Abstract
Background
The aim of this study was to investigate the effect of virtual reality (VR) technology on balance and gait in patients with Parkinson’s disease (PD).
Material/Methods
The study design was a single-blinded, randomized, controlled study. Twenty-eight patients with PD were randomly divided into the experimental group (n=14) and the control group (n=14). The experimental group received VR training, and the control group received conventional physical therapy. Patients performed 45 minutes per session, 5 days a week, for 12 weeks. Individuals were assessed pre- and post-rehabilitation with the Berg Balance Scale (BBS), Timed Up and Go Test (TUGT), Third Part of Unified Parkinson’s Disease Rating Scale (UPDRS3), and Functional Gait Assessment (FGA).
Results
After treatment, BBS, TUGT, and FGA scores had improved significantly in both groups (P<0.05). However, there was no significant difference in the UPDRS3 between the pre- and post-rehabilitation data of the control group (P>0.05). VR training resulted in significantly better performance compared with the conventional physical therapy group (P<0.05).
Conclusions
The results of this study indicate that 12 weeks of VR rehabilitation resulted in a greater improvement in the balance and gait of individuals with PD when compared to conventional physical therapy.
MeSH Keywords: Gait, Parkinsonian Disorders, Physical Therapy Modalities, Postural Balance, Virtual Reality Exposure Therapy
Background
Parkinson’s disease (PD) results from degenerative changes in the nervous system, leading to dysfunction of the cerebral basal ganglia [1]. Patients often have posture control disorders and mobility disorders [2], seriously affecting their quality of life [3]. Freezing of gait is one of the common complications of PD patients, often occurring in the advanced stages of the disease. With this complication, despite the patient’s attempt to walk, the forward progression of the feet is significantly reduced [4], increasing the risk of falls and creating difficulties in the patient’s care [5].
Currently, drugs that target freezing of gait in PD do not provide the patient with a fully effective response [6]. The literature suggests that physical therapy can further improve the motor function of patients with PD [7,8]. One of the most promising treatments is virtual reality (VR), which can provide visual, auditory, and somatosensory stimuli to assist in improving gait for individuals with PD. It enables people to interact with an artificial VR, while health professionals can monitor and evaluate their progress. External stimuli are beneficial in improving gait in patients with PD [9], with an additional increase in speed associated with the use of visual cues [10]. However, so far, there is not enough evidence to prove the effectiveness of VR technology in improving motor function in Parkinson’s patients.
The rapid development of artificial intelligence has led to emerging areas of research in rehabilitation medicine. A proof-of-concept study found that wearable sensors could gain objective measures of balance exercises in individuals with PD [11]. VR technology has attracted attention as a new means of rehabilitation, and in recent years, the literature in this area has expanded. VR can provide patients with more sensory stimulation, a more immersive environment, and real-time feedback during specific motor tasks [12], reflecting motor learning and neuroplasticity [13]. Therefore, this approach can be considered as a complement to traditional rehabilitation therapies. A meta-analysis indicated that in healthy older people, “exergaming” may improve balance and functional mobility [14]. A lack of functional gait can be compensated for with visual information [15]. The literature suggests that for individuals with PD, “exergaming” as an aided strategy using the Kinect sensor is a safe and appealing alternative to conventional physical therapy [16–18]. However, there is currently little clinical literature on VR and traditional exercise therapy, with a study length of less than 8 weeks for most observational studies. The purpose of the present study is to observe the effects of a 12-week VR training program on gait and balance in patients with PD.
Material and Methods
We recruited inpatients from the Rehabilitation Medicine Department of Heilongjiang Provincial Hospital who met the diagnosis of PD according to the United Kingdom Brain Bank Criteria [19]. Because the patient was limited by the length of stay, the patient continued treatment in the outpatient department after discharge. The inclusion criteria were as follows: (1) Improved Hoehn-Yahr classification [20] grade 2.5-4, in which there is balance dysfunction but independent walking; (2) age 50 to 70 years old; (3) signed informed consent. The exclusion criteria were as follows: (1) other causes of tremor, such as hereditary ataxia and cerebellar or vestibular lesions; (2) bone and joint diseases or serious diseases affecting organ function; (3) visual or hearing disorders; (4) unable to cooperate with the study. In addition, the study protocol was explained to all participants before their participation. The study was approved by the Institutional Review Board of Heilongjiang Provincial Hospital and performed in accordance with the Declaration of Helsinki. The participants were randomized to 2 groups as shown in Figure 1. The treatment group received VR training, and the control group received conventional physical therapy. Both groups received routine medication for PD, and 16 patients took dopamine agonists, and 12 patients took compound dopa (L-dopa-Bensom and or levodopa-carbidopa). The patients performed in the period of 2 h after medication. (Table 1)
Figure 1.
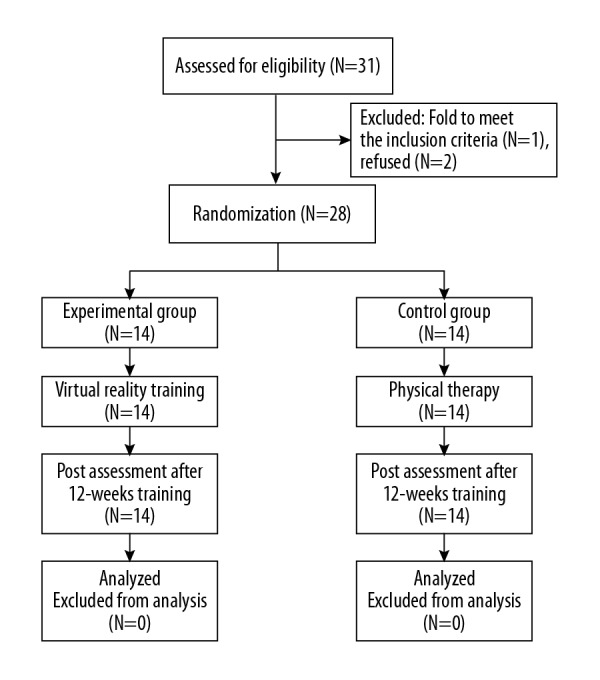
Disrtibution of study participants.
Table 1.
Characteristics of all participants.
| Experimental group (N=14) | Control group (N=14) | P-value | |
|---|---|---|---|
| Age(years) | 67.47±4.79 | 66.93±4.64 | 0.76 |
| Gender (male/female) | 8/7 | 9/6 | 0.37 |
| Disease duration (years) | 7.07±1.44 | 6.60±1.45 | 0.38 |
| Height (cm) | 167.07±5.54 | 165.8±5.83 | 0.55 |
| Weight (kg) | 59.87±5.78 | 59.07±5.57 | 0.70 |
| Education received (years) | 10.47±3.31 | 9.93±2.66 | 0.63 |
| Hoehn and Yahr grade | 3.03±0.55 | 2.97±0.58 | 0.77 |
| Mini Mental Status Examination | 27.07±2.09 | 26.29±2.49 | 0.29 |
| Levodopa equivalent daily dose (mg) | 203.6±47.2 | 227.5±54.3 | 0.23 |
The same therapist was employed to complete each patient’s 12 weeks of rehabilitation. The control group received traditional rehabilitation training according to the 2014 edition of the Chinese Guide to Treatment of PD [21], and the experimental group used VR technology to perform balance and gait training. Traditional rehabilitation training group exercise protocol used is shown in Table 2, and it includes: the center of gravity transfer training is carried out in different positions, and the force in different directions is given to patients in different contact areas and angles so that patients can control the balance by themselves; Visual, auditory and orthopedic mirror feedback methods were used to train the patients’ body posture control. Strength training and walking training; Physical therapist in-bed translation training; Exercise the left and right sides of the body while standing or walking; Throwing and catching training; Rhythm training. The experimental group exercise protocol used is shown in Table 3. According to the patient’s physical condition, the therapist conducted each treatment for 45 minutes, once a day, 5 times a week, for a total of 12 weeks.
Table 2.
Traditional rehabilitation training group exercise protocol.
| Traditional training | Time (minutes) | Action | Motor demand |
|---|---|---|---|
| Warm-up | 5 | Stretching all the joints and major muscle | Load bearing, drafting, full range of motion |
| Balance | 10 | The center of gravity transfer training is carried out in different positions, and the force in different directions is given to patients in different contact areas and angles so that patients can control the balance by themselves. Exercise the left and right sides of the body while standing or walking | Limb muscular strength, shifting the center of gravity, single leg weight, upper and lower extremity coordination |
| Physical condition | 10 | Strength training and walking training. Rhythm training | Quick response, shifting the center of gravity, limb flexibility, exercise adaptation |
| Coordination | 10 | Visual, auditory and orthopedic mirror feedback methods were used to train the patients’ body posture control | Fast moving, body turning, lower extremity coordination |
| Cool-down | 10 | Stretching all the joints | Relax muscles and take a deep breath |
Table 3.
The experimental group exercise protocol.
| Game training | Time (minutes) | Action | Motor demand |
|---|---|---|---|
| Warm-up | 5 | The face of the screen reaches all corners for the purpose of pulling the body | Load bearing, drafting, full range of motion |
| Hands and feet touch the ball | 10 | The ball appears in different positions on the screen, with the upper extremities and lower extremities each reaching to touch the ball | Limb muscular strength, shifting the center of gravity, single leg weight, upper and lower extremity coordination |
| Hard boating | 10 | Use your upper body to boat, while keeping balance to prevent your body from falling into the water | Quick response, shifting the center of gravity, limb flexibility, exercise adaptation |
| Take the maze | 10 | According to the situation, analyzing and selective walking in different directions until out of the maze | Fast moving, body turning, lower extremity coordination |
| Cool-down | 10 | In the original position, stretch all joints | Relax muscles and take a deep breath |
The outcomes of the sessions were assessed using the Berg Balance Scale (BBS) [22], the Timed Up and Go Test (TUGT) [23], the third part of the Unified Parkinson’s Disease Rating Scale test (UPDRS3) and the Functional Gait Assessment (FGA). The assessments were conducted by a single-blinded outcome assessor at the beginning of the study to obtain a baseline and at the end of the study period 12 weeks later.
BBS was used to assess the patient’s overall balance function. The scale includes 14 activities related to balance, such as unsupported sitting and unsupported standing, with a total score of 56 points. The higher the score, the better the balance, and a score below 40 suggests a risk of falling. The points are based on the time for which each position is held, the distance to which the upper limb is capable of reaching out in front of the body, and the time required to complete each task [24].
TUGT is conducted as follows: Let the patient seated in a chair with armrests stand up independently, walk forward 3 m, walk back to the chair, and sit down, while being timed. A total of 3 tests are conducted at an interval of 1 min, and the mean time is used. The test is done independently under guardianship. Guardians do not make any physical contact with the patient to avoid giving any practical assistance. In 2013, a systematic review [25] indicated that the TUGT is a sensitive assessment for gait and balance evaluation. A previous study also found that the TUGT had high reliability (ICC >0.87) for assessing balance in people with PD [26].
UPDRS3 is used in PD patients to assess motor function. There is a total score of 56 points, in which a higher score indicates more severely impaired motor function.
FGA [27] was used to assess gait. The FGA consists of 10 items in which the patient walks under increasingly difficult conditions, such as pivoting or walking with eyes closed. Each item is scored from zero to 3, in which a score of zero indicates an inability to perform the task, while 3 is normal. According to the FGA, the best score is the maximum of 30.
SPSS 24.0 statistical software was used for data analysis. Each group of data are expressed as (x±s). The normality of the data was tested using the Kolmogorov-Smirnov (KS) method, which was in accordance with the normal distribution. KS was an appropriate method to test the overall goodness of fit between a set of discontinuities. Data observation and this particular theoretical distribution. The independent samples t test was used to compare between groups. The paired-samples t test was used to compare the data before and after training. Significance level was set at α=0.05. The data analysts did not participate in clinical treatment or assessment.
Results
Figure 1 shows an overview about the patients’ progression of the study. 1 case failed to meet the inclusion criteria, and 2 cases declined to participate in clinical trial treatment. Therefore, the final 28 patients were included in the efficacy statistics. Participant characteristics are shown in Table 1. There was no significant difference between the 2 groups in their scores before treatment (P>0.05). After treatment, the BBS, TUGT and FGA scores had improved significantly in both groups (P<0.05). However, there was no significant difference in the UPDRS3 between the pre- and post-rehabilitation data of the control group (P>0.05). The scores of the BBS, TUGT, UPDRS3 and FGA in experimental group were better than those in the control group (P<0.05). These data are shown in Table 4.
Table 4.
Comparisons of patient results between the 2 groups (mean ±SD).
| Experimental group (N=14) | Mean ±SD difference | Control group (N=14) | Mean ±SD difference | |||
|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||
| BBSc | 30.64±3.91a | 36.71±4.60b | 6.07±0.35 | 30.07±3.87a | 32.00±4.82b | 1.93±0.70 |
| TUGTc | 34.21±6.41a | 30.93±5.55b | 3.29±0.94 | 37.86±3.92a | 35.14±5.07b | 2.71±0.97 |
| UPDRS3 | 25.14±7.01a | 21.50±6.81b | 3.64±1.25 | 24.71±6.60a | 21.36±8.15 | 3.36±1.93 |
| FGAc | 14.71±2.67a | 21.21±3.95b | 6.50±0.37 | 16.21±2.58a | 18.43±3.09b | 2.14±0.82 |
Difference between the groups before treatment not significant (P>0.05);
Significant differences before and after treatment (P<0.05);
Significant differences between improvement of the experimental group (P<0.05).
BBS – Berg Balance Scale; TUGT – Timed ‘Up and Go’ Test; UPDRS3 – The third part of Unified Parkinson’s Disease Rating Scale; FGA – Functional Gait Assessment.
Discussion
This study demonstrated that a 12-week program of VR training improved the gait and balance of patients with PD. The data revealed that the BBS score, TUGT time, UPDRS3 score and FGA score were all significantly improved in experimental group. However, compared with the VR rehabilitation, there was no significant difference in the UPDRS3 between the pre- and post-rehabilitation data of the control group.
The main reason for this change is that UPDRS3 is mainly composed of tremor, rigidity, speech, posture, gait and other parts. Compared with BBS, TUGT, and FGA assessment methods, UPDRS3 has different areas of focus, such as myotonia, posture tremor, and flexibility of the knee under knee flexion. As a comprehensive assessment of motor function in patients with Parkinson’s disease, BBS focuses on the balance and mobility test of activity ability, lack of the balance test in walking. TUGT mainly calculates the time to stand up to walk, and FGA can determine Parkinson whether the patient has a balance disorder that affects functional activities such as walking. Traditional rehabilitation methods, although able to maintain the body’s ability to maintain a certain posture, such as sitting, standing, standing on one leg and improve the ability to adjust and control the stability of the body during exercise. Improved but limited ability to make protective adjustment responses to maintain or establish a new balance when patients with Parkinson’s disease are physically disturbed. In patients with Parkinson’s disease, the muscles involved in posture control are in a state of dysregulation for a long time, and the tension of the limbs and trunk flexor muscles are increased, resulting in muscle spasm around the back, hips, knees, and ankle joints, and joint activity is limited. Abnormal movement patterns and abnormal muscle tone lead to decreased postural regulation in patients. The reason why the VR technology can reflect the difference of UPDRS3 rating scale may be that various stimuli increase the sensitivity of patients’ sensory organs, and rhythmic stimulation can compensate for the rhythm disorder of central nervous system, alleviate muscle spasm, and improve the instability of center of gravity distribution. These require further research and observation of our large sample in the future.
PD involves inadequate interactions between the vestibular, visual, and proprioceptive systems, with consequent changes in the biomechanics of the body [28]. Postural control is needed to adapt different environments, which also requires the visual, somatosensory and vestibular systems [29]. Externally guided movements are mediated by unique neural pathways [30]. In a VR environment, visual feedback may be an important factor for patients with PD during the rehabilitation process. For the external stimuli of movements, patients with PD performed better than healthy people in supporting their weight [31]. One study found that online visual feedback led to improvements in the gait of patients without any changes to their medication regimens [32]. Visual information is necessary to perform accurate goal-oriented tasks, and VR technology can be used in a completely immersive environment through simple simulations, from simple to complex. It mainly constructs an image realistic model on the computer, which finally forms a simulation environment, and can also immerse patients in this environment through some sensing devices. The feedback given by visual can strengthen the correct behavior of the patients, maintain the level of action and enthusiasm of the patients and can get a good emotional experience, so that it can continue to practice and finally master. The advantage of VR for rehabilitation is that it can provide 2 kinds of feedback for the rehabilitation, including feedback for each exercise and a set of subsequent feedback, which can improve the patient’s cognitive sensation, through the preparation of different environments, increases the interest, and stimulates and maintains the patient’s repeated motivation in various forms. Many trial results show that patients can learn the skills of exercise in a virtual environment and apply the technology to the real world. These are the advantages of VR rehabilitation technology compared to traditional rehabilitation. Overall, systems based on VR seem useful to study and treat patients’ motor skills. Specifically, the VR system presented in the abovementioned study allows the evaluation of alterations in rhythm formation in patients with PD and in the elderly. That study aimed to examine the effects of VR dance exercise on the balance, ADL, and depressive disorder status of PD patients. Within-group comparisons demonstrated that balance improved significantly in the experimental group. The between-group comparisons showed that the balance of the experimental group significantly improved relative to the control group. Since PD is a chronic progressive disease, we suggest that the visual feedback VR technique should be considered as a long-term treatment, in addition to physical therapy, to maintain gait and postural performances in PD patients.
In this study, we found that patients with PD had differences in onset time, age, and cognitive ability, which may affect the level of participation in the rehabilitation process. We also believe that patient interest in treatment is of paramount importance and may impact their active participation and therefore their prognosis. Rehabilitation treatment of PD is a long process and requires patient cooperation. Using both VR rehabilitation training and conventional exercise therapy, these 2 treatment modalities complement each other for the management of PD.
This study demonstrates that VR is a promising treatment for gait, balance and mobility in PD. The improvement of mobility also has a positive effect on patients’ self-care abilities and decreasing the burden of caregivers. Conventional balance training is mostly “one-on-one” training, which utilizes more medical resources; the training may seem monotonous or boring to patients; and after training, patients cannot integrate training into their daily life environment and so on. VR technology training uses computers to generate some interesting entertaining mini games or travel scenes for patients to participate in, and reward them after completing the task. This technique involves sensory input during operation, the brain’s judgment and integration of information, and the effective control of the nerves. In the process of completing the task, the patient could continuously receive feedback, prompting the adjustment of the motion pattern to form an optimized neural network. The exercise programs can involve exquisite pictures, beautiful music and positive feedback, etc., to divert the patient’s attention and make the patient psychologically reduce the fear of training, so as to achieve the effect of recovery. Applying VR technology to the field of rehabilitation medicine can effectively solve the limitations of traditional rehabilitation training methods. It breaks many shortcomings of traditional training and saves manpower. VR technology not only provides a training environment similar to the real world and meaningful task-oriented training, but also quantifies the patient’s functional status before and after rehabilitation. VR technology can improve their quality of life, so that their field of activity is no longer limited to a home, a room, or even a bed. One is the combination of games and treatments, that is, the screen provides an artificial scene that makes the patient feel like being in a game or travel environment, making the treatment process full of fun and improving the patient’s optimism. Second, the combination of psychological guidance and physical therapy, using screen technology, can use the language and words to carry out various psychological prompts and inducement to patients, fully mobilize the patient’s mental effects, and in turn strengthen the role of physiological treatment. Patients can deepen the sense of existence of the entire process through VR rehabilitation techniques with the 3 characteristics of immersion, interaction and imagination, and is now widely used in the field of rehabilitation medicine [33]. Patients with PD can adjust their trunk segmental alignment in VR games. In addition, VR games can also improve the standing posture stability of patients by increasing the organization and integration ability of vestibular organs [34]. VR games provide dynamic and static posture control activities to train the trunk control and center of gravity in order to adjust the segmental torso alignment of patients with PD. The visual feedback in the VR game allows the patient to sense their own position and movement direction in the space based on visual tracking and to coordinate their body position.
Conclusions
Compared with traditional rehabilitation methods, virtual reality rehabilitation technology has improved the BBS, TUGT, UPDRS3, and FGA scores of patients with Parkinson’s disease, which is of guiding significance for further research in the future. In addition, as a more high-tech intelligent treatment method, it is may be more maneuverable, easier to promote in community rehabilitation, and brings fun and enjoyment to patients’ recovery. Some limitations of our study include a relatively short time period and a small sample size. Further long-term clinical trials with large sample sizes are required to further confirm our findings. The effects of VR technology on the recovery of balance function in patients of different genders and age groups has not yet been elaborated and should also be further studied.
Footnotes
Source of support: Heilongjiang Health and Family Planning Commission [No. 2017-465]
References
- 1.Dibble LE, Nicholson DE, Shultz B, et al. Sensory cueing effects on maximal speed gait initiation in persons with Parkinson’s disease and healthy elders. Gait Posture. 2004;19:215–25. doi: 10.1016/S0966-6362(03)00065-1. [DOI] [PubMed] [Google Scholar]
- 2.Lord S, Godfrey A, Galna B, et al. Ambulatory activity in incident Parkinson’s: More than meets the eye? J Neurol. 2013;260:2964–72. doi: 10.1007/s00415-013-7037-5. [DOI] [PubMed] [Google Scholar]
- 3.Bloem BR, Grimbergen YAM, Cramer M, et al. Prospective assessment of falls in Parkinson’s disease. J Neurol. 2001;248:950–58. doi: 10.1007/s004150170047. [DOI] [PubMed] [Google Scholar]
- 4.Nutt JG, Bloem BR, Giladi N, et al. Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol. 2011;10:734–44. doi: 10.1016/S1474-4422(11)70143-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bloem BR, Hausdorff JM, Visser JE, Giladi N. Falls and freezing of gait in Parkinson’s disease: A review of two interconnected, episodic phenomena. Mov Disord. 2004;19:871–84. doi: 10.1002/mds.20115. [DOI] [PubMed] [Google Scholar]
- 6.Schaafsma JD, Balash Y, Gurevich T, et al. Characterization of freezing of gait subtypes and the response of each to levodopa in Parkinson’s disease. Eur J Neurol. 2003;10:391–98. doi: 10.1046/j.1468-1331.2003.00611.x. [DOI] [PubMed] [Google Scholar]
- 7.Tan SB, Williams AF, Kelly D. Effectiveness of multidisciplinary interventions to improve the quality of life for people with Parkinson’s disease: A systematic review. Int J Nurs Stud. 2014;51:166–74. doi: 10.1016/j.ijnurstu.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Petzinger GM, Fisher BE, McEwen S, et al. Exercise-enhanced neuroplasticity targeting motor and cognitive circuitry in Parkinson’s disease. Lancet Neurol. 2013;12:716–26. doi: 10.1016/S1474-4422(13)70123-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nieuwboer A, Kwakkel G, Rochester L, et al. Cueing training in the home improves gait-related mobility in Parkinson’s disease: The RESCUE trial. J Neurol Neurosurg Psychiatry. 2007;78:134–40. doi: 10.1136/jnnp.200X.097923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Suteerawattananon M, Morris GS, Etnyre BR, et al. Effects of visual and auditory cues on gait in individuals with Parkinson’s disease. J Neurol Sci. 2004;219:63–69. doi: 10.1016/j.jns.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Conradsson D, Håkan N, Löfgren N, et al. Monitoring training activity during gait related balance exercise in individuals with Parkinson’s disease: A proof-of-concept-study. BMC Neurology. 2017;17:19. doi: 10.1186/s12883-017-0804-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adamovich SV, Fluet GG, Tunik E, Merians AS. Sensorimotor training in virtual reality: A review. NeuroRehabilitation. 2009;25:29–44. doi: 10.3233/NRE-2009-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Bruin ED, Schoene D, Pichierri G, Smith ST. Use of virtual reality technique for the training of motor control in the elderly. Some theoretical considerations. Z Gerontol Geriatr. 2010;43(4):229–34. doi: 10.1007/s00391-010-0124-7. [DOI] [PubMed] [Google Scholar]
- 14.Donath L, Rössler R, Faude O. Effects of virtual reality training (exergaming) compared to alternative exercise training and passive control on standing balance and functional mobility in healthy community-dwelling seniors: A meta-analytical review. Sports Med. 2016;46(9):1293–309. doi: 10.1007/s40279-016-0485-1. [DOI] [PubMed] [Google Scholar]
- 15.Hanakawa T, Fukuyama H, Katsumi Y, et al. Enhanced lateral premotor activity during paradoxical gait in pd. Ann Neurol. 1999;45(3):329–36. doi: 10.1002/1531-8249(199903)45:3<329::aid-ana8>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 16.Shih MC, Wang RY, Cheng SJ, Yang YR. Effects of a balance-based exergaming intervention using the Kinect sensor on posture stability in individuals withParkinson’s disease: a single-blinded randomized controlled trial. J Neuroeng Rehabil. 2016;13:78. doi: 10.1186/s12984-016-0185-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silva KG, De Freitas TB, Doná F, et al. Effects of virtual rehabilitation versus conventional physical therapy on postural control, gait, and cognition of patients with Parkinson’s disease: study protocol for a randomized controlled feasibility trial. Pilot Feasibil Stud. 2017;3:68. doi: 10.1186/s40814-017-0210-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Natbony LR, Zimmer A, Ivanco LS, et al. Perceptions of a videogame-based dance exercise program among individuals with Parkinson’s disease. Games Health J. 2013;2(4):235–39. doi: 10.1089/g4h.2013.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55:181–84. doi: 10.1136/jnnp.55.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goetz GC, Poewe W, Rascol O, et al. Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: Status and recommendations. Mov Disord. 2004;19:1020–28. doi: 10.1002/mds.20213. [DOI] [PubMed] [Google Scholar]
- 21. [Chinese Medical Association Neurology Branch Parkinson’s disease and motor disorders group, Chinese Guide to Parkinson’s Disease Treatment]. Chinese Journal of Neurology. 2014;47:428–33. [in Chinese] [Google Scholar]
- 22.Berg K, Wood-Dauphinee S, Williams GD. Clinical and laboratory measures of postural balance in an elderly population. Physiotherapy Canada. 1992;41:304–11. [PubMed] [Google Scholar]
- 23.Karuka AH, Silva JA, Navega MT. Analysis of agreement of assessment tools of body balance in the elderly. Rev Bras Fisioter. 2011;15(6):460–66. [PubMed] [Google Scholar]
- 24.Lopes JB, Lameira de Melo GE, Lazzari RD, et al. Measures used for the evaluation of balance in individuals with Parkinson’s disease: A systematic review. J Phys Ther Sci. 2016;28:1936–42. doi: 10.1589/jpts.28.1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schoene D, Wu SM, Mikolaizak AS, et al. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: Systematic review and meta-analysis. J Am Geriatr Soc. 2013;61:202–8. doi: 10.1111/jgs.12106. [DOI] [PubMed] [Google Scholar]
- 26.Morris S, Morris ME, Iansek R. Reliability of measurements obtained with the Timed “Up & Go” test in people with Parkinson disease. Phys Ther. 2001;81:810–18. doi: 10.1093/ptj/81.2.810. [DOI] [PubMed] [Google Scholar]
- 27.Wrisley DM, Marchetti GF, Kuharsky DK, et al. Reliability, internal consistency, and validity of data obtained with the functional gait assessment. Phys Ther. 2004;84:906–18. [PubMed] [Google Scholar]
- 28.Abe PT, Vitorino DF, Guimarães LH, et al. [Análise do equilíbrio nos pacientes com doença de Parkinson grau leve e moderado através da fotogrametria]. Neurociencias. 2004;12:73–76. [in Portuguese] [Google Scholar]
- 29.Henderson A, Korner-Bitensky N, Levin M. Virtual reality in stroke rehabilitation: A systematic review of its effectiveness for upper limb motor recovery. Top Stroke Rehabil. 2007;14(2):52–61. doi: 10.1310/tsr1402-52. [DOI] [PubMed] [Google Scholar]
- 30.Adamovich SV, Fluet GG, Tunik E, Merians AS. Sensorimotor training in virtual reality: A review. Neurorehabilitation. 2009;25:29–44. doi: 10.3233/NRE-2009-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Praamstra P, Stegeman DF, Cools AR, Horstink MW. Reliance on external cues for movement initiation in Parkinson’s disease. evidence from movement-related potentials. Brain. 1998;121:167–77. doi: 10.1093/brain/121.1.167. [DOI] [PubMed] [Google Scholar]
- 32.Badarny S, Aharon-Peretz J, Susel Z, et al. Virtual reality feedback cues for improvement of gait in patients with Parkinson’s disease. Tremor Other Hyperkinet Mov (NY) 2014;4:225. doi: 10.7916/D8V69GM4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee NY, Lee DK, Song HS. Effect of virtual reality dance exercise on the balance, activities of daily living, and depressive disorder status of Parkinson’s disease patients. J Phys Ther Sci. 2015;27:145–47. doi: 10.1589/jpts.27.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crosbie JH, Lennon S, Basford JR, McDonough SM. Virtual reality in stroke rehabilitation: Still more virtual than real. Disabil Rehabil. 2007;29(14):1139–46. doi: 10.1080/09638280600960909. [DOI] [PubMed] [Google Scholar]


