Abstract
Background
Peritonitis is one of the limiting factors for the growth of peritoneal dialysis (PD) worldwide and is a major cause of technique failure. Several studies have examined the effectiveness of various catheter‐related interventions for lowering the risk of PD‐related peritonitis. This is an update of a review first published in 2004.
Objectives
To evaluate the role of different catheter implantation techniques and catheter types in lowering the risk of PD‐related peritonitis in PD patients.
Search methods
We searched the Cochrane Kidney and Transplant Register of Studies up to 15 January 2019 through contact with the Information Specialist using search terms relevant to this review. Studies in the Register are identified through searches of CENTRAL, MEDLINE, and EMBASE, conference proceedings, the International Clinical Trials Register (ICTRP) Search Portal and ClinicalTrials.gov.
Selection criteria
Studies comparing different catheter insertion techniques, catheter types, use of immobilisation techniques and different break‐in periods were included. Studies of different PD sets were excluded.
Data collection and analysis
Two authors independently assessed study quality and extracted data. Statistical analyses were performed using a random effects model and the results expressed as risk ratio (RR) with 95% confidence intervals (CI).
Main results
Forty‐two studies (3144 participants) were included: 18 evaluated techniques of catheter implantation, 22 examined catheter types, one assessed an immobiliser device, and one examined break‐in period. In general, study quality was variable and almost all aspects of study design did not fulfil CONSORT standards for reporting.
Catheter insertion by laparoscopy compared with laparotomy probably makes little or no difference to the risks of peritonitis (RR 0.90, 95% CI 0.59 to 1.35; moderate certainty evidence), exit‐site/tunnel infection (RR 1.00, 95% CI 0.43 to 2.31; low certainty evidence), catheter removal/replacement (RR 1.20, 95% CI 0.77 to 1.86; low certainty evidence), technique failure (RR 0.71, 95% CI 0.47 to 1.08; low certainty evidence), and death (all causes) (RR 1.26, 95% CI 0.72 to 2.20; moderate certainty evidence). It is uncertain whether subcutaneous burying of catheter increases peritonitis (RR 1.16, 95% CI 0.37 to 3.60; very low certainty evidence). Midline insertion compared to lateral insertion probably makes little or no difference to the risks of peritonitis (RR 0.65, 95% CI 0.32 to 1.33; moderate certainty evidence) and may make little or no difference to exit‐site/tunnel infection (RR 0.56, 95% CI 0.12 to 2.58; low certainty evidence). Percutaneous insertion compared with open surgery probably makes little or no difference to the exit‐site/tunnel infection (RR 0.16, 95% CI 0.02 to 1.30; moderate certainty evidence).
Straight catheters probably make little or no difference to the risk of peritonitis (RR 1.04, 95% CI 0.82 to 1.31; moderate certainty evidence), peritonitis rate (RR 0.91, 95% CI 0.68 to 1.21; moderate certainty evidence), risk of exit‐site infection (RR 1.12, 95% CI 0.94 to 1.34; moderate certainty evidence), and exit‐site infection rate (RR 1.05, 95% CI 0.77 to 1.43; moderate certainty evidence) compared to coiled catheter. It is uncertain whether straight catheters prevent catheter removal or replacement (RR 1.11, 95% CI 0.73 to 1.66; very low certainty evidence) but straight catheters probably make little or no difference to technique failure (RR 0.82, 95% CI 0.51 to 1.31; moderate certainty evidence) and death (all causes) (RR 0.95, 95% CI 0.62 to 1.46; low certainty evidence) compared to coiled catheter. Tenckhoff catheter with artificial curve at subcutaneous tract compared with swan‐neck catheter may make little or no difference to peritonitis (RR 1.29, 95% CI 0.85 to 1.96; low certainty evidence) and incidence of exit‐site/tunnel infection (RR 0.96, 95% CI 0.77 to 1.21; low certainty evidence) but may slightly improve exit‐site infection rate (RR 0.67, 95% CI 0.50 to 0.90; low certainty evidence).
Authors' conclusions
There is no strong evidence that any catheter‐related intervention, including the use of different catheter types or different insertion techniques, reduces the risks of PD peritonitis or other PD‐related infections, technique failure or death (all causes). However, the numbers and sizes of studies were generally small and the methodological quality of available studies was suboptimal, such that the possibility that a particular catheter‐related intervention might have a beneficial effect cannot be completely ruled out with confidence.
Plain language summary
Catheter type, placement and insertion techniques for preventing peritonitis in peritoneal dialysis patients
What is the issue?
People with kidney failure may be treated with peritoneal dialysis where a catheter is permanently inserted into the peritoneum (lining around abdominal contents) through the abdominal wall and sterile fluid is drained in and out several times overnight or during the day. The most common serious complication is infection of the peritoneum ‐ peritonitis. This may be caused by germs which may be accidentally introduced via the catheter into the peritoneum resulting in peritonitis.
What did we do?
We conducted a review of the literature to examine the effects of different methods of catheter insertion and different types of catheter in prevention of peritonitis in PD patients.
What did we find?
We identified 42 studies (3144 participants) examining the effects of different methods of catheter insertion and types of catheter on peritonitis. The risk of peritonitis was not affected by different types of insertion methods or types of catheters inserted.
Conclusions
There is no evidence to support a specific catheter insertion technique or type of catheter with the aim to prevent peritonitis in peritoneal dialysis patients.
Summary of findings
Background
Description of the condition
Peritonitis is a serious complication of peritoneal dialysis (PD) that is associated with appreciably higher rates of hospitalisation (Barraclough 2010; Edey 2010; Htay 2018), technique failure (Htay 2017; Kolesnyk 2010 ) and death (Boudville 2012). Moreover, a previous study (Campbell 2016) has shown that peritonitis has serious impacts on patients’ lifestyles (burden on family, financial burden) and quality of life (feeling of pain, loss of control and dignity). In addition, peritonitis and its complications can potentially increase the financial burden on healthcare systems (Li 2017).
Several factors can potentially contribute to a heightened risk of peritonitis, including older age (Kotsanas 2007; McDonald 2004), race (Lim 2011; McDonald 2004; Piraino 2002; Shen 2013), body mass index (Jegatheesan 2018; McDonald 2004), coexisting diseases (for example, diabetes mellitus) (Chow 2005), nasal carriage of Staphylococcus aureus (Schaefer 2003; Ong 2016), immunocompromised status, and connection methodology (Strippoli 2004a). However, PD‐related infection can be prevented by measures including administering antibiotic prophylaxis prior to catheter implantation (Strippoli 2004a), application of topical antimicrobial agent at catheter exit‐site (Xu 2009), and antibiotic prophylaxis prior to invasive gastrointestinal and gynaecological procedures (Wu 2013).
A previous observational study reported that double cuff catheters were associated with a lower risk of exit‐site infection compared with single cuff catheters (Lindblad 1988). However, this association was unable to be confirmed in an RCT (Eklund 1997) or meta‐analysis (Strippoli 2004; Strippoli 2004b).The International Society for Peritoneal Dialysis (ISPD) has recently issued updated guidelines for PD‐related peritonitis prevention, which do not recommend any specific method of catheter implantation or type of catheter for the prevention of peritonitis in PD patients (Li 2016; Szeto 2017). These guidelines are largely based on the previous Cochrane review (Strippoli 2004). Since the last review, there have been several RCTs published on the different catheter types and implantation techniques in PD patients. The present review examined the role of catheter‐related interventions, including different catheter types, placement and insertion techniques, in mitigating the risk of peritonitis in PD patients.
Description of the intervention
One of the key strategies employed to prevent PD‐related peritonitis is to reduce the risk of microbial contamination via PD catheters. Different catheter‐related interventions were examined in the review, including various catheter implantation methods (laparoscopic insertion, open surgery, percutaneous insertion, ureteroscope‐assisted insertion, cystoscopy‐assisted insertion, radiological insertion, midline or lateral insertion, implantation and subcutaneous burying of catheter with a resting period prior to catheter use, modified surgery with catheter fixation), different catheter types (single‐cuff, double‐cuff, triple‐cuff, straight catheter, coiled catheter, self‐locating catheter, swan‐neck catheter, Moncrief‐Popovich catheter, antibiotic‐treated catheter), use of silver rings at exit‐sites, immobilization of PD catheters, and break‐in periods.
How the intervention might work
A randomised study by Gadallah 1999 reported that early peritonitis episodes (within 2 weeks of catheter placement) were significantly lower in76 patients who underwent catheter insertion via a peritoneoscopic approach compared to 72 patients with surgically placed catheters (2.6% versus 12.5%, P = 0.02). The previous systematic review conducted in 2004 (Strippoli 2004) reported that no specific catheter implantation technique was beneficial in lowering the risk of peritonitis. Since then, the approaches in catheter insertion technique and types of available catheters have evolved, which may have impacted on the risk of peritonitis and in turn translated into improvements in catheter and/or technique survival
Why it is important to do this review
The ISPD guidelines do not recommend any specific implantation method or any specific type of catheter for prevention of peritonitis in PD patients. This recommendation was mainly based on the results of the previous review. Since then, more randomised controlled trials (RCTs) have been published on this topic which this update will include.
Objectives
To evaluate the role of different catheter implantation techniques and catheter types in lowering the risk of PD‐related peritonitis in PD patients.
Methods
Criteria for considering studies for this review
Types of studies
All RCTs and quasi‐RCTs (RCTs in which allocation to treatment was obtained by alternation, use of alternate medical records, date of birth or other predictable methods) investigating the effect of different catheter types, placement and insertion techniques for the prevention of peritonitis in PD patients.
Types of participants
Inclusion criteria
Adults and children undergoing PD treatment for end‐stage kidney disease.
Exclusion criteria
Patients not on PD.
Types of interventions
Surgical catheter insertion techniques (laparoscopy, laparotomy, subcutaneous burying and rest of catheter, standard insertion with resting but no subcutaneous burying of catheter, midline insertion, lateral insertion)
Catheter types (straight, coiled, self‐locating catheter, Tenckhoff catheter with an artificial curve at the subcutaneous tract, single‐cuffed, double‐cuffed, triple‐cuffed, antibiotic treated catheter
Use of immobilisation techniques
Break‐in periods
Use of silver ring at exit‐site (new intervention identified during updated search).
Types of outcome measures
Primary outcomes
Peritonitis: number of patients with peritonitis (peritonitis defined as dialysate count of > 100 cells/mm3 with > 50% being polymorphonuclear leukocytes) and peritonitis rate
Exit‐site and tunnel infection: number of patients with exit‐site and tunnel infection and exit‐site and tunnel infection rates.
Secondary outcomes
Catheter removal/catheter replacement
Technique failure (transfer from PD to haemodialysis)
Death (all causes)
Peritonitis relapse
Peritonitis‐related death
Time to first peritonitis episode.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Kidney and Transplant Register of Studies up to 15 January 2019 through contact with the Information Specialist using search terms relevant to this review. The Register contains studies identified from the following sources.
Monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL)
Weekly searches of MEDLINE OVID SP
Handsearching of kidney‐related journals and the proceedings of major kidney and transplant conferences
Searching of the current year of EMBASE OVID SP
Weekly current awareness alerts for selected kidney and transplant journals
Searches of the International Clinical Trials Register (ICTRP) Search Portal and ClinicalTrials.gov.
Studies contained in the Register are identified through searches of CENTRAL, MEDLINE, and EMBASE based on the scope of Cochrane Kidney and Transplant. Details of search strategies, as well as a list of handsearched journals, conference proceedings and current awareness alerts, are available in the Specialised Register section of information about Cochrane Kidney and Transplant.
See Appendix 1 for search terms used in strategies for this review.
Searching other resources
Reference lists of review articles, relevant studies and clinical practice guidelines.
Letters seeking information about unpublished or incomplete studies to investigators known to be involved in previous studies.
Data collection and analysis
Selection of studies
The search strategies described were used to obtain titles and abstracts of studies that may be relevant to the review. The titles and abstracts were screened independently by two authors, who discarded studies that were not applicable, however studies and reviews that may have included relevant data or information on studies were retained initially. Two authors independently assessed retrieved abstracts and, where necessary the full text, of these studies to determine which studies satisfied the inclusion criteria.
Data extraction and management
Data extraction was carried out independently by two authors using standard data extraction forms. It was planned that studies reported in non‐English language journals would be translated before assessment. Where more than one publication of one study existed, reports were grouped together and the publication with the most complete data was included.
Assessment of risk of bias in included studies
The following items were assessed independently by two authors using the risk of bias assessment tool (Higgins 2011) (see Appendix 2).
Was there adequate sequence generation (selection bias)?
Was allocation adequately concealed (selection bias)?
-
Was knowledge of the allocated interventions adequately prevented during the study?
Participants and personnel (performance bias)
Outcome assessors (detection bias)
Were incomplete outcome data adequately addressed (attrition bias)?
Are reports of the study free of suggestion of selective outcome reporting (reporting bias)?
Was the study apparently free of other problems that could put it at a risk of bias?
Measures of treatment effect
Data from individual studies were analysed using the risk ratio (RR) measure and its 95% confidence intervals (CI). Subgroup analysis was planned to explore potential sources of variability in observed treatment effect where possible (children versus adult population, diabetic versus non‐diabetic, study quality, timing of peritonitis or other outcome). Absolute effects were reported where appropriate.
Unit of analysis issues
Where data on the number of subjects with events (e.g. number of participants with one or more episodes of peritonitis) were available, the RR was calculated as the ratio of the incidence of the event (one or more episodes) in the experimental treatment group over the incidence in the control group. Where data on the number of episodes were available, then the RR was calculated as the ratio of the rate of the outcome (e.g. the peritonitis rate) in the experimental treatment group (given by number of episodes of the outcome over total patient months on PD) over the rate in the control group.
Dealing with missing data
Any further information or clarification required from the authors was requested by written or electronic correspondence and relevant information obtained in this manner was included in the review. Disagreements were resolved in consultation with the other two authors.
Assessment of heterogeneity
We first assessed the heterogeneity by visual inspection of the forest plot. We then quantified statistical heterogeneity using the I2 statistic, which describes the percentage of total variation across studies that is due to heterogeneity rather than sampling error (Higgins 2003). A guide to the interpretation of I2 values was as follows.
0% to 40%: might not be important
30% to 60%: may represent moderate heterogeneity
50% to 90%: may represent substantial heterogeneity
75% to 100%: considerable heterogeneity.
The importance of the observed value of I2 depends on the magnitude and direction of treatment effects and the strength of evidence for heterogeneity (e.g. P‐value from the Chi2 test, or a confidence interval for I2) (Higgins 2011).
Assessment of reporting biases
It was also planned that if sufficient RCTs were identified, an attempt would be made to assess for publication bias using a funnel plot (Egger 1997).
Data synthesis
When appropriate, summary estimators of treatment effects were calculated using a random effects model with RR and its 95% CI.
Subgroup analysis and investigation of heterogeneity
Subgroup analysis was used to explore possible sources of heterogeneity (e.g. study duration, participants, interventions and study quality). Heterogeneity among participants may have been related to age and co‐existing conditions, for example diabetes mellitus. Heterogeneity in interventions may have been related to prior prophylactic antibiotics used and the type and dose of therapy. If subgroup analysis was unable to be performed due to absence of other similar studies, this limitation was acknowledged and discussed in the manuscript.
Sensitivity analysis
Where sufficient studies were available we investigated the following:
Studies with data from RCTs only or quasi RCTs only
Studies with different risks of bias together, for example, studies with low attrition bias risk and studies with high attrition bias risk.
Summary of findings' tables
We presented the main results of the review in 'Summary of findings' tables. These tables present key information concerning the quality of the evidence, the magnitude of the effects of the interventions examined, and the sum of the available data for the main outcomes (Schünemann 2011a). The 'Summary of findings' tables also include an overall grading of the evidence related to each of the main outcomes using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach (GRADE 2008; GRADE 2011). The GRADE approach defines the quality of a body of evidence as the extent to which one can be confident that an estimate of effect or association is close to the true quantity of specific interest. The quality of a body of evidence involves consideration of within‐trial risk of bias (methodological quality), directness of evidence, heterogeneity, precision of effect estimates and risk of publication bias (Schünemann 2011b). We presented the following outcomes in the 'Summary of findings' tables.
Incidence of peritonitis (defined as number of patients with peritonitis)
Peritonitis rate (episode/patient‐months)
Incidence of exit‐site/tunnel infection (defined as number of patients of exit‐site/tunnel infection)
Exit‐site/tunnel infection rate (episode/patient‐months)
Catheter removal/replacement
Technique failure (death‐censored)
Death (all causes).
Results
Description of studies
Results of the search
The original Cochrane review contained 17 included studies (Akyol 1990; Danielsson 2002; Dasgupta 1998; Ejlersen 1990; Eklund 1994; Eklund 1995; Eklund 1997; Gadallah 1999; Lye 1996; Moncrief 1998; Nielsen 1995; Park 1998; Rubin 1990; Scott 1994; Tsimoyiannis 2000; Turner 1992; Wright 1999) and two ongoing studies.
For this update we searched Cochrane Kidney and Transplant's Specialised Register up to January 2019 and identified 49 new reports. After full‐text assessment 34 new studies were identified: 25 new studies (34 reports) were included (Akcicek 1995; Al‐Hwiesh 2016; Atapour 2011; Buijsen 1994; Chen 2014a; Johnson 2006; Jwo 2010; Li 2009e; Lo 2003b; Merrikhi 2014; Ouyang 2015; Qian 2014; Sanchez‐Canel 2016; SIPROCE 1997; Stegmayr 2005a; Stegmayr 2015; Sun 2015a; Timely PD 2010; Trooskin 1990; Voss 2012; Winch 2000; Xie 2011a; Yip 2010; Zhang 2016; Zhu 2015), 6 studies (6 reports) were excluded (Crabtree 2003; ISRCTN87054124; Moncrief 1994; N0547061060; O'Dwyer 2005; Williams 1989), and two ongoing studies were identified (NCT01023191; NCT02479295). Three studies are awaiting assessment (no data available and awaiting author response) (Ahmad 2010; LOCI 2011; Wong 2004b). We also identified three new reports of three existing included studies.
For this update a total of 42 studies (54 reports, 3144 participants) (Figure 1) were included.
1.
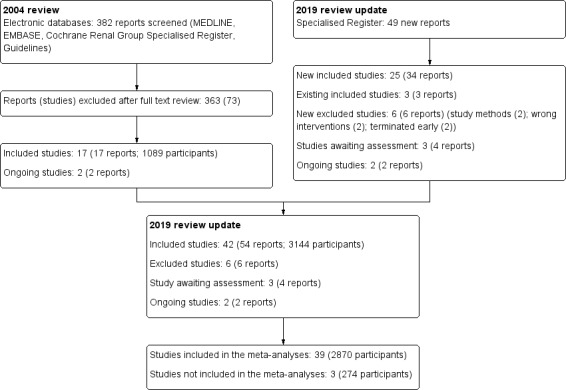
Study flow diagram.
Included studies
Eighteen studies (1314 randomised participants) examined different methods of catheter insertion.
Laparoscopy versus laparotomy: 4 studies (320 participants) (Gadallah 1999; Jwo 2010; Tsimoyiannis 2000; Wright 1999)
Subcutaneous burying with a period of resting of the catheter versus standard insertion: 3 studies (232 participants) (Danielsson 2002; Moncrief 1998; Park 1998)
Midline versus lateral insertion: 2 studies (122 participants) (Ejlersen 1990; Rubin 1990)
Open surgery versus percutaneous implantation: 2 studies (96 participants) (Atapour 2011; Merrikhi 2014)
Open surgery versus open surgery with omentum folding: 1 study (67 participants) (Chen 2014a)
Radiological versus surgical implantation: 1 study (113 participants) (Voss 2012)
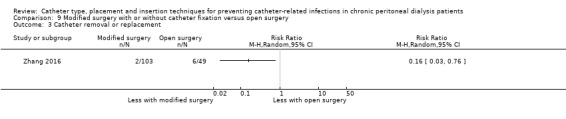
Open surgery versus modified open surgery with or without catheter fixation: 1 study (152 participants) (Zhang 2016)
Conventional open surgery versus vertical tunnel‐based low‐site implantation: 1 study (89 participant) (Sun 2015a)
Open surgery versus ureteroscopic‐assisted surgery: 1 study (72 participants) (Zhu 2015)
Cystoscopy‐assisted surgery versus open surgery: 1 study (29 participants) (Qian 2014)
Laparoscopic Moncrief‐Popovich technique versus blind trocar technique: 1 study (22 participants) (Akcicek 1995).
Twenty‐one studies (1447 randomised participants) examined different types of PD catheters.
Straight versus coiled catheters: 12 studies (878 participants) (Akyol 1990; Dasgupta 1998; Eklund 1994; Eklund 1995; Johnson 2006; Lo 2003b; Lye 1996; Nielsen 1995; Ouyang 2015; Scott 1994; Stegmayr 2005a; Xie 2011a)
Straight‐tip versus self‐locating tip catheters: 2 studies (139 participants) (Sanchez‐Canel 2016; Stegmayr 2015)
Swan‐neck straight‐tip versus straight‐tip with artificial curve at subcutaneous tunnel tract: 2 studies (140 participants) (Li 2009e; Yip 2010)
Single versus double cuff catheters: 2 studies (109 participants) (Buijsen 1994; Eklund 1997)
Double versus triple cuff catheters: 1 study (73 participants) (Al‐Hwiesh 2016)
Swan‐neck versus straight curled catheter: 1 study (22 participants) (Winch 2000)
Antibiotic‐treated versus standard catheters: 1 study (86 participants) (Trooskin 1990).
There were two additional studies that examined other interventions: one study (195 participants) (SIPROCE 1997) compared a silver ring versus no silver ring at the exit‐site, and one study (66 participants) (Turner 1992) compared immobilisation versus non‐immobilisation of PD catheters.
There was one study examining the different break‐in periods (122 participants) (Timely PD 2010).
Three studies could not be included in the meta‐analyses (Dasgupta 1998; Moncrief 1998; Timely PD 2010).
Excluded studies
Six studies did not meet our inclusion criteria and were excluded (Figure 1). The reasons for exclusion were wrong study methods (Crabtree 2003; N0547061060), wrong interventions (O'Dwyer 2005; Williams 1989), or terminated early (ISRCTN87054124; Moncrief 1994).
Risk of bias in included studies
The quality of the studies was difficult to assess because many details such as the use of intention‐to‐treat analysis and the number of patients lost to follow‐up were difficult to ascertain or were not provided. In general, study quality was variable and almost all aspects of study design did not fulfil CONSORT standards for reporting (CONSORT 2001). Risk of bias for the individual studies is presented in Figure 2 and the summary is presented in Figure 3.
2.
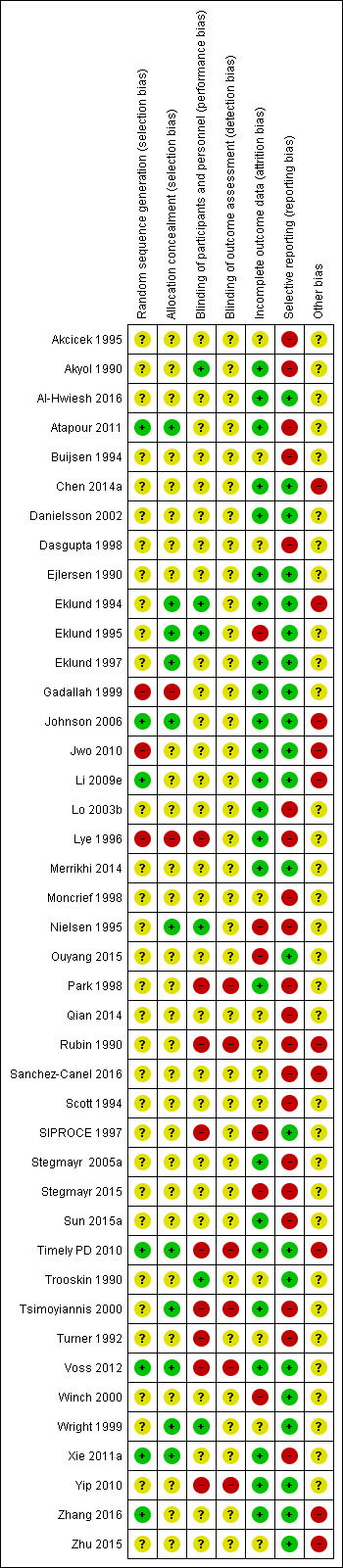
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
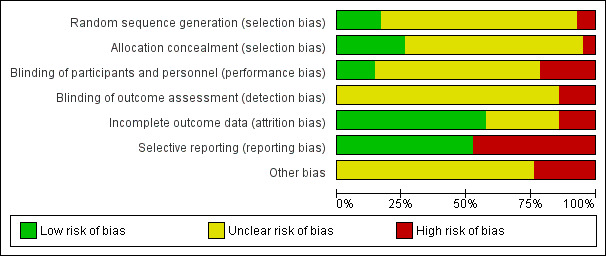
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Random sequence generation
Random sequence generation was judged to be at low risk of bias in seven studies (Atapour 2011; Johnson 2006; Li 2009e; Timely PD 2010; Voss 2012; Xie 2011a; Zhang 2016) and at high risk of bias in three studies (Gadallah 1999; Jwo 2010; Lye 1996). The risk of bias was unclear for the remaining 32 studies.
Allocation concealment
Allocation concealment was judged to be at low risk of bias in 11 studies (Atapour 2011; Eklund 1994; Eklund 1995; Eklund 1997; Johnson 2006; Nielsen 1995; Timely PD 2010; Tsimoyiannis 2000; Voss 2012; Wright 1999; Xie 2011a) and at high risk of bias in two studies (Gadallah 1999; Lye 1996). The risk of bias was unclear in the remaining 29 studies.
Blinding
Performance bias (blinding of participants and investigators) was judged to be at low risk of bias in six studies (Akyol 1990; Eklund 1994; Eklund 1995; Nielsen 1995; Trooskin 1990; Wright 1999) and at high risk of bias in nine studies (Lye 1996; Park 1998; Rubin 1990; SIPROCE 1997; Timely PD 2010; Tsimoyiannis 2000; Turner 1992; Voss 2012; Yip 2010). The risk of bias was unclear in the remaining 27 studies.
Detection bias (blinding of outcome assessors) was judged to be at high risk of bias in six studies (Park 1998; Rubin 1990; Timely PD 2010; Tsimoyiannis 2000; Voss 2012; Yip 2010). The risk of bias was unclear in the remaining 36 studies.
Incomplete outcome data
Attrition bias was judged to be at low risk of bias in 24 studies (Akyol 1990; Al‐Hwiesh 2016; Atapour 2011; Chen 2014a; Danielsson 2002; Ejlersen 1990; Eklund 1994; Eklund 1997; Gadallah 1999; Johnson 2006; Jwo 2010; Li 2009e; Lo 2003b; Lye 1996; Merrikhi 2014; Park 1998; Stegmayr 2005a; Sun 2015a; Timely PD 2010; Tsimoyiannis 2000; Voss 2012; Xie 2011a; Yip 2010; Zhang 2016) and at high risk of bias in six studies (Eklund 1995; Nielsen 1995; Ouyang 2015; SIPROCE 1997; Stegmayr 2015; Winch 2000). The risk of bias was unclear in the remaining 12 studies.
Selective reporting
Reporting bias was judged to be at low risk of bias in 22 studies (Al‐Hwiesh 2016; Chen 2014a; Danielsson 2002; Ejlersen 1990; Eklund 1994; Eklund 1995; Eklund 1997; Gadallah 1999; Johnson 2006; Jwo 2010; Li 2009e; Merrikhi 2014; Ouyang 2015; SIPROCE 1997; Timely PD 2010; Trooskin 1990; Voss 2012; Winch 2000; Wright 1999; Yip 2010; Zhang 2016; Zhu 2015) and at high risk of bias in 20 studies (Akcicek 1995; Akyol 1990; Atapour 2011; Buijsen 1994; Dasgupta 1998; Lo 2003b; Lye 1996; Moncrief 1998; Nielsen 1995; Park 1998; Qian 2014; Rubin 1990; Sanchez‐Canel 2016; Scott 1994; Stegmayr 2005a; Stegmayr 2015; Sun 2015a; Tsimoyiannis 2000; Turner 1992; Xie 2011a).
Other potential sources of bias
Ten studies (23%) were identified as high risk for other potential sources of bias. The potential sources of other risks of bias included: different baseline characteristics between the two groups (Johnson 2006; Jwo 2010; Sanchez‐Canel 2016; Zhang 2016; Zhu 2015; 511 participants); use of a different definition for peritonitis (Eklund 1994; 40 participants); premature study closure due to insufficient supply of the intervention (Li 2009e; 39 participants); examination of two distinct interventions (the new method of insertion and new catheter or new method insertion (Rubin 1990) and different connection methods (Chen 2014a)) in the treatment arm (152 participants); and violation of study protocols (Timely PD 2010; 122 participants).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7
Summary of findings for the main comparison. Laparoscopy versus laparotomy for preventing catheter‐related infections in chronic peritoneal dialysis patients.
| Laparoscopy versus laparotomy for preventing catheter‐related infections in chronic peritoneal dialysis patients | |||||
| Patient or population: chronic peritoneal dialysis patients Intervention: laparoscopy Comparison: laparotomy | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants or patient‐months (studies) | Certainty of the evidence (GRADE) | |
| Risk with laparotomy | Risk with laparoscopy | ||||
| Peritonitis | 242 per 1,000 | 218 per 1,000 (143 to 327) | RR 0.90 (0.59 to 1.35) | 315 (4) | ⊕⊕⊕⊝ MODERATE 1 |
| Peritonitis rate (patient‐months) | 59 per 1,000 | 52 per 1,000 (23 to 122) | RR 0.89 (0.39 to 2.07) | 375 (1) | ⊕⊝⊝⊝ VERY LOW 2 |
| Exit‐site/tunnel infection | 125 per 1,000 | 125 per 1,000 (54 to 289) | RR 1.00 (0.43 to 2.31) | 270 (3) | ⊕⊕⊝⊝ LOW 3 |
| Catheter removal or replacement | 281 per 1,000 | 337 per 1,000 (216 to 522) | RR 1.20 (0.77 to 1.86) | 167 (3) | ⊕⊕⊝⊝ LOW 3 |
| Technique failure | 293 per 1,000 | 208 per 1,000 (137 to 316) | RR 0.71 (0.47 to 1.08) | 283 (4) | ⊕⊕⊝⊝ LOW 3 |
| Death (all causes) | 140 per 1,000 | 176 per 1,000 (101 to 307) | RR 1.26 (0.72 to 2.20) | 270 (3) | ⊕⊕⊕⊝ MODERATE 1 |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded one level: suboptimal quality of studies
2 Downgraded two levels: single study with suboptimal quality and imprecision
3 Downgraded two levels: suboptimal quality and imprecision
Summary of findings 2. Buried (subcutaneous) versus non‐buried catheter for preventing catheter‐related infections in chronic peritoneal dialysis patients.
| Buried (subcutaneous) versus non‐buried catheter for preventing catheter‐related infections in chronic peritoneal dialysis patients | |||||
| Patient or population: chronic peritoneal dialysis patients Intervention: buried (subcutaneous) catheter Comparison: non‐buried catheter | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants or patient‐months (studies) | Certainty of the evidence (GRADE) | |
| Risk with non‐buried | Risk with buried (subcutaneous) | ||||
| Peritonitis rate (patient‐months) | 37 per 1,000 | 43 per 1,000 (14 to 133) | RR 1.16 (0.37 to 3.60) | 2511 (2) | ⊕⊝⊝⊝ VERY LOW 1 |
| Exit‐site/tunnel infection rate (patient‐months) | 31 per 1,000 | 36 per 1,000 (12 to 106) | RR 1.15 (0.39 to 3.42) | 2511 (2) | ⊕⊝⊝⊝ VERY LOW 1 |
| Technique failure | 367 per 1,000 | 268 per 1,000 (125 to 568) | RR 0.73 (0.34 to 1.55) | 60 (1) | ⊕⊝⊝⊝ VERY LOW 2 |
| Death (all causes) | 169 per 1,000 | 153 per 1,000 (66 to 353) | RR 0.90 (0.39 to 2.08) | 119 (2) | ⊕⊕⊕⊝ MODERATE 3 |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded three levels: suboptimal quality, inconsistency, and imprecision
2 Downgraded three levels: single study, suboptimal quality, and imprecision
3 Downgraded two levels: suboptimal quality of studies and imprecision
Summary of findings 3. Midline versus lateral insertion for preventing catheter‐related infections in chronic peritoneal dialysis patients.
| Midline versus lateral insertion for preventing catheter‐related infections in chronic peritoneal dialysis patients | |||||
| Patient or population: chronic peritoneal dialysis patients Intervention: midline insertion Comparison: lateral insertion | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with lateral | Risk with midline | ||||
| Peritonitis | 255 per 1,000 | 166 per 1,000 (82 to 339) | RR 0.65 (0.32 to 1.33) | 120 (2) | ⊕⊕⊕⊝ MODERATE 1 |
| Exit‐site/tunnel infection | 78 per 1,000 | 44 per 1,000 (9 to 202) | RR 0.56 (0.12 to 2.58) | 120 (2) | ⊕⊕⊝⊝ LOW 2 |
| Catheter removal or replacement | 514 per 1,000 | 293 per 1,000 (170 to 504) | RR 0.57 (0.33 to 0.98) | 83 (1) | ⊕⊝⊝⊝ VERY LOW 3 |
| Death (all causes) | 0 per 1,000 | 0 per 1,000 (0 to 0) | RR 8.50 (0.50 to 143.32) | 37 (1) | ⊕⊝⊝⊝ VERY LOW 3 |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded one level: suboptimal quality of studies
2 Downgraded two levels: suboptimal quality and imprecision
3 Downgraded three levels: single study, suboptimal quality study, and imprecision
Summary of findings 4. Percutaneous insertion versus open surgery for preventing catheter‐related infections in chronic peritoneal dialysis patients.
| Percutaneous insertion versus open surgery for preventing catheter‐related infections in chronic peritoneal dialysis patients | |||||
| Patient or population: chronic peritoneal dialysis patients Intervention: percutaneous insertion Comparison: open surgery | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with open surgery | Risk with percutaneous insertion | ||||
| Exit‐site/tunnel infection | 106 per 1,000 | 17 per 1,000 (2 to 138) | RR 0.16 (0.02 to 1.30) | 96 (2 RCTs) | ⊕⊕⊕⊝ MODERATE 1 |
| Catheter removal or replacement | 133 per 1,000 | 32 per 1,000 (4 to 272) | RR 0.24 (0.03 to 2.04) | 61 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 2 |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded one level: suboptimal quality of studies
2 Downgraded two levels: single study with suboptimal quality and imprecision
Summary of findings 5. Straight versus coiled catheters for preventing catheter‐related infections in chronic peritoneal dialysis patients.
| Straight versus coiled catheters for preventing catheter‐related infections in chronic peritoneal dialysis patients | |||||
| Patient or population: chronic peritoneal dialysis patients Intervention: straight Comparison: coiled | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants or patient‐months (studies) | Certainty of the evidence (GRADE) | |
| Risk with coiled | Risk with straight | ||||
| Peritonitis | 217 per 1,000 | 225 per 1,000 (178 to 284) | RR 1.04 (0.82 to 1.31) | 818 (9) | ⊕⊕⊕⊝ MODERATE 1 |
| Peritonitis rate (patient‐months) | 32 per 1,000 | 29 per 1,000 (22 to 39) | RR 0.91 (0.68 to 1.21) | 5882 (5) | ⊕⊕⊕⊝ MODERATE 1 |
| Exit‐site/tunnel infection | 281 per 1,000 | 314 per 1,000 (264 to 376) | RR 1.12 (0.94 to 1.34) | 826 (10) | ⊕⊕⊕⊝ MODERATE 1 |
| Exit‐site/tunnel infection rate (patient‐months) | 27 per 1,000 | 28 per 1,000 (21 to 39) | RR 1.05 (0.77 to 1.43) | 5286 (4) | ⊕⊕⊕⊝ MODERATE 1 |
| Catheter removal or replacement | 249 per 1,000 | 276 per 1,000 (181 to 413) | RR 1.11 (0.73 to 1.66) | 713 (9) | ⊕⊝⊝⊝ VERY LOW 1 2 3 |
| Technique failure | 131 per 1,000 | 108 per 1,000 (67 to 172) | RR 0.82 (0.51 to 1.31) | 442 (4) | ⊕⊕⊕⊝ MODERATE 1 |
| Death (all causes) | 124 per 1,000 | 117 per 1,000 (77 to 180) | RR 0.95 (0.62 to 1.46) | 703 (8) | ⊕⊕⊝⊝ LOW 1 3 |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded one level: most studies are of suboptimal quality
2 Downgrade one level: inconsistency
3 Downgraded one level: publication bias
Summary of findings 6. Tenckhoff catheter with artificial curve at tunnel tract versus swan‐neck for preventing catheter‐related infections in chronic peritoneal dialysis patients.
| Tenckhoff catheter with artificial curve at tunnel tract versus swan‐neck for preventing catheter‐related infections in chronic peritoneal dialysis patients | |||||
| Patient or population: preventing catheter‐related infections in chronic peritoneal dialysis patients Intervention: Tenckhoff catheter with artificial curve at tunnel tract Comparison: swan‐neck | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants or patient‐months (studies) | Certainty of the evidence (GRADE) | |
| Risk with swan‐neck | Risk with Tenckhoff | ||||
| Peritonitis | 329 per 1,000 | 424 per 1,000 (279 to 644) | RR 1.29 (0.85 to 1.96) | 140 (2) | ⊕⊕⊝⊝ LOW 1 |
| Peritonitis rate (patient‐months) | 47 per 1,000 | 57 per 1,000 (25 to 129) | RR 1.22 (0.54 to 2.75) | 2535 (2) | ⊕⊕⊝⊝ LOW 2 |
| Exit‐site/tunnel infection | 671 per 1,000 | 645 per 1,000 (517 to 812) | RR 0.96 (0.77 to 1.21) | 140 (2) | ⊕⊕⊕⊝ MODERATE 3 |
| Exit‐site/tunnel infection rate (patient‐months) | 83 per 1,000 | 55 per 1,000 (41 to 74) | RR 0.67 (0.50 to 0.90) | 2535 (2) | ⊕⊕⊕⊝ MODERATE 3 |
| Catheter removal or replacement | 229 per 1,000 | 194 per 1,000 (96 to 393) | RR 0.85 (0.42 to 1.72) | 140 (2) | ⊕⊕⊕⊝ MODERATE 3 |
| Technique failure | 157 per 1,000 | 101 per 1,000 (41 to 248) | RR 0.64 (0.26 to 1.58) | 140 (2) | ⊕⊕⊕⊝ MODERATE 3 |
| Death (all causes) | 114 per 1,000 | 85 per 1,000 (31 to 232) | RR 0.74 (0.27 to 2.03) | 140 (2) | ⊕⊕⊝⊝ LOW 1 |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded two levels: suboptimal quality of studies and imprecision
2 Downgraded two levels: suboptimal quality of studies and inconsistency
3 Downgraded one level: suboptimal quality of studies
Summary of findings 7. Self‐locating versus straight Tenckhoff catheter for preventing catheter‐related infections in chronic peritoneal dialysis patients.
| Self‐locating versus straight Tenckhoff catheter for preventing catheter‐related infections in chronic peritoneal dialysis patients | |||||
| Patient or population: chronic peritoneal dialysis patients Intervention: self‐locating catheter Comparison: straight Tenckhoff catheter | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with straight Tenckhoff | Risk with self‐locating | ||||
| Peritonitis | 684 per 1,000 | 773 per 1,000 (588 to 1,000) | RR 1.13 (0.86 to 1.49) | 78 (1) | ⊕⊝⊝⊝ VERY LOW 1 |
| Exit‐site/tunnel infection | 184 per 1,000 | 175 per 1,000 (68 to 451) | RR 0.95 (0.37 to 2.45) | 78 (1) | ⊕⊝⊝⊝ VERY LOW 1 |
| Catheter removal or replacement | 343 per 1,000 | 110 per 1,000 (10 to 1,000) | RR 0.32 (0.03 to 3.06) | 139 (2) | ⊕⊝⊝⊝ VERY LOW 2 |
| Technique failure | 414 per 1,000 | 265 per 1,000 (162 to 431) | RR 0.64 (0.39 to 1.04) | 139 (2) | ⊕⊕⊕⊝ MODERATE 3 |
| Death (all causes) | 71 per 1,000 | 73 per 1,000 (8 to 696) | RR 1.02 (0.11 to 9.75) | 139 (2) | ⊕⊕⊝⊝ LOW 4 |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded three levels: single study, suboptimal quality, and imprecision
2 Downgraded three levels: suboptimal quality, imprecision and inconsistency
3 Downgraded one level: suboptimal quality of study
4 Downgraded two levels: suboptimal quality and imprecision
Laparoscopy versus laparotomy
Laparoscopy insertion compared with laparotomy probably makes little or no difference to the incidence of peritonitis (Analysis 1.1 (4 studies, 315 participants): RR 0.90, 95% CI 0.59 to 1.35, P = 0.60; I2 = 5%; moderate certainty evidence; 24 fewer per 1000), exit site/tunnel infection (Analysis 1.3 (3 studies, 270 participants): RR 1.00, 95% CI 0.43 to 2.31, P = 0.99; I2 = 30%; low certainty evidence; 0 fewer per 1000), catheter removal or replacement (Analysis 1.4 (3 studies, 167 participants): RR 1.20, 95% CI 0.77 to 1.86, P = 0.42; I2 = 0%; low certainty evidence), technique failure (Analysis 1.5 (4 studies, 283 participants): RR 0.71, 95% CI 0.47 to 1.08, P = 0.11, I2 = 5%; low certainty evidence), and death (all causes) (Analysis 1.6 (3 studies, 270 participants): RR 1.26, 95% CI 0.72 to 2.20, P = 0.42; I2 = 0%; moderate certainty evidence) (Table 1). Wright 1999 reported no difference in peritonitis rate between laparoscopy and laparotomy (Analysis 1.2 (375 patient‐months): RR 0.89, 95% CI 0.39 to 2.07). Laparoscopy may make little or no difference to dialysate leak compared with laparotomy insertion (Analysis 1.7 (3 studies, 167 participants): RR 0.85, 95% CI 0.10 to 6.97, P = 0.88; I2 = 63%; low certainty evidence).
1.1. Analysis.
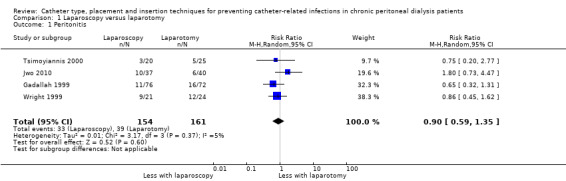
Comparison 1 Laparoscopy versus laparotomy, Outcome 1 Peritonitis.
1.3. Analysis.
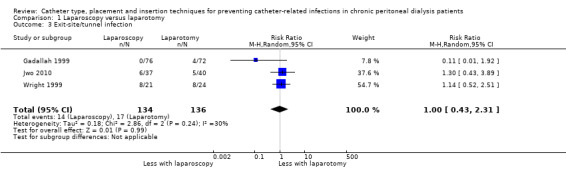
Comparison 1 Laparoscopy versus laparotomy, Outcome 3 Exit‐site/tunnel infection.
1.4. Analysis.
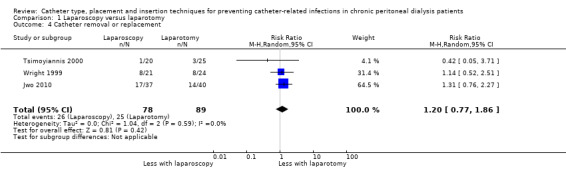
Comparison 1 Laparoscopy versus laparotomy, Outcome 4 Catheter removal or replacement.
1.5. Analysis.
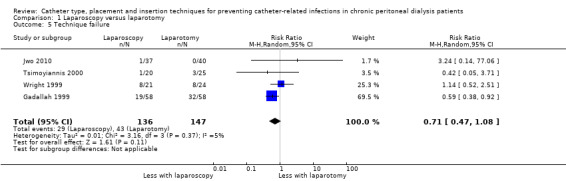
Comparison 1 Laparoscopy versus laparotomy, Outcome 5 Technique failure.
1.6. Analysis.
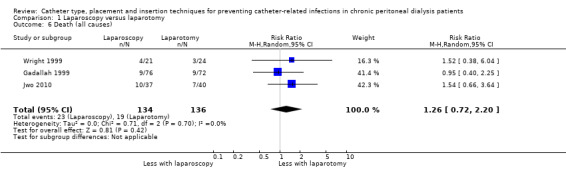
Comparison 1 Laparoscopy versus laparotomy, Outcome 6 Death (all causes).
1.2. Analysis.
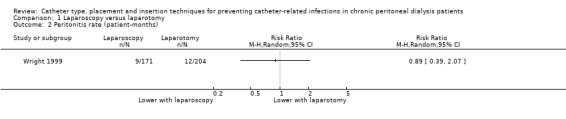
Comparison 1 Laparoscopy versus laparotomy, Outcome 2 Peritonitis rate (patient‐months).
1.7. Analysis.
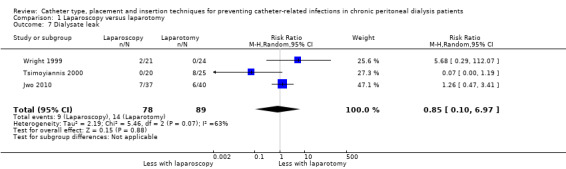
Comparison 1 Laparoscopy versus laparotomy, Outcome 7 Dialysate leak.
Moderate heterogeneity was resolved by subgroup analysis with different break‐in periods. Jwo 2010 reported 3 post‐operative bleeding (haematoma or haemoperitoneum) and 2 hernia in laparoscopic insertion compared with 8 bleed and 1 hernia in laparotomy (Table 8).
1. Adverse events.
| Study ID | Intervention group | Control group | ||
| Events | Total | Events | Total | |
| Haematoma or haemoperitoneum | ||||
| Atapour 2011 | 1 | 31 | 4 | 30 |
| Chen 2014a | 7 | 34 | 4 | 32 |
| Sanchez‐Canel 2016 | 7 | 40 | 6 | 38 |
| Al‐Hwiesh 2016 | 0 | 36 | 0 | 37 |
| Merrikhi 2014 | 0 | 18 | 2 | 17 |
| Ouyang 2015 | 3 | 99 | 2 | 90 |
| Eklund 1994 | 0 | 20 | 0 | 20 |
| Eklund 1995 | 0 | 20 | 0 | 20 |
| Li 2009e | 14 | 20 | 22 | 19 |
| Rubin 1990 | 1 | 48 | 1 | 35 |
| Scott 1994 | 0 | 30 | 1 | 59 |
| Zhang 2016 | 1 | 103 | 0 | 49 |
| Dialysate leak | ||||
| Chen 2014a | 2 | 34 | 1 | 32 |
| Sanchez‐Canel 2016 | 9 | 40 | 7 | 38 |
| Jwo 2010 | 7 | 40 | 6 | 37 |
| Atapour 2011 | 1 | 31 | 1 | 30 |
| Al‐Hwiesh 2016 | 2 | 36 | 3 | 37 |
| Akcicek 1995 | 2 | 10 | 4 | 12 |
| Akyol 1990 | 0 | 20 | 2 | 20 |
| Eklund 1994 | 0 | 20 | 4 | 20 |
| Eklund 1995 | 0 | 20 | 0 | 20 |
| Nielsen 1995 | 1 | 38 | 0 | 34 |
| Ouyang 2015 | 0 | 99 | 3 | 90 |
| Qian 2014 | 0 | 14 | 1 | 15 |
| Rubin 1990 | 6 | 48 | 3 | 35 |
| Scott 1994 | 2 | 30 | 0 | 59 |
| Stegmayr 2015 | 1 | 29 | 3 | 32 |
| Voss 2012 | 4 | 57 | 10 | 56 |
| Winch 2000 | 2 | 11 | 0 | 11 |
| Wright 1999 | 2 | 21 | 0 | 24 |
| Xie 2011a | 1 | 40 | 0 | 40 |
| Yip 2010 | 0 | 50 | 0 | 51 |
| Zhang 2016 | 0 | 103 | 1 | 49 |
| Viscus perforation | ||||
| Nielsen 1995 (bladder perforation) | 0 | 38 | 1 | 34 |
| Al‐Hwiesh 2016 (bowel perforation) | 0 | 36 | 0 | 37 |
| Merrikhi 2014 (hollow viscus perforation) | 0 | 18 | 0 | 17 |
| Atapour 2011 | 0 | 31 | 0 | 30 |
| Outflow failure or catheter tip migration | ||||
| Atapour 2011 | 1 | 31 | 4 | 30 |
| Li 2009e | 2 | 20 | 1 | 19 |
| Sanchez‐Canel 2016 | 12 | 40 | 25 | 38 |
| Voss 2012 | 3 | 57 | 4 | 56 |
| Al‐Hwiesh 2016 | 1 | 36 | 11 | 37 |
| Scott 1994 | 1 | 30 | 2 | 59 |
| Lye 1996 | 3 | 20 | 1 | 20 |
| Qian 2014 | 0 | 14 | 1 | 15 |
| Akcicek 1995 | 1 | 10 | 3 | 12 |
| Winch 2000 | 1 | 11 | 1 | 11 |
| Hernia | ||||
| Chen 2014a | 0 | 34 | 1 | 32 |
| Jwo 2010 | 2 | 40 | 1 | 37 |
| Sanchez‐Canel 2016 | 7 | 40 | 7 | 38 |
| Ouyang 2015 | 4 | 99 | 6 | 90 |
| Xie 2011a | 2 | 40 | 2 | 40 |
| Voss 2012 | 4 | 57 | 8 | 56 |
| Zhang 2016 | 0 | 103 | 1 | 49 |
Implantation and subcutaneous burying of the catheter versus standard insertion with resting but no subcutaneous burying of the catheter
It is uncertain whether the subcutaneous burying of a PD catheter 6 weeks before initiation of PD prevents peritonitis rates (Analysis 2.1 (2 studies, 2511 patient‐months): RR 1.16, 95% CI 0.37 to 3.60, P = 0.80; I2 = 84%; very low certainty evidence). Subcutaneous burying of catheter may make little or no difference to exit site/tunnel infection (Analysis 2.2 (2 studies, 2511 patient‐months): RR 1.15, 95% CI 0.39 to 3.42, P = 0.80; I2 = 67%; low certainty evidence) and probably makes little or no difference to death (all causes) (Analysis 2.4 (2 studies, 119 participants): RR 0.90, 95% CI 0.39 to 2.08, P = 0.81; I2 = 0%; moderate certainty evidence) compared with standard PD catheter insertion. Danielsson 2002 reported no difference in technique failure between the two groups (Analysis 2.3 (60 participants): RR 0.33, 95% CI 0.04 to 3.03) (Table 2).
2.1. Analysis.
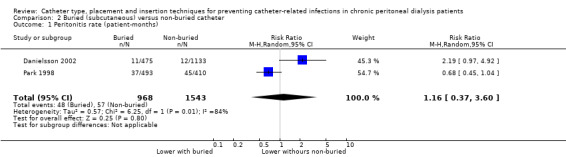
Comparison 2 Buried (subcutaneous) versus non‐buried catheter, Outcome 1 Peritonitis rate (patient‐months).
2.2. Analysis.
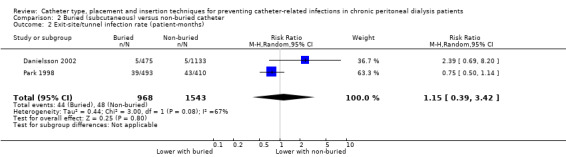
Comparison 2 Buried (subcutaneous) versus non‐buried catheter, Outcome 2 Exit‐site/tunnel infection rate (patient‐months).
2.4. Analysis.
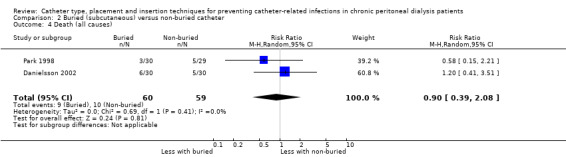
Comparison 2 Buried (subcutaneous) versus non‐buried catheter, Outcome 4 Death (all causes).
2.3. Analysis.
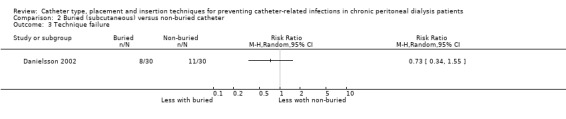
Comparison 2 Buried (subcutaneous) versus non‐buried catheter, Outcome 3 Technique failure.
There was considerable heterogeneity in the analysis of peritonitis rate and exit‐site/tunnel infection rate. A detailed subgroup analysis was unable to be performed given that only two studies were included. There were differences in study design (single versus multicentre study), catheter types (Moncrief‐Popovich catheter versus swan‐neck catheter), connection methodology (double bag versus either Y connector or standard spike), and follow‐up periods (0.4 to 44 months versus 12 months) between the two studies that could have introduced heterogeneity. Park 1998 reported no difference in post‐operative bleeding and dialysate leak between the two groups.
Midline versus lateral insertion of the PD catheter
The midline insertion compared with lateral insertion of PD catheters probably makes little or no difference to the risks of peritonitis (Analysis 3.1 (2 studies, 120 participants): RR 0.65, 95% CI 0.32 to 1.33, P = 0.24; I2 = 0%; moderate certainty evidence) and may make little or no difference to exit‐site/tunnel infection (Analysis 3.2 (2 studies, 120 participants): RR 0.56, 95% CI 0.12 to 2.58, P = 0.45; I2= 5%; low certainty evidence) compared with lateral insertion of PD catheter. Rubin 1990 reported midline insertion reduced the risk of catheter removal or replacement compared with lateral insertion (Analysis 3.3 (83 participants): RR 0.57, 95% CI 0.33 to 0.98, P = 0.04). Ejlersen 1990 reported no difference in death (all causes) between midline versus lateral insertion of catheter (Analysis 3.4 (37 participants): RR 8.50, 95% CI 0.50 to 143.32) (Table 3). Rubin 1990 reported 6 dialysate leaks in the midline compared with 3 leaks in the lateral insertion group and 1 haematoma at the exit‐site in each group.
3.1. Analysis.
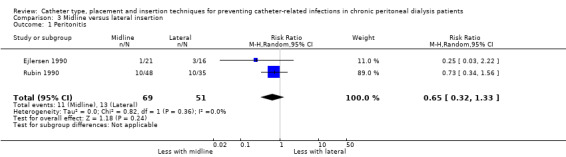
Comparison 3 Midline versus lateral insertion, Outcome 1 Peritonitis.
3.2. Analysis.
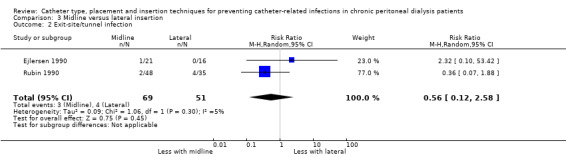
Comparison 3 Midline versus lateral insertion, Outcome 2 Exit‐site/tunnel infection.
3.3. Analysis.
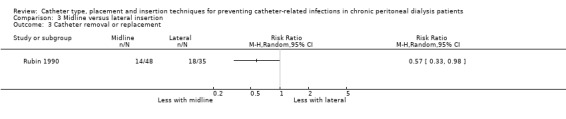
Comparison 3 Midline versus lateral insertion, Outcome 3 Catheter removal or replacement.
3.4. Analysis.
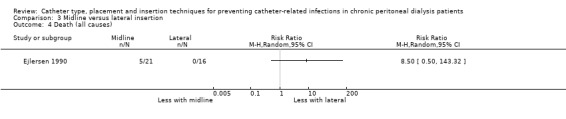
Comparison 3 Midline versus lateral insertion, Outcome 4 Death (all causes).
Percutaneous insertion versus open surgery
Percutaneous insertion compared with open surgical insertion of a PD catheter probably makes little or no difference to exit‐site/tunnel infection (Analysis 4.1 (2 studies, 96 participants): RR 0.16, 95% CI 0.02 to 1.30, P = 0.08; I2 = 0%; moderate certainty evidence). Atapour 2011 reported no episodes of early peritonitis in either group and similar risks of catheter removal or replacement between the two groups (Analysis 4.2 (1 study, 61 participants): RR 0.24, 95% CI 0.03 to 2.04) (Table 4). Percutaneous insertion makes little or no difference to post‐operative bleeding (haematoma or haemoperitoneum) compared to open surgery (Analysis 4.3 (2 studies, 96 participants) RR 0.22, 95% CI 0.04 to 1.26, I2= 0%; low certainty evidence). Atapour 2011) reported 1 outflow failure with percutaneous insertion compared with 4 with open surgery. Two studies (Atapour 2011; Merrikhi 2014) reported no viscus perforation or dialysate leak in either group.
4.1. Analysis.
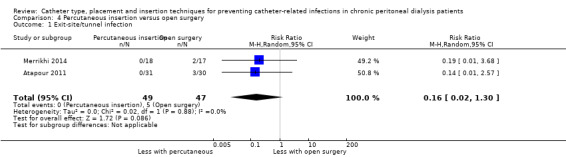
Comparison 4 Percutaneous insertion versus open surgery, Outcome 1 Exit‐site/tunnel infection.
4.2. Analysis.
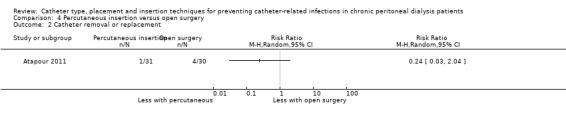
Comparison 4 Percutaneous insertion versus open surgery, Outcome 2 Catheter removal or replacement.
4.3. Analysis.
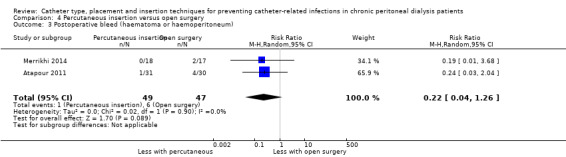
Comparison 4 Percutaneous insertion versus open surgery, Outcome 3 Postoperative bleed (haematoma or haemoperitoneum).
Straight versus coiled PD catheter
A straight catheter probably makes little or no difference to the risk of peritonitis (Analysis 5.1 (9 studies, 818 participants): RR 1.04, 95% CI 0.82 to 1.31, P = 0.74; I2 = 0%; moderate certainty evidence; 9 more per 1000), peritonitis rate (Analysis 5.2 (5 studies, 5882 patient‐months): RR 0.91, 95% CI 0.68 to 1.21, P = 0.51, I2 = 0% moderate certainty evidence), the risk of exit‐site/tunnel infection (Analysis 5.3 (10 studies, 826 participants): RR 1.12, 95% CI 0.94 to 1.34, P = 0.22; I2 = 0%; moderate certainty evidence; 34 more per 1000), and exit‐site/tunnel infection rate (Analysis 5.4 (4 studies, 5286 patient‐months): RR 1.05, 95% CI 0.77 to 1.43, P = 0.78; I2 = 0%; moderate certainty evidence) compared with a coiled catheter. It is uncertain whether straight catheters prevent catheter removal or replacement (Analysis 5.5 (9 studies, 713 participants): RR 1.11, 95% CI 0.73 to 1.66, P = 0.63; I2 = 50%; very low certainty evidence), however, a straight catheter probably makes little or no difference to technique failure (Analysis 5.6 (4 studies, 442 participants): RR 0.82, 95% CI 0.51 to 1.31, P = 0.4; I2 = 0%; moderate certainty evidence) and death (all causes) (Analysis 5.7 (8 studies, 703 participants): RR 0.95, 95% CI 0.62 to 1.46, P = 0.82; I2 = 3%; low certainty evidence) compared with coiled catheters, (Table 5). In a sensitivity analysis in which only studies with a low risk of attrition bias were included, similar results were observed for peritonitis (Analysis 5.8: RR 0.93, 95% CI 0.69 to 1.26), peritonitis rate (Analysis 5.9: RR 0.91, 95% CI 0.61 to 1.35), exit‐site infection (Analysis 5.10: RR 1.14, 95% CI 0.94 to 1.39), and exit‐site infection rate (Analysis 5.11; RR 1.18, 95% CI 0.76 to 1.82).
5.1. Analysis.
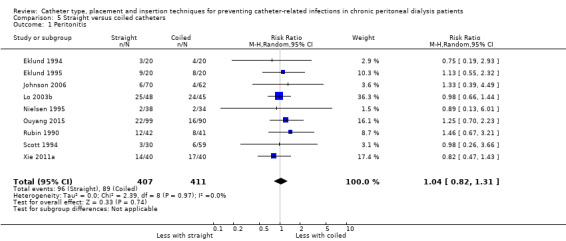
Comparison 5 Straight versus coiled catheters, Outcome 1 Peritonitis.
5.2. Analysis.
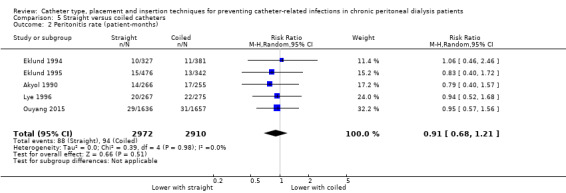
Comparison 5 Straight versus coiled catheters, Outcome 2 Peritonitis rate (patient‐months).
5.3. Analysis.
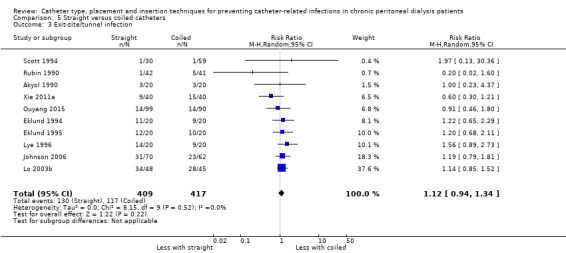
Comparison 5 Straight versus coiled catheters, Outcome 3 Exit‐site/tunnel infection.
5.4. Analysis.
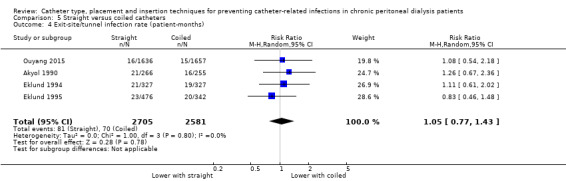
Comparison 5 Straight versus coiled catheters, Outcome 4 Exit‐site/tunnel infection rate (patient‐months).
5.5. Analysis.
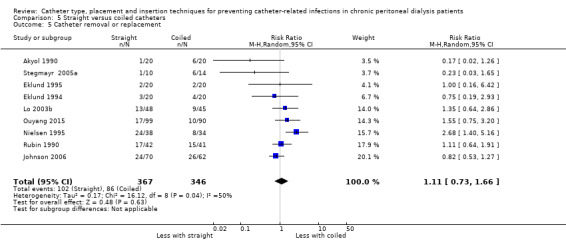
Comparison 5 Straight versus coiled catheters, Outcome 5 Catheter removal or replacement.
5.6. Analysis.
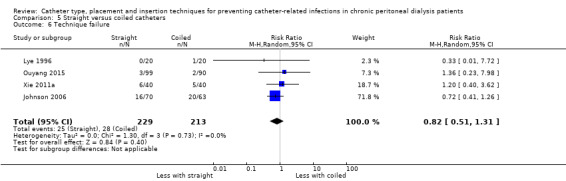
Comparison 5 Straight versus coiled catheters, Outcome 6 Technique failure.
5.7. Analysis.
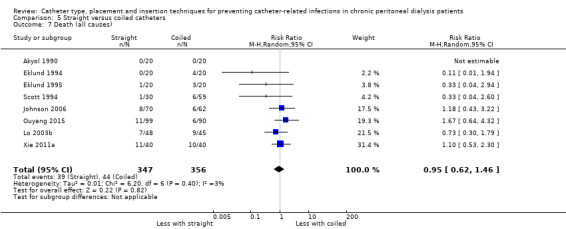
Comparison 5 Straight versus coiled catheters, Outcome 7 Death (all causes).
5.8. Analysis.
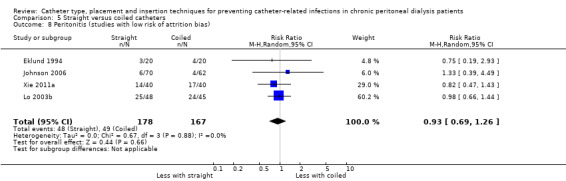
Comparison 5 Straight versus coiled catheters, Outcome 8 Peritonitis (studies with low risk of attrition bias).
5.9. Analysis.
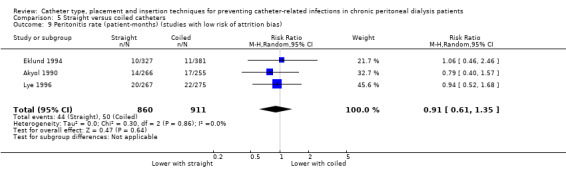
Comparison 5 Straight versus coiled catheters, Outcome 9 Peritonitis rate (patient‐months) (studies with low risk of attrition bias).
5.10. Analysis.
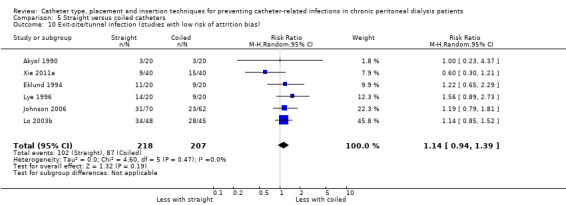
Comparison 5 Straight versus coiled catheters, Outcome 10 Exit‐site/tunnel infection (studies with low risk of attrition bias).
5.11. Analysis.
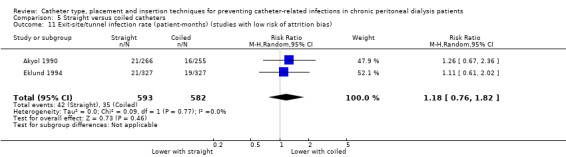
Comparison 5 Straight versus coiled catheters, Outcome 11 Exit‐site/tunnel infection rate (patient‐months) (studies with low risk of attrition bias).
There was moderate heterogeneity (50%) in the analysis of catheter removal/replacement between the two groups. This heterogeneity largely disappeared in a subgroup analysis that only included studies with follow‐up durations of ≥ 2 years, but increased to 74% when studies with follow‐up durations of < 2 years were included in the analysis. The substantial heterogeneity among studies with short follow‐up durations might have been due to different catheter types (double cuff versus single cuff and Tenckhoff versus swan‐neck catheter) and different follow‐up durations (ranged from 12 to 19 months) among the studies. Another possible explanation for the heterogeneity may relate to risk of attrition bias. In sensitivity analysis including only studies with a low risk of attrition bias, the observed heterogeneity was reduced (Analysis 5.12: RR 0.78, 95% CI 0.45 to 1.33; I2 = 32%).
5.12. Analysis.
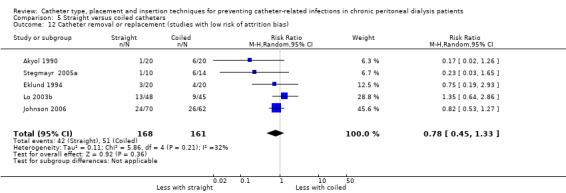
Comparison 5 Straight versus coiled catheters, Outcome 12 Catheter removal or replacement (studies with low risk of attrition bias).
Straight catheter makes little or no difference to dialysate leak compared with coiled catheter (Analysis 5.13 (7 studies, 550 participants): RR 0.74, 95% CI 0.16 to 3.49, P = 0.70; I2 = 37%; low certainty evidence). It is uncertain whether straight catheter lead to post‐operative bleeding (haematoma or haemoperitoneum) compared with coiled catheter (Analysis 5.14 (4 studies, 358 participants): RR 1.14, 95% CI 0.24 to 5.34, P = 0.87; I2 = 0%; very low certainty evidence). Nielsen 1995 reported one case of bladder perforation with coiled catheter but none in the straight catheter group.
5.13. Analysis.
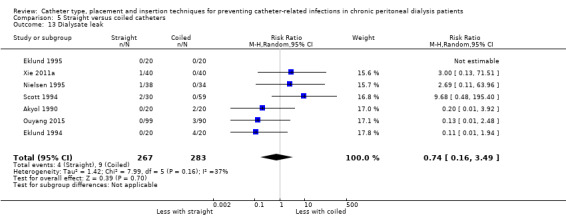
Comparison 5 Straight versus coiled catheters, Outcome 13 Dialysate leak.
5.14. Analysis.
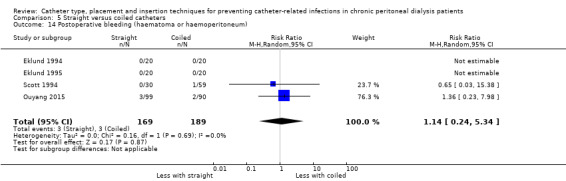
Comparison 5 Straight versus coiled catheters, Outcome 14 Postoperative bleeding (haematoma or haemoperitoneum).
Tenckhoff catheter with artificial curve at subcutaneous tunnel tract versus swan‐neck catheter
Catheter with artificial curve at subcutaneous tract compared with swan‐neck catheter may make little or no difference to peritonitis risk (Analysis 6.1 (2 studies, 140 participants): RR 1.29, 95% CI 0.85 to 1.96, P = 0.24; I2 = 0%; low certainty evidence), peritonitis rate (Analysis 6.2 (2 studies, 2535 patient‐months): RR 1.22, 95% CI 0.54 to 2.75, P = 0.63; I2 = 47%; low certainty evidence), exit‐site/tunnel infection (Analysis 6.3 (2 studies, 140 participants): RR 0.96, 95% CI 0.77 to 1.21, P = 0.75; I2 = 0%; moderate certainty evidence), but may improve exit‐site infection rate (Analysis 6.4 (2 studies, 2535 patient‐months): RR 0.67, 95% CI 0.50 to 0.90, P = 0.007; I2 = 0%; low certainty evidence), and probably makes little or no difference to catheter removal or replacement (Analysis 6.5 (2 studies, 140 participants): RR 0.85, 95% CI 0.42 to 1.72, P = 0.65; I2 = 15%; moderate certainty evidence), technique failure (Analysis 6.6 (2 studies, 140 participants): RR 0.64, 95% CI 0.26 to 1.58, P = 0.3;, I2 = 0%; moderate certainty evidence), and death, all causes (Analysis 6.7 (2 studies, 140 participants): (RR 0.74, 95% CI 0.27 to 2.03, P = 0.57; I2 = 0%; moderate certainty evidence) compared with insertion of PD catheters with an artificial curve at the tunnel tract (Table 6). Yip 2010 reported no dialysate leaks in either group but there was one superficial cuff extrusion in the swan‐neck catheter group but none in the other group. Li 2009e reported post‐operative bleeding from the main wound (5 versus 9) and exit‐site (9 versus 13) in Tenckhoff catheter and swan‐neck catheter respectively.
6.1. Analysis.
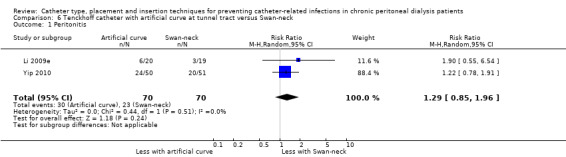
Comparison 6 Tenckhoff catheter with artificial curve at tunnel tract versus Swan‐neck, Outcome 1 Peritonitis.
6.2. Analysis.
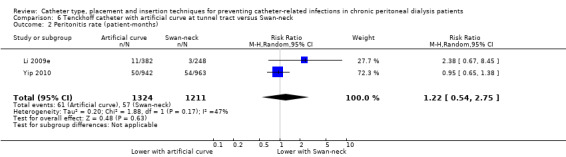
Comparison 6 Tenckhoff catheter with artificial curve at tunnel tract versus Swan‐neck, Outcome 2 Peritonitis rate (patient‐months).
6.3. Analysis.
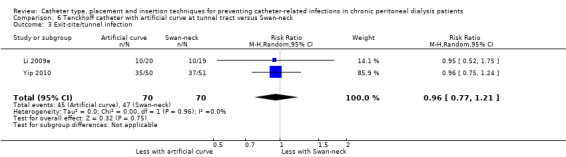
Comparison 6 Tenckhoff catheter with artificial curve at tunnel tract versus Swan‐neck, Outcome 3 Exit‐site/tunnel infection.
6.4. Analysis.
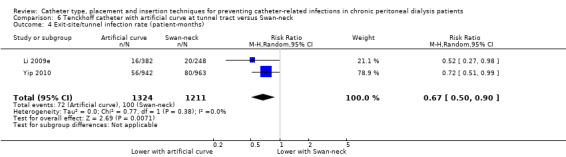
Comparison 6 Tenckhoff catheter with artificial curve at tunnel tract versus Swan‐neck, Outcome 4 Exit‐site/tunnel infection rate (patient‐months).
6.5. Analysis.
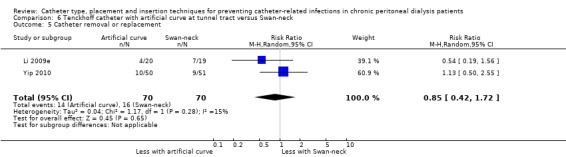
Comparison 6 Tenckhoff catheter with artificial curve at tunnel tract versus Swan‐neck, Outcome 5 Catheter removal or replacement.
6.6. Analysis.
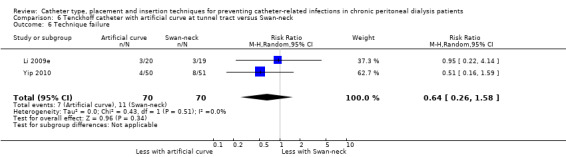
Comparison 6 Tenckhoff catheter with artificial curve at tunnel tract versus Swan‐neck, Outcome 6 Technique failure.
6.7. Analysis.
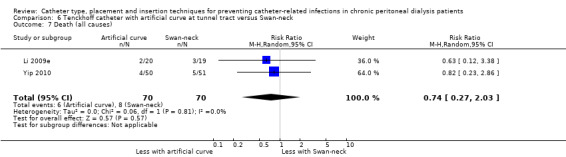
Comparison 6 Tenckhoff catheter with artificial curve at tunnel tract versus Swan‐neck, Outcome 7 Death (all causes).
Self‐locating catheter versus straight catheter
It is uncertain whether self‐locating catheter reduces catheter removal or replacement (Analysis 7.3 (2 studies, 139 participants): RR 0.32, 95% CI 0.03 to 3.06, P = 0.32; I2 = 64%; very low certainty of evidence). Self‐locating catheter probably slightly reduces technique failure (Analysis 7.4 (2 studies, 139 participants): RR 0.64, 95% CI 0.39 to 1.04, P = 0.07; I2 = 0%; moderate certainty evidence), but may make little or no difference to death (all causes) (Analysis 7.5 (2 studies, 139 participants): RR 1.02, 95% CI 0.11 to 9.75, P = 0.99; I2 = 49%; low certainty evidence) compared to a straight catheter. Sanchez‐Canel 2016 reported no difference in the incidence of peritonitis (Analysis 7.1 (78 participants): RR 1.13, 95% CI 0.86 to 1.49) and exit‐site infection (Analysis 7.2 (78 participants): RR 0.95, 95% CI 0.37 to 2.45) (Table 7). Moderate heterogeneity was observed with analysis for catheter removal/replacement and death (all causes), for which subgroup analysis was unable to be performed given the small number of studies. The potential explanation for heterogeneity might have related to the suboptimal quality of included studies, which did not report the method of randomisation, blinding and follow up duration. In addition, one study reported different baseline BMI values between the treatment and control groups and the other study interrupted recruitment early due to an observed significant reduction in the incidence of catheter removal/replacement in the treatment group. Self‐locating catheter makes little or no difference to dialysate leak compared with straight catheter (Analysis 7.6 (2 studies, 139 participants): RR 1.04, 95% CI 0.46 to 2.35, P = 0.93; I2 = 0%; low certainty evidence). Sanchez‐Canel 2016 reported post‐operative peritoneal bleed (7 versus 6) in self‐locating and straight catheter groups respectively.
7.3. Analysis.
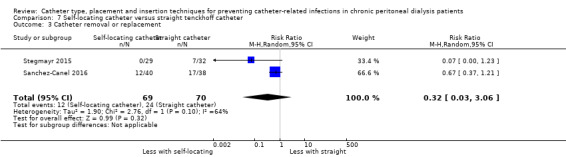
Comparison 7 Self‐locating catheter versus straight tenckhoff catheter, Outcome 3 Catheter removal or replacement.
7.4. Analysis.
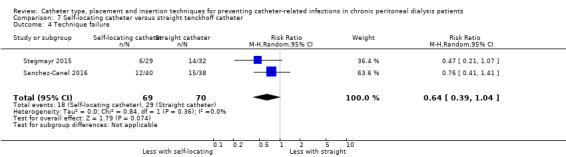
Comparison 7 Self‐locating catheter versus straight tenckhoff catheter, Outcome 4 Technique failure.
7.5. Analysis.
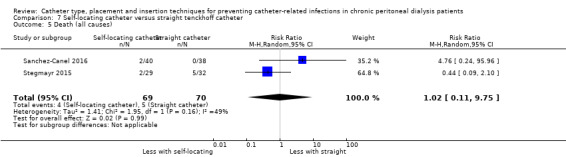
Comparison 7 Self‐locating catheter versus straight tenckhoff catheter, Outcome 5 Death (all causes).
7.1. Analysis.
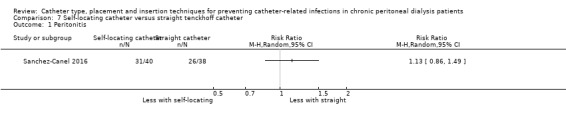
Comparison 7 Self‐locating catheter versus straight tenckhoff catheter, Outcome 1 Peritonitis.
7.2. Analysis.
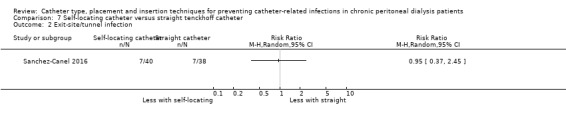
Comparison 7 Self‐locating catheter versus straight tenckhoff catheter, Outcome 2 Exit‐site/tunnel infection.
7.6. Analysis.
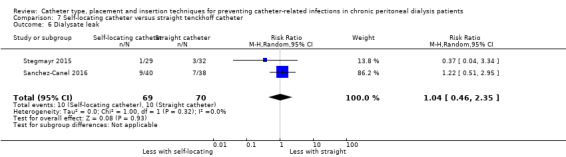
Comparison 7 Self‐locating catheter versus straight tenckhoff catheter, Outcome 6 Dialysate leak.
Other interventions
The risk of peritonitis and/or peritonitis rate were examined using:
Different insertion techniques: open surgery versus open surgery with omentum folding (Analysis 8.1), open surgery versus modified surgery with or without catheter fixation (Analysis 9.1), open surgery versus vertical tunnel‐based low‐site implantation (Analysis 10.1), open surgery versus ureteroscopic‐assisted surgery (Analysis 11.1), radiological versus surgical implantation (Analysis 12.1), cystoscopy‐assisted surgery versus open surgery (Analysis 13.1), laparoscopic Moncrief‐Popovich technique versus blind trocar technique (Analysis 14.1)
Different catheter types: single–cuff versus double‐cuff catheter (Analysis 15.1), double‐cuff versus triple‐cuff catheter (Analysis 16.1), swan‐neck versus straight curled catheter (Analysis 17.1), antibiotic‐treated catheters versus standard catheter (Analysis 18.1)
Immobilizer device versus no immobilizer device (Analysis 19.1)
Silver ring at exit‐site versus no silver ring (Analysis 20.1)
8.1. Analysis.
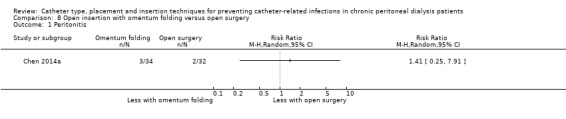
Comparison 8 Open insertion with omentum folding versus open surgery, Outcome 1 Peritonitis.
9.1. Analysis.
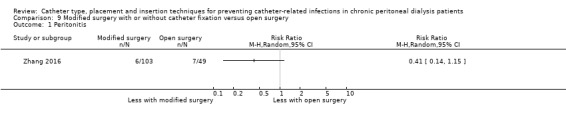
Comparison 9 Modified surgery with or without catheter fixation versus open surgery, Outcome 1 Peritonitis.
10.1. Analysis.
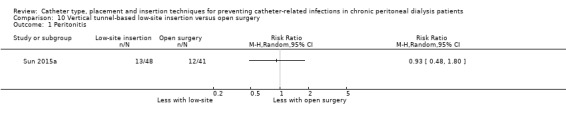
Comparison 10 Vertical tunnel‐based low‐site insertion versus open surgery, Outcome 1 Peritonitis.
11.1. Analysis.
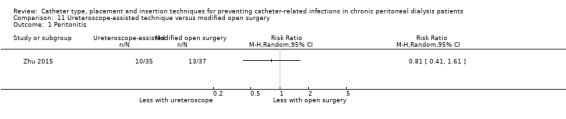
Comparison 11 Ureteroscope‐assisted technique versus modified open surgery, Outcome 1 Peritonitis.
12.1. Analysis.
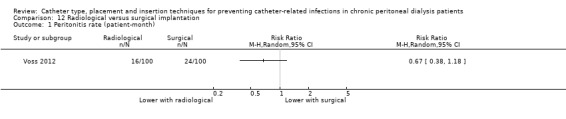
Comparison 12 Radiological versus surgical implantation, Outcome 1 Peritonitis rate (patient‐month).
13.1. Analysis.
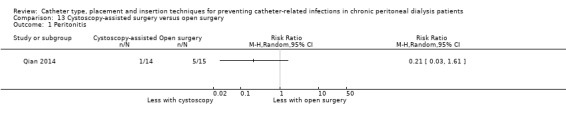
Comparison 13 Cystoscopy‐assisted surgery versus open surgery, Outcome 1 Peritonitis.
14.1. Analysis.
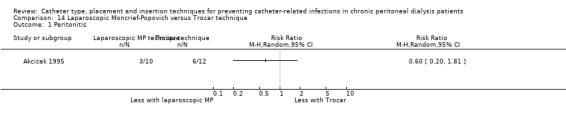
Comparison 14 Laparoscopic Moncrief‐Popovich versus Trocar technique, Outcome 1 Peritonitis.
15.1. Analysis.
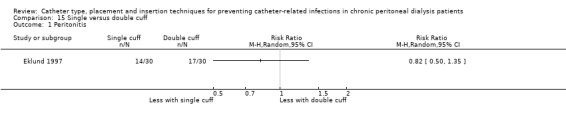
Comparison 15 Single versus double cuff, Outcome 1 Peritonitis.
16.1. Analysis.
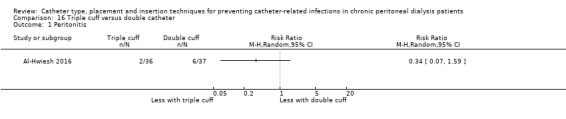
Comparison 16 Triple cuff versus double catheter, Outcome 1 Peritonitis.
17.1. Analysis.
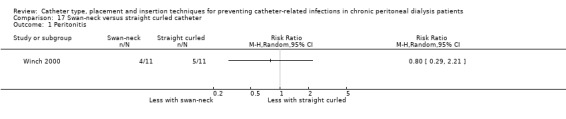
Comparison 17 Swan‐neck versus straight curled catheter, Outcome 1 Peritonitis.
18.1. Analysis.
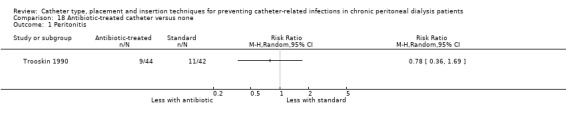
Comparison 18 Antibiotic‐treated catheter versus none, Outcome 1 Peritonitis.
19.1. Analysis.
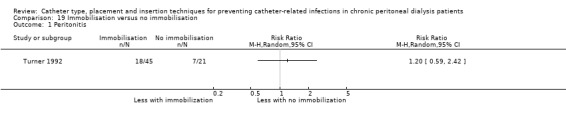
Comparison 19 Immobilisation versus no immobilisation, Outcome 1 Peritonitis.
20.1. Analysis.
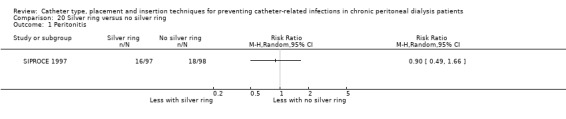
Comparison 20 Silver ring versus no silver ring, Outcome 1 Peritonitis.
See (Table 9).
2. Methods of insertion, catheter types and other interventions on the incidence of peritonitis and peritonitis rate.
| Name of studies | Relative risk | 95% CI | P value |
| Peritonitis | |||
| Methods of catheter implantation | |||
| Chen 2014a | 1.41 | 0.25 to 7.91 | 0.69 |
| Turner 1992 | 1.20 | 0.59 to 2.42 | 0.61 |
| Sun 2015a | 0.93 | 0.48 to 1.80 | 0.82 |
| Zhang 2016 | 0.39 | 0.11 to 1.42 | 0.15 |
| Zhu 2015 | 0.81 | 0.41 to 1.61 | 0.55 |
| Qian 2014 | 0.21 | 0.03 to 1.61 | 0.13 |
| Akcicek 1995 | 0.60 | 0.20 to 1.81 | 0.36 |
| Types of catheter | |||
| Eklund 1997 | 0.82 | 0.50 to 1.35 | 0.44 |
| Al‐Hwiesh 2016 | 0.34 | 0.07 to 1.59 | 0.17 |
| Winch 2000 | 0.80 | 0.29 to 2.21 | 0.67 |
| Trooskin 1990 | 0.78 | 0.6 to 1.69 | 0.53 |
| Other intervention | |||
| SIPROCE 1997 | 0.90 | 0.49 to 1.66 | 0.73 |
| Turner 1992 | 1.20 | 0.59 to 2.42 | 0.61 |
| Peritonitis rate (patient‐month) | |||
| Methods of catheter implantation | |||
| Chen 2014a | 1.40 | 0.23 to 8.34 | 0.71 |
| Voss 2012 | 0.67 | 0.38 to 1.18 | 0.16 |
| Types of catheters | |||
| Al‐Hwiesh 2016 | 0.34 | 0.07 to 1.69 | 0.19 |
| Winch 2000 | 0.69 | 0.19 to 2.53 | 0.57 |
CI: confidence interval
Dasgupta 1998 reported 14 episodes of peritonitis in 19 patients using Moncrief‐Popovich catheter compared with 22 episodes of peritonitis in 20 patients using Tenckhoff catheter. The other outcomes were not different among these studies except that Zhang 2016 reported that catheter removal/replacement was lower with modified surgery with or without catheter fixation compared with open surgery (Analysis 9.3 (152 participants): RR 0.16, 95% CI 0.03 to 0.76).
9.3. Analysis.
Comparison 9 Modified surgery with or without catheter fixation versus open surgery, Outcome 3 Catheter removal or replacement.
Break‐in periods
Timely PD 2010 (122 participants) examined the effect of different break‐in periods (1 week versus 2 weeks versus 4 weeks post catheter insertion) on the composite PD‐related infection (defined as exit‐site/tunnel infection and/or peritonitis) at 4 weeks after PD initiation and 8 weeks after catheter insertion reported that there was no difference across 3 groups. The study reported higher risk of dialysate leak in break‐in period of 1 week compared with 4 weeks (11 versus 1 respectively). There was one post‐operative wound haematoma observed in the break‐in period of 2 weeks but none in the other groups.
Discussion
Summary of main results
The review demonstrated that no specific PD catheter implantation technique or catheter type significantly reduced the risk of PD peritonitis. In a single study with a small number of participants, midline catheter insertion resulted in a lower risk of catheter removal/replacement compared with lateral insertion and in another small, single‐centre study, modified open surgery with or without catheter fixation resulted in a lower risk of catheter removal/replacement compared with open surgery. Similarly, in two other small, methodologically suboptimal studies involving 140 participants, a swan‐neck catheter was associated with a higher exit‐site/tunnel infection rate than a Tenckhoff catheter with an artificial curve at the subcutaneous tract.
Overall completeness and applicability of evidence
Since the last review in 2004, there have been limited RCTs examining the different new surgical techniques or PD catheter types in the last decade but none has been shown superior to any other in the reduction of peritonitis. However, it should also be acknowledged that there have been general improvements in peritonitis rates globally since the time of the last systematic review (Li 2017; Mehrotra 2016). The general trend in improvement of peritonitis rates might potentially make it difficult for any interventions in this area to achieve further major improvement.
Comparison between the different techniques of PD catheter implantation demonstrated that no specific technique was superior to any other in the prevention of peritonitis and/or exit‐site/tunnel infection. Generally, most of the studies were from single‐centres and involved small study populations followed for variable periods of time. There was no standardized method of reporting the infection‐related outcomes (peritonitis and exit‐site/tunnel infection); one study reported early and total infection (Gadallah 1999), two studies reported both early and late infection separately (Jwo 2010; Wright 1999), and the remainder of the studies reported total infection. The definitions of early infection (ranged from ≤ 2 weeks to ≤ 6 weeks) and late infection (ranged from > 2 weeks to > 6 weeks) also varied among studies. Gadallah 1999 postulated that the higher rate of early peritonitis (within 2 weeks of catheter placement) was likely contributed to by a higher exit‐site leak incidence related to the technique of catheter insertion. In the present review, the majority of included studies reported overall infection (peritonitis or exit‐site/tunnel infection) rather than separately reporting early and late infections. The potential benefit of catheter insertion technique on prevention of catheter‐related infection, especially in the early period of catheter insertion, was not able to be comprehensively assessed in this review.
Moreover, a majority of these studies only reported either the incidence of peritonitis or the peritonitis rate but not both. In addition, some studies did not report details about the use of prophylactic antibiotics prior to catheter implantation, which is a key intervention that has been shown to convincingly reduce the risk of early peritonitis in PD patients in the previous meta‐analysis (Strippoli 2004a).
Five studies examined the effects of laparoscopy versus laparotomy and demonstrated that the risks of peritonitis and exit‐site/tunnel infection were not significantly different between the two methods.
Moncrief 1998 reported that catheter implantation with subcutaneous burying for three to five weeks was associated with reduced incidence of peritonitis. However, in the present review, subcutaneous burying of a PD catheter for six weeks prior to PD initiation exerted comparable effects on peritonitis, exit‐site/tunnel infection and death (all causes) compared to the standard insertion technique. In view of the suboptimal methodologic quality and small numbers of studies and participants, there were insufficient data to draw conclusions regarding the value of this technique.
Spence 1985 reported that paramedian insertion was associated with reduction in the incidence of leak and extrusion of the cuff compared with midline insertion of the PD catheter. In the present review, midline versus lateral insertion of PD catheters did not significantly affect the risks of peritonitis, exit‐site/tunnel infection and death (all causes). However, in a single small study, midline insertion resulted in a lower risk of catheter removal/replacement than lateral insertion. In that particular study, there was a potential bias as the study introduced two different interventions (spiral versus straight catheters, and midline versus lateral insertion techniques) at the same time. In another RCT examining midline versus lateral catheter insertion (Ejlersen 1990), one‐year catheter survival rates were comparable between the two groups (midline 59% versus lateral 51%). In view of the suboptimal methodologic quality and small number of studies available, there are insufficient data to draw definitive conclusions regarding the effects of midline versus lateral insertion on the outcomes examined in this review.
In a single small study centre, Zhang 2016 reported that a modified catheter placement method, which was characterised by a low implant site, a short intra‐abdominal catheter segment and upward straight subcutaneous tunnel, significantly decreased the incidence of catheter removal/replacement compared with open surgery. The authors postulated that a long intra‐abdominal catheter segment following a traditional open surgical method might lead to an increased risk of catheter tip migration and omental wrap. However, in that study, there was a trend towards a high incidence of participants with prior abdominal surgery in the open surgery group (20.4%) versus modified open surgery group with or without catheter fixation (11.7%). In view of the single centre design, small study population and suboptimal methodologic quality, no firm conclusion can be drawn regarding the effect of open surgery versus modified open surgery with or without catheter fixation on the incidence of catheter removal/replacement.
The most commonly examined type of catheter was straight versus coiled catheters, which demonstrated no significant differences in peritonitis, exit‐site/tunnel infection, and catheter removal/replacement or death (all causes). There was moderate heterogeneity in the analysis of catheter removal/replacement between the two groups. The heterogeneity was resolved when only studies with follow‐up durations of ≥ 2 years were included in the analysis, but increased when studies with follow‐up durations of < 2 years were additionally included. The substantial heterogeneity among studies with short follow‐up durations might due to different catheter types (double cuff versus single cuff and Tenckhoff versus swan‐neck catheter) and different follow‐up durations (ranged from 12 to 19 months) among the studies.
Two small studies comparing swan‐neck catheters and PD catheters with artificial curves at the subcutaneous tract showed no significant differences in peritonitis risk, peritonitis rate, exit‐site/tunnel infection risk, catheter removal/replacement, technique failure and death (all causes). Though the analysis of the risk of exit‐site/tunnel infection found no significant difference between the two groups, the rate of exit‐site/tunnel infection was significantly higher in the swan‐neck catheter group. This finding might be explained by an increased number of participants with repeated/recurrent exit‐site/tunnel infection in the swan‐neck group. Alternatively, the result might have been a chance finding or related to bias stemming from suboptimal methodologic quality. Reassuringly, there was no difference in the risk of either catheter removal or technique failure.
Quality of the evidence
The methodological quality of evidence for most of the studies was considered suboptimal. The methods of randomisation and allocation concealment were not clearly described in most of the studies. The majority of included studies were single‐centre with small sample sizes and had widely variable follow‐up periods. A small number of studies (33%) analysed their data using the intention‐to‐treat method. In addition, most studies were not registered with the clinical trial databases, had not published a protocol of their study, and did not report on many patient‐level outcomes which could have contributed to the risk of selective reporting bias. Timely PD 2010 only reported a composite outcome of exit‐site infection and peritonitis such that analysis of the individual outcomes was unable to perform. Moreover, the types of interventions examined were numerous with very few studies (either one or two studies) in each category, such that definitive conclusions could not be drawn. Finally, the risk of peritonitis may have been modified by other unreported co‐interventions, including the centre protocol for prophylactic antibiotics prior to catheter implantation, PD training protocol and exit‐site care, other centre‐specific factors, and the skill and experience of interventionists, which were unable to be adjusted for in the review.
Potential biases in the review process
The present review was conducted as per published standardized Cochrane methodology. The review included the up‐to‐date publications through MEDLINE, EMBASE, and CENTRAL searches with the assistance of the Information Specialist. The review included RCTs and quasi‐RCTs. All potential publications were assessed by two independent authors who performed the data extraction, data analysis and assessment of quality of studies independently. Any dispute or concern about the data between the two authors was resolved with additional two authors. The primary authors were contacted to seek the additional data for analysis by the authors. A few abstracts/publications, which were published a decade ago, were not able to be included in the current review as we were unable to contact primary authors for further information. Finally, there is a potential for bias as one of the investigators of the present review (DWJ) was also an author of an included study (Johnson 2006).
Agreements and disagreements with other studies or reviews
Similar to the previously published review (Strippoli 2004), the present study has demonstrated that no specific type of catheter or implantation method was superior in reducing the risk of PD peritonitis. The previous meta‐analysis by Xie 2011a reported no significant difference in peritonitis (7 studies: RR 1.12, 95% CI 0.83 to 1.50) or exit‐site/tunnel infection (6 studies: RR 1.05, 95% CI 0.79 to 1.39) between straight versus coiled catheters. The results of the present updated review support the findings of the previous reviews.
A meta‐analysis by Hagen 2014 that included both RCTs and cohort studies comparing laparoscopic insertion and laparotomy also reported no significant differences in peritonitis (9 studies: OR 0.83, 95% CI 0.48 to 1.42) and exit‐site/tunnel infection (7 studies: OR 0.80, 95% CI 0.47 to 1.37) between the two groups. The present review only included RCTs of laparoscopy versus laparotomy and reported similar findings.
The review also demonstrated that catheter removal or replacement and technique failure were not significantly different among the different methods of implantation, including laparoscopically and surgically placed catheters. The finding was contrary to that of a previous meta‐analysis (Hagen 2014), which included both RCTs and cohort studies, and reported that one‐year catheter survival was significantly higher in the laparoscopy group compared with the laparotomy group. The finding from the previous meta‐analysis may have been biased due to the fact that the majority of included studies were non‐RCTs (8 cohort studies compared with 3 RCTs). To date, there have only been 4 RCTs comparing laparoscopic versus laparotomy methods: all 4 studies were single‐centre design, only 1 study was analysed by intention‐to‐treat method, all studies practised different antibiotic prophylaxis regimens with varying doses (2 g vancomycin versus 0.5 to 1 g cefazolin) prior to the procedure, and all initiated PD at different time points following the operative procedure (ranging from immediately after procedure to several days post‐procedure). The current available data suggested that laparoscopic insertion makes little or no difference to PD‐related infection, catheter removal/replacement, technique or patient survival compared to laparotomy.
In the current review, different catheter types, including straight versus coiled/curved (either at the tip or at the subcutaneous tract) catheters, were not significantly associated with catheter removal/replacement and technique failure in PD patients. There was moderate heterogeneity in the analysis of catheter removal/replacement in the review, which was potentially due to the fact that different studies used different types of catheter including different products from different manufacturing companies, single or double cuff catheters, and different methods of catheter placement (percutaneous versus open surgical methods). Heterogeneity was decreased but not totally resolved following subgroup analysis with straight tip versus coiled/curved tip catheters and straight versus curved catheter at the subcutaneous tract, open surgical method versus percutaneously inserted method, and single cuff versus double cuff catheters. Similarly, the previous meta‐analysis by Xie 2011a, which compared straight tip versus coiled tip catheters, reported that although there was a significantly increased risk of catheter tip migration with coiled catheters, overall catheter failure was not significantly different between the two groups.
The present review demonstrated there was no significant difference in death (all causes) between straight and coiled catheters. In contrast, our previous review (Strippoli 2004) reported that there was a survival advantage with straight catheters compared with curved catheters. The discrepancy in findings between the two reviews can be explained by the fact that the present review included a larger number of studies (8 RCTs versus 4 RCTs) and more well‐designed studies compared to the previous review.
Authors' conclusions
Implications for practice.
No specific catheter implantation method is superior to others in the prevention of PD‐related peritonitis or exit‐site/tunnel infection in PD patients.
No specific type of PD catheter is superior to others in the prevention of PD‐related peritonitis or exit‐site/tunnel infection in PD patients.
No other additional catheter‐related intervention is proven to be beneficial in the prevention of PD‐related peritonitis or exit‐site/tunnel infection in PD patients.
In general, most of the available studies to date on this topic were small, single centre studies which primarily examined non‐infection‐related outcomes.
The findings of this review support the current ISPD Guideline recommendations (Li 2016; Szeto 2017).
Implications for research.
Future well designed studies addressing the effects of catheter‐specific interventions on the risk of PD‐related infection (peritonitis and/or exit‐site/tunnel infection) as the primary outcome are needed.
These studies should examine the effects of the catheter‐related intervention on:
early (day 30) and late (day 90) peritonitis rather than overall peritonitis;
early (day 30) and late (day 90) catheter removal rather than overall catheter removal;
early (day 30) technique failure, in addition to overall technique failure.
Outcomes should be reported using consistent outcome measures, for example, standardised definition of the outcome 'technique failure'.
Future studies should also examine patient‐reported outcomes in addition to the other clinical outcomes.
What's new
| Date | Event | Description |
|---|---|---|
| 17 May 2019 | New search has been performed | New studies added |
| 17 May 2019 | New citation required but conclusions have not changed | 25 new studies added, no major change to conclusions |
History
Protocol first published: Issue 1, 2004 Review first published: Issue 4, 2004
| Date | Event | Description |
|---|---|---|
| 14 January 2010 | Amended | Contact details updated. |
| 13 May 2009 | Amended | Contact details updated. |
| 22 September 2008 | Amended | Converted to new review format. |
Acknowledgements
We are indebted to Dr R. Russo and Dr R. Curciulo of the University of Bari, Italy, who commented on the original project and provided useful background information. Particular thanks to Dr Paolo Strippoli, Director of Nephrology, Ospedale "A. Perrino", Brindisi, Italy, for his intellectual input in the manuscript with comments on the original review. The authors gratefully acknowledge the contribution of Chu‐Jun Ouyang, Shyh‐Chuan Jwo, Abdullah Khalaf Al‐Hwiesh, Guochun Chen, Terence Yip who responded to our queries about their studies. The authors gratefully acknowledge Narelle Willis and Gail Higgins from Cochrane Kidney and Transplant for their contribution.
Appendices
Appendix 1. Electronic search strategies
| Database searched | Search terms |
| CENTRAL |
|
| MEDLINE (OVID) |
|
| EMBASE (OVID) |
|
Appendix 2. Risk of bias assessment tool
| Potential source of bias | Assessment criteria |
|
Random sequence generation Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence |
Low risk of bias: Random number table; computer random number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing of lots; minimisation (minimisation may be implemented without a random element, and this is considered to be equivalent to being random). |
| High risk of bias: Sequence generated by odd or even date of birth; date (or day) of admission; sequence generated by hospital or clinic record number; allocation by judgement of the clinician; by preference of the participant; based on the results of a laboratory test or a series of tests; by availability of the intervention. | |
| Unclear: Insufficient information about the sequence generation process to permit judgement. | |
|
Allocation concealment Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment |
Low risk of bias: Randomisation method described that would not allow investigator/participant to know or influence intervention group before eligible participant entered in the study (e.g. central allocation, including telephone, web‐based, and pharmacy‐controlled, randomisation; sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes). |
| High risk of bias: Using an open random allocation schedule (e.g. a list of random numbers); assignment envelopes were used without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure. | |
| Unclear: Randomisation stated but no information on method used is available. | |
|
Blinding of participants and personnel Performance bias due to knowledge of the allocated interventions by participants and personnel during the study |
Low risk of bias: No blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding; blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken. |
| High risk of bias: No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding; blinding of key study participants and personnel attempted, but likely that the blinding could have been broken, and the outcome is likely to be influenced by lack of blinding. | |
| Unclear: Insufficient information to permit judgement | |
|
Blinding of outcome assessment Detection bias due to knowledge of the allocated interventions by outcome assessors. |
Low risk of bias: No blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding; blinding of outcome assessment ensured, and unlikely that the blinding could have been broken. |
| High risk of bias: No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement is likely to be influenced by lack of blinding. | |
| Unclear: Insufficient information to permit judgement | |
|
Incomplete outcome data Attrition bias due to amount, nature or handling of incomplete outcome data. |
Low risk of bias: No missing outcome data; reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size; missing data have been imputed using appropriate methods. |
| High risk of bias: Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size; ‘as‐treated’ analysis done with substantial departure of the intervention received from that assigned at randomisation; potentially inappropriate application of simple imputation. | |
| Unclear: Insufficient information to permit judgement | |
|
Selective reporting Reporting bias due to selective outcome reporting |
Low risk of bias: The study protocol is available and all of the study’s pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way; the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon). |
| High risk of bias: Not all of the study’s pre‐specified primary outcomes have been reported; one or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. sub‐scales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis; the study report fails to include results for a key outcome that would be expected to have been reported for such a study. | |
| Unclear: Insufficient information to permit judgement | |
|
Other bias Bias due to problems not covered elsewhere in the table |
Low risk of bias: The study appears to be free of other sources of bias. |
| High risk of bias: Had a potential source of bias related to the specific study design used; stopped early due to some data‐dependent process (including a formal‐stopping rule); had extreme baseline imbalance; has been claimed to have been fraudulent; had some other problem. | |
| Unclear: Insufficient information to assess whether an important risk of bias exists; insufficient rationale or evidence that an identified problem will introduce bias. |
Data and analyses
Comparison 1. Laparoscopy versus laparotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 4 | 315 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.59, 1.35] |
| 2 Peritonitis rate (patient‐months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Exit‐site/tunnel infection | 3 | 270 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.43, 2.31] |
| 4 Catheter removal or replacement | 3 | 167 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.77, 1.86] |
| 5 Technique failure | 4 | 283 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.47, 1.08] |
| 6 Death (all causes) | 3 | 270 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.72, 2.20] |
| 7 Dialysate leak | 3 | 167 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.10, 6.97] |
Comparison 2. Buried (subcutaneous) versus non‐buried catheter.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis rate (patient‐months) | 2 | 2511 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.37, 3.60] |
| 2 Exit‐site/tunnel infection rate (patient‐months) | 2 | 2511 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.39, 3.42] |
| 3 Technique failure | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Death (all causes) | 2 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.39, 2.08] |
Comparison 3. Midline versus lateral insertion.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 2 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.32, 1.33] |
| 2 Exit‐site/tunnel infection | 2 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.12, 2.58] |
| 3 Catheter removal or replacement | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Death (all causes) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 4. Percutaneous insertion versus open surgery.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Exit‐site/tunnel infection | 2 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.16 [0.02, 1.30] |
| 2 Catheter removal or replacement | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Postoperative bleed (haematoma or haemoperitoneum) | 2 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.04, 1.26] |
Comparison 5. Straight versus coiled catheters.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 9 | 818 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.82, 1.31] |
| 2 Peritonitis rate (patient‐months) | 5 | 5882 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.68, 1.21] |
| 3 Exit‐site/tunnel infection | 10 | 826 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.94, 1.34] |
| 4 Exit‐site/tunnel infection rate (patient‐months) | 4 | 5286 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.77, 1.43] |
| 5 Catheter removal or replacement | 9 | 713 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.73, 1.66] |
| 6 Technique failure | 4 | 442 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.51, 1.31] |
| 7 Death (all causes) | 8 | 703 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.62, 1.46] |
| 8 Peritonitis (studies with low risk of attrition bias) | 4 | 345 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.69, 1.26] |
| 9 Peritonitis rate (patient‐months) (studies with low risk of attrition bias) | 3 | 1771 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.61, 1.35] |
| 10 Exit‐site/tunnel infection (studies with low risk of attrition bias) | 6 | 425 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.94, 1.39] |
| 11 Exit‐site/tunnel infection rate (patient‐months) (studies with low risk of attrition bias) | 2 | 1175 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.76, 1.82] |
| 12 Catheter removal or replacement (studies with low risk of attrition bias) | 5 | 329 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.45, 1.33] |
| 13 Dialysate leak | 7 | 550 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.16, 3.49] |
| 14 Postoperative bleeding (haematoma or haemoperitoneum) | 4 | 358 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.24, 5.34] |
Comparison 6. Tenckhoff catheter with artificial curve at tunnel tract versus Swan‐neck.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.85, 1.96] |
| 2 Peritonitis rate (patient‐months) | 2 | 2535 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.54, 2.75] |
| 3 Exit‐site/tunnel infection | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.77, 1.21] |
| 4 Exit‐site/tunnel infection rate (patient‐months) | 2 | 2535 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.50, 0.90] |
| 5 Catheter removal or replacement | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.42, 1.72] |
| 6 Technique failure | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.26, 1.58] |
| 7 Death (all causes) | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.27, 2.03] |
Comparison 7. Self‐locating catheter versus straight tenckhoff catheter.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Catheter removal or replacement | 2 | 139 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.03, 3.06] |
| 4 Technique failure | 2 | 139 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.39, 1.04] |
| 5 Death (all causes) | 2 | 139 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.11, 9.75] |
| 6 Dialysate leak | 2 | 139 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.46, 2.35] |
Comparison 8. Open insertion with omentum folding versus open surgery.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Peritonitis rate (patient‐months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Exit‐site/tunnel infection rate (patient‐month) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Catheter removal or replacement | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Technique failure | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Death (all causes) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8 Dialysate leak | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9 Postoperative bleed (haematoma or haemoperitoneum) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
8.2. Analysis.
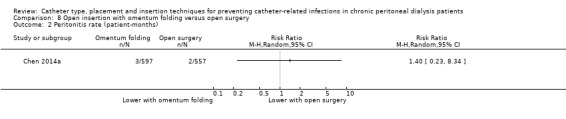
Comparison 8 Open insertion with omentum folding versus open surgery, Outcome 2 Peritonitis rate (patient‐months).
8.3. Analysis.
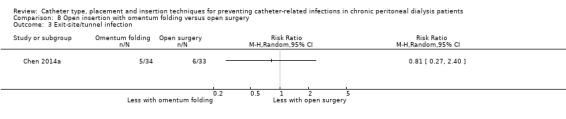
Comparison 8 Open insertion with omentum folding versus open surgery, Outcome 3 Exit‐site/tunnel infection.
8.4. Analysis.
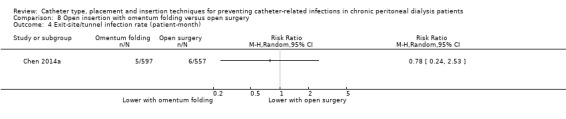
Comparison 8 Open insertion with omentum folding versus open surgery, Outcome 4 Exit‐site/tunnel infection rate (patient‐month).
8.5. Analysis.
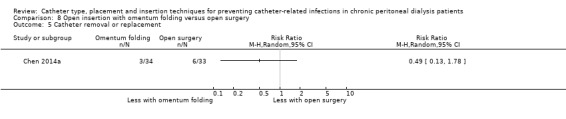
Comparison 8 Open insertion with omentum folding versus open surgery, Outcome 5 Catheter removal or replacement.
8.6. Analysis.
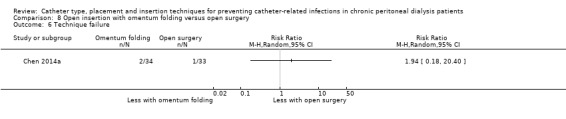
Comparison 8 Open insertion with omentum folding versus open surgery, Outcome 6 Technique failure.
8.7. Analysis.
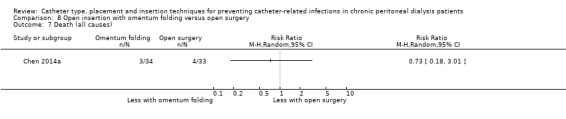
Comparison 8 Open insertion with omentum folding versus open surgery, Outcome 7 Death (all causes).
8.8. Analysis.
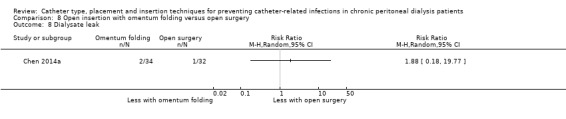
Comparison 8 Open insertion with omentum folding versus open surgery, Outcome 8 Dialysate leak.
8.9. Analysis.
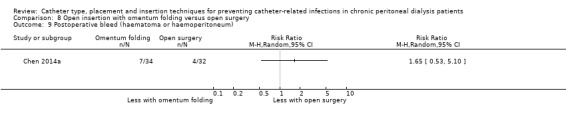
Comparison 8 Open insertion with omentum folding versus open surgery, Outcome 9 Postoperative bleed (haematoma or haemoperitoneum).
Comparison 9. Modified surgery with or without catheter fixation versus open surgery.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Catheter removal or replacement | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Dialysate leak | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Postoperative bleed (haematoma or haemoperitoneum) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
9.2. Analysis.
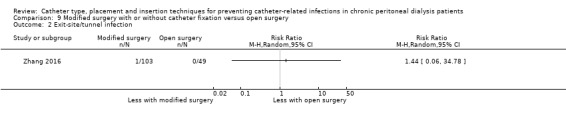
Comparison 9 Modified surgery with or without catheter fixation versus open surgery, Outcome 2 Exit‐site/tunnel infection.
9.4. Analysis.
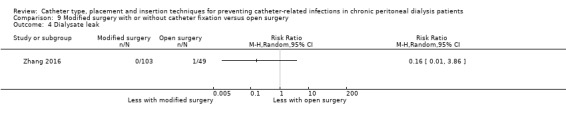
Comparison 9 Modified surgery with or without catheter fixation versus open surgery, Outcome 4 Dialysate leak.
9.5. Analysis.
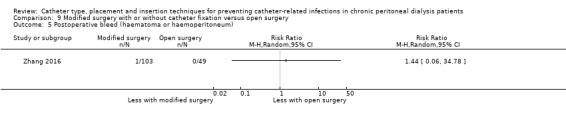
Comparison 9 Modified surgery with or without catheter fixation versus open surgery, Outcome 5 Postoperative bleed (haematoma or haemoperitoneum).
Comparison 10. Vertical tunnel‐based low‐site insertion versus open surgery.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
10.2. Analysis.
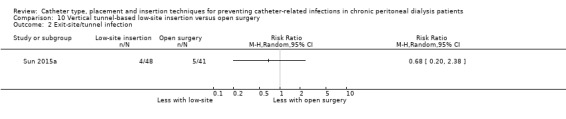
Comparison 10 Vertical tunnel‐based low‐site insertion versus open surgery, Outcome 2 Exit‐site/tunnel infection.
Comparison 11. Ureteroscope‐assisted technique versus modified open surgery.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Death (all causes) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
11.2. Analysis.
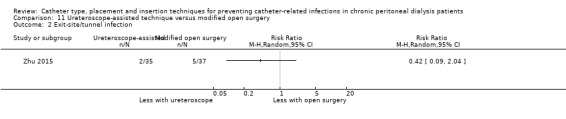
Comparison 11 Ureteroscope‐assisted technique versus modified open surgery, Outcome 2 Exit‐site/tunnel infection.
11.3. Analysis.
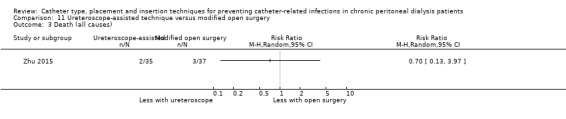
Comparison 11 Ureteroscope‐assisted technique versus modified open surgery, Outcome 3 Death (all causes).
Comparison 12. Radiological versus surgical implantation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis rate (patient‐month) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection (patient‐months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Catheter removal or replacement | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Death (all causes) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Dialysate leak | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
12.2. Analysis.
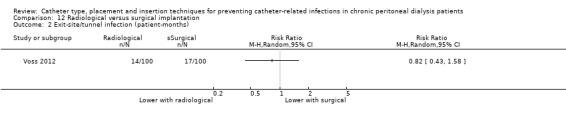
Comparison 12 Radiological versus surgical implantation, Outcome 2 Exit‐site/tunnel infection (patient‐months).
12.3. Analysis.
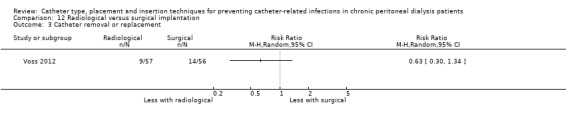
Comparison 12 Radiological versus surgical implantation, Outcome 3 Catheter removal or replacement.
12.4. Analysis.
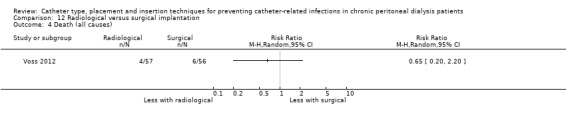
Comparison 12 Radiological versus surgical implantation, Outcome 4 Death (all causes).
12.5. Analysis.
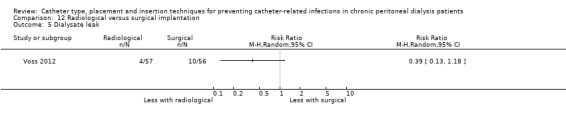
Comparison 12 Radiological versus surgical implantation, Outcome 5 Dialysate leak.
Comparison 13. Cystoscopy‐assisted surgery versus open surgery.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Dialysate leak | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
13.2. Analysis.
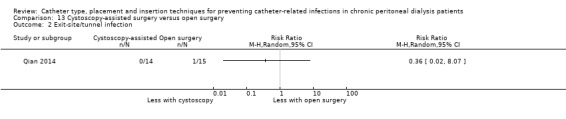
Comparison 13 Cystoscopy‐assisted surgery versus open surgery, Outcome 2 Exit‐site/tunnel infection.
13.3. Analysis.
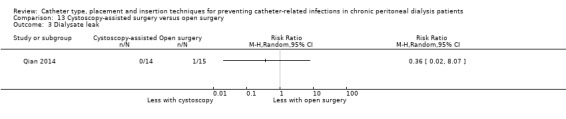
Comparison 13 Cystoscopy‐assisted surgery versus open surgery, Outcome 3 Dialysate leak.
Comparison 14. Laparoscopic Moncrief‐Popovich versus Trocar technique.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Dialysate leak | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
14.2. Analysis.
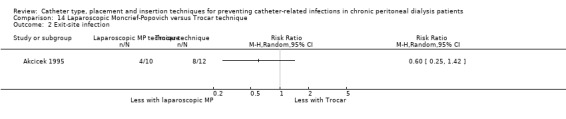
Comparison 14 Laparoscopic Moncrief‐Popovich versus Trocar technique, Outcome 2 Exit‐site infection.
14.3. Analysis.
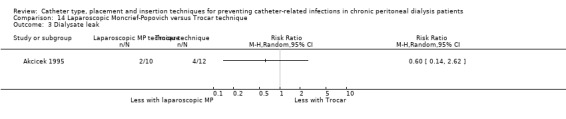
Comparison 14 Laparoscopic Moncrief‐Popovich versus Trocar technique, Outcome 3 Dialysate leak.
Comparison 15. Single versus double cuff.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Catheter removal or replacement | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Technique failure | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Death (all causes) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
15.2. Analysis.
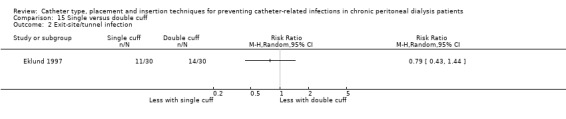
Comparison 15 Single versus double cuff, Outcome 2 Exit‐site/tunnel infection.
15.3. Analysis.
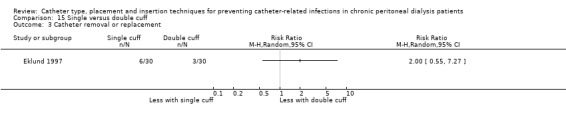
Comparison 15 Single versus double cuff, Outcome 3 Catheter removal or replacement.
15.4. Analysis.
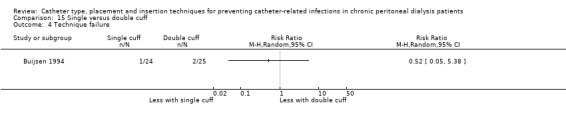
Comparison 15 Single versus double cuff, Outcome 4 Technique failure.
15.5. Analysis.
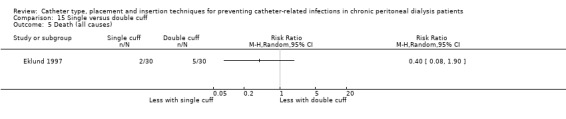
Comparison 15 Single versus double cuff, Outcome 5 Death (all causes).
Comparison 16. Triple cuff versus double catheter.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Peritonitis rate (patient‐months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Exit‐site/tunnel infection (patient‐months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Catheter removal or replacement | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Dialysate leak | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
16.2. Analysis.
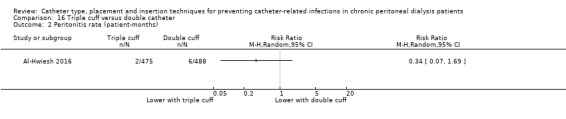
Comparison 16 Triple cuff versus double catheter, Outcome 2 Peritonitis rate (patient‐months).
16.3. Analysis.
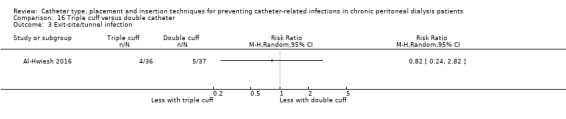
Comparison 16 Triple cuff versus double catheter, Outcome 3 Exit‐site/tunnel infection.
16.4. Analysis.
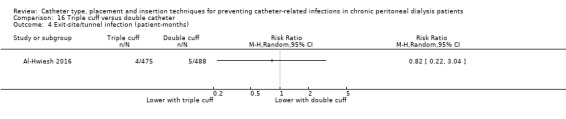
Comparison 16 Triple cuff versus double catheter, Outcome 4 Exit‐site/tunnel infection (patient‐months).
16.5. Analysis.
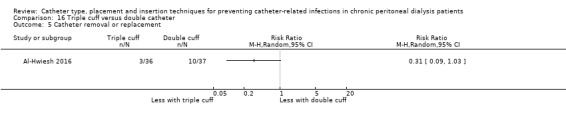
Comparison 16 Triple cuff versus double catheter, Outcome 5 Catheter removal or replacement.
16.6. Analysis.
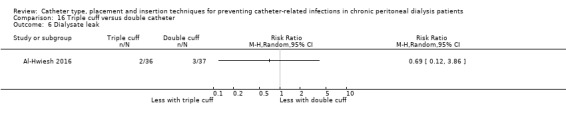
Comparison 16 Triple cuff versus double catheter, Outcome 6 Dialysate leak.
Comparison 17. Swan‐neck versus straight curled catheter.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Peritonitis rate (patient‐months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Exit‐site/tunnel infection rate (patient‐months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Technique failure | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Dialysate leak | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
17.2. Analysis.
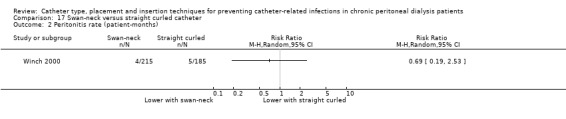
Comparison 17 Swan‐neck versus straight curled catheter, Outcome 2 Peritonitis rate (patient‐months).
17.3. Analysis.
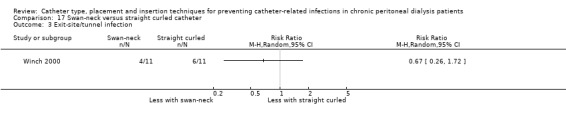
Comparison 17 Swan‐neck versus straight curled catheter, Outcome 3 Exit‐site/tunnel infection.
17.4. Analysis.
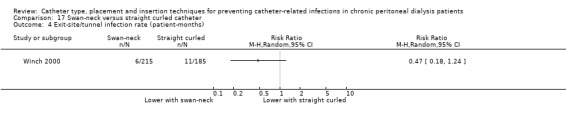
Comparison 17 Swan‐neck versus straight curled catheter, Outcome 4 Exit‐site/tunnel infection rate (patient‐months).
17.5. Analysis.
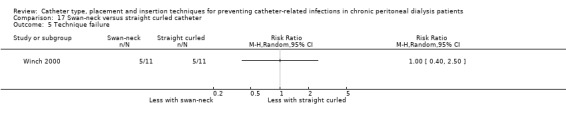
Comparison 17 Swan‐neck versus straight curled catheter, Outcome 5 Technique failure.
17.6. Analysis.
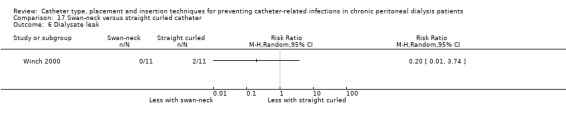
Comparison 17 Swan‐neck versus straight curled catheter, Outcome 6 Dialysate leak.
Comparison 18. Antibiotic‐treated catheter versus none.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Catheter removal or replacement | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Death (all causes) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
18.2. Analysis.
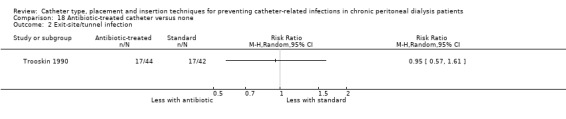
Comparison 18 Antibiotic‐treated catheter versus none, Outcome 2 Exit‐site/tunnel infection.
18.3. Analysis.
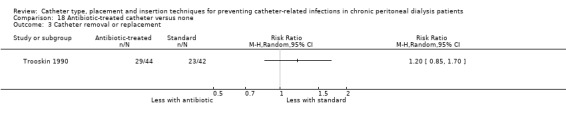
Comparison 18 Antibiotic‐treated catheter versus none, Outcome 3 Catheter removal or replacement.
18.4. Analysis.
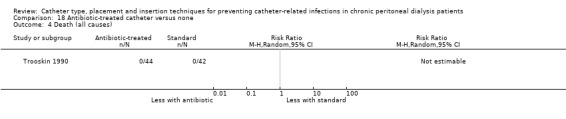
Comparison 18 Antibiotic‐treated catheter versus none, Outcome 4 Death (all causes).
Comparison 19. Immobilisation versus no immobilisation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
19.2. Analysis.
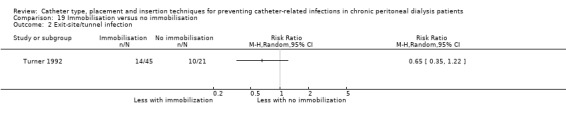
Comparison 19 Immobilisation versus no immobilisation, Outcome 2 Exit‐site/tunnel infection.
Comparison 20. Silver ring versus no silver ring.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peritonitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Exit‐site/tunnel infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Technique failure | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Death (all causes) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
20.2. Analysis.
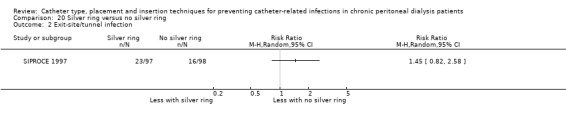
Comparison 20 Silver ring versus no silver ring, Outcome 2 Exit‐site/tunnel infection.
20.3. Analysis.
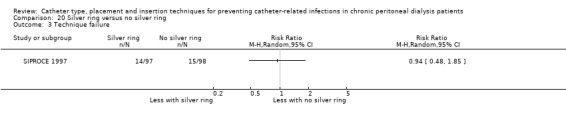
Comparison 20 Silver ring versus no silver ring, Outcome 3 Technique failure.
20.4. Analysis.
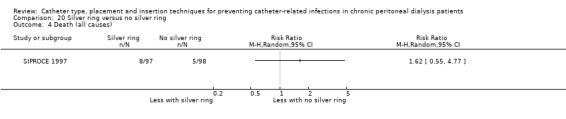
Comparison 20 Silver ring versus no silver ring, Outcome 4 Death (all causes).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Akcicek 1995.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Akyol 1990.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote " Neither the patients nor the staff supervising their care thereafter were aware of the type of catheter used." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5% dropout (2/40) |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Al‐Hwiesh 2016.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised using adaptive randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Most outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Atapour 2011.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation software |
| Allocation concealment (selection bias) | Low risk | Random allocation software |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | High risk | The incidence of infection was reported for the first two weeks only, did not report infection at the end of study |
| Other bias | Unclear risk | No information was provided for who performed the procedures for both groups |
Buijsen 1994.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Chen 2014a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All the outcomes are reported |
| Other bias | High risk | Assessment of presence of greater omentum was only possible during operation hence it is unclear randomisation was occurred after surgical incision was made |
Danielsson 2002.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1.5% dropout (1/60) |
| Selective reporting (reporting bias) | Low risk | Most outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Dasgupta 1998.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Reported few outcomes |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Ejlersen 1990.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Most outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Eklund 1994.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered sealed envelopes containing catheter configurations in random order |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | High risk | Definition of peritonitis was different from the ISPD guidelines |
Eklund 1995.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered sealed envelopes containing catheter configurations in random order |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout (14/40, transferred to HD or death) |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Eklund 1997.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Unclear, unable to totally exclude reporting bias |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Gadallah 1999.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation method was by alternate months, quasi‐RCT |
| Allocation concealment (selection bias) | High risk | Alternate months |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3% dropout (5/148) |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Johnson 2006.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number list with randomisation blocks of 20 |
| Allocation concealment (selection bias) | Low risk | Random number with randomisation blocks of 20 |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Low risk, most outcomes were reported |
| Other bias | High risk | Unequal baseline characteristics |
Jwo 2010.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Insufficient information to permit judgement, significantly high number of cirrhosis patients in laparoscopic group |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss of follow‐up |
| Selective reporting (reporting bias) | Low risk | All the outcomes were reported |
| Other bias | High risk | Different baseline characteristic between the two groups |
Li 2009e.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomising chart |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients were followed up and analysed |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | High risk | Procedures were performed by 3 nephrologists; the study was terminated earlier than planned as they ran out of catheters |
Lo 2003b.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | High risk | Not all of the outcomes were reported |
| Other bias | Unclear risk | Despite calculate power before the study, no significant difference in the outcomes was observed after complete the recruitment and finally the number of recruitment was increased by 50% |
Lye 1996.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate randomisation |
| Allocation concealment (selection bias) | High risk | Alternate randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 7% lost to follow‐up (3/40) |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Merrikhi 2014.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Study was registered with Iranian Registry of clinical trials |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Moncrief 1998.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Outcomes were not reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Nielsen 1995.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study described as randomised; method of randomisation not reported |
| Allocation concealment (selection bias) | Low risk | Sequentially number sealed envelopes with catheter type in random order |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Both participants and personnel are blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout rate (32/72) |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Ouyang 2015.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 22% dropout (43/189) |
| Selective reporting (reporting bias) | Low risk | All the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Park 1998.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2% dropout (1/60) |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Qian 2014.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Rubin 1990.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group (groups 1 and 3)
Control group (groups 2 and 4)
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | High risk | Introduced new type of catheter and new catheter insertion technique at the same time for the treatment group |
Sanchez‐Canel 2016.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Some of outcomes were not reported |
| Other bias | High risk | Different baseline characteristics; BMI significantly higher in the control group |
Scott 1994.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group 1
Control group 2
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement, unclear |
| Selective reporting (reporting bias) | High risk | Not all the outcomes of interest were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
SIPROCE 1997.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout 30% (59/195) |
| Selective reporting (reporting bias) | Low risk | Most of the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Stegmayr 2005a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | High risk | Few outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Stegmayr 2015.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A peritoneal dialysis nurse made randomization from envelopes and provided the surgeon with the respective catheter" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "A peritoneal dialysis nurse made randomization from envelopes and provided the surgeon with the respective catheter" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout; loss to follow‐up: died (7/61), transfer to HD (20/61), transplant (15/61) |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Significantly large number of patients from treatment group dropped out due to transplant |
Sun 2015a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout rate |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Timely PD 2010.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation sequence was generated using STATA software (permuted block) |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropout |
| Selective reporting (reporting bias) | Low risk | Published protocol before study |
| Other bias | High risk | Protocol violation present |
Trooskin 1990.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Low risk | Most of the outcomes of interest were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Tsimoyiannis 2000.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | Quote: "Closed envelope contained information regarding placement into group A or B" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10% dropout (5/50) |
| Selective reporting (reporting bias) | High risk | Not all the outcomes of interest were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Turner 1992.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Voss 2012.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "allocated by simple randomization... performed by the research staff not involved with the care of the subjects" |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Winch 2000.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout (8/22) |
| Selective reporting (reporting bias) | Low risk | Reported most of outcomes |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Wright 1999.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
Other information
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | "Sealed enveloped containing cards with 'laparoscopic" or "conventional". Cards stored in theatre anaesthetic room and one envelope opened after each patient was anaesthetized" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Low dropout rate (5/50) |
| Selective reporting (reporting bias) | Low risk | Most outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Xie 2011a.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated random numbers |
| Allocation concealment (selection bias) | Low risk | "Randomization was performed using sequentially numbered opaque sealed envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout (1/80) |
| Selective reporting (reporting bias) | High risk | Not all the outcomes were reported |
| Other bias | Unclear risk | Insufficient information to permit judgement |
Yip 2010.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout rate (6/101) |
| Selective reporting (reporting bias) | Low risk | All the outcomes were reported |
| Other bias | Unclear risk | No prophylactic antibiotic for exit site. The study reported the procedures were performed by trained nephrologists in the unit, but unclear about the grade and training experience of the procedurists |
Zhang 2016.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group 1
Treatment group 2
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All the outcomes were reported |
| Other bias | High risk | Percentage of patients with pervious abdominal surgery was appear to be higher than the other two modified surgery group (20.4% versus 10.2% and 13.0%) |
Zhu 2015.
| Methods |
|
|
| Participants |
|
|
| Interventions | Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization was done on the day of intervention using the closed envelope method" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Low risk | All the outcomes were reported |
| Other bias | High risk | Unequal baseline characteristics between groups, significantly more patients in the treatment had history of abdominal surgery |
AKI ‐ acute kidney injury; APD ‐ automated peritoneal dialysis; BMI ‐ body mass index; CAD ‐ coronary artery disease; CAPD ‐ continuous ambulatory peritoneal dialysis; CKD ‐ chronic kidney disease; COPD ‐ chronic obstructive pulmonary disease; ESKD ‐ end‐stage kidney disease; HD ‐ haemodialysis; HIV ‐ human immunodeficiency virus; IQR ‐ interquartile range; IPD ‐ intermittent peritoneal dialysis; IV ‐ intravenous; M/F ‐ male/female; MI ‐ myocardial infarction; PD ‐ peritoneal dialysis; PKD ‐ polycystic kidney disease; RCT ‐ randomised controlled trial; RRT ‐ renal replacement therapy; WCC ‐ white cell count
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Crabtree 2003 | Issues with randomisation: 5 patients entered the study twice, another 5 patients were not randomised |
| ISRCTN87054124 | Study terminated due to recruitment issues |
| Moncrief 1994 | Study terminated for incomplete recruitment |
| N0547061060 | Unable to obtain sufficient information on the study type, populations or interventions to determine if the study meets all the review criteria |
| O'Dwyer 2005 | Wrong intervention: compared two types of tunnelled HD catheters |
| Williams 1989 | Wrong intervention: compared different methods of therapy for peritonitis |
HD ‐ haemodialysis
Characteristics of studies awaiting assessment [ordered by study ID]
Ahmad 2010.
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
|
| Outcomes |
|
| Notes |
|
LOCI 2011.
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
|
| Outcomes |
|
| Notes |
|
Wong 2004b.
| Methods |
|
| Participants |
|
| Interventions | Treatment group
Control group
|
| Outcomes |
|
| Notes |
|
PD ‐ peritoneal dialysis; QoL ‐ quality of life; RCT ‐ randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
NCT01023191.
| Trial name or title | A prospective randomized controlled trial of local anaesthetic percutaneous insertion versus general anaesthetic open surgical placement of continuous peritoneal dialysis catheters in a university teaching hospital |
| Methods |
|
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Treatment group
Control group
|
| Outcomes |
|
| Starting date | December 2011 |
| Contact information | Contact: Ian C Chetter, MB ChB |
| Notes |
NCT02479295.
| Trial name or title | Randomized controlled trial of straight versus coiled peritoneal dialysis |
| Methods |
|
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Treatment group
Control group
|
| Outcomes |
|
| Starting date | June 2015 |
| Contact information | Kai Ming Chow, MBChB, FRCP |
| Notes |
PD ‐ peritoneal dialysis; RCT ‐ randomised controlled trial
Differences between protocol and review
Peritonitis relapse and time to the first episode of peritonitis and peritonitis‐related death were unable to examine in the review as all the included studies did not specifically report these outcomes.
Contributions of authors
Screening of titles and abstracts: HH, YJ
Study eligibility: HH, YJ
Data collection for the review was carried out independently by HH and YJ
Quality assessment, data analysis: HH, YJ, GFMS
Writing of review: HH, YC, DJ, GFMS, JC
Providing general advice on the review; DJ, GFMS, JC, FPS, AT
Disagreements were resolved in consultation with DJ, GFMS and JC
Declarations of interest
Professor David Johnson is a current recipient of a National Health and Medical Research Council Practitioner Fellowship. Professor David Johnson has received consultancy fees, research grants, speaker’s honoraria and travel sponsorships for Baxter Healthcare and Fresenius Medical Care. He has also received a consulting fee from AstraZeneca and travel grants from Amgen
Yeoungjee Cho is a current recipient of a National Health and Medical Research Council Early Career Fellowship and has in the past received research grants from Fresenius Medical Care.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Akcicek 1995 {published data only}
- Akcicek F, Ok E, Tokut Y, Cirit M, Kursal A, Unsul A, et al. Comparison the effect of laparoscopic Moncrief‐Popovich technique (LMPT) and blind Trocar technique (BTT) on early CAPD complications [abstract]. Nephrology Dialysis Transplantation 1995;10(6):1037. [CENTRAL: CN‐00261138] [Google Scholar]
Akyol 1990 {published data only}
- Akyol AM, Porteous C, Brown MW. A comparison of two types of catheters for continuous ambulatory peritoneal dialysis (CAPD). Peritoneal Dialysis International 1990;10(1):63‐6. [MEDLINE: ] [PubMed] [Google Scholar]
Al‐Hwiesh 2016 {published data only}
- Al‐Hwiesh A, Nasreldin M. The Saudi peritoneal dialysis catheter: Modified catheter and new technique: farewell to catheter migration [abstract no: SP456]. Nephrology Dialysis Transplantation 2016;31(Suppl 1):i244. [EMBASE: 72326558] [Google Scholar]
- Al‐Hwiesh AK. A modified peritoneal dialysis catheter with a new technique: farewell to catheter migration. Saudi Journal of Kidney Diseases & Transplantation 2016;27(2):281‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Atapour 2011 {published data only}
- Atapour A, Asadabadi HR, Karimi S, Eslami A, Beigi AA. Comparing the outcomes of open surgical procedure and percutaneously peritoneal dialysis catheter (PDC) insertion using laparoscopic needle: a two month follow‐up study. Journal of Research in Medical Sciences 2011;16(4):463‐8. [EMBASE: 2011292097] [PMC free article] [PubMed] [Google Scholar]
Buijsen 1994 {published data only}
- Buijsen JGM, Kox C, Boeschoten EW, Struijk DG. Randomized trial to compare single cuff (Sc) with double cuff (Dc) straight tenckhoff catheter (Tc) in CAPD patients (pt) [abstract]. Nephrology Dialysis Transplantation 1994;9(5):583. [CENTRAL: CN‐00444579] [Google Scholar]
- Struijk DG, Kox C, vd Heijden‐Buijsen JG. Randomized trial of single cuff (sc) versus double cuff (dc) peritoneal dialysis catheter [abstract]. 35th Congress. European Renal Association. European Dialysis and Transplantation Association; 1998 Jun 6‐9; Rimini, Italy. 1998:315. [CENTRAL: CN‐00486056]
Chen 2014a {published data only}
- Chen G, Liu H, Zhou L, Wang P, Peng Y, Liu FU. Greater omentum folding in open surgical placement of PD catheters: a randomized controlled study and systemic review [abstract no: FR‐PO965]. Journal of the American Society of Nephrology 2013;24:582A. [DOI] [PubMed] [Google Scholar]
- Chen G, Wang P, Liu H, Zhou L, Cheng M, Liu Y, et al. Greater omentum folding in the open surgical placement of peritoneal dialysis catheters: a randomized controlled study and systemic review. Nephrology Dialysis Transplantation 2014;29(3):687‐97. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Danielsson 2002 {published data only}
- Danielsson A, Blohme L, Tranaeus A, Hylander B. A prospective randomized study of the effect of a subcutaneously "buried" peritoneal dialysis catheter technique versus standard technique on the incidence of peritonitis and exit‐site infection. Peritoneal Dialysis International 2002;22(2):211‐9. [MEDLINE: ] [PubMed] [Google Scholar]
- Danielsson A, Blohme L, Tranaeus A, Hylander B. Prospective randomized study of the impact a subcutaneous rest‐peroid of a PD‐catheter has on the incidence of peritonitis [abstract no: A0832]. Journal of the American Society of Nephrology 1997;8(Program & Abstracts):178A. [CENTRAL: CN‐00444979] [Google Scholar]
Dasgupta 1998 {published data only}
- Dasgupta MK, Fox S, Card J, Maitland C, Perry D. Catheter survival is improved by the use of Moncrief‐Popovich catheters [abstract]. Journal of the American Society of Nephrology 1998;9(Program & Abstracts):190A. [CENTRAL: CN‐00444987] [Google Scholar]
Ejlersen 1990 {published data only}
- Ejlersen E, Steven K, Lokkergaard H. Paramedian versus midline incision for the insertion of permanent peritoneal dialysis catheters. A randomized clinical trial. Scandinavian Journal of Urology & Nephrology 1990;24(2):151‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Eklund 1994 {published data only}
- Eklund BH, Honkanen EO, Kala AR, Kyllonen LE. Catheter configuration and outcome in patients on continuous ambulatory peritoneal dialysis: a prospective comparison of two catheters. Peritoneal Dialysis International 1994;14(1):70‐4. [MEDLINE: ] [PubMed] [Google Scholar]
Eklund 1995 {published data only}
- Eklund BH, Honkanen EO, Kala AR, Kyllonen LE. Peritoneal dialysis access: prospective randomized comparison of the Swan neck and Tenckhoff catheters. Peritoneal Dialysis International 1995;15(8):353‐6. [MEDLINE: ] [PubMed] [Google Scholar]
Eklund 1997 {published data only}
- Eklund B, Honkanen E, Kyllonen L, Salmela K, Kala AR. Peritoneal dialysis access: prospective randomized comparison of single‐cuff and double‐cuff straight Tenckhoff catheters. Nephrology Dialysis Transplantation 1997;12(2):2664‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gadallah 1999 {published data only}
- Gadallah MF, Pervez A, El‐Shahawy M, Sorrells D, Zibari G, McDonald J, et al. Peritoneoscopic versus surgical placement of Tenckhoff catheters: a prospective study on outcome [abstract no: A0904]. Journal of the American Society of Nephrology 1996;7(9):1428. [CENTRAL: CN‐01658199] [DOI] [PubMed] [Google Scholar]
- Gadallah MF, Pervez A, el‐Shahawy MA, Sorrells D, Zibari G, McDonald J, et al. Peritoneoscopic versus surgical placement of peritoneal dialysis catheters: a prospective randomized study on outcome. American Journal of Kidney Diseases 1999;33(1):118‐22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Johnson 2006 {published data only}
- Johnson DW, Wong J, Wiggins KJ, Kirwan R, Griffin A, Preston J, et al. A randomized controlled trial of coiled versus straight swan‐neck Tenckhoff catheters in peritoneal dialysis patients. American Journal of Kidney Diseases 2006;48(5):812‐21. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Wong JS, Wiggins KJ, Campbell SB, Isbel NM, Mudge DW, Hawley CM, et al. A randomized, controlled trial of coiled versus straight swan neck tenckhoff catheters in peritoneal dialysis patients [abstract no: 1550]. Nephrology 2006;11(Suppl 2):A16. [DOI] [PubMed] [Google Scholar]
Jwo 2010 {published data only}
- Jwo SC, Chen KS, Lee CC, Chen HY. Prospective randomized study for comparison of open surgery with laparoscopic‐assisted placement of Tenckhoff peritoneal dialysis catheter‐‐a single center experience and literature review. Journal of Surgical Research 2010;159(1):489‐96. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Li 2009e {published data only}
- Li CL, Cui TG, Gan HB, Cheung K, Lio WI, Kuok UI. A randomized trial comparing conventional swan‐neck straight‐tip catheters to straight‐tip catheters with an artificial subcutaneous swan neck. Peritoneal Dialysis International 2009;29(3):278‐84. [MEDLINE: ] [PubMed] [Google Scholar]
Lo 2003b {published data only}
- Lo WK, Lui SL, Li FK, Choy BY, Lam MF, Tse KC, et al. A prospective randomized study on three different peritoneal dialysis catheters. Peritoneal Dialysis International 2003;23 Suppl 2:S127‐31. [MEDLINE: ] [PubMed] [Google Scholar]
Lye 1996 {published data only}
- Lye WC, Kour NW, Straaten JC, Leong SO, Lee EJ. A prospective randomized comparison of the Swan neck, coiled, and straight Tenckhoff catheters in patients on CAPD. Peritoneal Dialysis International 1996;16 Suppl 1:S333‐5. [MEDLINE: ] [PubMed] [Google Scholar]
Merrikhi 2014 {published data only}
- Merrikhi A, Beigi AA, Raji Asadabadi H, Gheisari A, Karimi SH. The outcomes of percutaneously peritoneal dialysis catheter placement in comparison with open surgical method in children [abstract no: P177]. Iranian Journal of Kidney Diseases 2011;5(Suppl 1):37. [EMBASE: 70539682] [Google Scholar]
- Merrikhi A, Raji Asadabadi H, Beigi AA, Marashi SM, Ghaheri H, Nasiri Zarch Z. Comparison of percutaneous versus open surgical techniques for placement of peritoneal dialysis catheter in children: a randomized clinical trial. Medical Journal of the Islamic Republic of Iran 2014;28:38. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Moncrief 1998 {published data only}
- Moncrief JW, Popovich PP. Subcutaneous buried versus standard peritoneal dialysis catheter [abstract]. XVIII Annual CAPD Conference; 1998 Feb 24; Nashville (TN). 1998. [CENTRAL: CN‐00776340]
Nielsen 1995 {published data only}
- Nielsen PK, Hemmingsen C, Friis SU, Ladefoged J, Olgaard K. Comparison of straight and curled Tenckhoff peritoneal dialysis catheters implanted by percutaneous technique: a prospective randomized study. Peritoneal Dialysis International 1995;15(1):18‐21. [MEDLINE: ] [PubMed] [Google Scholar]
Ouyang 2015 {published data only}
- Ouyang CJ, Huang FX, Yang QQ, Jiang ZP, Chen W, Qiu Y, et al. Comparing the incidence of catheter‐related complications with straight and coiled tenckhoff catheters in peritoneal dialysis patients‐a single‐center prospective randomized trial. Peritoneal Dialysis International 2015;35(4):443‐9. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 1998 {published data only}
- Park MS, Yim AS, Chung SH, Lee EY, Cha MK, Kim JH, et al. Effect of prolonged subcutaneous implantation of peritoneal catheter on peritonitis rate during CAPD: a prospective randomized study. Blood Purification 1998;16(3):171‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Qian 2014 {published data only}
- Qian X, Qi J. Preliminary report: cystoscopy‐assisted peritoneal dialysis catheter placement ‐ a direct, visual, safe, precise, easy, minimally invasive, and inexpensive technique. Clinical Nephrology 2014;81(4):247‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rubin 1990 {published data only}
- Rubin J, Didlake R, Raju S, Hsu H. A prospective randomized evaluation of chronic peritoneal catheters. Insertion site and intraperitoneal segment. ASAIO Transactions 1990;36(3):M497‐500. [MEDLINE: ] [PubMed] [Google Scholar]
Sanchez‐Canel 2016 {published data only}
- Sanchez‐Canel JJ, Garcia‐Perez H, Garcia‐Calvo R, Pascual MJ, Casado D. Prospective randomized study comparing a single‐cuff self‐locating catheter with a single‐cuff straight tenckhoff catheter in peritoneal dialysis. Peritoneal Dialysis International 2016;36(1):52‐9. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Scott 1994 {published data only}
- Scott PD, Bakran A, Pearson R, Riad H, Parrott N, Johnson RW, et al. Peritoneal dialysis access. Prospective randomized trial of 3 different peritoneal catheters‐‐preliminary report. Peritoneal Dialysis International 1994;14(3):289‐90. [MEDLINE: ] [PubMed] [Google Scholar]
SIPROCE 1997 {published data only}
- Pommer W. The efficiency of a silver ring to prevent exit‐site and other catheter‐related infections in PD‐patients‐final results of the SIPROCE study [abstract no: A0849]. Journal of the American Society of Nephrology 1997;8(Program & Abstracts):182A. [CENTRAL: CN‐00447255] [Google Scholar]
- Pommer W, Brauner M, Westphale HJ, Brunkhorst R, Kramer R, Bundschu D, et al. Effect of a silver device in preventing catheter‐related infections in peritoneal dialysis patients: silver ring prophylaxis at the catheter exit study. American Journal of Kidney Diseases 1998;32(5):752‐60. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- SIPROCE Study Group. Efficiency of a silver ring in preventing exit‐site infections in adult PD patients: results of the SIPROCE Study. Silver ring Prophylaxis of the Catheter Exit Site. Advances in Peritoneal Dialysis 1997;13:227‐32. [MEDLINE: ] [PubMed] [Google Scholar]
Stegmayr 2005a {published data only}
- Stegmayr BG, Wikdahl AM, Bergström M, Nilsson C, Engman U, Arnerlöv C, et al. A randomized clinical trial comparing the function of straight and coiled Tenckhoff catheters for peritoneal dialysis. Peritoneal Dialysis International 2005;25(1):85–8. [MEDLINE: ] [PubMed] [Google Scholar]
Stegmayr 2015 {published data only}
- Stegmayr BG, Sperker W, Nilsson CH, Degerman C, Persson SE, Stenbaek J, et al. Few outflow problems with a self‐locating catheter for peritoneal dialysis: a randomized trial. Medicine 2015;94(48):e2083. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sun 2015a {published data only}
- Sun C, Zhang M, Jiang C. Vertical tunnel‐based low‐site peritoneal dialysis catheter implantation decreases the incidence of catheter malfunction. American Surgeon 2015;81(11):1157‐62. [MEDLINE: ] [PubMed] [Google Scholar]
Timely PD 2010 {published data only}
- Ranganathan D, Baer R, Fassett RG, Williams N, Han T, Watson M, et al. Randomised controlled trial to determine the appropriate time to initiate peritoneal dialysis after insertion of catheter to minimise complications (Timely PD study). BMC Nephrology 2010;11:11. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranganathan D, John GT, Yeoh E, Williams N, O'Loughlin B, Han T, et al. A randomized controlled trial to determine the appropriate time to initiate peritoneal dialysis after insertion of catheter (Timely PD Study). Peritoneal Dialysis International 2017;37(4):420‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Trooskin 1990 {published data only}
- Trooskin SZ, Harvey RA, Lennard TW, Greco RS. Failure of demonstrated clinical efficacy of antibiotic‐bonded continuous ambulatory peritoneal dialysis (CAPD) catheters. Peritoneal Dialysis International 1990;10(1):57‐9. [MEDLINE: ] [PubMed] [Google Scholar]
Tsimoyiannis 2000 {published data only}
- Tsimoyiannis EC, Siakas P, Glantzounis G, Toli C, Sferopoulos G, Pappas M, et al. Laparoscopic placement of the Tenckhoff catheter for peritoneal dialysis. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 2000;10(4):218‐21. [MEDLINE: ] [PubMed] [Google Scholar]
Turner 1992 {published data only}
- Turner K, Edgar D, Hair M, Uttley L, Sternland R, Hunt L, et al. Does catheter immobilization reduce exit‐site infections in CAPD patients?. Advances in Peritoneal Dialysis 1992;8:265‐8. [MEDLINE: ] [PubMed] [Google Scholar]
Voss 2012 {published data only}
- Voss D. Prospective randomised trial of radiological and surgical tenckhoff catheter insertion [abstract no: 101]. Nephrology 2004;9(Suppl 1):A26. [CENTRAL: CN‐00509548] [Google Scholar]
- Voss D, Hawkins S, Poole G, Marshall M. Radiological versus surgical implantation of first catheter for peritoneal dialysis: a randomized non‐inferiority trial. Nephrology Dialysis Transplantation 2012;27(11):4196–204. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Winch 2000 {published data only}
- Winch P, Saltissi D, McGiffin C, Nathanson L, O'Loughlin B. Comparison between swan‐neck (SN) and straight curled (SC) double‐cuff catheters on peritoneal dialysis (PD) catheter‐related complications [abstract no: 29]. Nephrology 2000;5(1‐2 Suppl):A10. [CENTRAL: CN‐01657505] [Google Scholar]
Wright 1999 {published data only}
- Sellars L, Bel'eed K, Stoves J, Eadington D, Johnson B, Wright M, et al. Randomized trial of conventional vs laparoscopically assisted peritoneal catheter insertion techniques (interim report) [abstract]. Journal of the American Society of Nephrology 1997;8(Program & Abstracts):182A. [CENTRAL: CN‐00447669] [Google Scholar]
- Wright MJ, Bel'eed K, Johnson BF, Eadington DW, Sellars L, Farr MJ. Randomized prospective comparison of laparoscopic and open peritoneal dialysis catheter insertion. Peritoneal Dialysis International 1999;19(4):372‐5. [MEDLINE: ] [PubMed] [Google Scholar]
Xie 2011a {published data only}
- Xie J, Kiryluk K, Ren H, Zhu P, Huang X, Shen P, et al. Coiled versus straight peritoneal dialysis catheters: a randomized controlled trial and meta‐analysis. American Journal of Kidney Diseases 2011;58(6):946‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Yip 2010 {published data only}
- Yip T, Lui SL, Tse KC, Xu H, Ng FS, Cheng SW, et al. A prospective randomized study comparing Tenckhoff catheters inserted using the triple incision method with standard swan neck catheters. Peritoneal Dialysis International 2010;30(1):56‐62. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zhang 2016 {published data only}
- Zhang Q, Jiang C, Zhu W, Sun C, Xia Y, Tang T, et al. Peritoneal catheter fixation combined with straight upward tunnel and low implant position to prevent catheter malfunction. Nephrology 2016;23(3):247‐52. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zhu 2015 {published data only}
- Zhu W, Jiang C, Zheng X, Zhang M, Guo H, Yan X. The placement of peritoneal dialysis catheters: a prospective randomized comparison of open surgery versus "Mini‐Perc" technique. International Urology & Nephrology 2015;47(2):377‐82. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Crabtree 2003 {published data only}
- Crabtree JH, Burchette RJ, Siddiqi RA, Huen IT, Hadnott LL, Fishman A. The efficacy of silver‐ion implanted catheters in reducing peritoneal dialysis‐related infections. Peritoneal Dialysis International 2003;23(4):368‐74. [MEDLINE: ] [PubMed] [Google Scholar]
ISRCTN87054124 {published data only}
- Sudhindran S. Prospective randomised trial of laparoscopic versus closed insertion of tenckhoff catheters for peritoneal dialysis access. www.controlled‐trials.com/ISRCTN87054124 (first received 12 September 2003).
Moncrief 1994 {published data only}
- Moncrief JW, Popovich RP. Moncrief‐Popovich catheter: implantation technique and clinical results. Peritoneal Dialysis International 1994;14 Suppl 3:S56‐8. [MEDLINE: ] [PubMed] [Google Scholar]
N0547061060 {published data only}
- Rhodes M. Prospective randomised trial of laparoscopic sutured versus blind (conventional) insertion of tenckhoff peritoneal dialysis catheters. www.nihr.ac.uk/Profile/Pages/NRRResults.aspx?publication_id=N0547061060 (last accessed July 2004).
O'Dwyer 2005 {published data only}
- O'Dwyer H, Fotheringham T, O'Kelly P, Doyle S, Haslam P, McGrath F, et al. A prospective comparison of two types of tunneled hemodialysis catheters: the Ash Split versus the PermCath. Cardiovascular & Interventional Radiology 2005;28(1):23‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Williams 1989 {published data only}
- Williams AJ, Boletis I, Johnson BF, Raftery AT, Cohen GL, Moorhead PJ, et al. Tenckhoff catheter replacement or intraperitoneal urokinase: a randomised trial in the management of recurrent continuous ambulatory peritoneal dialysis (CAPD) peritonitis. Peritoneal Dialysis International 1989;9(1):65‐7. [MEDLINE: ] [PubMed] [Google Scholar]
References to studies awaiting assessment
Ahmad 2010 {published data only}
- Ahmad SF, Liu WJ, Mohd Y, Kandasami ND, Hooi LS, Gunn KB. Randomized controlled trial of peritoneoscopic vs open surgical placement of peritoneal dialysis catheters [abstract]. Peritoneal Dialysis International 2010;30(Suppl 2):S95. [EMBASE: 71928045] [Google Scholar]
LOCI 2011 {published data only}
- Hagen SM, Alphen AM, Ijzermans JN, Dor FJ. Laparoscopic versus open peritoneal dialysis catheter insertion, the LOCI‐trial: a study protocol. BMC Surgery 2011;11:35. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafranca JA, Hagen SM, Akkersdijk GP, Wever JJ, Kimenai HJ, Wabbijn M, et al. Laparoscopic vs open peritoneal dialysis catheter insertion, the LOCI‐trial [abstract]. European Surgical Research 2014;52(3‐4):139. [EMBASE: 71493264] [Google Scholar]
Wong 2004b {published data only}
- Wong FS, Chau S, Chow N, Ho JC, Cheng Y, Yu AW. Effect of changing transfer set on relapse of bacterial peritonitis. Hong Kong Journal of Nephrology 2004;6(2):87‐91. [EMBASE: 2004491078] [Google Scholar]
References to ongoing studies
NCT01023191 {published data only}
- Chetter IC. Open versus percutaneous insertion of CAPD catheters. www.clinicaltrials.gov/ct2/show/NCT01023191 (date first received 2 December 2009).
NCT02479295 {published data only}
- Chow KM. Straight versus coiled peritoneal dialysis catheter for peritoneal dialysis patients. www.clinicaltrials.gov/ct2/show/NCT02479295 (date first received 24 June 2015).
Additional references
Barraclough 2010
- Barraclough K, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, et al. Polymicrobial peritonitis in peritoneal dialysis patients in Australia: predictors, treatment, and outcomes. American Journal of Kidney Diseases 2010;55(1):121‐31. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Boudville 2012
- Boudville N, Kemp A, Clayton P, Lim W, Badve SV, Hawley CM, et al. Recent peritonitis associates with mortality among patients treated with peritoneal dialysis. Journal of the American Society of Nephrology 2012;23(8):1398–405. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2016
- Campbell DJ, Craig JC, Mudge DW, Brown FG, Wong G, Tong A. Patients' perspectives on the prevention and treatment of peritonitis in peritoneal dialysis: a semi‐structured interview study. Peritoneal Dialysis International 2016;36(6):631‐9. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chow 2005
- Chow KM, Szeto CC, Leung CB, Kwan BC, Law MC, Li PK. A risk analysis of continuous ambulatory peritoneal dialysis‐related peritonitis. Peritoneal Dialysis International 2005;25(4):374–9. [MEDLINE: ] [PubMed] [Google Scholar]
CONSORT 2001
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. Lancet 2001;357(9263):1191‐4. [MEDLINE: ] [PubMed] [Google Scholar]
Edey 2010
- Edey M, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, et al. Enterococcal peritonitis in Australian peritoneal dialysis patients: predictors, treatment and outcomes in 116 cases. Nephrology Dialysis Transplantation 2010;25(4):1272‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey‐Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple graphical test. BMJ 1997;315(7109):629‐34. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADE 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADE 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction‐GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383‐94. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hagen 2014
- Hagen SM, Lafranca JA, Ijzermans JN, Dor FJ. A systematic review and meta‐analysis of the influence of peritoneal dialysis catheter type on complication rate and catheter survival. Kidney International 2014;85(4):920–32. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Htay 2017
- Htay H, Cho Y, Pascoe EM, Darssan D, Nadeau‐Fredette AC, Hawley C, et al. Multicenter registry analysis of center characteristics associated with technique failure in patients on incident peritoneal dialysis. Clinical Journal of The American Society of Nephrology: CJASN 2017;12(7):1090‐9. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Htay 2018
- Htay H, Cho Y, Pascoe EM, Darssan D, Nadeau‐Fredette AC, Hawley C, et al. Center effects and peritoneal dialysis peritonitis outcomes: analysis of a national registry. American Journal of Kidney Diseases 2018;74(6):814‐21. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Jegatheesan 2018
- Jegatheesan D, Johnson DW, Cho Y, Pascoe EM, Darssan D, Htay H, et al. The relationship between body mass index and organism‐specific peritonitis. Peritoneal Dialysis International 2018;38(3):206‐14. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kolesnyk 2010
- Kolesnyk I, Dekker FW, Boeschoten EW, Krediet RT. Time‐dependent reasons for peritoneal dialysis technique failure and mortality. Peritoneal Dialysis International 2010;30(2):170‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kotsanas 2007
- Kotsanas D, Polkinghorne KR, Korman TM, Atkins RC, Brown F. Risk factors for peritoneal dialysis‐related peritonitis: can we reduce the incidence and improve patient selection?. Nephrology 2007;12(3):239–45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Li 2016
- Li PK, Szeto CC, Piraino B, Arteaga J, Fan S, Figueiredo AE, et al. ISPD peritonitis recommendations: 2016 update on prevention and treatment. Peritoneal Dialysis International 2016;36(5):481–508. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2017
- Li PK, Chow KM, Luijtgaarden MW, Johnson DW, Jager KJ, Mehrotra R, et al. Changes in the worldwide epidemiology of peritoneal dialysis. Nature Reviews Nephrology 2017;13(2):90‐103. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lim 2011
- Lim WH, Boudville N, McDonald SP, Gorham G, Johnson DW, Jose M. Remote indigenous peritoneal dialysis patients have higher risk of peritonitis, technique failure, all‐cause and peritonitis‐related mortality. Nephrology Dialysis Transplantation 2011;26(10):3366–72. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lindblad 1988
- Lindblad AS, Hamilton RW, Nolph KD, Novak JW. A retrospective analysis of catheter configuration and cuff type: a National CAPD Registry report. Peritoneal Dialysis International 1988;8(2):129–33. [EMBASE: 18252569] [Google Scholar]
McDonald 2004
- McDonald SP, Collins JF, Rumpsfeld M, Johnson DW. Obesity is a risk factor for peritonitis in the Australian and New Zealand peritoneal dialysis patient populations. Peritoneal Dialysis International 2004;24(4):340–6. [MEDLINE: ] [PubMed] [Google Scholar]
Mehrotra 2016
- Mehrotra R, Devuyst O, Davies SJ, Johnson DW. The current state of peritoneal dialysis. Journal of the American Society of Nephrology 2016;27(11):3238‐52. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ong 2016
- Ong LM, Ch'ng CC, Wee HC, Supramaniam P, Zainal H, Goh BL, et al. Risk of peritoneal dialysis‐related peritonitis in a multi‐racial Asian population. Peritoneal Dialysis International 2017;37(1):35‐43. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Piraino 2002
- Piraino B. Peritonitis as a complication of peritoneal dialysis. Journal of the American Society of Nephrology 2002;9(10):1956‐64. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schaefer 2003
- Schaefer F. Management of peritonitis in children receiving chronic peritoneal dialysis. Paediatric Drugs 2003;5(5):315‐25. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schünemann 2011a
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and 'Summary of findings' tables. In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Schünemann 2011b
- Schünemann HJ, Oxman AD, Higgins JP, Deeks JJ, Glasziou P, Guyatt GH. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Shen 2013
- Shen JI, Mitani AA, Saxena AB, Goldstein BA, Winkelmayer WC. Determinants of peritoneal dialysis technique failure in incident US patients. Peritoneal Dialysis International 2013;33(2):155‐66. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spence 1985
- Spence PA, Mathews RE, Khanna R, Oreopoulos DG. Improved results with a paramedian technique for the insertion of peritoneal dialysis catheters. Surgery, Gynecology & Obstetrics 1985;161(6):585‐7. [MEDLINE: ] [PubMed] [Google Scholar]
Strippoli 2004a
- Strippoli GF, Tong A, Johnson D, Schena FP, Craig JC. Antimicrobial agents for preventing peritonitis in peritoneal dialysis patients. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD004679.pub2] [DOI] [PubMed] [Google Scholar]
Szeto 2017
- Szeto CC, Li PK, Johnson DW, Bernardini J, Dong J, Figueiredo AE, et al. ISPD catheter‐related infection recommendations: 2017 update. Peritoneal Dialysis International 2017;37(2):141‐54. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wu 2013
- Wu HH, Li IJ, Weng CH, Lee CC, Chen YC, Chang MY, et al. Prophylactic antibiotics for endoscopy‐associated peritonitis in peritoneal dialysis patients. PLoS ONE [Electronic Resource] 2013;8(8):e71532. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2009
- Xu G, Tu W, Xu C. Mupirocin for preventing exit‐site infection and peritonitis in patients undergoing peritoneal dialysis. Nephrology Dialysis Transplantation 2010;25(2):587–92. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Strippoli 2003
- Strippoli GF, Tong A, Johnson D, Schena FP, Craig JC. Catheter type, placement and insertion techniques for preventing peritonitis in peritoneal dialysis patients. Cochrane Database of Systematic Reviews 2003, Issue 3. [DOI: 10.1002/14651858.CD004680] [DOI] [PubMed] [Google Scholar]
Strippoli 2004
- Strippoli GF, Tong A, Johnson D, Schena FP, Craig JC. Catheter type, placement and insertion techniques for preventing peritonitis in peritoneal dialysis patients. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD004680.pub2] [DOI] [PubMed] [Google Scholar]
Strippoli 2004b
- Strippoli GF, Tong A, Johnson D, Schena FP, Craig JC. Catheter‐related interventions to prevent peritonitis in peritoneal dialysis: a systematic review of randomized, controlled trials. Journal of the American Society of Nephrology 2004;15(10):2735‐46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


