Abstract
Background:
Patient activation is a significant predictor of health behaviors; however, the level of activation in people attending a pulmonary rehabilitation program and the effect of pulmonary rehabilitation on patient activation have not been measured. Furthermore, the potential determinants and relationship between patient activation and characteristics of people attending pulmonary rehabilitation have not previously been reported.
Methods:
The Patient Activation Measure (PAM) was measured in people with a chronic respiratory disease or congestive cardiac failure at a baseline pulmonary rehabilitation assessment and again at the completion of the 8-week outpatient program.
Results:
This study included 194 people with chronic respiratory disease or congestive cardiac failure (41% male; mean [standard deviation, SD] age: 73 [11] years; mean [SD] forced expiratory volume in 1 second % predicted: 60% [20%]). The pulmonary rehabilitation program was completed by 61% (n = 118) of participants. The mean (SD) PAM score at baseline was 60.5 (15.7), which improved to 65.4 (15.5) after completion of the pulmonary rehabilitation program (P = .001). In a stepwise forward multiple regression analysis, anxiety, lung information needs, and health-related quality of life impact were found to be significant determinants of baseline PAM. This model explained 12% (P < .001) of the variance.
Conclusion:
People with a chronic respiratory disease or congestive cardiac failure commencing a pulmonary rehabilitation program demonstrated a moderate level of activation, which improved following an 8-week hospital outpatient pulmonary rehabilitation program. Anxiety, a higher level of lung information needs, and greater health-related quality of life impact were significantly associated with poor patient activation.
Keywords: knowledge, skill, confidence, patient activation, pulmonary rehabilitation, anxiety, quality of life
Introduction
Patient activation is associated with health behaviors including lifestyle behaviors (exercise, diet), clinical indicators (body mass index [BMI], blood pressure, cholesterol), health service utilization (hospitalizations, use of emergency departments, participation in preventive screening and immunizations, and having regular checkup), and reporting better patient experience (1). Patient activation is defined as “having the knowledge, skill, and confidence to manage one’s health and health care” (2). Chronic disease self-management is important to manage symptoms, prevent complications, and participate in treatment decisions, and this requires a high level of activation (3). Previous research in people with chronic obstructive pulmonary disease (COPD) has shown that only a minority of people with COPD are activated for self-management, and patient activation can be influenced by anxiety, illness perception, BMI, age, disease severity, and comorbidities (4). An association between COPD and activation has also been shown to be dependent on social support (5).
Pulmonary rehabilitation is a comprehensive intervention which includes exercise training, education, and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence of health-enhancing behaviors (6). Pulmonary rehabilitation reduces dyspnea (7), increases exercise capacity, improves health-related quality of life (8), and reduces hospitalizations (9). The effect of pulmonary rehabilitation on self-management is less clear (10). The comprehensive nature of pulmonary rehabilitation lends itself to potentially modifying patient activation to improve disease self-management. However, the effect of pulmonary rehabilitation on patient activation has not been measured.
The primary aims of this study were to (i) identify the level of activation in people with a chronic respiratory disease or congestive cardiac failure attending a pulmonary rehabilitation program and to (ii) determine whether a structured group-based pulmonary rehabilitation program delivered in a hospital outpatient setting altered patient activation. Secondary aims included (iii) examining the relationship between patient activation and patient characteristics and (iv) examining potential determinants of patient activation in people attending pulmonary rehabilitation.
Methods
Study Design and Participants
This study was a retrospective review of pulmonary rehabilitation records of all people with a chronic respiratory disease or congestive cardiac failure attending a pulmonary rehabilitation program at a tertiary hospital in Australia over a 2-year period (April 2014 to April 2016). Patients attending the pulmonary rehabilitation program provided prospective written consent for the collection of clinical information for research purposes, and the analysis of data was approved by the South Eastern Sydney Local Health District Human Research Ethics Committee (HREC reference number 16/065 [LNR/16/POWH/145]).
The pulmonary rehabilitation program was delivered in an outpatient hospital setting for 8 weeks. The program consisted of 16 sessions including 1-hour, twice-weekly, supervised individualized exercise training, as well as weekly 30- to 60-minute structured education sessions delivered in a group setting by a team of multidisciplinary health professionals (Table 1).
Table 1.
Pulmonary Rehabilitation Program Education Sessions.
| Topic | Health Professional Lead |
|---|---|
| Exercise | Physiotherapist |
| Secretion clearance | Physiotherapist |
| Lung anatomy and physiology | Nurse |
| Healthy hearts | Nurse |
| Medical care | Doctor |
| Action plans | Doctor |
| Energy conservation | Occupational therapist |
| Falls prevention | Occupational therapist |
| Health eating | Dietitian |
| Medications | Pharmacist |
| Inhalation devices | Respiratory educator/nurse |
| Swallowing and dry mouth care | Speech pathologist |
| Community services | Social worker |
| Coping with heart and lung disease | Psychologist |
| Respiratory community outreach program | Nurse |
Data Collection
People with a chronic respiratory disease or congestive cardiac failure who despite optimal medical management remained dyspneic were referred to pulmonary rehabilitation and who attended a comprehensive baseline pulmonary rehabilitation assessment were included in this study. Demographic and clinical information collected during the pulmonary rehabilitation assessment are presented in Table 2. The initial assessment was completed the week prior to program commencement, and a post-program assessment was completed at the final rehabilitation session. A “completer” was defined as attendance at 12 or more sessions and attendance at a post-program assessment for a repeat assessment of all outcome measures.
Table 2.
Data Collected During the Baseline Pulmonary Rehabilitation Assessment.
| Assessment Content | Information Collected/Assessment Tool |
|---|---|
| Demographics | Sex, age, primary language, suburb of residence, Aboriginality |
| Medical history | Primary respiratory or cardiac diagnosis, past medical history, smoking status, home oxygen therapy |
| Pulmonary function | Spirometry (11) |
| Body composition | Height and weight (body mass index) |
| Exercise capacity | 6-minute walk test (12) |
| Health-related quality of life | St George’s Respiratory Questionnaire (13) or Minnesota Living with Heart Failure Questionnaire (14) |
| Mental health | Hospital Anxiety and Depression Scale (15) |
| Lung disease knowledge | Lung Information Needs Questionnaire (16) |
| Morbidity and mortality | Body mass index, airflow obstruction, dyspnea, and exercise capacity index (17) |
| Patient activation | Patient Activation Measure (18) |
Patient activation was measured using the Patient Activation Measure (PAM; Insignia Health, LLC, Portland, OR, USA, 2013). The PAM assesses a persons’ knowledge, skills, and confidence for self-management via 13 health statements in a self-administered questionnaire. A response to each statement from a 4-point scale with responses ranging from “disagree strongly” to “agree strongly” was recorded by the patient. A PAM activation score (0-100 scale) was calculated, which can be segmented into 1 of 4 progressively higher levels of activation (Table 3). Although patient activation was measured at the pulmonary rehabilitation program baseline assessment, the results were not specifically used to tailor the program to each individual’s level of knowledge, skills, and confidence.
Table 3.
Patient Activation Measure Levels of Activation.
| Activation Level | Activation Score | Description |
|---|---|---|
| Level 1 | 47.0 or lower | A person may not yet believe that their role is important and does not feel in charge of their own health and care, lacking confidence in their ability to manage their health |
| Level 2 | 47.1 to 55.1 | A person lacks confidence and knowledge to take action and has little experience or success with behavior change |
| Level 3 | 55.2 to 67.0 | A person has some confidence in handling limited aspects of their health and indicates the person is beginning to take action |
| Level 4 | 67.1 or above | A person has made most of the necessary behavior changes, but may have difficulty maintaining those behaviors over time or during times of stress |
Data Analysis
Data were analyzed using SPSS Statistics 23 (SPSS Inc, Chicago, Illinois). Descriptive statistics were used to summarize participant characteristics with categorical variables reported as frequencies and continuous variables expressed as mean and standard deviation (SD). Differences in frequency distributions were evaluated by χ2 test. Within-group comparisons were examined using a paired t test. Pearson correlation coefficients were calculated between the baseline PAM activation scores and participant characteristic variables. A stepwise forward multiple regression analysis for the dependent variable of baseline PAM activation score was performed for variables significantly related to baseline PAM activation score. Those explanatory variables which were associated at a significance level of 0.10 were included in the final model. The tolerance and variance inflation factor (VIF) statistics were used to assess multicollinearity, and variables were only contained in the model if the tolerance value was >0.1 and VIF was <10 (19). A P value of <.05 was considered statistically significant.
Results
Participant Characteristics
The characteristics of 194 consecutive people attending a baseline pulmonary rehabilitation assessment are reported in Table 4. The majority of participants were female (59%), with a primary diagnosis of moderate COPD and a mean PAM activation level consistent with level 3 (Table 4). Most participants referred to the program lived in areas of low socioeconomic disadvantage based on the Socio-Economic Indexes for Areas index (20), which is a measure of relative socioeconomic advantage or disadvantage.
Table 4.
Characteristics of Participants at Baseline Pulmonary Rehabilitation Assessment.a
| All Participants (N = 194) | Completers (n = 118) | Non-completers (n = 76) | Completers vs Non-completers P Value | |
|---|---|---|---|---|
| Age, years | 73 (11) | 73 (10) | 72 (12) | .572 |
| Gender, male, n (%) | 80 (41) | 50 (42) | 30 (40) | .691 |
| Aboriginal, n (%) | 7 (4) | 3 (3) | 4 (5) | .324 |
| English primary language, n (%) | 188 (97) | 113 (96) | 75 (99) | .254 |
| Current smoker, n (%) | 11 (6) | 5 (4) | 6 (8) | .285 |
| Home oxygen therapy, n (%) | 17 (9) | 6 (5) | 11 (15) | .024 |
| Body mass index, kg/m2 | 28 (7) | 28 (7) | 29 (8) | .554 |
| Primary diagnosis, n (%) | .501 | |||
| Asthma | 26 (13) | 14 (12) | 12 (16) | |
| Bronchiectasis | 15 (8) | 11 (9) | 4 (5) | |
| Congestive cardiac failure | 9 (5) | 6 (5) | 3 (4) | |
| COPD | 109 (56) | 64 (54) | 45 (59) | |
| Lung cancer | 7 (4) | 5 (4) | 2 (3) | |
| Interstitial lung disease | 13 (7) | 5 (4) | 8 (11) | |
| Pulmonary hypertension | 5 (3) | 4 (3) | 1 (1) | |
| Other | 10 (5) | 9 (8) | 1 (1) | |
| COPD GOLD stage, n (%) | n = 109 | n = 64 | n = 45 | .576 |
| I | 11 (10) | 9 (14) | 2 (4) | |
| II | 53 (49) | 24 (38) | 29 (64) | |
| III | 40 (37) | 28 (44) | 12 (27) | |
| IV | 5 (5) | 3 (5) | 2 (4) | |
| Pulmonary function | n = 185 | n = 112 | n = 73 | |
| FEV1 (L) | 1.41 (0.50) | 1.39 (0.48) | 1.45 (0.53) | .484 |
| FEV1 (% predicted) | 60 (20) | 60 (21) | 61 (20) | .696 |
| FVC (L) | 2.32 (0.72) | 2.33 (0.72) | 2.29 (0.72) | .740 |
| FVC (% predicted) | 80 (20) | 81 (21) | 78 (19) | .308 |
| FEV1/FVC | 62 (16) | 61 (16) | 65 (15) | .122 |
| 6-minute walk distance | ||||
| Meters | 348 (110) | 362 (106) | 326 (113) | .025 |
| % predicted | 59 (17) | 61 (17) | 55 (17) | .017 |
| St George’s Respiratory Questionnaire | n = 178 | n = 109 | n = 69 | |
| Total score | 47.3 (15.2) | 46.3 (15.3) | 48.8 (15.1) | .294 |
| Symptom score | 56.5 (20.8) | 55.9 (20.2) | 57.6 (21.8) | .587 |
| Activity score | 66.1 (16.8) | 64.8 (17.3) | 68.1 (15.9) | .199 |
| Impact score | 33.8 (18.3) | 32.7 (18.4) | 35.5 (18.2) | .327 |
| Hospital Anxiety and Depression Scale | n = 191 | n = 117 | n = 74 | |
| Anxiety score | 6.4 (3.9) | 6.2 (3.7) | 6.8 (4.2) | .294 |
| Depression score | 5.7 (3.6) | 5.5 (3.3) | 6.1 (3.9) | .223 |
| BODE index | n = 186 | n = 114 | n = 72 | |
| Score | 7.6 (2.01) | 7.5 (2.0) | 7.7 (2.0) | .584 |
| Lung Information Needs Questionnaire | n = 158 | n = 88 | n = 70 | |
| Score | 8.4 (3.6) | 8.7 (4.0) | 8.1 (3.0) | .281 |
| Patient Activation Measure | .170 | |||
| Level 1, n (%) | 28 (14) | 22 (19) | 6 (8) | |
| Level 2, n (%) | 35 (18) | 22 (19) | 13 (17) | |
| Level 3, n (%) | 72 (37) | 37 (31) | 35 (46) | |
| Level 4, n (%) | 59 (30) | 37 (31) | 22 (29) | |
| Activation score | 61.3 (15.1) | 60.5 (15.7) | 62.5 (14.2) | .358 |
a Data presented as mean (SD) unless otherwise stated.
Abbreviations: BODE, body mass index, airflow obstruction, dyspnea, and exercise; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; GOLD, Global Initiative for Chronic Obstructive Lung Disease; n, number; SD, standard deviation.
The pulmonary rehabilitation program was completed by 61% (n = 118) of participants. The primary reason for noncompletion of the program was medical issues unrelated to the program, such as a worsening of their chronic condition(s), new medical diagnoses, or chronic pain (51%). Other reasons included death (9%), disinterest (8%), transport/parking issues (7%), and caring duties/family issues (7%). In the small number of people with home oxygen therapy (n = 17), there was a significant difference between those who completed and those who did not complete the program (Table 4). Participants who completed the program had a significantly higher baseline mean 6-minute walk distance than those who did not complete the program (Table 4). There were no other significant characteristic differences between those who completed the program and those who did not. There was no significant difference in baseline PAM activation score between completers and non-completers of the pulmonary rehabilitation program (P = .358).
At baseline, the majority of participants (68%, n = 131) were activated, scoring a PAM level of 3 or 4. Poor activation (level 1) was present in 14% (n = 28) of the participants (Table 4). In people who completed the pulmonary rehabilitation program (n = 118), 63% (n = 74) scored a PAM level of 3 or 4 at baseline. Poor activation (level 1) was present in 19% (n = 22) of the completing participants at baseline assessment.
Effect of Pulmonary Rehabilitation
In people who completed the pulmonary rehabilitation program, the mean (SD) change in health outcomes were: 6-minute walk distance 52 (51) m, indicating an improvement in functional exercise capacity; St George’s Respiratory Questionnaire (SGRQ) total score –5 (10), indicating an improvement in health-related quality of life; Hospital Anxiety and Depression Scale (HADS) anxiety score –0.2 (3.4) and depression score –0.9 (2.7), indicating no change in anxiety and a slight decrease in depression; and Lung Information Needs Questionnaire (LINQ) score –3.0 (3.6), indicating an improvement in lung information knowledge.
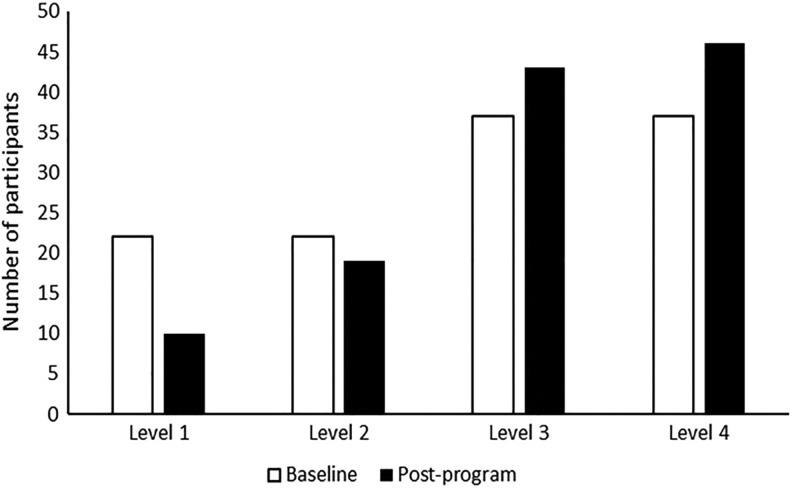
Effect of Pulmonary Rehabilitation on PAM
Patient Activation Measure scores improved significantly after completion of the pulmonary rehabilitation program. In people who completed the program, the mean (SD) PAM activation score improved from 60.5 (15.7) at baseline to 65.4 (15.5) after completion (P = .001). The number of participants categorized as PAM level 1 and 2 at baseline decreased post-program, while the number of participants categorized as PAM level 3 and 4 at baseline increased post-program (Figure 1). At post-program assessment, 75% (n = 89) were activated (PAM levels 3 and 4), with only 8% (n = 10) indicating poor activation (PAM level 1). Additionally, 37% of those who completed the program improved their PAM activation level, while 46% remained at the same level, and 17% saw a decline in their activation level (Table 5). There were no significant differences in participant demographics or in clinical variables between those participants whose PAM levels improved and those whose levels decreased or remained unchanged.
Figure 1.
Baseline and post-program PAM levels of people completing pulmonary rehabilitation.
Table 5.
Change in PAM Levels of People Completing Pulmonary Rehabilitation.
| Activation Level at Baseline | Activation Level Post-program | |||
|---|---|---|---|---|
| Level 1 | Level 2 | Level 3 | Level 4 | |
| Level 1 | Same level, n = 4 (18%) | 1 level increase, n = 9 (41%) | 2 level increase, n = 6 (27%) | 3 level increase, n = 3 (14%) |
| Level 2 | 1 level decrease, n = 4 (18%) | Same level, n = 5 (23%) | 1 level increase, n = 9 (41%) | 2 level increase, n = 4 (18%) |
| Level 3 | 2 level decrease, n = 2 (5%) | 1 level decrease, n = 3 (8%) | Same level, n = 19 (51%) | 1 level increase, n = 13 (35%) |
| Level 4 | 3 level decrease, n = 0 | 2 level decrease, n = 2 (5%) | 1 level decrease, n = 9 (24%) | Same level, n = 26 (70%) |
Relationships With PAM
The characteristics of participants and their association with baseline PAM score are reported as Pearson correlation coefficients in Table 6. The SGRQ impact and activity scores, HADS anxiety and depression scores, and LINQ score were significantly negatively associated with PAM activation score (P < .05; Table 6).
Table 6.
Correlation of Demographic and Clinical Variables With Baseline PAM Activation Score.
| All Participants (N = 194) | |||
|---|---|---|---|
| n | r | P Value | |
| Age, years | 194 | −0.04 | .581 |
| Gender, male | 194 | −0.02 | .820 |
| Aboriginal | 194 | −0.01 | .872 |
| English primary language | 194 | 0.07 | .362 |
| Current smoker | 194 | 0.00 | .959 |
| Home oxygen therapy | 194 | 0.07 | .350 |
| BMI, kg/m2 | 194 | 0.01 | .901 |
| Pulmonary function | |||
| FEV1, L | 185 | −0.02 | .784 |
| FVC, L | 185 | 0.01 | .910 |
| FEV1/FVC, % | 185 | −0.04 | .562 |
| 6-minute walk distance | 194 | 0.12 | .099 |
| SGRQ symptom score | 178 | −0.02 | .818 |
| SGRQ activity score | 178 | −0.18 | .016 |
| SGRQ impact score | 178 | −0.17 | .027 |
| HADS anxiety | 191 | −0.22 | .002 |
| HADS depression | 191 | −0.26 | <.001 |
| BODE index | 186 | −0.13 | .071 |
| LINQ | 158 | −0.22 | .006 |
Abbreviations: BODE, body mass index, airflow obstruction, dyspnea, and exercise; BMI, body mass index; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; HADS, Hospital Anxiety and Depression Scale; LINQ, Lung Information Needs Questionnaire; n, number; PAM, Patient Activation Measure; r, Pearson correlation coefficient; SGRQ, St George’s Respiratory Questionnaire.
Multiple Linear Regression Analysis
In a stepwise forward multiple regression analysis, higher HADS anxiety score, LINQ score, and SGRQ impact score were found to be significant determinants of baseline PAM (Table 7). This model explained 12% (P < .001) of the variance. The HADS anxiety score accounted for 6% of the variance in PAM.
Table 7.
Multiple Linear Regression Analysis Model for PAM.
| Adjusted r2 | 0.12 | |
|---|---|---|
| Variable | β | 95% CI |
| HADS anxiety score | −0.71 | −1.34 to −0.09 |
| LINQ score | −0.99 | −1.61 to −0.37 |
| SGRQ impact score | −0.15 | −0.28 to −0.02 |
Abbreviations: CI, confidence interval; HADS, Hospital Anxiety and Depression Scale; LINQ, Lung Information Needs Questionnaire; PAM, Patient Activation Measure; SGRQ, St George’s Respiratory Questionnaire.
Discussion
In this study, the majority of people commencing a pulmonary rehabilitation program demonstrated a moderate level of activation where they had some experience and success in making behavioral changes, had some confidence in handling aspects of their health, and were beginning to take action. Although patient activation was measured at the program baseline assessment, the results were not used to tailor the program to each individual’s level of knowledge, skills, and confidence. Despite this, overall, the level of activation improved following an 8-week hospital outpatient pulmonary rehabilitation program. Anxiety, a higher level of lung information needs, and greater health-related quality of life impact were significantly negatively associated with patient activation, although these factors only accounted for 12% of the variance.
People referred to and demonstrating a willingness to complete a pulmonary rehabilitation program by attending a baseline assessment self-reported a moderate level of activation. This population had a higher baseline PAM activation score (indicating better activation) than people with COPD attending primary or secondary care clinics in the Netherlands (4). This indicates that people attending a pulmonary rehabilitation program may be more activated than their peers with the same chronic health condition. In contrast, this group of people with predominantly moderate COPD and comorbidities, perhaps not surprisingly, had lower activation levels than their community peers living in the same socioeconomic areas, where 57% reported level 4 activation and a further 28% reported level 3 activation using the PAM (21).
To our knowledge, this is the first study demonstrating that pulmonary rehabilitation improves patient activation in addition to improving functional exercise capacity, quality of life, and lung information knowledge. To tailor care, the PAM guideline (Insignia Health, LLC, 2013) recommends using the information gleaned from the PAM to help guide a discussion and devise and negotiate an action plan using motivational interviewing techniques. In this study, open discussion of the patients’ responses to PAM items to gain insight as to how they view their situation and what barriers and facilitators they think may affect their ability to take positive steps was not performed. Using the PAM items to focus on building self-awareness knowledge, confidence or taking action appropriate to the individuals’ activation level was also not performed. This indicates that the comprehensive nature of pulmonary rehabilitation, including the combination of supervised exercise training, self-management education, and social support, is potentially sufficient to address the concepts of building activation and should be considered as part of the holistic management of people with a chronic respiratory disease or congestive cardiac failure with low activation levels. It is unclear which component of the rehabilitation program was responsible for the effect on patient activation; however, it is likely all components contributed in some way to affect the participants’ knowledge, skills, and self-efficacy of health behaviors.
Although patient activation improved overall in people who completed pulmonary rehabilitation, a proportion of people did not improve their PAM level following the program. This was most significant in people with a moderate to high baseline PAM level of 3 or 4. It is known that people with the lowest activation levels tend to increase the most (22). It is possible that in people already indicating higher activation, some of the PAM items may have a ceiling effect, which has been demonstrated in people with cardiac disease (23) and dysglycemia (24). The ceiling effect may be particularly pronounced when measuring change over time (24) as was conducted in this study. It is also possible that some of this population had high self-efficacy and overrated themselves at baseline, as indicated by the results showing that some patients did not change their PAM activation level, while others showed a decrease in their activation level. It is also possible that the group environment of a pulmonary rehabilitation program allows a comparison of one’s self to others with similar health conditions and gave them the ability to normalize their own condition and how well they were managing their chronic disease.
The determinants of patient activation in people with COPD have previously been examined. Similar to Korpershoek et al, this study found a significant association between anxiety and depression and activation. However, we also found that aspects of health-related quality of life (particularly the impact of chronic respiratory disease on health-related quality of life) could explain some of the variance in activation. Anxiety was found to be the greatest key determinant in patient activation in the models determined in both this study and that of Korpershoek et al. This highlights the importance of identifying and addressing anxiety in people with a chronic respiratory disease or congestive cardiac failure. The HADS was used to measure anxiety and depression levels in this study, and it is useful as a screening tool to identify people with these mental health conditions (15),which can easily be incorporated in a pulmonary rehabilitation assessment. The pulmonary rehabilitation program in this study included a group-based discussion with a clinical psychologist on living and coping with a chronic illness and dealing with unhelpful thoughts and beliefs. Individualized cognitive behavioral therapy is indicated in managing anxiety in this population (25) and thus should be considered in people with low activation. The LINQ score had a weak, significant correlation with the PAM activation score. A high LINQ score indicates from the patient’s perspective their learning and education need (26), and therefore, the association with a low PAM score may be attributed to people with a chronic respiratory disease or congestive cardiac failure feeling that they do not have enough knowledge and information to make good decisions about their health. The positive change in PAM activation scores found in people completing pulmonary rehabilitation may be a result of pulmonary rehabilitation filling knowledge gaps (26).
The low explanatory variance for activation in both our model (12%) and the Korpershoek et al study (17%) indicates that there are other factors contributing to patient activation which are unknown. The degree of self-efficacy may be one potential factor. Self-efficacy was not measured in this study; however, the Pulmonary Rehabilitation Adapted Index of Self-Efficacy tool is a reliable and sensitive measure of self-efficacy (27) and should be considered in future studies. Another unmeasured factor was the participant’s health-care providers. Interestingly, disease severity (as indicated by lung function and the prescription of home oxygen therapy) was not found to be a key determinant of activation in this study as had previously been shown when using a disease categorical staging system (4). Disease severity is a significant determinant of exercise capacity in people with COPD where the pathophysiology of the disease has been shown to impact the physical ability of the body to function (28). Our results indicate that underlying pathophysiology and the physical effect on the body are not associated with activation.
A strength of this study is the broad inclusion criteria which encompassed a large number of people with different chronic respiratory diseases and congestive cardiac failure. The pulmonary rehabilitation program was an evidence-based outpatient program, meaning the results could be generalized to many pulmonary rehabilitation programs across Australia and New Zealand (29). However, the PAM was administered by clinicians involved in the participants care and this may have introduced bias. There may have also been a degree of selection bias as the people included in this study had already been identified as suitable and referred to pulmonary rehabilitation at a large metropolitan center, and all had agreed to attend an initial assessment in preparation to commence the program. This study did not include those people referred to pulmonary rehabilitation but declining to attend an initial assessment and did not include people eligible for pulmonary rehabilitation but not referred. Furthermore, the people attending this pulmonary rehabilitation lived in low socioeconomic disadvantaged areas and there was a low representation of Aboriginal people. It is also not known whether the improvements found in patient activation following pulmonary rehabilitation are maintained over the longer term. It is known that the positive effects of pulmonary rehabilitation on important health outcomes such as exercise capacity and health-related quality of life wane over time (30). However, given existing evidence that suggests highly activated patients are more likely to engage in regular exercise than less activated people (1), it is possible that between 25% and 61% of patients (ie, post-program activation levels of 1, 2, and 3) may not maintain the short-term improvements in patient activation. A longer-term follow-up of outcomes could help to answer this question.
Clinically, this study demonstrates that it may be important to identify those patients with a low patient activation level at the baseline pulmonary rehabilitation assessment, especially if the patient presents with anxiety, a high level of lung information needs, and/or poor health-related quality of life. The results of the PAM may then need to be used to tailor the program to each individual’s level of knowledge, skills, and confidence. This warrants further investigation.
In conclusion, people with a chronic respiratory disease or congestive cardiac failure commencing a pulmonary rehabilitation program demonstrated a moderate level of activation, which improved following an 8-week hospital outpatient pulmonary rehabilitation program. Anxiety, a higher level of lung information needs, and greater health-related quality of life impact were significantly associated with poor patient activation.
Acknowledgment
The authors thank Rabia Khan who assisted with data analysis and South Eastern Sydney Research Collaboration Hub, South Eastern Sydney Local Health District for providing funding for analysis of data.
Author Biographies
Renae J McNamara is a clinical specialist physiotherapist in pulmonary rehabilitation at the Prince of Wales Hospital. Her research interests are investigating alternatives to traditional pulmonary rehabilitation including water-based exercise, telerehabilitation, community-based rehabilitation, and singing.
Rachel Kearns is a research officer working with the Centre for Primary Health Care and Equity at the University of New South Wales Sydney. Rachael has been involved in working on a number of research projects with a focus on integrated care and primary health care. This work has included projects investigating models of integrated primary health care centres in relation to integration, access and eHealth.
Sarah M Dennis is an associate professor Dennis is in the Discipline of Physiotherapy and Associate Professor of Allied Health in South Western Sydney Local Health District. Her research interests are in the prevention, diagnosis and management of chronic conditions, especially chronic respiratory conditions. The focus of this research is in the context of equity and access in primary health care, integration of care across health sectors and health literacy.
Mark F Harris is a professor and director, Centre for Primary Health Care and Equity, University of New South Wales and the Centre for Research Excellence in Obesity Management and Prevention in Primary Health Care, Sydney, New South Wales. His main area of research is on chronic illness prevention and management in primary health care.
Karen Gardner is a senior research fellow. She is a health services researcher with a background in sociology, a masters in population health and a PhD in primary health care. Karen’s research aims to improve the evidence base for policy and program implementation. Much of her research has been focused on the implementation of continuous quality improvement programs, primary care performance measurement and commissioning processes, and the evaluation of complex health interventions.
Julie McDonald is a senior research fellow and hub leader, South Eastern Sydney Research Collaboration Hub, Centre for Primary Health Care and Equity, University of New South Wales. Julie conducts research, evaluation and development that strengthens primary health care and address health inequities, with the aim of contributing to better, fairer health in the community. Her work addresses current issues in policy and practice, and she works with health and related services to implement the findings.
Authors’ Note: Ethics approval was provided by the South Eastern Sydney Local Health District Human Research Ethics Committee (HREC reference number 16/065).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The analysis of data from this project was funded by the South Eastern Sydney Research Collaboration Hub, South Eastern Sydney Local Health District.
References
- 1. Hibbard JH, Greene J, Shi Y, Mittler J, Scanlon D. Taking the long view. Med Care Res Rev. 2015;72:324–37. [DOI] [PubMed] [Google Scholar]
- 2. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the Patient Activation Measure. Health Serv Res. 2005;40:1918–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patients activation results in improved self-management behaviours? Health Serv Res. 2007;42:1443–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Korpershoek Y, Bos-Touwen ID, de Man-van Ginkel JM, Lammers JW, Schuurmans MJ, Trappenburg J. Determinants of activation for self-management in patients with COPD. Int J COPD. 2016;11:1757–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bos-Touwen I, Schuurmans M, Monninkhof EM, Korpershoek Y, Spruit-Bentvelzen L, Ertugrul-van der Graaf I, et al. Patient and disease characteristics associated with activation for self-management in patients with diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic renal disease: a cross-sectional survey study. PLoS One. 2015;10:e0126400 doi:10.1371/journal.pone.0126400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. ; ATS/ERS Task Force on Pulmonary Rehabilitation. An official American Thoracic Society/European Respiratory Society Statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:e13–64. doi:10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 7. Reardon J, Awad E, Normandin E, Vale F, Clark B, ZuWallack RL, et al. The effect of comprehensive outpatient pulmonary rehabilitation on dyspnea. Chest. 1994;105:1046–52. [DOI] [PubMed] [Google Scholar]
- 8. McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015:CD003793 doi:10.1002/14651858.CD003793.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Puhan MA, Gimeno-Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;12:CD005305 doi:10.1002/14651858.CD005305.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Effing T, Monninkhof EEM, van der Valk PPDLPM, Zielhuis GGA, Walters EH, van der Palen JJ, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007;4:CD002990 doi:10.1002/14651858.CD002990.pub2. [DOI] [PubMed] [Google Scholar]
- 11. American Thoracic Society (ATS). Standardization of spirometry, 1994 update. Am J Respir Crit Care. 1995;152:1107–36. [DOI] [PubMed] [Google Scholar]
- 12. Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respirir J. 2014;44:1428–46. [DOI] [PubMed] [Google Scholar]
- 13. Jones PW, Quirk FH, Baveystock CM. The St George’s Respiratory Questionnaire. Respir Med. 1991;85:25–31. [DOI] [PubMed] [Google Scholar]
- 14. Rector TS, Kubo SH, Cohn JN. Patients’ self-assessment of their congestive heart failure. Part 2: content, reliability and validity of a new measure, the Minnesota Living with Heart Failure Questionnaire. Heart Failure. 1987;3:198–209. [Google Scholar]
- 15. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- 16. Hyland ME, Jones RC, Hanney KE. Information needs in COPD patients: the Lung Information Needs Questionnaire. Airways J. 2005;3:142–4. [Google Scholar]
- 17. Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. New Engl J Med. 2004;350:1005–12. [DOI] [PubMed] [Google Scholar]
- 18. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39:1005–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Field A. Discovering Statistics Using SPSS. 3rd ed London: SAGE Publications Ltd; 2009. ISBN 978-1-84787-906-6. [Google Scholar]
- 20. Australian Bureau of Statistics. Socio-Economic Indexes for Areas (SEIFA) 2011. Retrieved May 15, 2018, from: http://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001.
- 21. Pifarre M, Frost K. Measuring Patient Activation in South Eastern Sydney. South Eastern Sydney Medicare Local 2015. Retrieved May 15, 2018, from: https://www.slideshare.net/MariaPifarre/pam-survey-final-for-web.
- 22. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences: fewer data on costs. Health Affairs. 2013;32:207–14. [DOI] [PubMed] [Google Scholar]
- 23. Ngooi BX, Packer TL, Kephart G, Warner G, Koh KW, Wong RC, et al. Validation of the Patient Activation Measure (PAM-13) among adults with cardiac conditions in Singapore. Qual Life Res. 2017;26:1071–80. [DOI] [PubMed] [Google Scholar]
- 24. Maindal HT, Sokolowski I, Vedsted P. Translation, adaption and validation of the American short form Patient Activation Measure (PAM13) in a Danish version. BMC Public Health. 2009;9:209 doi:10.1186/1471-2458-9-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hynninen MJ, Bjerke N, Pallesen S, Bakke PS, Nordhus IH. A randomized controlled trial of cognitive behavioral therapy for anxiety and depression in COPD. Respir Med. 2010:104:986–94. [DOI] [PubMed] [Google Scholar]
- 26. Jones RC, Wang X, Harding S, Bott J, Hyland M. Educational impact of pulmonary rehabilitation: Lung Information Needs Questionnaire. Respir Med. 2008;102:1439–45. [DOI] [PubMed] [Google Scholar]
- 27. Vincent E, Sewell L, Wagg K, Deacon S, Williams J, Singh S. Measuring a change in self-efficacy following pulmonary rehabilitation: an evaluation of the PRAISE tool. Chest. 2011;140:1534–39. [DOI] [PubMed] [Google Scholar]
- 28. Andrianopoulos V, Wagers SS, Groenen MT, Vanfleteren LE, Franssen FM, Smeenk FW, et al. ; CIRO+ Rehabilitation Network. Characteristics and determinants of endurance cycle ergometry and six-minute walk distance in patients with COPD. BMC Pulm Med. 2014;14:97 doi:10.1186/1471-2466-14-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Alison JA, McKeough ZJ, Johnston K, McNamara RJ, Spencer LM, Jenkins SC, et al. ; Lung Foundation Australia and the Thoracic Society of Australia and New Zealand Australian and New Zealand Pulmonary Rehabilitation Guidelines. Respirology. 2017;22:800–819. doi:10.1111/resp.13025. [DOI] [PubMed] [Google Scholar]
- 30. Troosters T, Gosselink R, Decramer M. Short- and long-term effects of outpatient rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Am J Med. 2000;109:207–12. [DOI] [PubMed] [Google Scholar]