ABSTRACT
Background: The World Health Organization(WHO) International Classification of Diseases, 11th version (ICD-11), has proposed a new trauma-related diagnosis of complex posttraumatic stress disorder (CPTSD), separate and distinct from posttraumatic stress disorder (PTSD). However, to date, no study has examined CPTSD over time.
Objectives: This prospective study aimed to examine predictors and outcomes of latent classes of PTSD and CPTSD following war captivity.
Method: A sample of 183 Israeli former prisoners of the 1973 Yom Kippur War (ex-POWs) participated in a 24-year longitudinal study with three waves of measurements (T1: 1991, T2: 2008, and T3: 2015). Participants completed validated self-report measures, and their cognitive performance was assessed using the Montreal Cognitive Assessment (MoCA).
Results: A Latent Class Analysis (LCA) identified three main classes at T2: (1) a small class with low probability to meet PTSD and CPTSD clusters criteria (15.26%); (2) a class high only in PTSD symptoms (42.37%) and (3) a class high only in CPTSD symptoms (42.37%). Importantly, higher levels of psychological suffering in captivity at T1 were associated with higher odds of being in the CPTSD class at T2. In addition, CPTSD at T2 was more strongly associated with low self-rated health, functional impairment, and cognitive performance at T3, compared to the PTSD only class.
Conclusions: Adulthood prolonged trauma of severe interpersonal intensity such as war captivity is related to CPTSD, years after the end of the war. Exposure to psychological suffering in captivity is a risk factor for future endorsement of CPTSD symptoms. CPTSD among ex-POWs is a marker for future dire mental health and functional consequences.
KEYWORDS: Complex PTSD, PTSD, ICD-11, prolonged trauma, war, ex-POWs
HIGHLIGHTS
• We examined predictors and outcomes of latent classes of PTSD and CPTSD among ex-POWs.• A Latent Class Analysis (LCA) identified three main classes.• Psychological suffering in captivity was associated with higher odds of being in the CPTSD.• CPTSD was more strongly associated with low self-rated health, functional and cognitive impairment.
Abstract
Antecedentes: La Clasificación Internacional de Enfermedades de la Organización Mundial de la Salud (OMS), 11ª versión (CIE-11), ha propuesto un nuevo diagnóstico relacionado con el trauma del trastorno de estrés postraumático complejo (TEPTC), separado y distinto del trastorno de estrés postraumático (TEPT). Sin embargo, hasta la fecha, ningún estudio ha examinado el TEPTC a lo largo del tiempo.
Objetivos: Este estudio prospectivo tuvo como objetivo examinar los factores predictivos y los resultados de las clases latentes del TEPT y el TEPTC después del cautiverio de la guerra.
Método: Una muestra de 183 prisioneros israelíes de la Guerra de Yom Kippur de 1973 (ex-prisioneros de guerra) participó en un estudio longitudinal de 24 años con tres momentos de mediciones (T1: 1991, T2: 2008, y T3: 2015). Los participantes completaron medidas validadas de autoinforme y su rendimiento cognitivo se evaluó mediante la Evaluación Cognitiva de Montreal (MoCA en sus siglas en inglés).
Resultados: Un Análisis de Clase Latente (LCA en sus siglas en inglés) identificó tres clases principales en T2: (1) un grupo pequeño con baja probabilidad de cumplir con los criterios sintomáticos del TEPT y TEPTC (15.26%); (2) un grupo alto solo en los síntomas del TEPT (42.37%), y (3) un grupo alto solo en los síntomas del TEPTC (42.37%). Es importante destacar que los niveles más altos de sufrimiento psicológico en cautiverio en T1 se asociaron con mayores probabilidades de estar en el grupo del TEPTC en T2. Además, el TEPTC en T2 se asoció más fuertemente con una baja autoevaluación de salud, deterioro funcional, y rendimiento cognitivo en T3, en comparación con el grupo del TEPT solamente.
Conclusiones: El trauma prolongado en la edad adulta de intensidad interpersonal severa, como el cautiverio de guerra, está relacionado con el TEPTC, años después de término de la guerra. La exposición al sufrimiento psicológico en cautiverio es un factor de riesgo para confirmación futura de los síntomas de TEPTC. El TEPTC entre los ex prisioneros de guerra es un marcador para la salud mental y las consecuencias funcionales futuras.
PALABRAS CLAVE: TEPT complejo, TEPT, CIE-11, trauma prolongado, guerra, ex-prisioneros de guerra
Abstract
背景:世界卫生组织(WHO)国际疾病分类第11版(ICD-11),提出了一种新的创伤相关的复杂性创伤后应激障碍(CPTSD)诊断,与创伤后应激障碍(PTSD)区分。然而,到目前为止,还没有研究对CPTSD进行追踪考察。
目标:这项前瞻性研究旨在研究战争囚禁后PTSD和CPTSD潜在类别的预测因素和结果。
方法:1973年赎罪日战争的183名以色列前囚犯(ex-POWs, 前战俘)参加了一项为期24年的纵向研究,其中有三次测量(T1:1991年,T2:2008年和T3:2015年)。参与者完成了自评问卷,并使用蒙特利尔认知评估工具(MoCA)评估了他们的认知表现。
结果:潜类分析(LCA)确定了T2的三个主要类别:(1)符合PTSD和CPTSD症状簇标准的概率较低的小类(15.26%); (2)仅有高PTSD症状(42.37%)和(3)仅有高CPTSD症状的大类(42.37%)。重要的是,在T1时被囚禁时更多的心理痛苦和出现在T2的CPTSD类别的更高的几率相关。此外,与PTSD类相比,T2的CPTSD类与T3的低自评健康、功能障碍和认知表现更强烈相关。
结论:成年后长期严重的人际剧烈创伤,如战争囚禁,与战争结束数年后的CPTSD有关。囚禁过程中遭受心理痛苦是未来出现CPTSD症状的风险因素。前战俘中的CPTSD是以后的心理健康和功能恶化的提示。
关键词: 复杂型PTSD, PTSD, ICD-11, 长期的创伤, 战争, 前战俘
1. Introduction
Since the establishment of the Posttraumatic Stress Disorder (PTSD) diagnosis, it has been argued that exposure to prolonged trauma is antecedent to more severe, varied and complex posttraumatic manifestations (e.g. Gilbar, Hyland, Cloitre, & Dekel, 2018). Recently, the World Health Organization (WHO) International Classification of Diseases, 11th version (ICD-11), has proposed including two distinct trauma-related diagnoses for PTSD and complex PTSD (CPTSD) (Maercker et al., 2013), which have been included in the draft version of the ICD-11. The ICD-11 model of PTSD encompasses three clusters: (1) re-experiencing, (2) avoidance and (3) sense of threat, while CPTSD comprises the three clusters of PTSD as well as an additional three clusters of disordered self-organization: (1) affect dysregulation, (2) negative self-concept and (3) interpersonal problems (Cloitre, Garvert, Brewin, Bryant, & Maercker, 2013). The proposal additionally states that repeated exposure to traumatic stressors like childhood abuse, domestic violence, genocide or torture is a risk factor for the development of self-regulation problems characteristic of CPTSD (Cloitre et al., 2013). These two ‘sibling disorders’ were formulated to improve the specificity of each disorder’s unique characteristics. Specifically, important for management and treatment, is a formulation of diagnoses comprised of a limited number of symptoms closely related to clinicians’ mental health taxonomies (Brewin et al., 2017).
Indeed, the ICD-11 CPTSD diagnosis proposal has set off a plethora of innovative research (Brewin et al., 2017), and a reliable measure for ICD-11 PTSD and CPTSD has been established (Cloitre et al., 2018). To date, most studies appear to support the construct validity and the proposed factor structure of the ICD-11 PTSD and CPTSD, as well as the distinction between the two diagnoses (e.g. Karatzias et al., 2017). Moreover, studies have utilized samples from different countries around the globe (e.g. Northern Uganda; Murphy, Elklit, Dokkedahl, & Shevlin, 2016) with heterogeneous exposure to types and severity of traumatic events (e.g. female Yazidi victims of sexual slavery; Hoffman et al., 2018). Importantly, following theoretical and clinical conceptualizations of CPTSD (e.g. Herman, 1992), the ICD-11 proposal for CPTSD diagnosis seems appropriate to identify a distinct group who have more often experienced multiple, repeated and prolonged traumas (e.g. refugees; Tay et al., 2018). This study aims to examine CPTSD in such a severely traumatized group: former prisoners of war.
Although still in its initial stage, the literature has also pointed to a number of factors that predict CPTSD as well as its clinical and functional outcomes. A number of sociodemographic variables such as unemployment and living alone or unmarried (Karatzias et al., 2016), as well as minority status, lower education and lower self-reported socio-economic status (SES; Perkonigg et al., 2016), have been linked to CPTSD relative to PTSD profiles. Mixed results regarding female gender as a risk factor for CPTSD vs. PTSD have also been documented (Hyland et al., 2017). Importantly, chronic traumatic experiences such as childhood sexual abuse (e.g. Murphy et al., 2016), but also prolonged trauma in adulthood (e.g. refugees; Nickerson et al., 2016), have been associated with elevated risk for CPTSD vs. PTSD. However, some adulthood single traumas can also develop CPTSD (Elklit, Hyland, & Shevlin, 2014). Individuals grouped into CPTSD classes are also at risk for greater functional impairment (e.g. Cloitre et al., 2013), as well as more profound psychiatric symptomatology and comorbidity than those with PTSD (Elklit et al., 2014; Hyland et al., 2017). Notwithstanding the contributions of the above-mentioned studies, their findings are somewhat tempered by their cross-sectional design and exclusive use of self-report methodology. To our knowledge, there have been no prospective studies that could enable more valid predictions of CPTSD following adulthood chronic traumatization such as war captivity and its possible associations with both self-reported and objective assessment of future ramifications.
Being exposed to a significant threat of death and injury, war represents the extreme of human aggression and destruction. However, the possibly traumatic experiences of war can become more profound for soldiers who fall into captivity. Captivity trauma occurs in circumstances under which a prisoner of war cannot escape, is deliberately traumatized and often aggressively tortured by his or her captors. Prisoners of war are often subjected to harsh interrogations, mock executions, and protracted periods of solitary confinement. Moreover, besides deprivation of physical needs such as food, drink and sleep, the trauma of war captivity is experienced over a prolonged period and in a unique interpersonal context. Thus, prisoners of war (POWs) can become totally dependent on their captors for the provision of their most basic needs, while their captors are also agents of malevolence (Herman, 1992). As a result, captivity has been consistently recognized as a highly pathogenic experience (Santiago et al., 2013), with extensive, wide-spread mental and physical ramifications. Indeed, studies of the psychosocial impact of war captivity have evidenced high rates of psychiatric symptomatology (e.g. Rintamaki, Weaver, Elbaum, Klama, & Miskevics, 2009) and most commonly, posttraumatic stress disorder (PTSD; Solomon et al., 2017).
In her seminal work, Herman (1992) proposed that prolonged interpersonal traumatic stressors, such as being a prisoner of war, can negatively impact self-organization, independent of PTSD symptoms. Indeed, in its detrimental physical and psychological ramifications (e.g. Lahav, Rodin, & Solomon, 2015), which are known to progress into a deterioration of self and other representations (Mikulincer, Solomon, Shaver, & Ein-Dor, 2014) and interpersonal relationship problems (Levin, Bachem, & Solomon, 2017), captivity may give birth to complex reactions after repatriation. It is therefore surprising to acknowledge the sparse literature regarding CPTSD among ex-POWs. To our knowledge, only two studies by our team examined this topic. In the first study (Zerach & Solomon, 2014), we found that compared to matched combat veterans, significantly higher rates of ex-POWs met the criteria for self-reported CPTSD diagnosis and CPTSD symptom clusters. Moreover, the total number of PTSD symptoms predicted the total number of ‘Disorders of Extreme Stress Not Otherwise Specified’ (DESNOS) symptoms, beyond the contribution of captivity-related stressors (e.g. weight loss). Recently, we found a high probability of ICD-11 criteria for the CPTSD class among samples of adulthood-prolonged trauma with severe interpersonal intensity, such as ex-POWs. The CPTSD class has also been correlated with the highest frequency of work-related functional impairment (Palic et al., 2016). However, these preliminary results were based on the DESNOS conceptualization and measurement of CPTSD that are not entirely consistent with the ICD-11 formulation. However, they provided preliminary evidence of some type of complex form of PTSD among ex-POWs.
The present longitudinal study aims to fill some of the above-mentioned gaps by investigation of ICD-11’s PTSD and CPTSD among Israeli male ex-POWs who were subjected as adults to the prolonged traumatization of severe interpersonal intensity. Specifically, using Latent Class Analysis (LCA), the study explores whether PTSD and CPTSD would be found as separate classes and their rates among ex-POWs. Moreover, the study aims to investigate the prospective prediction of war and captivity-related variables of the identified latent classes. In addition, we aim to examine the identified latent classes’ future ramifications in several domains: self-reported physical and mental health, and functional and objective cognitive impairment (the model is presented in Figure 1).
Figure 1.
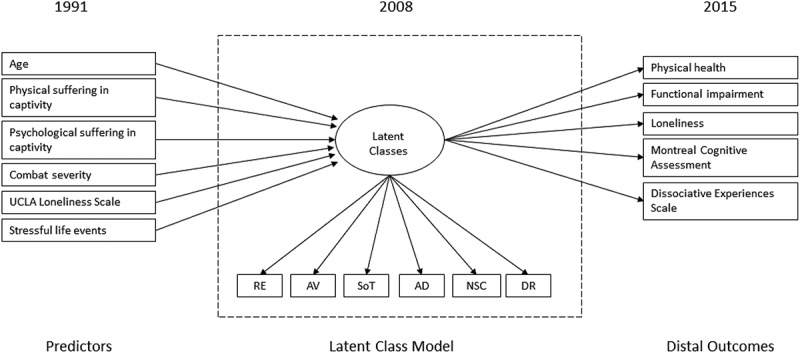
Latent class model for PTSD and CPTSD in 2008 with predictors (1991) and distal outcomes (2015).
We hypothesized that: (a) both PTSD and CPTSD as separate classes would be found among ex-POWs, with higher rates of CPTSD than PTSD; (b) exposure to psychological suffering during captivity will predict future CPTSD; and (c) the CPTSD class would be associated with significantly more physical and mental-health problems, and higher functional and cognitive impairment than in the PTSD alone class.
2. Methods
2.1. Participants
This research is part of a prospective study of the biopsychosocial implications of war captivity. A cohort of Israeli, Jewish males veterans who participated in the 1973 Yom Kippur War was followed up for 24 years. Participants served in the Israeli Army land forces during the 1973 Yom Kippur Warand were captured either on the Syrian front or on the Egyptian front. The POWs in both Syria and Egypt were subjected similarly to intense isolation and systematic torture, consisting of the infliction of severe physical pain and great mental pressure (Solomon et al., 2017).
The larger study included four waves of assessment. We used data from three points of assessment: 1991 (T1), 2008 (T2), and 2015 (T3). The index year for modelling PTSD and CPTSD, 2008, was chosen since it provided availability of the best items that represented the ICD symptom description, provided suitable previously measured predictors (1991) and measured subsequently important outcomes (2015). The 2003 wave assessment was not included, since the power of the test would have been reduced due to a lower number of participants, without adding a meaningful, distinct addition to the model. Of the 240 land forces soldiers captured during the 1973 Yom Kippur War: 164 agreed to participate in the study at T1; 183 participated at T2 (29 could not be located/refused, 6 could not participate due to mental deterioration, and 20 were deceased). This assessment included 109 ex-POWs who participated at T1 and 74 ex-POWs from the original sampling list who had not participated previously. At T3, 158 ex-POWs participated (36 refused to participate, 8 could not be located, 5 did not participate due to mental deterioration or other medical reasons, 5 were abroad, and 30 were deceased). At T3, the mean age of ex-POWs was 63.8 (SD = 3.4; range = 60–77). The mean years of education was 14 (SD = 13.7; range = 6–25 years). Of the ex-POWs, 29.9% were working in full-time jobs, 21.8% had part-time jobs, and 48.3% were unemployed. 75.5% reported an average or greater monthly income. No significant differences were found between those who participated in the follow-up assessments and those who dropped out, with regard to T1 through T3 levels of PTSD, rank, age, and education.
2.2. Measures
2.2.1. PTSD and complex PTSD
Three measures were used to assess the PTSD and complex PTSD symptoms. PTSD Inventory (PTSD-I; Solomon et al., 1993; used at T1, T2, and T3), the Symptom Checklist-90 (SCL-90; Derogatis, 1977; used at T1), and the Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983; used at T2 and T3), respectively. In the absence of validated self-report measures for CPTSD according to the ICD definitions at the time of the study, items used to evaluate the CPTSD construct were selected based on face validity (directly or closely representative of the symptoms) and following other studies of ICD-11 CPTSD (e.g. Cloitre et al., 2013), from the SCL-90 and the BSI. The items used to represent the symptoms of PTSD and complex PTSD are shown in Table 1. In 1991, demographic information was available on age, father’s country of origin, family status, religiosity, education and income level.
Table 1.
Items representing PTSD and CPTSD.
| Symptom cluster | Questionnaire item | ||
|---|---|---|---|
| PTSD | Re-experiencing | PTSD-I no. 2. | Recurrent nightmares about captivity |
| PTSD-I no. 3. | Feeling as though the event is happening again | ||
| Avoidance | PTSD-I no.5. | Avoiding thoughts and feelings associated with captivity | |
| PTSD-I no.6 | Avoiding activities that remind you of captivity | ||
| Sense of threat | PTSD-I no. 16 | Hypervigilance or feeling on guard | |
| PTSD-I no. 17 | Jumpy or easily startled | ||
| CPTSD | Affect dysregulation | SCL-90 no.24/BSI no.13. | Temper outbursts |
| SCL-90 no.34/BSI no.20. | Your feelings being easily hurt | ||
| Negative self-concept | SCL-90 no.79/BSI no.50. | Feelings of worthlessness | |
| SCL-90 no.89/BSI no.52. | Feelings of guilt | ||
| Interpersonal disturbances | SCL-90 no.88/BSI no.44. | Never feeling close to another person | |
| SCL-90 no.77/BSI no.14. | Feeling lonely even when you are with people | ||
2.2.2. PTSD inventory (PTSD-I)
PTSD inventory (PTSD-I; Solomon et al., 1993) taps the 17 PTSD symptoms listed in the DSM-IV-TR (APA, 2000). Participants were asked to rate how often they suffered from each symptom in the previous month on a scale ranging from 0 (not at all) to 4 (almost always). The number of positively endorsed symptoms was calculated by counting the items in which the respondents answered ‘3ʹ or ‘4ʹ. This symptom count was used to operationalize PTSD as a continuous variable. When compared to diagnoses based on structured clinical interviews, the PTSD-I scores showed high convergent validity (Solomon, 1988). In this study, reliability values in T1 to T3 were moderate to high (Cronbach’s alpha for subscales ranged between .62 and .85, and for the total score .81 and .90).
2.2.3. Symptom checklist-90 (SCL-90; Derogatis, 1977)
This measurement assesses 90 psychiatric symptoms during the 2 weeks preceding the assessment. The respondent is asked to indicate how frequently they experienced each symptom during the previous two weeks on a 5-point scale, ranging from 0 ‘not at all’ to 4 ‘extremely’. The subscale scores have high concurrent and convergent validity with similar scales in established psychiatric measurements, such as the Minnesota Multiphasic Personality Inventory (MMPI) (e.g. Derogatis, Rickles, & Rock, 1976). The SCL-90 has shown good test–retest reliability (e.g. Horowitz, Rosenberg, Baer, Ureno, & Villasenor, 1988), and in this study reliability values in T1 were moderate (Cronbach’s α for subscales ranged between .61 and .77, and for the total score .83).
2.2.4. The brief symptom inventory (BSI; Derogatis & Melisaratos, 1983)
The BSI is a 53-item self-report psychological symptom inventory with nine primary symptom dimensions that represents a short version of the SCl-90. The measure assesses how much a problem bothered or distressed a person using a 5-point Likert scale, ranging from 0 ‘not at all’ to 4 ‘extremely’. The BSI scores have shown high convergent and construct validity (Derogatis & Melisaratos, 1983). In this study, reliability values in T2 and T3 were moderate to high (Cronbach’s alpha for subscales ranged between .76 and .88, and for the total score .89 and .90, for T2 and T3, accordingly).
2.2.5. The 1991 (T1) predictors
2.2.5.1. Combat severity
Battlefield stressors were assessed using a specially designed self-report questionnaire of 23 items that tap the intensity of exposure to combat, i.e. encounters with death, active fighting, etc. A total exposure score across all items was calculated. This measure was also used in previous studies (e.g. Dekel, Mandl, & Solomon, 2011). In the present study, high internal consistency was found (Cronbach’s alpha = 0.90).
2.2.5.2. Physical and psychological suffering during captivity
Participants were asked to rate two items on a scale of 1 (not at all) to 5 (very much); (a) the severity of physical abuse, and (b) the severity of psychological abuse to which they had been subjected. This measure was also used in previous studies (e.g. Solomon & Dekel, 2005).
2.2.5.3. UCLA revised loneliness scale
UCLA revised loneliness scale (Russell, Peplau, & Cutrona, 1980) was used to measure feelings of loneliness. The scale consists of 20 items, measuring perceived social isolation through relational contexts (e.g. ‘I feel isolated from others’). Participants were asked to indicate how often they experienced the feelings mentioned in the items on a 4-point Likert scale: 1 (not at all) to 4 (very often). The total score is the sum of all 20 items. The scale possesses good psychometric properties, in both its English (Russell et al., 1980) and Hebrew (Solomon & Dekel, 2008) versions. In the present study, high internal consistency was found (Cronbach’s alpha .88).
2.2.5.4. Stressful life events after the war
Participants were asked about stressful life events they experienced between the end of the war and the time of the study. The measure is an adaptation of the Life Events Questionnaire (Solomon, Mikulincer, & Flum, 1988) that has been used in previous studies of Israeli combat veterans (e.g. Solomon, Mikulincer, & Waysman, 1991). It includes 14 stressful Experiences (e.g. bereavement, financial loss, severe motor vehicle accident). The score indicates the total number of events endorsed.
2.2.6. The 2015 (T3) outcomes
2.2.6.1. The montreal cognitive assessment (MoCA)
The MoCA is a screening test assessing global cognitive function that assesses memory, visuospatial ability, executive function, attention, concentration, working memory and orientation. This instrument is a widely used paper-based screening instrument that takes about 10 min to complete. Potential scores range from 0 to 30. A score of 26 or more is considered normal, and higher scores signify better cognitive performance. The Hebrew version is as it appears on the MoCA test Website (www.mocatest.org). This measure showed good sensitivity and specificity for identifying mild cognitive impairment in elderly individuals (Lifshitz, Dwolatzky, & Press, 2012).
2.2.6.2. Dissociative experiences scale-II (DES-II) (Bernstein & Putnam, 1986)
This revised version of the DES is a 28-item self-report questionnaire that measures the frequency of dissociative experiences (e.g. not recognizing friends or family). For convenience’s sake, in the current study respondents were asked to rate the frequency with which they experienced each of the 28 dissociative reactions on a 10-point scale (1 = never; 10 = all the time) and not an 11-point scale like the original DES-II (0 = never; 10 = all the time). Hence, only the respondent’s mean score was used in this study, representing his tendency to dissociate, with higher scores reflecting stronger tendencies. The DES-II has been used to assess dissociative tendencies in various populations and has been shown to have high validity and reliability (Frueh, Johnson, Smith, & Williams, 1996). The Cronbach alpha for the current sample was high (0.95).
2.2.6.3. Self-rated health (SRH)
SRH was assessed by a single-item question: ‘“How would you define your physical health status in general?”’ Responses were given on a 5-point scale (1 = ‘excellent’ to 5 = ‘bad’). The answers were coded so that higher scores represented better health. SRH is a widely used tool in health studies, with an independent contribution to prospective health outcomes, including mortality (Idler & Benyamini, 1997) and major chronic diseases (Latham & Peek, 2013).
2.2.6.4. Functional impairment
According to the DSM-5, PTSD diagnosis (F criterion) includes clinically significant distress or impairment in the social area, occupational area, or other important areas of functioning. Functioning was assessed by a single-item: ‘in the past month, has your mental state interrupted your routine?’. Responses were given on a 5-point scale (1 = ‘not at all’ to 5 = ‘very much’). The answers were coded so that higher scores represented worsened functioning.
2.2.6.5. Loneliness
was assessed by a single-item question: ‘to what extent do you feel lonely?’ Responses were given on a 5-point scale (1 = ‘Never’ to 5 = ‘Always’). The answers were coded so that higher scores represented a more profound subjective experience of loneliness in life. This item resembles the reversed Item # 4 of the UCLA (Russell et al., 1980), and has been chosen as a global and short assessment of loneliness.
2.3. Procedure
Before filling out the questionnaires, participants signed an informed consent agreement. Approval for this study was given by the Israel Defense Forces (IDF) and Tel Aviv University Ethics Committees. The names of ex-POWs were provided by IDF authorities to enable examination of veterans’ mental health after their military service. We contacted the participants by telephone, and after explaining the purpose of our study, asked them to take part. Questionnaires were administered in the participants’ homes or in another location of their choice.
2.4. Statistical analysis
The model presented in Figure 1 was specified and estimated using Mplus 7.4 (Muthén & Muthén, 2013). An LCA was performed to determine the appropriate number of classes based on the six variables from 2008, scored to represent the diagnostic thresholds for the three PTSD symptom clusters and the three disordered self-organization (DSO) symptom clusters. Six latent class models were assessed (classes 1 through 6) to determine optimal fit. The robust maximum likelihood estimator (Yuan & Bentler, 2000) was used, and models were estimated using all available information. To avoid solutions based on local maxima, 500 random sets of starting values were used initially, followed by 50 final stage optimizations. The relative fit of the models was compared by using three information theory-based fit statistics: The Akaike Information Criterion (AIC; Akaike, 1987), the Bayesian Information Criterion (BIC) and the sample size-adjusted Bayesian Information Criterion (ssaBIC; Sclove, 1987). The class solution that produced the lowest values for the information theory statistics can be judged as the best model. In addition, the Lo-Mendell-Rubin adjusted likelihood ratio test (LMR-A; Lo et al., 2001) was used to compare models with increasing numbers of latent classes. When a non-significant value (p > .05) occurs, this suggests that the model with one less class should be accepted. Entropy was also used to assess the solutions; values can range from 0 to 1, with higher values indicating better classification and class separation. Missing values were imputed using the maximum likelihood-based Expectation Maximization algorithm using SPSS 24.
Once the optimal number of classes was determined, two additional models were specified and tested. For both models, class membership was based on the latent class variable rather than ’a most likely class’ variable, thereby accounting for classification error. First, the covariates (Age, Physical suffering in captivity, 1991; Psychological suffering in captivity, 1991; Combat Severity, 1991; UCLA Loneliness scale, 1991; Stressful life events) were used as predictors of class membership using a multinomial logistic regression. The R3STEP method was employed so that the covariates did not influence the structure of the classes. Second, the 2015 outcome variables (Physical health; Functional impairment; Loneliness; Montreal Cognitive Assessment; Dissociative Experiences Scale) were specified as continuous distal outcomes in the LCA model. The test for equality of means of the distal outcomes across the classification-error corrected levels of the LCA solution was implemented using the DU3STEP command. This is the preferred method for modelling continuous distal outcomes (Asparouhov & Muthen, 2014). An overall test of equal means is provided and is supplemented with all pairwise comparisons.
3. Results
The endorsement rates for each of the PTSD and DSO symptom clusters in 2008 are reported in Table 2. Overall, the endorsement rates were high, and higher for the PTSD clusters than the DSO clusters. Table 3 shows the fit indices for the LCA models with 1 to 6 classes. The fit indices favoured a three-class solution, since the AIC, BIC and ssaBIC values were all lowest for this model, and the LRT became non-significant for the four-class solution. Entropy was .860, which represents good classification (Muthén & Muthén, 2007). Class 1 (15.26%, n = 27) was the smallest class and was characterized by low probabilities of meeting the diagnostic threshold for each of the PTSD and DSO symptom clusters. The probabilities of meeting the criteria for Avoidance and Sense of Threat were higher than the remainder, which were all close to zero. This class was labelled the ‘Baseline class’. Class 2 (42.37%, n = 75) was characterized by relatively high probabilities of meeting the diagnostic threshold for the three PTSD symptom clusters, and lower probabilities of meeting the threshold for the three DSO symptom clusters. This class was labelled the ‘PTSD class’. Class 3 (42.37%, n = 75) was characterized by high probabilities of meeting the threshold for all PTSD and DSO symptom clusters. This class was labelled the ‘CPTSD class’. The ’adjacent’ solutions were less theoretically defensible. The 2-class solution had no baseline class, and the 4-class solution had two PTSD classes (one with zero probability of endorsing the avoidance criterion). The profile plot of the three-class solution is shown in Figure 2, and the estimates are presented on a probability scale.
Table 2.
Rates of Endorsement of each PTSD and DSO Symptom Clusters.
| Count | % | |
|---|---|---|
| Re-experiencing (RE) | 149 | 84.2 |
| Avoidance (AV) | 138 | 78.9 |
| Sense of Threat (SoT) | 157 | 88.7 |
| Affective Dysregulation (AD) | 85 | 49.7 |
| Negative Self-Concept (NSC) | 48 | 28.6 |
| Disturbed Relationships (DR) | 79 | 46.5 |
Table 3.
Fit Statistics for Latent Class Analysis of PTSD and DSO Symptom Clusters.
| Classes | Log-likelihood | AIC | BIC | ssaBIC | LMR-A p |
Entropy |
|---|---|---|---|---|---|---|
| 1 | −566.440 | 1144.881 | 1163.937 | 1144.937 | ||
| 2 | −473.876 | 973.752 | 1015.042 | 973.873 | 180.157 .000 |
.770 |
| 3 | −451.349 | 942.699 | 1006.222 | 942.885 | 43.843 .000 |
.860 |
| 4 | −444.803 | 943.605 | 1029.361 | 943.857 | 12.742 .188 |
.875 |
| 5 | −440.551 | 949.103 | 1057.092 | 949.420 | 8.274 .034 |
.941 |
| 6 | −438.119 | 958.237 | 1088.460 | 958.620 | 4.735 .037 |
.913 |
AIC = Akaike Information Criteria, BIC = Bayesian Information Criteria, ssaBIC = Sample-size adjusted Bayesian Information Criteria, LMR-A = Lo-Mendell-Rubin adjusted likelihood ratio test.
Figure 2.
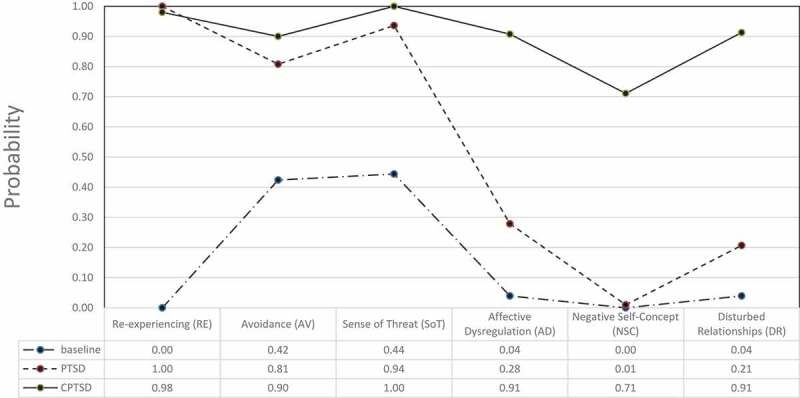
Three-class LCA profile plot.
Table 4 shows the results from the multinomial logistic regression; only two effects were significant.
Table 4.
Results from multinomial logistic regression predicting latent classes (2008).
| Predictors (1981) | Class 2: PTSD OR (95% CI) |
Class 3: CPTSD OR (95% CI) |
|---|---|---|
| Age | 1.74 (0.87–3.49) | 0.77 (0.62–0.97) |
| Physical suffering | 1.16 (0.54–2.48) | 0.61 (0.25–1.49) |
| Psychological suffering | 0.82 (0.32–2.11) | 3.00 (1.13–7.95) |
| Combat severity | 1.49 (0.51–4.35) | 1.91 (0.56–6.46) |
| UCLA Loneliness | 1.02 (0.92–1.14) | 2.61 (0.8–8.53) |
| Stressful life events | 1.74 (0.87–3.49) | 0.99 (0.89–1.11) |
Using the baseline class as a reference, scores on the Psychological suffering in captivity measure were associated with higher odds of being in the CPTSD class (OR = 3.00; 95% CI 1.13–7.95), and age was associated with lower odds of being in the CPTSD class (OR = 0.77; 95% CI 0.62–0.97). Table 5 shows the mean scores on the distal variables across the latent classes.
Table 5.
Distal Outcome Differences across Latent Classes.
| Physical Health |
Functional Impairment |
Loneliness |
Montreal Cognitive Assessment |
Dissociation |
|
|---|---|---|---|---|---|
| Mean (se) | Mean (se) | Mean (se) | Mean (se) | Mean (se) | |
| Baseline (Class 1) | 2.85 (.18) | 1.48 (.11) | 2.44 (.16) | 25.11 (.41) | 1.66 (.11) |
| PTSD (Class 2) | 3.12 (.10) | 2.12 (.09) | 2.63 (.09) | 24.72 (.24) | 2.06 (.09) |
| CPTSD (Class 3) |
3.65 (.10) |
2.85 (.13) |
3.35 (.09) |
23.48 (.31) |
2.98 (.17) |
| |
χ2 (df) p |
χ2 (df) p |
χ2 (df) p |
χ2 (df) p |
χ2 (df) p |
| Overall test | 20.82 (2) .00 | 59.42 (2) .00 | 40.50 (2).00 | 12.93 (2) .00 | 41.828 (2) .00 |
| Class 1 vs. 2 | 1.54 (1) .21 | 17.83 (1) .00 | 1.05 (1) .30 | 0.64 (1) .42 | 07.406 (1) .00 |
| Class 1 vs. 3 | 14.08 (1) .00 | 59.14 (1) .00 | 23.86 (1) .00 | 9.72 (1) .00 | 41.820 (1) .00 |
| Class 2 vs. 3 | 13.43 (1) .00 | 18.91 (1) .00 | 30.61 (1) .00 | 9.48 (1) .00 | 23.035 (1) .00 |
The overall effects were significant for all variables. For functional impairment and dissociation, all differences across classes were significant, with the highest scores associated with the CPTSD class and then the PTSD class, and Baseline class having the lowest means. For the physical health, functional impairment, and Montreal Cognitive Assessment variables, the Baseline and PTSD classes were not significantly different, but the differences between the PTSD and CPTSD classes were all statistically significant, with lower levels for CPTSD class in all the above-mentioned domains than for PTSD class.
4. Discussion
This is the first longitudinal study that examines risk factors as well as mental health, functional and cognitive impairment outcomes of LCA-driven classes of PTSD and CPTSD among ex-POWs. Examination of CPTSD following War captivity represents a unique effort to explore the sequelae of complex long-term reactions of adulthood-prolonged trauma with severe interpersonal characteristics. Our main results identified a 3-class solution that represented ‘baseline’ ‘PTSD’ and ‘CPTSD’ classes as per ICD-11 proposals. Moreover, a higher probability for CPTSD class at T2 has been predicted by more psychological suffering in captivity as measured in T1. Last, as compared to the PTSD class, the CPTSD class reported significantly higher levels of functional impairment, dissociative tendencies, worsened self-reported physical health and lower scores on an objective measure of cognitive assessment (MoCA), among ex-POWs.
The LCA statistics indicated that the 3-class solution provided the best fit. Both the ‘PTSD’ and the ‘CPTSD’ were the largest classes (42.3%). These classes are consistent with the PTSD and CPTSD classes reported in other studies (e.g. Cloitre et al., 2013; Elklit et al., 2014), and differ from the ‘baseline’ class (15.2%) that was found, possibly reflecting that group of ex-POWs previously classified as ‘resilient’ according to the DSM-IV PTSD criteria (Solomon et al., 2012). These findings add to the ICD-11 proposals’ body of evidence for two distinct disorders following exposure to trauma, and thus support the construct validity of ICD-11’s proposal. Given recent results from the only study of U.S. veterans that did not find this pattern of classes (i.e. PTSD and CPTSD; Wolf et al., 2015), our results strengthen previous results among this sample that did find indications of CPTSD symptoms that have been conceptualized (Pelcovits et al., 1997) and measured differently (SIDES-SR; Zerach & Solomon, 2014).
The finding that a significant portion of ex-POW samples experience high levels of DSO clusters and high levels of PTSD clusters highlights the specific interpersonal characteristics of War-captivity that occur within the relationship between the captives and their captors. The unique torments of captivity are part of a planned and concerted effort to ‘break’ individuals and are intentionally inflicted on them by captors whom they may relate to on a daily basis and on whom they are dependent for survival. The ramifications of these twisted relationships are well documented in ex-POWs’ distorted self and other attachment representations (Bachem, Levin, & Solomon, 2018), as well as interpersonal and marital discord (Zerach, Anat, Solomon, & Heruti, 2010). Interestingly, these patterns of results echo the ICD-11 proposal for the CPTSD clusters of ‘negative self-concept’ and ‘interpersonal disturbances’, respectively, and empirically validate Herman’s (1992) theoretical understandings and clinical observations about the interpersonal sequelae of prolonged, repeated and interpersonal traumatization of captivity.
The high rates of delayed-onset PTSD among Israeli ex-POW’s (Zerach, Karstoft, & Solomon, 2017) as well as their accelerated ageing process (Solomon et al., 2017) take their toll on the ex-POWs’ coping resources, so that ex-POWs are expected to experience higher levels of PTSD symptoms. It is therefore not surprising that we found the CPTSD class reported significantly higher levels of functional impairment, dissociative tendencies, worsened self-reported physical health and lower scores of cognitive assessment (MoCA), as compared to the PTSD class. These results are consistent with a number of studies that found impairment to be higher in the CPTSD class as compared to the PTSD class (e.g. Karatzias et al., 2017). Moreover, significantly higher functional impairment in the CPTSD class supports the validity of distinguishing between the two disorders (Brewin et al., 2017). CPTSD is, therefore, a disorder that should be considered as all-encompassing, and in this sense entails greater impairment than simple PTSD.
Our results extend current literature by pointing to the dire ramifications of CPTSD in varied domains. As previously hypothesized (Van der Kolk, Roth, Pelcovitz, Sunday, & Spinazzola, 2005) and demonstrated empirically (Zerach, Green, Ginsburg, & Solomon, 2014), ex-POWs might experience persistent dissociative manifestations over their life span that are closely linked not only to their PTSD symptoms but also to CPTSD. Interestingly, it seems that the severity of functional impairment, as well as greater psychiatric comorbidities (Murphy et al., 2016) characterizing the CPTSD class, might be allied with the subjective experience of deteriorated physical health and objective indications of lowered cognitive performance. Future studies should replicate the finding that CPTSD clusters, as compared to PTSD clusters, are more closely associated with physical and cognitive impairment.
Last, we found that higher probability for CPTSD class at T2 has been predicted by psychological suffering in captivity as measured in T1. Although some studies found correlates to the CPTSD class such as lower education (Perkonigg et al., 2016) and higher rates of childhood sexual abuse (e.g. Murphy et al., 2016), to our knowledge this is the first longitudinal study that might suggest temporal associations with CPTSD from previously measured variables. It seems that beyond mere tortures and physical deprivation, it is the psychological suffering in captivity that adds to future CPTSD symptoms. Because of the POW’s lack of control over his or her life, the captivity stressors of torture, humiliation, and deprivation might be greatly magnified (Basoǧlu, 2009). These might lead to heavy usage of dissociative mechanisms for the sake of survival but might have negative consequences in the long term. From another angle, the loss of emotional autonomy and the acceptance of defeat might contribute to a future negative self-concept, a proposed CPTSD cluster.
It is worth noting that in the present study, older age was associated with lower odds of being in the CPTSD class. The results regarding the age-CPTSD link are rather inconsistent (Brewin et al., 2017). On the one hand, childhood interpersonal trauma has been reported at significantly higher rates among participants with CPTSD as compared to PTSD (e.g. Karatzias et al., 2016). On the other hand, while most studies among adult samples did not find an association between age and CPTSD versus PTSD class (e.g. Cloitre et al., 2013), only one study found CPTSD associated with younger age (Perkonigg et al., 2016). It is possible that older age at the time of captivity may equate to a higher number and more varied repertoire of coping resources than younger POWs, which might then be associated with lower levels of mental health difficulties (e.g. Gold et al., 2000; Weiner, Monin, Mota, & Pietrzak, 2016). Moreover, older POWs might have had more firmly established personalities (i.e. self-concept, interpersonal relations, emotion regulation; Carstensen, Pasupathi, Mayr, & Nesselroade, 2000) which might be less affected by the twisted relationships of captor-captive that is known to contribute to the personality change characterizing CPTSD symptomatology.
This study has several limitations. First, the use of self-report measures, although very common in trauma studies, entails the risk of a reporting bias. Second, ICD-11’s PTSD and CPTSD have been modelled using a selection of symptoms from the SCL-90 scale because, at the time of this study, there were no measures specifically developed for these purposes. Third, the ‘Affect dysregulation’ cluster of the CPTSD should be treated with some caution, because it has been operationalized as ‘hyper-activation’ and not ‘hypo-activation (i.e. numbing) of the affective system, as might be suggested (Brewin et al., 2017). Fourth, our measurements did not cover the entire 42-year span since the war. Therefore, and due to the low number of participants, we were unable to monitor changes in the course of CPTSD and PTSD during the gap between the war and later measurement periods.
Despite these limitations, this study yielded several important findings. This study validated previous results (Zerach & Solomon, 2014) and emphasized the long-term and enduring CPTSD symptoms among former prisoners of war. As the first longitudinal study in this field, our results shed light on the long-term relations between captivity-related psychological suffering and future CPTSD symptoms. This study also validated previous reports (Brewin et al., 2017) regarding the factor structure of the ICD-11 PTSD and CPTSD proposal, and reveals the cognitive and physical health consequences of CPTSD. Thus, the implications of these results relate to the suitability of the ICD-11 to increase clinical recognition and, possibly, governmental compensation, for the CPTSD diagnosis following prolonged, repeated and inter-personal adulthood traumatization, such as war captivity. It also highlights the need to pay special attention during psychotherapy to the experience of psychological suffering during captivity, which might be a risk factor for future CPTSD.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Akaike H. (1987). Factor analysis and the AIC. Psychometrika, 52, 317–11. [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- Asparouhov T., & Muthén B. (2014). Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes, 21(2), 1–22. doi: 10.1080/10705511.2014.915181 [DOI] [Google Scholar]
- Bachem R., Levin Y., & Solomon Z. (2018). Trajectories of attachment in older age: Interpersonal trauma and its consequences. Attachment & Human Development, 1–20. [DOI] [PubMed] [Google Scholar]
- Başoǧlu M. (2009). A multivariate contextual analysis of torture and cruel, inhuman, and degrading treatments: Implications for an evidence‐based definition of torture. American Journal of Orthopsychiatry, 79(2), 135–145. doi: 10.1037/a0015681 [DOI] [PubMed] [Google Scholar]
- Bernstein E. M., & Putnam F. W. (1986). Development, reliability, and validity of a dissociation scale. Journal of Nervous and Mental Disease, 174, 727–735. [DOI] [PubMed] [Google Scholar]
- Brewin C. R., Cloitre M., Hyland P., Shevlin M., Maercker A., Bryant R. A., … Somasundaram D. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–15. [DOI] [PubMed] [Google Scholar]
- Carstensen L. L., Pasupathi M., Mayr U., & Nesselroade J. R (2000). Emotional experience in everyday life across the adult life span. Journal of Personality and Social Psychology, 79(4), 644–655. doi: 10.1037/0022-3514.79.4.644 [DOI] [PubMed] [Google Scholar]
- Cloitre M., Garvert D. W., Brewin C. R., Bryant R. A., & Maercker A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4, 20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M., Shevlin M., Brewin C. R., Bisson J. I., Roberts N. P., Maercker A., … Hyland P. (2018). The international trauma questionnaire: Development of a self‐report measure of ICD‐11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138, 536–546. [DOI] [PubMed] [Google Scholar]
- Dekel S., Mandl C., & Solomon Z. (2011). Shared and unique predictors of post‐traumatic growth and distress. Journal of Clinical Psychology, 67(3), 241–252. [DOI] [PubMed] [Google Scholar]
- Derogatis L. R. (1977). SCL-90: Administration, scoring, and procedure manual. Baltimore, MD: Johns Hopkins. [Google Scholar]
- Derogatis L. R., & Melisaratos N. (1983). The brief symptom inventory: An introductory report. Psychological Medicine, 13(3), 595–605. [PubMed] [Google Scholar]
- Derogatis L. R., Rickles K., & Rock A. F. (1976). SCL-90 and the MMPI: A step in the validation of a new self-report scale. British Journal of Psychiatry, 128, 280e289. [DOI] [PubMed] [Google Scholar]
- Elklit A., Hyland P., & Shevlin M. (2014). Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology, 5, 24221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frueh B. C., Johnson D. E., Smith D. W., & Williams M. A. (1996). A potential problem with the response format of the dissociative experiences scale: A significant correlation with intelligence among combat veterans with PTSD. Journal of Traumatic Stress, 9, 651–656. [DOI] [PubMed] [Google Scholar]
- Gilbar O., Hyland P., Cloitre M., & Dekel R. (2018). ICD-11 complex PTSD among Israeli male perpetrators of intimate partner violence: Construct validity and risk factors. Journal of Anxiety Disorders, 54, 49–56. [DOI] [PubMed] [Google Scholar]
- Gold P. B., Engdahl B. E., Eberly R. E., Blake R. J., Page W. F., & Frueh B. C. (2000). Trauma exposure, resilience, social support, and PTSD construct validity among former prisoners of war. Social Psychiatry and Psychiatric Epidemiology, 35(1), 36–42. [DOI] [PubMed] [Google Scholar]
- Herman J. L. (1992). Trauma and recovery. From domestic abuse to political terror. Kent: Pandora. [Google Scholar]
- Hoffman Y. S., Grossman E. S., Shrira A., Kedar M., Ben‐Ezra M., Dinnayi M., & Zivotofsky A. Z. (2018). Complex PTSD and its correlates amongst female Yazidi victims of sexual slavery living in post‐ISIS camps. World Psychiatry, 17(1), 112–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz L. M., Rosenberg S. E., Baer B. A., Ureno G., & Villasenor V. S. (1988). Inventory of interpersonal problems: Psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology, 56, 885e892. [DOI] [PubMed] [Google Scholar]
- Hyland P., Murphy J., Shevlin M., Vallières F., McElroy E., Elklit A., & Cloitre M. (2017). Variation in post-traumatic response: The role of trauma type in predicting ICD-11 PTSD and CPTSD symptoms. Social Psychiatry and Psychiatric Epidemiology, 52, 727–736. [DOI] [PubMed] [Google Scholar]
- Idler E. L., & Benyamini Y (1997). Self-rated health and mortality: A review of twenty-seven community studies Journal of Health and Social Behavior, 38, 21–37. [PubMed]
- Karatzias T., Shevlin M., Fyvie C., Hyland P., Efthymiadou E., Wilson D., & Cloitre M. (2016). An initial psychometric assessment of an ICD-11 based measure of PTSD and complex PTSD (ICD-TQ): Evidence of construct validity. Journal of Anxiety Disorders, 44, 73–79. [DOI] [PubMed] [Google Scholar]
- Karatzias T., Shevlin M., Fyvie C., Hyland P., Efthymiadou E., Wilson D., … Cloitre M. (2017). Evidence of distinct profiles of posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD) based on the new ICD-11 trauma questionnaire (ICD-TQ). Journal of Affective Disorders, 207, 181–187. [DOI] [PubMed] [Google Scholar]
- Lahav Y., Rodin R., & Solomon Z (2015). Somatic complaints and attachment in former prisoners of war: A longitudinal study. Psychiatry, 78(4), 354–366. doi: 10.1080/00332747.2015.1061311 [DOI] [PubMed] [Google Scholar]
- Latham K., & Peek C. W (2013). Self-rated health and morbidity onset among late midlife us adults. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 68(1), 107–116. doi: 10.1093/geronb/gbs104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin Y., Bachem R., & Solomon Z. (2017). Traumatization, marital adjustment, and parenting among veterans and their spouses: A longitudinal study of reciprocal relations. Family Process, 56(4), 926–942. [DOI] [PubMed] [Google Scholar]
- Lifshitz M., Dwolatzky T., & Press Y. (2012). Validation of the Hebrew version of the MoCA test as a screening instrument for the early detection of mild cognitive impairment in elderly individuals. Journal of Geriatric Psychiatry and Neurology, 25(3), 155–161. [DOI] [PubMed] [Google Scholar]
- Lo Y., Mendell N. R., & Rubin D. B (2001). Testing the number of components in a normal mixture. Biometrika, 88, 767–778. doi: 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- Maercker A., Brewin C. R., Bryant R. A., Cloitre M., Reed G. M., Van Ommeren M., … Saxena S. (2013). Proposals for mental disorders specifically associated with stress in the ICD-11. Lancet, 381, 1683–1685. [DOI] [PubMed] [Google Scholar]
- Mikulincer M., Solomon Z., Shaver P. R., & Ein-Dor T. (2014). Attachment-related consequences of war captivity and trajectories of posttraumatic stress disorder: A 17-year longitudinal study. Journal of Social and Clinical Psychology, 33(3), 207–228. [Google Scholar]
- Murphy S., Elklit A., Dokkedahl S., & Shevlin M. (2016). Testing the validity of the proposed ICD-11 PTSD and complex PTSD criteria using a sample from Northern Uganda. European Journal of Psychotraumatology, 7, 32678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., & Muthén B. O. (2007). Re: What is a good value of entropy. [Online comment]. Retrieved from http://www.statmodel.com/discussion/messages/13/2562.html?1237580237
- Muthén L. K., & Muthén B. O. (2013). Mplus 7.11. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nickerson A., Cloitre M., Bryant R. A., Schnyder U., Morina N., & Schick M. (2016). The factor structure of complex posttraumatic stress disorder in traumatized refugees. European Journal of Psychotraumatology, 7, 33253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palic S., Zerach G., Shevlin M., Zeligman Z., Elklit A., & Solomon Z. (2016). Evidence of complex posttraumatic stress disorder (CPTSD) among individuals who were exposed to prolonged trauma with different ages of onset and interpersonal intensity. Psychiatry Research, 246, 692–699. [DOI] [PubMed] [Google Scholar]
- Perkonigg A., Hofler M., Cloitre M., Wittchen H. U., Trautmann S., & Maercker A. (2016). Evidence for two different ICD-11 posttraumatic stress disorders in a community sample of adolescents and young adults. European Archives of Psychiatry and Clinical Neuroscience, 266, 317–328. [DOI] [PubMed] [Google Scholar]
- Rintamaki L. S., Weaver F. M., Elbaum P. L., Klama E. N., & Miskevics S. A. (2009). Persistence of traumatic memories in World War II prisoners of war. Journal of the American Geriatrics Society, 57, 2257–2262. [DOI] [PubMed] [Google Scholar]
- Russell D., Peplau L. A., & Cutrona C. E. (1980). The revised UCLA loneliness scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39(3), 472–480. [DOI] [PubMed] [Google Scholar]
- Santiago P. N., Ursano R. J., Gray C. L., Pynoos R. S., Spiegel D., Lewis-Fernandez R., … Coyne J. (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLoS ONE, 8(4), e59236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sclove S. L. (1987). Application of model-selection criteria to some problems in multivariate analysis. Psychometrika, 52, 333–343. [Google Scholar]
- Solomon Z. (1988). Convergent validity of posttraumatic stress disorder (PTSD) diagnosis: Self-report and clinical assessment. Israel Journal of Psychiatry and Related Sciences, 25, 46–55. [PubMed] [Google Scholar]
- Solomon Z., Benbenishty R., Neria Y., Abramowitz M., Ginzburg K., & Ohry A. (1993). Assessment of PTSD: Validation of the revised PTSD inventory. Israel Journal of Psychiatry and Related Sciences, 30, 110–115. [PubMed] [Google Scholar]
- Solomon Z., & Dekel R (2005). Posttraumatic stress disorder among Israeli ex-prisoners of war 18 and 30 years after release. The Journal of Clinical Psychiatry, 66(8), 1031–1037. doi: 10.4088/JCP.v66n0811 [DOI] [PubMed] [Google Scholar]
- Solomon Z., & Dekel R (2008). The contribution of loneliness and posttraumatic stress disorder to marital adjustment following war captivity: A longitudinal study. Family Process, 47(2), 261–275. doi: 10.1111/j.1545-5300.2008.00252.x [DOI] [PubMed] [Google Scholar]
- Solomon Z., Horesh D., Ein-Dor T., & Ohry A (2012). Predictors of PTSD trajectories following captivity: A 35-year longitudinal study. Psychiatry Research, 199(3), 188–194. doi: 10.1016/j.psychres.2012.03.035 [DOI] [PubMed] [Google Scholar]
- Solomon Z., Mikulincer M., & Flum H (1988). Negative life events, coping responses, and combat-related psychopathology: A prospective study. Journal of Abnormal Psychology, 97(3), 302–309. doi: 10.1037/0021-843X.97.3.302 [DOI] [PubMed] [Google Scholar]
- Solomon Z., Mikulincer M., & Waysman M (1991). Delayed and immediate onset posttraumatic stress disorder: The role of life events and social resources. Journal of Community Psychology, 19(3), 231–236. doi: 10.1002/(ISSN)1520-6629 [DOI] [Google Scholar]
- Solomon Z., Tsur N., Levin Y., Uziel O., Lahav M., & Ohry A. (2017). The implications of war captivity and long-term psychopathology trajectories for telomere length. Psychoneuroendocrinology, 81, 122–128. [DOI] [PubMed] [Google Scholar]
- Tay A. K., Mohsin M., Rees S., Tam N., Kareth M., & Silove D. (2018). Factor structures of complex posttraumatic stress disorder and PTSD in a community sample of refugees from West Papua. Comprehensive Psychiatry, 85, 15–22. [DOI] [PubMed] [Google Scholar]
- Van der Kolk B. A., Roth S., Pelcovitz D., Sunday S., & Spinazzola J (2005). Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 18(5), 389–399. doi: 10.1002/(ISSN)1573-6598 [DOI] [PubMed] [Google Scholar]
- Weiner M. R., Monin J. K., Mota N., & Pietrzak R. H. (2016). Age differences in the association of social support and mental health in male US Veterans: Results from the national health and resilience in veterans study. The American Journal of Geriatric Psychiatry, 24(4), 327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf E. J., Miller M. W., Kilpatrick D., Resnick H. S., Badour C. L., Marx B. P., ... Friedman M. J (2015). ICD–11 complex PTSD in US national and veteran samples: Prevalence and structural associations with PTSD. Clinical Psychological Science, 3(2), 215–229. doi: 10.1177/2167702614545480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K. H., & Bentler P. M (2000). Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology, 30(1), 165–200. doi: 10.1111/0081-1750.00078 [DOI] [Google Scholar]
- Zerach G., Anat B. D., Solomon Z., & Heruti R. (2010). Posttraumatic symptoms, marital intimacy, dyadic adjustment, and sexual satisfaction among ex-prisoners of war. Journal of Sexual Medicine, 7(8), 2739–2749. [DOI] [PubMed] [Google Scholar]
- Zerach G., Greene T., Ginzburg K., & Solomon Z (2014). The relations between posttraumatic stress disorder and persistent dissociation among ex-prisoners of war: A longitudinal study. Psychological Trauma: Theory, Research, Practice, and Policy, 6(2), 99–108. doi: 10.1037/a0031599 [DOI] [Google Scholar]
- Zerach G., Karstoft K. I., & Solomon Z. (2017, April 22). The roles of hardiness and sensation seeking in former prisoners of war’s posttraumatic stress symptoms trajectories over a 17-year period. Journal of Affective Disorders, 218, 176–181. [DOI] [PubMed] [Google Scholar]
- Zerach G., & Solomon Z. (2014). The relations between posttraumatic symptoms and disorder of extreme stress (not otherwise specified) symptoms following War captivity. Israel Journal of Psychiatry and Related Sciences, 50(3), 148–156. [PubMed] [Google Scholar]


