This cohort study of 16 741 older women from the Women’s Health Study examines associations of number of steps per day and stepping intensity with all-cause mortality.
Key Points
Question
Are increased numbers of steps per day associated with lower mortality rates among older women?
Findings
In this cohort study of 16 741 women with a mean age of 72 years, steps per day were measured over 7 days. Women who averaged approximately 4400 steps/d had significantly lower mortality rates during a follow-up of 4.3 years compared with the least active women who took approximately 2700 steps/d; as more steps per day were accrued, mortality rates progressively decreased before leveling at approximately 7500 steps/d.
Meaning
More steps taken per day are associated with lower mortality rates until approximately 7500 steps/d.
Abstract
Importance
A goal of 10 000 steps/d is commonly believed by the public to be necessary for health, but this number has limited scientific basis. Additionally, it is unknown whether greater stepping intensity is associated with health benefits, independent of steps taken per day.
Objective
To examine associations of number of steps per day and stepping intensity with all-cause mortality.
Design, Setting, and Participants
This prospective cohort study included 18 289 US women from the Women’s Health Study who agreed to participate by wearing an accelerometer during waking hours for 7 days between 2011 and 2015. A total of 17 708 women wore and returned their devices; data were downloaded successfully from 17 466 devices. Of these women, 16 741 were compliant wearers (≥10 h/d of wear on ≥4 days) and included in the analyses, which took place between 2018 and 2019.
Exposures
Steps per day and several measures of stepping intensity (ie, peak 1-minute cadence; peak 30-minute cadence; maximum 5-minute cadence; time spent at a stepping rate of ≥40 steps/min, reflecting purposeful steps).
Main Outcomes and Measures
All-cause mortality.
Results
Of the 16 741 women who met inclusion criteria, the mean (SD) age was 72.0 (5.7) years. Mean step count was 5499 per day, with 51.4%, 45.5%, and 3.1% of time spent at 0, 1 to 39 (incidental steps), and 40 steps/min or greater (purposeful steps), respectively. During a mean follow-up of 4.3 years, 504 women died. Median steps per day across low-to-high quartiles of distribution were 2718, 4363, 5905, and 8442, respectively. The corresponding quartile hazard ratios (HRs) associated with mortality and adjusted for potential confounders were 1.00 (reference), 0.59 (95% CI, 0.47-0.75), 0.54 (95% CI, 0.41-0.72), and 0.42 (95% CI, 0.30-0.60), respectively (P < .01). In spline analysis, HRs were observed to decline progressively with higher mean steps per day until approximately 7500 steps/d, after which they leveled. For measures of stepping intensity, higher intensities were associated with significantly lower mortality rates; however, after adjusting for steps per day, all associations were attenuated, and most were no longer significant (highest vs lowest quartile for peak 1-minute cadence, HR = 0.87 [95% CI, 0.68-1.11]; peak 30-minute cadence, HR = 0.86 [95% CI, 0.65-1.13]; maximum 5-minute cadence, HR = 0.80 [95% CI, 0.62-1.05]; and time spent at a stepping rate of ≥40 steps/min, HR = 1.27 [95% CI, 0.96-1.68]; P > .05).
Conclusions and Relevance
Among older women, as few as approximately 4400 steps/d was significantly related to lower mortality rates compared with approximately 2700 steps/d. With more steps per day, mortality rates progressively decreased before leveling at approximately 7500 steps/d. Stepping intensity was not clearly related to lower mortality rates after accounting for total steps per day.
Introduction
Wearable technologies, known as wearables, that can track a person’s physical activity behavior are popular consumer items with more than 125 million units shipped worldwide in 2017.1 Such wearables, as well as smartphones, measure number of steps taken via an accelerometer within the device. Worldwide, the average number of steps accrued daily (measured by smartphones) is approximately 5000; in the United States it is 4800.2 A common goal of 10 000 steps/d has been perpetuated by the lay press and is often used as the default by software programs on wearables and smartphones.3,4 However, the origin of the goal of 10 000 steps per day is unclear. It likely derives from the trade name of a pedometer sold in 1965 by Yamasa Clock and Instrument Company in Japan called Manpo-kei, which translates to “10 000 steps meter” in Japanese.5,6
There is limited information on how many daily steps are needed for health,7,8,9,10,11,12,13 particularly as related to clinical end points and mortality.14,15,16,17 Additionally, steps walked can be slow or fast, and it is unknown how stepping intensity is associated with health18 (though there are data on walking pace,19 a related but not identical concept20). An expert committee recently identified a critical gap in knowledge on the dose-response association of steps with health outcomes.18 The 2018 Physical Activity Guidelines Advisory Committee, in a scientific report underpinning the second edition of physical activity guidelines for Americans,18 explained why this information is important: “Steps are a basic unit of locomotion and as such, provide an easy-to-understand metric of ambulation.”18(p8) Furthermore, “…steps can be at light-, moderate-, and vigorous-intensity levels, providing a range of exertion choice to promote walking at all ages and for all levels of fitness. For these reasons, the measure of steps per day has the potential to significantly improve the translation of research findings into public health recommendations, policies, and programs.”18(p8)
To provide information, we addressed 2 key questions using data from a cohort of approximately 18 000 women asked to wear an accelerometer for 7 days and followed for mortality: (1) How many steps per day are associated with lower mortality rates? and (2) For a given step volume (ie, number of steps per day), is the intensity of stepping related to mortality?
Methods
Study Participants
Participants were included from the Women’s Health Study (WHS), a randomized trial evaluating the balance of risks and benefits of using low-dose aspirin and vitamin E for preventing cancer and cardiovascular disease (CVD) among 39 876 women 45 years and older in the United States during the years 1992 through 2004.21,22,23 When the trial ended, women were invited into an observational study, and 33 682 (89% of survivors) consented.
From 2011 through 2015, an ancillary study that assessed physical activity using accelerometers was conducted; details have been previously published.24 Briefly, 18 289 women (62% of survivors) agreed to participate and were eligible; of these, 17 708 subsequently wore and returned their devices. Data were downloaded successfully from the devices of 17 466 women (no data were available from 242 women owing to device failure). All women provided written informed consent to participate, and the study was approved by the Brigham and Women’s Hospital’s institutional review board committee.
Assessment of Steps
We mailed participants ActiGraph GT3X+ accelerometers (ActiGraph Corp, Pensacola, Florida) and asked them to wear the device on the hip for 7 consecutive days, removing it only during sleep and water-based activities. Women returned the devices by mail, and data were screened for wear time using standard techniques.24,25,26 Only women wearing the device for 10 h/d or more on 4 or more days (convention for compliant wear27) are included (n = 16 741; 96% of those with device data).
The accelerometer data were collected at 30 Hz and aggregated into 60-second, time-stamped epochs using the normal filter. Steps per day were determined using the manufacturer’s step algorithm. To calculate step volume, we summed steps across all compliant days and divided this by number of compliant days to obtain mean steps per day. For stepping intensity, we used several proposed measures that reflected a person’s best natural effort in a free-living environment (Table 1).28 Peak 1-minute cadence is the highest number of steps recorded in any single minute of the day; peak 30-minute cadence is the mean steps per minute of the 30 highest 1-minute epochs that need not be consecutive. Maximum 5-minute cadence is the mean steps per minute across any consecutive 5-minute span of the day with the highest number of steps. Maximum 10-minute cadence has also been proposed28; we omitted this for brevity because the correlation of maximum 5-minute and 10-minute cadences was very high (Spearman correlation, r = 0.99); thus, findings would be similar. Finally, we summed time spent at stepping rates of 0, 1 through 39 (incidental steps), and 40 steps/min or greater (purposeful steps).28 We also were interested in a stepping rate of 100 steps/min or greater because this corresponds to walking at moderate intensity or faster.28 However, women hardly stepped at this intensity (median, 0.2% of time); thus, only descriptive statistics are provided.
Table 1. Definitions of Step Variables Used.
| Term | Definition or Explanationa |
|---|---|
| Steps per day | Number of steps recorded for the day |
| Peak 1-min cadence | Number of steps recorded for the single highest minute of the day |
| Peak 30-min cadence | Mean steps/min from the 30 highest minutes of the day; the minutes do not need to be consecutive |
| Maximum 5-min cadence | Mean steps/min from the maximum number of steps recorded over any 5 continuous minutes of the day |
| Stepping rate of 1 to 39 steps/min | Corresponds to incidental or sporadic steps taken |
| Stepping rate of ≥40 steps/min | Corresponds to purposeful steps taken |
| Stepping rate of ≥100 steps/min | Corresponds to walking at moderate intensity (≥3 METs) and higher; equivalent to 2.5 mph and faster |
Abbreviation: METs, metabolic equivalents.
Only days when the device was worn for 10 or more hours (compliant wear) were used.
Assessment of Other Variables
Annual questionnaires about sociodemographic characteristics, health habits, and personal and family medical history were completed by participants. When women reported CVD and cancer, medical records were obtained to confirm diagnoses.9,10,11 We used information from the questionnaire closest to the time that the accelerometer was worn to ascertain weight, height, smoking status, alcohol use, postmenopausal hormone use, self-rated health, hypertension, high cholesterol, diabetes, CVD, cancer, cancer screening, and family medical history. Diet measured by a 131-item food frequency questionnaire was assessed at the start of the WHS.
Ascertainment of Mortality
Deaths were reported by family members or postal authorities, with medical records and death certificates obtained to confirm the reports, or they were ascertained through the National Death Index. Women were followed through December 31, 2017; mortality follow-up is more than 99% complete.29
Statistical Analyses
We categorized women into quartiles of mean steps taken per day, and compared characteristics across quartiles. We then examined the associations of steps per day with all-cause mortality using Cox proportional hazards models. Initial models (Model 1) estimated hazard ratios (HRs) of mortality, adjusting for age and accelerometer wear time (both continuous). Model 2 additionally adjusted for potential confounders: smoking (never, past, current); alcohol use (rarely, monthly, weekly, daily); intakes of saturated fat, fiber, fruit, and vegetables (quintiles of each); postmenopausal hormone therapy (never, past, current); self-rated health (excellent, very good, good, fair/poor); CVD; cancer; cancer screening; parental history of myocardial infarction before 60 years of age; family history of cancer (no or yes for each). Model 3 further adjusted for mediators through which steps may influence mortality rates: body mass index (BMI; calculated as weight in kilograms divided by height in meters squared; continuous); history of hypertension, high cholesterol, diabetes (no or yes for each). Because women who accrue more steps per day also are likely to be stepping at higher intensity, we additionally adjusted for stepping intensity in a fourth model (Model 4, adjusted for Model 2 variables plus peak 1-minute cadence).
To investigate dose-response associations, steps per day were analyzed 3 ways: (1) as quartiles, (2) in 1000-step/d units (modeled as a continuous variable, as well as in discrete categories comparing progressively higher 1000-step/d categories against a referent of 1-1999 steps/d [approximately 5% of women]), and (3) using restricted cubic splines, with 3 knots placed at the 5th, 50th, and 95th percentiles as recommended.30 Because of sparse data, we truncated analysis at 13 500 steps/d (99% of distribution).
We next examined stepping intensity measures and all-cause mortality. Because all stepping intensity variables correlated highly with steps per day (Spearman correlation, r ≥ 0.8; P < .001), we used the residual method31 to adjust for steps per day.
Finally, we conducted sensitivity analyses to minimize reverse causation bias (ie, spurious associations resulting from sick women who decreased their steps) by excluding: (1) the first year of follow-up and women with prevalent CVD, cancer, or diabetes, (2) women self-reporting their health as less than excellent/good, or (3) those with a BMI less than 18.5 kg/m2.
Results
Women included in this analysis had a mean (SD) age of 72.0 (5.7) years (range, 62-101 years) at baseline; they were younger and healthier than nonparticipants of the study. They were compliant with device wear (≥10 h/d) on a median of 7 days and wore the device for a mean (SD) of 14.9 (1.3) h/d. The mean step count was 5499 steps/d (median, 5094 steps/d). With regard to stepping intensity (Table 1), the mean peak 1-minute and 30-minute cadences were 92 and 58 steps/min, respectively, while the mean maximum 5-minute cadence was 63 steps/min (100 steps/min is approximately equivalent to walking at 2.5 mph28). On average, participants spent 51.4% of monitored time taking no steps, 45.5% of time stepping at 1 to 39 steps/min (incidental steps), and 3.1% of time at 40 steps/min or more (purposeful steps). Table 2 provides more details by quartiles of mean steps per day. Within each low-to-high quartile, median step counts were 2718, 4363, 5905, and 8442 steps/d, respectively.
Table 2. Baseline Characteristics of Participants by Quartiles of Mean Steps per Day.
| Characteristic | Quartiles of Mean Steps per Day, Mean (SD) | |||
|---|---|---|---|---|
| Quartile 1 (Lowest) | Quartile 2 | Quartile 3 | Quartile 4 (Highest) | |
| Total participants, No. | 4185 | 4185 | 4186 | 4185 |
| Age, y | 75.2 (6.4) | 72.3 (5.4) | 70.9 (4.8) | 69.7 (4.3) |
| BMI | 28.2 (5.9) | 26.9 (5.0) | 25.6 (4.2) | 24.2 (3.6) |
| Smokers, No. (%) | 235 (5.6) | 142 (3.4) | 135 (3.2) | 77 (1.8) |
| Alcohol use, No. (%) | 2179 (52.1) | 2498 (59.7) | 2782 (62.5) | 2908 (69.5) |
| Using postmenopausal hormones, No. (%) | 346 (8.3) | 395 (9.4) | 485 (11.6) | 432 (10.3) |
| Saturated fat intake, g/d | 20.9 (6.2) | 20.8 (5.9) | 20.3 (5.9) | 19.8 (6.0) |
| Fiber intake, g/d | 21.8 (6.9) | 22.0 (6.8) | 22.4 (7.7) | 23.0 (7.1) |
| Servings of fruits and vegetables per day | 6.6 (4.0) | 6.6 (3.7) | 6.8 (3.6) | 6.9 (3.6) |
| History of hypertension, No. (%) | 3506 (83.8) | 3018 (72.1) | 2638 (63.0) | 2273 (54.3) |
| History of high cholesterol, No. (%) | 3355 (80.2) | 3210 (76.7) | 2950 (70.5) | 2764 (66.1) |
| History of diabetes, No. (%) | 698 (16.7) | 403 (9.6) | 226 (5.4) | 175 (4.2) |
| Cardiovascular disease, No. (%) | 177 (4.2) | 106 (2.5) | 67 (1.6) | 50 (1.2) |
| Cancer, No. (%) | 607 (14.5) | 511 (12.2) | 449 (10.7) | 424 (10.1) |
| No. of days with compliant wear, median (IQR)a | 7 (6-7) | 7 (7-7) | 7 (7-7) | 7 (7-7) |
| H/d of wear on compliant daysa | 14.4 (1.4) | 14.8 (1.2) | 15.0 (1.2) | 15.3 (1.1) |
| Steps/d, median (IQR) | 2718 (2128-3202) | 4363 (3992-4738) | 5905 (5493-6403) | 8442 (7580-9954) |
| Peak cadence, steps/min | ||||
| 1 min | 63.1 (18.4) | 84.6 (15.9) | 97.9 (14.9) | 113.6 (14.6) |
| 30 min | 31.2 (9.5) | 48.1 (11.3) | 63.3 (15.0) | 88.0 (19.8) |
| Maximum 5 min-cadence, steps/min | 35.7 (13.3) | 54.2 (16.0) | 70.0 (19.2) | 93.8 (21.5) |
| Portion of day spent at stepping rate/min, % | ||||
| 0 | 61.3 | 52.7 | 48.1 | 43.4 |
| 1-39 | 37.9 | 45.3 | 48.5 | 50.1 |
| 40-99 | 0.7 | 1.7 | 2.5 | 4.3 |
| ≥100 | 0.1 | 0.3 | 0.7 | 2.2 |
Abbreviations: BMI, body mass index, calculated as weight in kilograms divided by height in meters squared; IQR, interquartile range.
Defined as 10 or more hours of device wear.
During an average follow-up of 4.3 years, 504 women died. Adjusting for age and wear time, the HRs for increasing quartiles of steps per day were 1.00 (reference), 0.51, 0.44, and 0.33, respectively (P < .01) (Table 3). Further adjustment for potential confounders attenuated the associations to 1.00, 0.59, 0.54, and 0.42, respectively (P < .01). The absolute rate reduction comparing extreme quartiles was 9.3 deaths per 1000 person-years. For every additional 1000 steps/d, the HR declined by 15%. Additional adjustment for BMI, hypertension, high cholesterol, and diabetes shifted quartile HRs to become more similar to those adjusted for age and wear time only (1.00, 0.54, 0.47, 0.34; P < .01). When adjusting for stepping intensity in addition to confounders, associations were attenuated but all remained significant (HRs per quartile: 1.00, 0.68, 0.68, 0.58; P < .01).
Table 3. Hazard Ratios and 95% CIs for All-Cause Mortality by Mean Steps per Day.
| Variable | No. of Cases | No. of Women | Hazard Ratio (95% CI)a | |||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 (Adjusted for Stepping Intensity) | |||
| Mean steps/d | ||||||
| Quartile 1 (lowest) | 275 | 4185 | [Reference] | [Reference] | [Reference] | [Reference] |
| Quartile 2 | 103 | 4185 | 0.51 (0.40-0.64) | 0.59 (0.47-0.75) | 0.54 (0.43-0.69) | 0.68 (0.53-0.89) |
| Quartile 3 | 77 | 4186 | 0.44 (0.34-0.58) | 0.54 (0.41-0.72) | 0.47 (0.35-0.62) | 0.68 (0.49-0.94) |
| Quartile 4 (highest) | 49 | 4185 | 0.33 (0.23-0.45) | 0.42 (0.30-0.60) | 0.34 (0.24-0.48) | 0.58 (0.38-0.88) |
| P value for trend | <.01 | <.01 | <.01 | <.01 | ||
| Per 1000 steps/d | 0.80 (0.76-0.84) | 0.85 (0.81-0.90) | 0.82 (0.78-0.87) | 0.89 (0.83-0.95) | ||
Model 1 is adjusted for age and wear time. Model 2 is adjusted for Model 1 variables plus smoking status; alcohol use; intakes of saturated fat, fiber, fruits, and vegetables; hormone therapy; parental history of myocardial infarction; family history of cancer; general health; history of cardiovascular disease; history of cancer; and cancer screening. Model 3 is adjusted for Model 2 variables plus body mass index, calculated as weight in kilograms divided by height in meters squared; history of hypertension, high cholesterol, and diabetes. Model 4 is adjusted for Model 2 variables plus peak 1-minute cadence.
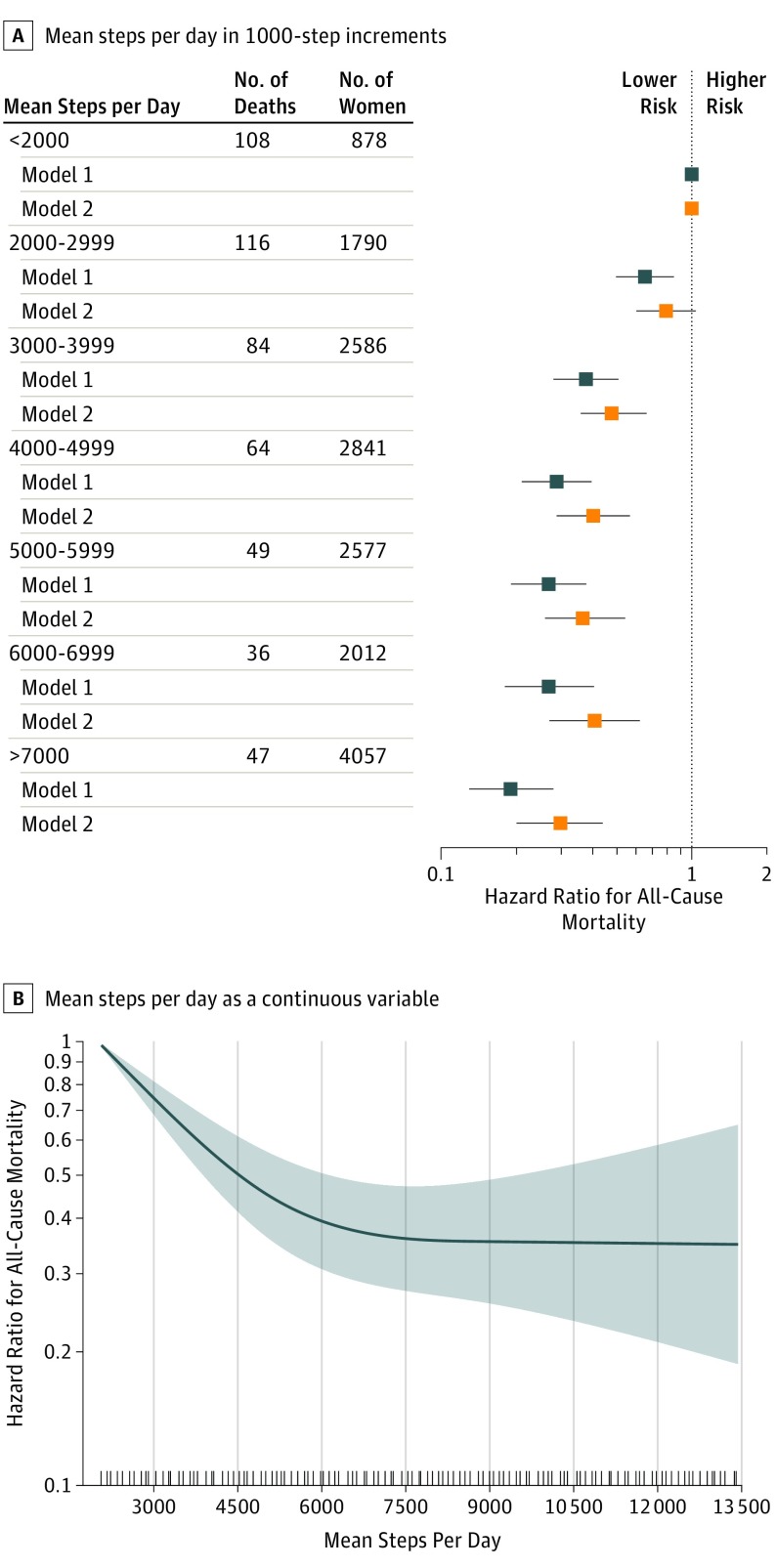
Next, we examined step counts in discrete 1000-step/d categories compared against 2000 steps/d or fewer (Figure, A). Hazard ratios declined significantly, beginning at 3000 to 3999 steps/d, with additional reductions observed at higher steps per day. Spline analyses yielded a similar, but more detailed, dose-response curve showing a steady decline in HRs with more steps per day until approximately 7500 steps/d, beyond which the curve leveled (Figure, B).
Figure. Dose-Response Association Between Mean Steps per Day and All-Cause Mortality.
A, The x-axis is a log scale. Data are shown as hazard ratios with 95% CIs. Model 1 is adjusted for age and wear time. Model 2 is adjusted for Model 1 variables plus smoking status; alcohol use; intakes of saturated fat, fiber, fruits, and vegetables; hormone therapy; parental history of myocardial infarction; family history of cancer; general health; history of cardiovascular disease; history of cancer; and cancer screening. B, The y-axis is a log scale with the shaded area representing 95% CIs (linear trend, P < .001; nonlinear trend, P < .001). The reference group is 2000 steps/d. Model is adjusted for age; wear time; smoking status; alcohol use; intakes of saturated fat, fiber, fruits, and vegetables; hormone therapy; parental history of myocardial infarction; family history of cancer; general health; history of cardiovascular disease; history of cancer; cancer screening.
In sensitivity analyses to minimize reverse causation bias, the results led to similar conclusions (eTables 1, 2, and 3 in the Supplement). For example, excluding the first year of follow-up and women with CVD, cancer, and diabetes, the Model 2 HR for the highest quartile of steps per day was 0.50 (95% CI, 0.32-0.78). Restricting analyses only to women reporting excellent/good health, the corresponding HR was 0.44 (95% CI, 0.31-0.62), and when including only women with a BMI of 18.5 kg/m2 or greater, the corresponding HR was 0.43 (95% CI, 0.30-0.60).
Table 4 shows results for measures of stepping intensity and all-cause mortality. For all measures, there were strong inverse associations. After adjusting for potential confounders (Model 2), comparing the highest with lowest quartiles of peak 1-minute and 30-minute cadences, maximum 5-minute cadence, and time spent at stepping rate of 40 steps/min or greater, the HRs were 0.53, 0.47, 0.50, and 0.52, respectively (P < 0.01). All quartile measures were highly correlated with steps per day (Spearman correlation, r = 0.80, 0.88, 0.81, and 0.91, respectively; P < .001); therefore, the findings may have reflected associations with steps per day. When we adjusted additionally for steps per day, all associations were attenuated, and most were no longer significant (highest vs lowest quartile for peak 1-minute cadence, HR = 0.87 [95% CI, 0.68-1.11]; peak 30-minute cadence, HR = 0.86 [95% CI, 0.65-1.13]; maximum 5-minute cadence, HR = 0.80 [95% CI, 0.62-1.05]; and time spent at stepping rate of ≥40 steps/min, HR = 1.27 [95% CI, 0.96-1.68]; P > .05).
Table 4. Hazard Ratios and 95% CIs for All-Cause Mortality by Stepping Intensity.
| Stepping Measurea | No. of Cases | No. of Women | Hazard Ratio (95% CI)b | ||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 4 (Adjusted for Steps/d) | |||
| Peak 1-min Cadence | |||||
| Quartile 1 (lowest) | 263 | 4197 | [Reference] | [Reference] | [Reference] |
| Quartile 2 | 98 | 4178 | 0.50 (0.39-0.63) | 0.60 (0.47-0.77) | 0.77 (0.60-0.98) |
| Quartile 3 | 81 | 4168 | 0.46 (0.35-0.59) | 0.59 (0.45-0.76) | 0.69 (0.53-0.90) |
| Quartile 4 (highest) | 62 | 4198 | 0.40 (0.30-0.53) | 0.53 (0.39-0.72) | 0.87 (0.68-1.11) |
| P value for trend | <.01 | <.01 | .12 | ||
| Peak 30-min Cadence | |||||
| Quartile 1 (lowest) | 272 | 4185 | [Reference] | [Reference] | [Reference] |
| Quartile 2 | 93 | 4185 | 0.46 (0.36-0.59) | 0.56 (0.43-0.71) | 0.83 (0.66-1.04) |
| Quartile 3 | 81 | 4186 | 0.46 (0.36-0.60) | 0.58 (0.45-0.76) | 0.82 (0.64-1.06) |
| Quartile 4 (highest) | 58 | 4185 | 0.36 (0.27-0.48) | 0.47 (0.34-0.64) | 0.86 (0.65-1.13) |
| P value for trend | <.01 | <.01 | .19 | ||
| Maximum 5-min Cadence | |||||
| Quartile 1 (lowest) | 263 | 4185 | [Reference] | [Reference] | [Reference] |
| Quartile 2 | 97 | 4185 | 0.50 (0.39-0.63) | 0.61 (0.48-0.78) | 0.72 (0.57-0.90) |
| Quartile 3 | 81 | 4184 | 0.47 (0.36-0.60) | 0.58 (0.44-0.75) | 0.75 (0.59-0.96) |
| Quartile 4 (highest) | 63 | 4187 | 0.38 (0.29-0.51) | 0.50 (0.37-0.67) | 0.80 (0.62-1.05) |
| P value for trend | <.01 | <.01 | .08 | ||
| Time Spent at Stepping Rate of ≥40 Steps/Min, % | |||||
| Quartile 1 (lowest) | 274 | 4185 | [Reference] | [Reference] | [Reference] |
| Quartile 2 | 86 | 4185 | 0.42 (0.33-0.54) | 0.50 (0.39-0.65) | 0.96 (0.72-1.28) |
| Quartile 3 | 82 | 4186 | 0.46 (0.36-0.60) | 0.58 (0.45-0.76) | 1.15 (0.87-1.52) |
| Quartile 4 (highest) | 62 | 4185 | 0.40 (0.30-0.53) | 0.52 (0.38-0.70) | 1.27 (0.96-1.68) |
| P value for trend | <.01 | <.01 | .03 | ||
Refer to Table 1 for definitions.
Model 1 is adjusted for age and wear time. Model 2 is adjusted for Model 1 variables plus smoking status; alcohol use; intakes of saturated fat, fiber, fruits, and vegetables; hormone therapy; parental history of myocardial infarction; family history of cancer; general health; history of cardiovascular disease; history of cancer; and cancer screening. Model 4 is adjusted for Model 2 variables plus steps per day.
Discussion
In this study of older women with a mean age of 72 years, we observed the second quartile of step volume distribution (approximately 4400 steps/d) to be associated with a 41% reduction in mortality rate compared with the lowest quartile (approximately 2700 steps/d). When analyzed in finer gradations using spline analysis, the dose-response curve was L-shaped and mirrored the curve seen in studies using self-reported physical activity but with larger risk reductions.32 We observed a steady decline in mortality rates with more steps accrued up to approximately 7500 steps/d, beyond which rates leveled. After accounting for number of steps taken, all stepping-intensity associations were attenuated with most becoming no longer significant, which suggests that step volume, rather than step intensity, may be more important in this population. There was little fast stepping among these older women (only 0.2% of time was spent at a stepping rate equivalent to walking at approximately 2.5 mph or faster). However, participants had comparable stepping intensity to other similarly aged samples (eg, peak 30-minute cadence was 58 steps/min in the WHS, 63 steps/min in community-dwelling, nondemented women aged 71 years,33 and 53 steps/min in National Health and Nutrition Examination Survey participants aged ≥70 years34).
The present study provides a unique contribution because there are few data on the association between steps and mortality. Many previous studies have examined walking in relation to health. A meta-analysis of walking intervention trials reported improvements in cardiovascular risk factors,35 while meta-analyses of observational studies found amounts of walking36 and faster pace19 (all self-reported) to be inversely related to mortality rates. Walking pace and stepping rate are related but not interchangeable measures; walking pace gauges intensity when walking purposefully (eg, for exercise or transportation), while stepping rate assesses overall best natural effort in a free-living environment.28 Additionally, walking pace in previous studies was self-reported.
In contrast to walking, there are few longitudinal studies of steps and clinical outcomes. The NAVIGATOR trial, which measured daily steps as part of its protocol, published findings from several observational analyses. NAVIGATOR is a completed randomized clinical trial that tested treatment of nateglinide and valsartan for reducing cardiovascular events among more than 9000 persons with impaired glucose tolerance or high cardiovascular risk worldwide over 6 years. At baseline and 12 months, participants wore a pedometer for 7 days and recorded their steps on a daily log. For every additional 2000 steps/d taken, risk of developing cardiovascular events decreased by 10%14, diabetes by 5.5%13, and metabolic syndrome risk score by 0.29 z score.11 Change in step counts over 12 months was inversely related to risk of cardiovascular events,14 and weakly and inversely related to 2-hour, but not fasting, glucose.12
For mortality, studies in Australia (n = 2576),15 Great Britain (n = 1655),17 and Japan (n = 419)16 noted higher step counts (pedometer or accelerometer assessed) to be associated with lower mortality rates during follow-up of 5 to 10 years. Among Australians, every 1000-step/d increment was associated with 6% risk reduction, and in British participants it was associated with a 14% risk reduction. In Japanese participants, only the most active quartile, with a mean of 10 241 steps/d, experienced a significant risk reduction; however, statistical power was limited.
Other studies have examined steps in relation to cardiometabolic markers. A Finnish 3-month walking intervention trial among 78 persons with abnormal oral glucose tolerance observed an average of 5576 steps/d (accelerometer assessed) in intervention participants vs 4434 steps/d in control participants, which yielded improvements in some cardiometabolic markers.10 A 5-year study of approximately 500 Australians observed a 13% decreased risk in the odds of developing dysglycemia for every 1000-step/d increment (pedometer assessed),8 and increases in step counts over 5 years related favorably to adiposity and insulin sensitivity.9
Current guidelines recommend 150 min/wk or more of moderate-intensity physical activity, such as brisk walking.37 When postmenopausal women with approximately 4600 steps/d at baseline underwent supervised walking over 6 months to achieve guideline levels, they accumulated approximately 16 400 steps/wk in their exercise sessions.38 This translates to approximately 2300 steps/d during exercise, if divided evenly over 7 days. Added to baseline levels, it suggests that approximately 7000 (4600 + 2300 = 6900) steps/d may be sufficient to achieve guideline levels.
We believe there a need for step data, even if there is a large body of research on walking, because in addition to not being identical constructs, steps are intuitively understood and, therefore, easily translated to clinical advice, wellness programs, public health recommendations, etc. Steps also are already measured by many using wearables or smartphones. Furthermore, steps can provide motivation: a review of exercise studies found that monitoring steps as part of an exercise intervention resulted in an increase of approximately 2200 steps/d.39
One issue that merits discussion is the validity of step counts. A recent study reported that in healthy individuals, step counts measured using the same device used in this study performed similarly, whether worn at the hip or ankle.40 In another study that compared the present study device with commercial devices, correlations were very high for step counts (Actigraph vs Fitbit Zip or Fitbit Charge [Fitbit, San Francisco, California]; Pearson correlation, r > 0.95), though absolute counts were underestimated (Actigraph, approximately 7400 steps/d; Fitbit Zip, approximately 8100 steps/d; and Fitbit Charge, approximately 8200 steps/d).41
A major strength of the present study is that it is substantially larger than previous studies. Accelerometers also capture step data continuously and store it in memory. Thus, WHS participants did not need to log their steps daily, which could have resulted in errors of transcription or misreporting, as well as missing data (eg, NAVIGATOR, the largest study to date, imputed 25%-45% of participant step data14). To our knowledge, this is also the first study to examine free-living stepping intensity and long-term health outcomes. We were able to control for many potential confounders, statistically minimizing bias to the extent possible in observational studies. Additionally, we conducted several sensitivity analyses to minimize bias from reverse causation; results from these analyses support the primary findings.
Limitations
Limitations of this study include its observational design. Although sensitivity analyses resulted in similar conclusions, reverse causation bias remains a possibility. Diet information was obtained at the start of the WHS and not at device wear. We only used a single assessment of steps; however, repeated assessments in a subgroup of participants showed good stability of steps over 2 to 3 years, with intraclass correlations of approximately 0.8.42 Findings may have reflected prior habitual stepping and associated healthy state. Only women who could walk outside of the home without assistance were eligible for participation, but we did not have detailed measures on disability or depression during device wear. Women in the WHS are primarily white, of higher socioeconomic status, and more active (mean, 5499 steps/d) than a national sample (women ≥60 years old had a mean of 4027 steps/d43). It is unclear whether our results apply to other populations who are less or more active (eg, Australians and Swiss nationals take approximately 9000-10 000 steps/d; Japanese persons, approximately 7000-7500 steps/d; the Old Order Amish, approximately 14 000-18 000 steps/d; and women accrue fewer daily steps than men43). Finally, only all-cause mortality was investigated. With longer follow-up and larger numbers of other clinical end points (eg, CVD and cancer), we will examine other health outcomes.
Conclusions
This large study of device-assessed steps and all-cause mortality among older women showed that an average of approximately 4400 steps/d was significantly associated with lower mortality rates compared with approximately 2700 steps/d. More steps per day accrued were associated with steady declines in mortality rates up to approximately 7500 steps/d, beyond which rates leveled. Number of steps, rather than stepping intensity, was the step metric consistently related to lower mortality rates. These findings may serve as encouragement to the many sedentary individuals for whom 10 000 steps/d pose an unattainable goal.
eTable 1. Hazard Ratios and 95% Confidence Intervals for All-Cause Mortality by Mean Steps per Day – Sensitivity analysis #1: excluding the first year of follow-up and women with prevalent cardiovascular disease, cancer or diabetes
eTable 2. Hazard Ratios and 95% Confidence Intervals for All-Cause Mortality by Mean Steps per Day – Sensitivity analysis #2: excluding women who self-reported their health as less than excellent/good
eTable 3. Hazard Ratios and 95% Confidence Intervals for All-Cause Mortality by Mean Steps per Day – Sensitivity analysis #3: excluding women with body mass index <18.5 kg/m2
References
- 1.International Data Corporation Worldwide quarterly wearables device tracker. Published June 21, 2017.
- 2.Althoff T, Sosič R, Hicks JL, King AC, Delp SL, Leskovec J. Large-scale physical activity data reveal worldwide activity inequality. Nature. 2017;547(7663):336-339. doi: 10.1038/nature23018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fitbit staff The magic of 10,000 steps. https://blog.fitbit.com/the-magic-of-10000-steps/. Published June 22, 2010. Accessed November 28, 2018.
- 4.Torjesen I. Sixty seconds on . . . exercise. BMJ. 2018;362:k3006. doi: 10.1136/bmj.k3006 [DOI] [PubMed] [Google Scholar]
- 5.Hatano Y. Prevalence and use of pedometer. Res J Walking. 1997;1(1):45-54. [Google Scholar]
- 6.Tudor-Locke C, Bassett DR Jr. How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004;34(1):1-8. doi: 10.2165/00007256-200434010-00001 [DOI] [PubMed] [Google Scholar]
- 7.Bassett DR Jr, Toth LP, LaMunion SR, Crouter SE. Step counting: a review of measurement considerations and health-related applications. Sports Med. 2017;47(7):1303-1315. doi: 10.1007/s40279-016-0663-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ponsonby AL, Sun C, Ukoumunne OC, et al. Objectively measured physical activity and the subsequent risk of incident dysglycemia: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2011;34(7):1497-1502. doi: 10.2337/dc10-2386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dwyer T, Ponsonby AL, Ukoumunne OC, et al. Association of change in daily step count over five years with insulin sensitivity and adiposity: population based cohort study. BMJ. 2011;342:c7249. doi: 10.1136/bmj.c7249 [DOI] [PubMed] [Google Scholar]
- 10.Herzig KH, Ahola R, Leppäluoto J, Jokelainen J, Jämsä T, Keinänen-Kiukaanniemi S. Light physical activity determined by a motion sensor decreases insulin resistance, improves lipid homeostasis and reduces visceral fat in high-risk subjects: PreDiabEx study RCT. Int J Obes (Lond). 2014;38(8):1089-1096. doi: 10.1038/ijo.2013.224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huffman KM, Sun JL, Thomas L, et al. Impact of baseline physical activity and diet behavior on metabolic syndrome in a pharmaceutical trial: results from NAVIGATOR. Metabolism. 2014;63(4):554-561. doi: 10.1016/j.metabol.2014.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yates T, Davies MJ, Haffner SM, et al. Physical activity as a determinant of fasting and 2-h post-challenge glucose: a prospective cohort analysis of the NAVIGATOR trial. Diabet Med. 2015;32(8):1090-1096. doi: 10.1111/dme.12762 [DOI] [PubMed] [Google Scholar]
- 13.Kraus WE, Yates T, Tuomilehto J, et al. Relationship between baseline physical activity assessed by pedometer count and new-onset diabetes in the NAVIGATOR trial. BMJ Open Diabetes Res Care. 2018;6(1):e000523. doi: 10.1136/bmjdrc-2018-000523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yates T, Haffner SM, Schulte PJ, et al. Association between change in daily ambulatory activity and cardiovascular events in people with impaired glucose tolerance (NAVIGATOR trial): a cohort analysis. Lancet. 2014;383(9922):1059-1066. doi: 10.1016/S0140-6736(13)62061-9 [DOI] [PubMed] [Google Scholar]
- 15.Dwyer T, Pezic A, Sun C, et al. Objectively measured daily steps and subsequent long term all-cause mortality: the Tasped Prospective Cohort Study. PLoS One. 2015;10(11):e0141274. doi: 10.1371/journal.pone.0141274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamamoto N, Miyazaki H, Shimada M, et al. Daily step count and all-cause mortality in a sample of Japanese elderly people: a cohort study. BMC Public Health. 2018;18(1):540. doi: 10.1186/s12889-018-5434-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jefferis BJ, Parsons TJ, Sartini C, et al. Objectively measured physical activity, sedentary behaviour and all-cause mortality in older men: does volume of activity matter more than pattern of accumulation? Br J Sports Med. 2018;bjsports-2017-098733. doi: 10.1136/bjsports-2017-098733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Physical Activity Guidelines Advisory Committee 2018. Physical activity guidelines advisory committee report. https://health.gov/paguidelines/second-edition/report/. Published February 2018. Accessed November 29, 2018.
- 19.Stamatakis E, Kelly P, Strain T, Murtagh EM, Ding D, Murphy MH. Self-rated walking pace and all-cause, cardiovascular disease and cancer mortality: individual participant pooled analysis of 50 225 walkers from 11 population British cohorts. Br J Sports Med. 2018;52(12):761-768. doi: 10.1136/bjsports-2017-098677 [DOI] [PubMed] [Google Scholar]
- 20.Wang H, Zhang YF, Xu LL, Jiang CM. Step rate–determined walking intensity and walking recommendation in Chinese young adults: a cross-sectional study. BMJ Open. 2013;3(1):e001801. doi: 10.1136/bmjopen-2012-001801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cook NR, Lee IM, Gaziano JM, et al. Low-dose aspirin in the primary prevention of cancer: the Women’s Health Study: a randomized controlled trial. JAMA. 2005;294(1):47-55. doi: 10.1001/jama.294.1.47 [DOI] [PubMed] [Google Scholar]
- 22.Lee I-M, Cook NR, Gaziano JM, et al. Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women’s Health Study: a randomized controlled trial. JAMA. 2005;294(1):56-65. doi: 10.1001/jama.294.1.56 [DOI] [PubMed] [Google Scholar]
- 23.Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352(13):1293-1304. doi: 10.1056/NEJMoa050613 [DOI] [PubMed] [Google Scholar]
- 24.Lee I-M, Shiroma EJ, Evenson KR, Kamada M, LaCroix AZ, Buring JE. Using devices to assess physical activity and sedentary behavior in a large cohort study: the Women’s Health Study. J Meas Phys Behav. 2018;1(2):60-69. doi: 10.1123/jmpb.2018-0005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357-364. doi: 10.1249/MSS.0b013e3181ed61a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi L, Ward SC, Schnelle JF, Buchowski MS. Assessment of wear/nonwear time classification algorithms for triaxial accelerometer. Med Sci Sports Exerc. 2012;44(10):2009-2016. doi: 10.1249/MSS.0b013e318258cb36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tudor-Locke C, Camhi SM, Troiano RP. A catalog of rules, variables, and definitions applied to accelerometer data in the National Health and Nutrition Examination Survey, 2003-2006. Prev Chronic Dis. 2012;9:E113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tudor-Locke C, Han H, Aguiar EJ, et al. How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. Br J Sports Med. 2018;52(12):776-788. doi: 10.1136/bjsports-2017-097628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shiroma EJ, Sesso HD, Moorthy MV, Buring JE, Lee I-M. Do moderate-intensity and vigorous-intensity physical activities reduce mortality rates to the same extent? J Am Heart Assoc. 2014;3(5):e000802. doi: 10.1161/JAHA.114.000802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29(9):1037-1057. [DOI] [PubMed] [Google Scholar]
- 31.Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124(1):17-27. doi: 10.1093/oxfordjournals.aje.a114366 [DOI] [PubMed] [Google Scholar]
- 32.Arem H, Moore SC, Patel A, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015;175(6):959-967. doi: 10.1001/jamainternmed.2015.0533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schuna JM Jr, Brouillette RM, Foil HC, Fontenot SL, Keller JN, Tudor-Locke C. Steps per day, peak cadence, body mass index, and age in community-dwelling older adults. Med Sci Sports Exerc. 2013;45(5):914-919. doi: 10.1249/MSS.0b013e31827e47ac [DOI] [PubMed] [Google Scholar]
- 34.Tudor-Locke C, Brashear MM, Katzmarzyk PT, Johnson WD. Peak stepping cadence in free-living adults: 2005-2006 NHANES. J Phys Act Health. 2012;9(8):1125-1129. doi: 10.1123/jpah.9.8.1125 [DOI] [PubMed] [Google Scholar]
- 35.Oja P, Kelly P, Murtagh EM, Murphy MH, Foster C, Titze S. Effects of frequency, intensity, duration and volume of walking interventions on CVD risk factors: a systematic review and meta-regression analysis of randomised controlled trials among inactive healthy adults. Br J Sports Med. 2018;52(12):769-775. doi: 10.1136/bjsports-2017-098558 [DOI] [PubMed] [Google Scholar]
- 36.Kelly P, Kahlmeier S, Götschi T, et al. Systematic review and meta-analysis of reduction in all-cause mortality from walking and cycling and shape of dose response relationship. Int J Behav Nutr Phys Act. 2014;11:132. doi: 10.1186/s12966-014-0132-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.US Department of Health and Human Services Physical activity guidelines for Americans, 2nd edition. https://health.gov/paguidelines/second-edition/pdf/Physical_Activity_Guidelines_2nd_edition.pdf. Published 2018. Accessed November 29, 2018.
- 38.Jordan AN, Jurca GM, Locke CT, Church TS, Blair SN. Pedometer indices for weekly physical activity recommendations in postmenopausal women. Med Sci Sports Exerc. 2005;37(9):1627-1632. doi: 10.1249/01.mss.0000177455.58960.aa [DOI] [PubMed] [Google Scholar]
- 39.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296-2304. doi: 10.1001/jama.298.19.2296 [DOI] [PubMed] [Google Scholar]
- 40.Campos C, DePaul VG, Knorr S, Wong JS, Mansfield A, Patterson KK. Validity of the ActiGraph activity monitor for individuals who walk slowly post-stroke. Top Stroke Rehabil. 2018;25(4):295-304. doi: 10.1080/10749357.2018.1446487 [DOI] [PubMed] [Google Scholar]
- 41.Toth LP, Park S, Springer CM, Feyerabend MD, Steeves JA, Bassett DR. Video-recorded validation of wearable step counters under free-living conditions. Med Sci Sports Exerc. 2018;50(6):1315-1322. doi: 10.1249/MSS.0000000000001569 [DOI] [PubMed] [Google Scholar]
- 42.Keadle SK, Shiroma EJ, Kamada M, Matthews CE, Harris TB, Lee I-M. Reproducibility of accelerometer-assessed physical activity and sedentary time. Am J Prev Med. 2017;52(4):541-548. doi: 10.1016/j.amepre.2016.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bassett DR Jr, Wyatt HR, Thompson H, Peters JC, Hill JO. Pedometer-measured physical activity and health behaviors in US adults. Med Sci Sports Exerc. 2010;42(10):1819-1825. doi: 10.1249/MSS.0b013e3181dc2e54 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Hazard Ratios and 95% Confidence Intervals for All-Cause Mortality by Mean Steps per Day – Sensitivity analysis #1: excluding the first year of follow-up and women with prevalent cardiovascular disease, cancer or diabetes
eTable 2. Hazard Ratios and 95% Confidence Intervals for All-Cause Mortality by Mean Steps per Day – Sensitivity analysis #2: excluding women who self-reported their health as less than excellent/good
eTable 3. Hazard Ratios and 95% Confidence Intervals for All-Cause Mortality by Mean Steps per Day – Sensitivity analysis #3: excluding women with body mass index <18.5 kg/m2