Abstract
Carcinoma cells that undergo an epithelial-mesenchymal transition (EMT) and display a predominantly mesenchymal phenotype (hereafter EMT tumor cells) are associated with immune exclusion and immune deviation in the tumor microenvironment (TME). A large body of evidence has shown that EMT tumor cells and immune cells can reciprocally influence each other, with EMT cells promoting immune exclusion and deviation and immune cells promoting, under certain circumstances, the induction of EMT in tumor cells. This cross-talk between EMT tumor cells and immune cells can occur both between EMT tumor cells and cells of either the native or adaptive immune system. In this article, we review this evidence and the functional consequences of it. We also discuss some recent evidence showing that tumor cells and cells of the immune system respond to similar stimuli, activate the expression of partially overlapping gene sets, and acquire, at least in part, identical functionalities such as migration and invasion. The possible significance of these symmetrical changes in the cross-talk between EMT tumor cells and immune cells is addressed. Eventually, we also discuss possible therapeutic opportunities that may derive from disrupting this cross-talk.
Keywords: EMT, immune exclusion, immune deviation, cross-talk, cytokines, chemokines, exosomes
1. Introduction
The tumor microenvironment (TME) comprises, in addition to tumor cells, several accessory cell types that contribute to tumor growth and progression. Such contribution is in many cases the result of cross-talk between tumor cells and accessory cells [1]. Angiogenic vascular cells, infiltrating immune cells, and cancer-associated fibroblasts are some of the accessory cells in the TME [1]. Infiltrating immune cells comprise cells of both the native as well as the adaptive immune system. Tumor-associated macrophages (TAMs), subsets of granulocytes, myeloid-derived suppressor cells (MDSCs), dendritic cells (DCs), natural killer (NK) cells, and mast cells are examples of accessory cells of the native immune system, while different T lymphocyte subpopulations, such as CD4+ T cells, CD8+ T cells, regulatory T cells (Tregs), and B lymphocytes, are examples of cells of the adaptive immune system that can infiltrate the TME.
Tumor cells themselves are not a rigorously homogeneous cell population. In fact, they are endowed with considerable plasticity, allowing them to express different functions and phenotypic markers. An epithelial-mesenchymal transition (EMT) is the main process underlying the heterogeneity of carcinoma cells. Tumor cells undergoing EMT lose properties of epithelial cells, such as the apical–basal axis of polarity and cell–cell adhesion, and acquire properties of mesenchymal cells, such as loose three-dimensional organization and increased motility [2]. EMT, however, is not an all-or-nothing event with tumor cells losing all epithelial markers and acquiring an entirely mesenchymal phenotype. Rather, tumor cells can display hybrid phenotypic and functional states reflecting intermediate tumor cell subpopulations between fully epithelial and fully mesenchymal cells [3].
Tumor cell EMT can occur in different conditions. First, it can occur in response to stressors from the TME, such as hypoxia, a low pH, immune responses, mechanical stress, and antitumor drugs. These responses are largely mediated by growth factors and cytokines such as transforming growth factor (TGF)-β [4]. Second, stressor-promoted epigenetic changes that induce heritable effects allow for retention of the mesenchymal state even when the stressors are no longer present [5]. Third, signaling pathways are activated independently of a stimulus due to the activation of oncogenic mutations or tumor-associated overexpression of pathway components [6]. From a functional point of view, tumor cells undergoing EMT are characterized by increased invasiveness and metastasis formation, resistance to apoptosis and antitumor drugs, and the acquisition of tumor-initiating potential [7].
EMT induced by extracellular stimuli is the result of cross-talk between tumor cells and accessory cells from the TME, including cells from the immune system [4]. EMT, however, can by itself induce phenotypic and functional changes in accessory cells of the TME, including cells of the innate and adaptive immune systems. In the following, we discuss the modalities of the cross-talk between tumor cells and cells of the immune system with regard to the induction of EMT by immune cells and EMT-driven changes in cells of the immune system.
2. The Cross-Talk between EMT Tumor Cells and Cells of the Immune System
The cross-talk between EMT tumor cells and cells of the immune system favors, by and large, the induction of EMT in tumor cells by immune cells and the inhibition of antitumor immune responses by tumor cells that have acquired mesenchymal traits as a consequence of an EMT (hereafter referred to as EMT tumor cells). While this is a general rule, there are exceptions, which will be discussed in the following. Before addressing in detail the main aspects that characterize this cross-talk, we will first discuss the evidence suggesting that the cross-talk between EMT tumor cells and the immune system is relevant in the human setting and of functional significance to overall tumor progression and patient prognosis. This is not a trivial issue, since, for example, it has been questioned over the years whether EMT actually occurs in the human setting and if it is of any pathophysiological significance [8].
2.1. Association of EMT and an Immunosuppressive TME in Patients
There is now considerable evidence, derived mainly from immunohistochemical and gene expression studies, suggesting that tumors enriched in EMT markers are associated with an immunosuppressive TME and a negative prognosis. In the following, we provide some examples of these studies.
Gene expression clustering studies in ovarian cancer have shown that the mesenchymal subtype, enriched in an EMT-related gene signature, has a worse prognosis and survival compared to other subtypes [9]. In this mesenchymal subtype, a decreased number of CD8+ tumor-infiltrating lymphocytes (TILs) were detected, suggesting an association between EMT tumor cells and exclusion of these immune cells from the TME. Similarly, in a study conducted in non-small cell lung cancer (NSCLC), EMT markers were associated with reduced tumor infiltration of CD4+ and CD8+ T cells, increased expression of immunosuppressive cytokines such as interleukin (IL)-10 and TGF-β, as well as overexpression of inhibitory immune checkpoint molecules such as cytotoxic T-lymphocyte antigen (CTLA)-4 and T-cell immunoglobulin and mucin domain-containing (TIM)-3 [10].
In an immunohistochemistry study performed in patients with gastric cancer, a high expression of EMT traits, the infiltration of TAMs, and the expression of TGF-β1 were associated with a negative prognosis [11]. In a study of lung adenocarcinoma [12], EMT markers were associated with enhanced tumor infiltration of CD4+Foxp3+ Tregs and upregulation of inhibitory immune checkpoint molecules such as programmed cell death (PD)-ligand (L) 1, PD-L2, TIM-3, B7-H3, and CTLA-4. B7-H3 was identified as a negative prognostic marker for NSCLC. Similarly, a genomic and proteomic analysis based on a tumor cell EMT signature conducted across almost 2000 different tumors [13] revealed a strong association between EMT and markers of inhibited or exhausted immune responses. Thus, a high expression of inhibitory immune checkpoint molecules such as PD-1, PD-L1, CTLA-4, OX40L, and PD-L2 was observed in tumors with the most mesenchymal EMT scores. An association between EMT tumor cells (mesenchymal and hybrid epithelial-mesenchymal phenotypes) and increased numbers of infiltrating PD-1+ cells was also observed in another study in patients with adenocarcinoma of the lung [14]. A very strong association was found between PD-L1 expression and the claudin-low subset of breast cancer, which is characterized by a high EMT score [15].
Overall, these studies allowed for the identification of two different scenarios: first, an association between EMT and a reduced infiltration of immune cells (i.e., a predominantly immune-excluded TME); and second, an association between EMT and the infiltration of suppressive or exhausted immune cells (i.e., a predominantly immune-deviated TME). In both cases, however, the conclusions are similar: EMT markers associate with a TME that has inhibitory effects (through immune exclusion or deviation) on antitumor immune responses.
2.2. EMT-Associated Changes in the Immunological Profile of Tumor Cells
EMT tumor cells undergo phenotypic alterations that have significant consequences for the recognition by cells of the native and adaptive immune systems. Both down- and upregulation of cell surface molecules of immunological significance have been described. In general, these changes are accompanied by immune resistance and evasion, but there are exceptions to this rule.
The first class of phenotypic alterations consists of the regulation of factors directly or indirectly involved in immune recognition. Thus, EMT-like alterations in melanoma cells have been reported to reduce the expression of multiple tumor antigens, with a consequent escape from being killed by T cells specific for these antigens [16]. However, when targeting antigens whose expression was unaltered during EMT, the capacity of T cells to kill melanoma cell lines in vitro was unaltered [17]. Similarly, T cell-driven immunoediting of breast tumors in neu-transgenic mice led to the emergence of antigen-loss variants that had undergone an EMT [18]. Reduced antigen presentation may depend on the downregulation of components of the antigen processing machinery. Thus, EMT NSCLC cells showed a significantly reduced expression of immunoproteasome components and their regulators [19]. The immunoproteasome generates antigenic peptides that bind to human leukocyte antigen (HLA)-I molecules for recognition by CD8+ T cells. Consequently, reduced expression of the immunoproteasome leads to reduced presentation of antigenic peptides. EMT-associated downregulation of molecules involved in the presentation of antigenic peptides can also lead to tumor cells hiding from immune recognition. This has been shown for HLA-I molecules, which were downregulated in epithelial cell lines of different tumors as a result of EMT [20,21], with a consequent reduction in antigen presentation and recognition by CD8+ cytotoxic T lymphocytes (CTLs) [20].
Upregulation in tumor cells of inhibitory immune checkpoint molecules of native and adaptive immunity can also occur in tumor cells in response to EMT. These molecules inhibit the onset or the continuation of ongoing antitumor immune responses. EMT has been associated with the upregulation of several inhibitory immune checkpoint molecules, such as PD-L1 [22,23], TIM-3 [24], B7-H3 [25], B7-H1 [26], or CD47 [27]. Upregulation of PD-L1 induced resistance to CTL-mediated killing [28]. Interestingly, some of these immune checkpoint molecules have been shown to act by themselves as EMT inducers and promote the acquisition of tumor-initiating potential [15,20,25,26,29], thereby contributing to the amplification of the EMT process and its associated functionalities [30].
Another broad class of EMT-associated tumor cell alterations consists of the acquisition of resistance to killing by cytotoxic effector cells independently of antigen display on the tumor cell surface. This has been shown for tumor cells overexpressing the EMT transcription factor (TF) brachyury and the consequent upregulation of the transmembrane glycoprotein mucin-1 (MUC-1). Overexpression of MUC-1 led to reduced susceptibility to killing by tumor necrosis-related apoptosis-inducing ligand (TRAIL) and to CTL lysis [31]. Brachyury has also been shown to reduce the susceptibility of tumor cells to cytotoxic lymphocytes (CD8+ T lymphocytes and NK cells) due to inefficient caspase-dependent apoptosis, but in the presence of normal levels of HLA-I molecules, antigenic peptides, or the various components of the antigen presentation machinery [32]. In fact, increased resistance to apoptosis is recognized as a hallmark of EMT [2]. Mechanisms other than resistance to apoptosis appear to operate in some other situations. Thus, it has recently been reported that hypoxia-exposed lung adenocarcinoma subclones with a predominant mesenchymal phenotype displayed resistance toward CTLs and NK cells through a mechanism involving defective immune synapse signaling [33]. In human breast adenocarcinoma cells, reduced susceptibility to CTL-mediated lysis depended on upregulation of the stem cell marker Kruppel-like factor-4 (KLF-4) and miR-7 downregulation [34]. Hypoxia-inducible miR-210 inhibited the susceptibility of lung carcinoma and melanoma cells to lysis by CTLs [35]. An interesting study has reported that acquisition of an EMT phenotype by breast cancer cells was associated with morphologic changes, actin cytoskeleton remodeling, and increased resistance to CTL-mediated lysis [36]. Resistant cells exhibited attenuation in the formation of an immunologic synapse with CTLs along with induction of autophagy. Autophagy appeared to be critical to resistance to CTL-mediated lysis because silencing of beclin1 to inhibit autophagy restored susceptibility to CTL-induced lysis. Thus, this article introduces autophagy as another player in EMT-associated resistance to immune effector mechanisms. EMT and autophagy are, in many instances, mutually exclusive mechanisms of tumor cell resistance, but in addition to the present article, other examples of coexistence or sequential acquisition of markers of EMT and autophagy have been described (discussed in Reference [37]).
While the EMT-associated changes of the immunological profile of tumor cells that have been discussed so far lead to the inhibition of antitumor immune responses, there are some significant exceptions. Thus, colon cancer cells undergoing EMT have been shown to undergo upregulation of ligands activating NK cells, as well as downregulation of HLA-I molecules [20,38]. These changes led to reduced recognition of the tumor cells by CD8+ CTLs and enhanced recognition by NK cells. Expression of the NK cell ligands, however, was very low in vivo in advanced tumors with invasive properties, and, concomitantly, enhanced infiltration of NK cells was observed [20]. These results suggested that NK cells had eliminated NK cell ligand-expressing tumor cells and had selected variants that were not recognized by NK cells.
Recent results have shown that EMT can directly increase tumor cell susceptibility to NK cells, thereby contributing, at least in part, to the inefficiency of the metastatic process [39]. The depletion of NK cells allowed spontaneous metastasis without affecting primary tumor growth. EMT-induced modulation of E-cadherin and cell adhesion molecule 1 (CADM1) mediated increased susceptibility to NK cytotoxicity. These results are of considerable interest because, contrary to most results published on this issue, they showed that tumor cell EMT could exert antimetastatic effects through enhanced susceptibility to NK cells. At odds with these results, a recent study showed that EMT-like changes in melanoma cells were induced by NK cells and were dependent on the engagement of the activating NK receptors NKp30 or NKG2D and the release of cytokines [40]. Moreover, an EMT-associated upregulation of HLA-I molecules was observed. This favored an escape from NK cell attack given the protective role of HLA-I molecules toward NK cell cytotoxicity and because of the contemporary downregulation of tumor-recognizing activating receptors on NK cells. On the other hand, upregulation of HLA-I molecules was expected to enhance CTL-mediated cytotoxicity toward tumor cells. How these results can be reconciled with the previous ones remains to be established, but may depend, among other things, on the timing of the tumor progression at which the experiments were performed [20]. Table 1 summarizes the findings that have demonstrated EMT-associated changes in the immunological profile of tumor cells.
Table 1.
Epithelial-mesenchymal transition (EMT)-associated changes in the immunological profile of tumor cells.
| Type of Alteration | Consequences | References |
|---|---|---|
| Reduced Expression of Tumor Antigens | ||
| Reduced expression of tumor antigens in melanoma cells | Escape from antigen-specific killing by CTLs | [16] |
| Emergence of antigen-loss variants in EMT tumor cells from neu-transgenic mice | Escape from antigen-specific killing by CTLs | [18] |
| Reduced Expression of Antigen-Presenting Molecules | ||
| Downregulation of HLA class I molecules | Reduced antigen presentation and escape from antigen-specific killing by CTLs. | [20,21] |
| Enhanced Expression of Inhibitory Immune Checkpoint Molecules | ||
| Upregulation of PD-L1, TIM-3, B7-H1, B7-H3, CD47 | Downregulation of antitumor immune responses, resistance to killing by CTLs, amplification of tumor cell EMT | [15,20,22,23,24,25,26,27,28,29,30] |
| Enhanced Resistance of EMT Tumor Cells to Killing by T Cells | ||
| Overexpression of MUC-1 | Reduced susceptibility to killing by TRAIL and CTLs | [31] |
| Expression of the EMT TF brachyury, leading to inefficient apoptosis, with normal levels of HLA class I, antigenic peptides, and components of antigen presentation machinery | Reduced susceptibility to killing by CTLs and NK cells | [32] |
| EMT tumor cells showing defective immune synapse signaling | Resistance to killing by CTLs and NK cells | [33] |
| Upregulation of KLF-4 and downregulation of miR-7 | Reduced susceptibility to killing by CTLs | [34] |
| Expression of hypoxia-inducible miR-210 | Reduced susceptibility to killing by CTLs | [35] |
| Actin cytoskeleton remodeling, autophagy, and attenuation of an immunological synapse | Autophagy-dependent reduced susceptibility to killing by CTLs | [36] |
| Downregulation of HL -I and upregulation of ligands activating NK cells | Reduced recognition by CTLs and enhanced recognition by NK cells | [20,38] |
| Modulation of E-cadherin and CADM1 | Increased susceptibility to killing by NK cells and reduced metastasis formation | [39] |
| EMT-like changes in melanoma cells accompanied by upregulation of HLA class I and downregulation of activating receptors on NK cells | Escape from killing by NK cells | [40] |
Abbreviations: CADM, cell adhesion molecule; CTL, cytotoxic T lymphocyte; EMT, epithelial-mesenchymal transition; HLA, human leukocyte antigen; KLF, Kruppel-like factor; MUC, mucin; NK, natural killer; PD-L, programmed cell death ligand; TF, transcription factor; TIM, T-cell immunoglobulin and mucin domain-containing.
2.3. EMT-Induced Effects on Cells of the Immune System
So far, we have discussed the consequences of EMT-associated alterations to the immunological recognition of tumor cells. An EMT in tumor cells, however, can also have direct effects on cells of the immune system. These effects can be twofold. The first is immune exclusion, i.e., reduced tumor infiltration of immune cells that mediate effective antitumor immune responses. The second is immune deviation, i.e., deviation from an effective antitumor immune response (suppressed and/or inefficient) without necessarily being accompanied by reduced tumor infiltration of cells of the immune system. The different effects can be present at the same time, albeit at varying degrees, with one predominating over the other. Of note, many EMT-induced effects on cells of the immune system are similar to those observed upon activation in tumor cells of oncogenic pathways that are also involved in the induction of EMT [41]. It appears obvious that these two events, i.e., the induction of EMT and immunosuppressive effects in the TME, are intimately linked in a causal relationship through the activation of oncogenic and EMT-promoting pathways in tumor cells.
With regard to immune exclusion, we have already discussed studies showing that EMT is associated with immune exclusion in human cancers [10,12]. A more direct demonstration has been brought in experimental systems showing that EMT tumor cells cause reduced infiltration of immune cells into the TME [22]. On the other hand, a large number of studies have shown that EMT tumor cells can induce enhanced tumor infiltration of deviated immune cells, such as polymorphonuclear MDSCs [42], myeloid cells [43], mast cells [44,45], or natural CD4+CD25− Tregs [46]. Pancreatic cancer cells resistant to anti-vascular endothelial growth factor (VEGF) treatment secreted increased levels of proinflammatory factors, which stimulated the recruitment of CD11b+ proangiogenic myeloid cells and acted also in an autocrine manner to induce and amplify tumor cell EMT [47]. In other situations, both the exclusion of effector CD8+ T lymphocytes and enhanced infiltration of immunosuppressive MDSCs have been demonstrated [48]. Immune deviation through EMT-mediated induction of an immunosuppressive phenotype has been reported for the M2 polarization of macrophages by bladder cancer cell lines [49] and the induction of the immunosuppressive molecule indoleamine 2,3-dioxygenase (IDO) in monocyte-derived macrophages. These IDO-expressing macrophages suppressed T cell proliferation and promoted the expansion of immunosuppressive Tregs [50]. Similarly, mesenchymal-like breast cancer cells were shown to induce activation of macrophages to acquire phenotype and functionalities of immunosuppressive TAMs [51]. EMT tumor cells also induced the generation of immunosuppressive regulatory DCs (DCreg), which induced immunosuppressive CD4+Foxp3+ Tregs and eventually impaired the induction of antitumor CTLs [52,53]. In an entirely in vitro system where lung, breast, or hepatocellular carcinoma cells were cocultured with T lymphocytes, B lymphocytes, and NK cells, EMT induction in tumor cells led to NK- and T-lymphocyte apoptosis, the inhibition of lymphocyte proliferation, and the stimulation of regulatory T and B cells. IDO was involved at least in part in these effects [54].
In several instances, a bidirectional cross-talk has been demonstrated, with EMT tumor cells inducing immunosuppressive changes in the TME and immune cells inducing further amplification of tumor cell EMT [51]. An interesting example of such a bidirectional cross-talk between EMT tumor cells and cells of the immune system has been brought recently [55]. Overexpression of the extracellular matrix protein secreted protein acidic and rich in cysteine (SPARC) in breast cancer cells reduced their growth rate and induced EMT. This led to the formation of an immunosuppressive TME with increased infiltration of Tregs, mast cells, and MDSCs. On the other hand, inhibition of the suppressive function of MDSCs could revert tumor cell EMT, thereby showing that MDSCs contributed to the induction and/or amplification of tumor cell EMT. In a KRASG12D-driven mouse model of lung cancer [56], tumor cells expressing the EMT transcription factor Snail secreted a soluble mediator, which increased Gr1+ neutrophil infiltration and secretion of the chemokine C-X-C motif chemokine ligand (CXCL) 2 by the neutrophils themselves. The neutrophils, on the other hand, favored tumor growth, reduced T cell homing in the tumor, prevented successful anti-PD-1 immunotherapy, and altered angiogenesis, leading to hypoxia and sustained Snail expression in the tumor cells [56]. Bladder cancer cells have been shown to recruit mast cells to the tumor [44]. Recruited mast cells could then enhance bladder cancer cell invasion. Thyroid cancer cells recruited and activated mast cells in the TME [57], which in turn released IL-8, which induced EMT and tumor-initiating features in the thyroid cancer cells [57].
So far, we have discussed the suppressive effects of EMT tumor cells on cells of the immune system. Recently, the consequences of the immunosuppressive effects of EMT tumor cells on epithelial tumor cells have also been described [58]. Mammary tumor cells arising from epithelial tumor cell lines expressed high levels of HLA-I, low levels of PD-L1, and were infiltrated by CD8+ T lymphocytes and M1-polarized (antitumor) macrophages. On the other hand, tumors arising from EMT carcinoma cell lines expressed low levels of HLA-I, high levels of PD-L1, and were infiltrated by Tregs, M2-polarized (protumor) macrophages, and exhausted CD8+ T cells. Importantly, the EMT tumor cells protected their epithelial counterparts from immune attack.
2.4. The Mediators of EMT-Induced Effects on Immune Cells
The effects of tumor cell EMT on cells of the immune system are largely mediated by soluble molecules such as cytokines or chemokines rather than by cell-to-cell contact. Recently, a new player, extracellular vesicles, or exosomes, has joined soluble molecules as a mediator of EMT effects on cells of the immune system.
Several molecules have been shown to directly mediate the effects of EMT tumor cells on cells of the immune system. Examples of these factors are the following: chemokines such as IL-8/CXCL8 [42,59], CXCL1, and CXCL2 [48]; C-C motif chemokine ligand (CCL) 2 [53]; CCL20 [50]; cytokines such as IL-6 [60]; TGF-β [46]; the other member of the TGF-β superfamily bone morphogenetic protein (BMP) 4 [49]; granulocyte–macrophage (GM) colony-stimulating factor (CSF) [51]; other soluble mediators such as thrombospondin-1 [52]; and lipocalin 2 [53]. Exosomes have been shown to promote the polarization of macrophages toward the immunosuppressive M2 phenotype upon engulfment by the cells [61]. Table 2 gives a synoptic view of the mediators of the EMT-induced effects on immune cells and the experimental or clinical settings in which the effects were observed.
Table 2.
Mediators (soluble mediators or exosomes) of the effects of EMT tumor cells on cells of the immune system.
| Mediator | Summary of Experimental Observations. | References |
|---|---|---|
| Cytokines | ||
| IL-2 | IL-2 from cholangiocarcinoma cells with EMT-like features induced generation of CD4+ CD25+ natural Tregs. | [46] |
| IL-6 | IL-6 induced macrophages to differentiate into M2-polarized macrophages. | [60] |
| TGF-β | TGF-β from cholangiocarcinoma cells with EMT-like features induced generation of CD4+ CD25+ natural Tregs. | [46] |
| BMP-4 | Recombinant BMP4 and BMP4-containing conditioned media from bladder cancer cell lines promoted monocyte/macrophage polarization toward an M2 phenotype. | [49] |
| GM-CSF | GM-CSF from mesenchymal-like breast cancer cells (BT-549, MDA-MB-436, and MDA-MB-231) promoted the acquisition of a TAM-like phenotype by macrophages. | [51] |
| Chemokines | ||
| IL-8/CXCL8 | IL-8 from claudin-low TNBC cells induced recruitment of PMN-MDSCs in vitro and in vivo, as determined through neutralization experiments with mAb HuMax-IL8. | [42] |
| CXCL1, CXCL2 | CXCL1 and CXCL2 from mouse ovarian cancer cells promoted tumor infiltration of MDSCs, as determined by knockdown of EMT transcription factor Snail. | [48] |
| CCL2 | CCL2 derived from various tumor cell lines induced, in cooperation with Lipocalin-2, DCregs, which in turn induced Tregs, and finally impaired the induction of tumor-specific CTLs. | [53] |
| CCL20 | CCL20 derived from EMT hepatoma cells induced IDO in monocyte-derived macrophages, which in turn suppressed T-cell proliferations and promoted the expansion of Tregs. | [50] |
| Other Soluble Mediators | ||
| Thrombospondin-1 | Snail-transduced melanoma cells with EMT features produced thrombospondin-1, which induced Tregs and impaired DCs in vitro and in vivo. | [52] |
| Lipocalin-2 | CCL2 derived from various tumor cell lines induced, in cooperation with Lipocalin-2, DCregs, which in turn induced Tregs and finally impaired the induction of tumor-specific CTLs. | [53] |
| Exosomes | ||
| Snail-expressing EMT human head and neck cancer cells activated the transcription of miR-21 to produce tumor-derived exosomes, which were engulfed by CD14+ human monocytes, suppressing the expression of M1 markers and increasing that of M2 markers. | [61] | |
Abbreviations: BMP, bone morphogenetic protein; CCL, C-C motif chemokine ligand; CTL, cytotoxic T lymphocyte; CXCL, C-X-C motif chemokine ligand; DCreg, regulatory dendritic cell; GM-CSF, granulocyte–macrophage colony-stimulating factor; ICAM, intercellular adhesion molecule; IDO, indoleamine 2,3-dioxygenase; IL, interleukin; MDSC, myeloid-derived suppressor cell; miR-21, micro-RNA; PAI, plasminogen activator inhibitor; PMN, polymorphonuclear; TAM, tumor-associated macrophage; TGF, transforming growth factor; TNBC, triple-negative breast cancer; Treg, regulatory T cell.
2.5. Induction of Tumor Cell EMT by Cells of the Immune System
In this and the following section, we discuss the other loop of the cross-talk, i.e., the induction of tumor cell EMT by cells of the immune system. Again, we will first discuss which immune cells promote EMT induction, and following that which factors mediate this induction. Both the cells of the native and adaptive immune systems have been shown to induce EMT: Cells of the native immune system include NK cells [40,62], MDSCs [55,63,64], lipopolysaccharide (LPS)-activated macrophages [65,66], TAMs [67,68,69,70,71,72,73], neutrophils [74], and mast cells [57]; cells of the adaptive immune system include TILs [75], activated T lymphocytes [76], CD4+ T lymphocytes [77], CD8+ T lymphocytes [78], and B lymphocytes [79]. In some cases, EMT induction in tumor cells has been shown to be accompanied, as one might expect, by the acquisition of tumor-initiating potential [78]. Moreover, the stimulation of immune cells with cell type-specific activators can enhance their potential for inducing EMT in tumor cells. Thus, M2-polarized TAMs induced EMT in pancreatic cancer cells in a manner dependent on the expression of the LPS coreceptor toll-like receptor (TLR) 4 and IL-10 secretion [73]. This induction was strongly enhanced upon LPS stimulation of TLR4. Eventually, as for EMT-induced effects on immune cells, immune cell-induced EMT in tumor cells can also be part of a bidirectional cross-talk. In addition to the examples cited in Section 2.3, in a mouse model of pancreatic cancer, tumor cells converted CD14+ peripheral blood monocytes into monocytic MDSCs, which in turn induced tumor cell EMT [80].
2.6. The Mediators of the Induction of Tumor Cell EMT by Cells of the Immune System
The induction of tumor cell EMT by cells of the immune system is also mediated by soluble factors or extracellular vesicles. Here, a bewilderingly large number of soluble molecules released by cells of the immune system have been shown to induce tumor cell EMT. Examples of these mediators are the following: cytokines such as interferon (IFN)-γ [40,62,81,82], tumor necrosis factor (TNF)-α [16,40,66,76,82,83,84,85], IL-6 [76,77,86,87,88,89,90,91], IL-17 [92,93], IL-18 [94], TGF-β [21,63,67,71,74,76,95], epidermal growth factor (EGF) [21,63,90], hepatocyte growth factor (HGF) [63], high-mobility group box 1 (HMGB1) [96], macrophage migration inhibitory factor (MIF) [97], B-cell activating factor [79], chemokines such as IL-8/CXCL8 [57,68,98,99], CCL2 [88], CCL18 [51,100], and CCL21 [101]. In one case, a cytokine, CSF-1, was shown to induce a partial EMT in inflammatory breast cancer cells. Partial EMT was characterized by upregulation of the mesenchymal marker vimentin, while expression of the epithelial marker E-cadherin was maintained [102]. This article is of interest, since it is one of the few that has investigated the mechanisms of induction of a partial EMT, where both epithelial and mesenchymal markers coexist.
Different soluble mediators may exert additive/synergistic effects on the induction of tumor cell EMT, as has been demonstrated with TGF-β and TNF-α in lung cancer cells [95]; TNF-α, IL-1β, and IL-6 in renal cell carcinoma (RCC) cells [85]; IL-6 and CCL2 in NSCLC cells [88]; TGF-β, IL-6, and TNF-α in inflammatory breast cancer cells [76]; IL-6 and EGF in ovarian carcinoma cells [90]; and IL-6 and TGF-β in NSCLC cells [103]. In one case, each of two soluble mediators, CCL20 and CXCL8, did not induce EMT by itself, but required the contemporary presence of the other chemokine [104]. EMT induction in tumor cells may also be the result of a sequential induction of soluble mediators. Thus, in RCC cells, TNF-α has been shown to induce EMT through increased expression of the chemokine receptors CXCR2 and CXCR3 and their related ligands [105]. In lung adenocarcinoma cells, TGF-β upregulated CXCR7 expression, which mediated the induction of EMT and the acquisition of tumor-initiating potential [106].
With regard to extracellular vesicles, exosomes derived from TILs have been shown to induce EMT in human esophageal squamous cell carcinoma cells [75].
Table 3 gives a synoptic view of the mediators of the induction of tumor cell EMT by cells of the immune system and the experimental or clinical settings in which the effects were observed.
Table 3.
Mediators (soluble mediators or exosomes) of the induction of EMT by cells of the immune system.
| Mediator | Summary of Experimental Observations. | References |
|---|---|---|
| Cytokines | ||
| IFN-γ | IFN-γ and other cytokines mediated NK cell-induced increased malignancy of melanoma cells; | [40,61,80,81] |
| IFN-γ mediated NK cell-induced EMT and HCC formation in hepatocytes from HBsAg transgenic mice; | ||
| IFN-γ induced EMT in prostate and papillary thyroid cancer cells. | ||
| TNF-α | TNF-α and other cytokines mediated NK cell-induced increased malignancy of melanoma cells; | [40,75,81,82,83,84] |
| TNF-α, with other cytokines, induced EMT in IBC cells in a manner similar to soluble factors from activated T cells; | ||
| TNF-α induced EMT in papillary thyroid cancer and HCC cells; | ||
| TNF-α induced EMT in HCC cells, with synergistic induction in combination with IL-1β and IL-6; | ||
| TNF-α derived from macrophages induced tumor cell EMT. | ||
| TGF-β | TGF-β induced HLA class I downregulation and EMT in prostate cancer cells; | [21,62,66,70,73,75,95] |
| TGF-β mediated, with other cytokines, EMT-like changes induced by MDSCs in melanoma cells; | ||
| TGF-β mediated EMT of HCCs induced by TAMs; | ||
| TGF-β was the main mediator of EMT induced in teratocarcinoma cells by macrophage-conditioned medium; | ||
| TGF-β mediated EMT in lung adenocarcinoma cells induced by polymorphonuclear neutrophils; | ||
| TGF-β, with other cytokines, induced EMT in IBC cells in a manner similar to soluble factors from activated T cells; | ||
| TGF-β induced EMT in lung adenocarcinoma cells, with synergistic effects with other cytokines from a macrophage cell line. | ||
| EGF | EGF induced HLA-I downregulation and EMT in prostate cancer cells; | [21,62,89] |
| EGF mediated, with other cytokines, EMT-like changes induced by MDSCs in melanoma cells; | ||
| EGF induced EMT and enhanced the migration of ovarian carcinoma cells. | ||
| HGF | HGF mediated, with other cytokines, EMT-like changes induced by MDSCs in melanoma cells. | [62] |
| IL-6 | IL-6, with other cytokines, induced EMT in IBC cells in a manner similar to soluble factors from activated T cells; | [75,76,85,86,87,88,89,90] |
| IL-6 from activated T cells induced EMT in premalignant pancreatic cells; | ||
| IL-6 induced EMT in breast cancer, CRC, NSCLC, cervical carcinoma, and ovarian carcinoma cells; | ||
| IL-17 | IL-6 induced EMT in prostate cancer cell lines. | [92,93] |
| IL-17 induced EMT and enhanced migration and invasion in nasopharyngeal carcinoma cell lines. | ||
| IL-18 | IL-18 induced EMT in lung adenocarcinoma cells. | [94] |
| HMGB1 | HMGB1 induced EMT in CRC cells. | [96] |
| MIF | MIF induced EMT in pancreatic cancer cells. | [97] |
| BAF | BAF induced EMT in pancreatic cancer cells. | [78] |
| Chemokines | ||
| IL-8 | IL-8 mediated mast cell-induced EMT in human thyroid cancer cells; | [57,67,91,98] |
| IL-8 mediated macrophage-induced EMT in HCC cells; | ||
| IL-8 induced EMT and migration in human ovarian cancer cells; | ||
| review of IL-8 as a mediator between inflammation and tumor cell EMT. | ||
| CCL2 | CCL2 enhanced IL-6 induced EMT and invasion of NSCLC cells. | [87] |
| CCL18 | CCL18 from TAM induced EMT in breast cancer cells; | [51,99] |
| CCL18 induced EMT and the invasion and migration of pancreatic cancer cells. | ||
| CCL21 | CCL21 induced EMT and metastasis in CD133+ pancreatic cancer CSCs. | [100] |
| Exosomes | ||
| Exosomes from TILs induced EMT in human esophageal squamous cell carcinoma cells. | [74] | |
Abbreviations: BAF, B-cell activating factor; CCL, C-C motif chemokine ligand; CRC, colorectal carcinoma; CSC, cancer stem-like cell; EMT, epithelial-mesenchymal transition; HBsAg, hepatitis B surface antigen; HCC, hepatocellular carcinoma; HGF, hepatocyte growth factor; HLA, human leukocyte antigen; HMGB, high-mobility group box; IBC, inflammatory breast cancer; IFN, interferon; IL, interleukin; MDSC, myeloid-derived suppressor cell; MIF, macrophage migration inhibitory factor; NK, natural killer; NSCLC, non-small cell lung cancer; TAM, tumor-associated macrophage; TGF, transforming growth factor; TIL, tumor-infiltrating lymphocyte; TNF, tumor necrosis factor.
3. Activation of Similar Programs in Response to Similar Stimuli in Tumor Cells and Immune Cells
We have discussed the evidence showing that tumor cells and cells of the immune system can undergo a vicious cross-talk favoring the induction of EMT in tumor cells and immune exclusion and/or deviation. In this section, we discuss some recent results suggesting that tumor cells and immune cells can respond to similar stimuli, activating similar programs leading to EMT in tumor cells and to immune exclusion and/or immune deviation. In the following, we also address the possible implications of these observations.
The fact that similar stimuli can induce both effects appears obvious, since several soluble mediators have been discussed in previous sections as being able to induce both tumor cell EMT and inhibition of antitumor immune responses. Of these, TGF-β is the best known and most deeply investigated of these factors. TGF-β is a potent inducer of EMT in general and of tumor cell EMT in particular [107,108,109]. In addition, it induces multiple effects on cells of the immune system. In general, these effects promote the exclusion of immune cells from the TME and the inhibition of immunological recognition and effector functions. Thus, TGF-β promotes the differentiation of naïve CD4+ T cell into Tregs [110], inhibits the differentiation of Th1 cells [111], and prevents the expression of Th2-specific cytokines [112]. In mouse models of metastatic colorectal cancer, it inhibited tumor infiltration by T lymphocytes and differentiation of effector Th1 lymphocytes [113]. TGF-β also inhibits effector functions in NK cells and macrophages and antigen presentation by DCs and macrophages [114], and it promotes upregulation of the EMT transcription factor Snail in human THP-1 macrophages, thereby inducing their M2 polarization [115]. An interesting article has reported that TGF-β induces in EMT tumor cells a cluster of genes that is specifically enriched in monocyte-derived macrophages, mast cells, and myeloid DCs (but less so in other types of immune cells) [116]. This was observed upon long-term treatment of mouse mammary EpRas tumor cells with TGF-β1 for two weeks. It was further shown that this gene cluster was enriched in human breast cancer cell lines displaying an EMT or a Basal B profile and in human breast tumors with EMT and undifferentiated characteristics. These are important results, since they show that a single soluble mediator, the cytokine TGF-β, can induce in tumor cells, along with other modifications typical of EMT, a cluster of genes typical of cells of the native immune system.
In the following, we discuss some other examples of mediators that also act on both tumor cells and cells of the immune system. Estrogen receptor-binding fragment-associated antigen 9 (EBAG9) is an estrogen-responsive gene that was originally identified in breast cancer cells. It is a cancer biomarker and promotes the immune escape of tumor cells. It has been recently shown that prostate cancer-derived extracellular vesicles containing EBAG9 can both promote EMT in prostate cancer cells as well as suppress the cytotoxicity of T lymphocytes [117].
HGF is another cytokine that is involved in EMT induction in tumor cells [63,71]. Expression of the specific HGF receptor Met in the immune system is limited to antigen-presenting cells, including DCs. HGF has been found to play a role in peripheral immune tolerance by directing DC differentiation toward a tolerogenic phenotype. In skin immunity, Met signaling drives the mobilization of DCs by regulating matrix metalloproteinase activities [118]. This is reminiscent of tumor cell mobilization in response to EMT induction by HGF and other mediators [2].
Further examples have shown that similar transcription factors can promote EMT in tumor cells and immunosuppressive changes in cells of the immune system. Thus, zinc finger E-box-binding homeobox (ZEB), an E-box transcriptional repressor involved in the induction of tumor cell EMT, has been shown to negatively regulate the expression of the co-stimulatory molecule CD4 in CD4 single-positive T lymphocytes [119] and to act as a transcriptional repressor of IL-2 by binding to the IL-2 promoter [120] and as a repressor of the immunoglobulin heavy chain enhancer [121].
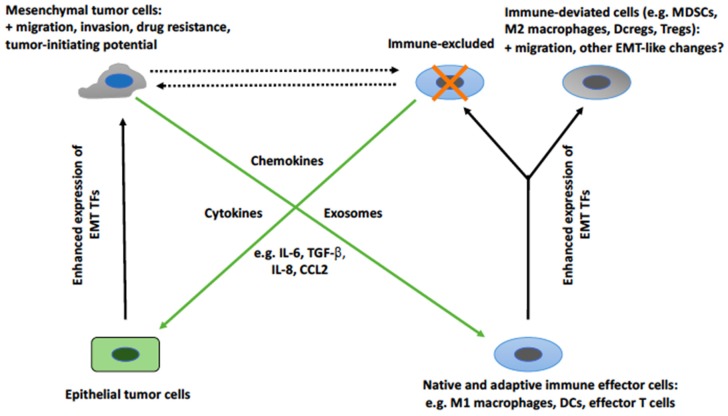
As already mentioned, overexpression of the other EMT transcription factor, Snail, in human THP-1 macrophages caused their M2 polarization by inhibiting proinflammatory cytokine release and promoting the expression of M2-specific markers [115]. In contrast, Snail knockdown promoted M1 polarization through the upregulation of proinflammatory cytokines. Snail overexpression has also been shown to induce EMT-like functionalities in keratinocytes [122], cells that can act as antigen-presenting cells [123]. These cells acquired an enhanced ability to attract monocytes and to invade a dense interstitial collagen matrix. The maturation of Langerhans cells, a subset of DCs of the skin, was accompanied by downregulation of a set of epithelial genes, including E-cadherin, and by upregulation of the mesenchymal marker N-cadherin (known to facilitate cell migration) [124]. Moreover, the EMT-associated transcription factors ZEB1 and ZEB2 were upregulated in migratory Langerhans cells. These results suggest that these modifications, reminiscent of an EMT, might facilitate the mobilization of Langerhans cells in a manner similar to the acquisition of migratory and invasive properties by EMT tumor cells. Before drawing a premature conclusion that expression of EMT transcription factors in immune cells is always accompanied by immunosuppressive effects, it is fair to note that, in several instances, expression of EMT transcription factors in cells of the immune system has been reported to induce immunostimulating effects [125,126,127]. It is at present unclear what causes an EMT transcription factor to promote immunosuppressive or immunostimulating effects in immune cells. In spite of this limitation, it appears clear that the expression of EMT transcription factors in immune cells can have effects that are not dissimilar to those induced in tumor cells. At present, it is difficult to precisely characterize the functional implications of these observations in the cross-talk between EMT tumor cells and immune cells. Figure 1 represents an attempt to depict and summarize the available knowledge about this cross-talk. It shows that tumor cells responding to soluble mediators released by cells of the immune system undergo an EMT. Vice versa, EMT tumor cells release mediators (soluble mediators or extracellular vesicles) that induce immunosuppressive effects. This cross-talk favors positive amplification loops that favor further recruitment of EMT tumor cells and excluded/deviated immune cells. We have also indicated that EMT cells and immune cells acquire, at least in part, overlapping functionalities such as migration and invasion.
Figure 1.
The relationship between changes induced by EMT tumor cells in cells of the immune system and the induction of tumor cell EMT by cells of the immune system. EMT tumor cells induce changes in cells of the immune system that promote their exclusion or deviation toward protumorigenic phenotypes. The mediators of these changes are cytokines, chemokines, or exosomes. At least part of these mediators induce both changes, possibly through the activation of a similar set of EMT transcription factors. Moreover, some of the changes that affect tumor cells and cells of the immune system are similar, such as enhanced migration. The dashed lines indicate an as yet unexplored aspect of this relationship, i.e., the possibility that EMT tumor cells and deviated immune cells regulate each other. Abbreviations: CCL, C-C motif chemokine ligand; DC, dendritic cell; DCreg, regulatory DC; EMT, epithelial-mesenchymal transition; IL, interleukin; MDSC, myeloid-derived suppressor cell; TGF, transforming growth factor; TF, transcription factor; Treg, regulatory T cell.
4. Some Therapeutic Implications
In this article, we have discussed the cross-talk between tumor cells and cells of the immune system. These two cell populations communicate with each other through soluble mediators and exosomes. Thus, the scenario appears quite simple, but the system appears highly redundant, with many types of immune cells and tumor cells that encompass different stages between a fully epithelial and a fully mesenchymal phenotype. Moreover, a countless number of soluble mediators have been reported to act as go-betweens. It is clear that this scenario poses significant problems from a therapeutic point of view. In fact, if the system is so highly complex and redundant, where is it appropriate to act? On the tumor cell side, on the immune cell side, or on the side of the mediators? From an experimental point of view, many approaches have been pursued, and many successful therapeutic interventions have been reported in the literature in experimental systems. In the following, we discuss a few examples of these approaches.
On the tumor cell side, many approaches have been described that aimed at inhibiting or reversing EMT or depleting EMT tumor cells [2], including those targeting TGF-β (which appears to play a pivotal role among EMT-inducing mediators) [128]. Interestingly, an active immunization approach against the EMT transcription factor brachyury has also been reported [129], and a phase I clinical trial with this vaccine, designated GI-6301, has been initiated in patients with advanced tumors. The inhibition of cytokine or chemokine signaling is another approach to interrupt EMT induction by immune cells or EMT-induced immunosuppressive effects and, for the reasons that were discussed in previous sections, may act on both sides of the cross-talk.
It would go beyond the scope of this article to enter a detailed discussion of the individual therapeutic approaches that have been tested in experimental models in order to interrupt the cross-talk between EMT cells and immune cells. It should be noted, however, that in spite of the multitude of successful experimental interventions that have been reported in the literature, clinical application has lagged behind for most of these. Thus, only a few of these approaches have progressed into a clinic, and positive results in the human setting have been very scarce, if any. This also holds true for the closely related field of anti-CSC candidate drugs [130,131]. The possible reasons for these failures are numerous. One of the reasons that we would like to mention here is that most of the experimental systems that are used for preclinical investigations reflect only to a very limited degree the human situation, which is likely much more complex than most “snapshot” animal models. The situation is likely further complicated by issues such as drug penetration and the onset of drug resistance [132], which certainly play a more important role in the human setting than in small-sized animal models.
Given this problematic background, one is led to ask which might be the most promising approaches to interrupting the cross-talk between EMT cells and immune cells. We envisage three possibilities: first, acting on EMT tumor cells; second, acting on cytokines or chemokines that act as mediators; and third, acting on immune cells. Targeting cytokines or chemokines appears to be very challenging, because this is probably the most redundant component of the cross-talk. Depleting EMT tumor cells appears to be more promising, but this should be combined with approaches aimed at depleting other tumor cells populations, such as differentiated epithelial cells and autophagic tumor cells [37]. The intrinsic phenotypic heterogeneity of EMT tumor cells [3], however, can be a potential problem that is difficult to estimate at present. Immune cells are also difficult to target because of the vast array of immune cell populations that can induce EMT. One possibility is to investigate antibodies targeting inhibitory immune checkpoints (e.g., anti-PD-1, anti-PD-L1, anti-CTLA-4). These antibodies have represented a turning point in cancer therapy [133]. The mechanism of action that is generally ascribed to these drugs is restoring an efficient antitumor immune response [133]. As discussed before, the induction of EMT tumor cells is mainly induced by deviated immune cells (e.g., Tregs, DCregs, MDSCs, M2-polarized TAMs), and it is reasonable to expect that restoring a non-deviated, efficient antitumor immune response may also have favorable consequences on the induction of tumor cell EMT.
5. Conclusions
We have discussed the fundamentals of the cross-talk between EMT tumor cells and immune cells. This cross-talk rests, on the one hand, on the induction of EMT in carcinoma cells (or a process bearing similarities with an EMT in noncarcinoma cells, such as melanoma cells) by cells of the immune system with an immune-deviated phenotype. On the other hand, it rests on the induction of immune exclusion and/or immune deviation by EMT tumor cells. While this picture is quite clear, there remain important unresolved questions. First, as already discussed, an EMT in tumor cells is per se a set of phenotypic states that range from a fully epithelial to a fully mesenchymal phenotype. We do not know if the intermediate, hybrid states differ in their capacity to promote immune-excluded or immunosuppressed states. Second, and vice versa, we do not know if the different cell populations with an immune-deviated phenotype differ in their capacity to induce tumor cell EMT or different hybrid states of EMT. Third, the bewildering number of soluble mediators (now also extracellular vesicles) that participate in the cross-talk may also differ in inducing different states of tumor cell EMT and different states of immune exclusion or immunosuppression. Fourth, and most intriguingly, we have seen that tumor cells and immune cells may respond to similar stimuli in a similar manner, i.e., activating similar transcriptional regulators and even similar functional activities. The significance of these “symmetrical” changes is obscure at present. Does it form the basis of a cross-talk between entities that have undergone similar changes and and that may impact tumor progression? In fact, the cross-talk that has been portrayed so far bears on the induction of EMT in differentiated, epithelial tumor cells by immune cells and suppression/deviation in immune cells by EMT tumor cells. Possible reciprocal effects between “full-blown” EMT tumor cells and “full-blown” suppressed/deviated immune cells have not been investigated so far. As can be easily seen from these few traits, much work remains to be done in this field, and many issues remain to be uncovered.
Author Contributions
E.R., C.A.C., C.R., and F.M. contributed to the conception of the work, drafted or revised it critically, approved the final version, and agreed to be accountable for all aspects of the work.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Hanahan D., Coussens L.M. Accessories to the crime: Functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21:309–322. doi: 10.1016/j.ccr.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 2.Marcucci F., Stassi G., De Maria R. Epithelial–mesenchymal transition: A new target in anticancer drug discovery. Nat. Rev. Drug Discov. 2016;15:311–325. doi: 10.1038/nrd.2015.13. [DOI] [PubMed] [Google Scholar]
- 3.Pastushenko I., Brisebarre A., Sifrim A., Fioramonti M., Revenco T., Boumahdi S., Van Keymeulen A., Brown D., Moers V., Lemaire S., et al. Identification of the tumour transition states occurring during EMT. Nature. 2018;556:463–468. doi: 10.1038/s41586-018-0040-3. [DOI] [PubMed] [Google Scholar]
- 4.Marcucci F., Bellone M., Caserta C.A., Corti A. Pushing tumor cells towards a malignant phenotype. Stimuli from the microenvironment, intercellular communications and alternative roads. Int. J. Cancer. 2014;135:1265–1276. doi: 10.1002/ijc.28572. [DOI] [PubMed] [Google Scholar]
- 5.Dumont N., Wilson M.B., Crawford Y.G., Reynolds P.A., Sigaroudinia M., Tlsty T.D. Sustained induction of epithelial to mesenchymal transition activates DNA methylation of genes silenced in basal-like breast cancers. Proc. Natl. Acad. Sci. USA. 2008;105:14867–14872. doi: 10.1073/pnas.0807146105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chung S.S., Giehl N., Wu Y.Y., Vadgama J.V. STAT3 activation in HER2-overexpressing breast cancer promotes epithelial−mesenchymal transition and cancer stem cell traits. Int. J. Oncol. 2014;44:403–411. doi: 10.3892/ijo.2013.2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thiery J.P., Adocque H., Huang R.Y.J., Nieto M.A. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 8.Chui M.H. Insights into cancer metastasis from a clinicopathologic perspective: Epithelial-Mesenchymal Transition is not a necessary step. Int. J. Cancer. 2013;132:1487–1495. doi: 10.1002/ijc.27745. [DOI] [PubMed] [Google Scholar]
- 9.Murakami R., Matsumura N., Mandai M., Yoshihara K., Tanabe H., Nakai H., Yamanoi K., Abiko K., Yoshioka Y., Hamanishi J., et al. Establishment of a novel histopathological classification of high-grade serous ovarian carcinoma correlated with prognostically distinct gene expression subtypes. Am. J. Pathol. 2016;186:1103–1113. doi: 10.1016/j.ajpath.2015.12.029. [DOI] [PubMed] [Google Scholar]
- 10.Chae Y.K., Chang S., Ko T., Anker J., Agte S., Iams W., Choi W.M., Lee K., Cruz M. Epithelial-mesenchymal transition (EMT) signature is inversely associated with T-cell infiltration in non-small cell lung cancer (NSCLC) Sci. Rep. 2018;8:2918. doi: 10.1038/s41598-018-21061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yan Y., Zhang J., Li J.H., Liu X., Wang J.Z., Qu H.Y., Wang J.S., Duan X.Y. High tumor-associated macrophages infiltration is associated with poor prognosis and may contribute to the phenomenon of epithelial-mesenchymal transition in gastric cancer. Onco. Targets Ther. 2016;9:3975–3983. doi: 10.2147/OTT.S103112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lou Y., Diao L., Cuentas E.R.P., Denning W.L., Chen L., Fan Y.H., Byers L.A., Wang J., Papadimitrakopoulou V.A., Behrens C., et al. Epithelial–mesenchymal transition is associated with a distinct tumor microenvironment including elevation of inflammatory signals and multiple immune checkpoints in lung adenocarcinoma. Clin. Cancer Res. 2016;22:3630–3642. doi: 10.1158/1078-0432.CCR-15-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mak M.P., Tong P., Diao L., Cardnell R.J., Gibbons D.L., William W.N., Skoulidis F., Parra E.R., Rodriguez-Canales J., Wistuba I.I., et al. A patient-derived, pan-cancer EMT signature identifies global molecular alterations and immune target enrichment following epithelial-to-mesenchymal transition. Clin. Cancer Res. 2016;22:609–620. doi: 10.1158/1078-0432.CCR-15-0876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim S., Koh J., Kim M.Y., Kwon D., Go H., Kim Y.A., Jeon Y.K., Chung D.H. PD-L1 expression is associated with epithelial-to-mesenchymal transition in adenocarcinoma of the lung. Hum. Pathol. 2016;58:7–14. doi: 10.1016/j.humpath.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Alsuliman A., Colak D., Al-Harazi O., Fitwi H., Tulbah A., Al-Tweigeri T., Al-Alwan M., Ghebeh H. Bidirectional crosstalk between PD-L1 expression and epithelial to mesenchymal transition: Significance in claudin-low breast cancer cells. Mol. Cancer. 2015;14:149. doi: 10.1186/s12943-015-0421-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Landsberg J., Kohlmeyer J., Renn M., Bald T., Rogava M., Cron M., Fatho M., Lennerz V., Wölfel T., Hölzel M., et al. Melanomas resist T-cell therapy through inflammation-induced reversible dedifferentiation. Nature. 2012;490:412–418. doi: 10.1038/nature11538. [DOI] [PubMed] [Google Scholar]
- 17.Woods K., Pasam A., Jayachandran A., Andrews M.C., Cebon J. Effects of epithelial to mesenchymal transition on T cell targeting of melanoma cells. Front. Oncol. 2014;4:367. doi: 10.3389/fonc.2014.00367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knutson K.L., Lu H., Stone B., Reiman J.M., Behrens M.D., Prosperi C.M., Gad E.A., Smorlesi A., Disis M.L. Immunoediting of cancers may lead to epithelial to mesenchymal transition. J. Immunol. 2006;177:1526–1533. doi: 10.4049/jimmunol.177.3.1526. [DOI] [PubMed] [Google Scholar]
- 19.Tripathi S.C., Peters H.L., Taguchi A., Katayama H., Wang H., Momin A., Jolly M.K., Celiktas M., Rodriguez-Canales J., Liu H., et al. Immunoproteasome deficiency is a feature of non-small cell lung cancer with a mesenchymal phenotype and is associated with a poor outcome. Proc. Natl. Acad. Sci. USA. 2016;113:E1555–E1564. doi: 10.1073/pnas.1521812113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.López-Soto A., Huergo-Zapico L., Galvan J.A., Rodrigo L., de Herreros A.G., Astudillo A., Gonzalez S. Epithelial-mesenchymal transition induces an antitumor immune response mediated by NKG2D receptor. J. Immunol. 2013;190:4408–4419. doi: 10.4049/jimmunol.1202950. [DOI] [PubMed] [Google Scholar]
- 21.Chen X.H., Liu Z.C., Zhang G., Wei W., Wang X.X., Wang H., Ke H.P., Zhang F., Wang H.S., Cai S.H., et al. TGF-β and EGF induced HLA-I downregulation is associated with epithelial-mesenchymal transition (EMT) through upregulation of snail in prostate cancer cells. Mol. Immunol. 2015;65:34–42. doi: 10.1016/j.molimm.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 22.Kumar S., Davra V., Obr A.E., Geng K., Wood T.L., De Lorenzo M.S., Birge R.B. Crk adaptor protein promotes PD-L1 expression, EMT and immune evasion in a murine model of triple-negative breast cancer. Oncoimmunology. 2017;7:e1376155. doi: 10.1080/2162402X.2017.1376155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen L., Gibbons D.L., Goswami S., Cortez M.A., Ahn Y.H., Byers L.A., Zhang X., Yi X., Dwyer D., Lin W., et al. Metastasis is regulated via microRNA-200/ZEB1 axis control of tumour cell PD-L1 expression and intratumoral immunosuppression. Nat. Commun. 2014;5:5241. doi: 10.1038/ncomms6241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shan B., Man H., Liu J., Wang L., Zhu T., Ma M., Xv Z., Chen X., Yang X., Li P. TIM-3 promotes the metastasis of esophageal squamous cell carcinoma by targeting epithelial-mesenchymal transition via the Akt/GSK-3β/Snail signaling pathway. Oncol. Rep. 2016;36:1551–1561. doi: 10.3892/or.2016.4938. [DOI] [PubMed] [Google Scholar]
- 25.Jiang B., Zhang T., Liu F., Sun Z., Shi H., Hua D., Yang C. The co-stimulatory molecule B7-H3 promotes the epithelial-mesenchymal transition in colorectal cancer. Oncotarget. 2016;7:31755–31771. doi: 10.18632/oncotarget.9035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhi Y., Mou Z., Chen J., He Y., Dong H., Fu X., Wu Y. B7H1 expression and epithelial-to-mesenchymal transition phenotypes on colorectal cancer stem-like cells. PLoS ONE. 2015;10:e0135528. doi: 10.1371/journal.pone.0135528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Noman M.Z., Van Moer K., Marani V., Gemmill R.M., Tranchevent L.C., Azuaje F., Muller A., Chouaib S., Thiery J.P., Berchem G., et al. CD47 is a direct target of SNAI1 and ZEB1 and its blockade activates the phagocytosis of breast cancer cells undergoing EMT. Oncoimmunology. 2018;7:e1345415. doi: 10.1080/2162402X.2017.1345415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Noman M.Z., Janji B., Abdou A., Hasmim M., Terry S., Tan T.Z., Mami-Chouaib F., Thiery J.P., Chouaib S. The immune checkpoint ligand PD-L1 is upregulated in EMT-activated human breast cancer cells by a mechanism involving ZEB-1 and miR-200. Oncoimmunology. 2017;6:e1263412. doi: 10.1080/2162402X.2016.1263412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Y., Wang H., Zhao Q., Xia Y., Hu X., Guo J. PD-L1 induces epithelial-to-mesenchymal transition via activating SREBP-1c in renal cell carcinoma. Med. Oncol. 2015;32:212. doi: 10.1007/s12032-015-0655-2. [DOI] [PubMed] [Google Scholar]
- 30.Marcucci F., Rumio C., Corti A. Tumor cell-associated immune checkpoint molecules – Drivers of malignancy and stemness. Biochim. Biophys. Acta. 2017;1868:571–583. doi: 10.1016/j.bbcan.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 31.David J.M., Hamilton D.H., Palena C. MUC1 upregulation promotes immune resistance in tumor cells undergoing brachyury-mediated epithelial-mesenchymal transition. Oncoimmunology. 2016;5:e1117738. doi: 10.1080/2162402X.2015.1117738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hamilton D.H., Huang B., Fernando R.I., Tsang K.-Y., Palena C. WEE1 inhibition alleviates resistance to immune attack of tumor cells undergoing epithelial–mesenchymal transition. Cancer Res. 2014;74:2510–2519. doi: 10.1158/0008-5472.CAN-13-1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Terry S., Buart S., Tan T.Z., Gros G., Noman M.Z., Jorens J.B., Mami-Chouaib F., Thiery J.P., Chouaib S. Acquisition of tumor cell phenotypic diversity along the EMT spectrum under hypoxic pressure: Consequences on susceptibility to cell-mediated cytotoxicity. Oncoimmunology. 2017;6:e1271858. doi: 10.1080/2162402X.2016.1271858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Akalay I., Tan T.Z., Kumar P., Janji B., Mami-Chouaib F., Charpy C., Vielh P., Larsen A.K., Thiery J.P., Sabbah M., et al. Targeting WNT1-inducible signaling pathway protein 2 alters human breast cancer cell susceptibility to specific lysis through regulation of KLF-4 and miR-7 expression. Oncogene. 2015;34:2261–2271. doi: 10.1038/onc.2014.151. [DOI] [PubMed] [Google Scholar]
- 35.Noman M.Z., Buart S., Romero P., Ketari S., Janji B., Mari B., Mami-Chouaib F., Chouaib S. Hypoxia-inducible miR-210 regulates the susceptibility of tumor cells to lysis by cytotoxic T cells. Cancer Res. 2012;72:4629–4641. doi: 10.1158/0008-5472.CAN-12-1383. [DOI] [PubMed] [Google Scholar]
- 36.Akalay I., Janji B., Hasmim M., Noman M.Z., André F., De Cremoux P., Bertheau P., Badoual C., Vielh P., Larsen A.K., et al. Epithelial-to-mesenchymal transition and autophagy induction in breast carcinoma promote escape from T-cell-mediated lysis. Cancer Res. 2013;73:2418–2427. doi: 10.1158/0008-5472.CAN-12-2432. [DOI] [PubMed] [Google Scholar]
- 37.Marcucci F., Rumio C. How tumor cells choose between epithelial-mesenchymal transition and autophagy to resist stress—Therapeutic implications. Front. Pharmacol. 2018;9:714. doi: 10.3389/fphar.2018.00714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huergo-Zapico L., Acebes-Huerta A., López-Soto A., Villa-Álvarez M., Gonzalez-Rodriguez P., Gonzalez S.L. Molecular bases for the regulation of NKG2D ligands in cancer. Front. Immunol. 2014;5:106. doi: 10.3389/fimmu.2014.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chockley P.J., Chen J., Chen G., Beer D.G., Standiford T.J., Keshamouni V.G. Epithelial-mesenchymal transition leads to NK cell-mediated metastasis-specific immunosurveillance in lung cancer. J. Clin. Investig. 2018;128:1384–1396. doi: 10.1172/JCI97611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huergo-Zapico L., Parodi M., Cantoni C., Lavarello C., Fernández-Martínez J.L., Petreto A., DeAndrés-Galiana E.J., Balsamo M., López-Soto A., Pietra G., et al. NK-cell editing mediates epithelial-to-mesenchymal transition via phenotypic and proteomic changes in melanoma cell lines. Cancer Res. 2018;78:3913–3925. doi: 10.1158/0008-5472.CAN-17-1891. [DOI] [PubMed] [Google Scholar]
- 41.Spranger S., Gajewski T.F. Impact of oncogenic pathways on evasion of antitumour immune responses. Nat. Rev. Cancer. 2018;18:139–147. doi: 10.1038/nrc.2017.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dominguez C., McCampbell K.K., David J.M., Palena C. Neutralization of IL-8 decreases tumor PMN-MDSCs and reduces mesenchymalization of claudin-low triple-negative breast cancer. JCI Insight. 2017;2:94296. doi: 10.1172/jci.insight.94296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Suarez-Carmona M., Bourcy M., Lesage J., Leroi N., Syne L., Blacher S., Hubert P., Erpicum C., Foidart J.M., Delvenne P., et al. Soluble factors regulated by epithelial-mesenchymal transition mediate tumour angiogenesis and myeloid cell recruitment. J. Pathol. 2015;236:491–504. doi: 10.1002/path.4546. [DOI] [PubMed] [Google Scholar]
- 44.Rao Q., Chen Y., Yeh C.R., Ding J., Li L., Chang C., Yeh S. Recruited mast cells in the tumor microenvironment enhance bladder cancer metastasis via modulation of ERβ/CCL2/CCR2 EMT/MMP9 signals. Oncotarget. 2016;7:7842–7855. doi: 10.18632/oncotarget.5467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Knab L.M., Ebine K., Chow C.R., Raza S.S., Sahai V., Patel A.P., Kumar K., Bentrem D.J., Grippo P.J., Munshi H.G. Snail cooperates with Kras G12D in vivo to increase stem cell factor and enhance mast cell infiltration. Mol. Cancer Res. 2014;12:1440–1448. doi: 10.1158/1541-7786.MCR-14-0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Qian Y., Yao W., Yang T., Yang Y., Liu Y., Shen Q., Zhang J., Qi W., Wang J. aPKC-ι/P-Sp1/Snail signaling induces epithelial-mesenchymal transition and immunosuppression in cholangiocarcinoma. Hepatology. 2017;66:1165–1182. doi: 10.1002/hep.29296. [DOI] [PubMed] [Google Scholar]
- 47.Carbone C., Moccia T., Zhu C., Paradiso G., Budillon A., Chiao P.J., Abbruzzese J.L., Melisi D. Anti-VEGF treatment–resistant pancreatic cancers secrete proinflammatory factors that contribute to malignant progression by inducing an EMT cell phenotype. Clin. Cancer Res. 2011;17:5822–5832. doi: 10.1158/1078-0432.CCR-11-1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taki M., Abiko K., Baba T., Hamanishi J., Yamaguchi K., Murakami R., Yamanoi K., Horikawa N., Hosoe Y., Nakamura E., et al. Snail promotes ovarian cancer progression by recruiting myeloid-derived suppressor cells via CXCR2 ligand upregulation. Nat. Commun. 2018;9:1685. doi: 10.1038/s41467-018-03966-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martínez V.G., Rubio C., Martínez-Fernández M., Segovia C., López-Calderón F., Garín M.I., Teijeira A., Munera-Maravilla E., Varas A., Sacedón R., et al. BMP4 induces M2 macrophage polarization and favors tumor progression in bladder cancer. Clin. Cancer Res. 2017;23:7388–7399. doi: 10.1158/1078-0432.CCR-17-1004. [DOI] [PubMed] [Google Scholar]
- 50.Ye L.Y., Chen W., Bai X.L., Xu X.Y., Zhang Q., Xia X.F., Sun X., Li G.G., Hu Q.D., Fu Q.H., et al. Hypoxia-induced epithelial-to-mesenchymal transition in hepatocellular carcinoma induces an immunosuppressive tumor microenvironment to promote metastasis. Cancer Res. 2016;76:818–830. doi: 10.1158/0008-5472.CAN-15-0977. [DOI] [PubMed] [Google Scholar]
- 51.Su S., Liu Q., Chen J., Chen J., Chen F., He C., Huang D., Wu W., Lin L., Huang W., et al. A positive feedback loop between mesenchymal-like cancer cells and macrophages is essential to breast cancer metastasis. Cancer Cell. 2014;25:605–620. doi: 10.1016/j.ccr.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 52.Kudo-Saito C., Shirako H., Takeuchi T., Kawakami Y. Cancer metastasis is accelerated through immunosuppression during Snail-induced EMT of cancer cells. Cancer Cell. 2009;15:195–206. doi: 10.1016/j.ccr.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 53.Kudo-Saito C., Shirako H., Ohike M., Tsukamoto N., Kawakami Y. CCL2 is critical for immunosuppression to promote cancer metastasis. Clin. Exp. Metast. 2013;30:393–405. doi: 10.1007/s10585-012-9545-6. [DOI] [PubMed] [Google Scholar]
- 54.Ricciardi M., Zanotto M., Malpeli G., Bassi G., Perbellini O., Chilosi M., Bifari F., Krampera M. Epithelial-to-mesenchymal transition (EMT) induced by inflammatory priming elicits mesenchymal stromal cell-like immune-modulatory properties in cancer cells. Br. J. Cancer. 2015;112:1067–1075. doi: 10.1038/bjc.2015.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sangaletti S., Tripodo C., Santangelo A., Castioni N., Portararo P., Gulino A., Botti L., Parenza M., Cappetti B., Orlandi R., et al. Mesenchymal transition of high-grade breast carcinomas depends on extracellular matrix control of myeloid suppressor cell activity. Cell Rep. 2016;17:233–248. doi: 10.1016/j.celrep.2016.08.075. [DOI] [PubMed] [Google Scholar]
- 56.Faget J., Groeneveld S., Boivin G., Sankar M., Zangger N., Garcia M., Guex N., Zlobec I., Steiner L., Piersigilli A., et al. Neutrophils and Snail orchestrate the establishment of a pro-tumor microenvironment in lung cancer. Cell Rep. 2017;21:3190–3204. doi: 10.1016/j.celrep.2017.11.052. [DOI] [PubMed] [Google Scholar]
- 57.Visciano C., Liotti F., Prevete N., Calì G., Franco R., Collina F., de Paulis A., Marone G., Santoro M., Melillo R.M. Mast cells induce epithelial-to-mesenchymal transition and stem cell features in human thyroid cancer cells through an IL-8-Akt-Slug pathway. Oncogene. 2015;34:5175–5186. doi: 10.1038/onc.2014.441. [DOI] [PubMed] [Google Scholar]
- 58.Dongre A., Rashidian M., Reinhardt F., Bagnato A., Keckesova Z., Ploegh H.L., Weinberg R.A. Epithelial-to-mesenchymal transition contributes to immunosuppression in breast carcinomas. Cancer Res. 2017;77:3982–3989. doi: 10.1158/0008-5472.CAN-16-3292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dominguez C., Tsang K.Y., Palena C. Short-term EGFR blockade enhances immune-mediated cytotoxicity of EGFR mutant lung cancer cells: Rationale for combination therapies. Cell Death Dis. 2016;7:e2380. doi: 10.1038/cddis.2016.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fu X.L., Duan W., Su C.Y., Mao F.Y., Lv Y.P., Teng Y.S., Yu P.W., Zhuang Y., Zhao Y.L. Interleukin 6 induces M2 macrophage differentiation by STAT3 activation that correlates with gastric cancer progression. Cancer Imunol. Immunother. 2017;66:1597–1608. doi: 10.1007/s00262-017-2052-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hsieh C.H., Tai S.K., Yang M.H. Snail-overexpressing cancer cells promote M2-like polarization of tumor-associated macrophages by delivering miR-21-abundant exosomes. Neoplasia. 2018;20:775–788. doi: 10.1016/j.neo.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chen Y., Hao X., Sun R., Wei H., Tian Z. Natural killer cell-derived interferon-gamma promotes hepatocellular carcinoma through the epithelial cell adhesion molecule-epithelial-to-mesenchymal transition axis in hepatitis B virus transgenic mice. Hepatology. 2018;69:1735–1750. doi: 10.1002/hep.30317. [DOI] [PubMed] [Google Scholar]
- 63.Toh B., Wang X., Keeble J., Sim W.J., Khoo K., Wong W.C., Kato M., Prevost-Blondel A., Thiery J.P., Abastado J.P. Mesenchymal transition and dissemination of cancer cells is driven by myeloid-derived suppressor cells infiltrating the primary tumor. PLoS Biol. 2011;9:e1001162. doi: 10.1371/journal.pbio.1001162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Caiado F., Carvalho T., Rosa I., Remédio L., Costa A., Matos J., Heissig B., Yagita H., Hattori K., da Silva J.P., et al. Bone marrow-derived CD11b+Jagged2+ cells promote epithelial-to-mesenchymal transition and metastasization in colorectal cancer. Cancer Res. 2013;73:4233–4246. doi: 10.1158/0008-5472.CAN-13-0085. [DOI] [PubMed] [Google Scholar]
- 65.De Cock J.M., Shibue T., Dongre A., Keckesova Z., Reinhardt F., Weinberg R.A. Inflammation triggers Zeb1-dependent escape from tumor latency. Cancer Res. 2016;76:6778–6784. doi: 10.1158/0008-5472.CAN-16-0608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li K., Dan Z., Hu X., Gesang L., Ze Y., Bianba Z. CD14 regulates gastric cancer cell epithelial-mesenchymal transition and invasion in vitro. Oncol. Rep. 2013;30:2725–2732. doi: 10.3892/or.2013.2733. [DOI] [PubMed] [Google Scholar]
- 67.Fan Q.M., Jing Y.Y., Yu G.F., Kou X.R., Ye F., Gao L., Li R., Zhao Q.D., Yang Y., Lu Z.H., et al. Tumor-associated macrophages promote cancer stem cell-like properties via transforming growth factor-beta1-induced epithelial-mesenchymal transition in hepatocellular carcinoma. Cancer Lett. 2014;352:160–168. doi: 10.1016/j.canlet.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 68.Fu X.T., Dai Z., Song K., Zhang Z.J., Zhou Z.J., Zhou S.L., Zhao Y.M., Xiao Y.S., Sun Q.M., Ding Z.B., et al. Macrophage-secreted IL-8 induces epithelial-mesenchymal transition in hepatocellular carcinoma cells by activating the JAK2/STAT3/Snail pathway. Int. J. Oncol. 2015;46:587–596. doi: 10.3892/ijo.2014.2761. [DOI] [PubMed] [Google Scholar]
- 69.Ravi J., Elbaz M., Wani N.A., Nasser M.W., Ganju R.K. Cannabinoid receptor-2 agonist inhibits macrophage induced EMT in non-small cell lung cancer by downregulation of EGFR pathway. Mol. Carcinog. 2016;55:2063–2076. doi: 10.1002/mc.22451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bonde A.K., Tischler V., Kumar S., Soltermann A., Schwendener R.A. Intratumoral macrophages contribute to epithelial-mesenchymal transition in solid tumors. BMC Cancer. 2012;12:35. doi: 10.1186/1471-2407-12-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Deng Y.R., Liu W.B., Lian Z.X., Li X., Hou X. Sorafenib inhibits macrophage-mediated epithelial-mesenchymal transition in hepatocellular carcinoma. Oncotarget. 2016;7:38292–38305. doi: 10.18632/oncotarget.9438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hu Y., He M.Y., Zhu L.F., Yang C.C., Zhou M.L., Wang Q., Zhang W., Zheng Y.Y., Wang D.M., Xu Z.Q., et al. Tumor-associated macrophages correlate with the clinicopathological features and poor outcomes via inducing epithelial to mesenchymal transition in oral squamous cell carcinoma. J. Exp. Clin. Cancer Res. 2016;35:12. doi: 10.1186/s13046-015-0281-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liu C.Y., Xu J.Y., Shi X.Y., Huang W., Ruan T.Y., Xie P., Ding J.L. M2-polarized tumor-associated macrophages promoted epithelial-mesenchymal transition in pancreatic cancer cells, partially through TLR4/IL-10 signaling pathway. Lab. Investig. 2013;93:844–854. doi: 10.1038/labinvest.2013.69. [DOI] [PubMed] [Google Scholar]
- 74.Hu P., Shen M., Zhang P., Zheng C., Pang Z., Zhu L., Du J. Intratumoral neutrophil granulocytes contribute to epithelial-mesenchymal transition in lung adenocarcinoma cells. Tumour Biol. 2015;36:7789–7796. doi: 10.1007/s13277-015-3484-1. [DOI] [PubMed] [Google Scholar]
- 75.Min H., Sun X., Yang X., Zhu H., Liu J., Wang Y., Chen G., Sun X. Exosomes derived from irradiated esophageal carcinoma-infiltrating T cells promote metastasis by inducing the epithelial-mesenchymal transition in esophageal cancer cells. Pathol. Oncol. Res. 2018;24:11–18. doi: 10.1007/s12253-016-0185-z. [DOI] [PubMed] [Google Scholar]
- 76.Cohen E.N., Gao H., Anfossi S., Mego M., Reddy N.G., Debeb B., Giordano A., Tin S., Wu Q., Garza R.J., et al. Inflammation mediated metastasis: Immune induced epithelial-to-mesenchymal transition in inflammatory breast cancer cells. PLoS ONE. 2015;10:e0132710. doi: 10.1371/journal.pone.0132710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Goebel L., Grage-Griebenow E., Gorys A., Helm O., Genrich G., Lenk L., Wesch D., Ungefroren H., Freitag-Wolf S., Sipos B., et al. CD4+ T cells potently induce epithelial-mesenchymal-transition in premalignant and malignant pancreatic ductal epithelial cells-novel implications of CD4+ T cells in pancreatic cancer development. Oncoimmunology. 2015;4:e1000083. doi: 10.1080/2162402X.2014.1000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Santisteban M., Reiman J.M., Asiedu M.K., Behrens M.D., Nassar A., Kalli K.R., Haluska P., Ingle J.N., Hartmann L.C., Manjili M.H., et al. Immune-induced epithelial to mesenchymal transition in vivo generates breast cancer stem cells. Cancer Res. 2009;69:2887–2895. doi: 10.1158/0008-5472.CAN-08-3343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Koizumi M., Hiasa Y., Kumagi T., Yamanishi H., Azemoto N., Kobata T., Matsuura B., Abe M., Onji M. Increased B cell-activating factor promotes tumor invasion and metastasis in human pancreatic cancer. PLoS ONE. 2013;8:e71367. doi: 10.1371/journal.pone.0071367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Panni R.Z., Sanford D.E., Belt B.A., Mitchem J.B., Worley L.A., Goetz B.D., Mukherjee P., Wang-Gillam A., Link D.C., Denardo D.G., et al. Tumor-induced STAT3 activation in monocytic myeloid-derived suppressor cells enhances stemness and mesenchymal properties in human pancreatic cancer. Cancer Immunol. Immunother. 2014;63:513–528. doi: 10.1007/s00262-014-1527-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lo U.G., Pong R.C., Yang D., Gandee L., Hernandez E., Dang A., Lin C.J., Santoyo J., Ma S., Sonavane R., et al. IFN-γ-induced IFIT5 promotes epithelial-to-mesenchymal transition in prostate cancer via microRNA processing. Cancer Res. 2018 doi: 10.1158/0008-5472.CAN-18-2207. [DOI] [PubMed] [Google Scholar]
- 82.Lv N., Gao Y., Guan H., Wu D., Ding S., Teng W., Shan Z. Inflammatory mediators, tumor necrosis factor-α and interferon-γ, induce EMT in human PTC cell lines. Oncol. Lett. 2015;10:2591–2597. doi: 10.3892/ol.2015.3518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Li X.M., Wang J.R., Shen T., Gao S.S., He X.S., Li J.N., Yang T.Y., Zhang S., Gan W.J., Li J.M., et al. Nur77 deficiency in mice accelerates tumor invasion and metastasis by facilitating TNFα secretion and lowering CSF-1R expression. PLoS ONE. 2017;12:e0171347. doi: 10.1371/journal.pone.0171347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhu Y., Cheng Y., Guo Y., Chen J., Chen F., Luo R., Li A. Protein kinase D2 contributes to TNF-α-induced epithelial mesenchymal transition and invasion via the PI3K/GSK-3β/β-catenin pathway in hepatocellular carcinoma. Oncotarget. 2016;7:5327–5341. doi: 10.18632/oncotarget.6633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chuang M.J., Sun K.H., Tang S.J., Deng M.W., Wu Y.H., Sung J.S., Cha T.L., Sun G.H. Tumor-derived tumor necrosis factor-alpha promotes progression and epithelial-mesenchymal transition in renal cell carcinoma cells. Cancer Sci. 2008;99:905–913. doi: 10.1111/j.1349-7006.2008.00756.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sullivan N.J., Sasser A.K., Axel A.E., Vesuna F., Raman V., Ramirez N., Oberyszyn T.M., Hall B.M. Interleukin-6 induces an epithelial-mesenchymal transition phenotype in human breast cancer cells. Oncogene. 2009;28:2940–2947. doi: 10.1038/onc.2009.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rokavec M., Öner M.G., Li H., Jackstadt R., Jiang L., Lodygin D., Kaller M., Horst D., Ziegler P.K., Schwitalla S., et al. IL-6R/STAT3/miR-34a feedback loop promotes EMT-mediated colorectal cancer invasion and metastasis. J. Clin. Investig. 2014;124:1853–1867. doi: 10.1172/JCI73531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chen W., Gao Q., Han S., Pan F., Fan W. The CCL2/CCR2 axis enhances IL-6-induced epithelial-mesenchymal transition by cooperatively activating STAT3-Twist signaling. Tumour Biol. 2015;36:973–981. doi: 10.1007/s13277-014-2717-z. [DOI] [PubMed] [Google Scholar]
- 89.Miao J.W., Liu L.J., Huang J. Interleukin-6-induced epithelial-mesenchymal transition through signal transducer and activator of transcription 3 in human cervical carcinoma. Int. J. Oncol. 2014;45:165–176. doi: 10.3892/ijo.2014.2422. [DOI] [PubMed] [Google Scholar]
- 90.Colomiere M., Ward A.C., Riley C., Trenerry M.K., Cameron-Smith D., Findlay J., Ackland L., Ahmed N. Cross talk of signals between EGFR and IL-6R through JAK2/STAT3 mediate epithelial-mesenchymal transition in ovarian carcinomas. Br. J. Cancer. 2009;100:134–144. doi: 10.1038/sj.bjc.6604794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Asgeirsson K.S., Olafsdóttir K., Jónasson J.G., Ogmundsdóttir H.M. The effects of IL-6 on cell adhesion and E-cadherin expression in breast cancer. Cytokine. 1998;10:720–728. doi: 10.1006/cyto.1998.0349. [DOI] [PubMed] [Google Scholar]
- 92.Zhang Q., Liu S., Parajuli K.R., Zhang W., Zhang K., Mo Z., Liu J., Chen Z., Yang S., Wang A.R., et al. Interleukin-17 promotes prostate cancer via MMP7-induced epithelial-to-mesenchymal transition. Oncogene. 2017;36:687–699. doi: 10.1038/onc.2016.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang L., Ma R., Kang Z., Zhang Y., Ding H., Guo W., Gao Q., Xu M. Effect of IL-17A on the migration and invasion of NPC cells and related mechanisms. PLoS ONE. 2014;9:e108060. doi: 10.1371/journal.pone.0108060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhang L.M., Zhang Y., Fei C., Zhang J., Wang L., Yi Z.W., Gao G. Neutralization of IL-18 by IL-18 binding protein ameliorates bleomycin-induced pulmonary fibrosis via inhibition of epithelial-mesenchymal transition. Biochem. Biophys. Res. Commun. 2019;508:660–666. doi: 10.1016/j.bbrc.2018.11.129. [DOI] [PubMed] [Google Scholar]
- 95.Kawata M., Koinuma D., Ogami T., Umezawa K., Iwata C., Watabe T., Miyazono K. TGF-β-induced epithelial-mesenchymal transition of A549 lung adenocarcinoma cells is enhanced by pro-inflammatory cytokines derived from RAW 264.7 macrophage cells. J. Biochem. 2012;151:205–216. doi: 10.1093/jb/mvr136. [DOI] [PubMed] [Google Scholar]
- 96.Zhu L., Li X., Chen Y., Fang J., Ge Z. High-mobility group box 1: A novel inducer of the epithelial-mesenchymal transition in colorectal carcinoma. Cancer Lett. 2015;357:527–534. doi: 10.1016/j.canlet.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 97.Funamizu N., Hu C., Lacy C., Schetter A., Zhang G., He P., Gaedcke J., Ghadimi M.B., Ried T., Yfantis H.G., et al. Macrophage migration inhibitory factor induces epithelial to mesenchymal transition, enhances tumor aggressiveness and predicts clinical outcome in resected pancreatic ductal adenocarcinoma. Int. J. Cancer. 2013;132:785–794. doi: 10.1002/ijc.27736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yin J., Zeng F., Wu N., Kang K., Yang Z., Yang H. Interleukin-8 promotes human ovarian cancer cell migration by epithelial-mesenchymal transition induction in vitro. Clin. Transl. Oncol. 2015;17:365–370. doi: 10.1007/s12094-014-1240-4. [DOI] [PubMed] [Google Scholar]
- 99.Long X., Ye Y., Zhang L., Liu P., Yu W., Wei F., Ren X., Yu J. IL-8, a novel messenger to cross-link inflammation and tumor EMT via autocrine and paracrine pathways (Review) Int. J. Oncol. 2016;48:5–12. doi: 10.3892/ijo.2015.3234. [DOI] [PubMed] [Google Scholar]
- 100.Meng F., Li W., Li C., Gao Z., Guo K., Song S. CCL18 promotes epithelial-mesenchymal transition, invasion and migration of pancreatic cancer cells in pancreatic ductal adenocarcinoma. Int. J. Oncol. 2015;46:1109–1120. doi: 10.3892/ijo.2014.2794. [DOI] [PubMed] [Google Scholar]
- 101.Zhang L., Wang D., Li Y., Liu Y., Xie X., Wu Y., Zhou Y., Ren J., Zhang J., Zhu H., et al. CCL21/CCR7 axis contributed to CD133+ pancreatic cancer stem-like cell metastasis via EMT and Erk/NF-κB pathway. PLoS ONE. 2016;11:e0158529. doi: 10.1371/journal.pone.0158529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kai K., Iwamoto T., Zhang D., Shen L., Takahashi Y., Rao A., Thompson A., Sen S., Ueno N.T. CSF-1/CSF-1R axis is associated with epithelial/mesenchymal hybrid phenotype in epithelial-like inflammatory breast cancer. Sci. Rep. 2018;8:9427. doi: 10.1038/s41598-018-27409-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shintani Y., Fujiwara A., Kimura T., Kawamura T., Funaki S., Minami M., Okumura M. IL-6 secreted from cancer-associated fibroblasts mediates chemoresistance in NSCLC by increasing epithelial-mesenchymal transition signaling. J. Thorac. Oncol. 2016;11:1482–1492. doi: 10.1016/j.jtho.2016.05.025. [DOI] [PubMed] [Google Scholar]
- 104.Cheng X.S., Li Y.F., Tan J., Sun B., Xiao Y.C., Fang X.B., Zhang X.F., Li Q., Dong J.H., Li M., et al. CCL20 and CXCL8 synergize to promote progression and poor survival outcome in patients with colorectal cancer by collaborative induction of the epithelial-mesenchymal transition. Cancer Lett. 2014;348:77–87. doi: 10.1016/j.canlet.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 105.Sun K.H., Sun G.H., Wu Y.C., Ko B.J., Hsu H.T., Wu S.T. TNF-α augments CXCR2 and CXCR3 to promote progression of renal cell carcinoma. J. Cell. Mol. Med. 2016;20:2020–2028. doi: 10.1111/jcmm.12890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wu Y.C., Tang S.J., Sun G.H., Sun K.H. CXCR7 mediates TGFβ1-promoted EMT and tumor-initiating features in lung cancer. Oncogene. 2016;35:2123–2132. doi: 10.1038/onc.2015.274. [DOI] [PubMed] [Google Scholar]
- 107.Xu J., Lamouille S., Derynck R. TGF-beta-induced epithelial to mesenchymal transition. Cell Res. 2009;19:156–172. doi: 10.1038/cr.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Heldin C.H., Vanlandewijck M., Moustakas A. Regulation of EMT by TGFβ in cancer. FEBS Lett. 2012;586:1959–1970. doi: 10.1016/j.febslet.2012.02.037. [DOI] [PubMed] [Google Scholar]
- 109.David C.J., Massagué J. Contextual determinants of TGFβ action in development, immunity and cancer. Nat. Rev. Mol. Cell. Biol. 2018;19:419–435. doi: 10.1038/s41580-018-0007-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chen W., Jin W., Hardegen N., Lei K.J., Li L., Marinos N., McGrady G., Wahl S.M. Conversion of peripheral CD4 + CD25- naive T cells to CD4 + CD25 + regulatory T cells by TGF-beta induction of transcription factor Foxp3. J. Exp. Med. 2003;198:1875–1886. doi: 10.1084/jem.20030152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gorelik L., Constant S., Flavell R.A. Mechanism of transforming growth factor beta-induced inhibition of T helper type 1 differentiation. J. Exp. Med. 2002;195:1499–1505. doi: 10.1084/jem.20012076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kuwahara M., Yamashita M., Shinoda K., Tofukuji S., Onodera A., Shinnakasu R., Motohashi S., Hosokawa H., Tumes D., Iwamura C., et al. The transcription factor Sox4 is a downstream target of signaling by the cytokine TGF-beta and suppresses T(H)2 differentiation. Nat. Immunol. 2012;13:778–786. doi: 10.1038/ni.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tauriello D.V.F., Palomo-Ponce S., Stork D., Berenguer-Llergo A., Badia-Ramentol J., Iglesias M., Sevillano M., Ibiza S., Cañellas A., Hernando-Momblona X., et al. TGFβ drives immune evasion in genetically reconstituted colon cancer metastasis. Nature. 2018;554:538–543. doi: 10.1038/nature25492. [DOI] [PubMed] [Google Scholar]
- 114.Chen W., Ten Dijke P. Immunoregulation by members of the TGFβ superfamily. Nat. Rev. Immunol. 2016;16:723–740. doi: 10.1038/nri.2016.112. [DOI] [PubMed] [Google Scholar]
- 115.Zhang F., Wang H., Wang X., Jiang G., Liu H., Zhang G., Wang H., Fang R., Bu X., Cai S., et al. TGF-β induces M2-like macrophage polarization via SNAIL-mediated suppression of a pro-inflammatory phenotype. Oncotarget. 2016;7:52294–52306. doi: 10.18632/oncotarget.10561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Johansson J., Tabor V., Wikell A., Jalkanen S., Fuxe J. TGF-β1-induced epithelial-mesenchymal transition promotes monocyte/macrophage properties in breast cancer cells. Front. Oncol. 2015;5:3. doi: 10.3389/fonc.2015.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Miyazaki T., Ikeda K., Sato W., Horie-Inoue K., Inoue S. Extracellular vesicle-mediated EBAG9 transfer from cancer cells to tumor microenvironment promotes immune escape and tumor progression. Oncogenesis. 2018;7:7. doi: 10.1038/s41389-017-0022-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hübel J., Hieronymus T. HGF/Met-signaling contributes to immune regulation by modulating tolerogenic and motogenic properties of dendritic cells. Biomedicines. 2015;3:138–148. doi: 10.3390/biomedicines3010138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Brabletz T., Jung A., Hlubek F., Löhberg C., Meiler J., Suchy U., Kirchner T. Negative regulation of CD4 expression in T cells by the transcriptional repressor ZEB. Int. Immunol. 1999;11:1701–1708. doi: 10.1093/intimm/11.10.1701. [DOI] [PubMed] [Google Scholar]
- 120.Wang J., Lee S., The C.E., Binting K., Ma L., Shannon M.F. The transcription repressor, ZEB1, cooperates with CtBP2 and HDAC1 to suppress IL-2 gene activation in T cells. Int. Immunol. 2009;21:227–235. doi: 10.1093/intimm/dxn143. [DOI] [PubMed] [Google Scholar]
- 121.Genetta T., Ruezinsky D., Kadesch T. Displacement of an E-box-binding repressor by basic helix-loop-helix proteins: Implications for B-cell specificity of the immunoglobulin heavy-chain enhancer. Mol. Cell Biol. 1994;14:6153–6163. doi: 10.1128/MCB.14.9.6153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lyons J.G., Patel V., Poue N.C., Fok S.Y., Soon L.L., Halliday G.M., Gutkind J.S. Snail up-regulates proinflammatory mediators and inhibits differentiation in oral keratinocytes. Cancer Res. 2008;68:4525–4530. doi: 10.1158/1078-0432.CCR-07-6735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Black A.P., Ardern-Jones M.R., Kasprowicz V., Bowness P., Jones L., Bailey A.S., Ogg G.S. Human keratinocyte induction of rapid effector function in antigen-specific memory CD4+ and CD8+ T cells. Eur. J. Immunol. 2007;37:1485–1493. doi: 10.1002/eji.200636915. [DOI] [PubMed] [Google Scholar]
- 124.Konradi S., Yasmin N., Haslwanter D., Weber M., Gesslbauer B., Sixt M., Strobl H. Langerhans cell maturation is accompanied by induction of N-cadherin and the transcriptional regulators of epithelial-mesenchymal transition ZEB1/2. Eur. J. Immunol. 2014;44:553–560. doi: 10.1002/eji.201343681. [DOI] [PubMed] [Google Scholar]
- 125.Postigo A.A., Dean D.C. Independent repressor domains in ZEB regulate muscle and T-cell differentiation. Mol. Cell Biol. 1999;19:7961–7971. doi: 10.1128/MCB.19.12.7961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Omilusik K.D., Best J.A., Yu B., Goossens S., Weidemann A., Nguyen J.V., Seuntjens E., Stryjewska A., Zweier C., Roychoudhuri R., et al. Transcriptional repressor ZEB2 promotes terminal differentiation of CD8+ effector and memory T cell populations during infection. J. Exp. Med. 2015;212:2027–2039. doi: 10.1084/jem.20150194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.van Helden M.J., Goossens S., Daussy C., Mathieu A.L., Faure F., Marçais A., Vandamme N., Farla N., Mayol K., Viel S., et al. Terminal NK cell maturation is controlled by concerted actions of T-bet and Zeb2 and is essential for melanoma rejection. J. Exp. Med. 2015;212:2015–2025. doi: 10.1084/jem.20150809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Colak S., Ten Dijke P. Targeting TGF-β signaling in cancer. Trends Cancer. 2017;3:56–61. doi: 10.1016/j.trecan.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 129.Hamilton D.H., Litzinger M.T., Jales A., Huang B., Fernando R.I., Hodge J.W., Ardiani A., Apelian D., Schlom J., Palena C. Immunological targeting of tumor cells undergoing an epithelial-mesenchymal transition via a recombinant brachyury-yeast vaccine. Oncotarget. 2013;4:1777–1790. doi: 10.18632/oncotarget.1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Marcucci F., Rumio C., Lefoulon F. Anti-cancer stem-like cell compounds in clinical development – An overview and critical appraisal. Front. Oncol. 2016;6:115. doi: 10.3389/fonc.2016.00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Marcucci F., Caserta C.A., Romeo E., Rumio C. Antibody-drug conjugates (ADC) against cancer stem-like cells (CSC)—Is there still room for optimism? Front. Oncol. 2019;9:167. doi: 10.3389/fonc.2019.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Marcucci F., Corti A. Improving drug penetration to curb tumor drug resistance. Drug Discov. Today. 2012;17:1139–1147. doi: 10.1016/j.drudis.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 133.Ribas A., Wolchok J.D. Cancer immunotherapy using checkpoint blockade. Science. 2018;359:1350–1355. doi: 10.1126/science.aar4060. [DOI] [PMC free article] [PubMed] [Google Scholar]