Abstract
American Indian women are more likely to die from cardiovascular disease (CVD) than White or African American women. Inflammatory processes may underlie CVD disparities by gender and race and may be critical to understanding population-specific drivers and potential buffers. Exposure to environmental air pollutants, especially particulate matter (PM), is known to be an important catalyst in CVD-associated inflammation. Positive psychological states, associated with low levels of inflammatory gene expression, could serve to moderate the inflammatory response to environmental air pollutants and ultimately lead to better cardiovascular health outcomes. The aim of the ongoing community-engaged and NIH-funded study described in this research protocol is to address the racial and gender gaps in CVD mortality by investigating the contextually relevant and culturally important determinants of health among American Indian women. In this paper we describe the procedures used to examine the relationship between environmental air pollutant exposures (PM10–2.5 and PM2.5), psychological factors (e.g., depressive symptoms, posttraumatic stress symptoms, eudemonic well-being, positive emotions), and cardiovascular-associated inflammation (hs-CRP, IL-6, Amyloid A, CBCs with differentials) in a sample of 150 women 18 to 50 years of age from the Lumbee Tribe in southeastern NC. We describe lessons learned and strategies used in developing a community-engaged approach to enhance recruitment of American Indian women in biomedical research. The empirical data and community infrastructure resulting from this study will be foundational in designing and testing future interventions to reduce CVD-associated morbidity and mortality in American Indian women.
Keywords: inflammation, physiological states, women’s health, cultural research, environment, adulthood, design development, community-based participatory research
Background
Cardiovascular disease (CVD) is a severe health threat among American Indian women in North Carolina (NC; Hutchinson & Shin, 2014). CVD accounts for 21.9% of all deaths occurring among this group, making it the leading cause of death (Avery et al., 2016). There are geographic disparities within the state, with a significant clustering of high CVD mortality rates among American Indian women over 35 years of age in the southeastern region (Centers for Disease Control and Prevention, 2018; see Figure 1). County-level data specific to CVD mortality rates reflect a significant disparity pattern by race and sex. In Robeson County, which has the largest population of American Indians in NC, the 2008–2012 CVD mortality rate among women was highest for American Indians at 198.3 per 100,000 compared to African Americans and Whites at 165.7 and 168.8 per 100,000 respectively. In contrast, American Indian men have the lowest CVD mortality rate (255.8 per 100,000) compared to White (305.3 per 100,000) and African American men (302.7 per 100,000) in Robeson County, despite having higher rates than American Indian women (Robeson County Health Department, 2014). This subgroup comparison reveals sex-based differences and a glaring disparity in CVD mortality among American Indian women.
Figure1:
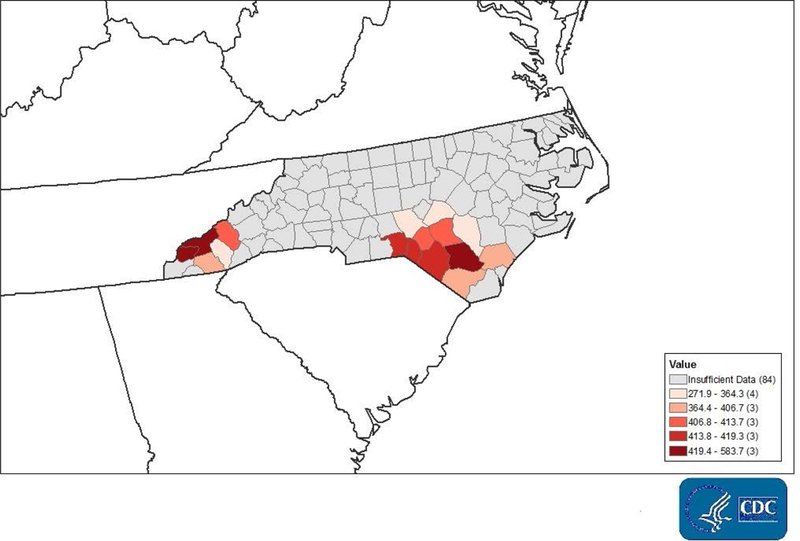
Total Cardiovascular Disease Death Rate per 100,000, 35+, American Indian and Alaskan Native, Women, 2014–2016.
Narrowing the racial and sex-based gaps in CVD mortality requires a paradigm shift in nursing research to widen the conceptual lens to examine broader social determinants that are of contextual relevance and cultural importance for cardiovascular health in Native North Carolinian women. Given the exceedingly high levels of environmental air pollutants in Robeson County, arising largely from agriculture, manufacturing, and the proximity to major interstates (e.g., Interstate 95), a focused effort is needed to uncover how this known – yet invisible – driver of CVD risk, morbidity and mortality is related to cardiovascular-associated inflammation in American Indian women (Community Health Needs Assessment, 2014; Hamanaka & Mutlu, 2018; Mannucci, Harari, Martinelli, & Franchini, 2015; Parker, Kravets, & Vaidyanathan, 2018). Particulate matter (PM), a composite of solid particles and liquid droplets suspended in air, is classified into two major categories: coarse particles (PM10–2.5) and fine particles (PM2.5) (Hamanaka & Mutlu, 2018). Particulate matter is closely linked to CVD, as reflected in a range of illness-relevant biomarkers, including C-reactive protein (CRP) and Interleukin-6 (IL-6), involved in systemic inflammation (Adams, Greenbaum, Shaikh, van Erp, & Russell, 2015; Du, Xu, Chu, Guo, & Wang, 2016; Pope et al., 2016; Tsai et al., 2012; Wu, Jin, & Carlsten, 2018). Nascent literature in positive psychology suggests that psychological factors (i.e., subjective well-being and mental health), hold potential to moderate inflammatory responses to environmental air pollutants, providing considerable promise as a future intervention focus (Fredrickson et al., 2015).
To understand more fully the interactive roles of environmental air pollutants and psychological factors in cardiovascular-associated inflammation among American Indian women, we designed a community-engaged research study based in Robeson County, NC. In the Hazardous Air Pollutants, Positivity, and Inflammation (HAPPI) Study, we are specifically exploring how PM and positive (and negative) psychological states are associated with cardiovascular-associated inflammatory markers and whether positive psychological states could moderate the inflammatory effects of environmental air pollutants in American Indian women. This research protocol paper has dual purposes: 1) to describe the procedures used in a community-engaged study funded by the NIH’s National Institute of Environmental Health Sciences, and 2) to describe strategies used to enhance recruitment of American Indian women in biomedical research.
Particulate Matter (PM) and Cardiovascular Disease
Chronic and acute exposure to PM, whose sources include industrial emissions, fossil fuel combustion, power generation, road traffic, and residential heating, has been linked to deleterious health effects, including increased cardiovascular disease risk and exacerbation of CVD (Hamanaka & Mutlu, 2018; Mannucci et al., 2015). Although the exact biological pathways underlying the cardiovascular health effects of PM inhalation remain largely debatable, both oxidative stress and systemic inflammation have been purported to play major independent, and interactive, roles (Hamanaka & Mutlu, 2018). Particulate matter-induced oxidative stress has been shown to activate the autonomic nervous system, producing a sympathetic response involving adverse physiological changes (e.g., hypertension and impaired heart rate variability [HRV]) which can compromise cardiovascular health (Hamanaka & Mutlu; 2018; Morishita, Thompson, & Brook, 2015). Ambient PM exposure has also been shown to be associated with an immunological response involving the release of proinflammatory cytokines, such as CRP, IL-6 (Du et al., 2016; Hamanaka & Mutlu, 2018; Ridker, Hennekens, Buring, & Rifai, 2000; Shrivastava, Singh, Raizada, & Singh, 2015), and other types of immune cells (e.g., white blood cells) circulating within the blood (Steenhof et al., 2014). Key biological markers, including CRP, Amyloid A, and IL-6, have been used as non-specific measures of inflammatory status in epidemiologic studies of CVD in women (Ridker et al., 2000; Shrivastava et al., 2015). Women appear to be more reactive to environmental air pollutants than men; in a review by Clougherty (2010), death from air pollution was better predicted among women than among men, possibly due to PM deposition patterns or sex differences in response to stress or exposure. These findings support the need to examine the effects of environmental air pollutants among women.
Psychological States, Environmental Air Pollutants, and Proinflammatory Gene Expression
Negative psychological states can exacerbate detrimental effects from exposure to environmental air pollutants (Hicken, Dvonch, Schulz, Mentz, & Max, 2014). The 2012–2017 National Institute of Environmental Health Sciences’ Strategic Plan and epidemiological researchers report links between both depression and lower socioeconomic status (SES) and increased adverse health effects from environmental air pollutant exposure (Gold & Mittleman, 2013; Hicken et al., 2013; Hicken, Dvonch, Schulz, Mentz, & Max, 2014). Connections among environmental air pollutants, negative psychological states, and inflammation may be mechanisms accounting for enhanced vulnerability to disease (see Figure 2).
Figure2:
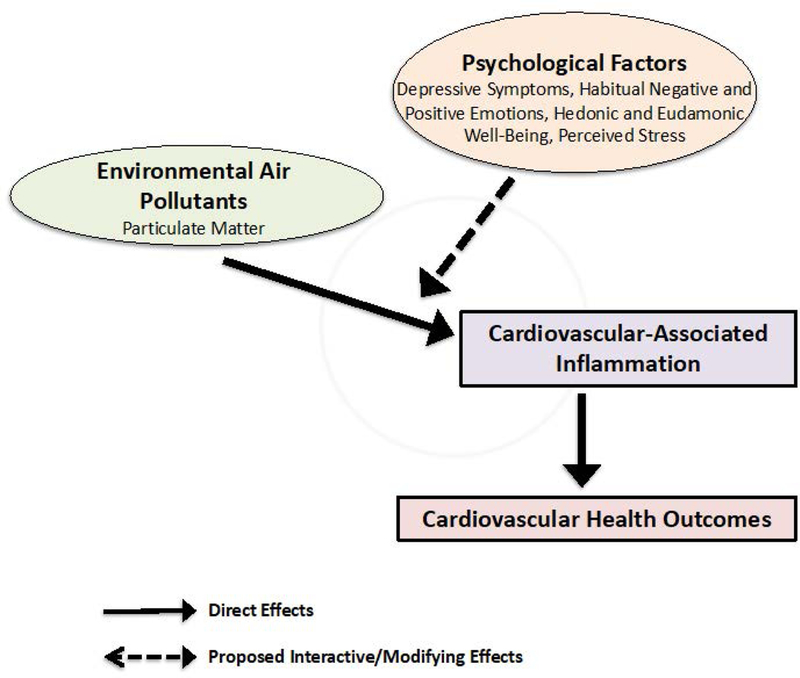
Conceptual Model for Enhanced Vulnerability to Adverse CVD Health Outcomes through Pathways Linking Environmental Pollutants and Psychological Factors to CVD-Associated Inflammation.
Although negative psychological states can intensify inflammatory responses to environmental air pollutants, less is known about how positive psychological states may moderate inflammatory responses to environmental air pollutants. Based on emerging evidence in social genomics, positive psychological states, specifically habitual positive emotions together with self-transcendent experiences (e.g., sense of purpose, positive social relations, contributing to one’s community; collectively termed “eudaimonic well-being”; Ryff, 2017) may alter the expression of proinflammatory cytokines (Fredrickson et al., 2013; Fredrickson et al., 2015). Indeed, researchers in a recent randomized controlled trial showed that an intervention based on acts of kindness both increases positive psychological states (Nelson, Layous, Cole, & Lyubomirsky, 2016) and decreases proinflammatory gene expression (Nelson et al., 2016; Nelson-Coffey, Fritz, Lyubomirsky, & Cole, 2017). There have been no published studies, however, designed to examine whether positive psychological states can moderate the adverse health effects of environmental air pollutants. The HAPPI Study described in this research protocol paper is designed to address this gap.
Purpose and Aims
In the HAPPI Study, we will examine the associations between PM and cardiovascular-associated inflammatory markers among American Indian women and test whether positive psychological states buffer (moderate) the inflammatory effects of PM in this population. We will address these specific aims:
1. Examine the associations between PM and cardiovascular-associated inflammatory markers in American Indian women.
We hypothesize that levels of PM (PM10–2.5 and PM2.5) will be positively associated with inflammatory marker levels (hs-CRP, IL-6, Amyloid A, CBCs with differentials) in American Indian women.
2. Examine the associations between psychological states and cardiovascular-associated inflammatory markers in American Indian women.
We hypothesize that inflammatory marker levels in American Indian women will be positivity associated with negative psychological states (e.g., negative emotions, depressive symptoms, posttraumatic stress symptoms, and perceived stress) and negatively associated with positive psychological states (e.g., eudemonic well-being, positive emotions, and positive affect).
3. Determine whether positive psychological states buffer (moderate) the association between PM and cardiovascular-associated inflammatory markers in American Indian women.
We hypothesize that among American Indian women with higher levels of positive psychological states the link between PM and inflammatory marker levels will be weaker.
Methods
Design
Using a community-engaged approach, we designed a correlational study to examine the inflammatory correlates of environmental and psychological variables among American Indian women ages 18 to 50 years. To enhance the community’s engagement in the research process, we organized a Community Partnership Committee (CPC) following our request for IRB approval and Tribal endorsement. Key community stakeholders who represented diverse professional backgrounds were considered with consultation from a cultural insider, who also joined the CPC. The CPC is comprised of six American Indian key stakeholders regarded as prominent healthcare providers, community members, or cultural experts in the Lumbee tribal community.
The CPC is designed to promote the open and equal exchange of information between the research team and community and affords active involvement of community members in all aspects of the research process to ensure responsiveness to community priorities. Using a shared decision-making model, CPC members provide oversight on (a) the cultural appropriateness of the study procedures and measures; (b) study protocols; (c) research methods; (d) sampling, recruitment, and retention strategies; and (e) interpretation and dissemination of findings (Balls-Berry & Acosta-Perez, 2017; Michener al., 2012). CPC members are invited to contribute as co-authors on manuscripts generated from this study, to be involved in the dissemination of information to the community, and to assist in the design of future studies. For attending quarterly, in-person meetings, CPC members are offered a $100 gift card (total of four gift cards annually) to offset expenses such as gas for travel. Compensation for community engagement has been supported through funds secured through the University of North Carolina at Chapel Hill.
To increase the community benefits from the study, we purposely utilize community-based resources and employ services from local Lumbee-owned businesses (e.g., printing) whenever possible. In a collaborative effort to design the study logo, we contracted with a local art professor and student at the University of North Carolina at Pembroke following the recommendation of a CPC member. The study logo design was an iterative process that involved the presentation of multiple drafts to the CPC that were critiqued for cultural congruence. Ultimately, the final study logo design (see Figure 3) featured elements of both the project and the Lumbee culture.
Figure3:
HAPPI Study Logo. Copyright 2018 by Jada L. Brooks and Jennifer M. Martinez. Reprinted with permission.
Setting
We are conducting the community-engaged study in Robeson County, NC. The racial and ethnic composition of Robeson County is diverse, with 51,646 American Indian residents (38.4%), 34,960 White residents (26%), 32,525 Black residents (24.2%), and 11,213 Latino residents (8.33%; Data United States of America [USA], 2018). The majority of Native residents identify as Lumbee Indian. With approximately 60,000 members, the Lumbee Tribe of NC is the largest American Indian population east of the Mississippi River and the ninth largest tribal group in the nation (United States Census Bureau, 2012). Although not designated a tribal land base by the United States federal government, according to historical records the Lumbee have been living in and around Robeson County since the early part of the eighteenth century. The Lumbee Tribe of NC has received recognition from the state of NC as an ethnically distinct group of American Indians. Data collection sites comprise one primary care and one urgent care clinic operated by Southeastern Health, a comprehensive healthcare system that operates over 40 primary care, specialty and urgent care clinics throughout Robeson and surrounding counties as well as the Southeastern Regional Medical Center.
Study Population
The sample includes women between 18 and 50 years of age who self-identify as Lumbee Indian and speak English. We do not include pregnant women because the expression of inflammatory markers may be increased during pregnancy (Robinson & Klein, 2012), which could interfere with the variables being measured. Other exclusion criteria are: (a) a history of chronic infections or immunodeficiency; (b) abnormal physical findings: temperature of >37.8° C; systolic BP > 150mm or < 85 mm Hg; or diastolic BP > 90 mm or < 50 mm Hg; (c) current mental illness or a history of drug or alcohol use that may interfere with the ability to comply with study requirements; and (d) immunosuppressive or anticoagulant medication use. Participants with an elevated temperature or blood pressure are referred to their health care provider for follow-up. In the case of a medical emergency, participants will be evaluated by medical staff at the clinic.
Sample Size
We performed power calculations to estimate the sample size needed to detect non-zero correlations between 1) PM exposure and inflammatory markers and 2) psychological states and inflammatory markers. A sample size of 150 participants provides 80% power to detect a non-zero correlation coefficient of ±0.23 or more. Regarding cases with missing data, even with a 20% rate of missing observations the resulting n = 120 provides 80% power to detect a correlation of ±0.25 or more. To test for a non-zero interaction between each psychological measure and each lagged (i.e., on days 1–3 prior to baseline) PM exposure measure, we will use multiple linear regression models and F tests (Erdfelder, Faul, Buchner, & Lang, 2009) with the interaction effect size measured by Cohen’s f2 (Selya, Rose, Dierker, Hedeker, & Mermelstein, 2012). A sample size of 150 participants yields approximately 80% power to detect a small effect size of 0.053 for the interaction between each psychological measure and PM exposure level. With a 20% rate of missing observations, the resulting n = 120 provides 80% power to detect an effect size of 0.067.
Human Subjects and Recruitment
We obtained tribal endorsement and approval from the University of North Carolina at Chapel Hill and Southeastern Health Institutional Review Boards. In a previous study (A Study to Help Manage Asthma in Children [ASTHMA-C Study]) conducted by the Principal Investigator (PI), 60 Lumbee women gave permission to be contacted about future studies. Eligible women from the ASTHMA-C registry were invited to participate in the HAPPI Study. We employed purposeful and snowball sampling methods to recruit additional women; participants were asked to refer eligible family members, friends, and peers to join the study. To identify potential participants, we also attended community events (e.g., Lumbee Homecoming and Pembroke Day) and displayed flyers and postcards in designated areas throughout the community (e.g., Southeastern Lifestyle Center of Pembroke), strategies recommended by the HAPPI CPC.
Measures
Inflammatory measures.
A trained phlebotomist collects approximately 14 milliliters (mL) of peripheral blood and the PI or Research Assistant (RA) distributes aliquots of approximately 500 microliters (uL) of plasma into four barcoded cryotubes. Any remaining red blood cells are discarded. Aliquots are stored at −80°C until they are transferred on dry ice to the University of North Carolina School of Nursing Biobehavioral Lab. Primary endpoints include inflammatory markers IL-6, hs-CRP, plasma Amyloid A, and CBCs with differentials.
Environmental air pollutant measures.
To measure both fine and coarse mode particles, we use epidemiological air emissions data collected by the Environmental Protection Agency (EPA) using outdoor monitors. PM emissions, reported in Tons per Square Mile, from the nearest active monitors are used to estimate levels of PM exposure for participants based on the current physical address at the time of the study visit. To assess for lagged associations between PM and inflammatory markers, we use PM data gathered during the three-day period preceding the date of the participant’s data collection session.
Psychological measures.
Mental Health Continuum – Short Form (MHC-SF).
We measure relative degrees of hedonic and eudaimonic well-being with the Mental Health Continuum – Short Form (MHC-SF; Keyes et al., 2008). The MHC-SF is a 14-item measure of positive emotional well-being (3 items); psychological well-being (6); and social well-being (5). Following Fredrickson and colleagues, we aggregate the items for psychological well-being and social well-being to create an index of eudaimonic well-being, whereas the emotional well-being subscale is taken as one index of hedonic well-being (Fredrickson et al., 2013; Fredrickson et al., 2015). On a 6-point Likert scale, participants indicate how often in the past month (never, once or twice a month, about once a week, two or three times a week, almost every day, every day) they felt various positive feelings (hedonic/emotional well-being), such as “happy” and “interested in life.” Participants also indicate the extent of their agreement or disagreement with various statements indicative of psychological and social well-being (eudaimonic). Sample statements include “people are basically good” and “your life has a sense of direction and meaning to it.”
All item responses are summed, yielding possible scores for the MHC-SF ranging from 0 – 70. Categorical diagnoses include: “Flourishing,” defined as 1 of the 3 hedonic wellbeing symptoms (items 1 – 3) answered with “every day” or “almost every day,” and 6 of the 11 positive functioning symptoms (items 4 – 14) answered with “every day” or “almost every day”; “Languishing,” defined as 1 of the 3 hedonic wellbeing symptoms (items 1 – 3) answered with “never” or “once or twice” and 6 of the 11 positive functioning symptoms (items 4 – 14) answered with “never” or “once or twice”; and “Moderately Mentally Healthy,” defined as neither “languishing” nor “flourishing.” This scale has demonstrated high internal consistency (α = .89) and moderate test-retest reliability (r = .65 to .70). Both convergent (r = .74 to .92) and discriminant validity (r = −.34) have been confirmed (Lamers, Westerhof, Bohlmeijer, ten Klooster, & Keyes, 2011).
Modified Differential Emotions Scale (mDES).
To capture a broader array of emotions, participants complete the Differential Emotions Scale (Izard, 1977) as modified by Fredrickson’s team (mDES; Fredrickson, 2013; Fredrickson, Cohn, Coffey, Pek, & Finkel, 2008). Participants rate the frequency of their experiences of 20 different emotions within the past 2 weeks using a 5-point scale (0 = not at all, 4 = most of the time). Scores are determined by computing the mean response to 10 positive (amusement, awe, gratitude, hope, joy, inspired, interest, love, pride, serenity) and 10 negative emotions (anger, contempt, disgust, embarrassment, fear, guilt, hate, sadness, shame, stress) to create overall positive and negative emotion scores. The mDES has been determined to be a valid and internally consistent (α = .751) measure of positive and negative emotions (Galanakis, Stalikas, Pezirkianidis, & Karakasidou, 2016).
Center for Epidemiological Studies – Depression Scale (CES-D).
We measure depressive symptoms and positive affect using the Center for Epidemiological Studies – Depression Scale (CES-D), a 20-item scale (Canady, Stommel, & Holzman, 2009). Items such as “I felt lonely” and “I talked less than usual” reflect depressive symptoms, whereas “I felt hopeful about the future” and “I was happy” reflect positive affect. Participants identify the frequency of these feelings on a 4-point Likert scale, ranging from 0 (rarely or none of the time) to 3 (all of the time). The scoring range for the CES-D is 0 – 60, with higher scores indicating more depressive symptoms. Scoring ranges for the CES-D is as follows: <15, the participant does not appear to be experiencing high levels of depressive symptoms at this time; 15–21, mild to moderate depression – the participant appears to be experiencing some mild to moderate symptoms of depression; >21, possibility of major depression – the participant appears to be experiencing a high level of depressive symptoms associated with major depression. The CES-D is correlated with other depression measures and has high internal consistency (α = .85 to α = .91; Carleton et al., 2013). In a meta-analysis, researchers have shown the stability of the four-factor structure (i.e., depressed affect, positive affect, somatic symptoms, and interpersonal problems) of the CES-D and congruence of structures across diverse racial-ethnic groups, including American Indians (Kim, DeCoster, Huang, & Chiriboga, 2011). We chose the CES-D over the CESD-Revised (CESD-R) because the CES-D was used successfully by the PI in a previous study (ASTHMA-C) with American Indian women, and the CESD-R does not include positive affect items.
One Week Screen for Posttraumatic Stress Symptoms (SPTSS).
We assess posttraumatic stress symptoms using the One Week Screen for Posttraumatic Stress Symptoms (SPTSS). The SPTSS is a 17-item scale designed to assess posttraumatic stress disorder symptoms over the preceding week. Symptoms are not linked to any specific event, which makes the SPTSS similarly useful in measuring symptoms in participants who have never experienced trauma and in those with numerous traumatic events. The SPTSS measures the frequency of feelings and is scaled using a 5-point Likert scale, ranging from 0 (not at all) to 4 (more than once each day). Sample items include: “I avoid doing things or being in situations that might remind me of something terrible that happened to me in the past,” and “I have trouble getting to sleep or staying asleep.” The SPTSS score is the total of all item responses; a score of 20 suggests a PTSD diagnosis (Carlson, 2001). The SPTSS is correlated with other posttraumatic stress measures and has high internal consistency (α = .86; Carlson et al., 2016).
Perceived Stress Scale (PSS).
The Perceived Stress Scale (PSS) is a 10-item scale designed to assess the experiences of stress over the preceding month (Cohen, Kamarck, & Mermelstein, 1983). Participants report the frequency of feelings and thoughts using a 5-point Likert scale (0 = Never to 4 = Very Often). Sample items include: “In the last month, how often have you felt that you were on top of things?” and “In the last month, how often have you felt that things were going your way?” Positive responses are scored in reverse (4 = Never to 0 = Very Often). The PSS score is determined by totaling all responses and ranges from 0 to 40. The PSS has been determined to be an internally consistent (α = .74 to α = .91) measure of general stress (Lee, 2012).
Physical/Physiological Measures.
Body Mass Index.
We calculate body mass index (BMI) using the average height and weight with this formula: BMI = weight (kg) / [height (meters)]2. For reference, individuals with BMI values <18.5 are considered underweight, those with values 18.5 to 24.9 are considered normal/healthy, those with values 25.0 to 29.9 are considered overweight, and those with values ≥ 30.0 are considered obese (Healthy Weight, 2017). We measure height using a Detecto stadiometer, calibrated in 1/8-centimeter (cm) intervals. Height is measured twice and averaged. We measure weight to the nearest 0.1 kilograms (kg) using a factory-calibrated Health o meter Professional 500kl Digital Scale. The scale has a maximum capacity of 220 kg (500 pounds) and measures in graduations of 0.1 kg. Weight is measured twice and averaged.
Central adiposity.
We determine central adiposity using waist-to-hip ratio, calculated as waist circumference divided by hip circumference. We measure waist and hip circumference using a spring-loaded tape measure, which provides constant tension for consistency with anthropometric measurements. The landmark for the measurement of waist circumference is the midpoint between the lower margin of the rib cage and the top of the iliac crest (WHO, 2008). Waist circumference measurement is performed at the end of expiration, with the arms by the side and participant standing with the feet together. Hip circumference is measured at the maximum circumference of the gluteus maximus in this same standing position. We measure women’s waist and hip circumference in a private space and record the measures to the nearest 0.1 centimeters (cm). Waist and hip circumference are measured twice and averaged.
Blood pressure and temperature.
We assess blood pressure (recorded to the nearest whole number in millimeters of mercury [mmHg]) using a Welch Allyn digital blood pressure monitor machine with the participant in a seated position (Drawz, Abdalla, & Rahman, 2012). Selection of an appropriately-sized cuff is based on arm circumference. Blood pressure is measured three times. The first blood pressure is discarded and the second and third measures are averaged. We collect temperature readings in Celsius (recorded to the nearest 0.1 degrees) twice using a Welch Allyn digital oral thermometer and average them.
Socio-Demographic Measures.
We assess subjective socioeconomic status (SES), or perceived SES compared to others, using two items from the MacArthur Scale of Subjective Social Status, following Brown-Iannuzzi and colleagues (Adler, Epel, Castellazzo, & Ickovics, 2000; Brown-Iannuzzi, Payne, Rini, Duhamel, & Redd, 2014). Using a graphic format of a ladder featuring ten rungs, participants are asked to “think of the ladder as representing where people stand in the United States. At the top of the ladder are the people who are best off – those who have the most money, the most education, and the most respected jobs. At the bottom are the people who are worst off – those who have the least money, the least education, and the least respected jobs or no jobs.” Participants select the rung which indicates their position relative to others in the US. Participants answer a second, identical item, where the comparison group is “your community” rather than “other people in the United States.” A measure of subjective SES is created by averaging and standardizing the responses on the two ladders (Brown-Iannuzzi et al., 2014). Participants complete additional surveys to provide information on demographics, health behaviors, chronic medical conditions, recent history of minor illness symptoms, family health history, medications, environmental exposures, spirituality, perceived psychological safety, and perceived environmental injustice.
Measure Validation
Because American Indians are generally underrepresented in psychometric studies of measurement instruments, we will use data from our sample of American Indian women to examine the psychometric properties and factorial validity of the MHC-SF, mDES, SWLS, and CES-D (Council of National Psychological Associations for the Advancement of Ethnic Minority Interests, 2016). To confirm the factorial validity of each scale (i.e., that each scale measures the same number of domains among American Indian women as established in prior studies of the broader population), we will fit a confirmatory factor analysis (CFA) model and determine if there is evidence of good model fit. For the MHC-SF, we will include two factors to correspond to hedonic and eudaimonic well-being. For the mDES scale, we will include two factors to correspond to positive and negative emotions. For the SWLS, one factor will correspond to subjective well-being. For the CES-D, two factors will correspond to depressive symptoms and positive affect.
Due to the ordinality of each scale, we will compute polychoric correlations between observed ordinal variables to estimate the correlation between the underlying factors, which are assumed to be Normal in CFA (Drasgow, 2014). Factorial validity for each scale will be confirmed if the root-mean-square error of approximation (RMSEA) is less than the threshold value of 0.06, which indicates a good model fit (Dimitrov, 2010). For each scale, we will also compute Cronbach’s alpha to measure the internal consistency of each domain, with .7 indicating adequate internal consistency. If for certain domain(s) of specific scales factorial validity is not confirmed, or internal consistency is weak, we will determine whether particular items can be removed to help improve results by identifying problematic items with item-total correlations, i.e., correlations of less than 0.3 between the item score and total domain score (Nunnally & Bernstein, 1994). If the removal of these items does not improve factorial validity and internal consistency for any of the measurement scales, we will use only the CES-D scale in subsequent analyses, because its criterion validity and internal consistency have been confirmed for American Indian women in previous studies (Baron, Mason, Ackerson & Brenneman, 1990; Somervell et al., 1992, 1993).
Procedures
Women who contact the Project Manager (PM) or PI are screened for study eligibility. If deemed eligible, the PM schedules an in-person study visit at a location convenient to the woman. Within three days of the study visit, women complete an electronic consent and a short set of online study surveys (e.g., family health history). At the study visit, the PM or PI explains the study and collects a second electronic informed consent. Women provide blood specimens, have physical and physiological measurements taken, and complete psychological surveys (see Table 1). Study visits last approximately 60–90 minutes. Participants are compensated with a $50 gift card upon completion of the study visit.
Table 1.
Summary of Measures
| Measures | |||||
|---|---|---|---|---|---|
| Inflammatory | High Sensitivity | Interleukin-6 | Plasma Amyloid A | CBCs with Differentials | |
| C-Reactive Protein | |||||
| Environmental | PM2.5–10 | PM10 | |||
| Air Pollutants | |||||
| Psychological | MHC-SF | mDES | CESD | SPTSS | PSS |
| Hedonic well-being | Positive emotions | Depressive symptoms | Posttraumatic stress | Perceived stress | |
| Eudaimonic well-being | Negative emotions | Positive affect | symptoms | ||
| Physical | Height | Weight | Waist Circumference | Hip Circumference | |
| Physiological | Blood Pressure | Temperature | |||
| Demographic | MacArthur Ladder | Demographics | Health History | ||
Note. PM = Particulate Matter; MHC-SF = Mental Health Continuum Short Form; mDES = Modified Differential Emotions Scale; CES-D = Center for Epidemiological Studies-Depression; SPTSS = Screen for Posttraumatic Stress Symptoms; PSS = Posttraumatic Stress Symptoms
Data Analyses
We will analyze data using SAS (Version 9.4), and summarize continuous variables with their mean (+) standard deviation (SD) and five-number summary (minimum, maximum, median, first and third quartiles). We will use scatterplots to inspect for outliers. We will compute frequencies and percentages for each categorical variable and set statistical significance at α = .05.
To examine associations between PM exposure and inflammatory markers, we will compute the Pearson correlation between each inflammatory marker and each lagged PM exposure level, possibly transforming these variables to satisfy the assumption of bivariate normality. To identify potential covariates, we will determine whether the year of study recruitment or any of the demographic health/history, physical, and physiological measures is significantly correlated (as determined by the Benjamini-Hochberg FDR control approach) with each inflammatory marker (Benjamini & Hochberg, 2000). To determine if prior conclusions still hold after adjustment for covariates, we will use linear regression to model each inflammatory marker as a function of each lagged PM exposure variable and all identified covariates. To address regression assumptions, we will transform inflammatory marker variables if needed and examine residual and normal probability plots. To examine the relationships between psychological measures and inflammatory markers will use the same approach as described above.
To determine whether positive psychological states buffer (moderate) the association between PM and cardiovascular-associated inflammatory markers, we will use linear regression to model each inflammatory marker as a function of each lagged PM exposure measure, each psychological factor, and the associated interaction. We will fit one model for every combination of inflammatory and psychological factor. Then we will adjust for covariates as described above. We will test for a non-zero slope for the resulting interaction terms and, when significant, plot estimated mean outcome values as a function of the associated PM exposure measure for alternative values of the associated psychological factors.
Discussion
In this protocol paper, we have described our innovative study, which is the first to use a community-engaged approach to investigate both the independent and combined effects of environmental pollutants and psychological factors on cardiovascular-associated inflammation in American Indian women. After examining the associations between positive (and negative) psychological states, inflammation, and environmental pollutants in this population, we will have a fuller understanding of mechanisms influencing cardiovascular health among American Indian women. We will use our findings to develop a culturally relevant and community-based intervention to reduce American Indian women’s risk for poor cardiovascular outcomes. Data collection was ongoing at the time of manuscript preparation.
Employing a community-engaged approach has, without doubt, promoted study recruitment success. After being funded, we established and met with the CPC to solicit feedback on the cultural appropriateness of the study procedures and measures. We received input on study protocols and recruitment, which we incorporated into the research methods. Meeting with the CPC quarterly gives us continuing guidance and feedback as we progress throughout the study. We also considered skill set and cultural background carefully in our decision to hire community-based RAs, one with Lumbee ancestry, to ensure the composition and dynamics of the research team mirrored the community (Matsuda, Brooks, & Beeber, 2016).
Community-engaged studies are not exempt from challenges. Despite a thoughtful planning phase and liberal timeline, the startup of our research was delayed significantly by (a) the requirement to obtain tribal endorsement and study approval from two ethical review boards; (b) the formation of relationships with new stakeholders; (c) the process of organizing and engaging a CPC; and (d) the development of an online data management system. Barriers to recruitment of women from the ASTHMA-C registry for our study stemmed from inaccurate, changed or missing phone contact information; however, our decision to mail letters to women in the registry who were not reachable by phone resulted in additional enrollments. Although initial recruitment using snowball sampling techniques yielded few participants, we experienced a sharp increase in recruitment by leveraging participants’ social networks and expanding recruitment strategies to include social media, and by attending community events as recommended by the CPC. Based on feedback from participants and to appeal to a broader audience of potential participants, we modified recruitment materials and increased the upper age limit inclusion criteria by five years (from 45 to 50 years) because of consistent interest in study participation expressed by somewhat older women.
The HAPPI Study is led by a Lumbee academic nurse scientist and supported by an interdisciplinary research team with expertise in environmental pollutants (David B. Peden), community engagement with minorities (Giselle M. Corbie-Smith), positive psychology and psychological correlates of inflammation (Barbara L. Fredrickson), and depressive symptomatology (Linda S. Beeber); and by a CPC comprised of healthcare providers, community members and cultural experts (Reggie Brewer, Brenda Dial Deese, Tona Jacobs, Kimberly Locklear, Phyllis M. Rocco, and Kim Pevia). Our research team links disparate disciplines with little history of collaboration—nursing, environmental health, and positive psychology—and includes several biological/ physiological focal points; we are thus undertaking innovative interdisciplinary research to address the origins and progression of racial health disparities among American Indian women.
Summary
Based on our recruitment challenges thus far, we strongly urge other investigators to involve a CPC, a critical mechanism to identify and respond to barriers to the successful implementation of a community-engaged study. Although initial contact of potential participants was more difficult than expected, the community response has been positive and welcoming in their reception of our team and study. With continued support from our community partners and study participants, we experienced a significant increase in enrollment over a short period. We have learned that being flexible in location and timing of study visits, using frequent text messages and phone reminders, and providing incentive payments upon completion of data collection facilitate the completion of study visits. By incorporating ideas and suggestions from the CPC on recruitment strategies, we have increased our enrollment already and anticipate further success as we implement their recommendations.
Acknowledgement of Funding Source
This research was supported by a K23 grant (K23 ES027026) from the National Institute of Environmental Health Science (NIEHS) to the first author and a K24 grant (K24 HL105493) from the National Heart, Lung, and Blood Institute (NHLBI) to the last author. Additional funding support was provided by EPA Assistance Agreement 83578501 to David B. Peden.
Footnotes
Declaration of Conflicting Interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Adams K, Greenbaum DS, Shaikh R, van Erp AM, & Russell AG (2015). Particulate matter components, sources, and health: Systematic approaches to testing effects. Journal of the Air & Waste Management Association, 65(5), 544–558. doi: 10.1080/10962247.2014.1001884 [DOI] [PubMed] [Google Scholar]
- Adler NE, Epel ES, Castellazzo G, & Ickovics JR (2000). Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychology, 19(6), 586–592. [DOI] [PubMed] [Google Scholar]
- Avery M, Daye R, Enright D, Farmer AH, Jones-Vessey K, & Schafer ZP (2016, October). North Carolina Vital Statistics 2015. Retrieved from https://schs.dph.ncdhhs.gov/data/vital/volume1/2015/ [Google Scholar]
- Balls-Berry JE & Acosta-Perez E (2017). The use of community engaged research principles to improve health: Community academic partnerships for research. Puerto Rico Health Sciences Journal, 36(2), 84–85. [PMC free article] [PubMed] [Google Scholar]
- Baron AE, Manson SM, Ackerson LM, & Brenneman DL (1990). Depressive symptomatology in older American Indians with chronic disease In Attkisson C & Zich J (Eds.), Screening for depression in primary care (pp. 217–231). New York, NY: Routledge, Kane & Company. [Google Scholar]
- Benjamini Y & Hochberg Y (2000). On the adaptive control of the false discovery rate in multiple testing with independent statistics. Journal of Educational and Behavioral Statistics, 25, 60–83. [Google Scholar]
- Brown-Iannuzzi JL, Payne BK, Rini C, Duhamel KN, & Redd WH (2014). Objective and subjective socioeconomic status and health symptoms in patients following hematopoietic stem cell transplantation. Psycho-Oncology, 23(7), 740–748. doi: 10.1002/pon.3473 [DOI] [PubMed] [Google Scholar]
- Canady RB, Stommel M, & Holzman C (2009). Measurement properties of the Centers for Epidemiological Studies Depression Scale (CES-D) in a sample of African American and non-Hispanic White pregnant women. Journal of Nursing Measurement, 17(2), 91–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson EB (2001). Psychometric study of a brief screen for PTSD: Assessing the impact of multiple traumatic events. Assessment, 8(4), 431–441. doi: 10.1177/107319110100800408 [DOI] [PubMed] [Google Scholar]
- Carlson EB, Field NP, Ruzek JI, Bryant RA, Dalenberg CJ, Keane TM, & Spain DA (2016). Advantages and psychometric validation of proximal intensive assessments of patient reported outcomes collected in daily life. Quality of Life Research, 25(9), 507–516. doi: 10.1007/s11136-015-1170-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton RN, Thibodeau MA, Teale MJN, Welch PG, Abrams MP, Robinson T, & Asmundson GJG (2013). The Center for Epidemiologic Studies Depression Scale: A review with a theoretical and empirical examination of item content and factor structure. PLOS One, 8(3), e58067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2018, October 15). Interactive Atlas of Heart Disease and Stroke. Retrieved from https://www.cdc.gov/dhdsp/maps/atlas
- Clougherty JE (2010). A growing role for gender analysis in air pollution epidemiology. Environmental Health Perspectives, 118(12), 167–176. doi: 10.1289/ehp.0900994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [PubMed] [Google Scholar]
- Community Health Needs Assessment. Lumberton, NC: Robeson County Health Department, Southeastern Health, and Healthy Robeson Task Force; 2014.
- Council of National Psychological Associations for the Advancement of Ethnic Minority Interests (2016). Testing and assessment with persons & communities of color. Washington, DC: American Psychological Association; Retrieved from https://www.apa.org/pi/oema [Google Scholar]
- Data USA. (2018). Robeson County, NC. Retrieved from https://datausa.io/profile/geo/robeson-county-nc/#demographics
- Dimitrov DM (2010). Testing for factorial invariance in the context of construct Validation. Measurement and Evaluation in Counseling and Development, 43(2), 121–149. doi: 10.1177/0748175610373459 [DOI] [Google Scholar]
- Drasgow F (2014). Polychoric and Polyserial Correlations. Wiley StatsRef: Statistics Reference Online. doi: 10.1002/9781118445112.stat02493 [DOI] [Google Scholar]
- Drawz PE, Abdalla M, & Rahman M (2012). Blood pressure measurement: Clinic, home, ambulatory, and beyond. American Journal of Kidney Diseases: The Official Journal of the National Kidney Foundation, 60(3), 449–462. doi: 10.1053/j.ajkd.2012.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y, Xu X, Chu M, Guo Y, & Wang J (2016). Air particulate matter and cardiovascular disease: The epidemiological biomedical and clinical evidence. Journal of Thoracic Disease, 8(1), E8–E19. doi: 10.3978/j.issn.2072.-1439.2015.11.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdfelder E, FaAul F, Buchner A, & Lang AG (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. doi: 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- Fredrickson BL (2013). Positive emotions Broaden and Build. Advances in Experimental Social Psychology, 47, 1–53. doi: 10.1016/B978-0-12-407236-7.00001-2 [DOI] [Google Scholar]
- Fredrickson BL, Cohn MA, Coffey KA, Pek J, & Finkel SM (2008). Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology, 95(5), 1045–1062. doi: 10.1037/a0013262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, Grewen KM, Algoe SB, Firestine AM, Arevalo JMG, Ma J, & Cole SW (2015). Psychological well-being and the human conserved transcriptional response to adversity. PloS One, 10(3), e0121839. doi: 10.1371/journal.pone.0121839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, Grewen KM, Coffey KA, Algoe SB, Firestine AM, Arevalo JMG, … Cole SW (2013). A functional genomic perspective on human well-being. Proceedings of the National Academy of Sciences, 110(33), 13684–13689. doi: 10.1073/pnas.1305419110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanakis M, Stalikas A, Pezirkianidis C, & Karakasidou I (2016). Reliability and validity of the Modified Differential Emotions Scale (mDES) in a Greek sample. Psychology, 7(1), 101–113. doi: 10.4236/psych.2016.71012 [DOI] [Google Scholar]
- Gold DR, & Mittleman MA (2013). New insights into pollution and the cardiovascular system: 2010 to 2012. Circulation, 127(18), 1903–1913. doi: 10.1161/CIRCULATIONAHA.111.064337 [DOI] [PubMed] [Google Scholar]
- Hamanaka RB & Mutlu GM (2018). Particulate matter air pollution: Effects on the cardiovascular system. Frontiers in Endocrinology, 9, 680. doi: 10.3389/fendo.2018.00680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthy Weight. (2017, August 29). Retrieved from https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
- Hicken MT, Adar SD, Diez Roux AV, O’Neill MS, Magzamen S, Auchincloss AH, & Kaufman JD (2013). Do psychosocial stress and social disadvantage modify the association between air pollution and blood pressure?: The multi-ethnic study of atherosclerosis. American Journal of Epidemiology, 178(10), 1550–1562. doi: 10.1093/aje/kwt190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken MT, Dvonch JT, Schulz AJ, Mentz G, & Max P (2014). Fine particulate matter air pollution and blood pressure: the modifying role of psychosocial stress. Environmental Research, 133, 195–203. doi: 10.1016/j.envres.2014.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson RN & Shin S (2014). Systematic review of health disparities for cardiovasular diseases and associated factors among American Indian and Alaska Native populations. PLOS One, 9(1), e80973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izard CE (1977). Human emotions. New York: Plenum Press. [Google Scholar]
- Keyes CLM, Wissing M, Potgieter JP, Temane M, Kruger A, & van Rooy S (2008). Evaluation of the mental health continuum- short form (MHC-SF) in Setswana-speaking South Africans. Clinical Psychology and Psychotherapy, 15(3), 181–192. doi: 10.1002/cpp.572 [DOI] [PubMed] [Google Scholar]
- Kim G, DeCoster J, Huang CS, & Chiriboga DA (2011). Race/ethnicity and the factor structure of the Center for Epidemiological Studies Depression Scale: A meta-analysis. Cultural Diversity and Ethnic Minority Psychology, 17(4), 381–396. doi: 10.1037/a0025434 [DOI] [PubMed] [Google Scholar]
- Lamers SM, Westerhof GJ, Bohlmeijer ET, ten Klooster PM, & Keyes CLM (2011). Evaluating the psychometric properties of the mental health Continuum Short Form (MHC SF). Journal of Clinical Psychology, 67(1), 99–110. doi: 10.1002/jclp.20741 [DOI] [PubMed] [Google Scholar]
- Lee E (2012). Review of the psychometric evidence of the Perceived Stress Scale. Asian Nursing Research, 6(4), 121–127. [DOI] [PubMed] [Google Scholar]
- Mannucci PM, Harari S, Martinelli I, & Franchini M (2015). Effects on health of air pollution: A narrative review. Internal and Emergency Medicine, 10(6), 657–662. doi: 10.1007/s11739-015-1276-7 [DOI] [PubMed] [Google Scholar]
- Matsuda Y, Brooks JL, & Beeber LS (2016). Guidelines for research recruitment of underserved populations (EERC). Applied Nursing Research, 32, 164–170. doi: 10.1016/j.apnr.2016.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michener L, Cook J, Ahmed SM, Yonas MA, Coyne-Beasley T, & Aguilar-Gaxiola S (2012). Aligning the goals of community-engaged research: Why and how academic health centers can successfully engage with communities to improve health. Academic Medicine, 87(3), 285–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morishita M, Thompson KC, & Brook RD (2015). Understanding air pollution and cardiovascular diseases: Is It Preventable? Current Cardiovascular Risk Reports, 9(6), 30. doi: 10.1007/s12170-015-0458-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson SK, Layous K, Cole SW, & Lyubomirsky S (2016). Do unto others or treat yourself? The effects of prosocial and self-focused behavior on psychological flourishing. Emotion, 16(6), 850–861. doi: 10.1037/emo0000178 [DOI] [PubMed] [Google Scholar]
- Nelson-Coffey SK, Fritz MM, Lyubomirsky S, & Cole SW (2017). Kindness in the blood: A randomized control trial of the gene regulatory impact of prosocial behavior. Psychoneuroendocrinology, 81, 8–13. doi: 10.1016/j.psyneuen.2017.03.025 [DOI] [PubMed] [Google Scholar]
- Nunnally R & Bernstein I (1994). Psychometric Theory (3rd ed). New York, NY: McGraw-Hill. [Google Scholar]
- Parker JD, Kravets N, & Vaidyanathan A (2018). Particulate matter air pollution exposure and heart disease mortality risks by race and ethnicity in the United States: 1997 to 2009 National Health Interview Survey with mortality follow-up through 2011. Circulation, 137(16), 1688–1697. doi: 10.1161/CIRCULATIONAHA.117.029376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope CA, Bhatnagar A, McCracken JP, Abplanalp W, Conklin DJ, & O’Toole T (2016). Exposure to fine particulate air pollution is associated with endothelial injury and systemic inflammation. Circulation Research, 119, 1204–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridker PM, Hennekens CH, Buring JE, & Rifai N (2000). C-Reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. New England Journal of Medicine, 342(12), 836–843. doi: 10.1056/NEJM200003233421202 [DOI] [PubMed] [Google Scholar]
- Robeson County Health Department (2014, September). Community Needs Health Assessment. Retrieved from http://www.robesoncountyhealthdepartment.com/
- Robinson DP & Klein SL (2012). Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis. Hormones and Behavior, 62(3), 263–271. doi: 10.1016/j.yhbeh.2012.02.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD (2017). Eudaimonic well-being, inequality, and health: Recent findings and future directions. International Review of Economics, 64, 159–178. doi: 10.1007/s12232-017-0277-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selya AS, Rose JS, Dierker LC, Hedeker D, & Mermelstein RJ (2012). A practical guide to calculating Cohen’s f 2, a measure of local effect size, from PROC MIXED. Frontiers in Psychology, 3, 111. doi: 10.3389/fpsyg.2012.00111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrivastava AK, Singh HV, Raizada A, & Singh SK (2015). C-reactive protein, inflammation and coronary heart disease. Egyptian Heart Journal, 67(2), 89–97. doi: 10.1016/j.ehj.2014.11.005 [DOI] [Google Scholar]
- Somervell PD, Beals J, Kinzie JD, Boehnlein J, Leung P, & Manson SM (1992). Use of the CES-D in an American Indian village. Culture, Medicine and Psychiatry, 16(4), 503–517. doi: 10.1007/BF00053590 [DOI] [PubMed] [Google Scholar]
- Somervell PD, Beals J, Manson SM, Kinzie JD, Boehnlein J, & Leung P (1993). Criterion validity of the center for epidemiologic studies depression scale in a population sample from an American Indian village. Psychiatry Research, 47(3), 255–266. doi: 10.1016/0165-1781(93)90083-S [DOI] [PubMed] [Google Scholar]
- Steenhoff M, Janssen NA, Strak M, Hoek G, Gosens I, Mudway IS, … Brunekreef B (2014). Air pollution exposure affects circulating white blood cell counts in healthy subjects: The role of particle composition, oxidative potential and gaseous pollutants - the RAPTES project. Inhalation Toxicology, 26(3), 141–165. [DOI] [PubMed] [Google Scholar]
- Tsai DH, Amyai N, Marques-Vidal P, Wang J, Riediker M, Mooser V, … Bochud M (2012). Effects of particulate matter on inflammatory markers in the general adult population. Particle and Fibre Toxicology, 9(24). doi: 10.1186/1743-8977-9-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau (2012, January). The American Indian and Alaska Native population: 2010. Retrieved from https://www.census.gov/content/dam/Census/library/publications/2012/dec/c2010br-10.pdf
- Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation December 8–11, 2008. In: Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation December 8–11, 2008. WHO; 2011. http://apps.who.int/iris/bitstream/handle/10665/44583/9789241501491_eng.pdf; jsessionid=623C17224CFA60FCC846DFF73A3A8DD2?sequence=1. [Google Scholar]
- Wu W, Jin Y, & Carlsten C (2018). Inflammatory health effects of indoor and outdoor particulate matter. The Journal of Allergy and Clinical Immunology, 141(3), 833–844. doi: 10.1016/j.jaci.2017.12.981 [DOI] [PubMed] [Google Scholar]


