Abstract
Background:
Anxiety disorder (AD) and substance use disorder (SUD) highly co-occur with bipolar disorder (BD). AD and/or SUD co-occurrence is associated with poorer clinical outcomes in BD. However, respective associations between AD and/or SUD diagnoses and BD outcomes require clarification. Baseline data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) were therefore utilized to investigate independent and simultaneous contributions of ADs and SUDs on clinical variables in BD.
Methods:
Two latent factors, “pathological anxiety” and “substance use problems,” were derived from presence/absence of lifetime AD and SUD diagnoses. Latent dimensions’ associations with clinical variables, obtained from the Affective Disorders Evaluation, Mini-International Neuropsychiatric Interview and Range of Impaired Functioning, were estimated via structural equation modeling (SEM).
Results:
Modeled independently, pathological anxiety and substance use problems were significantly associated with several variables. Yet when modeled simultaneously, pathological anxiety’s associations with functional impairment, past-year rapid cycling, and past-year %time spent anxious and depressed remained while most variables’ associations with substance use problems became non-significant. The only significant latent- factor interaction evidenced was for age of BD onset.
Limitations:
Analyses were limited to lifetime diagnoses and causality may not be inferred given cross-sectional data.
Conclusions:
ADs and SUDs impact on BD was mostly additive rather than synergistic. Findings highlight the potentially understated importance of treating inter-episodic anxiety in BD as it may exacerbate mood symptoms, increasing functional impairment and risk for subsequent mood episodes.
Keywords: bipolar disorder, clinical outcomes, anxiety, substance dependence, structural equation modeling, STEP-BD
1. Introduction
Psychiatric disorder co-occurrence is the norm rather than the exception in bipolar disorder (BD) (Bauer et al., 2005; McElroy et al., 2001). In fact, approximately 65 to 92% of BD individuals will meet lifetime diagnostic criteria for an additional axis I disorder(s) (McElroy et al., 2001; Merikangas et al., 2007). Lifetime anxiety disorder (AD) and substance use disorder (SUD) are the most common co-occurring psychiatric disorders in BD (Boylan et al., 2004; Cassidy et al., 2001; Goldstein and Levitt, 2008). Despite the high prevalence of AD and/or SUD in BD, there remains a continued need for novel investigations of their impact on bipolar illness. Clarification of respective associations between AD, SUD, and BD outcomes may inform understanding of BD’s etiology and course while potentially providing insight for targeted intervention.
It is known that AD and/or SUD co-occurrence in BD is associated with significantly poorer clinical outcomes versus BD alone (Farren et al., 2012; Pavlova et al., 2015). BD and co- occurring AD (BD+AD) is associated with earlier age of BD onset, increased rapid cycling, greater symptom severity and persistence, greater functional impairment across a range of life domains, increased substance abuse, and increased risk for attempted suicide (Gao et al., 2010; Hawke et al., 2013; Simon et al., 2004; Thibodeau et al., 2013). Similarly, co-occurring SUD in BD (BD+SUD) is associated with earlier age of BD onset, greater functional impairment, and history of attempted suicide (Farren et al., 2012; Ongür et al., 2009; Oquendo et al., 2010). While these findings are convergent and compelling, an important limitation is that independent associations between AD, SUD, and BD clinical outcomes have been examined without accounting for concomitant associations between AD and SUD. This is problematic because associations between SUD and BD outcomes may have been spuriously produced by unaccounted for associations with AD and vice versa. Moreover, the impact of AD on SUD trajectory or the impact of SUD on AD trajectory in people with BD remains unclear.
Only two known studies examined simultaneous associations between lifetime AD and SUD diagnoses and clinical outcomes in BD; both employed multiple regression approaches with cross-sectional data (Bauer et al., 2005; Goldstein and Levitt, 2008). Bauer and colleagues (2005) examined lifetime co-occurring AD and SUD associations with age of BD onset, number of past-year episodes (depressive, manic, or mixed), mental and physical component scores (MCS and PCS, respectively), and general assessment scores (GAS). Lifetime AD was significantly associated with lower MCS scores while lifetime SUD was unassociated with any of the aforementioned predictors. Lifetime AD+SUD significantly associated with earlier age of BD onset, and lower MCS, PCS, and GAS scores. The other study, by Goldstein and Levitt (2008), examined lifetime prevalence of mixed mania (presence or absence), prolonged mood episodes, forensic history, 12-month prevalence of mania and depression, BD-related treatment utilization, and general mental-health functioning as outcomes. Lifetime AD significantly associated with prolonged depressive episodes and 12-month prevalence of depression, mixed episodes, BD-related treatment utilization, and worse general mental health functioning. Additionally, lifetime SUD was significantly associated with forensic history. Taken together, lifetime co-occurring AD (±SUD) may be more associated cross-sectionally with negative clinical variables in BD.
The statistical approaches employed by Bauer and colleagues (2005) and Goldstein and Levitt (2008) allow for more accurate estimates of the unique effects of each co-occurring disorder on BD clinical variables. However, both studies analyzed ADs and SUDs broadly rather than as specific DSM diagnoses, examining the presence or absence of any AD or SUD diagnosis, thereby reducing statistical power to detect effects between co-occurring disorders. Moreover, this approach assumes multiple ADs and/or SUDs have similar clinical variable outcomes as single AD and/or SUD diagnoses in BD, which is unlikely (Sala et al., 2014). Also, a limited range of ADs were considered in each of these studies.
The present manuscript utilized baseline data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) (Sachs et al., 2003) to investigate cross-sectional independent and simultaneous contributions of lifetime ADs and SUDs on BD clinical variables. A structural equation modeling (SEM) statistical framework was employed which accounted for the presence of multiple co-occurring ADs and SUDs; simultaneously modeling the impact of ADs and SUDs on clinical variables while minimizing measurement error. Clinical variables (beyond age of BD onset, functional impairment, and legal problem history) included: suicide attempt history, history of violence, rapid cycling, and past-year %time spent irritable and %time spent anxious as well as %time elevated and %time depressed. Rapid cycling and %time spent symptomatic variables were specifically selected because of their associations with negative clinical outcomes including reduced responsiveness to treatment (Blanco et al., 2014; Goldstein and Levitt, 2007; Tondo and Baldessarini, 1998).
2. Methods
2.1. Participants and procedures
STEP-BD was a multi-site longitudinal study that evaluated clinical outcomes in a large cohort of outpatients with BD (Sachs et al., 2003). Individuals meeting DSM-IV criteria for BD at the 21-plus participating sites were eligible to participate. Exclusion criteria were minimal: non-desire or inability to provide consent and/or complete study assessments, and/or inpatient detoxification required upon enrollment (Kogan et al., 2004). Participants provided written informed consent, and 15–17 year-old participants provided parental assent, prior to completing baseline assessments.
2.2. Measures
Bipolar diagnoses, along with most clinical variables of interest (i.e., age of bipolar disorder onset [patient’s report of age of first (hypo)manic episode], lifetime history of suicide attempt, violence, or legal problems, past-year rapid cycling [total number of past-year (hypo)manic or depressive episodes ≥ 4], and past-year %time [percentage of days] spent depressed, elevated, irritable, or anxious) were assessed via the Affective Disorders Evaluation (Sachs, 1990), a semi-structured assessment including the mood/psychosis modules of the Structured Clinical Interview for DSM-IV (First et al., 1995); lifetime comorbid Axis I diagnoses (including PD, agoraphobia, SP, obsessive compulsive disorder [OCD], posttraumatic stress disorder [PTSD], GAD, alcohol abuse, alcohol dependence, drug abuse, and drug dependence; presence or absence of particular drug use disorders [e.g., cocaine versus opiate use disorder] was not available) were assessed using the Mini-International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998). Functional impairment in work, recreational activity, interpersonal relations, and overall satisfaction was assessed via the clinician/rater-administered Range of Impaired Functioning Tool (LIFE-RIFT) (Leon et al., 1999). A maximum sample of 4,107 individuals was available from baseline STEP-BD data, however effective sample sizes varied slightly across analyses due to missing data. 80% of tested statistical models had <1.5% missing data; in contrast, models involving past-year rapid cycling and LIFE-RIFT had <3% and 7% missing data, respectively. Taken together, missing data reflected a very small proportion of total data suggesting results would yield similar inferences withstanding.
2.3. Analytic Strategy
Latent variable models were estimated in a logistic modeling framework, with study center entered as a clustering variable, using maximum likelihood with robust standard errors in MPlus 6.11 (Muthén and Muthén, 1998–2011). A two-factor model of “pathological anxiety” and “substance use problems” represented by binary (0=absent, 1=present) lifetime diagnoses of panic disorder (PD), agoraphobia, social phobia (SP), OCD, PTSD, and generalized anxiety disorder (GAD) and alcohol abuse, alcohol dependence, drug abuse and drug dependence, respectively, was estimated. Latent factors were free to covary and factor loadings were freely estimated, with factor variances fixed to “1.” Item response theory (IRT) discrimination and difficulty/severity parameters were calculated per Muthén and Muthén (Muthén and Muthén, 2010). Discrimination parameters are conceptually equivalent to factor loadings whereas difficulty parameters indicate the severity level on a latent factor (e.g., pathological anxiety) at which an individual has a 50% of receiving a disorder diagnosis. Associations between latent factors and the 10 clinical variables of interest (age of BD onset, lifetime history of suicide, violence, or legal problems, past-year rapid cycling, past-year %time spent depressed, elevated, irritable, or anxious, and functional impairment [across life domains; i.e., social relationships, work/school, and recreational activity]) were each estimated via separate SEMs using a model building approach. First, models were estimated with each latent variable individually predicting each clinical variable to ascertain zero-order associations between pathological anxiety, substance use problems, and clinical variables. Next, models were estimated with both latent variables simultaneously predicting each clinical variable to demonstrate how zero-order associations between latent variables and clinical variables changed when both latent variables were modeled simultaneously. Finally, a third set of models tested simultaneous latent variables as well as their interaction predicting each clinical variable to evaluate whether latent variables’ associations varied depending on levels of substance use problems and vice versa (Klein and Moosbrugger, 2000). Interaction models were retained and probed only if they provided superior parsimony-adjusted fit to the data (indicated by a smaller Bayesian Information Criterion; BIC) (Schwarz, 1978) relative to non-interaction models. Interaction models that significantly improved parsimony-adjusted model fit (ΔBIC > 10) (Raftery, 1995) were probed with simple slopes (Preacher et al., 2006). Across models, associations between latent variables and binary and continuous clinical variables were represented by odds ratios and standardized betas, respectively.
3. Results
See Table 1 for observed frequencies of anxiety and substance use disorders as well as parameters from the two-factor logistic model of “pathological anxiety” and “substance use problems.” Forty-three point one percent of participants were without an AD diagnosis, 49.6% were without an SUD diagnosis, and 25.3% had neither an AD nor SUD diagnosis. Lifetime prevalence of ADs ranged from 11.6% (OCD) to 22.8% (GAD) and lifetime prevalence of SUDs ranged from 19.6% (drug dependence) to 34.1% (alcohol abuse). On average, participants had1.19 (SD = 1.39) lifetime ADs and 1.06 (SD = 1.28) SUDs. In the two-factor logistic model of lifetime ADs and SUDs, agoraphobia (standardized loading = 0.94) and drug dependence (standardized loading = 0.85) were most strongly associated with the latent factors. Relative to other diagnoses, OCD (difficulty = 2.72) and drug dependence (difficulty = 0.99) indicated the most severe levels of pathological anxiety and substance use problems, respectively. Latent factors were moderately intercorrelated (r = 0.32, p < 0.001).
Table 1.
Observed frequencies of anxiety and substance disorders and results from a two-factor logistic model of “Pathological Anxiety” and “Substance Use Problems.”
| Axis I Disorder | Freq (%) | Std Loading | Discrimination | Difficulty |
|---|---|---|---|---|
| Factor 1:“Pathological Anxiety” | ||||
| Panic Disorder | 22.0 | 0.82 | 1.53 | 0.93 |
| Agoraphobia | 20.5 | 0.94 | 3.04 | 0.87 |
| Social Phobia | 22.3 | 0.54 | 0.69 | 1.34 |
| PTSD | 20.1 | 0.46 | 0.56 | 1.70 |
| GAD | 22.8 | 0.39 | 0.45 | 1.77 |
| OCD | 11.6 | 0.42 | 0.49 | 2.72 |
| Factor 2: “Substance Use Problems” | ||||
| Alcohol Abuse | 34.1 | 0.68 | 0.98 | 0.59 |
| Alcohol Dependence | 28.4 | 0.72 | 1.09 | 0.78 |
| Drug Abuse | 24.2 | 0.84 | 1.66 | 0.83 |
| Drug Dependence | 19.6 | 0.85 | 1.74 | 0.99 |
Note. Freq = Frequency; Std = Standardized; PTSD = Posttraumatic Stress Disorder; GAD = Generalized Anxiety Disorder; OCD = Obsessive Compulsive Disorder
See Table 2 for SEM results involving associations between latent factors, both individually and simultaneously, and clinical variables of interest. When evaluated separately, substance use problems significantly predicted all clinical variables and pathological anxiety significantly predicted all clinical variables except legal problem history. When evaluated simultaneously, pathological anxiety continued to predict all clinical variables with the exception of history of legal problems. In contrast, formerly significant associations between substance use problems and several clinical variables were no longer significant once levels of pathological anxiety were statistically controlled. This pattern of associations suggests substance use problems were only associated with past-year rapid cycling, functional impairment, and past-year %time spent depressed or anxious due to their association with pathological anxiety.
Table 2.
Associations between “Pathological Anxiety,” “Substance Use Problems,” and clinical variables from separate and simultaneous SEM models.
| Separate Models | Simultaneous Model | |||||||
|---|---|---|---|---|---|---|---|---|
| “Pathological Anxiety” | “Substance Use Problems” | “Pathological Anxiety” | “Substance Use Problems” | |||||
| Outcome | OR/β | p | OR/β | p | OR/β | p | OR/β | p |
| Categorical (OR) | ||||||||
| Hx Suicide | 1.75 | <.001 | 1.43 | <.001 | 1.65 | <.001 | 1.24 | <.001 |
| Hx Violence | 1.55 | 0.001 | 1.93 | <.001 | 1.32 | 0.037 | 1.78 | <.001 |
| Hx Legal Problems | 1.14 | 0.354 | 1.78 | <.001 | 0.96 | 0.790 | 1.80 | <.001 |
| Rapid Cycling | 1.81 | <.001 | 1.36 | 0.003 | 1.74 | <.001 | 1.14 | 0.145 |
| Continuous (β) | ||||||||
| Age of BD onset | −0.29 | <.001 | −0.24 | <.001 | −0.24 | <.001 | −0.16 | <.001 |
| Functional impairment | 0.30 | <.001 | 0.13 | <.001 | 0.29 | <.001 | 0.04 | 0.311 |
| % depressed | 0.30 | <.001 | 0.10 | <.001 | 0.30 | <.001 | 0.01 | 0.754 |
| % elevated | 0.12 | <.001 | 0.14 | <.001 | 0.09 | 0.018 | 0.11 | <.001 |
| % irritable | 0.28 | <.001 | 0.15 | <.001 | 0.27 | <.001 | 0.06 | 0.004 |
| % anxious | 0.41 | <.001 | 0.11 | <.001 | 0.42 | <.001 | −0.02 | 0.506 |
Note. SEM = Structural Equation Modeling; Hx = History of.
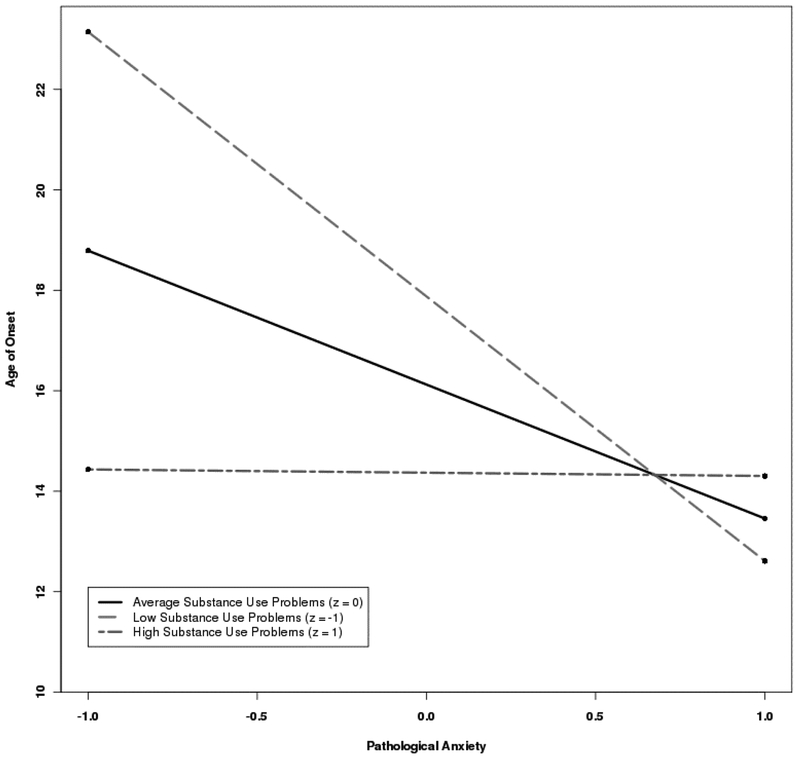
For all clinical variables except age of BD onset and functional impairment, BIC values were larger (indicating poorer parsimony-adjusted fit) for models featuring latent factor interaction terms versus models without such interaction terms. For functional impairment, BIC was smaller for the interaction model; however, the difference between models was minimal (ΔBIC = 2.53). In contrast, for age of BD onset (interaction OR = 2.60, p < 0.001) BIC values suggested significantly improved parsimony-adjusted fit for the interaction model (BIC = 63120.94) versus the non-interaction model (BIC = 63293.52; ΔBIC = 172.58). Simple slopes analyses demonstrated that pathological anxiety was significantly associated with age of BD onset at average (t = −12.86, p < 0.001) and 1 SD below average (t = −12.66, p < 0.001) levels of substance use problems but not at 1 SD above average (t = −0.16, p = 0.87) levels of substance use problems (see Figure 1 for a plot of these results). This pattern of simple slopes suggests the presence of increased levels of substance use problems substantially reduced the magnitude of the association between pathological anxiety and age of BD onset.
Figure 1.
Pathological anxiety predicting age of BD onset, moderated by substance use problems
Note. Age of onset in years; Pathological anxiety factor represented by binary lifetime diagnoses of PD, agoraphobia, SP, OCD, PTSD, and GAD; Substance use problems factor represented by lifetime diagnoses of alcohol abuse, alcohol dependence, drug abuse, and drug dependence; Factor severity standardized with z-scores: high (+ 1 SD), low (−1 SD), with a mean of 0.
4. Discussion
The present manuscript investigated associations between lifetime ADs, SUDs, and a range of important clinical variables collected through STEP-BD. SEM was used to examine individual and simultaneous associations between latent factors of lifetime ADs and SUDs and clinical BD variables. Modeled individually, substance use problems and pathological anxiety were each associated with most clinical variables of interest. However, when modeled simultaneously, pathological anxiety’s associations with clinical variables remained while many but not all (e.g., past suicide attempts) of clinical variable associations with substance use problems diminished. This echoes Bauer and colleagues (2005) and Goldstein and Levitt (2008) who found ADs, rather than SUDs, to be predominantly associated with cross-sectional clinical variables in BD. The pattern of findings may suggest that individuals with BD, who also have substance use problems, may only have elevated past-year rapid cycling, functional impairment, and past-year %time spent with depressive and anxious symptomatology due to co-occurring elevations in pathological anxiety.
Modern conceptualizations of BD highlight the role that inter-episodic residual depressive and/or (hypo)manic symptoms play in clinical outcomes and treatment response (Fagiolini et al., 2013). However, in BD (+AD, +SUD, or +AD+SUD), anxiety symptoms may also persist inter-episode (Blanco et al., 2014), exacerbating mood symptoms and increasing risk for subsequent mood episodes; an interplay suggested by the unique association between pathological anxiety and past-year rapid cycling. This association, along with others found, align with research demonstrating co-occurring AD(s), rather than SUD(s), relate more prospective depressive and (hypo)manic episodes, prolonged depressive periods, and worse general mental health functioning in BD (Goldstein and Levitt, 2007, 2008).
Interestingly, pathological anxiety rather than substance use problems retained sole statistical significance associating with functional impairment. Though perhaps counterintuitive, this is consistent with general psychiatric comorbidity (sans SUD) being associated with more functional impairment compared to SUDs in isolation (Johnson et al., 1995). Increased functional impairment in social support, work, and finances in BD+AD(s) compared to BD without AD(s) has been demonstrated which may be due to the aforementioned interactions between anxiety, depressive, and/or (hypo)manic symptoms (Boylan et al., 2004; Sala et al., 2014).
The present study also demonstrated that the impact of substance use problems and pathological anxiety on clinical variables was primarily additive as opposed to multiplicative or synergistic. The sole variable deviating from this finding was age of BD onset. Pathological anxiety only significantly associated with age of BD onset given low-moderate levels of substance use problems. Inferences from this finding, as with others, are tempered since temporal relations between AD(s), SUD(s), and age of BD onset are unclear, leaving the proverbial chicken or the egg causality dilemma.
Several studies show ADs to predict BD onset (Meier et al., 2016; Sala et al., 2012b) with several potential explanations for this relationship. One reason may simply be a function of AD age of onset as some of the modeled ADs in the present study (Social Phobia and OCD, specifically) often emerge in late-childhood or adolescence prior to average age of BD onset (American Psychiatric Association, 2013). Therefore, anxiety symptoms could precede mood episodes and/or substance use in some study participants. With respect to moderation findings, assuming low-to-moderate substance use problems, AD(s) may negatively influence the expression of prodromal unipolar or bipolar depression symptoms. Perhaps shared mechanistic features of AD(s), SUD(s), and BD results in the expression of anxiety symptoms first. To this end, pharmacological treatment of AD(s) prior to BD onset, such as selective serotonin reuptake inhibitors (SSRIs) or benzodiazepines, may in fact increase risk for BD onset among vulnerable individuals by triggering or destabilizing early symptoms of BD (Provencher et al., 2012; Sala et al., 2012a). At-risk individuals also may have a propensity for developing substance use problems. To this end, a strong interplay between pathological anxiety, substance use, and prodromal symptoms could occur thereby diminishing pathological anxiety’s influence on BD onset.
“Self-medicating” with illicit substances may occur prior to the frank onset of BD. Heavy substance use is known to reorganize neural circuity through neurotransmitter-mediated (i.e., glutamate and y-aminobutyric acid [GABA]) neuroplasticity (Kalivas and O’Brien, 2008). Recent magnetic resonance spectroscopy findings implicate abnormally low levels of prefrontal GABA and glutamate in individuals with co-occurring BD and alcohol dependence, compared to BD or alcohol dependence alone, which the authors suggest may be due to alcohol dependence’s modification of the effects of BD on these neurotransmitter concentrations (Prisciandaro et al., 2017). How and whether such mechanisms increase risk for BD in predisposed individuals with SUD(s) remains to be precisely determined, yet these findings and others suggest further investigation is warranted (Freeman et al., 2002). These considerations aside, the interaction between substance use problems and pathological anxiety implies a threshold between these factors determining their respective contributions to age of BD onset. From a statistical standpoint, given both latent factors were uniquely associated with age of BD onset, and age of onset naturally has a limited lower boundary, individuals whom developed severe substance use problems may have eclipsed said boundary and therefore pathological anxiety cannot drive age of onset down further.
The present study benefits from notable strengths resulting from the rigorousness of data collection paired with the statistical methods employed. Nevertheless, there are limitations worth noting. Although current diagnoses were available in STEP-BD data, lifetime diagnoses were chosen because the authors thought them more relevant to clinical outcome measurement. Current diagnoses would be redundant with past-year outcomes. Bipolar spectrum disorders were examined collectively despite that there may be unique pathological anxiety and substance use effects within BD subtypes (Albert et al., 2008; Chengappa et al., 2000). Finally, data were cross-sectional and the statistical approach also prohibits direct causal inferences to be made though it does make them more tenable (Bollen and Pearl, 2013). Future longitudinal or prospective studies are therefore required to substantiate present cross-sectional findings before making meaningful inferences with respect to causality. Although there has been growing scientific interest in BD+AD in recent decades it seems to have reached a plateau. There remains a critical need for more systematic studies examining anxiety across bipolar mood states, exploration of overlapping pathophysiological mechanisms, and controlled psychotherapy treatment studies targeting co-occurring anxiety symptoms (and syndromes) in BD. The latter point is especially concerning since effective treatment of co-occurring anxiety in BD remains to be such a critically unmet need (Ellard et al., 2012).
Relatively new psychotherapies with demonstrated efficacy, such as the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP) (Ellard et al., 2010; Farchione et al., 2012) which is specifically designed to target core processes underlying bipolar mood and anxiety disorders, may help address this gap. In hope, the present manuscript provides further impetus for a resurgence of BD+AD investigations and the development and empirical evaluation of more novel treatments for improved BD outcomes.
Supplementary Material
Highlights.
Anxiety (AD) and/or substance use disorders (SUD) are common in bipolar disorder
Unique and joint AD and SUD contributions to bipolar disorder outcomes were tested
AD and SUD solely interacted in association with age of bipolar disorder onset
SUD was associated with some outcomes but mostly only in the presence of AD
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
On behalf of all authors, the corresponding author reports no conflicts of interest.
References
- Albert U, Rosso G, Maina G, Bogetto F, 2008. Impact of anxiety disorder comorbidity on quality of life in euthymic bipolar disorder patients: differences between bipolar I and II subtypes. J. Affect. Disord 105, 297- [DOI] [PubMed] [Google Scholar]
- Association, A.P., 2013. Diagnostic and statistical manual of mental disorders (DSM-5®).American Psychiatric Pub. [DOI] [PubMed] [Google Scholar]
- Bauer MS, Altshuler L, Evans DR, Beresford T, Williford WO, Hauger R, Team VCS, 2005. Prevalence and distinct correlates of anxiety, substance, and combined comorbidity in a multi-site public sector sample with bipolar disorder. J. Affect. Disord 85, 301–315. [DOI] [PubMed] [Google Scholar]
- Blanco P, Guglielmo R, Righino E, 2014. Comorbidity of affective disorders, alcohol use, and gambling, New perspectives on generalized anxiety disorder, pp. 95–105. [Google Scholar]
- Bollen KA, Pearl J, 2013. Eight myths about causality and structural equation models. Springer, Dordecht, Handbook of causal analysis for social research, pp. 301–328. [Google Scholar]
- Boylan KR, Bieling PJ, Marriott M, Begin H, Young LT, MacQueen GM, 2004. Impact of comorbid anxiety disorders on outcome in a cohort of patients with bipolar disorder. J. Clin. Psychiatry 65, 1106–1113. [DOI] [PubMed] [Google Scholar]
- Cassidy F, Ahearn EP, Carroll BJ, 2001. Substance abuse in bipolar disorder. Bipolar Disord 3, 181–188. [PubMed] [Google Scholar]
- Chengappa KN, Levine J, Gershon S, Kupfer DJ, 2000. Lifetime prevalence of substance or alcohol abuse and dependence among subjects with bipolar I and II disorders in a voluntary registry. Bipolar Disord 2, 191–195. [DOI] [PubMed] [Google Scholar]
- Ellard KK, Deckersbach T, Sylvia LG, Nierenberg AA, Barlow DH, 2012. Transdiagnostic treatment of bipolar disorder and comorbid anxiety with the unified protocol: a clinical replication series. Behav. Modif 36, 482–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH, 2010. Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cogn. Behav. Pract 17, 88–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagiolini A, Forgione R, Maccari M, Cuomo A, Morana B, Dell’Osso MC, Pellegrini F, Rossi A, 2013. Prevalence, chronicity, burden and borders of bipolar disorder. J. Affect. Disord 148, 161–169. [DOI] [PubMed] [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, Gallagher MW, Barlow DH, 2012. Unified protocol for transdiagnostic treatment of emotional disorders: a randomized controlled trial. Behav. Ther 43, 666–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farren CK, Hill KP, Weiss RD, 2012. Bipolar disorder and alcohol use disorder: a review. Curr Psychiatry Rep 14, 659–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon MW, Williams JB, 1995. Structured clinical interview for DSM-IV axis I disorders New York State Psychiatric Institute, New York. [Google Scholar]
- Freeman MP, Freeman SA, McElroy SL, 2002. The comorbidity of bipolar and anxiety disorders: prevalence, psychobiology, and treatment issues. J. Affect. Disord 68, 1–23. [DOI] [PubMed] [Google Scholar]
- Gao K, Chan PK, Verduin ML, Kemp DE, Tolliver BK, Ganocy SJ, Bilali S, Brady KT, Findling RL, Calabrese JR, 2010. Independent predictors for lifetime and recent substance use disorders in patients with rapid-cycling bipolar disorder: focus on anxiety disorders. Am. J. Addict 19, 440–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein BI, Levitt AJ, 2007. Prevalence and correlates of bipolar I disorder among adults with primary youth-onset anxiety disorders. J. Affect. Disord 103, 187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein BI, Levitt AJ, 2008. The specific burden of comorbid anxiety disorders and of substance use disorders in bipolar I disorder. Bipolar Disord 10, 67–78. [DOI] [PubMed] [Google Scholar]
- Hawke LD, Provencher MD, Parikh SV, Zagorski B, 2013. Comorbid anxiety disorders in Canadians with bipolar disorder: clinical characteristics and service use. Can. J. Psychiatry 58, 393–401. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Spitzer RL, Williams JB, Kroenke K, Linzer M, Brody D, deGruy F,Hahn S, 1995. Psychiatric comorbidity, health status, and functional impairment associated with alcohol abuse and dependence in primary care patients: findings of the PRIME MD-1000 study. J. Consult. Clin. Psychol 63, 133–140. [DOI] [PubMed] [Google Scholar]
- Kalivas PW, O’Brien C, 2008. Drug addiction as a pathology of staged neuroplasticity.Neuropsychopharmacology 33, 166–180. [DOI] [PubMed] [Google Scholar]
- Klein A, Moosbrugger H, 2000. Maximum likelihood estimation of latent interaction effects with the LMS method. Psychometrika, pp. 457–474. [Google Scholar]
- Kogan JN, Otto MW, Bauer MS, Dennehy EB, Miklowitz DJ, Zhang HW, Ketter T,Rudorfer MV, Wisniewski SR, Thase ME, 2004. Demographic and diagnostic characteristics of the first 1000 patients enrolled in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Bipolar Disorders 6, 460–469. [DOI] [PubMed] [Google Scholar]
- Leon AC, Solomon DA, Mueller TI, Turvey CL, Endicott J, Keller MB, 1999. The Range of Impaired Functioning Tool (LIFE-RIFT): a brief measure of functional impairment. Psychological Medicine, pp. 869–878. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Altshuler LL, Suppes T, Keck PE, Frye MA, Denicoff KD, Nolen WA, Kupka RW, Leverich GS, Rochussen JR, Rush AJ, Post RM, 2001. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am. J. Psychiatry 158, 420–426. [DOI] [PubMed] [Google Scholar]
- Meier SM, Uher R, Mors O, Dalsgaard S, Munk-Olsen T, Laursen TM, Mattheisen M,Nordentoft M, Mortensen PB, Pavlova B, 2016. Specific anxiety disorders and subsequent risk for bipolar disorder: a nationwide study. World Psychiatry 15, 187–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M,Kessler RC, 2007. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch. Gen. Psychiatry 64, 543–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO, 1998–2011. Mplus User’s Guide, Sixth Edition ed. Muthén & Muthén, Los Angeles, CA. [Google Scholar]
- Muthén LK, Muthén BO, 2010. Mplus: Statistical analysis with latent variables: User’s guide Muthén & Muthén, Los Angeles. [Google Scholar]
- Ongür D, Lin L, Cohen BM, 2009. Clinical characteristics influencing age at onset in psychotic disorders. Compr. Psychiatry 50, 13–19. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Currier D, Liu SM, Hasin DS, Grant BF, Blanco C, 2010. Increased risk for suicidal behavior in comorbid bipolar disorder and alcohol use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J. Clin. Psychiatry 71, 902–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlova B, Perlis RH, Alda M, Uher R, 2015. Lifetime prevalence of anxiety disorders in people with bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry 2, 710–717. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ, 2006. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of educational and behavioral statistics, pp. 437–448. [Google Scholar]
- Prisciandaro JJ, Tolliver BK, Prescot AP, Brenner HM, Renshaw PF, Brown TR,Anton RF, 2017. Unique prefrontal GABA and glutamate disturbances in co-occurring bipolar disorder and alcohol dependence. Transl Psychiatry 7, e1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provencher MD, Guimond AJ, Hawke LD, 2012. Comorbid anxiety in bipolar spectrum disorders: a neglected research and treatment issue? J. Affect. Disord 137, 161–164. [DOI] [PubMed] [Google Scholar]
- Raftery AE, 1995. Bayesian model selection in social research. Sociological methodology, pp. 111–163. [Google Scholar]
- Sachs GS, 1990. Use of clonazepam for bipolar affective disorder. J. Clin. Psychiatry 51 Suppl,31–34; discussion 50–33. [PubMed] [Google Scholar]
- Sachs GS, Thase ME, Otto MW, Bauer M, Miklowitz D, Wisniewski SR, Lavori P, Lebowitz B, Rudorfer M, Frank E, Nierenberg AA, Fava M, Bowden C, Ketter T, Marangell L, Calabrese J, Kupfer D, Rosenbaum JF, 2003. Rationale, design, and methods of the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol. Psychiatry 53, 1028–1042. [DOI] [PubMed] [Google Scholar]
- Sala R, Axelson DA, Castro-Fornieles J, Goldstein TR, Goldstein BI, Ha W, Liao F, Gill MK, Iyengar S, Strober MA, Yen S, Hower H, Hunt JI, Dickstein DP, Ryan ND, Keller MB, Birmaher B, 2012a. Factors associated with the persistence and onset of new anxiety disorders in youth with bipolar spectrum disorders. J. Clin. Psychiatry 73, 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sala R, Goldstein BI, Morcillo C, Liu SM, Castellanos M, Blanco C, 2012b. Course of comorbid anxiety disorders among adults with bipolar disorder in the U.S. population. J. Psychiatr. Res 46, 865–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sala R, Strober MA, Axelson DA, Gill MK, Castro-Fornieles J, Goldstein TR,Goldstein BI, Ha W, Liao F, Iyengar S, Yen S, Hower H, Hunt J, Dickstein DP, Ryan ND, Keller MB, Birmaher B, 2014. Effects of comorbid anxiety disorders on the longitudinal course of pediatric bipolar disorders. J. Am. Acad. Child Adolesc. Psychiatry 53, 72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz G, 1978. Estimating the dimension of a model. The annals of statistics, pp. 461–464. [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T,Baker R, Dunbar GC, 1998. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59 Suppl 20, 22–33;quiz 34–57. [PubMed] [Google Scholar]
- Simon NM, Otto MW, Wisniewski SR, Fossey M, Sagduyu K, Frank E, Sachs GS,Nierenberg AA, Thase ME, Pollack MH, 2004. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am. J. Psychiatry 161, 2222–2229. [DOI] [PubMed] [Google Scholar]
- Thibodeau MA, Welch PG, Sareen J, Asmundson GJ, 2013. Anxiety disorders are independently associated with suicide ideation and attempts: propensity score matching in two epidemiological samples. Depress. Anxiety 30, 947–954. [DOI] [PubMed] [Google Scholar]
- Tondo L, Baldessarini RJ, 1998. Rapid cycling in women and men with bipolar manic-depressive disorders. Am. J. Psychiatry 155, 1434–1436. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.