Abstract
The Prospective comparison of Angiotensin Receptor-neprilysin inhibitor (ARNI) with Angiotensin converting enzyme inhibitor (ACEI) to Determine Impact on Global Mortality and morbidity in Heart Failure (HF) trial (PARADIGM-HF) showed that adding a neprilysin inhibitor (sacubitril) to a renin-angiotensin system blocker (and other standard therapy) reduced morbidity and mortality in ambulatory patients with chronic HF with reduced ejection fraction (HFrEF). In PARADIGM-HF, valsartan combined with sacubitril (a so-called ARNI) was superior to the current gold standard of an ACEI, specifically enalapril, reducing the risk of the primary composite outcome of cardiovascular (CV) death or first HF hospitalization by 20% and all-cause death by 16%. Following the results of PARADIGM-HF, sacubitril/valsartan was approved by American and European regulatory authorities for the treatment of HFrEF. The burden of HF in Asia is substantial, both due to the huge population of the region and as a result of increasing CV risk factors and disease. Both the prevalence and mortality associated with HF are high in Asia. In the following review, we discuss the development of sacubitril/valsartan, the prototype ARNI, and the available evidence for its efficacy and safety in Asian patients with HFrEF.
Keywords: Asians, Sacubitril/valsartan, Heart failure
INTRODUCTION
Heart failure (HF) is a major global public health problem affecting an estimated 26 million people around the world.1) Asia accounts for more than 60% of the global population and more than two-thirds of the continent's countries are categorized as low- and middle-income countries. The increasing burden of cardiovascular (CV) disease in Asia is usually attributed to the increasing prevalence of risk factors such as obesity and diabetes.2),3),4) Consequently, the burden of HF has also increased, with prevalence estimates in Asia ranging from 1–5%, compared to 1–2% in Europe and North America. The overall prevalence in is estimated to be 4.2 million in China and 1.3–4.6 in India.2),3),4),5) Moreover, unlike the West, where HF incidence rates have been stabilizing, the incidence of HF continues to rise in Asia, with an estimated 500,000 new cases in China alone and another 0.5–1.8 million new cases in India each year.3) As a result of its large population, and the changing epidemiology of CV risk factors and disease in the region, more people are now living with HF in Asia than anywhere else in the world.
Of added concern, Asian patients with HF are younger and show worse survival than the global average.2),3) It has also been suggested that there may be differences between Asians and other races in the tolerability, efficacy and safety of CV drugs, potentially diminishing their value.6),7)
The most recent breakthrough in the pharmacological management of HF was the demonstration that adding a neprilysin inhibitor (sacubitril) to a renin-angiotensin system blocker (and other standard therapy) reduced morbidity and mortality in patients with chronic, symptomatic, ambulatory HF with reduced ejection fraction (HFrEF). In the Prospective comparison of Angiotensin Receptor-neprilysin inhibitor (ARNI) with Angiotensin converting enzyme inhibitor (ACEI) to Determine Impact on Global Mortality and morbidity in HF trial (PARADIGM-HF), valsartan combined with sacubitril (ARNI) was superior to the current gold standard of an ACEI, specifically enalapril, reducing the risk of the primary composite outcome of CV death or first HF hospitalization by 20% and all-cause death by 16%.8) The results of PARADIGM-HF led to the approval of sacubitril/valsartan by American and European regulatory authorities, among others, for the treatment of HFrEF and its recommendation in international guidelines.9),10)
In light of the considerable burden of HFrEF and disease associated mortality in Asia, the purpose of this article is to review the development of ARNIs and the evidence for their efficacy and safety in Asian patients with HFrEF.
NATRIURETIC PEPTIDES AND NEPRILYSIN
Myocardial damage, most commonly as a result of poorly controlled hypertension, myocardial ischaemia or infarction, results in activation of the renin-angiotensin-aldosterone system (RAAS). Whilst initially compensatory to help maintain cardiac output, prolonged and sustained RAAS activation can have detrimental effects including increasing cardiac afterload due to vasoconstriction, promoting myocardial fibrosis and fluid retention secondary to an anti-natriuretic action. Ultimately these processes become deleterious and result in the development of the syndrome of HF and its progressive worsening over time.
The natriuretic peptides (NPs) are a family of vasoactive peptides which are released by the heart, in response to increased myocardial wall stress, and from blood vessels and the kidneys. The NPs help to nullify the harmful effects of an overactive RAAS. The first NP to be described was atrial NP (ANP), when in 1981, de Bold et al.11) demonstrated the increased urinary sodium and water excretory effect of atrial extracts. Subsequently, B-type NP (BNP), C-type NP (CNP) and urodilatin were identified, sharing the beneficial vasodilatory, natriuretic, anti-fibrotic and anti-hypertrophic properties of ANP.12)
The potential benefits of the NPs, including amelioration of the effects of RAAS overactivity, led to several lines of research into how these peptides might be used therapeutically. One obvious approach was short-term intravenous administration of supra-physiological does of exogenous NP in patients hospitalised with decompensated HF. However, in 2 trials neither nesiritide (a recombinant form of BNP) nor ularitide (a recombinant form of urodilatin) reduced mortality or re-hospitalization.13),14)
The alternative, and ultimately successful, approach was to augment level of endogenous NPs by reducing their elimination which occurs through 2 major pathways. One is through a NP clearance receptor (NPRC or NPRC3) and the other is through degradation by the enzyme neprilysin (also known as membrane metallo-endopeptidase or neutral endopeptidase [NEP]), a membrane bound endopeptidase found in many tissues, most prominently in the kidney.15),16)
It is important to note that neprilysin also plays a role in the degradation several other peptides including bradykinin, adrenomedullin, substance P and calcitonin, apelin, glucagon-like peptide-1, vasoactive intestinal peptide, and enkephalins and these other substrates may contribute to the benefits of neprilysin inhibition.17),18)
NEPRILYSIN INHIBITION
Roques and colleagues in 1980 reported the first neprilysin inhibitor, thiorphan in animal models with demonstration of favourable hemodynamic and hormonal responses.19),20) Early reports showed that acute inhibition of neprilysin with oral racecadotril (formerly acetorphan) and intravenous candoxatrilat demonstrated stimulation of natriuresis and diuresis along with increases in circulating ANP levels in humans without any associated deleterious activation of RAAS or sympathetic activity as observed with loop diuretics.21),22),23),24) Furthermore, it was also seen that candoxatrilat and ecadotril reduced pulmonary capillary wedge pressure in patients with HF.21),23)
However, it was subsequently demonstrated that chronic dosing with candoxatril did not lead to a sustained reduction in blood pressure and development of the drug was consequently halted.25) The amelioration of the hypotensive action of this agent likely resulted from accumulation of angiotensin II, the breakdown of which was inhibited by candoxatril, and which offset the vasodilatory effects of NP accumulation.26),27) In retrospect, this finding demonstrated the need to combine neprilysin inhibition with blockade of the renin-angiotensin system.
ANGIOTENSIN CONVERTING ENZYME-NEUTRAL ENDOPEPTIDASE INHIBITION
The first approach to combining neprilysin inhibition with renin-angiotensin system blockade was using molecules that inhibited both ACE and NEP, the most studied of which was omapatrilat.28)
In the Inhibition of Metalloprotease by Omapatrilat in a Randomized Exercise and Symptoms Study (IMPRESS) in HF trial, omapatrilat was compared to lisinopril to assess for improvement in functional capacity and clinical outcomes in 573 patients with HFrEF.29) While there was no significant difference seen in the primary outcome of exercise tolerance, a positive trend was seen in favour of omapatrilat in reducing the composite of death, admission or discontinuation of study treatment for worsening HF.
Two years later, the results of the Omapatrilat Versus Enalapril Randomized Trial of Utility in Reducing Events (OVERTURE) trial, a randomised controlled trial of omapatrilat 40 mg once daily compared to enalapril 10 mg twice daily, were published.30) There was no benefit of omapatrilat over enalapril in reduction of the primary endpoint of all-cause death or HF hospitalization. However, a nominally statistically significant 9% reduction in the secondary endpoint of all-cause death and CV hospitalization was seen in patients randomized to receive omapatrilat. Moreover, in a post hoc analysis of the primary end point using the definition used in the Studies Of Left Ventricular Dysfunction (SOLVD) treatment trial there was an 11% lower risk in patients treated with omapatrilat (nominal, p=0.012).30) In retrospect, it also appeared that the single large daily dose of omapatrilat used in OVERTURE led to excessive hypotension and study drug discontinuation, while at the same time failed to provide sustained 24-hour inhibition of either neprilysin or the renin-angiotensin system. Together, these considerations suggested that, used in the right way, combined neprilysin and renin-angiotensin system inhibition might still be useful in HF. However, further development of omapatrilat was halted because of an excessively high rate of serious angioedema, particularly in the Omapatrilat Cardiovascular Treatment Assessment Versus Enalapril trial (OCTAVE) in hypertension where 2.2% of patients randomized to omapatrilat had angioedema compared to 0.7% of those randomized to enalapril.31) The higher rate of angioedema observed with omapatrilat was felt to be secondary to the accumulation of bradykinin, resulting from combined ACE and neprilysin inhibition (because both enzymes breakdown bradykinin). Omapatrilat was later found to also inhibit aminopeptidase-P, another key enzyme involved in degradation of bradykinin.32)
ANGIOTENSIN RECEPTOR-NEPRILYSIN INHIBITORS
The solution to the problem of safely combining neprilysin and renin-angiotensin system inhibition was solved by using an angiotensin receptor blocker (ARB), instead of an ACE inhibitor, and the development of sacubitril/valsartan.
Sacubitril/valsartan (originally named LCZ696) is the first in class ARNI, and is a 1:1 combination of AHU377 (sacubitril) and an ARB (valsartan).33) Upon oral administration, sacubitril/valsartan dissociates and sacubitril is converted to its active metabolite sacubitrilat. Sacubitrilat and valsartan have half-lives of approximately 12 and 9.9 hours respectively and given twice daily ensure sustained neprilysin and RAAS inhibition over the 24-hour period.34) The valsartan formulation in sacubitril/valsartan is more bioavailable than conventional valsartan, with a 40% higher systemic exposure per mg of drug.35) Consequently, the target dose of sacubitril/valsartan (97/103 mg twice daily) gives plasma concentrations of valsartan equivalent to 160 mg twice daily of the conventional compound (the dose as studied in the Valsartan Heart Failure Trial [Val-HeFT]).36) This dose also gives a sustained increase in cyclic guanosine monophosphate, reflecting the second-messenger response to the increase in natriuretic (and possibly other) peptides resulting from neprilysin inhibition by sacubitrilat.37)
PROSPECTIVE COMPARISON OF ANGIOTENSIN RECEPTOR-NEPRILYSIN INHIBITOR WITH ANGIOTENSIN CONVERTING ENZYME INHIBITOR TO DETERMINE IMPACT ON GLOBAL MORTALITY AND MORBIDITY IN HEART FAILURE (PARADIGM-HF) TRIAL
PARADIGM-HF was designed to test the efficacy and safety of adding a neprilysin inhibitor (sacubitril) to a renin-angiotensin system blocker (and other standard therapy), compared with a renin-angiotensin system blocker (and other standard therapy) alone. Specifically, sacubitril/valsartan 97/103 mg twice daily was compared to enalapril 10 mg twice daily.8) The choice of comparator, enalapril 10 mg twice daily, was based on the evidence from the SOLVD-Treatment trial, the only large-scale, long-term, trial in a broad ambulatory HFrEF population, demonstrating superiority of and ACE inhibitor compared to placebo in reducing morbidity and mortality in HFrEF.38) For this reason enalapril 10 mg twice daily has been the “gold-standard” comparator in other trials and is the most studied ACE inhibitor in HFrEF trials (Table 1).
Table 1. Characteristics of large trials in HF with enalapril.
| Trial | No. of patients assigned to enalapril | Target dose (mg) | Mean daily dose (mg) |
|---|---|---|---|
| CONSENSUS (1987)54) | 127 | 20 bid | 18.4 |
| SOLVD-T (1991)38) | 1,285 | 10 bid | 16.6 |
| SOLVD-P (1992)55) | 2,111 | 10 bid | 16.7 |
| V-HeFT II (1991)56) | 403 | 10 bid | 15.0 |
| OVERTURE (2002)30) | 2,884 | 10 bid | 17.7 |
| CARMEN (2004)57) | 190 enalapril only | 10 bid | 16.8 |
| 191 enalapril plus carvedilol | 10 bid | 14.9 | |
| CIBIS-3 (2005)58) | 505 enalapril first | 10 bid | 17.2 |
| 505 bisoprolol first | 10 bid | 15.8 | |
| ATMOSPHERE (2016)59) | 2,336 enalapril only | 5–10 bid | 18.6 |
| 2,340 aliskiren plus enalapril | 5–10 bid | 19.1 |
ATMOSPHERE = Aliskiren Trial to Minimize Outcomes in Patients with Heart Failure; CARMEN = Carvedilol ACE-Inhibitor Remodelling Mild CHF EvaluatioN; CIBIS = Cardiac Insufficiency Bisoprolol Study; CONSENSUS = Cooperative North Scandinavian Enalapril Survival Study; HF = heart failure; OVERTURE = Omapatrilat Versus Enalapril Randomized Trial of Utility in Reducing Events; SOLVD = Studies Of Left Ventricular Dysfunction; V-HeFT = Vasodilator-Heart Failure Trial.
Patients were recruited between 2009 and 2012. All patients underwent a sequential run-in period first with enalapril 10 mg twice daily followed by sacubitril/valsartan 97/103 mg twice daily for a total of 6–8 weeks. If no unacceptable side-effects were seen, patients were randomized 1:1 in a double-blind fashion to either sacubitril/valsartan 97/103 mg twice daily or enalapril 10 mg twice daily and followed up for occurrence of prespecified outcomes (or adverse events). PARADIGM-HF was terminated early in March 2014 on the recommendation of the Data Monitoring Committee due to overwhelming benefit observed with sacubitril/valsartan therapy. The median duration of follow-up in PARADIGM-HF was 27 months.
CLINICAL EFFICACY OF SACUBITRIL/VALSARTAN IN PARADIGM-HF
Sacubitril/valsartan significantly reduced the risk of the primary composite outcome (hazard ratio [HR], 0.80; 95% confidence interval [CI], 0.73–0.87) and each of its components i.e. CV death (HR, 0.80; 95% CI, 0.71–0.89) and HF hospitalization (HR, 0.79; 95% CI, 0.71–0.89). Equal and significant reductions in the risk of the 2 major modes of CV death, sudden death and death from worsening HF, were also observed, and there was a 16% (95% CI, 7–24%) reduction in the risk of all-cause mortality.39)
Hence, for every 1,000 patients switched from enalapril to sacubitril/valsartan, there would be 46 fewer primary composite endpoint events, 27 fewer first HF hospitalisations, 31 fewer CV deaths and 28 fewer deaths from any cause over a follow-up of 27 months.
In addition, subsequent post-hoc analyses of PARADIGM-HF have shown no difference in the benefit of therapy with sacubitril/valsartan compared to enalapril according to age or to geographical region of enrolment (which will be discussed more with respect to Asia in later sections).40),41) No other significant treatment effect interactions were seen in any of the other prespecified sub-groups or in relation to background drug or device therapy.8),42)
SAFETY AND TOLERABILITY OF SACUBITRIL/VALSARTAN IN PARADIGM-HF
Patients randomized to sacubitril/valsartan had significantly more hypotension than patients randomized to enalapril (14% vs. 9%; p<0.001) even though study-drug discontinuation as a result of hypotension was very rare and not significantly different between the treatment groups (0.9% vs. 0.7%; p=0.380). No significant difference in the rate of angioedema was reported (19 patients vs. 10 patients; p=0.130). Renal dysfunction, hyperkalaemia and cough were less commonly reported with sacubitril/valsartan compared to enalapril. Dementia and cognition related adverse events were not increased by sacubitril/valsartan in PARADIGM-HF.43)
REGULATORY APPROVAL AND STATISTICAL ROBUSTNESS OF RESULTS
The results of PARADIGM-HF were swiftly followed by regulatory approval of sacubitril/valsartan for use in patients with HFrEF and conforming to the main inclusion criteria used in the trial. Regulatory approval of a new drug requires that its effectiveness and safety be demonstrated in either 2 trials with a 2-sided p value<0.05, or a single, large, internally consistent multicentre study with a p value<0.00125. PARADIGM-HF was a large (8,399 patients), highly statistically significant (p value=0.0000004), internally consistent (lack of subgroup interaction), multicentre (sites in 47 countries) study with large treatment effects on morbidity and mortality. As a result of the robustness of the results of PARADIGM-HF it has been considered unethical to conduct a second large clinical trial with sacubitril/valsartan in patients HFrEF. With a p value of 0.0000004 for the primary composite outcome, the chance that sacubitril/valsartan is not superior to enalapril is less than one in a million.44)
On the basis of a single trial providing evidence of benefit, the American College of Cardiology (ACC) and the European Society of Cardiology guidelines have afforded sacubitril/valsartan a class I, level of evidence B treatment recommendation for use in HFrEF to reduce HF hospitalization and mortality in patients who remain symptomatic despite pharmacotherapy with ACE/ARB, a beta blocker and a mineralocorticoid antagonist.9),10) A meta-analysis of the 3 trials (PARADIGM-HF, IMPRESS, and OVERTURE) comparing combined neprilysin/RAAS inhibition to RAAS inhibition alone in HFrEF, reported a significant pooled HR in reducing the risk of a composite endpoint of all-cause mortality or HF hospitalisation (HR, 0.86; 95% CI, 0.76–0.97).45) Based on the results of this meta-analysis, as well as the degree of statistical certainty of benefit reported in PARADIGM-HF, we believe it can be reasonably argued that the body of evidence in favour of neprilysin inhibition supports a level of evidence A recommendation for treatment with sacubitril/valsartan in patients with symptomatic HFrEF, with now additional support for comParIson Of sacubitril/valsartaN versus Enalapril on Effect on nt-pRo-bnp in patients stabilized from an acute Heart Failure episode (PIONEER-HF; see below).
PARADIGM-HF required patients to be tolerant of a dose of an ACE-inhibitor or ARB equivalent to enalapril 10 mg/day prior to enrolment. Several trials now support the use of sacubitril/valsartan in ACE-inhibitor or ARB naïve patients including those stabilised from presentations of acutely decompensated HF (a proportion of which we first or “de novo” presentations). The ACC guidance permits prescription of sacubitril/valsartan to ACEI/ARB naïve patients, a strategy which is supported by the results of the TITRATION and TRANSITION studies.46),47) Sacubitril/valsartan was also found to result in a greater reduction in the N-terminal prohormone of BNP levels, compared to enalapril, among patients hospitalized for acute decompensated HF in the PIONEER-HF trial.48) A significant reduction in risk of rehospitalization for HF was also seen, although the trial was not powered for clinical outcomes.
There are a number of ongoing studies to assess the efficacy and safety of sacubitril/valsartan in other populations. Among them, the 2 that require mention here are the Prospective Comparison of ARNI with ARB Global Outcomes in HF With Preserved Ejection Fraction (PARAGON-HF; NCT01920711) trial and the Prospective ARNI vs. ACE Inhibitor Trial to Determine Superiority in Reducing HF Events After MI (PARADISE-MI; NCT02924727).49) PARAGON-HF will evaluate the efficacy of sacubitril/valsartan compared to valsartan in reducing morbidity and mortality in patients with HF with preserved ejection fraction (HFpEF). It is the largest and the most globally representative HFpEF clinical trial to date and the results are expected this year.50) PARADISE-MI will assess the effect of sacubitril/valsartan compared to ramipril in reducing the occurrence of the composite endpoint of CV death, HF hospitalization and outpatient HF in post-acute MI patients with left ventricular systolic dysfunction and/or pulmonary congestion with no prior history of chronic HF.
ASIANS IN THE PARADIGM-HF TRIAL
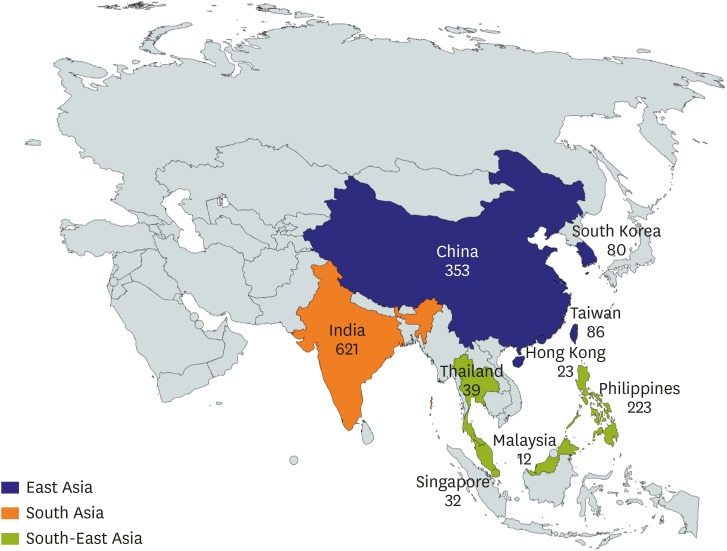
A total of 1,487 patients were enrolled from 9 countries in the Asia-Pacific region in PARADIGM-HF, accounting for 17.7% of the total cohort.8) For the purposes of this review, we have further divided Asia in PARADIGM-HF into 3 regions (East, South, and South-East Asia; Figure 1) and considered only those living in these countries who self-reported as being of Asian race.
Figure 1. Number of patients of Asian patients by region enrolled in PARADIGM-HF (Asian race only).
PARADIGM-HF = Prospective comparison of Angiotensin Receptor-neprilysin inhibitor with Angiotensin converting enzyme inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure trial.
A prior post-hoc analysis of PARADIGM-HF by region showed that patients from Asia were the youngest, had the lowest body mass index, lowest systolic blood pressure, reported a better quality of life and had fewer comorbidities.41) These findings were largely replicated in the Asian subgroups that we have analysed for this review and are shown in Table 2. In the analysis presented by Kristensen et al.,41) patients from Asia were most likely to receive digoxin and less likely to receive all other drugs and device therapies at the time of randomisation. It was also reported that while the risk of the primary composite end-point was highest in patients from Asia compared to North America (HR, 1.39; 95% CI, 1.06–1.80), there was no difference in treatment effect seen overall (p value for interaction-primary composite outcome=0.50).41)
Table 2. Baseline characteristics of all patients and by Asian regions enrolled in PARADIGM-HF.
| Overall (n=8,399) | All Asia (n=1,469) | East Asia (n=542) | South Asia (n=621) | South-East Asia (n=306) | |||
|---|---|---|---|---|---|---|---|
| Age (years) | 63.8±11.4 | 57.8±11.9 | 59.7±11.9 | 57.1±11.7 | 56.0±11.8 | ||
| Sex (female) | 1,832 (21.8) | 287 (19.5) | 96 (17.7) | 134 (21.6) | 57 (18.6) | ||
| SBP (mmHg) | 121±15 | 117±15 | 116±14.6 | 117±13 | 119±17 | ||
| Heart rate (bpm) | 72±12 | 75±11 | 73±12 | 77±9 | 75±13 | ||
| BMI (kg/m2) | 28.1±5.5 | 24.3±4.1 | 25.0±3.8 | 23.5±3.9 | 24.6±4.8 | ||
| Serum creatinine (mg/dL) | 1.12±0.3 | 1.06±0.3 | 1.05±0.3 | 1.03±0.3 | 1.15±0.3 | ||
| Clinical features of HF | |||||||
| Ischemic cardiomyopathy | 5,036 (60.0) | 855 (58.2) | 209 (38.6) | 449 (72.3) | 197 (64.4) | ||
| LVEF (%) | 29.5±6.2 | 28.1±5.9 | 29.5±5.3 | 27.5±5.8 | 27.0±6.6 | ||
| Median NT-proBNP (pg/mL) | 1,615 (888–3,231) | 1,731 (914–3,700) | 1,775 (934–3,828) | 1,530 (832–3,105) | 2,147 (1,077–4,679) | ||
| Median KCCQ CSS | 80 (63–92) | 89 (79–96) | 91 (82–97) | 87 (77–96) | 89 (71–97) | ||
| NYHA class | |||||||
| I | 389 (4.6) | 119 (8.1) | 23 (4.3) | 37 (6.0) | 59 (19.3) | ||
| II | 5,919 (70.6) | 1,164 (79.3) | 426 (78.7) | 503 (81.0) | 235 (76.8) | ||
| III | 2,018 (24.1) | 182 (12.4) | 92 (17.0) | 78 (12.6) | 12 (3.9) | ||
| IV | 60 (0.7) | 3 (0.2) | 0 (0.0) | 3 (0.5) | 0 (0.0) | ||
| Medical history | |||||||
| Hypertension | 5,940 (70.7) | 714 (48.6) | 276 (50.9) | 258 (41.5) | 180 (58.8) | ||
| Diabetes | 2,907 (34.6) | 510 (34.7) | 176 (32.5) | 230 (37.0) | 104 (34.0) | ||
| Atrial fibrillation | 3,091 (36.8) | 247 (16.8) | 155 (28.6) | 32 (5.2) | 60 (19.6) | ||
| MI | 3,634 (43.3) | 503 (34.2) | 150 (27.7) | 262 (42.2) | 91 (29.7) | ||
| Stroke | 725 (8.6) | 89 (6.1) | 42 (7.7) | 13 (2.1) | 34 (11.1) | ||
| Hospitalization for HF | 5,274 (62.8) | 888 (60.4) | 415 (76.6) | 288 (46.4) | 185 (60.5) | ||
| Pretrial use of ACEI | 6,532 (77.8) | 996 (67.8) | 334 (61.6) | 491 (79.1) | 171 (55.9) | ||
| Pretrial use of ARB | 1,892 (22.5) | 474 (32.3) | 207 (38.2) | 132 (21.3) | 135 (44.1) | ||
| Current smoker | 1,208 (14.4) | 967 (14.0) | 152 (28.0) | 50 (8.1) | 39 (12.7) | ||
| Clinical features | |||||||
| Dyspnoea at rest | 309 (3.7) | 19 (1.3) | 4 (0.7) | 11 (1.8) | 4 (1.3) | ||
| Dyspnoea on effort | 7,207 (86.0) | 1,146 (78.2) | 420 (77.6) | 570 (91.8) | 156 (51.3) | ||
| PND | 399 (4.8) | 40 (2.7) | 8 (1.5) | 27 (4.3) | 5 (1.7) | ||
| Orthopnoea | 608 (7.3) | 53 (3.6) | 5 (0.9) | 26 (4.2) | 22 (7.3) | ||
| JVD | 818 (9.8) | 83 (5.7) | 18 (3.3) | 62 (10.0) | 3 (1.0) | ||
| Peripheral oedema | 1,748 (20.8) | 175 (11.9) | 23 (4.3) | 203 (32.7) | 28 (9.2) | ||
| Treatment at randomization | |||||||
| Diuretic | 6,738 (80.2) | 1,080 (73.5) | 372 (68.6) | 545 (87.8) | 163 (53.3) | ||
| Digitalis | 2,539 (30.2) | 652 (44.4) | 219 (40.4) | 296 (47.7) | 137 (44.8) | ||
| Beta-blocker | 4,671 (55.6) | 825 (56.2) | 359 (66.2) | 285 (45.9) | 181 (59.2) | ||
| ICD | 1,243 (14.8) | 26 (1.8) | 23 (4.2) | 1 (0.2) | 2 (0.7) | ||
| CRT | 574 (6.8) | 42 (2.9) | 38 (7.0) | 3 (0.5) | 1 (0.3) | ||
Values are presented as mean±standard deviation or median (interquartile range) or number (%).
ACEI = angiotensin converting enzyme inhibitor; ARB = angiotensin receptor blocker; BMI = body mass index; CRT = cardiac resynchronization therapy; ICD = implantable cardioverter defibrillator; JVD = jugular venous distension; KCCQ CSS = Kansas city cardiomyopathy questionnaire clinical summary score; LVEF = left ventricular ejection fraction; MI = myocardial infarction; NT-proBNP = N terminal pro brain natriuretic peptide; NYHA = New York Heart Association; PARADIGM-HF = Prospective comparison of Angiotensin Receptor-neprilysin inhibitor with Angiotensin converting enzyme inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure trial; PND = paroxysmal nocturnal dyspnoea; SBP = systolic blood pressure.
CLINICAL EFFICACY OF SACUBITRIL/VALSARTAN IN ASIANS IN THE PARADIGM-HF TRIAL
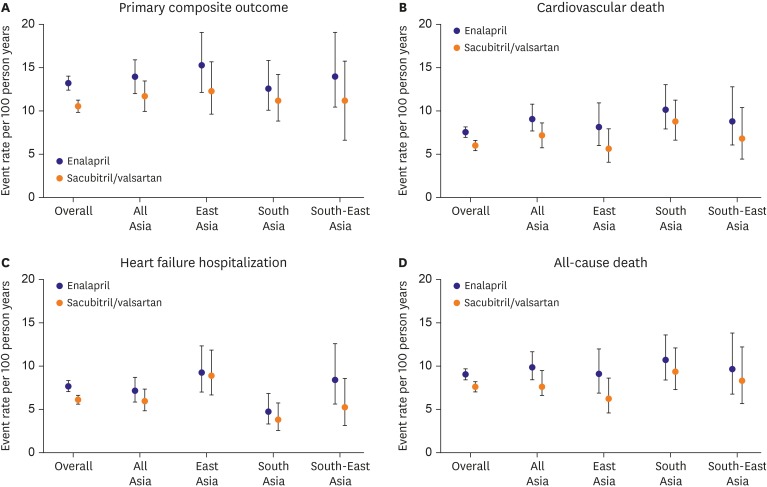
The Asian patients presented in this analysis were followed up for a median of 26 months. Across all the groups examined, event rates per 100-person years were lower in patients randomized to sacubitril/valsartan compared to enalapril (Figure 2). Overall, South Asians had a lower rate of hospitalization for HF and higher mortality when compared to the other groups, and overall mortality due to CV or any cause was highest in Asians compared to the total PARADIGM-HF cohort.
Figure 2. Event rates per 100 patient years by treatment in all patients and by Asian regions enrolled in PARADIGM-HF.
HF = heart failure; PARADIGM-HF = Prospective comparison of Angiotensin Receptor-neprilysin inhibitor with Angiotensin converting enzyme inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure trial.
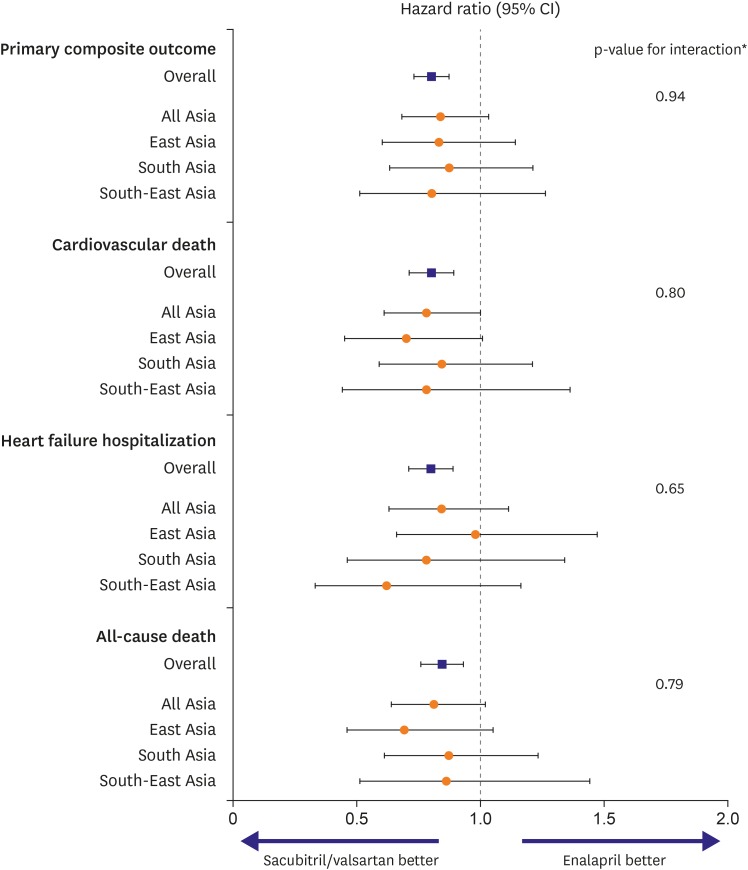
Importantly, no difference was seen between the benefits of treatment in Asians and the total PARADIGM-HF cohort or between the different regions of Asia (Figure 3).
Figure 3. Treatment effects by Asian regions in PARADIGM-HF.
CI = confidence interval; PARADIGM-HF = Prospective comparison of Angiotensin Receptor-neprilysin inhibitor with Angiotensin converting enzyme inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure trial.
*Interaction p value for Asia subgroups.
TOLERABILITY AND SAFETY OF SACUBITRIL/VALSARTAN IN ASIANS IN THE PARADIGM-HF TRIAL
Concerns regarding potential differences in drug tolerability and safety in Asians, compared to non-Asians, possibly secondary to physical characteristics such as a lower body weight and smaller size, have led the advocation of lower doses of drugs in Asian patients.6) Indeed, the ongoing Prospective comparison of ARNI with ACE inhibitor to determine the noveL beneficiaL trEatment vaLue in Japanese Heart Failure patients (PARALLEL-HF) trial in Japanese patients with HFrEF has lower run-in doses for both sacubitril/valsartan (100 mg BD with no up-titration) and enalapril (5 mg BD).51) However, the achieved doses of the 2 study treatments in PARADIGM-HF were similar in Asians to those in the overall trial patients. Mean daily dose of sacubitril/valsartan was 374.7±62.7 mg in the entire PARADIGM-HF cohort (compared with a target dose of 400 mg daily). The achieved daily dose was 373.88±66.0 mg in all Asians, 367.6±69.5 mg in East Asians, 374.2±71.8 mg in South Asians and 384.4±41.3 mg in South -East Asians. The mean daily dose of enalapril was 18.9±2.9 mg in PARADIGM-HF overall, and 19.0±2.9 mg, 18.8±3.1 mg, 19.1±2.9 mg, and 17.1±2.3 mg, in the Asian patient groups described above.
The reportedly high incidence of cough with ACEIs in Asians has led to ARBs becoming the preferred means of blocking the renin-angiotensin system in these individuals with HF or hypertension.52) In PARADIGM-HF, Asian patients randomized to sacubitril/valsartan overall had fewer complaints of cough compared to those randomized to enalapril, consistent with the overall findings in the total trial cohort (Table 3). Also, as seen in the total PARADIGM-HF population, hypotension was more common among Asians randomized to sacubitril/valsartan compared to enalapril. In Asian patients, as in the trial as a whole, patients randomized to sacubitril/valsartan had fewer adverse events leading to treatment discontinuation.
Table 3. Adverse events by treatment in all patients and by Asian regions enrolled in PARADIGM-HF.
| Overall | All Asia | East Asia | South Asia | South-East Asia | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Enalapril (n=4,212) | Sac/val (n=4,187) | Enalapril (n=731) | Sac/val (n=738) | Enalapril (n=271) | Sac/val (n=271) | Enalapril (n=307) | Sac/val (n=314) | Enalapril (n=153) | Sac/val (n=153) | |
| Cough | 601 (14.3) | 474 (11.3) | 211 (28.9) | 156 (21.1) | 68 (25.1) | 50 (18.5) | 83 (27.0) | 57 (18.2) | 60 (39.2) | 49 (32.0) |
| Hypotension | 388 (9.2) | 588 (14.0) | 51 (7.0) | 88 (11.9) | 21 (7.7) | 39 (14.4) | 23 (7.5) | 33 (10.5) | 7 (4.6) | 16 (10.5) |
| Hyperkalaemia | 455 (10.8) | 395 (9.4) | 57 (7.8) | 49 (6.6) | 14 (5.2) | 17 (6.3) | 38 (12.4) | 28 (8.9) | 5 (3.3) | 4 (2.6) |
| Angioedema | 11 (0.3) | 20 (0.5) | 2 (0.3) | 4 (0.5) | 0 (0.0) | 2 (0.7) | 1 (0.3) | 1 (0.3) | 1 (0.7) | 1 (0.7) |
| Any AE leading to study drug discontinuation | 129 (3.1) | 79 (1.9) | 13 (1.8) | 10 (1.4) | 6 (2.2) | 3 (1.1) | 2 (0.7) | 3 (1.0) | 5 (3.3) | 4 (2.6) |
AE = adverse event; PARADIGM-HF = Prospective comparison of Angiotensin Receptor-neprilysin inhibitor with Angiotensin converting enzyme inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure trial; Sac/val = Sacubitril/valsartan.
During the follow-up period, patients in Asia assigned to receive sacubitril/valsartan showed greater improvement in quality of life as indicated by the KCCQ clinical summary at 8 months compared to those receiving enalapril. Accordingly, more patients receiving enalapril had a clinically significant fall in KCCQ score at 8 months compared to sacubitril/valsartan (Table 4).
Table 4. Change in KCCQ clinical summary score by treatment in all patients and by Asian regions enrolled in PARADIGM-HF.
| Overall | All Asia | East Asia | South Asia | South-East Asia | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Enalapril (n=4,212) | Sac/val (n=4,187) | Enalapril (n=731) | Sac/val (n=738) | Enalapril (n=271) | Sac/val (n=271) | Enalapril (n=307) | Sac/val (n=314) | Enalapril (n=153) | Sac/val (n=153) | |
| KCCQ clinical summary score rise ≥5–8 months | 1,113 (26.60) | 1,132 (27.20) | 131 (18.10) | 130 (17.70) | 42 (15.60) | 47 (17.40) | 79 (26.20) | 76 (24.30) | 10 (6.50) | 7 (4.60) |
| KCCQ clinical summary score fall ≥5–8 months | 1,283 (30.70) | 1,124 (27.00) | 143 (19.70) | 118 (16.00) | 61 (22.60) | 35 (13.00) | 65 (21.50) | 70 (22.40) | 17 (11.10) | 13 (8.50) |
KCCQ = Kansas city cardiomyopathy questionnaire; PARADIGM-HF = Prospective comparison of Angiotensin Receptor-neprilysin inhibitor with Angiotensin converting enzyme inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure trial; Sac/val = Sacubitril/valsartan.
IMPLEMENTATION OF SACUBITRIL/VALSARTAN IN ASIAN GUIDELINES
Guidelines for management of HF vary across different Asian regions.53) We reviewed the most up to date HF management guidelines in the Asian countries in PARADIGM-HF to see if there were any recommendations pertaining to sacubitril/valsartan. There were very few countries with up to date clinical guidelines for HF and out of those only 3 countries recommended sacubitril/valsartan in their guidelines for management of HFrEF in their patients (Table 5).
Table 5. Sacubitril/valsartan in failure management guidelines in Asian countries in PARADIGM-HF.
| Country | Most recent year of publication | Name of issuing authority | Sacubitril/valsartan (ARNI) status | |
|---|---|---|---|---|
| East Asia | ||||
| China | 2018 | China Heart Society60) | IB recommendation in patients who have remained symptomatic despite optimal therapy with an ACEI/ARB, a beta-blocker and an MRA. | |
| South Korea | 2017 | Korean guidelines for diagnosis and management of chronic HF61) | Not included in recommendations. | |
| Taiwan | 2012 | Taiwan Society of Cardiology62) | No revised guidelines. | |
| South Asia | ||||
| India | 2018 | Cardiology Society of India63) | In patients who remain symptomatic despite optimal therapy with an ACEI, beta blocker and MRA, ARNI should be considered. | |
| South-East Asia | ||||
| Malaysia | 2014 | Academy of Medicine of Malaysia64) | No revised guidelines. | |
| Philippines | - | - | No revised guidelines. | |
| Thailand | 2019 | HF council of Thailand65),66) | IB recommendation in patients who have remained symptomatic despite optimal therapy with an ACEI/ARB, a beta-blocker and an MRA. | |
| IIbC recommendation for ACEI/ARB naïve patients who may be able to tolerate ARNI. | ||||
| Singapore | 2004 | Ministry of Health67) | No revised guidelines. | |
ACEI = angiotensin converting enzyme inhibitor; ARB = angiotensin receptor blocker; ARNI = angiotensin receptor neprilysin inhibitor; HF = heart failure; HFrEF = heart failure with reduced ejection fraction; MRA = mineralocorticoid receptor antagonist; PARADIGM-HF = Prospective comparison of Angiotensin Receptor-neprilysin inhibitor with Angiotensin converting enzyme inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure trial.
CONCLUSIONS
In PARADIGM-HF, adding a neprilysin inhibitor (sacubitril) to a renin-angiotensin system blocker (valsartan) reduced morbidity and mortality, compared to a renin-angiotensin system blocker (enalapril) alone, in ambulatory patients with chronic HFrEF. The data presented in this review support the use of sacubitril/valsartan in Asian patients with chronic, symptomatic, and ambulatory HFrEF.
Footnotes
Conflict of Interest: Dr. Docherty is conducting an investigator originated study funded by the British Heart Foundation (project grant No. PG/17/23/32850) using sacubitril/valsartan supplied by Novatis. The other authors have no financial conflicts of interest.
- Conceptualization: McMurray J, Dewan P, Docherty KF.
- Data curation: Dewan P, Docherty KF.
- Formal analysis: Dewan P, Docherty KF.
- Validation: Dewan P, Docherty KF.
- Visualization: Dewan P, Docherty KF.
- Writing - original draft: Dewan P, Docherty KF.
- Writing - review & editing: McMurray J, Dewan P, Docherty KF.
References
- 1.Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3:7–11. doi: 10.15420/cfr.2016:25:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lam CS, Teng TK, Tay WT, et al. Regional and ethnic differences among patients with heart failure in Asia: the Asian sudden cardiac death in heart failure registry. Eur Heart J. 2016;37:3141–3153. doi: 10.1093/eurheartj/ehw331. [DOI] [PubMed] [Google Scholar]
- 3.Dokainish H, Teo K, Zhu J, et al. Global mortality variations in patients with heart failure: results from the International Congestive Heart Failure (INTER-CHF) prospective cohort study. Lancet Glob Health. 2017;5:e665–72. doi: 10.1016/S2214-109X(17)30196-1. [DOI] [PubMed] [Google Scholar]
- 4.Dewan P, Jhund PS, Shen L, et al. Heart failure with reduced ejection fraction: comparison of patient characteristics and clinical outcomes within Asia and between Asia, Europe and the Americas. Eur J Heart Fail. 2019;21:577–587. doi: 10.1002/ejhf.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reyes EB, Ha JW, Firdaus I, et al. Heart failure across Asia: same healthcare burden but differences in organization of care. Int J Cardiol. 2016;223:163–167. doi: 10.1016/j.ijcard.2016.07.256. [DOI] [PubMed] [Google Scholar]
- 6.Teng TK, Tromp J, Tay WT, et al. Prescribing patterns of evidence-based heart failure pharmacotherapy and outcomes in the ASIAN-HF registry: a cohort study. Lancet Glob Health. 2018;6:e1008–18. doi: 10.1016/S2214-109X(18)30306-1. [DOI] [PubMed] [Google Scholar]
- 7.Hasan MS, Basri HB, Hin LP, Stanslas J. Genetic polymorphisms and drug interactions leading to clopidogrel resistance: why the Asian population requires special attention. Int J Neurosci. 2013;123:143–154. doi: 10.3109/00207454.2012.744308. [DOI] [PubMed] [Google Scholar]
- 8.McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004. doi: 10.1056/NEJMoa1409077. [DOI] [PubMed] [Google Scholar]
- 9.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the heart failure society of America. Circulation. 2017;136:e137–e161. doi: 10.1161/CIR.0000000000000509. [DOI] [PubMed] [Google Scholar]
- 10.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 11.de Bold AJ, Borenstein HB, Veress AT, Sonnenberg H. A rapid and potent natriuretic response to intravenous injection of atrial myocardial extract in rats. Life Sci. 1981;28:89–94. doi: 10.1016/0024-3205(81)90370-2. [DOI] [PubMed] [Google Scholar]
- 12.Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007;50:2357–2368. doi: 10.1016/j.jacc.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 13.O'Connor CM, Starling RC, Hernandez AF, et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;365:32–43. doi: 10.1056/NEJMoa1100171. [DOI] [PubMed] [Google Scholar]
- 14.Packer M, O'Connor C, McMurray JJ, et al. Effect of ularitide on cardiovascular mortality in acute heart failure. N Engl J Med. 2017;376:1956–1964. doi: 10.1056/NEJMoa1601895. [DOI] [PubMed] [Google Scholar]
- 15.Potter LR. Natriuretic peptide metabolism, clearance and degradation. FEBS J. 2011;278:1808–1817. doi: 10.1111/j.1742-4658.2011.08082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerr MA, Kenny AJ. The purification and specificity of a neutral endopeptidase from rabbit kidney brush border. Biochem J. 1974;137:477–488. doi: 10.1042/bj1370477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bayes-Genis A, Barallat J, Richards AM. A test in context: neprilysin: function, inhibition, and biomarker. J Am Coll Cardiol. 2016;68:639–653. doi: 10.1016/j.jacc.2016.04.060. [DOI] [PubMed] [Google Scholar]
- 18.McKinnie SM, Fischer C, Tran KM, et al. The metalloprotease neprilysin degrades and inactivates apelin peptides. ChemBioChem. 2016;17:1495–1498. doi: 10.1002/cbic.201600244. [DOI] [PubMed] [Google Scholar]
- 19.Roques BP, Fournié-Zaluski MC, Soroca E, et al. The enkephalinase inhibitor thiorphan shows antinociceptive activity in mice. Nature. 1980;288:286–288. doi: 10.1038/288286a0. [DOI] [PubMed] [Google Scholar]
- 20.Shepperson NB, Barclay PL, Bennett JA, Samuels GM. Inhibition of neutral endopeptidase (EC 3.4.24.11) leads to an atrial natriuretic factor-mediated natriuretic, diuretic and antihypertensive response in rodents. Clin Sci (Lond) 1991;80:265–269. doi: 10.1042/cs0800265. [DOI] [PubMed] [Google Scholar]
- 21.Kahn JC, Patey M, Dubois-Rande JL, et al. Effect of sinorphan on plasma atrial natriuretic factor in congestive heart failure. Lancet. 1990;335:118–119. doi: 10.1016/0140-6736(90)90595-v. [DOI] [PubMed] [Google Scholar]
- 22.Gros C, Souque A, Schwartz JC, et al. Protection of atrial natriuretic factor against degradation: diuretic and natriuretic responses after in vivo inhibition of enkephalinase (EC 3.4.24.11) by acetorphan. Proc Natl Acad Sci U S A. 1989;86:7580–7584. doi: 10.1073/pnas.86.19.7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Northridge DB, Jardine AG, Alabaster CT, et al. Effects of UK 69 578: a novel atriopeptidase inhibitor. Lancet. 1989;2:591–593. doi: 10.1016/s0140-6736(89)90714-9. [DOI] [PubMed] [Google Scholar]
- 24.Northridge DB, Newby DE, Rooney E, Norrie J, Dargie HJ. Comparison of the short-term effects of candoxatril, an orally active neutral endopeptidase inhibitor, and frusemide in the treatment of patients with chronic heart failure. Am Heart J. 1999;138:1149–1157. doi: 10.1016/s0002-8703(99)70082-7. [DOI] [PubMed] [Google Scholar]
- 25.Bevan EG, Connell JM, Doyle J, et al. Candoxatril, a neutral endopeptidase inhibitor: efficacy and tolerability in essential hypertension. J Hypertens. 1992;10:607–613. [PubMed] [Google Scholar]
- 26.Ferro CJ, Spratt JC, Haynes WG, Webb DJ. Inhibition of neutral endopeptidase causes vasoconstriction of human resistance vessels in vivo. Circulation. 1998;97:2323–2330. doi: 10.1161/01.cir.97.23.2323. [DOI] [PubMed] [Google Scholar]
- 27.Dalzell JR, Seed A, Berry C, et al. Effects of neutral endopeptidase (neprilysin) inhibition on the response to other vasoactive peptides in small human resistance arteries: studies with thiorphan and omapatrilat. Cardiovasc Ther. 2014;32:13–18. doi: 10.1111/1755-5922.12053. [DOI] [PubMed] [Google Scholar]
- 28.Robl JA, Sun CQ, Stevenson J, et al. Dual metalloprotease inhibitors: mercaptoacetyl-based fused heterocyclic dipeptide mimetics as inhibitors of angiotensin-converting enzyme and neutral endopeptidase. J Med Chem. 1997;40:1570–1577. doi: 10.1021/jm970041e. [DOI] [PubMed] [Google Scholar]
- 29.Rouleau JL, Pfeffer MA, Stewart DJ, et al. Comparison of vasopeptidase inhibitor, omapatrilat, and lisinopril on exercise tolerance and morbidity in patients with heart failure: IMPRESS randomised trial. Lancet. 2000;356:615–620. doi: 10.1016/s0140-6736(00)02602-7. [DOI] [PubMed] [Google Scholar]
- 30.Packer M, Califf RM, Konstam MA, et al. Comparison of omapatrilat and enalapril in patients with chronic heart failure: the Omapatrilat Versus Enalapril Randomized Trial of Utility in Reducing Events (OVERTURE) Circulation. 2002;106:920–926. doi: 10.1161/01.cir.0000029801.86489.50. [DOI] [PubMed] [Google Scholar]
- 31.Kostis JB, Packer M, Black HR, Schmieder R, Henry D, Levy E. Omapatrilat and enalapril in patients with hypertension: the Omapatrilat Cardiovascular Treatment vs. Enalapril (OCTAVE) trial. Am J Hypertens. 2004;17:103–111. doi: 10.1016/j.amjhyper.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 32.Fryer RM, Segreti J, Banfor PN, et al. Effect of bradykinin metabolism inhibitors on evoked hypotension in rats: rank efficacy of enzymes associated with bradykinin-mediated angioedema. Br J Pharmacol. 2008;153:947–955. doi: 10.1038/sj.bjp.0707641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feng L, Karpinski PH, Sutton P, et al. LCZ696: a dual-acting sodium supramolecular complex. Tetrahedron Lett. 2012;53:275–276. [Google Scholar]
- 34.Ayalasomayajula S, Langenickel T, Pal P, Boggarapu S, Sunkara G. Clinical pharmacokinetics of sacubitril/valsartan (LCZ696): a novel angiotensin receptor-neprilysin inhibitor. Clin Pharmacokinet. 2017;56:1461–1478. doi: 10.1007/s40262-017-0543-3. [DOI] [PubMed] [Google Scholar]
- 35.Cada DJ, Baker DE, Leonard J. Sacubitril/valsartan. Hosp Pharm. 2015;50:1025–1036. doi: 10.1310/hpj5011-1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohn JN, Tognoni G Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–1675. doi: 10.1056/NEJMoa010713. [DOI] [PubMed] [Google Scholar]
- 37.Gu J, Noe A, Chandra P, et al. Pharmacokinetics and pharmacodynamics of LCZ696, a novel dual-acting angiotensin receptor-neprilysin inhibitor (ARNi) J Clin Pharmacol. 2010;50:401–414. doi: 10.1177/0091270009343932. [DOI] [PubMed] [Google Scholar]
- 38.Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325:293–302. doi: 10.1056/NEJM199108013250501. [DOI] [PubMed] [Google Scholar]
- 39.Desai AS, McMurray JJ, Packer M, et al. Effect of the angiotensin-receptor-neprilysin inhibitor LCZ696 compared with enalapril on mode of death in heart failure patients. Eur Heart J. 2015;36:1990–1997. doi: 10.1093/eurheartj/ehv186. [DOI] [PubMed] [Google Scholar]
- 40.Jhund PS, Fu M, Bayram E, et al. Efficacy and safety of LCZ696 (sacubitril-valsartan) according to age: insights from PARADIGM-HF. Eur Heart J. 2015;36:2576–2584. doi: 10.1093/eurheartj/ehv330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kristensen SL, Martinez F, Jhund PS, et al. Geographic variations in the PARADIGM-HF heart failure trial. Eur Heart J. 2016;37:3167–3174. doi: 10.1093/eurheartj/ehw226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Okumura N, Jhund PS, Gong J, et al. Effects of sacubitril/valsartan in the PARADIGM-HF trial (Prospective Comparison of ARNI with ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure) according to background therapy. Circ Hear Fail. 2016;9:e003212. doi: 10.1161/CIRCHEARTFAILURE.116.003212. [DOI] [PubMed] [Google Scholar]
- 43.Cannon JA, Shen L, Jhund PS, et al. Dementia-related adverse events in PARADIGM-HF and other trials in heart failure with reduced ejection fraction. Eur J Heart Fail. 2017;19:129–137. doi: 10.1002/ejhf.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pocock SJ, McMurray JJ, Collier TJ. Making sense of statistics in clinical trial reports: part 1 of a 4-part series on statistics for clinical trials. J Am Coll Cardiol. 2015;66:2536–2549. doi: 10.1016/j.jacc.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 45.Solomon SD, Claggett B, McMurray JJ, Hernandez AF, Fonarow GC. Combined neprilysin and renin-angiotensin system inhibition in heart failure with reduced ejection fraction: a meta-analysis. Eur J Heart Fail. 2016;18:1238–1243. doi: 10.1002/ejhf.603. [DOI] [PubMed] [Google Scholar]
- 46.Senni M, McMurray JJ, Wachter R, et al. Initiating sacubitril/valsartan (LCZ696) in heart failure: results of TITRATION, a double-blind, randomized comparison of two uptitration regimens. Eur J Heart Fail. 2016;18:1193–1202. doi: 10.1002/ejhf.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wachter R, Senni M, Belohlavek J, Butylin D, Noe A, Pascual-Figal D. Sacubitril/valsartan initiated in hospitalized patients with heart failure with reduced ejection fraction after hemodynamic stabilization: primary results of the TRANSITION study. J Card Fail. 2018;24:S15. [Google Scholar]
- 48.Velazquez EJ, Morrow DA, DeVore AD, et al. Angiotensin-neprilysin inhibition in acute decompensated heart failure. N Engl J Med. 2019;380:539–548. doi: 10.1056/NEJMoa1812851. [DOI] [PubMed] [Google Scholar]
- 49.Solomon SD, Rizkala AR, Gong J, et al. Angiotensin receptor neprilysin inhibition in heart failure with preserved ejection fraction: rationale and design of the PARAGON-HF trial. JACC Heart Fail. 2017;5:471–482. doi: 10.1016/j.jchf.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 50.Solomon SD, Rizkala AR, Lefkowitz MP, et al. Baseline characteristics of patients with heart failure and preserved ejection fraction in the PARAGON-HF trial. Circ Hear Fail. 2018;11:e004962. doi: 10.1161/CIRCHEARTFAILURE.118.004962. [DOI] [PubMed] [Google Scholar]
- 51.Tsutsui H, Momomura S, Saito Y, et al. Efficacy and safety of sacubitril/valsartan (LCZ696) in Japanese patients with chronic heart failure and reduced ejection fraction: rationale for and design of the randomized, double-blind PARALLEL-HF study. J Cardiol. 2017;70:225–231. doi: 10.1016/j.jjcc.2016.11.011. [DOI] [PubMed] [Google Scholar]
- 52.Woo KS, Nicholls MG. High prevalence of persistent cough with angiotensin converting enzyme inhibitors in Chinese. Br J Clin Pharmacol. 1995;40:141–144. [PMC free article] [PubMed] [Google Scholar]
- 53.Mentz RJ, Roessig L, Greenberg BH, et al. Heart failure clinical trials in East and Southeast Asia: understanding the importance and defining the next steps. JACC Heart Fail. 2016;4:419–427. doi: 10.1016/j.jchf.2016.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS) N Engl J Med. 1987;316:1429–1435. doi: 10.1056/NEJM198706043162301. [DOI] [PubMed] [Google Scholar]
- 55.Yusuf S, Pitt B, Davis CE, Hood WB, Jr, Cohn JN SOLVD Investigators. Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med. 1992;327:685–691. doi: 10.1056/NEJM199209033271003. [DOI] [PubMed] [Google Scholar]
- 56.Cohn JN, Johnson G, Ziesche S, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med. 1991;325:303–310. doi: 10.1056/NEJM199108013250502. [DOI] [PubMed] [Google Scholar]
- 57.Komajda M, Lutiger B, Madeira H, et al. Tolerability of carvedilol and ACE-inhibition in mild heart failure. Results of CARMEN (Carvedilol ACE-Inhibitor Remodelling Mild CHF EvaluatioN) Eur J Heart Fail. 2004;6:467–475. doi: 10.1016/j.ejheart.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 58.Willenheimer R, van Veldhuisen DJ, Silke B, et al. Effect on survival and hospitalization of initiating treatment for chronic heart failure with bisoprolol followed by enalapril, as compared with the opposite sequence: results of the randomized Cardiac Insufficiency Bisoprolol Study (CIBIS) III. Circulation. 2005;112:2426–2435. doi: 10.1161/CIRCULATIONAHA.105.582320. [DOI] [PubMed] [Google Scholar]
- 59.McMurray JJ, Krum H, Abraham WT, et al. Aliskiren, enalapril, or aliskiren and enalapril in heart failure. N Engl J Med. 2016;374:1521–1532. doi: 10.1056/NEJMoa1514859. [DOI] [PubMed] [Google Scholar]
- 60.Heart Online Technology (CN) Guide: chronic HFrEF drug treatment, a summary! [Internet] Beijing: Heart Online Technology; 2018. [cited 2019 Apr 10]. Available from: http://www.heartonline.cn/themes/TPL_XZX003/views/details.html?id=5bd81316e12b371d4a5b8591&category=/information/infoSub&mark=/information/infoSub. [Google Scholar]
- 61.Kim MS, Lee JH, Kim EJ, et al. Korean guidelines for diagnosis and management of chronic heart failure. Korean Circ J. 2017;47:555–643. doi: 10.4070/kcj.2017.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang CC, Chen JH, Yu WC, et al. 2012 Guidelines of the Taiwan Society of Cardiology (TSOC) for the diagnosis and treatment of heart failure. Acta Cardiol Sin. 2012;28:161–195. [Google Scholar]
- 63.Guha S, Harikrishnan S, Ray S, et al. CSI position statement on management of heart failure in India. Indian Heart J. 2018;70(Suppl 1):S1–72. doi: 10.1016/j.ihj.2018.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ministry of Health Malaysia. Management of heart failure [Internet] Putrajaya: Ministry of Health Malaysia; 2014. [cited 2019 Apr 10]. Available from: http://www.moh.gov.my/moh/resources/Penerbitan/CPG/CARDIOVASCULAR/8.pdf. [Google Scholar]
- 65.Buakhamsri A, Chirakarnjanakorn S, Sanguanwong S, Porapakkham P, Kanjanavanich R. Heart Failure Council of Thailand (HFCT) 2019 heart failure guideline: pharmacologic treatment of chronic heart failure - part I. J Med Assoc Thai. 2019;102:240–244. [Google Scholar]
- 66.Yingchoncharoen T, Kanjanavanich R. Heart Failure Council of Thailand (HFCT) 2019 heart failure guideline: pharmacologic treatment of chronic heart failure - part II. J Med Assoc Thai. 2019;102:368–372. [Google Scholar]
- 67.Ministry of Health, Singapore. Clinical practice guidelines: heart failure [Internet] Singapore: Ministry of Health, Singapore; 2004. [cited 2019 Apr 10]. Available from: https://www.moh.gov.sg/docs/librariesprovider4/guidelines/cpg_heart-failure-aug-2004.pdf. [Google Scholar]