Abstract
Objectives
The purpose of this study was to adapt, test and evaluate the implementation of a primary care “Preventive care and Screening” meaningful use quality measure for tobacco use, in dental institutions.We determined the percentage of dental patients screened for tobacco use, and the percentage of tobacco users who received cessation counseling.
Methods
We implemented the dental quality measure, in three dental schools and a large accountable care dental organization. An automated electronic health record (EHR) query identified patients 18 years and older who were screened for tobacco use one or more times within 24 months, and who received cessation counseling intervention if identified as a tobacco user. We evaluated EHR query performance with a manual review of a sub-sample of charts.
Results
Across all four sites, in the reporting calendar year of 2015, a total of 143,675 patients met the inclusion criteria for the study. Within 24 months, including 2014 & 2015 calendar years, percentages of tobacco screening ranged from 79.7% to 99.9%, while cessation intervention percentages varied from 1%−81% among sites. By employing DQM research methodology, we identified intervention gaps in clinical practice.
Conclusions
We demonstrated the successful implementation of a dental quality measure to evaluate screening rates for tobacco use and cessation intervention. There is substantial variation in the cessation intervention rates across sites, and these results are a call for action for the dental profession to employ tobacco evidence-based cessation strategies to improve oral health and general health outcomes.
Keywords: oral health, quality improvement, dental quality measures, tobacco use cessation
Introduction
Although smoking rates have declined for the past forty years, tobacco use and the rise in non-cigarette tobacco products including e-cigarettes and water pipes (hookah) remains a public health problem (1, 2). Screening for tobacco use and delivering tobacco counseling cessation interventions have proven to be effective strategies and dental professionals play a pivotal role in these efforts (3). Currently tobacco screening and cessation is not implemented consistently in dental offices (4, 5). Although the majority of dentists appear to screen for tobacco use, less than half deliver cessation intervention (6). Barriers to dental office based tobacco screening and cessation interventions include insufficient financial reimburment (3, 6), time pressures and lack of referral options (7), and insufficient training for delivering tobacco cessation interventions (8). Training and confidence in delivering tobacco cessation counseling in clinical dentistry is a skill ideally first acquired during dental school. A recent survey of third and fourth year medical and dental students reported higher levels of confidence and comfort in delivering tobacco cessation strategies to patients among medical students than dental students (9). In response to this identified gap, several US dental schools have initiated clinically-oriented programs to treat tobacco dependence and deliver cessation efforts (10–12).
Through the 2009 HITECH (Health Information Technology for Economic and Clinical Health) Act, the US government developed the Meaningful Use (MU) incentive program to incentivize the adoption and “meaningful use” of certified electronic health records (EHRs) by providers, including dentists. This opened the door for the development of standardized quality improvement initiatives within dental practices (13). Coupled with recent efforts of development (14–16) and implementation (17–20) of standardized dental diagnostic terminologies, it is now possible to evaluate longitudinal patient data collected for quality metrics research. MU stage 2 includes several clinical quality care measures targeting tobacco cessation (21).
For this study we selected the process-of-care Meaningful Use Stage 2 measure “National Quality Forum (NQF) 0028 Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention.”(21) This MU measure evaluates the percentage of adult patients (18 years and older) who were screened for tobacco use defined as the use of any tobacco/nicotine products including cigarette, cigars, pipes, smokeless tobacco (snuff, chew, and bidis) one or more times within 24 months and who received cessation counseling intervention if identified as a tobacco user.
The aims of our study were to:
Adapt and revise the specifications of the Meaningful Use NQF 0028 measure originally designed for electronic medical records for electronic dental records;
Evaluate the feasibility and performance of the adapted measure by comparing the measure scores of the automated query to a manual chart review;
Evaluate the screening rates for tobacco use in our patient population and cessation interventions rates for tobacco users in our dental clinics.
Methods
We adapted, tested and evaluated the feasibility and usability of Meaningful Use (MU) Stage 2 measure NQF 0028 (21) in three dental schools located in different metropolitan US cities and a large accountable care dental organization with several dental offices in urban and rural locations. Following the MU Stage 2 specifications, we limited our analyses to adult patients of record, 18 years and older as our study population in the 2015 reportingyear. The collaborating institutions located in different geographical regions in the US, used axiUm (Exan Group, Henry Schein) as their EHR and obtained Institutional Review Board (IRB) approval for this research study.
Quality measure adaptation and design
We made adaptations to the MU measure for implementation into our dental EHR and to better characterize our patient population. We indicated the MU measure as the Primary Measure and subdivided the primary measure into three sub-measures (Tobacco use, Tobacco screening, Tobacco cessation intervention). Tobacco use was defined as the use of any tobacco/nicotine products including cigarette, cigars, pipes, smokeless tobacco (snuff, chew, and bidis). Table 1 outlines the measure description, numerator and denominator specifications for the primary measure and each of the three sub-measures with the objective to evaluate tobacco screening and cessation interventions separately.
Table 1.
Dental Quality Measure Specifications for the Primary Measure and Sub-Measures.
| Measure | Measure Description | Denominator | Numerator |
|---|---|---|---|
| Primary Measure | Proportion of adult patients, 18 years and older, who were patients of record at the dental institutions during the one year measurement period and were screened for tobacco use one or more times within 24 months (reporting year and the year prior to the reporting year) AND who received cessation counseling intervention if identified as a tobacco user during the same period | All patients aged 18 years and older seen for at least one clinical dental visit as defined by CDT codes D0120; D0150; D0180 during the measurement period (2015) | Patients who were screened for tobacco use at least once within 24 months (measurement period 2014&2015) AND who received tobacco cessation counseling intervention if identified as a tobacco user |
| Sub Measure 1 (Tobacco Screening) | Proportion of adult patients screened for tobacco use at least once during a two-year measurement period | Adults with at least one completed comprehensive (D0150) or periodic oral (D0120) examination or comprehensive periodontal evaluation (D0180) in 2015 | Adults screened for tobacco use at least once during the two year measurement period |
| Sub Measure 2 (Tobacco Use) | Proportion of adult patients identified as tobacco users during a two-year measurement period | Adults screened for tobacco use at least once during the two year measurement period (2014–2015) | Adults who were screened and identified as tobacco users during the two year measurement period |
| Sub Measure 3 (Tobacco Cessation Intervention) | Proportion of adult patients identified as a tobacco-users, who received cessation-counseling intervention at least once during a two-year measurement period | Adults who were screened and identified as tobacco users during the two year measurement period (2014–2015) | Adults who received tobacco cessation counseling intervention during the two year measurement period |
For measure adaptation, implementation and testing, we followed our previously described 5-step methodology(20).
A Structured Query Language (SQL) script was developed to extract data for denominator and numerator populations using EHR codes and medical history form questions to generate reports for all sites. After customizing the script as needed, sites executed the script and performed the initial testing. Initial pilot testing consisted of a review of 20 randomly selected charts at each site with manually review to confirm accuracy of the information generated by the script. Based on these testing results, the script was finalized.
Step 1. Denominator eligibility: the Meaningful Use Measure (21) denominator included “all patients aged 18 years and older seen for at least two visits OR at least one preventive visit during the measurement period”. For adaptation in dental EHRs, the Primary Measure denominator included adult patients who received a completed or in progress D0120 (periodic oral evaluation), D0150 (comprehensive oral evaluation) and/or D0180 (comprehensive periodontal evaluation) clinical procedures in the reporting year. The methodology for determining the denominator has been described previously (22). We excluded patients with the following statuses as of the last day of the reporting period: Inactive patients, Virtual or manikin patients,. patients attending special events including Give Kids a Smile day and board licensure examinations screenings or specialist care appointments.
Step 2. Sample size calculations: In order to evaluate the performance of the SQL script, a random sample of queried charts were selected for manual review that served as the “gold standard” assessment. The sample size estimation for the primary and sub-measures were formulated using the Cochran sample size formula for categorical data (23). Each estimate required the following initial values; 1) a sample proportion (given by the queried measure score), 2) a stated significance level (z=1.96), and 3) a projected margin for error (d=0.05)(23).
Step 3. Numerator eligibility: For the primary measure, we followed the specifications described in the MU measure NQF 0028 “The number of patients who were screened for tobacco use at least once within 24 months AND who received tobacco cessation intervention if identified as a tobacco user”. Additionally, we established three numerator definitions for each of the three sub-measures (Table 1). To evaluate cessation intervention, we adhered to the definition of The MU measure where “Cessation counseling intervention includes brief counseling (3 minutes or less), and/or pharmacotherapy”. To identify cessation counseling intervention in dental EHRs, we evaluated the following: a) the use of Codes on Dental Procedures and Nomenclature (CDT) (24) code D1320: “Tobacco counseling for the control and prevention of oral disease”; b) Cessation intervention questions as included in the EHR medical history and tobacco history forms;and c) Pharmacotherapy, following medications included in the prescription module of the dental EHR. Table 2 displays the EHR form names and the relevant questions.
Table 2.
Electronic Health Record Documentation in Participating Sites
| Site 1 | Site 2 | Site 3 | Site 4 | |
|---|---|---|---|---|
| EHR-Forms | Medical history screening (MHS) Medical history (MH) Tobacco history (TH) |
Medical history (MH) | Medical history (MH) | Medical history (MH) |
| Tobacco Screening (SM-1) |
MHS: Any significant Family/Social History (Tobacco, alcohol, recreational drugs)? Yes/No MH: Do you use any tobacco/nicotine products (Cigarette, cigars, pipes, smokeless tobacco)? Yes/No TH: Multiple questions. Patient screened if form was completed. |
MH (Q1): How often do you smoke? MH (Q2): If over 12, do you use or have you used tobacco? (smoking, snuff, chew, bidis) |
MH (Q1): Did you use or have you used tobacco (smoking, snuff, chew, bidis)? MH (Q2): Reviewed Medical History Yes/No and Include date |
MH (Q1): Did you use or have you used tobacco (smoking, snuff, chew, bidis)? MH (Q2): Reviewed Medical History Yes/No and Include date |
| Tobacco Use (SM-2) |
MHS: Any significant Family/Social History (Tobacco, alcohol, recreational drugs)? Yes/No MH: Do you use any tobacco/nicotine products (Cigarette, cigars, pipes, smokeless tobacco)? Yes/No TH: Multiple questions. Form only completed for tobacco users. |
MH (Q1): How often do you smoke? MH (Q2): If over 12, do you use or have you used tobacco? (smoking, snuff, chew, bidis) |
MH (Q1): Did you use or have you used tobacco (smoking, snuff, chew, bidis)? MH (Q2): Reviewed Medical History Yes/No and Include date |
MH (Q1): Did you use or have you used tobacco (smoking, snuff, chew, bidis)? MH (Q2): Reviewed Medical History Yes/No and Include date |
| Tobacco Cessation Intervention (SM-3) | D1320 procedure code1 Pharmacotherapy2 |
D1320 procedure code1 MH (Cessation Counseling Referral): How interested are you in quitting: Very/Somewhat/No Pharmacotherapy2 |
D1320 procedure code1 MH (Cessation Counseling Referral): Assessed interest in quitting. Yes/No If yes, Are you interested in stopping tobacco use? Yes: Please call 1–800-NOBUTTS Pharmacotherapy2 |
D1320 procedure code1 MH: Are you interested in stopping tobacco use? Yes/No. If yes, Cessation Counselling Referral provided Pharmacotherapy2 |
Tobacco counseling for the control and prevention of oral disease
Prescriptions included Chantix® and Zyban® available in the EHR medications mod
Step 4. Manual chart reviews. Two calibrated and independent reviewers at each institution performed manual chart reviews. To assess the calibration among paired reviewers within each institution, we audited 50 random charts and calculated the interrater reliabilityusing Cohen’s kappa coefficient (25). Reviewers discussed and resolved all discrepancies before a single reviewer completed subsequent manual chart reviews.
Step 5. Validity testing - evaluating the performance of the automated query: We evaluated the concordance between the automated query and manual chart reviews by calculating sensitivity, specificity, positive and negative predictive values for each of the sub-measures. Because the primary measure score included calculations from two denominators, we were not able to conduct validity analysis for the primary measure.
Results
We described our results in the subsequent paragraphs following the three aims of our study defined in the Introduction section:
Aim 1. Adapt and revise the specifications of the Meaningful Use NQF 0028 measure originally designed for electronic medical records for electronic dental records: Table 1 described the dental quality measure specifications for the primary measure and each of the three sub-measures, as adapted and revised from electronic medical records. Table 2 presented the names of the EHR forms containing tobacco use information and tobacco-related questions in each of the participating sites.
Aim 2. Evaluate the feasibility and performance of the adapted measure by comparing the measure scores of the automated query to a manual chart review: As the first step to evaluate the feasibility and performance of the adapted measure, we calculated interrater reliability for the first 50 random charts using Cohen’s kappa coefficient (Table 3).. A Cohen’s kappa coefficient of at least 0.80 (κ = 0.80) indicated “high agreement” in all sites except on site 3 for sub-measures 1, 2 and 3, and Site 2 for sub-measures 2 and 3. Reasons for the discrepancies were inaccurate documentation in the EHR. For example, a record may not had an answer for tobacco screening, but reported a date.. In this case, reviewersdiscussed and came to a force decisionconsensus to classify this patient as “not screened”. Overall, sensitivity, specificity, positive and negative predictive values indicated the automated query performed well (Table 3). A Lower sensitivity of 66.7% in site 2 was noted in sub-measure 2 (tobacco use), because a an EHR medical history question assessed both past and current use of tobacco “if over 12, do you use or have you used tobacco?” thus the query identified the patient as a current and past tobacco user., The lower sensitivity of 50% in site 1, sub-measure 3, cessation intervention, resulted from only two patients included in the manual review. Finally, in sub-measure 3, cessation intervention, there was a change in the numbering of the questions in the medical history form in site 4 during 2015 reporting year, which impacted how the query extracted the data. In conclusion, our validity analyses results are relevant and show the importance of well-designed and unambiguous form questions in order to create high-quality data for analysis.
Table 3.
Interrater Reliability and Validity Analysis for the Primary Measure and Sub-measures by Site
| SITE | Kappa values§ | 1Sensitivity | 2Specificity | 3PPV | 4NPV |
|---|---|---|---|---|---|
| Tobacco Screening (Sub-Measure-1) | |||||
| Site 1 308 (0.89)* | k=0.898 | 99.3% (276/278) | 100% (30/30) | 100% (276/276) | 93.8% (30/32) |
| Site 2 203 (0.91)* | k=0.898 | 100% (179/179) | 100% (24/24) | 100% (179/179) | 100% (24/24) |
| Site 3 269 (0.80)* | k=0.730 | 92.6% (213/230) | 100% (39/39) | 100% (213/213) | 69.6% (39/56) |
| Site 4 160 (1.0)* | k=1.000 | 100% (160/160) | - (0/0) | 100% (160/160) | - (0/0) |
| Tobacco Use (Sub-Measure-2) | |||||
| Site 1 235 (0.18)* | k=1.000 | 100% (38/38) | 98.7% (235/238) | 92.7% (38/41) | 100% (235/235) |
| Site 2 127 (0.95)* | k=0.788 | 66.70% (8/12) | 93.4% (156/167) | 42.1% (8/19) | 97.5% (156/160) |
| Site 3 117 (0.09)* | k=0.652 | 94.1% (16/17) | 100% (196/196) | 100% (16/16) | 99.5% (196/197) |
| Site 4 172 (0.19)* | k=0.920 | 94.1% (16/17) | 98.1% (152/155) | 84.2% (16/19) | 99.3% (152/153) |
| Tobacco Cessation Intervention (Sub-Measure-3) | |||||
| Site 1 99 (0.02)* | k=1.000 | 50% (1/2) | 100% (90/90) | 100% (1/1) | 98.9% (90/91) |
| Site 2 149 (0.28)* | k=0.677 | 100% (41/41) | 100% (17/17) | 100% (41/41) | 100% (17/17) |
| Site 3 147 (0.82)* | k=0.657 | 100% (109/109) | 96.9% (31/32) | 99.1% (109/110) | 100% (31/31) |
| Site 4 330 (0.31)* | k=1.000 | 80.3% (110/137) | 100% (182/182) | 100% (110/110) | 87.1% (182/209) |
Sensitivity – when the manual review confirmed that the query correctly identified the patient in the numerator and met the eligibility criteria for each of the sub-measures.
Specificity when the manual review confirmed that the patient, as identified by the query, was not part of the numerator.
Positive Predictive Value (PPV) – when the query confirmed that the patient was part of the numerator as identified by the manual query.
Negative Predictive Value (NPV) – when the query confirmed that the patient was only part of the denominator as defined by the manual query.
Number of charts reviewed manually as determined by sample size calculation and sample proportions (given by the queried measure score)
Kappa values calculated for the first 50 random manual review charts to assess the calibration among paired reviewers within each institution
3. Evaluate the screening rates for tobacco use in our patient population and cessation interventions rates for tobacco users in our dental clinics: Table 4 displayed the demographic characteristics for our study population. In the reporting calendar year of 2015, a total of 143,675 patients met the inclusion criteria.The proportion of males ranged from 41.4% in site 4 to 47.4% in site 3. We had a higher proportion of females across all sites.
Table 4.
Demographic Characteristics for Sites 1 – 4
| Frequency (%) | Site 1 (N3=6309) | Site 2 (N1=3314) | Site 3 (N2=5926) | Site 4 (N4=128126) |
|---|---|---|---|---|
| Gender | ||||
| Male | 2633 (41.7) | 1452 (43.8) | 2808 (47.4) | 53063 (41.4) |
| Female | 3645 (57.8) | 1859 (56.1) | 3117 (52.6) | 75057 (58.6) |
| Unknown* | 31 (0.5) | 3 (0.1) | 1 (0.0) | 6 (0.0) |
| Age Category | ||||
| <=34 | 1502 (23.8) | 1110 (33.5) | 1039 (17.5) | 42951 (33.5) |
| 35–54 | 2211 (35.1) | 1185 (35.8) | 1875 (31.6) | 53616 (41.9) |
| 55–64 | 1297 (20.6) | 532 (16.1) | 1379 (23.3) | 22309 (17.4) |
| 65–74 | 957 (15.2) | 359 (10.8) | 1098 (18.5) | 7213 (5.6) |
| 74–85 | 302 (4.8) | 101 (3.1) | 443 (7.5) | 1713 (1.3) |
| >85 | 40 (0.6) | 27 (0.8) | 92 (1.5) | 324 (0.3) |
| Age, Mean (Standard Deviation) | 49.2 ( 16.6) | 44.9 (16.5) | 53.0 (16.7) | 42.8 (14.8) |
| Race | ||||
| White | 940 (14.9) | 1332 (40.2) | 1183 (20.0) | 57210 (44.7) |
| African-American | 417 (6.6) | 291 (8.8) | 21(3.6) | 2265 (1.8) |
| Native American | 15 (0.24) | 6 (0.2) | 12 (0.2) | 664 (0.5) |
| Asian | 257 (4.1) | 315 (9.5) | 454 (7.7) | 4728 (3.7) |
| Pacific Islander | 1 (0.02) | 2 (0.1) | 20 (0.3) | 578 (0.5) |
| Other | 0 | 541 (16.3) | 154 (2.6) | 5792 (4.5) |
| Unknown | 4679(74.2) | 827 (25.0) | 3888 (65.6) | 56889 (44.4) |
| Ethnicity | ||||
| Hispanic | 471 (7.5) | 9 (0.3) | 314 (5.3) | 477 (0.4) |
| Non-Hispanic | 36 (0.6) | 13 (0.4) | 121 (2.0) | 5611 (4.4) |
| Unknown | 4172 (66.1) | 3292 (99.3) | 5491 (92.7) | 122038 (95.2) |
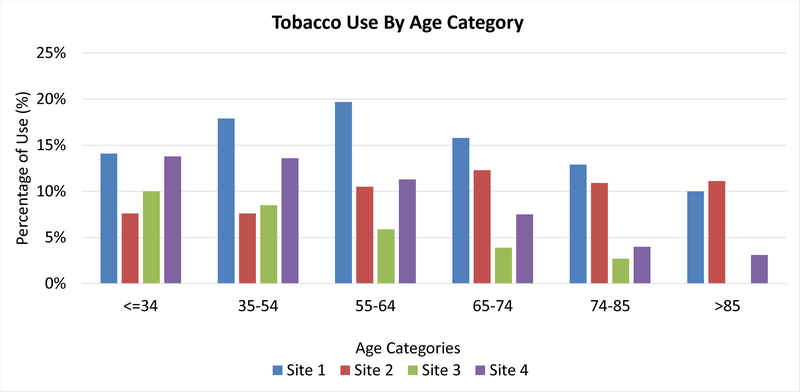
The mean age of our patient population was 49.2; 44.9; 53.0 and 42.8 for Site 1, Site 2, Site 3 and Site 4 respectively. Figure 1 shows the distribution of tobacco use by age. In our study population, tobacco use was higher among patients in the age categories younger than 74–85 years. For example, among patients at Site 1, the majority of tobacco users are 55–64 years, while at Site 3 they are 35–54 age category. Our sites show a racial and ethnically diverse study population; however, our results need to be interpreted with caution, as, with exception of Site 2, over 60% of our patients did not have race and ethnicity recorded in the EHR (Table 4).
Figure 1.
Tobacco Use by Age Category
Table 5 displays the automated query measure scores, calculated as the ratio of the Numerator/Denominator for each site, primary measure, and each sub-measure. The p-value <0.0001 indicated measure scores differed across sites. The primary measure score was 87.4% (95% CIs; 87.2–97.5). On the sub-measure analysis, our results show that 98.9% of patients were screened for tobacco use (sub-measure 1), with measure scores ranging from 79.6% in Site 3, to 99.9% in Site 4 (Table 5). The sub-measure 2 overall score indicated that 12.8% of our patients are tobacco users, below the National cigarette use prevalence of 15.1% (26). Site 1 showed a higher percentage of smokers (18.8%) when compared to sites 1, 2 and 3. Finally, sub-measure 3 indicated significant variations across sites, with percentages ranging from 1% - 81%.
Table 5.
Automated Query Measure Scores by Site
| SITE | NUMERATOR/DENOMINATOR | QUERY MEASURE SCORE (95% CI†) |
|---|---|---|
| Primary Measure | ||
| Site 1 | 4561/6309 | 72.3% (95% CI, 71.2–73.4) |
| Site 2 | 2755/3314 | 83.1%; (95% CI, 81.8–84.4) |
| Site 3 | 4587/5296 | 77.4%; (95% CI, 76.3–78.5) |
| Site 4 | 113080/128126 | 88.3%; (95% CI, 88.1–88.5) |
| Total | 124983/143045 | 87.4% (95% CI, 87.2 – 87.5) |
| χ2 Test Statistic (df=3)* | 1902.9 | |
| Tobacco Screening (Sub-Measure 1) | ||
| Site 1 | 5610/6309 | 88.9%; (95% CI, 88.1–89.7) |
| Site 2 | 3028/3314 | 91.4%; (95% CI, 90.4–92.4) |
| Site 3 | 4720/5296 | 79.6%; (95% CI, 78.5–80.7) |
| Site 4 | 128111/128126 | 99.9%; (95% CI, 99.9–99.9) |
| Total | 141469/143045 | 98.9%; (95% CI, 98.8–99.0) |
| χ2 Test Statistic (df=3)* | 34165.3 | |
| Tobacco Use (Sub-Measure 2) | ||
| Site 1 | 1055/5610 | 18.8%; (95% CI, 17.8–19.8) |
| Site 2 | 288/3028 | 9.5%; (95% CI, 8.5–10.5) |
| Site 3 | 400/4720 | 8.5%; (95% CI, 7.7–9.3) |
| Site 4 | 16375/128111 | 12.8%; (95% CI, 12.2–13.4) |
| Total | 18118/141469 | 12.8%; (95% CI, 12.6–13.0) |
| χ2 Test Statistic (df=3)* | 260.8 | |
| Tobacco Cessation Counseling (Sub Measure 3) | ||
| Site 1 | 16/1055 | 1.8%; (95% CI, 0.1–2.6) |
| Site 2 | 80/288 | 27.8%; (95% CI, 22.6–33.0) |
| Site 3 | 326/400 | 81.5%; (95% CI, 77.7–85.3) |
| Site 4 | 5113/16375 | 31.2%; (95% CI, 30.5–31.9) |
| Total | 5535/18118 | 30.5% (95% CI, 30.0–31.2) |
| χ2 Test Statistic (df=3)* | 904.7 |
P-value <0.001
Confidence Interval
In summary, the primary measure score is a result of the combination of sub-measures 1, 2 and 3. A high measure score of 87.1% can be misleading, as it does not reflect the relevant details of each of the participating sites that will allow for identification of gaps in clinical practice and opportunities for quality improvement.
Discussion
The Centers for Medicare & Medicaid Services (CMS) describes quality measures in part as tools that help “measure or quantify healthcare processes, outcomes, patient perceptions, and organizational structure and/or systems.”(21) Quality measures should inform clinicians where improvement is needed (27) in an effort to improve care to be more effective, safe, efficient, patient-centered, equitable, and/or timely. MU Stage 1 years 1 and 2 was implemented in primary care setting to identify gaps in clinical practice and opportunities for improvement. After six-months of a quality improvement plan, 76% of the primary care practices reached the goal of providing tobacco use screening and cessation interventions to 90% of the patients(28).
The methodology and quality measure specifications described in this paper are generalizable and provides tools for dental professionals to use data available in the EHR to identify opportunities for improvement that will likely benefit our patients. Specifically, the analysis of sub-measures stratification highlighted how “tobacco use screening” and “tobacco cessation counseling” are not implemented at equal levels at the participating sites. This study shows that using longitudinal patient-level data readily available in the EHR allows for the measurement and quantification of specific healthcare processes and outcomes (tobacco use screening and cessation counseling intervention). Additionally, once an institution develops and implement an improvement plan, rerunning the script, will allow the organization to measure if this specific care process has become more effective and timely. As such, our dental quality measure (DQM) meets the definition of a quality measure.
Our study employed a process-of-care quality measure and provided information on identified to identify gaps in practice that can inform future improvement efforts. Study sites results showed significant variability. For example, Site 3 patients showed the lowest rates of tobacco use and highest rates of cessation referrals to a quit line. We surmise that low rates of tobacco use in this state are likely the result of public health initiatives implemented over a decade ago.(29) We postulate that possible reasons for the low cessation intervention rates at Site 1, as calculated by the automated query, may include the fact that referral to cessation programs was not documented in a structured format in the medical history form, and thus not captured in the automated query, and lack of a formal tobacco cessation protocol. We also noted the very low use of pharmacological intervention for cessation protocols across all sites. A common finding across all sites suggest that in dental clinics cessation referral protocols appear to be limited to behavioral referral interventions and that dentists may be uncomfortable with the management of patients on tobacco-cessation medications.
Healthy People 2020 (1) includes an oral health objective to increase “the proportion of adults who received information from a dentist or dental hygienist focusing on reducing tobacco use or on smoking cessation in the past year” from 10.5% to 13.5%. Our four study sites showed excellent results with the Healthy People 2020 objective on tobacco screening, with rates of screening patients for tobacco use between 79.3% −99.9% across all sites. Results for tobacco cessation programs showed larger variation, from a low of 1% to a high of 81%. Tobacco cessation counseling and referral is an endorsed and evidence-based practice, and hence tobacco users should be offered information and cessation management as standard practice in annual or semi-annual dental examinations. The lack of financial reimbursement is often claimed as a barrier by dental professionals for providing cessation treatment. Donna Shelly et al. noted that “lack of data on intervention efficacy” is a main reason why tobacco cessation insurance reimbursement increased for medical offices but not dental clinics, even though the relevance of providing tobacco cessation in dental offices was well recognized.(30) Therefore, results from quality measures research evaluations such as this project, can be a valuable contribution towards providing data to inform decision-makers.
Tobacco cessation is a prime example of an intervention that benefits from inter-professional practice as repeated cessations provided by multiple providers from different disciplines can make a difference. Quitting is hard and different tobacco users respond to different triggers. Thus, to support cessation intervention in dental institutions, collaborations between dentists, dental hygienists and physicians is crucial—an approach that dental education institutions may want to initiate with emerging health profession students in inter-professional education and inter-professional practice (IPE/IPP) experiences. Such efforts are further facilitated when dental and medical EHRs are not only designed interoperable, but also have meaningful and streamlined reminder and notification functions that ensure an effective intervention strategy across provider groups; e.g. sharing the burden of monitoring side effects of medications prescribed as quit-smoking aids.
In conclusion, our results show that a meaningful use measure can successfully evaluate quality of care related to tobacco screening, use and cessation interventions, using data from dental EHRs. There are opportunities for dental professionals to deliver comprehensive cessation interventions including counseling and, if indicated, cessation medications, and position themselves as leaders in tobacco screening and tobacco cessation. The development and distribution of impactful continuing education courses on appropriate training will need to provide the knowledge and develop the skills for dental professionals to deliver tobacco cessation intervention. Results of implementation of evidence-based tobacco cessation strategies in dental practices may further improve if the dental workforce receives additional training and practitioners position themselves as an integral member of the inter-professional team with the ultimate goal of improving the oral and general health of our patients.
Limitations
There are several limitations to this study. First, quality evaluation is dependent on the data available for measurement (31). It was challenging to make adaptations in the measure specifications to reflect and include different medical history and screening-form questions at each institution. When clinical information is not captured in a structured, standardized format (i.e. treatment codes), it lowers the validity of the quality measure evaluation. Second, although patterns of tobacco use are changing(2) we did not collect information on newer and increasingly popular tobacco products, such as electronic cigarettes or water pipes because they were not captured in the EHRs during the reporting years (2014 and 2015). In future quality measure research, it may be appropriate to include emerging tobacco products to screen for use and provide appropriate counseling intervention. In addition, measure specifications can be adapted to include a population younger than 18 years of age. Third, the cross-sectional design of this process-of-care quality measure did not allow for the evaluation of barriers for cessation intervention within and across the sites, and if cessation-counseling referrals, included in this evaluation, resulted in higher rates of quitting.
Conclusion
This research study demonstrated the successful testing, adaptation, and validity of an EHR-based, tobacco screening and cessation quality measure originally designed for medical practices. In evaluating tobacco screening, use and cessation interventions in three dental schools and a large group practice we noted that good rates of tobacco screening in the dental office, however that tobacco cessation efforts are inconsistent across different dental organizations.
Acknowledgments
Research reported in this publication was supported in part by award R01DE024166 from the National Institute of Dental and Craniofacial Research (NIDCR) of the National Institutes of Health. The content is solely responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Source of support:
Research reported in this publication was supported in part by award R01DE024166 from the National Institute of Dental and Craniofacial Research, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Name of group and date and presentation: American Association for Dental Research Annual Meeting & Exhibition. Fort Lauderdale, Fla., USA - March 23, 2018
Knowledge Transfer Agreement: The results of this study can be used by clinicians when evaluating quality of care related to tobacco screening, use and cessation interventions, using data from dental electronic health records. Results from quality evaluation research on tobacco screening and cessation, could lead to improved oral and general health of our patients.
Footnotes
Declaration of Conflicting Interests:
The author(s) declare that they have no competing interests.
References
- 1.Healthy People 2020. Increase the proportion of adults who received information from a dentist or dental hygienist focusing on reducing tobacco use or on smoking cessation in the past year Washington, DC [Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/oral-health/objectives.
- 2.Couch ET, Chaffee BW, Gansky SA, Walsh MM. The changing tobacco landscape: What dental professionals need to know. Journal of the American Dental Association. 2016;147(7):561–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amemori M, Korhonen T, Michie S, Murtomaa H, Kinnunen TH. Implementation of tobacco use cessation counseling among oral health professionals in Finland. J Public Health Dent. 2013;73(3):230–6. [DOI] [PubMed] [Google Scholar]
- 4.Gordon JS, Lichtenstein E, Severson HH, Andrews JA. Tobacco cessation in dental settings: research findings and future directions. Drug Alcohol Rev. 2006;25(1):27–37. [DOI] [PubMed] [Google Scholar]
- 5.Rindal DB, Rush WA, Schleyer TK, Kirshner M, Boyle RG, Thoele MJ, et al. Computer-assisted guidance for dental office tobacco-cessation counseling: a randomized controlled trial. Am J Prev Med. 2013;44(3):260–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jannat-Khah DP, McNeely J, Pereyra MR, Parish C, Pollack HA, Ostroff J, et al. Dentists’ self-perceived role in offering tobacco cessation services: results from a nationally representative survey, United States, 2010–2011. Preventing chronic disease. 2014;11:E196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prakash P, Belek MG, Grimes B, Silverstein S, Meckstroth R, Heckman B, et al. Dentists’ attitudes, behaviors, and barriers related to tobacco-use cessation in the dental setting. J Public Health Dent. 2013;73(2):94–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu S, Pallonen U, McAlister AL, Howard B, Kaminski R, Stevenson G, et al. Knowing how to help tobacco users. Dentists’ familiarity and compliance with the clinical practice guideline. J Am Dent Assoc. 2006;137(2):170–9. [DOI] [PubMed] [Google Scholar]
- 9.Allen SR, Kritz-Silverstein D. Dental vs. Medical Students’ Comfort with Smoking Cessation Counseling: Implications for Dental Education. J Dent Educ. 2016;80(8):959–65. [PubMed] [Google Scholar]
- 10.Singleton JA, Carrico RM, Myers JA, Scott DA, Wilson RW, Worth CT. Tobacco cessation treatment education for dental students using standardized patients. J Dent Educ. 2014;78(6):895–905. [PubMed] [Google Scholar]
- 11.Christen AG. Tobacco cessation, the dental profession, and the role of dental education. J Dent Educ. 2001;65(4):368–74. [PubMed] [Google Scholar]
- 12.Shibly O Effect of tobacco counseling by dental students on patient quitting rate. J Dent Educ. 2010;74(2):140–8. [PubMed] [Google Scholar]
- 13.Kalenderian E, Walji M, Ramoni RB. “Meaningful use” of EHR in dental school clinics: how to benefit from the U.S. HITECH Act’s financial and quality improvement incentives. J Dent Educ. 2013;77(4):401–15. [PubMed] [Google Scholar]
- 14.Kalenderian E, Ramoni RL, White JM, Schoonheim-Klein ME, Stark PC, Kimmes NS, et al. The development of a dental diagnostic terminology. J Dent Educ. 2011;75(1):68–76. [PMC free article] [PubMed] [Google Scholar]
- 15.Tokede O, White J, Stark PC, Vaderhobli R, Walji MF, Ramoni R, et al. Assessing use of a standardized dental diagnostic terminology in an electronic health record. J Dent Educ. 2013;77(1):24–36. [PMC free article] [PubMed] [Google Scholar]
- 16.White JM, Kalenderian E, Stark PC, Ramoni RL, Vaderhobli R, Walji MF. Evaluating a dental diagnostic terminology in an electronic health record. J Dent Educ. 2011;75(5):605–15. [PMC free article] [PubMed] [Google Scholar]
- 17.Kalenderian E, Tokede B, Ramoni R, Khan M, Kimmes N, White J, et al. Dental clinical research: an illustration of the value of standardized diagnostic terms. J Public Health Dent. 2016;76(2):152–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramoni R, Walji M, Kim S, Tokede O, McClellan L, Simmons K, et al. Attitudes toward and beliefs about the use of a dental diagnostic terminology. Journal of the American Dental Association. 2015;146(6):390–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramoni RB, Etolue J, Tokede O, McClellan L, Simmons K, Yansane A, et al. Adoption of dental innovations: The case of a standardized dental diagnostic terminology. J Am Dent Assoc. 2017;148(5):319–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhardwaj A, Ramoni R, Kalenderian E, Neumann A, Hebballi NB, White JM, et al. Measuring up: Implementing a dental quality measure in the electronic health record context. Journal of the American Dental Association. 2016;147(1):35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services. National Quality Forum 0028. Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention Baltimore, MD: Department of Health and Human Services; 2014. [Available from: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/2014_CQM_AdultRecommend_CoreSetTable.pdf. [Google Scholar]
- 22.Neumann A, Kalenderian E, Ramoni R, Yansane A, Tokede B, Etolue J, et al. Evaluating quality of dental care among patients with diabetes: Adaptation and testing of a dental quality measure in electronic health records. J Am Dent Assoc. 2017;148(9):634–43 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cochran WG. Sampling techniques 3rd ed. ed. New York: John Wiley & Sons; 1977. [Google Scholar]
- 24.American Dental Association. Code on Dental Procedures and Nomenclature (CDT Code 2017). Chicago, IL: 2017. p. 180. [Google Scholar]
- 25.Cohen J A coefficient of agreement for nominal scales. Educational and Psychological Measurement. 1960;20(1):37–46. [Google Scholar]
- 26.Centers for Disease Control and Prevention. State Tobacco Activities Tracking & Evaluation (STATE) System. Map of Current Cigarette Use Among Adults (Behavioral Risk Factor Surveillance System) 2015. 2014.
- 27.O’Connor PJ, Bodkin NL, Fradkin J, Glasgow RE, Greenfield S, Gregg E, et al. Diabetes performance measures: current status and future directions. Diabetes care. 2011;34(7):1651–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.gov; HI. Improving Tobacco Use Screening and Smoking Cessation in a Primary Care Practice 2013. [Available from: https://www.healthit.gov/case-study/improving-tobacco-use-screening-and-smoking-cessation-primary-care-practice.
- 29.Messer K, Pierce JP, Zhu SH, Hartman AM, Al-Delaimy WK, Trinidad DR, et al. The California Tobacco Control Program’s effect on adult smokers: (1) Smoking cessation. Tob Control. 2007;16(2):85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shelley D, Wright S, McNeely J, Rotrosen J, Winitzer RF, Pollack H, et al. Reimbursing dentists for smoking cessation treatment: views from dental insurers. Nicotine Tob Res. 2012;14(10):1180–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kahn MG, Brown JS, Chun AT, Davidson BN, Meeker D, Ryan PB, et al. Transparent reporting of data quality in distributed data networks. EGEMS (Wash DC) 2015;3(1):1052. [DOI] [PMC free article] [PubMed] [Google Scholar]