Abstract
Background
Development of drug resistance caused by self-medication with antibiotics, can be seen as one of the growing global threats. Self-medication is defined as the selection and use of medicines by individuals to treat self-recognized illnesses or symptoms. The purpose of this study is to assess the practice of self-medication with antibiotics and associated factors among the community of Asmara, Eritrea.
Methods
This was a community based descriptive cross-sectional study conducted in 16 selected sub-districts of Asmara from September to November 2017. A Two-stage cluster sampling was employed to select study sites and participants. Data was collected in a face to face interview with a structured questionnaire and entered to CSPro version 6.2. Descriptive statistics, cross-tabulation and logistic regression were executed using SPSS version 22.
Results
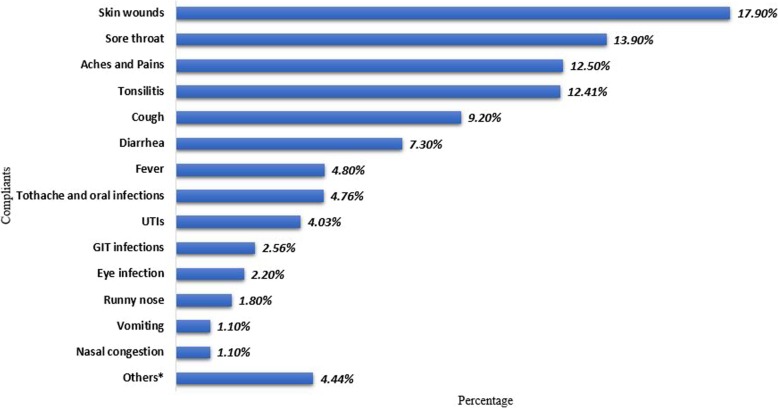
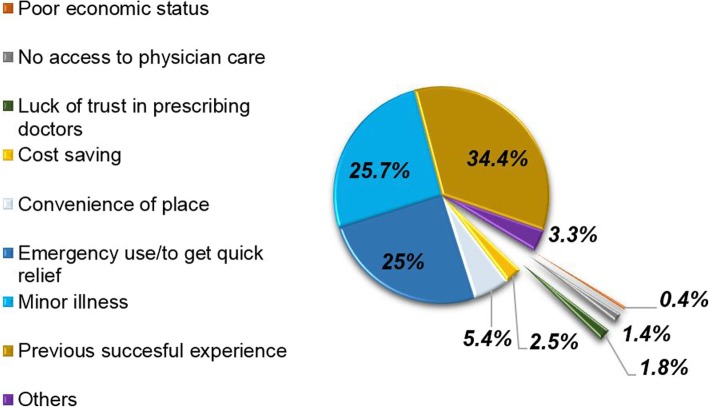
A total of 580 study participants were recruited with a response rate of 99.5% (N = 577). The prevalence of Self-medication with antibiotics (SMA) in this study was found to be 45.1% [95% CI (40.5, 49.6)] and majority of them practiced once or twice in a period of 12 months. The main reasons for SMA were previous successful experience (34.4%) and the illness being ‘not serious enough to seek medical care’ (25.7%). Of those who self-medicated, 84.1% of used amoxicillin at least once. Wound infection (17.9%) and sore throat (13.9%) were the most self-recognized complaints that required self-medication. Antibiotics were supplied and recommended mostly by the community drug outlets. Only Sex (p = 0.046), knowledge (p = 0.019) and attitude (p < 0.001) of the participants were found significantly associated with the practice of SMA in the multivariate logistic regression.
Conclusions
Though majority of the respondents considered self-medication with antibiotics as inappropriate practice, about half of them were practicing it anyway. Therefore immediate attention from relevant bodies is required.
Electronic supplementary material
The online version of this article (10.1186/s12889-019-7020-x) contains supplementary material, which is available to authorized users.
Keywords: Self-medication, Antibiotics, Prevalence, Asmara, Community
Background
Self-medication with antimicrobial is frequently noted as one of the major factors contributing to drug resistance [1]. The World Health Organization (WHO) defines self-medication as “the selection and use of medicines by individuals to treat self-recognized illnesses or symptoms” [2]. Antibiotics are substances produced by a microorganism, or a chemical synthesis, which in low concentrations can inhibit the growth and/or kill bacteria [3]. Unlike other drugs and virtually all other technologies, antibiotics suffer from transmissible loss of efficacy over time [4].
Antibiotic resistance refers to the phenomena when an antibiotic, which at its therapeutic level was once able to effectively stop the growth of the bacteria, has lost its ability to do so [5]. Self-medication with and overuse/misuse of antibiotics have been identified among the main risk factors for antibiotic resistance [6]. Moreover; lack of knowledge is a major factor responsible for inappropriate antimicrobial use and hence resistance globally [6].
Antibiotic resistance may result in prolonged illnesses, more health facility visits, extended hospital stays, the need for more expensive medications, and even death [7]. If the current trend continues, 10 Million deaths are attributable to AMR worldwide by 2050 [8].
A retrospective study conducted in Eritrea in 2016, regarding bacterial pathogen resistance to antimicrobials, showed an overall growth of resistant bacteria is 37.4% [9]. One of the effective strategies to prevent AMR had been staying one step ahead of the pathogens through discovery of new antibiotics. This could no longer be as productive since 15 out of the 18 largest pharmaceutical companies, owing to the financial burden over other drugs such as those used for chronic illnesses, abandoned the antibiotic field [10]. The only weapon to save the currently effective antibiotics from developing resistance is therefore handling them with care.
This study was conducted to establish the status of SMA among the community of Asmara. Moreover, it is aimed at identifying common perceived illnesses that required SMA, determining commonly used antibiotics, finding out the sources of information as well as antibiotics for the practice of SM. And the results from this study are expected to help in the planning of educational and regulatory interventions to promote the rational use of antibiotics.
Methods
Study designs and setting
This was a descriptive cross-sectional study conducted in selected sub-districts of Asmara, Eritrea from September to November 2017. Asmara is the capital city of Eritrea with 13 districts and 37 sub-districts.
Source and study population
The source population of this study were the residents of Asmara. According to the Municipality of Asmara, during the study period (2017) there was a total of 108, 896 households and a population of 422,309 distributed in an area of 44.99 km2.
Randomly selected residents of Asmara aged 18 years and above who were willing to participate in the study and without any hearing, speech or mental disability were included in the study population.
Sample size determination
Sample size was calculated using the single proportion formula without correction for continuity n = Z2P (1-P)/d2. At 95% confidence interval, the Z statistic value is 1.96 and P, estimated value for the particular indicator, was determined to be 0.39 from a pilot study. Assuming degree of precision (in proportion of one, d = 0.05), and a 5% non-response rate and finally adjusting by considering design effect (1.5), the sample size (n) was found to be 577 persons.
Sampling technique
A two-stage cluster sampling was employed and sixteen out of the total 37 sub-districts of Asmara were selected.
In the first stage, the sub-districts were the sampling units. Probability proportionate to size sampling technique that gives the highest share and hence, chance of selection to the sub-districts with the highest number of households they consist was used.
In the second stage, the participants (head of the households or any family member of it in the absence of the head) from the selected sub-districts were identified using systematic random sampling.
Data collection tool and approach
A structured questionnaire (Additional file 1) was developed on the basis of similar study conducted previously [11]. The questionnaire consisted both close-ended and open-ended questions and encompassed two parts. The first part inquired about the sociodemographic characteristics, whereas the second part was designed to capture data about previous self-use of antibiotics in the past 12 months (during initiation of the study), condition(s) for which antibiotics were self-prescribed, source of antibiotics, source of information, name(s) of antibiotics used. Moreover, few questions were included to probe the knowledge about antibiotics and attitude toward self-medication with antibiotics (SMA).
Selected participants were interviewed for about 15-20 minutes in their respective residence. Antibiotics commonly used in Eritrea were used as samples to help participants recall the name of the antibiotics they took. Data collection was conducted during the weekends or in the evening of the weekdays to include male participants who would leave their homes for work, as observed from the pilot study.
Data processing and statistical analysis
Data was entered into CSPro version 6.2 and was analyzed with SPSS version 22. First, descriptive analysis was performed using frequency, percentage, median and interquartile range. Cross-tabulation was then carried out to look for possible association between self-medication with antibiotics and the independent variables. Finally, univariate and multivariate logistic regression at 95% CI were computed. Variables found to be significant at univariate level were included in the multivariate logistic regression analysis to control other potential confounders. Statistical significance for all analyses was set at p < 0.05.
Operational definitions
Knowledgeable and unknowledgeable
Participants whose answers to the questions about what antibiotics are, what they are used for, and whether antibiotics could treat common cold or not were correct and, continued till the completion of course of treatment with antibiotics were classified as Knowledgeable. Any incorrect answer for any of these questions and discontinuing before completion of the regimen renders the respondent Unknowledgeable.
Positive attitude and negative attitude
Respondents were asked on what they think of self-medication with antibiotics. Those who had a notion that self-medication with antibiotics is inappropriate practice were considered as having positive attitude. Whilst, those who had a belief that it is unacceptable practice were categorized as respondents with negative attitude.
Results
Socio-demographic characteristics and prevalence of self-medication with antibiotics
A total of 580 study participants were recruited and this yielded a response rate of 99.5% (N = 577). The study participants were dominated by females (58.8%) and the median age was37 years (IQR = 24) (Table 1). Majority (27.9%) of participants were in the age group of 25–34 years and 61.9% of them were married. A quarter of the study participants (24.3%) had secondary level of education and the median monthly income was 1500 (IQR = 1650).
Table 1.
Socio-demographics of the participants
| Variables | Frequency | Percentage | Prevalence % | CI at 95% |
|---|---|---|---|---|
| Gender | ||||
| Male | 238 | 41.2 | 55 | [47.9, 62.2] |
| Female | 339 | 58.8 | 38.3 | [32.5, 44.0] |
| Age | ||||
| < 24 | 111 | 19.2 | 60.4 | [50.5, 70.4] |
| 25–34 | 161 | 27.9 | 43.1 | [34.0, 52.3] |
| 35–44 | 125 | 21.7 | 12.2 | [32.4, 51.9] |
| 45–54 | 74 | 12.8 | 12.9 | [30.3, 55.4] |
| > 55 | 106 | 18.4 | 36.0 | [25.8, 46.1] |
| Median age | 37 | |||
| IQR | 24 | |||
| Marital status | ||||
| Single | 163 | 61.9 | 59.3 | [50.9, 67.7] |
| Married | 357 | 28.2 | 38.8 | [33.1, 44.5] |
| Divorced | 23 | 4.0 | 47.4 | [22.6, 72.1] |
| Widowed | 34 | 5.9 | 38.7 | [20.5, 56.9] |
| Educational level | ||||
| Illiterate | 32 | 5.5 | 34.8 | [13.7, 55.8] |
| Primary | 64 | 11.1 | 34.0 | [20.8, 47.1] |
| Junior | 95 | 16.5 | 35.2 | [23.8, 46.6] |
| Secondary | 246 | 42.6 | 45.0 | [38.1, 52.0] |
| College | 140 | 24.3 | 58.1 | [49.0, 67.2] |
| Occupation | ||||
| Governmental | 170 | 29.5 | 46.1 | [37.8, 54.4] |
| Private service | 58 | 10.1 | 47.9 | [33.3, 62.6] |
| Self-employed | 58 | 10.1 | 47.7 | [32.4, 63.1] |
| Unemployed | 60 | 10.4 | 50.0 | [35.0, 65.0] |
| House wife | 191 | 33.1 | 35.8 | [28.0, 43.5] |
| Student | 40 | 6.9 | 66.7 | [50.5, 82.8] |
| Monthly income | ||||
| Non incomersa | 291 | 50.4 | 43.3 | [36.9, 49.8] |
| ≤ 1000 | 92 | 15.9 | 41.3 | [29.9, 52.7] |
| 1001–2500 | 136 | 23.6 | 48.2 | [38.9, 57.6] |
| > 2500 | 58 | 10.1 | 52.3 | [36.9, 67.6] |
| Median | 1500 | |||
| IQR | 1650 | |||
Note: CI Confidence Interval, IQR Interquartile range
a Unemployed, housewife, student
The prevalence of self-medication with antibiotics in the past 12 months prior to the data collection was found to be 45.1% [95% CI (40.5, 49.6)]. As depicted in Table 1, The Median of SMA practice was 1 (IQR=1), the maximum was 8 times and majority of the respondents practiced once or twice during the 12 months period.
Perceived complaints and reasons for self-medication with antibiotics
Self-medication with antibiotics was practiced for wound infection (17.9%), sore throat (13.9%), aches and pains (12.5%), Tonsillitis (12.41%), cough (9.2%), diarrhea (7.3%), fever (4.8%) etc. (Fig. 1). The main reasons for self-medication with antibiotics were previous successful experience (34.4%), the illness being minor to seek medical attention (25.7%) and with intention of getting quick relief/ for emergency use (25%) (Fig. 2).
Fig. 1.
Perceived complaints that required SMA. Others include broken bone, dysentery, internal illness, knee injury, leg infection, post labor infection, RTIs, and whitlow
Fig. 2.
Reasons for self-medication with antibiotics. Others include easy availability of antibiotics, frequency of illness, practitioner being a health professional, to save time
Frequently used antibiotics and their source of antibiotics
Of those who self-medicated, 84.1% used amoxicillin at least once in the 12 months period. It was followed by ciprofloxacin (6.7%), tetracycline (2.51%), co-trimoxazole (2.09%), metronidazole (1.67%) etc. Antibiotics used for self-medication were obtained mainly from pharmacy retail outlets (68.0%), leftovers (15.2%), friends and/or relatives (10.4%) and sent from abroad (6.4%). Their source of information for the use of the antibiotics among others were pharmacy professionals (46.9%), previous doctor’s prescription (28.5%), friends/ relatives (8.8%), and internet/mobile applications (5.3%). Additionally, of those who self-medicated, 10.1% guessed the dosage of the antibiotics.
Knowledge, attitude and practice of the respondents
Of all the study participants, 466 (80.8%) of them at least once in their life took antibiotics either prescribed by a qualified clinician or self-prescribed. Less than half (42.6%) of the participants completed their course of treatment as recommended. About a quarter (23.9%) of those who self-medicated disclosed that they discontinued their antibiotics when symptoms disappeared, 6.2% when they felt better and 2.3% stopped it after few days regardless of the outcome (Table 2).
Table 2.
Course of treatment with antibiotics
| When do you stop taking the antibiotics? | Frequency | % |
|---|---|---|
| After a few days regardless of the outcome | 11 | 2.3 |
| After the symptoms disappeared | 115 | 23.9 |
| A few days after the recovery | 30 | 6.2 |
| After antibiotics run out | 110 | 22.9 |
| At the completion of the course of treatment | 205 | 42.6 |
| After consulting a medical personnel/ pharmacist | 9 | 1.9 |
| For one day | 1 | 0.2 |
Out of the 210 respondents who self-medicated, 18 (8.6%) respondents admitted they changed the dose of the antibiotics they used for self-medication every time they practice SMA, whereas 31(14.8%) quoted they sometimes deliberately changed the dose for the following reasons: condition improved (71.2%), condition worsened (11.5%), drug insufficient for complete treatment (7.7%), to reduce ADRs (7.7%) and 1.9% of them believed they were knowledgeable to decide to change the dose. Majority (76.7%) of them however, have never changed the dose of the antibiotics they used during the course of the practice of SMA.
About three-fourth (70.7%) of the study participants had a belief that use of self-medication with antibiotics is inappropriate (had positive attitude) while the rest (29.3%) believed that self-medication with antibiotics is acceptable practice (Table 3). Overall, 84.7% of the participants had inadequate knowledge on antibiotics and only 15.3% were found to be knowledgeable.
Table 3.
The respondents’ responses regarding the knowledge and attitude questions
| Frequency | % | |
|---|---|---|
| Do you know what antibiotics are? | ||
| Yes | 422 | 73.1 |
| No | 155 | 26.9 |
| What do you think about SMA? | ||
| Good practice | 39 | 6.8 |
| Acceptable practice | 130 | 22.5 |
| Not acceptable practice | 408 | 70.7 |
| Are antibiotics good for common cold? | ||
| Yes | 128 | 22.2 |
| No | 281 | 48.7 |
| Don’t know | 168 | 29.1 |
| What are antibiotics used for? | ||
| Bacterial infection | 277 | 43.8 |
| Viral infection | 82 | 13.0 |
| Bacterial and Viral infections | 53 | 9.2 |
| Don’t know | 270 | 42.7 |
| aOthers | 3 | 0.5 |
a Fungal infections, helminthic infections, skin wounds
Factors associated with self-medication practices
Being male (adjusted OR = 1.81; 95%CI: 1.01, 3.26), inadequate knowledge (adjusted OR = 2.13; 95%CI: 1.12, 4.05) and having negative attitude (OR = 7.47; 95%CI: 4.54, 12.29) were found to be significantly associated with self-medication of antibiotics (Table 4).
Table 4.
The relationship between SMA practice and socio-demographic variables
| Variable | COR (95% CI) | AOR (95% CI) |
|---|---|---|
| Gender | ||
| Female | Ref | |
| Male | 1.97 (1.36, 2.87)*** | 1.81 (1.01, 3.26)* |
| Age | ||
| < 24 | 2.72 (1.49, 4.93)** | 1.12 (0.43, 2.91) |
| 25–34 | 1.35 (0.77, 2.38) | 0.75 (0.36, 1.72) |
| 35–44 | 1.30 (0.72, 2.33) | 1.04 (0.48, 2.64) |
| 45–54 | 1.34 (0.69, 2.59) | 1.09 (0.49, 2.41) |
| > 55 | Ref | |
| Marital status | ||
| Single | 2.30 (1.04, 5.13)* | 1.34 (0.43, 4.21) |
| Married | 1.00 (0.47, 2.15) | 0.98 (0.37, 2.59) |
| Divorced | 1.14 (0.45, 4.52) | 1.03 (0.26, 4.06) |
| Widowed | Ref | |
| Educational Level | ||
| Illiterate | Ref | |
| Primary | 0.96 (0.34, 2.70) | 1.96 (0.56, 6.88) |
| Junior | 1.02 (0.38, 2.73) | 1.62 (0.46, 5.72) |
| Secondary | 1.54 (0.62, 3.79) | 1.92 (0.55, 6.69) |
| College | 2.60 (1.02, 6.62)* | 2.80 (0.74, 10.63) |
| Occupation | ||
| Governmental | Ref | |
| Private service | 1.08 (0.56, 2.07) | 1.06 (0.48, 2.32) |
| Self employed | 1.07 (0.54, 2.10) | 0.76 (0.33, 1.79) |
| Unemployed | 1.17 (0.60, 2.28) | 2.27 (0.95, 5.45) |
| House wife | 0.65 (0.40, 1.04) | 1.45 (0.67, 3.10) |
| Student | 2.34 (1.09, 5.04)* | 0.72 (0.24, 2.10) |
| Monthly income | ||
| Non incomers | Ref | |
| Less than or equal to 1000 | 0.92 (0.54, 1.56) | NA |
| 1001 to 2500 | 1.22 (0.78, 1.19) | NA |
| Greater than 2500 | 1.43 (0.75, 2.73) | NA |
| Knowledge | ||
| Knowledgeable | Ref | |
| Non- knowledgeable | 2.17 (1.30,3.61)** | 2.13 (1.12, 4.05)* |
| Attitude | ||
| Positive Attitude | Ref | |
| Negative attitude | 6.56 (4.23,10.16)*** | 7.47 (4.54, 12.29)*** |
Note: *** = p < 0.001, ** = p < 0.01, * = p < 0.05, AOR = Adjusted Odd’s Ratio CI = Confidence Interval, COR = Crude Odd’s Ratio, NA = Not Applicable, Ref = Reference category
Discussion
In this study, self-medication seeking behavior was found to be prevalent. This finding is comparable with findings of similar studies conducted in Sudan, Greece and Kenya [12–14]. It was however lower than reported in Indonesia, Ethiopia, Southern Spain, Slovenia and Lithuania [15–17] and higher than studies conducted in Pakistan, Saudi Arabia, Nigeria, Yemen, other Kenyan study and Sudanese [11, 19–25]. The difference in prevalence of self-medication with antibiotics might be due to differences in study design, community awareness, and definitions.
This study revealed that amoxicillin was the most frequently used antibiotic for self-medication. This might be explained by the fact that it is a well-known antibiotic to the community compared to other antibiotics and its ease of accessibility. The pharmacy retail outlets were found to be the main source for obtaining the antibiotics, targeted intervention is therefore recommended to halt the sale of antibiotics without prescription. During the conduction of this study, scheduling of medicines was not in place in Eritrea and thus, the public had easy access to medicines without prescription. To overcome the problem, strict regulation, and continuous public sensitization on rational use of antibiotics should be enforced.
It is however encouraging that majority of the study participants had a good understanding that antibiotics are indicated for bacterial infections (not viral infections). In contrary, studies conducted in Saudi Arabia and Indonesia reported a higher community belief that antibiotics work against viral infections [11, 15]. Most of the respondents in this study had the notion that self-medication with antibiotics is an inappropriate practice. That being said, the high prevalence of self-medication despite the positive attitude reflects further interventions are required to hammer the issue of antibiotic use without prescription by all available means.
Self-medication with antibiotics was significantly associated with male gender, inadequate knowledge and negative attitude. While the links between SMA and both inadequate knowledge and negative attitude are self explained, the difference in gender could be attributed to the work related injuries that males suffer more frequently than females as wound infections were the most reported complaints that required SMA in this study.
This result was found to be harmonious with some studies [18, 21, 27], and contradicts with other studies [22, 23] when it comes to gender. Some studies showed no significant association of socio-demographic factors with the practice of SMA [22, 23, 27] and other studies showed educational level [12, 22, 26], age, [12, 28, 29] and socioeconomic status [12, 26] to have statistically significantly associated with SMA.
Strength and limitation
Accommodations such as collecting the data during the weekends and in the evening of the weekdays was done to include different sociodemographic dimensions evenly in number and hence, high response rate was obtained. Additionally, this study assessed the SMA practice for the past 12 months. This can be regarded as a strength but on the other hand, it has resulted in recall bias.
Conclusion
Though majority of the respondents considered self-medication with antibiotics as inappropriate practice, their antibiotic seeking behavior without prescription was found to be prevalent. Respondents’ poor knowledge about antibiotics and antibiotic resistance as well as overestimating the power of antibiotics, and accessibility of antibiotics without prescriptions in retail outlets could be the possible drives for self-medication. Therefore, corrective measures such as enforcement of existing laws and scheduling of medicines to regulate their access to the public would protect consumers from misuse. Besides, healthcare professionals and media outlets should play their role in counselling consumers to refrain from use of antibiotics without prescription.
Additional file
Questionnaire for obtaining the prevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea. (DOCX 18 kb)
Acknowledgements
The authors would like to acknowledge the contributions of Dr. Eyob Azaria, Department of Public health, ACHS, for their enriching comments and Mr. Teklu Tsegai. They would also like to acknowledge the study participants for their commitment and willingness to be part of the study
Abbreviations
- ACHS
Asmara College of Health Sciences
- ADRs
Adverse Drug Reactions
- AMR
Antimicrobial Resistance
- AOR
Adjusted Odds Ratio
- CI
Confidence Interval
- COR
Crude Odds Ratio
- CSPro
Census and Survey Processing System
- ERN
Eritrean Nakfa
- IQR
Inter Quartile Range
- MOH
Ministry of Health
- RTIs
Respiratory Tract Infections
- SM
Self-medication
- SMA
Self-Medication with Antibiotic
- SPSS
Statistical Package for Social Sciences
- UTIs
Urinary Tract Infections
- WHO
World Health Organization
Authors’ contributions
BW, IP, and MR contributed to the design of study and the questionnaire, supervised the data collection, and reviewed the manuscript for intellectual content. EH contributed to design of study and the questionnaire, analyzed the data, interpreted the results, and reviewed the manuscript. BB, FM, YA, and YE contributed to the design of the questionnaire, collected, entered and analyzed the data, and wrote the first manuscript. All authors read and approved the final manuscript.
Funding
There was no source of funding for the study and manuscript preparation.
Availability of data and materials
The complete dataset used and/or analyzed during the current study are available from the corresponding author and can be accessed upon reasonable request.
Ethics approval and consent to participate
Administrative and ethical approval has been granted by the Asmara College of Health Sciences Research Ethical Clearance Committee and, Research Ethics and Protocol Review Committee of the Ministry of Health, Eritrea. Study participants were informed about the objective of the study and a written informed consent was obtained from each respondent. All the information obtained was and will be held confidential and it was and will be used only for this study’s purpose.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yonatan Ateshim, Phone: +291-7451080, Email: yonatesh23@gmail.com.
Batseba Bereket, Email: batsebamebrahtu984@gmail.com.
Feruz Major, Email: feruzmajor23@gmail.com.
Youel Emun, Email: yoelemun1@gmail.com.
Biruck Woldai, Email: brookpharm@gmail.com.
Ismail Pasha, Email: ismailpash@gmail.com.
Eyasu Habte, Email: yohoshua79@yahoo.com.
Mulugeta Russom, Email: satiswt@gmail.com.
References
- 1.Vuckovic N, Nichter M. Changing patterns of pharmaceutical practice in the United States. Soc Sci Med. 1997;44:1285–1302. doi: 10.1016/S0277-9536(96)00257-2. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . The role of the pharmacist in self-care and self-medication. Report of the 4th WHO Consultive group on the role of the pharmacist. Geneva: World Health Organization; 1998. [Google Scholar]
- 3.Hugo WB, Denyer SP, Hodges NA, Gorman SP, editors. Hugo and Russell’s pharmaceutical microbiology. 7. Malden, Mass: Blackwell Science; 2004. [Google Scholar]
- 4.Antibiotic Resistance in Humans and Animals [Internet] National Academy of Medicine. 2016. [Google Scholar]
- 5.Sharif M. A survey on practice and prevalence of self-medication with antibiotic by parents of children. Bangladesh: East West University; 2017.
- 6.Organization WH . WHO global strategy for containment of antimicrobial resistance. 2001. [Google Scholar]
- 7.Centres for disease control and prevention . Antibiotic resistance threats in the United States, 2013: Centres for disease control and prevention, US Department of health and human services. 2013. [Google Scholar]
- 8.O’Neil J. Tackling a crisis for the health and wealth of nations. Antimicrob Resist. 2014. https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf.
- 9.Seyoum Y. A retrospective documentary review study of bacterial pathogen resistance to antimicrobials: a six months (July to December, 2016), at National Health Laboratory, Asmara, Eritrea. J Bacteriol Mycol: Open Access [Internet] 2017;5(3):00133. [Google Scholar]
- 10.Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40:277–283. [PMC free article] [PubMed] [Google Scholar]
- 11.Yousif M, Abubaker I. Prevalence, determinants and practices of self-medication with antibiotics–a population based survey in Taif, Kingdom of Saudi Aarabiaksa. Age. 2015;228(172):57.50. [Google Scholar]
- 12.Awad A, Eltayeb I, Matowe L, Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum state, Sudan. J Pharm Pharm Sci. 2005;8(2):326–331. [PubMed] [Google Scholar]
- 13.Arwa H, Idris B, Mahmoud M. Pattern of selfmedication with antibiotics in Khartoum state, Sudan. World J Pharm Res. 2014;3(5):678–692. [Google Scholar]
- 14.Skliros E, Merkouris P, Papazafiropoulou A, Gikas A, Matzouranis G, Papafragos C, et al. Self-medication with antibiotics in rural population in Greece: a cross-sectional multicenter study. BMC Fam Pract [Internet] 2010;11:58. doi: 10.1186/1471-2296-11-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Widayati A, Suryawati S, de Crespigny C, Hiller JE. Self medication with antibiotics in Yogyakarta City Indonesia: a cross sectional population-based survey. BMC Research Notes. 2011;4:491. doi: 10.1186/1756-0500-4-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Väänänen MH, Pietilä K, Airaksinen M. Self-medication with antibiotics—does it really happen in Europe? Health Policy. 2006;77:166–171. doi: 10.1016/j.healthpol.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 17.Čižman M, Haaijer-Ruskamp F, Grigoryan L. Self-medication with antibiotics in Slovenian general population. Slov Med J. 2005;74(5):293–7.
- 18.Berzanskyte A, Valinteliene R, Haaijer-Ruskamp F, Gurevicius R, Grigoryan L. Self-medication with antibiotics in Lithuania. Int J Occup Med Environ Health. 2006;19:246–53 [Internet] [cited 2018 May 25] Available from: https://www.degruyter.com/downloadpdf/j/ijmh.2006.19.issue-4/v10001-006-0030-9/v10001-006-0030-9.xml. [DOI] [PubMed]
- 19.Israel E, Emmanuel E, Sylvester E, Chukuma E. Self-medication with antibiotics amongst civil servants in Uyo, southern Nigeria. J Adv Med Pharm Sci. 2015;2:89–97. [Google Scholar]
- 20.Abdulraheem I, Adegboye A, Fatiregun A. Self-medication with antibiotics: empirical evidence from a Nigerian rural population. Br J Pharm Res. 2016;11:1–13. doi: 10.9734/BJPR/2016/25268. [DOI] [Google Scholar]
- 21.Nyambega JO. Antibiotic use and misuse among adults in Magwagwa Ward, Nyamira County in Kenya. IOSR J Pharm Biolog Sci. 2017;12:87–92. [Google Scholar]
- 22.Albawani SM, Hassan YB, Abd-Aziz N, Gnanasan S. Self-medication with antibiotics in Sana’a City, Yemen. Trop J Pharm Res. 2017;16:1195. doi: 10.4314/tjpr.v16i5.30. [DOI] [Google Scholar]
- 23.Eldin NSH, Abdalla OE. Self-medication with antibiotics among patients attending community pharmacies in Khartoum City. Sudan J Ration Med. 2014;6:14–15. [Google Scholar]
- 24.Al Rasheed A, Yagoub U, Alkhashan H, Abdelhay O, Alawwad A, Al Aboud A, et al. Prevalence and predictors of self-medication with antibiotics in Al Wazarat health center, Riyadh City, KSA. Biomed Res Int. 2016;2016:1–8. doi: 10.1155/2016/3916874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grigoryan L, Burgerhof JGM, Haaijer-Ruskamp FM, Degener JE, Deschepper R, Monnet DL, et al. Is self-medication with antibiotics in Europe driven by prescribed use? J Antimicrob Chemother. 2006;59:152–156. doi: 10.1093/jac/dkl457. [DOI] [PubMed] [Google Scholar]
- 26.Alhomoud F, Aljamea Z, Almahasnah R, Alkhalifah K, Basalelah L, Alhomoud FK. Self-medication and self-prescription with antibiotics in the Middle East—do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis. 2017;57:3–12. doi: 10.1016/j.ijid.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 27.Bilal M. Self-medication with antibiotics among people dwelling in rural areas of Sindh. J Clin Diagn Res. 2016;10(5):OC08–OC13. doi: 10.7860/JCDR/2016/18294.7730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Azzam S, Al-Husein B, Alzoubi F, Masadeh M, Al-Horani MA. Self-Medication with Antibiotics in Jordanian Population. Int J Occup Med Environ Health. 2007;20(4):373–80 [Internet] [cited 2018 May 25] Available from: https://www.degruyter.com/downloadpdf/j/ijmh.2007.20.issue-4/v10001-007-0038-9/v10001-007-0038-9.xml. [DOI] [PubMed]
- 29.Shah SJ, Ahmad H, Rehan RB, Najeeb S, Mumtaz M, Jilani MH, et al. Self-medication with antibiotics among non-medical university students of Karachi: a cross-sectional study. BMC Pharmacol Toxicol. 2014;15:74. doi: 10.1186/2050-6511-15-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Questionnaire for obtaining the prevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea. (DOCX 18 kb)
Data Availability Statement
The complete dataset used and/or analyzed during the current study are available from the corresponding author and can be accessed upon reasonable request.