban clinic patients—to integrate measures of each individual’s local environment into the analysis. In a process the project termed “contextualization” for its descriptive value, individual patient/participant’s residential information was used to identify their local neighborhood environment in order to add relevant measures of the physical and social environments to which they are exposed. This type of linking permitted multilevel analyses to determine the how much of the variance in an outcome is between individuals and how much is between neighborhoods. It was noteworthy that, in nearly every study in which social determinants were incorporated, a significant amount of the variance in one or more study outcomes was attributed to a social determinant at the neighborhood level.50
ACKNOWLEDGMENTS
Research reported in this paper was supported by the Mid-South Transdisciplinary Collaborative Center for Health Disparities Research through the National Institute on Minority Health and Health Disparities of NIH under Award Number U54MD008176. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.CDC. Healthy People 2020. www.cdc.gov/nchs/healthy_people/hp2020.htm. Accessed April 14, 2016.
- 2.Romero CX, Romero TE, Shlay JC, Ogden LG, Dabelea D. Changing trends in the prevalence and disparities of obesity and other cardiovascular disease risk factors in three racial/ethnic groups of USA adults. Adv Prev Med 2012;201:172–180. 10.1155/2012/172423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation 2005;111(10):1233–1241. 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 4.Jeffery RW, Utter J. The changing environment and population obesity in the United States. Obes Res 2003;11(Suppl 10):12S–22S. 10.1038/oby.2003.221. [DOI] [PubMed] [Google Scholar]
- 5.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among U.S. adults, 1999–2010. JAMA 2012;307(5):491–497. 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 6.Hempe JM, McCarter RJ, Chalew SA. Comment on: Wilson et al. Persistence of individual variations in glycated hemoglobin: analysis of data from the juvenile diabetes research foundation continuous glucose monitoring randomized trial. Diabetes Care. 2011;34:1315–1317. Diabetes care. 2011;34(11):e170; author’s reply e171. 10.2337/dc11-1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011–2012. NCHS Data Brief 2013(131):1–8. [PubMed] [Google Scholar]
- 8.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003;299(5608):853–855. 10.1126/science.1079857. [DOI] [PubMed] [Google Scholar]
- 9.Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q 2009;87(1):123–154. 10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diez Roux AV. Investigating Neighborhood and Area Effects on Health. Am J Public Health. 2001;91(11):1783–1789. 10.2105/AJPH.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior In: Glanz K, Rimer BK, Viswanath K, eds. Health Behavior and Health Education: Theory, Research and Practice. 4th ed. San Francisco: Jossey-Bass; 2008:465–486. [Google Scholar]
- 12.Diez Roux AV. Integrating social and biologic factors in health research: a systems view. Ann Epidemiol. 2007;17(7):569–574. 10.1016/j.annepidem.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Ding D, Gebel K. Built environment, physical activity, and obesity: what have we learned from reviewing the literature? Health Place. 2012;18(1):100–105. 10.1016/j.healthplace.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 14.Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med 2004;58(10):1929–1952. 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 15.Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav 2010;51(Suppl 1):S15–27. 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of U.S. socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156(5):471–482. 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 17.Jacquez GM, Sabel CE, Shi C. Genetic GIScience: Toward a Place-Based Synthesis of the Genome, Exposome, and Behavome. Ann Assoc Am Geogr 2015;105(3):454–472. 10.1080/00045608.2015.1018777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenberg MR. Healthography. Am J Public Health. 2014;104(11):2022 10.2105/AJPH.2014.302232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldstein DS, McEwen B. Allostasis, homeostats, and the nature of stress. Stress. 2002;5(1):55–58. 10.1080/102538902900012345. [DOI] [PubMed] [Google Scholar]
- 20.McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Horm Behav 2003;43(1):2–15. 10.1016/S0018-506X(02)00024-7. [DOI] [PubMed] [Google Scholar]
- 21.McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci 1998;840:33–44. 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 22.Juster RP, Bizik G, Picard M, et al. A transdisciplinary perspective of chronic stress in relation to psychopathology throughout life span development. Dev Psychopathol. 2011;23(3):725–776. 10.1017/S0954579411000289. [DOI] [PubMed] [Google Scholar]
- 23.Hertzman C, Boyce T. How experience gets under the skin to create gradients in developmental health. Annu Rev Public Health 2010;31:329–347 323p following 347. 10.1146/annurev.publhealth.012809.103538. [DOI] [PubMed] [Google Scholar]
- 24.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009;31:7–20. 10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
- 25.Schneider S, Gruber J. Neighbourhood deprivation and outlet density for tobacco, alcohol and fast food: first hints of obesogenic and addictive environments in Germany. Public Health Nutr 2013;16(7):1168–1177. 10.1017/S1368980012003321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swinburn B, Egger G. Preventive strategies against weight gain and obesity. Obes Rev 2002;3(4):289–301. 10.1046/j.1467-789X.2002.00082.x. [DOI] [PubMed] [Google Scholar]
- 27.Moubarac JC, Martins AP, Claro RM, Levy RB, Cannon G, Monteiro CA. Consumption of ultra-processed foods and likely impact on human health. Evidence from Canada. Public Health Nutr 2013;16(12):2240–2248. 10.1017/S1368980012005009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med 2006;62(7):1650–1671. 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 29.Krieger N, Waterman P, Chen JT, Soobader MJ, Subramanian SV, Carson R. Zip code caveat: bias due to spatiotemporal mismatches between zip codes and U.S. census-defined geographic areas--the Public Health Disparities Geocoding Project. Am J Public Health 2002;92(7):1100–1102. 10.2105/AJPH.92.7.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gruenewald PJ, Millar AB, Treno AJ, Yang Z, Ponicki WR, Roeper P. The geography of availability and driving after drinking. Addiction 1996;91(7):967–983. 10.1111/j.1360-0443.1996.tb03594.x. [DOI] [PubMed] [Google Scholar]
- 31.Cliff AD, Ord JK. Spatial Processes: Models and Applications. London: Pion Limited; 1981. [Google Scholar]
- 32.Waller LA, Gotway CA. Applied Spatial Statistics for Public Health Data. New Jersey: John Wiley and Sons; 2004. 10.1002/0471662682. [DOI] [Google Scholar]
- 33.Theall KP, Scribner R, Broyles S, et al. Impact of small group size on neighbourhood influences in multilevel models. J Epidemiol Community Health. 2011;65(8):688–695. 10.1136/jech.2009.097956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sampson RJ, Morenoff JD, Goodchild MF, Janelle DG. Spatial (Dis)Advantage and Homicide in Chicago Neighborhoods Spatially Integrated Social Science. New York, NY: Oxford; 2004:145–170. [Google Scholar]
- 35.Hamilton CM, Strader LC, Pratt JG, et al. The PhenX Toolkit: get the most from your measures. Am J Epidemiol. 2011;174(3):253–260. 10.1093/aje/kwr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Massey DS, Rothwell J, Domina T. The Changing Bases of Segregation in the United States. Ann Am Acad Pol Soc Sci 2009;626(1). 10.1177/0002716209343558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Massey DS, ed. Residential Segregation and Neighborhood Conditions U.S. Metropolitan Areas Washington, DC: National Academy Press; 2001. Smelser NJ, Wilson WJ, Mitchell F, eds. American Becoming: Racial Trends and Their Consequences; No. 1. [Google Scholar]
- 38.ESRI. ArcGIS Desktop: Release 10. Redlands, CA: Environmental Systems Research Institute; 2011. [Google Scholar]
- 39.Larson NI, Story MT, Nelson MC. Neighborhood Environments: Disparities in Access to Healthy Foods in the U.S. Am J Prev Med 2009;36(1):74–81. 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 40.Rundle A, Neckerman KM, Freeman L, et al. Neighborhood Food Environment and Walkability Predict Obesity in New York City. Environ Health Perspect. 2009;117(3):442 10.1289/ehp.11590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. Am J Prev Med 2004;27(3):211–217. 10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 42.Berrigan D, Pickle LW, Dill J. Associations between street connectivity and active transportation. Int J Health Geogr 2010;9:20 10.1186/1476-072X-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frank LD, Saelens BE, Chapman J, et al. Objective assessment of obesogenic environments in youth: geographic information system methods and spatial findings from the Neighborhood Impact on Kids study. Am J Prev Med 2012;42(5):e47–55. 10.1016/j.amepre.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 44.Greenwald M, Boarnet M. Built environment as determinant of walking behavior: analyzing nonwork pedestrian travel in Portland, Oregon. Transp Res Rec 2001;1780:33–42. 10.3141/1780-05. [DOI] [Google Scholar]
- 45.Saelens BE, Sallis JF, Frank LD. Environmental correlates of walking and cycling: findings from the transportation, urban design, and planning literatures. Ann Behav Med 2003;25:80 10.1207/S15324796ABM2502_03. [DOI] [PubMed] [Google Scholar]
- 46.Nelson MC, Gordon-Larsen P, Song Y, Popkin BM. Built and social environments associations with adolescent overweight and activity. Am J Prev Med 2006;31(2):109–117. 10.1016/j.amepre.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 47.Chalew SA. The continuing challenge of outcome disparities in children with diabetes. Pediatrics. 2015;135(3):552–553. 10.1542/peds.2014-4136. [DOI] [PubMed] [Google Scholar]
- 48.Merkin SS, Basurto-Davila R, Karlamangla A, et al. Neighborhoods and cumulative biological risk profiles by race/ethnicity in a national sample of U.S. adults: NHANES III. Ann Epidemiol 2009;19(3):194–201. 10.1016/j.annepidem.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.King KE, Morenoff JD, House JS. Neighborhood context and social disparities in cumulative biological risk factors. Psychosom Med 2011;73(7):572–579. 10.1097/PSY.0b013e318227b062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Coulon SJ, Velasco-Gonzalez C, Scribner R, et al. Racial differences in neighborhood disadvantage, inflammation and metabolic control in black and white pediatric type 1 diabetes patients. Pediatric Diabetes. In press. Online January 18, 2016. 10.1111/pedi.12361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci 2010;1186:125–145. 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 52.Chetty R, Stepner M, Abraham S, et al. The Association Between Income and Life Expectancy in the United States, 2001–2014. JAMA. 2016;315(16)1750–1766. 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health 2003;80(4):569–589. 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]