Abstract
This study explored potential gender and racial/ethnic disparities in overall health risk related to 24 health risk indicators selected across six domains: socioeconomic, health status and health care, lifestyle, nutritional, clinical, and environmental. Using the 2003–2006 National Health and Nutrition Examination Surveys (NHANES), it evaluated cross-sectional data for 5,024 adults in the United States. Logistic regression models were developed to estimate prevalence odds ratios (PORs) adjusted for smoking, health insurance status, and age. Analyses evaluated disparities associated with 24 indicator variables of health risk, comparing females to males and four racial/ethnic groups to non-Hispanic Whites. Non-Hispanic Blacks and Mexican Americans were at greater risk for at least 50% of the 24 health risk indicators, including measures of socioeconomic status, health risk behaviors, poor/fair self-reported health status, multiple nutritional and clinical indicators, and blood lead levels. This demonstrates that cumulative health risk is unevenly distributed across racial/ethnic groups. A similarly high percentage (46%) of the risk factors was observed in females. Females as compared to males were more likely to have lower income, lower blood calcium, poor/fair self-reported health, more poor mental health days/month, higher medication usage and hospitalizations, and higher serum levels of some clinical indicators and blood cadmium. This analysis of cumulative health risk is responsive to calls for broader-based, more integrated assessment of health disparities that can help inform community assessments and public health policy.
Keywords: health disparities, gender, race/ethnicity, cumulative health screening, determinates of health
INTRODUCTION
Public health research, policy, and practice literatures report substantial disparities in life expectancy, morbidity, health risk factors, and quality of life among segments of the population, as well as persistence of these disparities (Dominguez, 2008; Institute of Medicine, 2006b; Levine et al., 2001; Murray et al., 2006; Truman et al., 2011). Health inequalities are related to socioeconomic, environmental, nutritional, and lifestyle factors, and are reflected in unequal access to and quality of health care (Adler & Newman, 2002). The effectiveness of public health initiatives and interventions for identifying and reducing health disparities depends upon the appropriate analysis of how health inequalities are distributed across subgroups, yet little research has comprehensively analyzed how a broad range of health risk indicators, including socioeconomic, health status and health care, lifestyle, nutritional, clinical, and environmental health risks, are distributed by gender, race, and ethnicity.
Disease prevalence and health inequalities are often disproportionately distributed among minorities and low-income persons (Frieden, 2011). Higher income is continuously associated with longer life expectancy, and gaps in life expectancy between low- and high-income individuals increased from 2001 to 2014 (Chetty et al., 2016). African Americans have a lower life expectancy at birth compared to the White population due in part to diseases such as heart disease, cancer, and diabetes (Kochanek, Arias, & Anderson, 2013), though this life expectancy gap has narrowed in recent years (CDC, 2016). While national mortality rates have declined for both males and females, Kindig and Cheng (2013) show that female mortality rates increased from 1992–1996 to 2002–2006 in 43% of U.S. counties. Speculations on the causes of these partial reversals include the impact of tobacco usage by females, changing levels of obesity, and changes in a range of socio-economic factors. Poorer people and people of color are disproportionately exposed to environmental contaminants and air pollution, and have a higher prevalence of diseases influenced by air pollution (Frumkin, 2002). The causes of these differences are likely related to a wide range of physical, social, and environmental stressors or burdens.
This paper presents a cumulative assessment of health disparities across gender and race/ethnic groups in the U.S., with a focus on six domains of health risk: socioeconomic, health status and health care, lifestyle, nutritional, clinical, and environmental. It examines the extent to which pervasive and persistent gender and racial/ethnic differences remain after controlling for obesity, smoking, and health insurance status, factors known to substantially contribute to disease prevalence. In addition to lifestyle and clinical attributes regularly studied in relation to health outcomes, a particular focus was on evaluation of differences in early blood-based indicators of nutrition and disease and cumulative chemical exposure, factors rarely considered when using national health survey data to investigate overarching health disparities.
METHODS
This paper evaluates racial, ethnic, and gender disparities in the U.S. related to 24 health risk indicators. Physical, medical, laboratory clinical data, and participant data from questionnaires were extracted from the publically available National Health and Nutrition Examination Surveys (NHANES) data from survey years 2003–2004 and 2005–2006. NHANES assesses the health and nutritional status of adults and children in the U.S. and is administered by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention (CDC, 2003–2006). The target population for NHANES is the civilian, non-institutionalized U.S. population. Written informed consent is obtained from each subject. More information about data collection is available online, including information regarding NCHS Research Ethics Review Board approval (CDC, 2003–2006). Data on a broad array of subjective and objective respondent characteristics, including socioeconomic indicators, nutritional and clinical measures, and lifestyle factors, were obtained from interviewer administrated computer-assisted personal interviews and clinical visits conducted as part of the NHANES household interview and mobile examination center (CDC, 2003–2004, 2005–2006).
Study Population
The study population includes 5,042 twenty to fifty year old participants in the 2003–2006 NHANES that had non-missing data for age, smoking status, health insurance, and obesity, variables with close connections to health status used as controls throughout the analysis. These years were chosen because they are the most recent data releases that include measurements for all of the blood biomarkers of chemical exposure of interest in this analysis. Race/ethnicity was derived from responses to the NHANES questions on race and Hispanic origin. Participants who self-reported they were Hispanic of Mexican-American origin or ancestry were categorized as “Mexican-American;” those who self-reported being of other Hispanic origins or ancestries (e.g., Puerto Rican, Cuban, and Dominican) were categorized as “other Hispanic.” Those who self-reported being Black with no Hispanic origins or ancestries were categorized as “non-Hispanic Black.” Participants who self-reported being “other non-Hispanic,” including Asian, Native American, Pacific and Caribbean Islander, Alaska Native, and multiracial, were categorized as “other race/ethnicity.” Smoking status was determined using measured serum cotinine levels, a metabolite of nicotine that is widely used as a biomarker of exposure to tobacco and both active and secondhand tobacco smoke (Benowitz, 1996). Participants with cotinine ≥10 ng/mL were considered smokers for this analysis and those with cotinine <10 ng/mL were considered nonsmokers based on prior research on cotinine levels of smokers and non-smokers (Hukkanen, Jacob & Benowitz, 2005). Participants without cotinine measurements were categorized as nonsmokers if they reported on the NHANES questionnaire that they had never smoked 100 cigarettes in their lifetime. Participants with body mass index ≥30 were characterized as obese (CDC 2012). Participants were categorized as having health insurance if they responded, “yes” to the question, “Are you covered by health insurance or some other kind of health care plan?” This includes private and government health insurance coverage. The specific number of individuals in subsequent analyses varies because of non-response, missing data, or legitimate skips for the indicator variables discussed below.
Health Risk Indicator Variables
Health risk indicator variables were created for 24 participant characteristics across six domains. Variables were selected because of their salience for the domains of interest, and were designed to be representative of all possible variables that could be included in each domain. Domain 1 focused on socioeconomic status (SES), including respondents’ poverty-income ratio, high school education attainment, and whether they worried they would run out of food or could not afford balanced meals in the past year. Domain 2 focused on health status and health care factors, including self-reported health status, self-reported poor mental health, and hospitalization and prescription medication use in the last year. Domain 3 focused on lifestyle factors including hours spent watching TV and duration of moderate and vigorous monthly physical activity. Domain 4 focused on serum nutritional indicators, including calcium, Vitamin C, and Vitamin D levels (all below median levels). Domain 5 focused on clinical indicators of poor health or pre-disease status, including high blood pressure and serum levels of high-density lipoprotein (HDL) cholesterol (below 60), C-reactive protein (CRP; ≥1 mg/dL), glucose (above median), and glycohemoglobin (≥7%). Domain 6 focused on blood biomarkers of environmental exposures including lead, cadmium, mercury, benzene, and toluene.
Each participant was assigned a value of 1 or 0 for each indicator, with a value of 1 representing an indicator of a poorer health quality (e.g., CRP ≥1 mg/dl or watching television >3 hours per day). For indicators without a commonly used cut-off indicating greater health risk (e.g., serum vitamin D levels), we used the median value of the study participants to derive the indicator variables. The full set of characteristics and health indicators can be found in Table 1, which displays the frequency and weighted percent of the characteristics of the study participants and the indicators.
Table 1 –
Sociodemographic, lifestyle, and health characteristics of the study population (20 to 50 years)
| Weighted | ||
|---|---|---|
| N | Percenta (SE) | |
| Female (N=5,042) | ||
| Male | 2337 | 49.4 (0.6) |
| Female | 2705 | 50.6 (0.6) |
| Race/Ethnicity (N=5,042) | ||
| Mexican American | 1159 | 10.4 (1.2) |
| Other Hispanic | 200 | 4.1 (0.6) |
| Non-Hispanic White | 2274 | 67.1 (2.2) |
| Non-Hispanic Black | 1163 | 12.5 (1.4) |
| Other Race (including Multi-Racial) | 246 | 5.9 (0.6) |
| Obesity (N=5,042) | ||
| BMI <30 | 3333 | 67.8 (1.1) |
| BMI ≥30 | 1709 | 32.2 (1.1) |
| Smoking Status (N=5,042) | ||
| Nonsmoker | 3431 | 65.6 (1.3) |
| Smoker | 1611 | 34.4 (1.3) |
| Health Insurance (N=5,042) | ||
| None | 1511 | 24.4 (1.2) |
| Insured | 3531 | 75.6 (1.2) |
| Education (N=5,041) | ||
| < High School | 1200 | 16.0 (1.0) |
| ≥ High School | 3841 | 84.0 (1.0) |
| Family Poverty Income Ratio (N=4,839) | ||
| ≤ 2 | 2152 | 33.4 (1.5) |
| ≥ 2 | 2687 | 66.6 (1.5) |
| Worried would run out of foodb (N=4,937) | ||
| Often/Sometimes true | 1175 | 17.1 (0.9) |
| Never true/Screened out | 3762 | 82.9 (0.9) |
| Worried couldn’t afford balanced mealsb (N=4,934) | ||
| Often/Sometimes true | 789 | 11.9 (0.8) |
| Never true/Screened out | 4145 | 88.1 (0.8) |
| TV Watching (N=5,042) | ||
| < 3 hours per day | 3247 | 67.4 (1.0) |
| ≥ 3 per day | 1795 | 32.6 (1.0) |
| Moderate Activity (N=5,042) | ||
| < 10 minutes | 2198 | 38.2 (1.3) |
| ≥ 10 minutes | 2844 | 61.8 (1.3) |
| Vigorous Activity (N=5,042) | ||
| < 10 minutes | 3129 | 58.4 (1.1) |
| ≥ 10 minutes | 1913 | 41.6 (1.1) |
| Self-reported health status (N=5,042) | ||
| Good/Very Good/Excellent | 4203 | 86.9 (0.7) |
| Poor/fair | 834 | 13.1 (0.7) |
| Mental Health (N=4,582) | ||
| ≥ 1 day with poor mental health | 1852 | 42.2 (1.0) |
| No days | 2730 | 57.8 (1.0) |
| Medication Usec (N=5,036) | ||
| Rx in past 12 months | 1847 | 42.7 (0.9) |
| None | 3189 | 57.3 (0.9) |
| Hospitalizations (N=5,042) | ||
| 1 or more in past 12 months | 476 | 8.3 (0.4) |
| None | 4566 | 91.7 (0.4) |
| Blood Pressured (N=4,784) | ||
| High BP (diastolic ≥90 or systolic ≥140) | 492 | 10.8 (0.5) |
| Low BP | 4292 | 89.2 (0.5) |
| HDL (N=4,815) | ||
| < 60 mg/dL | 3252 | 70.0 (0.9) |
| ≥ 60 mg/dL | 1563 | 30.0 (0.9) |
| CRP (n=4,822) | ||
| ≥ 1 mg/dL | 551 | 9.7 (0.4) |
| < 1 mg/dL | 4271 | 90.3 (0.4) |
| Glycohemoglobin (N=4,828) | ||
| < 7% | 4709 | 97.8 (0.2) |
| ≥ 7% | 119 | 2.2 (0.2) |
Data Analysis
Multivariable logistic regression models were developed to estimate prevalence odds ratios (PORs) for the 24 poor health indicator variables with race/ethnicity and gender, adjusting for age, smoking status, and health insurance status. All analyses were carried out using SAS 9.3 and incorporated appropriate NHANES sampling weights. The stratification and clustering design variables were used in the logistic regression models to obtain proper standard errors of the estimates.
RESULTS
The study population consisted of 5,042 twenty to fifty year old 2003–2006 NHANES participants that had non-missing data for smoking status, health insurance status, and obesity. Table 1 presents descriptive statistics of categorical variables, and Table 2 presents descriptive statistics of continuous variables, all weighted for population characteristics of the NHANES sample. Study participants had a median age of 35, and 51% were female. The majority of the participants were non-Hispanic White (67%), while 10% were Mexican American, 4% were other Hispanic, 13% were non-Hispanic Black, and 6% were other race/ethnicity. Approximately one-third of the participants were classified as obese (32%), one-third were smokers (34%), and one-quarter lacked health insurance (24%).
Table 2 –
Distribution of continuous variables of interest in the study population (20 to 50 years)
| Participant Characteristic | Arithmetic Mean (SE) | Geometric Mean (95% CI) | Median | IQR | 5th, 95th percentile | LOD | % below LOD |
|---|---|---|---|---|---|---|---|
| Age (years) | 35.3 (0.22) | 34.1 (33.7,34.5) | 35.1 | 15.6 | 20.5, 48.4 | ||
| Nutritional/Clinical Indicators | |||||||
| BMI | 28.2 (0.17) | 27.5 (27.2,27.7) | 26.9 | 8.1 | 19.6, 40.5 | ||
| Total calcium (mg/dL) | 9.51 (0.01) | 9.51 (9.49,9.52) | 9.46 | 0.45 | 8.92, 10.00 | 2 | 0 |
| Vitamin C (mg/dL) | 0.89 (0.02) | 0.7 (0.7,0.8) | 0.90 | 0.63 | 0.15, 1.64 | 0.012 | 0 |
| Vitamin D (ng/mL) | 23.6 (0.40) | 21.6 (20.8,22.3) | 22.5 | 11.9 | 8.5, 39.2 | 5 | 0.21 |
| Systolic BP (mm Hg) | 117.8 (0.32) | 117.0 (116.5,117.5) | 115.6 | 17.2 | 96.0, 141.3 | ||
| Diastolic BP (mm Hg) | 71.1 (0.29) | 70.2 (69.7,70.7) | 70.0 | 15.3 | 51.0, 90.0 | ||
| HDL-Cholesterol (mg/dL) | 53.4 (0.33) | 51.3 (50.7,51.8) | 50.3 | 20.7 | 32.0, 82.1 | a | |
| CRP (mg/dL) | 0.41 (0.02) | 0.17 (0.16,0.18) | 0.17 | 0.36 | 0.02, 1.48 | 0.02 | 2.8 |
| Glucose, serum (mg/dL) | 92.2 (0.37) | 90.3 (89.8,90.8) | 88.0 | 12.7 | 73.4, 115.7 | 3 | 0 |
| Glycohemoglobin (%) | 5.3 (0.01) | 5.3 (5.2,5.3) | 5.2 | 0.4 | 4.6, 5.9 | ||
| Environmental Exposure | |||||||
| Serum Cotinine (ng/ml) | 75.8 (4.02) | 0.88 (0.69,1.12) | 0.15 | 109 | 0.01, 372.7 | 0.015 | 21.7 |
| Blood Lead (μg/dL) | 1.52 (0.03) | 1.22 (1.19,1.26) | 1.19 | 1.00 | 0.49, 3.59 | 0.3, 0.25 | 0.4 |
| Blood Cadmium (μg/L) | 0.52 (0.01) | 0.34 (0.33,0.35) | 0.30 | 0.45 | 0.10, 1.70 | 0.14, 0.2 | 34.7 |
| Blood Mercury, total (μg/L) | 1.60 (0.06) | 0.97 (0.90,1.04) | 0.93 | 1.31 | 0.20, 5.09 | 0.2, 0.33 | 7.6 |
| Blood Benzene (ng/mL) | 0.08 (0.004) | 0.04 (0.037,0.043) | 0.03 | 0.05 | 0.02, 0.31 | 0.024 | 57.2 |
| Blood Toluene (ng/mL) | 0.27 (0.02) | 0.13 (0.12,0.14) | 0.11 | 0.17 | 0.03, 0.79 | 0.025 | 4.4 |
IQR, interquartile range; LOD, limit of detection; BMI, body mass index; CRP, C-reactive protein
The detection limit for HDL is not found in the NHANES laboratory method for HDL.
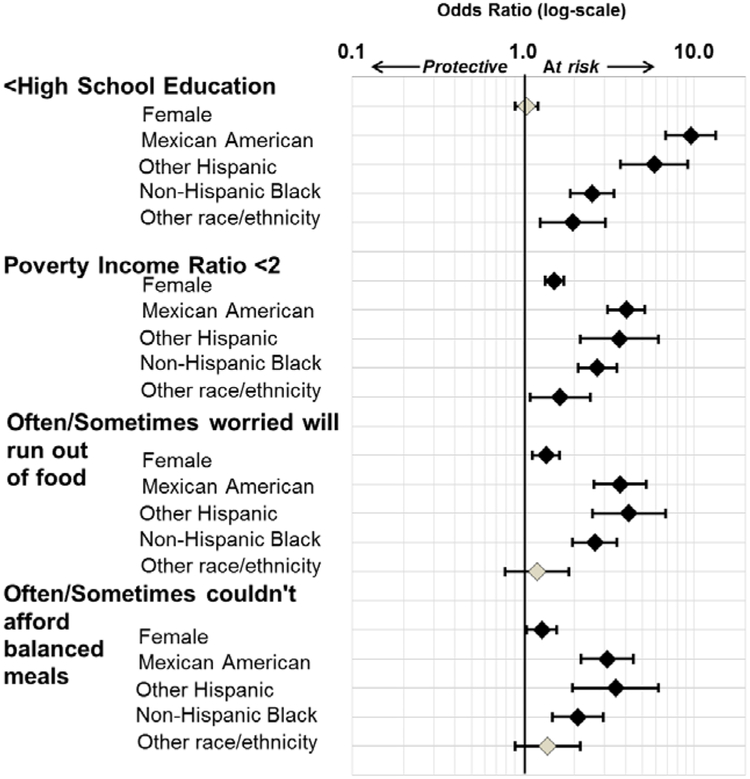
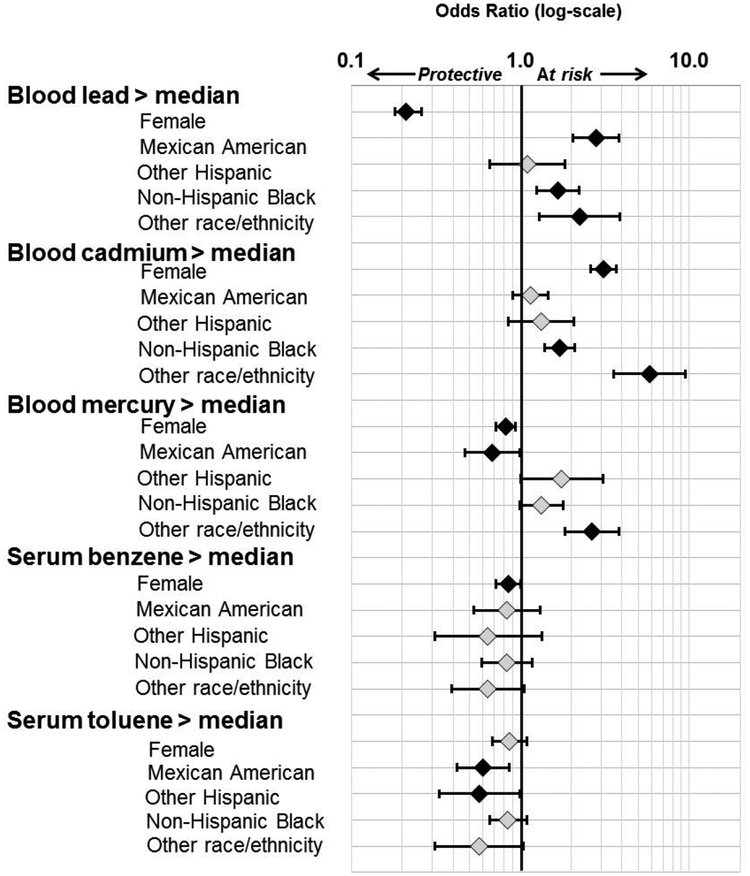
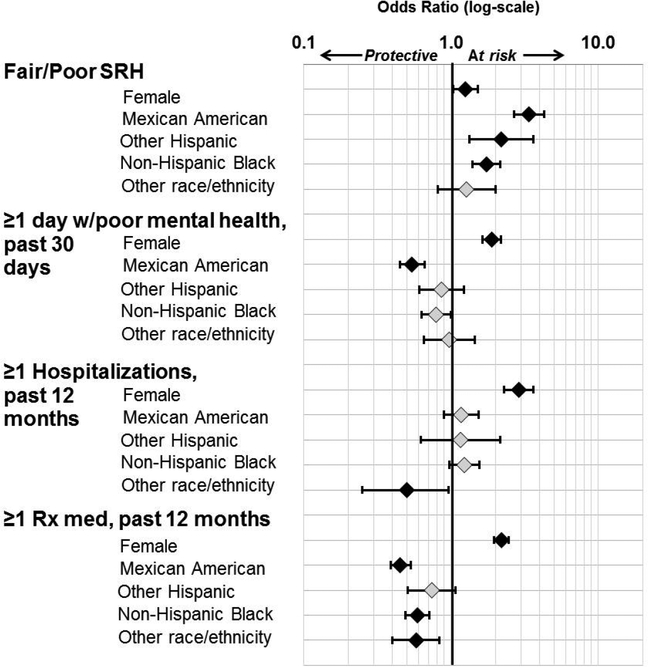
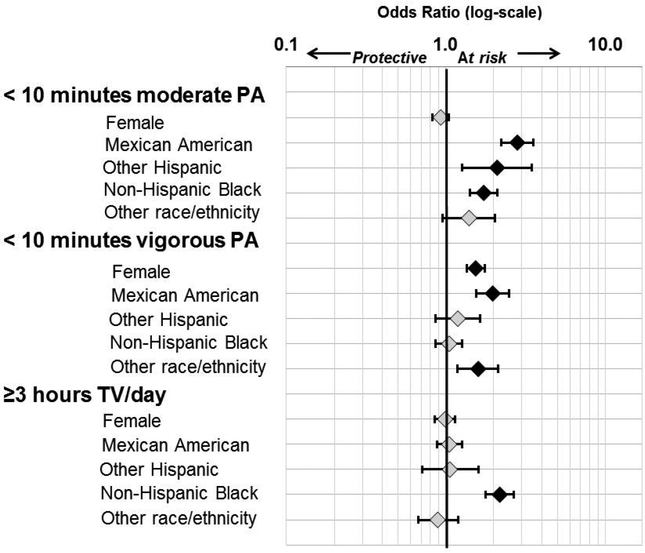
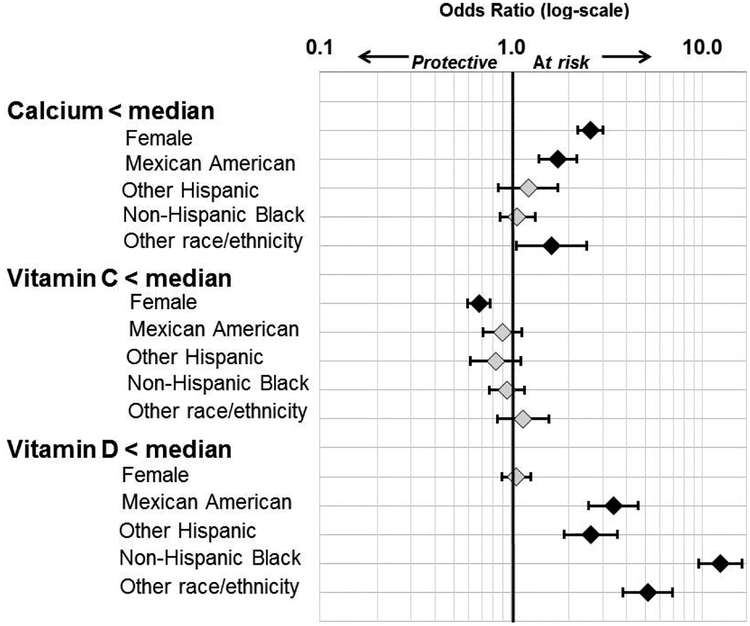
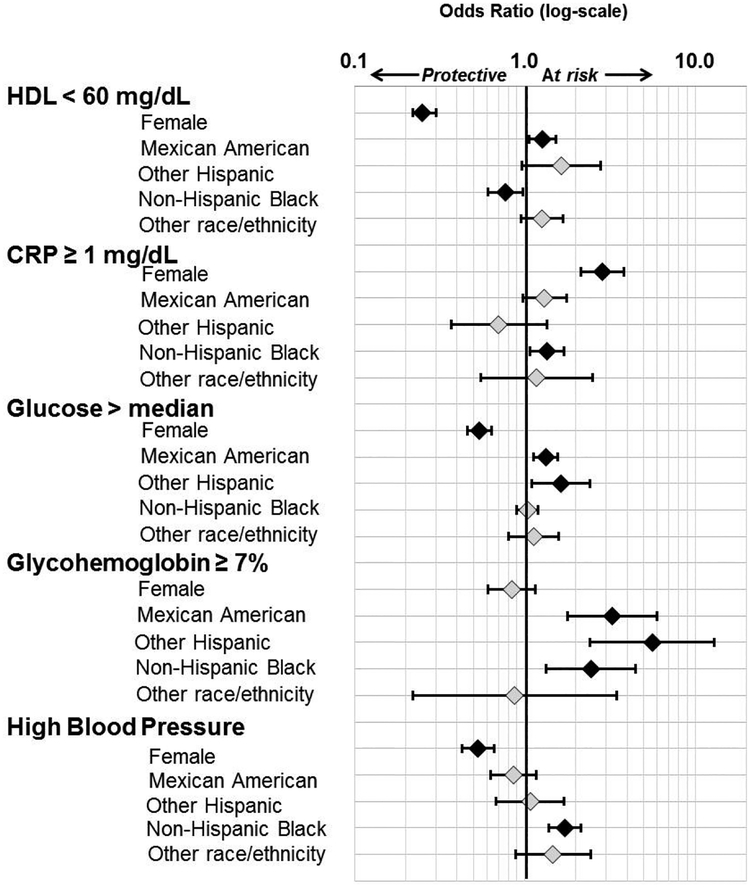
Figures 1 through 6 correspond to these six domains of health risk indicators and present PORs by gender and race/ethnicity. All PORs are adjusted for age, obesity, smoking status, and health insurance status, factors known to influence health risks.
FIGURE 1.
Prevalence odds ratios and 95% CI for socioeconomic indicators for gender (adjusted for race/ethnicity, age, smoking, obesity, and health insurance status) or race/ethnicity (adjusted for gender, age, smoking, obesity, and health insurance status). Female compared to male; racial/ethnic groups compared to non-Hispanic White. Black fill indicates significant at p<0.05.
FIGURE 6.
Prevalence odds ratios and 95% CI for socioeconomic indicators for gender (adjusted for race/ethnicity, age, smoking, obesity, and health insurance status) or race/ethnicity (adjusted for gender, age, smoking, obesity, and health insurance status). Female compared to male; racial/ethnic groups compared to non-Hispanic White. Black fill indicates significant at p<0.05.
Health Risks and Race/Ethnicity
SES:
Significant disparities existed across racial/ethnic groups in terms of socioeconomic status, food security, and lifestyle variables (Figure 1). Compared to non-Hispanic Whites, all racial/ethnic groups had lower incomes and were less likely to have graduated from high school. These associations were strongest with Mexican Americans and other Hispanic participants, with Mexican Americans nearly 10 times as likely as non-Hispanic Whites to have less than a high school education (POR 9.58 [95%CI: 6.82, 13.46]). Food security concerns were also elevated. Mexican American, other Hispanic, and Non-Hispanic Black participants were significantly more likely than non-Hispanic Whites to indicate that they often or sometimes worried they would run out of food.
Health Status and Health Care:
The likelihood of a poor or fair self-report of health was significantly higher for Mexican Americans, other Hispanics, and Non-Hispanic Blacks compared to non-Hispanic Whites (Figure 2). Mexican Americans, non-Hispanic Blacks, and those of other races were less likely to use prescription medication in the past year than non-Hispanic Whites (POR: 0.45 [95% CI: 0.39, 0.53], POR: 0.59 [95% CI: 0.49, 0.71], POR: 0.58, [95% CI: 0.40, 0.83], respectively).
FIGURE 2.
Prevalence odds ratios and 95% CI for socioeconomic indicators for gender (adjusted for race/ethnicity, age, smoking, obesity, and health insurance status) or race/ethnicity (adjusted for gender, age, smoking, obesity, and health insurance status). Female compared to male; racial/ethnic groups compared to non-Hispanic White. Black fill indicates significant at p<0.05.
Lifestyle:
Some racial/ethnic differences were observed regarding lifestyle indicators (Figure 3). Non-Hispanic Black participants were more likely than non-Hispanic Whites to watch more than three hours of TV per day, and Mexican Americans and those of other races were less likely to engage in physical activity.
FIGURE 3.
Prevalence odds ratios and 95% CI for socioeconomic indicators for gender (adjusted for race/ethnicity, age, smoking, obesity, and health insurance status) or race/ethnicity (adjusted for gender, age, smoking, obesity, and health insurance status). Female compared to male; racial/ethnic groups compared to non-Hispanic White. Black fill indicates significant at p<0.05.
Clinical and Nutrition:
Many health risk indicators of clinical health and nutrition were elevated for non-Hispanic Blacks, Mexican Americans, and those of other races (Figures 4 and 5). Mexican Americans were more likely than non-Hispanic Whites to have lower levels of serum calcium, lower levels of HDL cholesterol, and elevated serum glucose and glycohemoglobin levels. Non-Hispanic Blacks were more likely to have high blood pressure (POR: 1.72 [95% CI: 1.38, 2.14]), higher CRP levels (POR: 1.35 [95% CI: 1.07, 1.70]) and lower vitamin D levels compared to non-Hispanic Whites. The association with less than the median level of vitamin D is most pronounced in non-Hispanic Blacks, with a POR of 12.36 (95% CI: 9.54, 16.01). For vitamin C, no statistically significant differences were seen between the four racial/ethnic groups and the reference group.
FIGURE 4.
Prevalence odds ratios and 95% CI for socioeconomic indicators for gender (adjusted for race/ethnicity, age, smoking, obesity, and health insurance status) or race/ethnicity (adjusted for gender, age, smoking, obesity, and health insurance status). Female compared to male; racial/ethnic groups compared to non-Hispanic White. Black fill indicates significant at p<0.05.
FIGURE 5.
Prevalence odds ratios and 95% CI for socioeconomic indicators for gender (adjusted for race/ethnicity, age, smoking, obesity, and health insurance status) or race/ethnicity (adjusted for gender, age, smoking, obesity, and health insurance status). Female compared to male; racial/ethnic groups compared to non-Hispanic White. Black fill indicates significant at p<0.05.
Environmental Chemicals:
Mexican Americans, non-Hispanic Blacks, and those of other races were more likely to have higher blood lead levels compared to non-Hispanic Whites (Figure 6). Non-Hispanic Blacks and those of other race were more likely to have higher blood cadmium levels compared to non-Hispanic Whites. Those of other race also had blood mercury levels above the median. No statistically significant racial differences were observed in blood benzene levels. All racial/ethnic groups other than non-Hispanic Whites were less likely to have blood toluene levels above the median when compared to non-Hispanic Whites, with Mexican Americans and other Hispanics having statistically significant lower PORs (0.60 [95% CI: 0.42, 0.86] and 0.57 [95% CI: 0.33, 0.99], respectively).
Gender
Non-chemical health risk indicators:
Females were at higher risk for multiple indicators of poor health (Figures 1–5). Relative to males, females were significantly more likely to report lower income levels, have poor/fair SRH, and engage in lower levels of physical activity. Compared to males, females were more likely to have used prescription medication or been hospitalized in the past year. Females also had more days of poor mental health, lower serum calcium levels, and higher CRP levels than males. However, females were less likely than males to have high blood pressure, higher levels of HDL (good cholesterol), higher levels of serum vitamin C, and lower levels of serum glucose and glycohemoglobin levels that equaled or exceeded 7%.
Environmental Chemicals:
Females compared to males had significantly higher levels of blood cadmium (Figure 6). In contrast, females had lower blood lead, mercury, and benzene levels compared to males.
DISCUSSION
Studies suggest that health and environmental inequalities are the result of both social attributes (e.g., income, education, and health care access) and individual behaviors (e.g., smoking, obesity, and physical activity) (Adler & Newman, 2002; Dubowitz et al., 2008; Institute of Medicine, 2006a; Kant & Graubard, 2007). Stark racial/ethnic disparities in morbidity and mortality have persisted for many decades (CDC; Dominguez, 2008; Flores, Escala, & Hall, 2015; Institute of Medicine, 2012). In this analysis of a representative sample of the U.S. population, we identified numerous racial/ethnic and gender differences across all six domains investigated. Some of these health risk factors are modifiable and can be improved through changes in lifestyle or environment. For example, Case and Deaton (2015) attributed increases in morbidity and mortality among U.S. non-Hispanic White men ages 45–54 to drug and alcohol poisoning, suicide, and liver diseases. This underscores the need for more targeted public health communication and public health interventions that can reduce inequalities related to disease outcomes rather than waiting for diseases to emerge. Other health risk factors reflect systematic inequalities related to environmental exposures and access to health care. The ability to achieve health equity is often hampered by poverty and education, but also by numerous aspects of the social structure (Koh, Piotrowski, Kumanyika, & Fielding, 2011).
Current initiatives in public and community health support a focus on cumulative health risk assessment. For example, the Healthy People initiative tracks 26 health indicators across 12 domains (e.g., access to health care, clinical preventive services, environmental quality, tobacco use) (ODPHP). However, the majority of the indicators are not delineated by gender or race/ethnicity. Without these subgroup analyses, which often highlight disproportionate and/or cumulative impacts, community public health initiatives and interventions may be less effective.
In this study, we found gender and race/ethnicity disparities associated with lower income, lack of a high school education, food security concerns, and self-reported poor/fair health. Income and education level are inversely related to morbidity and mortality rates (Deaton, 2002), and high school graduation is a leading indicator of healthy adult behaviors and health status (Woolf & Braveman, 2011). Poor/fair self-reported health correlates with mortality rates (Idler & Benyamini, 1997) and is considered to reflect psychological aspects of health that take into consideration stress and well-being, important influences on health that are difficult to capture in laboratory or clinical assessments.
Lack of physical activity accounts for approximately 20% of coronary heart disease, colon cancer, and osteoporotic fractures, 12% of diabetes and hypertension, and 5% of breast cancer, with health care expenditures estimated at $24 billion a year (Lewis & Hennekens, 2015). In our study, females compared to males and Mexican Americans and other Hispanics compared to non-Hispanic Whites were less likely to exercise moderately or vigorously every month. Non-Hispanic Blacks watched significantly more television compared to any other race/ethnicity, which may, in part, reflect higher unemployment rates (Rhodes, Mark, & Temmel, 2012). Prior research has shown that minorities continue to face significant discrimination in employment (Pager, 2007; Pager & Shepherd, 2008).
Clinical and nutritional indicators also showed striking variation across race/ethnicity and gender. Non-Hispanic Blacks had high blood pressure even after controlling for obesity, smoking, and health insurance status, indicating increased risk for heart disease and stroke. Blood pressure is a potentially modifiable risk factor influenced by social, environmental, and lifestyle factors (Pickering, 1997). Approximately 50% of individuals in the U.S. took at least one prescription drug in the past month (CDC 2014). In the present study, females and non-Hispanic Whites (despite their lower prevalence of some diseases compared to males and some racial/ethnic groups) were shown to have significantly higher prescription drug use. There is a paucity of studies exploring the possible influences of life styles, social, and environmental factors on prescription drugs use, although such analyses may give insight into the differential impact of individual lifestyle factors including psychosocial and environmental influences, as well as how these patterns may be related to health care access and treatment.
Although measuring cumulative health risks is undeniably useful for community health assessment and health risk screening, few studies have investigated pre-disease clinical, nutritional, and environmental markers of health risk alongside of socioeconomic, lifestyle, and health status indicators. Consistent with other reports, we observed that Non-Hispanic Blacks and, to a lesser extent, Hispanic Americans have a markedly higher prevalence of low vitamin D levels (Ginde, Liu, & Camargo, 2009). Wintertime vitamin D insufficiency is pervasive among minority populations, most notably in non-Hispanic Blacks and Mexican Americans (Taksler, Cutler, Giovannucci, & Keating, 2015), but relatively little epidemiological and clinical research has been conducted with diverse populations (Robinson-Cohen et al., 2013). Nearly all non-Hispanic Blacks (97%) and most Mexican-Americans (90%) have vitamin D insufficiency (Ginde et al., 2009). Vitamin D insufficiency can lead to mild hyperparathyroidism, suboptimal calcium absorption, and reduced bone density (Chapuy et al., 1997) and is associated with cardiovascular disease (Beveridge & Witham, 2013) and diabetes mellitus (Palmer et al., 2008), though recent research suggests that low vitamin D levels are not associated with these same negative health risks in populations of color (Robinson-Cohen et al., 2013).
Mexican Americans, other Hispanics, and non-Hispanic Blacks were more likely to have elevated glycohemoglobin compared to non-Hispanic Whites. Glycohemoglobin levels at or above 7% correlate with increased diabetes risk. Mexican Americans were also more likely than non-Hispanic Whites to have high blood glucose levels, another indicator of diabetes risk. Diabetes is a condition known to have a higher prevalence in populations of color (Peek, Cargill, & Huang, 2007).
Similar to research by Nazmi and Victora (2007), this study found that females and non-Hispanic Blacks had higher levels of CRP, a general marker of inflammation and a risk factor for cardiovascular disease and mortality (Smith et al., 2004). Elevated CRP levels are also associated with smoking (O’Loughlin et al., 2008) and obesity (Visser, Bouter, McQuillan, Wener, & Harris, 1999). This study found differential CRP levels across racial/ethnic groups even after controlling for these risk factors. Numerous studies have observed racial and socioeconomic gradients in CRP levels (Nazmi & Victora, 2007). Paul et al. showed that CRP was a strong predictor of reported stressful life events in a non-pregnant cohort of women (Paul, Boutain, Agnew, Thomas, & Hitti, 2008). Alley and colleagues suggest that elevated CRP levels may in part reflect psychosocial factors such as lack of social support and other stress factors (Alley et al., 2006).
Cumulative health risk assessments by gender or race/ethnicity rarely include evaluation of blood levels for mercury, cadmium, or lead, despite these substances’ well-known toxic health effects in humans. Mexican Americans, non-Hispanic Blacks, and those of other race were more likely to have higher blood lead compared to non-Hispanic Whites. Participants of other races also had blood levels above the median level for mercury and cadmium. Males had higher blood levels of lead, mercury, and benzene compared to females. Choudhury et al. reported premenopausal females absorb 2–4 times more of ingested cadmium compared to males or postmenopausal females (Choudhury et al., 2001), perhaps explaining why blood cadmium levels were higher in females in our study. Public health strategies aimed at minimizing cadmium exposure in women of reproductive age are needed, especially based on recent finding that show correlations between elevated maternal blood cadmium and lower birth weight of off-spring (Vidal et al., 2015).
A limitation of this study is that NHANES provides only cross-sectional data, which does not allow for assessments of causality or changes over time for any variables. Our analysis also does not take into account geographic variation, though many health risks and exposure to chemicals are known to vary across the U.S. and between different types of communities (e.g., urban versus rural). Additionally, our analysis examines each health risk factor individually, though there is likely significant collinearity between them. In particular, our study is unable to distinguish the independent effects on cumulative health risks due to race/ethnicity from the effects of income. We restricted our analysis to 20–50 year olds because the elderly have significantly higher rates of some morbidities, and children and teens are undergoing rapid developmental changes. Thus, these results may not apply to individuals younger than 20 or older than 50. Subgroup analysis for two of the race/ethnicity groupings (other Hispanic and other race/ethnicity) combined racial and ethnic groups, thus limiting our ability to identify important race/ethnicity-specific differences.
CONCLUSION
In this analysis of a representative sample of the U.S. population, we identified numerous racial/ethnic and gender differences across indices related to domains that are potential upstream, modifiable determinants of health and wellbeing: SES, lifestyle, health status/care, nutritional, clinical, and markers of blood chemical exposure. Though we did not identify statistically significant differences across all variables in all domains, Non-Hispanic Blacks and Mexican Americans were at greater risk for at least 50% of the 24 health risk indicators. In contrast, non-Hispanic Whites were at greater health risk for only 20% of indicators when compared to Mexican Americans, 12% of indicators when compared to non-Hispanic Blacks, and 4% of indicators when compared to those of other race/ethnicity. Females were at greater risk than males for a high percentage (46%) of the health risk factors, while males were at greater risk for only 29% of the health risk indicators. This demonstrates that cumulative health risk is unevenly distributed across racial/ethnic groups and between sexes. Research on cumulative health disparities is essential for understanding and addressing those disparities (Institute of Medicine, 2006b).
Despite the many studies evaluating gender and racial/ethnic associations with morbidity and mortality rates, few studies examining gender and racial/ethnic inequality have comprehensively assessed health risk factors alongside of early biomarkers of exposure, laboratory-based blood indicators of disease risk, and cumulative health risk burden across multiple domains of health and well-being. Focusing on a wide range of indicators allows the cumulative impact of these disparities to become more evident. This type of analysis could be further extended to investigate local and regional differences in overall health risk. By identifying racial/ethnic groups at greatest risk at the national, regional, and community level, this type of broad-based, integrated cumulative risk assessment can be used to conduct more informative community assessments and inform public health policy decision-making, particularly community-participatory prevention efforts.
Contributor Information
Alissa Cordner, Whitman College.
Adrien A. Wilkie, Oak Ridge Institute for Science and Education,
Timothy J. Wade, U.S. Environmental Protection Agency
Edward E. Hudgens, U.S. Environmental Protection Agency
Rebecca J. Birch, Westat
Jane E. Gallagher, U.S. Environmental Protection Agency
REFERENCES
- Adler NE, & Newman K (2002). Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood), 21(2), 60–76. [DOI] [PubMed] [Google Scholar]
- Alley DE, Seeman TE, Ki Kim J, Karlamangla A, Hu P, & Crimmins EM (2006). Socioeconomic status and C-reactive protein levels in the US population: NHANES IV. Brain Behav Immun, 20(5), 498–504. doi: 10.1016/j.bbi.2005.10.003 [DOI] [PubMed] [Google Scholar]
- Benowitz NL (1996). Cotinine as a biomarker of environmental tobacco smoke exposure. Epidemiol Rev, 18(2), 188–204. [DOI] [PubMed] [Google Scholar]
- Beveridge LA, & Witham MD (2013). Vitamin D and the cardiovascular system. Osteoporos Int, 24(8), 2167–2180. doi: 10.1007/s00198-013-2281-1 [DOI] [PubMed] [Google Scholar]
- Case A, & Deaton A (2015). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A, 112(49), 15078–15083. doi: 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2003–2004). National Health and Nutrition Examination Suvery Questionnaire, Examination Protocol, and Laboratory Protocol. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Retrieved from http://wwwn.cdc.gov/nchs/nhanes/search/nhanes03_04.aspx. [Google Scholar]
- CDC. (2003–2006). National Health and Nutrition Examination Survey Data. Retrieved from http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm [Google Scholar]
- CDC. (2005–2006). National Health and Nutrition Examination Survey Questionnaire, Examination Protocol, and Laboratory Protocol. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Retrieved from http://wwwn.cdc.gov/nchs/nhanes/search/nhanes05_06.aspx. [Google Scholar]
- CDC. (2011) Fact Sheet -- CDC Health Disparities and Inequalities Report -- U.S., 2011. Retrieved from http://www.cdc.gov/minorityhealth/CHDIR/2011/FactSheet.pdf
- CDC. (2012). Defining Adult Overweight and Obesity. Retrieved from http://www.cdc.gov/obesity/adult/defining.html
- CDC. (2014). Therapeutic Drug Use. Retrieved from http://www.cdc.gov/nchs/fastats/drug-use-therapeutic.htm
- CDC. (2016). Health, United States, 2015: With special feature on racial and health disparities. Retrieved from Hyattsville, MD: http://www.cdc.gov/nchs/data/hus/hus15.pdf - specialfeature [PubMed] [Google Scholar]
- Chapuy MC, Preziosi P, Maamer M, Arnaud S, Galan P, Hercberg S, & Meunier PJ (1997). Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int, 7(5), 439–443. [DOI] [PubMed] [Google Scholar]
- Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, … Cutler D (2016). The Association Between Income and Life Expectancy in the United States, 2001–2014. Jama, 315(16), 1750–1766. doi: 10.1001/jama.2016.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choudhury H, Harvey T, Thayer WC, Lockwood TF, Stiteler WM, Goodrum PE, … Diamond GL (2001). Urinary cadmium elimination as a biomarker of exposure for evaluating a cadmium dietary exposure--biokinetics model. J Toxicol Environ Health A, 63(5), 321–350. doi: 10.1080/15287390152103643 [DOI] [PubMed] [Google Scholar]
- Deaton A (2002). Policy implications of the gradient of health and wealth. Health Aff (Millwood), 21(2), 13–30. [DOI] [PubMed] [Google Scholar]
- Dominguez TP (2008). Race, racism, and racial disparities in adverse birth outcomes. Clin Obstet Gynecol, 51(2), 360–370. doi: 10.1097/GRF.0b013e31816f28de [DOI] [PubMed] [Google Scholar]
- Dubowitz T, Heron M, Bird CE, Lurie N, Finch BK, Basurto-Davila R, … Escarce JJ (2008). Neighborhood socioeconomic status and fruit and vegetable intake among whites, blacks, and Mexican Americans in the United States. Am J Clin Nutr, 87(6), 1883–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores G, Escala MK, & Hall BG (2015). Dead wrong: the growing list of racial/ethnic disparities in childhood mortality. J Pediatr, 166(4), 790–793. doi: 10.1016/j.jpeds.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frieden TR (2011). Forward: CDC Health Disparities and Inequalities Report - United States, 2011. MMWR Surveill Summ, 60 Suppl, 1–2. [PubMed] [Google Scholar]
- Frumkin H (2002). Urban sprawl and public health. Public Health Rep, 117(3), 201–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginde AA, Liu MC, & Camargo CA Jr. (2009). Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Arch Intern Med, 169(6), 626–632. doi: 10.1001/archinternmed.2008.604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hukkanen J, Jacob P 3rd, & Benowitz NL (2005). Metabolism and disposition kinetics of nicotine. Pharmacol Rev, 57(1), 79–115. doi: 10.1124/pr.57.1.3 [DOI] [PubMed] [Google Scholar]
- Idler EL, & Benyamini Y (1997). Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav, 38(1), 21–37. [PubMed] [Google Scholar]
- Institute of Medicine. (2006a). Committee on Assessing Interactions Among Social, Behavioral, Genetic Factors in Health. The National Academies Collection: Reports funded by National Institutes of Health In Hernandez LM & Blazer DG (Eds.), Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. Washington (DC): National Academies Press (US) National Academy of Sciences. [Google Scholar]
- Institute of Medicine. (2006b). Committee on the Review Assessment of the NIH’s Strategic Research Plan Budget to Reduce and Ultimately Eliminate Health Disparities. The National Academies Collection: Reports funded by National Institutes of Health In Thomson GE, Mitchell F, & Williams MB (Eds.), Examining the Health Disparities Research Plan of the National Institutes of Health: Unfinished Business. Washington (DC): National Academies Press (US) National Academy of Sciences. [PubMed] [Google Scholar]
- Institute of Medicine. (2012). The National Academies Collection: Reports funded by National Institutes of Health How Far Have We Come in Reducing Health Disparities? Progress Since 2000: Workshop Summary. Washington (DC): National Academies Press (US) National Academy of Sciences. [PubMed] [Google Scholar]
- Kant AK, & Graubard BI (2007). Secular trends in the association of socio-economic position with self-reported dietary attributes and biomarkers in the US population: National Health and Nutrition Examination Survey (NHANES) 1971–1975 to NHANES 1999–2002. Public Health Nutr, 10(2), 158–167. doi: 10.1017/s1368980007246749 [DOI] [PubMed] [Google Scholar]
- Kindig DA, & Cheng ER (2013). Even as mortality fell in most US counties, female mortality nonetheless rose in 42.8 percent of counties from 1992 to 2006. Health Aff (Millwood), 32(3), 451–458. doi: 10.1377/hlthaff.2011.0892 [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Arias E, & Anderson RN (2013). How did cause of death contribute to racial differences in life expectancy in the United States in 2010? NCHS Data Brief(125), 1–8. [PubMed] [Google Scholar]
- Koh HK, Piotrowski JJ, Kumanyika S, & Fielding JE (2011). Healthy people: a 2020 vision for the social determinants approach. Health Educ Behav, 38(6), 551–557. doi: 10.1177/1090198111428646 [DOI] [PubMed] [Google Scholar]
- Levine RS, Foster JE, Fullilove RE, Fullilove MT, Briggs NC, Hull PC, … Hennekens CH (2001). Black-white inequalities in mortality and life expectancy, 1933–1999: implications for healthy people 2010. Public Health Rep, 116(5), 474–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis S, & Hennekens CH (2015). Regular Physical Activity: Forgotten Benefits. Am J Med. doi: 10.1016/j.amjmed.2015.07.016 [DOI] [PubMed] [Google Scholar]
- Murray CJ, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, & Ezzati M (2006). Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med, 3(9), e260. doi: 10.1371/journal.pmed.0030260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazmi A, & Victora CG (2007). Socioeconomic and racial/ethnic differentials of C-reactive protein levels: a systematic review of population-based studies. BMC Public Health, 7, 212. doi: 10.1186/1471-2458-7-212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Loughlin J, Lambert M, Karp I, McGrath J, Gray-Donald K, Barnett TA, … Paradis G (2008). Association between cigarette smoking and C-reactive protein in a representative, population-based sample of adolescents. Nicotine Tob Res, 10(3), 525–532. doi: 10.1080/14622200801901997 [DOI] [PubMed] [Google Scholar]
- ODPHP. Healthy People 2020 [Internet]. U.S. Department of Health and Human Services. Retrieved from http://www.healthypeople.gov/2020/leading-health-indicators/Healthy-People-2020-Leading-Health-Indicators%3A-Progress-Update
- Pager D (2007). The Use of Field Experiments for Studies of Employment Discrimination: Contributions, Critiques, and Directions for the Future. The Annals of the American Academy of Political and Social Science, 609, 104–133. [Google Scholar]
- Pager D, & Shepherd H (2008). The Sociology of Discrimination: Racial Discrimination in Employment, Housing, Credit, and Consumer Markets. Annu Rev Sociol, 34, 181–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer JR, Boggs DA, Krishnan S, Hu FB, Singer M, & Rosenberg L (2008). Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch Intern Med, 168(14), 1487–1492. doi: 10.1001/archinte.168.14.1487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul K, Boutain D, Agnew K, Thomas J, & Hitti J (2008). The relationship between racial identity, income, stress and C-reactive protein among parous women: implications for preterm birth disparity research. J Natl Med Assoc, 100(5), 540–546. [DOI] [PubMed] [Google Scholar]
- Peek ME, Cargill A, & Huang ES (2007). Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev, 64(5 Suppl), 101s–156s. doi: 10.1177/1077558707305409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering TG (1997). The effects of environmental and lifestyle factors on blood pressure and the intermediary role of the sympathetic nervous system. J Hum Hypertens, 11 Suppl 1, S9–18. [PubMed] [Google Scholar]
- Rhodes RE, Mark RS, & Temmel CP (2012). Adult sedentary behavior: a systematic review. Am J Prev Med, 42(3), e3–28. doi: 10.1016/j.amepre.2011.10.020 [DOI] [PubMed] [Google Scholar]
- Robinson-Cohen C, Hoofnagle AN, Ix JH, Sachs MC, Tracy RP, Siscovick DS, … de Boer IH (2013). Racial differences in the association of serum 25-hydroxyvitamin D concentration with coronary heart disease events. Jama, 310(2), 179–188. doi: 10.1001/jama.2013.7228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SC Jr., Anderson JL, Cannon RO 3rd, Fadl YY, Koenig W, Libby P, … Rosenson R (2004). CDC/AHA Workshop on Markers of Inflammation and Cardiovascular Disease: Application to Clinical and Public Health Practice: report from the clinical practice discussion group. Circulation, 110(25), e550–553. doi: 10.1161/01.cir.0000148981.71644.c7 [DOI] [PubMed] [Google Scholar]
- Taksler GB, Cutler DM, Giovannucci E, & Keating NL (2015). Vitamin D deficiency in minority populations. Public Health Nutr, 18(3), 379–391. doi: 10.1017/s1368980014000457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truman BI, Smith KC, Roy K, Chen Z, Moonesinghe R, Zhu J, … Zaza S (2011). Rationale for regular reporting on health disparities and inequalities - United States. MMWR Surveill Summ, 60 Suppl, 3–10. [PubMed] [Google Scholar]
- Vidal AC, Semenova V, Darrah T, Vengosh A, Huang Z, King K, … Hoyo C (2015). Maternal cadmium, iron and zinc levels, DNA methylation and birth weight. BMC Pharmacol Toxicol, 16, 20. doi: 10.1186/s40360-015-0020-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser M, Bouter LM, McQuillan GM, Wener MH, & Harris TB (1999). Elevated C-reactive protein levels in overweight and obese adults. Jama, 282(22), 2131–2135. [DOI] [PubMed] [Google Scholar]
- Woolf SH, & Braveman P (2011). Where health disparities begin: the role of social and economic determinants--and why current policies may make matters worse. Health Aff (Millwood), 30(10), 1852–1859. doi: 10.1377/hlthaff.2011.0685 [DOI] [PubMed] [Google Scholar]