Key Points
Question
Is the incidence of myocardial infarction affected by different weather conditions?
Findings
In this nationwide population-based study, a higher incidence of myocardial infarction in Sweden was observed at days with low air temperature, low atmospheric air pressure, high wind velocity, and shorter sunshine duration.
Meaning
This study adds to knowledge on the role of weather as potential trigger of myocardial infarction.
Abstract
Importance
Whether certain weather conditions modulate the onset of myocardial infarction (MI) is of great interest to clinicians because it could be used to prevent MIs as well as guide allocation of health care resources.
Objective
To determine if weather is associated with day-to-day incidence of MI.
Design, Setting, and Participants
In this prospective, population-based and nationwide setting, daily weather data from the Swedish Meteorological and Hydrological Institute were extracted for all MIs reported to the Swedish nationwide coronary care unit registry, Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART), during 1998 to 2013 and then merged with each MI on date of symptom onset and coronary care unit. All patients admitted to any coronary care unit in Sweden owing to MI were included. A total of 280 873 patients were included, of whom 92 044 were diagnosed as having ST-elevation MI. Weather data were available for 274 029 patients (97.6%), which composed the final study population. Data were analyzed between February 2017 and April 2018.
Exposures
The nationwide daily mean air temperature, minimum air temperature, maximum air temperature, wind velocity, sunshine duration, atmospheric air pressure, air humidity, snow precipitation, rain precipitation, and change in air temperature.
Main Outcomes and Measures
The nationwide daily counts of MI as outcome.
Results
In 274 029 patients, mean (SD) age was 71.7 (12) years. Incidence of MI increased with lower air temperature, lower atmospheric air pressure, higher wind velocity, and shorter sunshine duration. The most pronounced association was observed for air temperature, where a 1-SD increase in air temperature (7.4°C) was associated with a 2.8% reduction in risk of MI (unadjusted incidence ratio, 0.972; 95% CI, 0.967-0.977; P <.001). Results were consistent for non–ST-elevation MI as well as ST-elevation MI and across a large range of subgroups and health care regions.
Conclusions and Relevance
In this large, nationwide study, low air temperature, low atmospheric air pressure, high wind velocity, and shorter sunshine duration were associated with risk of MI with the most evident association observed for air temperature.
This population-based study investigates whether weather is associated with day-to-day incidence of myocardial infarction in Sweden.
Introduction
A circadian variation in acute myocardial infarction (MI) and seasonality in cardiovascular disease mortality has been previously reported.1,2,3,4,5 In an early report from 1926, Wolff and White6 observed that most cases of coronary thrombosis in New England occurred during winter. Several reports have confirmed this finding and have proposed a possible role of environmental factors on the occurrence of MI.
In the last decades, evidence linking the incidence of MI to colder temperatures and snow has been published.7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22 However, most studies have used surrogate variables, such as International Statistical Classification of Diseases, Tenth Revision codes, as indicators of MI, and many studies have only looked at air temperature and snow; other meteorological parameters have not been as widely investigated.
The objective of this study was to investigate day-to-day weather and occurrence of MI in Sweden using data from the Swedish Meteorological and Hydrological Institute (SMHI) and the Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART). By combining clinical data with weather station meteorologic variables collected in proximity to coronary care units (CCUs), we were able to investigate the associations of all major weather parameters and risk of MI in a nationwide study, covering 16 years of MI data.
Methods
National Registries
The SWEDEHEART registry enrolls all consecutive patients with symptoms suggestive of an acute coronary syndrome admitted to a coronary intensive care unit or coronary catheterization laboratories in Sweden.23 Information on background characteristics, such as age, body mass index, smoking status, and electrocardiographic findings, as well as other examinations, interventions, complications, discharge medications, and diagnoses, were collected prospectively. Myocardial infarction diagnosis was set based by the treating physician’s assessment of patient at discharge.
Meteorologic data were obtained from SMHI, a Swedish government agency operating within the Ministry of Environment and Energy. The SMHI registers data from 132 weather stations scattered across Sweden. The collected data are readily available for research purposes and can be downloaded from the agency’s website (http://www.smhi.com).
Study Design and Population
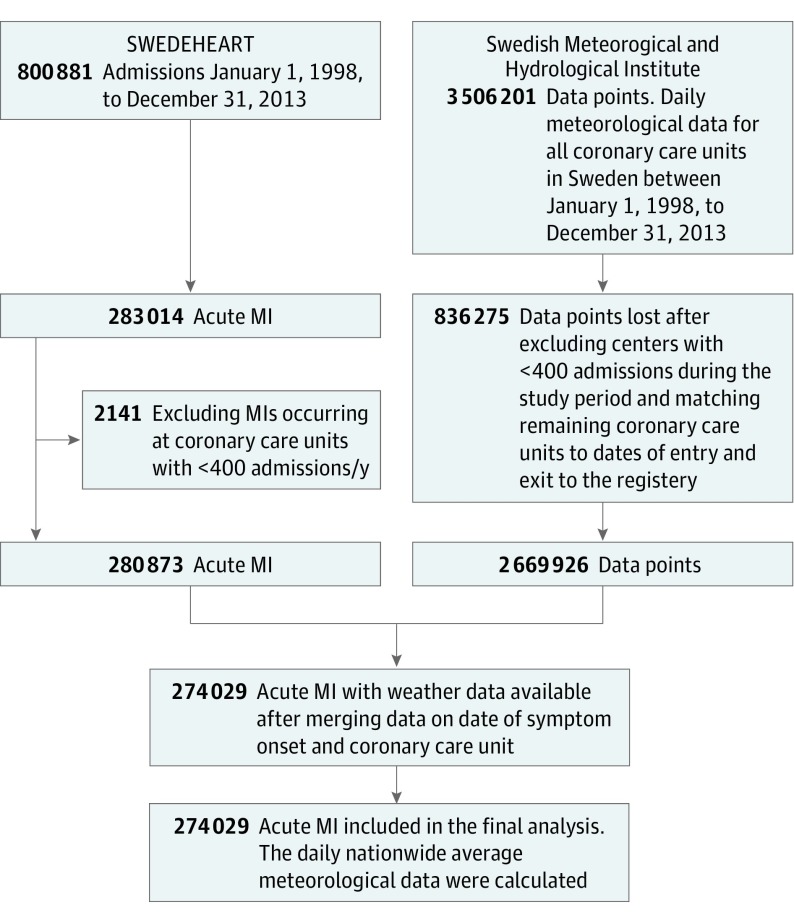
A flowchart depicting the data management process and study design is presented in Figure 1. The study period was set to January 1, 1998, to December 31, 2013, and daily data on air temperature, minimum air temperature, maximum air temperature, wind, sunshine duration, atmospheric air pressure, air humidity, snow, and rain precipitation were extracted from the SMHI database for each city with a CCU in Sweden during this period. Change in air temperature was calculated as the difference between maximum and minimum air temperature, and effective air temperature is the perceived temperature taking into consideration wind velocity and was calculated using the Osczevskis and Bluestein equation available on the SMHI website: T-eff = 13.12 + 0.6215 × T − 13.956 × v0.16 + 0.48669 × T × v0.16, where T is temperature and v is wind velocity. This formula is only valid for temperatures less than 10°C, and days with higher temperatures were considered as missing (20%). All MI events admitted to a CCU were included. Cities with CCUs admitting less than 400 patients with MI during the entire study period were excluded to minimize outliers and include a more homogenous group of CCUs to improve data quality. Data were then combined with SWEDEHEART data using date of symptom onset and city of admission. A total of 2 669 926 weather data points were merged to a total of 280 873 patients with MI enrolled during the study period. Nationwide and regional means of each weather parameter were then calculated and studied with regard to MI and subtypes of MI: ST-elevation MI (STEMI) and non–ST-elevation MI (NSTEMI). The primary analysis was air temperature with regard to total number of MIs. Secondary analyses were other weather variables with regard to total number of MIs, STEMI, and NSTEMI. Regional analyses were conducted for each major health care region (South, Southeast, West, Stockholm, Uppsala/Orebro, and North). Lagged analyses of 1, 3, 5, and 7 days were conducted as exploratory analyses together with seasonal analyses. Season was defined as quartile of a year and divided into January to March, April to June, July to September, and October to December. This study adheres to the STROBE guidelines for observational studies. The regional ethical review board at Lund University Hospital approved the study. The SWEDEHEART registry is a nationwide quality registry and all patients are admitted without the need for any consent. However, all patients have the right to be removed from the registry if they wish so. Therefore, the review board did not ask for patient consent to be obtained.
Figure 1. Data Collection and Data Management.
All acute myocardial infarctions (MIs) within the Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART) registry between 1998 and 2013 were included. Weather data were then merged with each MI on date of symptom onset and coronary care unit. Because a nationwide daily mean of weather parameters was calculated, weather data from small cities admitting less than 400 MIs during the study period were omitted.
Statistical Analyses
Continuous variables are presented as mean (SD). Categorical variables are displayed as counts and percentages. A Poisson regression model was fitted as the primary statistical model to assess the independency of each weather parameter, with daily counts of MI as outcome and weather parameters as predictors. Zero inflation was not an issue in the nationwide or regional analyses. However, overdispersion was present, and a negative binomial regression model was used instead. Univariable models were assessed for each weather parameter as a continuous variable as well as a multivariable model using minimum air temperature, precipitation, air humidity, air pressure, wind velocity, change in air temperature, and sunshine duration, with daily counts of MI as outcome. Snow was analyzed separately during the winter season (October through March) in univariable as well as multivariable analyses. Results from regression analyses were reported as incidence rate ratios (IRRs) and interpreted as change for 1-SD increase of weather parameter. For visual assessment, smoothed conditional mean plots were plotted showing the nationwide incidence rates per day in association with daily weather condition. A conversion formula of daily incidence rates to incidence rates per 100 000 persons per year with a calculation example can be found in the eAppendix in the Supplement. Family-wise error rate was applied using the Hochberg method to control for type 1 errors owing to multiple testing. The main analyses, regional, seasonal, lagged, sensitivity, and subgroups analyses were adjusted separately within strata (total MI, NSTEMI, and STEMI). All statistical analyses were performed using R, version 3.2.2 (The R Foundation for Statistical Computing) and Stata, version 14.1 (StataCorp). A 2-sided P value less than .05 was considered statistically significant.
Subgroups
The primary end point was explored in predefined subgroups. These were men vs women, 75 years and older vs younger than 75 years, current smoker vs nonsmoker, diabetes mellitus vs no diabetes mellitus, hypertension vs no hypertension, previous coronary artery disease vs no previous coronary artery disease, as well as MIs occurring in patients with previous medications, ie, calcium inhibitors, β-blockers, aspirin, statin, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, and diuretics.
Sensitivity Analysis
Sensitivity analyses adjusted for day of week as well as year to control for trends in MI during the study period were conducted. We also performed an analysis adjusted for time of year, with calendar weeks as a categorical variable to control for potential behavioral factors. Air pollution has been suggested as a trigger of MI and could potentially bias the results of weather. To assess independency of weather variables on risk of MI, sensitivity analyses controlling for major air pollutant levels were conducted. Hourly data on carbon monoxide, nitrogen oxide, nitrogen dioxide, particulate matter 10 mm or less, and ozone were collected from the Swedish Environmental Research Institute for the 3 major urban cities in Sweden: Stockholm, Gothenburg, and Malmo. The daily sum of carbon monoxide, nitrogen oxide, nitrogen dioxide, particulate matter 10 mm or less, and ozone was calculated independently for each city and merged with the MI and weather data on day of symptom onset and city. The mean daily sum of carbon monoxide, nitrogen oxide, nitrogen dioxide, particulate matter 10 mm or less, and ozone; weather variables; and the daily sum of MI for all 3 cities were then calculated and analyzed as previously described.
Results
Patient Characteristics
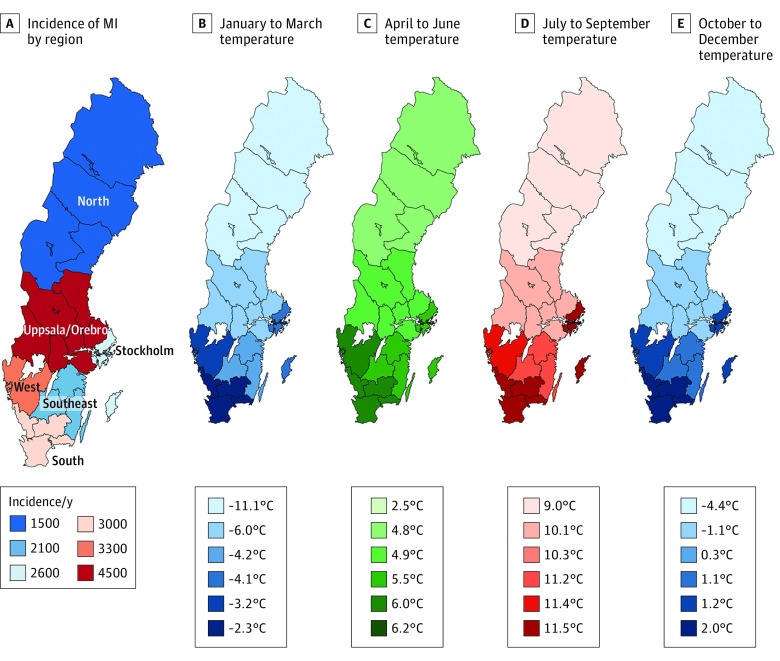
Weather data were available for 274 029 patients (97.6%), which composed the final study population. A map of Sweden depicting the annual incidence rate of MI for each region is presented in Figure 2. Of the total study population, 92 044 were diagnosed as having STEMI. The mean (SD) age was 71.7 (12) years, with patients with STEMI being slightly younger. Patients with NSTEMI had higher rates of kidney dysfunction, diabetes, hypertension, coronary artery disease, MI, previous percutaneous coronary intervention, previous coronary artery bypass graft, chronic heart failure, and stroke, with an accompanying increased number of cardiovascular medications (eTable 1 in the Supplement). Conservative treatment was more common in the NSTEMI group, while revascularization was more often used in the STEMI group.
Figure 2. Incidence of Myocardial Infarction (MI) and Temperature Variation by Season.
A map of Sweden stratified by the 6 health care regions in the country. A, Incidence of myocardial infarction per year. B-E, Temperature variation for each season and health care region.
Meteorologic Characteristics
Minimum air temperature for each season and region is presented in Figure 2. Remaining meteorologic variables for Sweden as well as each health care region are presented in eTable 2 in the Supplement.
End Points
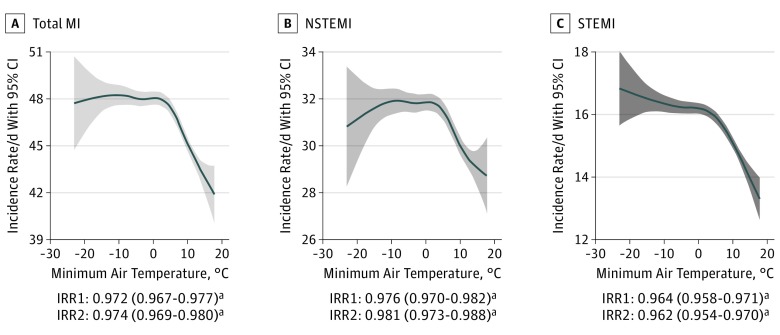
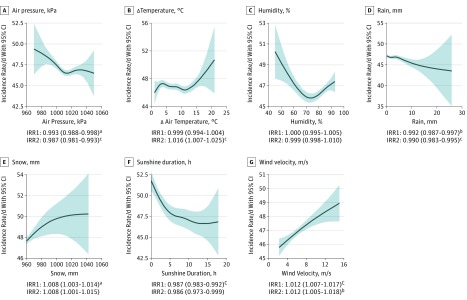
Minimum air temperature was negatively associated with MI, with similar results obtained with mean and maximum air temperature. A 1-SD increase (7.4°C) in minimum air temperature was associated with a 2.8% reduction in MI (unadjusted IRR, 0.972; 95% CI, 0.967-0.977; P <.001). Results were consistent after adjustment for other weather parameters and after stratifying into NSTEMI and STEMI (Figure 3). Sunshine duration was negatively associated with overall MI (Figure 4), but no association was observed in the multivariable analyses of STEMI (eFigure 1 in the Supplement). Higher precipitation and air pressure were both negatively associated with STEMI (eFigure 1 in the Supplement), with a minor risk increase of MI in both univariable as well as multivariable analyses (eFigure 1 in the Supplement). A positive association was observed for wind velocity, with a small increase in IRR for MI (Figure 4). Change in air temperature was associated with increased risk of overall MI (Figure 4) and NSTEMI in multivariable analyses but not STEMI (eFigure 1 in the Supplement).
Figure 3. Nationwide Daily Incidence Rate of Myocardial Infarction (MI) by Air Temperature.
Smoothed conditional mean plots visualizing the variation of daily nationwide incidence rates of MI with 95% CI at different temperatures. Unadjusted and adjusted incidence rate ratio (IRR) and 95% CI from regression analyses are presented. Results from the regression analyses are interpreted as change per increase in standard deviation (7.4°C). IRR1 indicates univariable model; IRR2, multivariable model; NSTEMI, non–ST-elevation MI; and STEMI, ST-elevation MI.
aP < .001.
Figure 4. Nationwide Daily Incidence Rate of Myocardial Infarction by Air Pressure, Change in Temperature, Humidity, Precipitation, Sunshine Duration, and Wind Velocity.
Smoothed conditional mean plots visualizing the variation of incidence rates of myocardial infarction with 95% CI by different weather parameters. Unadjusted and adjusted incidence rate ratio (IRR) and 95% CI from regression analyses are presented with each graph. Results from the regression analyses are interpreted as change per increase in standard deviation. One standard deviation for air pressure, 10.9 kPa; change in temperature (Δ temperature), 3.4°C; humidity, 9.6%; rain, 2.6 mm; snow, 0.25 mm; sunshine duration, 4.2 hours; wind velocity, 1.9 m/s. IRR1 indicates univariable model; IRR2, multivariable model; NSTEMI, non–ST-elevation myocardial infarction; and STEMI, ST-elevation myocardial infarction.
aP < .05.
bP < .01.
cP < .001.
Regional Analyses
Air temperature was negatively associated with risk of MI and remained significant after stratifying into NSTEMI and STEMI in all health care regions except in the north (eFigure 2 and eTable 3 in the Supplement). Wind velocity and snow precipitation were the only weather parameters associated with higher risk of MI, NSTEMI, and STEMI in the north, with the highest association observed for wind velocity and NSTEMI (unadjusted IRR, 1.077; 95% CI, 1.055-1.098; P <.001) (eTable 3 in the Supplement). Results for wind velocity in the north health care region were consistent after adjustment for other weather parameters, while snow did not reach statistical significance (eTable 3 in the Supplement).
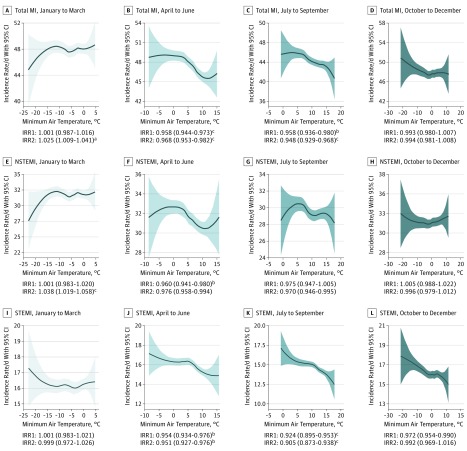
Seasonal Analyses
With the exception of the coldest season (January-March), consistent results were observed, with a negative association for air temperature and risk of MI, with the highest association observed during July through September and the highest associated risk observed in STEMI. This translated into a 9.5% reduction in STEMI for each increase in standard deviation in air temperature (3.1°C) (adjusted IRR, 0.905; 95% CI, 0.873-0.938; P <.001) (eTable 3 in the Supplement). However, the coldest season (January-March) showed a reverse association compared with the results previously described, with a positive association of increased air temperature and MI, owing to increased rates of NSTEMI (Figure 5 and eTable 3 in the Supplement). In contrast, sunshine duration during January through March was negatively associated with risk of NSTEMI but not with STEMI (eTable 3 in the Supplement).
Figure 5. Nationwide Daily Incidence Rate of Myocardial Infarction (MI) by Air Temperature Stratified by Season of the Year.
Smoothed conditional mean plots visualizing the variation of nationwide daily incidence rates of MI at different temperatures by season. Unadjusted and adjusted incidence rate ratio (IRR) and 95% CI from regression analyses are presented. Results from the regression analyses are interpreted as change per increase in standard deviation. One standard deviation of air temperature in January through March, 5.2°C; April through June, 4.4°C; July through September, 3.1°C; October through December, 5.4°C. Seasonal analyses of remaining weather parameters are shown in eTable 3 in the Supplement. IRR1 indicates univariable model; IRR2, multivariable model; NSTEMI, non–ST-elevation MI; and STEMI, ST-elevation MI.
aP < .05.
bP < .01.
cP < .001.
Lagged Effects and Results Across Subgroups
Lagged analyses of 1, 3, 5, and 7 days showed consistent results with negative association of MI, NSTEMI, and STEMI with increased temperature, with similar effect estimates to nonlag analyses (eFigure 3 and eFigure 4 in the Supplement). The primary end point was investigated in a variety of subgroups with consistent results, with an associated higher risk of MI with lower air temperatures (eTable 4 in the Supplement).
Sensitivity Analyses
Consistent results were observed after adjustment for long-term trends in MI and day of week (eTable 3 in the Supplement). After adjustment for air pollutant levels, only air temperature remained significantly associated with risk of MI. Air pressure and change in air temperature were associated with risk of MI after adjusting for calendar week but not air temperature.
Discussion
In this large, nationwide study covering 16 years of MI and weather data, low air temperature, low atmospheric air pressure, high wind velocity, and shorter sunshine duration were associated with risk of MI. The strongest association was observed for air temperature, with a higher incidence of MI on days with air temperatures less than 0°C, with rates of MI declining when temperatures rose to greater than 3°C to 4°C. The results were consistent across a large range of subgroups and health care regions. Seasonal analyses showed more pronounced association of air temperature during warmer seasons, and regional analyses showed a pronounced and positive association of MI with snow and wind in the northernmost region.
Whereas a few studies have previously reported similar findings with regard to air temperature, most of these studies have been geographically limited, with a relatively small sample size and/or use of administrative data with International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes, ambulance records, and death certificates as surrogate for MI.10,11,13,14,15,17,18,19,20,21,22,24 To our knowledge, this study not only constitutes the largest of its kind but also the only one investigating a wider spectrum of weather variables to clinical data with electrocardiographic and biomarker-positive MI from a well-known nationwide register. We performed a number of subgroup, regional, seasonal, and sensitivity analyses to complement our primary analysis. Our results not only suggest that weather is independently associated with the incidence of MI but also that the association may differ with regard to season and electrocardiographic subtypes.
A number of physiologic mechanisms have been proposed to explain the association of cold weather and MI, among which, coronary vasoconstriction is the most probable cause. Cold as a pressor for coronary vasoconstriction was proposed as early as in the 1970s, and whereas cold did not alter coronary vascular resistance in healthy individuals, it was significantly altered in patients with coronary heart disease.25 Coronary vasoconstriction owing to cold could alter the arterial wall shear stress and possibly induce plaque fracture but could also in theory be associated with type 2 infarction, ie, MI secondary to ischemia owing to decreased oxygen supply. Although lower temperatures were associated with higher incidence rates in both STEMI and NSTEMI, the association across various subgroups and sensitivity analyses was stronger for STEMI. Thus, our results are more in line with the first theory because type 2 infarctions generally do not present as STEMI.26 β-Blockers and aspirin, among other medications, could blunt the possible associations of external triggers through coronary vasodilation and endothelium stabilization. However, our results remained significant across a large range of subgroups with similar effect estimates.
A number of conditions associated with an increased risk of MI are more prevalent during colder weather. Respiratory tract infections and influenza are known risk factors for MI that have a clear seasonal variation that may contribute to our findings.27 A 2018 study showed a 6-fold increase of MI 7 days after a respiratory infection.28 Ongoing randomized trials are currently evaluating the role of influenza vaccinations in patients after MI and risk of reinfarction and mortality.29 Season-dependent behavioral patterns, such as reduced physical activity, dietary changes, and depression, may also contribute to the increased occurrence of MI during cold weather.30 Vitamin D has been proposed to play an important role in the seasonality of cardiovascular disease and mortality, and this could explain the associated risk of MI and sunshine duration. Previous studies have reported that blood pressure as well as cholesterol levels are minimally lower during summer, possibly contributing to the lower associated risk of MI in our study.31,32,33,34,35,36,37 However, randomized studies have failed to show any effect of vitamin D supplementation on MI risk.38,39 Seasonal analyses and analyses adjusted for time of the year are therefore plausible but should be interpreted cautiously because weather is strongly correlated with time of the year.
Our results were consistent and statistically highly significant. However, the observed effect estimates were moderate. A direct comparison with previous studies is difficult owing to inconsistency in study design and statistical method. However, similar size of effect estimates has been reported from the World Health Organization Monitoring Trends and Determinants in Cardiovascular Disease (MONICA) project study, an observational study including 21 countries, among which northern Sweden and Gothenburg were included, as well as a systematic review.18,40 In our study, no association of air temperature on risk of MI was observed in the northernmost health care region. Instead, a significant, positive association with higher snow precipitation and wind velocities was observed. Previous studies have shown higher mortality during colder winters in warm countries as compared with warmer winters, with a higher percentage increase in warm as opposed to cold countries, indicating adaptation effects.1,7,13 Although snow did not reach statistical significance in the multivariable analyses, adjusting for weather parameters can be debated because weather parameters correlate to a certain degree. Regardless, these findings, although paradoxical, are indicative of an adaptation to long winters and low temperatures in the north and are further in line with one of the main findings in our study, with static incidence rates of MI at days with subzero temperatures, declining when temperatures rose to greater than 3°C to 4°C (Figure 2). This is also supported by the lack of association during the coldest parts of the year (January-March), when higher air temperature was associated with a higher risk of NSTEMI. Although the day-to-day association of weather on incidence of MI is complex, with a number of factors possibly interacting and affecting the results, a strong association between air temperature and risk of MI is evident. Adaptation to cold may blunt this association, but whether reducing cold exposure by staying indoors and/or wearing warm clothes reduces the risk of MI remains unknown and has to be prospectively studied.
Strengths and Limitations
Weather varies significantly across Sweden, and whether the calculation of daily nationwide mean may have affected the results cannot be ruled out. Although regional analyses accounted for this to some extent, results for meteorologic variables with local effect, such as precipitation, must be interpreted cautiously. Whereas time at symptom onset can be considered fairly accurate for patients with STEMI, it may be less reliable for patients with NSTEMI, and thus a lag effect cannot be ruled out; however, lagged analyses should account for this. Although the results observed in our study were statistically highly significant, the effect estimates were modest. Our study benefits from a number of strengths, of which the most prominent are the high quality and validated diagnoses from a comprehensive nationwide registry spanning 16 years of MI data as well as the precise meteorologic data obtained from a national agency.23,41
Conclusions
In this large, nationwide study, low air temperature, low atmospheric air pressure, high wind velocity, and shorter sunshine duration were associated with risk of MI, with the most evident association observed for air temperature. This study adds to knowledge on the role of weather as a potential trigger of myocardial infarction.
eAppendix.
eTable 1. Baseline Demographics for Study Population
eTable 2. Average Weather Variable for Sweden and the 6 Healthcare Regions Stratified by Each Quarter
eTable 3. Results of Primary and Secondary Analyses Including Seasonal and Sensitivity Analyses
eTable 4. Results of Subgroup Analyses
eFigure 1. Nationwide Daily Incidence Rate of Myocardial Infarction by Air Pressure, δ Temperature, Humidity, Precipitation, Sunshine Duration, and Wind Velocity for STEMI and NSTEMI
eFigure 2. Incidence of Myocardial Infarction by Air Temperature and Region
eFigure 3. Nationwide Daily Incidence Rate of Myocardial Infarction by Temperature With Lag Effect
eFigure 4. Lag of 1, 3, 5, and 7 Days
References
- 1.Marti-Soler H, Gonseth S, Gubelmann C, et al. Seasonal variation of overall and cardiovascular mortality: a study in 19 countries from different geographic locations. PLoS One. 2014;9(11):e113500. doi: 10.1371/journal.pone.0113500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker-Blocker A. Winter weather and cardiovascular mortality in Minneapolis-St. Paul. Am J Public Health. 1982;72(3):261-265. doi: 10.2105/AJPH.72.3.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muller JE, Stone PH, Turi ZG, et al. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med. 1985;313(21):1315-1322. doi: 10.1056/NEJM198511213132103 [DOI] [PubMed] [Google Scholar]
- 4.Ornato JP, Peberdy MA, Chandra NC, Bush DE. Seasonal pattern of acute myocardial infarction in the National Registry of Myocardial Infarction. J Am Coll Cardiol. 1996;28(7):1684-1688. doi: 10.1016/S0735-1097(96)00411-1 [DOI] [PubMed] [Google Scholar]
- 5.Spencer FA, Goldberg RJ, Becker RC, Gore JM. Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. J Am Coll Cardiol. 1998;31(6):1226-1233. doi: 10.1016/S0735-1097(98)00098-9 [DOI] [PubMed] [Google Scholar]
- 6.Wolff L, White PD. Acute coronary occlusion. Boston Med Surg J. 1926;195(13). [Google Scholar]
- 7.The Eurowinter Group Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet. 1997;349(9062):1341-1346. doi: 10.1016/S0140-6736(96)12338-2 [DOI] [PubMed] [Google Scholar]
- 8.Medina-Ramón M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup Environ Med. 2007;64(12):827-833. doi: 10.1136/oem.2007.033175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Donaldson GC, Keatinge WR. Early increases in ischaemic heart disease mortality dissociated from and later changes associated with respiratory mortality after cold weather in south east England. J Epidemiol Community Health. 1997;51(6):643-648. doi: 10.1136/jech.51.6.643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerber Y, Jacobsen SJ, Killian JM, Weston SA, Roger VL. Seasonality and daily weather conditions in relation to myocardial infarction and sudden cardiac death in Olmsted County, Minnesota, 1979 to 2002. J Am Coll Cardiol. 2006;48(2):287-292. doi: 10.1016/j.jacc.2006.02.065 [DOI] [PubMed] [Google Scholar]
- 11.Wang H, Matsumura M, Kakehashi M, Eboshida A. Effects of atmospheric temperature and pressure on the occurrence of acute myocardial infarction in Hiroshima City, Japan. Hiroshima J Med Sci. 2006;55(2):45-51. [PubMed] [Google Scholar]
- 12.Madrigano J, Mittleman MA, Baccarelli A, et al. Temperature, myocardial infarction, and mortality: effect modification by individual- and area-level characteristics. Epidemiology. 2013;24(3):439-446. doi: 10.1097/EDE.0b013e3182878397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnett AG, Dobson AJ, McElduff P, Salomaa V, Kuulasmaa K, Sans S; WHO MONICA Project . Cold periods and coronary events: an analysis of populations worldwide. J Epidemiol Community Health. 2005;59(7):551-557. doi: 10.1136/jech.2004.028514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bayentin L, El Adlouni S, Ouarda TB, Gosselin P, Doyon B, Chebana F. Spatial variability of climate effects on ischemic heart disease hospitalization rates for the period 1989-2006 in Quebec, Canada. Int J Health Geogr. 2010;9:5. doi: 10.1186/1476-072X-9-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Enquselassie F, Dobson AJ, Alexander HM, Steele PL. Seasons, temperature and coronary disease. Int J Epidemiol. 1993;22(4):632-636. doi: 10.1093/ije/22.4.632 [DOI] [PubMed] [Google Scholar]
- 16.Auger N, Potter BJ, Smargiassi A, Bilodeau-Bertrand M, Paris C, Kosatsky T. Association between quantity and duration of snowfall and risk of myocardial infarction. CMAJ. 2017;189(6):E235-E242. doi: 10.1503/cmaj.161064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morabito M, Modesti PA, Cecchi L, et al. Relationships between weather and myocardial infarction: a biometeorological approach. Int J Cardiol. 2005;105(3):288-293. doi: 10.1016/j.ijcard.2004.12.047 [DOI] [PubMed] [Google Scholar]
- 18.Danet S, Richard F, Montaye M, et al. Unhealthy effects of atmospheric temperature and pressure on the occurrence of myocardial infarction and coronary deaths: a 10-year survey: the Lille-World Health Organization MONICA project (Monitoring Trends and Determinants in Cardiovascular Disease). Circulation. 1999;100(1):E1-E7. doi: 10.1161/01.CIR.100.1.e1 [DOI] [PubMed] [Google Scholar]
- 19.Sharovsky R, César LA, Ramires JA. Temperature, air pollution, and mortality from myocardial infarction in São Paulo, Brazil. Braz J Med Biol Res. 2004;37(11):1651-1657. doi: 10.1590/S0100-879X2004001100009 [DOI] [PubMed] [Google Scholar]
- 20.Claeys MJ, Coenen S, Colpaert C, et al. Environmental triggers of acute myocardial infarction: results of a nationwide multiple-factorial population study. Acta Cardiol. 2015;70(6):693-701. doi: 10.1080/AC.70.6.3120182 [DOI] [PubMed] [Google Scholar]
- 21.Wolf K, Schneider A, Breitner S, et al. ; Cooperative Health Research in the Region of Augsburg Study Group . Air temperature and the occurrence of myocardial infarction in Augsburg, Germany. Circulation. 2009;120(9):735-742. doi: 10.1161/CIRCULATIONAHA.108.815860 [DOI] [PubMed] [Google Scholar]
- 22.Bhaskaran K, Hajat S, Haines A, Herrett E, Wilkinson P, Smeeth L. Short term effects of temperature on risk of myocardial infarction in England and Wales: time series regression analysis of the Myocardial Ischaemia National Audit Project (MINAP) registry. BMJ. 2010;341:c3823. doi: 10.1136/bmj.c3823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jernberg T, Attebring MF, Hambraeus K, et al. The Swedish Web-system for enhancement and development of evidence-based care in heart disease evaluated according to recommended therapies (SWEDEHEART). Heart. 2010;96(20):1617-1621. doi: 10.1136/hrt.2010.198804 [DOI] [PubMed] [Google Scholar]
- 24.Liu S, Ducas RA, Hiebert B, Koley L, Philipp RK, Tam JW. It’s not just the snow; it’s also the cold. CMAJ. 2017;189(14):E546. doi: 10.1503/cmaj.732931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mudge GH Jr, Grossman W, Mills RM Jr, Lesch M, Braunwald E. Reflex increase in coronary vascular resistance in patients with ischemic heart disease. N Engl J Med. 1976;295(24):1333-1337. doi: 10.1056/NEJM197612092952401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baron T, Hambraeus K, Sundström J, Erlinge D, Jernberg T, Lindahl B; TOTAL-AMI study group . Type 2 myocardial infarction in clinical practice. Heart. 2015;101(2):101-106. doi: 10.1136/heartjnl-2014-306093 [DOI] [PubMed] [Google Scholar]
- 27.Barnes M, Heywood AE, Mahimbo A, Rahman B, Newall AT, Macintyre CR. Acute myocardial infarction and influenza: a meta-analysis of case-control studies. Heart. 2015;101(21):1738-1747. doi: 10.1136/heartjnl-2015-307691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378(4):345-353. doi: 10.1056/NEJMoa1702090 [DOI] [PubMed] [Google Scholar]
- 29.Fröbert O, Götberg M, Angerås O, et al. Design and rationale for the Influenza vaccination After Myocardial Infarction (IAMI) trial: a registry-based randomized clinical trial. Am Heart J. 2017;189:94-102. doi: 10.1016/j.ahj.2017.04.003 [DOI] [PubMed] [Google Scholar]
- 30.Rosengren A, Hawken S, Ounpuu S, et al. ; INTERHEART investigators . Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):953-962. doi: 10.1016/S0140-6736(04)17019-0 [DOI] [PubMed] [Google Scholar]
- 31.Kunes J, Tremblay J, Bellavance F, Hamet P. Influence of environmental temperature on the blood pressure of hypertensive patients in Montréal. Am J Hypertens. 1991;4(5 Pt 1):422-426. doi: 10.1093/ajh/4.5.422 [DOI] [PubMed] [Google Scholar]
- 32.Woodhouse PR, Khaw KT, Plummer M. Seasonal variation of blood pressure and its relationship to ambient temperature in an elderly population. J Hypertens. 1993;11(11):1267-1274. doi: 10.1097/00004872-199311000-00015 [DOI] [PubMed] [Google Scholar]
- 33.Rostand SG. Ultraviolet light may contribute to geographic and racial blood pressure differences. Hypertension. 1997;30(2, pt 1):150-156. doi: 10.1161/01.HYP.30.2.150 [DOI] [PubMed] [Google Scholar]
- 34.Ockene IS, Chiriboga DE, Stanek EJ III, et al. Seasonal variation in serum cholesterol levels: treatment implications and possible mechanisms. Arch Intern Med. 2004;164(8):863-870. doi: 10.1001/archinte.164.8.863 [DOI] [PubMed] [Google Scholar]
- 35.Råstam L, Hannan PJ, Luepker RV, Mittelmark MB, Murray DM, Slater JS. Seasonal variation in plasma cholesterol distributions: implications for screening and referral. Am J Prev Med. 1992;8(6):360-366. doi: 10.1016/S0749-3797(18)30780-3 [DOI] [PubMed] [Google Scholar]
- 36.Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med. 2008;168(11):1174-1180. doi: 10.1001/archinte.168.11.1174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dobnig H, Pilz S, Scharnagl H, et al. Independent association of low serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med. 2008;168(12):1340-1349. doi: 10.1001/archinte.168.12.1340 [DOI] [PubMed] [Google Scholar]
- 38.Beveridge LA, Struthers AD, Khan F, et al. ; D-PRESSURE Collaboration . Effect of vitamin D supplementation on blood pressure: a systematic review and meta-analysis incorporating individual patient data. JAMA Intern Med. 2015;175(5):745-754. doi: 10.1001/jamainternmed.2015.0237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scragg R, Stewart AW, Waayer D, et al. Effect of monthly high-dose vitamin D supplementation on cardiovascular disease in the vitamin D assessment study : a randomized clinical trial. JAMA Cardiol. 2017;2(6):608-616. doi: 10.1001/jamacardio.2017.0175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bhaskaran K, Hajat S, Haines A, Herrett E, Wilkinson P, Smeeth L. Effects of ambient temperature on the incidence of myocardial infarction. Heart. 2009;95(21):1760-1769. doi: 10.1136/hrt.2009.175000 [DOI] [PubMed] [Google Scholar]
- 41.Lagerqvist B, Fröbert O, Olivecrona GK, et al. Outcomes 1 year after thrombus aspiration for myocardial infarction. N Engl J Med. 2014;371(12):1111-1120. doi: 10.1056/NEJMoa1405707 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix.
eTable 1. Baseline Demographics for Study Population
eTable 2. Average Weather Variable for Sweden and the 6 Healthcare Regions Stratified by Each Quarter
eTable 3. Results of Primary and Secondary Analyses Including Seasonal and Sensitivity Analyses
eTable 4. Results of Subgroup Analyses
eFigure 1. Nationwide Daily Incidence Rate of Myocardial Infarction by Air Pressure, δ Temperature, Humidity, Precipitation, Sunshine Duration, and Wind Velocity for STEMI and NSTEMI
eFigure 2. Incidence of Myocardial Infarction by Air Temperature and Region
eFigure 3. Nationwide Daily Incidence Rate of Myocardial Infarction by Temperature With Lag Effect
eFigure 4. Lag of 1, 3, 5, and 7 Days