Abstract
Objective:
Active surgical drains minimize fluid accumulation in the post-operative period. The “Jackson-Pratt” (JP) system consists of a silicone drain connected by flexible tubing to a bulb. When air in the bulb is evacuated, negative pressure is applied at the surgical site to aspirate fluid. The objective of this study was to determine if the evacuation method and volume of accumulated fluid affect the pressure generated by the bulb.
Methods:
Bulbs were connected to a digital manometer under various experimental conditions. A random number generator determined the initial evacuation method for each bulb, either side-in or bottom-up. Subsequent evacuations were alternated until data was collected in triplicate for each method. Pre-determined amounts of water were placed into the bulb, air was evacuated, and pressure was recorded. All setups were allowed to equilibrate for 1 minute prior to data acquisition.
Results:
The average amount of pressure after a side-in evacuation of a JP bulb was 87.4 cm H2O compared to 17.7 cm H2O for a bottom-up evacuation (p < 0.0001). When the drain contained 25 mL, 50 mL, 75 mL, and 100mL of fluid, the pressure applied dropped to 72.6, 41.3, 37.0 and 35.6 cm H2O respectively.
Conclusions:
JP drains generate negative pressure in order to reduce fluid accumulation at surgical sites. While its function is frequently taken for granted, this study demonstrates that both the specific method for evacuating the bulb as well as the amount of fluid in the bulb significantly affect the performance of this device.
Keywords: JP drain, Jackson Pratt, surgical drain
INTRODUCTION:
Surgical drains are placed intra-operatively or post-operatively to allow for egress of fluid or air from the wound bed. Fluid collections such as a seroma are a fairly common occurrence after extensive tissue dissection that results in a large space or cavity [1]. Drains are therefore commonly used in head and neck surgery post-operative care, in particular following parotidectomy, thyroidectomy, neck dissection, laryngectomy, and other major head and neck resection and reconstruction [2–4].
Drains can be classified in two ways: open or closed, and passive or active. Open drains allow for wound drainage directly to the outside environment, whereas closed drains typically utilize a reservoir to collect wound drainage. Passive drains allow excess fluid to drain via the wound’s natural pressure gradient, whereas active drains generate negative pressure to facilitate the removal of fluid or air from the wound bed.
The “Jackson-Pratt” (JP) system is a closed, active drainage system that consists of a silicone drain connected by flexible tubing to a bulb (Figure 1). Compared to other closed drainage systems, the JP bulb is a relatively low pressure system [5]. The bulb itself consists of 2 ports, one of which allows for 2-way flow and has an attached stopper, while the other is one-way, only allowing for intake from the attached drain. To apply negative pressure to the attached drain, the bulb is compressed with the stopper disengaged, which expels air from the bulb and not into drain. When the stopper is engaged, a gentle negative pressure is transmitted to the silicon drain that resides within the closed-space surgical site, thereby aspirating fluid from the wound and into the bulb. Markings on the bulb allow for approximation of the aspirated volume. Based on our experience, while the bulb is typically compressed perpendicular to the long axis (Figure 2A), occasionally bulbs will be compressed perpendicular to the short axis (Figure 2B). Additionally, standard practice at our institution is to instruct nursing staff to empty and record the JP bulb every 4 or 8 hours depending on the acuity of care. At times, especially in the immediate 24-hour post-operative period, the bulb can gather a considerable volume in a short duration. Two approaches of emptying the bulb are often observed - either emptying and recording the bulb contents at frequent intervals as the bulb fills, or only emptying the bulb according to the indicated time frame.
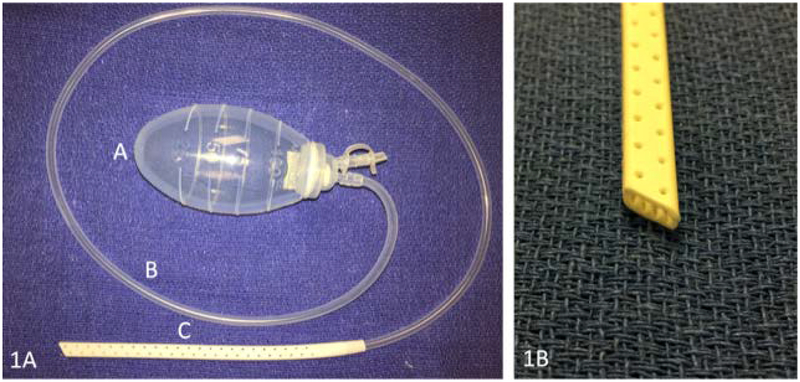
Figure 1 – A typical Jackson-Pratt drain.
1A) The Jackson-Pratt drain consists of a reservoir bulb (A) that transmits negative pressure through flexible tubing (B) to the drain (C), which contains internal ridges and multiple perforations along the sides. 1B) Close up view of the drain. Note the internal ridges and multiple holes along the tubing.
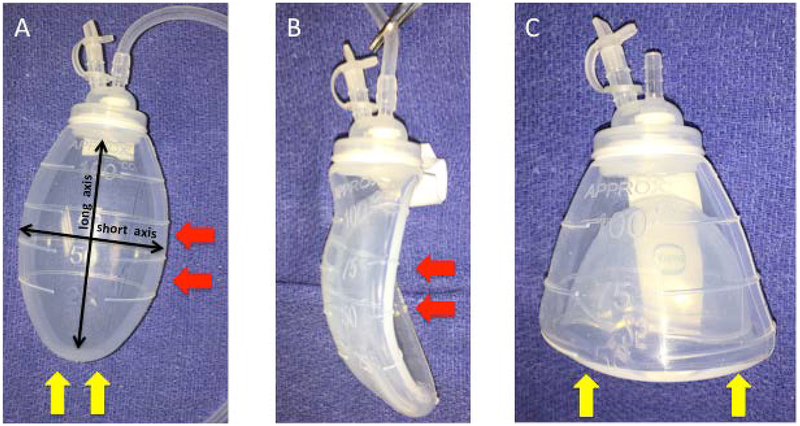
Figure 2 – Methods of bulb compression.
2A) JP bulb with labeled axes of compression. The red arrows indicate compression via the side-in method along the bulb’s horizontal axis. The yellow arrows indicate compression via the bottom-up method along the bulb’s longitudinal axis. 2B) Compression of the bulb via side-in method. 2C) Compression of the bulb via the bottom-up method. Note how in this configuration the drain remains stented in its compressed form without requiring a clamp or attached tubing.
The use of surgical drains is ubiquitous in the post-operative care of head and neck surgery patients and the JP drain is a commonly used system. We thus felt compelled to scrutinize a system which is so heavily relied upon, and ensure that it was in fact being utilized appropriately as we have witnessed both methods being used for compressing the bulb. Through our data, we hope to change the arbitrary practice of compressing a JP bulb to a more deliberate, purposeful aspect of post-operative patient care.
The purpose of this study was to determine if the two methods of compressing the bulb resulted in similar amounts of negative pressure and to examine the effect of various baseline reservoir volumes on bulb suction.
MATERIALS AND METHODS:
Suction bulbs were Davol 100cc Silicon closed wound suction evacuators (C.R. Bard Inc, Covington, GA). All pressure recordings were measured with a PYLE Meters PDMM01 Digital Manometer after the system was allowed to equilibrate for 60 seconds. Triplicate values from three separate bulbs were used for each measurement. A random number generator determined the initial evacuation method for each bulb, either by squeezing it perpendicular to the long axis (side-in; even number generated) or perpendicular to the short axis (bottom-up; odd number generated). Subsequent evacuations were alternated until data was collected in triplicate for each method for each bulb.
Negative pressure was then tested while squeezing the bulb in the side-in manner while the bulb reservoir contained specific measurements of water, specifically 25mL, 50mL, 75mL and 100mL of water. The measured volumes of water were placed into the bulb, air was evacuated and pressure was recorded.
Statistical analysis was performed using GraphPad Prism 5.0.
RESULTS:
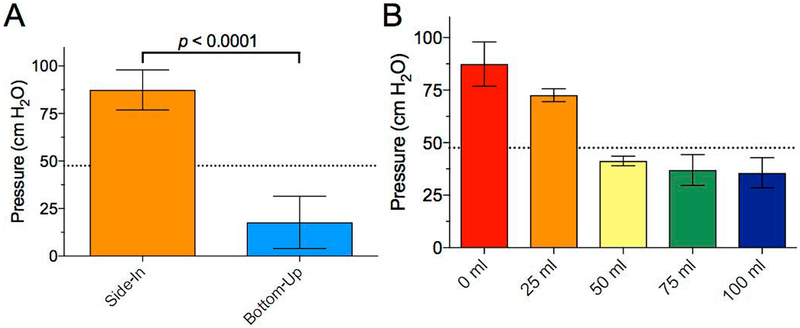
The average pressure after a side-in evacuation of a JP bulb was 87.4 cm H2O (95% C.I. 76.9 – 97.9 cm H2O) compared to 17.7 cm H2O (95% C.I. 4.0 – 31.5 cm H2O) for a bottom-up evacuation (p < 0.0001; Figure 3).
Figure 3 – Setup to record drain pressure.
The JP bulb was connected to the manometer using 10 cm of flexible silicone tubing.
The average pressure with no liquid in the bulb using the side-in evacuation method was 87.4 cm H2O (95% C.I. 77.8 – 97.9 cm H2O). Upon the addition of 25mL, 50mL, 75mL, and 100mL of water, the pressure generated using the side-in compression method dropped to 72.6 cm H2O (95% C.I. 69.5 – 75.7), 41.3 cm H2O (95% C.I. 39.0 – 43.6 cm H2O), 37.0 cm H2O (95% C.I. 29.7 – 44.3 cm H2O). and 35.6 cm H2O (95% C.I. 28.4 – 42.8) respectively (Figure 4).
Figure 4 – The performance of the JP drain can be significantly affected by the methods of charging the bulb as well as the amount of fluid that has accumulated.
A) Maximum negative pressure generated by bulb compression via side-in and bottom-up compression methods. B) Negative pressure measurements with increasing amounts of JP bulb filling. The dashed line represents approximate level of suction accomplished by low intermittent wall suction for comparison (47.5 cm H2O). Error bars represent 95% confidence intervals.
DISCUSSION:
While management of closed drainage systems is frequently debated in the literature [2, 6, 7], we generally agree that these systems use negative pressure to facilitate the egress of serous fluid, blood, and air from the wound bed. Our study demonstrates that this simple expectation depends both on the way the bulb is compressed and how often the bulb is emptied.
The incidence of fluid collection and therefore utility of post-operative suction drainage systems likely depends on multiple factors, including patient health, nature of disease, prior therapy, and type of surgery performed. Samraj et al [4] found that amongst high quality studies that compared suction drainage to no drainage after thyroidectomy, there was no difference between groups in incidence of fluid collection requiring aspiration or drainage. Conversely, Thomas et al highlighted the relevance of post-operative suction drainage in head and neck oncologic cases with flap reconstruction[8], noting that reoperation is a common post-operative complication with incision and drainage of the neck comprising 11.2% of reoperations overall. The amount of pressure required to keep cervical skin flaps approximated to the wound bed in the post-surgical patient is unknown. We postulate that this is a dynamic range of pressures because wound bed output depends on multiple factors such as post-operative day, extent of dissection, and patient comorbidities. Typically, higher volume drainage is observed in the first 24–48 hours post-operatively. Low intermittent wall suction is capable of generating a negative pressure of 41 – 54 cm cm H2O, a pressure range also achievable by the JP bulb system. We have observed that this is a sufficient negative pressure to keep cervical skin flaps approximated to the wound post-operatively.
There is no current recommendation at our institution as to the maintenance of the JP bulb suction in everyday practice, as evidenced by the sporadic use of the bottom-up versus side-in evacuation methods observed while on the wards. Our study showed that these two methods of charging the JP bulb are not equal. The side-in method resulted in significantly higher level of suction upon initial compression as compared to the bottom-up method. Furthermore, the addition of increasing volume of fluid caused a corresponding decrease in measured negative pressure within the bulb. During testing we found that compression via the bottom-up method occasionally resulted in the bulb being locked in the compressed position so that it could not spontaneously expand. This problem rendered the drain useless as re-expansion of the bulb is necessary to create a vacuum and ultimately aspirate fluid from a wound bed.
Given that many institutions utilize wall suction occasionally instead of JP bulb drain systems, the question arose as to the comparability of wall suction to JP bulb suction. Physicians will occasionally use wall suction instead of a JP bulb if there is an air leak or for various other reasons. A typical wall suction can be set to intermittent or continuous suction, and at “low” pressure setting has a negative pressure of approximately 41 – 54 cm H2O. The JP bulb apparatus is able to achieve this same level of suction needed to evacuate fluid from a wound bed post-operatively, but has the added benefit of encouraging patient ambulation without tethering them to a stationary wall suction apparatus.
We found that the side-in method of bulb compression generated higher negative pressure compared to the bottom-up method, and that negative pressure decreased with bulb filling. It is important to note that the bottom-up method can achieve a low level of suction, and therefore could have some utility if a lower negative pressure is required such as in post-op management of a low volume chyle leak. However, as shown in Fig 2C, the bottom-up compression method may cause the bulb to stent itself open and generate no suction in the wound bed. In this case, the JP drain tubing becomes only a foreign body in the wound and source of wound infection. For this reason, if a lower negative pressure is desired, we would recommend partial compression of the bulb via the side-in method as opposed to using the bottom-up method.
We observed that adequate suction pressure declines sharply for bulb volumes beginning at approximately 50cc. It may be prudent, therefore, to revise the practice of emptying JP drain bulbs based on the amount of volume filled rather than an hourly time schedule. The motivation behind the bulb emptying is to prevent a high volume from accumulating in the JP bulb, and therefore maintain the highest possible suction while the drain is in place.
Our conclusion supports the recommendations of other studies that bulbs should be emptied more frequently based on bulb filling. Carruthers et al [9] along with several other groups [3, 10, 11] have demonstrated similar findings that maximal pressures were generated when the bulb was empty and negative pressure values decreased with bulb filling. Further supporting our recommendation, Yue et al demonstrated that accuracy of drainage volume decreases at extreme volumes [12]. Based on their findings concerning accuracy regarding volumes in the bulb, they recommended allowing bulbs to fill to only 45 ml prior to empting. Our findings in conjunction with the findings of Yue et al support the idea that bulb emptying should occur when the bulb is approximately 25% full for optimal accuracy and maintenance of adequate suction.
Grobmyer et. al have published on complications such as fistulae formation and vascular compromise in tissue flaps as being associated with negative pressure drains [10] and it would be readily extrapolated that additional negative pressure may cause complications in some select scenarios. However, in our practice, if a suction drain is being used, it is only utilized in the in areas where there is little concern for fistula formation or disruption of a vascular pedicle.
SUMMARY:
The purpose of the JP drain is to prevent fluid accumulation in surgical sites and promote wound healing; it follows that maintenance of the drain’s negative pressure should be a priority in post-operative wound care. Our results suggest compressing the JP bulb by squeezing perpendicular to its long axis is the optimal method of establishing negative pressure in this closed, active drainage system. Furthermore, the bulb should not be compressed perpendicular to its short axis as it risks allowing the bulb to remain in its compressed state and not transmit negative pressure to the wound. We also support the recommendation of prior studies that drains should be emptied frequently in order to maintain consistent negative pressure on a post-surgical site. Further studies are needed to determine the utility of active, closed drainage after selected procedures, as recommendations may depend on the procedure in question.
We depend on JP drainage systems to achieve the best post-operative healing in our head and neck patients. Our study shows that with improper technique, the JP will not function as intended. Without a functioning vacuum, the JP drain tubing merely becomes a foreign body in a wound bed and a nidus for infection. This simple observation should change everyday clinical practice, as there is clearly one way of compressing the JP bulb that leads to superior vacuum drainage of the wound bed and thus improved post-operative healing.
Acknowledgments
Financial Disclosures: The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR002490 (AJK) and UL1TR002489 (FCL). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of Interest: No authors have any conflicts of interest.
REFERENCES:
- 1.Zawaneh PN and Putnam D, Materials in surgery: a review of biomaterials in postsurgical tissue adhesion and seroma prevention. Tissue Eng Part B Rev, 2008. 14(4): p. 377–91. [DOI] [PubMed] [Google Scholar]
- 2.Kasbekar AV, et al. , The management of vacuum neck drains in head and neck surgery and the comparison of two different practice protocols for drain removal. Ann R Coll Surg Engl, 2016. 98(1): p. 53–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams J, Toews D, and Prince M, Survey of the use of suction drains in head and neck surgery and analysis of their biomechanical properties. J Otolaryngol, 2003. 32(1): p. 16–22. [DOI] [PubMed] [Google Scholar]
- 4.Samraj K and Gurusamy KS, Wound drains following thyroid surgery. Cochrane Database Syst Rev, 2007(4): p. Cd006099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Durai R and Ng PC, Surgical vacuum drains: types, uses, and complications. Aorn j, 2010. 91(2): p. 266–71; quiz 272–4. [DOI] [PubMed] [Google Scholar]
- 6.Tian J, et al. , Comparison of drain versus no-drain thyroidectomy: a meta-analysis. Eur Arch Otorhinolaryngol, 2017. 274(1): p. 567–577. [DOI] [PubMed] [Google Scholar]
- 7.Li L, et al. , The effect of no drainage in patients who underwent thyroidectomy with neck dissection: A systematic review and meta-analysis. Medicine (Baltimore), 2017. 96(50): p. e9052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas WW, et al. , Clinical Factors Associated With Reoperation and Prolonged Length of Stay in Free Tissue Transfer to Oncologic Head and Neck Defects. JAMA Facial Plast Surg, 2018. 20(2): p. 154–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carruthers KH, et al. , Optimizing the closed suction surgical drainage system. Plast Surg Nurs, 2013. 33(1): p. 38–42; quiz 43–4. [DOI] [PubMed] [Google Scholar]
- 10.Grobmyer SR, et al. , High-pressure gradients generated by closed-suction surgical drainage systems. Surg Infect (Larchmt), 2002. 3(3): p. 245–9. [DOI] [PubMed] [Google Scholar]
- 11.Whitson BA, et al. , Not every bulb is a rose: a functional comparison of bulb suction devices. J Surg Res, 2009. 156(2): p. 270–3. [DOI] [PubMed] [Google Scholar]
- 12.Yue B, et al. , Accuracy of surgical wound drainage measurements: an analysis and comparison. ANZ J Surg, 2015. 85(5): p. 327–9. [DOI] [PubMed] [Google Scholar]