Abstract
Importance
Vision loss is the third most common impairment worldwide. Although cost-effective interventions are available for preventing or curing most causes of vision loss, availability of these interventions varies considerably between countries and districts. Knowledge of the association between vision loss and socioeconomic factors is informative for public health planning.
Objectives
To explore correlations of the prevalence of visual impairment with socioeconomic factors at country levels and to model and estimate a socioeconomic-adjusted disease burden based on these data.
Design, Setting, and Participants
In this cross-sectional study, the following data were collected from 190 countries and territories: the age-standardized prevalence of moderate to severe visual impairment (MSVI) and blindness from January 1 to December 31, 2010, across countries, human development index (HDI), gross domestic product (GDP) per capita, total health expenditure, total health expenditure as percentage of GDP (total health expenditure/GDP), public health expenditure as percentage of total health expenditure (public/total health expenditure), and out-of-pocket expenditure as percentage of total health expenditure (out-of-pocket/total health expenditure). Countries were divided into 4 levels (low, medium, high, and very high) by HDI. Data analysis was conducted from September 1, 2016, to July 1, 2017.
Main Outcomes and Measures
The correlations between prevalence data and socioeconomic indices were assessed.
Results
A strong negative association between prevalence rates of MSVI and blindness and socioeconomic level of development was observed. The mean (SD) age-standardized prevalence of MSVI decreased from 4.38% (1.32%) in low-HDI regions to 1.51% (1.00%) in very-high-HDI regions (P < .001). The national HDI level was attributable to 56.3% of global variation in prevalence rates of MSVI and 67.1% of global variation in prevalence rates of blindness. Higher prevalence rates were also associated with lower total health expenditure per capita, total health expenditure/GDP (β = −0.236 [95% CI, −0.315 to −0.157] for prevalence of MSVI; β = −0.071 [95% CI, −0.100 to −0.042] for prevalence of blindness), public/total health expenditure (β = −0.041 [95% CI, −0.052 to −0.031] for prevalence of MSVI; β = −0.014 [95% CI, −0.018 to −0.010] for prevalence of blindness), and higher percentage of out-of-pocket/total health expenditure (β = 0.044 [95% CI, 0.032-0.055] for prevalence of MSVI; β = 0.013 [95% CI, 0.009-0.017] for prevalence of blindness). Countries with increased burden of visual impairment and blindness can be easily identified by the results of the linear models. Socioeconomic factors could explain 69.4% of the global variations in prevalence of MSVI and 76.3% of the global variations in prevalence of blindness.
Conclusions and Relevance
Burden of visual impairment and socioeconomic indicators were closely associated and may help to identify countries requiring greater attention to these issues. The regression modeling described may provide an opportunity to estimate appropriate public health targets that are consistent with a country’s level of socioeconomic development.
This cross-sectional study explores correlations of the prevalence of visual impairment with socioeconomic factors at country levels and models and estimates a socioeconomic-adjusted disease burden based on these data.
Key Points
Question
What is the association between the burden of visual impairment and national level of socioeconomic development?
Findings
In this cross-sectional study, socioeconomic factors explained 69.4% of global variations in moderate to severe visual impairment and 76.3% of global variations in prevalence of blindness.
Meaning
The close association of burden of visual impairment and socioeconomic indicators may help to identify countries requiring greater attention; regression modeling also provides an opportunity to estimate appropriate public health targets that are consistent with a country’s level of socioeconomic development.
Introduction
Vision loss ranks as the third most common impairment worldwide.1 In 2010, the Global Burden of Diseases (GBD), Injuries and Risk Factors Study estimated that 223.4 million people globally had visual impairment (VI): 191 million with moderate to severe VI (MSVI) and 32.4 million with blindness.2 With a marked increase in life expectancy and population growth worldwide, the incidence of vision loss is projected to rise. The World Health Organization estimates that approximately 90% of individuals with VI reside in low-income settings,3 posing considerable concerns for social and economic development in these areas.
Previous analyses have demonstrated that avoidable blindness is closely linked with socioeconomic realities and has been described as both the cause and consequence of poverty.4 However, the way in which the levels of socioeconomic development are associated with the scale of vision loss for a particular country remains unclear. Gross domestic product (GDP) per capita is a commonly used macroeconomic indicator, which is sometimes criticized for its sole focus on economy in monetary terms.5,6 The human development index (HDI) is a combination of social and economic factors.7,8 Although GDP and the HDI are widely used worldwide, to our knowledge, no previous study has examined these indicators together with prevalence of VI.
In 2013, the World Health Assembly endorsed the Global Action Plan (Universal Eye Health: A global action plan 2014-2019) that set a target to reduce the global prevalence of avoidable vision loss by 25% before the year 2020.9,10 However, it is important that countries of different economic levels of development set national targets, taking into account varying disease burdens, diagnostic capacity, and access to cost-effective interventions.11,12,13,14 A clearer understanding of the association between the magnitude of VI and socioeconomic factors at a national level may provide an insight into approaches to prioritize resource allocation in public health planning. The potential correlation is useful for the health planner. The socioeconomic-adjusted prevalence of VI in a country may serve as a surrogate target for prevalence of VI to remain consistent with other, comparable countries’ proportional economic spending.
To fill the knowledge gap, this study explored the association between national levels of socioeconomic development and health expenditures with the scale of VI and blindness by linking socioeconomic indicators to the age-standardized prevalence rates of blindness and MSVI. The objectives of this study were to identify countries with higher levels of socioeconomic development without proportional lower levels of VI and to estimate the socioeconomic-adjusted prevalence of VI in a country through linear regression models.
Method
Data Sources
The GBD study provided a resource for gaining insight into factors influencing the efficacy of blindness and MSVI control in 190 counties or territories in 21 GBD regions. To examine the effects of socioeconomic factors on burden of blindness and MSVI, we linked established socioeconomic indices and health expenditure indicators to the GBD estimates of age-standardized prevalence of blindness and MSVI from January 1 to December 31, 2010. Age-standardized prevalence rates of blindness and MSVI were extracted from publications.2,10 Corresponding HDI levels, reflecting levels of socioeconomic development at a national level, were obtained from the United Nations Development Programme Human Development Reports (http://hdr.undp.org/en/data). Data on national GDP per capita in 2010 were retrieved from the World Bank (http://data.worldbank.org/). Health expenditure indicators were obtained from the World Health Organization Global Health Expenditure Database (http://apps.who.int/nha/database/). The latest health burden of eye disease (disability-adjusted life-year [DALY]) in each country was obtained from the Global Health Estimates 2015.15 The corresponding population of each country in 2015 was obtained from the World Population Prospects.16 The DALY rate was calculated by dividing DALY by population size. Institutional review board approval was not needed for this study because all data were extracted from open databases and published data; no individual patient data were collected.
Variables
The HDI is a well-recognized indicator that incorporates economic measures of development together with social measures.7 As of 2010, the United Nations Development Programme has defined the components of HDI across the following 3 domains: health index, education index, and income index. The HDI, which ranges between 0 and 1, is calculated based on the following 4 indicators: life expectancy at birth, mean years of schooling, expected years of schooling, and gross national income per capita. To characterize the disease burden according to social development and resource utility, we further separated the United Nations Development Programme predefined cutoffs into 4 categories, which were defined as low (0.326-0.529), medium (0.544-0.681), high (0.696-0.786), and very high (0.792-0.940).7
Gross domestic product per capita is the most commonly used indicator for economic development. Total health expenditure per capita is defined as the sum of general government public and private health expenditures as a ratio of total population in a given year, which reflects a national true investment in health regardless of its GDP per capita.11 To avoid the potential confounder of currency exchange rates between countries and to negate the effects of inflation, a database on purchasing power parity was converted to international dollars in 2011. Total health expenditure as a percentage of GDP (total health expenditure/GDP) is defined as the ratio of total health expenditure to total GDP in a given year. Public sector as a share of total health expenditure (public/total health expenditure) is defined as the ratio of spending to total health expenditure from government budgets, foreign loans and grants, and social health insurance funds. Out-of-pocket health expenditure as a share of total health expenditure (OOP/total health expenditure) is defined as the ratio of direct outlay by households to total health expenditure, and forms part of private health expenditure.11
Statistical Analysis
Statistical analysis was conducted from September 1, 2016, to July 1, 2017. To explore the associations between indicators, scatterplots were constructed using GraphPad Prism, version 5.0, software (GraphPad Software Inc). One-way analysis of variance was used to compare prevalence rates between groups with different levels of human development. A univariate linear model was used to examine the cross-sectional associations between age-standardized prevalence rates of blindness and MSVI with HDI and its components, logarithmic values of GDP per capita and total health expenditure per capita, total health expenditure/GDP, public/total health expenditure, and OOP/total health expenditure. Linear regression estimation and its 95% CIs were used to project socioeconomically adjusted prevalence rate ranges for blindness and MSVI. Overburdening of VI in countries was defined as a positive difference between actual rates and the projected socioeconomically adjusted rates. Stepwise multivariate regression models were constructed to explore the spread of how these factors affect the variations in prevalence rates between countries. R2 statistics were used to determine how well the model fits the data statistically. Sensitivity analyses were performed by assessing the association between HDI or per capita GDP and the DALY rate. All statistical analyses were conducted by STATA, version 12.0 SE (Stata Corp LP). P < .05 was considered statistically significant.
Results
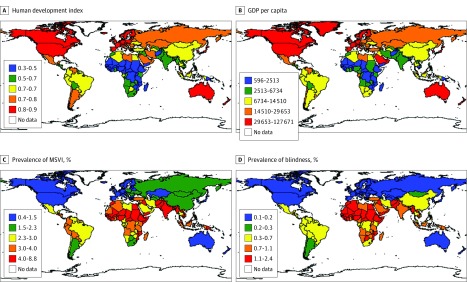
The distribution of prevalence scales and corresponding socioeconomic status were mapped in Figure 1. A strong correlation between HDI or GDP per capita levels and prevalence rates was observed, with the prevalence of MSVI and blindness highest in countries with very high HDI or GDP per capita levels. Examination of trends of age-standardized prevalence rates of MSVI and blindness across HDI levels revealed strongly negative dose-response associations (eFigure 1 in the Supplement). The age-standardized mean (SD) prevalence of MSVI declined with increasing HDI (low HDI, 4.38% [1.32%]; medium HDI, 3.70% [1.55%]; high HDI, 2.46% [0.68%]; and very high HDI, 1.51% [1.00%]; P < .001). Similarly, the mean (SD) prevalence of blindness declined with increasing HDI, from 1.41% [0.49%] in low HDI regions, 0.78% [0.41%] in medium HDI regions, 0.40% [0.22%] in high HDI regions, and 0.25% [0.34%] in very high HDI regions (P < .001).
Figure 1. Distribution of Prevalence Scales and Corresponding Socioeconomic Status.
A, The 5 levels of the human development index estimated by the United Nations Development Programme. B, Gross domestic product (GDP) per capita. C, Age-standardized prevalence of moderate to severe visual impairment (MSVI) for all ages in 2010. D, Age-standardized prevalence of blindness for all ages in 2010.
Table 1 summarizes the univariate linear regression analyses. Both MSVI and blindness prevalence were negatively correlated with all socioeconomic indicators (P < .001). The linear models were as follows: (y = –7.595 × HDI + 8.015; R2 = 0.563; P < .001), (y = –2.976 × HDI + 2.683; R2 = 0.671; P < .001), (y = –0.855 × ln (GDP per capita) + 10.609; R2 = 0.475; P < .001), and (y = –0.314 × ln (GDP per capita) + 3.509; R2 = 0.466; P < .001). The national HDI level was accountable for 56.3% of global variations in the prevalence of MSVI and 67.1% of global variations in the prevalence of blindness. On further examination of the 3 components of HDI, education index was identified as the most influential factor, accounting for 63.8% of variations in the prevalence of MSVI and 76.4% variations in the prevalence blindness.
Table 1. Univariate Regression Analysis of Age-Standardized Prevalence of MSVI and Blindness With National Levels of Socioeconomic Development.
| Socioeconomic Indicator | Prevalence of MSVI (×100) | Prevalence of Blindness (×100) | ||||
|---|---|---|---|---|---|---|
| β (95% CI) | P Value | R2 | β (95% CI) | P Value | R2 | |
| HDI | −7.595 (−8.578 to −6.613) | <.001 | 0.563 | −2.976 (−3.281 to −2.670) | <.001 | 0.671 |
| Health index | −6.99 (−8.361 to −5.619) | <.001 | 0.356 | −3.006 (−3.440 to −2.573) | <.001 | 0.506 |
| Education index | −7.307 (−8.114 to −6.499) | <.001 | 0.638 | −2.868 (−3.102 to −2.634) | <.001 | 0.764 |
| Income index | −5.861 (−6.805 to −4.917) | <.001 | 0.452 | −2.126 (−2.462 to −1.790) | <.001 | 0.461 |
| ln (GDP per capita)a | −0.855 (−0.986 to −0.723) | <.001 | 0.475 | −0.314 (−0.363 to −0.265) | <.001 | 0.466 |
| ln (THE per capita)a | −0.899 (−1.015 to −0.783) | <.001 | 0.563 | −0.312 (−0.355 to −0.269) | <.001 | 0.528 |
| THE/GDP | −0.236 (−0.315 to −0.157) | <.001 | 0.161 | −0.071 (−0.100 to −0.042) | <.001 | 0.115 |
| Public/THE | −0.041 (−0.052 to −0.031) | <.001 | 0.244 | −0.014 (−0.018 to −0.010) | <.001 | 0.225 |
| OOP/THE | 0.044 (0.032 to 0.055) | <.001 | 0.234 | 0.013 (0.009 to 0.017) | <.001 | 0.166 |
Abbreviations: GDP, gross domestic product; HDI, human development index; MSVI, moderate to severe visual impairment; OOP/THE, out-of-pocket health expenditure as a percentage of THE; Public/THE, public sector as a percentage of THE; THE, total health expenditure; THE/GDP, THE as a percentage of GDP.
Purchasing power parity method (constant 2011 international $).
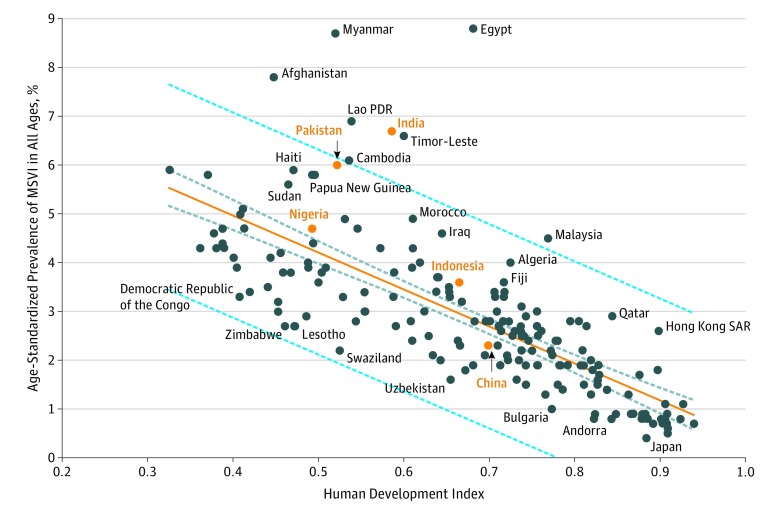
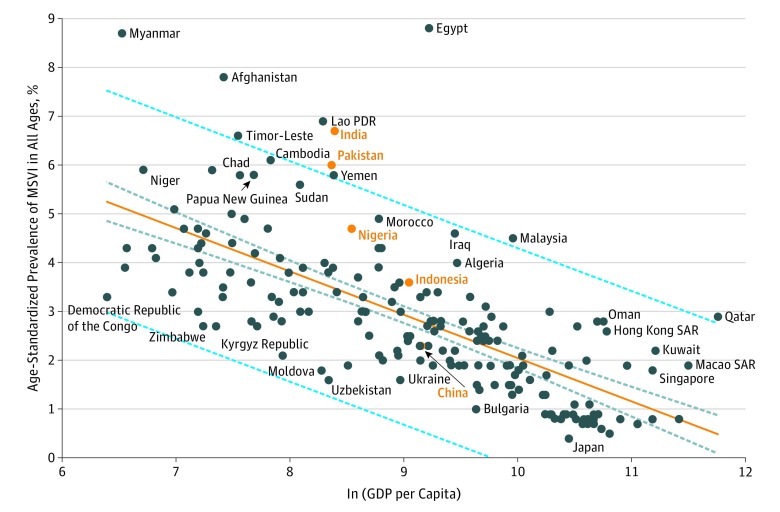
Figure 2 illustrates the modeling associations of HDI vs the prevalence of MSVI. The prevalence of MSVI with respect to HDI levels in some countries (eg, Indonesia and China) was similar to the level projected by the linear regression, indicating that the MSVI remained consistent with an economy-adjusted projection. However, a much greater disparity in the prevalence of MSVI with respect to HDI levels compared with the projected value was noted for other countries, including Myanmar, Egypt, Pakistan, India, Timor-Leste, Cambodia, Malaysia, and Afghanistan. Similar trends were observed when logarithm values of GDP per capita were used as estimators of MSVI prevalence (Figure 3). Consistent phenomenon was observed for blindness prevalence.
Figure 2. Scatterplots of the Prevalence of Moderate to Severe Visual Impairment (MSVI) vs National Level of Human Development Index in 2010.
The 5 countries with the largest number of blind people (a total of more than one-half of the world’s blind people) are displayed in orange lettering. PDR indicates People’s Democratic Republic; and SAR, Special Administrative Region. Orange line indicates linear regression model; dark-blue dashed line, 95% CI; and light-blue dashed line, 95% prediction interval.
Figure 3. Scatterplots of the Prevalence of Moderate to Severe Visual Impairment (MSVI) vs Gross Domestic Product (GDP) per Capita in 2010.
The 5 countries with the largest number of blind people (a total of more than one-half of the world’s blind people) are displayed in orange lettering. The GDP per capita is in purchasing power parity constant $. PDR indicates People’s Democratic Republic; and SAR, Special Administrative Region. Orange line indicates linear regression model; dark-blue dashed line, 95% CI; and light-blue dashed line, 95% prediction interval.
With regards to health expenditure metrics, higher prevalence rates were associated with lower total health expenditure per capita, total health expenditure/GDP, public/total health expenditure, and higher percentage of OOP/total health expenditure (Table 1; eFigure 2 in the Supplement). Total health expenditure as percentage of GDP was also closely associated with GDP per capita (β = 0.875; R2 = 0.900; P < .001). To eliminate colinearity, stepwise multivariate regression analyses were performed (Table 2). When the composite HDI was used, HDI, total health expenditure/GDP, and OOP/total health expenditure were included in the model, which explained 63.6% of global variations in prevalence of MSVI. In addition, 72.9% of global variations in prevalence of blindness were attributable to HDI, total health expenditure per capita, and total health expenditure/GDP. When the 3 components of HDI were used, 4 indicators (health index, education index, total health expenditure per capita, and OOP/total health expenditure) accounted for 69.4% of variations in the prevalence of MSVI. Finally, education index alone was attributed to 76.3% of global variation in the prevalence of blindness.
Table 2. Stepwise Multivariate Regression Analysis of Age-Standardized Prevalence of MSVI and Blindness With Socioeconomic Indicators.
| Socioeconomic Indicator | Prevalence of MSVI (×100) | Prevalence of Blindness (×100) | ||||
|---|---|---|---|---|---|---|
| β (95% CI) | P Value | R2 | β (95% CI) | P Value | R2 | |
| Model 1a | ||||||
| HDI | −6.385 (−7.368 to −5.402) | <.001 | .636 | −5.396 (−6.310 to −4.482) | <.001 | .729 |
| ln (THE per capita)b | NA | NA | 0.340 (0.225 to 0.456) | <.001 | ||
| THE/GDP | −0.106 (−0.163 to −0.049) | <.001 | −0.055 (−0.076 to −0.034) | <.001 | ||
| OOP/THE | 0.014 (0.005 to 0.022) | .003 | NA | NA | ||
| Model 2c | ||||||
| Health index | 2.198 (0.493 to 3.902) | .01 | .694 | NA | NA | .763 |
| Education index | −5.919 (−7.407 to −4.431) | <.001 | −2.850 (−3.086 to −2.614) | <.001 | ||
| ln (THE per capita)b | −0.332 (−0.542 to −0.121) | .002 | NA | NA | ||
| OOP/THE | 0.011 (0.003 to 0.019) | .009 | NA | NA | ||
Abbreviations: HDI, human development index; MSVI, moderate to severe visual impairment; NA, not applicable; OOP/THE, out-of-pocket health expenditure as a percentage of THE; THE, total health expenditure; THE/GDP, THE as a percentage of gross domestic product.
Model 1 included HDI and excluded its components in the analysis.
Purchasing power parity method (constant 2011 international $).
Model 2 included the 3 components of HDI in the analysis while it excluded the HDI.
The sensitivity analyses obtained consistent conclusions (eFigures 3 and 4 in the Supplement). The results showed that DALY rates were correlated with HDI and logarithmic values of per capita GDP, although countries such as India and Pakistan remained outliers.
Discussion
This study demonstrated a strong association between global variations in vision loss and socioeconomic factors at a national level, and provided a model for socioeconomically adjusted levels of blindness and MSVI for countries. A strong dose-response association was observed between a higher HDI and a lower prevalence of blindness and MSVI. Furthermore, associations between the burden of vision loss and national health expenditure metrics were identified, highlighting the importance of optimal strategies to prevent and manage vision-threatening diseases at a population level.
The national levels of HDI account for more than 70% of the variation in prevalence of blindness and MSVI worldwide. This observation is in line with those in previous analyses based on income group (low-, moderate-, and high-income countries), which reported that a higher burden of VI was found in low-income countries.2,3 Reciprocal effects may help to explain these associations. In 2010, it was estimated that global blindness resulted in $27 billion loss of GDP, while the total cost of VI reached $3 trillion.12,13 Eye care services were the most unaffordable and inaccessible in low-income countries, where there are more people with uncorrected refractive errors and inadequate access to cataract surgical services. Efforts to reduce the prevalence of VI have been shown to increase productivity and income and provide other economic benefits.17 Despite this finding, the burden of VI is highest in low-income countries owing to a reduction of both absolute (total health expenditure per capita) and relative (total health expenditure/GDP) resource allocation.
Although one would expect an inverse association between socioeconomic development and vision loss, our analyses may provide additional information for health planners. For example, they may help to quickly identify outlier countries. Some countries, such as India and Pakistan, did not fit the regression line. Possible causes for the disproportionally higher prevalence of VI in these countries may include the inadequate execution of eye care plans at national levels, limited resources allocated to eye health owing to competing health demands, a substantial backlog of individuals with VI considering the big population base, economic effect and cost, and lack of human resources for eye care.
Across the 3 domains of HDI, educational index contributed the most influence on the prevalence of MSVI and blindness. This finding is consistent with data from the United Kingdom that suggest the odds of MSVI and blindness were nearly 2 times higher in people with no educational qualifications than those with university level or other professional qualification.18 Likewise, a randomized clinical trial in rural China showed that educational interventions successfully promoted the acceptance of cataract surgery and increased willingness to pay for surgery.19 Among children, educational programs can effectively increase the diagnostic accuracy of retinopathy of prematurity.20 In the elderly Korean population, lifetime use of eye care was influenced by educational level.21 A study in India also demonstrated that educational intervention may increase the use of eye care by targeting the rural population.22 Such findings highlight the importance and challenge of translating wealth to social welfare in some countries. Therefore, educational interventions and additional counseling services are warranted for populations with a low educational level.
Projecting the prevalence of MSVI and blindness for a given HDI or GDP per capita value is an important component of health policy, enabling estimations for health budgeting and insurance planning. The results of our study demonstrate that both prevalence of MSVI and blindness were closely associated with HDI and logarithmic GDP per capita in a linear fashion. Despite this finding, discrepancies were identified for some countries (eg, Myanmar, Egypt, and Pakistan) with a disproportionally higher prevalence of MSVI and blindness. One of the major intents of this study was to identify the countries with a prevalence of VI that was greater than their economy-adjusted targets using the rest of the world as a benchmark standard, and perhaps provide a starting point to evaluate the reasons for relatively higher rates of prevalence of VI, and to target ophthalmic policies and priorities that may require further attention and planning.
The regression model developed from this study may be a useful tool for estimating the levels of vision loss for each country, using other countries’ socioeconomic data as comparison standards. For instance, the actual prevalence of MSVI in several countries including Egypt, Pakistan, India, Cambodia, and Timor-Leste were much higher than the projected rates. This finding indicates that greater investment and resource allocation may be required for health policy planners and leaders to address the relatively higher prevalence of vision loss. It is arguable from a socioeconomic perspective that these countries may be able to achieve lower rates of VI with respect to their socioeconomic development levels. Blindness prevention models in countries with levels of VI consistent with their socioeconomic projections may be considered as templates for countries with higher levels of VI. For a country with limited resources and prevalence data, the socioeconomic-adjusted targets from this model may help health policy planning to initially estimate spending requirements, before more accurate and comprehensive evaluation processes are in place. However, these values are socioeconomic-projected suggestions only, and they should be interpreted within each country’s context factoring in demand for surgery and cultural expectations.
Health expenditure metrics were consistently correlated with the prevalence of MSVI and blindness in our study. Wealthier countries tend to proportionally allocate more resources to health care, although the distribution of these resources may not necessarily be needs based or equal throughout the region.23 It is recommended that government expenditure for health care should account for at least of 5% of GDP in any given country; however, only 3% of low-income countries and 37% of middle-income countries achieve this target.11,24 Low-income countries may allocate a disproportionally small fraction of their government expenditure to health care resources, exacerbating the burden of MSVI and blindness. The observed association between OOP/total health expenditure and the rate of MSVI and blindness is noteworthy, as it may reflect patients’ inability or reluctance to pay for services in some countries with a high proportion of OOP health service expenses.
This study provides novel data linking the most widely recognized socioeconomic indicators to rates of blindness worldwide. Although the mechanisms of how socioeconomic development affects the scale of vision loss are ubiquitous (ie, affordability and accessibility to services and density of ophthalmologist practices), this information is useful to the health planner as a supplementary guide of adjusted VI prevalence targets, particularly for developing countries with limited study resources and prevalence data. For example, many countries and territories, such as Monaco, Nauru, Niue, Palau, and Tuvalu, did not have epidemiologic data on eye disease. However, socioeconomic or wealth data are often available. Thus, one can use the socioeconomic data to estimate the prevalence of VI by using our models.
Limitations
The limitations of this study should not be ignored. First, the prevalence of blindness and MSVI from the GBD were calculated based on a hierarchical model, whereby accuracy depends on the accessibility and quality of information resources at a given time. Remodeling associations of socioeconomic factors with up-to-date population-based prevalence data will yield more accurate findings in the future. Second, expressing blindness and MSVI using socioeconomic indicators may oversimplify the interactions between the causes of blindness worldwide. We were most interested in the outcomes of total blindness and MSVI, but further studies are warranted to clarify the associations of socioeconomic indicators with blindness of varying severities and causes. Third, the national levels of socioeconomic indicator data may not be representative for particular populations within a country, as socioeconomic development may vary greatly across regions. In addition, larger countries may face additional challenges with respect to access to and delivery of health care. To demonstrate efficiency of resource expenditures, future studies will need to examine expenditures relative to eye health services per country. Fourth, this is an ecological analysis with inherent limitations for drawing inferences regarding cause and effect. Despite this, our data produce a setpoint for discussion at a population level that is otherwise not feasible with other designs such as randomized clinical trials.25 Fifth, our models were based on cross-sectional data. It was more informative to use longitudinal data for each country by using a mixed-effects model. Finally, developing models backward may overestimate the reliability of data used for the study. Thus, suggestion of investments from countries with limited budgets based on our models was not strong enough.
Conclusions
The prevalence of MSVI and blindness appears to be closely associated with national socioeconomic indicator data. Socioeconomic factors should be taken into account when implementing strategies aimed at improving blindness prevention worldwide. The projected targets for VI may help to identify countries with greater needs, where the prioritization and implementation of resource-appropriate strategies is particularly important, taking into account the socioeconomic development data from other countries worldwide as reference.
eFigure 1. National Age-Standardized Prevalence of Moderate to Severe Visual Impairment (MSVI) and Blindness in 2010 According to Different Human Development Levels
eFigure 2. Scatter Plots of the Country-Level Indices of Absolute and Relative Health Expenditure vs Age-Standardized Prevalence of Moderate to Severe Visual Impairment (MSVI)
eFigure 3. Scatter Plots of the Disability-Adjusted Life-Years (DALY) Rate Caused by Vision Loss vs National Level of Human Development Index in 2015
eFigure 4. Scatter Plots of the Prevalence of Disability-Adjusted Life-Years (DALY) Rate Caused by Vision Loss vs Gross Domestic Product (GDP) Per Capita in 2015
References
- 1.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stevens GA, White RA, Flaxman SR, et al. ; Vision Loss Expert Group . Global prevalence of vision impairment and blindness: magnitude and temporal trends, 1990-2010. Ophthalmology. 2013;120(12):2377-2384. [DOI] [PubMed] [Google Scholar]
- 3.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614-618. [DOI] [PubMed] [Google Scholar]
- 4.Gilbert CE, Shah SP, Jadoon MZ, et al. ; Pakistan National Eye Survey Study Group . Poverty and blindness in Pakistan: results from the Pakistan national blindness and visual impairment survey. BMJ. 2008;336(7634):29-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verguet S, Alkire BC, Bickler SW, et al. Timing and cost of scaling up surgical services in low-income and middle-income countries from 2012 to 2030: a modelling study. Lancet Glob Health. 2015;3(suppl 2):S28-S37. [DOI] [PubMed] [Google Scholar]
- 6.Alkire BC, Shrime MG, Dare AJ, Vincent JR, Meara JG. Global economic consequences of selected surgical diseases: a modelling study. Lancet Glob Health. 2015;3(suppl 2):S21-S27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Nations Development Programme Human development data (1990-2015). http://hdr.undp.org/en/data. Accessed January 1, 2017.
- 8.Giebel S, Labopin M, Ehninger G, et al. ; Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation . Association of Human Development Index with rates and outcomes of hematopoietic stem cell transplantation for patients with acute leukemia. Blood. 2010;116(1):122-128. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization Universal eye health: a global action plan 2014-2019. http://www.who.int/blindness/actionplan/en/. Accessed August 1, 2016.
- 10.Bourne RR, Stevens GA, White RA, et al. ; Vision Loss Expert Group . Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Health. 2013;1(6):e339-e349. [DOI] [PubMed] [Google Scholar]
- 11.Dieleman JL, Templin T, Sadat N, et al. National spending on health by source for 184 countries between 2013 and 2040. Lancet. 2016;387(10037):2521-2535. [DOI] [PubMed] [Google Scholar]
- 12.Gordois A, Cutler H, Pezzullo L, et al. An estimation of the worldwide economic and health burden of visual impairment. Glob Public Health. 2012;7(5):465-481. [DOI] [PubMed] [Google Scholar]
- 13.Frick KD, Foster A. The magnitude and cost of global blindness: an increasing problem that can be alleviated. Am J Ophthalmol. 2003;135(4):471-476. [DOI] [PubMed] [Google Scholar]
- 14.Shrime MG, Dare AJ, Alkire BC, O’Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health. 2015;3(suppl 2):S38-S44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Global health estimates (GHE). http://www.who.int/healthinfo/global_burden_disease/en/. Accessed August 30, 2017.
- 16.United Nations. World population prospects 2017. https://esa.un.org/unpd/wpp/. Accessed August 30, 2017.
- 17.Baltussen R, Smith A. Cost effectiveness of strategies to combat vision and hearing loss in sub-Saharan Africa and South East Asia: mathematical modelling study. BMJ. 2012;344:e615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cumberland PM, Rahi JS; UK Biobank Eye and Vision Consortium . Visual function, social position, and health and life chances: the UK Biobank Study. JAMA Ophthalmol. 2016;134(9):959-966. [DOI] [PubMed] [Google Scholar]
- 19.Liu T, Congdon N, Yan X, et al. A randomized, controlled trial of an intervention promoting cataract surgery acceptance in rural China: the Guangzhou Uptake of Surgery Trial (GUSTO). Invest Ophthalmol Vis Sci. 2012;53(9):5271-5278. [DOI] [PubMed] [Google Scholar]
- 20.Patel SN, Martinez-Castellanos MA, Berrones-Medina D, et al. ; GEN-ROP; i-ROP Research Consortium . Assessment of a tele-education system to enhance retinopathy of prematurity training by international ophthalmologists-in-training in Mexico. Ophthalmology. 2017;124(7):953-961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park YS, Heo H, Ye BJ, et al. ; Epidemiologic Survey Committee of the Korean Ophthalmological Society . Prevalence and factors associated with the use of eye care services in South Korea: Korea National Health and Nutrition Examination Survey 2010-2012. Korean J Ophthalmol. 2017;31(1):58-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Su Z, Wang BQ, Staple-Clark JB, Buys YM, Forster SH. Willingness to use follow-up eye care services after vision screening in rural areas surrounding Chennai, India. Br J Ophthalmol. 2014;98(8):1009-1012. [DOI] [PubMed] [Google Scholar]
- 23.Ono K, Hiratsuka Y, Murakami A. Global inequality in eye health: country-level analysis from the Global Burden of Disease Study. Am J Public Health. 2010;100(9):1784-1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu C, Schneider MT, Gubbins P, Leach-Kemon K, Jamison D, Murray CJ. Public financing of health in developing countries: a cross-national systematic analysis. Lancet. 2010;375(9723):1375-1387. [DOI] [PubMed] [Google Scholar]
- 25.Roy A, Roe MT, Neely ML, et al. Impact of human development index on the profile and outcomes of patients with acute coronary syndrome. Heart. 2015;101(4):279-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. National Age-Standardized Prevalence of Moderate to Severe Visual Impairment (MSVI) and Blindness in 2010 According to Different Human Development Levels
eFigure 2. Scatter Plots of the Country-Level Indices of Absolute and Relative Health Expenditure vs Age-Standardized Prevalence of Moderate to Severe Visual Impairment (MSVI)
eFigure 3. Scatter Plots of the Disability-Adjusted Life-Years (DALY) Rate Caused by Vision Loss vs National Level of Human Development Index in 2015
eFigure 4. Scatter Plots of the Prevalence of Disability-Adjusted Life-Years (DALY) Rate Caused by Vision Loss vs Gross Domestic Product (GDP) Per Capita in 2015