Abstract
Falls are the leading cause of trauma-related mortality in geriatric patients. We hypothesized that frailty and anticoagulation status are risk factors for readmission and mortality following falls in patients >80 years. A retrospective review was performed on patients over 80 years old who presented to our level 1 trauma center for a fall and underwent a computed tomography of the head between January 2014 and January 2016. Frailty was assessed via the Rockwood Frailty Score. Clinical outcomes were death, readmission, recurrent falls, and delayed intracranial hemorrhage. Of 803 fall-related encounters, 173 patients over 80 years old were identified for inclusion. The 30-day readmission rate was 17.5% and was associated with an increased 6-month mortality (P = 0.01). One-year and 2-year mortality rates were 28% and 47%, respectively. Frailty was the strongest predictor of 6-month and overall mortality (P < 0.01). Anticoagulation status did not significantly influence these outcomes. The recurrent fall rate was 21%, and delayed intracranial hemorrhage did not occur in this study. Mortality of octogenarians after a fall is most influenced by patient frailty. Acknowledgment of frailty, risk of recurrent falls, and increased mortality should direct goals of care for geriatric trauma patients.
Keywords: Anticoagulation, falls, frailty, geriatric trauma, traumatic brain injury
In 2014, falls were the leading cause of injury-related mortality in adults ≥65 years old, at >27,000 deaths.1 Falls account for 2.8 million emergency department (ED) visits, 800,000 hospitalizations, and $31 billion in Medicare spending.1,2 The elderly patient is more likely to suffer a traumatic brain injury (TBI) from a fall than from any other traumatic mechanism.3 TBI in elderly patients is associated with decreased survival and worse functional outcomes compared to TBI in younger patients.3–5 Advanced age and anticoagulation status have long been considered risk factors for hemorrhagic events and mortality in geriatric trauma patients6,7; however, it is our experience that most fall-related ED encounters result in normal findings from computed tomography (CT) of the head with no other significant injuries identified. Current research suggests that the incidence of delayed intracranial hemorrhage in the anticoagulated patient is low (<1%).8–10 However, the true “risk” of delayed intracranial hemorrhage or progression in this age group is difficult to assess.
The aging population and increased incidence of geriatric trauma have led to the development of numerous methodologies to estimate mortality in the injured geriatric trauma patient.11–14 However, these studies fail to recognize that most geriatric patients who suffer a fall are discharged from the ED without injury. It remains at the physician’s discretion and the institutional support structure to guide protocols on disposition of these patients. The purpose of this study was to quantify readmission and mortality rates in patients over 80 years old who suffered a fall, including those who were discharged from the ED. In addition, we analyzed the impact of frailty, oral antiplatelet (OAP)/oral anticoagulant (OAC) status, and patient-specific comorbidities on these outcomes.
Patients and methods
A retrospective, institutional review board–approved review was performed of the electronic medical record (EMR) at an American College of Surgeons–accredited and state-verified level 1 trauma center. Patients who had suffered a fall were selected from a database of all blunt trauma patients seen in the ED from January 2014 to January 2016, including cases of falls, motor vehicle collisions, and motorcycle. Patients seen following a sentinel fall were identified by fall-related International Classification of Diseases, Ninth Revision, codes (E880–E888). Patients were included in the analysis if their age was ≥80 years and they underwent a head CT in the ED at the index fall assessment. Only patients with active malignancy or age <80 years were excluded.
The first encounter for a fall during that time period was considered the patient’s sentinel fall. The mechanism of the fall and patient demographics, including age, gender, ambulatory status (independent, with assistance, or wheelchair/bedbound), and place of residence (home or nursing facility) were verified in the EMR. Frailty was assessed retrospectively using the Rockwood Frailty Score, also known as the Canadian Study of Health and Aging Clinical Frailty Scale.15 All patients were assigned a frailty number (from 1, very fit, to 7, severely frail) based on functional data from the initial history and physical, progress notes, physical and occupational therapist notes, rehabilitation assessment, impact of comorbidities on independence, and ability to complete or perform activities of daily living. As an example, a score of 4, apparently vulnerable, is defined as those who are not frankly dependent but commonly complain of being slowed down or having disease symptoms, and a score of 7, moderately frail, describes those who require help with both instrumental and noninstrumental activities of daily living.
Anticoagulation status was determined from the reconciled medication list as documented in the EMR on the day of the patient’s fall. These medications were rarely verified from lab tests aside from international normalized ratio levels for patients taking warfarin. OAP therapy included aspirin and clopidogrel. OAC therapy included warfarin, apixaban, dabigatran, and rivaroxaban. Also considered OAC for the study but not identified on any medication list were prasugrel, ticagrelor, edoxaan, fondaparinux, and dipyridamole. Other variables included in the analysis were the presence of intracranial hemorrhage on the initial head CT scan, disposition from the ED, and patient-specific comorbidities. These included dementia, hypertension, hyperlipidemia, diabetes, atrial fibrillation, congestive heart failure, chronic obstructive pulmonary disease, chronic kidney disease, and history of stroke or cerebrovascular disease.
Clinical outcomes analyzed in the study were 30-day readmission rates, 2-year mortality rates, recurrent falls, and repeat head CTs. Readmission was defined as any admission to any Baylor Scott & White hospital for any reason within 30 days of the sentinel fall. Date of readmission was identified from the EMR and validated using Centers for Medicare and Medicaid Services institutional data. Mortality rates were calculated at 1, 6, 12, and 24 months following the sentinel fall. Mortality dates were collected from our EMR and/or published obituaries and validated with the Social Security Death Index. Mortality was calculated in months from the date of the sentinel fall. Recurrent falls were calculated by the number of repeat ED visits for the chief complaint of a fall. Repeat head CTs were calculated by the number of head CT scans performed by our hospital system for any indication.
Statistical analysis was performed using SAS 9.4 and R Ver 3.1.0 for the graphs. Kruskal-Wallis, chi-square, and Fisher’s exact tests were used to compare variables when appropriate. Univariate and multivariate Cox regression models were used to model readmission and mortality as a function of variables of interest. Backward, forward, and stepwise selection methods were used to find possible predictors of readmission and mortality at 30 days, 6 months, and overall. Schoenfeld residuals were used to assess the fit of the model. A log-rank test was used to compare the distribution of readmission and mortality by Rockwood scores. P values < 0.05 were considered to be statistically significant.
Results
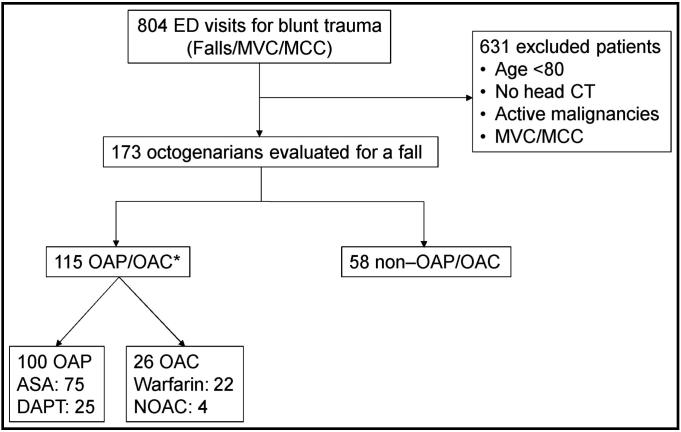
Eight hundred four patients were seen in our ED for blunt trauma–related injuries over the 2-year study period, and 173 patients over 80 years were identified for inclusion in this study. Figure 1 is a flow diagram of included patients. One hundred fifteen patients were taking OAP and/or OAC at the time of the fall. In the OAP group, 75 patients took aspirin and 25 patients took clopidogrel. In the OAC group, 22 patients took warfarin, 2 took rivaroxaban, 1 took dabigatran, and 1 took apixaban. Demographic data and patient disposition are shown in Table 1.
Figure 1.
Flow diagram of patients included in the study. *Eleven patients were taking OAP and OAC. ASA indicates acetylsalicylic acid; CT, computed tomography; DAPT, dual antiplatelet therapy; ED, emergency department; MCC, motorcycle collision; MVC, motor vehicle collision; NOAC, novel oral anticoagulants; OAC, oral anticoagulation; OAP, oral antiplatelet.
Table 1.
Demographics and disposition of OAP/OAC and nonanticoagulated cohortsa
| Variable | OAP/OAC (n = 115) | No OAP/OAC (n = 58) | P |
|---|---|---|---|
| Age (years) | 86.9 ± 5.0 | 87.1 ± 4.7 | 0.84 |
| Female | 67 (58%) | 40 (69%) | 0.19 |
| Ambulatory status | |||
| Independent | 75 (65%) | 21 (36%) | <0.001 |
| With assistance | 31 (27%) | 33 (57%) | <0.001 |
| Nonambulatory | 9 (8%) | 4 (7%) | 0.99 |
| Residence | |||
| Home | 65 (57%) | 30 (52%) | 0.63 |
| Nursing facility | 50 (43%) | 28 (48%) | |
| Intracranial hemorrhage | |||
| Yes | 16 (14%) | 6 (10%) | 0.63 |
| No | 99 (84%) | 52 (90%) | |
| Disposition | |||
| Floor | 49 (43%) | 18 (31%) | 0.19 |
| Intensive care unit | 14 (12%) | 6 (10%) | 0.81 |
| Discharged | 52 (45%) | 34 (59%) | 0.11 |
| Oral antiplatelet | 100 (87%) | n/a | n/a |
| Oral anticoagulant | 26 (23%) | n/a | n/a |
OAP indicates oral antiplatelet; OAC, oral anticoagulant.
aAge shown as mean ± SD. Categorical variables shown as n (%).
Delayed intracranial hemorrhage did not occur in any patient discharged from the ED after the initial fall. However, 28 patients were readmitted to our hospital within 30 days of their sentinel fall, for an overall readmission rate of 17.5% (95% confidence interval [CI], 11.4–23.2). This group had a higher 6-month mortality (43%) than the group that did not get readmitted (16%, P = 0.01). Results of the univariate analysis for readmission are shown in Table 2. Living status (home vs nursing facility) was the only variable in the univariate analysis that was considered statistically significant and included in the multivariate analysis for 30-day readmission. OAP/OAC status was also included in the multivariate analysis because it was a variable of interest in the study. Multivariate analysis demonstrated that the hazard ratio for 30-day readmission was 2.9 times higher for patients living at home compared to those in a nursing facility (P = 0.02; 95% CI, 1.28–7.31). OAP/OAC status did not have a significant impact on 30-day readmission (hazard ratio 1.28; P = 0.35; 95% CI, 0.58–3.10).
Table 2.
Univariate analysis for 30-day readmission
| Variable | Hazard ratio (95% CI) | P |
|---|---|---|
| Age | 0.9 (0.6–1.3) | 0.46 |
| Rockwood score | 1.0 (0.7–1.4) | 0.90 |
| Dementia | 1.7 (0.8–4.0) | 0.22 |
| Hypertension | 1.3 (0.5–2.7) | 0.55 |
| Atrial fibrillation | 0.5 (0.2–1.1) | 0.06 |
| CHF | 0.7 (0.3–1.6) | 0.40 |
| COPD | 1.2 (0.4–5.0) | 0.78 |
| CKD | 0.8 (0.3–1.9) | 0.54 |
| CAD | 0.4 (0.2–0.9) | 0.03 |
| CVD/stroke/TIA | 0.9 (0.4–2.2) | 0.72 |
| Hyperlipidemia | 0.6 (0.3–1.2) | 0.13 |
| Diabetes mellitus | 0.7 (0.3–2.2) | 0.54 |
| Intracranial hemorrhage | 0.5 (0.2–1.3) | 0.11 |
| OAP/OAC | 0.8 (0.3–1.7) | 0.50 |
| Nursing nome | 0.3 (0.1–0.8) | 0.01 |
| Disposition | 0.89 | |
| Floor | 1.1 (0.5–2.6) | |
| ICU | 0.8 (0.3–3.5) |
CAD indicates coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CVD, cerebrovascular disease; ICU, intensive care unit; OAC, oral anticoagulant; OAP, oral antiplatelet; TIA, transient ischemic attack.
Mortality rates at 1, 6, 12, and 24 months were 8.9% (95% CI, 4.5–13.1), 22.6% (95% CI, 15.9–28.8), 28.0% (95% CI, 20.7–34.7), and 46.7% (95% CI, 36.7–55.2), respectively. Univariate and multivariate analyses were performed to determine patient-specific risk factors for 30-day, 6-month, and overall mortality. Results of the univariate analyses are shown in Table 3. Significant variables in the univariate analyses were included in the multivariate analyses for 30-day, 6-month, and overall mortality. Results of the multivariate analyses are shown in Table 4. Risk factors for mortality were time dependent. For 6-month mortality, each unit of the Rockwood Frailty Score increased the hazard ratio by 76%. For overall mortality, each unit of the Rockwood Frailty Score increased the hazard ratio by 60%. As demonstrated in the multivariate analyses, OAP/OAC status did not have a significant impact on 30-day, 6-month, and overall mortality.
Table 3.
Univariate analysis for 30-day, 6-month, and overall mortality
| Variable | 30-day mortality |
6-month mortality |
Overall mortality |
|||
|---|---|---|---|---|---|---|
| Hazard ratio (95% CI) | P | Hazard ratio (95% CI) | P | Hazard ratio (95% CI) | P | |
| Age | 1.3 (0.8–2.0) | 0.32 | 1.2 (0.9–1.6) | 0.30 | 1.3 (1.0–1.7) | 0.03 |
| Rockwood score | 1.3 (0.8–1.9) | 0.28 | 1.5 (1.2–2.1) | 0.002 | 1.7 (1.3–2.1) | <0.001 |
| Dementia | 1.0 (0.4–2.8) | 0.98 | 0.8 (0.4–1.4) | 0.40 | 0.6 (0.3–0.9) | 0.02 |
| Hypertension | 1.7 (0.6–4.4) | 0.25 | 1.2 (0.6–2.4) | 0.53 | 1.4 (0.8–2.3) | 0.19 |
| Atrial fibrillation | 0.8 (0.3–2.2) | 0.58 | 0.7 (0.4–1.3) | 0.23 | 0.9 (0.5–1.5) | 0.60 |
| CHF | 0.5 (0.2–1.5) | 0.20 | 0.6 (0.3–1.1) | 0.07 | 0.5 ( 0.3–0.8) | 0.004 |
| COPD | 1.1 (0.3–7.1) | 0.88 | 1.0 (0.4–2.9) | 1.00 | 1.2 (0.6–2.9) | 0.66 |
| CKD | 1.3 (0.4–5.7) | 0.66 | 1.1 (0.5–2.5) | 0.87 | 0.8 (0.4–1.3) | 0.31 |
| CAD | 0.7 (0.3–1.9) | 0.49 | 0.8 (0.4–1.7) | 0.60 | 0.7 (0.5–1.2) | 0.21 |
| CVD/stroke/TIA | 1.0 (0.4–3.5) | 0.99 | 0.9 (0.5–2.1) | 0.86 | 1.1 (0.6–2.1) | 0.86 |
| Hyperlipidemia | 1.1 (0.4–2.9) | 0.87 | 1.1 (0.6–2.1) | 0.82 | 1.0 (0.6–1.7) | 0.96 |
| Diabetes mellitus | 2.8 (0.6–51.3) | 0.31 | 1.6 (0.6–5.3) | 0.39 | 0.9 (0.5–1.9) | 0.82 |
| Intracranial hemorrhage | 0.1 (0.1–0.4) | <0.001 | 0.4 (0.2–0.8) | 0.01 | 0.6 (0.3–1.1) | 0.07 |
| OAP/OAC | 0.6 (0.2–1.5) | 0.30 | 1.1 (0.6–2.1) | 0.80 | 1.2 (0.8–2.0) | 0.40 |
| Place of residence | ||||||
| Nursing home | 0.4 (0.1–1.2) | 0.12 | 0.9 (0.5–1.7) | 0.84 | 1.3 (0.8–2.0) | 0.36 |
| Disposition | ||||||
| Floor | 0.4 (0.1–1.4) | <0.001 | 0.3 (0.1–0.8) | 0.02 | 1.2 (0.7–2.0) | 0.42 |
| ICU | 0.1 (0.06–0.3) | 0.5 (0.2–1.2) | 0.7 (0.4–1.5) | |||
CAD indicates coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CVD, cerebrovascular disease; ICU, intensive care unit; OAC, oral anticoagulant; OAP, oral antiplatelet; TIA, transient ischemic attack.
Table 4.
Multivariate analysis for 30-day, 6-month, and overall mortality
| Mortality | Variable | Chi-square value | Hazard ratio (95% CI) | P |
|---|---|---|---|---|
| 30-day | ICH | 16.00 | 6.8 (2.6–17.4) | <0.001 |
| OAP/OAC | 0.49 | 1.5 (0.5–5.3) | 0.49 | |
| 6-month | Rockwood | 12.75 | 1.8 (1.3–2.4) | <0.001 |
| Dispo-ICU | 13.34 | 5.7 (2.2–14.3) | <0.001 | |
| A Fib | 3.93 | 2.0 (1.0–3.8) | 0.047 | |
| OAP/OAC | 0.70 | 0.8 (0.4–1.5) | 0.40 | |
| Overall | Rockwood | 16.50 | 1.6 (1.3–2.0) | <0.001 |
| CHF | 5.43 | 1.8 (1.1–3.0) | 0.02 | |
| OAP/OAC | 0.27 | 0.9 (0.5–1.4) | 0.60 |
Dispo-ICU indicates disposition to the intensive care unit; ICH, intracranial hemorrhage; OAC, oral anticoagulant; OAP, oral antiplatelet.
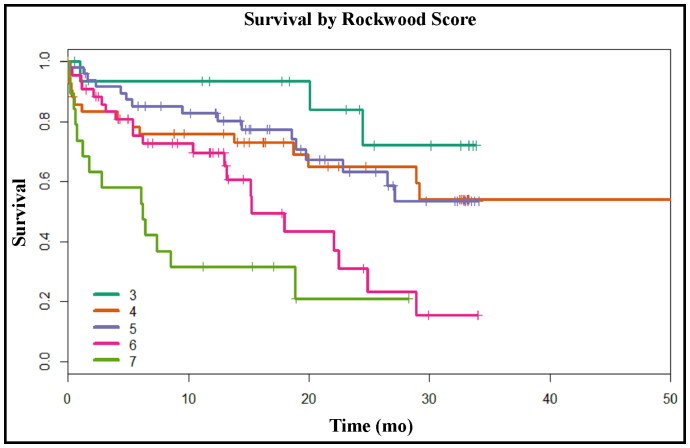
Among the patients, 9% had a Rockwood Score of 3; 26%, 4; 29%, 5; 25%, 6; and 11%, 7. We did not identify any patients with a score of <3, and 36% of patients included in the study had a score ≥6. The Kaplan-Meier curve shown in Figure 2 demonstrates that patients over 80 years old with higher Rockwood frailty scores were much more likely to die following a fall compared to their less frail counterparts (P < 0.01).
Figure 2.
Kaplan-Meier curve for mortality by Rockwood score.
We wanted to determine whether admission to the floor following a negative head CT had long-term benefits on octogenarians regarding the incidence of recurrent falls and the need for repeat head CTs. Sixty-one patients were admitted to the floor following their sentinel fall, and 12 of these patients returned to the ED for at least one recurrent fall during our follow-up period, for a repeat fall rate of 20%, which was lower than the 30% repeat fall rate (25 of 83 patients) seen in patients discharged following their sentinel fall. However, this failed to reach statistical significance (P = 0.18). Patients admitted to the floor following their sentinel fall underwent 51 repeat head CTs within our hospital system for a rate of 0.84 head CTs per patient. Patients discharged from the ED underwent 91 repeat head CTs for a rate of 1.1 head CTs per patient (P = 0.15).
Discussion
Despite the high incidence of falls, very little is known about the long-term outcomes of geriatric patients who have suffered a fall, especially those who are not significantly injured. The observed readmission rate in this patient population is higher than the 5% to 10% published readmission rates in younger trauma patients.16,17 Our observed mortality is similar to a 2014 study by Ayoung-Chee et al that demonstrated a 1-year mortality rate of 33% in patients over the age of 65 who suffered a ground-level fall.18
Readmissions were strongly associated with 6-month mortality, and home living status at the time of the fall was a predictor of 30-day readmission. This was an unexpected finding on multivariate analysis; a general physician tendency is to assume that patients living at home have better outcomes than patients living in a nursing facility. The aforementioned study by Ayoung-Chee et al found that patients who were discharged home with outpatient rehabilitation or home nursing care were protected from 30-day readmissions, and patients who required intensive care unit (ICU) care were at risk of 30-day readmission.18 Other studies suggested that trauma patients discharged to a rehabilitation facility or skilled nursing facility are more likely to be readmitted than those who are discharged home.19 Polypharmacy is also a major concern in elderly trauma patients and has been shown to be a significant risk factor for 30-day readmission.17 Elderly trauma patients are a heterogeneous population with a variety of comorbidities and physical limitations. It is difficult to make generalized recommendations on patient disposition and other factors that may influence readmission, but our study suggests that a reduction in readmissions may also help reduce subsequent mortality.
We found that mortality in patients over 80 years old following a fall was multifactorial and time dependent. Intracranial hemorrhage and ICU admission were predictors of earlier mortality, which is consistent with risk factors identified by other studies.12,13,18 We also identified the Rockwood Frailty Score to be a significant predictor of 6-month and overall mortality. The Rockwood Frailty Score is based on the Canadian Study for Health and Aging Frailty Index, which consists of 70 items that define a person’s comorbidities, independence with activities of daily living, and neurological limitations.15 Versions of this frailty score have been previously validated and are associated with worse morbidity and mortality in trauma and emergency general surgery patients.20,21 Joseph et al developed a Trauma-Specific Frailty Index, which is similar in design to the Canadian Study for Health and Aging Frailty Index but contains only 15 variables that have been modified for trauma patients. They have shown that over one-third of geriatric trauma patients are clinically frail, and these patients are much more likely to suffer an unfavorable discharge disposition.22,23
OAP/OAC status did not have a significant impact on readmission and mortality rates in this study. In another study, Fortuna et al combined antiplatelet and anticoagulant patients into a single cohort and also did not identify a significant difference in mortality following TBI.24 Larger studies have shown that OAC therapy, specifically warfarin, increases mortality rates in elderly patients with TBI.25 More recent studies have also suggested that direct oral anticoagulants are associated with decreased mortality and transfusion requirements compared to warfarin in patients with TBI and severe blunt trauma.26,27 OAP/OAC status must always be considered a potential contributor to mortality in geriatric trauma patients, and the decision to restart these medications must be made on an individualized basis.
Finally, we wanted to determine whether patients with a negative head CT benefited from admission to the hospital compared to patients who were discharged from the ED. Recent literature supports fall prevention programs and suggests that overall they are effective in the community and within nursing facilities.28,29 Olufajo et al demonstrated that integrating routine geriatric consults into the management of geriatric trauma patients significantly improved advanced care planning and was associated with a trend toward reduced ICU readmissions.30 It is possible that these geriatric assessments could be performed in the outpatient setting; however, that is largely dependent on an institution’s resources and the patient’s ability to be evaluated in the outpatient setting.
Limitations of this study include the small sample size. We chose to include patients over 80 years old based on the retrospective feasibility of the study, and we wanted to start with the most vulnerable population in terms of age, comorbidities, and frailty. A larger sample size could be achieved by including patients younger than 80 years old or by extending the target dates for data collection. This may help identify additional patients who are at risk for mortality following a fall. Furthermore, this was a single-institution study within a large hospital system, which has several limitations in data collection and patient follow-up. Prospective studies are needed to minimize these limitations.
In conclusion, readmissions following falls in patients >80 years old are common and contribute to high mortality rates. Home living status may have a negative impact on readmissions. Frailty was a significant risk factor for readmissions and mortality in these patients. OAP and OAC status did not significantly contribute to these outcomes. The results of this study demonstrate the importance of geriatric-specific trauma guidelines that incorporate rehabilitation and palliation practices that are appropriate for this patient population.
References
- 1.Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged ≥65 years—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(37):993–998. doi: 10.15585/mmwr.mm6537a2. [DOI] [PubMed] [Google Scholar]
- 2.Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults—United States. J Safety Res. 2016;58:99–103. doi: 10.1016/j.jsr.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006;54(10):1590–1595. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jager TE, Weiss HB, Coben JH, Pepe PE. Traumatic brain injuries evaluated in US emergency departments, 1992–1994. Acad Emerg Med. 2000;7(2):134–140. doi: 10.1111/j.1553-2712.2000.tb00515.x. [DOI] [PubMed] [Google Scholar]
- 5.Susman M, DiRusso SM, Sullivan T. Traumatic brain injury in the elderly: increased mortality and worse functional outcome at discharge despite lower injury severity. J Trauma. 2002;53(2):219–223. doi: 10.1097/01TA.0000024249.40070.BD. [DOI] [PubMed] [Google Scholar]
- 6.Franko J, Kish KJ, O'Connell BG, Subramanian S, Yuschak JV. Advanced age and preinjury warfarin anticoagulation increase the risk of mortality after head trauma. J Trauma. 2006;61(1):107–110. doi: 10.1097/01.ta.0000224220.89528.fc. [DOI] [PubMed] [Google Scholar]
- 7.Fang MC, Go AS, Hylek EM, et al. Age and the risk of warfarin-associated hemorrhage: the anticoagulation and risk factors in atrial fibrillation study. J Am Geriatr Soc. 2006;54(8):1231–1236. doi: 10.1111/j.1532-5415.2006.00828.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller J, Lieberman L, Nahab B, et al. Delayed intracranial hemorrhage in the anticoagulated patient: a systematic review. J Trauma Acute Care Surg. 2015;79(2):310–313. doi: 10.1097/TA.0000000000000725. [DOI] [PubMed] [Google Scholar]
- 9.Peck KA, Sise CB, Shackford SR, et al. Delayed intracranial hemorrhage after blunt trauma: are patients on preinjury anticoagulants and prescription antiplatelet agents at risk? J Trauma. 2011;71(6):1600–1604. doi: 10.1097/TA.0b013e31823b9ce1. [DOI] [PubMed] [Google Scholar]
- 10.Nishijima DK, Offerman SR, Ballard DW, et al. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460–467. doi: 10.1016/j.annemergmed.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao FZ, Wolf SE, Nakonezny PA, et al. Estimating geriatric mortality after injury using age, injury severity, and performance of a transfusion: the geriatric trauma outcome score. J Palliat Med. 2015;18(8):677–681. doi: 10.1089/jpm.2015.002.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson MS, Konda S, Seymour R, Karunakar M. Early predictors of mortality in geriatric trauma patients. J Orthop Trauma. 2016;30(9):e299–e304. doi: 10.1097/BOT.0000000000000615. [DOI] [PubMed] [Google Scholar]
- 13.Hranjec T, Sawyer RG, Young JS, Swenson BR, Calland JF. Mortality factors in geriatric blunt trauma patients: creation of a highly predictive statistical model for mortality using 50,765 consecutive elderly trauma admissions from the national sample project. Am Surg. 2012;78(12):1369–1375. [PMC free article] [PubMed] [Google Scholar]
- 14.Pandit V, Rhee P, Hashmi A, et al. Shock index predicts mortality in geriatric trauma patients: an analysis of the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76(4):1111–1115. doi: 10.1097/TA.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 15.Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petrey LB, Weddle RJ, Richardson B, et al. Trauma patient readmissions: why do they come back for more? J Trauma Acute Care Surg. 2015;79(5):717–724. doi: 10.1097/TA.0000000000000844. [DOI] [PubMed] [Google Scholar]
- 17.Housley BC, Stawicki SPA, Evans DC, Jones C. Comorbidity-polypharmacy score predicts readmission in older trauma patients. J Surg Res. 2015;199(1):237–243. doi: 10.1016/j.jss.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 18.Ayoung-Chee P, McIntyre L, Ebel BE, Mack CD, McCormick W, Maier RV. Long-term outcomes of ground-level falls in the elderly. J Trauma Acute Care Surg. 2014;76(2):498–503; discussion 503. doi: 10.1097/TA.0000000000000102. [DOI] [PubMed] [Google Scholar]
- 19.Strosberg DS, Housley BC, Vazquez D, Rushing A, Steinberg S, Jones C. Discharge destination and readmission rates in older trauma patients. J Surg Res. 2017;207:27–32. doi: 10.1016/j.jss.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 20.Farhat JS, Velanovich V, Falvo AJ, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg. 2012;72(6):1526–1531. doi: 10.1097/TA.0b013e3182542fab. [DOI] [PubMed] [Google Scholar]
- 21.Jokar TO, Ibraheem K, Rhee P, et al. Emergency general surgery specific frailty index: a validation study. J Trauma Acute Care Surg. 2016;81(2):254–260. doi: 10.1097/TA.0000000000001120. [DOI] [PubMed] [Google Scholar]
- 22.Joseph B, Orouji Jokar T, Hassan A, et al. Redefining the association between old age and poor outcomes after trauma. J Trauma Acute Care Surg. 2017;82(3):575–581. doi: 10.1097/TA.0000000000001329. [DOI] [PubMed] [Google Scholar]
- 23.Joseph B, Pandit V, Zangbar B, et al. Validating trauma-specific frailty index for geriatric trauma patients: a prospective analysis. J Am Coll Surg. 2014;219(1):10–17.e1. doi: 10.1016/j.jamcollsurg.2014.03.020. [DOI] [PubMed] [Google Scholar]
- 24.Fortuna GR, Mueller EW, James LE, Shutter LA, Butler KL. The impact of preinjury antiplatelet and anticoagulant pharmacotherapy on outcomes in elderly patients with hemorrhagic brain injury. Surgery. 2008;144(4):598–605. doi: 10.1016/j.surg.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 25.Grandhi R, Harrison G, Voronovich Z, et al. Preinjury warfarin, but not antiplatelet medications, increases mortality in elderly traumatic brain injury patients. J Trauma Acute Care Surg. 2015;78(3):614–621. doi: 10.1097/TA.0000000000000542. [DOI] [PubMed] [Google Scholar]
- 26.Feeney JM, Santone E, DiFiori M, Kis L, Jayaraman V, Montgomery SC. Compared to warfarin, direct oral anticoagulants are associated with lower mortality in patients with blunt traumatic intracranial hemorrhage. J Trauma Acute Care Surg. 2016;81(5):843–848. doi: 10.1097/TA.0000000000001245. [DOI] [PubMed] [Google Scholar]
- 27.Feeney JM, Neulander M, DiFiori M, et al. Direct oral anticoagulants compared with warfarin in patients with severe blunt trauma. Injury. 2017;48(1):47–50. doi: 10.1016/j.injury.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 28.Neyens JC, van Haastregt JC, Dijcks BP, et al. Effectiveness and implementation aspects of interventions for preventing falls in elderly people in long-term care facilities: a systematic review of RCTs. J Am Med Dir Assoc. 2011;12(6):410–425. doi: 10.1016/j.jamda.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 29.Choi M, Hector M. Effectiveness of intervention programs in preventing falls: a systematic review of recent 10 years and meta-analysis. J Am Med Dir Assoc. 2012;13(2):188.e13–188.e21. doi: 10.1016/j.jamda.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 30.Olufajo OA, Tulebaev S, Javedan H, et al. Integrating geriatric consults into routine care of older trauma patients: one-year experience of a level i trauma center. J Am Coll Surg. 2016;222(6):1029–1035. doi: 10.1016/j.jamcollsurg.2015.12.058. [DOI] [PubMed] [Google Scholar]