Abstract
Sri Lanka harbors over 3000 plant species, and most of these plants have been of immense importance in the traditional systems of medicine in the country. Although there is a rich reserve of indigenous knowledge on medicinal plants, in-depth studies have not been pursued yet to compile the ethnoflora with traditional medicinal applications for the scientific community. Thus, as a continuation of our ethnobotanical inventory work in different regions in the country, the present study was carried out in one of the administrative districts in the North Central area of Sri Lanka known as Polonnaruwa district. The information on the significance of medicinal plants as curative and preventive agents of diseases was collected through semistructured and open-ended interviews from 284 volunteers who were randomly recruited for the study. Ethnobotanical data were analyzed using relative frequency of citation (RFC), family importance value (FIV), and use value (UV). Out of the total participants, 53.7% claimed the use of herbal remedies. A total of 64 medicinal plants belonging to 42 plant families were recorded, out of which Coriandrum sativum L. (RFC = 0.163) was the most cited species. Out of the 42 plant families recorded, the FIV was highest in Zingiberaceae. Coscinium fenestratum (Goetgh.) Colebr. was found as the plant with the highest use value. Furthermore, the majority of the nonusers of the herbal remedies were willing to adopt herbal products upon the scientific validation of their therapeutic potential. This study revealed that the indigenous herbal remedies are still popular among the local communities in the study area.
1. Introduction
Medicinal plants have been used since time immemorial in both developing and developed countries; for example, plants were considered as the material basis of traditional Chinese medicine (TCM) as well as many other ethnic medicine traditions in China [1], while the utilization of medicinal plants as a fundamental component of the African traditional health-care system is believed as the oldest and the most assorted of all therapeutic systems [2]. Similarly, the Indian subcontinent is considered as a vast repository of medicinal plants that have been used in indigenous medical treatments, and even in the present era of modern medicine, traditional health-care systems based on plants and plant-derived products are therapeutically employed on the Indian subcontinent [3]. In the Sri Lankan context, indigenous systems of medicine are widely popular among large segments of the Sri Lankan population despite the influx of modern Western medicine. In general, the traditional systems of medicine available in the country are of four types, namely, Ayurveda, Siddha, Unani, and Deshiya Chikitsa. Plants and plant-based formulations are considered as essential components of the Ayurveda and Deshiya Chikitsa systems [4]. Among the native flora of Sri Lanka, more than 1400 plants are employed for medicinal purposes [5]. Considering the ethnobotanical data in other developing countries in the world, particularly in the neighboring country (India) [6], we could speculate that herbal preparations are more popular among the rural communities in Sri Lanka as well. Hence, a rich reserve of indigenous knowledge of herbal remedies for various ailments is expected to have accumulated especially in the rural areas of the country. The documentation of Sri Lankan medicinal plants to the scientific community was initiated during the colonial period of the country, specially with the descriptions of plant specimens collected by Paul Hermann in the 1670s and also with Icones Plantarum Malabaricarum (1694–1718) [7, 8]. Although these sources represent a rich source of ethnobotanical knowledge from colonial Ceylon, only a handful of ethnobotanical studies have been conducted over the recent years to document the traditional knowledge on medicinal values of plant species used in indigenous medicine [9, 10]. In addition, the book series written by Jayaweera in 1982 on “Medicinal plants (indigenous and exotic) used in Ceylon” [11] are still popular among scientists who are working on medicinal plants and their bioactivities; however, the scientific validation of these traditional claims is still at its infancy. Thus, as a continuation of our ethnobotanical inventory work in different administrative areas in Sri Lanka, the present study was undertaken to assess the significance and contribution of medicinal plants/herbal therapeutics to the day-to-day life of the inhabitants of Polonnaruwa district in the North Central region in Sri Lanka.
As evident from the ethnobotanical studies conducted in other South Asian countries as well as in Africa, the rural communities exploit plants that are easily available in their surroundings for food and medicaments [12–14]. For example, a recent study conducted in Northern Pakistan revealed that the local communities have a rich accessibility of medicinal plants; thus, they opt herbal remedies as low-cost health care for respiratory disorders [15]. Moreover, in the case of herbal therapeutics, people are generally aware about the harmful effects of synthetic medicines, thus realize the importance of a more natural way of life [10]. Moreover, the factors like low financial conditions and unavailability of modern health-care facilities would also limit the access of rural people to synthetic medicines [16]. Hence, the study area for this research has a high potential for utilization and consumption of medicinal plants due to the wide availability of valuable medicinal plants that are unique to the dry zone of Sri Lanka, as well as the presence of rural agricultural communities. Considering all these factors, we hypothesized that the inhabitants in the study area for this research widely utilize medicinal plants as easy and reliable remedies for common disease conditions.
2. Materials and Methods
2.1. Study Area
Polonnaruwa district is located in the North Central Province of Sri Lanka (Figure 1, Supplementary 1) and has an area of 3,293 km2. The district is divided into seven divisional secretariat divisions, which are further subdivided into 295 “Grama Niladhari” divisions. There are 637 villages, and the total population of the district is reported as 403,335. The majority of the people in the district are engaged in agriculture and animal husbandry. The forest coverage, including the grasslands and marshy lands, is estimated as 346,638.2 ha [17]. Twelve government hospitals located within the district provide modern health-care facilities, while 16 Ayurvedic hospitals and a large number of traditional healers within the local communities are responsible for the provision of traditional health-care system.
Figure 1.
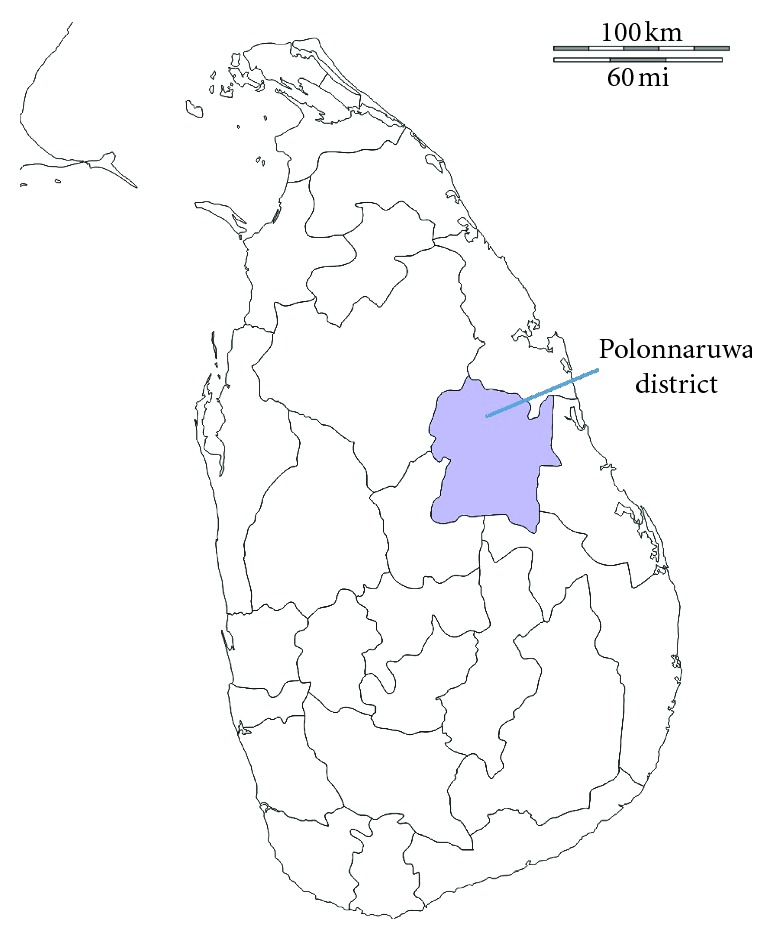
Location of Polonnaruwa district.
2.2. Ethnobotanical Field Survey and Data Collection
Medicinal plant use was documented in all seven divisional secretariat areas (i.e., Dimbulagala, Elahera, Hingurakgoda, Lankapura, Medirigiriya, Thamankaduwa, Welikanda; see Supplementary 1) in Polonnaruwa district. This survey was carried out from August 2015 to March 2018, and the data were collected from 284 volunteers from the general population of the district who were aged above 30 years, following the method described by Napagoda et al. [10]. In brief, the participants were selected randomly from a list of households in each divisional secretariat area, and visits were made to each of those households for data collection. Informed consent was obtained from each participant in writing prior to the study. A questionnaire was used to collect the information on local name of the plants, source, part(s) used, method of traditional preparation, and some demographic information of the informants such as age, gender, and educational background (Supplementary 2).
The ethical approval was obtained from the ethical review committee, Faculty of Medicine, University of Ruhuna, Sri Lanka. SPSS version 20 was used to recode the collected data.
2.3. Plant Specimen Collection and Preservation
Plant species used as herbal remedies were collected, dried, preserved, and mounted on herbarium sheets. The plant materials were identified by one of the authors (MTN), who is a botanist. Botanical names and families were verified using book series titled “Revised Handbook to the Flora of Ceylon” [18] and “Medicinal plants (indigenous and exotic) used in Ceylon” [11]. The botanical names have also been checked with the data available at http://www.theplantlist.org. The specimens were deposited at the Herbarium in the Department of Biochemistry, Faculty of Medicine, University of Ruhuna, Sri Lanka.
2.4. Quantitative Analysis of the Ethnobotanical Information
The knowledge on the usage of medicinal plants was quantitatively assessed by the relative frequency of citation (RFC), family importance value (FIV) of a plant family, and use value (UV) as described in our previous study [10] and the method of Kayani et al. [15] by substituting in the relevant equations given below. RFC and FIV were calculated to quantitatively determine the consensus between informants on the use of medicinal plants in the region as it gives the local importance of a species or a family [15, 19, 20].
The value of RFC for a particular species of medicinal plants is based on the citing percentage of informants for that particular species, where RFC = FC/N (0 < RFC < 1), in which RFC is the relative frequency of citation, FC is the number of informants who mentioned the species, and N is the total number of informants participating in the study.
Family importance value (FIV) of a plant family was calculated by taking the percentage of informants mentioning the family, where FIV = FC (family)/N × 100, in which FC is the number of informants mentioning the plant family and N is the total number of informants participating in the study.
Use value indicates the relative importance of plant species known locally, and the following formula was used to determine UV: UV i=∑U i/N i, in which U i is the number of use reports described by each informant for species i and N is the total number of informants describing the specific species i.
3. Results and Discussion
As speculated, the results of this study revealed that the majority of the inhabitants who have participated in this study depended on the indigenous plant resources as treatments and preventive measures against a number of disease conditions.
Out of the total of 284 informants, 132 (53.7%) claimed the use of medicinal plants for the treatment of various ailments such as diabetes, inflammatory conditions, and skin diseases, while the rest of the informants (46.3%) mentioned the nonadherence to herbal remedies. In addition, these plants are also used as energy boosters and cosmetics. Among those people, 47.6% firmly believed in the safety and low adverse effects associated with the herbal formulations and mentioned this as a reason for their preference. In addition, the previous success with herbal remedies (35.86%) was also a main contributing factor for the people to continue with plant-based therapies. Unlike the observations of our previous ethnobotanical study conducted in Gampaha District, Western Province of Sri Lanka [10], some people (2.76%) stated that the nonavailability of modern health-care facilities in their villages was a reason for them to opt for herbal remedies. The majority of the users (67.9%) claimed the use of herbal preparations at the initial stage of a disease before going for any other medications, while 26.01% have mentioned the simultaneous usage with other medications. Only 6.1% stated the use of herbal therapeutics as a last resort, when other treatment methods have failed. The knowledge of the herbal remedies had transferred through generations while the influence of media in promoting the use of herbal therapeutics could not be neglected (Table 1).
Table 1.
Statistics on the usage of herbal therapeutics.
| Parameter | Percentage |
|---|---|
| Demographic data of regular users | |
| Gender | |
| Male | 59.8 |
| Female | 40.2 |
| Age group (years) | |
| 30–45 | 34.09 |
| 46–60 | 38.64 |
| 61–75 | 24.24 |
| >75 | 3.03 |
| Educational background | |
| University degree/diploma and above | 2.3 |
| 12 years of school education | 15.2 |
| 1–11 years of school education | 82.5 |
| No schooling | 0 |
|
| |
| Source of information/knowledge | |
| From parents/grandparents | 60.42 |
| Neighbours/friends | 13.89 |
| Doctors/traditional physicians | 7.64 |
| Media | 13.19 |
| Own experience | 4.86 |
|
| |
| Reason for usage | |
| Safe/less side effects | 47.59 |
| Previous success | 35.86 |
| Easy access to the plant materials | 13.79 |
| High cost of other treatment methods | 0 |
| Nonavailability of modern health-care facilities | 2.76 |
The study revealed the use of 64 medicinal plants belonging to 42 plant families, out of which Coriandrum sativum L. (RFC = 0.163) was the most cited species, followed by Zingiber officinale Roscoe (RFC = 0.146) and Hygrophila auriculata (Schumach.) Heine (RFC = 0.109). The family importance value was highest in Zingiberaceae (22.8%) (Table 2). The highest use value was reported for Coscinium fenestratum (Goetgh.) Colebr. The most dominant life form of the species reported was herbs (37.5%; Figure 2). The most frequently used part of the plant was leaves (36.2%; Figure 3), followed by seeds/fruits (18.9%). Medicinal plants used in folk herbal remedies were prepared and administered in various forms. The most common preparation method was infusion (34.4%) while 14.9% were used in the form of a paste (Figure 4). The percentage of oral administration (71.1%) of herbal preparation was much higher than the external or topical application (24.3%) and inhalation (4.6%). Most of the crude drugs were prepared from single plant species; however, combinations of multiple species as well as the use of adjuvants such as honey, sugar, coconut milk, salt, and coconut oil have also been reported. For example, a paste prepared from the fruit of Myristica fragrans Houtt. with the juice of Citrus aurantifolia (Christm.) Swingle is a common remedy for stomachache while honey or sugar is added to most of the infusions to reduce the bitter taste.
Table 2.
Family importance value (FIV) of the ten plant families with the highest FIV.
| Family | FIV (%) |
|---|---|
| Zingiberaceae | 22.8 |
| Apiaceae | 19.9 |
| Acanthaceae | 18.3 |
| Rutaceae | 12.6 |
| Fabaceae | 10.2 |
| Amaranthaceae | 9.7 |
| Menispermaceae | 9.3 |
| Apocynaceae | 8.9 |
| Cucurbitaceae | 8.1 |
| Meliaceae | 7.7 |
Figure 2.
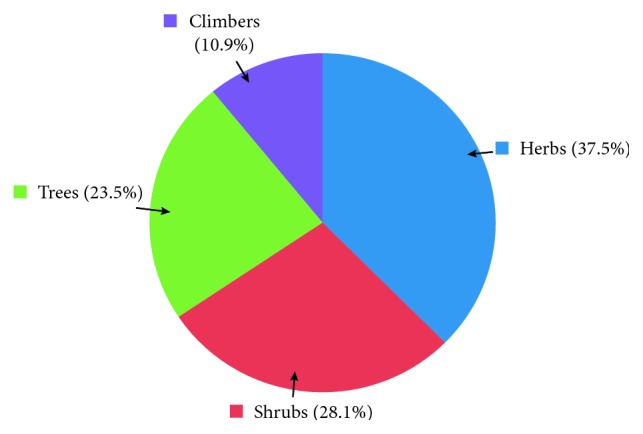
Life form of the plants used as herbal remedies.
Figure 3.
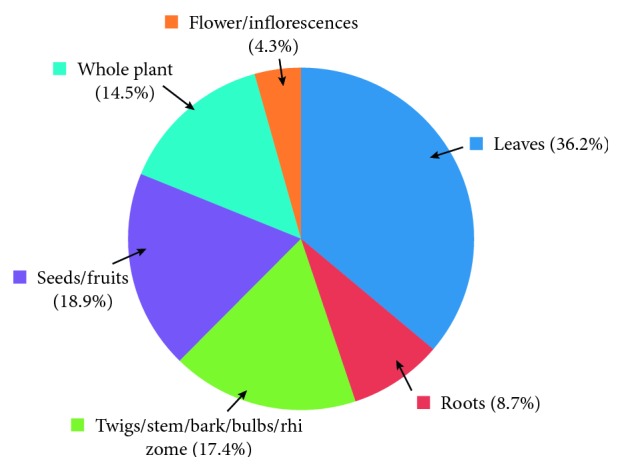
Plant parts used in herbal preparations.
Figure 4.
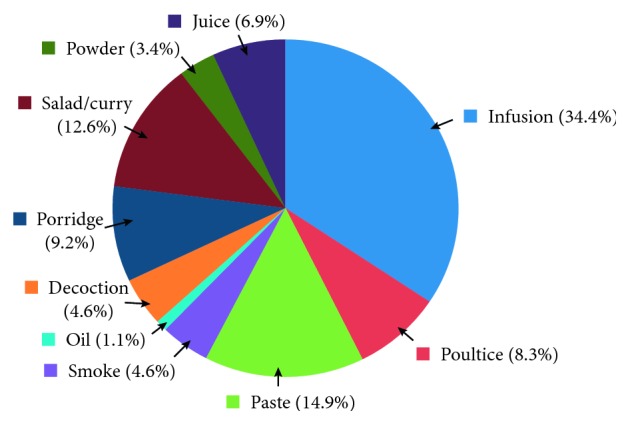
Mode of utilization of plants to treat various disease conditions.
The summary of the medicinal plant species used in Polonnaruwa district to treat various disease conditions is given in Table 3.
Table 3.
Medicinal plant species used in Polonnaruwa district to treat different disease conditions.
| Family | Scientific name and voucher specimen number | Vernacular name (in Sinhala) | Life form | Parts used | Preparation | Disease conditions treated | RFC | UV | Reported usage in literature [13] |
|---|---|---|---|---|---|---|---|---|---|
| Acanthaceae |
Adhatoda vasica Nees MN-NCP-01 |
Adhatoda | Shrub | Leaves, twigs, roots | Infusion, poultice | Swellings in joints, cough, asthma, catarrh | 0.073 | 1.56 | Diarrhea, fever, asthma |
|
Hygrophila auriculata (Schumach.) Heine MN-NCP-02 |
Neermulli | Herb | Whole plant | Infusion, decoction, porridge | Urinary diseases and urinary calculi, headache | 0.109 | 1.1 | Oedema, kidney stones, jaundice, rheumatism | |
|
| |||||||||
| Acoraceae |
Acorus calamus L. MN-NCP-03 |
Wadakaha | Herb | Root | Infusion, paste made with milk | Cough, worm infestation | 0.004 | 1.0 | Asthma, rheumatism, bowel complaints, internal ulceration |
|
| |||||||||
| Amaranthaceae |
Aerva lanata (L.) Juss. MN-NCP-04 |
Polpala | Herb | Whole plant | Infusion, porridge | Urinary diseases, as an energy booster, to purify blood, body pain | 0.085 | 1.57 | Kidney stones, cough, headache |
|
Alternanthera sessilis (L.) R. Br. ex DC. MN-NCP-05 |
Mukunuwenna | Herb | Whole plant | Salad, porridge | Body pain, as an energy booster | 0.012 | 1.67 | Liver diseases, acute and chronic pyelitis, snake bites | |
|
| |||||||||
| Amaryllidaceae |
Allium sativum L. MN-NCP-06 |
Sudulunu | Herb | Bulb | Infusion, porridge | Asthma stomachache, body pain | 0.024 | 2.5 | Asthma, gout |
|
| |||||||||
| Anacardiaceae |
Spondias dulcis Parkinson MN-NCP-07 |
Amberella | Tree | Fruit | Cook with coconut milk | High blood pressure | 0.008 | 1.0 | Dysentery, rheumatism, earache |
|
| |||||||||
| Apiaceae |
Centella asiatica (L.) Urb. MN-NCP-08 |
Gotu kola | Herb | Whole plant | Salad, juice, porridge | Catarrh, eye diseases, as an energy booster | 0.016 | 2.0 | Kidney diseases, skin diseases, rheumatism, fever, dysentery, pains, epilepsy |
|
Coriandrum sativum L. MN-NCP-09 |
Koththamalli | Herb | Seeds | Infusion | Cold, fever, asthma, body pain | 0.163 | 1.7 | Cold, fever, cough | |
|
Trachyspermum Roxburghianum (DC.) H. Wolff MN-NCP-10 |
Asamodagum | Herb | Leaves | Salad | Stomachache, worm infestation | 0.020 | 1.4 | Cough, asthma, dysentery | |
|
| |||||||||
| Apocynaceae |
Hemidesmus indicus (L.) R. Br. ex Schult. MN-NCP-11 |
Iramusu | Herb | Root, whole plant | Infusion, porridge | Cold, fever, to purify blood, body pain, diabetes | 0.089 | 1.32 | Purification of blood, oedema, skin rashes, cough, asthma |
|
| |||||||||
| Araceae |
Lasia spinosa (L.) Thwaites MN-NCP-12 |
Kohila | Herb | Whole plant | Porridge | As an energy booster | 0.004 | 1.0 | Piles |
|
| |||||||||
| Arecaceae |
Cocos nucifera L. MN-NCP-13 |
Kurumba | Tree | Tender coconut water | Drink | Fever | 0.004 | 1.0 | Diuretic, anthelmintic |
|
| |||||||||
| Asparagaceae |
Asparagus racemosus Willd. MN-NCP-14 |
Hathawariya | Climber | Whole plant | Infusion | Urinary diseases and urinary calculi | 0.024 | 1.0 | Diuretic, dysentery, rheumatism, urinary and kidney diseases |
|
| |||||||||
| Asphodelaceae |
Aloe vera (L.) Burm. f. MN-NCP-15 |
Komarika | Herb | Leaves | Grind to get the juice | Burns, for the growth of hair | 0.008 | 1.5 | Swellings, burns, skin diseases, urinary diseases, fever |
|
| |||||||||
| Asteraceae |
Acanthospermum hispidum DC. MN-NCP-16 |
Katu-nerinchi | Herb | Leaves | Paste | Pain in the joints | 0.004 | 1.0 | Arthritis, rheumatism, leprosy |
|
Eclipta prostrata (L.) L. MN-NCP-17 |
Keekirindiya | Herb | Whole plant | Paste | For the growth of hair | 0.012 | 1.0 | Skin diseases, ulcers, stimulate the growth of hair, fever, arthritis | |
|
| |||||||||
| Capparaceae |
Cleome gynandra L. MN-NCP-18 |
Wela | Herb | Whole plant | Infusion | Pain in joints | 0.004 | 1.0 | Arthritis, rheumatism |
| Crateva adansonii DC. MN-NCP-19 | Lunuwarana | Tree | Bark | Decoction | Urinary calculi | 0.036 | 1.0 | Urinary calculi | |
|
| |||||||||
| Celastraceae |
Pleurostylia opposita (Wall.) Alston MN-NCP-20 |
Panakka | Shrub | Leaves | Salad | Urinary diseases | 0.004 | 1.0 | Urinary diseases |
|
| |||||||||
| Combretaceae |
Terminalia chebula Retz. MN-NCP-21 |
Aralu | Tree | Fruit | Powder | Fever | 0.016 | 1.0 | Fever, eye diseases, piles, chronic dysentery |
| Terminalia bellirica (Gaertn.) Roxb. MN-NCP-22 | Bulu | Tree | Fruit | Powder | Fever, diarrhea | 0.012 | 1.67 | Diarrhea, fever, sore eyes | |
|
| |||||||||
| Costaceae |
Costus speciosus (J. Koenig) Sm. MN-NCP-62 |
Thebu | Shrub | Leaves | Salad, infusion | Diabetes | 0.020 | 1.0 | Fever, cough, skin diseases |
|
| |||||||||
| Crassulaceae |
Kalanchoe laciniata (L.) DC. MN-NCP-23 |
Akkapana | Herb | Leaves | Infusion | Cough, asthma, cold | 0.008 | 2.0 | Urinary diseases, diarrhea, dysentery, cough, cold |
|
| |||||||||
| Cucurbitaceae |
Coccinia grandis (L.) Voigt MN-NCP-24 |
Kowakka | Vine | Leaves | Salad, infusion | Diabetes | 0.081 | 1.0 | Diabetes, urinary calculi, skin diseases |
|
| |||||||||
| Elaeocarpaceae |
Elaeocarpus serratus L. MN-NCP-25 |
Veralu | Tree | Tender leaves | Juice | For the growth of hair | 0.004 | 1.0 | Dandruff, abscesses, joint swellings |
|
| |||||||||
| Euphorbiaceae |
Phyllanthus emblica L. MN-NCP-26 |
Nelli | Tree | Fruit | Poultice | Redness and swellings in eye | 0.016 | 1.0 | Inflammation in eye, gonorrhea, diarrhea, urinary diseases |
|
Ricinus communis L. MN-NCP-27 |
Enderu | Shrub | Leaves | Poultice | Headache, joint pains, swellings | 0.020 | 1.6 | Headache, boils, rheumatism | |
|
| |||||||||
| Fabaceae | Bauhinia racemosa Lam. MN-NCP-28 |
Maila | Shrub | Leaves | Salad | Urinary diseases | 0.004 | 1.0 | Pain, fever, urinary diseases |
|
Cassia auriculata L. MN-NCP-29 |
Ranawara | Shrub | Flower, leaves | Infusion | Urinary diseases and urinary calculi, to purify blood | 0.045 | 1.27 | Fever, diabetes, urinary diseases, rheumatism, eye conjunctivitis, skin diseases | |
|
Sesbania grandiflora (L.) Pers. MN-NCP-30 |
Kathurumurunga | Shrub | Leaves | Salad | Fissuring of lip, ulcers in mouth | 0.032 | 1.0 | Oedema, wounds, eye diseases, coughs, fever, skin diseases | |
|
Tamarindus indica L. MN-NCP-31 |
Siyabala | Tree | Leaves | Paste | Swelling in joints | 0.020 | 1.0 | Boils, rheumatism | |
|
| |||||||||
| Hippocrateaceae |
Salacia reticulata Wight MN-NCP-32 |
Kothala himbutu | Climbing shrub | Stem | Infusion | Diabetes | 0.061 | 1.0 | Diabetes, skin diseases, rheumatism |
|
| |||||||||
| Lamiaceae |
Leucas zeylanica (L.) W. T. Aiton MN-NCP-33 |
Gata thumba | Herb | Leaves | Salad | Worm infestation | 0.016 | 1.0 | Fever, gout, skin diseases, worm infestation |
|
Vitex negundo L. MN-NCP-60 |
Nika | Shrub | Leaves | Smoke, paste | Cough, asthma, fever, swellings in joints, cold | 0.041 | 1.4 | Rheumatic swellings, headache, catarrh, asthma | |
|
| |||||||||
| Loganiaceae |
Strychnos potatorum L. f. MN-NCP-34 |
Ingini | Tree | Seeds | Paste | Swellings in joints | 0.008 | 1.0 | Eye diseases, diarrhea |
|
| |||||||||
| Lythraceae | Punica granatum L. MN-NCP-46 | Delum | Shrub | Leaves | Infusion to wash eyes | Eye diseases | 0.012 | 1.0 | Eye infections, dysentery, cough, asthma, fever |
|
| |||||||||
| Malvaceae |
Sida acuta Burm. f. MN-NCP-35 |
Babila | Herb | Roots | Infusion, decoction | Fever, pain | 0.008 | 1.5 | Fever, impotency, rheumatism |
|
| |||||||||
| Meliaceae |
Azadirachta indica A. Juss. MN-NCP-36 |
Kohomba | Tree | Leaves, stem | Poultice, paste, infusion | Pain in joints, itching diabetes, worm infestation | 0.077 | 1.21 | Catarrh, leprosy and skin diseases, rheumatism, ulcers and wounds |
|
| |||||||||
| Menispermaceae |
Coscinium fenestratum (Goetgh.) Colebr. MN-NCP-37 |
Veniwelgata | Woody climber | Stem | Infusion | Fever, cough, pain, asthma, skin diseases in children | 0.081 | 2.6 | Fever, tetanus, dressing wounds and ulcers |
|
Tinospora cordifolia (Willd.) Miers MN-NCP-38 |
Rasakida | Climber | Stem | Infusion | Fever | 0.012 | 1.0 | Fever, skin diseases, diabetes, dysentery, rheumatism | |
|
| |||||||||
| Moraceae |
Ficus racemosa L. MN-NCP-39 |
Attikka | Tree | Fruit | As a curry | Diabetes | 0.020 | 1.0 | Urinary diseases, dysentery, diabetes |
|
Artocarpus heterophyllus Lam. MN-NCP-40 |
Kos | Tree | Root | Infusion | Diabetes | 0.004 | 1.0 | Skin diseases, asthma, diabetes, swellings and abscesses | |
|
| |||||||||
| Moringaceae |
Moringa oleifera Lam. MN-NCP-41 |
Murunga | Shrub | Bark | Infusion, poultice | Asthma, swellings | 0.041 | 1.3 | Asthma, rheumatism, gout, remedy for snake-bite poisoning |
|
| |||||||||
| Myristicaceae |
Myristica fragrans Houtt. MN-NCP-42 |
Sadikka | Shrub | Fruit | Paste prepared with lime juice | Stomachache | 0.032 | 1.0 | Nausea, vomiting, stomachache |
|
| |||||||||
| Piperaceae |
Piper betle L. MN-NCP-43 |
Bulath | Climber | Leaves | Paste | Stomachache | 0.008 | 1.0 | Cough, antiseptic |
|
Piper nigrum L. MN-NCP-44 |
Gammiris | Climber | Seeds | Paste | Stomachache | 0.012 | 1.0 | Cough, fever, piles | |
|
| |||||||||
| Poaceae |
Eleusine indica (L.) Gaertn. MN-NCP-45 |
Belatana | Herb | Whole plant | Poultice | Swellings and sprains | 0.024 | 1.0 | Sprains and dislocations |
|
| |||||||||
| Rubiaceae |
Coffea arabica L. MN-NCP-47 |
Kopi | Shrub | Fruit | Infusion | Stomachache | 0.049 | 1.0 | Diarrhea, bleeding wounds |
|
Ixora coccinea L. MN-NCP-48 |
Rathmal | Shrub | Flowers | Infusion | Skin diseases in children | 0.004 | 1.0 | Dysentery, reddened eyes and eruptions in children, catarrh | |
|
| |||||||||
| Rutaceae |
Aegle marmelos (L.) Corrêa MN-NCP-49 |
Beli | Tree | Leaves, roots, flower | Decoction, infusion | Asthma, fever | 0.008 | 2.5 | Fever, asthma, dysentery, piles, dyspepsia, |
|
Citrus aurantium L. MN-NCP-50 |
Embul dodam | Tree | Fruit | Juice | Cough, to draw out phlegm | 0.004 | 1.0 | Chronic cough | |
|
Citrus aurantifolia (Christm.) Swingle MN-NCP-51 |
Dehi | Tree | Leaves | Smoke, juice | Cough, cold, headache, stomachache | 0.073 | 1.22 | Cough, stomachache, cleaning wounds, dysentery | |
|
Murraya koenigii (L.) Spreng. MN-NCP-52 |
Karapincha | Shrub | Leaves | Porridge | High blood pressure | 0.041 | 1.0 | Constipation, diarrhea, dysentery | |
|
| |||||||||
| Santalaceae |
Santalum album L. MN-NCP-53 |
Sudu handun | Shrub | Bark | Paste | Swellings, pain | 0.016 | 1.0 | Fever, diarrhea, dysentery, gastric irritation, skin diseases, local inflammation |
|
| |||||||||
| Sapotaceae |
Madhuca longifolia (J. Koenig ex L.) J. F. Macbr. MN-NCP-54 |
Mee | Tree | Seeds | Oil, poultice | Swellings and pain in joints | 0.036 | 1.0 | Fractures, rheumatism, snake bites |
|
| |||||||||
| Scrophulariaceae | Scoparia dulcis L. MN-NCP-55 |
Wal koththamalli | Herb | Whole plant | Infusion | Diabetes | 0.016 | 1.0 | Ear and eye diseases, liver diseases, leprosy, nasopharyngeal infections |
|
| |||||||||
| Solanaceae |
Solanum xanthocarpum Schrad. and H. Wendl. MN-NCP-56 |
Katuwelbatu | Herb | Leaves | Infusion | Fever, cough, asthma | 0.053 | 1.46 | Cough, asthma, colic fever, toothache |
|
Solanum surattense Burm. f. MN-NCP-57 |
Ela batu | Herb | Leaves | Porridge, smoke | Cough, asthma | 0.004 | 2.0 | Rheumatism, cough, diarrhea | |
|
| |||||||||
| Theaceae |
Camellia sinensis (L.) Kuntze MN-NCP-58 |
Tea | Shrub | Leaves | Infusion | Stomachache | 0.008 | 1.0 | Catarrh, urinary diseases |
|
| |||||||||
| Verbenaceae |
Lantana camara L. MN-NCP-59 |
Gandapana | Shrub | Leaves | Smoke | Fever, cough, asthma | 0.008 | 1.5 | Asthma, fever, cough |
|
| |||||||||
| Zingiberaceae |
Alpinia galanga (L.) Willd. MN-NCP-61 |
Araththa | Herb | Rhizome | Infusion | Fever | 0.057 | 1.0 | Rheumatism, bronchitis |
|
Curcuma longa L. MN-NCP-63 |
Kaha | Herb | Rhizome | Paste, powder | Wounds, skin diseases, sprains | 0.024 | 1.5 | Sprains, wounds, dysentery, jaundice, rheumatism, skin diseases | |
|
Zingiber officinale Roscoe MN-NCP-64 |
Inguru | Herb | Rhizome | Infusion | Fever, cold, asthma, cough | 0.146 | 1.44 | Cold, cough, fever, asthma | |
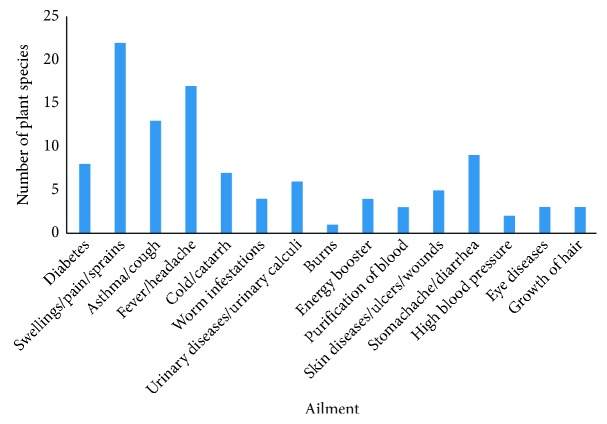
As depicted in Figure 5, herbal remedies were used by the inhabitants of Polonnaruwa district against 15 broad categories of ailments/conditions reporting the highest number of species against swellings/pains or sprains. Further, the local people in the study area utilize medicinal plants (around 30 plant species) for the treatment of other classical inflammatory symptoms like fever [10, 21] or chronic inflammatory diseases like asthma [22].
Figure 5.
Number of plants used against different disease conditions.
Interestingly, the medicinal uses of some of the plants mentioned by the informants have not been documented in the literature particularly in the popular book series on Sri Lankan medicinal plants by Jayaweera [11], for example, the use of Spondias dulcis Parkinson for high blood pressure and Hemidesmus indicus (L.) R. Br. ex Schult., Artocarpus heterophyllus Lam, and Scoparia dulcis L. for diabetes. Therefore, the documentation of this rich undocumented ethnobotanical knowledge could offer new avenues for pharmacological investigations on prospective new drugs of herbal origin. Moreover, plant species like Asparagus racemosus Willd, Terminalia bellirica (Gaertn.) Roxb., Piper betle L., Murraya koenigii (L.) Spreng., Citrus aurantium L., Citrus aurantifolia (Christm.) Swingle, and Zingiber officinale Roscoe have been identified as remedies for snake bites in a recent ethnobotanical study conducted in Western and Sabaragamuwa Provinces in Sri Lanka [9]; however, none of the informants participated in the present study mentioned about the utility of those plants in the treatment of snake bites. Besides, some of the informants mentioned that the wealth of knowledge is rapidly diminishing due to the dearth of elderly people who are knowledgeable on folklore medicine as well as lack of interest in younger generation to systematically study these traditional healing systems. Thus, our findings would enable the preservation of local knowledge which is obtained by trial and error and transferred over generations. In addition, a dramatic degradation of habitat due to construction work and the ruthless use and overexploitation of medicinal plants by local people and the traders of medicinal plants solely for commercial purposes were observed during the field survey. As an example, it has been mentioned that there is a high demand in the local market specially for Salacia reticulata Wight, a plant which was also documented in Icones Plantarum Malabaricarum as an endemic species [8]. S. reticulata Wight is widely popular among Sri Lankans as an effective remedy for diabetes; thus, there is an increased demand for commercial products prepared from stems of this plant, which could make it highly vulnerable for extinction. Hence, appropriate conservation measures are urgently required to cultivate such valuable medicinal plants and thereby to reduce the pressure on overexploitation from natural habitats. On the other hand, plant species like Zingiber officinale Roscoe and Coriandrum sativum L. are not threatened by overharvesting despite the high demand, particularly due to the cultivation of Z. officinale Roscoe in most of the home gardens throughout the country not only for medicinal but also for culinary purposes as well as the availability of C. sativum L. as an imported spice in the local markets in Sri Lanka.
Although the majority of the people in the nonuser category (50.9%) had used some kind of herbal therapeutics at some stage of their lives, the usage was discontinued mainly due to the difficulty in the preparation and collection of plant materials from their surroundings (59%). In addition, the relatively long period of time taken for healing, unpleasant smell, and the taste has also hindered their use. Moreover, some have profusely refused such remedies, due to the unavailability of scientific records on the safety and the efficacy of herbal formulations. Interestingly, 75.4% of these nonusers mentioned that they would shift to herbal products if the efficacy of these products could be scientifically validated.
4. Conclusion
This study reports the first in-depth ethnobotanical survey in the North Central Province of Sri Lanka, where agriculture is the primary livelihood of the inhabitants of the area. Among 64 medicinal plants belonging to 42 reported plant families, the family importance value was highest in Zingiberaceae. The most popular medicinal plants among the inhabitants of Polonnaruwa district include Coriandrum sativum L., Zingiber officinale Roscoe, and Hygrophila auriculata (Schumach.) Heine. Despite the eroding folkloric knowledge that depended on the oral tradition for its transmission to successive generations, the indigenous herbal remedies are still popular among the local communities in the study area. Moreover, even the majority of the nonusers are ready to shift to herbal products upon the scientific validation of the therapeutic efficiency, and it signifies the necessity of comprehensive pharmacological and phytochemical investigations of these traditional formulations.
Acknowledgments
The authors gratefully acknowledge “Faculty of Medicine-Research Grant 2015” from University of Ruhuna, Sri Lanka.
Abbreviations
- RFC:
Relative frequency of citation
- FIV:
Family importance value
- UV:
Use value.
Data Availability
The data used to support the findings of this study are included within the article.
Ethical Approval
The ethical approval was obtained from the ethical review committee, Faculty of Medicine, University of Ruhuna, Sri Lanka.
Consent
Informed consent was obtained in writing prior to the study.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Supplementary Materials
Supplementary 1: the map of Polonnaruwa district (the district boundary is marked in purple, and the sites where the data were collected are marked with squares). Supplementary 2: the questionnaire which was used to collect the information on utility of herbal preparations and some demographic information of the informants.
References
- 1.Zhang L., Zhuang H., Zhang Y., et al. Plants for health: an ethnobotanical 25-year repeat survey of traditional medicine sold in a major marketplace in North-West Yunnan, China. Journal of Ethnopharmacology. 2018;224:119–125. doi: 10.1016/j.jep.2018.05.029. [DOI] [PubMed] [Google Scholar]
- 2.Mahomoodally M. F. Traditional medicines in Africa: an appraisal of ten potent African medicinal plants. Evidence-Based Complementary and Alternative Medicine. 2013;2013:14. doi: 10.1155/2013/617459.617459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pandey M. M., Rastogi S., Rawat A. K. S. Indian traditional ayurvedic system of medicine and nutritional supplementation. Evidence-Based Complementary and Alternative Medicine. 2013;2013:12. doi: 10.1155/2013/376327.376327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weragoda P. B. The traditional system of medicine in Sri Lanka. Journal of Ethnopharmacology. 1980;2(1):71–73. doi: 10.1016/0378-8741(80)90033-1. [DOI] [PubMed] [Google Scholar]
- 5.Wijesundera D. S. A. Inventory, documentation and medicinal plant research in Sri Lanka. Medicinal Plant Research in Asia. 2004;1:184–195. [Google Scholar]
- 6.Unial A. K., Singh C., Singh B., Kumar M., da Silva J. A. T. Ethnomedicinal use of wild plants in Bundelkhand Region, Uttar Pradesh, India. Journal of Medicinal and Aromatic Plant Science and Biotechnology. 2011;5:81–86. [Google Scholar]
- 7.van Andel T., Barth N. Paul Hermann’s ceylon herbarium (1672–1679) at Leiden, the Netherlands. Taxon. 2011;67(5):977–988. [Google Scholar]
- 8.van Andel T., Scholman A., Beumer M. Icones plantarum malabaricarum: early 18th century botanical drawings of medicinal plants from colonial Ceylon. Journal of Ethnopharmacology. 2018;222:11–20. doi: 10.1016/j.jep.2018.04.033. [DOI] [PubMed] [Google Scholar]
- 9.Dharmadasa R. M., Akalanka G. C., Muthukumarana P. R. M., Wijesekara R. G. S. Ethnopharmacological survey on medicinal plants used in snakebite treatments in Western and Sabaragamuwa provinces in Sri Lanka. Journal of Ethnopharmacology. 2016;179:110–127. doi: 10.1016/j.jep.2015.12.041. [DOI] [PubMed] [Google Scholar]
- 10.Napagoda M. T., Sundarapperuma T., Fonseka D., Amarasiri S., Gunaratna P. An ethnobotanical study of the medicinal plants used as anti-inflammatory remedies in Gampaha District-Western Province, Sri Lanka. Scientifica. 2018;2018:8. doi: 10.1155/2018/9395052.9395052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jayaweera D. M. A. Medicinal Plants (Indigenous and Exotic) used in Ceylon, Part 1–5. Colombo, Sri Lanka: National Science Council; 1982. [Google Scholar]
- 12.Namsa N. D., Tag H., Mandal M., Kalita P., Das A. K. An ethnobotanical study of traditional anti-inflammatory plants used by the Lohit community of Arunachal Pradesh, India. Journal of Ethnopharmacology. 2009;125(2):234–245. doi: 10.1016/j.jep.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Umair M., Altaf M., Abbasi A. M. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district, Punjab-Pakistan. PLoS One. 2017;12(6) doi: 10.1371/journal.pone.0177912.e0177912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Towns A. M., Ruysschaert S., van Vliet E., van Andel T. Evidence in support of the role of disturbance vegetation for women’s health and childcare in Western Africa. Journal of Ethnobiology and Ethnomedicine. 2014;10(1):p. 42. doi: 10.1186/1746-4269-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kayani S., Ahmad M., Zafar M., et al. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies—Abbottabad, Northern Pakistan. Journal of Ethnopharmacology. 2014;156:47–60. doi: 10.1016/j.jep.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Diallo D., Hveem B., Mahmoud M. A., Berge G., Paulsen B. S., Maiga A. An ethnobotanical survey of herbal drugs of Gourma district, Mali. Pharmaceutical Biology. 1999;37(1):80–91. doi: 10.1076/phbi.37.1.80.6313. [DOI] [Google Scholar]
- 17.Department of Census and Statistics. District Statistical Hand Book Polonnaruwa. Battaramulla, Sri Lanka: Department of Census and Statistics; 2016. [Google Scholar]
- 18.Dassanayake M. D., Fosberg F. R. A Revised Handbook to the flora of Ceylon. 1–14. New Delhi, India: Amerind Publishers; 1980-2000. [Google Scholar]
- 19.Šavikin K., Zdunić G., Menković N., et al. Ethnobotanical study on traditional use of medicinal plants in South-Western Serbia, Zlatibor district. Journal of Ethnopharmacology. 2013;146(3):803–810. doi: 10.1016/j.jep.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 20.Vitalini S., Iriti M., Puricelli C., Ciuchi D., Segale A., Fico G. Traditional knowledge on medicinal and food plants used in Val San Giacomo (Sondrio, Italy)–an alpine ethnobotanical study. Journal of Ethnopharmacology. 2013;145(2):517–529. doi: 10.1016/j.jep.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 21.Ferrero-Miliani L., Nielsen O. H., Andersen P. S., Girardin S. E. Chronic inflammation: importance of NOD2 and NALP3 in interleukin-1beta generation. Clinical and Experimental Immunology. 2007;147(2):227–235. doi: 10.1111/j.1365-2249.2006.03261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishmael F. T. The inflammatory response in the pathogenesis of asthma. Journal of the American Osteopathic Association. 2011;111(11):S11–S17. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary 1: the map of Polonnaruwa district (the district boundary is marked in purple, and the sites where the data were collected are marked with squares). Supplementary 2: the questionnaire which was used to collect the information on utility of herbal preparations and some demographic information of the informants.
Data Availability Statement
The data used to support the findings of this study are included within the article.