Abstract
The proportion of older adults is increasing around the world and most wish to live in their home until they die. To achieve this, many will require services in the home to remain living independently. To maintain function (ie, strength, balance, and endurance), physical activity needs to be undertaken on a regular basis, and is essential as a person ages. Unfortunately, as people age there is a tendency to reduce activity levels, which often leads to loss of function and frailty, and the need for home care services. This updated systematic review includes a mix of study methodologies and meta-analysis, and investigated the effectiveness of physical activity/exercise interventions for older adults receiving home care services. Eighteen studies including ten randomized controlled trials meeting the selection criteria were identified. Many of the studies were multi-factorial interventions with the majority reporting aims beyond solely trying to improve the physical function of home care clients. The meta-analysis showed limited evidence for effectiveness of physical activity for older adults receiving home care services. Future exercise/physical activity studies working with home care populations should consider focusing solely on physical improvements, and need to include a process evaluation of the intervention to gain a better understanding of the association between adherence to the exercise program and other factors influencing effectiveness.
Keywords: exercise, physical function, community care, reablement, seniors
Introduction
Populations throughout the world are increasing in age, with greater proportions of older people than previously observed.1 Most older people have a desire to live in their home until they die2 and to do this, they need to be able to complete activities of daily living (ADLs) such as showering, dressing, eating, and toileting independently. For some older adults these tasks become increasingly difficult due to health issues, frailty or disability, and they require assistance to continue living in their home.3 This assistance is often provided by home or community care services and is predominantly funded by the government in high income countries such as Australia, Canada, and a number of European countries.4–6
Home care services can be delivered over the short or longer term.7 Some short-term reablement services (ie, goal-oriented, person-centered, often aimed at reduced long-term services) include physical activity or exercise programs, whereas the longer term services such as personal care (ie, showering), domestic assistance (ie, cleaning), gardening, transport, and social support usually do not. In order to assist an older person to continue living in their home and complete their ADLs, they need to maintain strength, balance, and endurance.8,9
Improving or maintaining strength, balance, and endurance requires a desire to be active, the knowledge of what to do, and the opportunity to be active.10,11 The World Health Organization and many individual countries (ie, United States, Canada, Great Britain, Australia) have produced National Physical Activity Guidelines for older adults.12–15 They predominantly recommend 30 minutes of moderate intensity endurance physical activity every day such as walking or swimming, in addition to strength and balance training twice a week.12–15 The strength and balance components are essential for maintaining independence and completing ADLs.16 Strength and balance training also leads to many health benefits such as increased strength and bone density, reduction in sarcopenia, frailty, and chronic illness9,16–18 and has the strongest evidence for preventing falls for older adults living in the community.19 Unfortunately, these exercise modalities are often overlooked when promoting physical activity recommendations to older adults, particularly those receiving home care services.20
Many older home care clients walk to be active, however few participate in strength and balance programs.21 It can be difficult for home care clients to leave their home, and typically, shopping and medical appointments are prioritized, particularly when assistance with transport is required. To support older adults receiving home care services to, at a minimum, maintain their strength and balance, and at best, improve it over time, promoting physical activity within the home is required. Organizations delivering home care services have the ideal opportunity to do this, as many home care workers deliver services from once a week to multiple times each week. A previous systematic review22 evaluated the effectiveness of physical activity (exercise) programs for home care clients, however, at the time only eight articles were identified. The evidence (ie, outcomes and assessments) varied widely and was limited, as such, a meta-analysis could not be undertaken. Therefore, as the focus on older adults receiving home care services continues to increase, it is essential to identify whether further studies have been undertaken. This will help guide home and community care organizations to provide evidence-based care for their older clients and assist policy-makers to understand the benefits of improved physical function for this older population whom they heavily fund (eg, Irish government spends €408 million on home support each year which equates to 17 million visits).6 This current systematic review looks at the recent evidence and where possible combines the randomized controlled trials (RCTs) (n=2) from the previous systematic review with more recently published studies, to determine the effectiveness of physical activity/exercise programs delivered specifically to older adults receiving home care services.
Material and methods
Eligibility criteria
The review is limited to studies that met the following eligibility criteria:
population: aged 65 years and older (at least 50% of sample) and receiving home care services during the intervention. Home care services may include (but not limited to) personal care (showering), domestic assistance, transport, shopping or social care. These services are delivered in an older persons home by home or community care organizations (ie, municipalities etc) and can be short-term or long-term ongoing services.
Intervention: has to have a physical activity or exercise aspect to the intervention.
Comparison: for RCTs the comparison group will be usual care (ie, which may include a current physical activity or exercise program used) or a non-active control group.
Outcomes: the physical activity or exercise intervention has to have been assessed using at least one physical performance outcome (ie, mobility, endurance, strength, balance).
Setting: community-dwelling people only.
Any quantitative study could be included, eg, pilot or feasibility, pre- and post-test, retrospective, controlled trials or RCTs. Only peer-reviewed journal articles in English were included. No unpublished data (ie, reports), books, conference proceedings, theses, or poster abstracts were included. Exclusion criteria were: those living in residential care, and samples with >50% with a diagnosis of dementia or neurodegenerative disorder because they often require greater supervision and/or carer input to complete the physical activity/exercise intervention and therefore may not be representative of a typical home care service.
Information sources
Five databases were searched between October 2012 and August 2018: Medline (Proquest); CINAHL; PubMed; PsycInfo; and SportDiscus. The previous systematic review search included articles between January 1982 to September 2012. Reference lists from these papers were also scanned.
Search strategy
The search included the same mix of keywords as used in the previous systematic review. However, this updated review also included “reablement” as a search term. An example of the search strategy is presented in Table 1.
Table 1.
Search strategy
| 1 | Community care |
| 2 | Community health care |
| 3 | Home care |
| 4 | Community nursing |
| 5 | Home and community care |
| 6 | Home support |
| 7 | Community rehabilitations |
| 8 | Restorative care |
| 9 | Reablement |
| 10 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 |
| 11 | Physical activity |
| 12 | Exercis* |
| 13 | 11 or 12 |
| 14 | Ageing |
| 15 | Aging |
| 16 | Aged |
| 17 | Older |
| 18 | Elderly |
| 19 | 14 or 15 or 16 or 17 or 18 |
| 20 | 10 and 13 and 19 |
Study selection
Study selection was conducted in three stages. Stage one was the initial screening of the titles and scanning the abstracts against the eligibility criteria to identify potential articles (completed by KF). Stage two included screening the full articles by two authors (EB and KF) to identify whether they met the eligibility criteria. In stage three, disagreements were resolved through discussion between EB and KF to achieve consensus, after referring to the eligibility criteria and protocol. The PRISMA checklist was used to ensure the results were reported systematically.23
Data collection process
Each study in the review was evaluated using a standardized extraction form, which included study design; purpose; intervention; study characteristics including sample size, sex proportion, participant age, intervention type; and length of follow-up (Tables 2 and 3).
Table 2.
Summary of included randomized controlled trial (RCT) studies
| Reference (country) study design | Study purpose | Sample size; % female; age (years)(SD) comparator | Population | Outcomes and measurement; follow-up |
Intervention effect |
|---|---|---|---|---|---|
| Burton et al,28 (Australia) Pragmatic randomized controlled trial | Determine whether LiFE would be undertaken more often and result in greater functional gains than the current structured exercise program delivered as part of a restorative home care service | LiFE =40; 75%; 80.2 years (6.4) Structured exercise =40; 90%; 79.6 years (6.2) Yes |
Living in Perth suburbs (Western Australia) referred for a restorative home care service | Functional reach, chair sit-to-stand (1 and 5), TUG, Tandem walk, FES, ABC Scale, Vitality Plus Scale, The Late Life Function and Disability instruments 8 weeks |
LiFE group significantly improved in 95% (19 of 20) of outcome measures, compared with the structured exercise group, which significantly improved in 70% (14 of 20). |
| Burton et al,29 (Australia) Pragmatic randomized controlled trial | Examine over the longer term, the effectiveness and maintenance of a (modified) LiFE compared to the current, structured exercise program used in a restorative home care service | LiFE =40; 75%; 80.2 years (6.4) Structured exercise =40; 90%; 79.6 years (6.2) Yes |
Living in Perth suburbs (Western Australia) referred for a restorative home care service | Functional reach, chair sit-to-stand (1 and 5), TUG, Tandem walk, FES, ABC Scale, Vitality Plus Scale, The Late Life Function and Disability instruments, 6 month fall history 8 weeks and 6 months |
A significant main effect of time was found for all measures. LiFE showed significantly greater improvement than the structured exercise group for tandem walk, ABC score, and Vitality Plus scale |
| Danilovich et al,30 (USA) Randomized controlled trial | To test the effects of SFL exercise program on the physical performance and self-rated health of older adults enrolled in the Community Care Program, a Medicaid waiver program | 42; 83%; 74.8 years Intervention =24; 83%; 74.1 years Control =18; 83%; 75.6 years Yes |
Community-dwelling older adults receiving HCA services through the Community Care Systems, Inc. in Illinois | Grip and quadriceps strength using a hand-held dynamometer, TUG, 10 ft gait speed, Self-Efficacy for Exercise, pain, and PROMIS-global health 12 weeks |
Effect sizes were moderate for grip strength, pain, and PROMIS-global health. SFL participants significantly improved median quadriceps and TUG (median only) scores compared to controls. No adverse health events and high program satisfaction were reported. Frailty prevalence in the control group increased whereas it decreased in the SFL group. |
| Danilovich et al,31 (USA) Randomized controlled trial | Determine the feasibility of training HCAs to lead the SFL program with their Community Care Program clients | 42; 83%; 74.8 years (8.8) Intervention =24; 83%; 74.1 years (9.9) Control =18; 83%; 75.6 years (8.1) Yes |
Community-dwelling older adults receiving HCA services through the Community Care Systems, Inc. in Illinois | Client and HCA program satisfaction rates, HCA SFL training evaluation information and SFL fidelity rates 12 weeks |
It is feasible for HCAs to implement SFL safely with clients. Participants viewed SFL as highly satisfactory and HCAs were able to adapt SFL for their clients. HCAs have high job satisfaction, and leading SFL enhances work achievement and pride |
| King et al,32 (New Zealand) Cluster randomized controlled trial | Evaluate the impact of a restorative home care service, compared with usual care for community-dwelling older people | 186; 74%; 79 years Restorative =93; 69.9%; 78.4 years (6.5) Control =93; 77.4%; 80.5 years (6.3) Yes |
Older people receiving assistance from a home care agency in New Zealand | SF-36, Nottingham Extended ADL, TUG, Mastery scale, DSSI 4 and 7 months |
Significant benefit in health-related quality of life (SF-36) at 7 months compared to usual care, particularly in the mental health component. A significantly higher number of older people in the intervention group were identified for reduced paid caregiver support or discharge |
| Parsons et al,33 (New Zealand) Cluster randomized controlled trial | To determine the impact of a restorative model of home care on social support and physical function among community-dwelling older people | Intervention =108; 71.3%; 79.1 years (6.9) Usual care =97; 60.8%; 76.9 years (7.6) Yes |
Community-dwelling people older than 65 years (55 years if Maori or Pacific Islander) were eligible if they were new referrals to the care coordination agency for home care in New Zealand | SPPB, DSSI 6 months |
Intervention group had a greater mean increase in physical function over time than the usual care group as determined by overall SPPB |
| Renehan et al,36 (Australia) Randomized controlled trial | Determine feasibility and acceptability of a community-delivered post-hospital falls prevention program, incorporating exercise, medication review, and education | 13; 53.8%; 82.2 years (9.7) Intervention =7; 57.1%; 84.0 years (6.4) Control =6; 50% 75.8 years (11.6) Yes |
Recently discharged from a hospital within metropolitan Melbourne, Australia after being admitted for a fall and a new or existing client of the community home care organization | Quality of life (AQoL-8D), falls, fall risk (FROP-Com), FES-I, Fried Frailty Criteria, Katz ADL, qualitative falls interview. Intervention only: five times sit-to-stand, 4 test balance scale (feet together, semi-tandem, tandem and one leg stand), TUG 6 months |
The exercise component of the multifactorial intervention was highly valued by intervention participants. Five falls during intervention period: intervention group: 3; control group: 2. No significant changes in physical outcome measures. |
| Saeterbakken et al,37 (Norway) Randomized controlled trial | Determine the effects of a 10-week home-based strength training program on physical function tests, level of physical activity, muscle strength, and RFD among frail old adults receiving home care services | 23; 73.9% Intervention =11; 86.5 years (6.4) Control =12; 83.5 years (5.7) Yes |
Older adults living at home and in need of home care due to functional disabilities and/or medication | Leg extension and elbow flexion maximal strength and RFD, preferred/max walking speed, stair climb, 5x chair rise and physical activity (accelerometer) 10 weeks |
Intervention group significantly improved peak RFD in leg extension |
| Stevens-Lapsley et al,34 (USA) Randomized controlled trial | To determine whether a progressive multicomponent physical therapy intervention in the home setting can improve functional mobility for deconditioned older adults following acute hospitalization compared to usual care rehabilitation | 22; 63.6%; 85.4 years (7.8) Intervention =12; 70%; 83 years (6.8) Usual care =9; 58.3%; 87 years (8.8) Yes |
Older adults with multiple chronic conditions, who were discharged from the Acute Care for the Elderly unit of the University of Colorado Hospital, with physician referrals for home health physical therapy | 4 m walking speed, modified Physical Performance Test, SPPB, six minute walk test 30 and 60 days |
Intervention group had significantly greater improvements in walking speed, modified physical performance test, and SPPB scores compared with the usual care group at 60 days |
| Tuntland et al,35 (Norway) Randomized controlled trial | Investigate the effectiveness of reablement (multicomponent home-based rehabilitation) in older adults compared with usual care in relation to daily activities, physical functioning, and health-related quality of life | Intervention =31; 71%; 79.9 years (10.4) Control =30; 63.3%; 78.1 years (9.8) Yes |
People applying for, or referred to, home-based services due to functional decline in one or more ADL in a rural municipality in Norway | COPM was used to measure self-perceived activity performance and satisfaction with performance. Health-related quality of life (COOP/Wonka), TUG, grip strength 3 and 9 months |
Significant improvements in mean scores favoring reablement in COPM performance at 3 and 9 months and overall treatment, and for COPM satisfaction at 9 months and overall treatment |
Abbreviations: LiFE, Lifestyle-integrated Functional Exercise program; TUG, Timed Up and Go; FES, Falls self-Efficacy Scale; ABC, Activities specific-Balance Confidence Scale; SFL, Strong For Life; HCA, home care aide; ADL, activities of daily living; DSSI, Duke Social Support Index; SPPB, Short Performance Physical Battery; FROP-Com, Falls Risk for Older People – Community Setting; FES-I, Falls self-Efficacy Scale – International; RFD, Rate of Force Development; COPM, Canadian Occupational Performance Measure.
Table 3.
Summary of intervention implementation for randomized controlled trial (RCT) studies
| Reference | Implementation strategy | Intervention |
|---|---|---|
| Burton et al,28,29 | LiFE and structured exercise program were delivered by care managers as part of a restorative home care service. Clients were visited every 10–14 days by their care manager (average 3 visits) to offer support, encouragement and to progress exercises. Exercise was just one aspect of their service that was discussed during these visits | LiFE intervention =7 balance and 6 lower limb strength exercises incorporated into everyday activities. Exercises were explained by care manager and a descriptive manual was given to clients. Control group: structured exercises =3x per day 5 repetitions of 6 strength and 2 balance exercises (15–20 minutes). Exercises were provided on a sheet illustrating exercises. |
| Danilovich et al,30,31 | HCAs attended a half-day SFL training session. HCAs completed SFL with their clients 2x per week for the first 2 weeks of the program with clients completing a third session independently. After the initial 2-week period, HCAs provided their clients motivation at each usual care visit (2–3x per week) to perform SFL 3 times a week for an additional 10 weeks. | 12 weeks SFL; 35-minute DVD that includes a warm up, 11 upper and lower extremity exercises using therabands for resistance, and a cool down. |
| King et al,32 | Paid caregivers undertook 2 training programs based on a restorative care philosophy designed to optimize independence in older people, taking approximately 5 and 18 weeks. Coordinator (experienced registered nurse) undertook an initial in-depth assessment with the participant using TARGET, leading to a support plan for paid caregivers to implement at visits with participants, ranging from daily to fortnightly. Coordinators provided enhanced supervision for paid caregivers by undertaking compulsory 2-hour fortnightly meetings and also provided follow-up consultations with participant (phone call or visit) every 3 months, and a full re-assessment at 12 months | Repetitive ADL exercises designed to optimize independence and to further support participant in reaching their goals |
| Parsons et al,33 | Intervention group completed a goal facilitation tool (TARGET) with a needs assessor to determine their needs and to establish the aims for the episode of care. Services were structured according to the principles of restorative home care (independence focused with individually tailored activity programs). HCAs then completed tasks outlined in the support plan for each individual. | Home care services included domestic tasks, personal care, shopping, and individualized activities (walking or exercise programs/other activities aimed at improving functional ability). In the intervention group 61.7% (n=66) of the support plans described such individualized activities as opposed to 15% (n=14) in the usual care group. |
| Renehan et al,36 | Participants were approached 1–2 weeks after discharge, intervention included a medication review, falls prevention education, and home-based exercise individually prescribed and modified according to pre-existing frailty by exercise physiologist (visits at weeks 1, 2, 4, and 8 for exercise progression), participants were provided diagrams of exercises and instruction on exercise safety. Participant’s primary nurse who regularly visited for other matters provided encouragement. | Three to five times per week 20–30 minutes graduated lower limb strengthening and balance exercises (Otago Exercise Programme) |
| Saeterbakken et al,37 | A professional training instructor was present at every training session to make sure of the correct technique, intensity, and numbers of sets. | Supervised progressive strength training programme 60 minutes 2x week for 10 weeks, 10–12 repetitions 2–3 sets squats, box lifts, seated row, chest press, and biceps curl. |
| Stevens-Lapsley et al,34 | Patients placed in the progressive multicomponent intervention group were referred to home health agency and were seen by a single physical therapist who was trained to provide the progressive intervention. Two to three physical therapy visits per week for 30 days. | Progressive multicomponent physical therapy intervention consisted of ADL training (bathroom transfers, bed mobility, and car transfers), evidence-based mobility training (indoor walking, gait training on flat ground and stairs, and outdoor walking transitioning to an independent daily walking program) and progressive strength training (3 sets 8 repetitions max supine leg press, standing hip extension, body-weight resisted plantar flexion, seated press and seated row using the Shuttle Mini Press). Participants were given a home exercise program to continue basic exercises after discharge. |
| Tuntland et al,35 | Occupational and physical therapists used COPM to identify activity limitations perceived as important by the participant and developed a rehabilitation plan with a maximum rehabilitation period of 3 months. Therapists supervised HCA whose focus was on stimulating the participants to perform the daily activities themselves, rather than letting others do it for them, physiotherapist and/or occupational therapist visited participants for a minimum of 1 hour each week. All HCAs attained training before the intervention was implemented. Therapists had weekly informal lunch meetings with HCAs in order to ensure good communication and follow-up of individual participants | Individualized reablement program including training in daily activities (dressing, food preparation, vacuuming, bus transport), adaptations to the environment or the activity to simplify activity performance, and exercise programs such as indoor or outdoor walking with or without walking aids, climbing stairs, transferring, and performing exercises to improve strength, balance or fine motor skills. The exercises were incorporated into daily routines and participants were given a manual explaining each of the exercises and encouraged to train on their own |
Abbreviations: LiFE, Lifestyle-integrated Functional Exercise program; SFL, Strong For Life; HCA, home care aide; TARGET, Towards Achieving Realistic Goals in Elders Tool; ADL, activities of daily living; COPM, Canadian Occupational Performance Measure.
Study quality
Study quality for the RCTs was assessed by two independent researchers (KF and RG) using the Cochrane’s Risk of Bias Tool.24 Categories assessed by the tool include sequence generation, allocation concealment, blinding of participants, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias.24 RCT studies were assessed as having “low”, “medium” or “high” risk of bias. Discussions were undertaken between the reviewers and where required, a third researcher (EB), to form consensus.
Study quality was reviewed by two researchers (KF, EB) for all other included papers, using the National Institute for Health and Care Excellence (NICE) guidelines appraisal checklist.25 The internal and external validity of the included papers were assessed by addressing key aspects of study design such as participant characteristics, allocation and intervention details, outcomes assessed, and methods of analyses.25 Each study was awarded an overall study quality grading (ie, ++ all or most of the checklist criteria have been satisfied, where they have not, it was deemed unlikely to alter the conclusions; + some of the checklist criteria have been satisfied, where they have not, it is unlikely these will alter the conclusions; and – few or no checklist criteria have been satisfied and are likely or very likely to alter the conclusions).25
Data analysis
Physical performance outcome measures from the RCTs included in this current review and the previous review22 were collated to determine whether there were two or more studies that utilized the same outcome measures.26 For those studies that did, a meta-analysis was undertaken. Authors were contacted if data were not available within the published article. Four performance outcomes were utilized in the meta-analyses and all were measured using continuous data: Timed Up and Go (TUG), sit-to-stand five times, grip strength, and walking speed. The mean difference (MD) and 95% CIs were calculated. Review Manager (RevMan) version 5.3 was used to conduct the analyses and generate forest plots with a random effects model applied and using the inverse variance DerSimonian and Laird method.27 Heterogeneity was assessed using the I2 statistic and by visual inspection of the forest plots. Statistical significance was set at p<0.05 for all analyses.
Results
Study selection
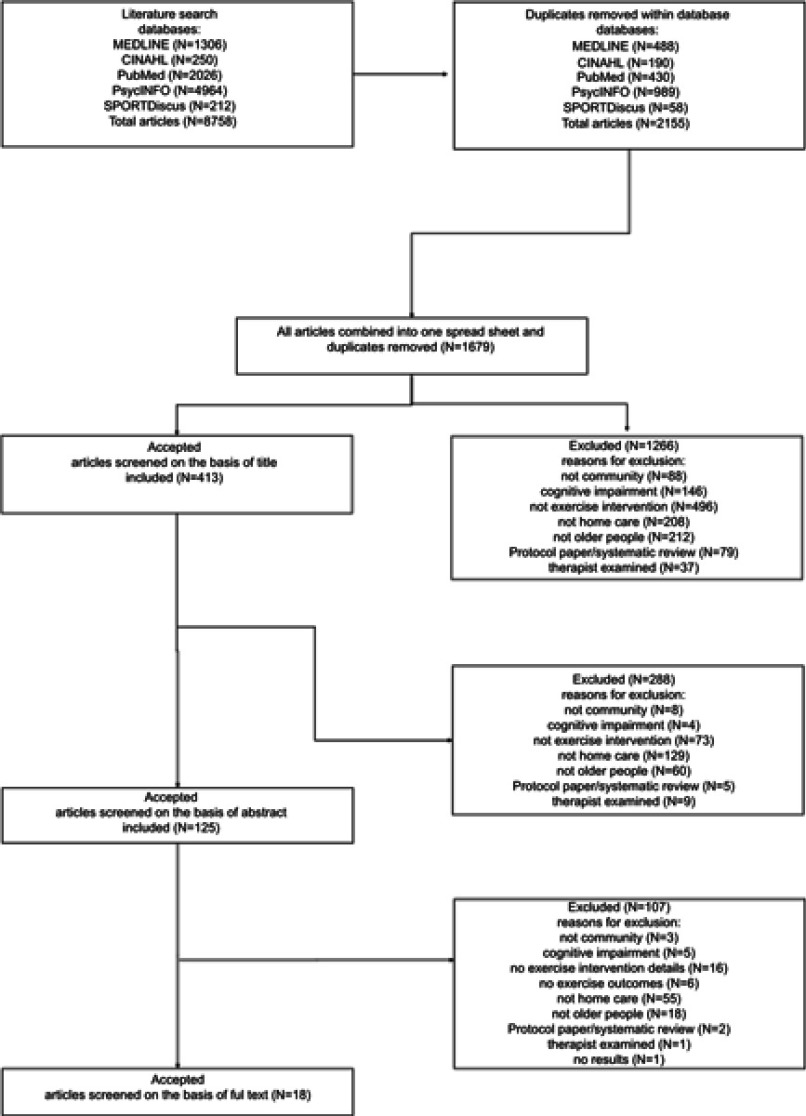
Eight thousand seven hundred and fifty eight papers were found in the five databases. After removing duplicates from each database and then across databases, 1,679 articles remained. Articles were screened by title and 1,266 were excluded. Reasons for exclusion are presented in Figure 1 – the study flow chart. Article abstracts were then read and a further 288 excluded, leaving 125 articles to be screened by full text. One hundred and seven studies were excluded and 18 studies were accepted to be included in the review.
Figure 1.
Flow chart of study selection.
Study characteristics
The 18 studies in the review included ten RCTs;28–37 six single group pre- and post-test studies;38–43 one feasibility study;44 and one retrospective study.45
There were 1,118 participants across the 18 studies, ranging from eight in a pilot study39 to 228 in the retrospective study.45 The average age of all participants was 80.4 (±3.3) years and ranged from 74.5–85.4 years; 71.8% of the participants were female. Seven studies were conducted in the United States;30,31,34,38,41,42,45 six in Australia;28,29,36,39,43,44 two in New Zealand32,33 and Norway;35,37 and one in Hong Kong.40
Interventions
RCTs
The average age of the 656 participants in the ten RCTs was 80.4 (±3.7) years, ranging from 74.5–85.4 years and included an average of 69.6% females. A number of different interventions were trialed. However, the majority focused on strength and balance training. Table 2 presents a summary of the included RCT studies and Table 3 outlines the interventions implemented.
The two Burton et al28,29 RCTs utilized the Lifestyle-integrated Functional Exercise (LiFE) program which incorporates seven balance and seven strength exercises into an older person’s daily living activities.46,47 The intervention was compared with a structured exercise program that focused on strength and balance also in an RCT over two time periods; 8-week intervention28 and a 4-month maintenance period.29 It must be noted the control group was active and received the structured exercise program that was delivered within the usual restorative care service. Whereas, Danilovich et al created the Strong For Life (SFL) resistance training program, which included a 35-minute DVD to assist home care aides to deliver the program.30,31
The exercise intervention in King et al’s study32 used exercises that optimized independence, incorporating repetitive functional ADLs. Parsons et al33 used a similar exercise intervention, again with the aim of optimizing independence and improving functional ability by incorporating individualized activities, 62% of the support plans described included these activities with their participants compared to 15% for the control group (ie, usual care).
Stevens-Lapsley et al34 utilized a progressive multicomponent physical therapy intervention for 60 days to improve functional mobility for older adults who had just left hospital. Tuntland et al35 trialed a reablement intervention, which was individualized for each participant. The exercise programs typically included indoor or outdoor walking, climbing stairs, transferring, engaging in strength and balance training, and improving fine motor skills. Similar to the LiFE program utilized by Burton et al,28 many of the exercises were incorporated into ADLs. In a further study by Saeterbakken et al,37 they conducted a 10-week fully-supervised strength training intervention which was delivered twice a week to participants.
Other studies
The other eight studies that were not RCTs included 462 participants, with an average age of 80.5 (±3.0) ranging from 76.8–83.8 years and included an average of 74.8% females. Table 4 presents a summary of the included studies that are not RCTs and Table 5 the interventions implemented. Bamgbase and Dearmon38 reported delivering a 6-month individualized home exercise program with no other detail, and the main aim was preventing falls by using a multi-factorial intervention.
Table 4.
Summary of included non-randomized controlled trial (RCT) studies
| Reference (country) Study design | Study purpose | Sample size; % female; age (years)(SD) comparator | Population | Outcomes and measurement follow-up | Intervention effect |
|---|---|---|---|---|---|
| Bamgbade and Dearmon,38 (USA) Quasi-experimental single group study pre and post-test | Evaluate the impact of a fall assessment tools and patient-specific fall prevention programs in reducing the incidence of falls and fall-related injuries among older patients receiving home HHS | 30; sex unknown; aged 65 and over No |
Receiving nursing care services on a long-term basis. Suffer varying degrees of physical, mobility, or cognitive impairments, such as diabetes, stroke, and urinary incontinence | Number of falls and falls with injuries 6 months | Reduction of falls and major injuries. |
| Burton et al,39 (Australia) Quasi-experimental single group study pre- and post-test (pilot) | Determine whether a LiFE was suitable for delivery in a restorative home care service | 8; 75%; 80.8 years (5.9) No |
Current restorative home care clients, living in Perth (Western Australia) | Functional reach, chair sit-to-stand (1 and 5), TUG, Tandem walk, FES, ABC Scale, Vitality Plus Scale, The Late Life Function and Disability instruments, PASE, Accelerometer, LiFE Assessment tool, 8 weeks |
Difficulties using the accelerometer and LiFE Assessment tool. Significant improvement in FES, tandem walk, Late Life Function total score, and PASE |
| Burton et al,44 (Australia) Feasibility study | To investigate the feasibility of community care workers delivering a falls prevention exercise program to older clients, at low or medium risk of falling, as part of an existing service provision | 29; 65.5%; 82.7 (8.7) years No |
Older adults receiving at least one community care service from a participating community care organization or an RAS assessment, living in Perth, Western Australia | FROP-Com, Physical Activity Readiness Questionnaire (PARQ) and LiFE assessment tool measured at baseline. Client and staff program satisfaction measured post-test. 8 weeks |
LiFE exercise program was safely delivered by RAS assessors and support workers, with no adverse events reported. The majority of clients (82%) reported enjoying the exercises, 59% felt it made a positive change to their health. Exercise adherence: 4.8 (SD: 2.2) days per week. |
| Gallagher et al,45 (USA) Retrospective | Determine concurrent based validity of the MAHC-10 with the Performance Oriented Mobility Scale (Tinetti), and determine the benefit of the Balanced Approach rehabilitation program. | 228; sex unknown; aged 65 and over No |
Patients referred for home care services to Catholic Home Care | MAHC-10 and Tinetti scores 6 months |
There was weak but significant negative relationship between the MAHC-10 and pre-Tinetti scores. Significant differences in Tinetti scores between pre- and post-intervention |
| Henwood et al,43 (Australia) Single group study pre- and post-test | Develop an HCA-led exercise program for older adults with aged care needs and evaluate the benefits from both the perspective of the HCA and the person receiving the program | 50; 74%; 82.1 years (6.1) No |
Older adults receiving government-funded domestic assistance or personal care in Brisbane, Australia | SPPB, falls, hours of sleep, visits to a general or clinical practice health professional, emergency department/hospital, exercise compliance, SF-36 18 weeks |
Significantly improved SPPB score, 19% reduction in participants classified as frail and a reduction in health care service access of 47% across the intervention |
| Kwok et al,40 (Hong Kong) Quasi-experimental pre- and post-test | Compare the effects of an exercise program supervised by a physiotherapist at a day training center with an exercise program delivered by a care worker at home on physical function, quality of life, and fall incidence in community-dwelling older adults | Center-based =24; 70.8%; 84.4 years (6.9) Home-based =26; 73.1%; 83.2 years (7.0) 5 center-based and 4 home-based participants had MMSE <12 Yes |
Clients admitted to the Enhanced Home and Community Care Service team, residing in the Wong Tai Sin District (Hong Kong). Suffering from chronic diseases with moderate or severe level of impairment | Elderly Mobility Scale, BBS, Numeric Pain Rating Scale, SF-12, and fall incidence 6 months |
Center-based participants had significant improvement in all outcomes and less falls compared to home-based participants |
| Muramatsu et al,41 (USA) Single group study pre- and post-test | Test and enhance the feasibility of HM program delivered by HCAs for community-dwelling older adults in a Medicaid-funded home care setting | 54; 78%; 77 (63–101) years; almost 1/3 had mild cognitive impairment No |
Receiving in-home support services through the Illinois Department on Aging Community Care Program, Chicago | Daily activity difficulties and dependency (HM6, BADL, IADL), performance of 3 HM movements, SSPB, self-rated general health and pain, FES-I, falls, and exercise related social support 4 months |
Clients‘ daily activity function and health outcomes improved significantly. The program was well-received by clients, high retention rates among clients (93%) |
| Park and Chodzko-Zajko,42 (USA) Single group study pre- and post-test | Assess the feasibility of implementing simple, safe, non-equipment evidence-based movements (HM program) using an affordable and sustainable HCA based delivery model that reaches the maximum possible number of frail older adults living at home but who are at risk of nursing home admission | 13; 84.6%; 76.8 years (11.4) No |
Older adults receiving home care services provided by Help at Home and Family Service; home visit programs funded by Older American’s Act in the State of Illinois | Evaluation surveys and interviews with clients, HCAs, and site directors. Functional ability of clients: 30-seconds chair stand, 30-seconds arm curl (5 pounds for females, 8 pounds for males) and chair sit and reach 4 months |
Clients significantly improved number of arm curls in 30 seconds. No significant improvement in chair stand or chair sit and reach. Most participants had a positive perception and high satisfaction with the program. HM could be safely and successfully disseminated to frail older adults |
Abbreviations: MAHC-10, Missouri Alliance for Home Care tool; LiFE, Lifestyle-integrated Functional Exercise program; FES, Falls self-Efficacy Scale; ABC, Activities specific-Balance Confidence Scale; TUG, Timed Up and GoPASE, Physical Activity Scale for the Elderly; RAS, Regional Assessment Service; HCA, home care aide; SPPB, Short Performance Physical Battery; FROP-Com, Falls Risk for Older People – Community Setting; MMSE, Mini Mental State Examination; BBS, Berg Balance Scale; BADL, Basic Activities of Daily Living; IADL, Instrumental Activities of Daily Living; HM, Healthy Moves; FES-I, Falls self-Efficacy Scale – International.
Table 5.
Intervention implementation of included non-randomized controlled trial (RCT) studies
| Reference | Implementation strategy | Intervention |
|---|---|---|
| Bamgbade and Dearmon,38 | Staff providing nursing care to patients of the privately owned home health care agency were educated on the fall prevention program | MAHC-10 fall risk assessment tool, medication review process and management plan, home safety assessment, patient- and family-specific education, individualized home-based exercise regimen |
| Burton et al,39 | LiFE program was delivered by care managers as part of a restorative home care service. Care managers explained to the client the different exercises and how these exercises could be incorporated into their daily routines, manual also provided. Clients were visited every 10–14 days by their care manager (average 3 visits) to monitor how well the client was performing the first exercises agreed to and to encourage the client to start doing others. Exercise was just one aspect of their service that was discussed during these visits | 7 balance and 6 lower limb strength exercises incorporated into everyday activities |
| Burton et al,44 | Staff completed a 4-hour training session on delivering the LiFE exercise program. Each staff member received 3 client folders, a staff folder and a LiFE trainer’s manual. Community care workers followed-up with their clients either during their usual services or on a fortnightly basis | 7 balance and 6 strength exercises to complete whilst undertaking usual daily activities |
| Gallagher et al,45 | Staff was trained in assessing risk factors and in fall prevention measures. The training sessions took place over a 6-hour period and were followed-up by performance-based competencies and case studies. Patients were evaluated with MAHC-10, scores ≥4 of 10 (indication of high risk for falls) started on the Balanced Approach rehabilitation program. The CHC falls screening and Balanced Approach rehabilitation program was designed to reduce the risk of falls in a home care population using an interdisciplinary approach | Treatment from physical and occupational therapists aims to improve gait, balance, balance confidence and reduce fall risk through individualized home exercise program designed to address impairments and home safety/mobility adaptations. The home program is in place for as long as the patient demonstrates a benefit or until safety/independence is achieved (average 8 visits, 45–60 minutes each) |
| Henwood et al,43 | HCAs attended a 1-day workshop and received a printed manual containing detailed instructions for each exercise, information on healthy lifestyle behaviors, and an overview of common barriers and enablers to exercise participation. HCAs visited clients weekly or fortnightly for 60–90 minutes with at least 10 minutes assisting and monitoring client participation in the exercise program | 5 strength exercises (chair stand, seated leg extension, standing calf raise, wall push-ups, theraband seated rows, progressing to 3 sets of 12 repetitions), 3 balance exercises (single leg stand for up to 20 seconds on each side, tight rope walk of 10 steps forward and back, 10 repetitions side to side step). Clients were encouraged to exercise on most, preferably all days |
| Kwok et al,40 | Participants chose to receive exercise training at either a day training center under supervision of a physiotherapist (groups of 6–10 participants) or individually at home assisted by a care worker. Physiotherapists provided training to all care workers and monitored their performance every 2–3 months through on-site supervision to ensure quality of the training program at home | 6 month flexibility, strength, balance, and aerobic exercise program with pain management, 1–2 sessions per week lasting approximately 60 minutes |
| Muramatsu et al,41 | HCAs received 4 hours of training on how to deliver the HM program. At the initial visit (average 27 minutes, range 10–45 minutes) HCAs assessed readiness for PA, had their clients set personally meaningful goals, and taught the 3 chair-bound movements. HCAs reminded their clients of their personal PA goal/routines as part of their regular home care and logged their HM activities. Frequency of HCA home visits depended on the client’s care needs assessed by the Illinois Determination of Needs instrument (typically 3x per week or 12 hours per week) | Each day clients completed 15 arm curls 2 times (holding a 1-pound weight supplied by the project, or a soup can or water bottle), ankle point and flex up to 30 seconds on each foot 3 times and seated step-in-place up to 1 minute |
| Park and Chodzko-Zajko,42 | HCAs attended a training session to deliver HM, this included how to teach the clients the 3 chair bound movements whilst utilizing Brief Negotiation techniques as a motivational tool. HCAs visited the client in the home and were asked to deliver the HM program on a regular basis for a 4-month time period | Each day clients completed 15–20 arm curls 2 times (holding a 1-pound weight, either soup can or water bottle), ankle point and flex working up to 30 seconds on each foot 3 times and seated step-in-place working up to 1 minute |
Abbreviations: MAHC-10, Missouri Alliance for Home Care tool; LiFE, Lifestyle-integrated Functional Exercise program; CHC, Catholic Home Care; HCA, home care aide; PA, physical activity; HM, Healthy Moves.
Burton et al39 conducted a feasibility study utilizing the LiFE program (previously described) to determine whether this intervention type could be delivered more broadly within a restorative care service. In a more recent study, Burton et al44 conducted a feasibility study that explored whether community care support workers who are non-allied health trained could deliver the LiFE exercise program to community care clients. It was determined that there were no adverse events and it was possible for this population to deliver this falls prevention exercise program.44
The home care clients in Gallagher et al’s study45 received an individualized home exercise program which was designed to address clients’ identified impairments and falls hazards in the home. This study found that the Missouri Alliance for Home Care tool (MAHC-10) and interdisciplinary program was effective in identifying and managing those who had fallen in their home.45
The 6-month intervention delivered by Kwok and Tong40 was a multicomponent exercise program, consisting of flexibility, strength, balance, and aerobic exercises, either delivered by a physiotherapist in a center or by a care worker in the home. The physiotherapy-led center-based intervention was found to improve physical function, quality of life, and fall incidence, whereas the home-based care worker led program had no effect on physical function and self-rated health.40
Muramatsu et al41 conducted a motivational enhancement and three chair-bound movements program delivered by home care aides for their clients over a 4-month intervention. Results showed a significant improvement in physical fitness, self-rated health, pain interference, Short Physical Performance Battery (SPPB) total score, SPPB balance tests, and fear of falling.41 Park and Chodzko-Zajko42 also conducted a 4-month intervention called “Healthy moves for aging well” which incorporated a physical activity intervention with a lifestyle behavior change counseling method called Brief Negotiation. The activity portion of the intervention was the same as that used by Muramatsu et al.41 Arm curl was the only functional ability outcome that reported improvement between pre- and post-testing (p=0.021).42
Henwood et al’s43 Active@Home 18-week program included weight bearing and balance exercises and was tailored to the level of the participant. The exercise program was delivered by home care support workers, with at least 10 minutes of their service time spent monitoring the exercises.43 Significant improvement was found for functional capacity as measured by the SPPB and a 19% reduction in participants classified as frail.43
Outcome measures
RCTs
There was a variety of outcome measures utilized by the included studies. The main physical test utilized by five of the RCTs was the TUG test.28–30,32,35 Unfortunately Danilovich et al30 could only provide medians and interquartile ranges rather than means and SDs for the TUG, and only the intervention phase data of Burton et al’s28 study were included to provide similarity with the other studies included which assessed the post-intervention period. Four of the RCTs28,33,37,48 used the sit-to-stand five times test and these data have been included in a meta-analysis.
Two RCTs33,34 utilized SPPB but unfortunately, after many emails, the authors were unable to obtain the data required for the Stevens-Lapsley et al34 study. Therefore, no meta-analysis could be conducted. The grip strength test30,35 and gait speed/walking tests were used in two RCTs each respectively.30,34 The data from the Stevens-Lapsley et al34 study were not available, however, Tinetti et al’s study which was included in the previous systematic review, measured walking speeds and was included in the meta-analysis.
Other studies
The SPPB test was used in two of the non-RCT studies38,43 and five of these studies also collected data on falls,38,40,41,43,45 as did Renehan et al36 in their RCT. Other physical performance measures used by single studies included functional reach, sit-to-stand one time, tandem walk (including tandem walk errors), and the six minute walk test. Health-related quality of life was measured using the SF-36, SF-12, EQ5D, AQol-8D, and the COOP/Wonka. Falls related assessments included the falls efficacy scale, activity-specific balance scale, the Falls Risk for the Older Person living in the Community and the MAHC-10 falls assessment tool.
Dropout and adherence to exercise interventions
Participant withdrawal rates ranged from 3.9%–33 23.3%,37 with an average dropout rate of 13.5% (±7.0). Adherence rates were reported in seven of the studies.28,29,37,38,41,43,44 Bamgbade and Dearmon38 stated 17% (n=5) of their participants performed the exercises as instructed over the 2 months. In Burton et al’s28,29 RCT studies, the intervention group reported completing the activities 4.9 times/week during the intervention period (8 weeks) and 4.1 times/week across the 6-month study, and the control group 4.4 times/week during the intervention (8 weeks) and 3.7 times/week across the 6 months. In the 8-week study, adherence to exercise interventions delivered by community care support workers was reported at 4.9 (±2.2) times per week.44 Henwood et al43 reported adherence of 5.1 (±0.6) sessions per week across the 18-week intervention and Saeterbakken et al37 noted 84% adherence in the 10-week intervention. Muramatsu et al41 reported half of their participants had completed 5–7 days training each week at the end of the intervention (4 months), 32% (n=16) 2–7 days/week at the end, 16% “low“ (“low“ not described) and 2% did not do any of the exercises.
Quality of the studies
In general, the quality of the ten RCT studies was rated “medium” to “high”, suggesting low risk of bias. Assessment details for potential bias in each study is presented in Table 6. The two Burton et al28,29 studies and Saeterbakkan et al's study37 did not blind their participants, assessors or those delivering the intervention (ie, care managers) and were therefore deemed to be high risk for blinding. Allocation concealment was unclear for five of the studies and some were deemed not free of bias by the reviewers due to uneven or small sample size groups. Sequence generation and incomplete outcome data appeared to be well described and were at low risk of bias for the majority of studies.
Table 6.
Randomized controlled trial (RCT) – assessment of risk of bias of RCTs
| Study | Sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective outcome reporting | Free of other bias |
|---|---|---|---|---|---|---|
| Burton et al,28 | + | + | - | + | + | ? |
| Burton et al,29 | + | + | - | + | + | ? |
| Danilovich et al,30 | + | ? | + | + | ? | - |
| Danilovich et al,31 | + | ? | + | + | ? | - |
| King et al,32 | + | ? | + | + | + | ? |
| Parsons et al,33 | ? | ? | + | + | + | - |
| Stevens-Lapsley et al,34 | + | ? | + | + | + | - |
| Tuntland et al,35 | + | + | ? | + | + | - |
| Saeterbakken et al,37 | + | + | - | - | ? | - |
| Renehan et al,36 | + | + | + | + | - | - |
Similar to the RCTs, the quality of the eight other studies was between ++ and + on the assessments, where it was deemed that most had satisfied the criteria for internal and external validity. It must be noted however, that all but one study did not have a comparison group, which meant a number of criteria were consequently not reported. Table 7 presents the assessment of quality for the non-RCT studies included in the review.
Table 7.
Randomized controlled trial (RCT) – assessment of quality of non-RCT papers
| Study | 1.1 | 1.2 | 1.3 | 2.1 | 2.2 | 2.3 | 2.4 | 2.5 | 2.6 | 2.7 | 2.8 | 2.9 | 2.10 | 3.1 | 3.2 | 3.3 | 3.4 | 3.5 | 3.6 | 4.1 | 4.2 | 4.3 | 4.4 | 4.5 | 4.6 | 5.1 | 5.2 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bamgbade and Dearmon,38 | + | NR | NR | NA | + | NA | NA | NA | NA | NA | ++ | ++ | ++ | + | ++ | + | ++ | NA | + | NA | NA | NR | NR | + | NR | - | + |
| Burton et al,44 | ++ | + | + | NA | ++ | NA | NA | NA | NA | NA | ++ | ++ | ++ | ++ | + | ++ | ++ | NA | ++ | NA | NA | NR | NR | ++ | ++ | + | ++ |
| Henwood et al,43 | ++ | + | + | NA | ++ | NA | NA | NA | NA | NA | + | ++ | + | + | + | ++ | ++ | NA | + | NA | NA | NR | NR | ++ | + | - | + |
| Kwok and Tong,40 | ++ | ++ | ++ | + | + | - | + | + | ++ | + | ++ | + | ++ | + | ++ | + | ++ | ++ | + | ++ | ++ | + | ++ | ++ | + | ++ | + |
| Muramatsu et al,41 | + | + | ++ | NA | ++ | NA | NA | NA | NA | NA | ++ | ++ | ++ | + | ++ | + | ++ | NA | + | NA | NA | NR | NR | ++ | + | + | + |
| Park and Chodzko-Zajko,42 | ++ | + | + | NA | + | NA | NA | NA | NA | NA | ++ | ++ | ++ | + | ++ | + | + | NA | ++ | NA | NA | NR | NR | ++ | + | + | + |
| Burton et al,44 | ++ | + | + | NA | ++ | NA | NA | NA | NA | NA | ++ | ++ | ++ | + | ++ | ++ | ++ | NA | ++ | NA | NA | NR | NR | ++ | NR | + | ++ |
| Gallagher et al,45 | + | + | + | NA | + | NA | NA | NA | NA | NA | NA | ++ | ++ | ++ | ++ | + | ++ | NA | + | NA | NA | ++ | ++ | ++ | ++ | + | + |
Notes: 1.1: Is the source population or source area well described?; 1.2 :Is the eligible population or area representative of the source population or area?; 1.3: Do the selected participants or areas represent the eligible population or area?; 2.1: Allocation to intervention (or comparison). How was selection bias minimized?; 2.2: Were interventions (and comparisons) well described and appropriate?; 2.3: Was the allocation concealed?; 2.4: Were participants or investigators blind to exposure and comparison?; 2.5: Was the exposure to the intervention and comparison adequate?; 2.6: Was contamination acceptably low?; 2.7: Were other interventions similar in both groups?; 2.8: Were all participants accounted for at study conclusion?; 2.9: Did the setting reflect usual UK practice?; 2.10: Did the intervention or control comparison reflect usual UK practice?; 3.1: Were outcome measures reliable?; 3.2: Were all outcome measurements complete?; 3.3: Were all important outcomes assessed?; 3.4: Were outcomes relevant?; 3.5: Were there similar follow-up times in exposure and comparison groups?; 3.6: Was follow-up time meaningful?; 4.1: Were exposure and comparison groups similar at baseline? If not, were these adjusted?; 4.2: Was intention to treat analysis conducted?; 4.3: Was the study sufficiently powered to detect an intervention effect (if one exists); 4.4: Were the estimates of effect size given or calculable?; 4.5: Were the analytical methods appropriate?; 4.6: Was the precision of intervention effects given or calculable? Were they meaningful?; 5.1: Are the study results internally valid (ie, unbiased)?; 5.2: Are the findings generalizable to the source population (ie, externally valid)?
Effectiveness of intervention programs
Results from seven of the RCTs were included in the meta-analyses.28,30,32,33,35,37,48,49 Two authors responded to data requests30,35 and their data have been included in the meta-analysis, one other author responded but did not provide their data.34
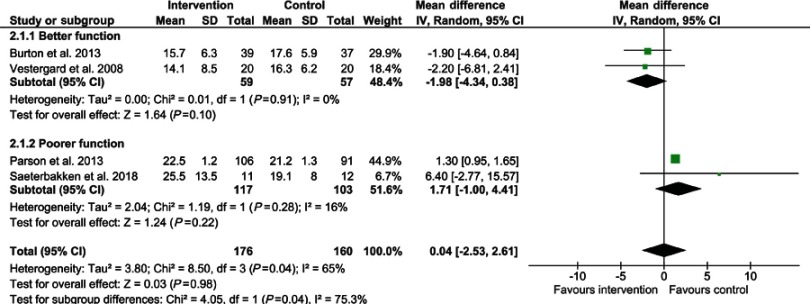
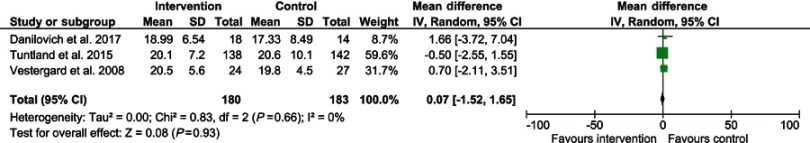
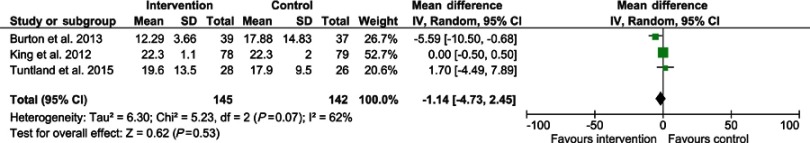
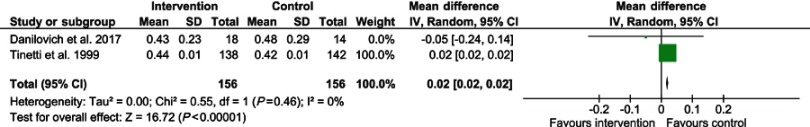
Figures 2–5 present the data in forest plots for the TUG, sit-to-stand five time, grip strength, and walking speed respectively. Heterogeneity for TUG (I2=62%) and sit-to-stand five times (I2=65%) was high. The grip strength and walking speed (meters per second) analyses had no heterogeneity (I2=0). Sit-to-stand five times was also analyzed in subgroups because there appeared to be two samples that had better function28,48 and two poorer function.33,37 The difference between those with better function and those with poorer function was significant (χ2=4.05, df=1 (p=0.04), I2=75.3%). However, heterogeneity was high and there was no significant improvement overall between the intervention and control groups for sit-to-stand five times across the four studies. Walking speed was the only test which reported an overall significant (MD: 0.02, p<0.001) difference. In this case, it favored the usual care (ie, control) group in Tinetti et al's49 study. TUG, sit-to-stand five times, and grip strength showed no statistically significant difference between the groups for these tests.
Figure 3.
Sit-to-stand five times.
Figure 4.
Grip strength.
Figure 2.
Timed Up and Go.
Figure 5.
Walking speed.
Discussion
This systematic review identified a further 18 studies, since the previous systematic review was published,22 which examined the effectiveness of physical activity/exercise interventions for older adults receiving home care services. Previously there were no studies included from Australia, however, in the last 6 years, six studies have been conducted, providing evidence for Australian home care agencies and national and state governments who fund these services. Disappointingly, we found no published studies from a number of large countries who provide home care services to older adults such as the United Kingdom, European countries (ie, the Netherlands, Ireland, Germany), and Scandinavia (other than Norway), and no studies from low to middle income countries.
Lack of consistency in methodology and measures has limited the potential to conduct meaningful meta-analyses in this area. Of the four outcomes that were analyzed by meta-analysis, only walking speed changed significantly between the intervention and control groups. On this occasion, the control group demonstrated faster walking speeds than the intervention group. This was predominantly due to Tinetti et al’s49 study, which reported a faster walking speed (m/s) for the usual care group at 6 months than the intervention group. However, walking speeds were found to be the same for each group at 12 months, which was 6 months post-intervention.49 Tinetti et al49 did note that the intervention group was significantly more likely to be using a walking stick than the control group at the end of the 6-month intervention. The intervention group also had more visits from home health aides, which perhaps meant they did not do as much physically in their daily activities.49 This may have contributed to the intervention group improving at a slower rate than the usual care group that received fewer visits from their aides and needed to do more of their own chores such as cleaning and cooking.49
The other three measures tested in the meta-analysis (TUG, sit-to-stand five times, and grip strength), showed no significant difference between the groups overall. For the TUG meta-analysis only three studies were included, two with small sample sizes (ie, under 100) and one with a total sample size of 157; heterogeneity was high and there was little difference between the intervention and control groups at post-testing, except for Burton et al,28 whose study appeared to have greater emphasis on the exercise intervention. Similar results were found for the sit-to-stand five times test where Burton et al28 and Vestergard et al48 both reported significant improvements, compared to the other two studies,33,37 and showed a significant difference in the subgroup meta-analysis. Parson et al33 also had a considerably larger sample than the other three studies, which meant greater weighting of their results within the overall meta-analysis, similar to the TUG. This also occurred for walking speed where Tinetti et al49 reported the control group experiencing significant improvements compared to the intervention group, and their total sample size was 280 compared to Danilovich et al,30 with 32 participants. It must be noted however, that individual RCTs reported significant improvement and six of the eight non-RCT studies also reported significant improvements in physical function tests between pre- and post-testing.39–43,45 This gives a positive indication of an effect and indicates that additional, high quality RCTs with larger samples sizes are required to determine the true effect of the interventions.
Five of the eight RCT studies30,32,33,35,48 did not report on adherence to the exercise program section of their intervention. Previous research of older adults receiving home care services has reported this population often does not enjoy structured exercise.50 They also reported feeling too old to exercise or being in too much pain as the major reasons for not wanting to be active or exercise.21,50 The research is well established for exercise/physical activity improving function and disability,9,16 yet a vulnerable group, such as those receiving home care services, may not understand its importance and may not have participated in the exercises as often as recommended. Future research looking at physical activity/exercise with this population should report adherence in order to determine whether the intervention needs improving (ie, increased loads) or whether adherence was inadequate. It is also recommended that where possible, RCTs include a comprehensive process evaluation to improve understanding of factors influencing outcomes positively or negatively, particularly for exercise interventions.
Also of note, was that only four of the studies37,40,42,43 appeared to be specifically about delivering an exercise intervention. The other 14 studies included other intervention strategies as well as exercise, such as education, home safety assessments, medication reviews, and home help. Including a number of strategies within an intervention may mean the focus on exercise or physical activity is reduced and therefore the clients’ functional ability, strength, balance or mobility does not improve as much as anticipated. It may therefore be more beneficial to ensure older people receiving home care services are not being recommended too many interventions at one time. Having an emphasis on selecting one or a small number of targeted interventions initially (with one of these being exercise), and doing this using a collaborative, person-centered approach with the older person may show more positive outcomes.51
The interventions were also delivered by people with a variety of levels of formal training, ranging from allied health staff (ie, physiotherapists, occupational therapists, and registered nurses) delivering the whole intervention, health professionals mentoring non-health professionals, and those without formal tertiary qualifications, such as home care workers or aides assessing and delivering participants independently. Health professionals delivering physical activity interventions has substantial cost implications compared to non-health trained professionals, which may be a reason why some studies have more recently attempted to train and utilize home care staff instead. Further RCTs are required to show whether non-allied health trained home care staff can effectively deliver physical activity interventions to improve physical function for their clients. This also raises the need for economic evaluations to be undertaken with these types of programs that have been shown to be effective, because it may also mean a reduction in the costs of home care. If this occurred it may be viewed as an investment rather than a cost to society.
Strengths and limitations
The strength of the review is that a systematic methodology was implemented to identify studies relevant to the area, that the quality of the RCTs within the review was assessed, and several meta-analyses were able to be conducted in this updated review. There are however some limitations. Although a number of large databases were searched, there is always the possibility that relevant papers may not have been included. Because the search only included peer-reviewed publications, there is always the chance that publication bias may have occurred because of unpublished and grey literature, or organizational reports being excluded. Language bias may also have resulted because only studies published in English were accepted.
Conclusion
This systematic review updated the evidence on the effectiveness of physical activity programs for older people receiving home care services. Although limited research is available, as evident from this review, there is absolutely none from the low middle income country context where nearly 70% of the world’s old reside. Many of the studies reported significant improvements for the intervention group, particularly the single-group pre-, post-test studies. However, there is little evidence within the meta-analyses that current exercise trials are effective and none of the included studies conducted an economic evaluation, which should be considered in future studies. Greater emphasis is needed on delivering exercise as a single intervention rather than as part of a multi-factorial intervention for this population. Conducting a comprehensive process evaluation that includes adherence to the exercise intervention and how it is associated with its effectiveness is essential and recommended for future studies.
Acknowledgment
This project was funded by the Western Australian Department of Health Merit Award.
Disclosure
Dr Elissa Burton reports grants from Western Australian Department of Health Merit Award, during the conduct of the study. This grant was provided to assist with completing the paper (researcher time and paying for the open access). The authors report no other conflicts of interest in this work.
References
- 1.United Nations. World population prospects: the 2017 revision, key findings and advance tables. Working Paper No. ESA/P/WP/248. New York, NY: Department of Economic and Social Affairs, Population Division - United Nations; 2017. [Google Scholar]
- 2.Productivity Commission. Introducing Competition and Informed User Choice into Human Services: Reforms to Human Services, Draft Report. Canberra: Productivity Commission; 2017. [Google Scholar]
- 3.Australian Government Department of Health and Ageing. Home and Community Care Program Minimum Data Set 2009–2010 Annual Bulletin. Canberra: Australian Government Department of Health and Ageing; 2009. [Google Scholar]
- 4.Australian Government Department of Social Services. Home and Community Care Program Minimum Data Set 2013–14 Annual Bulletin. Canberra, ACT: Australian Government Department of Social Services; 2014. [Google Scholar]
- 5.Gilmour H. Health Reports: Formal Home Care Use in Canada. Ottawa, Canada: Statistics Canada; 2018. [Google Scholar]
- 6.Health Service Executive. National Service Plan 2018. Dublin, Ireland: Health Service Executive; 2017. [Google Scholar]
- 7.Cochrane A, Furlong M, McGilloway S, Molloy D, Stevenson M, Donnelly M. Time-limited home-care reablement services for maintaining and improving the functional independence of older adults. Cochrane Database Syst Rev 2016. 2016;(10). Art. No.: CD010825. doi: 10.1002/14651858.CD010825.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kingston A, Collerton J, Davies K, Bond J, Robinson L, Jagger C. Losing the ability in activities of daily living in the oldest old: a hierarchic disability scale from the Newcastle 85+ Study. PLoSOne. 2012;7(2):e31665. doi: 10.1371/journal.pone.0031665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Issue 3. Art No.: CD002759. Cochrane Database Syst Rev. 2009;(3). Art. No.: CD002759. doi: 10.1002/14651858.CD002759.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burton E, Farrier K, Lewin G, et al. Motivators and barriers for older people participating in resistance training: a systematic review. J Aging Phys Act. 2017;25:311–324. doi: 10.1123/japa.2015-0289 [DOI] [PubMed] [Google Scholar]
- 11.Burton E, Lewin G, Boldy D. Barriers and motivators to being physically active for older home care clients. Phys Occup Ther Geriatr. 2013;31(1):21–36. doi: 10.3109/02703181.2012.751474 [DOI] [Google Scholar]
- 12.Canadian Society for Exercise Physiology. Canadian physical activity guidelines: for older adults - 65 years & older; 2012. Availble from: http://www.csep.ca/CMFiles/Guidelines/CSEP_PAGuidelines_older-adults_en.pdf. Accessed March26, 2013.
- 13.Sims J, Hill K, Hunt S, Haralambous B. Physical activity recommendations for older Australians. Australasian J Ageing. 2010;29(2):81–87. doi: 10.1111/j.1741-6612.2009.00388.x [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed. Washington, DC: Department of Health and Human Services; 2018. [Google Scholar]
- 15.World Health Organisation. Global recommendations on physical activity for health 65 years and above; 2011. Available from: http://www.who.int/dietphysicalactivity/physical-activity-recommendations-65years.pdf. Accessed July26, 2017.
- 16.Liu C, Latham N. Can progressive resistance strength training reduce physical disability in older adults? A meta-analysis. Disabil Rehabil. 2011;33(2):87–97. doi: 10.3109/09638288.2010.487145 [DOI] [PubMed] [Google Scholar]
- 17.Taylor A, Cable N, Faulkner G, Hillsdon M, Narici M, Van Der Bij A. Physical activity and older adults: a review of health benefits and the effectiveness of interventions. J Sports Sci. 2004;22(8):703–725. doi: 10.1080/02640410410001712421 [DOI] [PubMed] [Google Scholar]
- 18.Warburton D, Nicol C, Bredin S. Health benefits of physical activity: the evidence. Can Med Assoc J. 2006;174(6):801–809. doi: 10.1503/cmaj.051351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database of Syst Rev. 2012;(9). Art. No.: CD007146. doi: 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milton K, Ramirez Varela A, Strain T, Cavill N, Foster C, Mutrie N. A review of global surveillance on the muscle strengthening and balance elements of physical activity recommendations. J Frailty Sarcopenia Falls. 2018;3(2):114–124. doi: 10.22540/JFSF-03-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burton E, Lewin G, Pettigrew S, et al. Identifying motivators and barriers to older community-dwelling people participating in resistance training: a cross-sectional study. J Sports Sci. 2017;35(15):1523–1532. doi: 10.1080/02640414.2016.1223334 [DOI] [PubMed] [Google Scholar]
- 22.Burton E, Lewin G, Boldy D. A systematic review of physical activity programs for older people receiving home care services. J Aging Phys Act. 2015;23(3):460–470. doi: 10.1123/japa.2014-0086 [DOI] [PubMed] [Google Scholar]
- 23.Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins J, Altman D, Gøtzsche P, et al. The Cochrane Collaboration‘s tool for assessing risk of bias in randomised trials. Br Med J. 2011;343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Institute for Health and Care Excellence. Methods for the Development of NICE Public Health Guidance. Third ed. London: NICE; 2012. Available from: https://www.nice.org.uk/process/pmg4/chapter/appendix-f-quality-appraisal-checklist-quantitative-intervention-studies. Accessed October18, 2018. [PubMed] [Google Scholar]
- 26.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. [Updated March 2011]. The Cochrane Collaboration; 2011. Available from: www.cochrane-handbook.org. [Google Scholar]
- 27.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. [DOI] [PubMed] [Google Scholar]
- 28.Burton E, Lewin G, Clemson L, Boldy D. Effectiveness of a lifestyle exercise program for older people receiving a restorative home care service: a pragmatic randomized controlled trial. Clin Interv Aging. 2013;8:1591–1601. doi: 10.2147/CIA.S44614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burton E, Lewin G, Clemson L, Boldy D. Long term benefits of a lifestyle exercise program for older people receiving a restorative home care service: a pragmatic randomized controlled trial. Healthy Aging Clin Care Elderly. 2014;6:1–9. doi: 10.4137/HACCE.S13445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Danilovich M, Eisenstein A, Marquez D, Corcos D, Hughes S. The impact of strong for life on the physical functioning and health of older adults receiving home and community-based services. Aging Soc. 2017;7(2):1–10. doi: 10.18848/2160-1909/CGP/v07i02/1-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Danilovich M, Hughes S, Corcos D, Marquez D, Eisenstein A. Translating strong for life into the community care program: lessons learned. J Appl Gerontol. 2017;36(5):553–569. doi: 10.1177/0733464815625833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.King A, Parsons M, Robinson E, Jorgensen D. Assessing the impact of a restorative home care service in New Zealand: a cluster randomised controlled trial. Health Social Care Community. 2012;20(4):36–374. doi: 10.1111/j.1365-2524.2011.01039.x [DOI] [PubMed] [Google Scholar]
- 33.Parsons J, Sheridan N, Rouse P, Robinson E, Connolly M. Randomized controlled trial to determine the effect of a model of restorative home care on physical function and social support among older people. Archives Phys Med Rehabiliation. 2013;94:1015–1022. doi: 10.1016/j.apmr.2013.02.003 [DOI] [PubMed] [Google Scholar]
- 34.Stevens-Lapsley J, Loyd B, Falvey J, et al. Progressive multi-component home-based physical therapy for deconditioned older adults following acute hospitalization: a pilot randomized controlled trial. Clin Rehabil. 2016;30(8):776–785. doi: 10.1177/0269215515603219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tuntland H, Aaslund M, Espehaug B, Førland O, Kjeken I. Reablement in community-dwelling older adults: a randomised controlled trial. BMC Geriatr. 2015;15:145. doi: 10.1186/s12877-015-0142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Renehan E, Meyer C, Elliott R, et al. Post-hospital falls prevention intervention: a mixed-methods study. J Aging Phys Act. 2019;27(2):155–165. doi:10.1123/japa.2017-0406 [DOI] [PubMed] [Google Scholar]
- 37.Saeterbakken A, Bardstu H, Brudeseth A, Andersen V. Effects of strength training on muscle properties, physical function, and physical activity among frail older people: a pilot study. J Aging Res. 2018;2018:8916274. doi: 10.1155/2018/8916274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bamgbade S, Dearmon V. Fall prevention for older adults receiving home healthcare. Home Healthcare Now. 2016;34(2):68–75. doi: 10.1097/NHH.0000000000000333 [DOI] [PubMed] [Google Scholar]
- 39.Burton E, Lewin G, Clemson L, Boldy D. Determining the feasibility of a lifestyle activity program for inclusion in a restorative home care service: a pilot study. Act Adapt Aging. 2014;38(2):79–93. [Google Scholar]
- 40.Kwok T, Tong C. Effects on centre-based training and home-based training on physical function, quality of life and fall incidence in community dwelling older adults. Physiother Theory Pract. 2014;30(4):243–248. doi: 10.3109/09593985.2013.867387 [DOI] [PubMed] [Google Scholar]
- 41.Muramatsu N, Yin L, Berbaum M, et al. Promoting seniors’ health with home care aides: a pilot The Gerontologist 2018;58(4): 779–788. doi: 10.1093/geront/gnx101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park C-H, Chodzko-Zajko W. Feasibility of integrating the “Healthy moves for aging well” program into home care aide services for frail older adults. J Exercise Rehabil. 2014;10(3):191–197. doi: 10.12965/jer.140116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Henwood T, Hetherington S, Purss M, Rouse K, Morrow J, Smith M. Active@Home: investigating the value of a home care worker-led exercise program for older adults with complex care needs. J Aging Phys Act. 2019;27(2):284–289. doi: 10.1123/japa.2017-0443 [DOI] [PubMed] [Google Scholar]
- 44.Burton E, Lewin G, O’Connell H, Petrich M, Boyle E, Hill K. Can community care workers deliver a falls prevention exercise program? A feasibility study. Clin Interv Aging. 2018;13:485–495. doi: 10.2147/CIA.S162728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gallagher R, Stith N, Southard V. Evaluation of the missouri alliance for home care fall risk assessment tool and home-based “Balanced approach” fall reduction initiative. Home Health Care Manag Pract. 2013;25(5):224–228. doi: 10.1177/1084822313487203 [DOI] [Google Scholar]
- 46.Clemson L, Munro J, Fiatarone Singh M. Lifestyle-Integrated Functional Exercise (Life) Program to Prevent Falls: Trainers Manual. Sydney, NSW: Sydney University Press; 2014. [Google Scholar]
- 47.Clemson L, Singh M, Bundy A, et al. LiFE pilot study: a randomised trial of balance and strength training embedded in daily life activity to reduce falls in older adults. Aust Occup Ther J. 2010;57:42–50. doi: 10.1111/j.1440-1630.2009.00848.x [DOI] [PubMed] [Google Scholar]
- 48.Verstergaard S, Kronborg C, Puggaard L. Home-based video exercise intervention for community-dwelling frail older women: a randomized controlled trial. Aging Clin Exp Res. 2008;20:479–486. [DOI] [PubMed] [Google Scholar]
- 49.Tinetti M, Baker D, Gottschalk M, et al. Home-based multicomponent rehabilitation program for older persons after hip fracture: a randomized trial. Arch Phys Med Rehabil. 1999;80:916–922. [DOI] [PubMed] [Google Scholar]
- 50.Burton E, Lewin G, Boldy D. Physical activity preferences of older home care clients. Int J Older People Nurs. 2014;10:170–178. doi: 10.1111/opn.12065 [DOI] [PubMed] [Google Scholar]
- 51.Meyer C, Dow B, Hill K, Tinney J, Hill S. “The right way at the right time”: insights on the uptake of falls prevention strategies from people with Dementia and their caregivers. Front Public Health. 2016;4:1–10. doi: 10.3389/fpubh.2016.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]