Abstract
This study assessed the impact of respiratory syncytial virus–confirmed hospitalizations (RSVH) on caregivers of high-risk preterm infants. Caregivers for infants born at 29 to 35 weeks’ gestational age and hospitalized for confirmed RSV disease responded to measures of self-rated and perceived infant stress (1-7; 7 = very stressful), perceived infant health (0-100; 100 = best imaginable health), and productivity impairment. Data were collected at hospital discharge through 1 month post-discharge. Caregiver responses indicated high stress levels, poor health, and productivity loss were reported at discharge; however, steady improvements were seen through 1 month post-discharge: caregiver-rated stress (from 6 to 2), infant stress (5 to 1), caregiver-perceived infant health (64 to 84), and productivity loss (mothers: 91% to 31%; fathers: 81% to 18%). Qualitative results indicated emotional impact, family routine disruption, financial concerns, and medical concerns persisted at 1 month post-discharge. This study found the caregiver burden of RSVH persists at least 1 month beyond discharge.
Keywords: respiratory syncytial virus, caregiver burden, preterm, infant, hospitalization
Background
Respiratory syncytial virus (RSV) is the leading cause of infant hospitalizations in the United States.1 Children at greatest risk for severe RSV disease include preterm infants ≤35 weeks’ gestational age (wGA) as well as children ≤24 months of age with chronic lung disease of prematurity (CLDP) and hemodynamically significant congenital heart disease (HS-CHD).2,3 The preterm infant ≤35 wGA population constitutes the largest of these high-risk populations.
No vaccine is currently available to prevent RSV disease and there is no treatment to cure the disease. The only available option for prevention is seasonal RSV immunoprophylaxis (IP) with palivizumab, a humanized monoclonal antibody targeting the RSV F-protein. RSV IP has been shown to effectively reduce hospitalizations in high-risk preterm infants ≤35 wGA and children ≤24 months of age with CLDP and HS-CHD compared with placebo in randomized controlled trials.4-6
The American Academy of Pediatrics Committee on Infectious Diseases (COID) provides guidance on the use of RSV IP. In the 2014 update to this guidance, the COID no longer recommended the use of RSV IP in US preterm infants 29 to 35 wGA, except for those with other qualifying medical conditions, such as CLDP or HS-CHD.7 Previously, the COID recommendations included all preterm infants born at <32 wGA and a subset of high-risk infants born at 32 to 35 wGA.8,9
The SENTINEL1 observational study provided insight into the impact of the guidance change by characterizing RSV-confirmed hospitalizations (RSVH) in US preterm infants born at 29 to 35 wGA who were not receiving RSV IP during the 2014-2015 RSV season.10 RSVH, which among high-risk infants can frequently result in intensive care unit (ICU) admissions,10 creates significant distress for the infants (eg, need for supplemental oxygen, impacts on functional status, and pain). Although there are studies that document the impact of hospitalization for any reason on caregivers and families, there is limited information on the experience of caregivers of infants hospitalized specifically for RSV disease.11-16 The aim of this research was to understand the impact of RSVH on high-risk preterm infants born at 29 to 35 wGA and their caregivers.
Materials, Subjects, and Methods
Study Design
This study was a secondary analysis of data collected during the SENTINEL1 study, a multicenter, noninterventional, observational cohort study of preterm infants 29 to 35 wGA and aged <12 months who were hospitalized for laboratory-confirmed RSV disease and who did not receive RSV IP (ClinicalTrials.gov identifier: NCT02273882).10 Data were collected from October 1, 2014, through April 30, 2015, across 43 sites in the United States. Among the 702 infants with community-acquired RSVH identified in the SENTINEL1 study, a subset of 212 infants were enrolled for in-depth characterization of their RSV illness and to gain an understanding of infant and caregiver stress and infant health. An independent ethics committee/institutional review board approved the final study protocol, including the final version of the informed consent form and other written information and materials provided to the caregivers. Written informed consent was obtained for all enrolled participants in the study.
Measures
Sociodemographic and clinical data were collected for both infants and caregivers. Data were gathered from caregivers at RSVH discharge, 1 week post-discharge, 2 weeks post-discharge, and 1 month post-discharge. The caregivers completed multiple study measures including ratings of caregiver stress (during the past 24 hours and 7 days), caregiver’s perception of infant stress (during the past 24 hours and 7 days), and the caregiver’s perception of the infant’s current health (past 24 hours).13 The Work Productivity Assessment Inventory in Caregivers of Children Hospitalized for Respiratory Illness (WPAI:CHRI) was also utilized to measure the effect of RSVH on caregiver work productivity and regular activities during the past 7 days (Table 1).17,18 Additionally, an open-ended question designed for the study was asked of each caregiver: “Please describe the impact this illness has had on you and your family, including any information that you have not already shared.” In general, the caregivers were asked this question at each time point, but for infants enrolled after their hospital discharge, caregivers were asked to retrospectively report this information.
Table 1.
Assessments Collected at Discharge, 1 Week Post-Discharge, 2 Weeks Post-Discharge, and 1 Month Post-Discharge.
| Study Measures | Details About the Study Measure |
|---|---|
| Caregiver rating of infant stress | Two items were used for caregivers to rate infant stress. One asked caregivers to measure infant stress in the past 24 hours, and the second asked caregivers to rate infant stress in the past 7 days. Both stress measures ranged from 1 (not stressful at all) to 7 (very stressful). Caregivers who were present at each particular time point completed the infant stress ratings. The measure was adapted from a similar one used in Leidy et al.13 |
| Caregiver self-rating of stress | Two items were used for caregivers to rate their own stress. One asked caregivers to measure their stress in the past 24 hours, and the second asked caregivers to rate their stress in the past 7 days. Both stress measures ranged from 1 (not stressful at all) to 7 (very stressful). Caregivers who were present at each particular time point completed the self-reported stress ratings. The measure was adapted from a similar one used in Leidy et al.13 |
| Caregiver rating of infant’s global health | Caregivers were asked to rate the infant’s global health in the past 24 hours. The global health rating ranged from 0 (worst imaginable health) to 100 (best imaginable health). Caregivers who were present at each particular time point completed the self-reported stress ratings. The measure was adapted from a similar one used in Leidy et al.13 |
| Work Productivity Assessment Inventory (WPAI:CHRI) | The WPAI:CHRI is a 6-item paper/pencil questionnaire that assesses health-related work absenteeism and presenteeism.17,18 It asks questions such as “During the past 7 days, how many hours did you actually work?” and contains 4 domains: absenteeism (work time missed), presenteeism (impairment at work/reduced on-the-job effectiveness), work productivity loss (overall work impairment/absenteeism plus presenteeism), and activity impairment. Each subscale ranges from 0 to 100 with higher scores indicating greater impairment. |
| Open-ended hospitalization impact question | An open-ended question was asked of all available caregiver respondents at each follow-up time point in the SENTINEL1 study. The open-ended question consisted of the following request: “Please describe the impact this illness has had on you and your family, including any information that you have not already shared.” |
Analytic Approach
Defining a Caregiver
“Caregiver” was defined as the infant’s mother, father, grandparent, or other adult family member. Consistent caregiver representation was not a prerequisite for analyses, resulting in varied caregiver appraisals over time. For example, there might have been one appraisal from a father at one time point and multiple caregiver appraisals (eg, mother, father, and grandmother) at other time points. Grandparent(s) and family member caregivers who were not the mother or the father were combined for analysis and listed as “other” caregivers. One infant had same-sex parents, so both caregivers were included in the mother cohort.
Quantitative Caregiver Assessments
Quantitative data were analyzed using SAS software version 9.4 (SAS Institute Inc, Cary, NC). Descriptive statistics (eg, mean, median, range, and standard deviation) were used to characterize the sample, including sociodemographic and clinical characteristics, the caregiver’s perception of their infant’s stress during the past 24 hours and past 7 days relative to each respective time point, the caregiver’s self-rating of stress during the past 24 hours and past 7 days, and the caregiver’s perception of their infant’s current health during the past 24 hours. Group means by caregiver type and time point for caregiver’s ratings of stress and health were analyzed. The WPAI:CHRI data were scored according to the developer’s manual.17,18 Not all caregivers provided data. Absenteeism, presenteeism, and overall work productivity loss were calculated for caregivers who were currently employed. Daily activity impairment was calculated for caregivers regardless of their current employment status.
Open-Ended Question About Hospitalization Impact
A thematic narrative analysis approach was used for the qualitative analysis. Thematic narrative analysis involves a systematic analysis of narratives with the goal of capturing patterns or themes.18 All available data were used in the analyses, across all caregiver types. The caregiver comments were entered into an electronic data capture tool by clinic site staff in note form and subsequently transferred to a Microsoft Excel file for analysis; some comments were entered using first-person narrative and some in third-person narrative.
Comments were reviewed, impact themes were identified, and the data were coded by the identified themes. Themes were discussed among researchers and agreement on the codes was reached. Each line of data (ie, each infant’s caregiver comment by time point) was then coded using the themes. It should be noted that a single comment could have multiple themes assigned, and the data were not mutually exclusive to the themes. For example, the following quotation reported by the mother of a 34 wGA infant at discharge was coded with both Emotional Impact and Routine Disruption: “Huge impact. We now are very aware and nervous about RSV. Very worried about his health. Running to the doctor every time he is sick now.” Themes were assigned, then, sorted by time point, caregiver type, infant gestational age group (29 to 32 wGA, 33 to 34 wGA, and 35 wGA), ICU admission status, and the need for invasive mechanical ventilation.
The qualitative data were quantified by counting the number of responses in each impact theme at each time point. The numerator was the number of coded responses in each impact theme; the denominator was the number of caregiver respondents.
Results
Sample
Among the 212 enrolled infants, 53% were males, 42% of infants were 29 to 32 wGA, 38% were 33 to 34 wGA, and 20% were 35 wGA. The majority of infants were White and not Hispanic. Additional infant characteristics and caregiver characteristics are presented in Tables 2 and 3, respectively.
Table 2.
Infant Characteristics.
| Infant Characteristics | Enrolled Infants (n = 212) |
|---|---|
| Male, n (%) | 113 (53) |
| Race, n (%) | |
| White | 140 (66) |
| Black or African American | 49 (23) |
| Asian | 3 (1) |
| American Indian or Alaska Native | 3 (1) |
| Other | 17 (8) |
| Ethnic group, n (%)a | |
| Hispanic or Latino | 40 (19) |
| Not Hispanic or Latino | 170 (80) |
| Gestational age, weeks, n (%) | |
| 29 to 32 | 89 (42) |
| 33 to 34 | 81 (38) |
| 35 | 42 (20) |
| Age at admission, months | |
| Mean (SD) | 3 (3) |
| Median (IQR) | 2 (4) |
| Range | 0-11 |
| Hospital LOS, days | |
| Mean (SD) | 8 (9) |
| Range | 1-67 |
| ICU admission, n (%) | 108 (51) |
| Of the ICU admissions required IMV, n (%) | 45 (21) |
Abbreviations: ICU, intensive care unit/neonatal intensive care unit; IMV, invasive mechanical ventilation; IQR, interquartile range; LOS, length of stay.
1% stated “unknown.”
Table 3.
Caregiver Characteristics.
| Caregiver Characteristics | Enrolled Infants (n = 212) |
|---|---|
| Infant’s caregivers at home,a n (%) | |
| Mother | 126 (59) |
| Father | 59 (28) |
| Mother and father | 82 (39) |
| Grandparent(s) | 27 (13) |
| Other | 22 (10) |
| Mother’s age at infant’s birth, years | |
| Mean (SD) | 29 (6) |
| Range | 15-46 |
| Mother’s education,b n (%) | |
| Less than 12th grade, no diploma | 45 (22) |
| High school graduate or GED | 57 (27) |
| Some college or associate degree | 52 (25) |
| College degree (bachelor’s, master’s, or doctorate) | 55 (26) |
| Mother works outside the home, n (%) | 120 (48) |
| Total number of people in household, including the infant | |
| Mean (SD) | 5 (2) |
| Range | 2-12 |
| Other children in the household, excluding the infant, n (%) | 178 (84) |
| Total number of children in household, excluding infant | |
| Mean (SD) | 2 (1) |
| Range | 1-8 |
| Age of children in household, excluding infant, years | |
| Mean (SD) | 5 (4) |
| Range | 0-17 |
Abbreviations: GED, General Equivalency Diploma; SD, standard deviation.
Multiple caregivers could be counted for an infant.
3 (1%) missing.
Quantitative Caregiver Assessment Results
Although data from the sample of 212 infants’ caregivers were collected, some time points did not gain responses for all 212 infants. The number of caregivers providing a response at each time point is presented in Table 4. For example, at discharge, caregiver data about stress and health from 206 infants were reported.
Table 4.
Summary of Stress and Current Infant Health Over Time by Caregivers.
| At Discharge | 1 Week Post-Discharge | 2 Weeks Post-Discharge | 1 Month Post-Discharge | Total | |
|---|---|---|---|---|---|
| Overall stress for infant last 24 hoursa | |||||
| N | 206 | 181 | 178 | 193 | 758 |
| Mean (SD) | 4.8 (2.06) | 3.8 (2.12) | 2.7 (1.85) | 2.1 (1.65) | 3.4 (2.19) |
| Median | 5.0 | 4.0 | 2.0 | 1.0 | 3.0 |
| Interquartile range | 3.5 | 4.0 | 3.0 | 2.0 | 4.0 |
| Range | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 |
| Overall stress for caregiver last 24 hoursa | |||||
| N | 206 | 181 | 178 | 193 | 758 |
| Mean (SD) | 5.3 (1.89) | 4.3 (2.15) | 3.0 (1.93) | 2.4 (1.83) | 3.8 (2.27) |
| Median | 6.0 | 5.0 | 2.0 | 1.0 | 4.0 |
| Interquartile range | 3.0 | 4.0 | 3.0 | 2.5 | 5.0 |
| Range | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 |
| Overall stress for infant last 7 daysa | |||||
| N | 206 | 181 | 178 | 193 | 758 |
| Mean (SD) | 5.5 (1.84) | 3.9 (2.06) | 2.7 (1.93) | 2.1 (1.70) | 3.6 (2.30) |
| Median | 6.0 | 4.0 | 2.0 | 1.0 | 3.3 |
| Interquartile range | 2.0 | 4.0 | 3.0 | 2.0 | 5.0 |
| Range | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 |
| Overall stress for caregiver last 7 daysa | |||||
| N | 206 | 181 | 178 | 193 | 758 |
| Mean (SD) | 5.8 (1.65) | 4.3 (2.03) | 3.1 (2.02) | 2.4 (1.85) | 3.9 (2.30) |
| Median | 6.4 | 5.0 | 3.0 | 1.0 | 4.0 |
| Interquartile range | 2.0 | 3.0 | 4.0 | 3.0 | 5.0 |
| Range | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 | 1.0-7.0 |
| Scale of current infant healthb | |||||
| N | 206 | 181 | 178 | 193 | 758 |
| Mean (SD) | 64.3 (26.87) | 71.8 (21.59) | 79.0 (22.56) | 84.0 (22.70) | 74.6 (24.78) |
| Median | 70.0 | 80.0 | 87.3 | 94.0 | 80.0 |
| Interquartile range | 35.0 | 35.0 | 25.0 | 20.0 | 35.0 |
| Range | 0.0-100.0 | 0.0-100.0 | 0.0-100.0 | 5.0-100.0 | 0.0-100.0 |
| Who contributed to this score | |||||
| Mother, n (%) | 125 (60.7) | 126 (69.6) | 128 (71.9) | 128 (66.3) | 507 (66.9) |
| Father, n (%) | 5 (2.4) | 13 (7.2) | 10 (5.6) | 10 (5.2) | 38 (5.0) |
| Other only, n (%) | 2 (1.0) | 2 (1.1) | 2 (1.1) | 4 (2.1) | 10 (1.3) |
| Parents, n (%) | 63 (30.6) | 36 (19.9) | 34 (19.1) | 47 (24.4) | 180 (23.7) |
| Mother + grandparent, n (%) | 5 (2.4) | 1 (0.6) | 1 (0.6) | 2 (1.0) | 9 (1.2) |
| Mother + other family, n (%) | 1 (0.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.1) |
| Mother plus 2+ responders, n (%) | 5 (2.4) | 3 (1.7) | 3 (1.7) | 2 (1.0) | 13 (1.7) |
Abbreviation: SD, standard deviation.
Response options ranged from 1 = not stressful at all to 7 = very stressful.
Response options ranged from 0 = worst imaginable health to 100 = best imaginable health.
Infant’s Health and Stress Ratings
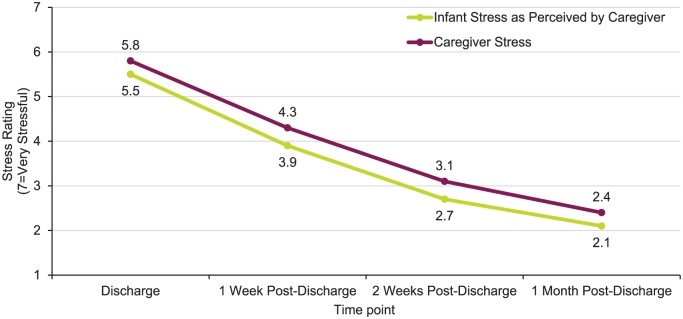
Descriptive results from the caregiver’s report about the infant’s stress, the caregiver’s stress, and the caregiver’s perception of the infant’s health are presented by time point in Table 4. Figure 1 illustrates caregivers’ perceptions of infants’ stress over the past 7 days and the caregiver’s self-reported stress over the past 7 days by time point. The mean stress reduced for caregivers and caregivers’ perception of infant stress over time. The stress for both was still present even 1 month post-discharge. The mean caregivers’ stress was consistently higher than the caregivers’ perception of infant stress over time.
Figure 1.
Caregiver rating of stress, past 7 days.
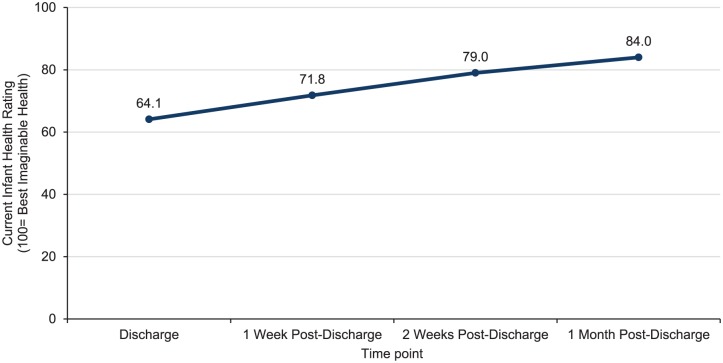
The caregivers’ perception of the infant’s current health improved after discharge and continued to improve to the 1 month post-discharge time point; caregivers reported a 20% improvement in the infant’s health from discharge to 1 month post-discharge (Figure 2). However, the caregivers’ mean health rating at 1 month post-discharge was not “best imaginable health.”
Figure 2.
Caregiver rating of current infant health.
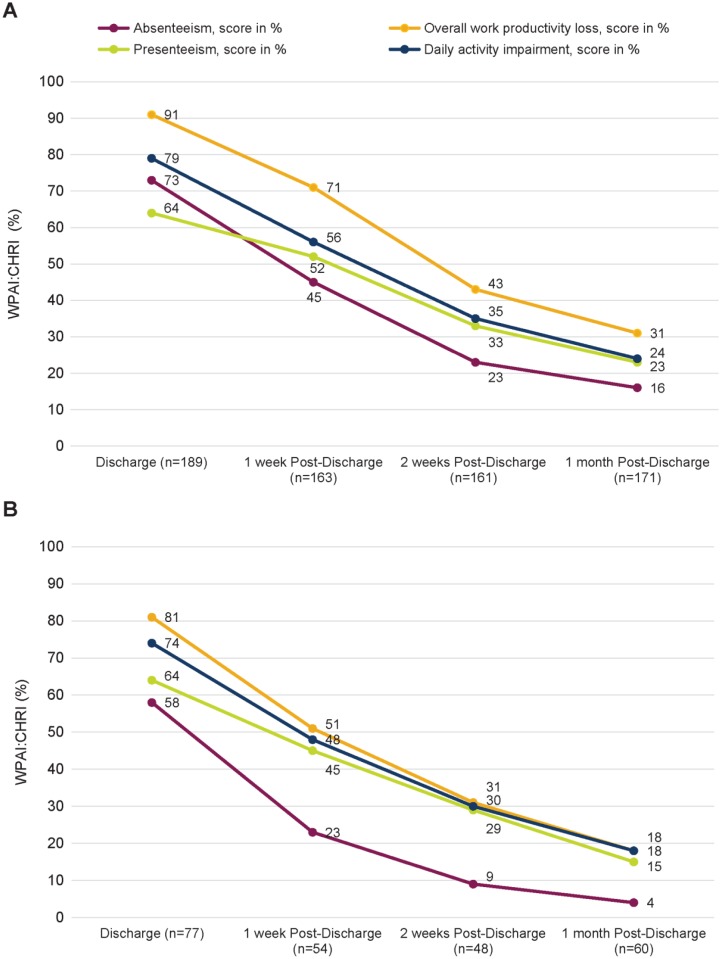
Work Productivity Assessment Inventory in Caregivers of Children Hospitalized for Respiratory Illness
As reported using the WPAI:CHRI, impacts on 4 types of productivity parameters (absenteeism, presenteeism, overall work productivity loss, and daily activity impairment) were seen among the sample of caregivers (Table 5 and Figure 3). At discharge, 73% of mothers and 58% of fathers reported absenteeism; at 1 month post-discharge, absenteeism declined for mothers and fathers (15% and 4%). This translated to employed mothers missing an average of 23, 14, 7, and 4 hours of work and employed fathers missing an average of 24, 9, 4, and 2 hours of work at discharge, 1 week, 2 weeks, and 1 month post-discharge, respectively. Presenteeism and daily activity impairment trended similarly for both mothers and fathers; however, mothers were more affected. Although the impact on overall productivity declined over time, productivity impacts were still present for all caregivers at 1 month post-discharge.
Table 5.
Work Productivity Assessment Inventory for Caregivers of Children Hospitalized for Respiratory Illness (WPAI:CHRI)a Results Mothers/Fathers.
| At Discharge | 1 Week Post-Discharge | 2 Weeks Post-Discharge | 1 Month Post-Discharge | |
|---|---|---|---|---|
| Mothers | ||||
| N = 189 | N = 163 | N = 161 | N = 171 | |
| Absenteeism (%) | ||||
| Mean (SD) | 73 (32) | 45 (39) | 23 (37) | 15 (32) |
| Median (IQR) | 83 (50) | 50 (71) | 0 (33) | 0 (19) |
| Presenteeism (%) | ||||
| Mean (SD) | 64 (41) | 52 (41) | 33 (34) | 23 (31) |
| Median (IQR) | 80 (90) | 50 (90) | 20 (50) | 10 (40) |
| Overall work productivity loss (%) | ||||
| Mean (SD) | 91 (21) | 71 (35) | 43 (38) | 31 (36) |
| Median (IQR) | 100 (5) | 88 (50) | 40 (80) | 10 (63) |
| Daily activity impairment (%) | ||||
| Mean (SD) | 79 (28) | 56 (33) | 35 (32) | 24 (30) |
| Median (IQR) | 90 (30) | 60 (50) | 30 (60) | 10 (50) |
| Fathers | ||||
| N = 77 | N = 54 | N = 48 | N = 60 | |
| Absenteeism (%) | ||||
| Mean (SD) | 58 (36) | 23 (33) | 9 (20) | 4 (16) |
| Median (IQR) | 53 (71) | 0 (36) | 0 (5) | 0 (0) |
| Presenteeism (%) | ||||
| Mean (SD) | 64 (35) | 45 (32) | 29 (32) | 15 (20) |
| Median (IQR) | 70 (60) | 50 (50) | 10 (60) | 10 (20) |
| Overall work productivity loss (%) | ||||
| Mean (SD) | 81 (26) | 51 (36) | 31 (35) | 18 (25) |
| Median (IQR) | 91 (30) | 58 (56) | 10 (60) | 10 (30) |
| Daily activity impairment (%) | ||||
| Mean (SD) | 74 (28) | 48 (33) | 30 (34) | 18 (24) |
| Median (IQR) | 80 (40) | 55 (60) | 10 (55) | 10 (30) |
Abbreviations: IQR, interquartile range; SD, standard deviation; WPAI, Work Productivity Assessment Inventory.
Absenteeism, presenteeism, and overall work productivity loss were only calculated for caregivers who were currently employed. Daily activity impairment was calculated for caregivers regardless of current employment status. For each WPAI score, higher values on a scale of 0 to 100 indicate greater impairment and less productivity (ie, worse outcome).
Figure 3.
Work Productivity Assessment Inventory in Caregivers of Children Hospitalized for Respiratory Illness (WPAI:CHRI) results. Panel A, Mothers; Panel B, Fathers.
Caregiver Comments About Hospitalization Impact
From the open-ended question about hospitalization impact, there were a total of 974 comments across all caregiver types and all time points. After removing duplicate data, missing data, and comments that were equivalent to missing data (eg, “n/a,” “no comment”), there were 742 comments to review across the 4 time points. The comments were specific to an infant; multiple caregivers could have responded about the same infant.
At discharge, 235 total caregiver comments were recorded, and these comments could have been from multiple caregivers for the same infant. Post-discharge comments were also recorded: 174 comments at 1 week post-discharge, 151 comments at 2 weeks post-discharge, and 182 comments at 1 month post-discharge. Mothers of infants contributed the most comments. Specifically, the percentage of comments from mothers were 75% at discharge, 80% at 1 week post-discharge, 79% at 2 weeks post-discharge, and 78% at 1 month post-discharge. Fathers contributed 21% of comments at discharge, 18% at 1 week post-discharge, 18% at 2 weeks post-discharge, and 19% at 1 month post-discharge. Other caregivers provided 4% of comments at discharge, 2% at 1 week post-discharge, 3% at 2 weeks post-discharge, and 3% at 1 month post-discharge.
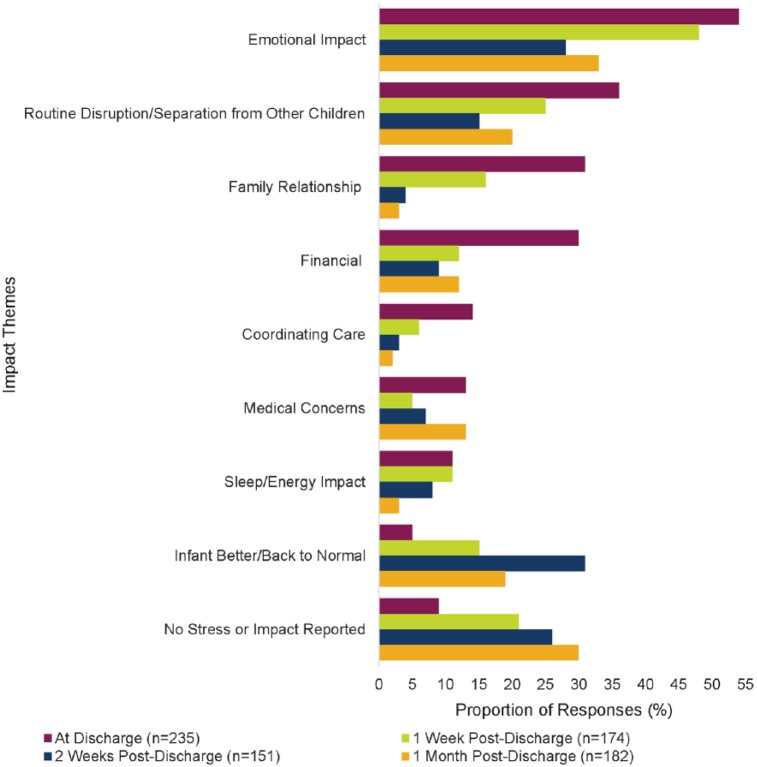
Nine themes characterizing the impact of RSVH on the caregiver were identified: emotional impacts; routine disruption/separation from other children; family relationship impacts; financial impacts; coordinating care; medical concerns; sleep/energy impacts; no impacts on the family; and miscellaneous comments. Additionally, some comments were grouped under the theme, “Better/infant back to normal.” The 742 comments were coded; themes were not mutually exclusive. A selection of caregiver comments by time point is presented in Table 6. The caregiver comments represented 86% of infants at discharge, 72% at 1 week post-discharge, 63% at 2 weeks post-discharge, and 73% at 1 month post-discharge. As a visual representation, Figure 4 presents the open-ended stress impacts by theme and time point for the combined caregiver responses. Emotional impacts (eg, stress, worry, and fear) were the most common theme reported among the comments for each time point. Emotional impacts were still being reported even at 1 month post-discharge. Disruption to the family routine (eg, needing to travel for medical visits), financial concerns, and medical concerns (eg, monitoring infant’s breathing) were also among the most frequently raised issues that persisted through 1 month post-discharge.
Table 6.
Select Caregiver Comments About Impact of Infant’s RSVH.
| Impact Theme | Time Point, Discharge, or Time Since Discharge | Caregiver Comment (Infant’s wGA, Caregiver Rating of Infant’s Health, M/F/Oa) |
|---|---|---|
| Emotional impact | Discharge | I had to miss 2 days of school, which is stressful because I have a lot of school work to make up. Seeing him sick worried me and I cried like 5 times over it. I missed 5 hours of work, which makes me stress over money. It has been very stressful. (34 wGA, 90, M) |
| Discharge | Mother states: I’m a new Mom. I’m stressed and worried. Anything that happens to my child is a huge weight on me. He was born so premature. He is so fragile. When he had difficulty breathing, I was terrified. (32 wGA, 0, M) | |
| Discharge | They [parents] would have done everything possible to avoid this illness. It was so stressful hearing the doctor say that he [infant] could have died. (34 wGA, 90, M) | |
| Discharge | Extremely stressful on whole family especially because the hospital is 50 miles away from home. Parents had to be apart because 3-year-old son stayed home with dad and mom was at hospital with patient. Taken son out of daycare because they don’t want him to expose a risk to the baby. Father has had to take more time off of work. Witnessing baby be so sick in the hospital were very traumatic to witness. Baby almost died. Still think back to the first few days. Staying isolated is hard. (32 wGA, 60, M) Note this quote was repeated under Routine Disruption/Separation From Other Children at Discharge. | |
| Discharge | Huge impact. We now are very aware and nervous about RSV. Very worried about his health. Running to the doctor every time he is sick now. (34 wGA, 70, M) | |
| Discharge | It was a huge impact! Life stopped. We had to re-clean everything in our house. There was a lot of back and forth driving which totaled about 3 hours/day. There was a large snowstorm in between in which we couldn’t leave our house and couldn’t see our kids at the hospital. All 3 of our kids were hospitalized with RSV at the same time so it was very hard and very stressful. (33 wGA, 60, O) Note this quote was repeated under Routine Disruption/Separation From Other Children at Discharge. | |
| Discharge | Makes me want to keep her in a bubble. (35 wGA, 90, F) | |
| 2 weeks | He was in a lot of pain and was screaming all the time due to his ear infection. He wasn’t feeding well. It was very difficult for me to see him in pain and there was nothing I could do to soothe him. It was very draining for the both of us. He hasn’t been himself since he got RSV. (33 wGA, 50, M) | |
| 1 month | The hospitalization was very stressful on all of us. This illness is very worrisome. I had stress headaches and couldn’t sleep. (35 wGA, 90, M) | |
| Routine disruption/separation from other children | Discharge | Husband has missed work. Other children [siblings] are upset. Grandmother had to babysit a lot [for siblings], and it interrupted her normal daily activities. (32 wGA, 70, M) |
| Discharge | The other children want mother and dad and they are not available and the children are not used to this. They are used to their parents being around a lot because of the home-based business. (34 wGA, 80, M) | |
| 1 month | We are still being very cautious with the baby. I don’t want to take him to the store with the public and all the germs so I have to do my shopping on line. If I knew about RSV immunoprophylaxis, I would have paid for it myself. We are wiser from this experience but it’s been tough. We watch his every movement and re-think his every cry. I don’t have comfort anymore. I am afraid that something else can happen and he can become that sick again. (35 wGA, 90, M) Note this quote was repeated under Other Comments at 1 Month. | |
| Family relationship | Discharge | It has been terrible. It is very stressful. I haven’t been able to be with my wife and child when I need to be because of work. (35 wGA, 65, F) |
| 1 week | Alarming, stressful, gut wrenching. Initially separated the family and then brought everyone closer together ultimately. Nothing more important than our children. Gelled the family together. Increased our faith. (31 wGA, 40, F) | |
| 1 month | It has been very draining emotionally and physically. It has affected his father’s job. Stressful and I am still trying to get back into my routine. (33 wGA, 100, M) | |
| Financial | Discharge | I lost my job during this time because of missed work. I was working 32 hours a week but when he got put in the hospital I just couldn’t go to work. (32 wGA, 50, M) |
| Discharge | Son missed 1 week of school because staying with mother-in-law in another town; $25/day for food ($200 total), won’t be able to pay all the bills this month. (34 wGA, 70, M) Note this quote was repeated under Routine Disruption/Separation from Other Children at Discharge | |
| 2 weeks | Very worried. Mother lost job due to time away from work to care for baby. Family evicted from home and moved in with family. (35 wGA, 40, M) | |
| 1 week | Got laid off mostly because of her being sick, so that’s a pretty big impact. Her breathing is still not too great. (34 wGA, 80, F) | |
| 1 week | Mom had to quit a job she only held for a few weeks to stay home with the babies until they were well enough to go back to day care. (29 wGA, 70, M) | |
| Coordinating care | Discharge | It was very difficult as I have 3 other children who were staying at their grandparents’ house. It was hard since they didn’t see me at all during the hospitalization. It took a huge toll on all of us. It was very draining. (33 wGA, 95, M) Note this quote was repeated under Sleep/Energy Impact at Discharge. |
| Discharge | I missed my fifth anniversary with my husband. I canceled 2 meetings, one work related and one personal. Other family had to miss work to help with other children. (32 wGA, 40, M) | |
| Discharge | She is a constant worry. I have another child who I cannot see when she is in hospital. I worry about other illnesses, flu and GI. My 3-year-old stayed with her dad but he doesn’t want to watch her again and says he won’t help anymore. My job gets upset when I cannot work and I need to work to provide. (30 wGA, 30, M) | |
| Discharge | Sister-in-law had to change her flight since longer hospitalization than expected. Father-in-law drove 2200 miles to help. Husband had to take time off work and multitask making a bigger deal. Two different hospital ED visits, ambulance ride, and office visit. (34 wGA, 70, M) | |
| Medical concerns | 1 week | A lot. He was intubated 3 times, has severe damage to the throat, and emergency tracheotomy. (34 wGA, 50, M) |
| 1 month | Infant continues to struggle with breathing through her nose. She has a hard time drinking bottles, swallowing more solid foods due to congestion and is still breathing mostly through her mouth. (31 wGA, 50, M) | |
| Sleep/energy impact | Discharge | It has been very difficult. The baby [patient] got sick first and then my 13-month-old child got it. It’s very scary. Even when I was working, I had to call home every hour because I was so worried about the baby. I haven’t slept in days. There is nothing worse to see then your child having trouble breathing. (29 wGA, 50, M) Note this quote was repeated under Other Comments at Discharge. |
| 1 week | Mom wakes up at night and worries when he’s asleep, afraid he’ll get sick and will have to be hospitalized again. (34 wGA, 70, M) | |
| 1 week | I am a working/single parent of 6 kids; live 1-hour away. Infant illness has been very stressful. There is no time for other kids. I leave work at 5 pm to go the hospital to care for my sick baby. I leave the hospital at 10 pm; get home at 11 pm to do household work. I get little sleep. This has been going on for 2 weeks now. I’m worried about my baby’s health. I’m willing to do anything to help. I feel this study is important. (34 wGA, 80, M) | |
| Discharge | I have been so worried about my grandson. I also worry about my daughter because she is so worried about the baby. None of us have been sleeping because we are so worried. (32 wGA, 0, O) | |
| Infant better/-back to normal | 2 weeks | [Baby’s name] is doing great. It was like waking up after a bad dream. We had a follow-up appointment with the PCP who was very happy with [Baby’s name]’s fast recovery. (35 wGA, 95, M) |
| Other comments | 1 week | They are relieved and thankful for the good care he got at [hospital]. They really wanted the shot and are very disappointed that they had to go through all of this [hospitalization]. (34 wGA, 70, F) |
| 2 weeks | This has been very stressful. I wish there had been some way I could have prevented my child from getting sick. (32 wGA, 45, O) |
Abbreviations: ED, emergency department; PCP, primary care physician; RSVH, respiratory syncytial virus-confirmed hospitalization; wGA, weeks’ gestational age.
Open-ended, qualitative responses include the infant’s gestational age, caregiver rating (scale of 0 to 100) of infant’s current health at the respective time point, and caregiver type (M = mother; F = father; and O = other).
Figure 4.
Caregiver-reported impact of infant’s RSVH. Caregiver responses could be grouped into multiple impact themes so the percentage at each time point will be >100%. More than one caregiver could provide responses for an infant.
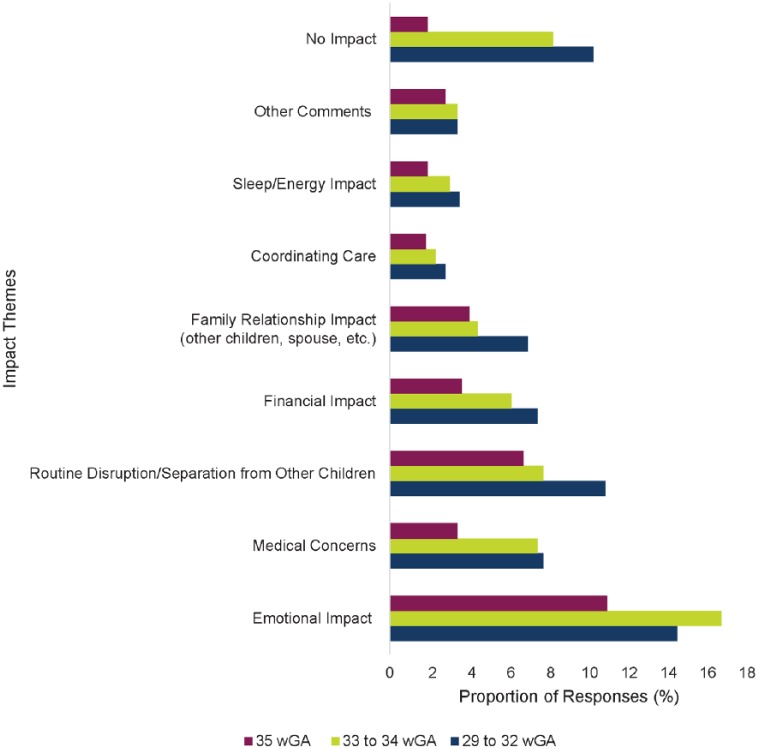
Caregiver Comments by Infant Gestational Age
To explore potential caregiver impact differences by infant gestational age, all time points and all caregiver responses were combined and the proportions of themes by the gestational age of the infant were produced (Figure 5). The most frequently raised issues (emotional impact, routine disruption/separation from other children, medical concerns, financial impact, and family relationship impact) that were uncovered by time point were still the most highly endorsed when viewing the data by infant gestational age. There were some variations in caregiver responses by infant gestational age. For example, caregivers of infants 33 to 34 wGA reported a greater number of emotional impacts than caregivers of infants 29 to 32 wGA or 35 wGA. The caregivers of infants 29 to 32 wGA reported more disruptions to their routines than caregivers of infants in the other gestational age groups. Medical concerns were reported in similar frequency by caregivers in the 29 to 32 wGA and 33 to 34 wGA groups but much less in the 35 wGA group.
Figure 5.
Caregiver-reported impact of infant’s RSVH by gestational age group. The caregiver comments by wGA (weeks’ gestational age) cohort included 311 caregiver comments from the 29 to 32 wGA group, 283 comments from the 33 to 34 wGA group, and 148 comments from the 35 wGA group.
Discussion
The SENTINEL1 observational study aimed to characterize the infant and caregiver experience of RSVH among families of preterm infants 29 to 35 wGA who did not receive RSV IP following the 2014 update of the COID guidance.7 Caregivers of preterm infants hospitalized with confirmed RSV disease reported the highest levels of family and infant stress, absenteeism, presenteeism, and activity impairment at the time their infant was discharged from the hospital. Stress and impairment levels declined over time for all outcomes, but still persisted at 1 month post-discharge.
Leidy et al13 studied the magnitude of infant and family stress associated with RSV-related hospitalization and included a control cohort. The control group was matched on infant age, similar geographic area, preterm birth, and recruitment from hospital pediatric or neonatal ICU records. The sample included 46 RSV infants and 45 control infants. The study found that caregiver distress persisted after the infant was discharged from the hospital. Although the levels of anxiety among the caregivers declined after the infants were discharged, the levels of caregiver anxiety were still significantly higher than the caregiver control anxiety levels after 2 months from discharge (P < 0.001). Our findings were similar, in that the levels of caregiver stress improved after the infant’s discharge but were still present 1 month later.
The caregiver comments support the quantitative findings from this study and provide a description of the impacts from the perspective of caregivers. The caregivers reported impacts on all areas of their daily lives, including missed work, disruption in their routines, separation from their other children, impacts on their family relationships, needing to coordinate care for their children, and financial impacts. Although caregiver stress, infant stress, and caregiver-perceived infant health improved over time, the caregivers continued to report impacts such as emotional stress, disruption to their daily routines, financial concerns, and infant health concerns at the 1 month post-discharge time point. These impacts are often difficult to measure quantitatively, but the factors impacting the caregivers, the magnitude of the impacts, and the lasting nature of these impacts on caregivers should be considered when evaluating the RSV disease burden in preterm infants.
The caregiver comments from this research provide caregiver perspective into previously published RSVH research. For example, Leader et al19 studied time and out-of-pocket costs associated with RSVH. The research involved 36 full-term and 48 preterm infants (33 to 35 wGA). Caregivers were interviewed about their time and costs at discharge and 1 month post-discharge. The primary caregivers of the preterm infants reported an average total travel time of 6.8 hours (range = 0.13-48 hours) and an average of 133.6 hours in the hospital (range = 14-1080 hours).19 The out-of-pocket expenses for the preterm cohort was an average of $643.69 ($21-$16 867; standard deviation = $2403).19 The caregiver comments collected in this study illuminate quantified economic impact reports and present a humanistic quality to the caregiver’s experience.
Preventing severe RSV disease in this vulnerable preterm infant population could provide health benefits for the infants and avoidance of RSVH-related stress, as well as avoidance of stress and productivity loss for their caregivers. Our research quantifies the stress the caregivers were experiencing and their perception of the infant’s stress and includes qualitative data that have been systematically organized to summarize the caregiver burden. Caregiver stress should not be trivialized, particularly for caregivers of infants who were born preterm and may already be under stress from their newborn’s early arrival. Research among parents of hospitalized children from general pediatric wards shows elevated stress, which persisted after discharge. Franck et al20 conducted a prospective study among 107 parents who had a child hospitalized for at least 3 nights. The parents completed a questionnaire during their child’s hospitalization and again 3 months post-discharge. Even at 3 months post-discharge, 32.7% of the parents reported some post-traumatic stress symptoms.20 Another study, a meta-analysis of 13 studies, found that caregivers of children with chronic illness (asthma, cancer, cystic fibrosis, diabetes, epilepsy, juvenile rheumatoid arthritis, and/or sickle cell disease) had significantly higher general parenting stress than caregivers of healthy children (effect size d = 0.40, 95% confidence interval = 0.19-0.61, P ≤ .0001).21 Although the cohort included in this research among preterm infants with RSVH is different from other studies of caregiver stress, the insights to the caregivers’ ongoing stress are enlightening. The qualitative data throughout the caregiver experience demonstrate an impact that should be considered for holistic treatment and RSVH indirect burden. The data from this research suggest that there is a burden of RSVH on caregivers that would be important to have represented when assessing the impact of RSV. Often economic modeling of preterm birth is limited to health care resource utilization and caregiver productivity lost due to the infant’s hospitalization. Hodek et al22 suggest including intangible costs such as emotional distress and impacts on quality of life.
Unlike other countries, in the United States many mothers return to work when their infants are only a few weeks old, and they may not have the family support structure to help care for their newborns. A severe illness that results in hospitalization has many ramifications for the family, including inability of the parents to work. A substantial burden among caregivers was reported using the WPAI:CHRI and shown by the negative impact on absenteeism, presenteeism, daily activity impairment, and overall work productivity loss. The WPAI:CHRI scores at index RSVH discharge were higher for mothers compared with fathers, and this trend continued out to 1 month post-discharge. Notably, absenteeism scores indicated that fathers had far less absenteeism than mothers at 1 month post-discharge. A Canadian study by Mitchell et al23 also showed lost work productivity for both parents associated with their infant’s RSVH. The study included 67 infants and 19.4% were preterm (born before 34.5 weeks).23 The study revealed that average absenteeism was 49.0%, presenteeism was 51.4%, overall work impairment was 77.8%, and activity impairment was 81.7%.23 Although working fathers experienced more absenteeism, presenteeism, and overall work impairment compared with working mothers, working mothers reported more activity impairment than working fathers.23 In the Canadian study, only 9% of the mothers were employed or working at the time of the study. Although results cannot be directly compared, both the Canadian study and our study showed a negative impact on productivity for both mothers and fathers. The data from our research support the need for representation of the caregiver burden in decision-making for severe RSV disease.
There are several limitations to this study that should be noted. This research was observational, and no control group was included. The caregiver reports were collected by hospital research staff; therefore, verbatim quotations may not have been collected. Recall bias may be a factor as some caregivers reported their outcome information for all time points at 1 month post-discharge rather than at each time point as it occurred. Because the infants’ health and infant/caregiver stress levels improved over time, potential recall bias would likely be toward better health and less stress.
This research is consistent with previous findings reporting caregiver stress related to infant RSV-related hospitalization.13 The qualitative reports from caregivers over time provide a unique contribution to the literature. Data directly from the caregiver’s perspective open a window to the degree and breadth of the impacts on the whole family. These impacts should be considered when evaluating RSV disease burden.
Conclusions
Preterm infant RSVH adversely affects caregivers, resulting in missed work, diminished work productivity, emotional stress, disruption of family routine, and financial concerns. The impact of RSVH continues through at least 1 month post-discharge and should be included in evaluations of RSV disease burden in preterm infants. Preventing severe RSV disease in this vulnerable population would provide health benefits for the infant while avoiding RSVH-related stress for these infants and their caregivers.
Author Contributions
All authors participated in data analysis and interpretation and contributed to the development of the manuscript. The authors maintained control over the final content of the manuscript.
Acknowledgments
This study was sponsored by AstraZeneca. The authors would like to thank the families for participating in the SENTINEL1 study, the hospital study teams for their research, Maxine Langenfeld, MPH, for her analysis support, and Nancy K. Leidy, PhD, of Evidera for her comments on earlier versions of this article. Editorial support was provided by The Lockwood Group, which was in accordance with Good Publication Practice (GPP3) guidelines and funded by AstraZeneca.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Robin Pokrzywinski and Laura Swett are employees of Evidera, a contract research organization that received funds from AstraZeneca to conduct these analyses. Pia Pannaraj has received personal compensation for research support from AstraZeneca/MedImmune during the conduct of the study, and research support from Pfizer. Jumi Yi has received personal compensation from AstraZeneca/MedImmune for participation in speaker bureau activities. Veena Kumar was an employee of AstraZeneca at the time the study was completed. Melissa Pavilack and Kimmie McLaurin are employees of AstraZeneca.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this secondary analysis of the SENTINEL1 data was provided by AstraZeneca (Gaithersburg, MD).
ORCID iD: Robin Pokrzywinski  https://orcid.org/0000-0002-1781-8197
https://orcid.org/0000-0002-1781-8197
References
- 1. Leader S, Kohlhase K. Recent trends in severe respiratory syncytial virus (RSV) among US infants, 1997 to 2000. J Pediatr. 2003;143(suppl 51):S127-S132. [DOI] [PubMed] [Google Scholar]
- 2. Boyce TG, Mellen BG, Mitchel EF, Jr, Wright PF, Griffin MR. Rates of hospitalization for respiratory syncytial virus infection among children in Medicaid. J Pediatr. 2000;137:865-870. [DOI] [PubMed] [Google Scholar]
- 3. Hall CB, Weinberg GA, Blumkin AK, et al. Respiratory syncytial virus-associated hospitalizations among children less than 24 months of age. Pediatrics. 2013;132:e341-e348. [DOI] [PubMed] [Google Scholar]
- 4. The Impact-RSV Study Group. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics. 1998;102(3 pt 1):531-537. [PubMed] [Google Scholar]
- 5. Blanken MO, Rovers MM, Molenaar JM, et al. ; Dutch RSV Neonatal Network. Respiratory syncytial virus and recurrent wheeze in healthy preterm infants. N Engl J Med. 2013;368:1791-1799. [DOI] [PubMed] [Google Scholar]
- 6. Feltes TF, Cabalka AK, Meissner HC, et al. ; Cardiac Synagis Study Group. Palivizumab prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant congenital heart disease. J Pediatr. 2003;143:532-540. [DOI] [PubMed] [Google Scholar]
- 7. American Academy of Pediatrics Committee on Infectious Diseases; American Academy of Pediatrics Bronchiolitis Guidelines Committee. Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics. 2014;134:415-420. [DOI] [PubMed] [Google Scholar]
- 8. American Academy of Pediatrics. Respiratory syncytial virus. In: Pickering LK, Kimberlin DW, Long SS, eds. Red Book: 2012 Report of the Committee on Infectious Diseases. 29th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2012:609-618. [Google Scholar]
- 9. Committee on Infectious Diseases. From the American Academy of Pediatrics: policy statements–modified recommendations for use of palivizumab for prevention of respiratory syncytial virus infections. Pediatrics. 2009;124:1694-1701. [DOI] [PubMed] [Google Scholar]
- 10. Anderson EJ, Krilov LR, DeVincenzo JP, et al. SENTINEL1: an observational study of respiratory syncytial virus hospitalizations among US infants born at 29 to 35 weeks’ gestational age not receiving immunoprophylaxis. Am J Perinatol. 2017;34:51-61. [DOI] [PubMed] [Google Scholar]
- 11. Busse M, Stromgren K, Thorngate L, Thomas KA. Parents’ responses to stress in the neonatal intensive care unit. Crit Care Nurse. 2013;33:52-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Franck LS, Cox S, Allen A, Winter I. Parental concern and distress about infant pain. Arch Dis Child Fetal Neonatal Ed. 2004;89:F71-F75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Leidy NK, Margolis MK, Marcin JP, et al. The impact of severe respiratory syncytial virus on the child, caregiver, and family during hospitalization and recovery. Pediatrics. 2005;115:1536-1546. [DOI] [PubMed] [Google Scholar]
- 14. Miles MS, Burchinal P, Holditch-Davis D, Brunssen S, Wilson SM. Perceptions of stress, worry, and support in Black and White mothers of hospitalized, medically fragile infants. J Pediatr Nurs. 2002;17:82-88. [DOI] [PubMed] [Google Scholar]
- 15. Spear ML, Leef K, Epps S, Locke R. Family reactions during infants’ hospitalization in the neonatal intensive care unit. Am J Perinatol. 2002;19:205-213. [DOI] [PubMed] [Google Scholar]
- 16. Kopacz NY, Predeger E, Kelley CM. Experiences of Alaskan parents with children hospitalized for respiratory syncytial virus treatment. J Pediatr Nurs. 2013;28:e19-e21. [DOI] [PubMed] [Google Scholar]
- 17. Reilly MC, Mitchell I, Gooch K, et al. PRM29 preliminary validation of the work productivity activity impairment (WPAI) in caregivers of children hospitalized for respiratory illness (WPAI:CHRI) in Germany and Canada. Value Health. 2012;15:A650. [Google Scholar]
- 18. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353-365. [DOI] [PubMed] [Google Scholar]
- 19. Leader S, Yang H, DeVincenzo J, Jacobson P, Marcin JP, Murray DL. Time and out-of-pocket costs associated with respiratory syncytial virus hospitalization of infants. Value Health. 2003;6:100-106. [DOI] [PubMed] [Google Scholar]
- 20. Franck LS, Wray J, Gay C, Dearmun AK, Lee K, Cooper BA. Predictors of parent post-traumatic stress symptoms after child hospitalization on general pediatric wards: a prospective cohort study. Int J Nurs Stud. 2015;52:10-21. [DOI] [PubMed] [Google Scholar]
- 21. Cousino MK, Hazen RA. Parenting stress among caregivers of children with chronic illness: a systematic review. J Pediatr Psychol. 2013;38:809-828. [DOI] [PubMed] [Google Scholar]
- 22. Hodek JM, von der Schulenburg JM, Mittendorf T. Measuring economic consequences of preterm birth—methodological recommendations for the evaluation of personal burden on children and their caregivers. Health Econ Rev. 2011;1:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mitchell I, Defoy I, Grubb E. Burden of respiratory syncytial virus hospitalizations in Canada. Can Respir J. 2017;2017:4521302. [DOI] [PMC free article] [PubMed] [Google Scholar]